Abstract
Background:
An anterior cruciate ligament (ACL) tear is a risk factor for early osteoarthritis (OA) onset. Generally, ACL reconstruction (ACLR) is associated with better outcomes. However, there is a lack of evidence regarding the effect of operative versus nonoperative treatment for preventing premature knee OA in isolated ACL tears while achieving good functional outcomes.
Purpose/Hypothesis:
The purpose of the study was to compare the outcomes of ACLR to primarily nonoperative management of isolated ACL tears. It was hypothesized that the outcomes between treatment types would be similar.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
This systematic review was registered on the International Prospective Register of Systematic Reviews (PROSPERO) (registration No. CRD42021285901) and was conducted according to the Cochrane Handbook guidelines. We systematically searched for randomized and nonrandomized studies that compared ACLR with nonoperative treatments in isolated ACL tears in 3 databases until October 25, 2021. The risk of bias and quality of evidence of the included studies was assessed in accordance with the Cochrane guidelines. The primary outcome was radiologic signs of OA, and the secondary outcomes were functional parameters. Using the common effects model, we calculated pooled mean differences (MDs) and odds ratios (ORs) with 95% CIs.
Results:
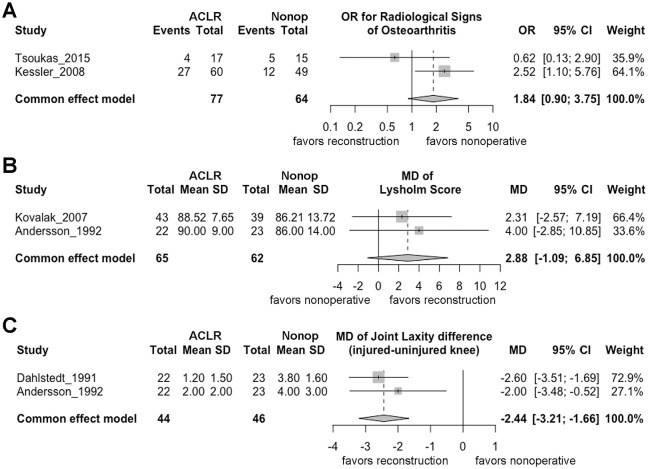
Five studies—2 randomized controlled trials (RCTs) and 3 retrospective non-RCTs—were included. There was a moderate risk of bias in 2 studies and a serious risk of bias in 1 study. The quality of evidence was rated low because of the higher risk of bias and inconsistency. Nonoperatively treated knees showed a trend toward lower odds of developing radiological signs of OA (OR, 1.84 [95% CI, 0.90 to 3.75]); however, surgically reconstructed knees had significantly better stability (MD, –2.44 [95% CI, –3.21 to −1.66 ]) and a trend toward better but clinically not meaningful Lysholm scores (MD, 2.88 [95% CI, –1.09 to 6.85]). The qualitative synthesis showed that surgical reconstruction was protective against subsequent injuries but not superior when returning to previous activity levels or various functional tests.
Conclusion:
Findings indicated that there is no certain evidence that ACLR for an isolated ACL tear is superior to nonoperative treatment. Clinicians should consider nonoperative treatments with a well-designed rehabilitative program as a primary option. However, these findings must be interpreted with caution because of low study quality and high risk of bias.
Keywords: anterior cruciate ligament, cartilage, conservative, knee, nonoperative, reconstruction, surgery
Isolated tear of the anterior cruciate ligament (ACL) is among the most common knee injuries, with an incidence of 68.6 in 100,000 per person-year in the United States. 31 The ACL is one of the most important ligaments for adequate knee kinematics, and its deficiency leads to instability, which is a risk factor for the early onset of osteoarthritis (OA). 12 After an ACL rupture, cartilage degeneration incidence ranges 22 from 16% to 70%.
Surgical reconstruction is the gold standard treatment for younger and more active patients, while nonoperative treatment is mainly reserved for older and less active patients. 19 From >200,000 ACL ruptures per year, around 130,000 are reconstructed in the United States. 23 Although ACL reconstruction (ACLR) often provides adequate knee stability, the long-term effect on the articular cartilage still needs to be clarified. 20 However, with rigorous rehabilitation, dynamic stability through muscle function can be effectively regained, reducing the risk of complications. 35 A previous literature review—without mathematical analysis—reported that ACLR did not reduce the incidence of further osteoarthritic development and concluded that the risk of knee degeneration remains high regardless of treatment. 9 In 2022, Cuzzolin et al 7 reported a systematic review and meta-analysis, and Saueressig et al 32 published a “living” systematic review and meta-analysis (to be updated yearly as the evidence develops), addressing the same question. However, these studies did not focus on isolated ruptures of the ACL, and only a small number of randomized controlled trials (RCTs) were included. Although ACL injuries have been well studied, we still do not understand which option is better for preventing knee OA 10 while achieving good functional outcomes.
Given this uncertainty, we sought the best practice to prevent early-onset OA after an isolated ACL tear. Therefore, this systematic review and meta-analysis aimed to compare the radiological and functional outcomes of primarily ACLR versus primarily nonoperative management of isolated ACL tears. We hypothesized that nonoperative management of isolated ACL tears would result in similar outcomes with ACLR.
