Abstract
Electrical storm (ES) is a state of electrical instability, manifesting as recurrent ventricular arrhythmias (VAs) over a short period of time (three or more episodes of sustained VA within 24 h, separated by at least 5 min, requiring termination by an intervention). The clinical presentation can vary, but ES is usually a cardiac emergency. Electrical storm mainly affects patients with structural or primary electrical heart disease, often with an implantable cardioverter-defibrillator (ICD). Management of ES requires a multi-faceted approach and the involvement of multi-disciplinary teams, but despite advanced treatment and often invasive procedures, it is associated with high morbidity and mortality. With an ageing population, longer survival of heart failure patients, and an increasing number of patients with ICD, the incidence of ES is expected to increase. This European Heart Rhythm Association clinical consensus statement focuses on pathophysiology, clinical presentation, diagnostic evaluation, and acute and long-term management of patients presenting with ES or clustered VA.
Keywords: Electrical storm, Arrhythmia, Ventricular tachycardia, Ventricular fibrillation, Sudden cardiac death, Consensus document
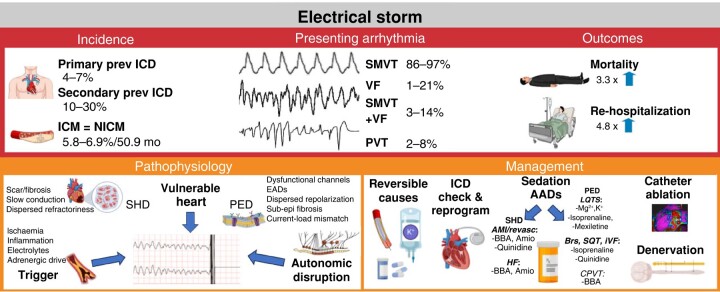
Graphical Abstract
Graphical abstract.
Table of contents
1. Background
2. Aim of the document
3. Review of evidence
4. Definitions
5. Scope of the problem
6. Pathophysiological aspects
6.1. The vulnerable heart—underlying structural heart disease
6.2. The vulnerable heart—underlying primary electrical disease
6.3. External precipitation factors or triggers
6.4. The autonomic nervous system
7. Clinical presentation
8. Acute management
8.1. Initial evaluation, assessment of external precipitating factors, and reversible causes
8.1.1. History
8.1.2. Twelve-lead electrocardiogram
8.1.3. Documentation of ventricular arrhythmia and immediate implantable cardioverter-defibrillator interrogation
8.1.4. Blood tests
8.1.5. Coronary angiogram, cardiac imaging, and additional diagnostic studies
8.2. Treatment
8.2.1. Electrical storm with haemodynamic instability
8.2.2. Disease-specific aspects
8.2.3. Implantable cardioverter-defibrillator reprogramming
8.2.4. Deep sedation and mechanical ventilation
8.2.4.1. Agents used for (deep) sedation
8.2.5. Pharmacotherapy for the acute management of electrical storm
8.2.5.1. Structural heart disease
8.2.5.2. Primary electrical disease
8.2.6. Mechanical circulatory support
8.2.6.1. Rescue therapy in acute haemodynamic decompensation because of refractory, haemodynamically intolerant ventricular arrhythmia
8.2.6.2. Rescue therapy in peri-procedural acute haemodynamic decompensation because of refractory unstable ventricular arrhythmia in patients undergoing ventricular tachycardia ablation
8.2.6.3. Prophylactical mechanical circulatory support implantation prior to ventricular tachycardia ablation in patients at high risk of developing haemodynamic instability
8.2.7. Acute catheter ablation
8.2.8. Autonomic modulation
8.2.8.1. Stellate ganglion block
8.2.8.2. Thoracic epidural anaesthesia
8.2.8.3. Surgical/thoracoscopic sympathetic cardiac denervation
8.2.8.4. Renal denervation
8.2.9. Overdrive pacing
8.2.10. Bailout strategies
9. Stabilized patient
9.1. Long-term treatment
9.2. Anti-arrhythmic drugs to prevent electrical storm recurrence
9.2.1. Chronic anti-arrhythmic drug therapy in patients with structural heart disease
9.2.2. Chronic pharmacotherapy in primary electrical disease
9.3. Catheter ablation to prevent electrical storm recurrence
9.3.1. Ischaemic heart disease
9.3.2. Non-ischaemic cardiomyopathy
9.3.3. Primary electrical disease
9.4. Autonomic modulation
10. Psychological counselling
11. Special patient groups
11.1. Patients with left ventricular assist device
11.2. Patients with advanced heart failure
12. When not to perform interventional treatment
References
1. Background
Ventricular electrical storm (ES) is defined as three or more episodes of sustained ventricular arrhythmias (VAs) occurring within 24 h, separated by at least 5 min, requiring termination by an intervention.1 According to this definition, the clinical presentation can vary from asymptomatic or mildly symptomatic episodes of well-tolerated ventricular tachycardia (VT) to a life-threatening electrical instability, often aggravated by enhanced sympathetic tone. Similarly, clustered VAs, defined as ≥2 episodes of sustained VA within 3 months, can encompass a wide spectrum of clinical presentations.2 Electrical storm and clustered VA are frequently encountered in patients with ICDs. Most patients have underlying structural heart disease (SHD), with monomorphic sustained VT (MSVT) as the most common initiating arrhythmia. Electrical storm due to polymorphic VT (PVT) or primary ventricular fibrillation (VF) also occurs and is more likely in the setting of acute cardiac ischaemia or in patients with channelopathies [primary electrical diseases (PEDs)].3 Electrical storm with recurrent ICD shocks has been associated with psychological disorders, heart failure (HF), and increased mortality and is considered a cardiac emergency. Management of ES requires a multi-faceted approach and involvement of multi-disciplinary teams.
2. Aim of the document
In 2022, the European Society of Cardiology (ESC) released guidelines for management of patients with VA and the prevention of sudden cardiac death (SCD).1 In 2017, a document on the same topic was released by the Heart Rhythm Society (HRS), the American College of Cardiology, and the American Heart Association.4,5 A consensus statement addressing, specifically, catheter ablation (CA) of VA was issued by the HRS and the European Heart Rhythm Association (EHRA) in 2019, in collaboration with the Asia Pacific HRS (APHRS) and the Latin American HRS (LAHRS).6 This document aims to complement the prior ESC guidelines and consensus statements by providing detailed practical advice on diagnostic evaluation and acute and long-term management of patients presenting with ES or clustered VA. The definition of the different categories of advice is provided in Table 1. The used categories for strength of advice and supportive evidence are listed in Table 2. It should be emphasized that this EHRA Clinical Consensus statement is not intended as a guideline.
Table 1.
Category of advice
| Definition | Categories of advice |
|---|---|
| Evidence or general agreement that a given measure is clinically useful and appropriate | Advice TO DO |
| Evidence or general agreement that a given measure may be clinically useful and appropriate | May be appropriate TO DO |
| Evidence or general agreement that a given measure is not appropriate or harmful | Advice NOT TO DO |
| No strong advice can be given, lack of data, inconsistency of data | Area of uncertainty |
Table 2.
Strength of advice and strength of evidence
| Strength of advice | Symbol |
|---|---|
| Clinical advice, based on robust published evidence |

|
| Clinical advice, based on consensus of the writing group |

|
| May be appropriate, based on published evidence |

|
| May be appropriate, based on consensus of the writing group |

|
| Areas of uncertainty |

|
| Strength of evidence | Abbreviation |
| Meta-analysis of RCTs | META |
| RCT | RCT |
| Observational studies | OBS |
| Expert opinion | OPN |
META: evidence from >1 high-quality RCT or >1 meta-analyses of high-quality RCTs. RCT: evidence from 1 high-quality RCT, >1 moderate-quality RCTs, or meta-analyses of moderate-quality RCTs. OBS: observational or registries studies or meta-analyses of such studies. OPN: randomized, non-randomized, observational studies, or registries with limitations of design or execution. Meta-analyses of such studies. Physiological or mechanistic studies in human subjects. Consensus of expert opinion based on clinical experience. Case series.
RCT, randomized clinical trial.
3. Review of evidence
The EHRA Task Force prepared this consensus document with HRS, LAHRS, and APHRS representatives. Members of the Task Force were asked to review English-language literature across multiple databases, including PubMed, Embase, and the Cochrane Library, incorporating studies up to November 2023. Search was focused on all aspects of ES, including prevalence, pathophysiology, clinical manifestation, and management. Advices were constructed considering the strength of evidence supporting particular management or procedure and estimated patient outcomes. Potential sources of bias or factors that might have modified the results (e.g. number and characteristics of patients, duration of follow-up, patient groups’ heterogeneity, physician/patient preferences, etc) were identified and considered when establishing the strength of advices. In controversial or poorly evidenced areas, a consensus was reached by agreement of the expert group. Writing and reviewing were both iterative and collaborative, aligning with the principles of the Delphi process, and ensuring a broad range of expert opinions were considered. All advices were voted on using an online voting system, and consent of ≥80% of voters was required to accept the advice. The document underwent a thorough, two-round external review.
4. Definitions
5. Scope of the problem
The reported incidence of ES depends on the definition, studied population, and observation period.7–10 Electrical storm occurs in 10–30% of patients who have received an ICD for secondary prevention of SCD. The average time after device implantation to ES is 4–9 months.7,11,12 The incidence of ES is lower in patients who undergo ICD implantation for primary prevention of SCD and is estimated to be 4–7%, 18–24 months after ICD implantation.8–10,12 The reported incidence of clustered VA was 26% during 40 months in ICD recipients for primary or secondary SCD prevention.2
The incidence of ES is not significantly different in primary prevention ICD recipients with chronic coronary artery disease (cCAD) or non-ischaemic cardiomyopathy (NICM) during long-term follow-up (5.8 vs. 6.9%, respectively, within 50.9 ± 33.9 months after implantation).10,13,14 Cardiac resynchronization therapy (CRT) may influence the occurrence of ES. In a retrospective observational study of a mixed cohort of patients with cCAD and NICM, patients with CRT-defibrillator had a lower ES incidence compared with propensity-matched ICD recipients. However, in some patients with CRT, left ventricular (LV) pacing may cause ES and should be disabled in such cases. Nevertheless, CRT-responders had lower ES rates,12 which may be explained by the association between higher LV ejection fraction (LVEF) and lower risk of ES.15 With the growing number of patients with ICDs, the number of patients requiring ES management is likely to increase.
Data on ES in patients with PED are scarce and based on case reports or small series. Though ES incidence among PED patients seems to be low, increasing ICD use and improved survival are likely to also increase the rate of ES in this group.16 In patients with catecholaminergic PVT (CPVT), ICD shocks are sometimes ineffective and may trigger ES.17 Clustered VA and ES, according to the definition above, are more common in patients with known SHD and ICDs, but occasionally, ES may be the first manifestation of a previously not known cardiac disease.
Electrical storm is associated with high morbidity and mortality, particularly in the presence of additional factors (including amiodarone use, chronic kidney disease, and LVEF < 35%).18–22 Electrical storm was associated with a 2.5-fold higher risk of all-cause mortality compared with patients with sporadic episodes of VT and a 3.3-fold higher risk compared with patients without sustained VAs during follow-up.13 In a mixed cohort (cCAD and NICM) of ICD recipients, those who were admitted with an ES had a 4.8-fold higher risk of re-hospitalization and a 1.8-fold higher risk of major adverse cardiac events [defined as a composite of acute myocardial infarction (AMI), target vessel revascularization, and all-cause mortality], compared with patients with VT or VF but without ES.20 Clustered VA was also associated with a 2.7-fold increased risk of death compared with ICD recipients without arrhythmia, and mortality risk increased with higher VA burden (number of VA episodes in a cluster) and shorter cluster length (the time frame during which a specified number of VA events occurred).2 A 5-year survival free of death or heart transplant was 67 and 87%, respectively, in patients with and without clusters.23
6. Pathophysiological aspects
The pathophysiological mechanisms leading to ES are difficult to study in humans and differ depending on the underlying structural or electrical heart disease.
In a rabbit model, a complex interplay among enhanced sympathetic tone, calcium-related signalling abnormalities, dysregulation of protein phosphorylation, and a susceptible arrhythmogenic substrate was shown to contribute to VF episodes.24 It has been suggested that three key factors are prerequisite or contribute to ES, namely (i) a ‘vulnerable’ heart—which is a ‘conditio sine qua non’ of ES (i.e. the presence of a pre-existing heart disease that creates the necessary anatomical or electrical ‘substrate’), (ii) external precipitating factors or triggers, and (iii) a disruption of autonomic nervous system activity, particularly sympathetic activation. Although several external factors may be involved (see Sections 6.3. and 8.2.2.), a likely initiating trigger has, however, only been identified in 13% of ICD recipients with SHD.7,25 The role of the autonomic system in promoting and maintaining ES has been recognized.26,27 Genetic predisposition may play a role as well. Rare genetic variants in genes associated with inherited syndromes of sudden cardiac death may also predispose to ES in patients with cCAD.28 Early repolarization patterns have been described in patients with cCAD or NICM presenting with ES.29 A significant correlation between early repolarization patterns and VA recurrences in patients with idiopathic VF (IVF) could be observed.30
6.1. The vulnerable heart—underlying structural heart disease
Most patients presenting with ES or clustered VA have SHD. The critical VA substrate is typically related to areas of heterogeneous fibrosis, which can be observed in patients with cCAD and different cardiomyopathy phenotypes, including arrhythmogenic right ventricular cardiomyopathy (ARVC), dilated cardiomyopathy (DCM), and hypertrophic cardiomyopathy (HCM). Ventricular arrhythmia due to a diseased conduction system (e.g. Purkinje system-related) also needs to be recognized.31
Patients with SHD presenting with an ES are older, more often male, with a lower LVEF, advanced HF, and higher cardiovascular comorbidities compared with those without ES.32,33 In an observational study of ICD patients, chronic renal failure, depressed LVEF, and MSVT as index arrhythmia were independent predictors of an ES.33 Among patients who underwent radiofrequency CA (RFCA) for MSVT, those with history of ES had failed more anti-arrhythmic drugs (AADs), had more inducible VTs, and required longer procedure times and radiofrequency delivery time to control VT, suggesting a more complex or advanced VA substrate.14 In a study of patients with cCAD, ES patients had more diseased LV segments and more often anterior, septal, and apical endocardial LV scar. In contrast, a recent observational study of 152 consecutive patients with cCAD (43% with ES) undergoing VT ablation found no differences in the incidence of ES between patients after anterior and inferior AMI.34 In patients with NICM, the overall extent of the electroanatomical scar was similar, but lateral LV endocardial scar was more frequently observed in ES patients than in non-ES patients.32
6.2. The vulnerable heart—underlying primary electrical disease
All inherited arrhythmia syndromes carry a significant risk of SCD secondary to malignant VAs. In patients with long QT syndromes (LQTS) (acquired or congenital), torsade de pointes (TdP), with or without deterioration into VF, is the signature arrhythmia, and in the other arrhythmia syndromes, rapid PVT or VF is pertinent.35
In LQTS, adrenergic stimulation exerts genotype-specific effects.36 In LQT1, in which most arrhythmic events are triggered by exercise, sustained β stimulation enhances Ca2+ L-type inward current (ICaL), which is not counterbalanced by a slowly rectifying IKs potassium current, due to a dysfunctional pore-forming α-subunit. This results in the prolongation of action potential duration (APD). Sudden adrenergic surges (like during arousal) do not induce this effect due to the protective role of intact fast rectifying IKr current.37,38 On the contrary, in LQT2, in which VA is evoked commonly by sudden arousal (e.g. loud noise, startle), abrupt adrenergic drive causes imbalance between APD-prolonging ICaL and dysfunctional IKr currents, with resulting prolongation in APD, whereas more sustained adrenergic stimulation (like during exercise) does not have such an effect due to the protective role of the intact countervailing IKs current.39 In CPVT, adrenergic stimulation plays an essential role in increasing calcium leak through ryanodine receptor Type 2, triggering delayed afterdepolarizations, and VAs,40 especially from Purkinje cells.41
In contrast, in Brugada syndrome (BrS) and early repolarization syndrome (ERS), bradycardia, beta-adrenergic blockade, or vagal stimulation and fever are considered pro-arrhythmic.42–46 Conventionally, an epicardial to endocardial repolarization gradient was assumed as one of the underlying mechanisms for arrhythmia initiation.36,47,48 More recently, microstructural abnormalities of the extracellular matrix (fibrosis), particularly within right ventricular subepicardial myocardium, manifesting as epicardial regions of abnormal, fractionated potentials, were found in patients with BrS and less frequently in ERS and IVF.49–51 This suggests the presence of subtle subepicardial cardiomyopathy, rather than purely electric disease.52–56. Subepicardial conduction in right ventricular outflow tract (RVOT) epicardial regions can be further compromised by impaired Na+ current due to the SCN5A pathogenic variant, Na+ channel blockade, or pacing, leading to slow/asynchronous conduction, areas of localized block, and creating large potential difference relative to the body of the right ventricle (RV; depolarization theory).57 Excitation failure due to current-to-load mismatch and localized RV epicardial activation delay may manifest as J-point/ST-segment elevation and predispose to re-entry and PVT/VF.58 Short QT (SQT) syndrome is a rare arrhythmogenic syndrome associated with several genetic mutations, including gain-of-function mutations of potassium channels and loss-of-function mutations of calcium and sodium channels, resulting in a shortened repolarization phase of the action potential and transmural repolarization dispersion.59,60
The diagnosis of idiopathic VF requires exclusion of an underlying structural, channelopathic, metabolic, or toxicological aetiology.1 Detailed invasive mapping studies have revealed subtle microstructural changes, leading to depolarization abnormalities that allow for re-entry and VF in a subset of patients diagnosed with idiopathic VF.51,54 In patients with idiopathic VF, ES can be triggered by premature ventricular complexes (PVCs), originating from the Purkinje system, RVOT, or the papillary muscle.61 Of importance, overlapping mechanism may exist that contribute to arrhythmogenicity. For example, in Purkinje-related idiopathic VF, repolarization abnormalities may play an important role, such as in overexpression of dipeptidyl peptidase-like protein-6.62,63
6.3. External precipitation factors or triggers
External and reversible factors that may provoke an ES (see Section 8.2.2.) include acute myocardial ischaemia, electrolyte imbalance (e.g. hypokalaemia), fever (e.g. in BrS), hypothermia (e.g. in ERS), hormonal factors (e.g. hyperthyirodism), sepsis, starvation, decompensated HF, physical exertion or emotional stress, and non-compliance to medical advices/or medications. However, a specific trigger is only identified in the minority of cases.25
6.4. The autonomic nervous system
Structural heart disease is associated with an imbalance between the sympathetic and parasympathetic limbs of the autonomic nervous systems. Myocardial infarction (MI) and HF result in neural remodelling. In animal models and humans post-MI, sympathetic remodelling occurs due to injury and denervation of sympathetic fibres within scar areas, subsequent localized nerve sprouting in the border zone regions, and loss of efferent sympathetic nerves in non-infarcted areas, distal (apical) to the infarcted area.64–66 This remodelling is followed by increased systemic but decreased cardiac levels of catecholamines and regional super-sensitivity to catecholamines in the scarred (denervated) areas.66 Changes in the parasympathetic limb are less well defined, with diminished acetylcholine release at the nerve–myocyte interface caused by the high norepinephrine levels and other sympathetic cotransmitters (galanin and neuropeptide Y) as one of the suspected mechanisms.67,68 The sympathetic/parasympathetic imbalance promotes arrhythmogenesis in many ways: by both shortening and creating heterogeneities of APD, by increasing dispersion of repolarization (and consequently of refractoriness), and by promoting early and late afterdepolarizations.69
In PED patients, the role of the autonomic system is crucial and disease -specific (see Sections 6.2. and 9.2.2.).
7. Clinical presentation
Patients with clustered VA or ES, according to the definition used, can be asymptomatic or can present with a broad spectrum of symptoms. Symptoms can range from palpitations due to tolerated VT [often with VT cycle length (CL) below ICD detection] or VT terminated by anti-tachycardia pacing (ATP), through pre-syncope or syncope despite VT termination by ATP or ICD shocks, to haemodynamically unstable VT or VF, requiring advanced cardiovascular life support (ACLS), multiple external cardioversions (CVs)/defibrillations (DFs), or even arrhythmic death.70 Arrhythmias responsible for an ES are MSVT in the majority of cases (86–97%), followed by primary VF (1–21%), both MSVT/VF (3–14%) and PVT (2–8%) (Table 3 and Figure 1). In more than half of patients with an ES, the intervals between VT/VF episodes are shorter than 1 h.7,9,11,25,33,71–73
Table 3.
Definitions for VA subtypes
| Definitions of VA | |
|---|---|
| Incessant VT | Continuous sustained VT that recurs promptly despite repeated intervention for termination over several hours |
| Sustained VT | VT for at least 30 s or which requires an acute intervention for termination |
| Non-sustained VT | Run of consecutive ventricular beats persisting for at least 3 beats to <30 s duration |
| Monomorphic VT | VT with the same QRS morphology from beat to beat |
| PVT | VT showing an abrupt morphological change of the 12-lead ECG VT morphology during an ongoing VT episode |
| Bidirectional VT | VT with beat-to-beat alternation of the frontal QRS axis |
| PVT | VT with continually changing QRS morphology |
| TdP | Subtype of a PVT in the context of QT prolongation, with continually changing QRS complexes that appear to spiral around the baseline of the ECG lead in a sinusoidal pattern |
| Short coupled ventricular complexes | A PVC that interrupts the T-wave of the preceding conducted beat |
| VF | A chaotic rhythm with undulations that are irregular in timing and morphology, without discrete QRS complexes on the surface ECG |
| ES | Three or more episodes of sustained VA occurring within 24 h, separated by at least 5 min, each requiring termination by an intervention |
| Clustered VAs | Two or more sustained VA events within 3 months |
ECG, electrocardiogram; ES, electrical storm; PVC, premature ventricular complex; TdP, torsade de pointes; VA, ventricular arrhythmia; VF, ventricular fibrillation; VT, ventricular tachycardia.
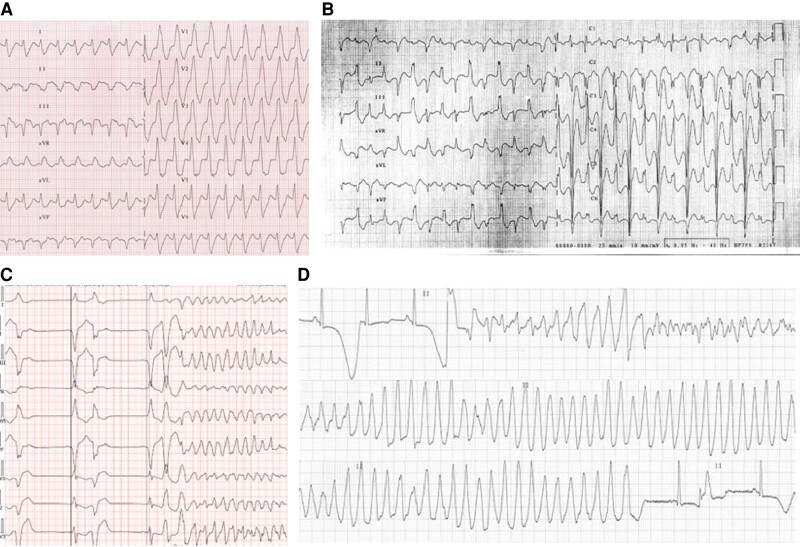
Figure 1.
Types of ventricular arrhythmias: (A) monomorphic VT, (B) bidirectional VT, (C) polymorphic VT initiated by shortly coupled monomorphic premature ventricular complexes, (D) torsade de pointes in long QT syndrome; macroscopic T-wave alternans prior to VT. VT, ventricular tachycardia.
The clinical presentation depends on multiple factors, including the underling cardiac disease, biventricular function, the type and CL of the VA, and the time to and mode of termination.74 Both cardiac function and non-cardiac comorbidities (including renal impairment, chronic pulmonary disease, and sepsis) influence the clinical presentation, electrical stability, and prognosis.75–78 Identification of patients at high risk and early transfer to a dedicated unit allowing for mechanical ventilation and mechanical circulatory support (MCS) is important.
Patients with ICDs, in whom the VA episode is terminated promptly by ATP, are likely to improve earlier than patients with prolonged VT episodes terminated by ICD shocks after ATP failure.79 Of note, even in patients with ICDs and good functional status, frequent episodes of slow, acutely tolerated and appropriately terminated VTs, can aggravate ventricular dysfunction and increase New York Heart Association (NYHA) class and cardiac mortality.80
Electrical storm can induce or exaggerate cardiac ischaemia, leading to cardiogenic shock and renal failure with metabolic acidosis and electrolyte disturbance, further promoting electrical instability.
8. Acute management
8.1. Initial evaluation, assessment of external precipitating factors, and reversible causes
Assessment of vital signs and the haemodynamic status (consciousness level, body temperature, heart rate, respiratory rate, and blood pressure), followed by continuous assessment of the rhythm and haemodynamic monitoring, is mandatory in patients presenting with an ES.18,81,82
8.1.1. History
Collecting all information on the underlying heart disease and the patient’s functional status and comorbidities are essential. Thorough family history, including a history of sudden cardiac deaths or diagnosed PED, plays a critical role, especially in young patients with the first presentation. The drug history, including all prescribed and free available drugs, in particular, if recently initiated or up-titrated, may give a first suspicion of drug-induced arrhythmias [e.g. QRS or QT-prolonging drugs (http://www.crediblemeds.org) or drugs that unmask Type 1 Brugada pattern (https://www.brugadadrugs.org)], drug–drug interaction, or electrolyte abnormalities (e.g. thiazide and loop diuretics) that may contribute to electrical instability. Recent changes in the clinical status (e.g. chest pain, dyspnoea, new signs of cardiac decompensation, infection, or palpitations) or non-cardiac symptoms (vomiting, diarrhoea, and dehydration that can contribute to electrolyte abnormalities) should be noted. Factors that may be associated with an ES should be gathered from family members/accompanying persons in case of unconscious patients.25
8.1.2. Twelve-lead electrocardiogram
Recording the 12-lead electrocardiogram (ECG) after VA termination and, whenever possible, during the VA episodes is mandatory. The ECG can be diagnostic for ST-elevation MI (STEMI) but may also show signs of myocardial ischaemia, which may be the consequence of VA. Therefore, repeated ECGs are required to evaluate whether ECG changes consistent with ischaemia (e.g. ST depression) resolve shortly after VA termination or persist. The ECG after VA termination may also point towards precipitating factors (e.g. prolonged QT interval, Brugada pattern, signs of hypokalaemia) but may also indicate a yet undiagnosed underlying heart disease (Tables 4 and 5 and Figure 2). The ECG of the VA can also contribute to the diagnosis of a potential underlying disease (e.g. bidirectional VT for CPVT or TdP for LQT) but may also provide important information on substrate location (Table 6).
Table 4.
Baseline ECG changes suspicious for precipitation factors/underlying aetiologies
| Baseline 12-lead ECG | Condition/diagnosis | |
|---|---|---|
| PED | QTc ≥ 460 ms | LQTS (including acquired LQT) |
| Type 1 Brugada ECG J-point elevation ≥2 mm with coved ST-elevation and T-wave inversion in at least one right precordial lead |
Brugada syndrome Exclude other conditions (phenocopies) |
|
| Early repolarization pattern J-point elevation ≥1 mm in ≥2 adjacent inferior and/or lateral ECG leads |
Early repolarization syndrome | |
| SHD | Pathological Q waves: >40 ms, >0.2 mV, >25% of QRS amplitude, any in V1–3 except LBBB | cCAD |
| QRS fragmentationa | cCAD, SHD | |
| ST-segment elevation : J-point elevation ≥2 mm in V2/V3 in men, ≥1.5 mm in women, or ≥1 mm in 2 other contiguous chest leads or limb leads | STEMI | |
| Epsilon wave V1–V3: low amplitude signal occurring after the QRS complex and before the onset of the T wave | ARVC, cardiac sarcoidosis | |
aAn additional R′, notching of the R wave, notching of the S wave, or the presence of multiple (>2) R waves, in the absence of a wide QRS.65
ARVC, arrhythmogenic right ventricular cardiomyopathy; cCAD, coronary artery disease; ECG, electrocardiogram; LBBB, left bundle branch block; LQTS, long QT syndrome; PED, primary electrical disease; QTc, corrected QT; SHD, structural heart disease; STEMI, ST-elevation MI.
Table 5.
Electrolyte disturbances—ECG, causes and management
| Hypokalaemia | Hyperkalaemia | |
|---|---|---|
| ECG findings |
|
|
| Causes |
|
|
| Management |
|
|
| Hypocalcaemia | Hypercalcaemia | |
|---|---|---|
| ECG findings |
|
|
| Causes |
|
|
| Management |
|
|
| Hypomagnesaemia | Hypermagnesaemia | |
|---|---|---|
| ECG findings |
|
|
| Causes |
|
|
| Management |
|
|
ACE, angiotensin-converting enzyme; AF, atrial firbrillation; ARB, angiotensin receptor blocker; AV, atrioventricular; BB, beta-blocker; ECG, electrocardiogram; PVC, premature ventricular complex; PVT, polymorphic ventricular tachycardia; TdP, torsade de pointes; VF, ventricular fibrillation; VT, ventricular tachycardia.
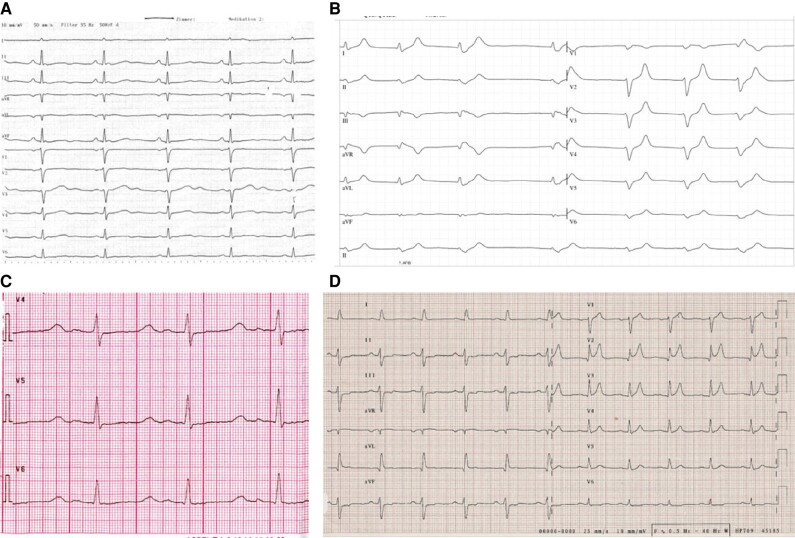
Figure 2.
Manifestations of electrolyte-level disturbances on ECG: (A) hypokalaemia, (B) hyperkalaemia, (C) hypocalcaemia, (D) hypercalcaemia. ECG, electrocardiogram.
Table 6.
Twelve-lead ECG during VT
| ECG during VT | Description | Suggestive cause of ES/site of origin |
|---|---|---|
| TdP | PVT with ‘QRS twisting' | Acquired or congenital LQT |
| PVT | VT with continually changing QRS morphology | Acute ischaemia, primary electrical disease (BrS, SQT, IVF, CPVT, ERS) |
| Bidirectional VT | Alternating QRS morphology (beat-to-beat) | CPVT, digitalis intoxication, Andersen–Tawil syndrome |
| LBBB-like and inferior axisa | ARVC, idiopathic VT from the RVOT (normal heart) | |
| RBBB-like VT with left superior axis (LAH-like, less frequently right inferior axis LPH-likea)83 | Narrow QRS (100–140 ms), short RS interval (onset of R wave to nadir of S wave of 60–80 ms), r < R′ in V1 | Left ventricular fascicular VT (usually normal heart) |
| QRS broad (≥150 ms), absence of rsR′ in V1 | Papillary muscle VT | |
| QRS broad (≥155 ms), R ≥ s in V5, may be positive QRS concordance | Peri-mitral VT | |
| Fast (>200 b.p.m.) LBBB-like VT, with rapid downstroke of S wave in the anterior precordial leads, QRS during sinus rhythm (usually broad) may be identical to QRS duringa VT84,85 | Short QRS onset—the R-wave peak time (R-wave peak time) and fast downstroke of S wave in V1–V2 | Bundle branch re-entrant tachycardia (SHD) |
| RBBB-like VT with pseudo-delta wave and broad RS interval,4 absence of q waves in inferior leads and presence in Leada I86–88 | Pseudo-delta wave ≥34 ms (interval from the earliest ventricular activation to the earliest fast deflection in any precordial lead) R-wave peak time in V2 ≥85 ms Shortest RS complex ≥121 ms (in any precordial lead) |
VT with epicardial origin (SHD) |
aLBBB-like pattern is characterized by a negative net amplitude of QRS complexes in leads V1 and/or V2 and RBBB-like by a positive net QRS amplitude in these leads.
ARVC, arrhythmogenic right ventricular cardiomyopathy; BrS, Brugada syndrome; CPVT, catecholaminergic polymorphic ventricular tachycardia; ECG, electrocardiogram; ES, electrical storm; ERS, early repolarization syndrome; IVF, idiopathic ventricular fibrillation; LAH, left anterior hemiblock; LBBB, left bundle branch block; LPH, left posterior hemiblock; LQT, long QT; PVT, polymorphic ventricular tachycardia; RBBB, right bundle branch block; RVOT, right ventricular outflow tract; SHD, structural heart disease; SQT, short QT; TdP, torsade de pointes; VT, ventricular tachycardia.
8.1.3. Documentation of ventricular arrhythmia and immediate implantable cardioverter-defibrillator interrogation
Evaluation of the appropriateness, necessity, and effectiveness of ATP and ICD shocks is required in all patients with an ICD—(Flowcharts 1 and 2). Collecting the available information on the initiation and mode of termination of all VA episodes from 12-lead ECG, wearables, cardiac monitor rhythm stripes, tracings stored in automated external defibrillator, or intra-cardiac electrograms obtained from ICD interrogation is crucial for the acute and chronic management of ES.50,56 If PVC-induced VF is likely, continuous recording of the 12 lead ECG is helpful to capture the morphology and to determine the likely site of origin in case of unifocal PVCs and helps to mark sites just in case of electrophysiologic study and ablation.89
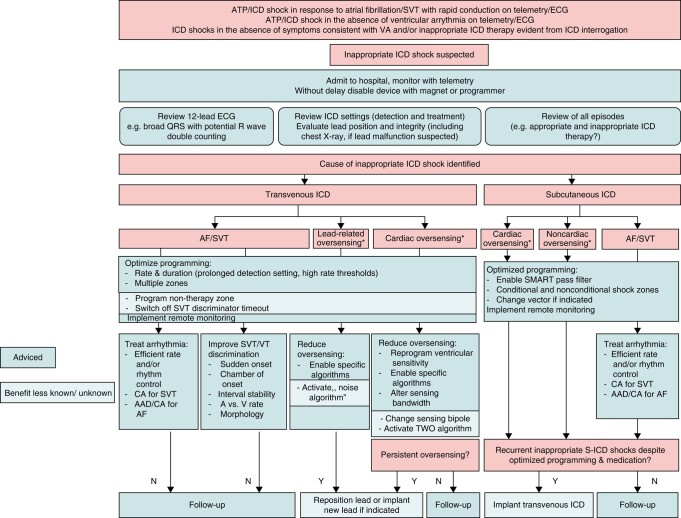
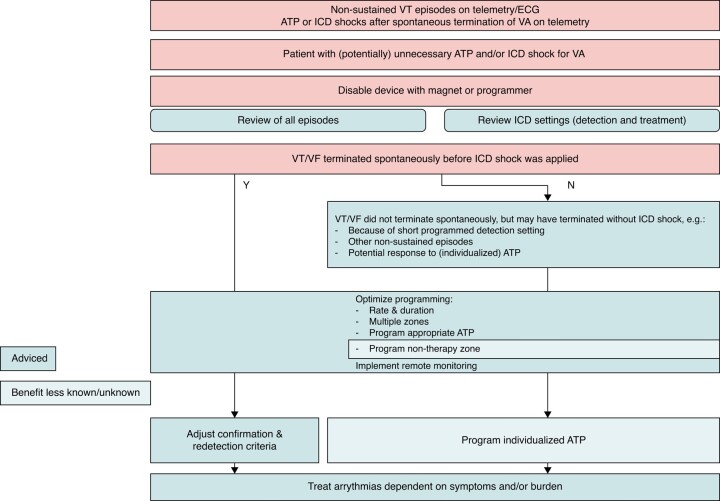
Flowchart 1.
ICD interrogation and reprogramming—inappropriate therapy suspected.139*Cardiac oversensing: T-wave oversensing (most common cause of inappropriate shocks in S-ICD); P-wave oversensing; R-wave double counting. #Lead-related oversensing: conductor fracture; insulation breaches; connection problems; lead–lead interaction; air entrapment in the header. @Extracardiac oversensing: myopotentials from skeletal muscle activity (diaphragmatic, pectoral, intercostal rarely); electromagnetic interference (alternating current line breakdown, interference from medical sources). AAD, anti-arrhythmic drug; AF, atrial fibrillation; ATP, anti-tachycardia pacing; CA, catheter ablation; ECG, electrocardiogram; ICD, implantable cardioverter-defibrillator; SVT, supraventricular tachycardia; S-ICD, subcutaneous ICD; TWO, T-wave oversensing.
Flowchart 2.
ICD interrogation and reprogramming—unnecessary therapy suspected.139 ICD, implantable cardioverter-defibrillator.
8.1.4. Blood tests
Evaluation of serum electrolyte levels (Na+, K+, Mg2+, and Ca2+) is part of the initial evaluation.25,72,73,90,91 Hypomagnesaemia and/or hypokalaemia can be associated with TdP. Initial blood tests should also include thyroid-stimulating hormone to exclude hypothyroidism or hyperthyroidism as a potential trigger of ES (e.g. in amiodarone-induced thyrotoxicosis92). In addition, renal77 and liver function tests, impairment of which may lead to drug toxicity (e.g. sotalol), and blood tests for infection and inflammation may provide important diagnostic information on circumstances that require prompt treatment.
Initial lab testing should also include serum troponin, even though following ES, the diagnostic performance of cardiac injury markers alone is limited. In general, VA, in particular, if poorly haemodynamically tolerated, can cause myocardial injury and may lead to an increase in these markers.93 Therefore, troponin should be monitored sequentially and interpreted in the context of symptoms (angina pectoris), and ECG changes to identify and treat acute coronary syndrome (ACS). Toxicology screening for cocaine, alcohol, and other drugs may be appropriate in selected cases as abuse of those agents may lead to VA and even SCD.94,95 According to ESC guidelines, blood should be collected for potential later analysis.1
8.1.5. Coronary angiogram, cardiac imaging, and additional diagnostic studies
Transthoracic echocardiography (TTE) should be performed early to assess cardiac function, dimensions, and disease progression in patients with known cardiac disease and to identify SHD in those without prior history of cardiac disease. Urgent coronary angiography (CAG) is essential in case of STEMI or electrical instability with suspicion of ongoing myocardial ischaemia.96 Of note, termination of incessant VT with intracoronary administration of radiographic contrast media, with subsequent haemodynamic stabilization, has been reported.97 If acute myocarditis is suspected, endomyocardial biopsy (EMB) is the gold standard for the diagnosis, which has important implications in cases of, e.g. giant cell myocarditis.98 18F-fluorodeoxyglucose positron emission tomography can be useful in diagnosing arrhythmic myocarditis or cardiac sarcoidosis (CS), particularly when cardiac magnetic resonance (CMR) is contraindicated and is unsuitable because of irregular rhythm or ICD–related artefacts or when there is a diagnostic mismatch between CMR and EMB.99,100
Advice Table 1.
Initial evaluation—general aspects
| Evidence | Strength | |
|---|---|---|
| Advice TO DO | ||
| Admit patients to a dedicated unit allowing multi-disciplinary patient management and continuous monitoring18 | OBS |

