Abstract
Objective
To explore the coping strategies of caregivers of children who have survived paediatric cancer in Jordan.
Materials and methods
This study used a cross-sectional survey design and convenient sampling. The sample included 102 caregivers of children who have survived cancer, and outcome measures included the Arabic-translated Brief COPE, and caregiver and child demographic and condition questionnaire. Data analyses included descriptive statistics, analysis of frequencies, Spearman-rank order correlations and linear regression.
Results
Caregivers most frequently used religion coping (mean=6.42, SD=1.85), followed by acceptance (mean=5.95, SD=1.96) and planning (mean=5.05, SD=1.94). The least used coping strategies were humour (mean=2.98, SD=1.24) and behavioural disengagement as coping strategies (mean=3.01, SD=1.42). Having a female child predicted more self-distraction utilisation (β=0.265, p=0.007).
Conclusion
Caregivers of children who have survived cancer in Jordan frequently use passive coping strategies like religion and acceptance coping to overcome daily life stressors. Caregivers might benefit from psychosocial occupational therapy interventions to support their engagement in more active or problem-focused coping strategies.
Keywords: caregivers, psychology
WHAT IS ALREADY KNOWN ON THIS TOPIC.
Caregivers of adults’ cancer survivors engage in emotion-focused coping more than problem-focused coping. Caregivers’ coping strategies in families of children who have cancer are associated to certain demographic factors like gender and educational levels. Caregiver coping after surviving cancer is poorly understood.
WHAT THIS STUDY ADDS
Caregivers of children who have survived cancer mostly use religious and acceptance coping when dealing with everyday stressors. Also, having a girl child cancer survivor predicted caregivers’ utilisation of more self-distraction coping strategy.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Future research should investigate if caregivers’ coping change between having the cancer diagnosis and after surviving the cancer condition. Care providers should evaluate caregiver coping and provide psychosocial interventions to support caregivers’ engagement in active coping strategies.
According to the American Cancer Society, cancer is the second leading cause of death in children aged 1–14 years, after accidents.1 Cancer is a serious medical condition that affects not only people who have this condition but also their surrounded families and friends.2 After surviving the cancer condition, many children and caregivers deal with residual physical,3 cognitive4 and/or psychosocial challenges that may affect their daily life functioning.5 A number of studies have investigated caregiver coping during paediatric cancer treatments.6 7 However, limited evidence investigated how caregivers cope after surviving the cancer condition. To the authors’ knowledge, there were no studies in this area in Jordan or the Arab world. Therefore, this study aimed to explore the coping strategies of caregivers of children who have survived cancer in Jordan.
Literature review
Caregivers of children who have cancer experience elevated stress levels as compared with other medical and/or educational childhood conditions.8 There are several cancer-related factors that contribute to caregivers’ stress including disruption in everyday routine changes, and participation restrictions while being on the cancer treatment.9 The nature of the cancer condition and invasive procedures (eg, lumbar punctures, bone marrow aspirations) associated with cancer treatments also contribute to caregiver stress and poor quality of life.10 While stress is greater in caregivers of recently diagnosed individuals, it continues to affect caregivers during treatment and even after cancer recovery.11 There is accumulating evidence that looked at caregivers’ negative psychological states like stress, anxiety or depression12 13; however, there is little evidence on how caregivers of children with or who have survived cancer cope with these states. Ways of coping influence people’s adaptations to various conditions14 and contribute to their health and well-being.15
Coping refers to the thoughts and actions people use to manage stressful situations.16 Coping strategies are highly individualised because of people’s differences in resources, experiences, motivation, preferences and skills for coping. The early work of Carver and Scheier characterised people’s coping into several different coping strategies, including planning, use of emotional support and denial.17 Researchers differ in how they classify different coping strategies, like problem-focused or emotion-focused18; and adaptive or maladaptive coping.19 Engaging in adaptive or problem-focused coping strategies like planning or active coping contributes to better caregiver psychosocial and physical health and quality of life.20 On the other hand, maladaptive coping strategies like substance use negatively affect the health and quality of life of caregivers and surrounding family members.21
Unlike stress in caregivers of children with cancer, caregivers’ coping strategies were scarcely studied in the literature. A study by Gage-Bouchard et al investigated caregiver coping strategies in families of children with cancer and found associations between caregiver coping and a number of sociodemographical factors.6 For example, mothers used active coping, instrumental support, religious coping and emotional support, more than fathers. Also, gender and educational levels were linked to certain maladaptive coping strategies like substance use.6 While this later study investigated potential factors that affect caregiver coping during paediatric cancer, evidence on caregiver coping after surviving paediatric cancer remains poorly understood. A relatively recent study of caregivers of lung and colorectal cancer survivors found that caregivers engaged in emotion-focused coping (ie, religion, acceptance, positive reframing and emotional support) more than problem-focused coping.9 Care recipients in this study were adult cancer survivors, not children.