Methods
We reported our systematic review and meta-analysis based on the recommendation of the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 guidelines 25 ; we also followed the Cochrane Handbook guidelines. 15 The study protocol was registered on the International Prospective Register of Systematic Reviews (PROSPERO) (registration No. CRD42021285901).
Eligibility Criteria
The eligibility of the articles was determined using the PICO (Population, Intervention, Comparison, and Outcome) framework. Full-text studies that assessed the clinical and radiological results (Outcome) of isolated ACL-injured patients (Population) treated with reconstruction (Intervention) versus nonsurgical treatment (Comparison) were included. All forms of rehabilitation exercises and protocols were included as nonsurgical treatments. The following outcomes were investigated in the meta-analysis: radiologic assessment of OA by the Kellgren-Lawrence and International Knee Documentation Committee (IKDC) classification systems, joint laxity according to arthrometry, and patient-reported (subjective) knee function according to the Lysholm knee scoring scale. We included both randomized and nonrandomized comparative studies (prospective and retrospective observational studies) because of the small number of RCTs.
Search Strategy
We conducted our systematic search on October 27, 2021, using the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE (via PubMed), and Embase. During the systematic search, the following search keys were used in all databases: (“ACL” OR “anterior cruciate ligament”) AND (surgery OR replacement OR reconstruction) AND (conservative OR rehabilitation OR exercise). No filters (eg, language, full-text, or date) were applied during the search. The reference lists of included studies and previous systematic reviews were also screened for additional articles. Gray literature—non-peer reviewed material—was excluded.
Selection Process
The records of the systematic search were extracted from the databases and combined into a reference manager software (EndNote X9; Clarivate Analytics). After the automatic and manual removal of duplicate records, studies were selected by 2 authors independently (R.D.J. and M.M.). First, the titles and abstracts were screened to remove ineligible articles. Available full texts of the remaining studies were evaluated to decide whether they were eligible for inclusion. Disagreements were resolved by consensus with the supervision of a third author (G.P.). The Cohen kappa coefficient (κ) was calculated to measure the interrater reliability of the 2 reviewers during the study selection process—that is, the proportion of identical articles selected by the reviewers.
Data Collection and Data Items
The raw data were extracted from the included publications by 2 authors (R.D.J. and M.M.) independently into a standardized data collection form created in Microsoft Excel 365 (Microsoft Corp). The following data were extracted from each eligible study: authors, publication year, digital object identifier, study design, study period, study site, patient characteristics (sex, age), inclusion and exclusion criteria, subgroups, definitions of interventions and comparators, follow-up periods, and outcomes. A third party (G.P.) resolved discrepancies.
Risk of Bias Assessment
Two authors (R.D.J. and M.M.) performed the risk of bias assessment independently using the revised Cochrane Risk of Bias 2 (RoB 2) 37 tool for the included RCTs and the Cochrane Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) 36 for the eligible nonrandomized studies. Disagreements were resolved by consensus with the supervision of a third author (G.P.).
Quality of Evidence
Two authors (R.D.J. and M.M.) independently evaluated the quality of the evidence of the included studies using the Grades of Recommendation, Assessment, Development, and Evaluation (GRADE)13,33 workgroup recommendations. The GRADE assigns 4 levels of quality: very low (the true effect is probably markedly different from the estimated effect), low (the true effect might be markedly different from the estimated effect), medium (the true effect is probably close to the estimated effect), and high (there is a high degree of confidence that the true effect is similar to the estimated effect). Evidence from RCTs starts at high quality, and evidence from observational data starts at low quality. Disagreements were resolved by consensus with the supervision of a third author (G.P.).
Statistical Methods
The statistical analysis was performed in R Version 4.1.3 (R Core Team), using the {metra} package Version 5.2.0. The goal of pooling was primarily representation because of the small number of studies.
In the case of categorical outcomes (eg, radiological signs of OA), the affected and total counts were extracted for both the intervention group (ACLR) and the reference group (nonoperative treatments). In the case of continuous outcomes (eg, the Lysholm score at the endpoint, the side-to-side difference in anterior knee laxity), we extracted the counts and means with standard deviations for the respective groups. For categorical data, odds ratios (OR) were calculated and pooled using a fixed-effects model applying the Mantel-Haenszel method. Continuity correction was not necessary as there were no zero observations. Mean differences (MDs) were calculated and pooled using a fixed-effects model for continuous data.
We used forest plots to represent study levels and pooled estimates. The confidence level (1-α) was 95% in all cases. Because very few studies were pooled, the statistical assessment of heterogeneity and publication bias was not conducted. Outcomes that we could not include in our meta-analysis were included in the narrative review.
Results
Search and Selection
Overall, 13,089 potential publications were revealed through the initial electronic database search. After we had completed our study selection algorithm, 5 studies2,8,17,18,38 were determined as eligible for our systematic review and meta-analysis (Figure 1). 27 Regarding interrater reliability of the selected articles, there was almost perfect agreement between the 2 reviewers during the screening and final inclusion processes (Figure 1).
