Abstract
Angioleiomyoma is a benign soft tissue tumor originating in the smooth muscle of blood vessels. It most frequently presents as a painful, free-moving subcutaneous nodule in the lower extremities and is most common in middle-aged women. Angioleiomyoma is rare amongst benign foot neoplasms, and a preoperative diagnosis of angioleiomyoma is rare. We present a case of angioleiomyoma involving the ankle of a 28-year-old female. To prevent patient suffering, we emphasize the importance of an early and accurate diagnosis. Furthermore, we highlight the salient features of angioleiomyoma, which help with the early detection and differentiation of similar malignant variants, including leiomyosarcoma.
Keywords: soft tissue tumor, leiomyosarcoma, imaging, dermatopathology, surgery, pain, ankle, angioleiomyoma
Introduction
Angioleiomyomas are benign subcutaneous tumors typically arising from the smooth muscle of the tunica media [1]. Angioleiomyoma is rare amongst benign foot neoplasms, making up roughly 4.4% of all benign soft tissue tumors and 0.2% of benign foot and ankle lesions [2-4]. The majority of angioleiomyomas are under 2 cm in diameter and are associated with pain in roughly 60% of cases [5,6]. Angioleiomyoma is more common in women than in men, with a male-to-female ratio of 1:1.7, with 67% of cases occurring in patients between 30 and 60 years old with an average age of 47 years [2]. While angioleiomyoma may present anywhere on the body, 67% of cases appear on the lower extremities, but of the cases involving the foot and ankle, only 15.7% are located on the ankle [4]. Since involvement of the ankle is rarely documented, preoperative diagnosis is rare, leading to delays in treatment and prolonged suffering [5]. This is especially important since there are reported cases of malignant transformation, calcification, hemorrhage, hyalinization, and myxoid degeneration associated with angioleiomyoma [7].
Case presentation
A 28-year-old female presented to a podiatrist with a one-year history of pain above the medial malleolus of the left ankle. She described that discomfort initially arose only when wearing shoes or touching the area. This pain worsened over the course of a year and began to occur spontaneously. Upon presentation, her pain was described as sharp at a level of 7/10 on the numeric rating scale, occurred spontaneously several times a day, worsening with palpation, and lasted up to five minutes with radiation up the left aspect of her ankle. No other associated symptoms were present.
Initial clinical examination revealed a small non-fluctuant firm nodule that measured approximately 2-3 mm in size appearing fixed to the skin. No erythema or adjacent swelling were noted. Furthermore, no lymphadenopathy was noted.
MRI was requested due to a reported worsening of symptoms in both intensity and frequency. An MRI of her ankle revealed an ovoid 0.5x0.3x0.4 cm enhancing mass in the subcutaneous soft tissues just deep to the skin surface at the level of the distal tibia medially (Figure 1). Impression noted a differential, including neoplasms alongside other etiologies necessitating biopsy.
Figure 1. Ankle MRI sagittal images of a small lesion in the subcutaneous fat just below the skin surface at the lateral ankle measuring 3x4x5 mm.
A: Lesion is hyperintense (black arrow); proton density fat saturation MRI sequence. B: Lesion is hypointense (black arrow); T1-weighted MRI sequence. C: Lesion is avidly enhancing (black arrow); T1-weighted fat saturation MRI sequence with gadolinium contrast.
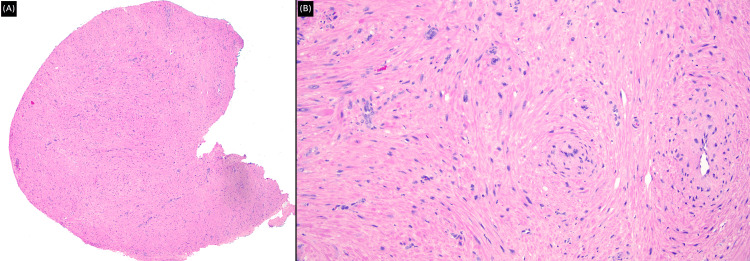
We subsequently performed an excisional biopsy (Figure 2). Histopathology examination showed a circumscribed nodule composed of smooth muscle fibers with straight, blunt-edged nuclei and several capillary-type vascular channels, consistent with the solid subtype of angioleiomyoma (Figure 3). The patient reported a complete resolution of symptoms following the excision of the lesion, with a two-year follow-up noting no recurrence of the lesion or her symptoms.
