Abstract
Anterior cruciate ligament (ACL) tears are among the most common injuries to the knee. With recent improvements in imaging that allow for more precise identification of ACL tear patterns, improved techniques for repair, and advancements in biological augmentation, there has been a re-emerging interest in primary ACL repair, especially for acute proximal ACL tears. This article aims to describe a surgical technique for primary ACL repair using a re-tensionable all-suture–based construct.
Technique Video
Anterior cruciate ligament (ACL) tears are among the most common ligamentous injuries to the knee, with a steadily increasing incidence and more than 300,000 surgical procedures performed annually in the United States alone.1,2 ACL tears are often a result of non-contact decelerating, cutting, or pivoting injuries and are most prevalent in young, athletic individuals.3 The subsequent instability and rotational laxity in an ACL-deficient knee may lead to further chondral and meniscal injury with advanced progression to osteoarthritis.4
Owing to the poor capacity of the ACL to heal, ACL tears have historically been treated with ACL reconstruction (ACLR) with autograft or allograft tissue.5 Despite the success of ACLR in restoring functional stability to the knee, over the past several decades, outcomes after ACLR have remained less than ideal, with a variety of different studies reporting high rates of donor-site morbidity, suboptimal return-to-sport (RTS) rates, and variable patient satisfaction levels.6,7 Compared with primary ACLR, revision ACLR yields outcomes that are often less predictable, with decreased rates of functional outcomes, patient satisfaction, and activity levels.8,9 Additionally, there is an increased rate of graft failure, complications, and cartilage abnormality with revision ACLR.10, 11, 12
Primary ACL repair is an alternative surgical option to address these limitations. Although open techniques for ACL repair have been described in the past, such techniques were met with high failure rates and subsequently abandoned.13 With advancements in imaging, arthroscopic surgical instrumentation and techniques, and biological augmentation, there has been a renewed interest in ACL repair for specific tear patterns in a subset of patients.13 Potential advantages of ACL repair include improved knee kinematics and proprioception, more anatomic positioning, preserved bone stock, and no donor-site morbidity from autograft harvest.14, 15, 16
Several techniques have been described with the renewed interest in ACL repair. The primary aim of this article is to describe our step-by-step technique for primary ACL repair using a re-tensionable all-suture–based construct, including high-strength nonabsorbable FiberRing sutures (Arthrex, Naples, FL) linked to an ACL-Repair TightRope implant (Arthrex) with internal brace (IB) suture augmentation. The advantages of this all-arthroscopic technique include (1) the ability to perform multiple suture passages through anteromedial and posterolateral bundles of the native ACL to allow for a more anatomic repair, (2) the use of a re-tensionable adjustable-loop design for tensioning of the ACL repair to the femoral attachment, and (3) the preservation of femoral and tibial bone stock through the use of small drill holes that allow for conversion to ACLR in the event of rerupture.
Surgical Technique
Patient Evaluation, Imaging, and Indications
The treatment of all patients undergoing arthroscopic ACL repair begins with a complete history, physical examination, and preoperative imaging. An isolated ACL injury is rare, and assessment for associated injuries, including meniscal tears, cartilage lesions, and/or concomitant ligament injuries, is essential.17 Clinical evaluation begins with a comprehensive history addressing the mechanism of injury, presence of a “pop,” generalized pain, and immediate onset of swelling. With an acute injury, the physical examination is often limited by guarding, and ligamentous laxity can be challenging to assess. Increased anterior translation with Lachman and anterior drawer testing is indicative of a tear. Rotatory laxity and concomitant soft-tissue injury are evaluated with pivot-shift testing.18 Ligamentous laxity should be confirmed with examination under anesthesia intraoperatively. Radiographs are evaluated to determine the presence of a Segond fracture and/or deep sulcus sign with anteroposterior, lateral, and Merchant (or sunrise) views. Magnetic resonance imaging is performed to confirm clinical suspicion of an ACL tear and evaluate for additional pathology. The overall evaluation should also take into account the patient’s native posterior tibial slope, coronal alignment, and degree of ligamentous laxity.
Two classification systems can be used to predict whether an ACL tear is amenable to repair. The Sherman classification categorizes ACL tears by location to the proximal half of the ACL. Primary ACL repair is commonly recommended only for acute to subacute type I tears (proximal avulsion from the femur) compared with type III or IV (midsubstance) tears.19,20 Although the Sherman classification is specific, suboptimal interobserver reliability and a lack of clinical application between type III and IV tears guided van der List et al.21, 22, 23 to develop the modified Sherman classification system. By use of this system, type I (proximal avulsion tear, located at >90% of distal-proximal length) and type II (proximal tear, located at 75%-90% of distal-proximal length) tears are determined to have the highest likelihood of healing.24, 25, 26 The modified Sherman classification broadens the applicability of ACL repair by including tears in the proximal 25% of the ligament rather than only avulsion tears. It is important to note that the patient is counseled that the ultimate decision for ACL repair versus ACLR will be made intraoperatively based on tear type and tissue quality, and possible grafts for reconstruction are discussed.21
Surgical Positioning
After anesthesia is induced, the patient is transitioned to the operating table and positioned supine. A lateral post is placed to allow for intraoperative valgus stress, and a footrest is placed to assist with holding the knee at 90°. Wide surgical preparation is performed, and the patient is draped in traditional fashion to allow for possible ACL graft harvest if needed.
