Abstract
The link between bipolar disorder (BP) and immune dysfunction remains controversial. While epidemiological studies have long suggested an association, recent research has found only limited evidence of such a relationship. To clarify this, we performed an exploratory study of the contributions of immune-relevant genetic factors to the response to lithium (Li) treatment and the clinical presentation of BP. First, we assessed the association of a large collection of immune-related genes (4925) with Li response, defined by the Retrospective Assessment of the Lithium Response Phenotype Scale (Alda scale), and clinical characteristics in patients with BP from the International Consortium on Lithium Genetics (ConLi+Gen, N = 2374). Second, we calculated here previously published polygenic scores (PGSs) for immune-related traits and evaluated their associations with Li response and clinical features. Overall, we observed relatively weak associations (p < 1 × 10−4) with BP phenotypes within immune-related genes. Network and functional enrichment analyses of the top findings from the association analyses of Li response variables showed an overrepresentation of pathways participating in cell adhesion and intercellular communication. These appeared to converge on the well-known Li-induced inhibition of GSK-3β. Association analyses of age-at-onset, number of mood episodes, and presence of psychosis, substance abuse and/or suicidal ideation suggested modest contributions of genes such as RTN4, XKR4, NRXN1, NRG1/3 and GRK5 to disease characteristics. PGS analyses returned weak associations (p < 0.05) between inflammation markers and the studied BP phenotypes. Our results suggest a modest relationship between immunity and clinical features in BP. More research is needed to assess the potential therapeutic relevance.
Subject terms: Genetics, Bipolar disorder
Introduction
Bipolar disorder (BP) has been associated with some degree of immune dysfunction. Epidemiological data has linked immune-related medical comorbidities, including autoimmune and metabolic diseases, and chronic low-grade inflammation with BP. In particular, increases in pro-inflammatory cytokines are observed during affective episodes in patients with BP [1]. In addition, genomic studies have revealed weak yet significant genetic correlation between BP and immune-related diseases [2]. Nevertheless, as a number of these observations originated from underpowered studies [3], further investigations are required to elucidate the proposed relationships.
Lithium (Li), mainly used in the treatment of BP, is an effective pharmacological agent in the treatment of an array of psychiatric conditions [4, 5]. In addition to its mood-stabilizing effects, Li shows anti-viral and immune cell regulatory properties [6, 7]. The immune regulatory activity of Li has been partially attributed to the modulation of pro-inflammatory cytokines and GSK-3β. Therefore, it has been suggested that the mechanism through which Li improves symptom progression may be via anti-inflammatory effects [8, 9]. The Retrospective Assessment of the Lithium Response Phenotype Scale (Alda scale) is the most widely used clinical measure of Li response. Most often, it is dichotomized such that individuals with scores ≥7 are classified as “responders” and those with scores <7 as “non-responders” [10, 11]. Using this metric, previous genetic studies have implicated human leukocyte antigen (HLA) and inflammatory cytokine genes in the response to Li treatment in BP [12, 13]. Therefore, we hypothesized that single nucleotide polymorphisms (SNPs) in immune-related genes contribute, to some extent, to Li response and further, may impact specific clinical features within BP. To test our hypothesis, we performed association studies of a comprehensive collection of immune-related genes in 2374 patients with BP from the International Consortium on Lithium Genetics (ConLi+Gen) [14]. Additionally, we tested associations with published polygenic scores (PGSs) for immune-relevant traits.
Methods
Since our study follows a candidate approach to selected genes, pathways and networks, a diagram summarizing the methodology employed can be found in the Supplementary File 1: Fig. S1.
Study sample
The ConLi+Gen cohort has been previously described in detail [15]. Briefly, peripheral blood samples from individuals with diagnosis of a bipolar spectrum disorder (in accordance with the criteria established in the Diagnostic and Statistical Manual of Mental Disorders—DSM—versions III or IV) that had taken Li for a minimum of 6 months (with no additional mood stabilizers), were collected from 2003 to 2013 at various sites in Europe, the United States, Australia and East Asia. The isolated DNA was genotyped in two phases. This resulted in two sample batches originally referred to as “GWAS1” and “GWAS2”, comprising 1162 and 1401 individuals, respectively. Long-term responses to Li treatment were assessed in both sample batches using the Alda scale. Here, the A subscale rates the degree of response on a 10-point scale, and the B subscale reflects the relationship between improvement and treatment. A total score, ranging from 0–10, is obtained by subtracting the B score from the A score of these subscales. Negative scores are set to 0. Data on age-at-onset (AAO), age (at sample collection and phenotyping), sex and diagnostic subtype were available for both sample batches. Diagnoses included bipolar disorder type I and type II, schizoaffective bipolar disorder and bipolar disorder not otherwise specified. Additionally, information on psychiatric features, namely the number of episodes of depression, mania and hypomania, the presence of psychosis, alcohol and substance abuse, and suicidal ideation, were available for patients in the “GWAS1” batch.
The Ethics Committee at the University of Heidelberg provided central approval for the ConLi+Gen Consortium. Written informed consent from all participants was obtained according to the study protocols of each of the participating sites and their institutions. All procedures were performed in accordance with the guidelines of the Declaration of Helsinki.
Immune gene collection
A comprehensive set of immune-related genes was collated from gene lists available in the online databases MSigDB [16] and InnateDB [17]. From MSigDB (https://www.gsea-msigdb.org/gsea/msigdb/), the following gene sets contained in the C2 “curated gene sets” collection were retrieved: M1036: Reactome-innate immune system, M1058: Reactome-adaptive immune system, M39895: WikiPathways (WP)-neuroinflammation, M39711: WP-cytokines and inflammatory response, and M39641: WP-inflammatory response pathway. From InnateDB (https://www.innatedb.com/index.jsp), the curated gene lists derived from the Immunology Database and Analysis Portal (ImmPort), the Immunogenetic Related Information Source (IRIS) and the Immunome Database, were downloaded. Chromosomal locations were annotated from Ensembl using the hg19 build. Herein, the combined collection is referred to as the ImmuneSet and contained 4925 autosomal genes to be included in association analyses.
Genotype data
Schubert et al. [18] have previously described the creation of the genotype dataset used herein. Briefly, DNA samples were originally genotyped using either Affymetrix or Illumina SNP arrays. These genotype data from multiple cohorts were separately imputed using the 1000 Genomes Project reference panel phase 3 v5. Each imputed dataset underwent a basic quality control (QC) step to keep variants with minor allele frequency (MAF) > 0.01, Hardy-Weinberg equilibrium p value (HWE) ≥ 1 × 10−6 and imputation quality score (Rsq) ≥ 0.6. Genotype calls were derived from the imputed dosage scores and all datasets were merged by retaining only common sets of SNPs. To update this dataset and obtain a higher number of good quality variants, we re-imputed the genotype data via the Michigan Imputation Server [19] using the Haplotype Reference Consortium (HRC) panel for European ancestry. The re-imputed genotypes underwent a QC step to keep variants with Rsq ≥ 0.8, MAF ≥ 0.01 and HWE ≥ 1 × 10−6. Additionally, individuals were removed if they failed the heterozygosity test and/or showed relatedness, according to the tests performed using the plinkQC R package [20]. In the latter case, one individual from each pair of related individuals (PI-HAT > 0.25) was removed. For analysis of the ImmuneSet, SNPs within each gene’s boundaries (±0 kb) were retained. The final ImmuneSet genotype datasets contained 701,031 SNPs from 1024 and 1350 individuals in “GWAS1” and “GWAS2”, respectively.
