Abstract
Background: Medical care is impacted by uncertainty caused by various factors. The uncertainty that exists in medical care can cause patient distrust and lead to conflict. This study compared the tolerance of uncertainty in medical care between non-medical professionals and nurses.
Methods: We conducted a cross-sectional Internet-based survey. Participants included 2,100 individuals (600 nurses and 1,500 non-medical professionals; aged ≥ 20 years) from different parts of Japan. Of these, we excluded 70 participants who were classified as non-medical professionals but were registered nurses. Finally, we analyzed data from 2,030 participants (600 nurses and 1,430 non-medical professionals). Three registered nurses and nursing researchers developed an original questionnaire on tolerance of uncertainty in medical care. Data regarding participants’ characteristics (age, sex, education level, marital status, having children, population size of the residential area, medical care usage, and occupation) were obtained. We performed a one-way analysis of variance (ANOVA) to compare the data between non-medical professionals and nurses. Additionally, we employed a multiple regression model to investigate factors related to tolerance of uncertainty in medical care scores.
Results: A significant portion of participants (36.7%) were aged 40-50 years (n = 745). Most were women (n = 1,210, 59.6%), and a considerable percentage were medical care users (n = 1,309, 64.5%). Non-medical professionals were less tolerant of uncertainty than nurses, and uncertainty scores were associated with medical care usage, occupation, and population size of the residential area.
Conclusions: Our findings revealed variations in perceptions of uncertainty in medical care between non-medical professionals and medical care providers. To mitigate conflicts related to medical issues, medical care providers should enhance non-medical professionals' education regarding perceptions of uncertainty in medical care.
Keywords: citizen, nurse, medical care, tolerance, uncertainty
Introduction
Medical accident victims often experience feelings of frustration and anger after such accidents, while medical staff, as secondary victims, may experience fear concerning malpractice, contributing to burnout [1, 2]. Conflicts arising from medical accidents between patients and staff cause frustration for both parties. Medical personnel provide medical care and support to patients, aiming to prevent casualties and medical accidents. However, human factors, including memory lapses and slips, can contribute to errors in practice.
Medical care is impacted by uncertainty caused by various factors. Han et al. clarified that scientific uncertainty encompasses uncertainties about diagnosis, prognosis, causal explanations, and treatment recommendations [3, 4]. Practical uncertainty applies to the structures and processes of care, the competence of one’s physicians, and the rules and procedures of institutions [3, 4]. Mackintosh et al. reported that conceptual uncertainty in healthcare is related to moral and normative dimensions, such as patients’ experiences of diseases or their culture and social practices [5]. Particularly, five factors leading to uncertainty have been identified: patients’ biological variability (e.g., constitutional predisposition), patient and physician bias, error in test interpretation, differing values and opinions of patients and physicians, and uncertainty surrounding decision-making [6]. Divergent perspectives on treatment goals contribute to disagreements between physicians and patients. Patients tend to think that their condition is getting better, which may be because the patient’s wishes are reflected or the patient may not have enough information to set the correct goal. Effective communication of evolving treatment goals by physicians is essential, as changes occur during treatment [7, 8]. Patients often express dissatisfaction with the perceived lack of empathy and insufficient information provided by medical staff, resulting in complaints. Concrete instances include concerns regarding medicines, examinations, and treatment [9].
The World Health Organization (WHO) emphasizes that engaging patients and families in healthcare is critical [10]. However, it is not confirmed whether a gap exists in perceptions and awareness regarding medical care between medical professionals and the public that could lead to complaints and medical litigation. Nurses have the role of advocating for people’s rights, supporting people in making decisions and choices, and spending most of their time interacting with patients. Therefore, the purpose of this study is to compare the tolerance of uncertainty in healthcare between non-medical professionals and nurses. The definition of non-medical professionals in this study excluded people with medical qualifications, such as nurses, public health nurses, physicians, dentists, and pharmacists.
This research paper focuses on the perceptions of non-medical and medical professionals that contribute to patient safety, mutual understanding between patients and medical professionals in clinical settings, and the avoidance of disputes and litigation. The results may help improve communication between patients and healthcare professionals, as well as eliminate misunderstandings in the area of informed consent.
This article was previously posted to the Research Square Preprints server on October 9, 2023, but the preprints were not reviewed and are unofficial.
Materials and methods
Study design
The study developed a cross-sectional Internet survey for non-medical professionals and nurses aged ≥ 20 years. Members of the survey company who met this study’s eligibility criteria were provided with a document explaining this survey’s purpose, specifically to compare the tolerance of uncertainty in medical care between non-medical professionals and nurses. Those who read the document and expressed interest were included.
Eligibility criteria
Participants were nurses and non-medical professionals aged ≥ 20 years from different parts of Japan. Mandatory criteria were access to a computer or similar devices with an Internet connection and being registered monitors with the Internet survey company.
Study setting
We conducted an Internet-based cross-sectional survey using the platform of an Internet survey company that maintains a database of over three million individuals. The recruitment and survey period lasted two weeks in March 2023.
Ethical considerations
This study was approved by the ethics committee of Gifu University of Health Science, Gifu, Japan (approval no.: 2022_19). We outsourced the Internet survey administration to an online research company, which contacted the survey monitors and collected the study data. The purpose of the survey was provided at the beginning of the questionnaire, and only those who agreed were allowed to proceed with the questions (Q). Informed consent was sought from participants through the Internet system. All methods were performed in accordance with relevant guidelines and regulations. The data were anonymized by the company and subsequently sent to the researchers.
Measures
The survey tool included questions about participant characteristics such as age, sex, education level, marital status, having children, medical care use as inpatient or outpatient at a medical institution, the population size of the residential area, occupation, and their perceptions of uncertainty in healthcare.
