Abstract
Alzheimer’s disease (AD) is a neurodegenerative disorder and the most common cause of dementia globally. The pathogenesis of AD remains still unclear. The three main features of AD are extracellular deposits of amyloid beta (Aβ) plaque, accumulation of abnormal formation hyper-phosphorylated tau protein, and neuronal loss. Mitochondrial impairment plays an important role in the pathogenesis of AD. There are problems with decreased activity of multiple complexes, disturbed mitochondrial fusion, and fission or formation of reactive oxygen species (ROS). Moreover, mitochondrial transport is impaired in AD. Mouse models in many research show disruptions in anterograde and retrograde transport. Both mitochondrial transportation and network impairment have a huge impact on synapse loss and, as a result, cognitive impairment. One of the very serious problems in AD is also disruption of insulin signaling which impairs mitochondrial Aβ removal.
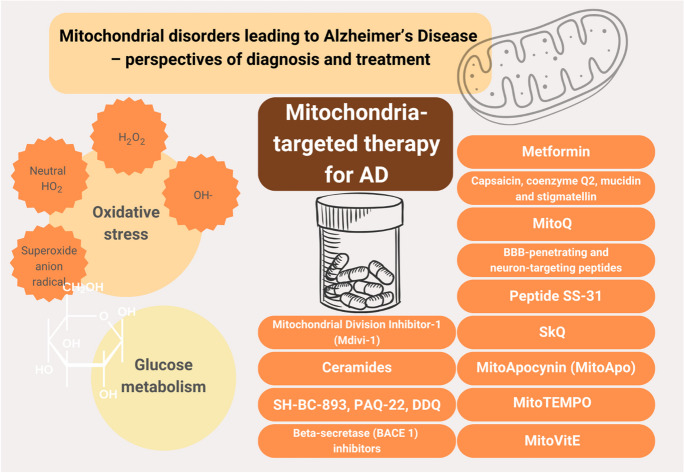
Discovering precise mechanisms leading to AD enables us to find new treatment possibilities. Recent studies indicate the positive influence of metformin or antioxidants such as MitoQ, SS-31, SkQ, MitoApo, MitoTEMPO, and MitoVitE on mitochondrial functioning and hence prevent cognitive decline. Impairments in mitochondrial fission may be treated with mitochondrial division inhibitor-1 or ceramide.
Graphical Abstract
(Graphic content via Canva Pro)
Keywords: Mitochondrial dysfunction, Alzheimer’s disease, Oxidative stress, ROS, Antioxidants, MitoQ
Introduction
Alzheimer’s disease (AD) is a progressive neurodegenerative disorder characterized by cognitive impairment and mental symptoms. AD is responsible for up to 80% of dementia diagnoses [1]. In 2020, about 44 million people worldwide suffered from AD and this is estimated to double by 2050 [2]. Most AD patients exhibit non-hereditary, late-onset Alzheimer’s disease (LOAD) which is sporadic. Only 5% of all cases of AD are a result of dominant mutations of APP, PSEN1, and PSEN2 genes. The risk of AD increases with older age and genetic factors, such as the ApoE gene, which occurs in 16% of the population. Also, lifestyle and dietary factors increase the probability of Alzheimer’s disease [3–5]. Pathological criteria for AD diagnosis include increased levels of Aβ peptide and hyperphosphorylated tau (p-tau) [5]. β-amyloid forms structures called plaques and tau forms neurofibrillary tangles. Both of the proteins are indicators of AD as they are responsible for cell death resulting in loss of brain tissue [6]. The pathogenesis of AD is complex and multifactorial. Although the mechanism of AD pathogenesis is still unclear, the growing evidence suggests that damaged mitochondria play a fundamental role in AD pathogenesis [7]. Several mitochondrial alterations are found in AD [1]. The mitochondrial dysfunction affects amyloid precursor protein (APP) production, APP cleavage, and Aβ accumulation. Moreover, mitochondrial dysfunction can stimulate other molecular changes associated with AD, such as impaired tau phosphorylation and inflammation [7].
2. Mitochondrial impairment in AD
Mitochondria are the cell’s energy source, providing most of the ATP through oxidative phosphorylation (OXPHOS). Of all cell types, neurons have one of the highest rates of ATP utilization, which is used primarily to maintain the ionic gradients required for continuous electrophysiological activity, neurotransmission, and short-term synaptic plasticity [8]. Mitochondria involve energy production, communication between brain cells, and detoxification. They regulate temperature and maintain redox balance in cells [9]. Mitochondrial dysfunction causes many pathological cellular processes, such as the production of reactive oxygen species (ROS) and associated oxidative stress, as well as intracellular calcium deregulation and apoptosis. In Alzheimer’s disease, decreased activity of multiple complexes such as complex I (NADH ubiquinone oxidoreductase), complex IV (cytochrome oxidase (COX), and complex V (ATPase) [10] which cooperate in ATP producing process [11], pyruvate dehydrogenase complex, and α-ketoglutarate dehydrogenase complex is observed. In comparison to the age-matched non-AD brains also, activity of phosphofructokinase (PFK), phosphoglycerate mutase, aldolase, glucose-6-phosphate isomerase, and lactate dehydrogenase are reduced. On the other hand, the activity and number of reactive oxygen species (ROS) increased. In the brains of transgenic mice that overexpress human APP, translocase progressively accumulates mitochondrial Aβ, it is connected with reduced activity of ETC complexes III and IV, and the rate of oxygen consumption decreases [10]. The results of the studies revealed that mitochondrial impairment occurs before plaque deposition and, what is more, Aβ-associated mitochondria were observed even 4 months before extracellular Aβ deposits. AD mitochondria not only are small and fragmented but also, as mouse models have shown, have impaired function of mitochondrial fusion and fission [10]]. Fusion and fission are necessary to maintain mitochondrial homeostasis. Imbalance in this process leads to mitochondrial swelling, depolarisation, and fragmentation, increases susceptibility to many forms of neuronal stress, and, as a result, leads to cell death [11]. Mitochondrial trafficking also is impaired by Aβ [10]. Rat model studies have shown that the addition of Aβ to the isolated mitochondria causes mitochondrial dysfunction such as mitochondrial membrane depolarization, ATP/ADP ratio decrease, cytochrome c expulsion, and activation of caspase-3 can be a trigger to the apoptotic cascade [12]. Also, Aβ makes connections between mitochondria and endoplasmic reticulum abnormally tight and impairs Ca2 + signaling, autophagy, motility, and apoptosis. Recently it was shown that the mitochondrial large-conductance Ca2 + -activated potassium channels are directly blocked by Aβ [2]. Ca2 + efflux is also blocked by tau which inhibits mitochondrial Na + /Ca2 + exchanger. Mitochondria are not only energy producers, but also calcium signaling, an important element in cell death. Blocking the Na + /Ca2 + exchanger leads to calcium overload, opening the mitochondrial permeability transition pore (mPTP), and as a result induces cell death [13]. Moreover, the experimental models of AD showed a dysfunction of mitochondrial transport. Mitochondria moves through neurons by kinesin, toward the nerve terminal (anterograde direction), and dynein, toward the soma (retrograde direction). Intracellular movement is necessary to maintain neuronal polarity, neurotransmission, and membrane potential. In AD even before Aβ and tau aggregation, axonal degeneration, as a result of excessive accumulation of mitochondria, is observed. The APP mouse models indicate impairment in anterograde transport while APP/PSEN1 and PSEN1 mouse models are characterized by dysfunction of anterograde and retrograde transport. Other mouse models (Tg2576 APP transgenic mice and APP/PS1) performed damaged, round, and swollen mitochondria coinciding with loss of oxidative activity and preceding the beginning of cognitive impairment and β-amyloid plaque creation. Both mitochondrial transportation and network impairment have a huge impact on synapse loss and, as a result, cognitive impairment [11]. Also APOE status may have an impact on mitochondrial function as non‐demented APOE ε4 individuals in comparison to non-APOE ε4 individuals have lower mitochondrial COX activity in the brain. It influences not only ETC but also glucose metabolism [14]. Alterations in genes related to mitochondrial energy metabolism and apoptosis were reported in young transgenic AD mice, which persisted throughout adulthood [15]. Early damage to genes involved in glucose metabolism and mitochondrial function, including AMP-activated protein kinase (AMPK), NRF1 and NRF2, and PGC-1α, as well as changes in oxidative phosphorylation complexes (OXPHOS) in APP/PS1 mice before atherosclerotic plaque, has been demonstrated [16]. All of this has the effect of decreasing mitochondrial activity and function. An increase in PGC-1α, which stimulates PPAR or sirtuin, reduces Aβ plaques so it has a neuroprotective effect in AD [17].