|
| Assess vital signs and haemodynamic status, including conscious level, heart rate, respiratory rate, blood pressure, body temperature, and arterial haemoglobin oxygen saturation. | OPN |

|
| Investigate for external precipitating factors and reversible causes77,90–92 | OBS |

|
| Collect data on current drug treatment and prior drug failure for VA | OPN |

|
| Record a 12-lead ECG of VA, whenever possible | OPN |

|
| Record a 12-lead ECG after VA termination and repeat 12-lead ECG at least on a daily basis in selected cases (ST changes, QT prolongation) | OPN |

|
| Perform TTE after VA termination For initial evaluation in patients without known disease For disease progression in patients with known structural cardiac disease |
OPN |

|
| Evaluate appropriateness and necessity of ICD therapies101–103 | OBS |

|
| Reprogramme and/or inactivate ICD therapies in case of malfunction, inappropriate, or unnecessary therapies104–106 | OBS |

|
| Collect all available information on type, initiation, and termination of all VA episodes, including telemetry strips and recordings from cardiac implantable electronic devices (CIEDs)89,101 | OBS |

|
| Perform urgent CAG in case of STEMI107,108 Persistent electrical instability and suspected ongoing ischaemia |
OBS |

|
| May be appropriate TO DO | ||
| Initiate continuous 12-lead ECG monitoring in case of PVC-induced PVT/VF to determine similarity and likely site of origin of PVCs89 | OBS |

|
| Advice NOT TO DO | ||
| Do not perform routine toxicology screening | OPN |

|
8.2. Treatment
8.2.1. Electrical storm with haemodynamic instability
In case of haemodynamic instability, initiation of immediate ACLS is indicated.1,109 Unstable patients need to be managed by an interdisciplinary team, including a cardiologist with expertise in cardiac electrophysiology and cardiac implantable devices, an anaesthesiologist or intensive care specialist, and, in selected cases, a HF specialist or a cardiac surgeon. Patients may be haemodynamically unstable because of frequent episodes of VT or incessant VT with haemodynamic compromise. Haemodynamical instability may also persist after VT termination due to a delayed recovery after long episodes of VT and/or several ICD shocks or CVs, in particular in patients with poor cardiac function.
Patients with ES and ongoing haemodynamically unstable VT or VF should be managed according to the general principles of ACLS (Figure 3).110 Basic airway techniques and a stepwise approach (bag-mask ventilation, supraglottic device or intratracheal intubation, and mechanical ventilation75) are advised until adequate ventilation is achieved. High-quality chest compressions with minimal interruption and early DF remain priorities. Rapid DF or CV may be delivered from the ICD or with an external defibrillator. When using external DF/CV in ICD patients, patches or paddles should be placed at least 8 cm from the ICD and, if possible, in a front-to-back position.110 External CV was shown to be similarly safe but superior to ICD shock for restoring sinus rhythm in patients with atrial fibrillation (AF) in a recent meta-analysis, but data on DF or CV for VT/VF are lacking.111 In a cluster-randomized trial including 405 patients with refractory VF, double sequential external defibrillation (DSED; rapid sequential shocks from two defibrillators) and vector change (VC) DF (switching DF pads to an anterior-posterior position) were associated with higher survival to hospital discharge and DSED (but not VC) with a better neurologic outcome.112 In patients with a non-shockable rhythm, adrenaline (1 mg i.v./i.o.) should be used immediately and repeated every 3–5 min during ACLS; in shockable rhythm, it should be administered after the third DF/CV and repeated every 3–5 min in case of persistent arrhythmia. Amiodarone (300 mg iv/io) is advised after three shocks in patients with VF/PVT, followed by 150 mg iv/io after five shocks. If amiodarone is unavailable, lidocaine (100 mg iv/io) can be alternatively used after three shocks and repeated (50 mg iv/io) after five DFs.
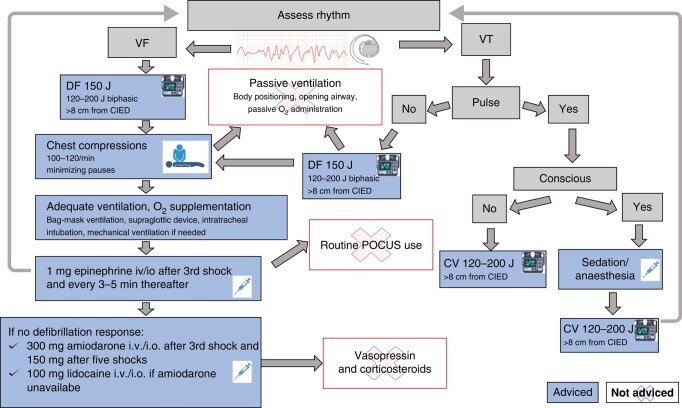
Figure 3.
ACLS in an electrical storm.110,113 ACLS, advanced cardiovascular life support; CV, cardioversion; DF, defibrillation; POCUS, point of-care ultrasound.
Conscious patients require deep sedation or anaesthesia before delivering synchronized CV (see Section 8.2.4.). Guidelines-recommended management of patients with VT and a palpable pulse advices a 120–150 J for the initial CV.110 The energy can be increased if the first shock fails.110 Even in haemodynamically tolerated VT, prompt termination, preferably by CV, is recommended by the current ESC guidelines, as haemodynamic deterioration may occur.1 Pharmacological treatment may be an alternative if the risk of sedation/anaesthesia is high (see Section 8.2.5.). Mechanical circulatory support may be appropriate in selected patients in whom conventional cardiopulmonary resuscitation (CPR) is not effective114 (see Section 8.2.6.). The role of therapeutic hypothermia in patients with ES is unknown.
Advice Table 2.
Advanced life support
| Evidence | Strength | |
|---|---|---|
| Advice TO DO | ||
| Apply standardized advanced life support (ALS) algorithms including high-quality chest compression with minimal interruption109,115 | RCT |

|
| Use vasopressors (epinephrine) early for non-shockable cardiac arrest following ES116–118 | RCT |

|
| May be appropriate TO DO | ||
| MCS may be appopriate when haemodynamical stabilization can not be achieved by conventional therapy119 | OBS |