Participants were split into three categories based on their age: 20-39 years, 40-59 years, and ≥ 60 years. Education levels were classified as university/graduate school, vocational school/junior college, and junior high school/high school; junior colleges included two- or three-year courses. Marital status was categorized as married, which included divorced and widowed, or unmarried. Child status was categorized as without children and having children, which included those children living with the participant and those not. The population size of the residential area was categorized as follows: capital, including 23 wards of Tokyo or ordinance-designated cities with a population of 500,000 people or more; city, with a population of 200,000 people or more; middle city, with a population of 100,000 people or more; town, with a population of less than 100,000 people; and small town, with a population of less than 10,000 people. Regarding hospitalization or medical institution visit status, binary variables were used; the participant answered “yes” if they were currently an inpatient or outpatient at a medical institution (designated “medical care user”) or “no” if they were not. Occupations were classified as nurses and non-medical professionals. Additionally, occupation details included six categories: nurses, office workers (company workers and civil servants), self-employed (farmers, fishermen, and owners), housewives and students, unemployed, and others.
Questions about perceptions of uncertainty in healthcare were as follows: “Do you think that the saying ‘humans make mistakes’ applies to medical professionals as well?” (Q1); “Do you think that doctors may not be able to make a diagnosis in one visit?” (Q2); “Do you think that there are individual differences in how the effects of treatments and drugs appear?” (Q3); “Do you think that some people will have severe side effects even if they take the same medicine, while others will not?” (Q4); “Do you think that sudden deterioration (sudden worsening of the condition) or death that medical professionals cannot predict will occur?” (Q5); and “What do you think is the probability of neuropathy (numbness, sensation, movement abnormalities, etc.) from blood collection?” (Q6). The responses to Q1 through Q5 were rated on a seven-point Likert scale (absolutely agree: one; absolutely disagree: seven); Q3 and Q5 were reverse-scored. Higher scores indicated a lower tolerance of uncertainty in healthcare, and vice versa.
Item Q6 indicated the probability of neuropathy owing to blood sampling through seven options: one in 100 chances of developing neuropathy; one in 1,000; one in 100,000; one in 1,000,000; one in 10,000,000; one in 100,000,000; and no chance of developing neuropathy.
As shown in Appendix 1, a new questionnaire was created for this study by three nurse researchers based on previous research on uncertainty in healthcare (internal validity). A pre-study was conducted with five people (including registered nurses and non-medical professionals) to test the questionnaire. Based on their feedback, we revised the survey sheet so that it could be more easily understood by respondents. The questionnaire had 25 questions. Participants answered all questions within five to 10 minutes.
Sample size
Participants were randomly sampled from among the monitors of the Internet survey company, stratified according to age, sex groups (in similar proportions), and residential area. Regarding the residential area, the number of participants to be selected from the monitors was determined according to the population composition ratio of the prefecture. The Internet survey company sent a questionnaire to all participants and collected questionnaire responses until the target number was reached. To allow a 6.5% margin of error with a 95% confidence level and assume the population composition published by the Statistics Bureau of the Ministry of Internal Affairs and Communications [11], 228 participants were required for each category constructed by age and sex. The target number of participants was set at 1,430, allowing for invalid responses. For the nurses, the sex ratio of Japanese nurses was biased, with the percentage of female and male nurses being 91.9% and 8.1%, respectively [12]. Therefore, nurses were randomly sampled and stratified according to age. Similarly, 228 participants were calculated for 40-59 years, and fewer participants with a wider margin were set for the remaining age categories owing to a lack of nurses based on a survey of employed nurses by age group in 2020 [12]. The target number of nurses was set at 600 since it was unlikely that medical professionals would give invalid answers.
Analysis
Data were analyzed using t-tests and chi-square tests to compare the scores on the awareness of uncertainty in medical care questionnaires between non-medical professionals and nurses. We estimated the regression coefficients using a multiple regression model. In the model, the medical uncertainty scores of items Q1-Q6 served as the dependent continuous variables, while age, sex, education level, marital status, child status, population size of the residential area, medical care user, and occupations were all independent categorical variables. All statistical analyses were performed using SAS software version 9.4 (SAS Institute, Cary, NC) and Stata version 11.0 (StataCorp LLC, College Station, TX).
Results
Participants’ flowchart
Data were collected from 2,100 participants, including non-medical professionals (n = 1,500) and nurses who currently work in medical institutions (n = 600). We excluded 70 participants who were classified as non-medical professionals but were medically licensed. Finally, we analyzed data from 2,030 participants (non-medical professionals: 1,430; nurses: 600). Figure 1 presents the participant flowchart.
Figure 1. Flowchart showcasing the participant selection process.
Study characteristics
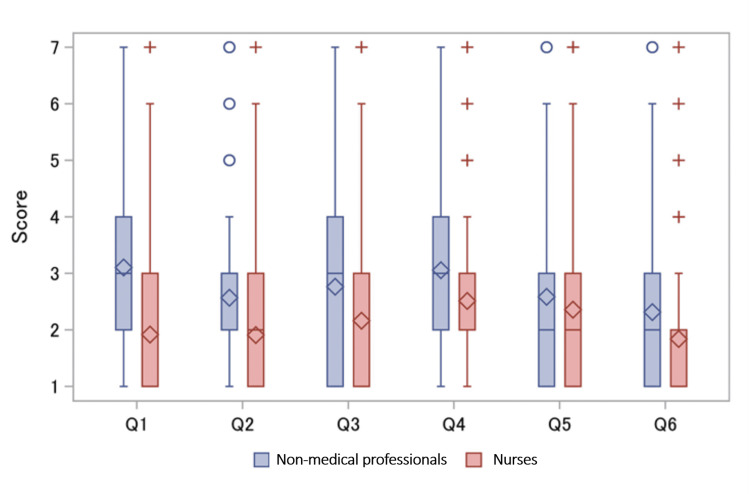
Table 1 shows the study participants’ characteristics. A higher proportion of non-medical professionals were aged 60 years and older compared to nurses and held a university or graduate school degree. Scores on the perceptions of uncertainty in medical care and comparisons between non-medical professionals and nurses are presented in Figure 2. All the means of non-medical professionals were higher than those of nurses (p <.01 for Q1-Q6).
