Abstract
Background: Autism spectrum disorder (ASD) is a complex neurodevelopmental condition characterized by social communication challenges and repetitive behaviors. Recent research has increasingly focused on the genetic underpinnings of ASD, with the Neurexin 1 (NRXN1) gene emerging as a key player. This comprehensive systematic review elucidates the contribution of NRXN1 gene variants in the pathophysiology of ASD. Methods: The protocol for this systematic review was designed a priori and was registered in the PROSPERO database (CRD42023450418). A risk of bias analysis was conducted using the Joanna Briggs Institute (JBI) critical appraisal tool. We examined various studies that link NRXN1 gene disruptions with ASD, discussing both the genotypic variability and the resulting phenotypic expressions. Results: Within this review, there was marked heterogeneity observed in ASD genotypic and phenotypic manifestations among individuals with NRXN1 mutations. The presence of NRXN1 mutations in this population emphasizes the gene’s role in synaptic function and neural connectivity. Conclusion: This review not only highlights the role of NRXN1 in the pathophysiology of ASD but also highlights the need for further research to unravel the complex genetic underpinnings of the disorder. A better knowledge about the multifaceted role of NRXN1 in ASD can provide crucial insights into the neurobiological foundations of autism and pave the way for novel therapeutic strategies.
Keywords: NRXN1, autism spectrum disorder, gene variants, synaptic function, genotype–phenotype correlation, genetic predisposition
1. Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by reduced communication, repetitive behaviors, and restricted interests [1,2,3,4]. ASD can vary in severity from mild to severe. It not only imposes social and personal challenges on the affected individuals and their families or caregivers but also leads to significant financial impacts on them and the healthcare system [5]. Individuals diagnosed with ASD often need comprehensive interventions from an early age, such as physical therapy, occupational therapy, behavioral therapy, medical treatments, specialized education, and assistive technology [6,7]. Additionally, the economic implications are further compounded for those with more severe forms of ASD, who may struggle to achieve financial independence in adulthood.
The prevalence of ASD is gradually increasing leading to a growing economic impact. A study assessed past economic impacts to forecast future financial burdens in the United States at the state level by 2029. Their findings suggest that, if ASD prevalence remains consistent with 2019 levels, the economic impact would reach USD 11.5 trillion by 2029. However, if the prevalence continues to increase as it has in previous decades, the cost could soar to USD 15 trillion [7]. The financial implications of ASD are comparable to those of diabetes and exceed those of stroke and hypertension [6]. The escalating prevalence and substantial economic strain underscore the importance of understanding ASD’s etiology and identifying potential therapeutic targets. While the causes of ASD are multifaceted, genetic factors, combined with possible environmental factors, have been significantly linked to its development [8], with numerous genes potentially associated with it.
The Simons Foundation Autism Research Initiative (SFARI) (https://www.sfari.org/resource/sfari-gene/; Accessed on 15 October 2023) has assembled an open-access evolving database to comprehensively evaluate the role of individual genes in ASD, SFARI Gene. Using stringent and rigorous criteria, SFARI Gene is one of the most reliable databases for the autism research community to delve into the genetic underpinnings of ASD. A key feature of this database is the gene scoring system, where each gene is assigned a rating from 1 to 3, reflecting the robustness of evidence supporting its association with ASD. A designation of 1 indicates genes that have been clearly implicated in ASD with at least three de novo likely gene-disrupting mutations reported, each of which meets a threshold false discovery rate of <0.1. Designations 2 and 3 are genes with two or one reported de novo gene-disrupting mutations, respectively. Genes with the designation 1 are most likely to be truly implicated, while those designated 2 and 3 have an increasing likelihood of being a false positive. In addition, genes can have the designation of S, which means syndromic, indicating these genes carry a substantially increased risk with repeated evidence of their role in ASD. While numerous genes have been identified as having potential links to ASD, establishing a definitive causal relationship presents a greater challenge. SFARI uses an Evaluation of Autism Gene Link Evidence (EAGLE) score designation to help understand the causative relationship of a particular gene with ASD. The higher the EAGLE score for a gene, the higher the probability of it being causative in ASD. For genes with an EAGLE score of 12 or higher, their causative role in ASD is supported by consistent and repeated evidence from both research and clinical settings, and this relationship has been demonstrated over time. A designation of 12 and over also means there are no published papers that contradict its role in ASD. In this review, we have focused on NRXN1, which is a category 1 gene with the highest EAGLE score of 146. NRXN1 has been repeatedly and consistently shown to be strongly associated with ASD [9,10,11,12,13,14,15,16,17].
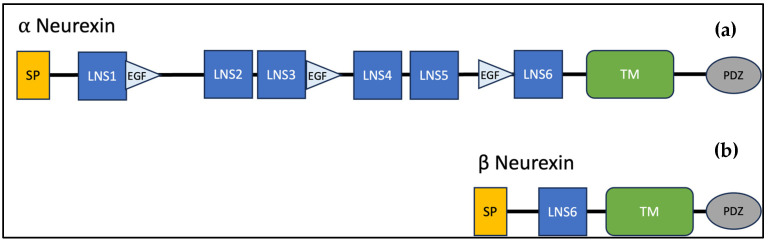
Increasingly, there is evidence that dysfunction at the level of the synapse is central to the pathophysiology of ASD [18,19,20,21,22,23,24,25]. NRXN1, located at 2p16.3, encodes neurexins, which are a family of presynaptic cell adhesion molecules that are central to creating and modifying synaptic connections and have been implicated in the pathophysiology of ASD and other neuropsychiatric disorders (Supplemental Figure S1) [8,11,13,25,26,27,28,29,30,31,32,33,34,35,36,37,38]. Neurexins are encoded by three genes (NRXN1, NRXN2, NRXN3), each of which contain two promoters, one for a longer alpha isoform and the other for a shorter beta isoform (Figure 1). The first promoter is located upstream of exon 1 and allows for transcription of alpha isoforms and the second promoter is located medially, between exon 17 and 18, to code the beta isoforms. These isoforms undergo extensive alternative splicing yielding over 1000 neurexin mRNAs. NRXN1 and NRXN3 are two of the largest mammalian genes. NRXN1 is 1.12 Mb long containing 24 exons, and multiple splice sites [8,39,40,41,42]. The translated protein is a transmembrane protein, which contains an extracellular domain, a transmembrane region, and an intracellular motif that controls downstream events (Figure 2). Alpha neurexin is comprised of six extracellular domains with three epidermal growth factor (EGF)-like regions [13,43,44]. Beta neurexins are smaller and contain only one extracellular domain. Both alpha and beta neurexins have been implicated in the pathophysiology of ASD [12,45,46,47]. The precise structure of neurexins has yet to be fully elucidated in humans but has been modeled from other mammals such as mice and rats.
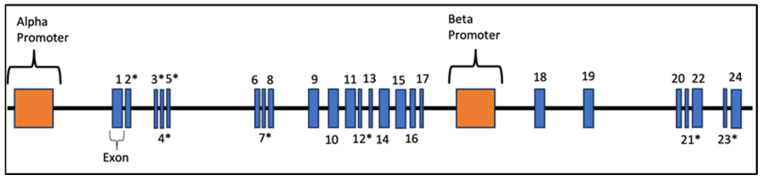
Figure 1.
NRXN1 gene structure. A schematic illustrating the organization of NRXN1 gene. Exons are depicted as blue boxes and numbered. Asterisks indicate exons where alternative splicing occurs. This image indicates the relative size and location of its exons and introns, as well as promoters. * indicates alternative splice site.
Figure 2.
Structural domain organization of both alpha and beta isoforms of neurexin. (a). Alpha neurexin. (b). Beta neurexin. SP, signal peptide; LNS, laminin/neurexin/sex hormone binding domain; EGF, epidermal factor-like region; TM, transmembrane domain; PDZ, PSD-95, DLG1, ZO-1 domains.
NRXN1 is essential for synaptic health in central nervous system (CNS) and peripheral nervous system (PNS) activity. It has been implicated in various neuropsychiatric conditions including ASD, attention deficit hyperactivity disorder (ADHD), seizures, schizophrenia, psychosis, and bipolar disorder [9,48,49,50,51,52,53]. NRXN1 plays a major role in the differentiation of synapses and is found in high concentrations in the supporting cells of the brain [54,55,56,57,58,59]. Deficits in NRXN1 have been associated with intellectual/learning disability and speech/language/global development delay, which are some of the hallmarks of ASD [12,29,45,60,61,62,63,64,65]. Moreover, research shows that children who harbor NRXN1 gene variants have behavioral problems such as aggression and tantrums, as well as balance and motor skill deficits [66]. These phenotypic expressions are consistent with those commonly observed in some individuals with ASD, providing important insights that could enhance our understanding of the relationship between ASD and NRXN1 mutations.
NRXN1 interacts with protein structures called Neuroligins. Neuroligins are postsynaptic molecules that bind with NRXNs to create a calcium-dependent complex [67,68]. This complex is crucial for neurotransmission and allows for the recruitment of neurotransmitter receptors as well as other structural proteins required for effective neurotransmission. Precise control over excitation and inhibition at the level of the synapse is vital for the appropriate function of the nervous system, with alterations having been linked to ASD pathology. Mutations in NRXN1 and other associated gene regions have been linked to both reduced and increased excitatory synaptic activity as well as decreased neurotransmitter release [69]. Notably, ASD is related to an imbalance of excitation and inhibition at the level of the synapse; however, the exact mechanism and direction of the imbalance is still under investigation [70].
The objective of this systematic review article is to comprehensively review the role of NRXN1 gene variants in the manifestations of ASD as well as to analyze the phenotypic outcomes. Enhancing our knowledge of the involvement of NRXN1 gene variants in the pathophysiology of ASD holds important clinical implications. This knowledge would facilitate the creation of tailored genetic counseling for affected individuals, informing patients as well as families and caregivers of more individualized disease outcomes and expectations. Additionally, this understanding could enable the development of effective treatment approaches, leveraging advanced genomic editing technologies such as CRISPR/Cas9 as well as more traditional drug regiments [71,72,73,74,75].
2. Materials and Methods
2.1. Search Strategy
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). The protocol for this systematic review was designed a priori and was registered in the PROSPERO database (registration number: CRD42023450418). A literature search was performed in PubMed, Embase, Web of Science, and SCOPUS databases using the MeSH terms; “NRXN1” AND “autism”; “Genetic impact of NRXN1” AND “autism”; “NRXN1 in ASD”; “NRXN1-associated autism”; “Neurexin 1 variants” AND “ASD clinical outcomes”; “Functional implications of NRXN1” IN “autism spectrum disorders”; and “NRXN1 and ASD/autism phenotypic manifestations”.