|
8.2.2. Disease-specific aspects
Optimal HF management is mandatory and may help to stabilize the rhythm.120,121 In case of suspicion of ongoing myocardial ischaemia,122 urgent CAG is essential and is indicated in case of STEMI following current guidelines.96 In patients with cCAD but no STEMI, the potential benefit of (complete) revascularization should be carefully weighed against risk.123,124 Noteworthy, MSVT is rarely caused by ischaemia,125 and ischaemic evaluations in patients with monomorphic VT storm without ACS did not improve procedural outcomes or mortality after ablation.126
In the rare case of acute giant cell myocarditis, promptly initiated immunosuppression can be curative.127 In patients with CS and VA, corticoid therapy is advised by the ESC Working Group on Myocardial and Pericardial Diseases.127 Data on the acute effect of steroids in patients with active CS and ES are lacking, and AAD or RFCA may be needed.128 Anti-inflammatory therapy with corticosteroids or other immunosuppressive treatments may also be appropriate in myocarditis, if an autoimmune mechanism is suspected (circulating serum cardiac auto-antibodies and ongoing inflammation) and no active viral replication has been detected.129 In case of electrical instability in the inflammatory phase, AAD therapy and RFCA in case of drug-refractory storm may be appropriate. In a small cohort of patients with biopsy-proven chronic active myocarditis and drug-refractory VTs, RFCA effectively controlled MSVT.130
Acute illness and fever should be aggressively treated with fever-reducing medications, particularly in patients with BrS.131 Emotional stress should be considered as the potential trigger in patients with CPVT, and elevated sympathetic tone needs to be addressed in all patients with ES (see Sections 8.2.5.2. and 8.2.8.). Bradycardia may facilitate VA initiation, in particular in the setting of QT prolongation, and may require appropriate measures to increase heart rate (see Sections 8.2.3., 8.2.5.2., and 8.2.9.). Of note, the corrected QT (QTc)/corrected JT (JTc) interval can be significantly prolonged after resuscitation or in the setting of hypothermia, independently from QT-prolonging drugs, and normalization should be only expected beyond Day 6 after the acute event.132,133 Any potentially offending drug must be withdrawn, and drugs known to prolong the QT interval, except AADs used to treat the ES, must be avoided. Early correction of serum electrolyte levels (K+, Mg2+, and Ca2+) is indicated134–136; in cases of TdP, i.v. magnesium is effective even in the absence of hypomagnesaemia.137 I.v. potassium is usually effective, and K levels should be brought to the upper limits of normal range.
8.2.3. Implantable cardioverter-defibrillator reprogramming
Inappropriate ICD therapy can be due to supraventricular tachycardias or AF with a rapid ventricular response (Figure 4). Inappropriate ICD therapy can also result from cardiac or extracardiac oversensing or lead defects. Unnecessary ICD therapy may be triggered by non-sustained VTs, particularly if short detection times are programmed. In these cases, ICD therapies must be interrupted and prevented by disabling and reprogramming the device.104 If there is no immediate access to a device programmer and ICD malfunction or inappropriate ICD treatment is suspected from the telemetry or ECG recordings, ICD therapy can be transiently disabled by placing a magnet on the device can (although this is a manufacturer and model-specific feature, which can be programmable).
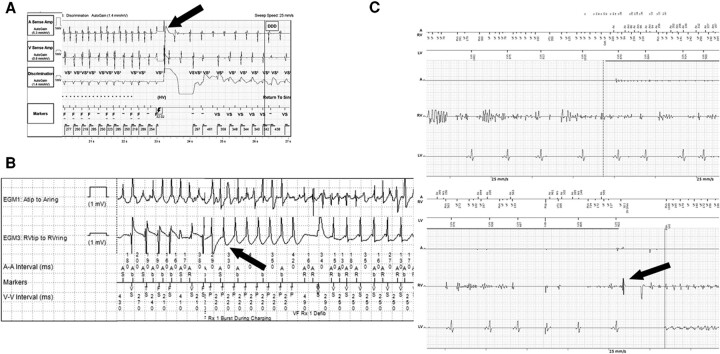
Figure 4.
Inappropriate ICD therapy. (A) Fast conducting AF misdetected as VF with ICD shock (arrow), (B) fast conducting AF misdetected as VT with ATP delivered (arrow), (C) noise caused by damaged RV electrode misdetected as VF with ICD shock (arrow). Shock initiates VF. A, atrial signal; AF, atrial fibrillation; Aring, ring pole of atrial electrode; Atip, tip pole of atrial electrode; ATP, anti-tachycardia pacing; CRT, cardiac resynchronization therapy; EGM, intra-cardiac electrogram; F, ventricular fibrillation detected; ICD, implantable cardioverter-defibrillator; LV, signal received by electrode in left ventricle in CRT device; RV, signal received by electrode in the right ventricle; RVring, ring pole of electrode in the right ventricle; RVtip, tip pole of electrode in the right ventricle; STIM, stimulation; VF, ventricular fibrillation; VS or RVs, ventricular sensed event; VT, ventricular tachycardia.
Recurrent, appropriate ICD shocks may not only be due to ineffective ATP or CV/DF and acceleration of VT by ATP (e.g. RAMP protocol set as a first mode) but also be due to programmed low VF detection rates, in particular if ATP during charging is not available or disabled.104 Programming of longer detection times and longer and less aggressive ATP therapies may reduce or avoid ICD shocks. In particular, in patients with haemodynamically well-tolerated VT, terminated by ICD shocks, disabling the device therapy and termination of episodes by commanded ATP or AADs are advised. Recurrent ICD shocks are traumatic events associated with increased mortality, and the related hyperadrenergic state may trigger recurrent episodes. Accordingly, patient sedation (see Section 8.2.4.) and inactivation of unnecessary ICD shocks, even if appropriate, may mitigate the ES.105,106
In addition, and depending on the mode of VA initiation, increasing the lower rate thresholds for anti-bradycardic pacing to avoid bradycardia and short-long-short sequences may prevent VA episodes101—(see Flowcharts 1 and 2; Section 8.2.9.). Although adequate LV or biventricular pacing of CRT is desirable, recently initiated effective LV stimulation may be arrhythmogenic, and disabling LV pacing may sometimes terminate or mitigate the ES.138
8.2.4. Deep sedation and mechanical ventilation
In conscious patients with recurrent ICD shocks or symptomatic VTs, mild-to-moderate sedation is essential for patient comfort and to reduce sympathetic tone (Table 7). Deep sedation and mechanical ventilation have successfully controlled drug-refractory ES.140,141 An acute response, defined as the termination of ES within 15 min without recurrent episodes over the following 24 h, occurred in 47% of a mixed cohort of 116 ES patients who were refractory to AADs. Response to deep sedation was an independent predictor of in-hospital survival.141
Table 7.
Medication for sedation in ES patients
| Sedation90–92 | ||
|---|---|---|
| Agents | Initial dose | Infusion rate |
| Benzodiazepines | ||
| Midazolam | 0.01–0.05 mg/kg, repeat q5–15 min | 0.02–0.1 mg/kg/h, titrate up/down by 25–50% |
| Lorazepam | 0.02–0.04 mg/kg | 0.01–0.1 mg/kg/h (not exceed 10 mg/h) |
| Propofol | 0.8–1.2 mg/kg | 5–50 μg/kg/min (0.3–3 mg/kg/h) Up-titrate every 5–10 min by 5–10 μg/kg/h |
| Opioids | ||
| Fentanyl | 1–2 μg/kg | 1–2 μg/kg/h |
| Remifentanyl | 0.5–1.5 μg/kg | 0.05–2 μg/kg/min |
| Dexmedetomidine | 1 μg/kg over 10 min | 0.2–0.7 μg/kg/h |
ES, electrical storm.
8.2.4.1. Agents used for (deep) sedation
Benzodiazepines. Short-acting agents like midazolam are commonly used in patients with an ES. With no negative inotropic effect, benzodiazepines are considered first-line sedation drugs, often used for initial mild sedation.140,142
Propofol. Propofol is a potent intravenous hypnotic agent used for deep sedation in the context of an ES.140,143 Propofol may substantially inhibit sympathetic nerve activity; 144 it has a rapid onset of action within 2–3 min, a short half-life of 1–3 h, and good amnestic potential. This agent must be used cautiously in patients with SHD because of its negative inotropic effect.
In a retrospective study of 46 subjects presenting with VT storm or incessant VT, 15 patients refractory to AAD underwent propofol-induced deep sedation. After propofol administration, a complete resolution of VT/VF within minutes to hours was achieved in 12 patients (80%), and partial resolution in 2 (13%), with no VA recurrence after 3 h.140 Hypotension was the most common side effect managed primarily with norepinephrine infusion. One case of necrosis of the caecum was attributed to the complications of norepinephrine. Uncommon complications are hypertriglyceridaemia, pancreatitis, allergic reactions, and propofol-related infusion syndrome, which is an often lethal complication of high-dose propofol infusions, characterized by severe metabolic acidosis, bradyarrhythmias, acute renal failure, rhabdomyolysis, and hyperkalaemia.145 Propofol may occasionally significantly prolong QT interval.146
Opioids. Short-acting opioid agents are also considered first-line treatment because of their mild negative inotropic and potent analgesic effects.74,147 Fentanyl/remifentanil are used for the induction of general anaesthesia. The onset of action of fentanyl is <2 min, with a peak of 2–5 min after administration. The half-life is 90 min, and the duration of action is 30–60 min. Remifentanil has a distribution half-life of 2–4 min and elimination half-time of 10–20 min. Its offset of action (3–5 min) is not affected by the duration of drug infusion (no accumulation with repeated and prolonged administration), and its pharmacokinetics is not affected by renal nor hepatic impairment.
Dexmedetomidine. Dexmedetomidine is a highly selective α2-adrenoreceptor agonist with a short half-life (6 min) that reduces sympathetic activity by enhancing central vagal tone and inhibiting presynaptic catecholamine release. It provides both sedation and analgesia without respiratory depression and was shown to decrease the incidence of VT in critically ill patients.148 However, it should be used with caution as it may cause severe hypotension and bradycardia.
8.2.5. Pharmacotherapy for the acute management of electrical storm
8.2.5.1. Structural heart disease
Anti-arrhythmic drugs are the cornerstone of therapy for the acute management of ES (Table 8). The specific AAD treatment depends on the type of VA, the (likely) underlying aetiology, patient’s characteristics, including comorbidities and patient-specific contraindications, and the availability of drugs. In patients with SHD, suppressing sympathetic tone with beta-blockers (BBs), preferably non-selective (e.g. propranolol), is the first-line treatment unless contraindicated.26 In a randomized controlled trial (RCT), the combination of i.v. amiodarone and oral propranolol was safe, effective, and superior to the combination of i.v. amiodarone and oral metoprolol in the management of ES in ICD patients.149 In patients with an ES due to VT/VF after a recent (<3 months) MI, sympathetic blockade with i.v. esmolol or i.v. propranolol (160–320 mg/24 h) or left stellate ganglion blockade was superior to lidocaine i.v (followed by procainamide i.v. or bretylium, if not effective) for VT/VF suppression and survival.26 In patients with recurrent PVT in the early post-MI phase [but also post-coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI)], quinidine has been reported to be effective after BB and amiodarone treatment failure.150,151 In patients with recurrent, haemodynamically unstable VT despite amiodarone, landiolol (ultra-short-acting β1-selective blocker) was effective for arrhythmia suppression in two smaller studies.152,153
Table 8.
Pharmacotherapy for acute treatment of patients with ES
| Acute treatment | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Vaughan Williams Class | Drug | Channels affected | Dose (i.v.) | Pharmacokinetics | Specific use | Caution | Monitoring | Adverse effects | ||
| Half-life | Desired plasma concentration | Metabolism | ||||||||
| Class I | Quinidine | INa, IKr, ITo, M, α | Loading dose: 800 mg/50 mL Maintenance intravenous: 50 μg/min |
6–8 h | 1.5–3.5 μg/mL | Hepatic | VT, VF, ES after MI, PCI, CABG, BrS, SQT syndrome IVF |
Severe bradycardia and/or high-degree AV block in the absence of a pacemaker, myasthenia gravis, decompensated heart failure | ECG (QRS duration and QT interval), heart rate, platelet count | QTc prolongation, TdP, QRS prolongation, increase in defibrillation threshold, hypotension, bradycardia, heart failure exacerbation, diarrhoea, immune thrombocytopenia |
| Procainamide | INa, IKr ganglionic block | 100 mg bolus, can be repeated after 5 min if no effect, alternatively 10–17 mg/kg administered at a rate of 20–50 mg/min, max 500–750 mg (max 50 mg/min) and then 2–6 mg/min | 3–4 h | 4–12 μg/mL | Hepatic and renal | VT, pre-excited AF | Severe sinus node disease, severe AV conduction disturbance, previous myocardial infarction, reduced LVEF, hypotension, BrS, myasthenia gravis | ECG (QRS duration and QT interval), blood pressure | Rash, myalgia, vasculitis, agranulocytosis, hypotension, bradycardia, QT prolongation | |
| Lidocaine | INa | 50–200 mg bolus and then 2–4 mg/min (25–50 μg/kg/min) | 7–30 min | 2–6 μg/mL | Hepatic | Ischaemic VT/VF | Severe sinus node/AV heart block in the absence of pacemaker, cardiogenic shock, hypersensitivity to lidocaine or amide-type local anaesthetist | ECG (PR interval and QRS duration), temperature | Hypotension, confusion, tremors, methemoglobinaemia, malignant hyperthermia, anaphylactoid reactions | |
| Mexiletine | INa | Intravenous: not recommended Loading dose: 400 mg initially followed by 600 mg in the first 24 h Maintenance dose: 600–1200 mg |
10–14 h | 0.6–1.7 mg/mL | Hepatic | VT/VF, LQT3 LQT2 |
Cardiogenic shock, pre-existing sinus node disease, or second/third-degree AV block without pacemaker, hypotension, history of seizures | ECG (QT interval), hepatic function | Ataxia, tremors, hypotension, angina | |
| Class II (BBs) | Esmolol | β1-receptor | Bolus dose: 0.5 mg/kg for 1 min Infusion: 25–50 μg /kg/min up to 250 μg /kg/min (titrate every 5–10 min) |
5–10 min | NA | RBC esterase | VT | Severe sinus bradycardia/severe sinus node disease/AV conduction disturbances without pacemaker, Decompensated heart failure, Prinzmetal’s angina, asthma/chronic obstructive airway disease, myasthenia gravis | Heart rate, blood pressure | Bronchospasm, hypotension, sinus bradycardia, AV block, fatigue, depression |
| Propranolol | Non-selective BB | Bolus dose: 0.15 mg/kg over 10 min, 160 mg/24 h | 3–6 h | NA | Hepatic | VT, PVCs, LQT |
||||
| Metoprolol | β1-receptor | Bolus dose: 2–5 mg every 5 min, up to 3 doses in 15 min | Tartarate: 3–4 h Succinate: 3–7 h |
NA | Hepatic | VT, PVCs | ||||
| Class III | Amiodarone | INa, ICa, IKr, IK1, IKs, Ito, α, β | Loading dose: 5 mg/kg in 20 min to 2 h, 2–3 times in 24 h and then 600–1200 mg/ 24 h 8–10 days | 4–14 weeks | 1–2.5 μg/mL | Hepatic | VT, VF, PVCs | Concomitant digoxin administration, concomitant warfarin administration | Heart rate, blood pressure | Increases DFT, hypotension, bradycardia, AV block, QT prolongation, TdP (rare), hypothyroidism/hyperthyroidism, nausea, photosensitivity, skin discolouration, peripheral neuropathy, tremor, hepatitis, pulmonary fibrosis/pneumonitis |
| Beta agonist | Isoproterenol | β1 and β2 | 0.5–10 μg/min | 2.5–5 min | NA | Hepatic and pulmonary | IVF TdP, ES in Brugada syndrome, SQT syndrome, VAs secondary to AV block |
Coronary artery disease, myocardial ischaemia convulsions, renal disease, hyperthyroidism | Heart rate, blood pressure, ECG for ST-elevation | Tachycardia, hypertension, angina, tremors |
AF, atrial fibrillation; BB, beta-blocker; BrS, Brugada syndrome; CABG, coronary artery bypass grafting; DFT, defibrillation threshold testing; ECG, electrocardiogram; ES, electrical storm; IVF, idiopathic ventricular fibrillation; LVEF, left ventricular ejection fraction; LQT, long QT; MI, myocardial infarction; NA, not applicable; PCI, percutaneous coronary intervention; PVC, premature ventricular complex; QTc, corrected QT; RBC, red blood cell; SQT, short QT; TdP, torsade de pointes; VF, ventricular fibrillation; VA, ventricular arrhythmia; VT, ventricular tachycardia.
Amiodarone i.v. (5 mg/kg/20 min) is frequently used in patients with SHD who present with an ES. It terminated haemodynamically tolerated VT in 38% of patients, the majority (80%) with SHD.154 Effects of oral vs. intravenous loading with amiodarone may differ; combined i.v. and oral loading may shorten the time to VA control compared with oral loading alone and may lower the cumulative dose required.155 Patients already on amiodarone therapy may benefit from acute reloading with this AAD.142
In patients with SHD and haemodynamically tolerated VT without acute ischaemia, procainamide can also be used. In the PROCAMIO trial, procainamide was superior to amiodarone in terminating haemodynamically tolerated VT of unknown aetiology, with fewer major adverse events.154 Lidocaine is only moderately effective (and worse than procainamide i.v.156 and sotalol i.v.157) in stable MSVT but has been considered potentially useful in the context of acute ischaemia (bolus 1–1.5 mg/kg followed by infusion rate of 0.02 mg/kg/min).158 Its prophylactic use had little or no effect on mortality or VF in AMI patients in a meta-analysis of controlled RCTs.159 As negative inotropic effects of lidocaine have been demonstrated in animal studies,160 the drug needs to be used with caution in patients with impaired ventricular function. Ranolazine, an antianginal and anti-ischaemic drug, also exerts anti-arrhythmic properties, presumably due to the inhibition of the late sodium and the delayed rectifier potassium current.161 In a double-blind RCT including 1012 ICD patients with SHD (54% with cCAD), ranolazine significantly reduced the risk of recurrent VT or VF requiring ICD therapy (pre-specified secondary endpoint) without an impact on mortality during a mean follow-up of 28 ± 16 months.162 The use of other AADs depends on the underlying aetiology and the type of VA.163
8.2.5.2. Primary electrical disease
In patients with PED, treatment of an ES is disease specific. In LQTS, it involves the immediate elimination of eventual triggers [acquired LQTS (aLQTS) and congenital LQTS (cLQTS)], BBs, ideally non-selective (nadolol or propranolol), intravenous extracellular magnesium and potassium supplementation (aLQTS and cLQTS),134,135,137 isoproterenol (aLQTS), mexiletine (cLQTS), and temporary pacemaker therapy with supra-normal rates (aLQTS and cLQTS Type 2).3 Class III AADs should be avoided.
In BrS and IVF, an ES is best treated with isoproterenol i.v.164–166 Quinidine with or without isoproterenol has also been used successfully in individual cases.167–172 Class Ic drugs should be avoided. Short QT syndrome is very rare, and data regarding the treatment of ES are very limited; isoproterenol may be efficient in such cases.173
In CPVT, ES is rare and almost exclusively triggered by adrenergic stressors (including erroneous administration of epinephrine during resuscitation efforts). Treatment should therefore be directed towards the radical removal of all adrenergic triggers. Beta-blockers remain the first line of therapy, and epinephrine should be avoided, including in the setting of cardiac arrest/resuscitation.174
In all inherited arrhythmic syndromes or arrhythmogenic cardiomyopathies, where adrenergic stress is causally involved, the ultimate therapeutic option is deep anaesthesia (see Section 8.2.4.).
8.2.6. Mechanical circulatory support
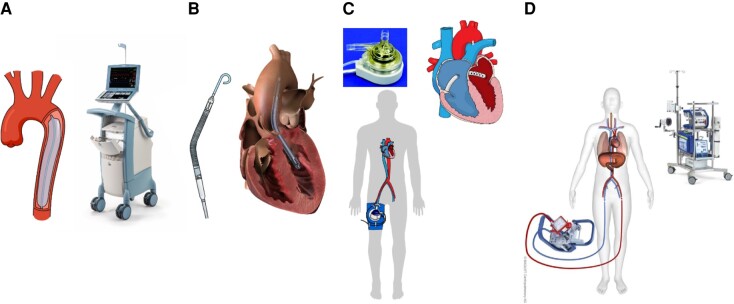
Temporary MCS may be beneficial in treating life-threatening, refractory, haemodynamically non-tolerated VA, providing maintenance of organ perfusion while allowing for the treatment of the precipitating arrhythmia. However, MCS is associated with non-negligible rates of complications (vascular access-related, bleeding, etc.), procedural logistics/complexity/availability, and increased costs. The lack of robust evidence on MCS use in the setting of ES makes it difficult to draw any definitive conclusions about its role in this scenario.
Current temporary modalities for MCS include the intra-aortic balloon pump (IABP), the Impella devices (Abiomed, Danvers, MA, USA), Tandem Heart left atrial-to-femoral bypass (Cardiac Assist Inc., Pittsburgh, PA, USA), extracorporeal membrane oxygenation (ECMO), and peripheral cardiopulmonary bypass. Their main characteristics are depicted in Table 9 and Figure 5. Mechanical circulatory support device selection depends on the patient’s characteristics, required support level, local expertise, and logistics. Notably, the use of temporary MCS is highly complex and should only be performed by experienced multi-disciplinary teams in specialized centres. The role of temporary MCS in ES has not been extensively investigated. Mechanical circulatory support may be helpful in patients presenting with ES in the following scenarios:
Table 9.
Types of mechanical cardiac support
| Pros | Cons | Contraindications | |||
|---|---|---|---|---|---|
| IABP | Indirect LV support by aortic counterpulsation, with afterload reduction and diastolic aortic pressure augmentation | Percutaneous arterial access (7–8 Fr) Modest cardiac output increase (0.5–1.0 L/min) |
Simple set-up Indirectly unloads LV Availability Affordable Low complication rate |
Very limited LV support Requires stable rhythm |
Moderate-severe aortic regurgitation Severe peripheral artery disease Aortic dissection |
| Impella CP | Microaxial continuous anterograde flow pump LV aorta | Maximum average flow 3.7 L/min Percutaneous arterial access (femoral/axillary) Introducer diameter 14 Fr Pump motor 14 Fr |
Relatively simple set-up and implantation Unloads LV Availability Percutaneous removal |
Partial LV support Electromagnetic interference in mapping system. Difficult catheter manipulation during ablation May require transeptal access for CA High costs |
Moderate-severe aortic regurgitation Mechanic aortic prosthesis LV thrombus Severe peripheral artery disease Severe RV failure |
| Impella 5.5 | Microaxial continuous anterograde flow pump LV aorta | Maximum average flow 5.5 L/min Surgical axillary cut-down Introducer diameter 23 Fr Pump motor 19 Fr |
Full LV support Unloads LV Prolonged support duration Allows early mobilization |
Requires surgical team/complex logistics Surgical insertion and removal High costs |
Moderate-severe aortic regurgitation Mechanic aortic prosthesis LV thrombus Severe peripheral artery disease Severe RV failure |
| Impella RP | Type of MCS | Main characteristics | Technical details | Anecdotical experience in ES or VT ablation Only available in selected sites High costs |
Mechanical valves, severe valvular stenosis/regurgitation of the tricuspid or pulmonary valve Right atrium or vena cava thrombus Presence of a vena cava filter or caval interruption device |
| TandemHeart | Left atrial-to-femoral artery bypass using external centrifugal pump | Percutaneous or surgical access Transseptal puncture required Generated output up to 5 L/min Inflow cannula 21 Fr Outflow cannula 15 Fr |
LV support Indirectly unloads LV Prolonged support duration |
Complex logistics. Multi-disciplinary team May impede transeptal approach for CA Large bore cannulas |
Moderate-severe aortic regurgitation RV failure Ventricular septal defect Severe peripheral artery disease |
| VA-ECMO | Cardiopulmonary support system integrated by a centrifugal pump and an oxygenation membrane | Percutaneous/surgical vascular access 17–21 Fr outflow cannula 19–25 Fr inflow cannula Maximum output up to 8 L/min |
Full biventricular support Prolonged support duration Default choice in isolated RV failure May be percutaneously removed |
Complex logistics. Multi-disciplinary team Requires often arterial distal perfusion cannula to prevent leg ischaemia High complication rates |
Severe aortic regurgitation Aortic dissection Severe peripheral artery disease (in peripheral cannulation) Uncontrollable bleeding or contraindications to systemic anticoagulation |
ES, electrical storm; IABP, intra-aortic balloon pump; LV, left ventricle; MCS, mechanical circulatory support; RV, right ventricle; VA-ECMO, veno-arterial extracorporeal membrane oxygenation; VT, ventricular tachycardia
Figure 5.
Types of mechanical circulatory support: (A) intra-aortic balloon pump, (B) transvalvular microaxial flow pump (Impella), (C) tandem heart, (D) veno-arterial extracorporeal membrane oxygenator.
8.2.6.1. Rescue therapy in acute haemodynamic decompensation because of refractory, haemodynamically intolerant ventricular arrhythmia
Because of the level of support provided and its rapid instauration, veno-arterial ECMO is the most attractive option for patients presenting with haemodynamic deterioration due to VA (ES, VT refractory to AADs, recurrent VF, or refractory cardiogenic shock after VA cessation).18 In an RCT in patients with incessant shockable rhythm (VT/VF), extracorporeal CPR (ECPR) was associated with lower mortality to hospital discharge compared with conventional CPR (7 vs. 43%).175 On the other hand, in another RCT including 256 patients with out-of-hospital cardiac arrest (OHCA) of presumably cardiac cause (61% with VF as presenting rhythm), ECPR failed to show a significant benefit in mortality when compared with conventional CPR (32 vs. 22%, P = 0.09).176 In a recent multi-centre RCT on 160 patients with OHCA due to refractory VT/VF, ECPR was not superior to conventional CPR in terms of mortality at 30 days (20 vs. 16%, P = 0.52).177 Systematic selection of optimal candidates and refinement of patient care through the process remain the cornerstone for a successful ECPR programme. The use of other MCS devices in this context, such as Impella, is anecdotal and only supported by small case series.
8.2.6.2. Rescue therapy in peri-procedural acute haemodynamic decompensation because of refractory unstable ventricular arrhythmia in patients undergoing ventricular tachycardia ablation
Acute haemodynamic deterioration during VT ablation may occur in up to 11% of patients and is associated with increased mortality, both in the short and long term.178 Veno-arterial ECMO is the preferred rescue MCS modality in patients with ES undergoing CA. However, reported mortality rates in the short-term are high, ranging from 38 to 76%, despite successful CA.179,180 Of note, rescue MCS during CA was associated with a higher mortality rate than pre-emptive MCS or no-MCS.181
8.2.6.3. Prophylactical mechanical circulatory support implantation prior to ventricular tachycardia ablation in patients at high risk of developing haemodynamic instability
Clinical evidence is scarce despite the potentially rational arguments for adopting this strategy. The selection of patients is the cornerstone of the strategy. The PAINESD score (Table 10) may help to estimate the risk of peri-procedural haemodynamic decompensation in patients with scar-related VTs requiring ablation.119,178 The risk of haemodynamic deterioration during the procedure may be influenced by the mapping strategy, in particular if repeated VT induction or mapping during VT is deemed necessary. In patients with a high PAINESD score (≥ 15), prophylactic MCS may reduce mortality.182,183 Prophylactic use of MCS was associated with survival benefits, as shown by a meta-analysis of 2465 patients with ES or high PAINESD scores.119 However, MCS as a support for ablation was associated with higher complication risk and procedural time/fluoroscopy burden.184 The vascular access strategy, the need for LV venting, and the expected duration of support time are mandatory to consider before the procedure.
Table 10.
PAINESD scores
| Parameter | Points |
|---|---|
| Pulmonary disease (COPD) | 5 |
| Age > 60 years | 3 |
| IHD | 6 |
| NYHA Class III and IV | 6 |
| EF < 25% | 3 |
| Storm electrical | 5 |
| DM | 3 |
| Low risk: ≤8, median risk: 9–14, high risk: ≥15 points | |
COPD, chronic obstructive pulmonary disease; DM, diabetes; EF, ejection fraction; IHD, ischaemic heart disease; NYHA, New York Heart Association;
Advice Table 3.
Mechanical circulatory support
| Evidence | Strength | |
|---|---|---|
| May be appropriate TO DO | ||
| MCS may be appropriate in patients with acute ES for optimizing haemodynamics18,175–177 | RCT |

|
| MCS may be appropriate in patients undergoing ablation of non-tolerated VAs to support mapping and ablation179,180 | OBS |

|
| MCS if started before ablation may be extended to aid elective CA | OPN |

|
| Initiation of MCS prophylactically before CA may be appropriate in high-risk patients, presenting with an ES or clustered VA119,181,182 | OBS |

|
8.2.7. Acute catheter ablation
Catheter ablation is the treatment of choice for monomorphic VT refractory to drug therapy in the acute phase and is advised in all eligible patients to reduce ES recurrence.1,185
In haemodynamically stable patients, expedited CA may be appropriate if non-invasive strategies cannot achieve prompt rhythm control. Catheter ablation aims to suppress VA and to prevent prolonged low-output state that can lead to acute multi-organ failure. Consideration of early CA is reasonable in patients with incessant VA or recurrent episodes of PVC-induced VA (also PVTs) that are haemodynamically significant despite AAD and deep sedation.
The ideal timing for CA remains unclear. However, in a recent meta-analysis, stabilization of patients with an ES using elective MCS prior to CA of VT appeared to be beneficial, compared with urgent MCS or non-MCS (see Section 8.2.6.).119 Rescue CAs within the first 24 h after ES onset with ongoing cardiogenic shock due to sustained VA episodes are associated with a higher rate of ablation failure and VA/ES recurrence.186 Evidence also suggested that CA performed after the first 48 h from admission is associated with lower mortality at 30 days compared with conservative therapy or very early ablation.187 Therefore, haemodynamic stabilization and arrhythmia suppression before proceeding with CA should be attempted but may not always be possible.
Catheter ablation in patients presenting with ES and PVT/VFs can be challenging. Trigger elimination is an effective strategy to achieve short-term and long-term ES freedom in post-MI patients with focally triggered VF storm (see Sections 8.1. and 8.2.2.).188–190 Epicardial approach may be needed in refractory cases in NICM, but also in cCAD patients.191–193 Due to the complex nature of VA ablations in ES that often require MCS, epicardial access, skilled operators, and support of multi-disciplinary staff, performing these ablations in experienced centres after initial stabilization is advised.
Urgent heart transplantation may be an option for selected patients who have a VA storm refractory to the therapy.
Advice Table 4.
Acute treatment of ES in SHD
| Evidence | Strength | |
|---|---|---|
| Advice TO DO | ||
| Design a management plan for each ES patient in a multi-disciplinary team | OPN |

|
| Start i.v. amiodarone (in combination with propranolol) in patients with SHD and reduced systolic function149 | RCT |

|
| Quinidine is appropriate in patients with recurrent PVT resistant to amiodarone and BBs, in the early post-MI phase or post-coronary revascularization intervention150,151 | OBS |

|
| Perform VT ablation in patients with recurrent MSVT despite optimal medical therapy, provided that an experienced team is available14,186 | OBS |

|
| Perform CA in patients with recurrent episodes of VF triggered by a similar PVC despite optimal medical therapy, provided that an experienced team is available189,190 | OBS |

|
| Transfer patients with recurrent MSVT or recurrent episodes of VF triggered by a similar PVC despite optimal medical therapy to a specialized centre for VA ablation, whenever possible18 | OBS |

|
| Advice NOT TO DO | ||
| Do not apply invasive treatment in case of specific directive or ‘do not resuscitate’ orders | OPN |

|
Advice Table 5.
Acute treatment of unstable ES in PED
| Evidence | Strength | |
|---|---|---|
| Advice TO DO | ||
| Isoproterenol infusion is beneficial in BrS patients presenting with an ES164,166–169,172 | OBS |

|
| Intravenous magnesium and potassium supplementation is useful in the acute phase of LQTS-associated TdP. Remove or correct external triggers (i.e. drugs, electrolyte imbalance).134,135,137 | OBS |

|
| May be appropriate TO DO | ||
| Isoproterenol or quinidine may be clinically useful to acutely treat an ES in patients with idiopathic VF194–196 | OBS |

|
| Isoproterenol infusion may be appropriate in ERS patients presenting with ES197 | OBS |

|
| Isoproterenol may be appropriate in SQTS patients with an ES173 | OPN |

|
| Verapamil may be clinically useful to acutely treat an ES in patients with idiopathic VF195 | OPN |

|
| Advice NOT TO DO | ||
| Catecholamines such as epinephrine and isoproterenol are not appropriate in CPVT patients with an ES174 | OBS |