Diagnostic Arthroscopy
A diagnostic arthroscopy is performed. The inferolateral portal is established first. We prefer to make this portal “high and tight” to the edge of the patellar tendon to allow for easier visualization of the lateral wall. Next, the inferomedial portal is established. We prefer to make this portal “low and loose” relative to the patellar tendon, typically a few millimeters more inferior and medial than our standard anteromedial portal to allow appropriate drilling access to the femoral ACL attachment. Alternatively, an accessory medial portal may be used.
The ACL stump and the quality of the remaining ACL tissue are assessed (Fig 1). Intraoperatively, if the ACL tear is determined to be a type I or II tear using the modified Sherman classification system with good to excellent tissue quality, primary ACL repair can be considered. If the ACL tear is not a femoral avulsion tear or a tear in the proximal 25% of the ligament or if the tissue quality is poor, surgical treatment is transitioned to a remnant-preserving technique or traditional ACLR.19 Any additional intra-articular pathology is addressed at this time.
Fig 1.
Arthroscopic view from anterolateral portal of left knee identifying anterior cruciate ligament (ACL) proximal avulsion tear (blue arrow).
Lateral Femoral Wall Preparation and ACL Preparation
While the lateral wall is visualized from the anterolateral portal, a combination shaver is used from the medial portal and can be applied in bone-cutting mode to gently decorticate the notch to stimulate increased bleeding in an effort to encourage ACL tissue primary healing. Next, with the knee hyperflexed to about 110° to 120°, a spade-tip Beath pin is drilled from the anteromedial portal through the femoral footprint of the ACL (Fig 2). A SutureTape FiberLink suture (Arthrex) is passed through the femoral tunnel (for future TightRope shuttling) and secured via a hemostat. Next, a cannula (PassPort; Arthrex) is placed in the medial portal (Table 1). Of note, the previously placed passing FiberLink suture is kept outside the portal to optimize suture management. A self-retrieving suture-passing device (FastPass Scorpion Suture Passer; Arthrex) is used to pass between 1 and 3 FiberRing sutures through the ACL remnant tissue (Fig 3). For each FiberRing, outside the joint, the FiberRing suture is prepared for passage by placing the small ringed portion of the FiberRing over the end of the suture passer (which will allow for a luggage-tag repair construct) and loading the single end of suture into the bottom jaw of the suture passer, leaving approximately 2 cm of the suture as a “tail.” The FiberRing is then passed through the ACL remnant via the medial portal. Once the suture passer is removed from the joint, the suture is released, and tension is pulled on the tail (which will exit through the ringed portion of the FiberRing if set up appropriately), securing the ring of suture around the ACL remnant in a luggage-tag fashion. This is repeated for each FiberRing suture. The senior author (R.M.F.) prefers to use 2 sutures for the vast majority of ACL repair tear patterns. With the ACL-Repair TightRope Implant, the TightRope comes disassembled, allowing the surgeon to assemble the TightRope incorporating the FiberRings. Therefore, at this point, the TightRope free end is shuttled through the FiberRing sutures one at a time, with the shuttle loops inside the knee via the anteromedial portal (Fig 4). Once the free end has been shuttled through both FiberRings, the TightRope can be assembled outside the knee. Outside the joint, scissors are used to cut the FiberRing shuttle loop just below the splice, leaving 2 tails. The TigerWire “leader” suture (Arthrex) on the ACL repair TightRope assembly card is passed through the shuttle loop on the FiberRing; then, the free blue tail of the FiberRing is used to shuttle the leader suture through the luggage-tagged FiberRing suture and back out of the PassPort cannula. This is repeated for each FiberRing suture, with sequential loading of the sutures onto the TightRope. The TightRope is then assembled to completion using its included assembly card.
Fig 2.
Arthroscopic view from anterolateral portal of left knee positioning drill at center of anterior cruciate ligament footprint (blue arrow) (A) for drilling of femoral tunnel (blue arrow) (B).
Table 1.