2.2. Study Selection
At least three reviewers (A.K., D.K., and J.C.) independently reviewed all searched articles, abstracts, and full-text publications. Any disagreements on the exclusion or inclusion of results were resolved by a fourth reviewer or senior author. All included studies required a diagnosis of ASD by gold-standard diagnostic criteria such as DSM 5, ADOS-2, and ADI. Study inclusion criteria included participant diagnosis of ASD at any age and publication between November 2018 and September 2023, as there were previous reviews available that updated the literature until November 2018. Study exclusion criteria included no formal ASD diagnosis, publication not in a peer-reviewed article, reviews, commentaries, conference proceedings, case reports/studies, non-human studies, ex-vivo or in-vitro studies, and studies not originally published in English.
2.3. Data Extraction
Three investigators (A.S., A.K., D.K., and J.C.) independently reviewed included articles. The information gathered includes: study type, population, comparison/study, ASD diagnosis criteria, outcomes/conclusions. After initial data extraction, each investigator gathered data on the zygosity, specific mutation, inheritance, intellectual abilities, speech abilities, physical characteristics, behavioral diagnoses, consanguinity, and gender.
2.4. Quality Assessment
A Risk of Bias (RoB) analysis was conducted using the Joanna Briggs Institute (JBI) Critical Appraisal Tool. The appropriate checklist was utilized based on the type of study. This assessment was completed by four reviewers (A.K., D.K., A.S., and J.C.) independently, with discrepancies resolved by discussion and consensus or discussion with the senior author.
3. Results and Discussion
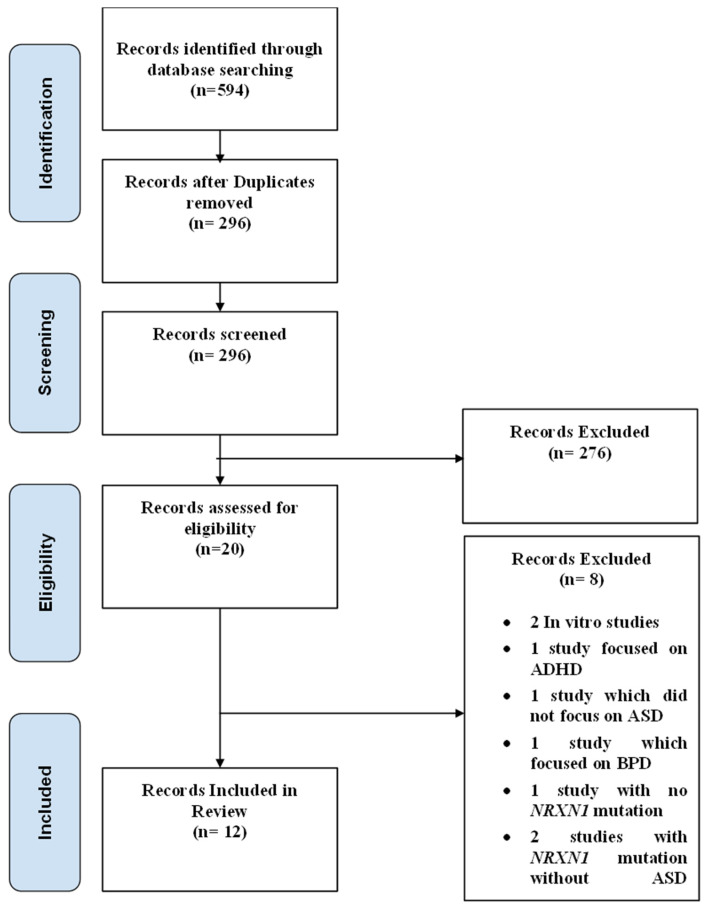
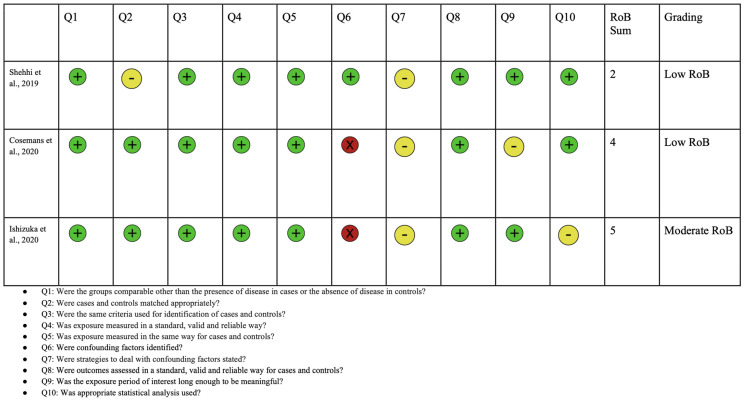
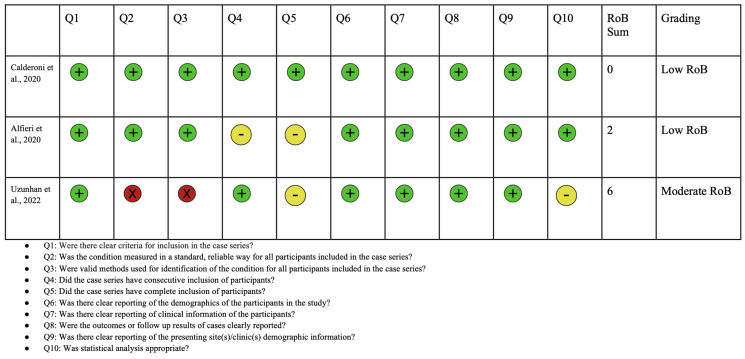
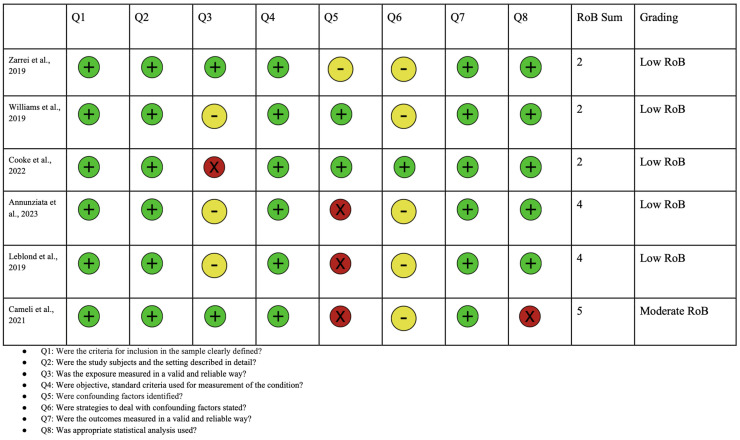
A PRISMA diagram showing the criteria for included studies in this systematic review article is shown in Figure 3. Following the initial search, a total of 594 studies were identified. Through screening, 296 records were selected excluding duplicates and irrelevant articles. After conducting a full-text review, 12 articles were chosen for inclusion in this study. This selection was made after excluding studies for reasons detailed in the PRISMA diagram, including irrelevance of outcomes to this study or to ASD. Each of the included articles provided data on mutations in the NRXN1 gene and their association with ASD. A risk of bias analysis was performed using the JBI critical appraisal checklist. Risk of bias analyses for case control, case series, and cross-sectional studies are shown in Figure 4, Figure 5, and Figure 6, respectively. Overall, the studies included in this systematic review were found to have a low risk of bias and were deemed to be of suitable quality for inclusion.
Figure 3.
PRISMA flow diagram for study selection: This figure represents a PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram, showing the detailed process of study selection for this systematic review.
Figure 4.
Risk of bias analysis using Joanna Briggs Institute for case control studies. Green circle represents low bias, yellow circle represents unclear, and red indicates high bias [60,76,77].
Figure 5.
Risk of bias analysis using Joanna Briggs Institute for case series studies. Green circle represents low bias, yellow circle represents unclear, and red indicates high bias [78,79,80].
Figure 6.
Risk of bias analysis using Joanna Briggs Institute for cross sectional studies. Green circle represents low bias, yellow circle represents unclear, and red indicates high bias [27,36,81,82,83,84].
3.1. Patient Population and Diagnosis
The total number of individuals with ASD included in this study is 2247, with a subset of 71 participants found to also carry a mutation in NRXN1. Of those with both ASD and an NRXN1 mutation 57.8% were male and 21% were female (21% of the cohort had no gender specified in the study). The diagnostic methods used for ASD in each study has been summarized in Table 1.
Table 1.
Diagnostic tests for ASD.
| Study | Diagnostic Test for ASD |
|---|---|
| Alfieri et al. [78], 2020 | ADOS2 |
| Annunziata et al. [81], 2023 | DSM5 |
| Calderoni et al. [79], 2020 | DSM 5 |
| Cameli et al. [82], 2021 | ADOS |
| Cooke et al. [27], 2022 | DSM 5 or ICD |
| Cosemans et al. [76], 2020 | DSM 5 |
| Ishizuka et al. [77], 2020 | DSM 5 |
| Leblond et al. [36], 2019 | ICD-10 criteria for childhood autism/autistic disorder Gillberg criteria for Asperger syndrome ICD-10 criteria for atypical autism with the added requirement that a case thus diagnosed could not meet full criteria for childhood autism or Asperger syndrome ICD-10 criteria for disintegrative disorder |
| Shehhi et. Al. [60], 2019 | Gold standard test—unspecified |
| Uzunhan et al. [80], 2022 | Gold standard test—unspecified |
| Williams et al. [83], 2019 | DSM 4 |
| Zarrei et al. [84], 2019 | ICD11 or DSMV |
3.2. Genotypic Variants of NRXN1 in Individuals with ASD
As genetic sequencing becomes more affordable and accessible, delving into the genetic underpinnings of variable clinical presentations has been at the forefront of research. In line with this, each included study in our review conducted genetic testing on groups of individuals with ASD to explore genetic factors. The estimated rate of NRXN1 variants in the general population is thought to be around 0.21% [85]. The prevalence of NRXN1 mutation in this population is 3.1% of all patients included who had a diagnosis of ASD.