Figure 1.
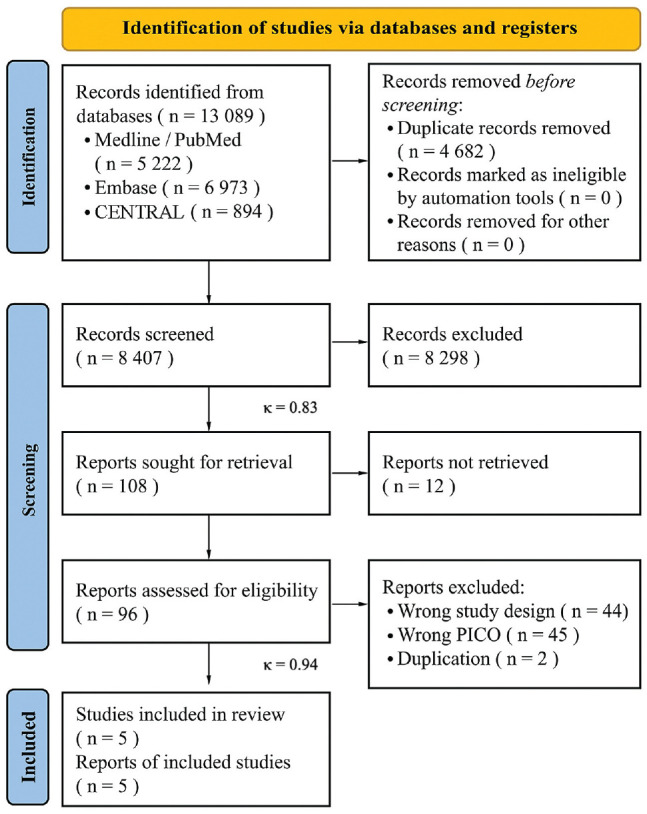
A PRISMA flow diagram of the study inclusion process. 27 CENTRAL, Cochrane Central Register of Controlled Trials; κ, Cohen kappa coefficient; PICO, Population, Intervention, Comparison, and Outcome framework; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Basic Characteristics of Included Studies
The systematic search yielded 3 retrospective nonrandomized studies8,17,18 and 2 RCTs.2,38 The articles were published in 4 countries (Sweden,2,8 Germany, 17 Turkey, 18 and Greece 38 ) between 1991 and 2017. These articles reported the outcomes on 324 patients, with mean follow-up periods between 3.4 and 11.1 years. The characteristics of the included publications are summarized in Table 1, with further information in Supplemental Tables S1 and S2 (available separately).
Table 1.
Characteristics of the Included Studies a
| Lead Author (Year) | Study Design | Study Period | Intervention | Age, Years b | Female Sex, % | No. of Patients | Follow-up b | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Andersson (1992) 2 | RCT | 1980-1985 | ACL tear was sutured and augmented (with a strip of the iliotibial band.) | NA | NA | 55 | 52 (35-74) mo | Knee laxity, knee performance test, Tegner, Lysholm |
| Dahlstedt (1991) 8 | Retrospective cohort | 1982-1989 | ACL tear was sutured and augmented (with a strip of patellar tendon) | ACLR: 22 (14-40) Nonop: 23 (14-39) |
NA | ACLR: 22 Nonop: 23 |
ACLR: 45 (24-53) mo
c
Nonop: 46 (24-78) mo c |
Lysholm, Tegner, modified knee score of Marshall et al, 24 pivot-shift test; knee laxity |
| Kessler (2008) 17 | Retrospective cohort | Jan 1989- Sept 1997 | BPTB graft | 30.7 (12.5-54) | 41 | 109 | 11.1 (7.5-16.3) y | IKDC examination grade; Kellgren-Lawrence score; Tegner score |
| Kovalak (2017) 18 | Retrospective comparative study with match-paired groups | NA | 4-stranded ST-G tendon autograft | ACLR: 32.56 ± 4.89 Nonop: 31.67 ± 7.27 |
0 | 82 | ACLR: 8.25 ± 1.82 y Nonop: 8.10 ± 2.43 y |
Lysholm; single-leg hop test; joint position sense; muscle strength; SF-36 |
| Tsoukas (2015) 38 | RCT | NA | 4-stranded ST-G tendon autograft | ACLR: 31 (20-36) Nonop: 33 (25-39) |
0 | 33 | Median, 10.1 (10-11) y b | IKDC evaluation score; knee laxity; IKDC examination grade; Tegner |
ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstructed population; BPTB, bone–patellar tendon–bone; IKDC, International Knee Documentation Committee; NA, not available; Nonop, nonoperatively treated population; RCT, randomized controlled trial; SF-36, 36-Item Short Form Survey; ST-G, semitendinosus-gracilis.
Data are reported as mean ± SD or mean (range) unless otherwise indicated.
Median (range).