|
8.2.8. Autonomic modulation
The autonomic nervous system plays an important role in the genesis of VT/VF.198–201 (see Section 6.4.). Beta-blocker therapy can decrease the risk of sudden cardiac death.202 Specifically, in the setting of ES, propranolol has demonstrated better efficacy compared with metoprolol.149 Of note, the effects of sympathetic activation extend beyond those influenced by BB therapy. Elevated sympathetic tone also leads to the release of sympathetic cotransmitters, such as neuropeptide Y, that likely decrease APD and influence arrhythmogenesis.203,204
In addition to increasing sympathetic efferent tone, sympathetic afferent activation may also play a role by inhibiting vagal tone. Therefore, sympathetic neuromodulatory therapies, such as stellate ganglion blockade (SGB), thoracic epidural anaesthesia (TEA), cardiac sympathetic denervation (CSD), and renal denervation (RDN), by changing efferent and afferent sympathetic signalling of the heart (afferent renal and efferent heart signalling in case of RDN), address mechanisms beyond blockade of beta-adrenergic receptors.
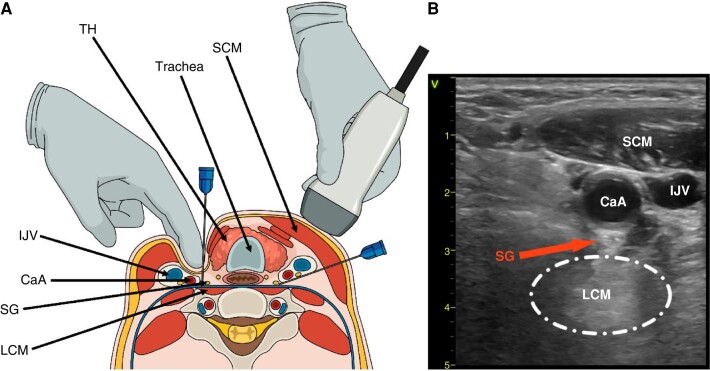
8.2.8.1. Stellate ganglion block
Stellate ganglion block is performed with an anaesthetic agent (bupivacaine or ropivacaine) at the left or bilateral stellate ganglia level under ultrasound and/or fluoroscopic guidance (Figure 6).205,206 In several case series, pharmacological SGB reduced VT burden in patients with refractory VT or VT storm and was more effective than standard ACLS protocol using amiodarone, though prospective and randomized data are needed.26,205–208 Continuous infusion of anaesthetic agents using a catheter placed near the stellate ganglion can provide better control of VA than a single bolus injection.209 Of note, efficacy of cryoenergy-induced and radiofrequency-induced SGBs have been reported in small case series.210,211 In a recent RCT in 26 patients with refractory ES, transcutaneous magnetic stimulation (a new, non-invasive method of modulating a patient’s nervous system activity) that targeted the left stellate ganglion was no better than a sham procedure in preventing VT recurrence within 24 h but was more effective in reducing VT burden (incidence rate ratio, 0.42; P < 0.001) and number of AADs.212
Figure 6.
Stellate ganglion block. (A) Neck cross-section showing SGB guided by surface landmark technique and palpation (left) and ultrasound (right). (B) Transverse sonographic view of the neck at the level of sixth cervical vertebrae (C6). CaA, carotid artery; IJV, internal jugular vein; LCM, longus colli muscle; SCM, sternocleidomastoid muscle; SG, stellate ganglion; SGB, SG blockade; TH, thyroid.
8.2.8.2. Thoracic epidural anaesthesia
Thoracic epidural anaesthesia provides greater sympatholysis, as administration of an anaesthetic in the C7-T4 epidural space can block sympathetic activity along the stellate and thoracic sympathetic ganglia bilaterally. This procedure is performed under fluoroscopic guidance. Contraindications include active infection, dual anti-platelet therapy, and the requirement for uninterrupted anticoagulation. Similar to SGB, TEA has been shown to reduce VT burden in small case series of patients with VT storm or refractory VT by ≥80%, though prospective and randomized data are lacking.213,214 Notably, SGB and TEA are temporary measures used as a bridge to more definitive therapy, such as CA, CSD, or occasionally, heart transplantation.
8.2.8.3. Surgical/thoracoscopic sympathetic cardiac denervation
The role of surgical CSD has been studied in patients with LQTS and CPVT (see Section 6.4.), as well as in those with refractory VT/VF storm and SHD.215 Left CSD (LCSD) effectively reduces the burden of VT in LQTS and CPVT patients and has been used in cases of BB intolerance or refractoriness.216–220 In a series of 147 high-risk LQTS patients, 75% of whom were symptomatic despite BB therapy, and the mean yearly number of cardiac events, including syncope, was reduced by 91% after CSD.219 Bilateral CSD has shown better results in patients with SHD,221–225 and in the largest multi-centre series of 121 patients (mean LVEF 30 ± 13%, 71% with NICM, 75% with VT storm, and 92% on BB combined with an AAD), bilateral CSD was associated with a 58% 1-year ICD shock/transplant-free survival and a >90% reduction in ICD shock burden in the year after compared with the year prior to CSD.224 In another series of 21 patients of which >70% had presented with ES, 76.9% were free from recurrent ICD shocks and 38.5% were free from any VA during a mean follow-up of ∼9 months.215 Notably, in patients with SHD, CSD may be efficacious in both monomorphic VT and PVT or VF,215 and utilization of CSD at an early stage, compared with performing the procedure urgently or emergently, may lead to better outcomes.226 Cardiac sympathetic denervation is currently being evaluated in randomized clinical trials to treat refractory VT (NCT01013714). A retrospective study of patients undergoing CSD suggested that CSD may also reduce the burden of PVCs, potentially playing a role in reducing triggers for VT/ES.227
8.2.8.4. Renal denervation
Renal denervation involves the ablation of renal nerves surrounding the renal arteries. This procedure can be performed under electroanatomic mapping and fluoroscopic guidance.228,229 In several case series of patients with cardiomyopathy, including DCM and Chagas cardiomyopathy, RDN with or without VT ablation was reported to reduce the burden of VT.230–232 In a meta-analysis of 121 pooled patients from multiple studies/case series (mean LVEF of 30.5 ± 10.3%, 76% men, 99% on BB, and 79% on amiodarone therapy), RDN reduced ICD shocks and ATP episodes.229 Primary challenges with RDN include a lack of clear procedural endpoints and anatomic variability of structures surrounding the arteries that can affect ablation biophysics and efficacy.233 Prospective randomized data are lacking.
Advice Table 6.
Sedation and autonomic modulation
| Evidence | Strength | |
|---|---|---|
| Advice TO DO | ||
| Initiate sympathetic blockade (esmolol, propranolol) in preference to lidocaine i.v. in ES patients with recent (<3 months) MI26 | RCT |

|
| The combination of i.v. amiodarone and oral propranolol is preferred to the combination of i.v. amiodarone and oral metoprolol in the management of ES in ICD patients149 | RCT |

|
| Initiate mild-to-moderate sedation (benzodiazepine) in all patients with an ES and ongoing/recurrent arrhythmia140,141 | OBS |

|
| May be appropriate TO DO | ||
| Deep sedation/general anaesthesia and mechanical ventilation may be appropriate in case of drug-refractory ES140,141 | OBS |

|
| Stellate ganglion block or TEA may be appropriate in SHD in the setting of ES or incessant VT/VF to reduce burden of VAs and ICD shocks as a bridge to more definitive therapy26,205–207,213 | OBS |

|
| Areas of uncertainty | ||
| The role of RDN as adjunct to ablation in patients with recurrent VAs and ES is uncertain | OBS |

|
8.2.9. Overdrive pacing
Overdrive pacing (ODP) may extinguish abnormal ventricular automaticity by overriding the ectopic pacemaker, which permits capturing and suppressing the ectopic pacemaker. Overdrive pacing may also cause an exit block from the ectopic focus. In re-entry VT, fast pacing may disrupt the re-entry circuit by altering the conduction rate, changing the excitation pathway, shortening, and decreasing dispersion of refractoriness of tissues in the re-entrant circuit and restitution of more uniform repolarization.234 By reducing ventricular refractory period, ODP may also reduce the susceptibility to the R on T phenomenon. These effects can be augmented by addition of AAD.235
Overdrive pacing can be carried out with an implanted pacemaker or ICD or through a temporary electrode inserted into the RV, by pacing at a rate of 10–20 b.p.m. greater than the native rate. Of note, decremental ODP (with progressively shorter inter-stimuli intervals) was superior to fixed overdrive burst pacing (with constant intervals) in interrupting VT and auto-decremental pacing (a 10 ms decrement) and was superior to scheme using a 5 ms coupling decrement.236,237 Temporary overdrive atrial or ventricular pacing in patients without ICD demonstrated its efficiency in preventing recurrence of drug-resistant VA in several case reports, mainly in the context of acute or recent myocardial ischaemia.238,239 Moreover, bradycardia pacing might be useful in some patients with brady-mediated PVT.
8.2.10. Bailout strategies
The inability to create transmural or deep intramural lesions in the ventricular myocardium is one of the reasons for VT CA failure. One solution is sequential radiofrequency applications from adjacent opposite sites, including epicardial access. However, this might not be sufficient, and several bailout strategies have been proposed and described in the literature.240–248 These optional strategies include prolonged or high-power applications, bipolar ablation, simultaneous unipolar ablation, use of low-ionic solution (half normal saline), retractable needle ablation, septal coronary venous mapping, intracoronary artery wire mapping/ablation, ethanol ablation, coil embolization, or stereotactic radiotherapy. All these techniques have not been utilized in large or randomized series and have been described/adopted by highly skilled operators working in high-volume centres.
9. Stabilized patient
9.1. Long-term treatment
Without specific anti-arrhythmic interventions, ES recurs in >50% of patients with SHD. The risk of ES recurrence is highest within the first year after the event. Independent predictors of ES recurrence were LVEF ≤30%, age >65 years, and lack of optimal HF treatment in one observational study.249.
Beta-blockers,120 angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs),250 spironolactone,251 and angiotensin receptor-neprilysin inhibitor (ARNI; valsartan–sacubitril)252 have been associated with a reduced risk of arrhythmia and SCD in patients with HF with reduced LVEF (HFrEF). There is limited evidence that statins253 may reduce the occurrence of VA. Preliminary data suggest a beneficial effect of sodium-glucose co-transporter-2 (SGLT-2) inhibitors.254 Although there are no data evaluating the effect on ES recurrence specifically, optimization of HF treatment is important and should follow current guidelines.255 In patients with cCAD, complete revascularization may be beneficial.256
Precipitating factors, including potential pro-arrhythmic drugs, excessive alcohol consumption,257–259 illicit drugs,260 and electrolyte imbalances, must be avoided.
9.2. Anti-arrhythmic drugs to prevent electrical storm recurrence
9.2.1. Chronic anti-arrhythmic drug therapy in patients with structural heart disease
Randomized controlled trials or large observational studies evaluating the efficacy of AAD to prevent specifically ES recurrence are scarce. However, the potential efficacy may be extrapolated from studies that addressed the efficacy of AAD in preventing VT recurrence in general. Anti-arrhythmic drugs used to prevent ES recurrence are listed in Table 11.
Table 11.
Pharmacotherapy for chronic treatment of patients with ES
| Chronic treatment | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Vaughan Williams class | Drug | Channels effected | Dose (p.o.) | Half-life | Metabolism | Specific use | Adverse effect | Monitoring | Counter indications/warnings |
| Class I | Quinidine | INa, IKr, Ito, M, α | 600–1600 mg Loading dose: start 200 mg every 3 h until effect, maximum 3 g in first 24 h | 6–8 h | Hepatic | VT, VF, IVF, BrS, SQT |
QTc prolongation, TdP, QRS prolongation, increases DFT, hypotension, bradycardia HF exacerbation, diarrhoea, immune thrombocytopenia |
ECG (QRS duration and QT interval), heart rate, platelet count | Severe bradycardia and/or high-degree AV block in the absence of a pacemaker, myasthenia gravis Use with caution in HF |
| Procainamide | INa, IKr ganglionic block | 500–1250 mg q6 h | 3–4 h | Hepatic and renal | VT, pre-excited AF |
QTc prolongation, TdP, QRS prolongation, increases DFT, lupus-like syndrome, bone marrow aplasia |
ECG (QRS duration and QT interval), blood pressure | Myasthenia gravis Use with caution in HF |
|
| Disopyramide | INa, IKr,M | 250–750 mg | 4–10 h | Hepatic | VT, PVCs | Negative inotrope, QRS prolongation, AV block, pro-arrhythmia (atrial flutter, monomorphic VT, TdP), anticholinergic effects |
Heart rate, blood pressure, ECG (QRS duration, QT interval) | Severe bradycardia and/or high-degree AV block and/or severe intraventricular conduction delay in the absence of a pacemaker, decompensated HF, congenital QT prolongation, myasthenia gravis | |
| Mexiletine | INa | 600–1200 mg Loading dose: 400 mg initially followed by 600 mg in the first 24 h | 10–14 h | Hepatic | VT/VF, LQTS3 LQT2 |
Tremor, nausea, paresthesia, numbness | ECG (QT interval), hepatic function | ||
| Flecainide | INa | 200–400 mg | 12–27 h | Hepatic | VT, PVCs, CPVT | QRS prolongation, negative inotrope, AV block, sinus bradycardia, pro-arrhythmia (atrial flutter, monomorphic VT, occasional TdP), increase pacing threshold | Heart rate, blood pressure, ECG (QRS duration, QT interval) | Severe bradycardia and/or high-degree AV block and/or severe intraventricular conduction delay in the absence of a pacemaker, ischaemia, SHD, BrS, myasthenia gravis | |
| Class II | Metoprolol | β1-receptor | 25–400mg | Tartarate: 3–4 h Succinate: 3–7 h |
Hepatic | VT, PVCs | Bradycardia, AV block, hypotension, nausea, dizziness |
Heart rate, blood pressure | Severe bradycardia and/or high-degree AV block in the absence of a pacemaker, decompensated HF, cardiogenic shock, myasthenia gravis |
| Propranolol | Non-selective BB | 80–320 mg | 3–6 h | Hepatic | VT, PVCs, LQTS | Bradycardia, AV block, hypotension, nausea, dizziness bronchospasm |
Severe bradycardia and/or high-degree AV block in the absence of a pacemaker, decompensated HF, cardiogenic shock, myasthenia gravis | ||
| Nadolol | Non-selective BB | 40–120 mg | 20–24 h | Renal | VT, PVC, LQTS, CPVT |
Bradycardia, AV block, hypotension, nausea, dizziness, bronchospasm | Severe bradycardia and/or high-degree AV block in the absence of a pacemaker, decompensated HF, cardiogenic shock, myasthenia gravis | ||
| Class III | Amiodarone | INa, ICa, IKr, IK1, IKs, Ito, α, β | 200–400 mg Loading dose: 600–1200 mg/ 24 h 8–10 days | 4–14 weeks | Hepatic | VT, VF, PVCs | Increases DFT, hypotension, bradycardia, AV block, QT prolongation, TdP (rare), hypothyroidism/hyperthyroidism, nausea, photosensitivity, skin discolouration, peripheral neuropathy, tremor, hepatitis, pulmonary fibrosis/pneumonitis | Heart rate, blood pressure, ECG (QT interval), hepatic function | Severe bradycardia and/or high-degree AV block in the absence of a pacemaker, decompensated HF, cardiogenic shock |
| Sotalol | IKr, β | 160–640 mg | 12 h | Renal | VT, VF, PVCs | Bradycardia, AV block, QT prolongation, TdP, hypotension, nausea, dizziness, bronchospasm | Heart rate, blood pressure, ECG (QT interval) | Severe bradycardia and/or high-degree AV block in the absence of a pacemaker, decompensated HF, cardiogenic shock | |
| Class IV | Verapamil | ICa | 120–480 mg | 3–7 h | Fascicular VT | Bradycardia, AV block, negative inotrope, hypotension | Heart rate, blood pressure, hepatic function | Severe bradycardia and/or high-degree AV block in the absence of a pacemaker, decompensated HF, cardiogenic shock, myasthenia gravis | |
BB, beta-blocker; BrS, Brugada syndrome; CPVT, catecholaminergic polymorphic ventricular tachycardia; ECG, electrocardiogram; ES, electrical storm; HF, heart failure; IVF, idiopathic ventricular fibrillation; LQT, long QT; LQTS, LQT syndrome; PVC, premature ventricular complex; QTc, corrected QT; SHD, structural heart disease; SQT, short QT; TdP, torsade de pointes; VF, ventricular fibrillation; VT, ventricular tachycardia.
Beta-blockers are a cornerstone of drug treatment of patients with VA in the context of SHD. In a large retrospective registry of VT/VF survivors, chronic BB use was associated with improved survival at 3 years compared with a propensity-matched group not taking BBs.261
Amiodarone, preferably in combination with BB, can reduce VA recurrence and ICD shocks. Several studies and meta-analyses have demonstrated its superior anti-arrhythmic effect in reducing recurrent VTs or appropriate ICD therapies compared with other AADs.208–211 In a recent meta-analysis of 22 RCTs, including 3828 patients, amiodarone use was associated with a 70% relative risk reduction for VT recurrence [hazard ratio (HR) = 0.34; 95% confidence interval (CI) = 0.15–0.74] and appropriate ICD therapies (HR = 0.33; 95% CI = 0.15–0.76), compared with standard optimal medical therapy, including BBs, in patients with ICD and a history of VA.262 In the Optic study, the combination of BB and amiodarone was superior to sotalol or BB monotherapy in reducing the risk of appropriate ICD shocks during 1 year observation in ICD patients implanted for secondary prevention.263 However, treatment-attributed adverse events need to be considered, including hypothyroidism and hyperthyroidism, pulmonary and liver toxicity, and drug-related mortality.264 In a recent RCT meta-analysis, amiodarone use was associated with an increased risk of death (odds ratio 3.36, 95% CI 1.36–8.30, P = 0.009).265 Similarly, in a large observational study of 281 patients with DCM undergoing RFCA for drug-refractory VT (ES 35%, incessant VT 20%), amiodarone at discharge was independently associated with mortality or heart transplantation (HR 3.23, 95% CI 1.43–7.33, P < 0.01).266 Whether this is directly amiodarone related or whether amiodarone is just a marker for sicker patients is not clear yet.
Sotalol is a racemic mixture of two isomers, of which the d-isomer blocks potassium channels and the l-isomer acts as a non-selective BB together with Class 3 properties. Lower doses exert mainly a beta-blocking effect, whereas higher doses are needed for the Class III effect; however, significant QT prolongation has been observed after a single low dose.267,268 In the Optic trial, sotalol was superior to BBs alone in reducing the risk of ICD shocks.263 Of note, the number of all episodes terminated by ATP or ICD shock was not significantly different between patients on sotalol or BBs.262 In the d,l-Sotalol Implantable Cardioverter-Defibrillator randomized trial, sotalol reduced the mean number of ICD shocks compared with placebo (1.43 vs. 3.89 per year, P = 0.008), irrespectively from the LVEF.269 However, pro-arrhythmic side effects, including TdP, are of concern, and careful monitoring of the QTc interval, in particular in patients with impaired renal function, is mandatory. Sotalol should be used with caution in patients with HF and poor LVEF due to its negative inotropic effect. However, it may be useful in patients with ARVC.
Mexiletine is a Class IB AAD with high bioavailability (80%) that allows for its oral administration. It acts by blocking rapid sodium channels and was used as adjunctive therapy to amiodarone to prevent VA in case of amiodarone inefficacy or intolerable side effects.270–272 There are little data on the long-term safety of its use in patients with advanced SHD. Rapid loading (1 × 400 mg per os) was associated with HF decompensation in patients with severe LV dysfunction.273 It has also been shown to increase DF thresholds.274
Procainamide is a Class IA AAD, prolonging APD at faster rates (through the blockade of the rapid inward Na depolarization current in a use-dependent fashion) and prolonging repolarization via the blockade of the delayed rectifier K channel. It reduced spontaneous VA and suppressed VT inducibility in the ESVEM Trial and small, single-centre studies.275,276 In a recent small single-centre observational study, oral procainamide reduced ICD therapies in patients with VT refractory to other AADs, including amiodarone.277 However, severe side effects, including a drug-induced lupus erythematosus-like syndrome, are of concern. Of note, procainamide is not available in many countries.
Quinidine is a Class IA AAD, available in oral formulations, which has been shown to have only a modest negative inotropic effect.278 Quinidine plays a role in suppressing PVC-induced PVTs and VF in the subacute phase of MI (but also after revascularization: CABG and PCI) and in patients without SHD.150,197 However, quinidine showed limited tolerability and long-term efficacy when used in the management of amiodarone-refractory scar-related MSVT.279,280
While flecainide should be avoided in patients with cCAD or HFrEF,281,282 it can be effective, in combination with BBs or sotalol, in preventing recurrent VT in patients with ARVC refractory to single AAD or ablation.283,284 However, there is also the potential risk of myocardial depression and right (and left) ventricular failure in these patients, so caution is mandatory also in this population.
9.2.2. Chronic pharmacotherapy in primary electrical disease
Beta-blockers remain the cornerstone of chronic treatment in LQT syndromes, and non-selective agents (propranolol, preferably long-acting and nadolol, usually starting from doses 80 and 40 mg 1× daily, respectively) proved to be more effective.285 Of note, the effectiveness of BBs not only as a group but also of a given drug (e.g. nadolol and propranolol > atenolol and metoprolol) might depend on the LQTS genotype (LQT1 > LQT2 ≥ LQT3).286
Mexiletine or ranolazine can be useful in Type 3 LQTS and mexiletine probably also in other LQTS subtypes.287–289 If adequate ICD interventions or ES episodes recur despite optimal beta-blockade, LCSD was shown to protect against VA in LQTS effectively (see Section 8.2.8.).216,218,219
The role of pharmacotherapy is limited in BrS, but quinidine was beneficial in preventing VA (start dose is 250 or 300 mg bid), ES, and frequent ICD shocks.290 In the randomized QUIDAM study, hydroquinidine seemed to be effective in preventing life-threatening VA, however, at the cost of frequent (68%, mainly gastrointestinal) side effects.291
Catecholaminergic polymorphic ventricular tachycardia respond well to BBs; those who experience recurrent syncope or bidirectional VT while on BBs may benefit from adding flecainide.292–294 Left cardiac sympathetic denervation is an option if VA recur despite drugs.216 In ERS and IVF patients with ES, quinidine may prevent VA.197 Long-term treatment with hydroquinidine was efficient in short QT syndrome, but data are limited.295,296
Implantable cardioverter-defibrillator treatment is indicated, in general, in secondary prevention or case of arrhythmic syncope unless there is a clear unequivocal trigger underlying the arrhythmias (i.e. drug use in LQTS).1
9.3. Catheter ablation to prevent electrical storm recurrence
Catheter ablation for VA is increasingly performed and offers an alternative to AAD treatment, in particular, if AAD are not tolerated, not effective, or not desired. Most of the data on ablation outcome are derived from patients with cCAD, DCM subgroups, or ARVC who were treated in highly experienced centres.
Procedural risks and expected outcome depend on individual patient characteristics (including the specific underlying aetiology, substrate location and extent, comorbidities, prior surgery, and prior ablation attempts), and the experience of the treating centres and operators. It is adviced to provide the patient with detailed information on the procedural aspects, risks, and expected outcomes for shared decision-making.
9.3.1. Ischaemic heart disease
While ischaemic heart disease (IHD) represents one of the most common ES substrates, limited data are available addressing specifically the benefit of CA after ES stabilization. A systemic review of randomized clinical trials, including the SMS, VANISH, CALYPSO, VTACH, SMASH VT trials, and the more recent BERLIN VT trial, showed that CA significantly reduces the occurrence of ES and appropriate ICD therapies, including ICD shocks.297–301 Of note, CA was efficient in controlling VA resistant to AADs302,303 and was more effective than amiodarone escalation or adjunctive mexiletine.264,299,300,304,305 A recent observational study demonstrated that early CA appears superior to initial medical therapy regarding VT and ES recurrence, iatrogenic complications, cardiovascular hospitalizations, and cumulative days in the hospital.306 There are insufficient data to evaluate mortality reduction by CA in patients with ES. While CA did not significantly improve survival or cardiovascular hospitalizations in a meta-analysis of RCTs, non-randomized studies have reported survival benefits.14,186,307,308 In stabilized patients with cCAD, who present with an ES on chronic amiodarone therapy RFCA is advised.299,300 In patients without chronic amiodarone therapy CA may be appropriate dependent on patient’s characteristics, comorbidities, and preferences.187
9.3.2. Non-ischaemic cardiomyopathy
Patients presenting with ES from NICM comprise a heterogeneous group of different phenotypes, including DCM, HCM, and ARVC phenotypes. In particular, DCM can be due to an inherited or acquired aetiology. Whether CA is beneficial to prevent ES recurrence in patients with NICM is unknown. Patients with NICM undergoing VT ablations had higher VA recurrence compared with patients with cCAD.309 Among the different non-ischaemic aetiologies, outcome after RFCA differs and was poorer in patients with HCM, valvular heart disease, (active) CS, and inherited DCM. This is often attributed to a more complex VA substrate (e.g. more intramural, epicardial, and septal involvement) as well as disease progression.310–312. Observational data suggest that CA may be associated with lower in-hospital mortality compared with medical management in selected patients.313
Whether to pursue endocardial or epicardial ablation can vary according to the specific aetiologies and suspected disease substrates. Patients with ARVC might benefit more from the epicardial–endocardial ablation strategy.314 Combined epicardial–endocardial ablation may also be considered at the index procedure in VTs caused by Chagas disease, as the epicardial scars are often more extensive than endocardial scars with a high number of epicardial circuits.315,316 Ventricular tachycardia ablation in stabilized NICM patients presenting with an ES under chronic AAD treatment may be appropriate. In individual patients with ARVC, chronic myocarditis, or VT substrate location that are expected to be approachable by RFCA based on pre-procedural evaluation, it is appropriate to carefully discuss this treatment option as an alternative to chronic AAD treatment.
However, considering the complex procedure, with often required epicardial–endocardial approach and bailout strategies, in particular for deep intramural substrates, transferring these patients to high-volume, experienced centres is advised.
9.3.3. Primary electrical disease
In PED, CA is not a first-line option. Recent advancements, however, raised interest in the ablation of an epicardial arrhythmic RVOT substrate in BrS. The sentinel study by Nademanee et al.,317,318 demonstrating epicardial RVOT CA as a viable option in high-risk symptomatic patients, was followed by a series from Italy and a long-term follow-up study of an international cohort.319,320 These studies showed a high success rate (also in the long term) and low complication rates. It should, however, be noted that these procedures were performed in highly experienced, high-volume centres. Before considering prophylactic CA of symptomatic or even asymptomatic patients as an addition to ICD placement, further research including prospective randomized study is required.321
Preliminary reports of successful CA in patients with LQTS have been published.322 In three of the four patients who underwent mapping, the ectopy originated from the specialized conduction system in the LV (ramifications of the anterior and posterior fascicles). In a recent study, Pappone et al.323 identified electrophysiological abnormalities in the RV epicardium in a small series of LQTS patients. Eliminating these abnormal electrical activities successfully prevented malignant VA recurrences during a mean follow-up period of 1 year. Adoption of this approach requires further research.
In CPVT, recent experimental studies suggest a Purkinje fibre-related origin of the ventricular ectopy.324 However, clinical studies in occasional patients are inconclusive, demonstrating Purkinje fibre origin in some, but not all cases.63
In drug-resistant cases on ERS and IVF, in whom similar PVCs trigger VF, CA may be pertinent if performed in experienced centres.325
9.4. Autonomic modulation
Electrical storm recurrences are common, especially within the first year after the acute event. The pro-arrhythmic effect of sympathetic–parasympathetic imbalance may still play an important role beyond the acute phase,249,326 and initiation of long-term BB therapy is appropriate.26,149
While SGB and TEA are usually considered as acute interventions327 with a transient effect, surgical or thoracoscopic left or bilateral CSD results in permanent afferent and efferent CSD (see Section 8.2.8.).
Advice Table 7.
Chronic treatment of patients with SHD who present with an ES after initial stabilization
| Evidence | Strength | |
|---|---|---|
| Advice TO DO | ||
| Optimize HF treatment in patients with HFrEF, including BBs, ACE inhibitors/ARB/ARNI, MRAs, and SGLT-2 inhibitors, according to the latest ESC Guidelines on HF management120,250–252,254 | RCT |

|
| Perform CA, rather than AAD drug escalation in cCAD patients, if ES due to MSVT has recurred on chronic amiodarone therapy264,299 | RCT |

|
| Perform CA in patients with cCAD and ES due to MSVT if AADs are contraindicated, not tolerated, or not desired302,303 | OBS |