3. Oxidative stress AD
Oxidative stress is a condition in which the production of reactive oxygen species (ROS) exceeds the cell’s antioxidant defense system. It occurs through various pathways. Oxidative stress is associated with DNA defects, abnormal gene expression, defective enzyme activities, and energy failure. Reactive oxygen species (ROS) are by-products of metabolism. They are essential for the physiological functioning of the cells, but at high levels, they can be toxic [18]. Mitochondrial dysfunction, which causes increased production of reactive oxygen species (ROS), seems to contribute to the neurodegenerative mechanisms of Alzheimer’s disease. In this process, neurons are damaged and occur in various pathways. In AD, oxidative stress plays a very important role. In the cell, antioxidant enzymes such as superoxide dismutase (SOD), glutathione peroxidase (GPX), thioredoxins, glutaredoxins, and catalase, as well as non-enzymatic antioxidant factors such as vitamin E, vitamin A, vitamin C, uric acid, and carotenoids, perform the most important defense functions [19]. One of the first markers of AD is increased mtDNA oxidation. Having an age-related decline in mitochondrial function may be one of the first events in the pathogenesis of sporadic late-onset Alzheimer’s disease. According to the mitochondrial cascade hypothesis, age-related loss of mitochondrial function affects the expression and processing of APP, producing amyloid beta oligomers that accumulate in atherosclerotic plaques in Alzheimer’s disease [20]. The brain has a lot of readily oxidizable fatty acids and has a high demand for paramagnetic O2 and transition metal ions. In the oxidative production of ATP, the generation of ROS is inevitable and is a major cause of macromolecular damage (Table 1) [21]. ROS are typically reactive oxygen-containing molecules. The most common ROS is superoxide anion radical. It is mainly produced in complex I of the electron transport chain (ETC) in the inner mitochondrial membrane. The anions of this radical can move within 30 nm of formation; upon protonation, the superoxide becomes neutral HO2, which can cross the inner mitochondrial membrane and then accumulate in the cytoplasm [22]. The net effect of these ROS oxygen radicals is damage and death of vulnerable neurons in AD. Another ROS is H2O2. It diffuses easily across the inner mitochondrial membrane because it has a zero dipole moment, moving at least 1 µm from the site of production. H2O2 is less reactive than superoxide but can interact with reduced iron (Fe2 +), from iron-sulfur proteins or heme proteins, through Fenton chemistry, forming one of the most reactive ROS, free hydroxyl radicals (OH–) [23]. Hydroxyl radicals are the most reactive and have many possible interactions. They are formed at the metal site hence their higher site specificity. Disruption of metal metabolism has been observed in Alzheimer’s disease.
Table 1.
Characteristics of the ROS
| Reaction oxygen–containing molecules | Description |
|---|---|
| Superoxide anion radical | Move within 30 nm of formation; upon protonation, the superoxide becomes neutral HO2 |
| Neutral HO2 | Able to cross the inner mitochondrial membrane and then accumulate in the cytoplasm |
| H2O2 | Diffuses easily across the inner mitochondrial membrane; it has a zero dipole moment; moving at least 1 µm; less reactive than superoxide |
| OH– (free hydroxyl radicals) | Most reactive ROS; have wide range of possible interactions; they are formed of the metal site, hence their higher site specificity |
Glucose metabolism in AD
The human brain utilizes up to 25% of total body glucose which makes it one of the highest energy-consuming organs [7]. Multiple studies proved a connection between glucose metabolism impairment and the pathogenesis of Alzheimer’s disease. Impaired energy metabolism implicates mitochondrial dysfunction. Global reductions in glucose metabolism were detected by positron emission tomography (PET) with [18F]-fluoro-deoxyglucose (FDG) in AD brains 3 [10]. In the earliest stages of AD, decreased glucose metabolism predominates in posterior brain regions [24]. Glucose hypometabolism occurs decades before the onset of Alzheimer’s disease [7] and could be useful in the detection of AD at the early stages [24]. As glucose metabolism impairment and insulin resistance in AD brains are similar to abnormalities in type 2 diabetes, it is suggested that AD may be a brain representation of type 2 diabetes [25], and de la Monte et al. have named AD “type 3 diabetes” [10].
Glucose metabolism is a multi-stage process. It consists of glucose transportation and intracellular metabolism [7]. Transportation is provided by glucose transporters (GLUTs) [26]. Due to decreased GLUT1 and GLUT3 concentration in the AD patient’s brains, there is reduced glucose uptake. Aβ interferes with GLUT3 and impairs membrane translocation which is regulated by CKMP. Aβ inhibits CKMP which leads to glucose hypometabolism, higher glucose concentration in the brain, and is related to the severity of AD [10]. A decrease of GLUT4 in mouse models of AD has shown exacerbation of neurodegeneration and amyloid pathology and worsens cognitive function [10]. GLUT4 is insulin-regulated as insulin stimulates the expression of the GLUT4 gene and glucose transportation from the cytosol to the plasma membrane [27]. GLUT4 plays an important role in memory acquisition in the hippocampus; consequently, impairment in GLUT4 functioning may manifest as cognitive impairment [10].
In early AD stages, insulin levels are decreased, and as AD progresses insulin signaling and as a result glucose metabolism worsens [10], and insulin resistance increases. Insulin resistance reduces the level of insulin-degrading enzyme (IDE) [28] which metabolizes mitochondrial β-amyloids [10]. That leads to the conclusion that insulin signaling impairment disrupts mitochondrial Aβ removal. Mitochondrial Aβ might prompt mitochondrial dysfunction by Aβ-binding alcohol dehydrogenase (ABAD) which causes apoptosis and oxidative stress. In Du et al.’s study, the bound component of a transition pore–cyclophilin D also leads to oxidative stress and apoptosis and, as a study on AβPP mice showed, impacts on preservation of cognitive function [29].
Mitochondria-targeted therapy for AD
Despite the significant development in medicine over recent years, no satisfying medication for AD is available. The current drugs only delay the progression of the disease. A better knowledge of particular molecular pathways, including mitochondrial dysfunction, may lead to novel therapeutic strategies for treatments. Table 2 summarizes the potential mitochondria-target therapy useful in AD.
Table 2.