Research in this area is needed to build on the evidence about caregivers coping during and after surviving paediatric cancer. The novelty of this study is to investigate what coping strategies caregivers of children who have survived cancer used to overcome daily life challenges. Up to the authors’ knowledge, there were no studies about caregivers’ coping in Jordan. We hypothesised—since children have survived the cancer condition—that caregivers will use more problem-focused coping strategies to overcome daily life challenges. Characterising caregiver coping strategies is important to investigate intervention strategies that promote the selection of adaptive or problem-focused coping strategies, and therefore, enhance caregivers’ psychosocial health. Therefore, this study aimed to explore the coping strategies of caregivers of children who have survived cancer.
Materials and methods
Design
This study used a cross-sectional survey design to explore the coping strategies of caregivers of children who have survived paediatric cancer.
Participants and settings
The study recruited caregivers of children who have survived cancer through the paediatric quality of life clinic at King Hussein Cancer Centre (KHCC) in Jordan. Care providers in this clinic (paediatric oncologist and specialised oncology nurses) follow up yearly with children and their caregivers in relation to child and family health and quality of life after surviving the cancer condition. Eligibility criteria for caregivers to participate in this study included: (a) caregivers of children who have survived cancer, (b) children who were clients in the paediatric survivors’ clinic at KHCC, (c) children who were off cancer treatment for at least 2 years and (d) caregiver who can read and write in Arabic in order to complete the study survey. The study excluded caregivers who did not meet the inclusion criteria mentioned above.
Instruments
The Brief COPE
It is a shorter version of the COPE Inventory and measures individuals’ ways of coping in different life situations. The Brief COPE consists of 14 coping subscales with two items in each (28 items in total): Self-distraction (eg, I’ve been turning to work or other activities to take my mind off things); Active coping (eg, I’ve been concentrating my efforts on doing something about the situation I’m in); Denial (eg, I’ve been saying to myself ‘this isn’t real’); Substance use (eg, I’ve been using alcohol or other drugs to make myself feel better); Use of emotional support (eg, I’ve been getting emotional support from others); Use of instrumental support (eg, I’ve been getting help and advice from other people); Behavioural disengagement (eg, I’ve been giving up trying to deal with it); Venting (eg, I’ve been giving up trying to deal with it); Positive reframing (eg, I’ve been trying to see it in a different light, to make it seem more positive); Planning (eg, I’ve been trying to come up with a strategy about what to do); Humour (eg, I’ve been making jokes about it); Acceptance (eg, I’ve been accepting the reality of the fact that it has happened); Religion (eg, I’ve been trying to find comfort in my religion or spiritual beliefs) and Self-blame (I’ve been criticising myself).17
Subscales’ scores are generated by summing items for each subscale. Higher subscale scores indicate a respondent’s tendency to engage in a particular coping strategy.22 Several studies explored the psychometric properties of Brief COPE. For example, Hagan et al, which sampled individuals newly diagnosed with incurable lung and gastrointestinal cancers, suggested that the Brief COPE had good psychometric properties among this population.23 Also, Nunes et al found that the Brief COPE is a psychometrically sound instrument that shows measurement invariance across samples and good reliability.24
Researchers in this study performed the forward–backward translation of the original English Brief COPE into the Arabic language (after obtaining permission from the primary COPE author Dr Carver by email) according to WHO’s recommendations for forward–backward translations of assessment tools.25 NI (who knows Arabic and English very well, is a healthcare professional and an expert in the terms of the Brief COPE) performed the forward translation of the Brief COPE from English into Arabic. An expert panel (NI and SM) reviewed the Arabic translated Brief COPE terminology, discussed any conflicts and agreed on the pre-final Arabic version. This expert panel took into consideration cultural adaptation, common language use and conceptual equivalence of the scale. Then, a bilingual healthcare professional (occupational therapist, had a master’s degree in rehabilitation and expert in the language of the Brief COPE) performed the backward translation of the Arabic-translated Brief COPE into English. An expert panel (NI and SM) reviewed the backward translated version, discussed conflicts in wordings, changed and agreed on the final Arabic version.
The demographic and condition questionnaire
Researchers in this study designed this questionnaire to collect child and caregiver demographic and condition information, like child age, gender, diagnosis, medical and educational services, and caregiver education and social status.
