Abstract
Anxiety disorders constitute the largest group of mental disorders in most western societies and are a leading cause of disability. The essential features of anxiety disorders are excessive and enduring fear, anxiety or avoidance of perceived threats, and can also include panic attacks. Although the neurobiology of individual anxiety disorders is largely unknown, some generalizations have been identified for most disorders, such as alterations in the limbic system, dysfunction of the hypothalamic–pituitary–adrenal axis and genetic factors. In addition, general risk factors for anxiety disorders include female sex and a family history of anxiety, although disorder-specific risk factors have also been identified. The diagnostic criteria for anxiety disorders varies for the individual disorders, but are generally similar across the two most common classification systems: the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) and the International Classification of Diseases, Tenth Edition (ICD-10). Despite their public health significance, the vast majority of anxiety disorders remain undetected and untreated by health care systems, even in economically advanced countries. If untreated, these disorders are usually chronic with waxing and waning symptoms. Impairments associated with anxiety disorders range from limitations in role functioning to severe disabilities, such as the patient being unable to leave their home.
Anxiety disorders (FIG. 1), including separation anxiety disorder, selective mutism, specific phobia, social anxiety disorder, panic disorder, agoraphobia and generalized anxiety disorder, constitute the largest group of mental disorders in most western societies and are a leading cause of disability1–3. In 2010, >60 million Europeans had an anxiety disorder2, resulting in a total cost of >74 billion euros1, which was largely due to indirect costs such as disability. The essential features of anxiety disorders are excessive and enduring fear, anxiety and/or the avoidance of perceived threats either in the external (for example, social situations) or internal (for example, bodily sensations) environment. In addition, panic attacks can be a feature of anxiety disorders as a type of abrupt fear response. The avoidance behaviours that are features of some anxiety disorders can range from a refusal to enter certain situations to a subtle reliance on objects or people to cope.
Figure 1 |. Anxiety disorders.
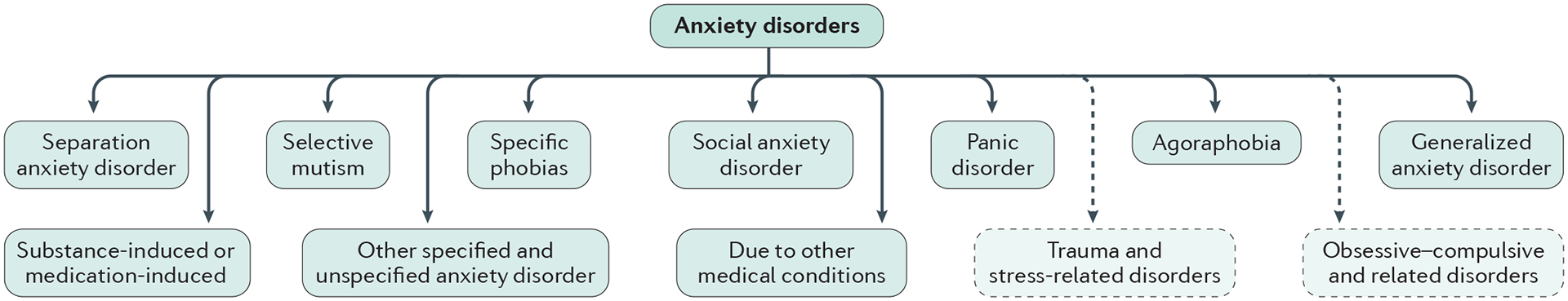
Several individual disorders can be classified under the broad heading of anxiety disorders. Although these disorders can present throughout life, some individual disorders have specific ages of onset. For example, most cases of separation anxiety and specific phobias develop in childhood, and most cases of social anxiety disorder develop in adolescence or early adulthood. In addition, the age at onset for panic disorder, agoraphobia and generalized anxiety disorder tends to vary but is typically early in adulthood, although generalized anxiety disorder can occur for the first time later in life4,19. Although previously listed under the anxiety disorder Diagnostic and Statistical Manual of Mental Disorders (DSM) classification, obsessive–compulsive disorder and post-traumatic stress disorder are no longer classified as such and are in separate categories in the DSM-5 (indicated by dashed arrows).
The onset of most anxiety disorders occurs during childhood, adolescence or early adulthood4. If untreated, anxiety disorders tend to be chronic with waxing and waning symptoms5, although symptom reduction might occur for ~40% of patients6,7. Anxiety disorders are often followed by depression and several other conditions, meaning that they can also be a risk marker for disease burden8.
The diagnostic criteria for anxiety disorders are similar across the two most common classification systems: the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)9 and the International Classification of Diseases, Tenth Edition (ICD-10)10. Anxiety disorders can also be conceptualized as dimensional, ranging from mild to severe. To illustrate, social anxiety covers mild social anxiety (for example, anxiety in performance situations that impairs functioning in work meetings), moderate social anxiety (for example, anxiety in several interactive and performance situations that impairs work performance and social relationships) and severe social anxiety (for example, anxiety in most social situations that results in job loss and social isolation).
Although post-traumatic stress disorder (PTSD) and obsessive–compulsive disorder (OCD) were historically included in the anxiety disorder category of the DSM, they were moved to adjoining chapters in the DSM-5. Given that both of these disorders were previously considered anxiety disorders, research pertaining to these conditions contributes to our understanding of anxiety disorders as a whole. Consequently, these disorders are occasionally referenced throughout this Primer.
This Primer discusses the epidemiology, diagnosis and management of anxiety disorders as a whole, referring to individual anxiety disorders where possible. In addition, this Primer describes the neurobiology of anxiety disorders and the techniques used to study these disorders in the laboratory and the clinic.
Epidemiology
Prevalence
According to the World Mental Health Survey11, approximately one in four individuals are likely to have, or have previously had, an anxiety disorder (note that these data include agoraphobia, generalized anxiety disorder, OCD, panic disorder, PTSD, social phobia and specific phobia). The lifetime prevalence estimate ranges from 4.8% in China to 31% in the United States. The global 12-month prevalence for anxiety disorders has been estimated to be ~14%12 (FIG. 2). Country-specific 12-month prevalence rates vary, ranging from 2.4% in Italy to 29.8% in Mexico. When these data are controlled for variations in characterization and methodology, the 12-month prevalence in the United States and European countries tends to be higher than other areas of the world12. Some data also indicate that low-income countries have a lower prevalence of anxiety disorders than high-income countries13.
Figure 2 |. Prevalence and sex ratio of anxiety disorders.
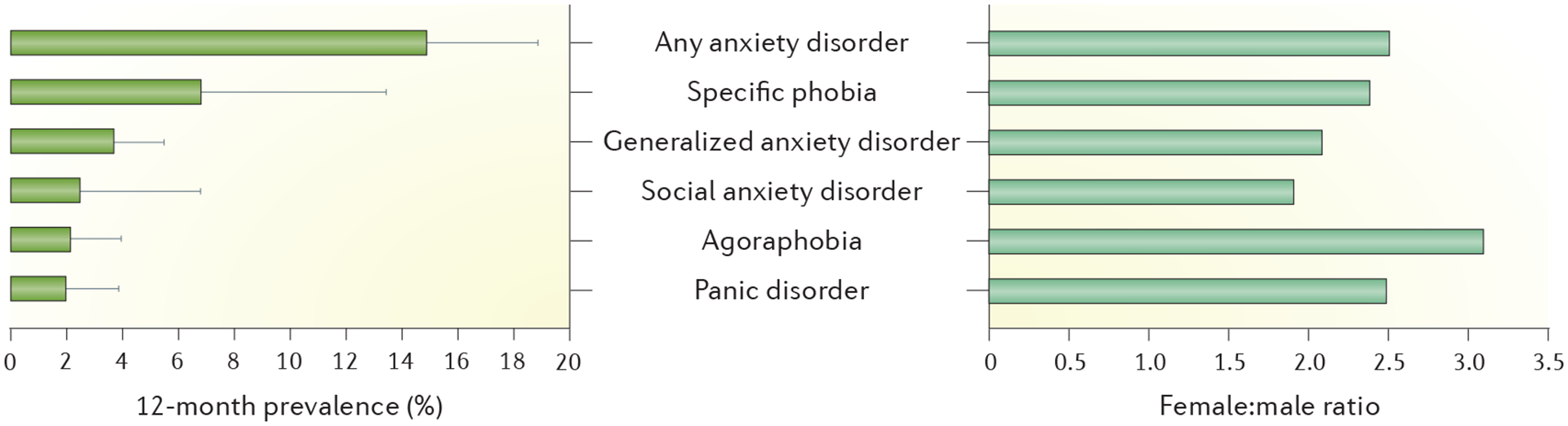
The 12-month prevalence estimate of anxiety disorders in 14 European countries is 14%, meaning that 61.5 million individuals in Europe alone have had an anxiety disorder in the past 12 months1. Within the anxiety disorders, the 12-month prevalence for specific phobia is higher than the other disorders. In general, anxiety disorders are at least twice as common in women as in men. Error bars represent the range in prevalence estimates across the 14 countries. Data from REF. 1.
Globally, the 12-month prevalence is slightly lower than the lifetime prevalence, indicating that anxiety disorders are relatively persistent. The projected lifetime risk of anxiety disorders is only slightly higher than the 12-month prevalence, indicating that these disorders typically occur early in life.
Most epidemiological studies have not yet used the diagnostic classification of the DSM-5; thus, estimates of the prevalence of separation anxiety disorder and selective mutism are lacking. However, on the basis of expert consensus, the 12-month prevalence estimates for separation anxiety disorder is 0.9–1.9% in adults and ~4% in children, and the prevalence of selective mutism is 0.03–1% in youths up to 18 years of age. The inclusion of these disorders in the prevalence of anxiety disorders as a whole is unlikely to substantially affect the overall estimate owing to the high rate of comorbidity across these disorders. That is, more than half of patients with an anxiety disorder have multiple anxiety disorders14. The effect of the changes in the DSM diagnostic criteria for anxiety disorders (from DSM-IV to DSM-5) on the prevalence of each disorder is unknown; however, the prevalence of anxiety disorders as a diagnostic group is likely to decrease with the exclusion of PTSD, and, to a lesser degree, OCD.
Age at onset
According to retrospective and prospective data in child and adolescent populations, most anxiety disorders start early in life, and the 12-month prevalence in childhood and adolescence is similar to that in adults5. Phobias and separation anxiety have a particularly early onset, with the highest incidence risk between 6 and 17 years of age11. Nonetheless, for some anxiety disorders, anxiety can emerge in adulthood and late in life (for example, generalized anxiety disorder)4,15–17.
Culture-specific anxiety disorders
Some culture-bound forms of anxiety have been identified18, but determining the extent to which these are unique categories or cultural variations of a common pathology is challenging. For example, taijin kyo-fusho is a disorder that is related to social anxiety in East Asian cultures, in which the core fear is of offending (or embarrassing) others (rather than themselves)13. Another example is ataques de nervios, a stress-induced panic attack-like syndrome described in Puerto Rican and Dominican cultures13.
Vulnerability and associated risk factors
Several vulnerability and risk factors promote the course from normal to dysfunctional anxiety. Some of these factors convey risk for developing any anxiety disorder, but others convey risk for certain disorders only. Vulnerability and risk factors for all anxiety disorders include female sex and a family history of anxiety or depressive disorders. For example, female sex almost doubles the risk for anxiety disorders (FIG. 2); sex differences are relatively small during childhood but develop throughout adolescence19,20. Children of individuals who have at least one anxiety disorder have a twofold to fourfold increased risk for anxiety disorders, which also develop significantly earlier in life than children of individuals without anxiety21. In addition, having parents with anxiety and depression amplifies this risk, particularly for panic disorder and generalized anxiety disorder, also revealing that parental depression is an independent risk factor for child anxiety21. The familial risk for anxiety disorders partially reflects a heritable component22; however, specific and replicable genetic risk loci have yet to be determined (see below)23.
PTSD and, to a lesser degree, other anxiety disorders have been consistently associated with adverse childhood experiences, including but not limited to physical and sexual abuse24,25, parental separation26 and emotional maltreatment27. Most of these studies are limited by the reporting of adverse childhood experiences at the same time as diagnosis, usually in adulthood. Nonetheless, early-life adversity can predict the subsequent development of anxiety disorders in longitudinal studies; for example, more childhood and adolescent major adversities reported at ~17 years of age predicted the subsequent onset of anxiety disorders over the next several years28.
Early-life risk factors for anxiety disorders include specific temperamental vulnerabilities (especially withdrawn or inhibited temperaments)29, parent interactions that are characterized by over-involvement and negativity30, and reduced peer relationships31. In addition, episodic life stressors (such as financial strain, family illness and divorce) in young adults can predict subsequent anxiety symptoms and diagnoses32,33. Extant data have not compared the role of stress across different anxiety disorders.
Prospective longitudinal evidence suggests that all anxiety disorders, but particularly panic disorder, agoraphobia and social anxiety disorder, are powerful risk factors for the development of depressive disorders and substance abuse34. The presence of these disorders in childhood, adolescence or early adulthood increases the risk of depressive disorders and the probability of a more severe course of depression (for example, with chronicity or suicide attempts). For example, social anxiety disorder confers a relative risk of 1.49–1.85 for depression when the data are controlled for age and sex35,36. The predictive relationship between anxiety and subsequent substance abuse is smaller and seems to be confined to panic disorder and social anxiety disorder37.
Smoking and alcohol abuse are also risk factors for anxiety disorders in the sense that they are associated epidemiologically; however, the associations are bidirectional and causality is unproved38.
Mechanisms/pathophysiology
Neural circuitry
Neural systems model.
Anxiety disorders are a diverse group of conditions, and the current understanding of the neuropathophysiological mechanisms underlying the pathological forms of anxiety reflects this heterogeneity. However, certain generalities have emerged regarding the neurobiology of fear and anxiety. These generalities have been gained through a large body of work investigating the processing of negative emotions using different tasks in humans39–41 and the use of Pavlovian ‘fear/threat’ learning procedures in humans and rodents28,29 (BOX 1). Several brain regions have been implicated in the modulation of anxiety-relevant outputs and responses to threat, including the (extended) amygdala, hippocampus and medial prefrontal cortex (including the ventromedial prefrontal and anterior cingulate cortices). The hypothalamus, mid-brain (for example, the raphe nuclei) and brainstem (for example, the periaqueductal grey) are also implicated in anxiety disorders. Overall, these data have led to an influential neural systems model involving amygdala-driven fear and anxiety (FIG. 3). Currently, the functional neuroimaging literature is not at a point that permits systematic distinctions to be made between individual anxiety disorders based on differing profiles of neural abnormalities in these regions. However, neural patterns have been associated with states of fear versus anxiety as key clinical features of anxiety disorders. The distinction between fear-specific and anxiety-specific responses is most commonly based on the imminence of threat and the duration of responses. For example, fear responses are typically due to a clearly perceived and imminent threat, which triggers an immediate fight-or-flight response and usually subsides once the fear-inducing cue is removed. By contrast, anxiety-specific responses are typically due to distal or uncertain threat cues and tend to last longer than fear-based responses. In addition, further research of the neural regions proposes mechanisms that explain the subjective experience of fear within the fear/threat neural system42.
Box 1 |. Tools to investigate the neurobiology of anxiety and fear.