Mitochondria-targeted AD treatment
| Potential drug | Mechanism of action | Results |
|---|---|---|
| Metformin | Inhibition of mitochondrial complex I | Activation of 5′-AMP-activated protein kinase (AMPK) |
| Capsaicin, coenzyme Q2, mucidin, and stigmatellin | Partial inhibition of mitochondrial complex I | Reduction of ROS level |
| MitoQ | Regulation of autophagy by induction of a pseudo mitochondrial membrane potential (PMMP) | Reduction of ROS level |
| BBB-penetrating and neuron-targeting peptides | Delivery antioxidants into neuronal mitochondria | Suppression of neuronal death and mitigating oxidative stress |
| Peptide SS-31 | Inhibition cardiolipin peroxidation | Reduction of ROS level |
| SkQ | Direct neutralization of ROS due to the oxidation of plastoquinone, reduction of mitochondrial membrane potential | Reduction of ROS level, the hyperphosphorylation of amyloid-β1-42 (Abeta) and its precursor APP |
| MitoApocynin (MitoApo) | Inhibition NOX2 activation | Reduction of oxidative and nitrative stress, glial activation, and inflammatory reactions |
| MitoTEMPO | Increasing superoxide dismutase activity | Reduction of production of ROS and Aβ-induced lipid peroxidation |
| MitoVitE | Inhibition of lipid peroxidation | Reduction of peroxide-mediated oxidative stress, peroxide-induced caspase activation, and oxidative stress–induced cell death |
| Mitochondrial division inhibitor-1 (Mdivi-1) | Regulation of mitochondrial fusion | Reduction of production of ROS and lipid peroxidation |
| Ceramides | Induction Drp1 and activation caspases and inhibition of mitochondrial fission | Reduction of oxidative stress |
| SH-BC-893, PAQ-22, DDQ | Inhibition of mitochondrial fission | Reduction of oxidative stress |
| Beta-secretase (BACE 1) inhibitors | Reduction of mitochondrial membrane potential affects mitochondrial recycling and, as a result, upregulates cellular apoptotic signaling | Upregulation cellular apoptotic signaling |
Metformin
This well-known medicine is applied to many patients around the world. The data shows that DMT 2 is one of the risk factors for cognitive impairments, vascular dementia, and AD [30], one of the first therapeutic choices for diabetes mellitus type 2 (DMT2). It is also used to cure obesity, liver diseases, cardiovascular diseases, renal diseases, and even some types of cancer like breast cancer, endometrial cancer, or colorectal cancer [31]. Recent studies show its possible beneficial influence on mitochondrial dysfunctions. Metformin could inhibit mitochondrial complex I to result in defective cyclic AMP and protein kinase A signaling in response to glucagon and the stimulation of AMPK [32]. In some clinical trials, it was confirmed that taking metformin significantly improved the cognition of the patients compared to a placebo [33]. However, in the longitudinal study by Wu et al., there was no correlation between metformin treatment and longitudinal memory change found [34]. What is more, a case–control study by Imfeld et al. showed that long-term metformin uptake correlates with a slightly higher risk of developing AD [35]. This is why this topic must be further investigated.
Partial mitochondrial complex I inhibition
Inhibition of the mitochondrial respiratory chain complex I, which contributes to creating reactive oxygen species (ROS), using small molecules, leads to a reduction in oxidative metabolism. There are various inhibitors of this part of the mitochondria membrane. They differ from each other according to the impact on ROS creation or the effect on the enzyme’s kinesthetics. Among those inhibitors that also prevent ROS, we may list the following substances such as capsaicin, coenzyme Q2, mucidin, and stigmatellin. Inhibitors that increase the level of ROS in the cell are piericidin A or rolliniastatin 1 and 2 [36]. What is more, there are some mutations in complex I that prevent NADH oxidation which at the same time stop ROS production [37]. Interestingly, one of the inhibitors of complex I, a small molecule called tricyclic pyrone compound (CP2), is presumed to be a perfect drug considering its safety profile and low toxicity and does not interfere with human receptors and ion channels [38]
CP2, even during stress conditions, reduced the proton leak. Many studies show that long molecule uptake resulted in considerable improvement of the nervous system homeostasis and the reduction of oxidative stress and inflammation which prevented neurodegeneration. At the same time, no signs of toxicity were observed [30]. Another advantage of CP2 is the fact that it prevents the formation of Aβ aggregates which prevents AD [39].
The mitochondria-targeted antioxidant MitoQ
MitoQ is a mitochondria-targeted antioxidant with good neuroprotective features. By inducing a pseudo-mitochondrial membrane potential, it may affect mitochondrial respiration and cause autophagy. This process allows the cell to eliminate dysfunctional components [40]. MitoQ may be a renewable antioxidant [41]. The research on mice revealed that daily administration of this substance results in the improvement of the physical parameters and oxygen consumption [42]. Other studies show that daily addition of MitoQ to their drinking water prevented mice, which had mutant human transgenes responsible for AD early onset, from cognitive decline and AD-like pathologies [43]. However, MitoQ is not functioning when there is no coenzyme Q in mitochondria. This is because complex III cannot oxidize the reduced quinol form of MitoQ [44].
New methods of drug administration to the neuronal mitochondria—biomimetic engineered nanosystems
Recent developments in biomimetic technology allow the development of new methods of treatment. The problems caused by the toxicity of synthetic materials were a serious complication in obtaining efficient transport to the neuronal mitochondria. In the past, there were used nanomaterials made of gold or silica, newly founded biomaterials such as human serum albumin red blood cell membrane–coated nanoparticle. It is modified to successfully reach the neuronal mitochondria. In the first studies, curcumin was used as a model drug [45].
Human serum albumin seems to be a perfect substance for medicine delivery due to its non-toxicity. The modified albumin could reach mitochondria in the nervous cell thanks to the positron emission tomography agent 7-(6-nitropyridin-3-yl) − 5H-pyrido[4,3-bindole (T807) which binds specifically to the nervous cells [46]. To reach the highest biocompatibility and to prevent interference with the RBC membranes, the lipid-insertion method was developed. The ligand may be thanks to this covering on the surface. The ligands after such a process are named with a special prefix such as DSPE-PEG3400-T807 [45].
Antioxidant peptide SS-31
Antioxidant tetrapeptide SS-31 (D-Arg-Dmt-Lys-Phe-NH2; Dmt-2′,6′-dimethyl tyrosine) also known as MTP-131 decreases the impact of oxygen stress for the cell and stabilizes cardiolipin cytochrome c complex [47, 48]. In the research, it was revealed that administration of SS-31 to mice improves lipopolysaccharide (LPS)-induced memory, which is impaired due to oxidative stress. It also results in normal gene expression of antioxidant enzymes. The advantages of using SS-31 as a drug in neuro dysfunctional diseases may be also added to the fact of better administration of brain-derived neurotrophic factor (BDNF) signaling [49, 50].
SkQ
It was the first mitochondria-targeted medicine used in clinical practice. It effectively eliminates ROS from the cells thanks to its structure—plastoquinone or thymoquinone which are antioxidants and responsible for electrophoretic transport of triphenylphosphonium—as an alternative rhodamine 19. They are bonded together by a linker of 10 carbon atoms [51].
Mitochondria-targeted antioxidants, such as SkQ, have a big advantage in that they may be used in very low concentrations which also limits the possibility of side effects on the organism. SkQ is a great hope for Alzheimer patients not only because of its limitation of ROS from the mitochondria. In the research, it was also confirmed that long-term administration of this drug declines the hyperphosphorylation of amyloid-β1-42 (Abeta) and its precursor APP [52]. However, the positive results were observed after a single administration of the molecule—the increase of the synaptic transmission was meaningful [51, 53].