The type and technique of ACLR were different among the studies. In 2 studies, the ACL remnant was sutured: Andersson and Gillquist 2 augmented it with a strip of the iliotibial band, whereas Dahlstedt et al 8 augmented it with a patellar tendon strip. Kessler et al 17 used a bone–patellar tendon–bone (BPTB) graft with extra-articular screw fixation of the tibia and femur. Kovalak et al 18 and Tsoukas et al 38 used gracilis and semitendinosus tendon autografts fixed by an EndoButton loop at the femoral side and a bioabsorbable screw at the tibial side. Nonoperative treatments were also different among studies. Information about these rehabilitation protocols is summarized in Supplementary Table S1.
Kessler et al 17 reported their radiological findings according to the Kellgren-Lawrence grading, and Tsoukas et al 38 used the IKDC grading. Although these are different scales, both are categorized by the radiological signs of OA, and there is a clear cutoff for normal knees and knees with OA. Therefore, we were able to compare these outcomes.
Regarding joint laxity, Andersson and Gillquist 2 used the Stryker knee arthrometer, and Dahlstedt et al 8 used the KT-1000 arthrometer. Despite the different types of equipment, both used the same force (90 and 89 N) to measure joint laxity; thus, we could compare their results.
Risk of Bias Assessment and Quality of Evidence
During the risk of bias assessment with the ROBINS-I tool for nonrandomized trials, we found a moderate risk of bias in 2 articles (Kessler et al 17 and Kovalak et al 18 ) and a serious risk of bias in 1 article (Dahlstedt et al 8 ). The main concerns were bias due to confounding, bias due to the selection of participants, bias in the classification of interventions, and bias due to deviations from intended interventions. Further details can be found in Supplemental Figures S1 to S11. With the RoB 2.0 tool for the RCTs, we found a high risk of bias for the study by Andersson and Gillquist 2 and a moderate risk of bias (labeled “some concerns”) for the study by Tsoukas et al. 38 The main concern was bias due to missing data regarding outcomes. Further details can be found in Supplemental Figures S12 to S19.
The quality of evidence for radiological signs of OA, knee laxity, and the Lysholm score was considered low according to the GRADE assessment, with the main concerns being higher risk of bias and inconsistency (Supplementary Table S3).
Radiological Signs of OA
In the study 38 by Tsoukas et al, 4 of 17 knee joints with radiological signs of OA were found in the ACLR group, and 5 of 15 were found in the nonoperative group. In the study 17 by Kessler et al, 27 of 60 knees with OA were found in the ACLR group compared with 12 of 60 knees in the nonoperative group. The pooled OR of these studies was 1.84 (95% CI, 0.90-3.75); thus, overall, there was no significant difference (Figure 2A), but the results were inconsistent.
Figure 2.
Forest plots of results from meta-analyses for (A) radiological signs of OA, (B) the Lysholm knee score, and (C) the side-to-side difference in joint laxity. ACLR, anterior cruciate ligament reconstruction; MD, mean difference; Nonop, nonoperative; OA, osteoarthritis; OR, odds ratio.
Lysholm Score
In both studies that reported this outcome (Kovalak et al 18 and Andersson and Gillquist 2 ), the mean Lysholm scores were better in the ACLR group. The pooled MD was 2.88 (95% CI, –1.09 to 6.85), indicating no significant group differences in the pre- to postoperative improvement (Figure 2B).
Knee Laxity
In the 2 studies2,8 that reported this outcome, the ACLR knees had lower laxity than the nonoperatively treated knees. Dahlstedt et al 8 reported an MD of −2.60 between the 2 groups (95% CI, –3.51 to −1.69), and in the Andersson and Gillquist 2 study, the MD between the 2 groups was −2 (95% CI, –3.48 to −0.52). The pooled MD was −2.44 (95% CI, –3.21 to −1.66), indicating significantly better stability for the patients who had ACLR (Figure 2C).
Qualitative Synthesis
We were only able to analyze the outcomes for radiological signs of OA, the Lysholm score, and knee laxity statistically because there was no common reporting of the same outcome or because of a lack of baseline and/or follow-up data regarding the rest of the outcomes. However, we included the results of all provided outcomes in a summary table (Table 2). This table shows that the individual studies found no significant differences between the 2 groups in most outcomes. Table 3 summarizes subsequent injuries and surgical interventions that occurred during the follow-ups. Further details can be found in the Supplemental Material.
Table 2.
Summary of Provided Outcomes a
| Study | Radiological Signs of OA c | Laxity c | Lysholm Score c | IKDC Examination Grade | IKDC Evaluation Score | Tegner Score | Single-Leg Hop Test | Joint Position Sense | Proprioception | SF-36 Health Profile | Muscle Strength |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Andersson and Gillquist 2 (1992) | — | Sig better for ACLR b | Favors ACLR b | — | — | Favors ACLR | No sig diff | — | — | — | No sig diff |
| Dahlstedt et al 8 (1991) | — | Sig better for ACLR b | — | — | — | Not comparable | — | — | — | — | — |
| Kessler et al 17 (2008) | Favors Nonop b | Favors ACLR | — | Favors ACLR | — | No sig diff | — | — | — | — | — |
| Kovalak et al 18 (2017) | — | — | Favors ACLR b | — | — | Not comparable | No sig diff | No sig diff | No sig diff | No sig diff | No sig diff |
| Tsoukas et al 38 (2015) | Favors ACLR b | Favors ACLR | — | — | Sig better for ACLR | Favors ACLR | — | — | — | — | — |
| Analysis results | No sig diff, favors Nonop | Sig better for ACLR | No sig diff, favors ACLR, clinically not meaningful | Favors ACLR | Favors ACLR | No clear result | No sig diff | No sig diff | No sig diff | No sig diff | No sig diff |
Dashes indicate that the outcome was not included in that study. ACLR, anterior cruciate ligament reconstruction; diff, difference; IKDC, International Knee Documentation Committee; Nonop, nonoperative treatment; OA, osteoarthrosis; SF-36, 36-Item Short Form Survey; sig, significant.