Many of the studies investigating the processing of negative emotions and emotional conflict have presented participants with stimuli of negative affect, such as the International Affective Picture System (IAPS), a standardized set of pictures used to study emotion, or rating of human faces based on their emotional expressions39,41. Other studies have focused on Pavlovian fear conditioning (that is, when a neutral stimulus is paired with a noxious stimulus, eventually resulting in the initiation of a conditional fear response to the neutral stimulus) and extinction paradigms (that is, loss of a conditional fear response after repeated occasions when the neutral stimulus is presented in the absence of the noxious stimulus); generalization of fear acquisition and deficits in fear extinction are considered to be central to the onset and maintenance of anxiety disorders209,210. Alternatively, the mechanisms of blocking the reconsolidation of conditioned fear in both rodents and humans, as a means of erasing fear memories, have been analysed40,211.
Figure 3 |. Key brain regions involved in the generation and regulation of emotions and threat detection.
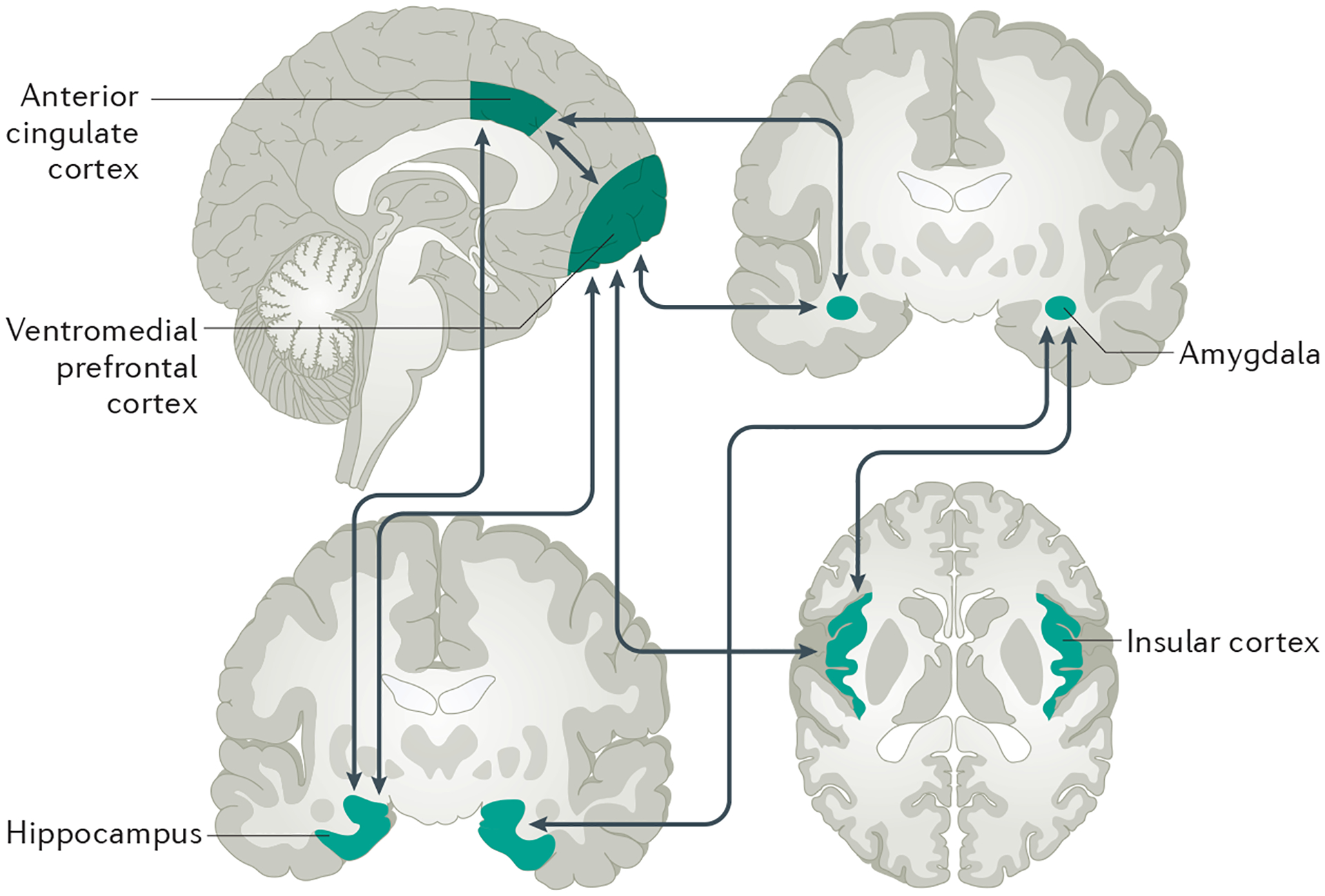
In this model, amygdala-driven fear and anxiety are regulated through bidirectional connections to the ventromedial prefrontal cortex (vmPFC) and the anterior cingulate cortex (ACC), along with functional crosstalk between these regions and the hippocampus76,217,218. This model translates across species and fits well with observations in patients. For example, differences in the degree and coordination of amygdala, vmPFC and hippocampus activity correlate with how well mice, rats or humans can suppress anxiety, extinguish fear and avoid cognitive bias to potential threat217,219,220. Notably, consistent with the crucial contribution of the amygdala to the formation and expression of conditioned fear memories in rodents217,219,220, amygdala hyperactivation along with diminished vmPFC activity to threat cues have repeatedly been found in patients, albeit mainly patients with post-traumatic stress disorder (PTSD)221 and with exceptions in certain symptomatically distinct populations222. In addition, functional connectivity between the amygdala, hippocampus and vmPFC, and the dorsal ACC and anterior insula is deficient in PTSD39,40,223,224. Interestingly, normalization of these disturbances parallels the symptom attenuation observed with cognitive–behavioural therapy in social anxiety disorder225,226.
On the one hand, the identification of brain regions involved in the processing of fear and anxiety suggests a substantial overlap in the neural correlates underlying the key clinical features of anxiety disorders43,44. Such observations have increased interest in exploring the neurobiology of anxiety disorders using dimensional approaches that span diagnostic criteria; for example, the Research Domain Criteria approach45 (BOX 2). On the other hand, different clusters of symptoms clearly distinguish one anxiety disorder from another in the DSM46. Learning how these differences in diagnostic symptoms map to differences in the underlying brain mechanisms and pathologies is an important goal. Research using rats and mice has revealed partially dissociable neural circuits associated with, for example, footshock-conditioned fear, fear of predators and induced panic-like states47,48.
Box 2 |. Research Domain Criteria.
The Research Domain Criteria (RDoC) is an initiative from the US National Institutes of Mental Health that aims to understand the full range of human behaviour, including behaviours found in healthy individuals and those with mental health disorders. The RDoC proposes a set of five domains for studying psychopathology: negative valence systems (that is, systems controlling responses to aversive situations); positive valence systems (that is, systems controlling responses to positive situations); cognitive systems; systems for social processes; and arousal or regulatory systems212,213. The RDoC drives a units-of-analysis approach to the study of psychopathology, including behavioural neuroscience, clinically relevant variation, genetic, molecular and cellular factors.
One goal is to translate the understanding of the neural substrates of anxiety into clinically tractable biomarkers for predicting risk for anxiety disorders49. Growing evidence suggests that the aforementioned neural systems are functionally compromised (that is, they are over-activated (for example, the amygdala) or under-activated (for example, parts of the ventromedial prefrontal cortex)) by exposure to childhood adversity50,51. These findings raise the possibility that measurable aberrations in these systems might predict the later presence of a disorder. Interestingly, enhanced amygdala activation in response to a threat was shown to predict risk for anxiety (and depression) in subsequent years in one study52. Whether anatomical variations (for example, the size or thickness of these regions) that are functionally implicated in anxiety disorders can provide a reliable correlate of disease risk is unclear53,54.
Hypothalamic–pituitary–adrenal axis.
Another approach to identify biomarkers of anxiety disorders is via blood-based markers that reflect dysfunction in the hypothalamic–pituitary–adrenal (HPA) axis, as well as the peripheral immune system55. Reduced circulating cortisol levels and glucocorticoid hypersensitivity have been noted in PTSD56, which links with genetic studies that have associated variations in glucocorticoid-related genes (such as FKBP5) with PTSD risk57. The preclinical literature has also demonstrated that the HPA axis is hyperactivated in a wide range of models of stress and anxiety58. In turn, these findings connect back to the cortical and limbic disturbances found in anxiety disorders by showing, for example, that glucocorticoids are crucial mediators of functional and anatomical abnormalities in these brain systems (acting through glucocorticoid and mineralocorticoid receptors)59. However, a relationship between the HPA axis and anxiety is not found in all studies of PTSD, and might be even less robust in studies of other anxiety disorders56,60. The reasons for this variability are yet to be fully understood, but seem to stem from differences in the developmental time course of the disorder, the chronicity of trauma exposure and sex differences.
Genetics
Genetic factors.
Anxiety disorders have a strong heritable basis; most disorders have heritability estimates of between 30% and 40%, largely based on data from studies investigating twins22,61,62. However, as is the case for other neuropsychiatric diseases, the specific genetic risk loci and mechanisms of familial transmission have yet to be reliably established23. Data from twin studies indicate a considerable genetic overlap between the different anxiety disorders and their associated symptoms in adults63, children and adolescents64. In addition, this genetic overlap extends to include depression in adults63 and children64. Data from twins also provide some evidence that genetic influences on individual anxiety disorders are not entirely shared, involving some specificity, particularly regarding the distinction between disorders characterized by fear (for example, phobias) versus disorders characterized by negative affect (for example, generalized anxiety disorder)65, although this distinction might only apply from young adulthood64. Overall, the expectation is that most genetic variants associated with anxiety disorders will contribute to a general anxiety-related risk, but that in addition, some genetic variants will be disorder specific.
Collaborative studies have pointed to several candidate genes (for example, CRHR1 (encoding corticotropin-releasing factor receptor 1)66 and COMT (encoding catechol-O-methyltransferase))67 as risk factors for panic disorder, although replication is needed. However, in general, the field of psychiatric genetics has concluded that exploring individual candidate genes leads over-whelmingly to false positives. Genome-wide association studies (GWAS) are considered more ‘hypothesis neutral’ than the candidate gene approach. Indeed, GWAS are beginning to identify23 and, in some cases, replicate genetic risk markers for anxiety disorders and anxiety-related traits such as neuroticism68, albeit largely for genes with a poorly understood function in the brain. However, sample size should ideally be in the tens of thousands to identify genetic variants that can account for a reasonable proportion of the variance in psychiatric disorders. Once they are identified, variants can be combined into a polygenic risk score (that is, a quantitative metric capturing all relevant genetic variance)69. Although the initial work to generate robust polygenic scores will require large sample sizes, subsequent studies to test whether these scores can predict a significant proportion of variance in the same or a related phenotype can be performed in smaller samples70. Encouragingly, several initiatives, including various national BioBank repositories, are now under way that will produce the large sample sizes required to enable the detection of anxiety-associated genetic variants. Emerging findings from large-scale GWAS in disorders that are frequently comorbid with anxiety, notably depression, are also likely to inform our understanding of the genetic factors moderating anxiety.
An important complement to bridging the link between genetics and anxiety is to identify genetic influences at the neural systems level, including genes implicated in the activity and interconnectivity of brain regions that are affected in anxiety49. This approach has been valuable for understanding how certain genes might confer a greater risk for anxiety disorders by altering ways in which threat is processed in regions such as the ventromedial prefrontal cortex and amygdala. For example, FKBP5, which encodes a glucocorticoid receptor regulating molecule71, FAAH, which encodes the endocannabinoid degrading enzyme72, and PACAP (also known as ADCYAP1)73 have been associated with increased amygdala reactivity and reduced amygdala coupling to other regions such as the hippocampus. Taken together with large-scale GWAS, these more mechanistically focused analyses should identify the neurobiological substrates mediating the genetic moderation of anxiety disorders. Nonetheless, we remain far from a time when a person can be screened for ‘the anxiety genes’, and whether such a time will ever exist is questionable owing to the polygenic and multifactorial nature of these conditions.
Gene–environment interactions.
Genetic risk (and resilience) factors can exert a moderating influence on anxiety in the context of the environment74,75. These clinical observations are in agreement with work from animal models investigating the effect of stress in adulthood and early life on the brain and neural circuits thought to promote anxiety76–78.
The interplay between genes and the environment can take several forms. Data from twin studies indicate that almost all types of environmental stress, such as parenting and negative life events, are partially genetically influenced79 (that is, gene–environment correlation). In turn, genetic influences on the environment overlap with those on anxiety80, indicating a shared vulnerability that might be mediated by factors such as cognitive biases (that is, a style of attending to and/or interpreting events in an overly threat-related manner), which also overlap genetically with anxiety81. Further illustrating the complexity of gene–environment correlations, parental mental health and aspects of parenting style (such as over-control and/or negativity), are both associated with, and share genetic influence with, child anxiety82, suggesting that their co-occurrence might arise from this shared genetic vulnerability. Thus, the association between such parental factors and child anxiety might not be causal, as was initially assumed, but might reflect either shared genetic influences affecting both parental traits and child anxiety or, in some instances, might indicate that child anxiety elicits certain parenting behaviours. However, twin studies have indicated that the association between anxiety in parent and anxiety in child holds even when genetic transmission has been controlled for, indicating a partial environmental mechanism underlying the association83.
Fewer studies investigating gene–environment interactions have been conducted in anxiety disorders than in other psychiatric disorders, and results are somewhat mixed. Data from a twin study found no interaction with respect to the diathesis–stress hypothesis (that is, the idea that anxiety manifests as a function of interaction between predisposing vulnerabilities, including genetic factors, and stressful life events) for three phobias (agoraphobia, social phobia and specific phobia)84. Similarly, a twin study investigating general anxiety, panic disorder, social anxiety and separation anxiety disorder symptoms in children and adolescents produced only very modest evidence for genetic effects varying as a function of the level of negative life events85. Specifically, although genetic effects on separation anxiety symptoms increased at ~8 years of age and panic symptoms at ~15 years of age, no interactions were observed at other ages or at any age for general anxiety or social anxiety.
Gene–environment interactions in anxiety have been explored far more often using the candidate gene approach. The most widely examined genetic variant is the 5-HTTLPR polymorphism of SLC6A4 (which encodes the serotonin transporter), a functional marker with two variants associated with different levels of serotonin transcription. The 5-HTTLPR polymorphism is associated with anxiety-related traits86 and interacts with maltreatment and other negative life events to increase the risk of depression87. In addition, 5-HTTLPR interacts with maltreatment to yield higher anxiety sensitivity (that is, belief that symptoms of anxiety are harmful), which is associated with increased risk for anxiety disorders88. These observations aligned well with preclinical studies using rats and mice with a loss-of-function mutation in Slc6a4; these rodents exhibited increased levels of anxiety-like behaviour and stress reactivity89,90. However, the 5-HTTLPR–environment interaction is controversial; conflicting data have been reported in meta-analyses91,92, which is reflective of data from the candidate gene approach that is more widely used in psychiatric genetics. The reasons for the inconsistency still need to be understood and probably involve numerous interacting factors and study variables that are not always clear or well controlled93.
The field broadly agrees with the greater use of genome-wide methods and large clinical populations to identify genetic influences not just on the development of anxiety but also on response to psychological treatment94. In one study, a genome-wide polygenic score was created consisting of hundreds of genetic variants reflecting differential emotional responsivity to the environment, which interacted with negative parenting to produce higher rates of anxiety-related symptoms in an independent sample. Furthermore, children with high polygenic scores for environmental responsivity benefited more than those with low polygenic scores from individual (but not parent-led) cognitive–behavioural therapy (CBT)94,95. Thus, taking into account environmental interactions when exploring the role of genetic factors on anxiety disorders is essential both for understanding the complex interplay between different types of risk and for better understanding responses to environmentally mediated interventions such as psychological therapies.