Figure 2. Tissue removed from surgical excision.
The lesion is round, smooth, and spherical, with a roughly 3 mm diameter.
Figure 3. Histopathology examination.
A: Low-power image showing a circumscribed nodule (H&E stain, magnification x40). B: High-power image exhibiting smooth muscle fibers with straight, blunt-edged nuclei and several capillary-type vascular channels (H&E stain, magnification x200).
Discussion
Angioleiomyomas can be designated into three different subtypes: solid, cavernous, and venous, with solid subtypes (67% of cases) outnumbering cavernous (23%) or venous (11%) subtypes [2,4]. These subtypes vary slightly in their typical clinical presentations. Solid subtypes are accompanied by pain in 70% of cases, as opposed to 30% in cavernous cases or 37% in venous cases. Previous literature has attributed the pain associated with angioleiomyoma to the compression of interstitial nerve fibers and ischemia [4]. The pain has been described as burning with electrical aspects and rapidly worsens with light contact or exposure to cold [2]. In the case of our patient, pressure from footwear caused significant pain and occasionally interfered with daily function. A study by Hachisuga et al. also found some subtypes, such as the cavernous subtype, appeared more commonly in men with a male-to-female ratio of 4:1, with a predilection for the head and upper extremities [2]. It should be noted that the venous subtype only slightly favored men and had a roughly even distribution of lower extremity vs upper extremity/head cases. This contrasts with the typical solid presentation that favors females (78% of cases), in whom angioleiomyoma favors the lower extremities (83% of cases).
The primary method of differentiating these subtypes involves histopathology. The solid subtype of angioleiomyoma is typically composed of smooth muscle cells surrounding vascular channels, which may be capillary-sized but abundant in quantity [2,6]. The cavernous subtype of angioleiomyoma is identified by the dilation of vascular channels and the lowered presence of smooth muscle. Finally, the venous subtype of angioleiomyoma can be characterized by less compact smooth muscle bundles and thickened muscular walls, potentially surrounding the vessels in an organized manner. Some authors note that organizing thrombus, mature fat cells, or lymphocytic infiltrate may be found in some cases of angioleiomyoma [1]. Previous literature also describes cases of hyaline or myxoid degeneration and attributes it to circulatory disturbances, but a clinicopathological reappraisal of cases found that this degeneration didn't frequently accompany painful variants of angioleiomyoma, nor did thrombosis or hemorrhage [1,2]. Although histopathology is diagnostic, immunohistochemistry can be performed in diagnostically difficult cases. Immunohistochemically, angioleiomyomas are generally positive for smooth muscle actin (SMA), HHF35, calponin, caldesmon, and desmin, and vascular markers CD34 and CD31 [8, 9].
While angioleiomyoma has no clear etiology, previous literature has proposed trauma-induced venous stasis, genetic factors, vascular malformations, and hormonal changes with a focus on estrogen as potential factors in the development of angioleiomyoma [4,10]. The differential diagnosis for angioleiomyoma includes ganglionic cyst, giant cell tumor, fibroma, desmoid tumor, tophi, neurofibroma, schwannoma, sarcoma, gouty tophus, glomus tumor, lipoma, hemangioma, foreign-body granuloma, superficial acral fibromyxoma, and leiomyosarcoma.
While histology remains the gold standard in diagnosing angioleiomyoma of the ankle, previous literature has discussed the use of radiography in narrowing down angioleiomyoma in the differential diagnosis [4]. Roughly 30% of all foot and ankle angioleiomyoma cases feature calcifications identifiable by radiography, potentially from minor repetitive traumas. Ultrasonography may show homogeneous structures with well-defined margins, typically showing hypoechogenicity and low-medium vascular density. MRIs detect angioleiomyomas as well defined and bordered by hypointense fibrous capsules. See Table 1 for further information on imaging for angioleiomyoma. It should be noted that histologic examination is necessary to identify whether an angioleiomyoma is solid, cavernous, or venous in nature.