Table 1. Participant characteristics: non-medical professionals and nurses.
Numbers shown (%); results based on chi-square test.
| Particulars | All | Non-medical professionals | Nurses | P-value |
| n = 1,430 | n = 600 | |||
| Age (years) | ||||
| 20-39 | 670 (33.0) | 470 (32.9) | 200 (33.3) | < .001 |
| 40-59 | 745 (36.7) | 474 (33.1) | 271 (45.2) | |
| ≥ 60 | 615 (30.3) | 486 (34.0) | 129 (21.5) | |
| Sex | ||||
| Male | 820 (40.4) | 725 (50.7) | 95 (15.8) | < .001 |
| Female | 1210 (59.6) | 705 (49.3) | 505 (84.2) | |
| Education level | ||||
| University/graduate school | 825 (40.6) | 664 (46.4) | 161 (26.8) | < .001 |
| Vocational school/junior college | 726 (35.8) | 295 (20.6) | 431 (71.8) | |
| Junior high school/high school | 479 (23.6) | 471 (33.0) | 8 (1.4) | |
| Marital status | ||||
| Unmarried | 698 (34.4) | 535 (37.4) | 163 (27.2) | < .001 |
| Married | 1332 (65.6) | 895 (62.6) | 437 (72.8) | |
| Child status | ||||
| Without children | 970 (47.8) | 732 (51.2) | 238 (39.7) | < .001 |
| Having children | 1060 (52.2) | 698 (48.8) | 362 (60.3) | |
| Population size in the living area | ||||
| Capital | 706 (34.8) | 509 (35.6) | 197 (32.8) | .114 |
| City | 472 (23.3) | 323 (22.6) | 149 (24.8) | |
| Middle city | 332 (16.4) | 245 (17.1) | 87 (14.5) | |
| Town | 410 (20.2) | 272 (19.0) | 138 (23.0) | |
| Small town | 110 (5.4) | 81 (5.7) | 29 (4.8) | |
| Medical care user | ||||
| Yes | 721 (35.5) | 501 (35.0) | 220 (36.7) | .483 |
| No | 1309 (64.5) | 929 (65.0) | 380 (63.3) | |
| Occupation details | ||||
| Nurses | 600 (29.6) | - | 600 (100.0) | - |
| Office workers | 599 (29.5) | 599 (41.9) | - | |
| Self-employed | 72 (3.5) | 72 (5.0) | - | |
| Housewives and students | 247 (12.2) | 247 (17.3) | - | |
| Unemployed | 254 (12.5) | 254 (17.8) | - | |
| Others | 258 (12.7) | 258 (18.0) | - |
Figure 2. Scores on perceptions of medical uncertainty: comparisons between non-medical professionals and nurses .
Diamonds represent mean scores.
Q1: “Do you think that the saying ‘humans make mistakes’ applies to medical professionals as well?”
Q2: “Do you think that doctors may not be able to make a diagnosis in one visit?”
Q3: “Do you think that there are individual differences in how the effects of treatments and drugs appear?”
Q4: “Do you think that some people will have severe side effects even if they take the same medicine, while others will not?”
Q5: “Do you think that sudden deterioration (sudden worsening of the condition) or death that medical professionals cannot predict will occur?”
Q6: “What do you think is the probability of neuropathy (numbness, sensation, movement abnormalities, etc.) from blood collection?”
Q: question
Table 2 presents the perception of uncertainty scores from the multiple regression model. These present comparisons between the various characteristics of non-medical professionals and nurses. The scores of all the questions were associated with ages 20-39 and occupations. Ages 20-39 and occupation among non-medical professionals were strongly positively associated with Q1-Q6. Small towns (a population size of residential area) were positively associated with all questions except Q3. Moreover, being a medical care user was negatively associated with all questions except Q3. A negative association was noted between male participants and Q1, but junior high school/high school education was positively associated with Q1. The variable without children was negatively associated with the scores of items Q3 and Q5. Appendices 2-3 show scores on perceptions of medical uncertainty between nurses' and non-medical professionals' occupations.
Table 2. Multiple regression analysis of the scores on perceptions of medical uncertainty.