Another avenue of research is delineation of the biological processes by which the environment can reshape gene expression, through epigenetic mechanisms, to alter brain functions, behaviour and risk for anxiety disorders. For example, growing evidence suggests that stress is transmitted over time and across generations through epigenetic processes (or ‘marks’)96,97. Candidates for specific genes that might be subject to epigenetic changes with stress include NR3C1 (which encodes the glucocorticoid receptor) and other genes that regulate glucocorticoid function (such as FKBP5)57,98.
Sex differences
Sex and gender differences in the neurobiology of fear have been identified, which have substantial implications for anxiety disorders99. Although women are twice as likely to have an anxiety disorder, the reasons for this increased risk are unclear100,101. Emerging evidence suggests that men and women differ in how they form conditional fear memories and extinguish fear memories102. In addition, gonadal hormones, such as oestrogens, can influence neurogenesis, synaptic plasticity and the expression of receptors that are key substrates for learning and memory100. For example, oestrogen receptors are expressed in key nodes of the fear network, including the medial prefrontal cortex, hippocampus and amygdala, and their expression fluctuates across the oestrous cycle in the female rat103. Increased oestrogen levels during extinction learning significantly enhance the recall of extinction memory when tested at 24 hours in the majority of studies conducted in female rodents and in women104. This enhanced extinction recall in women correlated with increased activation within the ventromedial prefrontal cortex, hippocampus and amygdala105. Data are not available to link alterations in gonadal hormones between men and women to differences in symptom duration or expression, or to the epidemiological differences. However, alterations in oestrogens in women with PTSD are associated with fear extinction deficits, which could contribute to more persistent anxiety disorders106–108. This topic is clearly a crucial area of future research, as the neurobiology underlying sex differences could explain epidemiological findings and could also inform the development of sex-specific treatments.
Diagnosis, screening and prevention
Clinical diagnosis
The spectrum of anxiety disorders is marked by different clinical presentations, which means that the diagnostic criteria for individual disorders can vary. Although the specific criteria for individual anxiety disorders are highly detailed, BOX 3 presents some of the major diagnostic features of some disorders specified by the DSM-5 and the ICD-10.
Box 3 |. Major diagnostic features of anxiety disorders.
The major diagnostic criteria for anxiety disorders according to the two most common classification systems, the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) and the International Classification of Diseases, Tenth Edition (ICD-10) are summarized below. An asterisk denotes features stated in the DSM-5, and a double-dagger symbol denotes features stated in the ICD-10.
Separation anxiety disorder
Marked fear or anxiety about separation from attachment figures (such as family members) to a degree that is developmentally inappropriate
Persistent fear or anxiety about harm coming to attachment figures and events that could lead to loss or separation from them
Reluctance to leave attachment figures
Nightmares and physical symptoms of distress, such as stomach aches
Symptoms usually develop throughout childhood but can also develop throughout adulthood*
Diagnosis requires a 4-week duration in childhood, and a longer duration, typically of at least 6 months, in adulthood*
Selective (elective) mutism
Consistent failure to speak in particular social situations (for example, school) in which an expectation to speak exists, despite speaking in other situations
Not limited to interaction with adults
Not explained by absence of familiarity with the spoken language
Persists for at least 1 month (beyond the first month of school)*
Specific phobias
Marked fear, anxiety or avoidance of circumscribed objects or situations
Fear is out of proportion to the actual threat posed*
The individual recognizes that the symptoms are excessive or unreasonable‡
Typically persists for at least 6 months*
Subtypes include animal, natural environment (for example, heights or storms), blood–injection–injury (for example, needles), situational (for example, aeroplanes) or other phobias
Social anxiety disorder
Marked fear, anxiety or avoidance of social interactions and situations in which one is scrutinized, or situations in which one is the focus of attention (such as being observed while speaking, eating or performing)
Fear of negative judgment from others, in particular, fear of being embarrassed, humiliated, rejected or of offending others
Fear is out of proportion to the actual threat posed*
The individual recognizes that the symptoms are excessive or unreasonable‡
Physical symptoms and symptoms of blushing, fear of vomiting, or urgency or fear of micturition or defaecation‡
Typically persists for at least 6 months*
Social anxiety can be limited to performance situations only
Panic disorder
Recurrent unexpected (for example, occur without an apparent cue) panic attacks
Concern or worry about having more panic attacks or maladaptive behavioural changes*
Persists for at least 1 month*
Agoraphobia
Marked fear, anxiety or avoidance of situations such as public transportation, open spaces, enclosed places, lines or crowds, or outside the home alone
Fears that escape might be difficult or help is not available in the event of panic-like symptoms or other incapacitating or embarrassing symptoms*
Fear is out of proportion to the actual threat posed*
Individual recognizes the symptoms are excessive or unreasonable‡
Typically persists for at least 6 months*
Generalized anxiety disorder
Anxiety and worry, more days than not, about various domains, such as work and school performance, that are difficult to control
Physical symptoms of tension, such as restlessness, being keyed up or on edge, easily fatigued, difficulty concentrating, muscle tensions and sleep disturbance
Symptoms of autonomic arousal (such as hyperventilation and tachycardia)‡
Typically persists for at least 6 months*
In research settings, the diagnosis of anxiety disorders in adults is ascertained from structured clinical interviews that have an established reliability and validity. Examples of such surveys include the Structured Clinical Interview for DSM-5 (SCID-5)109, the MINI-International Neuropsychiatric Interview110 and the World Health Organization Composite International Diagnostic Interview (CIDI)111, supplemented by dimensional ratings scales to characterize the severity of symptoms or of diagnoses. In children, diagnosis also requires systematic clinical interviews with parents or caregivers and sometimes teachers112. However, these standards are rarely used in clinical practice113,114, which has been attributed to a lack of clinician training, limited time and emphasis on the physical aspects of the presentation115. In addition, mental health clinicians do not systematically apply diagnostic criteria for mental health disorders116. The reasons for this are not clearly understood, and more research is needed to identify ways in which diagnoses are established without reliance on diagnostic criteria; one possibility is that clinicians match an individual’s presentation with their own internalized prototypes for disorders116.
The underuse of the diagnostic criteria for anxiety disorder probably contributes to the high rates of misdiagnosis in clinical practice settings, particularly in primary care settings where individuals with anxiety disorders (at least those in developed countries) are likely to seek care117,118. For example, in primary care settings in Canada, clinicians’ rates of misdiagnosis were ~86% for panic disorder, 71% for generalized anxiety disorder and 98% for social anxiety disorder115. Several factors can hinder the diagnosis of anxiety disorders (BOX 4).
Box 4 |. Factors that can hinder diagnosis.
Multiple factors can hinder or delay the diagnosis of anxiety disorders. Misdiagnosis might occur owing to clinicians frequently not taking anxiety disorders as serious disorders that deserve attention, and patients sometimes presenting with unspecified somatic symptoms (for example, sleep problems and pain) or complications of anxiety (for example, depression)214. In addition, as the diagnosis of anxiety disorders rests almost entirely on the patient describing their symptoms and concerns to the clinician, any neurocognitive disorders that impair the individual’s ability to communicate will make diagnosis difficult. Shame, guilt or concerns about stigmatization might also lessen the likelihood of accurate reporting and thereby hinder diagnosis. Similarly, particular cultural beliefs or cultural expressions of anxiety might render diagnosis difficult215; consequently, cultural competency on the part of the assessing clinician is strongly encouraged. The diagnosis of anxiety disorders in children might be particularly difficult as they might present with avoidance or somatic complaints (for example, abdominal pain) without the developmental capacity to explain the cognitions underlying their behaviours. For younger children or children with poor communication, relying on parents and third parties (for example, teachers) for diagnosis is common.
Differential diagnosis
The differential diagnosis of anxiety disorders involves distinguishing anxiety disorders from other psychiatric disorders and from other medical conditions. Determining the diagnosis of a specific anxiety disorder and distinguishing it from other psychiatric disorders are achieved by interviewing the patient using DSM-5 or ICD-10 criteria. This process includes enquiring about the features of the patient’s anxiety symptoms and the situations in which these symptoms occur (for example, whether the symptoms are episodic or chronic, or if they occur unexpectedly or in certain situations). Enquiring about the thoughts and beliefs that accompany the anxiety is also necessary, as such queries can help to elucidate a specific anxiety disorder (for example, concerns about being embarrassed when around others might signify social anxiety disorder, but myriad and changing worries might signify generalized anxiety disorder). Determining whether the anxiety symptoms (for example, panic attacks) are occurring as a manifestation of another mental disorder (such as major depression or bipolar disorder) is also important. However, the presence of more than one psychiatric disorder in an individual (for example, major depression and social anxiety disorder) is very common; thus, it is often less a matter of achieving differential diagnosis than it is assigning a multiplicity of diagnoses and prioritizing their management for the individual patient.
Differentiating anxiety from other medical or physical causes is vital. Drug intoxication (for example, the use of stimulants) and withdrawal (for example, from alcohol use) can cause prominent anxiety symptoms. For substance-induced or medication-induced anxiety disorders, panic attacks or anxiety are prominent and develop soon after substance intoxication or withdrawal (or in the case of medication-induced anxiety, after exposure to a medication). In addition, the substance or medication can produce the anxiety symptoms that cannot be better explained by another anxiety disorder and do not occur only during delirium (that is, confusion)9.
As previously mentioned, PTSD and OCD were previously grouped as anxiety disorders in the DSM-IV but are now grouped in adjacent chapters in the DSM-5 to reflect their close but distinct relationships with anxiety disorders. In addition, the DSM-5 includes illness anxiety disorder (which is the DSM-5 successor to hypochondriasis in DSM-IV, albeit with some changes to the criteria) as part of the ‘Somatic symptom and related disorders’ category, not under the ‘Anxiety disorders’ category.
In the DSM-5, anxiety disorders associated with another medical condition can involve prominent panic attacks or anxiety. These symptoms are due to the direct pathophysiological consequence of a medical condition, are not better explained by another condition and do not occur only during delirium. Disorders that can present with prominent anxiety symptoms include cardiopulmonary (for example, asthma), endocrine (for example, thyroid disease) and neurological (for example, complex partial seizures) disorders, among others. Differential diagnosis is achieved through a detailed medical history and physical examination and, when warranted, specific blood (for example, thyroid-stimulating hormone levels) or other tests (for example, electrocardiograph or electroencephalogram)119 (TABLE 1).
Table 1 |.
Differential diagnosis
| Diagnosis | Signs and symptoms | Recommended test or evaluation |
|---|---|---|
| Alcohol and other substance use disorders | Anxiety, tremor, sweating, palpitations during intoxication (for example, with methamphetamine), withdrawal (for example, from alcohol) and panic attacks (with marijuana use) |
|
| Caffeine and other stimulant use (for example, ephedrine and pseudoephedrine) | Panic attacks or chronic anxiety, insomnia, palpitations and tremor* |
|
| Hyperthyroidism | Heat intolerance, weight loss, tremor, palpitations, ocular signs (with Graves disease, an autoimmune cause of hyperthyroidism), panic attacks or persistent anxiety |
|
| Adrenal medullary tumours (pheochromocytoma) | Diaphoresis, headaches, palpitations, hypertension and panic attacks |
|
| Cardiac disease (for example, angina, myocardial infarction or arrhythmia) | Palpitations or chest pain |
|
| Mitral valve prolapse | Palpitations |
|
| Respiratory disease (such as asthma or chronic obstructive pulmonary disease) | Shortness of breath and ‘air hunger’ (might be symptoms of panic attacks)‡ |
|
| Epilepsy (complex partial seizures) | Anxiety and other emotional symptoms in addition to changes in awareness§ |
|
Patients prone to anxiety may be more sensitive to caffeine and other stimulants.
Asthma or chronic obstructive pulmonary disease may co-occur with an anxiety disorder.
Anxiety and other emotional symptoms may occur as part of the aura or as the initial manifestation of seizures.
Imaging, histology and biomarkers
Currently, neither radiographic imaging nor brain histology has a role in the diagnosis of anxiety disorders, other than for exclusionary purposes. For example, the onset of obsessive–compulsive symptoms in a previously mentally healthy 45-year-old man would necessitate a thorough medical work-up, possibly including CT or MRI of the brain to rule out a lesion (for example, a tumour) causing these symptoms. Although structural (for example, voxel-based morphometric) and functional MRI have been used to learn more about the pathophysiology of anxiety disorders, they are not currently useful for diagnostic purposes120.
The search for biomarkers of anxiety disorders is under way. Genetic and epigenetic markers have been discussed elsewhere in this Primer. Blood tests (for example, levels of cortisol, neuropeptide Y or other substances) have not yet yielded sufficient sensitivity or specificity to be useful as biomarkers. Psychophysiological testing involving measurement of cardiorespiratory (for example, heart rate or vagal tone) and electrophysiological (for example, electroencephalogram activity such as evoked potentials) parameters have also been evaluated. However, although subtle differences between individuals with and without anxiety disorders are often seen at the group level, psychophysiological testing has so far proved limited for individual diagnostic purposes. Another reason for the failure of these measures to be useful diagnostically (or prognostically) to date might be that dysfunction resides more at a cognitive (belief) level than at a physiological (fight or flight) level42.
Screening
Nonspecific screening for anxiety disorder in adults can be accomplished using the Generalized Anxiety Disorder-7 (GAD-7), a 7-item self-report questionnaire121 that was originally written in English but has now been translated into several different languages. The GAD-7 can identify generalized anxiety disorder122, but might identify any anxiety disorder with adequate sensitivity and specificity, although further research is needed. Other screening tools include the Hospital Anxiety and Depression Scale123 and the Overall Anxiety Severity and Impairment Scale (OASIS)124.
Anxiety disorders in children and adolescents can be screened using the child and parent versions of the Screen for Child Anxiety Related Disorders (SCARED)125 or the revised SCARED126 self-report questionnaires, which measure symptoms of panic disorder, generalized anxiety disorder, separation anxiety disorder, social phobia and school anxiety (or school refusal). The SCARED has a strong sensitivity and specificity for anxiety disorders and has been translated into several different languages. In addition, the child (for individuals 8–15 years of age) and parent versions of the Spence Children’s Anxiety Scale127 can be used to screen for anxiety disorders and have been translated into many languages128. Given that anxiety is a universal phenomenon, it is unsurprising that most of these screening instruments have been implemented across many cultures. The Preschool Anxiety Scale (Revised) can be used to identify anxiety in children 3–6 years of age129. This scale is completed by the parents and describes four core anxiety types: separation anxiety, social anxiety, generalized anxiety and specific fears.
Prevention
Prevention of anxiety disorders has lagged behind the prevention of other conditions, such as depression, perhaps partly owing to the chronic nature of this condition. Nonetheless, universal, indicated and selective interventions have been evaluated130. Given the early age of onset of most anxiety disorders4, most preventive efforts have targeted young people; some have targeted adults and older adults, but the effects tend to be small and inconsistent131.
Universal preventive interventions (such as FRIENDS for life132) have mostly been conducted in elementary and high school settings (targeting children 6–17 years of age), where they are usually delivered to entire classes or schools, often by teachers, and usually involve teaching students low-level anxiety management skills. Meta-analyses have demonstrated small, significant effects on the prevention of anxiety disorders133, and the maintenance of this preventive effect for up to 12 months133,134. Surprisingly, given the purpose of prevention, long-term effects have not been evaluated.