Table 1. Clinical information to help differentiate between angioleiomyoma and leiomyosarcomas.
| Diagnostic considerations | Angioleiomyoma | Leiomyosarcoma |
| Clinical Appearance | Typically under 2 cm and rarely over 4 cm. Typically encapsulated [2,10]. | Median size of 6 cm with a large range: 0.3-45 cm. Typically not encapsulated [10,15]. |
| Age | The average age is 47 years [2]. | The average age is 57 years [15]. |
| Gender distribution | More common in females (roughly 2:1) [2,10]. | Roughly even distribution with a slight male preference [16]. |
| Locality | 67% in the lower extremity (83% for women) [2]. | Disregarding uterine cases, 48% occur in the extremities (more common in the lower extremities), 41% in abdominal or retroperitoneal, and 11% in the trunk [14,15,17]. |
| Recurrence following excision | Less than 1% of cases [2]. | Up to 60% of cases [18]. |
| Pain | Up to 70% of cases for the solid subtype [2]. | Often presents without pain [10,14]. |
| Imaging | Generally, smaller but small size and non-aggressive lesion features do not exclude sarcoma. Isointense signal to muscle is seen on T1-weighted images and intermediate-high signal on T2-weighted images. T2 hypointense rim may be predictive of angioleiomyoma diagnosis [19]. | Areas of internal necrosis or hemorrhage, with masses visible with computed tomography. Isointense signal to the muscle is seen on T1-weighted images and intermediate-high signal on T2-weighted images. Aggressive features, such as surrounding soft tissue invasion, larger size, and peritumoral edema/enhancement [20]. |
| Histology | Three main subtypes [1]: solid, closely compacted smooth muscle with small vascular channels; cavernous, dilated vascular channels and less smooth muscle; venous, thick muscular walls and less compact smooth muscle bundles. | Well-defined intersecting bundles of spindle cells with increased eosinophilic cytoplasm and elongated/hyperchromatic nuclei. Increased mitotic activity may suggest a malignant character [16]. |
While it is rare, there are recorded cases of angioleiomyoma's malignant evolution to leiomyosarcoma and angioleiomyosarcoma, an aggressive vascular tumor with a five-year survival rate estimated between 20% and 35% [4,11,12]. It should be noted that cases of angioleiomyosarcoma are rare in literature, often not being defined as an independent category of sarcoma, resulting in few reported cases that make generalizations difficult; leiomyosarcoma should be a significant consideration in the differential diagnosis of angioleiomyoma [13]. Leiomyosarcoma makes up about 1% of all soft tissue tumors and 7% of all soft tissue sarcomas [14]. As such, healthcare providers should remain vigilant in treating angioleiomyoma despite its benign nature, even in the absence of pain. Physicians should consult Table 1 to ensure accurate diagnosis of angioleiomyoma. Fortunately, excision is incredibly effective in treating angioleiomyoma, and less than 1% of patients experience recurrence following excision [2].
Conclusions
We present the case of angioleiomyoma in the ankle of a 28-year-old female. Angioleiomyoma is rare amongst benign foot neoplasms, and our case highlights the importance of interdisciplinary cooperation in achieving an early and accurate diagnosis while minimizing patient suffering. Clinicians should remember that while angioleiomyoma is most common in the lower extremities of middle-aged women, its different subtypes may present anywhere on the body. While angioleiomyoma is benign, clinicians should include aggressive soft tissue tumors such as leiomyosarcomas in their differential diagnosis. As a whole, angioleiomyoma has an excellent prognosis following excision, and our patient reports complete resolution of symptoms following her treatment with no recurrence of the lesion or symptoms.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Michael Kozlov, Eyal Levit, Sameera Husain, Edward Mardakhaev
Acquisition, analysis, or interpretation of data: Michael Kozlov, Eyal Levit, Sameera Husain, Edward Mardakhaev
Drafting of the manuscript: Michael Kozlov, Eyal Levit, Sameera Husain, Edward Mardakhaev
Critical review of the manuscript for important intellectual content: Michael Kozlov, Eyal Levit, Sameera Husain, Edward Mardakhaev