Q: question; coef.: regression coefficient; ref.: reference
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | |||||||
| Coef. | P | Coef. | P | Coef. | P | Coef. | P | Coef. | P | Coef. | P-value | |
| Age (years) (ref. = 40-59) | ||||||||||||
| 20-39 | 0.174 | 0.045 | 0.209 | 0.002 | 0.201 | 0.015 | 0.185 | 0.008 | 0.272 | 0.002 | 0.26 | 0.004 |
| ≥ 60 | 0.104 | 0.252 | -0.06 | 0.401 | -0.12 | 0.179 | -0.08 | 0.252 | -0.06 | 0.495 | 0.187 | 0.045 |
| Sex (ref. = female) | ||||||||||||
| Male | -0.33 | < .001 | -0.11 | 0.071 | -0.07 | 0.346 | 0.036 | 0.568 | 0.036 | 0.637 | 0.142 | 0.076 |
| Education level (ref. = university/graduate school) | ||||||||||||
| Vocational school/junior college | 0.043 | 0.631 | -0 | 0.963 | 0.063 | 0.459 | -0.05 | 0.486 | 0.002 | 0.982 | 0.004 | 0.963 |
| Junior high school/high school | 0.337 | < .001 | 0.135 | 0.064 | 0.008 | 0.932 | 0.079 | 0.172 | -0.09 | 0.343 | 0.21 | 0.029 |
| Marital status (ref. = married) | ||||||||||||
| Unmarried | -0.06 | 0.585 | 0.034 | 0.698 | 0.093 | 0.392 | 0.078 | 0.387 | 0.042 | 0.701 | -0.02 | 0.898 |
| Having children (ref. = having children) | ||||||||||||
| Without children | -0.16 | 0.131 | -0.1 | 0.222 | -0.26 | 0.01 | -0.11 | 0.172 | -0.3 | 0.003 | 0.058 | 0.590 |
| Population size in the living area (ref. = capital) | ||||||||||||
| City | -0.03 | 0.765 | 0.021 | 0.774 | 0.093 | 0.298 | 0.008 | 0.921 | 0.123 | 0.186 | 0.008 | 0.934 |
| Middle city | 0.018 | 0.866 | 0.038 | 0.648 | 0.158 | 0.114 | 0.033 | 0.699 | 0.182 | 0.081 | -0.03 | 0.756 |
| Town | 0.137 | 0.163 | 0.055 | 0.473 | 0.051 | 0.586 | 0.048 | 0.548 | 0.057 | 0.559 | -0.04 | 0.726 |
| Small town | 0.573 | < .001 | 0.775 | < .001 | 0.215 | 0.162 | 0.952 | < .001 | 0.52 | 0.001 | 0.057 | 0.001 |
| Medical care user (ref. = no) | ||||||||||||
| Yes | -0.19 | 0.014 | -0.24 | < .001 | -0.13 | 0.073 | -0.29 | < .001 | -0.2 | 0.01 | -0.31 | < .001 |
| Occupations (ref. = nurses) | ||||||||||||
| Non-medical professionals | 1.227 | < .001 | 0.662 | < .001 | 0.314 | < .001 | 0.417 | < .001 | 0.65 | < .001 | 0.393 | < .001 |
Discussion
This study examined the perceptions of medical uncertainty among non-medical professionals and nurses in Japan. Our study findings are similar to previous results in that a gap exists in the perceptions of patients’ health beliefs between medical care professionals and patients [13]. Healthcare is affected by uncertainty in structures and processes of care and not all situations in medical institutions can be strictly controlled [4]. Street et al. reported that physicians may not necessarily be good judges of patients’ health beliefs and recommended the implementation of partnership-building strategies to encourage active patient participation [13]. Our results revealed that, compared with nurses, non-medical professionals are less tolerant of uncertainty regarding four points: 1) people making mistakes; 2) diagnosis, treatment, or drug uncertainty; 3) sudden deterioration; and 4) injury from blood collection.
To fill the gap between non-medical professionals and healthcare providers, the latter should inform the former regarding any uncertainty in medical care provision, and non-medical professionals should recognize the uncertainties inherent in medical care.
Non-medical professionals are less tolerant of human error
We found that non-medical professionals’ scores on perceptions of medical uncertainty were higher than those of nurses for item Q1, suggesting that non-medical professionals were less accepting of medical uncertainty owing to human errors than nurses. Item Q1 includes the term “humans make mistakes,” stated as a common saying in the fields of health and safety, indicating that human error is natural [14]. The probability of the occurrence of human error cannot be zero; however, we noted a gap of 1.2 points in the scores for item Q1 between non-medical professionals and nurses. In the multiple regression model, after adjusting for other variables, non-medical professionals appear to be less tolerant than nurses of uncertainty in healthcare. Informed consent involves processes through which healthcare providers educate patients about the risks and benefits of and alternatives to treatment procedures or interventions [15]. However, informed consent does not include explanations regarding errors that can occur because healthcare providers are humans. As such, general non-medical professionals may be unaware that human error can occur in healthcare. Therefore, non-medical professionals must be educated that errors cannot be completely prevented, even if healthcare providers confront human errors from an individual or organizational standpoint.
Compared to nurses, non-medical professionals are less tolerant of diagnostic, treatment, or drug uncertainty
Our findings revealed an association between medical care users and their tolerance of medical uncertainty. Moreover, regarding the population size of residential areas, small towns were positively associated with diagnostic uncertainty and side effects of drugs, and the age group of 20-39 years and non-medical professionals were positively associated with diagnostic uncertainty, effects of treatment, and drugs, and side effects of drugs.
Medical litigation includes issues such as intraoperative negligence, inadequate informed consent, ineffective explanations regarding complications, and poor teamwork or communication [16]. Medical providers must communicate with their patients about uncertainties in medical care. Dahm et al. reported that physicians used two main communication strategies to manage diagnostic uncertainty, and patient-centered communication was associated with positive patient reactions [17]. A study of physicians’ tolerance in medical care indicated that tolerance of uncertainty is associated with the characteristics and experience of physicians and that less tolerance is associated with burnout [18], which has been prominently displayed during the coronavirus disease 2019 (COVID-19) pandemic. Although the medical situation in the early days of the COVID-19 pandemic was dire and a standard treatment was lacking, medical care had to be provided. In addition, there was uncertainty about when this situation would end. The ability to tolerate uncertainty was needed to prevent burnout among healthcare providers [19, 20]. Outside of the COVID-19 pandemic, medical care is generally fraught with uncertainty. All treatments and drugs have individual differences in efficiency, and some patients develop serious complications and side effects. To prevent burnout and conflicts related to medical issues, healthcare providers must communicate with patients about uncertainty in medical care.
Prior research has reported an association between tolerance of uncertainty in medical care and the size of residential areas, demonstrating how access to health information and its use differ between rural and urban areas [21]. This also shows that differences in health literacy between rural and urban populations are not atypical and are associated with social factors [22]. Differences based on the population size of residential areas should be examined further in future research.
Non-medical professionals are less tolerant of sudden deterioration
The gap between healthcare providers’ and patients’ perceptions of prognostic uncertainty can be attributed to poor communication between patients and care providers. Examples of poor communication include physicians’ reluctance to communicate the uncertain circumstances that can lead to a patient’s death, while the family prefers to acquire all necessary details regarding the loss of their loved one [23,24]. Akiyama et al. reported that healthcare providers did not have risk perceptions of patients’ accidental choking, although choking has caused severe disabilities or even led to patient deaths [25]. Medical care users demonstrated a tolerance for sudden deterioration, but all occupations, excluding self-employment, and those living in small towns were associated with an intolerance of uncertainty in medical care. We believe that the reasons for this trend are similar to those for the population’s low tolerance of diagnosis, treatment, or drug uncertainty. Healthcare providers cannot fully anticipate all the sudden changes a patient may experience. However, in some cases, preventive efforts can be taken by providing appropriate explanations to patients and their families or by predicting risks and taking necessary measures.