In all studies, the parents of affected children who also harbored NRXN1 mutations were found to be undiagnosed with ASD, thereby serving as carriers of the genetic variations. This finding highlights the multifaceted nature of ASD and the idea that multiple factors occurring together may be needed for the phenotypic clinical expression. The predominant trend observed was exonic deletion mutations [49,63,71,72,73,74,75,85]. An overview of genotypic information is shown in Table 2. Exons are segments of the gene that are translated into proteins, thereby directly affecting synaptic health and function. This finding is particularly significant given that NRXN1 expression is predominantly found in the CNS and reaches its highest expression levels during periods of critical neurodevelopment [8,86]. As previously stated, the two main isoforms for NRXN1 are a longer alpha isoform and a shorter beta isoform. Six of the included studies observed that the alpha isoforms were affected, comprising 20 individuals, and two studies found the beta isoform to be affected across three individuals [78,80,83]. There is a low penetrance of NRXN1 mutations, as evidenced by the lack of ASD manifestation in all parental or sibling carriers involved in these studies as well as data from previous studies [87]. However, it appears that these mutations still confer a risk for ASD development when combined with other genetic factors or exposure to environmental factors such as environmental toxins, drugs, pollution, or gestational/perinatal events. In the studies reviewed, three reported participants with heterozygous mutations, one observed a homozygous mutation, and six did not specify the mutation status of the patients. Previously, heterozygous NRXN1 mutations have been associated with ASD among other reported neuropsychiatric disorders [46]. Overall, deletions comprised a majority of the mutations described in these studies. Given the observed association between NRXN1 mutations and ASD, these genetic modifications are considered crucial in understanding not only ASD but also other neuropsychiatric and behavioral disorders. Therefore, a deeper examination of the connection between the NRXN1 gene and ASD is vital to comprehend how this gene influences the ASD phenotype and its prognosis. Table 3 has an overview of the mutations found in each patient from the included studies.
Table 2.
An overview of genotypic information.
| Reference | Total ASD Cases | Total ASD and NRXN1 Nutation Cases | Mutation in Alpha Isoform | Mutation in Beta Isoform | Unspecified Mutated Isoform | Number of Exonic Deletion | Number of Intronic Deletions | Frequency of Exonic Deletion | Frequency of Intronic Deletion | Homozygous Mutation | Heterozygous Mutation |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Alfieri et al. [78], 2020 | 5 | 3 | NR | NR | 3 | 0 | 0 | NR | NR | 0 | 3 |
| Annunziata et al. [81], 2023 | 209 | 3 | NR | NR | 3 | 0 | 0 | NR | NR | NR | NR |
| Calderoniet al. [79], 2020 | 93 | 2 | NR | NR | 2 | 0 | 0 | NR | NR | NR | NR |
| Cameli et al. [82], 2021 | 104 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | NR | NR |
| Cooke et al. [27], 2022 | 69 | 12 | NR | NR | 12 | 0 | 0 | NR | NR | NR | NR |
| Cosemans et al. [76], 2020 | 43 | 17 | NR | NR | 17 | 0 | 0 | NR | NR | NR | NR |
| Ishizuka et al. [77], 2020 | 192 | 5 | 3 | 0 | 2 | 3 | 0 | 0.6 | 0 | 0 | 5 |
| Leblond et al. [36], 2019 | 36 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | NR | NR |
| Shehhi et. Al. [60], 2019 | 20 | 20 | 13 | 2 | 5 | 13 | 7 | 0.65 | 0.35 | NR | NR |
| Uzunhan et al. [80], 2022 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 |
| Williams et al. [83], 2019 | 48 | 1 | 1 | 0 | 0 | 0 | 0 | NR | NR | 0 | 1 |
| Zarrei et al. [84], 2019 | 1838 | 6 | NR | NR | 6 | 6 | 0 | 1 | 0 | NR | NR |
NR: not recorded.
Table 3.
Mutations in the review population.
| Reference | Mutation Location |
|---|---|
| Alfieri et al. [78], 2020 | arr[GRCh37] 2p16.3(50432664_50536137)x1 mat, arr[GRCh37] 2p16.3(51086847_51411126) x1 mat, arr [GRCh37] 2p16.3(51037104_52339655)x1 pat. |
| Annunziata et al. [81], 2023 | arr[GRCh37/hg19] 2p16.3(51066578_51100412)x1, arr[GRCh37/hg19] 2p16.3(51175725_51328842)x1 mat, arr[GRCh37/hg19] 2p16.3(50039172_50735499)x1 mat, |
| Calderoni et al. [79], 2020 | arr[GRCh37/hg19] 2p16.3 (50909765_51083469) 1x pat |
| Cameli et al. [82], 2021 | 2p16.3 (NC_000002.11:g.50170766_50982172del) |
| Cooke et al. [27], 2022 | unspecified from SynaG cohort |
| Cosemans et al. [76], 2020 | arr[GRCh37/hg19] 2p16.3 (50453695_50662935), arr[GRCh37/hg19] 2p16.3 (50879191_50953066) mat, arr[GRCh37/hg19] 2p16.3 (50620243_50970739), arr[GRCh37/hg19] 2p16.3 (51017528_51302432) mat, arr[GRCh37/hg19] 2p16.3 (50898653_51104632) pat, arr[GRCh37/hg19] 2p16.3 (50923553_51034676) pat, arr[GRCh37/hg19] 2p16.3 (51033135_51074619), arr[GRCh37/hg19] 2p16.3 (51033989_51062766), arr[GRCh37/hg19] 2p16.3 (50992089_51026709), arr[GRCh37/hg19] 2p16.3 (51027631_51390231), arr[GRCh37/hg19] 2p16.3 (51039779_51297569) mat, arr[GRCh37/hg19] 2p16.3 (50497204_50514746) mat, arr[GRCh37/hg19] 2p16.3 (50497204_50514746) mat, arr[GRCh37/hg19] 2p16.3 (51053925_51319222) mat, arr[GRCh37/hg19] 2p16.3 (50975806_51005275), arr[GRCh37/hg19] 2p16.3 (51063155_51278187), arr[GRCh37/hg19] 2p16.3 (51160878_51356269) pat |
| Ishizuka et al. [77], 2020 | rs201336161, rs201881725, rs1457374261, rs199970666 |
| Leblond et al. [36], 2019 | del(2p16:51125625-51255427) |
| Shehhi et. Al. [60], 2019 | Del(2p16.3:50,138,031–50,214,776), Del(2p16.3: Del(2p16.3:50,138,031–50,214,776), Del(2p16.3: Del(2p16.3: 50,483,652–50,495,891), Del(2p16.3: Del(2p16.3: 50,483,652–50,495,891), Del(2p16.3: Del(2p16.3: 50,690,984–50,870,064), Del(2p16.3: Del(2p16.3: 50,881,995–50,947,729), Del(2p16.3: Del(2p16.3: 50,947,670–50,964,907), Del(2p16.3: Del(2p16.3: 50,957,455–51,251,557), Del(2p16.3: Del(2p16.3: 50,964,848–51,251,557), Del(2p16.3: Del(2p16.3: 50,968,453–51,260,612), Del(2p16.3: Del(2p16.3: 50,982,113–51,446,873), Del(2p16.3: Del(2p16.3: 51,057,824–51,142,908), Del(2p16.3: Del(2p16.3: 51,083,410–51,172,182), Del(2p16.3: Del(2p16.3: 51,122,091–51,314,430), Del(2p16.3: Del(2p16.3: 51,122,091–51,382,872), Del(2p16.3: Del(2p16.3: 51,122,091–51,606,257), Del(2p16.3: Del(2p16.3: 51,137,071–51,314,430), Del(2p16.3: Del(2p16.3: 51,148,508–51,251,557), Del(2p16.3: Del(2p16.3: 51,153,052–51,260,612), Del(2p16.3: Del(2p16.3: 51,237,000–51,260,612) |
| Uzunhan et al. [80], 2022 | Del(2p16.3:chr2:51149007–51255411) |
| Williams et al. [83], 2019 | chr2:50847195; rs78540316 |
| Zarrei et al. [84], 2019 | Del(2p16.3:50,138,031–50,996,179)pat, Del(2p16.3: 50,986,743–51,644,735), Del(2p16.3: 51,125,058–51,263,149), Del(2p16.3: 51,141,571–51,363,855)pat, Del(2p16.3: 51,163,235–51,285,498)pat, Del(2p16.3: 51,163,990–51,285,498)pat |
This review focuses on the mutations found within NRXN1 and its subsequent phenotypic and genotypic profiles. When examining the included articles an unexpected finding was the role of non-coding RNA regions, which affected the expression of genes. These were discussed by Williams et al., Zarrei et al., and Annunziata et al. While not a focal point of this review, these adjacent mutations are important to discuss. Williams et al. found that SNV in miR-873-5p affect the expression of 109 SFARI candidate genes. Zarrei et al. and Annunziata et al. found mutations that disrupted the transcription of AK127244 (LOC730100), which is a non-coding RNA of unknown function adjacent to NRXN1 [81,84]. Annunziata et al. also found a mutation in a small segment distal to NRXN1 that similarly impacted the functioning of the gene products. This emerging field of study involving the pathological effects of long non-coding RNAs (lncRNAs) is gaining interest, especially since they are more abundant in the human brain when compared to protein-coding RNAs [88]. This abundance hints at their potential role in neuropsychiatric diseases [77]. lncRNAs also play a critical role in the normal functioning of various physiological systems in humans and are associated with various disease states, including cancers, neurological disorders, and cardiovascular diseases [83]. AK127244 is associated with deletions in 2p16.3, which is located within close proximity to NRXN1 and has been noted to induce similar clinical characteristics as mutations directly affecting NRXN1 [89,90]. These mutations are not, on their own, causative of ASD. However, in conjunction with another mutation, such as those from the SFARI database, they play a role in expression of the ASD phenotype.
Consanguinity is often investigated in relation to genetic disorders, particularly those that are transmitted recessively across generations, such as NRXN1. When two individuals who are closely related have children, it increases the occurrence of recessive genetic disorders when compared with unrelated pairings. Uzunhan et al. studied two specific cases—two siblings with consanguineous parents, each with an NRXN1 deletion. One sibling had a diagnosis of West syndrome while the other had a diagnosis of ASD. West syndrome is an encephalopathy that presents as infantile spasms and may include neurodevelopmental delays/regression. It should be noted that up to 20% of people with West syndrome have a diagnosis of ASD at some point in their lifetime [80,91,92,93]. CNV analyses of these patients found an NRXN1 exon 2–5 homozygous deletion that affected the alpha-isoform in both siblings. This mutation was confirmed with gel electrophoresis and compared with four healthy control individuals.