Pearls and Pitfalls of Anterior Cruciate Ligament Repair Using Re-tensionable All-Suture Construct
| Pearls | Pitfalls |
|---|---|
| The FiberRing shuttle suture should be retrieved from the lateral portal prior to passing subsequent FiberRings. | Suture bridges can easily occur without the use of a cannula in the medial portal. |
| The majority of the tensioned suture of the TightRope construct should be passed through the loop portion before passing through the nitinol loop to keep the TightRope balanced. | The TightRope sutures can become unbalanced. |
| The sutures should be passed through the midsubstance fibers to allow for better purchase. Additional FiberRing sutures may be added (up to 3). | Poor purchase in the ACL stump can occur with FiberRing sutures. |
ACL, anterior cruciate ligament.
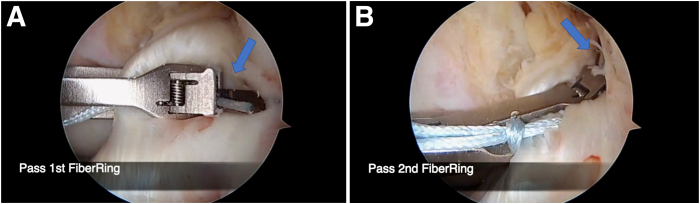
Fig 3.
Arthroscopic view from anterolateral portal of left knee. (A) The first FiberRing suture is passed through the intact remnant of the anterior cruciate ligament using the anteromedial portal (blue arrow). (B) A second FiberRing suture is passed (blue arrow).
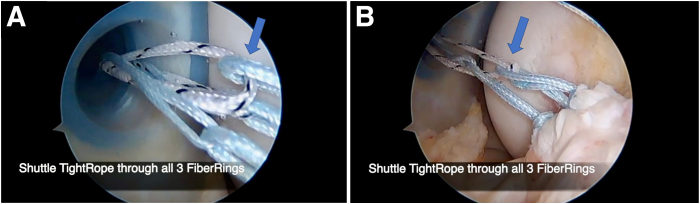
Fig 4.
Arthroscopic view from anterolateral portal of left knee. (A) The TightRope is shuttled through the FiberRing loop (blue arrow). (B) The TightRope is shuttled through all 3 FiberRing loops (blue arrow).
TightRope Passage and Tensioning of Repair
The FiberLink suture that was previously docked outside the anteromedial portal cannula is retrieved from within the cannula and is used to shuttle the TightRope into the femoral tunnel by pulling on both the white TightRope tensioning suture limbs and the blue TightRope passing suture limbs (Fig 5). The button is flipped onto the lateral femoral cortex. Intraoperative fluoroscopy is used to confirm that the button has flipped appropriately. Tension can be placed on the IB FiberTape sutures (preassembled on the button) to give countertraction, making it easier to sense the “flip.” Next, the ACL stump is reduced to the lateral femoral wall by tensioning the TightRope approximately 90%, but final tightening is not yet performed (Fig 6).
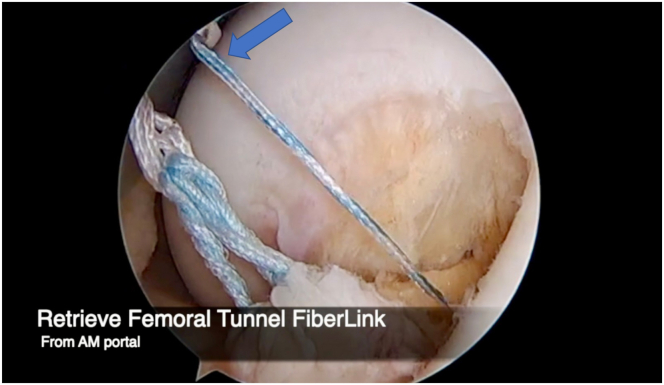
Fig 5.
Arthroscopic view of left knee showing FiberLink suture tape being retrieved from anteromedial (AM) portal (blue arrow) to shuttle TightRope into femoral tunnel.
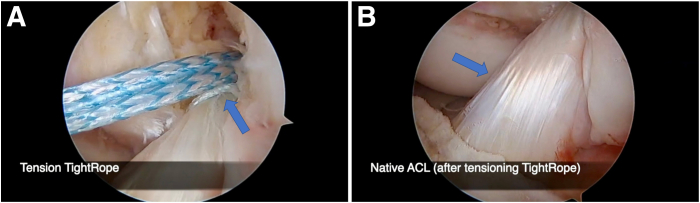
Fig 6.
Arthroscopic view from anterolateral portal of left knee showing tensioned TightRope (blue arrow) (A) and native anterior cruciate ligament (blue arrow) after tensioning (B).