Procedures
Researchers prepared the study survey, which consisted of the Child and Caregiver Demographic and Condition Questionnaire and the Arabic version of the Brief COPE. A registered nurse at the paediatric survivors’ clinic at KHCC. SAA initiated contact with caregivers who were waiting for their appointment and invited them to participate in this study. The nurse explained the study to caregivers and assured them that their participation was voluntary, and that they could quit the study at any time. Caregivers who agreed to participate provided informed consent and completed the study survey. Data collection took place only at the paediatric survivors’ clinic at KHCC. All completed survey papers are kept in a secure place at Jordan University of Science and Technology.
Data analyses
All data analyses procedures used the SPSS.26 After data cleaning, normality and homogeneity of variance were inspected. Then Brief COPE subscales were calculated by summing items for each subscale. Considering the Likert scale used in the Brief COPE (1=Never to 4=Always), the minimum score a participant can obtain is 2 while the maximum score is 8. Therefore, subscales’ scores from 6 to 8 reflect greater coping strategy utilisation.27 Data analyses included calculating descriptive statistics (mean, median, range and SD) and analysis of frequencies of child and caregiver demographics, and the Brief COPE subscale scores. Spearman-rank order correlation was used to explore if there were relationships between child and caregiver demographics, and caregiver utilisation of certain coping strategies. This study referred to Akoglu in classifying the strengths of correlations as follows: Negligible (0 to 0.09), Weak (0.1 to 0.19), Moderate (0.2 to 0.29), Strong (0.3 to 0.59), Very strong (0.6 to 0.89) and Perfect (0.9 to 1).28 Then, linear regression analysis explored how significant correlates affect caregiver coping strategy utilisation. The significance level was set at 0.05 for the correlations and regression analyses.
Results
102 caregivers participated in this study and completed the study survey. Around 66% of the caregivers were mothers, 83% were married, only 18% had a bachelor’s degree and almost half of them were unemployed. Around half of the children who have survived cancer were males, and 34.3% were in elementary school grades 1–6. Around 60% of the children had between 3 and 5 siblings, and 22.5% were first in order among their siblings. The most common cancer condition was acute leukaemia 43.1%, followed by Rhabdomyosarcoma (11.8%), bone tumours (10.8%) and Wilms (8.8%). 35% had current health problems, and 56% did not receive rehabilitative services (occupational therapy, physical therapy, special education and/or speech and language services) (see tables 1 and 2 for additional demographic-related and condition-related characteristics).
Table 1.
Demographic characteristics of caregivers and children, N=102
| Caregiver demographics | Child demographics | ||||
| Relationship to child | Mother | 65 (63.7) | Child gender | Male | 53 (52) |
| Father | 31 (30.4) | Female | 45 (44.1) | ||
| Others | 4 (3.9) | Prefer not to report | 4 (3.9) | ||
| Prefer not to report | 2 (2) | ||||
| Child school grade | Elementary | 35 (34.3) | |||
| Social status | Married | 85 (83.3) | Middle | 35 (34.3) | |
| Divorced | 1 (1) | High | 16 (15.7) | ||
| Other | 14 (13.7) | ||||
| Prefer not to report | 2 (2) | Number of Siblings | <3 | 28 (27.5) | |
| 3–5 | 61 (59.8) | ||||
| Educational status | Elementary | 22 (21.6) | >5 | 12 (11.8) | |
| High school | 45 (44.1) | ||||
| Diploma | 13 (12.7) | Order of child | 1st | 23 (22.5) | |
| Bachelors | 16 (15.7) | 2nd | 28 (27.5) | ||
| Graduate | 3 (2.9) | 3rd | 21 (20.6) | ||
| Prefer not to report | 3 (2.9) | 4th–7th | 29 (28.4) | ||
| Prefer not to report | 1 | ||||
| Employment status | Full-time | 30 (29.4) | Total family members | <5 | 12 (11.8) |
| Part-time | 9 (8.8) | >5 | 86 (84.3) | ||
| Unemployed | 50 (49) | Prefer not to report | 4 (3.9) | ||
| Prefer not to report | 13 (12.7) | ||||
| Residence type | House | 30 (29.4) | |||
| Monthly income | <500 | 62 (60.8) | Apartment | 71 (69.6) | |
| 500–1000 | 27 (26.5) | Prefer not to report | 1 (1) | ||
| >1000 | 5 (4.9) | ||||
| Prefer not to report | 6 (5.9) | ||||
Notes: N=total sample number, n (%)=number and per cent of participants.
Table 2.
Condition-related characteristics of children, N=102
| Cancer diagnosis | n (%) |
| Acute leukaemia | 44 (43.1) |
| Rhabdomyosarcoma | 15 (14.7) |
| Bone tumours | 11 (10.8) |
| Wilms | 9 (8.8) |
| Lymphoma | 5 (4.9) |
| Neuroblastoma | 2 (2) |
| Germ-cell tumours | 2 (2) |
| Brain tumours | 1 (1) |
| Nasopharyngeal cancer | 1 (1) |
| Optic pathway glioma | 1 (1) |
| Prefer not to report | 11 (10.8) |
Notes: N=total sample number, n (%)=number and per cent of participants.