Outcomes could be analyzed mathematically.
Outcomes were included in the meta-analysis.
Table 3.
Subsequent Injuries and Surgical Interventions a
| Study | Need for ACLR (Nonop Group) | Need for Revision ACLR | Bilateral ACL Tears at Follow-up | Need for Meniscal Surgery | Knee Instability |
|---|---|---|---|---|---|
| Andersson and Gillquist 2 (1992) | 6 | — | ACLR: 1 Nonop: 1 |
— | 6 |
| Kessler et al 17 (2008) | 19 (28); 18 meniscal lesions with 12 concomitant instabilities | 8 (12); 6 for instabilities with ACL rerupture and/or 7 meniscal lesions | — | ACLR: 7 (10) Nonop: 18 (26) |
ACLR: 6 (9) Nonop: 12 (18) |
Dashes indicate intervention was not needed. Data are reported as n (%) unless otherwise indicated. Dahlstedt et al 8 did not report the rate of complications in their study. Regarding the study of Kovalak et al, 18 no patients needed surgical intervention during the follow-up period (ie, there was no cross-over or reinjury). Regarding the study of Tsoukas et al, 38 no complications occurred and no revision surgeries were performed. No patients required any further meniscus surgery or surgery due to persistent instability. ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; Nonop, nonoperative.
Discussion
Our results did not find enough proof that ACLR is superior to nonoperative treatment for isolated ACL-injured patients in the general population aged between 20 and 50 years. Therefore, we can confirm the statement by Kessler et al 17 that the concept of ACLR to prevent premature OA and maintain activity and function cannot be accepted unquestionably, especially regarding an isolated injury, where various factors should be considered when deciding whether to perform a surgical intervention or proceed with nonoperative treatment. However, in most cases, when simultaneous injuries to the menisci or collateral ligaments occur, reconstruction is regularly indicated to prevent further damage to these structures.
We found that the odds of having knee OA were 50% lower with nonoperative treatment on radiological findings compared with ACLR. Although this is a strong effect, the difference was not significant. However, there is heterogeneity between the analyzed studies. Both studies used different types of grafts and reported the grade of OA on different scales. While the study by Kessler et al 17 was larger and favored nonoperative care, this study was considerably lower in quality than the study by Tsoukas et al. 38
Only a few systematic literature reviews are available on isolated ACL injury with which to compare our results. Sailhan and Ribinik 30 concluded that the development of osteoarthritic changes did not alter between the 2 groups after an isolated ACL injury and did not relate to the reconstruction technique either. The pivot-shift test was the only clinical sign corresponding with the degenerative osteoarthritic changes, supporting the link between residual instability and degenerative changes. Other reviews assessing the results of nonisolated ACL injuries observed no significant difference in the radiographic progression of OA between ACLR and nonoperative treatments.5,11 The meta-analysis by Smith et al 35 showed no statistically significant difference between the treatment groups for the development of OA after 5 to 10 years of ACL injury. However, there was a small statistically significant difference after >10 years of injury, where the ACLR group showed a greater chance of developing osteoarthritic changes. Pernin et al 28 reported that after ACLR (at a mean time of 24.5 years), 31% of patients who had undergone total medial meniscectomy versus 61% of patients with a healthy medial meniscus had satisfying IKDC grade A or B radiographs. In contrast, Järvelä et al 16 found no differences between patients with an ACL injury, isolated, or concomitant injuries 5 to 9 years after ACLR, while tibiofemoral OA was rare. Although the study by Nordenvall et al 26 was observational, it evaluated >64,000 ACL-reconstructed knees to study posttraumatic OA. They concluded that reconstructive surgery does not seem to have a protective effect on long-term OA. 26
Because of insufficient data, we could not perform a subgroup analysis for the different graft types in our article. Both BPTB and soft tissue grafts (hamstring and quadriceps tendons) can provide successful outcomes in terms of knee stability; nonetheless, their impact on the risk of developing OA is still a subject of debate. The meta-analysis by Xie et al 40 found a significantly increased incidence of OA after ACLR in their BPTB group compared with hamstring tendon autografts at a minimum of 5 years. However, the differences in OA risk between the graft types are generally small, and other factors can also influence these results.