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Angioleiomyoma: a clinical, pathological and radiological review. Ramesh P, Annapureddy SR, Khan F, Sutaria PD. Int J Clin Pract. 2004;58:587–591. doi: 10.1111/j.1368-5031.2004.00085.x. [DOI] [PubMed] [Google Scholar]
- 2.Angioleiomyoma. A clinicopathologic reappraisal of 562 cases. Hachisuga T, Hashimoto H, Enjoji M. Cancer. 1984;54:126–130. doi: 10.1002/1097-0142(19840701)54:1<126::aid-cncr2820540125>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 3.A review of 2,720 lesions of the foot. Berlin SJ. J Am Podiatry Assoc. 1980;70:318–324. doi: 10.7547/87507315-70-7-318. [DOI] [PubMed] [Google Scholar]
- 4.Current concepts of foot and ankle angioleiomyoma. Matos M, Soares S, Agaoua M. J Foot Ankle Surg. 2023;62:746–749. doi: 10.1053/j.jfas.2023.02.006. [DOI] [PubMed] [Google Scholar]
- 5.Angioleiomyoma-rare soft tissue tumor of the foot and ankle, review of two patients and review of the literature. Bodapati VS, Sunderamoorthy D. J Surg Case Rep. 2021;2021:0. doi: 10.1093/jscr/rjab535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mechanism of pain and cytoskeletal properties in angioleiomyomas: an immunohistochemical study. Hasegawa T, Seki K, Yang P, Hirose T, Hizawa K. Pathol Int. 1994;44:66–72. doi: 10.1111/j.1440-1827.1994.tb02587.x. [DOI] [PubMed] [Google Scholar]
- 7.Angioleiomyoma of the hand with nerve compression. Jin Q, Lu H. J Int Med Res. 2020;48:1–8. doi: 10.1177/0300060520928683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Angioleiomyoma of the forearm. Dey B, Bharti JN, Gautam P, Kaushal S. J Lab Physicians. 2014;6:53–54. doi: 10.4103/0974-2727.129094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Angioleiomyoma: a clinicopathologic and immunohistochemical reappraisal with special reference to the correlation with myopericytoma. Matsuyama A, Hisaoka M, Hashimoto H. Hum Pathol. 2007;38:645–651. doi: 10.1016/j.humpath.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 10.Angioleiomyoma of the lower extremity. Hanft JR, Carbonell JA, Do HQ. J Am Podiatr Med Assoc. 1997;87:388–391. doi: 10.7547/87507315-87-8-388. [DOI] [PubMed] [Google Scholar]
- 11.Angioleiomyoma masquerading as shoulder pain. Ravi S, Chandy LJ, Kumar G, Jacob B, Emmanuel AM. Clin Shoulder Elb. 2021;24:32–35. doi: 10.5397/cise.2020.00192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dermal angiomyoma of the upper extremity. Neviaser RJ, Newman W. J Hand Surg Am. 1977;2:271–274. doi: 10.1016/s0363-5023(77)80125-1. [DOI] [PubMed] [Google Scholar]
- 13.Reed syndrome: an atypical presentation of a rare disease. Perkins J, Scarbrough C, Sammons D, Magro C. Dermatol Online J. 2015;21:6. [PubMed] [Google Scholar]
- 14.Soft tissue leiomyosarcoma-diagnostics, management, and prognosis: data of the registry cancer of the center of Tunisia. Mestiri S, Elghali MA, Bourigua R, et al. Rare Tumors. 2019;11:1–7. doi: 10.1177/2036361318820171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Predictors of survival and recurrence in primary leiomyosarcoma. Gladdy RA, Qin LX, Moraco N, Agaram NP, Brennan MF, Singer S. Ann Surg Oncol. 2013;20:1851–1857. doi: 10.1245/s10434-013-2876-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leiomyosarcoma. Serrano C, George S. Hematol Oncol Clin North Am. 2013;27:957–974. doi: 10.1016/j.hoc.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 17.Leiomyosarcoma of somatic soft tissues: a tumor of vascular origin with multivariate analysis of outcome in 42 cases. Farshid G, Pradhan M, Goldblum J, Weiss SW. Am J Surg Pathol. 2002;26:14–24. doi: 10.1097/00000478-200201000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Leiomyosarcoma of the skin and subcutaneous tissue. Jegasothy BV. Arch Dermatol. 1981;117:478–481. [PubMed] [Google Scholar]
- 19.Angioleiomyoma in soft tissue of extremities: MRI findings. Yoo HJ, Choi JA, Chung JH, et al. AJR Am J Roentgenol. 2009;192:0–4. doi: 10.2214/AJR.07.3952. [DOI] [PubMed] [Google Scholar]
- 20.Radiological imaging features of non-uterine leiomyosarcoma. O'Sullivan PJ, Harris AC, Munk PL. Br J Radiol. 2008;81:73–81. doi: 10.1259/bjr/18595145. [DOI] [PubMed] [Google Scholar]