The genotypic findings of these articles are non-uniform and cannot be used to make conclusive relationships between NRXN1 mutations and ASD. Many included articles had only a handful of participants with both ASD and NRXN1 mutations and contain inconsistent reporting of genetic information across studies. Further studies having large cohorts are warranted to decipher the precise role of NRXN1 mutations in the pathophysiology of ASD.
3.3. Phenotypic Features of NRXN1 Mutations and ASD
3.3.1. Intellectual Abilities
The phenotype of individuals harboring NRXN1 variants is vast and heterogenous. ASD is known to affect males at a rate almost four times higher than for females, which is reflected in this cohort [94]. Intellectual abilities were recorded in six studies, 24% of participants with both ASD and a NRXN1 mutation were observed to have an intellectual disability and 14% were found to have no intellectual disability as measured by a standard questionnaire. The remaining 62% of participants had no recording of intellectual ability or were unable to complete the required tests for a determination of intellectual ability, which is in line with previous findings of diagnosed intellectual disability in those with NRXN1 mutations [66].
3.3.2. Speech Abilities
One major challenge was the lack of consistent reporting on both genotypic and phenotypic data from all included articles, many primarily focused on the genetic or phenotypic aspects of ASD, with minimal emphasis on the alternative aspect. In the included individuals with ASD and an NRXN1 mutation, 2.7% were verbal, 5.5% were non-verbal, and 29% were designated as having a speech delay; the remainder had no recorded information on verbal abilities [60,78,79,82,95].
3.3.3. Behavior/Neuropsychiatric Diagnosis
Many of the participants had behavioral problems including aggression and attention deficits. Alfieri et al. found two of their three individuals with ASD to be aggressive and Ishizuka et al. found one patient with a diagnosis of oppositional defiant disorder. Al Shehhi et al. and Ishizuka et al. had participants with diagnosed ADHD. Cameli et al. found their participant with ASD and an NRXN1 mutation to have hyperactive behaviors, but no confirmed ADHD diagnosis. The remainder of the studies did not collect data on comorbid ADHD, or it was not reported. These behavioral findings coincide with prior studies that found NRXN1 to be associated with aggression and attention deficits in animal models [96,97].
Cosemans et al. evaluated the association between having a diagnosis of a neurodevelopmental or neuropsychiatric condition and possessing the NRXN1 deletion [76]. This study used two cohorts of patients: a literature cohort of 670 individuals and a Leuven cohort of 43 individuals. Controls included patients who were screened for intellectual disability, developmental disorder, ASD, or schizophrenia. In this study, they found that individuals in the literature cohort who did not have a confirmed neurodevelopmental and neuropsychiatric condition were less likely to have the NRXN1 deletion than those who had the phenotype. The authors suggested that this relationship had concerns about reporting bias as the phenotypes associated with intrinsic patients are not commonly reported. Two exon deletions were analyzed: exons 1–5 and 5–24. The deletions for exon 1–5 was seen in 20 controls (12.59 penetrance) and the deletions for exon 6–24 was seen 2 times in 100,000 individuals (32.43 penetrance). In patients who were diagnosed with intellectual or developmental disability, 133/260 had deletions in the NRXN1 gene. Deletions were seen in 245/458 individuals with a psychiatric diagnosis. Additionally, psychiatric diagnoses were seen the most with deletions in exon 1- 5 and intron 5. Deletions in exons 6–24 had the greatest association with diagnoses of intellectual and developmental disability (43/68). Our analysis only included that of the Leuven cohort as these data are previously unanalyzed. In the Leuven cohort, they found that patients with de novo deletions of exons 1–5 had phenotypes of intellectual disability and autism. Patients with a maternally inherited deletion of exons 1–5 had ASD with some intellectual disability and psychiatric symptoms (delusions and psychotic episodes). Patients with maternally inherited deletions of exons 6–9 had developmental delay, hypertelorism, and inner epicanthal folds. Patients with a de novo exon 19 deletion had ASD, intellectual disability, and anxiogenic and behavioral deficits. These NRXN1 deletions were also seen in 143/258, 73/144, 63/125, and 44/88 individuals with ASD, schizophrenia, congenital abnormalities, and epilepsy, respectively. This study serves as an outstanding model for integrating genotypic as well as phenotypic information and should be a guiding reference for future analyses involving NRXN1 and ASD.
3.3.4. Physical Characteristics
Physically, there were no recurrent abnormalities observed to be present across the included cohorts. Macrocephaly or relative macrocephaly was noted in two participants and facial dysmorphia in four. There are single incidences of physical abnormalities such as pyloric stenosis, sensorineural hearing loss and pectus excavatum but no incidences of repeated patterns of these disorders. Prior studies have noted the presence of epilepsy in those with ASD and NRXN1 mutations. Eight participants were noted to have seizures but no documented epilepsy diagnoses. There were no incidences of brain, cardiac, or urogenital abnormalities in the included cohort.
Many of the participants in this review had comorbid motor and behavioral symptoms; however, the precise symptoms varied greatly. A comprehensive overview of the phenotypic manifestations reported in the included studies along with patient population summary and diagnosis has been shown in Table 4. Expanding the scope of research to include larger studies that meticulously document all phenotypic information of the participants could lead to a more comprehensive understanding of phenotypic patterns. These studies, by encompassing a broader range of phenotypic data, can provide deeper insights into variations and commonalities among individuals. This in turn might reveal subtler correlations or trends that smaller studies might miss. By gathering a comprehensive range of phenotypic information, researchers are able to more effectively identify and understand the subtleties within these patterns, potentially leading to more targeted and effective interventions or therapies.
Table 4.
A comprehensive summary of included studies in this systematic review.
| Reference | NRXN1 Isoform Effected |
Other Molecular Findings |
Parental Consanguinity |
Family History | Developmental Delay |
Intellectual Disability | Seizures | EEG | Motor Abnormalities (Movement, Speech) |
Sensory abnormalities (Hearing, Vision) |
Behavioral Abnormalities |
Other |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Calderoni et al. [79], 2020. Case 1 |
NR | NR | NR | NR | NR | Normal IQ (>70) | NR | NR | Verbal/non-verbal | none | none | n/a |
| Calderoni et al. [79], 2020. Case 2 |
NR | duplication at Xp22.33 | NR | NR | NR | Low IQ (<70) | NR | NR | none | none | none | n/a |
| Alfieri et al. [78], 2020. Case 1 | NR | None | NR | NR | NR | Below average on TDQ (30) | - | - | Hypotonia, no speech | none | Tantrums, aggression, self-injurious behavior | Trichotillomania, teeth grinding |
| Alfieri et al. [78], 2020. Case 2 | NR | None | NR | NR | NR | Below average TDQ (44) | - | - | Chewing difficulties only babbles | none | none | Smoking and medication exposure in utero |
| Alfieri et al. [78], 2020. Case 3 | NR | None | NR | NR | NR | Below average NVIQ (74) | + | - | Motor dysregulation | none | Attention problems | Multiple ear infections |
| Alfieri et al. [78], 2020. Case 4 | NR | None | NR | NR | NR | Below average FSIQ (50) | - | - | none | none | Paranoid ideation, aggressive behavior | allergies, sIgA deficiency, recurrent respiratory infections |
| Alfieri et al. [78], 2020. Case 5 | NR | None | NR | NR | NR | Below average NVIQ (72) | n/a | n/a | none | soliloquy | Shy, withdrawing, avoidant behavior | IUGR, sleep problems |
| Zarrei et al. [84], 2019 | NR | AK12724 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Cooke et al. [27], 2022 | Alpha, beta, theta | n/a | n/a | ASD, ADHD, anxiety, depression | yes | Below average to average | no | yes | Eye movements/gaze patterns | no | Repetitive and restrictive behaviors | n/a |
| Cosemans et al. [76], 2020 | beta | n/a | n/a | ASD, psychiatric problems, intellectual disability, IQ | yes | yes | no | no | Repetitive movements | no | Anxiety behaviors | n/a |
| Shehhi et. Al. [60], 2019 | Alpha and beta | n/a | n/a | Congenital heart disease, global development delay, epilepsy, intellectual disability, speech delay | yes | yes | Hallucinations, yes in some cases | yes | Gross motor delay | Sensorineural hearing loss | Speech and language delay, learning disability—32/34 had speech delay | n/a |
| Annunziata et al. [81], 2023 | n/a | Maternal inheritance in ⅘ subjects; incomplete penetrance | n/a | n/a | Developmental delay | Intellectual disability | n/a | Epileptiform discharge while sleeping or falling asleep | n/a | n/a | n/a | n/a |
| Williams et al. [83], 2019 | Alpha | Paternal inheritance of miR-873-5p variant; maternal inheritance of NRXN1 loss of function | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| Leblond et al. [36], 2019 | alpha | none | yes | NR | NR | Intellectual disability | no | NR | NR | NR | NR | Congenital torticollis and dental carries |
| Uzunhan et al. [80], 2022 | NR | alpha | yes | no | NR | NR | No | NR | Yes | NR | Yes | Macrocephaly, frontal bossing, bitemporal narrowing, wide forehead, long face, thin upper lip |
| Cameli et al. [82], 2021 | NR | Other rare variants found unspecified | NR | Maternal history of mutation—no family history of ASD | Yes | NR | NR | Predominance of a slow background activity in the R temporal region | Yes, delayed with motor stereotypies (hand flapping); limited speech (four words) | Yes, manipulating materials for visual, acoustic, tactile stimulation | Yes—hyperactivity, short attention span | |
| Ishizuka et al. [77], 2020 | Alpha | NR | NR | Maternally inherited | NR | Yes, No | NR | NR | NR | NR | NR | [ODD (oppositional defiant disorder)], [Depression, ADHD] |
NR: not recorded.
This review provides insights into the genotypic and phenotypic outcomes observed in the included studies. It reveals significant diversity in both the genetic variants and physical characteristics of individuals harboring the NRXN1 gene variants in line with previous findings [98]. There is speculation that the size and the location of the NRXN1 mutation may influence the phenotypic presentation of autism [27]. Large studies with a dual focus on genotype and phenotype are essential to understanding the relationship of NRXN1 mutations with its various clinical presentations.