In the present review, the ACLR knees were found to have significantly better stability as assessed by arthrometry. These results are expected since ACLR aims to restore knee joint stability; therefore, patients without an ACL are expected to have greater anteroposterior translation during passive, instrumentally measured stability tests. Earlier studies have reported that nonoperative treatment could provide adequate knee stability for patients from the general population who avoid high-risk sports and activities.3,4,6,34 Studies comparing nonoperative treatment and surgical reconstruction showed similar return to play rates 1 to 11 years after the initial injury.1,14,17,29 In most of the trials in our study, patients who had undergone primary ACLR returned to a higher level of sports at the follow-up time than patients who had nonoperative treatment; nonetheless, significant differences could not be proven. Tsoukas et al 38 demonstrated that the mean activity level significantly decreased in the nonoperatively treated group but not for the reconstructed patients compared with the preinjury level.
Based on our results, the Lysholm score was higher in the ACLR group. However, this result did not differ significantly, and we considered that an MD of <3 points on a scale from 0 to 100 should not be considered clinically meaningful. Therefore, as this result was neither mathematically nor clinically significant, our interpretation was that it favors nonoperative treatment. Furthermore, this reflection has already been stated by previous studies,5,11,35 and Smith et al 35 even referred to the result as “no statistically or clinically significant difference between the groups.”
With respect to subsequent surgical procedures, Smith et al 35 found no statistically significant difference between the ACLR and nonoperative treatment during follow-up periods of 5 to 10 years. However, when the follow-up was >10 years, they reported a small, statistically significant difference, suggesting that patients undergoing ACLR had a lower probability of later partial meniscectomy. Logerstedt et al 21 stated that patients with increased knee laxity after ACL injury had a greater chance of later meniscal surgery. In a meta-analysis, Chalmers et al 5 reported that further surgical intervention was required approximately twice as frequently in the nonoperatively treated group than the operative group.
Cuzzolin et al 7 and Saueressig et al 32 recently published separate meta-analyses comparing ACLR to nonoperative treatment. Although they did not focus on isolated ACL injuries, they included some of our included papers (Kessler et al 17 and Tsoukas et al 38 ), and their results and conclusions were almost identical to ours. This supports the findings of each of the studies.
There was a lack of guideline on how to report the results of ACL studies; therefore, we found a high variety of outcomes reported incompletely in some studies, making it even harder to perform a mathematical analysis from the small number of studies. We suspect this could be because of the various publication times and sites and the authors’ interest in different outcomes. Future studies should use a standardized reporting system. For example, the recent OPTIKNEE 2022 consensus provides recommendations to develop, test, and implement evidence-based rehabilitation programs and facilitate data synthesis to reduce the burden of OA. 39
Limitations
As for the interpretation of our work, different aspects should be considered. The present literature has limitations, which are reflected in our study. A few publications could be included, of which only 2 were RCTs, and most of the studies were nonrandomized trials. We included studies investigating ACLR techniques, which are considered outdated today (ACLR with sutures and augmentation; Andersson and Gillquist 2 ; Dahlstedt et al 8 ). However, these surgical procedures were commonly used earlier, and these patients had reached the age where they could develop osteoarthritic symptoms. Furthermore, almost all included studies had low quality because of the higher risk of bias and inconsistency. In addition, 4 studies included only male patients. ACLR and nonoperative treatment techniques were heterogeneous; nonoperative treatment exercises were generally described and differed among the studies. Because of the poor and inappropriate data reporting and the wide variety of outcomes across studies, data pooling was impeded, and we could analyze only 3 outcomes mathematically. Finally, the statistical assessment of heterogeneity and publication bias was not performed during our analysis because of the small number of studies.
Despite these limitations, we followed our strictly developed protocol and applied a rigorous methodology during our analysis.
Conclusion
Based on our findings, there is no certain evidence that reconstruction of an isolated ACL injury is superior or that patients would benefit more from it compared with nonoperative treatment in terms of prevention of osteoarthritic changes, subjective outcome, and return to play. However, ACLR knees showed significantly better passive stability and a trend to be protective against subsequent injuries. We suggest that clinicians consider nonoperative treatment with a well-designed rehabilitative program as a primary option for this special subgroup of ACL-injured patients in the general population. However, these findings must be interpreted with caution because of the low study quality and high risk of bias. There is a need for further well-designed and well-conducted RTCs with standardized research protocols and outcomes based on the current reporting guidelines.
Supplemental Material
Supplemental material, sj-pdf-1-ojs-10.1177_23259671241239665 for Nonoperative Treatment as an Option for Isolated Anterior Cruciate Ligament Injury: A Systematic Review and Meta-analysis by Robert de Jonge, Miklós Máté, Norbert Kovács, Marcell Imrei, Károly Pap, Gergely Agócs, Szilárd Váncsa, Péter Hegyi and Gergely Pánics in Orthopaedic Journal of Sports Medicine
Supplemental material, sj-pdf-2-ojs-10.1177_23259671241239665 for Nonoperative Treatment as an Option for Isolated Anterior Cruciate Ligament Injury: A Systematic Review and Meta-analysis by Robert de Jonge, Miklós Máté, Norbert Kovács, Marcell Imrei, Károly Pap, Gergely Agócs, Szilárd Váncsa, Péter Hegyi and Gergely Pánics in Orthopaedic Journal of Sports Medicine
Acknowledgments
The authors thank Professor László Hangody for his valuable professional insights and guidance.