MitoApocynin (MitoApo)
MitoApo is a recently synthesized and orally administered derivative of apocynin. It targets mitochondria where it protects against oxidative damage and glial-mediated inflammation. Its efficiency in Parkinson’s disease (PD) was confirmed in numerous research; however, it is presumed to be also a possibility for treatment in other neurodegenerative diseases like AD. It must be taken under further investigation [54, 55].
MitoTEMPO
It contains a free radical electron which is capable of eliminating mitochondrial superoxide. Its full name is 2,2,6,6-tetramethylpiperidin-1-yl)oxyl (TEMPO). This molecule highly improves the functioning of the mitochondrium—and limits the production of ROS and Aβ-induced lipid peroxidation. MitoTEMPO also mitigates Aβ-induced mitochondrial DNA (mtDNA) depletion. It was also confirmed that it limits the expression of mtDNA replication–related DNA polymerase gamma (DNA pol γ) [56, 57].
MitoVitE
Mitochondrially targeted vitamin E reduces H2O2, inhibits caspase activation, and staves off apoptosis. Its full name is [2–3,4dihydro-6-hydroxy-2,5,7,8tetra-methyl-2H-1-benzopyran-2-yl], and this molecule is built of aromatic head with two ring structures and triphenylphosphonium bromide group (TPPB). MitoVitE is, due to TPPB, hydrophobic, which facilitates contact with mitochondrial membranes.
MitoVitE efficacy, even with a very small, nanomolecular portion during administration, is significantly high [10, 56].
Mitochondrial division inhibitor-1 (Mdivi-1)
A new promising drug in fighting AD may be mitochondrial division inhibitor-1 (Mdivi-1). It is a dynamin-related protein 1 (Drp1)-specific inhibitor. Drp-1 is a mitochondrial protein responsible for membrane fragmentation [58, 59]. This small molecule has a big influence on mitochondria bioenergetics by influencing its dynamics, autophagy, ATP production, or the immune response. Mdivi-1 administration led to a reduction in H2O2 production and lipid peroxidation [57, 60].
In the research, it was found that Mdivi-1 improves mitochondrial function by limiting Aβ deposition [61]. What is more, it also positively influences mitochondrial fragmentation and deficit distribution [59].
Ceramides
Ceramides are responsible for the regulation of many processes in the cells like proliferation or cellular aging. They are lipids built from sphingosine and a fatty acid [62]. The levels of ceramides in the serum or cerebrospinal fluid (CSF) are increased in patients with AD. They are responsible for the generation and aggregation of Aβ [63]. In the mitochondria, ceramides induced Drp1 and activated caspases. What is more, these lipids mediate the binding of Aβ to VDAC. Those processes led to neuronal cell death [64].
A new possibility of treatment would be to inhibit ceramides in Aβ-mediated toxicity in patients with AD. Research shows that the synthetic sphingolipid SH-BC-893 may be successfully used in rapid inhibition of ceramide-induced mitochondrial fission. What is more, it may lead to weight loss due to causing a similar effect as caloric restriction obtained in reducing food intake [65].
Other inhibitors of mitochondrial fission
Mitochondrial fission is an important process in maintaining homeostasis, and it is a promising strategy for mitigating mitochondrial dysfunction. SH-BC-893 blocks palmitate, and ceramide-induced mitochondrial dysfunction prevents oxidative stress. Among other substances with these features, we may list 3-[2,6-diethylphenyl]quinazoline-2,4-dione (PAQ-22) [66], 1H-pyrrole-2-carboxamide [67], or DDQ (diethyl (3,4-dihydroxy phenethylamine) quinolin-4-yl]methylphosphonate) [68]. These molecules seem to be a new possibility of treatment for AD patients.
Beta-secretase (BACE) inhibitors
Recently, there have been beta-secretase (BACE) inhibitors such as 5XFAD proposed. At present, their effectiveness was not confirmed in the research. However, this may be one of the brand-new investigation fields that may result in the future new treatment of AD [69].
Lifestyle modifications
Many epidemiological studies suggest the beneficial impact of lifestyle modifications, including diet and physical activity. Physical activity improves the regulation of metabolic pathways, including insulin signaling, glucose, carbohydrates, and fatty acid metabolism. Exercises improve cognitive deficits in the APP/PS1 transgenic mouse. In the research, after 5 months of treadmill exercises, the level of APP phosphorylation and PS1 expression declined significantly [70]. Results of studies have shown that regular aerobic exercises have a positive influence on neurological skills. Among many improved areas, we may list concentration, learning capacity, and executive function. Regular activity also increased cortical thickness [71]. It has an anti-inflammatory effect and reduces the cardiovascular risk [72]. More frequent exercises stimulate the neurological system to restore thanks to enlarged levels of neurotrophins like brain-derived neurotrophic factors. They are secreted under the influence of ketone bodies, lactate, or muscle-derived myokines whose amount is increased after exercises [73]
Even though during exercises the level of oxidative stress is increased, regular physical exercises improve redox status thanks to vasodilatation and increasing the release of nitric oxide [74]. The level of the Aβ plaques in the patients with AD has also decreased thanks to the exercises [75], the same as the level of neuronal damage markers—neuron-specific enolase or catalase activity and ROS levels [10].
Thanks to the regular exercises, both mitochondrial biogenesis and regeneration [76], it also improves healthy aging and increases antioxidant capacities [77]. The beneficial influence of psychical effort in AD patients with mild variants of the disease preserved cognition [78, 79] awareness and problem-solving spheres of the memory score [80].
Research shows that also our dietary habits have a big influence on our neurological health. The Mediterranean diet is said to be balanced in the best possible way, providing the patient with the highest amount of nutrients and at the same time the lowest dose of saturated fats [81, 82]. Inherence of long-chain polyunsaturated fatty acids (PUFAs) in the daily diet is connected with a decreased risk of AD [83]. There were also benefits of a ketogenic diet on brain metabolism confirmed. It is explained by compensation for the AD brain glucose insufficient level [84]. Not only providing good products but also calorie restriction has a positive impact on cognition. Limitation of calories, however, with preservation of nutrients and avoidance of malnutrition, results in improving cognitive skills and slows down the aging process [85]. There are some substances like caffeine, curcumin, dapsone, metformin, resveratrol, or spermidine, which have similar effects as caloric restriction [86].
To sum up, exercise and diet may be a safe possibility for treatment, with many other advantages for the whole patient’s body, not only considering treating AD. Of course, it should be under the control of the patient’s doctor to adjust the intensity of the exercises and to choose an appropriately balanced diet.
Summary
Alzheimer’s disease is the most common cause of dementia in the older population. The number of patients is predicted to significantly increase in the coming years. Currently, the therapy is limited to the symptomatic treatment. A better knowledge of pathogenesis has a crucial role in finding a novel therapy. The main aspect of this research was to focus on mitochondrial disorders leading to AD. Many studies show that oxidative stress is responsible for many neuronal damage as well as Aβ deposits. Modern therapy possibilities focus on decreasing ROS levels. The urgent concern is also developing new methods to transport drugs directly into the mitochondria, without causing any reactions with other body tissues. Much research is conducted by many scientists all over the world which gives hope for further investigation of this topic.
Author contribution
MP: conceptualization, methodology, data curation, formal analysis, investigation, writing—review and editing; KW, WM, and MM: formal analysis, investigation, writing—review and editing; JL: conceptualization, investigation, writing—review and editing; JCŁ: review and editing.