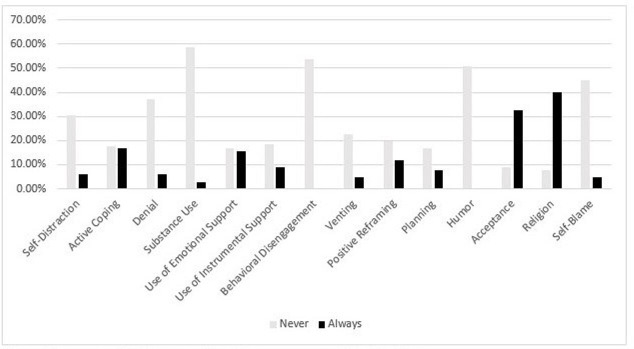
Caregivers in this study mostly used religious coping (M=6.42, SD=1.85), followed by acceptance (M=5.95, SD=1.96) and planning (M=5.05, SD=1.94) (see table 3). Caregivers rarely used humour (M=2.98, SD=1.24) and behavioural disengagement as coping strategies (M=3.01, SD=1.42). Out of the 102, four caregivers almost always use substance use as a coping strategy (see figure 1).
Table 3.
Descriptive statistics of the Brief COPE subscale scores, N=102
| Brief COPE subscales | Mean | Median | Range | Min | Max |
| Religion | 6.42 | 7.00 | 6.00 | 2.00 | 8.00 |
| Acceptance | 5.95 | 6.00 | 6.00 | 2.00 | 8.00 |
| Planning | 5.10 | 5.00 | 6.00 | 2.00 | 8.00 |
| Active coping | 5.01 | 5.00 | 6.00 | 2.00 | 8.00 |
| Positive reframing | 4.96 | 5.00 | 6.00 | 2.00 | 8.00 |
| Use of emotional support | 4.89 | 5.00 | 6.00 | 2.00 | 8.00 |
| Use of instrumental support | 4.83 | 5.00 | 6.00 | 2.00 | 8.00 |
| Venting | 4.30 | 4.00 | 6.00 | 2.00 | 8.00 |
| Self-distraction | 4.10 | 4.00 | 6.00 | 2.00 | 8.00 |
| Denial | 3.69 | 3.00 | 6.00 | 2.00 | 8.00 |
| Self-blame | 3.52 | 3.00 | 6.00 | 2.00 | 8.00 |
| Substance use | 3.11 | 2.00 | 6.00 | 2.00 | 8.00 |
| Behavioural disengagement | 3.09 | 2.00 | 5.00 | 2.00 | 7.00 |
| Humour | 2.98 | 2.00 | 5.00 | 2.00 | 7.00 |
Notes: N=Total sample size.
Max, maximum subscale score; Min, minimum subscale score.
Figure 1.
Caregivers’ utilisation of different coping strategies. Responses 1=Never and 4=Always were used in this figure. Religion and acceptance coping were mostly used by caregivers of children who have survived paediatric cancer, while humour and behavioural disengagement were the least used coping strategies.
A number of caregiver and child demographics were correlated with using different coping strategies. For example, caregiver educational levels were negatively associated with self-distraction (r s=−0.273, p=0.006), use of instrumental support (r s=−0.268, p=0.007) and self-blame (r s=−0.217, p=0.031). In specific, elementary school education (a lower level of education) was positively associated with using more self-distraction (r s=0.227, p=0.022) and more self-blame (r s=0.248, p=0.012), while having a bachelor’s degree (a higher level of education) was associated with less self-distraction (r s=−0.206, p=0.038). Also, having a graduate degree was associated with more use of instrumental support (r s=0.249, p=0.012). Besides caregiver education, having a female child was positively associated with using more self-distraction (r s=0.284, p=0.004), use of emotional support (r s=0.201, p=0.043) and use of instrumental support (r s=0.205, p=0.038). Also, having current health or educational problems in children who have survived cancer was positively associated with more caregiver substance use utilisation (r s=0.245, p=0.015) (see table 4 for additional significant correlations). Linear regression showed that having a female child predicted more self-distraction utilisation (β=0.265, p=0.007).
Table 4.