Tibial Drilling and Passing of IB
Next, attention is turned to tibial tunnel drilling. An ACL tibial guide is used to drill a 2.4-mm cannulated drill pin, with the trajectory aiming just anterior to the remnant ACL tissue (Fig 7). We prefer to set the guide at 60° to 65° to allow for adequate tunnel length in the event of future/revision ACLR surgery. Often after drilling, bone will be caught at the end of the drill, so one pearl is to twist the trocar back onto the drill to push out any bone at the very end (Table 1). Next, a lasso wire is placed up the cannulation of the tibial pin and retrieved from the anteromedial portal cannula. The FiberTape IB sutures, which should already be out of the anteromedial portal cannula, are passed through the lasso wire, which is then shuttled down via the anteromedial portal through the tibial tunnel (Fig 8). The FiberTape IB sutures are secured distally with a 3.5- or 4.75-mm SwiveLock Suture Anchor (Arthrex), depending on bone quality, after drilling a pilot hole for the anchor approximately 1 cm distal to the aperture of the tibial tunnel. The ACL repair is examined through a full range of motion (ROM) and cycled multiple times. With the knee in full extension, the ACL repair tissue is finally tightened by pulling on the TightRope tensioning sutures while visualizing arthroscopically (Fig 9). Lachman and anterior drawer examinations are performed while viewing arthroscopically to ensure no gapping or fraying of the repair and a satisfactory stability examination. Finally, marrow venting can be performed using an awl in the femoral notch anterior to the ACL repair, depending on surgeon preference (Fig 10). Of note, if there is a concern regarding ACL tissue viability and/or final repair construct (Fig 11) at any point throughout the repair process (Video 1), consideration can be given to converting to ACLR.
Fig 7.
Arthroscopic view from anterolateral portal of left knee showing tibial tunnel drill guide with cannulated drill pin (blue arrow).
Fig 8.
Arthroscopic view from anterolateral portal of left knee showing internal brace sutures shuttled through tibial tunnel (blue arrow).
Fig 9.
Arthroscopic view from anterolateral portal of left knee showing anterior cruciate ligament repair (blue arrow) with knee in full extension.
Fig 10.
Arthroscopic view from anterolateral portal of left knee showing notch venting being performed through anteromedial portal (blue arrow).
Fig 11.
Arthroscopic view from anterolateral portal of left knee showing internal brace (blue arrow) (A), FiberRing sutures after TightRope re-tensioning (blue arrow) (B), and final anterior cruciate ligament repair (blue arrow) (C).
Rehabilitation Protocol
Postoperatively, rehabilitation is essentially the same as that after isolated ACLR, including weight bearing as tolerated and ROM as tolerated, pending any concomitant procedures performed, such as meniscal repair. Crutches are used early on to minimize potential tissue damage as the patient regains strength and normal gait; their use is discontinued once the gait has normalized. The senior author prefers that patients use a brace during the first 3 to 4 weeks after surgery, especially while quadriceps control and/or function is limited.27 Formal physical therapy begins at 1 to 2 days postoperatively. Quadriceps strengthening and gentle ROM exercises are initiated. Proprioceptive and neuromuscular training is essential during the early weeks and is continued throughout the recovery process. As quadriceps strength and ROM recover, closed kinetic chain exercises are gradually introduced. At approximately 12 to 16 weeks, plyometric exercises begin and are advanced to include sport-specific movements with RTS consideration by 6 to 9 months postoperatively. A functional RTS performance test is recommended to ensure readiness and safety for physical performance.
Discussion
This article describes a technique for ACL repair of proximal avulsion ACL tears.16,19,20 One of the known challenges associated with successful ACL repair surgery is poor vascularity of the remnant ACL tissue, resulting in poor healing capability. Notably, the most proximal portion of the ACL has been found to have a robust blood supply, resulting in high healing potential.5,28, 29, 30 Thus, primary ACL repair is most likely to succeed when used for modified Sherman classification type I and II tears in the proximal 25% of the ligament with good to excellent tissue quality.24, 25, 26 Notably, when considering ACL repair, patient selection is critical. Although diagnostic imaging can be useful in determining whether patients are possible repair candidates, the final determination for repair should be made with an arthroscopic evaluation. This allows for a full evaluation of the remaining ACL stump and the quality of the tissue.
A delay between injury and ACL surgery may result in degeneration and shrinkage of the ACL stump, making primary repair a less viable option.19,20,24,31 Repair within 4 weeks has been shown to provide patients with the highest likelihood of repairability. However, the decision ultimately depends on the tear type and tissue quality. Numerous cases of patients with chronic ACL tears being repaired have been published, including 1 patient who underwent successful repair 11 years after injury.20,25
Compared with ACLR, primary ACL repair has some inherent advantages, such as preserving the native anatomy and eliminating donor-site morbidity, in addition to being a dramatically less morbid procedure and having a quicker recovery than ACLR (Table 2). However, there are some potential disadvantages. This procedure is not feasible for all ACL tear patterns; it is associated with a higher failure rate compared with ACLR, particularly in younger patient populations; and long-term outcome data are not currently available (Table 2). Of note, long-term data are scarce because of the rapid emergence of techniques (and their associated implants) becoming available, such as that presented in this article. Because of these factors, the importance of patient selection cannot be understated.