4. Limitations
A significant limitation of our review stems from the limited pool of participants exhibiting both ASD and NRXN1 genetic variations within the studies we have analyzed for this article. The dearth of individuals with this specific combination of traits may impact the generalizability and reliability of our findings. The small sample size not only hinders statistical power but also raises concerns about the applicability for a broader population. It is essential to acknowledge this limitation as it highlights the need for further research with more extensive and diverse cohorts to establish more robust conclusions regarding the relationship between ASD and NRXN1 variations. Additionally, there were inconsistencies in the information reported in the included studies. The articles predominantly focused on either the genotype or phenotype, offering limited information on the other aspect. To compensate for this, the reviewers had to rely on Supplemental Information, especially for articles centered on genotypes, to gain a clearer understanding of the phenotypic outcomes. Ultimately, more comprehensive research involving individuals with ASD is necessary to better understand the relationship between NRXN1 gene variants and phenotypic expression.
5. Conclusions and Future Directions
This systematic review article delves deep into the phenotypic manifestations of ASD in individuals carrying NRXN1 gene variants. The included studies suggest heterogeneity in both the genotype and phenotype of individuals harboring NRXN1 gene variants. While the genotype and phenotype associated with NRXN1 is not fully elucidated, this review continues to shed light on the implication of this mutation on neuropsychiatric disorders, including ASD. Our findings were consistent with prior literature, which found exonic mutations to be commonly associated with neuropsychiatric disease and NRXN1 mutations [99], as well as found a low prevalence of dysmorphic features and a relatively high frequency of seizure disorders.
Although there have been advances in understanding the role of NRXN1 in ASD, there remain major research gaps. There is a need for more in-depth studies to elucidate the precise mechanisms by which NRXN1 gene variants contribute to the development and manifestation of ASD. Understanding the biological pathways involved is essential for targeted therapeutic strategies. Research has not fully explored the range of phenotypes associated with different NRXN1 mutations in ASD. Further studies are needed to clarify the relationship between specific NRXN1 variants and the spectrum of autism symptoms. In addition, the interaction between NRXN1 gene variants and environmental factors in the development of ASD is not well understood. Research in this area could provide insights into potential triggers or protective factors. Furthermore, much of the current research has been conducted in limited populations. There is a gap in studies involving diverse ethnic geographical, and gender populations, which is crucial for understanding the global impact of NRXN1 variants on ASD. Furthermore, there is a lack of long-term, longitudinal studies following individuals with NRXN1 gene variants from early childhood into adulthood. Such studies could offer valuable insights into how these variants influence the progression and outcomes of autism over time.
Despite these research gaps, NRXN1 gene variants have been strongly associated with ASD. Thus, focusing on this specific gene could enhance the prognosis of ASD. It is well-known that treating genetic disorders is a complex challenge, typically addressed by a comprehensive, multi-faceted team employing various therapeutic modalities. One of the emerging approaches in treating genetic disorders involves gene editing [100,101,102]. This technique uses a biological system, such as CRISPR/Cas9, to precisely excise a specific gene segment and employ a biological vector to insert a desired sequence [103,104,105,106]. These treatments are ideal, as they are permanent, unlike the multimodal management that is currently being utilized [107]. Identifying likely genetic etiologies of ASD is the first major step in creating gene editing for this disease. In addition to genetic therapies, targeted drug therapies for NRXN1 related molecules may be useful in treating the associated clinical symptoms [108]. These therapies include RNAi, protein replacement, small molecule therapy, and chaperone therapy [109,110,111,112,113,114].
While ASD is believed to be influenced by multiple factors, NRXN1 stands out as a well-researched genetic factor in ASD. With an EAGLE score of 143.75, it has consistently been linked to, and potentially implicated in, the development of ASD. This positions it as an ideal candidate for gene-editing technologies. Conducting genetic testing in individuals with ASD, along with in-depth studies on the phenotypic effects of NRXN1 mutations, can enhance our understanding of how NRXN1 contributes to ASD. By directly targeting this gene, we could pave the way for developing innovative therapeutic approaches, potentially leading to improved treatment outcomes and prognoses for ASD in the future in pursuit of improving quality of life of affected individuals.
Acknowledgments
We are grateful to Valerie Gramling for the critical reading of the manuscript. The autism research in Eshraghi’s laboratory is supported by generous funding from the Autism Research Institute (ARI) and Brain Foundation.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm13072067/s1, Figure S1: Location of neurexins and their binding partners, neuroligins, in the synapse. Several neurexin–neuroligin pathway proteins are shown as well as synaptic vesicle-binding proteins. NMDAR, N-methyl-Daspartate receptor; mGluR5, metabolic glutamate receptor 5; PSD-95, post-synaptic density protein 95; Shank, SH3 and multiple ankyrin repeat domains protein. Taken from [29] under the terms of the Creative Com-mons Attribution License, which permits unrestricted use, provided the original author and source are credited.
Author Contributions
Conceptualization, J.N.C., J.M., A.S., D.L.K., A.M.K., M.Z., R.M. and A.A.E.; methodology, J.N.C., J.M., A.S., D.L.K., A.M.K., M.Z., R.M. and A.A.E.; validation, J.N.C., J.M., A.S., D.L.K., A.M.K., M.Z., R.M. and A.A.E.; formal analysis, J.N.C., J.M., A.S., D.L.K., A.M.K., M.Z., R.M. and A.A.E. investigation, J.N.C., J.M., A.S., D.L.K., A.M.K., M.Z., R.M. and A.A.E.; data curation, J.N.C., J.M., A.S., D.L.K., A.M.K., M.Z., R.M. and A.A.E.; writing—original draft preparation, J.N.C., J.M., A.S., D.L.K., A.M.K., M.Z., R.M. and A.A.E.; writing—review and editing, J.N.C., J.M., A.S., D.L.K., A.M.K., M.Z., R.M. and A.A.E.; supervision, R.M. and A.A.E.; project administration, J.N.C., R.M. and A.A.E. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Hirota T., King B.H. Autism Spectrum Disorder: A Review. JAMA. 2023;329:157–168. doi: 10.1001/jama.2022.23661. [DOI] [PubMed] [Google Scholar]
- 2.Hodges H., Fealko C., Soares N. Autism spectrum disorder: Definition, epidemiology, causes, and clinical evaluation. Transl. Pediatr. 2020;9:S55–S65. doi: 10.21037/tp.2019.09.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lord C., Elsabbagh M., Baird G., Veenstra-Vanderweele J. Autism spectrum disorder. Lancet. 2018;392:508–520. doi: 10.1016/S0140-6736(18)31129-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sato M., Nakai N., Fujima S., Choe K.Y., Takumi T. Social circuits and their dysfunction in autism spectrum disorder. Mol. Psychiatry. 2023;28:3194–3206. doi: 10.1038/s41380-023-02201-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davies C., Moosa M., McKenna K., Mittal J., Memis I., Mittal R., Eshraghi A.A. Quality of Life, Neurosensory Disorders and Co-Occurring Medical Conditions in Individuals on the Spectrum, with a Special Focus on Females Diagnosed with Autism: A Systematic Review. J. Clin. Med. 2023;12:927. doi: 10.3390/jcm12030927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anderson G.R., Aoto J., Tabuchi K., Földy C., Covy J., Yee A.X., Wu D., Lee S.J., Chen L., Malenka R.C., et al. β-Neurexins Control Neural Circuits by Regulating Synaptic Endocannabinoid Signaling. Cell. 2015;162:593–606. doi: 10.1016/j.cell.2015.06.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eckes T., Buhlmann U., Holling H.-D., Möllmann A. Comprehensive ABA-based interventions in the treatment of children with autism spectrum disorder—A meta-analysis. BMC Psychiatry. 2023;23:133. doi: 10.1186/s12888-022-04412-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jenkins A.K., Paterson C., Wang Y., Hyde T.M., Kleinman J.E., Law A.J. Neurexin 1 (NRXN1) splice isoform expression during human neocortical development and aging. Mol. Psychiatry. 2016;21:701–706. doi: 10.1038/mp.2015.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Béna F., Bruno D.L., Eriksson M., van Ravenswaaij-Arts C., Stark Z., Dijkhuizen T., Gerkes E., Gimelli S., Ganesamoorthy D., Thuresson A.C., et al. Molecular and clinical characterization of 25 individuals with exonic deletions of NRXN1 and comprehensive review of the literature. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2013;162:388–403. doi: 10.1002/ajmg.b.32148. [DOI] [PubMed] [Google Scholar]
- 10.Castronovo P., Baccarin M., Ricciardello A., Picinelli C., Tomaiuolo P., Cucinotta F., Frittoli M., Lintas C., Sacco R., Persico A.M. Phenotypic spectrum of NRXN1 mono- and bi-allelic deficiency: A systematic review. Clin. Genet. 2020;97:125–137. doi: 10.1111/cge.13537. [DOI] [PubMed] [Google Scholar]