Correlations between caregiver characteristics and coping strategies
| Relationship to child | Educational level | Employment status | Child gender | Current Health Problems |
Child order | Number of siblings | |
| Self-distraction | −0.273** 0.006 |
0.216* 0.042 |
0.297** 0.003 |
||||
| Substance use | 0.255* 0.011 |
||||||
| Use of emotional support | 0.201* 0.047 |
||||||
| Use of instrumental support | −0.268** 0.007 |
0.211* | −0.226* 0.023 |
||||
| Venting | −0.213* 0.034 |
−0.203* 0.042 |
|||||
| Self-blame | −0.236* 0.018 |
−0.217* 0.031 |
Notes: *p<0.05, **p<0.01.
Discussion
This study explored coping strategies among caregivers of children who have survived cancer in Jordan and analysed potential associations between caregiver and child demographics and the utilisation of different coping strategies. Caregivers most frequently used religion coping, followed by acceptance and planning. The least used coping strategies were humour and behavioural disengagement as coping strategies. More than half of the caregivers were mothers, and half of them were unemployed. Only a small percentage of the caregivers in this study had a bachelor’s or a graduate educational degree. Demographical characteristics in this study will help in discussing caregiver utilisation of different coping strategies in the following paragraphs.
Findings from this study showed that caregivers mostly used religious coping to overcome everyday stressors. Considering cancer as a very serious and life-threatening condition,29 individuals with cancer and/or their caregivers might view cancer as a hopeless condition that has no effective treatment.30 Therefore, caregivers might turn to spiritual and religious coping mechanisms as more powerful and alleviating treatment options.31 This finding is aligned with much previous research on individuals with cancer in the Eastern32 33 and Western countries.34 Religious coping, especially in the early stages of cancer treatment, may help caregivers in redefining potential stressors as beneficial,32 and accepting the condition and its consequences.35
The novel finding from this study is that caregivers may continue to use religion coping even after their children’s survival from the cancer condition. Closely looking at the characteristics of caregivers who frequently used religion, most of them were mothers and had only a school degree (66% for both). Also, almost all of them were unemployed. Given that religious coping does not involve scheduling appointments, planning treatments and paying for treatments, caregivers in this study might find it a suitable and comfortable way to overcome stress. In addition, caregivers in this study might feel thankful for their children’s survival and continue their spiritual practices seeking help for residual health problems. It is important to mention here that religious coping, even if it involves engaging in spiritual activities, does not solve the actual stressor and its consequences. Therefore, there is contradicting evidence about the effect of engaging in religious coping on individuals’ health and quality of life.35 36
While not as frequent as religion, caregivers in this study also engaged in acceptance and planning coping. Considering that this study was after cancer survival, and a significant amount of time was spent dealing with cancer, using acceptance coping might seem typical for this population. Acceptance is showed as a common way of coping in individuals with terminal illness, and can improve individuals’ quality of life.37 Acceptance is also viewed as the step after denial,38 and before searching for treatment options, and solving any related stressors. However, when individuals engage in acceptance coping, they are not actively solving their problem.39 Therefore, it might be considered as a passive way of coping and should be used with more active ways like planning and active coping. Caregivers also used planning, but this study did not investigate if planning complemented acceptance coping. It is worth studying in the future what coping strategies do caregiver combine to form their coping profile.
The least used coping strategies by caregivers in this study were humour and behavioural disengagement. In looking at the definition of humour as making jokes or fun of the situation, and the definition of behavioural disengagement as giving up coping, it is obvious that these coping mechanisms might be more relevant to early stages of the cancer experience. After battling a significant and serious disease with their beloved children, caregivers may turn into more mature and strong individuals for their children and families. Therefore, caregivers in this study might not find it appropriate to engage in humour, nor withdraw from their children’s condition. Instead, caregivers in this study were clients in the health and wellness clinic after cancer and continued to be part of the condition with their children. In some research, humour and behavioural disengagement along with substance use were considered as maladaptive and dysfunctional ways of managing stressors.40 41 In other studies, humour was viewed as a comforting and relaxing mechanism that promotes caregivers’ health.42 43 It is worth further investigating if promoting the use of humour in caregivers of children who have survived cancer can alleviate caregivers’ psychosocial health and improve the quality of life of caregivers and their families.
This study found that having a girl child cancer survivor predicted caregivers’ utilisation of more self-distraction as a coping strategy. Caregivers’ active engagement in activities other than thinking about current health problems of their girls might be a mechanism to forget the problem and its consequences. There is a strong cultural belief in the Arab world that girls’ role in the community comes from their ability to form families, and born and raise children.44 Caregivers in this study who were mostly mothers, might engage in self-distraction in a medium amount to stop thinking about their daughters’ abilities to be future wives and mothers. The invasive treatments and their side effects might impose many physical disabilities, and change body appearance and function.