Table 2.
Advantages and Disadvantages of Anterior Cruciate Ligament Repair Using Re-tensionable All-Suture Construct
| Advantages |
| Expedited recovery compared with traditional ACL reconstruction |
| Decreased morbidity compared with ACL reconstruction |
| Preserves native anatomy |
| Bone-preserving approach |
| Allows use of internal brace or biological augmentation |
| Disadvantages |
| Only indicated for Sherman type I or modified Sherman type I and II tears with good tissue quality |
| Technically challenging |
| Risk of retear but allows for easy conversion to ACL reconstruction |
ACL, anterior cruciate ligament.
Primary ACL repair using a suture anchor approach, as described by DiFelice and van der List,32 has been shown to be a safe and effective treatment option for modified Sherman type I and II tears in the proximal 25% of the ligament with good to excellent tissue quality in multiple studies.32, 33, 34, 35 DiFelice et al.24 also reported on their outcomes, with 10 of 11 ACL repairs achieving short-term clinical success. DiFelice and van der List36 assessed mid-term results in the same cohort, reporting that the clinical outcomes were maintained at mid-term follow-up. However, by using suture anchors, some of the area on the femoral wall is occupied by the anchor. The current technique allows surgeons to tension and re-tension the repair after ranging the knee, which is not possible with the suture anchor techniques.
Smith and Cook37 previously described a similar version of this technique. They described a knotless adjustable-loop design with IB suture augmentation for ACL repair in femoral avulsion tears. In their technique, they described using “0-Link” sutures (i.e., 0-TigerLink and 0-FiberLink sutures [Arthrex]) as a cinch and then passing the adjustable-loop device through the remaining loop in the cinch sutures.37
The use of IB suture augmentation for ligament repair and reconstruction has been discussed in dozens of basic science and clinical studies in a variety of joints, including the knee, elbow, and ankle, with an excellent safety profile and with overall improved biomechanical and clinical outcomes. Specifically, the use of an IB in ACL repair has been previously studied with excellent outcomes. Heusdens et al.38 reported 2-year data on the use of an independent IB through a femoral button with a 4.8% retear rate. Furthermore, Jonkergouw et al.33 compared retear rates of ACL repairs between patients who received an IB and patients who did not. At a 2-year follow-up, they found a retear rate of 7.4% in the IB group and 13.8% in the group without an IB. This has been supported by a biomechanical study that showed decreased overall displacement and gap formation of an ACL repair with the use of an IB.39
The efficacy of ACL repair compared with conventional ACLR was recently examined by Douoguih et al.40 They compared 30 patients who underwent suture-augmented ACL repair for proximal avulsion ACL tears or high-grade partial tears with 30 patients who underwent conventional ACLR. With a 2-year follow-up, they reported no significant difference in the retear rate, KT-1000 testing (MEDmetric, San Diego, CA), or percentage of patients who met or exceeded the minimal clinically important difference in outcome measures between the groups. Additionally, they reported significantly higher early patient-reported outcomes in the ACL repair group compared with the conventional ACLR group.40 Furthermore, in an attempt to provide high-quality evidence showing the advantages of primary ACL repair over reconstruction, Ferreira et al.41 performed propensity matching of 150 patients undergoing ACL repair to patients who underwent ACLR during the same period in a 1:1 ratio. They found that ACL repair was associated with superior hamstring muscle strength at 6 months and significantly better patient-reported outcome scores. As time passes and techniques emerge, the level of evidence regarding primary ACL repair is increasing.42
We describe a technique for arthroscopic ACL repair using TightRope with FiberRing sutures and an IB. Advantages of this technique include a knotless adjustable-loop device, simplicity of incorporating the TightRope by using FiberRing sutures, and graft augmentation with an IB. The potential disadvantages of this technique include limitations in ACL tear patterns that allow repair using this technique. In the correct patient, our arthroscopic ACL repair technique using TightRope with FiberRing sutures with an IB provides a practical and reproducible construct for an acute proximal avulsion tear of the ACL.