Polygenic scores
A set of 32 published PGSs available at the PGS Catalog [21] were used to approximate markers of inflammation and immune-related phenotypes that were not experimentally measured in the “GWAS1” ConLi+Gen sample. These PGSs, created and evaluated in large samples of predominantly European ancestry, stemmed from three recent publications and corresponded to the following traits: autoimmune disease [22], lymphocyte/monocyte/eosinophil/neutrophil/basophil percentage of white (blood) cells [23], and serum levels of 26 markers of inflammation [24]. After downloading and harmonizing weight files, we performed allelic scoring in ConLi+Gen using the sum method applied in Plink 1.9 [25]. Sum scores were standardized for statistical analysis.
Association analyses
The “GWAS1” (N = 853) and “GWAS2” (N = 1258) samples were tested separately for associations of 701,031 SNPs in the ImmuneSet with: (1) Li response (responder/non-responder, defined by Alda scores ≥7 or <7, respectively), (2) total Alda score, (3) Alda subscale A, and (4) Alda subscale B (total). Because the most reliable continuous Li response phenotype has been previously shown to be the Alda A score, when excluding individuals with Alda B scores >4 [10], we tested this as the primary continuous phenotype in our study. All association tests were performed applying an additive model in Plink 1.9, and all models were adjusted for age at recruitment, age-at-onset (AAO), sex, diagnosis and the first principal components (PCs) obtained for each ImmuneSet genotypes dataset. PCA plots were explored to determine the optimal number of PCs to be used as covariates for each sample. Therefore, the first five PCs were used as covariates for “GWAS1” while the first six PCs were used for “GWAS2”. Population stratification due to ancestry (i.e., European or East Asian) and recruitment site was corrected by the selected numbers of PCs (Supplementary File 1: Fig. S2). Next, the association results for Li response from “GWAS1” and “GWAS2” samples were meta-analyzed using the weighted-z (METAL) method applied in Plink 1.9. These meta-analysis results were QCed to exclude variants with I2 heterogeneity index (I) > 40 and p value for Cochran’s Q statistic (Q) < 0.1 (highly heterogeneous). We searched first for associations at the commonly accepted thresholds for GWASs (genome-wide association, p < 5 × 10−8, and suggestive association, p < 1 × 10−5). However, considering this a candidate gene rather than a genome-wide approach, we chose to look further into findings with p < 1 × 10−4, a threshold that has been previously used to select association findings for follow-up in GWASs [26] and, therefore, represents an acceptable exploratory threshold.
In “GWAS1”, the ImmuneSet was further tested for associations with other BP clinical phenotypes (i.e., AAO, the number of episodes of depression, mania and hypomania, as well as the presence of psychosis, alcohol and/or substance abuse, and suicidal ideation). These models were adjusted for age at recruitment, AAO (except when AAO was tested as phenotype), sex, diagnosis and the first five PCs. Statistical association and exploratory thresholds were considered as above.
Associations between PGSs and the various BP clinical phenotypes were tested using linear or binomial regression models, as appropriate, adjusted for age at recruitment, AAO (except when AAO was tested as phenotype), sex, diagnosis, recruitment site and the first 10 PCs obtained from the genotypes using the robustbase R package. Statistical association was set to false discovery rate (FDR) < 0.05. The exploratory threshold was set to p < 0.05.
Downstream analyses
All variants under the p < 1 × 10−4 threshold were annotated for known regulatory effects on gene expression (i.e., expression quantitative trait loci, eQTLs) in all human brain, blood, spleen and thyroid tissues, as well as in immune cells (e.g., monocytes and macrophages) using Qtlizer [27].
A protein-protein interaction (PPI) network to investigate the functional relevance of the genes linked to Li response by the exploratory analyses was created using the ReactomeFIViz app [28] for Cytoscape 3.7 [29]. This analysis used as input a list composed of the ImmuneSet genes showing associations at the p < 1 × 10−4 threshold with the dichotomous and continuous Li response phenotypes. The network also incorporated “linker” genes (i.e., genes not in the input gene list that create indirect connections between input genes) to increase biological interpretability. Moreover, pathway overrepresentation analysis was performed on the PPI network (including linker genes) using the pathway enrichment network function of the app. Because the linker genes were not drawn from the ImmuneSet collection, we used the standard background genes of the ReactomeFiViz app for this analysis. The resulting overrepresented pathways were filtered to exclude terms that: (1) had FDR > 0.05, (2) corresponded to a specific disease (e.g., bladder cancer, herpes virus infection), (3) had less than two genes overlapping between the pathway set and the network set, and/or (4) the overlap with the pathway set represented less than 3% of genes in the set. Additionally, we repeated the pathway overrepresentation analysis including not only the variant mapped genes, but also the annotated eQTL genes.
For associations with clinical phenotypes in the “GWAS1” sample, functional analyses were performed using the GENE2FUNC tool of the Functional Mapping and Annotation of Genome-Wide Association Studies (FUMA-GWAS) platform [30]. The input gene lists included mapped and eQTL genes annotated for variants below the p < 1 × 10−4 threshold for each studied phenotype. Because eQTL genes were not drawn from our ImmuneSet collection, we used all protein-coding genes as background for these analyses. Overrepresented gene sets were those that showed FDR < 0.05, following a hypergeometric test, and a minimum of two overlapping genes. Curated gene sets from pathway databases in the “canonical pathways” category were preferred when available. Otherwise, Gene Ontology biological processes (GO_BPs) or any other available category (including GWAS Catalog trait associations) were taken. For GTEx-based enriched tissues of expression, as our focus is on immune-brain relationships, we kept only those enrichments corresponding to brain expression, as these are the most relevant tissues for the analysis of Li response and clinical features of BP.
In addition, the relative importance for (dichotomous) Li response of the calculated PGSs in “GWAS1” was assessed through a machine learning (ML) screening approach using the Auto Model extension of RapidMiner Studio. This applied various classification algorithms to the raw PGS data. Auto Model provides the following models: Naïve Bayes, Generalized Linear Model, Logistic Regression, Fast Large Margin, Deep Learning, Decision Tree, Random Forest, Gradient Boosted Trees and Support Vector Machines. Because ML algorithms are sensitive to class imbalance, an equal number of responder and non-responder individuals were randomly selected for the analysis (N = 657) using the sample method of the Python’s Pandas library. The resulting file with balanced classes was used as input for the ML screening in Auto Model using default parameters for all algorithms, which included split validation with stratified sampling, where the sample was randomly divided into training (60%) and test (40%) sets. Given that different types of ML algorithms can differ in their feature selection procedure due to their inherent characteristics, here, features were considered important for Li response, with either a positive (i.e., favoring response) or a negative (i.e., favoring non-response) effect, when at least two algorithms selected the same feature with the same effect direction as important for the classification task.
Results
After excluding individuals with missing phenotypic data (age and/or AAO), the effective sample sizes for the association analyses in ConLi+Gen were 853 and 1258 in “GWAS1” and “GWAS2”, respectively. A basic description of both samples is shown in Table 1. In general, there were more female than male patients in both samples and there were minimal differences in the mean ages at recruitment and disease onset between “GWAS1” and “GWAS2”. Therefore, the total sample size of our meta-analyses of Li response was 2111, including 606 (28.7%) responders and 1505 non-responders for the dichotomized variable, which included 1224 (58%) females and 887 males, with mean age 47 (±14) years and mean AAO 25 (±11) years. For the continuous Li response phenotype (i.e., Alda A score, excluding individuals with Alda B score >4), the effective sample sizes were 828 for “GWAS1” and 1044 for “GWAS2”. After the post-meta-analysis exclusion of variants with heterogeneous effects between both ConLi+Gen samples, a mean of 556,196 SNPs remained in each set of summary statistics. This was higher for the continuous phenotype, in which 625,818 SNPs remained.
Table 1.