Although correlation analyses yielded low to medium associations, these were worth mentioning and discuss to contribute to the limited evidence in this area. Having the lowest level of education (elementary) was associated with using more self-blame and self-distraction, while having the highest level of education (graduate) was associated with using more instrumental support. Having higher forms of education might help caregivers to move from passive to active ways of coping. Instrumental use of support, which is using help and advice from other people who might be professionals in supporting caregivers, was minimally studied in the literature. One study showed that emotional social support seeking predicted better individual and family psychosocial functioning while instrumental social support seeking did not.45
In another association, having current medical and/or educational problems was associated with more substance use. While substance use was not a frequent coping mechanism by caregivers in this study, almost half of the caregivers responded ‘2=I’ve been doing this a little bit’ to one of the two items that for the substance use subscale. These two items involve using alcohol and/or drugs to overcome problems. Substance use affects the health and quality of life of individuals and their families.46 Almost half the caregivers, who had some degree of engagement in substance use in this study, had between 3 and 5 children, and almost half of them had a relatively low family income. These results suggested the need to promote caregivers’ limited time and financial resources towards solving their families’ medical and educational needs.
In summary, caregivers of children who have survived cancer in this study used mostly religion coping. This study did not investigate the reasons why caregivers did not frequently use other ways of coping that are defined in the literature as problem-focused like active coping, or that involve other professionals or family members like use of emotional and instrumental support coping. Given that coping is a highly individualised process, there might be factors, like the cultural and social contexts, that characterise this process and are still under-investigated. Further investigation of potential factors that affect caregiver coping will inform care providers on how to support caregivers’ utilisation of adaptive and active ways of coping that promote caregivers’ and families’ health and well-being.
Strengths and limitations
This study was novel in investigating coping of caregivers of children who have survived cancer in Jordan. While the study used a convenient sample of caregivers from KHCC, this later setting is the primary cancer centre in Jordan and serves clients from different Jordanian cities. The utilisation of the Brief COPE was helpful in investigating a wide variety of caregivers’ coping styles. While this study performed the forward and backward translation of the Brief COPE into Arabic, and a committee discussed the words and phrases in both languages before agreeing on the final Arabic version, it did not investigate the psychometric properties of the Arabic Brief COPE. There were missing data related to caregivers and child demographics (as reported in the tables), especially those related to age, and therefore, were not included in the analyses. Finally, this cross-sectional study did not investigate whether caregivers’ utilisation of different coping strategies changes from the diagnosis, during treatment and after surviving cancer.
Conclusions
Caregivers of children who have survived cancer in Jordan used mostly passive coping strategies like religious coping and acceptance. Also, having a girl cancer survivor predicted caregivers’ utilisation of more self-distraction coping. Psychosocial interventions to support caregivers’ utilisation of active coping strategies like active coping and use of emotional and instrumental support are important to promote caregivers’ and families’ psychosocial health and quality of life.
Supplementary Material
Acknowledgments
The research team would like to thank caregivers who had participated in this study and shared their time experiences for the purposes of this project.
Footnotes
Contributors: NI and TI researched literature and conceived the study. All authors were involved in protocol development. NI, TI and AJ were involved in gaining ethical approval, patient recruitment and data analysis. NI and TI wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript. The first author NI is the guarantor author. She accepts full responsibility for the work and/or the conduct of the study, has access to the data, and controls the decision to publish.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: There is no competing of interest.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Consent obtained from parent(s)/guardian(s)
Ethics approval
This study involves human participants and was approved by Institutional Review Board of King Hussein Cancer Center approved the study (Research # 17 KHCC 121). Participants gave informed consent to participate in the study before taking part.