Funding
This study received no extramural funding.
Data availability
All the data is available on the request of the authors.
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Calvo-Rodriguez M, Bacskai BJ. Mitochondria and calcium in Alzheimer’s disease: from cell signaling to neuronal cell death. Trends Neurosci. 2021;44:136–151. doi: 10.1016/j.tins.2020.10.004. [DOI] [PubMed] [Google Scholar]
- 2.Dumurgier J, Sabia S. Epidemiology of Alzheimer’s disease: latest trends. Rev Prat. 2020;70:149–151. [PubMed] [Google Scholar]
- 3.Long JM, Holtzman DM. Alzheimer disease: an update on pathobiology and treatment strategies. Cell. 2019;179:312–339. doi: 10.1016/j.cell.2019.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rostagno AA. Pathogenesis of Alzheimer’s disease. Int J Mol Sci. 2022;24:107. doi: 10.3390/ijms24010107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crous-Bou M, Minguillón C, Gramunt N, Molinuevo JL. Alzheimer’s disease prevention: from risk factors to early intervention. Alzheimers Res Ther. 2017;9:71. doi: 10.1186/s13195-017-0297-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khan S, Barve KH, Kumar MS. Recent advancements in pathogenesis, diagnostics and treatment of Alzheimer’s disease. Curr Neuropharmacol. 2020;18:1106–1125. doi: 10.2174/1570159X18666200528142429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang W, Zhao F, Ma X, Perry G, Zhu X. Mitochondria dysfunction in the pathogenesis of Alzheimer’s disease: recent advances. Mol Neurodegener. 2020;15:30. doi: 10.1186/s13024-020-00376-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levy M, Faas GC, Saggau P, Craigen WJ, Sweatt JD. Mitochondrial regulation of synaptic plasticity in the hippocampus. J Biol Chem. 2003;278:17727–17734. doi: 10.1074/jbc.M212878200. [DOI] [PubMed] [Google Scholar]
- 9.Reiss AB, Ahmed S, Dayaramani C, Glass AD, Gomolin IH, Pinkhasov A, Stecker MM, Wisniewski T, De Leon J. The role of mitochondrial dysfunction in Alzheimer’s disease: a potential pathway to treatment. Exp Gerontol. 2022;164:111828. doi: 10.1016/j.exger.2022.111828. [DOI] [PubMed] [Google Scholar]
- 10.Johri A. Disentangling mitochondria in Alzheimer’s disease. Int J Mol Sci. 2021;22:11520. doi: 10.3390/ijms222111520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharma C, Kim S, Nam Y, Jung UJ, Kim SR. Mitochondrial dysfunction as a driver of cognitive impairment in Alzheimer's Disease. Int J Mol Sci. 2021;22(9):4850. 10.3390/ijms22094850. [DOI] [PMC free article] [PubMed]
- 12.Faizi M, Seydi E, Abarghuyi S, Salimi A, Nasoohi S, Pourahmad J. A search for mitochondrial damage in Alzheimer’s disease using isolated rat brain mitochondria., Iran. J Pharm Res. 2016;15:185–195. [PMC free article] [PubMed] [Google Scholar]
- 13.Britti E, Ros J, Esteras N, Abramov AY. Tau inhibits mitochondrial calcium efflux and makes neurons vulnerable to calcium-induced cell death. Cell Calcium. 2020;86:102150. doi: 10.1016/j.ceca.2019.102150. [DOI] [PubMed] [Google Scholar]
- 14.Perez Ortiz JM, Swerdlow RH. Mitochondrial dysfunction in Alzheimer’s disease: role in pathogenesis and novel therapeutic opportunities. Br J Pharmacol. 2019;176:3489–3507. doi: 10.1111/bph.14585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reddy PH, McWeeney S, Park BS, Manczak M, Gutala RV, Partovi D, Jung Y, Yau V, Searles R, Mori M, Quinn J. Gene expression profiles of transcripts in amyloid precursor protein transgenic mice: up-regulation of mitochondrial metabolism and apoptotic genes is an early cellular change in Alzheimer’s disease. Hum Mol Genet. 2004;13:1225–1240. doi: 10.1093/hmg/ddh140. [DOI] [PubMed] [Google Scholar]
- 16.Pedrós I, Petrov D, Allgaier M, Sureda F, Barroso E, Beas-Zarate C, Auladell C, Pallàs M, Vázquez-Carrera M, Casadesús G, Folch J, Camins A. Early alterations in energy metabolism in the hippocampus of APPswe/PS1dE9 mouse model of Alzheimer’s disease. Biochim Biophys Acta - Mol Basis Dis. 2014;1842:1556–1566. doi: 10.1016/j.bbadis.2014.05.025. [DOI] [PubMed] [Google Scholar]
- 17.Wang J, Guo M-N, Liu Z-Z, Ma S-F, Liu W-J, Qian J-J, Zhang W-N. PGC-1α reduces Amyloid-β deposition in Alzheimer’s disease: effect of increased VDR expression. Neurosci Lett. 2021;744:135598. doi: 10.1016/j.neulet.2020.135598. [DOI] [PubMed] [Google Scholar]
- 18.Galaris D, Barbouti A, Pantopoulos K. Iron homeostasis, and oxidative stress: an intimate relationship. Biochim Biophys Acta Mol Cell Res. 2019;1866:118535. doi: 10.1016/j.bbamcr.2019.118535. [DOI] [PubMed] [Google Scholar]
- 19.Mecocci P, Boccardi V, Cecchetti R, Bastiani P, Scamosci M, Ruggiero C, Baroni M. A long journey into aging, brain aging, and Alzheimer’s disease following the oxidative stress tracks. J Alzheimer's Dis. 2018;62:1319–1335. doi: 10.3233/JAD-170732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cheignon C, Tomas M, Bonnefont-Rousselot D, Faller P, Hureau C, Collin F. Oxidative stress and the amyloid beta peptide in Alzheimer’s disease. Redox Biol. 2018;14:450–464. doi: 10.1016/j.redox.2017.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brand MD. The sites and topology of mitochondrial superoxide production. Exp Gerontol. 2010;45:466–472. doi: 10.1016/j.exger.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCord JM, Fridovich I. Superoxide dismutase. An enzymic function for erythrocuprein (hemocuprein) J Biol Chem. 1969;244:6049–55. doi: 10.1016/S0021-9258(18)63504-5. [DOI] [PubMed] [Google Scholar]
- 23.Gutteridge JMC. Iron and oxygen radicals in the brain. Ann Neurol. 1992;32:S16–S21. doi: 10.1002/ana.410320705. [DOI] [PubMed] [Google Scholar]
- 24.Weidling IW, Swerdlow RH. Mitochondria in Alzheimer’s disease and their potential role in Alzheimer’s proteostasis. Exp Neurol. 2020;330:113321. doi: 10.1016/j.expneurol.2020.113321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sędzikowska A, Szablewski L. Insulin and insulin resistance in Alzheimer’s disease. Int J Mol Sci. 2021;22:9987. doi: 10.3390/ijms22189987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dienel GA. Brain glucose metabolism: integration of energetics with function. Physiol Rev. 2019;99:949–1045. doi: 10.1152/physrev.00062.2017. [DOI] [PubMed] [Google Scholar]