Footnotes
Final revision submitted August 29, 2023; accepted September 18, 2023.
The authors have declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Supplemental Material: Supplemental Material for this article is available at https://journals.sagepub.com/doi/full/10.1177/23259671241239665#supplementarymaterials
References
- 1. Ageberg E, Thomeé R, Neeter C, Silbernagel KG, Roos EM. Muscle strength and functional performance in patients with anterior cruciate ligament injury treated with training and surgical reconstruction or training only: a two to five-year followup. Arthritis Rheum. 2008;59(12):1773-1779. [DOI] [PubMed] [Google Scholar]
- 2. Andersson C, Gillquist J. Treatment of acute isolated and combined ruptures of the anterior cruciate ligament. A long-term follow-up study. Am J Sports Med. 1992;20(1):7-12. [DOI] [PubMed] [Google Scholar]
- 3. Bonamo JJ, Fay C, Firestone T. The conservative treatment of the anterior cruciate deficient knee. Am J Sports Med. 1990;18(6):618-623. [DOI] [PubMed] [Google Scholar]
- 4. Buss DD, Min R, Skyhar M, et al. Nonoperative treatment of acute anterior cruciate ligament injuries in a selected group of patients. Am J Sports Med. 1995;23(2):160-165. [DOI] [PubMed] [Google Scholar]
- 5. Chalmers PN, Mall NA, Moric M, et al. Does ACL reconstruction alter natural history? A systematic literature review of long-term outcomes. J Bone Joint Surg Am. 2014;96(4):292-300. [DOI] [PubMed] [Google Scholar]
- 6. Ciccotti MG, Lombardo SJ, Nonweiler B, Pink M. Non-operative treatment of ruptures of the anterior cruciate ligament in middle-aged patients. Results after long-term follow-up. J Bone Joint Surg Am. 1994;76(9):1315-1321. [DOI] [PubMed] [Google Scholar]
- 7. Cuzzolin M, Previtali D, Zaffagnini S, et al. Anterior cruciate ligament reconstruction versus nonoperative treatment: better function and less secondary meniscectomies but no difference in knee osteoarthritis—a meta-analysis. Cartilage. 2021;13(suppl 1):S1658-S1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dahlstedt L, Dalén N, Jonsson U, Adolphson P. Cruciate ligament prosthesis vs. augmentation: a randomized, prospective 5-year follow-up of 41 cases. Acta Orthop Scand. 1993;64(4):431-433. [DOI] [PubMed] [Google Scholar]
- 9. Delince P, Ghafil D. Anterior cruciate ligament tears: conservative or surgical treatment? A critical review of the literature. Knee Surg Sports Traumatol Arthrosc. 2012;20(1):48-61. [DOI] [PubMed] [Google Scholar]
- 10. Duncan KJ, Chopp-Hurley JN, Maly MR. A systematic review to evaluate exercise for anterior cruciate ligament injuries: does this approach reduce the incidence of knee osteoarthritis? Open Access Rheumatol. 2016;8:1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Failla MJ, Arundale AJ, Logerstedt DS, Snyder-Mackler L. Controversies in knee rehabilitation: anterior cruciate ligament injury. Clin Sports Med. 2015;34(2):301-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gillquist J, Messner K. Anterior cruciate ligament reconstruction and the long-term incidence of gonarthrosis. Sports Med. 1999;27(3):143-156. [DOI] [PubMed] [Google Scholar]
- 13. GRADEpro . GDT: GRADEpro Guideline Development Tool [Computer Software]. McMaster University and Evidence Prime; 2024. gradepro.org [Google Scholar]
- 14. Grindem H, Eitzen I, Moksnes H, Snyder-Mackler L, Risberg MA. A pair-matched comparison of return to pivoting sports at 1 year in anterior cruciate ligament-injured patients after a nonoperative versus an operative treatment course. Am J Sports Med. 2012;40(11):2509-2516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. (ed). Cochrane handbook for systematic reviews of interventions version 6.3. (updated February 2022). Cochrane, 2022. www.training.cochrane.org/handbook
- 16. Järvelä T, Kannus P, Järvinen M. Anterior cruciate ligament reconstruction in patients with or without accompanying injuries: a re-examination of subjects 5 to 9 years after reconstruction. Arthroscopy. 2001;17(8):818-825. [DOI] [PubMed] [Google Scholar]
- 17. Kessler MA, Behrend H, Henz S, et al. Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc. 2008;16(5):442-448. [DOI] [PubMed] [Google Scholar]
- 18. Kovalak E, Atay T, Çetin C, Atay IM, Serbest MO. Is ACL reconstruction a prerequisite for the patients having recreational sporting activities? Acta Orthop Traumatol Turc. 2018;52(1):37-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Krause M, Freudenthaler F, Frosch KH, et al. Operative versus conservative treatment of anterior cruciate ligament rupture. Dtsch Arztebl Int. 2018;115(51-52):855-862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Linko E, Harilainen A, Malmivaara A, Seitsalo S. Surgical versus conservative interventions for anterior cruciate ligament ruptures in adults. Cochrane Database Syst Rev. 2005(2):CD001356. [DOI] [PubMed] [Google Scholar]