Compared to nurses, non-medical professionals are less tolerant of injuries during blood collection
Nerve injury during venipuncture can be caused by direct puncture or compression [26]. The incidence of nerve injury during venipuncture can vary, with estimates in the range of 0.02%-0.03% [27, 28]. Although the incidence is very low and recovery may occur after a few months, venipuncture is a common medical procedure; hence, public awareness about neuropathy is an important matter to be addressed by healthcare providers. Participants aged 20-39 years, those living in a small town, and those with non-medical occupations demonstrated a lower tolerance of uncertainty in medical care than did other participants. Tolerance of uncertainty in medical care was associated with medical care usage. Younger generations might be perceived as less tolerant because they have less experience using medical care. Non-medical professionals’ tolerance of uncertainty in blood collection is very low in comparison to that of nurses; thus, it is necessary to carefully explain the possibility of neuropathy to non-medical professionals.
Strengths and limitations of the research
Our study had some limitations. First, the characteristics of non-medical professionals and nurses differed. In general, most nurses are women, with research reporting 92.2% female nurses and 8.1% male nurses [29]. Thus, it was impossible to avoid biases related to sex and education level owing to occupational characteristics. Second, we implemented an online survey method. While this approach is convenient for collecting information from many non-medical professionals, information about the population distribution could not be obtained from the Internet survey monitors. In addition, Andrade et al. reported the possibility of respondents having biases toward this type of survey [30]. Thus, our findings may have limited generalization.
However, as a research strength, our study provides a different perspective on non-medical professionals’ tolerance of uncertainty in medical care. Nurses play an important role in medical care as they spend most of their time with patients. Our results demonstrate that perception gaps exist among non-medical professionals and nurses. This gap might be even greater for other medical professionals and non-medical professionals. Collecting data from non-medical professionals using controlled sampling strategies presents some difficulties. Despite these limitations, our study provides a different perspective on non-medical professionals’ tolerance of uncertainty in medical care.
Conclusions
Our results revealed that non-medical professionals are less tolerant of uncertainty in medical care than nurses are regarding the following four points: there are people making mistakes; diagnosis, treatment, drug uncertainty; sudden deterioration; or injury from blood collection.
The results demonstrate that patients who receive medical care are more tolerant of medical uncertainty than non-patients. In addition, young people were generally less tolerant than older respondents. The younger generation, those who are likely to be family members of patients, have a low tolerance for medical care uncertainty and may even become involved in medical conflicts through their families. Therefore, to reduce conflicts related to medical issues, healthcare providers need to inform non-medical professionals regarding the perception of uncertainty in medical care.
Acknowledgments
We thank the respondents of this Internet survey. Data are available on reasonable request. The data are stored as de-identified participant data, which are available on request to Naomi Akiyama (nakiyama888@gmail.com).
Appendices
Table 3. Questionnaire.
| Participants were randomly sampled from among the monitors of the Internet survey company and stratified according to age, sex (in similar proportions), and residential area. | |||||
| Please choose one appropriate answer to each of the following questions. | |||||
| Q1. Please let me know your sex. (single selection) | 1. Male | ||||
| 2. Female | |||||
| Q2. Please let me know your age. | ( )-years-old | ||||
| Q3. Please let me know your living prefecture. (single selection) | 1. Hokkaido | 2. Aomori | 3. Iwate | 4. Miyagi | 5. Akita |
| 6. Yamagata | 7. Fukushima | 8. Ibaragi | 9. Ibaraki | 10. Gunma | |
| 11. Saitama | 12. Chiba | 13. Tokyo | 14. Kanagawa | 15. Niigata | |
| 16. Toyama | 17. Ishikawa | 18. Fukui | 19. Yamanashi | 20. Nagano | |
| 21. Gifu | 22. Shizuoka | 23. Aichi | 24. Mie | 25. Shiga | |
| 26. Kyoto | 27. Osaka | 28. Hyogo | 29. Nara | 30. Wakayama | |
| 31. Tottori | 32. Shimane | 33. Okayama | 34. Hiroshima | 35. Yamaguchi | |
| 36. Tokushima | 37. Kagawa | 38. Ehime | 39. Kochi | 40. Fukuoka | |
| 41. Saga | 42. Nagasaki | 43. Kumamoto | 44. Ooita | 45. Miyagi | |
| 46. Kagoshima | 47. Okinawa | ||||
| Please choose one appropriate answer to the following questions. | |||||
| Q1. Are you married? (single selection) | 1. Unmarried | ||||
| 2. Married (separated/widowed) | |||||
| Q2. Do you have children? (single selection) | 1. Living with children | ||||