Description of the ConLi+Gen samples.
| Responders (Total Alda ≥ 7) | Non-responders (Total Alda < 7) | Total | |
|---|---|---|---|
| GWAS1 | |||
| N Effective sample (% from total) | 297 (34.8) | 556 (65.2) | 853 |
| N Females (%) | 178 (59.9) | 337 (60.6) | 515 (60.4) |
| Age (mean ± SD) | 52 ± 14 | 46 ± 14 | 48 ± 14 |
| Age-at-onset (mean ± SD) | 28 ± 11 | 23 ± 11 | 25 ± 11 |
| # Depressive episodes (mean) | 5 | 7 | 6 |
| # Hypomanic episodes (mean) | 2 | 6 | 4 |
| # Manic episodes (mean) | 4 | 6 | 5 |
| N Psychosis cases (%) | 72 (24.2) | 270 (48.6) | 342 (40.1) |
| N Alcohol abuse cases (%) | 18 (6.1) | 122 (21.9) | 140 (16.4) |
| N Substance abuse cases (%) | 30 (10.1) | 105 (18.9) | 135 (15.8) |
| N Suicidal ideation cases (%) | 75 (25.3) | 256 (46.0) | 331 (38.8) |
| GWAS2 | |||
| N Effective sample (% from total) | 309 (24.6) | 949 (75.4) | 1258 |
| Females (%) | 157 (50.8) | 552 (58.2) | 709 (56.4) |
| Age (mean ± SD) | 48 ± 15 | 46 ± 13 | 47 ± 14 |
| Age-at-onset (mean ± SD) | 25 ± 10 | 25 ± 11 | 25 ± 11 |
Immune-related genes showed modest associations with response to Li treatment in BP
We found no associations with Li response at the genome-wide GWAS threshold (p < 5 × 10−8). At the suggestive threshold for GWAS (p < 1 × 10−5), the dichotomous Li response phenotype and Alda B (total) showed associations with FAT3 (best SNP: rs4313539, p = 2.1 × 10−6, z = 4.744), and with ADAMTS5 (best SNP: rs162501, p = 9.18 × 10−7, z = 4.909) and GRID2 (best SNP: rs62312225, p = 2.71 × 10−6, z = 4.692), respectively (Supplementary File 2: Table 1).
At the exploratory threshold (p < 1 × 10−4), when considering linkage disequilibrium (LD), we identified between 9 and 12 genomic loci in relation with different aspects of Li response (Supplementary File 2: Table 1). The top SNPs from the analyses of the dichotomous and continuous phenotypes mapped to FAT3 and BMPR1A, respectively (Table 2). In total, 42 genes were linked to the response to Li in patients with BP from our exploratory analyses in the ConLi+Gen cohort (Supplementary File 3: Table 1). There was a number of gene-based overlaps between different aspects of Li response, particularly between the dichotomous variable and total Alda score, and between the continuous variable and the other Alda variables.
Table 2.
Summary findings from the genetic association meta-analyses of Li responses in ConLi+Gen.
| Meta-analysis summary | Response vs. No-response | Continuous Li response |
|---|---|---|
| # SNPs after QC | 557,037 | 625,818 |
| # SNPs p < 0.05 | 27,426 | 31,489 |
| # SNPs p < 1 × 10−4 | 124 | 33 |
| # Lead SNPs | 11 | 11 |
| Top lead SNP | rs4313539 | rs12776537 |
| Effect allele | C | A |
| p value | 2.1 × 10−6 | 2.5 × 10−5 |
| Z | 4.7 | −4.2 |
| Gene | FAT3 | BMPR1A |
| # SNPs p < 1 × 10−5 | 15 | 0 |
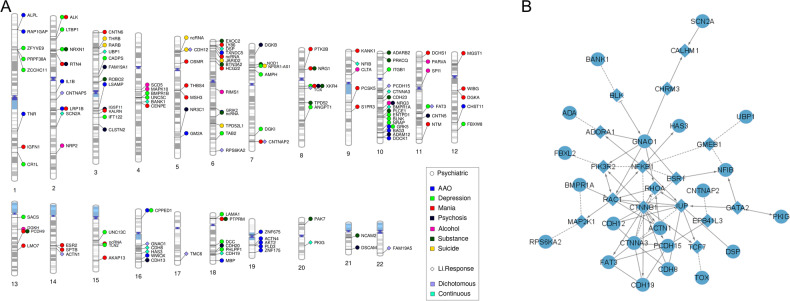
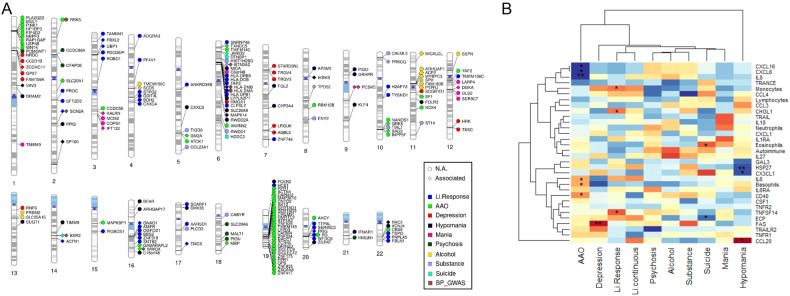
Twenty-four ImmuneSet genes were linked to the primary Li response phenotypes (i.e., dichotomous and continuous) in our exploratory analyses (Fig. 1A). These were used as input for a network analysis to facilitate biological interpretation of the findings. This network analysis provided known and predicted functional interactions between a subset of 21 input genes from our exploratory association results and 16 linkers drawn from the total of protein-coding genes in the background reference of the ReactomeFiViz app (Fig. 1B). Functional analysis of the network showed an overrepresentation (FDR < 0.05) of crucial developmental pathways and regulatory networks, including processes such as assembly and stability of the cell-cell signaling machinery (e.g., adherens junction, E-cadherin signaling, focal adhesion, integrin signaling, L1 cell adhesion molecule signaling), neuronal development and function (e.g., neurotrophic signaling, lysophosphatidic acid receptor mediated events, regulation of pluripotency, Wnt signaling), as well as activation of inflammatory (e.g., sphingolipid signaling, S1P pathways, toll-like receptor signaling) and adaptive immune pathways (e.g., T and B cell receptor signaling). Interestingly, processes such as angiogenesis, long-term potentiation, thyroid hormone signaling pathways, melanogenesis and sensory processing were also overrepresented in our network analysis (Supplementary File 3: Table 2). When eQTL genes were incorporated into the analysis, there was a marked overrepresentation of inflammatory and autoimmune disease pathways (e.g., asthma, type 1 diabetes mellitus, autoimmune thyroid disease, inflammatory bowel disease), and of vitamin D metabolism. The Wnt signaling, cell adhesion and adaptive immune pathways remained overrepresented (data not shown). All protein-coding eQTL genes annotated for Li response phenotypes are shown in Fig. 2A.
Fig. 1. Exploratory findings for the ImmuneSet in ConLi+Gen.
A Gene-based phenogram of associations of the ImmuneSet with Li response and clinical features in ConLi+Gen. B Protein-protein interaction network of Li response phenotype associations in the ImmuneSet. Circles represent input genes and diamonds represent linker genes. Dotted lines denote predicted interactions.
Fig. 2. Results of eQTL annotation and PGS association testing.
A Gene-based phenogram of eQTL annotations for the exploratory-level findings of the ImmuneSet in ConLi+Gen. Those eQTL genes that were different from the mapped gene and those that were the same are presented in circle and diamond shapes, respectively. Only protein-coding genes are shown. In addition, overlaps with BP genetic associations reported in the GWAS Catalog are presented. B Exploratory findings from the association analyses of immune-related polygenic scores and BP phenotypes in ConLi+Gen “GWAS1”. The heatmap shows the estimates (scaled by column) obtained for each PGS-phenotype pair. Increasing color darkness alludes to increasing effect, with red and blue colors representing positive and negative values, respectively. *p < 0.05, **p < 0.01.