Disclosures
The authors report the following potential conflicts of interest or sources of funding: P.A.S. reports the following: board member/owner/officer/committee appointments with American Orthopaedic Society for Sports Medicine (AOSSM) and Journal of Knee Surgery; royalties from Arthrex; speakers bureau/paid presentations for Arthrex; paid consultant or employee of Arthrex; research or institutional support from Arthrex; and stock or stock options in Spinal Simplicity. G.S.D. reports the following: board member/owner/officer/committee appointments with AOSSM and Journal of Knee Surgery; royalties from Arthrex; paid consultant or employee of Arthrex; research or institutional support from Arthrex; and stock or stock options in Embody. R.M.F. reports the following: board member/owner/officer/committee appointments with American Academy of Orthopaedic Surgeons, AOSSM, American Shoulder and Elbow Surgeons, AANA, International Cartilage Repair Society, International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine, Journal of Shoulder and Elbow Surgery, and Orthopedics Today; royalties from Elsevier; speakers bureau/paid presentations for Allosource, Arthrex, JRF, and Ossur; paid consultant or employee of Allosource, Arthrex, and JRF; and research or institutional support from Elsevier, Aesculap Biologics, and Arthrex. All other authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic anterior cruciate ligament (ACL) repair is performed with the patient in the supine position. We begin with a standard diagnostic arthroscopy of the left knee. With the scope in the anterolateral portal, the proximal ACL tear is identified using a probe through the anteromedial portal. The femoral tunnel is drilled at the center of the ACL footprint. Three FiberRing sutures are passed at an appropriate interval through the intact remnant of the ACL using the anteromedial portal. The TightRope is shuttled through each FiberRing loop. The FiberLink suture tape is retrieved from the anteromedial portal to shuttle the TightRope into the femoral tunnel and tensioned. The tibial tunnel is drilled with a cannulated drill pin, where a lasso wire is used to shuttle the internal brace sutures through the tibial tunnel. At this point, we recommend considering notch venting to improve biologics, as performed here. The knee is put through a full range of motion and re-tensioned, demonstrating the final repair construct.
References
- 1.Cohen S.B., Sekiya J.K. Allograft safety in anterior cruciate ligament reconstruction. Clin Sports Med. 2007;26:597–605. doi: 10.1016/j.csm.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 2.Murray M.M. Optimizing outcomes of ACL surgery—Is autograft reconstruction the only reasonable option? J Orthop Res. 2021;39:1843–1850. doi: 10.1002/jor.25128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Larwa J., Stoy C., Chafetz R.S., Boniello M., Franklin C. Stiff landings, core stability, and dynamic knee valgus: A systematic review on documented anterior cruciate ligament ruptures in male and female athletes. Int J Environ Res Public Health. 2021;18:3826. doi: 10.3390/ijerph18073826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lohmander L.S., Englund P.M., Dahl L.L., Roos E.M. The long-term consequence of anterior cruciate ligament and meniscus injuries: Osteoarthritis. Am J Sports Med. 2007;35:1756–1769. doi: 10.1177/0363546507307396. [DOI] [PubMed] [Google Scholar]
- 5.Petersen W., Tillmann B. Structure and vascularization of the cruciate ligaments of the human knee joint. Anat Embryol (Berl) 1999;200:325–334. doi: 10.1007/s004290050283. [DOI] [PubMed] [Google Scholar]
- 6.Kaeding C.C., Pedroza A.D., Reinke E.K., Huston L.J., Spindler K.P. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: Prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43:1583–1590. doi: 10.1177/0363546515578836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Samitier G., Marcano A.I., Alentorn-Geli E., Cugat R., Farmer K.W., Moser M.W. Failure of anterior cruciate ligament reconstruction. Arch Bone Jt Surg. 2015;3:220–240. [PMC free article] [PubMed] [Google Scholar]
- 8.Grassi A., Kim C., Marcheggiani Muccioli G.M., Zaffagnini S., Amendola A. What is the mid-term failure rate of revision ACL reconstruction? A systematic review. Clin Orthop Relat Res. 2017;475:2484–2499. doi: 10.1007/s11999-017-5379-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pullen W.M., Bryant B., Gaskill T., Sicignano N., Evans A.M., DeMaio M. Predictors of revision surgery after anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44:3140–3145. doi: 10.1177/0363546516660062. [DOI] [PubMed] [Google Scholar]