- 27.Matioli MNPS, Nitrini R. Mechanisms linking brain insulin resistance to Alzheimer’s disease. Dement Neuropsychol. 2015;9:96–102. doi: 10.1590/1980-57642015DN92000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kumar V, Kim S-H, Bishayee K. Dysfunctional glucose metabolism in Alzheimer’s disease onset and potential pharmacological interventions. Int J Mol Sci. 2022;23:9540. doi: 10.3390/ijms23179540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Swerdlow RH. Mitochondria and mitochondrial cascades in Alzheimer’s disease. J Alzheimer's Dis. 2018;62:1403–1416. doi: 10.3233/JAD-170585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Trushina E, Trushin S, Hasan MF. Mitochondrial complex I as a therapeutic target for Alzheimer’s disease. Acta Pharm Sin B. 2022;12:483–495. doi: 10.1016/j.apsb.2021.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lv Z, Guo Y. Metformin and its benefits for various diseases. Front Endocrinol (Lausanne). 2020;11:191. 10.3389/fendo.2020.00191. [DOI] [PMC free article] [PubMed]
- 32.Wang Y, An H, Liu T, Qin C, Sesaki H, Guo S, Radovick S, Hussain M, Maheshwari A, Wondisford FE, O’Rourke B, He L. Metformin improves mitochondrial respiratory activity through activation of AMPK. Cell Rep. 2019;29:1511–1523.e5. doi: 10.1016/j.celrep.2019.09.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cao B, Rosenblat JD, Brietzke E, Park C, Lee Y, Musial N, Pan Z, Mansur RB, McIntyre RS. Comparative efficacy and acceptability of antidiabetic agents for Alzheimer’s disease and mild cognitive impairment: a systematic review and network meta-analysis. Diabetes Obes Metab. 2018;20:2467–2471. doi: 10.1111/dom.13373. [DOI] [PubMed] [Google Scholar]
- 34.Wu C, Ouk M, Wong YY, Anita NZ, Edwards JD, Yang P, Shah BR, Herrmann N, Lanctôt KL, Kapral MK, MacIntosh BJ, Rabin JS, Black SE, Swardfager W. Relationships between memory decline and the use of metformin or DPP4 inhibitors in people with type 2 diabetes with normal cognition or Alzheimer’s disease, and the role APOE carrier status. Alzheimers Dement. 2020;16:1663–1673. doi: 10.1002/alz.12161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Imfeld P, Bodmer M, Jick SS, Meier CR. Metformin, Other antidiabetic drugs, and risk of Alzheimer’s disease: a population-based case–control study. J Am Geriatr Soc. 2012;60:916–921. doi: 10.1111/j.1532-5415.2012.03916.x. [DOI] [PubMed] [Google Scholar]
- 36.Fato R, Bergamini C, Bortolus M, Maniero AL, Leoni S, Ohnishi T, Lenaz G. Differential effects of mitochondrial complex I inhibitors on production of reactive oxygen species. Biochim Biophys Acta - Bioenerg. 2009;1787:384–392. doi: 10.1016/j.bbabio.2008.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stojakovic A, Trushin S, Sheu A, Khalili L, Chang S-Y, Li X, Christensen T, Salisbury JL, Geroux RE, Gateno B, Flannery PJ, Dehankar M, Funk CC, Wilkins J, Stepanova A, O’Hagan T, Galkin A, Nesbitt J, Zhu X, Tripathi U, Macura S, Tchkonia T, Pirtskhalava T, Kirkland JL, Kudgus RA, Schoon RA, Reid JM, Yamazaki Y, Kanekiyo T, Zhang S, Nemutlu E, Dzeja P, Jaspersen A, Kwon YIC, Lee MK, Trushina E. Partial inhibition of mitochondrial complex I ameliorate Alzheimer’s disease pathology and cognition in APP/PS1 female mice. Commun Biol. 2021;4:61. doi: 10.1038/s42003-020-01584-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gao H, Tripathi U, Trushin S, Okromelidze L, Pichurin NP, Wei L, Zhuang Y, Wang L, Trushina E. A genome-wide association study in human lymphoblastoid cells supports safety of mitochondrial complex I inhibitor. Mitochondrion. 2021;58:83–94. doi: 10.1016/j.mito.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hong H, Rana S, Barrigan L, Shi A, Zhang Y, Zhou F, Jin L, Hua DH. Inhibition of Alzheimer’s amyloid toxicity with a tricyclic pyrone molecule in vitro and in vivo. J Neurochem. 2009;108:1097–1108. doi: 10.1111/j.1471-4159.2008.05866.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bao X, Liu X, Wu Q, Ye F, Shi Z, Xu D, et al. Mitochondrial-targeted antioxidant MitoQ-Mediated autophagy: A novel strategy for precise radiation protection. Antioxidants (Basel). 2023;12(2):453. 10.3390/antiox12020453. [DOI] [PMC free article] [PubMed]
- 41.Young ML, Franklin JL. The mitochondria-targeted antioxidant MitoQ inhibits memory loss, neuropathology, and extends lifespan in aged 3xTg-AD mice. Mol Cell Neurosci. 2019;101:103409. doi: 10.1016/j.mcn.2019.103409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rodriguez-Cuenca S, Cochemé HM, Logan A, Abakumova I, Prime TA, Rose C, Vidal-Puig A, Smith AC, Rubinsztein DC, Fearnley IM, Jones BA, Pope S, Heales SJR, Lam BYH, Neogi SG, McFarlane I, James AM, Smith RAJ, Murphy MP. Consequences of long-term oral administration of the mitochondria-targeted antioxidant MitoQ to wild-type mice. Free Radic Biol Med. 2010;48:161–172. doi: 10.1016/j.freeradbiomed.2009.10.039. [DOI] [PubMed] [Google Scholar]
- 43.McManus MJ, Murphy MP, Franklin JL. The mitochondria-targeted antioxidant MitoQ prevents loss of spatial memory retention and early neuropathology in a transgenic mouse model of Alzheimer’s disease. J Neurosci. 2011;31:15703–15715. doi: 10.1523/JNEUROSCI.0552-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.James AM, Cochemé HM, Murphy MP. Mitochondria-targeted redox probes as tools in the study of oxidative damage and aging. Mech Ageing Dev. 2005;126:982–986. doi: 10.1016/j.mad.2005.03.026. [DOI] [PubMed] [Google Scholar]
- 45.Gao C, Wang Y, Sun J, Han Y, Gong W, Li Y, Feng Y, Wang H, Yang M, Li Z, Yang Y, Gao C. Neuronal mitochondria-targeted delivery of curcumin by biomimetic engineered nanosystems in Alzheimer’s disease mice. Acta Biomater. 2020;108:285–299. doi: 10.1016/j.actbio.2020.03.029. [DOI] [PubMed] [Google Scholar]
- 46.Xia C-F, Arteaga J, Chen G, Gangadharmath U, Gomez LF, Kasi D, Lam C, Liang Q, Liu C, Mocharla VP, Mu F, Sinha A, Su H, Szardenings AK, Walsh JC, Wang E, Yu C, Zhang W, Zhao T, Kolb HC. [(18)F]T807, a novel tau positron emission tomography imaging agent for Alzheimer’s disease. Alzheimers Dement. 2013;9:666–676. doi: 10.1016/j.jalz.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 47.Chen M, Liu B, Ma J, Ge J, Wang K. Protective effect of mitochondria-targeted peptide MTP-131 against oxidative stress-induced apoptosis in RGC-5 cells. Mol Med Rep. 2017;15:2179–2185. doi: 10.3892/mmr.2017.6271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Obi C, Smith AT, Hughes GJ, Adeboye AA. Targeting mitochondrial dysfunction with elamipretide. Heart Fail Rev. 2022;27:1925–1932. doi: 10.1007/s10741-021-10199-2. [DOI] [PubMed] [Google Scholar]