Immune-related genes showed modest associations with clinical phenotypes in BP
The association analyses of the ImmuneSet with specific clinical features that were available for the “GWAS1” sample showed no associations at the genome-wide GWAS threshold. However, at the suggestive GWAS threshold there were, collectively, 100 associations between the ImmuneSet and AAO (3), number of depressive (54) and manic (14) episodes, and the presence of psychosis (1), substance use disorder (15) and/or suicidal ideation (13). These covered 17 genes that associated to specific clinical features (i.e., no overlaps were observed at this threshold; Table 3).
Table 3.
Summary of findings from the association analyses of the ImmuneSet with clinical characteristics in the ConLi+Gen “GWAS1” sample.
| Phenotype | N | Exploratory threshold (p < 1e−4) | Suggestive GWAS threshold (p < 1e−5) | Top gene | ||||
|---|---|---|---|---|---|---|---|---|
| # SNPs | # Genes | # SNPs | # Genes | Genes | Symbol | p val | ||
| Age-at-onset | 853 | 54 | 21 | 3 | 2 | GRK5, PLD3 | GRK5 | 3.9 × 10−6 |
| # Depressive episodes | 692 | 107 | 31 | 54 | 6 | BLNK, PHLPP1, ZCCHC11, SACS, CPPED1, PRPF38A | BLNK | 1.7 × 10−7 |
| # Manic episodes | 665 | 116 | 32 | 14 | 4 | CNTN6, KALRN, LY86, PTK2B | CNTN6 | 2.4 × 10−6 |
| Psychosis | 692 | 45 | 13 | 1 | 1 | DSCAM | DSCAM | 7.6 × 10−6 |
| Alcohol abuse | 835 | 29 | 9 | 0 | 0 | – | SCD5 | 1.8 × 10−5 |
| Substance abuse | 832 | 78 | 17 | 15 | 3 | TPD52, NOD1, XKR4 | TPD52 | 4.5 x 10−7 |
| Suicidal ideation | 660 | 30 | 7 | 13 | 1 | JARID2 | JARID2 | 3.9 × 10−6 |
When we moved forward to the exploratory analysis, we identified 786 SNP-phenotype associations in total (Supplementary File 2: Tables 2–9). These involved 166 immune-related genes (Fig. 1A and Supplementary File 3: Table 1) mostly involved in adaptive immunity and inflammation. Beyond their immune functions, according to our functional analyses, these genes play important roles in the development of the nervous system, signal transduction, synaptic processes and cell adhesion (Supplementary File 3: Tables 3–9). In particular, large numbers of associations were suggested for AAO and mood episodes (Table 3). In addition, 156 eQTL genes were collectively annotated for these phenotypes. Figure 2A shows the protein-coding eQTL genes annotated for each clinical feature. These showed no overlaps among the clinical phenotypes. Nevertheless, there were some overlaps with the ImmuneSet genes given that, in some instances, the eQTL gene corresponded to the gene mapped to the variant while, in others, the eQTL gene was different from the mapped gene. A summary of exploratory findings for each clinical phenotype studied can be found in the Supplementary File 1: Supplementary Results.
Immune-related genes showed pleiotropy for BP phenotypes
A number of genes showed shared associations with the different phenotypes included in our exploratory ImmuneSet analyses in ConLi+Gen (Fig. 1A). These genes can be prioritized for follow-up studies due to their pleiotropic effects in Li response, clinical features, or both. In this way, we prioritized 21 genes linked with more than one BP phenotype in our exploratory analyses (Table 4). Here, we excluded genes linked to Alda A, total Alda B and/or Total Alda when there was no overlap with the dichotomous and/or continuous Li response phenotypes. However, a complete list of corresponding gene-phenotype exploratory findings (197 in total) is shown in Supplementary File 3: Table 1. Five of the prioritized genes (CNTNAP5, DSP, NFIB, BMPR1A, and HAS3) were associated with multiple Li response phenotypes, 10 of them (XKR4, NRXN1, RTN4, NRG1/3, ALK, GRK5, LRP1B, NPSR1-AS1 and CPPED1) were associated with multiple clinical features, and another six genes (BANK1, ROBO2, CNTNAP2, PCDH9, CDH12 and FAT3) were associated with Li response as well as with clinical features.
Table 4.
Prioritized ImmuneSet candidate genes for Li response and clinical characteristics in ConLi+Gen.
| Gene | Chr | Start | End | Priority | Phenotypes |
|---|---|---|---|---|---|
| ALK | 2 | 29415640 | 30144432 | Psychiatric | Depression, Mania |
| NRXN1 | 2 | 50145643 | 51259674 | Psychiatric | Depression, Hypomania, Substance |
| RTN4 | 2 | 55199325 | 55339757 | Psychiatric | Mania, Psychosis |
| CNTNAP5 | 2 | 124025287 | 124915287 | Li response | LiResponse, Alda_B, Alda_Total |
| LRP1B | 2 | 140988992 | 142889270 | Psychiatric | AAO, Mania |
| ROBO2 | 3 | 75906695 | 77649964 | Both | Alda_Total, Hypomania, Substance |
| BANK1 | 4 | 101411286 | 102074812 | Both | Continuous.LiResp, Alda_A, Alda_B, Alda_Total, Hypomania |
| CDH12 | 5 | 21750673 | 22853622 | Both | LiResponse, Suicide |
| DSP | 6 | 7541575 | 7586717 | Li response | Continuous.LiResp, Alda_Total |
| NPSR1-AS1 | 7 | 34386124 | 34911194 | Psychiatric | Depression, Suicide |
| CNTNAP2 | 7 | 146116002 | 148420998 | Both | LiResponse, Alda_Total, Mania |
| NRG1 | 8 | 31496902 | 32622548 | Psychiatric | Mania, Substance |
| XKR4 | 8 | 56014949 | 56454613 | Psychiatric | Depression, Mania, Psychosis, Substance |
| NFIB | 9 | 14081843 | 14398983 | Li response | Continuous.LiResp, Alda_B |
| NRG3 | 10 | 83635070 | 84746935 | Psychiatric | Alcohol, Psychosis |
| BMPR1A | 10 | 86756601 | 86932838 | Li response | Continuous.LiResp, Alda_A |
| GRK5 | 10 | 120967101 | 121215131 | Psychiatric | AAO, Depression |
| FAT3 | 11 | 92352096 | 92896470 | Both | LiResponse, Alda_Total, Depression |
| PCDH9 | 13 | 66302834 | 67230445 | Both | Alda_B, Mania, Substance |
| CPPED1 | 16 | 12756919 | 12897874 | Psychiatric | AAO, Depression |
| HAS3 | 16 | 69105564 | 69118719 | Li response | Continuous.LiResp, Alda_A, Alda_Total |
Polygenic scores for immune-related traits weakly associated with BP phenotypes
In addition to testing associations of the ImmuneSet with BP phenotypes, we calculated a set of 32 previously published immune-related PGSs, namely for: (1) (general) autoimmune disease, (2) the proportions of white blood cell populations and (3) inflammatory marker levels in serum (Supplementary File 3: Table 10). The overlap of variants between the PGS weight files obtained from PGS Catalog and the SNPs available in our ConLi+Gen “GWAS1” sample was, in general, better for the serum levels of inflammatory markers (80.6% in average) than for the other PGSs. The lowest valid SNP overlap was observed for the PGS of general autoimmune disease (38.8%). For the proportion of white blood cell populations, the valid SNP overlap was also not fully satisfactory (49.4% in average). Results from these analyses should be interpreted with caution, as the calculated PGSs may poorly index autoimmune disease and the proportion of white blood cell signatures.