|
| May be appropriate TO DO | ||
| Long-term treatment with amiodarone and BB (choosing BB depending on clinical context) may be useful to prevent ES recurrence263,265,328 | RCT |

|
| It may be appropriate to offer CA as first-line treatment in cCAD patients with ES due to MSVT, provided that the procedure is performed in experienced centres185,301,306 | OBS |

|
| It may be appropriate to perform CA in patients with NICM, if ES due to MSVT recurs despite AAD therapy and if AADs are contraindicated or not tolerated, provided the procedure is performed in experienced centres185,313 | OBS |

|
| It may be appropriate to perform left or bilateral surgical or thoracoscopic CSD, to reduce burden of MSVT and PVT in ischaemic and NICM in patients with arrhythmia recurrences/ES despite medical therapy and CA and/or those who are not candidates for CA213,224–226 | OBS |

|
Advice Table 8.
Chronic treatment of ES in stabilized primary electrical disease
| Evidence | Strength | |
|---|---|---|
| Advice TO DO | ||
| Perform LCSD in LQTS or CPVT patients with an ICD who are symptomatic on BB and who experience multiple shocks or ES refractory or intolerant to medical therapy216–219 | OBS |

|
| May be appropriate TO DO | ||
| Quinidine therapy may be appropriate in patients with BrS who have recurrent ICD shocks or ES290,291,329 | OBS |

|
| Quinidine in addition to an ICD may be appropriate for ES or recurrent VF in ERS, PVC triggered VF, or IVF patients197,325 | OBS |

|
| Catheter ablation by experienced electrophysiologists may be appropriate in patients with ERS or IVF with recurrent episodes of VF triggered by a similar PVC non-responsive to medical treatment197,325 | OBS |

|
| Catheter ablation of triggering PVCs and/or RVOT epicardial substrate may be appropriate in BrS patients with ES or recurrent appropriate ICD shocks317–319 | OBS |

|
10. Psychological counselling
Symptoms of depression and anxiety are observed in 24–87% of ICD patients and impact the mental and functional quality of life.330 Both the concern of receiving an ICD shock and the experience of ICD shocks contribute to psychological distress. Young age (<50 years), frequent ICD shocks, and poor understanding of their cardiac condition or their device have been associated with increased distress.330 In a recent subanalysis from the Danish Trial, shocks during follow-up were associated with depression, anxiety, and ICD concerns.331 Depression and anxiety are associated with increased mortality in HF patients,332 and anxiety was associated with an increased risk of VAs in ICD patients.333 As a consequence, psychological counselling is advised as part of the multi-disciplinary care for ES patients. Noteworthy, in a recent EHRA-initiated survey, only 46% of the surveyed European electrophysiology (EP) centres refer patients to psychological counselling after ES.334
Advice Table 9.
Informing the patient, end-of-life issues, and psychological councelling
| Evidence | Strength | |
|---|---|---|
| Advice TO DO | ||
| Provide the patient with detailed information on the procedural aspects, risks, and expected outcomes for shared decision-making, before undertaking CA or any invasive treatment, if possible | OPN |

|
| Psychological counselling is advised as a part of the multi-disciplinary care for ES patients331,335 | OBS |

|
| In the presence of significant comorbidities, particularly in the case of recurrent ES and intractable, end-stage HF, informed discussion with the patient and family about the options of ICD deactivation should be undertaken | OPN |