- 11.Kirov G., Gumus D., Chen W., Norton N., Georgieva L., Sari M., O’Donovan M.C., Erdogan F., Owen M.J., Ropers H.-H. Comparative genome hybridization suggests a role for NRXN1 and APBA2 in schizophrenia. Hum. Mol. Genet. 2008;17:458–465. doi: 10.1093/hmg/ddm323. [DOI] [PubMed] [Google Scholar]
- 12.Liu Y., Hu Z., Xun G., Peng Y., Lu L., Xu X., Xiong Z., Xia L., Liu D., Li W., et al. Mutation analysis of the NRXN1 gene in a Chinese autism cohort. J. Psychiatr. Res. 2012;46:630–634. doi: 10.1016/j.jpsychires.2011.10.015. [DOI] [PubMed] [Google Scholar]
- 13.Reissner C., Runkel F., Missler M. Neurexins. Genome Biol. 2013;14:213. doi: 10.1186/gb-2013-14-9-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roberts J.L., Hovanes K., Dasouki M., Manzardo A.M., Butler M.G. Chromosomal microarray analysis of consecutive individuals with autism spectrum disorders or learning disability presenting for genetic services. Gene. 2014;535:70–78. doi: 10.1016/j.gene.2013.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Styles M., Alsharshani D., Samara M., Alsharshani M., Khattab A., Qoronfleh M.W., Al-Dewik N.I. Risk factors, diagnosis, prognosis and treatment of autism. Front. Biosci. (Landmark Ed.) 2020;25:1682–1717. doi: 10.2741/4873. [DOI] [PubMed] [Google Scholar]
- 16.Tromp A., Mowry B., Giacomotto J. Neurexins in autism and schizophrenia—A review of patient mutations, mouse models and potential future directions. Mol. Psychiatry. 2021;26:747–760. doi: 10.1038/s41380-020-00944-8. [DOI] [PubMed] [Google Scholar]
- 17.Varghese M., Keshav N., Jacot-Descombes S., Warda T., Wicinski B., Dickstein D.L., Harony-Nicolas H., De Rubeis S., Drapeau E., Buxbaum J.D., et al. Autism spectrum disorder: Neuropathology and animal models. Acta Neuropathol. 2017;134:537–566. doi: 10.1007/s00401-017-1736-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bourgeron T. Cold Spring Harbor Symposia on Quantitative Biology. Cold Spring Harbor Laboratory Press; Cold Spring Harbor, NY, USA: 2007. The possible interplay of synaptic and clock genes in autism spectrum disorders; pp. 645–654. [DOI] [PubMed] [Google Scholar]
- 19.Bourgeron T. Synaptic Plasticity and the Mechanism of Alzheimer’s Disease. Springer; Berlin/Heidelberg, Germany: 2008. Genes, synapses and autism spectrum disorders; pp. 169–179. [Google Scholar]
- 20.Bourgeron T. A synaptic trek to autism. Curr. Opin. Neurobiol. 2009;19:231–234. doi: 10.1016/j.conb.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 21.Keller R., Basta R., Salerno L., Elia M. Autism, epilepsy, and synaptopathies: A not rare association. Neurol. Sci. 2017;38:1353–1361. doi: 10.1007/s10072-017-2974-x. [DOI] [PubMed] [Google Scholar]
- 22.Lepeta K., Lourenco M.V., Schweitzer B.C., Martino Adami P.V., Banerjee P., Catuara-Solarz S., de La Fuente Revenga M., Guillem A.M., Haidar M., Ijomone O.M., et al. Synaptopathies: Synaptic dysfunction in neurological disorders—A review from students to students. J. Neurochem. 2016;138:785–805. doi: 10.1111/jnc.13713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sauer A.K., Stanton J.E., Hans S., Grabrucker A.M. Autism Spectrum Disorders: Etiology and Pathology. In: Grabrucker A.M., editor. Autism Spectrum Disorders. Exon Publications Copyright; Brisbane, Australia: 2021. [PubMed] [Google Scholar]
- 24.Smith R., Sadee W. Synaptic Signaling and Aberrant RNA Splicing in Autism Spectrum Disorders. Front. Synaptic Neurosci. 2011;3:1. doi: 10.3389/fnsyn.2011.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Südhof T.C. Synaptic neurexin complexes: A molecular code for the logic of neural circuits. Cell. 2017;171:745–769. doi: 10.1016/j.cell.2017.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buxbaum J.D. Multiple rare variants in the etiology of autism spectrum disorders. Dialogues Clin. Neurosci. 2009;11:35–43. doi: 10.31887/DCNS.2009.11.1/jdbuxbaum. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cooke J., Molloy C.J., Cáceres A.S.J., Dinneen T., Bourgeron T., Murphy D., Gallagher L., Loth E. The Synaptic Gene Study: Design and Methodology to Identify Neurocognitive Markers in Phelan-McDermid Syndrome and NRXN1 Deletions. Front. Neurosci. 2022;16:806990. doi: 10.3389/fnins.2022.806990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Curran S., Ahn J.W., Grayton H., Collier D.A., Ogilvie C.M. NRXN1 deletions identified by array comparative genome hybridisation in a clinical case series—Further understanding of the relevance of NRXN1 to neurodevelopmental disorders. J. Mol. Psychiatry. 2013;1:4. doi: 10.1186/2049-9256-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cuttler K., Hassan M., Carr J., Cloete R., Bardien S. Emerging evidence implicating a role for neurexins in neurodegenerative and neuropsychiatric disorders. Open Biol. 2021;11:210091. doi: 10.1098/rsob.210091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dean C., Scholl F.G., Choih J., DeMaria S., Berger J., Isacoff E., Scheiffele P. Neurexin mediates the assembly of presynaptic terminals. Nat. Neurosci. 2003;6:708–716. doi: 10.1038/nn1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gauthier J., Siddiqui T.J., Huashan P., Yokomaku D., Hamdan F.F., Champagne N., Lapointe M., Spiegelman D., Noreau A., Lafrenière R.G. Truncating mutations in NRXN2 and NRXN1 in autism spectrum disorders and schizophrenia. Hum. Genet. 2011;130:563–573. doi: 10.1007/s00439-011-0975-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang A.Y., Yu D., Davis L.K., Sul J.H., Tsetsos F., Ramensky V., Zelaya I., Ramos E.M., Osiecki L., Chen J.A. Rare copy number variants in NRXN1 and CNTN6 increase risk for Tourette syndrome. Neuron. 2017;94:1101–1111.e7. doi: 10.1016/j.neuron.2017.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kember R., Ji X., Zhang J., Brown C., Rader D., Almasy L., Bucan M. Spectrum of common and rare mutations contributing to autism risk in families. Eur. Neuropsychopharmacol. 2019;29:S962–S963. doi: 10.1016/j.euroneuro.2017.08.322. [DOI] [Google Scholar]
- 34.Kim H.G., Kishikawa S., Higgins A.W., Seong I.S., Donovan D.J., Shen Y., Lally E., Weiss L.A., Najm J., Kutsche K., et al. Disruption of neurexin 1 associated with autism spectrum disorder. Am. J. Hum. Genet. 2008;82:199–207. doi: 10.1016/j.ajhg.2007.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Krueger D.D., Tuffy L.P., Papadopoulos T., Brose N. The role of neurexins and neuroligins in the formation, maturation, and function of vertebrate synapses. Curr. Opin. Neurobiol. 2012;22:412–422. doi: 10.1016/j.conb.2012.02.012. [DOI] [PubMed] [Google Scholar]
- 36.Leblond C.S., Cliquet F., Carton C., Huguet G., Mathieu A., Kergrohen T., Buratti J., Lemière N., Cuisset L., Bienvenu T., et al. Both rare and common genetic variants contribute to autism in the Faroe Islands. npj Genom. Med. 2019;4:1. doi: 10.1038/s41525-018-0075-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rujescu D., Ingason A., Cichon S., Pietiläinen O.P., Barnes M.R., Toulopoulou T., Picchioni M., Vassos E., Ettinger U., Bramon E. Disruption of the neurexin 1 gene is associated with schizophrenia. Hum. Mol. Genet. 2009;18:988–996. doi: 10.1093/hmg/ddn351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang J., Gong J., Li L., Chen Y., Liu L., Gu H., Luo X., Hou F., Zhang J., Song R. Neurexin gene family variants as risk factors for autism spectrum disorder. Autism Res. 2018;11:37–43. doi: 10.1002/aur.1881. [DOI] [PubMed] [Google Scholar]
- 39.Dai J., Aoto J., Südhof T.C. Alternative splicing of presynaptic neurexins differentially controls postsynaptic NMDA and AMPA receptor responses. Neuron. 2019;102:993–1008.e5. doi: 10.1016/j.neuron.2019.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Flaherty E., Zhu S., Barretto N., Cheng E., Deans P.J.M., Fernando M.B., Schrode N., Francoeur N., Antoine A., Alganem K., et al. Neuronal impact of patient-specific aberrant NRXN1α splicing. Nat. Genet. 2019;51:1679–1690. doi: 10.1038/s41588-019-0539-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Missler M., Südhof T.C. Neurexins: Three genes and 1001 products. Trends Genet. 1998;14:20–26. doi: 10.1016/S0168-9525(97)01324-3. [DOI] [PubMed] [Google Scholar]
- 42.Tabuchi K., Südhof T.C. Structure and evolution of neurexin genes: Insight into the mechanism of alternative splicing. Genomics. 2002;79:849–859. doi: 10.1006/geno.2002.6780. [DOI] [PubMed] [Google Scholar]
- 43.Miller M.T., Mileni M., Comoletti D., Stevens R.C., Harel M., Taylor P. The crystal structure of the α-neurexin-1 extracellular region reveals a hinge point for mediating synaptic adhesion and function. Structure. 2011;19:767–778. doi: 10.1016/j.str.2011.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zambonino M., Pereira P. The structure of Neurexin 1α (n1α) and its role as synaptic organizer. Bionatura. 2019;4:883–886. doi: 10.21931/RB/2019.04.02.12. [DOI] [Google Scholar]
- 45.Camacho-Garcia R.J., Planelles M.I., Margalef M., Pecero M.L., Martínez-Leal R., Aguilera F., Vilella E., Martinez-Mir A., Scholl F.G. Mutations affecting synaptic levels of neurexin-1β in autism and mental retardation. Neurobiol. Dis. 2012;47:135–143. doi: 10.1016/j.nbd.2012.03.031. [DOI] [PubMed] [Google Scholar]
- 46.Dachtler J., Ivorra J.L., Rowland T.E., Lever C., Rodgers R.J., Clapcote S.J. Heterozygous deletion of α-neurexin I or α-neurexin II results in behaviors relevant to autism and schizophrenia. Behav. Neurosci. 2015;129:765–776. doi: 10.1037/bne0000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Esclassan F., Francois J., Phillips K.G., Loomis S., Gilmour G. Phenotypic characterization of nonsocial behavioral impairment in neurexin 1α knockout rats. Behav. Neurosci. 2015;129:74. doi: 10.1037/bne0000024. [DOI] [PubMed] [Google Scholar]