We identified 15 PGS nominal (p < 0.05) associations with BP phenotypes (Fig. 2B): six with AAO (basophils, CD40, CXCL6/16, IL-6/8), three with the number of episodes of hypomania (CCL20, CX3CL1, HSP27) and Li response (monocytes, CHI3L1, TNFSF14), two with the presence of suicidal ideation (eosinophils, ECP), and one with the number of depressive episodes (FAS). However, none of these survived correction for multiple comparisons (Supplementary File 3: Table 10).
Finally, ML-based PGS ranking for the dichotomized Li response suggested relative importance of serum markers of inflammation such as ECP, HSP27, CHI3L1, TRAILR2 and TNFSF14 for the prediction of responses to Li treatment in ConLi+Gen (Supplementary File 1: Fig. S3).
Discussion
There is apparent mounting evidence of immune dysregulation in BP and other major psychiatric diseases. Nevertheless, some observations have originated from underpowered studies, resulting in a lack of reproducibility [3]. Therefore, it becomes crucial to gain a better understanding of the relationships between the immune and central nervous systems, and to discern between causes and consequences of disease. With this in mind, we sought to investigate how genetic factors relevant to immune activity relate to disease phenotypes, such as response to Li treatment, AAO and psychiatric symptoms, in patients with BP. Using an exploratory and extensive candidate gene approach, our study suggested various genes and inflammatory markers that appeared to represent potential pleiotropic factors with modest contributions to multiple BP phenotypes. However, we should note that, here, we refer to pleiotropy as the (suggested) association with multiple traits in the ConLi+Gen cohort and, by no means, have we implied that these features are independent from each other. In fact, it should be expected that, given the important correlation between psychiatric disorders, the features that we have studied in ConLi+Gen are, to some extent, also correlated with each other. Additionally, because genes can play different roles in different tissues and cell types, we observed widespread enrichments of biological pathways participating in the development and function of the brain. This suggested that the genes contributing to shape BP phenotypes might affect in parallel both the immune and nervous systems. Nevertheless, because we found no associations at the genome-wide GWAS threshold, and those observed at the suggestive GWAS threshold were limited, our findings are also consistent with a relatively weak effect of immune genetic factors over BP phenotypes.
The results of our exploratory assessment of associations of genetic polymorphisms in immune-related genes with Li response in the ConLi+Gen cohort suggest that variations in multiple inflammatory and adaptive immune processes might modestly contribute to the response to Li treatment in patients with BP. Importantly, our network and gene set enrichment analyses localized these modest contributions to numerous biological pathways that participate in cell adhesion, migration and intercellular communication, which help in the development and maintenance of the central and peripheral nervous systems, as well as of the immune and vascular systems. Interestingly, many of these processes appear to converge in the participation of GSK-3β (glycogen synthase kinase-3 beta), as assessed through comparative overlap analysis of the enriched KEGG and Reactome gene sets. GSK-3β is involved in multiple major developmental pathways, such as the Wnt, Notch and Hedgehog signaling pathways. Genetic manipulation in mouse models has shown an antidepressant-like behavior upon GSK-3β knockdown in hippocampus, as well as cognitive, behavioral and biochemical changes associated with psychiatric disorders, including Alzheimer’s disease, BP and schizophrenia, upon GSK-3β overexpression [31]. Li possesses a well-known inhibitory effect over GSK-3β [32]. Therefore, our analyses suggest that GSK-3β might be a relevant player in the biological response to Li treatment in BP. Our findings are also in agreement with other epidemiological and molecular investigations of Li effects. For example, we observed overrepresentation of various gene sets related to thyroid function, such as thyroid-stimulating hormone signaling and autoimmune thyroid disease. This is in line with the reports of a reversible association of Li treatment with hypothyroidism, particularly in women [33, 34].
Taken together, the encouraging literature supporting our exploratory findings sparked our interest in evaluating how a genetic measure (PGS) of immune-relevant traits, such as inflammatory marker levels in serum and the proportion of white blood cells, might associate with Li response in ConLi+Gen. Here, we observed only weak statistical associations. However, one might consider these results inconclusive given the limited overlap between PGS weight variants and our ConLi+Gen dataset. Moreover, it must be kept in mind that PGSs have an incomplete indexing of the trait and, in this case, do not reflect the real levels of inflammation markers present in the serum of these patients. Considering this, we adopted a different approach to explore the relationship between PGSs and the dichotomous Li response in ConLi+Gen. Here, we used RapidMiner’s Auto Model to probe various ML algorithms and extract the relative importance of each PGS to predict Li response. Given the PGS complications mentioned above and the well-known fitting issues arising from the use of small sample sizes in predictive modeling, we expected a relatively poor overall performance of the PGS model and, hence, we were not looking to evaluate predictive value. Indeed, the accuracy of the tested algorithms was only 43–56% (data not shown). These observations should be interpreted with caution due to the relatively low robustness of split validation in assessing model performance compared to other validation approaches used in predictive ML. Nevertheless, applied for feature importance ranking, this ML approach had the advantage of providing information on the PGS relationships with Li response when compared to one another.
The results of our exploratory assessment of associations of genetic polymorphisms in the ImmuneSet genes with BP’s AAO, numbers of mood episodes and psychiatric comorbidities in ConLi+Gen identified various genes potentially contributing to mood episodes and substance abuse, including XKR4, NRXN1, GRK5 and NRG1/3. These genes, besides their immune-related functionalities, seem to play important roles in neuronal development and function, according to our gene set enrichment analyses. Indeed, this could be corroborated by the literature in many instances. For example, NRXN1, a cell surface protein involved in cell-cell interactions, exocytosis of secretory granules and regulation of signal transmission, has been associated with autism, schizophrenia and nicotine dependence [35]. GRK5 has a role in the regulation of motility in polymorphonuclear leukocytes and inflammation [36, 37]. It also regulates the activity of various G-protein coupled receptors, including neurotransmitter receptors [38]. XKR4, a phospholipid scramblase strongly expressed in brain tissue and activated by caspases, has been suggested to participate in the remodeling of neural networks by triggering microglial responses to the exposure of phosphatidylserine on axons, dendrites and synapses [39].
It is worth noting that three of our potential candidate genes for depressive episodes have previously shown associations with either major depression at the gene-level (DCC) [40] or mapped to schizophrenia loci (CR1L and DGKI) [41] in large GWASs. Moreover, one of our suggested candidates for manic episodes, ESR2, and one for substance use disorder, BTN3A2, were previously associated at the gene-level with major depression in the large GWAS, while one of our candidates for hypomanic episodes and alcohol dependence, the BP-associated RIMS1 [26], mapped previously to schizophrenia loci. This, together with the overlaps with reported BP-associated genes that we observed, particularly concerning known eQTL genes, provides some support to the validity of our exploratory findings.
Finally, even when our assessment of PGS associations with clinical features resulted only in nominal associations that did not survive correction for multiple testing, we might (cautiously) draw a few interesting observations and new hypotheses for further exploration. For example, that activation of macrophages and neutrophils, reflected by the potential links with the PGSs for cytokines and chemokines produced by or targeting these cells (e.g., interleukin-6/8, CXCL6/16), might contribute to disease AAO in ConLi+Gen. These observations might be supported by studies that found increases in neutrophil counts in psychiatric disorders, including BP [42, 43], as well as association of genetic polymorphisms in interleukin-1β, a pro-inflammatory cytokine produced by activated immune cells, including neutrophils and macrophages, with age of onset of depression in geriatric patients [44]. In addition, if we consider that macrophage/neutrophil activation was also a suggested mechanism of Li response in our study, it would be easy to speculate that activation of these cells might be linked with some aspect of the disease onset.