| 2. We don’t live together, but we have children | |||||
| 3. No children | |||||
| Q3. Please let me know your occupation. (single selection) | 1. Working at a company | ||||
| 2. Company management | |||||
| 3. Civil servant, teacher, non-profit organization employee | |||||
| 4. Self-employed (business and industry services) | |||||
| 5. Agriculture, forestry, and fisheries | |||||
| 6. Doctor | |||||
| 7. Dentist | |||||
| 8. Pharmacist | |||||
| 9. Nurse | |||||
| 10. Assistant nurse | |||||
| 11. Public health nurse | |||||
| 12. Midwife | |||||
| 13. Physical therapist | |||||
| 14. Occupational therapist | |||||
| 15. Other health-related profession | |||||
| 16. Legal management | |||||
| 17. Professional such as a lawyer or tax accountant | |||||
| 18. Housewife/househusband | |||||
| 19. Student | |||||
| 20. Other occupation | |||||
| Q4. Do you have a medical license? (single selection) | 1. Yes | ||||
| 2. No | |||||
| Q5. Are you currently hospitalized or attending a medical institution (hospital or clinic)? (single selection) | 1. Yes | ||||
| 2. No | |||||
| Q6. Do you have experience working at a medical institution (hospital or clinic)? (single selection) | 1. Yes | ||||
| 2. No | |||||
| Q7. What is the current population size of your area? (single selection) | 1. Special wards (23 wards of Tokyo) or ordinance-designated cities with a population of 500,000 or more. | ||||
| 2. Core cities or special cities with a population of 200,000 or more | |||||
| 3. Cities with a population of 100,000 or more | |||||
| 4. Cities with a population of less than 100,000 people | |||||
| 5. Towns and villages with a population of less than 10,000 people | |||||
| Q8. Please indicate your highest educational background. (single selection) | 1. Junior high school graduate | ||||
| 2. High school graduate | |||||
| 3. Vocational school graduate | |||||
| 4. Junior college graduate | |||||
| 5. University graduate | |||||
| 6. Graduate school | |||||
| 7. Others | |||||
| Q9. Do you think that the saying “humans make mistakes” applies to medical professionals as well? (single selection) | 1. Totally true | ||||
| 2. Quite true | |||||
| 3. More or less likely | |||||
| 4. Neither agree nor disagree | |||||
| 5. Rather different | |||||
| 6. Quite different | |||||
| 7. Completely different | |||||
| Q10. Do you think that doctors may not be able to make a diagnosis in one visit? (single selection) | 1. Totally true | ||||
| 2. Quite true | |||||
| 3. More or less likely | |||||
| 4. Neither agree nor disagree | |||||
| 5. Rather different | |||||
| 6. Quite different | |||||
| 7. Completely different | |||||
| Q11. Do you think that there are individual differences in how the effects of treatments and drugs appear? (single selection) | 1. Totally true | ||||
| 2. Quite true | |||||
| 3. More or less likely | |||||
| 4. Neither agree nor disagree | |||||
| 5. Rather different | |||||
| 6. Quite different | |||||
| 7. Completely different | |||||
| Q12. Do you think that some people will have severe side effects even if they take the same medicine, while others will not? (single selection) | 1. Totally true | ||||
| 2. Quite true | |||||
| 3. More or less likely | |||||
| 4. Neither agree nor disagree | |||||
| 5. Rather different | |||||
| 6. Quite different | |||||
| 7. Completely different | |||||
| Q13. Do you think that sudden deterioration (sudden worsening of the condition) or death that medical professionals cannot predict will occur? (single selection) | 1. Totally true | ||||
| 2. Quite true | |||||
| 3. More or less likely | |||||
| 4. Neither agree nor disagree | |||||
| 5. Rather different | |||||
| 6. Quite different | |||||
| 7. Completely different | |||||
| Q14. What do you think is the probability of neuropathy (numbness, sensation, movement abnormalities, etc.) from blood collection? (single selection) | 1.Never (zero) | ||||
| 2.1 in 100 people | |||||
| 3.1 in 1000 people | |||||
| 4.1 to 1 in 100,000 people | |||||
| 5. 1 in 1 million people | |||||
| 6. 1 in 10 million people | |||||
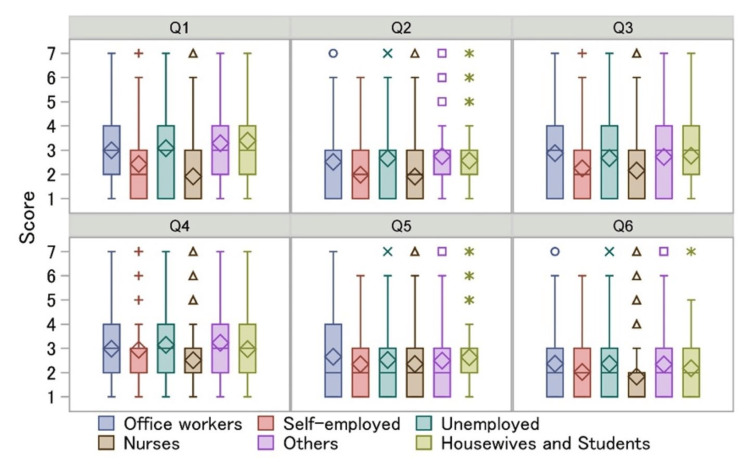
Figure 3. Scores on perceptions of medical uncertainty: comparisons between non-medical professionals' occupation details and nurses.
Diamonds represent mean scores.
Q1: ‘Do you think that the saying “humans make mistakes” applies to medical professionals as well’?
Q2: ‘Do you think that doctors may not be able to make a diagnosis in one visit’?
Q3: ‘Do you think that there are individual differences in how the effects of treatments and drugs appear’?
Q4: ‘Do you think that some people will have severe side effects even if they take the same medicine, while others will not’?
Q5: ‘Do you think that sudden deterioration (sudden worsening of the condition) or death that medical professionals cannot predict will occur’?
Q6: ‘What do you think is the probability of neuropathy (numbness, sensation, movement abnormalities, etc.) from blood collection’?
Q: question
Table 4. Multiple regression analysis of the scores on the perceptions of medical uncertainty segregated by non-medical professionals’ occupations.