- 49.Zhao W, Xu Z, Cao J, Fu Q, Wu Y, Zhang X, Long Y, Zhang X, Yang Y, Li Y, Mi W. Elamipretide (SS-31) improves mitochondrial dysfunction, synaptic and memory impairment induced by lipopolysaccharide in mice. J Neuroinflammation. 2019;16:230. doi: 10.1186/s12974-019-1627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ding X-W, Robinson M, Li R, Aldhowayan H, Geetha T, Babu JR. Mitochondrial dysfunction and beneficial effects of mitochondria-targeted small peptide SS-31 in diabetes mellitus and Alzheimer’s disease. Pharmacol Res. 2021;171:105783. doi: 10.1016/j.phrs.2021.105783. [DOI] [PubMed] [Google Scholar]
- 51.Isaev NK, Stelmashook EV, Genrikhs EE, Korshunova GA, Sumbatyan NV, Kapkaeva MR, Skulachev VP. Neuroprotective properties of mitochondria-targeted antioxidants of the SkQ-type. Rev Neurosci. 2016;27:849–855. doi: 10.1515/revneuro-2016-0036. [DOI] [PubMed] [Google Scholar]
- 52.Stefanova NA, Muraleva NA, Skulachev VP, Kolosova NG. Alzheimer’s disease-like pathology in senescence-accelerated OXYS rats can be partially retarded with mitochondria-targeted antioxidant SkQ1. J Alzheimer's Dis. 2013;38:681–694. doi: 10.3233/JAD-131034. [DOI] [PubMed] [Google Scholar]
- 53.Simoes Loureiro I, Lefebvre L. The SQK: a semantic knowledge questionnaire to specify the severity of semantic deterioration in Alzheimer’s disease patients. Geriatr Psychol Neuropsychiatr Vieil. 2015;13:225–33. doi: 10.1684/pnv.2015.0535. [DOI] [PubMed] [Google Scholar]
- 54.Langley M, Ghosh A, Charli A, Sarkar S, Ay M, Luo J, Zielonka J, Brenza T, Bennett B, Jin H, Ghaisas S, Schlichtmann B, Kim D, Anantharam V, Kanthasamy A, Narasimhan B, Kalyanaraman B, Kanthasamy AG. Mito-Apocynin prevents mitochondrial dysfunction, microglial activation, oxidative damage, and progressive neurodegeneration in MitoPark transgenic mice. Antioxid Redox Signal. 2017;27:1048–1066. doi: 10.1089/ars.2016.6905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ghosh A, Langley MR, Harischandra DS, Neal ML, Jin H, Anantharam V, Joseph J, Brenza T, Narasimhan B, Kanthasamy A, Kalyanaraman B, Kanthasamy AG. Mitoapocynin treatment protects against neuroinflammation and dopaminergic neurodegeneration in a preclinical animal model of Parkinson’s disease. J Neuroimmune Pharmacol. 2016;11:259–278. doi: 10.1007/s11481-016-9650-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Oliver DMA, Reddy PH. Small molecules as therapeutic drugs for Alzheimer’s disease. Mol Cell Neurosci. 2019;96:47–62. doi: 10.1016/j.mcn.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hu H, Li M. Mitochondria-targeted antioxidant mitotempo protects mitochondrial function against amyloid beta toxicity in primary cultured mouse neurons. Biochem Biophys Res Commun. 2016;478:174–180. doi: 10.1016/j.bbrc.2016.07.071. [DOI] [PubMed] [Google Scholar]
- 58.Liu X, Song L, Yu J, Huang F, Li Y, Ma C. Mdivi-1: a promising drug and its underlying mechanisms in the treatment of neurodegenerative diseases. Histol Histopathol. 2022;37:505–512. doi: 10.14670/HH-18-443. [DOI] [PubMed] [Google Scholar]
- 59.Oliver D, Reddy PH. Dynamics of dynamin-related protein 1 in Alzheimer's disease and other neurodegenerative diseases. Cells. 2019;8(9):961. 10.3390/cells8090961. [DOI] [PMC free article] [PubMed]
- 60.Bordt EA, Zhang N, Waddell J, Polster BM. The non-specific Drp1 inhibitor Mdivi-1 has modest biochemical antioxidant activity. Antioxidants. 2022;11:450. doi: 10.3390/antiox11030450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Baek SH, Park SJ, Jeong JI, Kim SH, Han J, Kyung JW, Baik S-H, Choi Y, Choi BY, Park JS, Bahn G, Shin JH, Jo DS, Lee J-Y, Jang C-G, Arumugam TV, Kim J, Han J-W, Koh J-Y, Cho D-H, Jo D-G. Inhibition of Drp1 ameliorates synaptic depression, Aβ deposition, and cognitive impairment in an Alzheimer’s disease model. J Neurosci. 2017;37:5099–5110. doi: 10.1523/JNEUROSCI.2385-16.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McGrath ER, Himali JJ, Xanthakis V, Duncan MS, Schaffer JE, Ory DS, Peterson LR, DeCarli C, Pase MP, Satizabal CL, Vasan RS, Beiser AS, Seshadri S. Circulating ceramide ratios and risk of vascular brain aging and dementia. Ann Clin Transl Neurol. 2020;7:160–168. doi: 10.1002/acn3.50973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Byeon SK, Madugundu AK, Jain AP, Bhat FA, Jung JH, Renuse S, Darrow J, Bakker A, Albert M, Moghekar A, Pandey A. Cerebrospinal fluid lipidomics for biomarkers of Alzheimer’s disease. Mol Omics. 2021;17:454–463. doi: 10.1039/D0MO00186D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Elsherbini A, Kirov AS, Dinkins MB, Wang G, Qin H, Zhu Z, Tripathi P, Crivelli SM, Bieberich E. Association of Aβ with ceramide-enriched astrosomes mediates Aβ neurotoxicity. Acta Neuropathol Commun. 2020;8:60. doi: 10.1186/s40478-020-00931-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jayashankar V, Selwan E, Hancock SE, Verlande A, Goodson MO, Eckenstein KH, et al. Drug-like sphingolipid SH-BC-893 opposes ceramide-induced mitochondrial fission and corrects diet-induced obesity. EMBO Mol Med. 2021;13(8):e13086. 10.15252/emmm.202013086. [DOI] [PMC free article] [PubMed]
- 66.Numadate A, Mita Y, Matsumoto Y, Fujii S, Hashimoto Y. Development of 2-thioxoquinazoline-4-one derivatives as dual and selective inhibitors of dynamin-related protein 1 (Drp1) and puromycin-sensitive aminopeptidase (PSA) Chem Pharm Bull (Tokyo) 2014;62:979–988. doi: 10.1248/cpb.c14-00333. [DOI] [PubMed] [Google Scholar]