In conclusion, we performed an exploratory study that suggests a modest relationship between immunity and clinically relevant BP phenotypes at the genetic level and identified various interesting potential candidates for follow-up studies. We acknowledge that our study was limited by a relatively small sample size, particularly for the episodes of hypomania, and by incomplete overlap between the variants in the PGSs and our ConLi+Gen dataset, likely resulting from a limited overlap among the different SNP arrays initially used to genotype samples in different collection centers. Moreover, although regulatory regions were out of the scope of our study due to their high complexity for interpretation, we acknowledge that restricting our analyses to the gene’s boundaries excluded potentially interesting regulatory SNPs involved in Li response and BP characteristics. Finally, aware that the inclusion of East Asian subsamples in our genetic analyses might rise some concerns, we performed a sensitivity analysis by excluding East Asian individuals from the genetic association tests of primary Li response phenotypes (data not shown). The QCed meta-analysis results of both dichotomous (Pearson r = 0.975) and continuous (Pearson r = 0.941) Li response variables performed with and without East Asian samples were highly correlated. Because we expected mild differences between analyses due to the loss in sample size, these results suggested that any potential bias that could be attributed to the different ancestries was addressed in our analyses. Despite the inherent limitations and the modest significance of our findings, we believe that our study provides plausible biological insights that might further the understanding of immune contributions to BP. Further studies are needed to elucidate if and how immune regulation might represent a feasible strategy to improve the symptomatology and treatment response in patients with BP.
Supplementary information
Author contributions
MHR planned the study, processed and analyzed the data, and prepared the manuscript. KGF performed the machine learning screenings. BTB conceived the study and critically revised the manuscript. All ConLi+Gen members contributed clinical and genetic data. All authors provided overall feedback on the manuscript.
Funding
The project received funding from the program “Profilbildung 2020”, an initiative of the Ministry of Culture and Science of the State of North Rhine Westphalia. The sole responsibility for the content of this publication lies with the authors. The primary sources of funding for ConLi+Gen were grants RI 908/7-1, FOR2107 and RI 908/11-1 from the Deutsche Forschungsgemeinschaft (Marcella Rietschel) and grant No. 246/10-1 (Markus M. Nöthen) and grant ZIA-MH00284311 from the Intramural Research Program of the National Institute of Mental Health (ClinicalTrials.gov identifier: NCT00001174). The genotyping was funded in part by the German Federal Ministry of Education and Research through the Integrated Network IntegraMent (Integrated Understanding of Causes and Mechanisms in Mental Disorders), under the auspices of the e:Med Programme (Thomas G. Schulze, Marcella Rietschel and Markus M. Nöthen). The Canadian part of the study was supported by grant #166098 from the Canadian Institutes of Health Research and by a grant from Genome Atlantic/Research Nova Scotia (Martin Alda). Collection and phenotyping of the Australian University of New South Wales sample was funded by Program Grant 1037196 from the Australian National Health and Medical Research Council (Philip B. Mitchell, Peter R. Schofield, Janice M. Fullerton), and acknowledges support from Lansdowne Foundation, Betty Lynch OAM (dec) and the Janette Mary O’Neill Fellowship. Azmeraw T. Amare is supported by the 2019–2021 National Alliance for Research on Schizophrenia and Depression (NARSAD) Young Investigator Grant from the Brain & Behaviour Research Foundation (BBRF) and National Health and Medical Research Council (NHMRC) Emerging Leadership Investigator Grant 2021–2008000. The collection of the Barcelona sample was supported by grants PI080247, PI1200906, PI12/00018, 2014SGR1636, 2014SGR398, and MSII14/00030 from the Centro de Investigación en Red de Salud Mental, Institut d’Investigacions Biomèdiques August Pi i Sunyer, the Centres de Recerca de Catalunya Programme/Generalitat de Catalunya, and the Miguel Servet II and Instituto de Salud Carlos III. The Swedish Research Council, the Stockholm County Council, Karolinska Institutet and the Söderström-Königska Foundation supported this research through grants awarded to Lena Backlund, Louise Frisen, Catharina Lavebratt and Martin Schalling. The collection of the Geneva sample was supported by grants Synapsy–The Synaptic Basis of Mental Diseases 51NF40-158776 and 32003B-125469 from the Swiss National Foundation. The work by the French group was supported by INSERM (Institut National de la Santé et de la Recherche Médicale), AP-HP (Assistance Publique des Hôpitaux de Paris), the Fondation FondaMental (RTRS Santé Mentale), and the labex Bio-PSY (Investissements d’Avenir program managed by the ANR under reference ANR-11-IDEX-0004-02). The collection of the Romanian sample was supported by a grant from UEFISCDI, Bucharest, Romania (grants PCCA-89/2012; PCE-203/2021) to Maria Grigoroiu-Serbanescu. The collection of the Czech sample was supported by the project Nr. LO1611 with a financial support from the MEYS under the NPU I program and by the Czech Science Foundation, grant Nr. 17-07070 S. Biju Viswanath is funded by the Intermediate (Clinical and PublicHealth) Fellowship (IA/CPHI/20/1/505266) of the DBT/Wellcome Trust India Alliance. Open Access funding enabled and organized by Projekt DEAL.
Data availability
The data that support the findings of this study are available from ConLi+Gen, but restrictions apply to their availability.
Competing interests
Eduard Vieta has received grants and served as consultant, advisor or CME speaker for the following entities: AB-Biotics, Abbvie, Almirall, Allergan, Angelini, AstraZeneca, Bristol-Myers Squibb, Dainippon Sumitomo Pharma, Farmindustria, Ferrer, Forest Research Institute, Gedeon Richter, GH Research, Glaxo-Smith-Kline, Janssen, Lundbeck, Orion, Otsuka, Pfizer, Roche, Rovi, Sanofi-Aventis, Servier, Shire, Sunovion, Takeda, the Brain and Behaviour Foundation, the Spanish Ministry of Science and Innovation (CIBERSAM), the Stanley Medical Research Institute and Viatris. Michael Bauer has received grants from the Deutsche Forschungsgemeinschaft (DFG), and Bundesministeriums für Bildung und Forschung (BMBF), and served as consultant, advisor or CME speaker for the following entities: Allergan, Aristo, Janssen, Lilly, Lundbeck, neuraxpharm, Otsuka, Sandoz, Servier and Sunovion outside the submitted work. Sarah Kittel-Schneider has received grants and served as consultant, advisor or speaker for the following entities: Medice Arzneimittel Pütter GmbH and Takeda. Bernhard T. Baune has received grants and served as consultant, advisor or CME speaker for the following entities: AstraZeneca, Bristol-Myers Squibb, Janssen, Lundbeck, Otsuka, Servier, the National Health and Medical Research Council, the Fay Fuller Foundation, the James and Diana Ramsay Foundation. Tadafumi Kato received honoraria for lectures, manuscripts, and/or consultancy, from Kyowa Hakko Kirin Co, Ltd, Eli Lilly Japan K.K., Otsuka Pharmaceutical Co, Ltd, GlaxoSmithKline K.K., Taisho Toyama Pharmaceutical Co, Ltd, Dainippon Sumitomo Pharma Co, Ltd, Meiji Seika Pharma Co, Ltd, Pfizer Japan Inc., Mochida Pharmaceutical Co, Ltd, Shionogi & Co, Ltd, Janssen Pharmaceutical K.K., Janssen Asia Pacific, Yoshitomiyakuhin, Astellas Pharma Inc, Wako Pure Chemical Industries, Ltd, Wiley Publishing Japan, Nippon Boehringer Ingelheim Co Ltd, Kanae Foundation for the Promotion of Medical Science, MSD K.K., Kyowa Pharmaceutical Industry Co, Ltd and Takeda Pharmaceutical Co, Ltd. Tadafumi Kato also received a research grant from Takeda Pharmaceutical Co, Ltd. Peter Falkai has received grants and served as consultant, advisor or CME speaker for the following entities Abbott, GlaxoSmithKline, Janssen, Essex, Lundbeck, Otsuka, Gedeon Richter, Servier and Takeda as well as the German Ministry of Science and the German Ministry of Health. Eva Reininghaus has received grants and served as consultant, advisor or CME speaker for the following entities: Janssen and Institut Allergosan. Mikael Landén has received lecture honoraria from Lundbeck. Kazufumi Akiyama has received consulting honoraria from Taisho Toyama Pharmaceutical Co, Ltd. Scott R. Clark has received grants and served as consultant, advisor or CME speaker for the following entities: Otsuka Austalia, Lundbeck Australia, Janssen-Cilag Australia, Servier Australia. The rest of authors have no conflicts of interest to disclose.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A list of authors and their affiliations appears at the end of the paper.