- 10.MARS Group Effect of graft choice on the outcome of revision anterior cruciate ligament reconstruction in the Multicenter ACL Revision Study (MARS) Cohort. Am J Sports Med. 2014;42:2301–2310. doi: 10.1177/0363546514549005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marx J.S., Plantz M.A., Gerlach E.B., et al. Revision ACL reconstruction has higher incidence of 30-day hospital readmission, reoperation, and surgical complications relative to primary procedures. Knee Surg Sports Traumatol Arthrosc. 2022;30:1605–1610. doi: 10.1007/s00167-021-06646-0. [DOI] [PubMed] [Google Scholar]
- 12.Ouillette R., Edmonds E., Chambers H., Bastrom T., Pennock A. Outcomes of revision anterior cruciate ligament surgery in adolescents. Am J Sports Med. 2019;47:1346–1352. doi: 10.1177/0363546519837173. [DOI] [PubMed] [Google Scholar]
- 13.Gee M.S.M., Peterson C.D.R., Zhou M.L., Bottoni C.R. Anterior cruciate ligament repair: Historical perspective, indications, techniques, and outcomes. J Am Acad Orthop Surg. 2020;28:963–971. doi: 10.5435/JAAOS-D-20-00077. [DOI] [PubMed] [Google Scholar]
- 14.Chun K.C., Lee S.H., Kim J.W., Jin E.J., Kim K.M., Chun C.H. Immunohistochemical and immunocytochemical study of mechanoreceptors in anterior cruciate ligament reconstruction with the remnant-preserving technique using Achilles tendon allografts. J Orthop Surg Res. 2017;12:93. doi: 10.1186/s13018-017-0593-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gao F., Zhou J., He C., et al. A morphologic and quantitative study of mechanoreceptors in the remnant stump of the human anterior cruciate ligament. Arthroscopy. 2016;32:273–280. doi: 10.1016/j.arthro.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 16.Takahashi T., Kondo E., Yasuda K., et al. Effects of remnant tissue preservation on the tendon graft in anterior cruciate ligament reconstruction: A biomechanical and histological study. Am J Sports Med. 2016;44:1708–1716. doi: 10.1177/0363546516643809. [DOI] [PubMed] [Google Scholar]
- 17.Spindler K.P., Wright R.W. Clinical practice. Anterior cruciate ligament tear. N Engl J Med. 2008;359:2135–2142. doi: 10.1056/NEJMcp0804745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Musahl V., Karlsson J. Anterior cruciate ligament tear. N Engl J Med. 2019;380:2341–2348. doi: 10.1056/NEJMcp1805931. [DOI] [PubMed] [Google Scholar]
- 19.Sherman M.F., Lieber L., Bonamo J.R., Podesta L., Reiter I. The long-term followup of primary anterior cruciate ligament repair. Defining a rationale for augmentation. Am J Sports Med. 1991;19:243–255. doi: 10.1177/036354659101900307. [DOI] [PubMed] [Google Scholar]
- 20.van der List J.P., Jonkergouw A., van Noort A., Kerkhoffs G., DiFelice G.S. Identifying candidates for arthroscopic primary repair of the anterior cruciate ligament: A case-control study. Knee. 2019;26:619–627. doi: 10.1016/j.knee.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 21.van der List J.P., DiFelice G.S. Preservation of the anterior cruciate ligament: Surgical techniques. Am J Orthop (Belle Mead NJ) 2016;45:E406–E414. [PubMed] [Google Scholar]
- 22.van der List J.P., DiFelice G.S. Preservation of the anterior cruciate ligament: A treatment algorithm based on tear location and tissue quality. Am J Orthop (Belle Mead NJ) 2016;45:E393–E405. [PubMed] [Google Scholar]
- 23.van der List J.P., Mintz D.N., DiFelice G.S. The location of anterior cruciate ligament tears: A prevalence study using magnetic resonance imaging. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117709966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.DiFelice G.S., Villegas C., Taylor S. Anterior cruciate ligament preservation: Early results of a novel arthroscopic technique for suture anchor primary anterior cruciate ligament repair. Arthroscopy. 2015;31:2162–2171. doi: 10.1016/j.arthro.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 25.van der List J.P., DiFelice G.S. Successful arthroscopic primary repair of a chronic anterior cruciate ligament tear 11 years following injury. HSS J. 2017;13:90–95. doi: 10.1007/s11420-016-9530-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van der List J.P., DiFelice G.S. Role of tear location on outcomes of open primary repair of the anterior cruciate ligament: A systematic review of historical studies. Knee. 2017;24:898–908. doi: 10.1016/j.knee.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 27.Wu J., Kator J.L., Zarro M., Leong N.L. Rehabilitation principles to consider for anterior cruciate ligament repair. Sports Health. 2022;14:424–432. doi: 10.1177/19417381211032949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Giuliani J.R., Kilcoyne K.G., Rue J.P. Anterior cruciate ligament anatomy: A review of the anteromedial and posterolateral bundles. J Knee Surg. 2009;22:148–154. doi: 10.1055/s-0030-1247742. [DOI] [PubMed] [Google Scholar]
- 29.Nguyen D.T., Ramwadhdoebe T.H., van der Hart C.P., Blankevoort L., Tak P.P., van Dijk C.N. Intrinsic healing response of the human anterior cruciate ligament: An histological study of reattached ACL remnants. J Orthop Res. 2014;32:296–301. doi: 10.1002/jor.22511. [DOI] [PubMed] [Google Scholar]