|
11. Special patient groups
11.1. Patients with left ventricular assist device
Ventricular arrhythmias and ES are common in patients with implanted LV assist device (LVAD), with reported incidences of 20–50 and 9%, respectively.336–338 Ventricular arrhythmia in patients with LVADs are usually well tolerated, especially in those with continuous flow LVAD. However, short-term mortality after an ES has been reported to be high, and recurrent ICD shocks while conscious are of concern.338–340 Ventricular arrhythmia in LVAD patients can be occasionally due to suction, which may be managed by changing the turbine speed.341 Mapping studies have demonstrated that the majority of MSVT is not related to apical inflow cannula, but rather to remote intrinsic myocardial scar.341,342 Anti-arrhythmic drug treatment, sedation, and autonomic modulation to control the ES do not differ between patients without or with LVADs.
Small case series from very experienced groups have reported favourable outcomes after RFCA in highly symptomatic patients with ES or recurrent ICD shocks, usually after the failure of AAD.341,342 Practical considerations include the following: the lack of pulsatile peripheral flow during vascular access and blood pressure monitoring and the potential absence of aortic valve opening, favouring transseptal access. A theoretical risk of catheter entrapment in the LVAD cannula/impeller and considerable noise interference on surface ECG and mapping from HeartMate 3 should also be taken into account.343 The mechanical haemodynamic support provided by the LVAD usually allows the advised transfer of patients to specialized centres experienced in the management of patients with LVADs and VA.
11.2. Patients with advanced heart failure
Patients with advanced HF are at high risk for VA,344 HF-related recurrent hospitalizations, and mortality. Ventricular arrhythmia and ES can be the consequence of end-stage HF but can also worsen cardiac function. Optimization of HF treatment in close collaboration with the HF specialist and cardiothoracic surgeon is mandatory to identify those who benefit from advanced HF treatment, including LVAD and heart transplantation. Anti-arrhythmic drug treatment is limited because of the negative inotropic effect of almost all AAD. Amiodarone and mexiletine, in selected cases, can be effective. Catheter ablation offers an alternative, particularly if substrate-based approaches are used, and recurrent VT induction is avoided. Patients with severe HF symptoms at rest (NYHA IV) are usually excluded from RCTs evaluating CA or are combined with patients with NYHA Class III. While VT ablation did not reduce mortality in patients with cCAD, it was superior to the escalation of anti-arrhythmic medication in reducing VT recurrences and ES during follow-up.264 The benefit was consistent across functional Class I through III. In a large international VT ablation registry of 1365 patients, 111 patients in NYHA IV were included.345 Although there was no significant difference in acute complications, NYHA IV patients required more haemodynamic support and had a higher in-hospital mortality. Patients with advanced HF have a higher risk of acute decompensation during VT ablation, which is associated with high mortality risk.178 Patients with advanced HF require a multi-disciplinary team to decide on the acute management of the ES and whether they are candidates for MCS (see Section 8.2.6.), LVAD (see Section 11.1.) or heart transplantation. Early evaluation for advanced HF management is advised for patients with DCM, LVEF ≤32%, and early VT recurrence after initial ablation for an ES, considering the high mortality independent from the arrhythmic outcome.266
12. When not to perform interventional treatment
In terminally ill patients or advanced cardiac disease, the type of treatment, the expected procedural success of invasive treatments, and the willingness and goals of care for the patient and family are important to consider. In the presence of significant comorbidities, particularly in the case of recurrent ES, a holistic approach and informed discussion with the patient and family about the options of ICD deactivation and treatments to relieve distress and provide patient comfort are advised.
Contributor Information
Radosław Lenarczyk, Medical University of Silesia, Division of Medical Sciences, Department of Cardiology and Electrotherapy, Silesian Center for Heart Diseases, Skłodowskiej-Curie 9, 41-800 Zabrze, Poland.
Katja Zeppenfeld, Department of Cardiology, Leiden University Medical Center, Leiden, The Netherlands.
Jacob Tfelt-Hansen, The Department of Cardiology, The Heart Centre, Copenhagen University Hospital, Rigshospitalet, Copenhagen, Denmark; The Department of Forensic Medicine, Copenhagen University Hospital, Rigshospitalet, Copenhagen, Denmark.
Frank R Heinzel, Cardiology, Angiology, Intensive Care, Städtisches Klinikum Dresden Campus Friedrichstadt, Dresden, Germany.
Thomas Deneke, Clinic for Interventional Electrophysiology, Heart Center RHÖN-KLINIKUM Campus Bad Neustadt, Bad Neustadt an der Saale, Germany; Clinic for Electrophysiology, Klinikum Nuernberg, University Hospital of the Paracelsus Medical University, Nuernberg, Germany.
Elena Ene, Clinic for Interventional Electrophysiology, Heart Center RHÖN-KLINIKUM Campus Bad Neustadt, Bad Neustadt an der Saale, Germany.
Christian Meyer, Division of Cardiology/Angiology/Intensive Care, EVK Düsseldorf, Teaching Hospital University of Düsseldorf, Düsseldorf, Germany.
Arthur Wilde, Department of Cardiology, Amsterdam UMC University of Amsterdam, Amsterdam, the Netherlands; Amsterdam Cardiovascular Sciences, Heart Failure and arrhythmias, Amsterdam, the Netherlands.
Elena Arbelo, Arrhythmia Section, Cardiology Department, Hospital Clínic, Universitat de Barcelona, Barcelona, Spain; IDIBAPS, Institut d'Investigació August Pi i Sunyer (IDIBAPS), Barcelona, Spain; Centro de Investigación Biomédica en Red de Enfermedades Cardiovasculares (CIBERCV), Madrid, Spain.
Ewa Jędrzejczyk-Patej, Department of Cardiology, Congenital Heart Diseases and Electrotherapy, Silesian Centre for Heart Diseases, Zabrze, Poland.
Avi Sabbag, The Davidai Center for Rhythm Disturbances and Pacing, Chaim Sheba Medical Center, Tel Hashomer, Israel; School of Medicine, Faculty of Medical and Health Sciences, Tel Aviv University, Tel Aviv, Israel.
Markus Stühlinger, Department of Internal Medicine III, Cardiology and Angiology, Medical University of Innsbruck, Innsbruck, Austria.
Luigi di Biase, Albert Einstein College of Medicine at Montefiore Hospital, New York, NY, USA.
Marmar Vaseghi, UCLA Cardiac Arrythmia Center, Division of Cardiology, Department of Medicine, University of California, Los Angeles, CA, USA.
Ohad Ziv, Case Western Reserve University, Cleveland, OH, USA; The MetroHealth System Campus, Cleveland, OH, USA.
William-Fernando Bautista-Vargas, Cardiac Electrophysiology, Fundacion CardioInfantil La Cardio, Bogota, Colombia.
Saurabh Kumar, Department of Cardiology, Westmead Hospital, Westmead Applied Research Centre, University of Sydney, Sydney, Australia.
Narayanan Namboodiri, University of Science and Technology Kochi, Kerala, India.
Benhur Davi Henz, Instituto Brasilia de Arritmias-Hospital do Coração do Brasil-Rede Dor São Luiz, Brasilia, Brazil.
Jose Montero-Cabezas, Department of Cardiology, Leiden University Medical Center, Leiden, The Netherlands.
Nikolaos Dagres, German Heart Center of the Charite, Berlin, Germany.
Petr Peichl, Department of Cardiology, IKEM, Prague, Czech Republic.
Antonio Frontera, Department of Electrophysiology, Great Metropolitan Hospital Niguarda, Milan, Italy.
Stylianos Tzeis, Cardoilogy Department, Mitera General Hospital, Hygeia Group, Athens, Greece.
Jose Luis Merino, Arrhythmia and Robotic EP Unit, Hospital Universitario La Paz, Madrid, Spain.
Kyoko Soejima, Department of Cardiovascular Medicine, Kyorin University Hospital, Tokyo, Japan.
Christian de Chillou, Department of Cardiology, University Hospital Nancy, Vandoeuvre les Nancy, France.
Roderick Tung, Division of Cardiology, Cardiovascular Clinical Research, Banner Heart Institute, The University of Arizona College of Medicine-Phoenix, AZ, USA.
Lars Eckardt, Department of Cardiology – Electrophysiology, University of Münster, Münster, Germany.
Philippe Maury, Cardiology, University Hospital Rangueil Toulouse, Toulouse, France.
Peter Hlivak, Department of Arrhythmias and Pacing, National Institute of Cardiovascular Diseases and the Slovak Medical University School of Medicine, Bratislava, Slovakia.
Larisa G Tereshchenko, Department of Cardiovascular Medicine, Heart, Vascular & Thoracic Institute, Department of Quantitative Health Sciences, Lerner Research Institute, Cleveland Clinic, Cardiology, USA.
Pipin Kojodjojo, Asian Heart and Vascular Center, Singapore, Singapore.
Jacob Atié, Hospital São Vicente – Rede Dor, Department of Cardiology, Federal University of Rio de Janeiro, Rio de Janeiro, Brazil.
References
- 1. Zeppenfeld K, Tfelt-Hansen J, de Riva M, Winkel BG, Behr ER, Blom NA et al. 2022 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J 2022;43:3997–4126. [DOI] [PubMed] [Google Scholar]
- 2. Elsokkari I, Parkash R, Tang A, Wells G, Doucette S, Yetisir E et al. Mortality risk increases with clustered ventricular arrhythmias in patients with implantable cardioverter-defibrillators. JACC Clin Electrophysiol 2020;6:327–37. [DOI] [PubMed] [Google Scholar]
- 3. Viskin S. Long QT syndromes and torsade de pointes. Lancet 1999;354:1625–33. [DOI] [PubMed] [Google Scholar]
- 4. Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm Society. Heart Rhythm 2018;15:e190–252. [DOI] [PubMed] [Google Scholar]
- 5. Könemann H, Ellermann C, Zeppenfeld K, Eckardt L. Management of ventricular arrhythmias worldwide: comparison of the latest ESC, AHA/ACC/HRS, and CCS/CHRS guidelines. JACC Clin Electrophysiol 2023;9:715–28. [DOI] [PubMed] [Google Scholar]
- 6. Cronin EM, Bogun FM, Maury P, Peichl P, Chen M, Namboodiri N et al. 2019 HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias. Europace 2019;21:1143–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Credner SC, Klingenheben T, Mauss O, Sticherling C, Hohnloser SH. Electrical storm in patients with transvenous implantable cardioverter-defibrillators: incidence, management and prognostic implications. J Am Coll Cardiol 1998;32:1909–15. [DOI] [PubMed] [Google Scholar]
- 8. Nedios S, Darma A, Stevanello C, Richter S, Doering M, Rolf S et al. Electrical storm in patients with implantable cardioverter-defibrillator in the era of catheter ablation: implications for better rhythm control. Heart Rhythm 2015;12:2419–25. [DOI] [PubMed] [Google Scholar]
- 9. Sesselberg HW, Moss AJ, McNitt S, Zareba W, Daubert JP, Andrews ML et al. Ventricular arrhythmia storms in postinfarction patients with implantable defibrillators for primary prevention indications: a MADIT-II substudy. Heart Rhythm 2007;4:1395–402. [DOI] [PubMed] [Google Scholar]
- 10. Streitner F, Kuschyk J, Dietrich C, Mahl E, Streitner I, Doesch C et al. Comparison of ventricular tachyarrhythmia characteristics in patients with idiopathic dilated or ischemic cardiomyopathy and defibrillators implanted for primary prevention. Clin Cardiol 2011;34:604–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Exner DV, Pinski SL, Wyse DG, Renfroe EG, Follmann D, Gold M et al. Electrical storm presages nonsudden death: the antiarrhythmics versus implantable defibrillators (AVID) trial. Circulation 2001;103:2066–71. [DOI] [PubMed] [Google Scholar]
- 12. Guerra F, Palmisano P, Dell’Era G, Ziacchi M, Ammendola E, Pongetti G et al. Cardiac resynchronization therapy and electrical storm: results of the OBSERVational registry on long-term outcome of ICD patients (OBSERVO-ICD). Europace 2018;20:979–85. [DOI] [PubMed] [Google Scholar]
- 13. Guerra F, Shkoza M, Scappini L, Flori M, Capucci A. Role of electrical storm as a mortality and morbidity risk factor and its clinical predictors: a meta-analysis. Europace 2014;16:347–53. [DOI] [PubMed] [Google Scholar]
- 14. Vergara P, Tung R, Vaseghi M, Brombin C, Frankel DS, Di Biase L et al. Successful ventricular tachycardia ablation in patients with electrical storm reduces recurrences and improves survival. Heart Rhythm 2018;15:48–55. [DOI] [PubMed] [Google Scholar]
- 15. Muller J, Behnes M, Ellguth D, Schupp T, Taton G, Reiser L et al. Prognostic impact of left ventricular ejection fraction in patients with electrical storm. J Interv Card Electrophysiol 2019;55:307–15. [DOI] [PubMed] [Google Scholar]
- 16. El-Battrawy I, Roterberg G, Kowitz J, Aweimer A, Lang S, Mugge A et al. Incidence, recurrence and management of electrical storm in Brugada syndrome. Front Cardiovasc Med 2022;9:981715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. van der Werf C, Lieve KV, Bos JM, Lane CM, Denjoy I, Roses-Noguer F et al. Implantable cardioverter-defibrillators in previously undiagnosed patients with catecholaminergic polymorphic ventricular tachycardia resuscitated from sudden cardiac arrest. Eur Heart J 2019;40:2953–61. [DOI] [PubMed] [Google Scholar]
- 18. Della Bella P, Baratto F, Tsiachris D, Trevisi N, Vergara P, Bisceglia C et al. Management of ventricular tachycardia in the setting of a dedicated unit for the treatment of complex ventricular arrhythmias: long-term outcome after ablation. Circulation 2013;127:1359–68. [DOI] [PubMed] [Google Scholar]
- 19. Gadula-Gacek E, Tajstra M, Niedziela J, Pyka L, Gasior M. Characteristics and outcomes in patients with electrical storm. Am J Cardiol 2019;123:1637–42. [DOI] [PubMed] [Google Scholar]
- 20. Behnes M, Muller J, Ellguth D, Schupp T, Taton G, Reiser L et al. Electrical storm is associated with impaired prognosis compared to ventricular tachyarrhythmias. Int J Cardiol 2019;292:119–25. [DOI] [PubMed] [Google Scholar]
- 21. Muller J, Behnes M, Ellguth D, Schupp T, Taton G, Reiser L et al. Prognostic impact of atrial fibrillation in electrical storm. Cardiology 2019;144:9–17. [DOI] [PubMed] [Google Scholar]
- 22. Jentzer JC, Noseworthy PA, Kashou AH, May AM, Chrispin J, Kabra R et al. Multidisciplinary critical care management of electrical storm: JACC state-of-the-art review. J Am Coll Cardiol 2023;81:2189–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stuber T, Eigenmann C, Delacretaz E. Characteristics and relevance of clustering ventricular arrhythmias in defibrillator recipients. Pacing Clin Electrophysiol 2005;28:702–7. [DOI] [PubMed] [Google Scholar]
- 24. Tsuji Y, Hojo M, Voigt N, El-Armouche A, Inden Y, Murohara T et al. Ca(2+)-related signaling and protein phosphorylation abnormalities play central roles in a new experimental model of electrical storm. Circulation 2011;123:2192–203. [DOI] [PubMed] [Google Scholar]
- 25. Hohnloser SH, Al-Khalidi HR, Pratt CM, Brum JM, Tatla DS, Tchou P et al. Electrical storm in patients with an implantable defibrillator: incidence, features, and preventive therapy: insights from a randomized trial. Eur Heart J 2006;27:3027–32. [DOI] [PubMed] [Google Scholar]
- 26. Nademanee K, Taylor R, Bailey WE, Rieders DE, Kosar EM. Treating electrical storm: sympathetic blockade versus advanced cardiac life support-guided therapy. Circulation 2000;102:742–7. [DOI] [PubMed] [Google Scholar]
- 27. Schwartz PJ, Billman GE, Stone HL. Autonomic mechanisms in ventricular fibrillation induced by myocardial ischemia during exercise in dogs with healed myocardial infarction. An experimental preparation for sudden cardiac death. Circulation 1984;69:790–800. [DOI] [PubMed] [Google Scholar]
- 28. Rangaraju A, Krishnan S, Aparna G, Sankaran S, Mannan AU, Rao BH. Genetic variants in post myocardial infarction patients presenting with electrical storm of unstable ventricular tachycardia. Indian Pacing Electrophysiol J 2018;18:91–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Patel RB, Ng J, Reddy V, Chokshi M, Parikh K, Subacius H et al. Early repolarization associated with ventricular arrhythmias in patients with chronic coronary artery disease. Circ Arrhythm Electrophysiol 2010;3:489–95. [DOI] [PubMed] [Google Scholar]
- 30. Rath B, Willy K, Ellermann C, Leitz P, Köbe J, Reinke F et al. Outcome of patients with idiopathic ventricular fibrillation and correlation with ECG markers of early repolarization. Clin Res Cardiol 2022;112:1748–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bansch D, Oyang F, Antz M, Arentz T, Weber R, Val-Mejias JE et al. Successful catheter ablation of electrical storm after myocardial infarction. Circulation 2003;108:3011–6. [DOI] [PubMed] [Google Scholar]
- 32. Kumar S, Fujii A, Kapur S, Romero J, Mehta NK, Tanigawa S et al. Beyond the storm: comparison of clinical factors, arrhythmogenic substrate, and catheter ablation outcomes in structural heart disease patients with versus those without a history of ventricular tachycardia storm. J Cardiovasc Electrophysiol 2017;28:56–67. [DOI] [PubMed] [Google Scholar]
- 33. Brigadeau F, Kouakam C, Klug D, Marquie C, Duhamel A, Mizon-Gerard F et al. Clinical predictors and prognostic significance of electrical storm in patients with implantable cardioverter defibrillators. Eur Heart J 2006;27:700–7. [DOI] [PubMed] [Google Scholar]
- 34. Wasmer K, Reinecke H, Heitmann M, Dechering DG, Reinke F, Lange PS et al. Clinical, procedural and long-term outcome of ischemic VT ablation in patients with previous anterior versus inferior myocardial infarction. Clin Res Cardiol 2020;109:1282–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Frommeyer G, Eckardt L. Drug-induced proarrhythmia: risk factors and electrophysiological mechanisms. Nat Rev Cardiol 2016;13:36–47. [DOI] [PubMed] [Google Scholar]
- 36. Shimizu W, Aiba T, Antzelevitch C. Specific therapy based on the genotype and cellular mechanism in inherited cardiac arrhythmias. Long QT syndrome and Brugada syndrome. Curr Pharm Des 2005;11:1561–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Han W, Wang Z, Nattel S. Slow delayed rectifier current and repolarization in canine cardiac Purkinje cells. Am J Physiol Heart Circ Physiol 2001;280:H1075–80. [DOI] [PubMed] [Google Scholar]
- 38. Abi-Gerges N, Small BG, Lawrence CL, Hammond TG, Valentin JP, Pollard CE. Gender differences in the slow delayed (IKs) but not in inward (IK1) rectifier K+ currents of canine Purkinje fibre cardiac action potential: key roles for IKs, beta-adrenoceptor stimulation, pacing rate and gender. Br J Pharmacol 2006;147:653–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Liu GX, Choi BR, Ziv O, Li W, de Lange E, Qu Z et al. Differential conditions for early after-depolarizations and triggered activity in cardiomyocytes derived from transgenic LQT1 and LQT2 rabbits. J Physiol 2012;590:1171–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Novak A, Barad L, Zeevi-Levin N, Shick R, Shtrichman R, Lorber A et al. Cardiomyocytes generated from CPVTD307H patients are arrhythmogenic in response to β-adrenergic stimulation. J Cell Mol Med 2012;16:468–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Willis BC, Pandit SV, Ponce-Balbuena D, Zarzoso M, Guerrero-Serna G, Limbu B et al. Constitutive intracellular na+ excess in Purkinje cells promotes arrhythmogenesis at lower levels of stress than ventricular myocytes from mice with catecholaminergic polymorphic ventricular tachycardia. Circulation 2016;133:2348–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kaufman ES. Mechanisms and clinical management of inherited channelopathies: long QT syndrome, Brugada syndrome, catecholaminergic polymorphic ventricular tachycardia, and short QT syndrome. Heart Rhythm 2009;6:S51–5. [DOI] [PubMed] [Google Scholar]
- 43. Antzelevitch C, Pollevick GD, Cordeiro JM, Casis O, Sanguinetti MC, Aizawa Y et al. Loss-of-function mutations in the cardiac calcium channel underlie a new clinical entity characterized by ST-segment elevation, short QT intervals, and sudden cardiac death. Circulation 2007;115:442–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Aizawa Y, Sato M, Ohno S, Horie M, Takatsuki S, Fukuda K et al. Circadian pattern of fibrillatory events in non-Brugada-type idiopathic ventricular fibrillation with a focus on J waves. Heart Rhythm 2014;11:2261–6. [DOI] [PubMed] [Google Scholar]
- 45. Miyazaki H, Nakagawa M, Shin Y, Wakisaka O, Shinohara T, Ezaki K et al. Comparison of autonomic J-wave modulation in patients with idiopathic ventricular fibrillation and control subjects. Circ J 2013;77:330–7. [DOI] [PubMed] [Google Scholar]
- 46. Ali SH, Nilsson KR. Electrical storm in a patient with Brugada syndrome and coronavirus disease 2019. J Innov Card Rhythm Manag 2022;13:5019–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Chen M, Xu DZ, Wu AZ, Guo S, Wan J, Yin D et al. Concomitant SK current activation and sodium current inhibition cause J wave syndrome. JCI Insight 2018;3:e122329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Antzelevitch C. Role of spatial dispersion of repolarization in inherited and acquired sudden cardiac death syndromes. Am J Physiol Heart Circ Physiol 2007;293:H2024–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Miles C, Asimaki A, Ster IC, Papadakis M, Gray B, Westaby J et al. Biventricular myocardial fibrosis and sudden death in patients with Brugada syndrome. J Am Coll Cardiol 2021;78:1511–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Martini B, Nava A, Thiene G, Buja GF, Canciani B, Scognamiglio R et al. Ventricular fibrillation without apparent heart disease: description of six cases. Am Heart J 1989;118:1203–9. [DOI] [PubMed] [Google Scholar]
- 51. Haïssaguerre M, Duchateau J, Dubois R, Hocini M, Cheniti G, Sacher F et al. Idiopathic ventricular fibrillation: role of Purkinje system and microstructural myocardial abnormalities. JACC Clin Electrophysiol 2020;6:591–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Jiang S, Yin X, Dong C, Xia Y, Liu J. Epicardial radiofrequency catheter ablation of Brugada syndrome with electrical storm during ventricular fibrillation: a case report. Med. (Baltim.) 2017;96:e8688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Shelke A, Tachil A, Saggu D, Jesuraj ML, Yalagudri S, Narasimhan C. Catheter ablation for electrical storm in Brugada syndrome: results of substrate based ablation. Indian Heart J 2018;70:296–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Haïssaguerre M, Nademanee W, Hocini M, Duchateau J, André C, Lavergne T et al. The Spectrum of idiopathic ventricular fibrillation and J-wave syndromes: novel mapping insights. Card Electrophysiol Clin 2019;11:699–709. [DOI] [PubMed] [Google Scholar]
- 55. Qifang L, Jing H, Yidong Z, Long Y. Ablation of premature ventricular contraction triggering ventricular fibrillation in a patient with early repolarization syndrome. Ann Noninvasive Electrocardiol 2021;26:e12792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Yoon N, Patocskai B, Antzelevitch C. Epicardial substrate as a target for radiofrequency ablation in an experimental model of early repolarization syndrome. Circ Arrhythm Electrophysiol 2018;11:e006511. [DOI] [PubMed] [Google Scholar]
- 57. Miles C, Boukens BJ, Scrocco C, Wilde AAM, Nademanee K, Haissaguerre M et al. Subepicardial cardiomyopathy: a disease underlying J-wave syndromes and idiopathic ventricular fibrillation. Circulation 2023;147:1622–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Hoogendijk MG, Potse M, Vinet A, de Bakker JM, Coronel R. ST segment elevation by current-to-load mismatch: an experimental and computational study. Heart Rhythm 2011;8:111–8. [DOI] [PubMed] [Google Scholar]
- 59. Brugada R, Hong K, Dumaine R, Cordeiro J, Gaita F, Borggrefe M et al. Sudden death associated with short-QT syndrome linked to mutations in HERG. Circulation 2004;109:30–5. [DOI] [PubMed] [Google Scholar]
- 60. Bellocq C, van Ginneken AC, Bezzina CR, Alders M, Escande D, Mannens MM et al. Mutation in the KCNQ1 gene leading to the short QT-interval syndrome. Circulation 2004;109:2394–7. [DOI] [PubMed] [Google Scholar]
- 61. Almahameed ST, Kaufman ES. Idiopathic ventricular fibrillation: diagnosis, ablation of triggers, gaps in knowledge, and future directions. J Innov Card Rhythm Manag 2020;11:4135–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Xiao L, Koopmann TT, Ördög B, Postema PG, Verkerk AO, Iyer V et al. Unique cardiac Purkinje fiber transient outward current β-subunit composition: a potential molecular link to idiopathic ventricular fibrillation. Circ Res 2013;112:1310–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Wilde AAM, Garan H, Boyden PA. Role of the Purkinje system in heritable arrhythmias. Heart Rhythm 2019;16:1121–6. [DOI] [PubMed] [Google Scholar]
- 64. Inoue H, Zipes DP. Time course of denervation of efferent sympathetic and vagal nerves after occlusion of the coronary artery in the canine heart. Circ Res 1988;62:1111–20. [DOI] [PubMed] [Google Scholar]
- 65. Cao JM, Fishbein MC, Han JB, Lai WW, Lai AC, Wu TJ et al. Relationship between regional cardiac hyperinnervation and ventricular arrhythmia. Circulation 2000;101:1960–9. [DOI] [PubMed] [Google Scholar]
- 66. Vaseghi M, Lux RL, Mahajan A, Shivkumar K. Sympathetic stimulation increases dispersion of repolarization in humans with myocardial infarction. Am J Physiol Heart Circ Physiol 2012;302:H1838–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Sridharan A, Bradfield JS, Shivkumar K, Ajijola OA. Autonomic nervous system and arrhythmias in structural heart disease. Auton Neurosci 2022;243:103037. [DOI] [PubMed] [Google Scholar]
- 68. Herring N, Cranley J, Lokale MN, Li D, Shanks J, Alston EN et al. The cardiac sympathetic co-transmitter galanin reduces acetylcholine release and vagal bradycardia: implications for neural control of cardiac excitability. J Mol Cell Cardiol 2012;52:667–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Paul M, Wichter T, Kies P, Gerss J, Wollmann C, Rahbar K et al. Cardiac sympathetic dysfunction in genotyped patients with arrhythmogenic right ventricular cardiomyopathy and risk of recurrent ventricular tachyarrhythmias. J Nucl Med 2011;52:1559–65. [DOI] [PubMed] [Google Scholar]
- 70. Tilz RR, Lin T, Eckardt L, Deneke T, Andresen D, Wieneke H et al. Ablation outcomes and predictors of mortality following catheter ablation for ventricular tachycardia: data from the German Multicenter Ablation Registry. J Am Heart Assoc 2018;7:e007045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Wood MA, Simpson PM, Stambler BS, Herre JM, Bernstein RC, Ellenbogen KA. Long-term temporal patterns of ventricular tachyarrhythmias. Circulation 1995;91:2371–7. [DOI] [PubMed] [Google Scholar]
- 72. Bansch D, Bocker D, Brunn J, Weber M, Breithardt G, Block M. Clusters of ventricular tachycardias signify impaired survival in patients with idiopathic dilated cardiomyopathy and implantable cardioverter defibrillators. J Am Coll Cardiol 2000;36:566–73. [DOI] [PubMed] [Google Scholar]
- 73. Gatzoulis KA, Andrikopoulos GK, Apostolopoulos T, Sotiropoulos E, Zervopoulos G, Antoniou J et al. Electrical storm is an independent predictor of adverse long-term outcome in the era of implantable defibrillator therapy. Europace 2005;7:184–92. [DOI] [PubMed] [Google Scholar]
- 74. Kowlgi GN, Cha YM. Management of ventricular electrical storm: a contemporary appraisal. Europace 2020;22:1768–80. [DOI] [PubMed] [Google Scholar]
- 75. Dubner S, Valero E, Pesce R, Zuelgaray JG, Mateos JC, Filho SG et al. A Latin American registry of implantable cardioverter defibrillators: the ICD-LABOR study. Ann Noninvasive Electrocardiol 2005;10:420–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Koizumi T, Kamada R, Watanabe M, Yokoshiki H, Temma T, Hagiwara H et al. Predictors of cardiovascular mortality after an electrical storm in patients with structural heart disease. J Cardiol 2022;80:167–71. [DOI] [PubMed] [Google Scholar]
- 77. Weidner K, Behnes M, Schupp T, Hoppner J, Ansari U, Mueller J et al. Chronic kidney disease impairs prognosis in electrical storm. J Interv Card Electrophysiol 2022;63:13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Weidner KJ, Schupp T, Rusnak J, Muller J, Taton G, Reiser L et al. Prognostic impact of age and gender on patients with electrical storm. Cardiol J 2023;30:204–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Sweeney MO, Sherfesee L, DeGroot PJ, Wathen MS, Wilkoff BL. Differences in effects of electrical therapy type for ventricular arrhythmias on mortality in implantable cardioverter-defibrillator patients. Heart Rhythm 2010;7:353–60. [DOI] [PubMed] [Google Scholar]
- 80. Biton Y, Daimee UA, Baman JR, Kutyifa V, McNitt S, Polonsky B et al. Prognostic importance of defibrillator-appropriate shocks and antitachycardia pacing in patients with mild heart failure. J Am Heart Assoc 2019;8:e010346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Priori SG, Blomstrom-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J et al. 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: the task force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J 2015;36:2793–867. [DOI] [PubMed] [Google Scholar]
- 82. Conti S, Pala S, Biagioli V, Del Giorno G, Zucchetti M, Russo E et al. Electrical storm: a clinical and electrophysiological overview. World J Cardiol 2015;7:555–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Al'Aref SJ, Ip JE, Markowitz SM, Liu CF, Thomas G, Frenkel D et al. Differentiation of papillary muscle from fascicular and mitral annular ventricular arrhythmias in patients with and without structural heart disease. Circ Arrhythm Electrophysiol 2015;8:616–24. [DOI] [PubMed] [Google Scholar]
- 84. Tchou P, Mehdirad AA. Bundle branch reentry ventricular tachycardia. Pacing Clin Electrophysiol 1995;18:1427–37. [DOI] [PubMed] [Google Scholar]
- 85. Mazur A, Kusniec J, Strasberg B. Bundle branch reentrant ventricular tachycardia. Indian Pacing Electrophysiol J 2005;5:86–95. [PMC free article] [PubMed] [Google Scholar]
- 86. Valles E, Bazan V, Marchlinski FE. ECG criteria to identify epicardial ventricular tachycardia in nonischemic cardiomyopathy. Circ Arrhythm Electrophysiol 2010;3:63–71. [DOI] [PubMed] [Google Scholar]
- 87. Berruezo A, Mont L, Nava S, Chueca E, Bartholomay E, Brugada J. Electrocardiographic recognition of the epicardial origin of ventricular tachycardias. Circulation 2004;109:1842–7. [DOI] [PubMed] [Google Scholar]
- 88. Reithmann C, Fiek M, Aynur Z, Ulbrich M. Electrocardiographic criteria of epicardial ventricular tachycardia with anterior origin. Clin Res Cardiol 2019;108:254–63. [DOI] [PubMed] [Google Scholar]
- 89. Nakamura T, Schaeffer B, Tanigawa S, Muthalaly RG, John RM, Michaud GF et al. Catheter ablation of polymorphic ventricular tachycardia/fibrillation in patients with and without structural heart disease. Heart Rhythm 2019;16:1021–7. [DOI] [PubMed] [Google Scholar]
- 90. Skogestad J, Aronsen JM. Hypokalemia-induced arrhythmias and heart failure: new insights and implications for therapy. Front Physiol 2018;9:1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Schupp T, Behnes M, Zworowsky MV, Kim SH, Weidner K, Rusnak J et al. Hypokalemia but not hyperkalemia is associated with recurrences of ventricular tachyarrhythmias in ICD recipients. Clin Lab 2020;66:e190645. [DOI] [PubMed] [Google Scholar]
- 92. Erdogan HI, Gul EE, Gok H, Nikus KC. Therapy-resistant ventricular tachycardia caused by amiodarone-induced thyrotoxicosis: a case report of electrical storm. Am J Emerg Med 2012;30:2092.e5–7. [DOI] [PubMed] [Google Scholar]
- 93. Kruse JM, Enghard P, Schroder T, Hasper D, Kuhnle Y, Jorres A et al. Weak diagnostic performance of troponin, creatine kinase and creatine kinase-MB to diagnose or exclude myocardial infarction after successful resuscitation. Int J Cardiol 2014;173:216–21. [DOI] [PubMed] [Google Scholar]
- 94. Ouali S, Guermazi O, Ben Halima M, Boudiche S, Khedher N, Adeljalil F et al. Ventricular tachycardia revealing drug abuse induced myocarditis: two case reports. Clin Case Rep 2018;6:1225–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Dominic P, Ahmad J, Awwab H, Bhuiyan MS, Kevil CG, Goeders NE et al. Stimulant drugs of abuse and cardiac arrhythmias. Circ Arrhythm Electrophysiol 2022;15:e010273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A et al. 2023 ESC guidelines for the management of acute coronary syndromes. G Ital Cardiol (Rome) 2024;25:e1–e112. [DOI] [PubMed] [Google Scholar]