Selective interventions for anxiety that are aimed at known risk factors have received the least amount of evaluation. Some work has targeted the children of parents with anxiety and has shown a lower incidence of anxiety disorders among children who received the active intervention at 1 year of follow-up135. Anxiety sensitivity is a risk factor for panic disorder, and some small trials have demonstrated a reduced onset of panic disorder after the targeting of selective interventions to children and adolescents or young adults who scored highly on anxiety sensitivity136. The most widely studied programme is Cool Little Kids, which is targeted at children with an inhibited temperament and overprotective parents (two risk factors for anxiety in preschool-age children). Cool Little Kids teaches parents of withdrawn and inhibited young children methods to help their children overcome fears, to be less protective of their children and to manage their own emotions137. University-based trials have shown a reduced prevalence of anxiety disorders in children that received Cool Little Kids than untreated children, up to 3 years after the intervention138. In one study, girls whose parents received the Cool Little Kids programme had fewer anxiety and mood disorders than the girls whose parents did not receive the programme when the girls reached mid-adolescence139.
Indicated interventions usually target those 7–18 years of age who already show high levels of anxiety symptoms but might not meet the full diagnostic criteria for an anxiety disorder. Several indicated programmes have been developed and most are delivered in school settings. Indicated programmes generally cover various anxiety-management strategies, such as relaxation, approaching feared objects or situations and realistic thinking. Meta-analyses have shown small, significant effects (that is, effect sizes of 0.2–0.3) for indicated interventions that are larger than for universal delivery133,134, in addition to maintenance for up to 12 months134.
Management
Owing to the low rates of detection of anxiety disorders, especially in primary care settings, most patients do not receive treatment. Indeed, 50–85% of patients do not receive treatment within 50 years after onset of the disorder in some countries (such as Colombia, Mexico, Lebanon, Nigeria and China)140. In general, treatment is not sought until two decades after the onset of anxiety disorders140, with the exception of panic disorder and generalized anxiety disorder for which the time lapse is significantly shorter in some studies1. From the WHO’s World Mental Health Survey, the median time to seek treatment following the initial onset of anxiety disorders ranged from 3 to 30 years, with significant differences across the 15 countries assessed140. Delays in the time to treatment were larger in low-income and middle-income countries (the longest median time to treatment was in Mexico and Lebanon) than in developed countries (the shortest median times was in Israel and the Netherlands)140.
Several psychological and pharmacological treatments are available for the management of anxiety disorders. Treatment paradigms can include various types of psychological therapy and/or various pharmacological therapies.
Standards of care
Psychological treatments.
CBT is the most empirically supported psychological treatment for childhood, adolescent and adult anxiety disorders. CBT is often the first-line treatment for certain anxiety disorders, as has been recommended by several heath practice guidelines in various countries, including the United Kingdom141, Canada142, Germany143 and Singapore144. However, national recommendations are likely to vary by the availability of treatment options, with CBT less available in low-to-middle-income countries than in higher-income countries. When both psychological and pharmacological treatment options are available, most patients prefer psychological treatments over pharmacological treatments145. Pharmacological therapies are often combined with psychological treatments for anxiety disorders, especially in patients with more-severe presentations or in patients with comorbid depression.
CBT is a short-term (for example, one session per week for 10–20 weeks), goal-oriented, skills-based treatment that can be used for the treatment of anxiety disorders and other psychiatric disorders (BOX 5). In CBT aimed at children and adolescents, especially children under 13 years of age, parents are directly involved in the treatment30. In some programmes, parents might be the only recipient of treatment; in other programmes, parents are present in the sessions to observe their child or parents are taught specific strategies to help their child alongside the child’s own treatment146.
Box 5 |. Cognitive–behavioural therapy.
Cognitive–behavioural therapy (CBT) reduces anxiety-driven biases to interpret ambiguous stimuli as threatening, replaces avoidant and safety-seeking behaviours with approach and coping behaviours, and reduces excessive levels of autonomic arousal216. As an umbrella term, CBT includes a broad array of therapeutic strategies, such as psychoeducation (that is, the self-monitoring of thoughts, physical feelings and behaviours or symptoms), cognitive restructuring (by identifying errors in thinking and replacing them with more evidence-based thoughts) and systematic and repeated exposure to feared stimuli, in real life (for example, driving to unfamiliar places), imaginally (for example, to catastrophic images that underlie the excessive worry of generalized anxiety disorder or trauma images in post-traumatic stress disorder) or through interoceptive exercises (which addresses the fear of bodily symptoms of anxiety), and breathing retraining or relaxation.
Several meta-analyses have indicated that CBT is an efficacious treatment for anxiety disorders in children, in adolescents, in adults and in late life. The largest effect sizes were seen when CBT was compared with waiting list controls147, but effect sizes were smaller than with psychological placebos148 and active psychological treatment comparators149. The presence of comorbid depression does not significantly attenuate the effects of CBT150. CBT can also result in a moderate improvement in quality of life compared with patients on the waiting list or those receiving placebo and active comparator treatments151. Indeed, a systematic review of 87 studies of CBT showed post-treatment response rates (that is, percent who achieve symptom reduction to within normative ranges) of 45–55% for individual anxiety disorders, including specific phobia (52.7%), social anxiety disorder (45.3%), panic disorder or agoraphobia (53.2%) and generalized anxiety disorder (47%)152. In data from children, the treatment response is more commonly expressed in terms of diagnostic remission; remission is ~60% immediately following treatment compared with ~15% in controls, and effects are maintained or increase up to 12 months later153.
The evidence base for other psychological treatments is much less robust than for CBT. Mindfulness and acceptance-based approaches (that is, focusing the individual’s attention and learning to accept feelings and experiences using a combination of meditation and breathing exercises) are growing in popularity, but conclusions regarding their efficacy are hampered by the low quality of the studies and a limited number of randomized controlled trials (RCTs). Nonetheless, mindfulness and acceptance-based approaches are reportedly superior to no treatment and placebo, and comparable to (or slightly less effective than) active control conditions in a meta-analysis154.
Few RCTs have evaluated psychodynamic approaches for anxiety disorders. For example, one meta-analysis reported only 14 RCTs for psychodynamic therapies (that is, understanding how unconscious thought processes can manifest as current thoughts and feelings) for anxiety disorders since 1970 (REF. 155), some of which did not include reliable or valid measures of diagnosis or of outcome.
Interpersonal therapy (a short-term treatment focused on interpersonal relationships, related to but different from psychodynamic therapy) was more effective for anxiety symptoms than inactive comparison conditions in three studies, although three other studies with a low risk of bias from the same meta-analysis showed smaller effect sizes for interpersonal therapy than for CBT156. For the treatment of specific anxiety disorders, interpersonal therapy was less effective than CBT for the treatment of panic disorder with agoraphobia157.
In individuals 7–17 years of age with anxiety, exposure, cognitive–behavioural techniques, modelling of strategies and psychoeducation showed the most consistent evidence and large effects across several studies in a meta-analysis, whereas play therapy, bio-feedback, client-centred therapy or attachment therapy showed small and inconsistent effects158. Aside from non-response rates152 and return of fear, there is no clear evidence for adverse effects from evidence-based psychological treatments for anxiety disorders.
Pharmacological treatment.
Pharmacological treatment of anxiety is viewed as an alternative or adjunct to psychological treatment. Although the pathophysiology of anxiety disorders is incompletely understood, targeting systems that are thought to underlie fear expression, learning and extinction is of considerable interest, including drugs that influence serotonergic, adrenergic, glutamatergic, various neuropeptide and endocannabinoid systems159,160.
Antidepressants are considered the first-line pharmacological treatment for most anxiety disorders (the exception being specific phobia) based on their evidence of efficacy from numerous RCTs, safety and the absence of abuse potential161. The most widely used antidepressants for treating anxiety disorder are selective serotonin reuptake inhibitors (SSRIs) and serotonin–noradrenaline reuptake inhibitors (SNRIs). SSRIs and SNRIs have demonstrated efficacy for all anxiety disorders, except for specific phobia, but within these classes, specific drugs are superior for the treatment of anxiety disorders; individual predictors of response that would enable a more personalized approach to pharmacotherapy are not yet available. Accordingly, the selection of a particular pharmacological therapy should be based on the prior response to a given drug (if the patient had previously been treated successfully), the preference of the patient and the familiarity of the physician with the drug. Treatment with SSRIs or SNRIs is not infrequently associated with (usually transient) adverse effects, including increased gastrointestinal dis-comfort, diarrhoea, jitteriness, insomnia and headache, among others162. Other antidepressants, such as tricyclic antidepressants and monoamine oxidase inhibitors, have been widely used in the past for the treatment of anxiety disorders, but their adverse effects and safety profiles have made them much less popular recently162. Bupropion, which is approved for the treatment of major depression, is probably ineffective for the treatment of anxiety disorders, and most antidepressants that have been recently marketed for depression have limited evidence of efficacy for anxiety disorders. Possible exceptions are vilazodone (a serotonin reuptake inhibitor and partial agonist of serotonin receptors) and agomelatine (a melatonin receptor agonist) for the treatment of generalized anxiety disorder163,164, although neither has regulatory approval for this indication.
Benzodiazepines are efficacious for the treatment of anxiety disorders, and most expert guidelines recommend their use as second-line or third-line agents142,165. However, concerns about possible abuse and dependence limit their use, and these drugs should be used cautiously (or not used at all) in individuals with alcohol or other substance use disorders. Adverse effects associated with benzodiazepine treatment include drowsiness, dizziness and, particularly in elderly individuals, increased risk of falls. Controversy persists about an association between chronic benzodiazepine use and dementia, although such an association, if it exists, is likely to be non-causal166. Anti-epileptic drugs that modulate γ-aminobutyric acid (GABA) signalling, such as gabapentin and pregabalin, are sometimes used as alternatives to benzodiazepines when there is concern about potential abuse or misuse (for example, in a patient with a history of alcohol or other drug abuse). Atypical antipsychotics (such as risperidone or quetiapine) might also be useful for the treatment of anxiety disorders, particularly as an adjunct to SSRIs or SNRIs. However, evidence for the usefulness of atypical antipsychotics to treat anxiety disorders is limited, although quetiapine has several positive RCTs for generalized anxiety disorder167. In addition, treatment with atypical antipsychotics is associated with risk of weight gain and metabolic syndrome; these risks should limit their use to patients with treatment-refractory anxiety. Other types of drugs used for the treatment of anxiety disorder include buspirone (a non-benzodiazepine anxiolytic) and β-adrenergic blockers. Buspirone is an effective treatment for generalized anxiety disorder, but none of the other anxiety disorders162. β-Adrenergic blockers (such as propranolol or atenolol) are efficacious for some individuals with the performance type of social anxiety disorder (that is, when speaking or performing in public), but evidence supporting their effectiveness for anxiety in general is lacking168.
Anxiety disorders in children and adolescents can be treated with SSRIs or SNRIs169,170, which are usually administered when psychological approaches are not available or are not working. Some caution is warranted given that some evidence has indicated increased rates of suicidality with SSRIs in children and adolescents and young adults171 (although the benefits of SSRI treatment with careful monitoring are considered to outweigh this risk).
Women with anxiety disorders during the perinatal period (including during pregnancy and breastfeeding) are probably best treated with CBT; some SSRIs (such as sertraline) can be considered for use in these patients when CBT is unavailable, has shown a lack of efficacy or when the patient prefers pharmacotherapy172.
Combination treatments.
Meta-analyses comparing the use of pharmacotherapy and psychotherapy for the treatment of anxiety disorders suggest that differences in overall efficacy are negligible173. Data from meta-analyses indicate a possible benefit of combining psychotherapy (mostly CBT) and pharmacotherapy compared with the use of pharmacotherapy alone in adults174, although additional research is needed. Some, albeit limited, evidence supports the superiority of combination treatment (for example, the use of CBT and SSRIs) for the treatment of anxiety disorders in children and adolescents169,175, although for most patients, a stepped care approach (that is, implementing one treatment and then adding another if needed) is usually recommended. Little evidence is available to guide the choice between combination treatment versus either CBT or pharmacological therapy alone.
Responses to therapy
Treatment response for anxiety disorders is usually measured by patient self-report, and is preferably assessed using validated disorder-specific questionnaires that are completed each treatment session. In research studies, the treatment response is also measured by clinical interviews conducted by independent raters at specific time points (for example, 3 months after treatment initiation). Given the skill-based nature of CBT, and the improvement that derives from skill practice between sessions, the response to treatment is cumulative and patients are encouraged to complete the full protocol of therapy (for example, 10–20 weekly sessions). Similarly, medication regimens are usually continued for 2–3 months before their effectiveness is judged, unless clear signs of worsening symptoms or poor toleration are observed. If treatment responses are suboptimal (for example, the persistence of symptoms despite an adequate number of sessions, time or medication dosage), then additional therapeutic strategies or pharmacotherapies might be considered. No biomarkers for drug response are currently available.
Treatment resistance
Although CBT is generally effective for the management of anxiety disorders, and effect sizes do not differ between post-assessment and follow-up assessments148, relapse can occur in up to ~40% of children and adolescents with anxiety176 and up to 30% of adults with panic disorder, 1–2 years after CBT discontinuation177,178. Relapse data are not available for other anxiety disorders in adults. Consequently, maintenance strategies are recommended, and evidence suggests their effectiveness. For example, maintenance CBT (that is, nine monthly sessions) was associated with greater reductions in anxiety symptoms in the long-term than with no additional treatment179. In addition, the larger the number of monthly CBT sessions via telephone following a brief CBT and medication treatment, the greater the reduction in anxiety symptoms in the long term180. Relapse within 3–6 months after the discontinuation of pharmacotherapy has been observed in one-third to one-half of individuals with social anxiety, generalized anxiety and panic disorder181; relapse can be reduced by either the continuation of medication182,183 or the use of CBT181, although the optimal length or doses for relapse prevention is unknown.
Although some studies have aimed to identify the predictors of non-response or relapse, the literature is plagued by relatively small sample sizes, mixed findings, a lack of replication and a lack of meta-analyses. Attempts to identify personalized treatments are mostly premature as the literature is too limited and variable in quality184. Nevertheless, one large study found that comorbid depression and conduct disorder predicted poorer outcomes from CBT in children with anxiety185.
Quality of life
Longitudinal studies have shown that anxiety disorders are among the most persistent mental health disorders, with spontaneous remission occurring in ≤23%34,186, although in one small-scale study, remission was noted for ~40% of participants6. Symptom progression models (FIG. 4), similar to models used in hypertension and diabetes research, indicate various pathways and factors that can promote chronicity and the onset of complications of anxiety disorders. Such symptom progression models with their trajectories (FIG. 4a) have proved useful for examining and quantifying the public health benefits resulting from implementing early targeted preventive interventions as well therapeutic interventions in clinical stages (FIG. 4b).
Figure 4 |. Symptom progression model of anxiety disorders.