- 48.Ching M.S., Shen Y., Tan W.H., Jeste S.S., Morrow E.M., Chen X., Mukaddes N.M., Yoo S.Y., Hanson E., Hundley R. Deletions of NRXN1 (neurexin-1) predispose to a wide spectrum of developmental disorders. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. 2010;153:937–947. doi: 10.1002/ajmg.b.31063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dabell M.P., Rosenfeld J.A., Bader P., Escobar L.F., El-Khechen D., Vallee S.E., Dinulos M.B.P., Curry C., Fisher J., Tervo R. Investigation of NRXN1 deletions: Clinical and molecular characterization. Am. J. Med. Genet. Part A. 2013;161:717–731. doi: 10.1002/ajmg.a.35780. [DOI] [PubMed] [Google Scholar]
- 50.Janz P., Bainier M., Marashli S., Schoenenberger P., Valencia M., Redondo R.L. Neurexin1α knockout rats display oscillatory abnormalities and sensory processing deficits back-translating key endophenotypes of psychiatric disorders. Transl. Psychiatry. 2022;12:455. doi: 10.1038/s41398-022-02224-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pak C., Danko T., Zhang Y., Aoto J., Anderson G., Maxeiner S., Yi F., Wernig M., Südhof T.C. Human Neuropsychiatric Disease Modeling using Conditional Deletion Reveals Synaptic Transmission Defects Caused by Heterozygous Mutations in NRXN1. Cell Stem Cell. 2015;17:316–328. doi: 10.1016/j.stem.2015.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Torres V.I., Vallejo D., Inestrosa N.C. Emerging Synaptic Molecules as Candidates in the Etiology of Neurological Disorders. Neural Plast. 2017;2017:8081758. doi: 10.1155/2017/8081758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zweier C., de Jong E.K., Zweier M., Orrico A., Ousager L.B., Collins A.L., Bijlsma E.K., Oortveld M.A., Ekici A.B., Reis A., et al. CNTNAP2 and NRXN1 are mutated in autosomal-recessive Pitt-Hopkins-like mental retardation and determine the level of a common synaptic protein in Drosophila. Am. J. Hum. Genet. 2009;85:655–666. doi: 10.1016/j.ajhg.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Graf E.R., Kang Y., Hauner A.M., Craig A.M. Structure Function and Splice Site Analysis of the Synaptogenic Activity of the Neurexin-1β LNS Domain. J. Neurosci. 2006;26:4256–4265. doi: 10.1523/JNEUROSCI.1253-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Graf E.R., Zhang X., Jin S.X., Linhoff M.W., Craig A.M. Neurexins induce differentiation of GABA and glutamate postsynaptic specializations via neuroligins. Cell. 2004;119:1013–1026. doi: 10.1016/j.cell.2004.11.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Missler M., Zhang W., Rohlmann A., Kattenstroth G., Hammer R.E., Gottmann K., Südhof T.C. Alpha-neurexins couple Ca2+ channels to synaptic vesicle exocytosis. Nature. 2003;423:939–948. doi: 10.1038/nature01755. [DOI] [PubMed] [Google Scholar]
- 57.Nam C.I., Chen L. Postsynaptic assembly induced by neurexin-neuroligin interaction and neurotransmitter. Proc. Natl. Acad. Sci. USA. 2005;102:6137–6142. doi: 10.1073/pnas.0502038102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sons M.S., Busche N., Strenzke N., Moser T., Ernsberger U., Mooren F.C., Zhang W., Ahmad M., Steffens H., Schomburg E.D., et al. alpha-Neurexins are required for efficient transmitter release and synaptic homeostasis at the mouse neuromuscular junction. Neuroscience. 2006;138:433–446. doi: 10.1016/j.neuroscience.2005.11.040. [DOI] [PubMed] [Google Scholar]
- 59.Uchigashima M., Cheung A., Suh J., Watanabe M., Futai K. Differential expression of neurexin genes in the mouse brain. J. Comp. Neurol. 2019;527:1940–1965. doi: 10.1002/cne.24664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Al Shehhi M., Forman E.B., Fitzgerald J.E., McInerney V., Krawczyk J., Shen S., Betts D.R., Ardle L.M., Gorman K.M., King M.D., et al. NRXN1 deletion syndrome; phenotypic and penetrance data from 34 families. Eur. J. Med. Genet. 2019;62:204–209. doi: 10.1016/j.ejmg.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 61.Girirajan S., Dennis M.Y., Baker C., Malig M., Coe B.P., Campbell C.D., Mark K., Vu T.H., Alkan C., Cheng Z., et al. Refinement and discovery of new hotspots of copy-number variation associated with autism spectrum disorder. Am. J. Hum. Genet. 2013;92:221–237. doi: 10.1016/j.ajhg.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hu Z., Xiao X., Zhang Z., Li M. Genetic insights and neurobiological implications from NRXN1 in neuropsychiatric disorders. Mol. Psychiatry. 2019;24:1400–1414. doi: 10.1038/s41380-019-0438-9. [DOI] [PubMed] [Google Scholar]
- 63.Kasem E., Kurihara T., Tabuchi K. Neurexins and neuropsychiatric disorders. Neurosci. Res. 2018;127:53–60. doi: 10.1016/j.neures.2017.10.012. [DOI] [PubMed] [Google Scholar]
- 64.Levy D., Ronemus M., Yamrom B., Lee Y.H., Leotta A., Kendall J., Marks S., Lakshmi B., Pai D., Ye K., et al. Rare de novo and transmitted copy-number variation in autistic spectrum disorders. Neuron. 2011;70:886–897. doi: 10.1016/j.neuron.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 65.Sanders S.J., Ercan-Sencicek A.G., Hus V., Luo R., Murtha M.T., Moreno-De-Luca D., Chu S.H., Moreau M.P., Gupta A.R., Thomson S.A., et al. Multiple recurrent de novo CNVs, including duplications of the 7q11.23 Williams syndrome region, are strongly associated with autism. Neuron. 2011;70:863–885. doi: 10.1016/j.neuron.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Viñas-Jornet M., Esteba-Castillo S., Gabau E., Ribas-Vidal N., Baena N., San J., Ruiz A., Coll M.D., Novell R., Guitart M. A common cognitive, psychiatric, and dysmorphic phenotype in carriers of NRXN1 deletion. Mol. Genet. Genom. Med. 2014;2:512–521. doi: 10.1002/mgg3.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Craig A.M., Kang Y. Neurexin–neuroligin signaling in synapse development. Curr. Opin. Neurobiol. 2007;17:43–52. doi: 10.1016/j.conb.2007.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ichtchenko K., Nguyen T., Südhof T.C. Structures, alternative splicing, and neurexin binding of multiple neuroligins. J. Biol. Chem. 1996;271:2676–2682. doi: 10.1074/jbc.271.5.2676. [DOI] [PubMed] [Google Scholar]
- 69.Guang S., Pang N., Deng X., Yang L., He F., Wu L., Chen C., Yin F., Peng J. Synaptopathology Involved in Autism Spectrum Disorder. Front. Cell. Neurosci. 2018;12:470. doi: 10.3389/fncel.2018.00470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Culotta L., Penzes P. Exploring the mechanisms underlying excitation/inhibition imbalance in human iPSC-derived models of ASD. Mol. Autism. 2020;11:32. doi: 10.1186/s13229-020-00339-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Alkanli S.S., Alkanli N., Ay A., Albeniz I. CRISPR/Cas9 Mediated Therapeutic Approach in Huntington’s Disease. Mol. Neurobiol. 2023;60:1486–1498. doi: 10.1007/s12035-022-03150-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bell S., Peng H., Crapper L., Kolobova I., Maussion G., Vasuta C., Yerko V., Wong T.P., Ernst C. A Rapid Pipeline to Model Rare Neurodevelopmental Disorders with Simultaneous CRISPR/Cas9 Gene Editing. Stem Cells Transl. Med. 2017;6:886–896. doi: 10.1002/sctm.16-0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hatada I., Morita S., Horii T. CRISPR/Cas9. Methods Mol. Biol. 2023;2637:41–47. doi: 10.1007/978-1-0716-3016-7_3. [DOI] [PubMed] [Google Scholar]
- 74.Ricci R., Colasante G. CRISPR/dCas9 as a Therapeutic Approach for Neurodevelopmental Disorders: Innovations and Limitations Compared to Traditional Strategies. Dev. Neurosci. 2021;43:253–261. doi: 10.1159/000515845. [DOI] [PubMed] [Google Scholar]
- 75.Tyumentseva M., Tyumentsev A., Akimkin V. CRISPR/Cas9 Landscape: Current State and Future Perspectives. Int. J. Mol. Sci. 2023;24:16077. doi: 10.3390/ijms242216077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Nele C., Laura V., Annick V., Koenraad D., Hilde Van E., Griet Van B., Hilde O., de Thomy R., Els O., Eric L., et al. The clinical relevance of intragenic NRXN1 deletions. J. Med. Genet. 2020;57:347. doi: 10.1136/jmedgenet-2019-106448. [DOI] [PubMed] [Google Scholar]
- 77.Ishizuka K., Yoshida T., Kawabata T., Imai A., Mori H., Kimura H., Inada T., Okahisa Y., Egawa J., Usami M., et al. Functional characterization of rare NRXN1 variants identified in autism spectrum disorders and schizophrenia. J. Neurodev. Disord. 2020;12:25. doi: 10.1186/s11689-020-09325-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Alfieri P., Scibelli F., Sinibaldi L., Valeri G., Caciolo C., Novello R.L., Novelli A., Digilio M.C., Tartaglia M., Vicari S. Further insight into the neurobehavioral pattern of children carrying the 2p16.3 heterozygous deletion involving NRXN1: Report of five new cases. Genes Brain Behav. 2020;19:e12687. doi: 10.1111/gbb.12687. [DOI] [PubMed] [Google Scholar]
- 79.Calderoni S., Ricca I., Balboni G., Cagiano R., Cassandrini D., Doccini S., Cosenza A., Tolomeo D., Tancredi R., Santorelli F.M., et al. Evaluation of Chromosome Microarray Analysis in a Large Cohort of Females with Autism Spectrum Disorders: A Single Center Italian Study. J. Pers. Med. 2020;10:160. doi: 10.3390/jpm10040160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Aksu Uzunhan T., Ayaz A. Homozygous exonic and intragenic NRXN1 deletion presenting as either West syndrome or autism spectrum disorder in two siblings. Clin. Neurol. Neurosurg. 2022;214:107141. doi: 10.1016/j.clineuro.2022.107141. [DOI] [PubMed] [Google Scholar]
- 81.Annunziata S., Bulgheroni S., D’Arrigo S., Esposito S., Taddei M., Saletti V., Alfei E., Sciacca F.L., Rizzo A., Pantaleoni C., et al. CGH Findings in Children with Complex and Essential Autistic Spectrum Disorder. J. Autism Dev. Disord. 2023;53:615–623. doi: 10.1007/s10803-020-04833-5. [DOI] [PubMed] [Google Scholar]