Contributor Information
Bernhard T. Baune, Email: Bernhard.Baune@ukmuenster.de
International Consortium on Lithium Genetics (ConLi+Gen):
Anbupalam Thalamuthu, Azmeraw T. Amare, Mazda Adli, Kazufumi Akiyama, Nirmala Akula, Raffaella Ardau, Bárbara Arias, Jean-Michel Aubry, Lena Backlund, Frank Bellivier, Antonio Benabarre, Susanne Bengesser, Abesh Kumar Bhattacharjee, Joanna M. Biernacka, Armin Birner, Micah Cearns, Pablo Cervantes, Hsi-Chung Chen, Caterina Chillotti, Sven Cichon, Scott R. Clark, Francesc Colom, Cristiana Cruceanu, Piotr M. Czerski, Nina Dalkner, Franziska Degenhardt, Maria Del Zompo, J. Raymond DePaulo, Bruno Etain, Peter Falkai, Ewa Ferensztajn-Rochowiak, Andreas J. Forstner, Josef Frank, Louise Frisén, Mark A. Frye, Janice M. Fullerton, Carla Gallo, Sébastien Gard, Julie S. Garnham, Fernando S. Goes, Maria Grigoroiu-Serbanescu, Paul Grof, Ryota Hashimoto, Roland Hasler, Joanna Hauser, Urs Heilbronner, Stefan Herms, Per Hoffmann, Liping Hou, Yi-Hsiang Hsu, Stéphane Jamain, Esther Jiménez, Jean-Pierre Kahn, Layla Kassem, Tadafumi Kato, John Kelsoe, Sarah Kittel-Schneider, Po-Hsiu Kuo, Ichiro Kusumi, Barbara König, Gonzalo Laje, Mikael Landén, Catharina Lavebratt, Marion Leboyer, Susan G. Leckband, Mario Maj, Mirko Manchia, Cynthia Marie-Claire, Lina Martinsson, Michael J. McCarthy, Susan L. McElroy, Vincent Millischer, Marina Mitjans, Francis M. Mondimore, Palmiero Monteleone, Caroline M. Nievergelt, Tomas Novák, Markus M. Nöthen, Claire O’Donovan, Norio Ozaki, Sergi Papiol, Andrea Pfennig, Claudia Pisanu, James B. Potash, Andreas Reif, Eva Reininghaus, Hélène Richard-Lepouriel, Gloria Roberts, Guy A. Rouleau, Janusz K. Rybakowski, Martin Schalling, Peter R. Schofield, Klaus Oliver Schubert, Eva C. Schulte, Barbara W. Schweizer, Giovanni Severino, Tatyana Shekhtman, Paul D. Shilling, Katzutaka Shimoda, Christian Simhandl, Claire M. Slaney, Alessio Squassina, Thomas Stamm, Pavla Stopkova, Fabian Streit, Fasil Tekola-Ayele, Alfonso Tortorella, Gustavo Turecki, Julia Veeh, Eduard Vieta, Biju Viswanath, Stephanie H. Witt, Peter P. Zandi, Martin Alda, Michael Bauer, Francis J. McMahon, Philip B. Mitchell, Marcella Rietschel, and Thomas G. Schulze
Supplementary information
The online version contains supplementary material available at 10.1038/s41398-024-02865-4.
References
- 1.Rosenblat JD, McIntyre RS. Bipolar disorder and immune dysfunction: epidemiological findings, proposed pathophysiology and clinical implications. Brain Sci. 2017;7:144. doi: 10.3390/brainsci7110144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tylee DS, Sun J, Hess JL, Tahir MA, Sharma E, Malik R, et al. Genetic correlations among psychiatric and immune-related phenotypes based on genome-wide association data. Am J Med Genet B Neuropsychiatr Genet. 2018;177:641–57. doi: 10.1002/ajmg.b.32652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yuan N, Chen Y, Xia Y, Dai J, Liu C. Inflammation-related biomarkers in major psychiatric disorders: a cross-disorder assessment of reproducibility and specificity in 43 meta-analyses. Transl Psychiatry. 2019;9:233. doi: 10.1038/s41398-019-0570-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bauer M. Lithium: what can we do to overcome the discrepancies between evidence, guideline recommendations and clinical practice? Eur Neuropsychopharmacol. 2022;60:1–3. doi: 10.1016/j.euroneuro.2022.03.007. [DOI] [PubMed] [Google Scholar]
- 5.Rybakowski JK. Lithium. Eur Neuropsychopharmacol. 2022;57:86–7. doi: 10.1016/j.euroneuro.2022.01.111. [DOI] [PubMed] [Google Scholar]
- 6.Spuch C, López-García M, Rivera-Baltanás T, Rodrígues-Amorím D, Olivares JM. Does lithium deserve a place in the treatment against COVID-19? A preliminary observational study in six patients, case report. Front Pharm. 2020;11:557629. doi: 10.3389/fphar.2020.557629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Landén M, Larsson H, Lichtenstein P, Westin J, Song J. Respiratory infections during lithium and valproate medication: a within-individual prospective study of 50,000 patients with bipolar disorder. Int J Bipolar Disord. 2021;9:4. doi: 10.1186/s40345-020-00208-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nassar A, Azab AN. Effects of lithium on inflammation. ACS Chem Neurosci. 2014;5:451–8. doi: 10.1021/cn500038f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Queissner R, Lenger M, Birner A, Dalkner N, Fellendorf F, Bengesser S, et al. The association between anti-inflammatory effects of long-term lithium treatment and illness course in bipolar disorder. J Affect Disord. 2021;281:228–34. doi: 10.1016/j.jad.2020.11.063. [DOI] [PubMed] [Google Scholar]
- 10.Manchia M, Adli M, Akula N, Ardau R, Aubry JM, Backlund L, et al. Assessment of response to lithium maintenance treatment in bipolar disorder: a Consortium on Lithium Genetics (ConLiGen) Report. PLoS ONE. 2013;8:e65636. doi: 10.1371/journal.pone.0065636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nunes A, Trappenberg T, Alda M, International Consortium on Lithium Genetics (ConLiGen). Asymmetrical reliability of the Alda score favours a dichotomous representation of lithium responsiveness. PLoS ONE. 2020;15:e0225353. doi: 10.1371/journal.pone.0225353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.International Consortium on Lithium Genetics (ConLi+Gen), Amare AT, Schubert KO, Hou L, Clark SR, Papiol S, et al. Association of polygenic score for schizophrenia and HLA antigen and inflammation genes with response to lithium in bipolar affective disorder: a genome-wide association study. JAMA Psychiatry. 2018;75:65–74. [DOI] [PMC free article] [PubMed]
- 13.Le Clerc S, Lombardi L, Baune BT, Amare AT, Schubert KO, Hou L, et al. HLA-DRB1 and HLA-DQB1 genetic diversity modulates response to lithium in bipolar affective disorders. Sci Rep. 2021;11:17823. [DOI] [PMC free article] [PubMed]
- 14.Schulze TG, Alda M, Adli M, Akula N, Ardau R, Bui ET, et al. The International Consortium on Lithium Genetics (ConLiGen): an initiative by the NIMH and IGSLI to study the genetic basis of response to lithium treatment. Neuropsychobiology. 2010;62:72–8. doi: 10.1159/000314708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hou L, Heilbronner U, Degenhardt F, Adli M, Akiyama K, Akula N, et al. Genetic variants associated with response to lithium treatment in bipolar disorder: a genome-wide association study. Lancet. 2016;387:1085–93. doi: 10.1016/S0140-6736(16)00143-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liberzon A, Subramanian A, Pinchback R, Thorvaldsdóttir H, Tamayo P, Mesirov JP. Molecular signatures database (MSigDB) 3.0. Bioinformatics. 2011;27:1739–40. doi: 10.1093/bioinformatics/btr260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Breuer K, Foroushani AK, Laird MR, Chen C, Sribnaia A, Lo R, et al. InnateDB: systems biology of innate immunity and beyond—recent updates and continuing curation. Nucleic Acids Res. 2013;41:D1228–33. doi: 10.1093/nar/gks1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schubert KO, Thalamuthu A, Amare AT, Frank J, Streit F, Adl M, et al. Combining schizophrenia and depression polygenic risk scores improves the genetic prediction of lithium response in bipolar disorder patients. Transl Psychiatry. 2021;11:606. doi: 10.1038/s41398-021-01702-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Das S, Forer L, Schönherr S, Sidore C, Locke AE, Kwong A, et al. Next-generation genotype imputation service and methods. Nat Genet. 2016;48:1284–7. doi: 10.1038/ng.3656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meyer HV. plinkQC: genotype quality control in genetic association studies. 2020. 10.5281/zenodo.3934294.