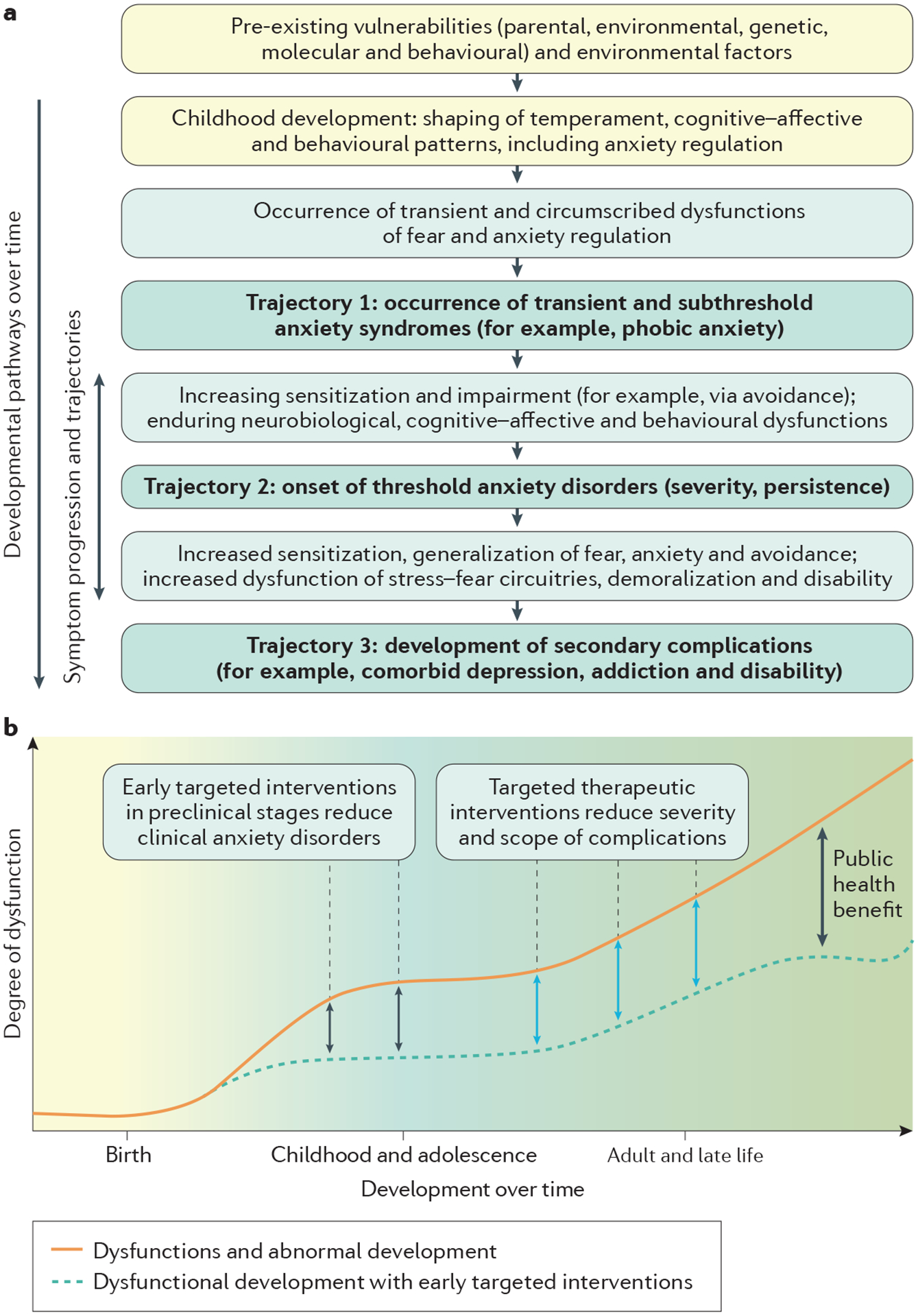
a | Symptom progression models describe the developmental pathways of vulnerability and risk factors over time that are typical of the expression of subclinical and transient early signs, the onset of the clinical disorder and the typical onset of complications and comorbidities associated with a persistent course of the disorder, if untreated. For anxiety disorders, broadly speaking, three main symptom onsets can be identified: subthreshold anxiety symptoms (trajectory 1), threshold anxiety disorders (trajectory 2) and secondary complications and comorbidities (trajectory 3). b | Targeted preventive therapies in the preclinical stages of anxiety could reduce the prevalence of clinically relevant anxiety disorders (black arrows). Targeted interventions after the onset of the disorder, such as cognitive–behavioural therapy, could reduce the severity of complications (blue arrows). Adapted with permission from REF. 227, Elsevier.
Anxiety disorders significantly impair several areas of cognitive development and social roles187–189 and are associated with adverse consequences, which results in an overall reduced quality of life, particularly in patients with comorbid depression189. Of the specific anxiety disorders, panic disorder and generalized anxiety disorder are typically more severe in terms of disability and comorbid complications, whereas specific phobias are less severe, and social anxiety lies in between37. Anxiety disorders rarely occur in isolation, with comorbid mental disorders1 such as depression and substance use disorders found in 60–90% of patients. Indeed, increased rates of depressive disorders and, to a lesser degree, substance use disorders develop in the years after anxiety disorder onset8,37. Increased mortality rates in patients with anxiety disorder are largely explained by comorbid depression190.
In addition to the personal consequences of anxiety disorders, overwhelming evidence supports an immense societal burden. Consequences of anxiety disorders, such as school failure, academic underachievement, unemployment and underemployment, in addition to interactional and marital problems, can combine into persistent escalations of further complications over the course of life. Anxiety disorders have been estimated as the second highest in terms of burden based on disability-adjusted life years. Although the attributable fraction of the burden for anxiety disorders is estimated to be 4.2% (FIG. 5a), the total burden, including anxiety disorders with comorbid depression, is considerably larger1,191 (FIG. 5b).
Figure 5 |. Disability-adjusted life years lost for mental disorders, neurological disorders and other disease groups.
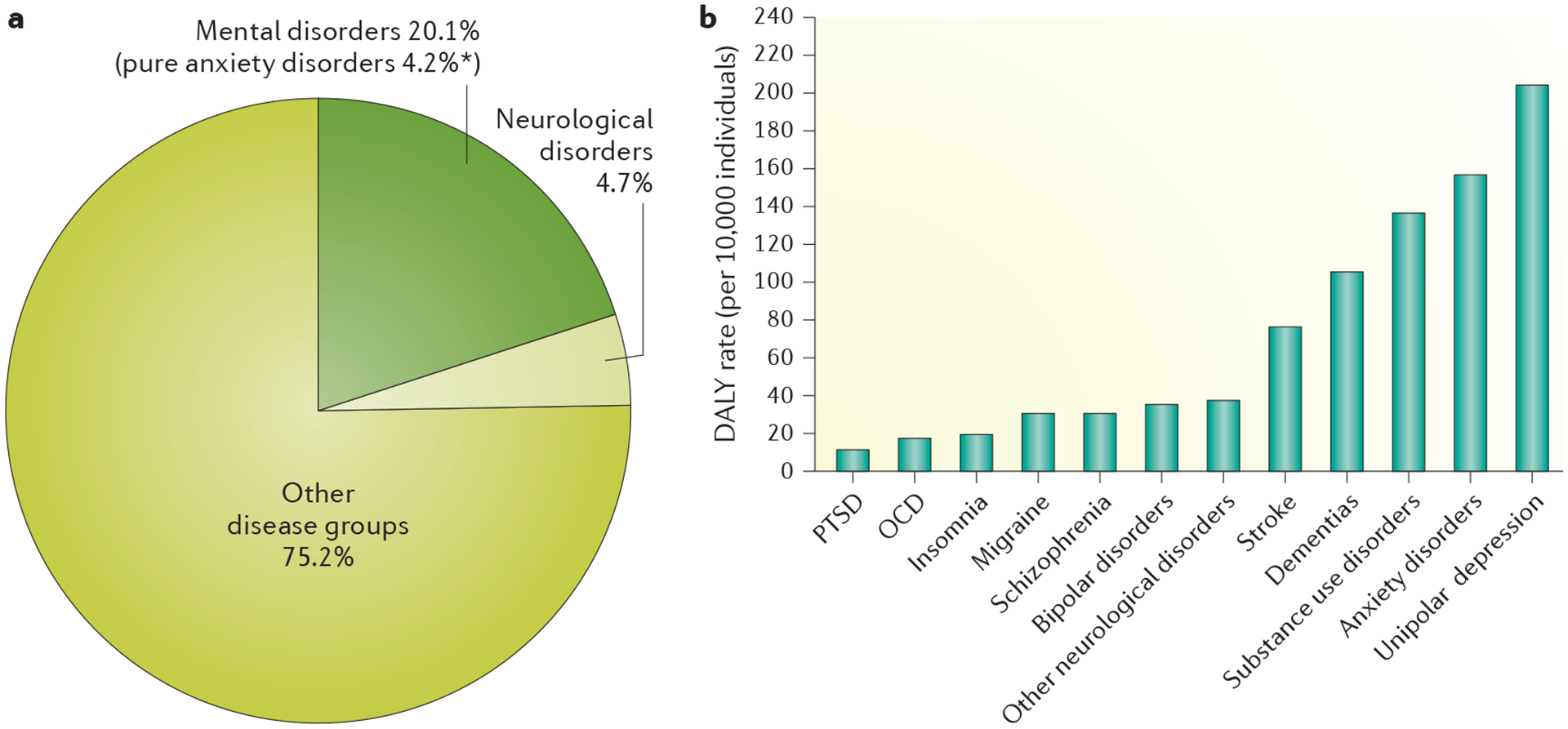
a | The total distribution (%) of disability-adjusted life years (DALYs) that are attributable to mental and neurological disorders, in addition to other somatic diseases and conditions. b | The DALYs for different disorders. OCD, obsessive–compulsive disorder; PTSD, post-traumatic stress disorder. *This value is a conservative estimate and does not reflect the total burden, because comorbid anxiety–depression cases are counted entirely towards depression. Data from REF. 1.
Above and beyond the extremely high monetary estimates, the cost of anxiety disorders extends towards friends and family. In addition, these burdens are passed on to the next generation via familial transmission, mediating an increased risk for mental health complications192.
Outlook
Risk factors and mechanisms
The outstanding research questions for anxiety disorders are many, starting with defining the precise risk factors and their underlying mechanisms that contribute to the onset and persistence of these disorders. A better understanding of the specific biological and genetic factors that underlie the vulnerability of some individuals to develop anxiety disorders in response to stress is needed. We also need to understand why individuals who are prone to anxiety disorders have deficits in the extinction of fear and greater generalization of conditional fear, which are factors that are likely to contribute to the persistence and pervasiveness of fears. Advances in neuroscience have elucidated neural circuits that are related to fear learning, extinction and generalization, but understanding how these neural circuits relate to risk factors for anxiety remains to be understood. Related to this aspect is the mechanism underlying the sex difference in the prevalence of anxiety disorders; although important, the influence of gonadal hormones on extinction is unlikely to fully explain sex differences. Answering these questions will require much more in-depth collaboration across basic science (including animal research) and clinical science193. Given the early onset of most anxiety disorders, considerable research is needed on crucial developmental windows so that we can identify processes that become dysregulated and contribute to anxiety disorder onset194.
Prevention
Improving the prevention of anxiety is still an important topic, especially given the damaging effects of anxiety on all aspects of life. As previously discussed, some universal, indicated and selective programmes have prevented anxiety, although their effects tend to be small to moderate in size. Conceivably, prevention strategies that more directly target the mechanisms responsible for the onset of anxiety disorders, such as overactivation of the amygdala to threat or cognitive biases to interpret information in a threat-related manner, might yield more substantial effects.
Management
Treatment efficacy.
As previously stated, psychological and pharmacological treatments, and sometimes their combination, are effective for anxiety disorders, perhaps more so than for many other psychiatric conditions. Nonetheless, an upper limit on effectiveness does occur and a clinically meaningful response (that is, anxiety levels within normative ranges) in adults is generally ~50%, and relapse does occur. Consequently, the development of more effective and lasting treatments, both psychological and biological, is required for anxiety disorders.
Development of new therapies.
A greater understanding of the mechanisms underlying anxiety disorders will facilitate the development of mechanism-specific treatments. These treatments might offer the potential for greater effects than current therapies, especially if they are matched to specific neural, hormonal, genetic, cognitive or behavioural processes that are dysregulated in anxiety disorders.
Basic science and neuroscience research might be highly informative for the development of targeted treatments. For example, of particular concern is the resurgence of conditional fear following treatment completion, which is consistent with the return of conditional fear when an extinguished stimulus is encountered in a context that differs from the extinction context, after an aversive reinstating event, or with time195. Methods for reducing this fear resurgence could improve long-term outcomes and this is being examined using both behavioural and pharmacological means for disrupting contextual renewal and reinstatement196.
In addition, enhancing retention of what is learned during exposure therapy is of interest. So far, the best-studied treatment for this condition is d-cycloserine, a partial N-methyl-d-aspartate (NMDA) receptor agonist. However, a Cochrane review of 21 studies found no evidence of clinical benefit of d-cycloserine augmentation of CBT for the management of anxiety disorders197, although benefits may be stronger for those who show most fear reduction during exposure. Further research is needed into other drugs that might enhance the acute and long-term effects of CBT.
Another area of interest is the interruption of the reconsolidation of fear memories, in order to erase these memories. Although early work showed some promise with both pharmacological (for example, propranolol, a β-blocker) and behavioural (for example, brief pre-exposure to the feared stimulus) methods for interruption of reconsolidation198, these results have not been widely replicated199. Eventual application of these strategies to disrupt reconsolidation in children will be essential, given the damaging effects of anxiety on social relations and academic achievement from early stages and the scarring impact of early impediments across a lifetime.
Use of computer-assisted, Internet-based and app treatments (that is, e-interventions) has grown rapidly over the past decade, given their provision of care to those who do not otherwise have access (for example, individuals in rural locations, economic limitations and/or long waiting lists) or in patients who prefer anonymity200. e-Interventions for anxiety disorders, the majority of which are CBT, have become validated alternatives to standard face-to-face treatment, and meta-analyses have confirmed their effectiveness for adults201, children and adolescents with anxiety202,203 compared with no treatment. However, attrition rates (that is, the proportion of patients who drop out of the study) are substantially higher when these programmes are completely automated and their efficacy for severe anxiety remains uncertain.
Other treatments currently under development include cognitive bias modification training programmes (for example, training attentional bias away from threat-relevant stimuli or training neutral or positive interpretations of ambiguous material). However, the interest in these programmes has been challenged by small effect sizes on anxiety symptoms in clinical samples204,205.
Global treatment.
As a group, anxiety disorders are the most prevalent mental health conditions, and the need for treatment vastly outstrips traditional treatment resources, particularly in low-to-middle-income countries. Greater attention has been given recently to models of treatment implementation for anxiety (and depression) in low-income regions, such as Africa, Pakistan, South America, Iraq and India206. The rapid explosion in Internet-based and other such technologies for assessing and treating anxiety disorders provides a partial solution to the treatment of anxiety in low-income countries, but with certain caveats. First, more regulation of online or app treatment programmes through carefully conducted RCTs is required. Second, existing programmes mostly consist of generic CBT; once the complex causal pathways of anxiety disorder have been established, and targeted treatments are available, then other online-based or app-based behavioural treatments can be developed to target those pathways more directly than current programmes. Third, further evaluation of the population for whom online-based or app-based programmes is best indicated, or conversely, for whom a highly trained clinician is most indicated, is required. In addition, task shifting or training non-professionals in the delivery of evidence-based psychological treatments, such as CBT, might address the global demand for anxiety treatments206. This approach has shown some clinically appreciable effects for the treatment of anxiety and depression, with stronger effects expected with greater assurance of fidelity with which the treatments are implemented194. Technology could also be a useful resource in this regard, as computer-based or online-based programmes exist not only for training of non-professionals207 but also to guide their delivery of behavioural treatments as they interact with patients with anxiety208.
Footnotes
Competing interests
M.B.S. has received consulting fees in the past 3 years from Actelion Pharmaceuticals, Janssen, Neurocrine Biosciences, and Pfizer, and stock options from Oxeia Biopharmaceuticals and Resilience Therapeutics. M.B.S. also receives editorial honoraria from the journal Biological Psychiatry, and in his role of Co-Editor-in-Chief for UpToDate in Psychiatry. All other authors declare no competing interests.