- 82.Cameli C., Viggiano M., Rochat M.J., Maresca A., Caporali L., Fiorini C., Palombo F., Magini P., Duardo R.C., Ceroni F., et al. An increased burden of rare exonic variants in NRXN1 microdeletion carriers is likely to enhance the penetrance for autism spectrum disorder. J. Cell. Mol. Med. 2021;25:2459–2470. doi: 10.1111/jcmm.16161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Williams S.M., An J.Y., Edson J., Watts M., Murigneux V., Whitehouse A.J.O., Jackson C.J., Bellgrove M.A., Cristino A.S., Claudianos C. An integrative analysis of non-coding regulatory DNA variations associated with autism spectrum disorder. Mol. Psychiatry. 2019;24:1707–1719. doi: 10.1038/s41380-018-0049-x. [DOI] [PubMed] [Google Scholar]
- 84.Zarrei M., Burton C.L., Engchuan W., Young E.J., Higginbotham E.J., MacDonald J.R., Trost B., Chan A.J.S., Walker S., Lamoureux S., et al. A large data resource of genomic copy number variation across neurodevelopmental disorders. npj Genom. Med. 2019;4:26. doi: 10.1038/s41525-019-0098-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lowther C., Speevak M., Armour C.M., Goh E.S., Graham G.E., Li C., Zeesman S., Nowaczyk M.J., Schultz L.A., Morra A., et al. Molecular characterization of NRXN1 deletions from 19,263 clinical microarray cases identifies exons important for neurodevelopmental disease expression. Genet. Med. 2017;19:53–61. doi: 10.1038/gim.2016.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Skiba A., Talarowska M., Szemraj J., Gałecki P. Is NRXN1 Gene Expression an Important Marker of Treatment of Depressive Disorders? A Pilot Study. J. Pers. Med. 2021;11:637. doi: 10.3390/jpm11070637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Todarello G., Feng N., Kolachana B.S., Li C., Vakkalanka R., Bertolino A., Weinberger D.R., Straub R.E. Incomplete penetrance of NRXN1 deletions in families with schizophrenia. Schizophr. Res. 2014;155:1–7. doi: 10.1016/j.schres.2014.02.023. [DOI] [PubMed] [Google Scholar]
- 88.Wilkinson B., Campbell D.B. Contribution of long noncoding RNAs to autism spectrum disorder risk. Int. Rev. Neurobiol. 2013;113:35–59. doi: 10.1016/b978-0-12-418700-9.00002-2. [DOI] [PubMed] [Google Scholar]
- 89.Duong L.T., Hoeffding L.K., Petersen K.B., Knudsen C.D., Thygesen J.H., Klitten L.L., Tommerup N., Ingason A., Werge T. Two rare deletions upstream of the NRXN1 gene (2p16.3) affecting the non-coding mRNA AK127244 segregate with diverse psychopathological phenotypes in a family. Eur. J. Med. Genet. 2015;58:650–653. doi: 10.1016/j.ejmg.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 90.Rizzo A., Alfei E., Zibordi F., Saletti V., Zorzi G., Freri E., Estienne M., Girgenti V., D’Arrigo S., Esposito S., et al. The noncoding RNA AK127244 in 2p16.3 locus: A new susceptibility region for neuropsychiatric disorders. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2018;177:557–562. doi: 10.1002/ajmg.b.32649. [DOI] [PubMed] [Google Scholar]
- 91.López-Cruz C., Cano-López I., Aliño M., Puig-Pérez S. West Syndrome and associated Autism Spectrum Disorder: Proposal for a neuropsychological assessment and intervention protocol. Papeles Psicól. 2022;43:125–132. doi: 10.23923/pap.psicol.2981. [DOI] [Google Scholar]
- 92.Ouss L., Saint-Georges C., Robel L., Bodeau N., Laznik M.-C., Crespin G.C., Chetouani M., Bursztejn C., Golse B., Nabbout R., et al. Infant’s engagement and emotion as predictors of autism or intellectual disability in West syndrome. Eur. Child Adolesc. Psychiatry. 2014;23:143–149. doi: 10.1007/s00787-013-0430-x. [DOI] [PubMed] [Google Scholar]
- 93.Strasser L., Downes M., Kung J., Cross J.H., De Haan M. Prevalence and risk factors for autism spectrum disorder in epilepsy: A systematic review and meta-analysis. Dev. Med. Child Neurol. 2018;60:19–29. doi: 10.1111/dmcn.13598. [DOI] [PubMed] [Google Scholar]
- 94.Schuck R.K., Flores R.E., Fung L.K. Brief Report: Sex/Gender Differences in Symptomology and Camouflaging in Adults with Autism Spectrum Disorder. J. Autism Dev. Disord. 2019;49:2597–2604. doi: 10.1007/s10803-019-03998-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Taşkıran E.Z., Karaosmanoğlu B., Koşukcu C., Ürel-Demir G., Akgün-Doğan Ö., Şimşek-Kiper P., Alikaşifoğlu M., Boduroğlu K., Utine G.E. Diagnostic yield of whole-exome sequencing in non-syndromic intellectual disability. J. Intellect. Disabil. Res. 2021;65:577–588. doi: 10.1111/jir.12835. [DOI] [PubMed] [Google Scholar]
- 96.Wu D., Zhu J., You L., Wang J., Zhang S., Liu Z., Xu Q., Yuan X., Yang L., Wang W., et al. NRXN1 depletion in the medial prefrontal cortex induces anxiety-like behaviors and abnormal social phenotypes along with impaired neurite outgrowth in rat. J. Neurodev. Disord. 2023;15:6. doi: 10.1186/s11689-022-09471-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Xu X., Hu Z., Zhang L., Liu H., Cheng Y., Xia K., Zhang X. Not all neuroligin 3 and 4X missense variants lead to significant functional inactivation. Brain Behav. 2017;7:e00793. doi: 10.1002/brb3.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gregor A., Albrecht B., Bader I., Bijlsma E.K., Ekici A.B., Engels H., Hackmann K., Horn D., Hoyer J., Klapecki J. Expanding the clinical spectrum associated with defects in CNTNAP2 and NRXN1. BMC Med. Genet. 2011;12:106. doi: 10.1186/1471-2350-12-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Schaaf C.P., Boone P.M., Sampath S., Williams C., Bader P.I., Mueller J.M., Shchelochkov O.A., Brown C.W., Crawford H.P., Phalen J.A. Phenotypic spectrum and genotype–phenotype correlations of NRXN1 exon deletions. Eur. J. Hum. Genet. 2012;20:1240–1247. doi: 10.1038/ejhg.2012.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Pena S.A., Iyengar R., Eshraghi R.S., Bencie N., Mittal J., Aljohani A., Mittal R., Eshraghi A.A. Gene therapy for neurological disorders: Challenges and recent advancements. J. Drug Target. 2020;28:111–128. doi: 10.1080/1061186X.2019.1630415. [DOI] [PubMed] [Google Scholar]
- 101.Preta G. Development of New Genome Editing Tools for the Treatment of Hyperlipidemia. Cells. 2023;12:2466. doi: 10.3390/cells12202466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sandhu A., Kumar A., Rawat K., Gautam V., Sharma A., Saha L. Modernising autism spectrum disorder model engineering and treatment via CRISPR-Cas9: A gene reprogramming approach. World J. Clin. Cases. 2023;11:3114–3127. doi: 10.12998/wjcc.v11.i14.3114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Gutiérrez-Rodríguez A., Cruz-Fuentes C.S., Genis-Mendoza A.D., Nicolini H. CRISPR/Cas9 Genome Editing Approaches for Psychiatric Research. Braz. J. Psychiatry. 2023;45:137–145. doi: 10.47626/1516-4446-2022-2913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Karimian A., Azizian K., Parsian H., Rafieian S., Shafiei-Irannejad V., Kheyrollah M., Yousefi M., Majidinia M., Yousefi B. CRISPR/Cas9 technology as a potent molecular tool for gene therapy. J. Cell. Physiol. 2019;234:12267–12277. doi: 10.1002/jcp.27972. [DOI] [PubMed] [Google Scholar]
- 105.Mani S., Jindal D., Singh M. Gene Therapy, A Potential Therapeutic Tool for Neurological and Neuropsychiatric Disorders: Applications, Challenges and Future Perspective. Curr. Gene Ther. 2023;23:20–40. doi: 10.2174/1566523222666220328142427. [DOI] [PubMed] [Google Scholar]
- 106.Thapar N., Eid M.A.F., Raj N., Kantas T., Billing H.S., Sadhu D. Application of CRISPR/Cas9 in the management of Alzheimer’s disease and Parkinson’s disease: A review. Ann. Med. Surg. 2024;86:329–335. doi: 10.1097/MS9.0000000000001500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Weuring W., Geerligs J., Koeleman B.P.C. Gene Therapies for Monogenic Autism Spectrum Disorders. Genes. 2021;12:1667. doi: 10.3390/genes12111667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ding Y., Howard L., Gallagher L., Shen S. Regulation and postsynaptic binding of neurexins—Drug targets for neurodevelopmental and neuropsychiatric disorders. Front. Biol. 2015;10:239–251. doi: 10.1007/s11515-015-1363-1. [DOI] [Google Scholar]
- 109.Chen X., Mangala L.S., Rodriguez-Aguayo C., Kong X., Lopez-Berestein G., Sood A.K. RNA interference-based therapy and its delivery systems. Cancer Metastasis Rev. 2018;37:107–124. doi: 10.1007/s10555-017-9717-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Jing X., Arya V., Reynolds K.S., Rogers H. Clinical Pharmacology of RNA Interference–Based Therapeutics: A Summary Based on Food and Drug Administration–Approved Small Interfering RNAs. Drug Metab. Dispos. 2023;51:193–198. doi: 10.1124/dmd.122.001107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Liguori L., Monticelli M., Allocca M., Hay Mele B., Lukas J., Cubellis M.V., Andreotti G. Pharmacological Chaperones: A Therapeutic Approach for Diseases Caused by Destabilizing Missense Mutations. Int. J. Mol. Sci. 2020;21:489. doi: 10.3390/ijms21020489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Vavilis T., Stamoula E., Ainatzoglou A., Sachinidis A., Lamprinou M., Dardalas I., Vizirianakis I. mRNA in the Context of Protein Replacement Therapy. Pharmaceutics. 2023;15:166. doi: 10.3390/pharmaceutics15010166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Weidemann F., Jovanovic A., Herrmann K., Vardarli I. Chaperone therapy in Fabry disease. Int. J. Mol. Sci. 2022;23:1887. doi: 10.3390/ijms23031887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Yadav D., Malviya R. Vector-Mediated Delivery of Transgenes and RNA Interference-Based Gene Silencing Sequences to Astrocytes for Disease Management: Advances and Prospectives. Curr. Gene Ther. 2024;24:110–121. doi: 10.2174/0115665232264527231013072728. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.