Q: question; coef.: regression coefficient; ref.: reference
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | ||||||||
| Coef. | P | Coef. | P | Coef. | P | Coef. | P | Coef. | P | Coef. | P | ||
| Age (years) (ref. = 40-59) | |||||||||||||
| 20-39 | 0.161 | 0.064 | 0.202 | 0.003 | 0.189 | 0.023 | 0.177 | 0.012 | 0.253 | 0.003 | 0.267 | 0.003 | |
| ≥ 60 | 0.100 | 0.287 | -0.090 | 0.198 | -0.120 | 0.190 | -0.094 | 0.214 | -0.040 | 0.633 | 0.169 | 0.082 | |
| Sex (ref. = female) | |||||||||||||
| Male | -0.290 | 0.001 | -0.080 | 0.203 | -0.090 | 0.276 | 0.007 | 0.921 | 0.036 | 0.671 | 0.176 | 0.044 | |
| Education level (ref. = university/graduate school) | |||||||||||||
| Vocational school/junior college | 0.037 | 0.681 | -0.010 | 0.874 | 0.073 | 0.395 | -0.044 | 0.544 | 0.012 | 0.896 | -0.010 | 0.922 | |
| Junior high school/high school | 0.316 | 0.001 | 0.104 | 0.159 | 0.023 | 0.796 | 0.084 | 0.273 | -0.070 | 0.439 | 0.178 | 0.068 | |
| Marital status (ref. = married) | |||||||||||||
| Unmarried | -0.040 | 0.697 | 0.025 | 0.771 | 0.099 | 0.351 | 0.068 | 0.450 | 0.058 | 0.600 | -0.020 | 0.083 | |
| Having children (ref. = having children) | |||||||||||||
| Without children | -0.150 | 0.153 | -0.100 | 0.207 | -0.260 | 0.010 | -0.119 | 0.158 | -0.300 | 0.004 | 0.056 | 0.605 | |
| Population size in the living area (ref. = capital) | |||||||||||||
| City | -0.030 | 0.739 | 0.021 | 0.783 | 0.092 | 0.302 | 0.008 | 0.917 | 0.120 | 0.194 | 0.008 | 0.934 | |
| Middle city | 0.013 | 0.899 | 0.067 | 0.744 | 0.153 | 0.127 | 0.026 | 0.761 | 0.178 | 0.087 | -0.030 | 0.759 | |
| Town | 0.140 | 0.156 | 0.053 | 0.490 | 0.054 | 0.565 | 0.048 | 0.547 | 0.062 | 0.524 | -0.040 | 0.699 | |
| Small town | 0.571 | < .001 | 0.750 | < .001 | 0.220 | 0.154 | 0.943 | < .001 | 0.530 | 0.001 | 0.551 | 0.001 | |
| Medical care user (ref. = no) | |||||||||||||
| Yes | -0.180 | 0.016 | -0.240 | < .001 | -0.140 | 0.062 | -0.294 | < .001 | -0.190 | 0.010 | -0.310 | < .001 | |
| Occupations (ref. = nurses) | |||||||||||||
| Office workers | 1.190 | < .001 | 0.608 | < .001 | 0.378 | < .001 | 0.465 | < .001 | 0.725 | < .001 | 0.301 | 0.008 | |
| Self-employed | 0.666 | 0.001 | 0.161 | 0.320 | 0.165 | 0.403 | 0.198 | 0.237 | 0.204 | 0.320 | 0.287 | 0.180 | |
| Housewives and students | 1.308 | < .001 | 0.657 | < .001 | 0.327 | 0.008 | 0.349 | 0.001 | 0.656 | < .001 | 0.399 | 0.003 | |
| Unemployed | 1.215 | < .001 | 0.827 | < .001 | 0.348 | 0.009 | 0.531 | < .001 | 0.624 | < .001 | 0.442 | 0.002 | |
| Others | 1.308 | < .001 | 0.783 | < .001 | 0.192 | 0.112 | 0.402 | < .001 | 0.597 | < .001 | 0.551 | < .001 | |
The authors have declared financial relationships, which are detailed in the next section.
Naomi Akiyama, Ryuji Uozumi, Tomoya Akiyama, Mie Morikawa declare(s) a grant from Grants-in-Aid for Scientific Research (grant numbers 20K18889, 20H01598, and 20H04147).
Author Contributions
Concept and design: Naomi Akiyama, Shihoko Kajiwara, Ryuji Uozumi, Kenshi Hayashida, Jasmine Sim, Mie Morikawa, Tomoya Akiyama
Acquisition, analysis, or interpretation of data: Naomi Akiyama, Shihoko Kajiwara, Ryuji Uozumi, Kenshi Hayashida, Jasmine Sim, Mie Morikawa, Tomoya Akiyama
Drafting of the manuscript: Naomi Akiyama, Shihoko Kajiwara, Ryuji Uozumi, Kenshi Hayashida, Jasmine Sim, Mie Morikawa, Tomoya Akiyama
Critical review of the manuscript for important intellectual content: Naomi Akiyama, Shihoko Kajiwara, Ryuji Uozumi, Kenshi Hayashida, Jasmine Sim, Mie Morikawa, Tomoya Akiyama
Supervision: Kenshi Hayashida, Jasmine Sim, Mie Morikawa, Tomoya Akiyama
Human Ethics
Consent was obtained or waived by all participants in this study. Ethics Committee, Gifu University of Health Science issued approval 2022_19
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.The association between fear of malpractice and burnout among Chinese medical workers: the mediating role of legal consciousness. Liang F, Hu S, Guo Y. BMC Psychiatry. 2022;22:358. doi: 10.1186/s12888-022-04009-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Second victim phenomenon: is 'just culture' a reality? An integrative review. White RM, Delacroix R. Appl Nurs Res. 2020;56:151319. doi: 10.1016/j.apnr.2020.151319. [DOI] [PubMed] [Google Scholar]
- 3.Varieties of uncertainty in health care: a conceptual taxonomy. Han PK, Klein WM, Arora NK. Med Decis Making. 2011;31:828–838. doi: 10.1177/0272989X11393976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uncertainty in health care: towards a more systematic program of research. Han PK, Babrow A, Hillen MA, Gulbrandsen P, Smets EM, Ofstad EH. Patient Educ Couns. 2019;102:1756–1766. doi: 10.1016/j.pec.2019.06.012. [DOI] [PubMed] [Google Scholar]
- 5.Understanding and managing uncertainty in health care: revisiting and advancing sociological contributions. Mackintosh N, Armstrong N. Sociol Health Illn. 2020;42 Suppl 1:1–20. doi: 10.1111/1467-9566.13160. [DOI] [PubMed] [Google Scholar]
- 6.Dealing with medical uncertainty: a physician's perspective. Ghosh AK. http://PMID: 15559102. Minn Med. 2004;87:48–51. [PubMed] [Google Scholar]