References
- 1.Wittchen HU et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur. Neuropsychopharmacol 21, 655–679 (2D). [DOI] [PubMed] [Google Scholar]; Provides the most recent state-of-the-art summary of epidemiological evidence of anxiety disorders and their associated burden in Europe.
- 2.Haro JM et al. ROAMER: roadmap for mental health research in Europe. Int. J. Methods Psychiatr. Res 23 (Suppl. 1), 1–14 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Christopher P & Murray JL Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388, 1659–1724 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kessler RC, Ruscio AM, Shear K & Wittchen H-U Epidemiology of anxiety disorders. Curr. Top. Behav. Neurosci 2, 21–35 (2010). [PubMed] [Google Scholar]; Overviews the prevalence of and risk factors for anxiety disorders.
- 5.Beesdo K, Knappe S & Pine DS Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatr. Clin. North Am 32, 483–524 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]; One of the few available prospective, longitudinal epidemiological studies that provides valid incidence data on anxiety disorders as well as the risk for secondary depression.
- 6.Batelaan NM, Rhebergen D, Spinhoven P, van Balkom AJ & Penninx BWJH Two-year course trajectories of anxiety disorders: do DSM classifications matter? J. Clin. Psychiatry 75, 985–993 (2014). [DOI] [PubMed] [Google Scholar]
- 7.Spinhoven P et al. Prediction of 6-yr symptom course trajectories of anxiety disorders by diagnostic, clinical and psychological variables. J. Anxiety Disord 44, 92–101 (2016). [DOI] [PubMed] [Google Scholar]
- 8.Beesdo K, Pine DS, Lieb R & Wittchen H-U Incidence and risk patterns of anxiety and depressive disorders and categorization of generalized anxiety disorder. Arch. Gen. Psychiatry 67, 47–57 (2010). [DOI] [PubMed] [Google Scholar]
- 9.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5® 5th edn (APA Publishing, 2013). [Google Scholar]
- 10.World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders. WHO; http://www.who.int/classifications/icd/en/bluebook.pdf (2010). [Google Scholar]
- 11.Kessler RC et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry 6, 168–176 (2007). [PMC free article] [PubMed] [Google Scholar]
- 12.Baxter AJ, Scott KM, Vos T & Whiteford HA Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol. Med 43, 897–910 (2013). [DOI] [PubMed] [Google Scholar]
- 13.Lewis-Fernández R et al. Culture and the anxiety disorders: recommendations for DSM-V. Depress. Anxiety 27, 212–229 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kessler RC, Chiu WT, Demler O, Walters EE & Walters EE Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 62, 617–627 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silove D et al. Pediatric-onset and adult-onset separation anxiety disorder across countries in the World Mental Health Survey. Am. J. Psychiatry 172, 647–656 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bögels SM, Knappe S & Clark LA Adult separation anxiety disorder in DSM-5. Clin. Psychol. Rev 33, 663–674 (2013). [DOI] [PubMed] [Google Scholar]
- 17.Zhang X et al. Generalized anxiety in community-dwelling elderly: prevalence and clinical characteristics. J. Affect. Disord 172, 24–29 (2015). [DOI] [PubMed] [Google Scholar]
- 18.Hofmann SG & Hinton DE Cross-cultural aspects of anxiety disorders. Curr. Psychiatry Rep 16, 450 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beesdo-Baum K & Knappe S Developmental epidemiology of anxiety disorders. Child Adolesc. Psychiatr. Clin. N. Am 21, 457–478 (2012). [DOI] [PubMed] [Google Scholar]
- 20.McLean CP, Asnaani A, Litz BT & Hofmann SG Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J. Psychiatr. Res 45, 1027–1035 (2D). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lieb R, Isensee B, Höfler M, Pfister H & Wittchen H-U Parental major depression and the risk of depression and other mental disorders in offspring: a prospective-longitudinal community study. Arch. Gen. Psychiatry 59, 365–374 (2002). [DOI] [PubMed] [Google Scholar]
- 22.Shimada-Sugimoto M, Otowa T & Hettema JM Genetics of anxiety disorders: genetic epidemiological and molecular studies in humans. Psychiatry Clin. Neurosci 69, 388–401 (2015). [DOI] [PubMed] [Google Scholar]
- 23.Otowa T et al. Meta-analysis of genome-wide association studies of anxiety disorders. Mol. Psychiatry 21, 1391–1399 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]; The largest genetic study of mixed anxiety disorders to date. This meta-analysis of anxiety disorders and related symptom scores indicates that the genetic aetiologies of anxiety disorders are similar to those of other common psychiatric disorders, such as depression.
- 24.Sareen J et al. Adverse childhood experiences in relation to mood and anxiety disorders in a population-based sample of active military personnel. Psychol. Med 43, 73–84 (2013). [DOI] [PubMed] [Google Scholar]
- 25.Afifi TO, Mota NP, Dasiewicz P, MacMillan HL & Sareen J Physical punishment and mental disorders: results from a nationally representative US sample. Pediatrics 130, 184–192 (2012). [DOI] [PubMed] [Google Scholar]
- 26.Otowa T, York TP, Gardner CO, Kendler KS & Hettema JM The impact of childhood parental loss on risk for mood, anxiety and substance use disorders in a population-based sample of male twins. Psychiatry Res. 220, 404–409 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taillieu TL, Brownridge DA, Sareen J & Afifi TO Childhood emotional maltreatment and mental disorders: results from a nationally representative adult sample from the United States. Child Abuse Negl. 59, 1–12 (2016). [DOI] [PubMed] [Google Scholar]
- 28.Vrshek-Schallhorn S et al. Validating new summary indices for the Childhood Trauma Interview: associations with first onsets of major depressive disorder and anxiety disorders. Psychol. Assess 26, 730–740 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pérez-Edgar K & Fox NA Temperament and anxiety disorders. Child Adolesc. Psychiatr. Clin. N. Am 14, 681–706 (2005). [DOI] [PubMed] [Google Scholar]; Provides a detailed overview of the relationship between temperamental factors (which are arguably the single most important risk factor) and anxiety.
- 30.Rapee RM, Schniering CA & Hudson JL Anxiety disorders during childhood and adolescence: origins and treatment. Annu. Rev. Clin. Psychol 5, 311–341 (2009). [DOI] [PubMed] [Google Scholar]
- 31.Greco LA & Morris TL Factors influencing the link between social anxiety and peer acceptance: contributions of social skills and close friendships during middle childhood. Behav. Ther 36, 197–205 (2005). [Google Scholar]
- 32.Hankin BL, Abramson LY, Miller N & Haeffel GJ Cognitive vulnerability-stress theories of depression: examining affective specificity in the prediction of depression versus anxiety in three prospective studies. Cognit. Ther. Res 28, 309–345 (2004). [Google Scholar]
- 33.Uliaszek AA et al. A longitudinal examination of stress generation in depressive and anxiety disorders. J. Abnorm. Psychol 121, 4–15 (2012). [DOI] [PubMed] [Google Scholar]
- 34.Wittchen HU, Kessler RC, Pfister H & Lieb M Why do people with anxiety disorders become depressed? A prospective-longitudinal community study. Acta Psychiatr. Scand. Suppl 2000, 14–23 (2000). [PubMed] [Google Scholar]
- 35.Beesdo K et al. Incidence of social anxiety disorder and the consistent risk for secondary depression in the first three decades of life. Arch. Gen. Psychiatry 64, 903–912 (2007). [DOI] [PubMed] [Google Scholar]
- 36.Stein MB et al. Social anxiety disorder and the risk of depression: a prospective community study of adolescents and young adults. Arch. Gen. Psychiatry 58, 251–256 (2001). [DOI] [PubMed] [Google Scholar]
- 37.Zimmermann P et al. Primary anxiety disorders and the development of subsequent alcohol use disorders: a 4-year community study of adolescents and young adults. Psychol. Med 33, 1211–1222 (2003). [DOI] [PubMed] [Google Scholar]
- 38.Moylan S, Jacka FN, Pasco JA & Berk M Cigarette smoking, nicotine dependence and anxiety disorders: a systematic review of population-based, epidemiological studies. BMC Med. 10, 123 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Phan K, Xie A, Di Eusanio M & Yan TD A meta-analysis of minimally invasive versus conventional sternotomy for aortic valve replacement. Ann. Thorac. Surg 98, 1499–1511 (2014). [DOI] [PubMed] [Google Scholar]
- 40.Kindt M, Soeter M & Vervliet B Beyond extinction: erasing human fear responses and preventing the return of fear. Nat. Neurosci 12, 256–258 (2009). [DOI] [PubMed] [Google Scholar]
- 41.Etkin A, Egner T & Kalisch R Emotional processing in anterior cingulate and medial prefrontal cortex. Trends Cogn. Sci 15, 85–93 (2D). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.LeDoux JE & Pine DS Using neuroscience to help understand fear and anxiety: a two-system framework. Am. J. Psychiatry 173, 1083–1093 (2016). [DOI] [PubMed] [Google Scholar]
- 43.Etkin A & Wager TD Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am. J. Psychiatry 164, 1476–1488 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fanselow MS Neural organization of the defensive behavior system responsible for fear. Psychon. Bull. Rev 1, 429–438 (1994). [DOI] [PubMed] [Google Scholar]
- 45.Cuthbert BN & Insel TR Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Med. 11, 126 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fonzo GA et al. Common and disorder-specific neural responses to emotional faces in generalised anxiety, social anxiety and panic disorders. Br. J. Psychiatry 206, 206–215 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gross CT & Canteras NS The many paths to fear. Nat. Rev. Neurosci 13, 651–658 (2012). [DOI] [PubMed] [Google Scholar]; Overviews the major brain circuits involved in the mediation of fear and threat behaviours in rodents; this work has been instrumental in informing current models of the dysfunctional neural systems underlying anxiety disorders.
- 48.Cryan JF & Holmes A Model organisms: the ascent of mouse: advances in modelling human depression and anxiety. Nat. Rev. Drug Discov 4, 775–790 (2005). [DOI] [PubMed] [Google Scholar]
- 49.Hariri AR & Holmes A Finding translation in stress research. Nat. Neurosci 18, 1347–1352 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Teicher MH, Samson JA, Anderson CM & Ohashi K The effects of childhood maltreatment on brain structure, function and connectivity. Nat. Rev. Neurosci 17, 652–666 (2016). [DOI] [PubMed] [Google Scholar]
- 51.Fonzo GA et al. Early life stress and the anxious brain: evidence for a neural mechanism linking childhood emotional maltreatment to anxiety in adulthood. Psychol. Med 46, 1037–1054 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Swartz JR, Knodt AR, Radtke SR & Hariri AR A neural biomarker of psychological vulnerability to future life stress. Neuron 85, 505–511 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.van Rooij SJH et al. Smaller hippocampal volume as a vulnerability factor for the persistence of post-traumatic stress disorder. Psychol. Med 45, 2737–2746 (2015). [DOI] [PubMed] [Google Scholar]
- 54.Yang RJ et al. Variation in mouse basolateral amygdala volume is associated with differences in stress reactivity and fear learning. Neuropsychopharmacology 33, 2595–2604 (2008). [DOI] [PubMed] [Google Scholar]
- 55.Hodes GE, Kana V, Menard C, Merad M & Russo SJ Neuroimmune mechanisms of depression. Nat. Neurosci 18, 1386–1393 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Daskalakis NP et al. New translational perspectives for blood-based biomarkers of PTSD: from glucocorticoid to immune mediators of stress susceptibility. Exp. Neurol 284, 133–140 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zannas AS & Binder EB Gene–environment interactions at the FKBP5 locus: sensitive periods, mechanisms and pleiotropism. Genes Brain Behav. 13, 25–37 (2014). [DOI] [PubMed] [Google Scholar]
- 58.Roozendaal B, McEwen BS & Chattarji S Stress, memory and the amygdala. Nat. Rev. Neurosci 10, 423–433 (2009). [DOI] [PubMed] [Google Scholar]
- 59.Myers B, McKlveen JM & Herman JP Glucocorticoid actions on synapses, circuits, and behavior: implications for the energetics of stress. Front. Neuroendocrinol 35, 180–196 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zorn JV et al. Cortisol stress reactivity across psychiatric disorders: a systematic review and meta-analysis. Psychoneuroendocrinology 77, 25–36 (2017). [DOI] [PubMed] [Google Scholar]
- 61.Kendler KS Twin studies of psychiatric illness: an update. Arch. Gen. Psychiatry 58, 1005–1014 (2001). [DOI] [PubMed] [Google Scholar]
- 62.Holmes A & Singewald N Individual differences in recovery from traumatic fear. Trends Neurosci. 36, 23–31 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kendler KS et al. The structure of genetic and environmental risk factors for syndromal and subsyndromal common DSM-IV axis I and all axis II disorders. Am. J. Psychiatry 168, 29–39 (2D). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Waszczuk MA, Zavos HMS, Gregory AM & Eley TC The phenotypic and genetic structure of depression and anxiety disorder symptoms in childhood, adolescence, and young adulthood. JAMA Psychiatry 71, 905–916 (2014). [DOI] [PubMed] [Google Scholar]
- 65.Kendler KS, Prescott CA, Myers J & Neale MC The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch. Gen. Psychiatry 60, 929–937 (2003). [DOI] [PubMed] [Google Scholar]
- 66.Weber H et al. Allelic variation in CRHR1 predisposes to panic disorder: evidence for biased fear processing. Mol. Psychiatry 21, 813–822 (2016). [DOI] [PubMed] [Google Scholar]
- 67.Howe AS et al. Candidate genes in panic disorder: meta-analyses of 23 common variants in major anxiogenic pathways. Mol. Psychiatry 21, 665–679 (2016). [DOI] [PubMed] [Google Scholar]
- 68.Smith DJ et al. Genome-wide analysis of over 106 000 individuals identifies 9 neuroticism-associated loci. Mol. Psychiatry 21, 749–757 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Euesden J, Lewis CM & O’Reilly PF PRSice: polygenic risk score software. Bioinformatics 31, 1466–1468 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Selzam S et al. Predicting educational achievement from DNA. Mol. Psychiatry 22, 267–272 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Arloth J et al. Genetic differences in the immediate transcriptome response to stress predict risk-related brain function and psychiatric disorders. Neuron 86, 1189–1202 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gunduz-Cinar O et al. Convergent translational evidence of a role for anandamide in amygdala-mediated fear extinction, threat processing and stress-reactivity. Mol. Psychiatry 18, 813–823 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Stevens JS et al. PACAP receptor gene polymorphism impacts fear responses in the amygdala and hippocampus. Proc. Natl Acad. Sci. USA 111, 3158–3163 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fernandes V & Osório FL Are there associations between early emotional trauma and anxiety disorders? Evidence from a systematic literature review and meta-analysis. Eur. Psychiatry 30, 756–764 (2015). [DOI] [PubMed] [Google Scholar]
- 75.Faravelli C et al. The role of life events and HPA axis in anxiety disorders: a review. Curr. Pharm. Des 18, 5663–5674 (2012). [DOI] [PubMed] [Google Scholar]
- 76.Maren S & Holmes A Stress and fear extinction. Neuropsychopharmacology 41, 58–79 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chattarji S, Tomar A, Suvrathan A, Ghosh S & Rahman MM Neighborhood matters: divergent patterns of stress-induced plasticity across the brain. Nat. Neurosci 18, 1364–1375 (2015). [DOI] [PubMed] [Google Scholar]
- 78.McEwen BS et al. Mechanisms of stress in the brain. Nat. Neurosci 18, 1353–1363 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kendler KS & Baker JH Genetic influences on measures of the environment: a systematic review. Psychol. Med 37, 615–626 (2007). [DOI] [PubMed] [Google Scholar]
- 80.Eley TC, Napolitano M, Lau JYF & Gregory AM Does childhood anxiety evoke maternal control? A genetically informed study. J. Child Psychol. Psychiatry 51, 772–779 (2010). [DOI] [PubMed] [Google Scholar]