- 67.Mallat A, Uchiyama LF, Lewis SC, Fredenburg RA, Terada Y, Ji N, Nunnari J, Tseng CC. Discovery and characterization of selective small molecule inhibitors of the mammalian mitochondrial division dynamin, DRP1. Biochem Biophys Res Commun. 2018;499:556–562. doi: 10.1016/j.bbrc.2018.03.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kuruva CS, Manczak M, Yin X, Ogunmokun G, Reddy AP, Reddy PH. Aqua-soluble DDQ reduces the levels of Drp1 and Aβ and inhibits abnormal interactions between Aβ and Drp1 and protects Alzheimer’s disease neurons from Aβ- and Drp1-induced mitochondrial and synaptic toxicities. Hum Mol Genet. 2017;26:3375–3395. doi: 10.1093/hmg/ddx226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Oblak AL, Cope ZA, Quinney SK, Pandey RS, Biesdorf C, Masters AR, Onos KD, Haynes L, Keezer KJ, Meyer JA, Peters JS, Persohn SA, Bedwell AA, Eldridge K, Speedy R, Little G, Williams S-P, Noarbe B, Obenaus A, Sasner M, Howell GR, Carter GW, Williams H, Lamb BT, Territo PR, Sukoff Rizzo SJ. Prophylactic evaluation of verubecestat on disease- and symptom-modifying effects in 5XFAD mice. Alzheimers Dement (N Y) 2022;8:e12317. doi: 10.1002/trc2.12317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Quan H, Koltai E, Suzuki K, Aguiar AS, Pinho R, Boldogh I, Berkes I, Radak Z. Exercise, redox system and neurodegenerative diseases. Biochim Biophys Acta - Mol Basis Dis. 2020;1866:165778. doi: 10.1016/j.bbadis.2020.165778. [DOI] [PubMed] [Google Scholar]
- 71.Castells-Sánchez A, Roig-Coll F, Dacosta-Aguayo R, Lamonja-Vicente N, Sawicka AK, Torán-Monserrat P, et al. Exercise and fitness neuroprotective effects: Molecular, brain volume and psychological correlates and their mediating role in healthy late-middle-aged women and men. Front Aging Neurosci. 2021;13:615247. 10.3389/fnagi.2021.615247. [DOI] [PMC free article] [PubMed]
- 72.Marques-Aleixo I, Beleza J, Sampaio A, Stevanović J, Coxito P, Gonçalves I, Ascensão A, Magalhães J. Preventive and therapeutic potential of physical exercise in neurodegenerative diseases. Antioxid Redox Signal. 2021;34:674–693. doi: 10.1089/ars.2020.8075. [DOI] [PubMed] [Google Scholar]
- 73.Valenzuela M, Sachdev P. Can cognitive exercise prevent the onset of dementia? Systematic review of randomized clinical trials with longitudinal follow-up. Am J Geriatric Psych. 2009;17:179–187. doi: 10.1097/JGP.0b013e3181953b57. [DOI] [PubMed] [Google Scholar]
- 74.López-Ortiz S, Pinto-Fraga J, Valenzuela PL, Martín-Hernández J, Seisdedos MM, García-López O, Toschi N, Di Giuliano F, Garaci F, Mercuri NB, Nisticò R, Emanuele E, Lista S, Lucia A, Santos-Lozano A. Physical exercise and Alzheimer’s disease: effects on pathophysiological molecular pathways of the disease. Int J Mol Sci. 2021;22:2897. doi: 10.3390/ijms22062897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Civelek M, Lusis AJ. Systems genetics approaches to understand complex traits. Nat Rev Genet. 2014;15:34–48. doi: 10.1038/nrg3575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Memme JM, Erlich AT, Phukan G, Hood DA. Exercise and mitochondrial health. J Physiol. 2021;599:803–817. doi: 10.1113/JP278853. [DOI] [PubMed] [Google Scholar]
- 77.Burtscher J, Burtscher M. Run for your life: tweaking the weekly physical activity volume for longevity. Br J Sports Med. 2020;54:759–760. doi: 10.1136/bjsports-2019-101350. [DOI] [PubMed] [Google Scholar]
- 78.Hoffmann K, Sobol NA, Frederiksen KS, Beyer N, Vogel A, Vestergaard K, Brændgaard H, Gottrup H, Lolk A, Wermuth L, Jacobsen S, Laugesen LP, Gergelyffy RG, Høgh P, Bjerregaard E, Andersen BB, Siersma V, Johannsen P, Cotman CW, Waldemar G, Hasselbalch SG. Moderate-to-high intensity physical exercise in patients with Alzheimer’s disease: a randomized controlled trial. J Alzheimer's Dis. 2016;50:443–453. doi: 10.3233/JAD-150817. [DOI] [PubMed] [Google Scholar]
- 79.Sobol NA, Dall CH, Høgh P, Hoffmann K, Frederiksen KS, Vogel A, Siersma V, Waldemar G, Hasselbalch SG, Beyer N. Change in fitness and the relation to change in cognition and neuropsychiatric symptoms after aerobic exercise in patients with mild Alzheimer’s disease. J Alzheimer's Dis. 2018;65:137–145. doi: 10.3233/JAD-180253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.de Farias JM, dos Santos Tramontin N, Pereira EV, de Moraes GL, Furtado BG, Tietbohl LTW, Da Costa Pereira B, Simon KU, Muller AP. Physical exercise training improves judgment and problem-solving and modulates serum biomarkers in patients with Alzheimer’s disease. Mol Neurobiol. 2021;58:4217–4225. doi: 10.1007/s12035-021-02411-z. [DOI] [PubMed] [Google Scholar]
- 81.Ngandu T, Lehtisalo J, Solomon A, Levälahti E, Ahtiluoto S, Antikainen R, Bäckman L, Hänninen T, Jula A, Laatikainen T, Lindström J, Mangialasche F, Paajanen T, Pajala S, Peltonen M, Rauramaa R, Stigsdotter-Neely A, Strandberg T, Tuomilehto J, Soininen H, Kivipelto M. A 2-year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet. 2015;385:2255–2263. doi: 10.1016/S0140-6736(15)60461-5. [DOI] [PubMed] [Google Scholar]
- 82.Brouwer-Brolsma EM, Benati A, van de Wiel A, van Lee L, de Vries JHM, Feskens EJM, van de Rest O. Higher Mediterranean diet scores are not cross-sectionally associated with better cognitive scores in 20- to 70-year-old Dutch adults: the NQplus study. Nutr Res. 2018;59:80–89. doi: 10.1016/j.nutres.2018.07.013. [DOI] [PubMed] [Google Scholar]
- 83.Gustafson DR, Bäckman K, Scarmeas N, Stern Y, Manly JJ, Mayeux R, Gu Y. Dietary fatty acids and risk of Alzheimer’s disease and related dementias: observations from the Washington Heights-Hamilton Heights-Inwood Columbia Aging Project (WHICAP) Alzheimers Dement. 2020;16:1638–1649. doi: 10.1002/alz.12154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Croteau E, Castellano C-A, Richard MA, Fortier M, Nugent S, Lepage M, Duchesne S, Whittingstall K, Turcotte ÉE, Bocti C, Fülöp T, Cunnane SC. Ketogenic medium chain triglycerides increase brain energy metabolism in Alzheimer’s disease. J Alzheimer's Dis. 2018;64:551–561. doi: 10.3233/JAD-180202. [DOI] [PubMed] [Google Scholar]
- 85.Müller T, Riederer P, Kuhn W. Aminoadamantanes: from treatment of Parkinson’s and Alzheimer’s disease to symptom amelioration of long COVID-19 syndrome? Expert Rev Clin Pharmacol. 2023;16:101–107. doi: 10.1080/17512433.2023.2176301. [DOI] [PubMed] [Google Scholar]
- 86.Singh R, Lakhanpal D, Kumar S, Sharma S, Kataria H, Kaur M, Kaur G. Late-onset intermittent fasting dietary restriction as a potential intervention to retard age-associated brain function impairments in male rats. Age (Omaha) 2012;34:917–933. doi: 10.1007/s11357-011-9289-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data is available on the request of the authors.