References
- 1. Viale PH. The American Cancer society’s facts & figures: 2020 edition. J Adv Pract Oncol 2020;11:135–6. 10.6004/jadpro.2020.11.2.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Song JI, Shin DW, Choi JY, et al. Quality of life and mental health in family Caregivers of patients with terminal cancer. Support Care Cancer 2011;19:1519–26. 10.1007/s00520-010-0977-8 [DOI] [PubMed] [Google Scholar]
- 3. Ness KK, Hudson MM, Ginsberg JP, et al. Physical performance limitations in the childhood cancer survivor study cohort. J Clin Oncol 2009;27:2382–9. 10.1200/JCO.2008.21.1482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bonner MJ, Hardy KK, Willard VW, et al. Additional evidence of a nonverbal learning disability in survivors of pediatric brain tumors. Children’s Health Care 2009;38:49–63. 10.1080/02739610802615849 [DOI] [Google Scholar]
- 5. Li HCW, Lopez V, Joyce Chung OK, et al. The impact of cancer on the physical, psychological and social well-being of childhood cancer survivors. Eur J Oncol Nurs 2013;17:214–9. 10.1016/j.ejon.2012.07.010 [DOI] [PubMed] [Google Scholar]
- 6. Gage-Bouchard EA, Devine KA, Heckler CE. The relationship between socio-demographic characteristics, family environment, and Caregiver coping in families of children with cancer. J Clin Psychol Med Settings 2013;20:478–87. 10.1007/s10880-013-9362-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kohlsdorf M, Costa Junior ÁL. Coping strategies and Caregiver’s anxiety in pediatric Oncohematology. Psicologia: Reflexão e Crítica 2011;24:272–80. [Google Scholar]
- 8. Pinquart M. Parenting stress in Caregivers of children with chronic physical condition—A Meta‐Analysis. Stress Health 2018;34:197–207. 10.1002/smi.2780 [DOI] [PubMed] [Google Scholar]
- 9. Litzelman K, Kent EE, Rowland JH. Interrelationships between health behaviors and coping strategies among informal Caregivers of cancer survivors. Health Educ Behav 2018;45:90–100. 10.1177/1090198117705164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vrettos I, Kamposioras K, Kontodimopoulos N, et al. Comparing health-related quality of life of cancer patients under chemotherapy and of their Caregivers. ScientificWorldJournal 2012;2012:135283. 10.1100/2012/135283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Üzar-Özçeti N YS, Dursun Sİ. Quality of life, Caregiver burden, and resilience among the family Caregivers of cancer survivors. Eur J Oncol Nurs 2020;48:101832. 10.1016/j.ejon.2020.101832 [DOI] [PubMed] [Google Scholar]
- 12. Fladeboe K, King K, Kawamura J, et al. Featured article: Caregiver perceptions of stress and Sibling conflict during pediatric cancer treatment. J Pediatr Psychol 2018;43:588–98. 10.1093/jpepsy/jsy008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pierce L, Hocking MC, Schwartz LA, et al. Caregiver distress and patient Health‐Related quality of life: Psychosocial screening during pediatric cancer treatment. Psychooncology 2017;26:1555–61. 10.1002/pon.4171 [DOI] [PubMed] [Google Scholar]
- 14. Biggs A, Drummond S, Brough P. Lazarus and Folkman’s psychological stress and coping theory. The handbook of stress and health: A guide to research and practice. 2017;349–64. 10.1002/9781118993811 [DOI]
- 15. Kirby LD, Qian W, Adiguzel Z, et al. Appraisal and coping predict health and Well‐Being during the COVID‐19 pandemic: an international approach. Int J Psycho 2022;57:49–62. [DOI] [PubMed] [Google Scholar]
- 16. Carver CS, Connor-Smith J. Personality and coping. Annu Rev Psychol 2010;61:679–704. 10.1146/annurev.psych.093008.100352 [DOI] [PubMed] [Google Scholar]
- 17. Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol 1989;56:267–83. 10.1037//0022-3514.56.2.267 [DOI] [PubMed] [Google Scholar]
- 18. Lazarus RS, Folkman S. Stress, Appraisal, and Coping. Springer publishing company, 1984. [Google Scholar]
- 19. O’Brien CW, Moorey S. Outlook and adaptation in advanced cancer: a systematic review. Psychooncology 2010;19:1239–49. 10.1002/pon.1704 [DOI] [PubMed] [Google Scholar]
- 20. Mayordomo T, Viguer P, Sales A. Resilience and coping as predictors of well-being in adults. Mental Health Psychopathol 2021;265–77. 10.4324/9781003243601 [DOI] [Google Scholar]
- 21. Knowles SR, Apputhurai P, O’Brien CL, et al. Exploring the relationships between illness perceptions, self-efficacy, coping strategies, psychological distress and quality of life in a cohort of adults with diabetes mellitus. Psychol Health Med 2020;25:214–28. 10.1080/13548506.2019.1695865 [DOI] [PubMed] [Google Scholar]
- 22. Greer TM. Measuring coping strategies among African Americans: an exploration of the latent structure of the COPE inventory. J Black Psychol 2007;33:260–77. 10.1177/0095798407302539 [DOI] [Google Scholar]
- 23. Hagan TL, Fishbein JN, Nipp RD, et al. Coping in patients with incurable lung and gastrointestinal cancers: a validation study of the brief COPE. J Pain Symptom Manage 2017;53:131–8. 10.1016/j.jpainsymman.2016.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nunes C, Pérez-Padilla J, Martins C, et al. The brief COPE: measurement Invariance and Psychometric properties among community and at-risk Portuguese parents. Int J Environ Res Public Health 2021;18:2806. 10.3390/ijerph18062806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. World Health Organization . Process of Translation and Adaptation of Instruments. Geneva: WHO, 2016. Available: https://www.scirp.org/reference/referencespapers?referenceid=3514337 [Google Scholar]
- 26. IBM Corp . Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp, 2015. [Google Scholar]
- 27. Ismael N, Lawson LM, Moqbel M, et al. Coping strategies among Caregivers of children with autism spectrum disorders: A cluster analysis. Int J Med Health Sci 2018;7. [Google Scholar]
- 28. Akoglu H. User’s guide to correlation coefficients. Turk J Emerg Med 2018;18:91–3. 10.1016/j.tjem.2018.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lee JW, Cho B. Prognostic factors and treatment of pediatric acute Lymphoblastic leukemia. Korean J Pediatr 2017;60:129–37:129. 10.3345/kjp.2017.60.5.129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rafferty KA. n.d. Everything remains uncertain: theorizing parents' communication about uncertainty, hope, and hopelessness while managing complex pediatric chronic conditions (Doctoral Dissertation, the University of Wisconsin-Milwaukee).