- 81.Eley TC, Gregory AM, Clark DM & Ehlers A Feeling anxious: a twin study of panic/somatic ratings, anxiety sensitivity and heartbeat perception in children. J. Child Psychol. Psychiatry 48, 1184–1191 (2007). [DOI] [PubMed] [Google Scholar]
- 82.Murray L, Creswell C & Cooper PJ The development of anxiety disorders in childhood: an integrative review. Psychol. Med 39, 1413–1423 (2009). [DOI] [PubMed] [Google Scholar]
- 83.Eley TC et al. The intergenerational transmission of anxiety: a children-of-twins study. Am. J. Psychiatry 172, 630–637 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kendler KS, Myers J & Prescott CA The etiology of phobias: an evaluation of the stress-diathesis model. Arch. Gen. Psychiatry 59, 242–248 (2002). [DOI] [PubMed] [Google Scholar]
- 85.Lau JYF, Gregory AM, Goldwin MA, Pine DS & Eley TC Assessing gene–environment interactions on anxiety symptom subtypes across childhood and adolescence. Dev. Psychopathol 19, 1129–1146 (2007). [DOI] [PubMed] [Google Scholar]
- 86.Lesch KP et al. Association of anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region. Science 274, 1527–1531 (1996). [DOI] [PubMed] [Google Scholar]
- 87.Caspi A et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 301, 386–389 (2003). [DOI] [PubMed] [Google Scholar]
- 88.Stein MB, Schork NJ & Gelernter J Gene-by-environment (serotonin transporter and childhood maltreatment) interaction for anxiety sensitivity, an intermediate phenotype for anxiety disorders. Neuropsychopharmacology 33, 312–319 (2008). [DOI] [PubMed] [Google Scholar]
- 89.Holmes A, Murphy DL & Crawley JN Abnormal behavioral phenotypes of serotonin transporter knockout mice: parallels with human anxiety and depression. Biol. Psychiatry 54, 953–959 (2003). [DOI] [PubMed] [Google Scholar]
- 90.Homberg JR & Lesch K-P Looking on the bright side of serotonin transporter gene variation. Biol. Psychiatry 69, 513–519 (2D). [DOI] [PubMed] [Google Scholar]
- 91.Sharpley CF, Palanisamy SKA, Glyde NS, Dillingham PW & Agnew LL An update on the interaction between the serotonin transporter promoter variant (5-HTTLPR), stress and depression, plus an exploration of non-confirming findings. Behav. Brain Res 273, 89–105 (2014). [DOI] [PubMed] [Google Scholar]
- 92.Karg K, Burmeister M, Shedden K & Sen S The serotonin transporter promoter variant (5-HTTLPR), stress, and depression meta-analysis revisited. Arch. Gen. Psychiatry 68, 444–454 (2D). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Caspi A, Hariri AR, Holmes A, Uher R & Moffitt TE Genetic sensitivity to the environment: the case of the serotonin transporter gene and its implications for studying complex diseases and traits. Am. J. Psychiatry 167, 509–527 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Keers R et al. A genome-wide test of the differential susceptibility hypothesis reveals a genetic predictor of differential response to psychological treatments for child anxiety disorders. Psychother. Psychosom 85, 146–158 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Coleman JRI et al. Genome-wide association study of response to cognitive–behavioural therapy in children with anxiety disorders. Br. J. Psychiatry 209, 236–243 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bale TL Lifetime stress experience: transgenerational epigenetics and germ cell programming. Dialogues Clin. Neurosci 16, 297–305 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dias BG, Maddox SA, Klengel T & Ressler KJ Epigenetic mechanisms underlying learning and the inheritance of learned behaviors. Trends Neurosci. 38, 96–107 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Turecki G & Meaney MJ Effects of the social environment and stress on glucocorticoid receptor gene methylation: a systematic review. Biol. Psychiatry 79, 87–96 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bale TL & Epperson CN Sex as a biological variable: who, what, when, why, and how. Neuropsychopharmacology 42, 386–396 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Cover KK, Maeng LY, Lebrón-Milad K & Milad MR Mechanisms of estradiol in fear circuitry: implications for sex differences in psychopathology. Transl Psychiatry 4, e422 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lebron-Milad K & Milad MR Sex differences, gonadal hormones and the fear extinction network: implications for anxiety disorders. Biol. Mood Anxiety Disord 2, 3 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Maeng LY & Milad MR Sex differences in anxiety disorders: interactions between fear, stress, and gonadal hormones. Horm. Behav 76, 106–117 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mendoza-garcés L et al. Differential expression of estrogen receptors in two hippocampal regions during the estrous cycle of the rat. Anat. Rec. (Hoboken) 294, 1913–1919 (2D). [DOI] [PubMed] [Google Scholar]
- 104.Hwang MJ et al. Contribution of estradiol levels and hormonal contraceptives to sex differences within the fear network during fear conditioning and extinction. BMC Psychiatry 15, 295 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zeidan F et al. Brain mechanisms supporting the modulation of pain by mindfulness meditation. J. Neurosci 31, 5540–5548 (2D). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Shvil E et al. Sex differences in extinction recall in posttraumatic stress disorder: a pilot fMRI study. Neurobiol. Learn. Mem 113, 101–108 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Glover E et al. Inhibition of fear is differentially associated with cycling estrogen levels in women. J. Psychiatry Neurosci 38, 341–348 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Inslicht SS et al. Sex differences in fear conditioning in posttraumatic stress disorder. J. Psychiatr. Res 47, 64–71 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.First MB, Williams JBW, Karg RS & Spitzer RL Structured Clinical Interview for DSM-5® Disorders — Clinician Version (SCID-5-CV) (APA Publishing, 2016). [Google Scholar]
- 110.Sheehan DV et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 59 (Suppl. 20), 22–33 (1998). [PubMed] [Google Scholar]
- 111.Robins LN et al. The Composite International Diagnostic Interview. An epidemiologic Instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch. Gen. Psychiatry 45, 1069–1077 (1988). [DOI] [PubMed] [Google Scholar]
- 112.Schniering CA, Hudson JL & Rapee RM Issues in the diagnosis and assessment of anxiety disorders in children and adolescents. Clin. Psychol. Rev 20, 453–478 (2000). [DOI] [PubMed] [Google Scholar]
- 113.Zimmerman M & Galione J Psychiatrists’ and nonpsychiatrist physicians’ reported use of the DSM-IV criteria for major depressive disorder. J. Clin. Psychiatry 71, 235–238 (2010). [DOI] [PubMed] [Google Scholar]
- 114.Zimmerman M & McGlinchey JB Why don’t psychiatrists use scales to measure outcome when treating depressed patients? J. Clin. Psychiatry 69, 1916–1919 (2008). [DOI] [PubMed] [Google Scholar]
- 115.Vermani M, Marcus M & Katzman MA Rates of detection of mood and anxiety disorders in primary care: a descriptive, cross-sectional study. Prim. Care Companion CNS Disord 13, e1–e10 (2D). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.First MB et al. How do clinicians actually use the diagnostic and statistical manual of mental disorders in clinical practice and why we need to know more. J. Nerv. Ment. Dis 202, 841–844 (2014). [DOI] [PubMed] [Google Scholar]
- 117.Kessler RC et al. Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. Am. J. Psychiatry 156, 115–123 (1999). [DOI] [PubMed] [Google Scholar]
- 118.Roy-Byrne PP et al. Anxiety disorders and comorbid medical illness. Gen. Hosp. Psychiatry 30, 208–225 (2008). [DOI] [PubMed] [Google Scholar]
- 119.Craske MG & Stein MB Anxiety. Lancet 388, 3048–3059 (2016). [DOI] [PubMed] [Google Scholar]
- 120.Bandelow B et al. Biological markers for anxiety disorders, OCD and PTSD — a consensus statement. Part I: neuroimaging and genetics. World J. Biol. Psychiatry 17, 321–365 (2016). [DOI] [PubMed] [Google Scholar]
- 121.Spitzer RL, Kroenke K, Williams JBW & Löwe B A brief measure for assessing generalized anxiety disorder. Arch. Intern. Med 166, 1092–1097 (2006). [DOI] [PubMed] [Google Scholar]
- 122.Plummer F, Manea L, Trepel D & McMillan D Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatry 39, 24–31 (2016). [DOI] [PubMed] [Google Scholar]
- 123.Zigmond AS & Snaith RP The hospital anxiety and depression scale. Acta Psychiatr. Scand 67, 361–370 (1983). [DOI] [PubMed] [Google Scholar]
- 124.Campbell-Sills L et al. Validation of a brief measure of anxiety-related severity and impairment: the Overall Anxiety Severity and Impairment Scale (OASIS). J. Affect. Disord 112, 92–101 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Birmaher B et al. The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J. Am. Acad. Child Adolesc. Psychiatry 36, 545–553 (1997). [DOI] [PubMed] [Google Scholar]
- 126.Muris P, Merckelbach H, Schmidt H & Mayer B The revised version of the Screen for Child Anxiety Related Emotional Disorders (SCARED-R): factor structure in normal children. Pers. Individ. Dif 26, 99–112 (1998). [Google Scholar]
- 127.Spence SH A measure of anxiety symptoms among children. Behav. Res. Ther 36, 545–566 (1998). [DOI] [PubMed] [Google Scholar]
- 128.Nauta MH et al. A parent-report measure of children’s anxiety: psychometric properties and comparison with child-report in a clinic and normal sample. Behav. Res. Ther 42, 813–839 (2004). [DOI] [PubMed] [Google Scholar]
- 129.Edwards SL, Rapee RM, Kennedy SJ & Spence SH The assessment of anxiety symptoms in preschool-aged children: the revised Preschool Anxiety Scale. J. Clin. Child Adolesc. Psychol 39, 400–409 (2010). [DOI] [PubMed] [Google Scholar]
- 130.Lyneham HJ, Rapee RM & Hudson JL in The Wiley Handbook of Anxiety Disorders (eds Emmelkamp P & Ehring T) 623–642 (John Wiley & Sons, 2014). [Google Scholar]
- 131.García-Campayo J et al. Primary prevention of anxiety disorders in primary care: a systematic review. Prev. Med 76, S12–S15 (2015). [DOI] [PubMed] [Google Scholar]
- 132.Higgins E & O’Sullivan S ‘What Works’: systematic review of the ‘FRIENDS for Life’ programme as a universal school-based intervention programme for the prevention of child and youth anxiety. Educ. Psychol. Pract 31, 424–438 (2015). [Google Scholar]
- 133.Fisak BJ, Richard D & Mann A The prevention of child and adolescent anxiety: a meta-analytic review. Prev. Sci 12, 255–268 (2D). [DOI] [PubMed] [Google Scholar]
- 134.Teubert D & Pinquart M A meta-analytic review on the prevention of symptoms of anxiety in children and adolescents. J. Anxiety Disord 25, 1046–1059 (2D). [Google Scholar]
- 135.Ginsburg GS, Drake KL, Tein J-Y, Teetsel R & Riddle MA Preventing onset of anxiety disorders in offspring of anxious parents: a randomized controlled trial of a family-based intervention. Am. J. Psychiatry 172, 1207–1214 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Gardenswartz CA & Craske MG Prevention of panic disorder. Behav. Ther 32, 725–737 (2001). [Google Scholar]
- 137.Rapee RM, Lau EX & Kennedy SJ The Cool Little Kids Anxiety Prevention Program — Therapist Manual (Centre for Emotional Health, 2010). [Google Scholar]
- 138.Rapee RM, Kennedy SJ, Ingram M, Edwards SL & Sweeney L Altering the trajectory of anxiety in at-risk young children. Am. J. Psychiatry 167, 1518–1525 (2010). [DOI] [PubMed] [Google Scholar]
- 139.Rapee RM The preventative effects of a brief, early intervention for preschool-aged children at risk for internalising: follow-up into middle adolescence. J. Child Psychol. Psychiatry 54, 780–788 (2013). [DOI] [PubMed] [Google Scholar]; Describes some of the longest outcomes in the mental health prevention literature; for example, early interventions in individuals with anxious temperament can have powerful long-term benefits.
- 140.Wang PS et al. Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry 6, 177–185 (2007). [PMC free article] [PubMed] [Google Scholar]
- 141.National Institute for Health and Care Excellence. Anxiety disorders: guidance and guidelines. NICE; https://www.nice.org.uk/guidance/qs53 (2014). [Google Scholar]
- 142.Katzman MA et al. Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive–compulsive disorders. BMC Psychiatry 14, S1 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Bandelow B, Lichte T, Rudolf S, Wiltink J & Beutel ME The German guidelines for the treatment of anxiety disorders. Eur. Arch. Psychiatry Clin. Neurosci 265, 363–373 (2015). [DOI] [PubMed] [Google Scholar]
- 144.Lim L et al. Ministry of Health clinical practice guidelines: anxiety disorders. Singapore Med. J 56, 310–315 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.McHugh RK, Whitton SW, Peckham AD, Welge JA & Otto MW Patient preference for psychological versus pharmacologic treatment of psychiatric disorders. J. Clin. Psychiatry 74, 595–602 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Manassis K et al. Types of parental involvement in CBT with anxious youth: a preliminary meta-analysis. J. Consult. Clin. Psychol 82, 1163–1172 (2014). [DOI] [PubMed] [Google Scholar]; This meta-analysis provides a strong and unique perspective on a controversial issue: whether treatments for child anxiety benefit from the inclusion of parents.
- 147.James AC, James G, Cowdrey FA, Soler A & Choke A Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database Syst. Rev 3, CD004690 (2013). [DOI] [PubMed] [Google Scholar]
- 148.Hofmann SG & Smits JAJ Cognitive–behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J. Clin. Psychiatry 69, 621–632 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Cuijpers P, Cristea IA, Karyotaki E, Reijnders M & Huibers MJH How effective are cognitive behavior therapies for major depression and anxiety disorders? A meta-analytic update of the evidence. World Psychiatry 15, 245–258 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]; This meta-analysis presents a large body of evidence demonstrating the efficacy of CBT for social anxiety disorder, panic disorder and generalized anxiety disorder.
- 150.Emmrich A et al. Depression does not affect the treatment outcome of CBT for panic and agoraphobia: results from a multicenter randomized trial. Psychother. Psychosom 81, 161–172 (2012). [DOI] [PubMed] [Google Scholar]
- 151.Hofmann SG, Wu JQ & Boettcher H Effect of cognitive–behavioral therapy for anxiety disorders on quality of life: a meta-analysis. J. Consult. Clin. Psychol 82, 375–391 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Loerinc AG et al. Response rates for CBT for anxiety disorders: need for standardized criteria. Clin. Psychol. Rev 42, 72–82 (2015). [DOI] [PubMed] [Google Scholar]
- 153.Ishikawa S, Okajima I, Matsuoka H & Sakano Y Cognitive behavioural therapy for anxiety disorders in children and adolescents: a meta-analysis. Child Adolesc. Ment. Health 12, 164–172 (2007). [DOI] [PubMed] [Google Scholar]
- 154.Vøllestad J, Nielsen MB & Nielsen GH Mindfulness- and acceptance-based interventions for anxiety disorders: a systematic review and meta-analysis. Br. J. Clin. Psychol 51, 239–260 (2012). [DOI] [PubMed] [Google Scholar]
- 155.Keefe JR, McCarthy KS, Dinger U, Zilcha-Mano S & Barber JP A meta-analytic review of psychodynamic therapies for anxiety disorders. Clin. Psychol. Rev 34, 309–323 (2014). [DOI] [PubMed] [Google Scholar]
- 156.Cuijpers P, Donker T, Weissman MM, Ravitz P & Cristea IA Interpersonal psychotherapy for mental health problems: a comprehensive meta-analysis. Am. J. Psychiatry 173, 680–687 (2016). [DOI] [PubMed] [Google Scholar]
- 157.Vos SPF, Huibers MJH, Diels L & Arntz A A randomized clinical trial of cognitive behavioral therapy and interpersonal psychotherapy for panic disorder with agoraphobia. Psychol. Med 42, 2661–2672 (2012). [DOI] [PubMed] [Google Scholar]
- 158.Higa-McMillan CK, Francis SE, Rith-Najarian L & Chorpita BF Evidence base update: 50 years of research on treatment for child and adolescent anxiety. J. Clin. Child Adolesc. Psychol 45, 91–113 (2016). [DOI] [PubMed] [Google Scholar]; This review provides a thorough and systematic evaluation of the key active components in treatments for anxious youths.