- 7.Principles of clinical ethics and their application to practice. Varkey B. Med Princ Pract. 2021;30:17–28. doi: 10.1159/000509119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Managing uncertainty in advanced liver disease: a qualitative, multiperspective, serial interview study. Kimbell B, Boyd K, Kendall M, Iredale J, Murray SA. BMJ Open. 2015;5:0. doi: 10.1136/bmjopen-2015-009241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patients' complaints regarding healthcare encounters and communication. Skär L, Söderberg S. Nurs Open. 2018;5:224–232. doi: 10.1002/nop2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patient engagement. [ May; 2023 ];https://apps.who.int/iris/bitstream/handle/10665/252269/9789241511629-eng.pdf 2016 12:2023. [Google Scholar]
- 11.Population by age (each age) and gender - total population, national population (as of October 1, 2020) (Website in Japanese) [ May; 2023 ];https://www.stat.go.jp/data/jinsui/2.html 2021 16:2023. [Google Scholar]
- 12.2020 health administration report example (employed medical personal) (Website in Japanese) [ Apr; 2023 ];https://www.mhlw.go.jp/toukei/saikin/hw/eisei/20/dl/gaikyo.pdf 2022 7:2023. [Google Scholar]
- 13.How well do doctors know their patients? Factors affecting physician understanding of patients' health beliefs. Street RL Jr, Haidet P. J Gen Intern Med. 2011;26:21–27. doi: 10.1007/s11606-010-1453-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reason J. Press. Cambridge, United Kingdom: Cambridge University Press; 1990. Human Error; pp. 20–33. [Google Scholar]
- 15.Shah P, Thornton I, Turrin D, Hipskind JE. Treasure Island: StatPearls Publishing. Treasure Island, FL: StatPearls [Internet], StatPearls Publishing; 2024. Informed Consent. [Google Scholar]
- 16.Analysis of factors associated with rhytidectomy malpractice litigation cases. Kandinov A, Mutchnick S, Nangia V, Svider PF, Zuliani GF, Shkoukani MA, Carron MA. JAMA Facial Plast Surg. 2017;19:255–259. doi: 10.1001/jamafacial.2016.1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Communication of diagnostic uncertainty in primary care and its impact on patient experience: an integrative systematic review. Dahm MR, Cattanach W, Williams M, Basseal JM, Gleason K, Crock C. J Gen Intern Med. 2023;38:738–754. doi: 10.1007/s11606-022-07768-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Factors associated with physician tolerance of uncertainty: an observational study. Begin AS, Hidrue M, Lehrhoff S, Del Carmen MG, Armstrong K, Wasfy JH. J Gen Intern Med. 2022;37:1415–1421. doi: 10.1007/s11606-021-06776-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.From resilience to burnout in healthcare workers during the COVID-19 emergency: the role of the ability to tolerate uncertainty. Di Trani M, Mariani R, Ferri R, De Berardinis D, Frigo MG. Front Psychol. 2021;12:646435. doi: 10.3389/fpsyg.2021.646435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Towards a model of uncertainty distress in the context of coronavirus (COVID-19) Freeston M, Tiplady A, Mawn L, Bottesi G, Thwaites S. Cogn Behav Therap. 2020;13:0. doi: 10.1017/S1754470X2000029X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Differences in rural and urban health information access and use. Chen X, Orom H, Hay JL, Waters EA, Schofield E, Li Y, Kiviniemi MT. J Rural Health. 2019;35:405–417. doi: 10.1111/jrh.12335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Health literacy in rural and urban populations: a systematic review. Aljassim N, Ostini R. Patient Educ Couns. 2020;103:2142–2154. doi: 10.1016/j.pec.2020.06.007. [DOI] [PubMed] [Google Scholar]
- 23.Communicating prognostic uncertainty in potential end-of-life contexts: experiences of family members. Krawczyk M, Gallagher R. BMC Palliat Care. 2016;15:59. doi: 10.1186/s12904-016-0133-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Family members' perceptions of end-of-life care across diverse locations of care. Gallagher R, Krawczyk M. BMC Palliat Care. 2013;12:25. doi: 10.1186/1472-684X-12-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Choking injuries: associated factors and error-producing conditions among acute hospital patients in Japan. Akiyama N, Uozumi R, Akiyama T, Koeda K, Shiroiwa T, Ogasawara K. PLoS One. 2022;17:0. doi: 10.1371/journal.pone.0267430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reducing the risk of nerve injuries. Arbique J, Arbique D. Nursing. 2007;37:20–21. doi: 10.1097/01.NURSE.0000298182.61285.04. [DOI] [PubMed] [Google Scholar]
- 27.Venipuncture nerve injuries in the upper extremity from more than 1 million procedures. Tsukuda Y, Funakoshi T, Nasuhara Y, Nagano Y, Shimizu C, Iwasaki N. J Patient Saf. 2019;15:299–301. doi: 10.1097/PTS.0000000000000264. [DOI] [PubMed] [Google Scholar]
- 28.Incidence and prognosis of persistent pain induced by venipuncture for blood sampling: an observational study over a 5-year period. Kato J, Araki H, Kimura M, et al. Pain Med. 2012;13:1627–1630. doi: 10.1111/j.1526-4637.2012.01490.x. [DOI] [PubMed] [Google Scholar]
- 29.Report on public health administration and services in 2020 (Website in Japanese) [ Apr; 2023 ];https://www.mhlw.go.jp/toukei/saikin/hw/eisei/20/dl/gaikyo.pdf Report on public health administration and services in. 2022 2022:20–28. [Google Scholar]
- 30.The limitations of online surveys. Andrade C. Indian J Psychol Med. 2020;42:575–576. doi: 10.1177/0253717620957496. [DOI] [PMC free article] [PubMed] [Google Scholar]