- 97. Arias MA, Peinado R, Sanchez AM, Merino JL. Incessant ventricular tachycardia acutely controlled with intracoronary injection of radiographic contrast media. Am J Emerg Med 2006;24:290–2. [DOI] [PubMed] [Google Scholar]
- 98. Ammirati E, Frigerio M, Adler ED, Basso C, Birnie DH, Brambatti M et al. Management of acute myocarditis and chronic inflammatory cardiomyopathy: an expert consensus document. Circ Heart Fail 2020;13:e007405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Peretto G, Busnardo E, Ferro P, Palmisano A, Vignale D, Esposito A et al. Clinical applications of FDG-PET scan in arrhythmic myocarditis. JACC Cardiovasc Imaging 2022;15:1771–80. [DOI] [PubMed] [Google Scholar]
- 100. Hoogendoorn JC, Venlet J, Out YNJ, Man S, Kumar S, Sramko M et al. The precordial R’ wave: a novel discriminator between cardiac sarcoidosis and arrhythmogenic right ventricular cardiomyopathy in patients presenting with ventricular tachycardia. Heart Rhythm 2021;18:1539–47. [DOI] [PubMed] [Google Scholar]
- 101. Sweeney MO, Ruetz LL, Belk P, Mullen TJ, Johnson JW, Sheldon T. Bradycardia pacing-induced short-long-short sequences at the onset of ventricular tachyarrhythmias: a possible mechanism of proarrhythmia? J Am Coll Cardiol 2007;50:614–22. [DOI] [PubMed] [Google Scholar]
- 102. Tseng ZH, Hayward RM, Clark NM, Mulvanny CG, Colburn BJ, Ursell PC et al. Sudden death in patients with cardiac implantable electronic devices. JAMA Intern Med 2015;175:1342–50. [DOI] [PubMed] [Google Scholar]
- 103. Yamamoto T, Takayama M, Sato N, Yodogawa K, Iwasaki YK, Kato K et al. Inappropriate analyses of automated external defibrillators used during in-hospital ventricular fibrillation. Circ J 2008;72:679–81. [DOI] [PubMed] [Google Scholar]
- 104. Guerra F, Palmisano P, Dell'Era G, Ziacchi M, Ammendola E, Bonelli P et al. Implantable cardioverter-defibrillator programming and electrical storm: results of the OBSERVational registry on long-term outcome of ICD patients (OBSERVO-ICD). Heart Rhythm 2016;13:1987–92. [DOI] [PubMed] [Google Scholar]
- 105. Lusebrink U, Duncker D, Hess M, Heinrichs I, Gardiwal A, Oswald H et al. Clinical relevance of slow ventricular tachycardia in heart failure patients with primary prophylactic implantable cardioverter defibrillator indication. Europace 2013;15:820–6. [DOI] [PubMed] [Google Scholar]
- 106. Sadoul N, Mletzko R, Anselme F, Bowes R, Schols W, Kouakam C et al. Incidence and clinical relevance of slow ventricular tachycardia in implantable cardioverter-defibrillator recipients: an international multicenter prospective study. Circulation 2005;112:946–53. [DOI] [PubMed] [Google Scholar]
- 107. Geri G, Dumas F, Bougouin W, Varenne O, Daviaud F, Pene F et al. Immediate percutaneous coronary intervention is associated with improved short- and long-term survival after out-of-hospital cardiac arrest. Circ Cardiovasc Interv 2015;8:e002303. [DOI] [PubMed] [Google Scholar]
- 108. Vyas A, Chan PS, Cram P, Nallamothu BK, McNally B, Girotra S. Early coronary angiography and survival after out-of-hospital cardiac arrest. Circ Cardiovasc Interv 2015;8:e002321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Crowley CP, Salciccioli JD, Kim EY. The association between ACLS guideline deviations and outcomes from in-hospital cardiac arrest. Resuscitation 2020;153:65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Soar J, Bottiger BW, Carli P, Couper K, Deakin CD, Djarv T et al. European resuscitation council guidelines 2021: adult advanced life support. Resuscitation 2021;161:115–51. [DOI] [PubMed] [Google Scholar]
- 111. Aggarwal G, Anantha-Narayanan M, Robles J, Bandyopadhyay D, Abed M, Henry BM et al. External versus internal cardioversion for atrial fibrillation: a meta-analysis of randomized controlled trials. J Interv Card Electrophysiol 2021;61:445–51. [DOI] [PubMed] [Google Scholar]
- 112. Cheskes S, Dorian P, Scales DC. Defibrillation strategies for refractory ventricular fibrillation. Reply. N Engl J Med 2023;388:861–3. [DOI] [PubMed] [Google Scholar]
- 113. Wyckoff MH, Greif R, Morley PT, Ng KC, Olasveengen TM, Singletary EM et al. 2022 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the basic life support; advanced life support; pediatric life support; neonatal life support; education, implementation, and teams; and first aid task forces. Resuscitation 2022;181:208–88. [DOI] [PubMed] [Google Scholar]
- 114. Conrad SA, Broman LM, Taccone FS, Lorusso R, Malfertheiner MV, Pappalardo F et al. The Extracorporeal Life Support Organization Maastricht Treaty for nomenclature in extracorporeal life support. A position paper of the extracorporeal life support organization. Am J Respir Crit Care Med 2018;198:447–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Wyckoff MH, Greif R, Morley PT, Ng KC, Olasveengen TM, Singletary EM et al. 2022 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the basic life support; advanced life support; pediatric life support; neonatal life support; education, implementation, and teams; and first aid task Forces. Circulation 2022;146:e483–557. [DOI] [PubMed] [Google Scholar]
- 116. Soar J, Bottiger BW, Carli P, Couper K, Deakin CD, Djarv T et al. [Adult advanced life support]. Notf Rett Med 2021;24:406–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Perkins GD, Ji C, Deakin CD, Quinn T, Nolan JP, Scomparin C et al. A randomized trial of epinephrine in out-of-hospital cardiac arrest. N Engl J Med 2018;379:711–21. [DOI] [PubMed] [Google Scholar]
- 118. Fernando SM, Mathew R, Sadeghirad B, Rochwerg B, Hibbert B, Munshi L et al. Epinephrine in out-of-hospital cardiac arrest: a network meta-analysis and subgroup analyses of shockable and nonshockable rhythms. Chest 2023;164:381–93. [DOI] [PubMed] [Google Scholar]
- 119. Mariani S, Napp LC, Lo Coco V, Delnoij TSR, Luermans J, Ter Bekke RMA et al. Mechanical circulatory support for life-threatening arrhythmia: a systematic review. Int J Cardiol 2020;308:42–9. [DOI] [PubMed] [Google Scholar]
- 120. Al-Gobari M, El Khatib C, Pillon F, Gueyffier F. Beta-blockers for the prevention of sudden cardiac death in heart failure patients: a meta-analysis of randomized controlled trials. BMC Cardiovasc Disord 2013;13:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Pitt B, White H, Nicolau J, Martinez F, Gheorghiade M, Aschermann M et al. Eplerenone reduces mortality 30 days after randomization following acute myocardial infarction in patients with left ventricular systolic dysfunction and heart failure. J Am Coll Cardiol 2005;46:425–31. [DOI] [PubMed] [Google Scholar]
- 122. Priori SG, Blomstrom-Lundqvist C. 2015 European Society of Cardiology guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death summarized by co-chairs. Eur Heart J 2015;36:2757–9. [DOI] [PubMed] [Google Scholar]
- 123. Cojocaru C, Nastasa A, Bogdan S, Iorgulescu C, Deaconu A, Onciul S et al. Non-revascularized chronic total occlusions impact on substrate and post-ablation results in drug-refractory electrical storm. Front Cardiovasc Med 2023;10:1258373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Muller J, Behnes M, Ellguth D, Schupp T, Taton G, Reiser L et al. Distribution and prognostic impact of coronary artery disease and nonischemic cardiomyopathies in patients with electrical storm. Coron Artery Dis 2022;33:403–12. [DOI] [PubMed] [Google Scholar]
- 125. Wit AL, Allessie MA, Bonke FI, Lammers W, Smeets J, Fenoglio JJ Jr. Electrophysiologic mapping to determine the mechanism of experimental ventricular tachycardia initiated by premature impulses. Experimental approach and initial results demonstrating reentrant excitation. Am J Cardiol 1982;49:166–85. [DOI] [PubMed] [Google Scholar]
- 126. Alkhalaileh F, Wazni OM, Kiang A, Parker J, Ellis S, Kanj M et al. Ischemic or coronary evaluations in patients with monomorphic VT electrical storm undergoing VT ablation. JACC Clin Electrophysiol 2023;9:1890–9. [DOI] [PubMed] [Google Scholar]
- 127. Caforio AL, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology working group on myocardial and pericardial diseases. Eur Heart J 2013;34:2636-48, 48a-48d. [DOI] [PubMed] [Google Scholar]
- 128. Papageorgiou N, Providência R, Bronis K, Dechering DG, Srinivasan N, Eckardt L et al. Catheter ablation for ventricular tachycardia in patients with cardiac sarcoidosis: a systematic review. Europace 2018;20:682–91. [DOI] [PubMed] [Google Scholar]
- 129. Frustaci A, Russo MA, Chimenti C. Randomized study on the efficacy of immunosuppressive therapy in patients with virus-negative inflammatory cardiomyopathy: the TIMIC study. Eur Heart J 2009;30:1995–2002. [DOI] [PubMed] [Google Scholar]
- 130. Dello Russo A, Casella M, Pieroni M, Pelargonio G, Bartoletti S, Santangeli P et al. Drug-refractory ventricular tachycardias after myocarditis: endocardial and epicardial radiofrequency catheter ablation. Circ Arrhythm Electrophysiol 2012;5:492–8. [DOI] [PubMed] [Google Scholar]
- 131. Roterberg G, El-Battrawy I, Veith M, Liebe V, Ansari U, Lang S et al. Arrhythmic events in Brugada syndrome patients induced by fever. Ann Noninvasive Electrocardiol 2020;25:e12723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Cohen RB, Dai M, Aizer A, Barbhaiya C, Peterson C, Bernstein S et al. QT interval dynamics and triggers for QT prolongation immediately following cardiac arrest. Resuscitation 2021;162:171–9. [DOI] [PubMed] [Google Scholar]
- 133. Lebiedz P, Meiners J, Samol A, Wasmer K, Reinecke H, Waltenberger J et al. Electrocardiographic changes during therapeutic hypothermia. Resuscitation 2012;83:602–6. [DOI] [PubMed] [Google Scholar]
- 134. Etheridge SP, Compton SJ, Tristani-Firouzi M, Mason JW. A new oral therapy for long QT syndrome: long-term oral potassium improves repolarization in patients with HERG mutations. J Am Coll Cardiol 2003;42:1777–82. [DOI] [PubMed] [Google Scholar]
- 135. Tan HL, Alings M, Van Olden RW, Wilde AA. Long-term (subacute) potassium treatment in congenital HERG-related long QT syndrome (LQTS2). J Cardiovasc Electrophysiol 1999;10:229–33. [DOI] [PubMed] [Google Scholar]
- 136. Eryol NK, Colak R, Ozdogru I, Tanriverdi F, Unal S, Topsakal R et al. Effects of calcium treatment on QT interval and QT dispersion in hypocalcemia. Am J Cardiol 2003;91:750–2. [DOI] [PubMed] [Google Scholar]
- 137. Tzivoni D, Banai S, Schuger C, Benhorin J, Keren A, Gottlieb S et al. Treatment of torsade de pointes with magnesium sulfate. Circulation 1988;77:392–7. [DOI] [PubMed] [Google Scholar]
- 138. Nayak HM, Verdino RJ, Russo AM, Gerstenfeld EP, Hsia HH, Lin D et al. Ventricular tachycardia storm after initiation of biventricular pacing: incidence, clinical characteristics, management, and outcome. J Cardiovasc Electrophysiol 2008;19:708–15. [DOI] [PubMed] [Google Scholar]
- 139. Wilkoff BL, Fauchier L, Stiles MK, Morillo CA, Al-Khatib SM, Almendral J et al. 2015 HRS/EHRA/APHRS/SOLAECE expert consensus statement on optimal implantable cardioverter-defibrillator programming and testing. Europace 2016;18:159–83. [DOI] [PubMed] [Google Scholar]
- 140. Bundgaard JS, Jacobsen PK, Grand J, Lindholm MG, Hassager C, Pehrson S et al. Deep sedation as temporary bridge to definitive treatment of ventricular arrhythmia storm. Eur Heart J Acute Cardiovasc Care 2020;9:657–64. [DOI] [PubMed] [Google Scholar]
- 141. Martins RP, Urien JM, Barbarot N, Rieul G, Sellal JM, Borella L et al. Effectiveness of deep sedation for patients with intractable electrical storm refractory to antiarrhythmic drugs. Circulation 2020;142:1599–601. [DOI] [PubMed] [Google Scholar]
- 142. Muser D, Santangeli P, Liang JJ. Management of ventricular tachycardia storm in patients with structural heart disease. World J Cardiol 2017;9:521–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Mulpuru SK, Patel DV, Wilbur SL, Vasavada BC, Furqan T. Electrical storm and termination with propofol therapy: a case report. Int J Cardiol 2008;128:e6–8. [DOI] [PubMed] [Google Scholar]
- 144. Ebert TJ, Muzi M, Berens R, Goff D, Kampine JP. Sympathetic responses to induction of anesthesia in humans with propofol or etomidate. Anesthesiology 1992;76:725–33. [DOI] [PubMed] [Google Scholar]
- 145. Smith H, Sinson G, Varelas P. Vasopressors and propofol infusion syndrome in severe head trauma. Neurocrit Care 2009;10:166–72. [DOI] [PubMed] [Google Scholar]
- 146. Sakabe M, Fujiki A, Inoue H. Propofol induced marked prolongation of QT interval in a patient with acute myocardial infarction. Anesthesiology 2002;97:265–6. [DOI] [PubMed] [Google Scholar]
- 147. Mandel JE, Hutchinson MD, Marchlinski FE. Remifentanil-midazolam sedation provides hemodynamic stability and comfort during epicardial ablation of ventricular tachycardia. J Cardiovasc Electrophysiol 2011;22:464–6. [DOI] [PubMed] [Google Scholar]
- 148. Zhong Q, Kumar A, Deshmukh A, Bennett C. Dexmedetomidine reduces incidences of ventricular arrhythmias in adult patients: a meta-analysis. Cardiol Res Pract 2022;2022:5158362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Chatzidou S, Kontogiannis C, Tsilimigras DI, Georgiopoulos G, Kosmopoulos M, Papadopoulou E et al. Propranolol versus metoprolol for treatment of electrical storm in patients with implantable cardioverter-defibrillator. J Am Coll Cardiol 2018;71:1897–906. [DOI] [PubMed] [Google Scholar]
- 150. Viskin S, Chorin E, Viskin D, Hochstadt A, Halkin A, Tovia-Brodie O et al. Quinidine-responsive polymorphic ventricular tachycardia in patients with coronary heart disease. Circulation 2019;139:2304–14. [DOI] [PubMed] [Google Scholar]
- 151. Viskin S, Hochstadt A, Chorin E, Viskin D, Havakuk O, Khoury S et al. Quinidine-responsive out-of-hospital polymorphic ventricular tachycardia in patients with coronary heart disease. Europace 2020;22:265–73. [DOI] [PubMed] [Google Scholar]
- 152. Ikeda T, Shiga T, Shimizu W, Kinugawa K, Sakamoto A, Nagai R et al. Efficacy and safety of the ultra-short-acting beta1-selective blocker landiolol in patients with recurrent hemodynamically unstable ventricular tachyarrhymias- outcomes of J-Land II study. Circ J 2019;83:1456–62. [DOI] [PubMed] [Google Scholar]
- 153. Miwa Y, Ikeda T, Mera H, Miyakoshi M, Hoshida K, Yanagisawa R et al. Effects of landiolol, an ultra-short-acting beta1-selective blocker, on electrical storm refractory to class III antiarrhythmic drugs. Circ J 2010;74:856–63. [DOI] [PubMed] [Google Scholar]
- 154. Ortiz M, Martin A, Arribas F, Coll-Vinent B, Del Arco C, Peinado R et al. Randomized comparison of intravenous procainamide vs. intravenous amiodarone for the acute treatment of tolerated wide QRS tachycardia: the PROCAMIO study. Eur Heart J 2017;38:1329–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Kerin NZ, Blevins RD, Frumin H, Faitel K, Rubenfire M. Intravenous and oral loading versus oral loading alone with amiodarone for chronic refractory ventricular arrhythmias. Am J Cardiol 1985;55:89–91. [DOI] [PubMed] [Google Scholar]
- 156. Gorgels AP, van den Dool A, Hofs A, Mulleneers R, Smeets JL, Vos MA et al. Comparison of procainamide and lidocaine in terminating sustained monomorphic ventricular tachycardia. Am J Cardiol 1996;78:43–6. [DOI] [PubMed] [Google Scholar]
- 157. Ho DS, Zecchin RP, Richards DA, Uther JB, Ross DL. Double-blind trial of lignocaine versus sotalol for acute termination of spontaneous sustained ventricular tachycardia. Lancet 1994;344:18–23. [DOI] [PubMed] [Google Scholar]
- 158. Lie KI, Wellens HJ, van Capelle FJ, Durrer D. Lidocaine in the prevention of primary ventricular fibrillation. A double-blind, randomized study of 212 consecutive patients. N Engl J Med 1974;291:1324–6. [DOI] [PubMed] [Google Scholar]
- 159. Marti-Carvajal AJ, Simancas-Racines D, Anand V, Bangdiwala S. Prophylactic lidocaine for myocardial infarction. Cochrane Database Syst Rev 2015;2015:CD008553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Tsuboi M, Chiba S. Effects of lidocaine on isolated, blood-perfused ventricular contractility in the dog. Heart Vessels 1999;14:289–94. [DOI] [PubMed] [Google Scholar]
- 161. Antzelevitch C, Burashnikov A, Sicouri S, Belardinelli L. Electrophysiologic basis for the antiarrhythmic actions of ranolazine. Heart Rhythm 2011;8:1281–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Zareba W, Daubert JP, Beck CA, Huang DT, Alexis JD, Brown MW et al. Ranolazine in high-risk patients with implanted cardioverter-defibrillators: the RAID trial. J Am Coll Cardiol 2018;72:636–45. [DOI] [PubMed] [Google Scholar]
- 163. Greene M, Newman D, Geist M, Paquette M, Heng D, Dorian P. Is electrical storm in ICD patients the sign of a dying heart? Outcome of patients with clusters of ventricular tachyarrhythmias. Europace 2000;2:263–9. [DOI] [PubMed] [Google Scholar]
- 164. Ohgo T, Okamura H, Noda T, Satomi K, Suyama K, Kurita T et al. Acute and chronic management in patients with Brugada syndrome associated with electrical storm of ventricular fibrillation. Heart Rhythm 2007;4:695–700. [DOI] [PubMed] [Google Scholar]
- 165. Ten Sande JN, Postema PG, Boekholdt SM, Tan HL, van der Heijden JF, de Groot NM et al. Detailed characterization of familial idiopathic ventricular fibrillation linked to the DPP6 locus. Heart Rhythm 2016;13:905–12. [DOI] [PubMed] [Google Scholar]
- 166. Watanabe A, Fukushima Kusano K, Morita H, Miura D, Sumida W, Hiramatsu S et al. Low-dose isoproterenol for repetitive ventricular arrhythmia in patients with Brugada syndrome. Eur Heart J 2006;27:1579–83. [DOI] [PubMed] [Google Scholar]
- 167. Furniss G. Isoprenaline and quinidine to calm Brugada VF storm. BMJ Case Rep 2012;2012:bcr0420114156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Jongman JK, Jepkes-Bruin N, Ramdat Misier AR, Beukema WP, Delnoy PP, Oude Lutttikhuis H et al. Electrical storms in Brugada syndrome successfully treated with isoproterenol infusion and quinidine orally. Neth Heart J 2007;15:151–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Maury P, Couderc P, Delay M, Boveda S, Brugada J. Electrical storm in Brugada syndrome successfully treated using isoprenaline. Europace 2004;6:130–3. [DOI] [PubMed] [Google Scholar]
- 170. Mok NS, Chan NY, Chiu AC. Successful use of quinidine in treatment of electrical storm in Brugada syndrome. Pacing Clin Electrophysiol 2004;27:821–3. [DOI] [PubMed] [Google Scholar]
- 171. Pellegrino PL, Di Biase M, Brunetti ND. Quinidine for the management of electrical storm in an old patient with Brugada syndrome and syncope. Acta Cardiol 2013;68:201–3. [DOI] [PubMed] [Google Scholar]
- 172. Sharif-Kazemi MB, Emkanjoo Z, Tavoosi A, Kafi M, Kheirkhah J, Alizadeh A et al. Electrical storm in Brugada syndrome during pregnancy. Pacing Clin Electrophysiol 2011;34:e18–21. [DOI] [PubMed] [Google Scholar]
- 173. Bun SS, Maury P, Giustetto C, Deharo JC. Electrical storm in short-QT syndrome successfully treated with isoproterenol. J Cardiovasc Electrophysiol 2012;23:1028–30. [DOI] [PubMed] [Google Scholar]
- 174. Bellamy D, Nuthall G, Dalziel S, Skinner JR. Catecholaminergic polymorphic ventricular tachycardia: the cardiac arrest where epinephrine is contraindicated. Pediatr Crit Care Med 2019;20:262–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Yannopoulos D, Bartos J, Raveendran G, Walser E, Connett J, Murray TA et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. Lancet 2020;396:1807–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Belohlavek J, Smalcova J, Rob D, Franek O, Smid O, Pokorna M et al. Effect of intra-arrest transport, extracorporeal cardiopulmonary resuscitation, and immediate invasive assessment and treatment on functional neurologic outcome in refractory out-of-hospital cardiac arrest: a randomized clinical trial. JAMA 2022;327:737–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Suverein MM, Delnoij TSR, Lorusso R, Brandon Bravo Bruinsma GJ, Otterspoor L, Elzo Kraemer CV et al. Early extracorporeal CPR for refractory out-of-hospital cardiac arrest. N Engl J Med 2023;388:299–309. [DOI] [PubMed] [Google Scholar]
- 178. Santangeli P, Muser D, Zado ES, Magnani S, Khetpal S, Hutchinson MD et al. Acute hemodynamic decompensation during catheter ablation of scar-related ventricular tachycardia: incidence, predictors, and impact on mortality. Circ Arrhythm Electrophysiol 2015;8:68–75. [DOI] [PubMed] [Google Scholar]
- 179. Chung FP, Liao YC, Lin YJ, Chang SL, Lo LW, Hu YF et al. Outcome of rescue ablation in patients with refractory ventricular electrical storm requiring mechanical circulation support. J Cardiovasc Electrophysiol 2020;31:9–17. [DOI] [PubMed] [Google Scholar]
- 180. Enriquez A, Liang J, Gentile J, Schaller RD, Supple GE, Frankel DS et al. Outcomes of rescue cardiopulmonary support for periprocedural acute hemodynamic decompensation in patients undergoing catheter ablation of electrical storm. Heart Rhythm 2018;15:75–80. [DOI] [PubMed] [Google Scholar]
- 181. Mathuria N, Wu G, Rojas-Delgado F, Shuraih M, Razavi M, Civitello A et al. Outcomes of pre-emptive and rescue use of percutaneous left ventricular assist device in patients with structural heart disease undergoing catheter ablation of ventricular tachycardia. J Interv Card Electrophysiol 2017;48:27–34. [DOI] [PubMed] [Google Scholar]
- 182. Muser D, Liang JJ, Castro SA, Hayashi T, Enriquez A, Troutman GS et al. Outcomes with prophylactic use of percutaneous left ventricular assist devices in high-risk patients undergoing catheter ablation of scar-related ventricular tachycardia: a propensity-score matched analysis. Heart Rhythm 2018;15:1500–6. [DOI] [PubMed] [Google Scholar]
- 183. Sroubek J, Vajapey R, Sipko JJ, Soltesz EG, Weiss AJ, Bhargava M et al. First-in-human experience with Impella 5.0/5.5 for high-risk patients with advanced heart failure undergoing VT ablation. J Am Coll Cardiol 2023;82:469–71. [DOI] [PubMed] [Google Scholar]
- 184. Luni FK, Zungsontiporn N, Farid T, Malik SA, Khan S, Daniels J et al. Percutaneous left ventricular assist device support during ablation of ventricular tachycardia: a meta-analysis of current evidence. J Cardiovasc Electrophysiol 2019;30:886–95. [DOI] [PubMed] [Google Scholar]
- 185. Tung R, Xue Y, Chen M, Jiang C, Shatz DY, Besser SA et al. First-line catheter ablation of monomorphic ventricular tachycardia in cardiomyopathy concurrent with defibrillator implantation: the PAUSE-SCD randomized trial. Circulation 2022;145:1839–49. [DOI] [PubMed] [Google Scholar]
- 186. Carbucicchio C, Santamaria M, Trevisi N, Maccabelli G, Giraldi F, Fassini G et al. Catheter ablation for the treatment of electrical storm in patients with implantable cardioverter-defibrillators: short- and long-term outcomes in a prospective single-center study. Circulation 2008;117:462–9. [DOI] [PubMed] [Google Scholar]
- 187. Jiménez Candil J, Castro JC, Hernández J, Fernández-Portales J, Durán M, Durán O et al. Timing of ablation and prognosis of patients with electrical storm and scar-related left ventricular dysfunction. Am J Cardiol 2020;136:87–93. [DOI] [PubMed] [Google Scholar]
- 188. Komatsu Y, Hocini M, Nogami A, Maury P, Peichl P, Iwasaki YK et al. Catheter ablation of refractory ventricular fibrillation storm after myocardial infarction. Circulation 2019;139:2315–25. [DOI] [PubMed] [Google Scholar]
- 189. Knecht S, Sacher F, Wright M, Hocini M, Nogami A, Arentz T et al. Long-term follow-up of idiopathic ventricular fibrillation ablation: a multicenter study. J Am Coll Cardiol 2009;54:522–8. [DOI] [PubMed] [Google Scholar]
- 190. Haissaguerre M, Shah DC, Jais P, Shoda M, Kautzner J, Arentz T et al. Role of Purkinje conducting system in triggering of idiopathic ventricular fibrillation. Lancet 2002;359:677–8. [DOI] [PubMed] [Google Scholar]
- 191. Brugada J, Berruezo A, Cuesta A, Osca J, Chueca E, Fosch X et al. Nonsurgical transthoracic epicardial radiofrequency ablation: an alternative in incessant ventricular tachycardia. J Am Coll Cardiol 2003;41:2036–43. [DOI] [PubMed] [Google Scholar]
- 192. Darma A, Bertagnolli L, Dinov B, Torri F, Shamloo AS, Lurz JA et al. Predictors of long-term mortality after catheter ablation of ventricular tachycardia in a contemporary cohort of patients with structural heart disease. Europace 2020;22:1672–9. [DOI] [PubMed] [Google Scholar]
- 193. Darma A, Bertagnolli L, Weber A, Dinov B, Torri F, Lurz JA et al. Epicardial ablation of ventricular tachycardia in patients with structural heart disease: a single-centre experience over 12 years. Europace 2021;23:1980–8. [DOI] [PubMed] [Google Scholar]
- 194. Belhassen B, Glick A, Viskin S. Excellent long-term reproducibility of the electrophysiologic efficacy of quinidine in patients with idiopathic ventricular fibrillation and Brugada syndrome. Pacing Clin Electrophysiol 2009;32:294–301. [DOI] [PubMed] [Google Scholar]
- 195. Leenhardt A, Glaser E, Burguera M, Nürnberg M, Maison-Blanche P, Coumel P. Short-coupled variant of torsade de pointes. A new electrocardiographic entity in the spectrum of idiopathic ventricular tachyarrhythmias. Circulation 1994;89:206–15. [DOI] [PubMed] [Google Scholar]
- 196. Aizawa Y, Chinushi M, Hasegawa K, Naiki N, Horie M, Kaneko Y et al. Electrical storm in idiopathic ventricular fibrillation is associated with early repolarization. J Am Coll Cardiol 2013;62:1015–9. [DOI] [PubMed] [Google Scholar]
- 197. Haïssaguerre M, Sacher F, Nogami A, Komiya N, Bernard A, Probst V et al. Characteristics of recurrent ventricular fibrillation associated with inferolateral early repolarization role of drug therapy. J Am Coll Cardiol 2009;53:612–9. [DOI] [PubMed] [Google Scholar]
- 198. Vaseghi M, Shivkumar K. The role of the autonomic nervous system in sudden cardiac death. Prog Cardiovasc Dis 2008;50:404–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Opthof T, Coronel R, Vermeulen JT, Verberne HJ, van Capelle FJ, Janse MJ. Dispersion of refractoriness in normal and ischaemic canine ventricle: effects of sympathetic stimulation. Cardiovasc Res 1993;27:1954–60. [DOI] [PubMed] [Google Scholar]
- 200. Priori SG, Mantica M, Schwartz PJ. Delayed afterdepolarizations elicited in vivo by left stellate ganglion stimulation. Circulation 1988;78:178–85. [DOI] [PubMed] [Google Scholar]
- 201. Yagishita D, Chui RW, Yamakawa K, Rajendran PS, Ajijola OA, Nakamura K et al. Sympathetic nerve stimulation, not circulating norepinephrine, modulates T-peak to T-end interval by increasing global dispersion of repolarization. Circ Arrhythm Electrophysiol 2015;8:174–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Hjalmarson A. Effects of beta blockade on sudden cardiac death during acute myocardial infarction and the postinfarction period. Am J Cardiol 1997;80:35J–9J. [DOI] [PubMed] [Google Scholar]
- 203. Hoang J, Salavatian S, Yamaguchi N, Swid MA, Vaseghi M. Cardiac sympathetic activation circumvents high dose beta-blocker therapy in part through release of neuropeptide-Y. JCI Insight 2020;5:e135519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Kalla M, Hao G, Tapoulal N, Tomek J, Liu K, Woodward L et al. The cardiac sympathetic co-transmitter neuropeptide Y is pro-arrhythmic following ST-elevation myocardial infarction despite beta-blockade. Eur Heart J 2019;40:1920–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. Fudim M, Boortz-Marx R, Ganesh A, Waldron NH, Qadri YJ, Patel CB et al. Stellate ganglion blockade for the treatment of refractory ventricular arrhythmias: a systematic review and meta-analysis. J Cardiovasc Electrophysiol 2017;28:1460–7. [DOI] [PubMed] [Google Scholar]
- 206. Meng L, Tseng CH, Shivkumar K, Ajijola O. Efficacy of stellate ganglion blockade in managing electrical storm: a systematic review. JACC Clin Electrophysiol 2017;3:942–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Cardona-Guarache R, Padala SK, Velazco-Davila L, Cassano A, Abbate A, Ellenbogen KA et al. Stellate ganglion blockade and bilateral cardiac sympathetic denervation in patients with life-threatening ventricular arrhythmias. J Cardiovasc Electrophysiol 2017;28:903–8. [DOI] [PubMed] [Google Scholar]
- 208. Fudim M, Qadri YJ, Waldron NH, Boortz-Marx RL, Ganesh A, Patel CB et al. Stellate ganglion blockade for the treatment of refractory ventricular arrhythmias. JACC Clin Electrophysiol 2020;6:562–71. [DOI] [PubMed] [Google Scholar]
- 209. Sanghai S, Abbott NJ, Dewland TA, Henrikson CA, Elman MR, Wollenberg M et al. Stellate ganglion blockade with continuous infusion versus single injection for treatment of ventricular arrhythmia storm. JACC Clin Electrophysiol 2021;7:452–60. [DOI] [PubMed] [Google Scholar]
- 210. Rao BH, Lokre A, Patnala N, Padmanabhan TNC. Stellate ganglion ablation by conventional radiofrequency in patients with electrical storm. Europace 2023;25:euad290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211. Chatzidou S, Kontogiannis C, Tampakis K, Episkopou E, Kanakakis I, Paraskevaidis I. Cryoablation of stellate ganglion for the management of electrical storm: the first reported case. Europace 2021;23:1105. [DOI] [PubMed] [Google Scholar]
- 212. Markman TM, Pothineni NVK, Zghaib T, Smietana J, McBride D, Amankwah NA et al. Effect of transcutaneous magnetic stimulation in patients with ventricular tachycardia storm: a randomized clinical trial. JAMA Cardiol 2022;7:445–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. Bourke T, Vaseghi M, Michowitz Y, Sankhla V, Shah M, Swapna N et al. Neuraxial modulation for refractory ventricular arrhythmias: value of thoracic epidural anesthesia and surgical left cardiac sympathetic denervation. Circulation 2010;121:2255–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214. Do DH, Bradfield J, Ajijola OA, Vaseghi M, Le J, Rahman S et al. Thoracic epidural anesthesia can be effective for the short-term management of ventricular tachycardia storm. J Am Heart Assoc 2017;6:e007080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215. Konig S, Schroter T, Borger MA, Bertagnolli L, Nedios S, Darma A et al. Outcomes following cardiac sympathetic denervation in patients with structural heart disease and refractory ventricular arrhythmia. Europace 2022;24:1800–8. [DOI] [PubMed] [Google Scholar]
- 216. Collura CA, Johnson JN, Moir C, Ackerman MJ. Left cardiac sympathetic denervation for the treatment of long QT syndrome and catecholaminergic polymorphic ventricular tachycardia using video-assisted thoracic surgery. Heart Rhythm 2009;6:752–9. [DOI] [PubMed] [Google Scholar]
- 217. De Ferrari GM, Dusi V, Spazzolini C, Bos JM, Abrams DJ, Berul CI et al. Clinical management of catecholaminergic polymorphic ventricular tachycardia: the role of left cardiac sympathetic denervation. Circulation 2015;131:2185–93. [DOI] [PubMed] [Google Scholar]
- 218. Schwartz PJ, Locati EH, Moss AJ, Crampton RS, Trazzi R, Ruberti U. Left cardiac sympathetic denervation in the therapy of congenital long QT syndrome. A worldwide report. Circulation 1991;84:503–11. [DOI] [PubMed] [Google Scholar]
- 219. Schwartz PJ, Priori SG, Cerrone M, Spazzolini C, Odero A, Napolitano C et al. Left cardiac sympathetic denervation in the management of high-risk patients affected by the long-QT syndrome. Circulation 2004;109:1826–33. [DOI] [PubMed] [Google Scholar]
- 220. Krych M, Janisz K, Kuriata J, Kusmierczyk M, Hoffman P, Biernacka EK. Successful cardiac sympathetic denervation for Andersen-Tawil syndrome. Europace 2023;25:1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221. Okada DR, Assis FR, Gilotra NA, Ha JS, Berger RD, Calkins H et al. Cardiac sympathectomy for refractory ventricular arrhythmias in cardiac sarcoidosis. Heart Rhythm 2019;16:1408–13. [DOI] [PubMed] [Google Scholar]
- 222. Saenz LC, Corrales FM, Bautista W, Traina M, Meymandi S, Rodriguez DA et al. Cardiac sympathetic denervation for intractable ventricular arrhythmias in Chagas disease. Heart Rhythm 2016;13:1388–94. [DOI] [PubMed] [Google Scholar]