- 159.Griebel G & Holmes A 50 years of hurdles and hope in anxiolytic drug discovery. Nat. Rev. Drug Discov 12, 667–687 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Murrough JW, Yaqubi S, Sayed S & Charney DS Emerging drugs for the treatment of anxiety. Expert Opin. Emerg. Drugs 20, 393–406 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Ravindran LN & Stein MB The pharmacologic treatment of anxiety disorders. J. Clin. Psychiatry 71, 839–854 (2010). [DOI] [PubMed] [Google Scholar]; A review paper focusing on advances in pharmacotherapy for anxiety disorders up to 2010.
- 162.Sadock BJ, Kaplan HI, Sadock VA & Ruiz P Kaplan and Sadock’s Comprehensive Textbook of Psychiatry 10th edn Vol. 1 (Lippincott Williams & Wilkins, 2017, forthcoming). [Google Scholar]
- 163.Gommoll C et al. A double-blind, randomized, placebo-controlled, fixed-dose phase III study of vilazodone in patients with generalized anxiety disorder. Depress. Anxiety 32, 451–459 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Stein DJ et al. Agomelatine in generalized anxiety disorder. J. Clin. Psychiatry 75, 362–368 (2014). [DOI] [PubMed] [Google Scholar]
- 165.Baldwin DS et al. Evidence-based pharmacological treatment of anxiety disorders, post-traumatic stress disorder and obsessive-compulsive disorder: a revision of the 2005 guidelines from the British Association for Psychopharmacology. J. Psychopharmacol 28, 403–439 (2014). [DOI] [PubMed] [Google Scholar]; Guidelines from the British Association for Psychopharmacology on pharmacological treatment options for anxiety disorders.
- 166.Gray SL Benzodiazepine use and risk of incident dementia or cognitive decline: prospective population based study. BMJ. 352, i90 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Kreys T-JM & Phan SVA Literature review of quetiapine for generalized anxiety disorder. Pharmacother. J. Hum. Pharmacol. Drug Ther 35, 175–188 (2015). [DOI] [PubMed] [Google Scholar]
- 168.Steenen SA et al. Propranolol for the treatment of anxiety disorders: systematic review and meta-analysis. J. Psychopharmacol 30, 128–139 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Mohatt J, Bennett SM & Walkup JT Treatment of separation, generalized, and social anxiety disorders in youths. Am. J. Psychiatry 171, 741–748 (2014). [DOI] [PubMed] [Google Scholar]
- 170.Wehry AM, Beesdo-Baum K, Hennelly MM, Connolly SD & Strawn JR Assessment and treatment of anxiety disorders in children and adolescents. Curr. Psychiatry Rep 17, 52 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Bridge JA et al. Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment. JAMA 297, 1683–1696 (2007). [DOI] [PubMed] [Google Scholar]
- 172.Marchesi C et al. Clinical management of perinatal anxiety disorders: a systematic review. J. Affect. Disord 190, 543–550 (2016). [DOI] [PubMed] [Google Scholar]
- 173.Cuijpers P et al. The efficacy of psychotherapy and pharmacotherapy in treating depressive and anxiety disorders: a meta-analysis of direct comparisons. World Psychiatry 12, 137–148 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Cuijpers P et al. Adding psychotherapy to antidepressant medication in depression and anxiety disorders: a meta-analysis. World Psychiatry 13, 56–67 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Piacentini J et al. 24- and 36-week outcomes for the Child/Adolescent Anxiety Multimodal Study (CAMS). J. Am. Acad. Child Adolesc. Psychiatry 53, 297–310 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Ginsburg GS et al. Naturalistic follow-up of youths treated for pediatric anxiety disorders. JAMA Psychiatry 71, 310–318 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Heldt E et al. Predictors of relapse in the second follow-up year post cognitive–behavior therapy for panic disorder. Rev. Bras. Psiquiatr 33, 23–29 (2D). [DOI] [PubMed] [Google Scholar]
- 178.van Apeldoorn FJ et al. A randomized trial of cognitive-behavioral therapy or selective serotonin reuptake inhibitor or both combined for panic disorder with or without agoraphobia. J. Clin. Psychiatry 71, 574–586 (2010). [DOI] [PubMed] [Google Scholar]
- 179.White KS et al. Does maintenance CBT contribute to long-term treatment response of panic disorder with or without agoraphobia? A randomized controlled clinical trial. J. Consult. Clin. Psychol 81, 47–57 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Craske MG et al. CBT intensity and outcome for panic disorder in a primary care setting. Behav. Ther 37, 112–119 (2006). [DOI] [PubMed] [Google Scholar]
- 181.Scholten WD, Batelaan NM, van Oppen P, Smit JH & van Balkom AJLM Discontinuation of antidepressants in remitted anxiety disorder patients: the need for strategies to prevent relapse. Psychother. Psychosom 82, 399–400 (2013). [DOI] [PubMed] [Google Scholar]
- 182.Donovan MR, Glue P, Kolluri S & Emir B Comparative efficacy of antidepressants in preventing relapse in anxiety disorders — a meta-analysis. J. Affect. Disord 123, 9–16 (2010). [DOI] [PubMed] [Google Scholar]
- 183.Perna G, Alciati A, Riva A, Micieli W & Caldirola D Long-term pharmacological treatments of anxiety disorders: an updated systematic review. Curr. Psychiatry Rep 18, 23 (2016). [DOI] [PubMed] [Google Scholar]
- 184.Schneider RL, Arch JJ & Wolitzky-Taylor KB The state of personalized treatment for anxiety disorders: a systematic review of treatment moderators. Clin. Psychol. Rev 38, 39–54 (2015). [DOI] [PubMed] [Google Scholar]
- 185.Hudson JL et al. Clinical predictors of response to cognitive–behavioral therapy in pediatric anxiety disorders: the Genes for Treatment (GxT) Study. J. Am. Acad. Child Adolesc. Psychiatry 54, 454–463 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Bittner A et al. What characteristics of primary anxiety disorders predict subsequent major depressive disorder? J. Clin. Psychiatry 65, 618–626 (2004). [DOI] [PubMed] [Google Scholar]
- 187.Castaneda AE, Tuulio-Henriksson A, Marttunen M, Suvisaari J & Lönnqvist J A review on cognitive impairments in depressive and anxiety disorders with a focus on young adults. J. Affect. Disord 106, 1–27 (2008). [DOI] [PubMed] [Google Scholar]
- 188.Eysenck MW, Derakshan N, Santos R & Calvo MG Anxiety and cognitive performance: attentional control theory. Emotion 7, 336–353 (2007). [DOI] [PubMed] [Google Scholar]
- 189.Kessler RC et al. The global burden of mental disorders: an update from the WHO World Mental Health (WMH) surveys. Epidemiol. Psichiatr. Soc 18, 23–33 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Saeed Mirza S, Ikram MA, Hofman A & Tiemeier H Anxiety does not predict mortality. A population-based study. World Psychiatry 14, 103–104 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Whiteford HA et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 382, 1575–1586 (2013). [DOI] [PubMed] [Google Scholar]
- 192.Hoagwood K & Olin SS The NIMH blueprint for change report: research priorities in child and adolescent mental health. J. Am. Acad. Child Adolesc. Psychiatry 41, 760–767 (2002). [DOI] [PubMed] [Google Scholar]
- 193.Holmes EA, Craske MG & Graybiel AM Psychological treatments: a call for mental-health science. Nature 511, 287–289 (2014). [DOI] [PubMed] [Google Scholar]
- 194.Waters AM & Craske MG Towards a cognitive-learning formulation of youth anxiety: a narrative review of theory and evidence and implications for treatment. Clin. Psychol. Rev 50, 50–66 (2016). [DOI] [PubMed] [Google Scholar]
- 195.Bouton ME Context, ambiguity, and unlearning: sources of relapse after behavioral extinction. Biol. Psychiatry 52, 976–986 (2002). [DOI] [PubMed] [Google Scholar]
- 196.Craske MG, Treanor M, Conway CC, Zbozinek T & Vervliet B Maximizing exposure therapy: an inhibitory learning approach. Behav. Res. Ther 58, 10–23 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Ori R et al. Augmentation of cognitive and behavioural therapies (CBT) with d-cycloserine for anxiety and related disorder. Cochrane Database Syst. Rev 10, CD007803 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Kredlow MA, Unger LD & Otto MW Harnessing reconsolidation to weaken fear and appetitive memories: a meta-analysis of post-retrieval extinction effects. Psychol. Bull 142, 314–336 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Hardwicke TE, Taqi M & Shanks DR Postretrieval new learning does not reliably induce human memory updating via reconsolidation. Proc. Natl Acad. Sci. USA 113, 5206–5211 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Christensen H, Batterham P & Calear A Online interventions for anxiety disorders. Curr. Opin. Psychiatry 27, 7–13 (2014). [DOI] [PubMed] [Google Scholar]
- 201.Olthuis JV, Watt MC, Bailey K, Hayden JA & Stewart SH Therapist-supported Internet cognitive behavioural therapy for anxiety disorders in adults. Cochrane Database Syst. Rev 12, CD011565 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]; This Cochrane review summarizes the evidence supporting the use of Internet-based CBTs for anxiety disorders.
- 202.Ye X et al. Effectiveness of Internet-based interventions for children, youth, and young adults with anxiety and/or depression: a systematic review and meta-analysis. BMC Health Serv. Res 14, 313 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Pennant ME et al. Computerised therapies for anxiety and depression in children and young people: a systematic review and meta-analysis. Behav. Res. Ther 67, 1–18 (2015). [DOI] [PubMed] [Google Scholar]
- 204.Cristea IA, Kok RN & Cuijpers P Efficacy of cognitive bias modification interventions in anxiety and depression: meta-analysis. Br. J. Psychiatry 206, 7–16 (2015). [DOI] [PubMed] [Google Scholar]
- 205.Heeren A, Mogoase C, Philippot P & McNally RJ Attention bias modification for social anxiety: a systematic review and meta-analysis. Clin. Psychol. Rev 40, 76–90 (2015). [DOI] [PubMed] [Google Scholar]
- 206.van Ginneken N et al. Non-specialist health worker interventions for the care of mental, neurological and substance-abuse disorders in low- and middle-income countries. Cochrane Database Syst. Rev 19, CD009149 (2013). [DOI] [PubMed] [Google Scholar]; This Cochrane review presents evidence for mental health treatments, including treatments for anxiety, delivered by non-specialists in low-to-middle-income countries.
- 207.Kobak KA, Craske MG, Rose RD & Wolitsky-Taylor K Web-based therapist training on cognitive behavior therapy for anxiety disorders: a pilot study. Psychotherapy 50, 235–247 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Craske MG et al. Disorder-specific impact of coordinated anxiety learning and management treatment for anxiety disorders in primary care. Arch. Gen. Psychiatry 68, 378–388 (2D). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Gilmartin MR, Balderston NL & Helmstetter FJ Prefrontal cortical regulation of fear learning. Trends Neurosci. 37, 455–464 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Dunsmoor JE & Paz R Fear generalization and anxiety: behavioral and neural mechanisms. Biol. Psychiatry 78, 336–343 (2015). [DOI] [PubMed] [Google Scholar]
- 211.Singewald N, Schmuckermair C, Whittle N, Holmes A & Ressler KJ Pharmacology of cognitive enhancers for exposure-based therapy of fear, anxiety and trauma-related disorders. Pharmacol. Ther 149, 150–190 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Insel T et al. Research Domain Criteria (RDoC): toward a new classification framework for research on mental disorders. Am. J. Psychiatry 167, 748–751 (2010). [DOI] [PubMed] [Google Scholar]
- 213.Sanislow CA et al. Developing constructs for psychopathology research: research domain criteria. J. Abnorm. Psychol 119, 631–639 (2010). [DOI] [PubMed] [Google Scholar]
- 214.Wittchen H-U et al. Generalized anxiety and depression in primary care: prevalence, recognition, and management. J. Clin. Psychiatry 63 (Suppl. 8), 24–34 (2002). [PubMed] [Google Scholar]
- 215.van de Water T, Suliman S & Seedat S Gender and cultural issues in psychiatric nosological classification systems. CNS Spectr. 21, 334–340 (2016). [DOI] [PubMed] [Google Scholar]
- 216.Craske MG Cognitive–Behavioral Therapy (American Psychological Association, 2010). [Google Scholar]
- 217.Milad MR & Quirk GJ Fear extinction as a model for translational neuroscience: ten years of progress. Annu. Rev. Psychol 63, 129–151 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.McNaughton N The conceptual nervous system of J.A. Gray: anxiety and neuroticism. Neurosci. Biobehav. Rev 28, 227–228 (2004). [DOI] [PubMed] [Google Scholar]
- 219.Harris AZ & Gordon JA Long-range neural synchrony in behavior. Annu. Rev. Neurosci 38, 171–194 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Robinson OJ et al. Towards a mechanistic understanding of pathological anxiety: the dorsal medial prefrontal–amygdala ‘aversive amplification’ circuit in unmedicated generalized and social anxiety disorder. Lancet Psychiatry 1, 294–302 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Shin LM & Liberzon I The neurocircuitry of fear, stress, and anxiety disorders. Neuropsychopharmacology 35, 169–191 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Lanius RA, Bluhm R, Lanius U & Pain C A review of neuroimaging studies in PTSD: heterogeneity of response to symptom provocation. J. Psychiatr. Res 40, 709–729 (2006). [DOI] [PubMed] [Google Scholar]
- 223.Fonzo GA et al. Exaggerated and disconnected insular-amygdalar blood oxygenation level-dependent response to threat-related emotional faces in women with intimate-partner violence posttraumatic stress disorder. Biol. Psychiatry 68, 433–441 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Marin M-F et al. Association of resting metabolism in the fear neural network with extinction recall activations and clinical measures in trauma-exposed individuals. Am. J. Psychiatry 173, 930–938 (2016). [DOI] [PubMed] [Google Scholar]
- 225.Freitas-Ferrari MC et al. Neuroimaging in social anxiety disorder: a systematic review of the literature. Prog. Neuropsychopharmacol. Biol. Psychiatry 34, 565–580 (2010). [DOI] [PubMed] [Google Scholar]
- 226.Cremers HR et al. Altered cortical–amygdala coupling in social anxiety disorder during the anticipation of giving a public speech. Psychol. Med 45, 1521–1529 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Wittchen H-U et al. The need for a behavioural science focus in research on mental health and mental disorders. Int. J. Methods Psychiatr. Res 23, 28–40 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]