- 31. Lagman RA, Yoo GJ, Levine EG, et al. Leaving it to God” religion and spirituality among Filipina immigrant breast cancer survivors. J Relig Health 2014;53:449–60. 10.1007/s10943-012-9648-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ahmadi F, Mohamed Hussin NA, Mohammad MT. Religion, culture and meaning-making coping: A study among cancer patients in Malaysia. J Relig Health 2019;58:1909–24. 10.1007/s10943-018-0636-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Elsheshtawy EA, Abo-Elez WF, Ashour HS, et al. Coping strategies in Egyptian ladies with breast cancer. Breast Cancer (Auckl) 2014;8:97–102. 10.4137/BCBCR.S14755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Thuné-Boyle ICV, Stygall J, Keshtgar MRS, et al. Religious coping strategies in patients diagnosed with breast cancer in the UK. Psychooncology 2011;20:771–82. 10.1002/pon.1784 [DOI] [PubMed] [Google Scholar]
- 35. Haghighi F. Correlation between religious coping and depression in cancer patients. Psychiatr Danub 2013;25:236–40. [PubMed] [Google Scholar]
- 36. Ng GC, Mohamed S, Sulaiman AH, et al. Anxiety and depression in cancer patients: the association with religiosity and religious coping. J Relig Health 2017;56:575–90. 10.1007/s10943-016-0267-y [DOI] [PubMed] [Google Scholar]
- 37. Nipp RD, El-Jawahri A, Fishbein JN, et al. The relationship between coping strategies, quality of life, and mood in patients with incurable cancer. Cancer 2016;122:2110–6. 10.1002/cncr.30025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kübler-Ross E, Kessler D. The Five Stages of Grief. InLibrary of Congress Catalogin in Publication Data (Ed.), On Grief and Grieving.2009:7–30. [Google Scholar]
- 39. Norberg AL, Lindblad F, Boman KK. Coping strategies in parents of children with cancer. Soc Sci Med 2005;60:965–75. 10.1016/j.socscimed.2004.06.030 [DOI] [PubMed] [Google Scholar]
- 40. Costas-Muñiz R. Hispanic adolescents coping with parental cancer. Support Care Cancer 2012;20:413–7. 10.1007/s00520-011-1283-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Parekh NK, Shah S, McMaster K. Effects of Caregiver burden on quality of life and coping strategies utilized by Caregivers of adult patients with inflammatory bowel disease. Aog 2016;30:89. 10.20524/aog.2016.0084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Christie W, Moore C. The impact of humor on patients with cancer. Clin J Oncol Nurs 2005;9:211–8. 10.1188/05.CJON.211-218 [DOI] [PubMed] [Google Scholar]
- 43. Tan T, Schneider MA. Humor as a coping strategy for adult-child Caregivers of individuals with Alzheimer’s disease. Geriatr Nurs 2009;30:397–408. 10.1016/j.gerinurse.2009.09.004 [DOI] [PubMed] [Google Scholar]
- 44. Douki S, Zineb SB, Nacef F, et al. Women’s mental health in the Muslim world: cultural, religious, and social issues. J Affect Disord 2007;102:177–89. 10.1016/j.jad.2006.09.027 [DOI] [PubMed] [Google Scholar]
- 45. Hill EM. Quality of life and mental health among women with ovarian cancer: examining the role of emotional and instrumental social support seeking. Psychol Health Med 2016;21:551–61. 10.1080/13548506.2015.1109674 [DOI] [PubMed] [Google Scholar]
- 46. Belizaire LS, Fuertes JN. Attachment, coping, Acculturative stress, and quality of life among Haitian immigrants. Jour of Counseling &Amp; Develop 2011;89:89–97. 10.1002/j.1556-6678.2011.tb00064.x [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request.