- 21. Logerstedt DS, Snyder-Mackler L, Ritter RC, Axe MJ, Godges JJ. Knee stability and movement coordination impairments: knee ligament sprain. J Orthop Sports Phys Ther. 2010;40(4):A1-a37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50(10):3145-3152. [DOI] [PubMed] [Google Scholar]
- 23. Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42(10):2363-2370. [DOI] [PubMed] [Google Scholar]
- 24. Marshall JL, Fetto JF, Botero PM. Knee ligament injuries: a standardized evaluation method. Clin Orthop Relat Res. 1977(123):115-129. [PubMed] [Google Scholar]
- 25. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nordenvall R, Bahmanyar S, Adami J, Mattila VM, Fellander-Tsai L. Cruciate ligament reconstruction and risk of knee osteoarthritis: the association between cruciate ligament injury and post-traumatic osteoarthritis. A population based nationwide study in Sweden, 1987-2009. PLoS One. 2014;9(8):e104681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Page MJ MJ, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Pernin J, Verdonk P, Si Selmi TA, Massin P, Neyret P. Long-term follow-up of 24.5 years after intra-articular anterior cruciate ligament reconstruction with lateral extra-articular augmentation. Am J Sports Med. 2010;38(6):1094-1102. [DOI] [PubMed] [Google Scholar]
- 29. Roos H, Ornell M, Gärdsell P, Lohmander LS, Lindstrand A. Soccer after anterior cruciate ligament injury—an incompatible combination? A national survey of incidence and risk factors and a 7-year follow-up of 310 players. Acta Orthop Scand. 1995;66(2):107-112. [DOI] [PubMed] [Google Scholar]
- 30. Sailhan F, Ribinik P. Conservative versus operative treatment for anterior cruciate ligament tear: Results and risk factors for osteoarthritis. Ann Phys Rehabil Med. 2015;58:e63-e64. [Google Scholar]
- 31. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med. 2016;44(6):1502-1507. [DOI] [PubMed] [Google Scholar]
- 32. Saueressig T, Braun T, Steglich N, et al. Primary surgery versus primary rehabilitation for treating anterior cruciate ligament injuries: a living systematic review and meta-analysis. Br J Sports Med. 2022;56(21):1241-1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Schünemann H BJ GG, Oxman A, editors. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group, 2013. guidelinedevelopment.org/handbook [Google Scholar]
- 34. Segawa H, Omori G, Koga Y. Long-term results of non-operative treatment of anterior cruciate ligament injury. Knee. 2001;8(1):5-11. [DOI] [PubMed] [Google Scholar]
- 35. Smith TO, Postle K, Penny F, McNamara I, Mann CJ. Is reconstruction the best management strategy for anterior cruciate ligament rupture? A systematic review and meta-analysis comparing anterior cruciate ligament reconstruction versus non-operative treatment. Knee. 2014;21(2):462-470. [DOI] [PubMed] [Google Scholar]
- 36. Sterne JAC HM, Reeves BC, Savović J, et al. ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ. 2016; 355; i4919. doi: 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sterne JAC SJ, Page MJ, Elbers RG, et al. : a revised tool for assessing risk of bias in randomised trials. BMJ. 2019; 366: l4898. [DOI] [PubMed] [Google Scholar]
- 38. Tsoukas D, Fotopoulos V, Basdekis G, Makridis KG. No difference in osteoarthritis after surgical and non-surgical treatment of ACL-injured knees after 10 years. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2953-2959. [DOI] [PubMed] [Google Scholar]
- 39. Whittaker JL, Culvenor AG, Juhl CB, et al. OPTIKNEE 2022: consensus recommendations to optimise knee health after traumatic knee injury to prevent osteoarthritis. Br J Sports Med. 2022;56(24):1393-1405. [DOI] [PubMed] [Google Scholar]
- 40. Xie X, Xiao Z, Li Q, et al. Increased incidence of osteoarthritis of knee joint after ACL reconstruction with bone-patellar tendon-bone autografts than hamstring autografts: a meta-analysis of 1,443 patients at a minimum of 5 years. Eur J Orthop Surg Traumatol. 2015;25(1):149-159. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-ojs-10.1177_23259671241239665 for Nonoperative Treatment as an Option for Isolated Anterior Cruciate Ligament Injury: A Systematic Review and Meta-analysis by Robert de Jonge, Miklós Máté, Norbert Kovács, Marcell Imrei, Károly Pap, Gergely Agócs, Szilárd Váncsa, Péter Hegyi and Gergely Pánics in Orthopaedic Journal of Sports Medicine
Supplemental material, sj-pdf-2-ojs-10.1177_23259671241239665 for Nonoperative Treatment as an Option for Isolated Anterior Cruciate Ligament Injury: A Systematic Review and Meta-analysis by Robert de Jonge, Miklós Máté, Norbert Kovács, Marcell Imrei, Károly Pap, Gergely Agócs, Szilárd Váncsa, Péter Hegyi and Gergely Pánics in Orthopaedic Journal of Sports Medicine