- 30.Scapinelli R. Vascular anatomy of the human cruciate ligaments and surrounding structures. Clin Anat. 1997;10:151–162. doi: 10.1002/(SICI)1098-2353(1997)10:3<151::AID-CA1>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 31.Achtnich A., Herbst E., Forkel P., et al. Acute proximal anterior cruciate ligament tears: Outcomes after arthroscopic suture anchor repair versus anatomic single-bundle reconstruction. Arthroscopy. 2016;32:2562–2569. doi: 10.1016/j.arthro.2016.04.031. [DOI] [PubMed] [Google Scholar]
- 32.DiFelice G.S., van der List J.P. Arthroscopic primary repair of proximal anterior cruciate ligament tears. Arthrosc Tech. 2016;5:e1057–e1061. doi: 10.1016/j.eats.2016.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jonkergouw A., van der List J.P., DiFelice G.S. Arthroscopic primary repair of proximal anterior cruciate ligament tears: Outcomes of the first 56 consecutive patients and the role of additional internal bracing. Knee Surg Sports Traumatol Arthrosc. 2019;27:21–28. doi: 10.1007/s00167-018-5338-z. [DOI] [PubMed] [Google Scholar]
- 34.Vermeijden H.D., Yang X.A., van der List J.P., DiFelice G.S. Role of age on success of arthroscopic primary repair of proximal anterior cruciate ligament tears. Arthroscopy. 2021;37:1194–1201. doi: 10.1016/j.arthro.2020.11.024. [DOI] [PubMed] [Google Scholar]
- 35.Vermeijden H.D., van der List J.P., DiFelice G.S. Acute and delayed anterior cruciate ligament repair results in similar short to mid-term outcomes. Knee. 2021;29:142–149. doi: 10.1016/j.knee.2021.01.028. [DOI] [PubMed] [Google Scholar]
- 36.DiFelice G.S., van der List J.P. Clinical outcomes of arthroscopic primary repair of proximal anterior cruciate ligament tears are maintained at mid-term follow-up. Arthroscopy. 2018;34:1085–1093. doi: 10.1016/j.arthro.2017.10.028. [DOI] [PubMed] [Google Scholar]
- 37.Smith P.A., Cook C.S. Knotless primary anterior cruciate ligament repair with adjustable loop device and internal brace augmentation. Arthrosc Tech. 2020;9:e1967–e1975. doi: 10.1016/j.eats.2020.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Heusdens C.H.W., Hopper G.P., Dossche L., Roelant E., Mackay G.M. Anterior cruciate ligament repair with independent suture tape reinforcement: A case series with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2019;27:60–67. doi: 10.1007/s00167-018-5239-1. [DOI] [PubMed] [Google Scholar]
- 39.Bachmaier S., DiFelice G.S., Sonnery-Cottet B., et al. Treatment of acute proximal anterior cruciate ligament tears—Part 2: The role of internal bracing on gap formation and stabilization of repair techniques. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967119897423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Douoguih W.A., Apseloff N.A., Murray J.C., Kelly R.L., Svoboda S.J. Suture-augmented ACL repair for proximal avulsion or high-grade partial tears shows similar side-to-side difference and no clinical differences at 2 years versus conventional ACL reconstruction for near-complete and mid-substance tears or poor ACL tissue quality. Arthroscopy. 2024;40:857–867. doi: 10.1016/j.arthro.2023.07.011. [DOI] [PubMed] [Google Scholar]
- 41.Ferreira A., Saithna A., Carrozzo A., et al. The minimal clinically important difference, patient acceptable symptom state, and clinical outcomes of anterior cruciate ligament repair versus reconstruction: A matched-pair analysis from the SANTI Study Group. Am J Sports Med. 2022;50:3522–3532. doi: 10.1177/03635465221126171. [DOI] [PubMed] [Google Scholar]
- 42.van der List J.P., Vermeijden H.D., Sierevelt I.N., DiFelice G.S., van Noort A., Kerkhoffs G. Arthroscopic primary repair of proximal anterior cruciate ligament tears seems safe but higher level of evidence is needed: A systematic review and meta-analysis of recent literature. Knee Surg Sports Traumatol Arthrosc. 2020;28:1946–1957. doi: 10.1007/s00167-019-05697-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic anterior cruciate ligament (ACL) repair is performed with the patient in the supine position. We begin with a standard diagnostic arthroscopy of the left knee. With the scope in the anterolateral portal, the proximal ACL tear is identified using a probe through the anteromedial portal. The femoral tunnel is drilled at the center of the ACL footprint. Three FiberRing sutures are passed at an appropriate interval through the intact remnant of the ACL using the anteromedial portal. The TightRope is shuttled through each FiberRing loop. The FiberLink suture tape is retrieved from the anteromedial portal to shuttle the TightRope into the femoral tunnel and tensioned. The tibial tunnel is drilled with a cannulated drill pin, where a lasso wire is used to shuttle the internal brace sutures through the tibial tunnel. At this point, we recommend considering notch venting to improve biologics, as performed here. The knee is put through a full range of motion and re-tensioned, demonstrating the final repair construct.