- 223. Tellez LJ, Garzon JC, Vinck EE, Castellanos JD. Video-assisted thoracoscopic cardiac denervation of refractory ventricular arrhythmias and electrical storms: a single-center series. J Cardiothorac Surg 2019;14:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224. Vaseghi M, Barwad P, Malavassi Corrales FJ, Tandri H, Mathuria N, Shah R et al. Cardiac sympathetic denervation for refractory ventricular arrhythmias. J Am Coll Cardiol 2017;69:3070–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225. Vaseghi M, Gima J, Kanaan C, Ajijola OA, Marmureanu A, Mahajan A et al. Cardiac sympathetic denervation in patients with refractory ventricular arrhythmias or electrical storm: intermediate and long-term follow-up. Heart Rhythm 2014;11:360–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226. Dusi V, Gornbein J, Do DH, Sorg JM, Khakpour H, Krokhaleva Y et al. Arrhythmic risk profile and outcomes of patients undergoing cardiac sympathetic denervation for recurrent monomorphic ventricular tachycardia after ablation. J Am Heart Assoc 2020;10:e018371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227. Sridharan A, Tang A, Sorg JM, Hoftman NN, Lee JM, Yanagawa J et al. Effect of bilateral cardiac sympathetic denervation on burden of premature ventricular contractions. Circ Arrhythm Electrophysiol 2023;16:e011546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228. Bradfield JS, Vaseghi M, Shivkumar K. Renal denervation for refractory ventricular arrhythmias. Trends Cardiovasc Med 2014;24:206–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229. Hawson J, Harmer JA, Cowan M, Virk S, Campbell T, Bennett RG et al. Renal denervation for the management of refractory ventricular arrhythmias: a systematic review. JACC Clin Electrophysiol 2021;7:100–8. [DOI] [PubMed] [Google Scholar]
- 230. Armaganijan LV, Staico R, Moreira DA, Lopes RD, Medeiros PT, Habib R et al. 6-Month outcomes in patients with implantable cardioverter-defibrillators undergoing renal sympathetic denervation for the treatment of refractory ventricular arrhythmias. JACC Cardiovasc Interv 2015;8:984–90. [DOI] [PubMed] [Google Scholar]
- 231. Evranos B, Canpolat U, Kocyigit D, Coteli C, Yorgun H, Aytemir K. Role of adjuvant renal sympathetic denervation in the treatment of ventricular arrhythmias. Am J Cardiol 2016;118:1207–10. [DOI] [PubMed] [Google Scholar]
- 232. Ukena C, Mahfoud F, Ewen S, Bollmann A, Hindricks G, Hoffmann BA et al. Renal denervation for treatment of ventricular arrhythmias: data from an International Multicenter Registry. Clin Res Cardiol 2016;105:873–9. [DOI] [PubMed] [Google Scholar]
- 233. Tzafriri AR, Keating JH, Markham PM, Spognardi AM, Stanley JR, Wong G et al. Arterial microanatomy determines the success of energy-based renal denervation in controlling hypertension. Sci Transl Med 2015;7:285ra65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234. Kowey PR, Engel TR. Overdrive pacing for ventricular tachyarrhythmias: a reassessment. Ann Intern Med 1983;99:651–6. [DOI] [PubMed] [Google Scholar]
- 235. Llewellyn MJ, Ramsdale DR. Termination of refractory ventricular tachycardia by a combination of intravenous sotalol and overdrive ventricular pacing. Clin Cardiol 1987;10:416–8. [DOI] [PubMed] [Google Scholar]
- 236. Charos GS, Haffajee CI, Gold RL, Bishop RL, Berkovits BV, Alpert JS. A theoretically and practically more effective method for interruption of ventricular tachycardia: self-adapting autodecremental overdrive pacing. Circulation 1986;73:309–15. [DOI] [PubMed] [Google Scholar]
- 237. Cook JR, Kirchhoffer JB, Fitzgerald TF, Lajzer DA. Comparison of decremental and burst overdrive pacing as treatment for ventricular tachycardia associated with coronary artery disease. Am J Cardiol 1992;70:311–5. [DOI] [PubMed] [Google Scholar]
- 238. Chalupova M, Suter P, Graf D, Cook S. Temporary atrial overdrive pacing during a drug-refractory electrical storm in acute myocardial infarction. BMJ Case Rep 2021;14:242100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239. Magdi M, Mubasher M, Alzaeem H, Hamid T. Resistant ventricular arrhythmia and the role of overdrive pacing in the suppression of the electrical storm. Case Rep Cardiol 2019;2019:6592927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240. Neira V, Santangeli P, Futyma P, Sapp J, Valderrabano M, Garcia F et al. Ablation strategies for intramural ventricular arrhythmias. Heart Rhythm 2020;17:1176–84. [DOI] [PubMed] [Google Scholar]
- 241. Di Biase L, Romero J, Zado ES, Diaz JC, Gianni C, Hranitzki PM et al. Variant of ventricular outflow tract ventricular arrhythmias requiring ablation from multiple sites: intramural origin. Heart Rhythm 2019;16:724–32. [DOI] [PubMed] [Google Scholar]
- 242. Romero J, Shivkumar K, Valderrabano M, Diaz JC, Alviz I, Briceno D et al. Modern mapping and ablation techniques to treat ventricular arrhythmias from the left ventricular summit and interventricular septum. Heart Rhythm 2020;17:1609–20. [DOI] [PubMed] [Google Scholar]
- 243. Mierke J, Loehn T, Pfluecke C, Ibrahim K. Troubleshooter in electrical storm: mechanical unloading leads to heart rhythm stabilization. J Electrocardiol 2017;50:678–80. [DOI] [PubMed] [Google Scholar]
- 244. van der Ree MH, Dieleman EMT, Visser J, Planken RN, Boekholdt SM, de Bruin-Bon RHA et al. Non-invasive stereotactic arrhythmia radiotherapy for ventricular tachycardia: results of the prospective STARNL-1 trial. Europace 2023;25:1015–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245. Kany S, Alken FA, Schleberger R, Baran J, Luik A, Haas A et al. Bipolar ablation of therapy-refractory ventricular arrhythmias: application of a dedicated approach. Europace 2022;24:959–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246. Herrera Siklody C, Schiappacasse L, Jumeau R, Reichlin T, Saguner AM, Andratschke N et al. Recurrences of ventricular tachycardia after stereotactic arrhythmia radioablation arise outside the treated volume: analysis of the Swiss cohort. Europace 2023;25:euad268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247. Grehn M, Mandija S, Miszczyk M, Krug D, Tomasik B, Stickney KE et al. Stereotactic arrhythmia radioablation (STAR): the standardized treatment and outcome platform for stereotactic therapy of re-entrant tachycardia by a multidisciplinary consortium (STOPSTORM.eu) and review of current patterns of STAR practice in Europe. Europace 2023;25:1284–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248. Nishimura T, Goya M, Takigawa M, Negishi M, Ikenouchi T, Yamamoto T et al. Transcoronary mapping with an over-the-wire multielectrode catheter in scar-related ventricular tachycardia patients. Europace 2023;26:euad365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249. Streitner F, Kuschyk J, Veltmann C, Mahl E, Dietrich C, Schimpf R et al. Predictors of electrical storm recurrences in patients with implantable cardioverter-defibrillators. Europace 2011;13:668–74. [DOI] [PubMed] [Google Scholar]
- 250. Domanski MJ, Exner DV, Borkowf CB, Geller NL, Rosenberg Y, Pfeffer MA. Effect of angiotensin converting enzyme inhibition on sudden cardiac death in patients following acute myocardial infarction. A meta-analysis of randomized clinical trials. J Am Coll Cardiol 1999;33:598–604. [DOI] [PubMed] [Google Scholar]
- 251. Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized aldactone evaluation study investigators. N Engl J Med 1999;341:709–17. [DOI] [PubMed] [Google Scholar]
- 252. Desai AS, McMurray JJ, Packer M, Swedberg K, Rouleau JL, Chen F et al. Effect of the angiotensin-receptor-neprilysin inhibitor LCZ696 compared with enalapril on mode of death in heart failure patients. Eur Heart J 2015;36:1990–7. [DOI] [PubMed] [Google Scholar]
- 253. Vyas AK, Guo H, Moss AJ, Olshansky B, McNitt SA, Hall WJ et al. Reduction in ventricular tachyarrhythmias with statins in the multicenter automatic defibrillator implantation trial (MADIT)-II. J Am Coll Cardiol 2006;47:769–73. [DOI] [PubMed] [Google Scholar]
- 254. Chen H-Y, Huang J-Y, Siao W-Z, Jong G-P. The association between SGLT2 inhibitors and new-onset arrhythmias: a nationwide population-based longitudinal cohort study. Cardiovasc Diabetol 2020;19:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255. McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 2021;42:3599–726. [DOI] [PubMed] [Google Scholar]
- 256. Goldenberg I, Moss AJ, McNitt S, Zareba W, Hall WJ, Andrews ML et al. Time dependence of defibrillator benefit after coronary revascularization in the multicenter automatic defibrillator implantation trial (MADIT)-II. J Am Coll Cardiol 2006;47:1811–7. [DOI] [PubMed] [Google Scholar]
- 257. Chiuve SE, Rimm EB, Mukamal KJ, Rexrode KM, Stampfer MJ, Manson JE et al. Light-to-moderate alcohol consumption and risk of sudden cardiac death in women. Heart Rhythm 2010;7:1374–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258. Dyer AR, Stamler J, Paul O, Berkson DM, Lepper MH, McKean H et al. Alcohol consumption, cardiovascular risk factors, and mortality in two Chicago epidemiologic studies. Circulation 1977;56:1067–74. [DOI] [PubMed] [Google Scholar]
- 259. Wannamethee G, Shaper AG. Alcohol and sudden cardiac death. Br Heart J 1992;68:443–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260. Schwartz BG, Rezkalla S, Kloner RA. Cardiovascular effects of cocaine. Circulation 2010;122:2558–69. [DOI] [PubMed] [Google Scholar]
- 261. Schupp T, Behnes M, Weiss C, Nienaber C, Lang S, Reiser L et al. Beta-blockers and ACE inhibitors are associated with improved survival secondary to ventricular tachyarrhythmia. Cardiovasc Drugs Ther 2018;32:353–63. [DOI] [PubMed] [Google Scholar]
- 262. Kheiri B, Barbarawi M, Zayed Y, Hicks M, Osman M, Rashdan L et al. Antiarrhythmic drugs or catheter ablation in the management of ventricular tachyarrhythmias in patients with implantable cardioverter-defibrillators: a systematic review and meta-analysis of randomized controlled trials. Circ Arrhythm Electrophysiol 2019;12:e007600. [DOI] [PubMed] [Google Scholar]
- 263. Connolly SJ, Dorian P, Roberts RS, Gent M, Bailin S, Fain ES et al. Comparison of beta-blockers, amiodarone plus beta-blockers, or sotalol for prevention of shocks from implantable cardioverter defibrillators: the OPTIC study: a randomized trial. JAMA 2006;295:165–71. [DOI] [PubMed] [Google Scholar]
- 264. Sapp JL, Wells GA, Parkash R, Stevenson WG, Blier L, Sarrazin JF et al. Ventricular tachycardia ablation versus escalation of antiarrhythmic drugs. N Engl J Med 2016;375:111–21. [DOI] [PubMed] [Google Scholar]
- 265. Santangeli P, Muser D, Maeda S, Filtz A, Zado ES, Frankel DS et al. Comparative effectiveness of antiarrhythmic drugs and catheter ablation for the prevention of recurrent ventricular tachycardia in patients with implantable cardioverter-defibrillators: a systematic review and meta-analysis of randomized controlled trials. Heart Rhythm 2016;13:1552–9. [DOI] [PubMed] [Google Scholar]
- 266. Zeppenfeld K, Wijnmaalen AP, Ebert M, Baldinger SH, Berruezo A, Catto V et al. Clinical outcomes in patients with dilated cardiomyopathy and ventricular tachycardia. J Am Coll Cardiol 2022;80:1045–56. [DOI] [PubMed] [Google Scholar]
- 267. Batul SA, Gopinathannair R. Intravenous sotalol—reintroducing a forgotten agent to the electrophysiology therapeutic arsenal. J Atr Fibrillation 2017;9:1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268. Somberg JC, Preston RA, Ranade V, Molnar J. QT prolongation and serum sotalol concentration are highly correlated following intravenous and oral sotalol. Cardiology 2010;116:219–25. [DOI] [PubMed] [Google Scholar]
- 269. Pacifico A, Hohnloser SH, Williams JH, Tao B, Saksena S, Henry PD et al. Prevention of implantable-defibrillator shocks by treatment with sotalol. d, l-sotalol implantable cardioverter-defibrillator study group. N Engl J Med 1999;340:1855–62. [DOI] [PubMed] [Google Scholar]
- 270. Chamberlain DA, Jewitt DE, Julian DG, Campbell RW, Boyle DM, Shanks RG. Oral mexiletine in high-risk patients after myocardial infarction. Lancet 1980;2:1324–7. [DOI] [PubMed] [Google Scholar]
- 271. Gao D, Van Herendael H, Alshengeiti L, Dorian P, Mangat I, Korley V et al. Mexiletine as an adjunctive therapy to amiodarone reduces the frequency of ventricular tachyarrhythmia events in patients with an implantable defibrillator. J Cardiovasc Pharmacol 2013;62:199–204. [DOI] [PubMed] [Google Scholar]
- 272. Luderitz B, Mletzko R, Jung W, Manz M. Combination of antiarrhythmic drugs. J Cardiovasc Pharmacol 1991;17:S48–52. [PubMed] [Google Scholar]
- 273. Gottlieb SS, Weinberg M. Cardiodepressant effects of mexiletine in patients with severe left ventricular dysfunction. Eur Heart J 1992;13:22–7. [DOI] [PubMed] [Google Scholar]
- 274. Crystal E, Ovsyshcher IE, Wagshal AB, Katz A, Ilia R. Mexiletine related chronic defibrillation threshold elevation: case report and review of the literature. Pacing Clin Electrophysiol 2002;25:507–8. [DOI] [PubMed] [Google Scholar]
- 275. Mason JW. A comparison of seven antiarrhythmic drugs in patients with ventricular tachyarrhythmias. Electrophysiologic study versus electrocardiographic monitoring investigators. N Engl J Med 1993;329:452–8. [DOI] [PubMed] [Google Scholar]
- 276. Myerburg RJ, Kessler KM, Kiem I, Pefkaros KC, Conde CA, Cooper D et al. Relationship between plasma levels of procainamide, suppression of premature ventricular complexes and prevention of recurrent ventricular tachycardia. Circulation 1981;64:280–90. [DOI] [PubMed] [Google Scholar]
- 277. Toniolo M, Muser D, Grilli G, Burelli M, Rebellato L, Daleffe E et al. Oral procainamide as pharmacological treatment of recurrent and refractory ventricular tachyarrhythmias: a single-center experience. Heart Rhythm O2 2021;2:840–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278. Hoffmeister HM, Hepp A, Seipel L. Negative inotropic effect of class-I-antiarrhythmic drugs: comparison of flecainide with disopyramide and quinidine. Eur Heart J 1987;8:1126–32. [DOI] [PubMed] [Google Scholar]
- 279. Deshmukh A, Larson J, Ghannam M, Saeed M, Cunnane R, Ghanbari H et al. Efficacy and tolerability of quinidine as salvage therapy for monomorphic ventricular tachycardia in patients with structural heart disease. J Cardiovasc Electrophysiol 2021;32:3173–8. [DOI] [PubMed] [Google Scholar]
- 280. Li DL, Cox ZL, Richardson TD, Kanagasundram AN, Saavedra PJ, Shen ST et al. Quinidine in the management of recurrent ventricular arrhythmias: a reappraisal. JACC Clin Electrophysiol 2021;7:1254–63. [DOI] [PubMed] [Google Scholar]
- 281. Kuck KH, Cappato R, Siebels J, Ruppel R. Randomized comparison of antiarrhythmic drug therapy with implantable defibrillators in patients resuscitated from cardiac arrest: the cardiac arrest study Hamburg (CASH). Circulation 2000;102:748–54. [DOI] [PubMed] [Google Scholar]
- 282. Echt DS, Liebson PR, Mitchell LB, Peters RW, Obias-Manno D, Barker AH et al. Mortality and morbidity in patients receiving encainide, flecainide, or placebo. The cardiac arrhythmia suppression trial. N Engl J Med 1991;324:781–8. [DOI] [PubMed] [Google Scholar]
- 283. Ermakov S, Gerstenfeld EP, Svetlichnaya Y, Scheinman MM. Use of flecainide in combination antiarrhythmic therapy in patients with arrhythmogenic right ventricular cardiomyopathy. Heart Rhythm 2017;14:564–9. [DOI] [PubMed] [Google Scholar]
- 284. Rolland T, Badenco N, Maupain C, Duthoit G, Waintraub X, Laredo M et al. Safety and efficacy of flecainide associated with beta-blockers in arrhythmogenic right ventricular cardiomyopathy. Europace 2022;24:278–84. [DOI] [PubMed] [Google Scholar]
- 285. Chockalingam P, Crotti L, Girardengo G, Johnson JN, Harris KM, van der Heijden JF et al. Not all beta-blockers are equal in the management of long QT syndrome types 1 and 2: higher recurrence of events under metoprolol. J Am Coll Cardiol 2012;60:2092–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286. Han L, Liu F, Li Q, Qing T, Zhai Z, Xia Z et al. The efficacy of beta-blockers in patients with long QT syndrome 1-3 according to individuals’ gender, age, and QTc intervals: a network meta-analysis. Front Pharmacol 2020;11:579525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287. Yang Y, Lv TT, Li SY, Zhang P. Sodium channel blockers in the management of long QT syndrome types 3 and 2: a system review and meta-analysis. J Cardiovasc Electrophysiol 2021;32:3057–67. [DOI] [PubMed] [Google Scholar]
- 288. Moss AJ, Windle JR, Hall WJ, Zareba W, Robinson JL, McNitt S et al. Safety and efficacy of flecainide in subjects with long QT-3 syndrome (DeltaKPQ mutation): a randomized, double-blind, placebo-controlled clinical trial. Ann Noninvasive Electrocardiol 2005;10:59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289. Moss AJ, Zareba W, Schwarz KQ, Rosero S, McNitt S, Robinson JL. Ranolazine shortens repolarization in patients with sustained inward sodium current due to type-3 long-QT syndrome. J Cardiovasc Electrophysiol 2008;19:1289–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290. Belhassen B, Glick A, Viskin S. Efficacy of quinidine in high-risk patients with Brugada syndrome. Circulation 2004;110:1731–7. [DOI] [PubMed] [Google Scholar]
- 291. Andorin A, Gourraud JB, Mansourati J, Fouchard S, le Marec H, Maury P et al. The QUIDAM study: hydroquinidine therapy for the management of Brugada syndrome patients at high arrhythmic risk. Heart Rhythm 2017;14:1147–54. [DOI] [PubMed] [Google Scholar]
- 292. Leren IS, Saberniak J, Majid E, Haland TF, Edvardsen T, Haugaa KH. Nadolol decreases the incidence and severity of ventricular arrhythmias during exercise stress testing compared with beta1-selective beta-blockers in patients with catecholaminergic polymorphic ventricular tachycardia. Heart Rhythm 2016;13:433–40. [DOI] [PubMed] [Google Scholar]
- 293. van der Werf C, Kannankeril PJ, Sacher F, Krahn AD, Viskin S, Leenhardt A et al. Flecainide therapy reduces exercise-induced ventricular arrhythmias in patients with catecholaminergic polymorphic ventricular tachycardia. J Am Coll Cardiol 2011;57:2244–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294. Pott C, Dechering DG, Reinke F, Muszynski A, Zellerhoff S, Bittner A et al. Successful treatment of catecholaminergic polymorphic ventricular tachycardia with flecainide: a case report and review of the current literature. Europace 2011;13:897–901. [DOI] [PubMed] [Google Scholar]
- 295. El-Battrawy I, Besler J, Liebe V, Schimpf R, Tulumen E, Rudic B et al. Long-term follow-up of patients with short QT syndrome: clinical profile and outcome. J Am Heart Assoc 2018;7:e010073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296. Giustetto C, Schimpf R, Mazzanti A, Scrocco C, Maury P, Anttonen O et al. Long-term follow-up of patients with short QT syndrome. J Am Coll Cardiol 2011;58:587–95. [DOI] [PubMed] [Google Scholar]
- 297. Lima da Silva G, Nunes-Ferreira A, Cortez-Dias N, de Sousa J, Pinto F, Caldeira D. Radiofrequency catheter ablation of ventricular tachycardia in ischemic heart disease in light of current practice: a systematic review and meta-analysis of randomized controlled trials. J Interv Card Electrophysiol 2020;59:603–16. [DOI] [PubMed] [Google Scholar]
- 298. Willems S, Tilz RR, Steven D, Kaab S, Wegscheider K, Geller L et al. Preventive or deferred ablation of ventricular tachycardia in patients with ischemic cardiomyopathy and implantable defibrillator (BERLIN VT): a multicenter randomized trial. Circulation 2020;141:1057–67. [DOI] [PubMed] [Google Scholar]
- 299. Deyell MW, Steinberg C, Doucette S, Parkash R, Nault I, Gray C et al. Mexiletine or catheter ablation after amiodarone failure in the VANISH trial. J Cardiovasc Electrophysiol 2018;29:603–8. [DOI] [PubMed] [Google Scholar]
- 300. Deyell MW, Doucette S, Parkash R, Nault I, Gula L, Gray C et al. Ventricular tachycardia characteristics and outcomes with catheter ablation vs. antiarrhythmic therapy: insights from the VANISH trial. Europace 2022;24:1112–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301. Ávila P, Berruezo A, Jiménez-Candil J, Tercedor L, Calvo D, Arribas F et al. Bayesian analysis of the substrate ablation vs. antiarrhythmic drug therapy for symptomatic ventricular tachycardia trial. Europace 2023;25:euad181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302. Marchlinski FE, Haffajee CI, Beshai JF, Dickfeld TL, Gonzalez MD, Hsia HH et al. Long-term success of irrigated radiofrequency catheter ablation of sustained ventricular tachycardia: post-approval THERMOCOOL VT trial. J Am Coll Cardiol 2016;67:674–83. [DOI] [PubMed] [Google Scholar]
- 303. Tanner H, Hindricks G, Volkmer M, Furniss S, Kuhlkamp V, Lacroix D et al. Catheter ablation of recurrent scar-related ventricular tachycardia using electroanatomical mapping and irrigated ablation technology: results of the prospective multicenter Euro-VT-study. J Cardiovasc Electrophysiol 2010;21:47–53. [DOI] [PubMed] [Google Scholar]
- 304. Samuel M, Rivard L, Nault I, Gula L, Essebag V, Parkash R et al. Comparative effectiveness of ventricular tachycardia ablation vs. escalated antiarrhythmic drug therapy by location of myocardial infarction: a sub-study of the VANISH trial. Europace 2022;24:948–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305. Farkowski MM, Karlinski M, Pytkowski M, de Asmundis C, Lewandowski M, Mugnai G et al. Mexiletine for recurrent ventricular tachycardia in adult patients with structural heart disease and implantable cardioverter defibrillator: an EHRA systematic review. Europace 2022;24:1504–11. [DOI] [PubMed] [Google Scholar]
- 306. Huang K, Bennett RG, Campbell T, Lee V, Turnbull S, Chik WWB et al. Early catheter ablation versus initial medical therapy for ventricular tachycardia storm. Circ Arrhythm Electrophysiol 2022;15:e011129. [DOI] [PubMed] [Google Scholar]
- 307. Tung R, Vaseghi M, Frankel DS, Vergara P, Di Biase L, Nagashima K et al. Freedom from recurrent ventricular tachycardia after catheter ablation is associated with improved survival in patients with structural heart disease: an international VT ablation center collaborative group study. Heart Rhythm 2015;12:1997–2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308. Vergara P, Tzou WS, Tung R, Brombin C, Nonis A, Vaseghi M et al. Predictive score for identifying survival and recurrence risk profiles in patients undergoing ventricular tachycardia ablation: the I-VT score. Circ Arrhythm Electrophysiol 2018;11:e006730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309. Acosta J, Cabanelas N, Penela D, Fernandez-Armenta J, Andreu D, Borras R et al. Long-term benefit of first-line peri-implantable cardioverter-defibrillator implant ventricular tachycardia-substrate ablation in secondary prevention patients. Europace 2017;19:976–82. [DOI] [PubMed] [Google Scholar]
- 310. Bai R, Di Biase L, Shivkumar K, Mohanty P, Tung R, Santangeli P et al. Ablation of ventricular arrhythmias in arrhythmogenic right ventricular dysplasia/cardiomyopathy: arrhythmia-free survival after endo-epicardial substrate based mapping and ablation. Circ Arrhythm Electrophysiol 2011;4:478–85. [DOI] [PubMed] [Google Scholar]
- 311. Bogun FM, Desjardins B, Good E, Gupta S, Crawford T, Oral H et al. Delayed-enhanced magnetic resonance imaging in nonischemic cardiomyopathy: utility for identifying the ventricular arrhythmia substrate. J Am Coll Cardiol 2009;53:1138–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312. Vaseghi M, Hu TY, Tung R, Vergara P, Frankel DS, Di Biase L et al. Outcomes of catheter ablation of ventricular tachycardia based on etiology in nonischemic heart disease: an international ventricular tachycardia ablation center collaborative study. JACC Clin Electrophysiol 2018;4:1141–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313. Briceno DF, Gupta T, Romero J, Kolte D, Khera S, Villablanca PA et al. Catheter ablation of ventricular tachycardia in nonischemic cardiomyopathy: a propensity score-matched analysis of in-hospital outcomes in the United States. J Cardiovasc Electrophysiol 2018;29:771–9. [DOI] [PubMed] [Google Scholar]
- 314. Towbin JA, McKenna WJ, Abrams DJ, Ackerman MJ, Calkins H, Darrieux FCC et al. 2019 HRS expert consensus statement on evaluation, risk stratification, and management of arrhythmogenic cardiomyopathy: executive summary. Heart Rhythm 2019;16:e373–407. [DOI] [PubMed] [Google Scholar]
- 315. Henz BD, do Nascimento TA, Dietrich Cde O, Dalegrave C, Hernandes V, Mesas CE et al. Simultaneous epicardial and endocardial substrate mapping and radiofrequency catheter ablation as first-line treatment for ventricular tachycardia and frequent ICD shocks in chronic chagasic cardiomyopathy. J Interv Card Electrophysiol 2009;26:195–205. [DOI] [PubMed] [Google Scholar]
- 316. Pisani CF, Romero J, Lara S, Hardy C, Chokr M, Sacilotto L et al. Efficacy and safety of combined endocardial/epicardial catheter ablation for ventricular tachycardia in Chagas disease: a randomized controlled study. Heart Rhythm 2020;17:1510–8. [DOI] [PubMed] [Google Scholar]
- 317. Nademanee K, Chung FP, Sacher F, Nogami A, Nakagawa H, Jiang C et al. Long-term outcomes of Brugada substrate ablation: a report from BRAVO (Brugada ablation of VF substrate ongoing multicenter registry). Circulation 2023;147:1568–78. [DOI] [PubMed] [Google Scholar]
- 318. Nademanee K, Veerakul G, Chandanamattha P, Chaothawee L, Ariyachaipanich A, Jirasirirojanakorn K et al. Prevention of ventricular fibrillation episodes in Brugada syndrome by catheter ablation over the anterior right ventricular outflow tract epicardium. Circulation 2011;123:1270–9. [DOI] [PubMed] [Google Scholar]
- 319. Pappone C, Ciconte G, Manguso F, Vicedomini G, Mecarocci V, Conti M et al. Assessing the malignant ventricular arrhythmic substrate in patients with Brugada syndrome. J Am Coll Cardiol 2018;71:1631–46. [DOI] [PubMed] [Google Scholar]
- 320. Pappone C, Brugada J, Vicedomini G, Ciconte G, Manguso F, Saviano M et al. Electrical substrate elimination in 135 consecutive patients with Brugada syndrome. Circ Arrhythm Electrophysiol 2017;10:e005053. [DOI] [PubMed] [Google Scholar]
- 321. Wilde AA, Nademanee K. Epicardial substrate ablation in Brugada syndrome: time for a randomized trial!. Circ Arrhythm Electrophysiol 2015;8:1306–8. [DOI] [PubMed] [Google Scholar]
- 322. Haïssaguerre M, Extramiana F, Hocini M, Cauchemez B, Jaïs P, Cabrera JA et al. Mapping and ablation of ventricular fibrillation associated with long-QT and Brugada syndromes. Circulation 2003;108:925–8. [DOI] [PubMed] [Google Scholar]
- 323. Pappone C, Ciconte G, Anastasia L, Gaita F, Grant E, Micaglio E et al. Right ventricular epicardial arrhythmogenic substrate in long-QT syndrome patients at risk of sudden death. Europace 2023;25:948–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324. Blackwell DJ, Faggioni M, Wleklinski MJ, Gomez-Hurtado N, Venkataraman R, Gibbs CE et al. The Purkinje-myocardial junction is the anatomic origin of ventricular arrhythmia in CPVT. JCI Insight 2022;7:e151893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325. Nademanee K, Haissaguerre M, Hocini M, Nogami A, Cheniti G, Duchateau J et al. Mapping and ablation of ventricular fibrillation associated with early repolarization syndrome. Circulation 2019;140:1477–90. [DOI] [PubMed] [Google Scholar]
- 326. van Weperen VYH, Vos MA, Ajijola OA. Autonomic modulation of ventricular electrical activity: recent developments and clinical implications. Clin Auton Res 2021;31:659–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327. Savastano S, Dusi V, Baldi E, Rordorf R, Sanzo A, Camporotondo R et al. Anatomical-based percutaneous left stellate ganglion block in patients with drug-refractory electrical storm and structural heart disease: a single-centre case series. Europace 2021;23:581–6. [DOI] [PubMed] [Google Scholar]
- 328. Boutitie F, Boissel JP, Connolly SJ, Camm AJ, Cairns JA, Julian DG et al. Amiodarone interaction with beta-blockers: analysis of the merged EMIAT (European myocardial infarct amiodarone trial) and CAMIAT (Canadian amiodarone myocardial infarction trial) databases. The EMIAT and CAMIAT investigators. Circulation 1999;99:2268–75. [DOI] [PubMed] [Google Scholar]
- 329. Mazzanti A, Tenuta E, Marino M, Pagan E, Morini M, Memmi M et al. Efficacy and limitations of quinidine in patients with Brugada syndrome. Circ.: Arrhythmia Electrophysiol. 2019;12:1–8. [Google Scholar]
- 330. Sears SF Jr, Conti JB. Quality of life and psychological functioning of ICD patients. Heart 2002;87:488–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331. Pedersen SS, Wehberg S, Nielsen JC, Riahi S, Larroude C, Philbert BT et al. Patients with an implantable cardioverter defibrillator at risk of poorer psychological health during 24 months of follow-up (results from the Danish national DEFIB-WOMEN study). Gen Hosp Psychiatry 2023;80:54–61. [DOI] [PubMed] [Google Scholar]
- 332. Gathright EC, Goldstein CM, Josephson RA, Hughes JW. Depression increases the risk of mortality in patients with heart failure: a meta-analysis. J Psychosom Res 2017;94:82–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333. Habibovic M, Pedersen SS, van den Broek KC, Theuns DA, Jordaens L, van der Voort PH et al. Anxiety and risk of ventricular arrhythmias or mortality in patients with an implantable cardioverter defibrillator. Psychosom Med 2013;75:36–41. [DOI] [PubMed] [Google Scholar]
- 334. Baldi E, Conte G, Zeppenfeld K, Lenarczyk R, Guerra JM, Farkowski MM et al. Contemporary management of ventricular electrical storm in Europe: results of a European Heart Rhythm Association survey. Europace 2023;25:1277–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335. Kohn CS, Petrucci RJ, Baessler C, Soto DM, Movsowitz C. The effect of psychological intervention on patients’ long-term adjustment to the ICD: a prospective study. Pacing Clin Electrophysiol 2000;23:450–6. [DOI] [PubMed] [Google Scholar]
- 336. Miller LW PF, Russell SD, John R, Boyle AJ, Aaronson KD, Conte JV et al. Use of a continuous-flow device in patients awaiting heart transplantation. N Engl J Med 2017;357:885–96. [DOI] [PubMed] [Google Scholar]
- 337. Cantillon DJ, Tarakji KG, Kumbhani DJ, Smedira NG, Starling RC, Wilkoff BL. Improved survival among ventricular assist device recipients with a concomitant implantable cardioverter-defibrillator. Heart Rhythm 2010;7:466–71. [DOI] [PubMed] [Google Scholar]
- 338. Martins RP, Leclercq C, Bourenane H, Auffret V, Boule S, Loobuyck V et al. Incidence, predictors, and clinical impact of electrical storm in patients with left ventricular assist devices: new insights from the ASSIST-ICD study. Heart Rhythm 2019;16:1506–12. [DOI] [PubMed] [Google Scholar]
- 339. Greet BD, Pujara D, Burkland D, Pollet M, Sudhakar D, Rojas F et al. Incidence, predictors, and significance of ventricular arrhythmias in patients with continuous-flow left ventricular assist devices: a 15-year institutional experience. JACC Clin Electrophysiol 2018;4:257–64. [DOI] [PubMed] [Google Scholar]
- 340. Galand V, Flecher E, Auffret V, Pichard C, Boule S, Vincentelli A et al. Early ventricular arrhythmias after LVAD implantation is the strongest predictor of 30-day post-operative mortality. JACC Clin Electrophysiol 2019;5:944–54. [DOI] [PubMed] [Google Scholar]
- 341. Sacher F, Reichlin T, Zado ES, Field ME, Viles-Gonzalez JF, Peichl P et al. Characteristics of ventricular tachycardia ablation in patients with continuous flow left ventricular assist devices. Circ Arrhythm Electrophysiol 2015;8:592–7. [DOI] [PubMed] [Google Scholar]
- 342. Moss JD, Flatley EE, Beaser AD, Shin JH, Nayak HM, Upadhyay GA et al. Characterization of ventricular tachycardia after left ventricular assist device implantation as destination therapy: a single-center ablation experience. JACC Clin Electrophysiol 2017;3:1412–24. [DOI] [PubMed] [Google Scholar]
- 343. Nof E, Peichl P, Stojadinovic P, Arceluz M, Maury P, Katz M et al. HeartMate 3: new challenges in ventricular tachycardia ablation. Europace 2022;24:598–605. [DOI] [PubMed] [Google Scholar]
- 344. Saxon LA, Bristow MR, Boehmer J, Krueger S, Kass DA, De Marco T et al. Predictors of sudden cardiac death and appropriate shock in the comparison of medical therapy, pacing, and defibrillation in heart failure (COMPANION) trial. Circulation 2006;114:2766–72. [DOI] [PubMed] [Google Scholar]
- 345. Tzou WS, Tung R, Frankel DS, Vaseghi M, Bunch TJ, Di Biase L et al. Ventricular tachycardia ablation in severe heart failure: an international ventricular tachycardia ablation center collaboration analysis. Circ Arrhythm Electrophysiol 2017;10:e004494. [DOI] [PubMed] [Google Scholar]