- 21.Lambert SA, Gil L, Jupp S, Ritchie SC, Xu Y, Buniello A, et al. The Polygenic Score Catalog as an open database for reproducibility and systematic evaluation. Nat Genet. 2021;53:420–5. doi: 10.1038/s41588-021-00783-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weissbrod O, Kanai M, Shi H, Gazal S, Peyrot WJ, Khera AV, et al. Leveraging fine-mapping and multipopulation training data to improve cross-population polygenic risk scores. Nat Genet. 2022;54:450–8. doi: 10.1038/s41588-022-01036-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu Y, Vuckovic D, Ritchie SC, Akbari P, Jiang T, Grealey J, et al. Machine learning optimized polygenic scores for blood cell traits identify sex-specific trajectories and genetic correlations with disease. Cell Genom. 2022;2:100086.. doi: 10.1016/j.xgen.2021.100086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Folkersen L, Gustafsson S, Wang Q, Hansen DH, Hedman ÅK, Schork A, et al. Genomic and drug target evaluation of 90 cardiovascular proteins in 30,931 individuals. Nat Metab. 2020;2:1135–48. doi: 10.1038/s42255-020-00287-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chang CC, Chow CC, Tellier LC, Vattikuti S, Purcell SM, Lee JJ. Second-generation PLINK: rising to the challenge of larger and richer datasets. Gigascience. 2015;4:7. doi: 10.1186/s13742-015-0047-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stahl EA, Breen G, Forstner AJ, McQuillin A, Ripke S, Trubetskoy V, et al. Genome-wide association study identifies 30 loci associated with bipolar disorder. Nat Genet. 2019;51:793–803. doi: 10.1038/s41588-019-0397-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Munz M, Wohlers I, Simon E, Reinberger T, Busch H, Schaefer AS, et al. Qtlizer: comprehensive QTL annotation of GWAS results. Sci Rep. 2020;10:20417. doi: 10.1038/s41598-020-75770-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wu G, Dawson E, Duong A, Haw R, Stein L. ReactomeFIViz: a Cytoscape app for pathway and network-based data analysis. F1000Res. 2014;3:146. doi: 10.12688/f1000research.4431.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shannon P, Markiel A, Ozier O, Baliga NS, Wang JT, Ramage D, et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 2003;13:2498–504. doi: 10.1101/gr.1239303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Watanabe K, Taskesen E, van Bochoven A, Posthuma D. Functional mapping and annotation of genetic associations with FUMA. Nat Commun. 2017;8:1826. doi: 10.1038/s41467-017-01261-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kaidanovich-Beilin O, Woodgett JR. GSK-3: functional insights from cell biology and animal models. Front Mol Neurosci. 2011;4:40. doi: 10.3389/fnmol.2011.00040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Freland L, Beaulieu JM. Inhibition of GSK3 by lithium, from single molecules to signaling networks. Front Mol Neurosci. 2012;5:14. doi: 10.3389/fnmol.2012.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shine B, McKnight RF, Leaver L, Geddes JR. Long-term effects of lithium on renal, thyroid, and parathyroid function: a retrospective analysis of laboratory data. Lancet. 2015;386:461–8. doi: 10.1016/S0140-6736(14)61842-0. [DOI] [PubMed] [Google Scholar]
- 34.Lieber I, Ott M, Öhlund L, Lundqvist R, Eliasson M, Sandlund M, et al. Lithium-associated hypothyroidism and potential for reversibility after lithium discontinuation: findings from the LiSIE retrospective cohort study. J Psychopharmacol. 2020;34:293–303. doi: 10.1177/0269881119882858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ching MS, Shen Y, Tan WH, Jeste SS, Morrow EM, Chen X, et al. Deletions of NRXN1 (neurexin-1) predispose to a wide spectrum of developmental disorders. Am J Med Genet B Neuropsychiatr Genet. 2010;153B:937–47. doi: 10.1002/ajmg.b.31063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Patial S, Shahi S, Saini Y, Lee T, Packiriswamy N, Appledorn DM, et al. G-protein coupled receptor kinase 5 mediates lipopolysaccharide-induced NFκB activation in primary macrophages and modulates inflammation in vivo in mice. J Cell Physiol. 2011;226:1323–33. doi: 10.1002/jcp.22460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.de Lucia C, Grisanti LA, Borghetti G, Piedepalumbo M, Ibetti J, Lucchese AM, et al. G protein-coupled receptor kinase 5 (GRK5) contributes to impaired cardiac function and immune cell recruitment in post-ischemic heart failure. Cardiovasc Res. 2022;118:169–83. doi: 10.1093/cvr/cvab044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gurevich EV, Gurevich VV. GRKs as modulators of neurotransmitter receptors. Cells. 2020;10:52. doi: 10.3390/cells10010052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Suzuki J, Imanishi E, Nagata S. Exposure of phosphatidylserine by Xk-related protein family members during apoptosis. J Biol Chem. 2014;289:30257–67. doi: 10.1074/jbc.M114.583419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wray NR, Ripke S, Mattheisen M, Trzaskowski M, Byrne EM, Abdellaoui A, et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat Genet. 2018;50:668–81. doi: 10.1038/s41588-018-0090-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schizophrenia Working Group of the Psychiatric Genomics Consortium. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511:421–7. [DOI] [PMC free article] [PubMed]
- 42.Çakır U, Tuman TC, Yıldırım O. Increased neutrophil/lymphoctye ratio in patients with bipolar disorder: a preliminary study. Psychiatr Danub. 2015;27:180–4. [PubMed] [Google Scholar]
- 43.Singh D, Guest PC, Dobrowolny H, Vasilevska V, Meyer-Lotz G, Bernstein HG, et al. Changes in leukocytes and CRP in different stages of major depression. J Neuroinflammation. 2022;19:74. doi: 10.1186/s12974-022-02429-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hwang JP, Tsai SJ, Hong CJ, Yang CH, Hsu CD, Liou YJ. Interleukin-1 beta -511C/T genetic polymorphism is associated with age of onset of geriatric depression. Neuromolecular Med. 2009;11:322–7. doi: 10.1007/s12017-009-8078-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from ConLi+Gen, but restrictions apply to their availability.