Abstract
Objectives
To identify the ultrasound methods used in the literature to measure traumatic scar thickness, and map gaps in the translation of these methods using evidence across the research-to-practice pipeline.
Design
Scoping review.
Data sources
Electronic database searches of Ovid MEDLINE, Embase, Cumulative Index of Nursing and Allied Health Literature and Web of Science. Grey literature searches were conducted in Google. Searches were conducted from inception (date last searched 27 May 2022).
Data extraction
Records using brightness mode (B-mode) ultrasound to measure scar and skin thickness across the research-to-practice pipeline of evidence were included. Data were extracted from included records pertaining to: methods used; reliability and measurement error; clinical, health service, implementation and feasibility outcomes; factors influencing measurement methods; strengths and limitations; and use of measurement guidelines and/or frameworks.
Results
Of the 9309 records identified, 118 were analysed (n=82 articles, n=36 abstracts) encompassing 5213 participants. Reporting of methods used was poor. B-mode, including high-frequency (ie, >20 MHz) ultrasound was the most common type of ultrasound used (n=72 records; 61% of records), and measurement of the combined epidermal and dermal thickness (n=28; 24%) was more commonly measured than the epidermis or dermis alone (n=7, 6%). Reliability of ultrasound measurement was poorly reported (n=14; 12%). The scar characteristics most commonly reported to be measured were epidermal oedema, dermal fibrosis and hair follicle density. Most records analysed (n=115; 97%) pertained to the early stages of the research-to-practice pipeline, as part of research initiatives.
Conclusions
The lack of evaluation of measurement initiatives in routine clinical practice was identified as an evidence gap. Diverse methods used in the literature identified the need for greater standardisation of ultrasound thickness measurements. Findings have been used to develop nine methodological considerations for practitioners to guide methods and reporting.
Keywords: patient-centered care, psychometrics, ultrasound, ultrasonography
STRENGTHS AND LIMITATIONS OF THIS STUDY
Use of the Australian Government Department of Health and Aged Care Medical Research Future Fund research-to-practice pipeline phases to categorise records allowed identification of gaps in the use of ultrasound for clinical practice.
Clinical, health service, implementation and feasibility outcomes related to ultrasound measurement in included records were summarised to determine what is needed to close the research-to-practice gap for ultrasound measurement of scar thickness.
A limitation is that only articles available in English or with an English abstract were considered for inclusion and data extraction, thus findings are likely most relevant to English-speaking countries.
Introduction
Traumatic cutaneous injury, caused by sharp object penetration (eg, surgery or vaccination) or burns (including thermal, chemical and friction) may result in the formation of hypertrophic scarring.1 Hypertrophic scars result from an aberrant cutaneous healing response that leads to the formation of red, raised scars, often accompanied by pruritus and skin tightening, which remain within the boundaries of the initial injury.2–7 The sequelae of hypertrophic scars can impact on patient’s physical and psychosocial quality of life.8 9
A characteristic of hypertrophic scarring that both patients and clinicians have identified as being important, and which has subsequently been used as a way to measure clinical and treatment outcomes, is scar thickness.9–17 Scar thickness can be measured both subjectively, through clinician assessment and patient-reported outcomes, or objectively, using medical imaging methods.18 19 The pathological complexity of hypertrophic scars means that they generally extend below the level of the surrounding skin, supporting the use of medical imaging modalities such as ultrasound for thickness quantification, as these are capable of providing information about subcutaneous structures and processes.19 20 Scar thickness measurement using ultrasound can be conducted in both clinical and research contexts. Where routine measurements like ultrasound are used to guide clinical decision-making and treatment, this practice is known as measurement-based care.21
Ultrasound is a safe, non-invasive and largely cost-effective (compared with other imaging modalities) imaging method with measurement utility in both adult and paediatric populations.22–24 Modern brightness mode (B-mode) ultrasound, particularly high-frequency (ie, ≥20 MHz) or ultra-high-frequency (30–100 MHz)25 ultrasonography, allows differentiation between the epidermis and dermis, which permits quantification of skin layer-specific scar characteristics. This differentiation may allow assessors to observe and understand the pathological mechanisms of individual scars and adjust treatment protocols accordingly.24 26–31 Additionally, B-mode ultrasound is commonly used as the basis for other imaging methods, such as colour Doppler ultrasound or elastography, which can allow quantification of additional scar characteristics, such as their elastic properties.26–29 32 33
Despite the clinical advantages of B-mode ultrasound for scar thickness measurement, methods are poorly reported and lack standardisation in the literature. This casts doubt on the validity of clinical decision-making in measurement-based care initiatives (eg, setting depth of ablative fractional carbon dioxide laser penetration) informed by research findings (eg, response to treatment) where ultrasound measurements are used.34 Lack of standardisation also makes between-study comparison, such as systematic reviews and meta-analyses, difficult,35 and poor methodological reporting hampers the ability to accurately replicate findings. This scoping review focuses on mapping and identifying gaps in ultrasound methods and evaluation reported in the current literature along the research-to-clinical practice pipeline.36 Methodological considerations for people performing ultrasound scar thickness measurements, including practitioners (herein termed assessors) using ultrasound in clinical practice, are presented based on the review findings.
Methods
Protocol publication and review structure
The protocol for this review has been published a priori.37 This scoping review was conducted and is reported according to the framework by Arksey and O’Malley.38 The steps outlined in this framework are: (1) identifying the research question; (2) identifying the relevant records; (3) selecting appropriate records; (4) charting extracted data; and (5) collating, summarising and reporting the results.38
Identifying the research question
The primary question of this scoping review was: “What do we know and not know about the measurement of traumatic cutaneous scar thickness using ultrasound?” This question was addressed through exploration of: methods used; reliability and measurement error; clinical, health service, implementation and feasibility outcomes; factors influencing ultrasound imaging and measurement methods; strengths and limitations of measurement methods and use of measurement guidelines and/or frameworks. While the focus of this review was the measurement of traumatic cutaneous scar thickness with ultrasound, methods used to measure the thickness of unscarred skin were reported where these were used in combination with measurement of scar thickness (eg, as control or comparator measurements).
Identifying the relevant records
A standardised search strategy was developed and piloted with the assistance of a medical librarian using the concepts ‘ultrasound’, ‘skin’, ‘thickness’ and ‘measure’, with associated terms and truncations (online supplemental box 1). Ovid MEDLINE, Embase, Cumulative Index of Nursing and Allied Health Literature (CINAHL) and Web of Science electronic databases were searched from conception to identify original studies (date last searched 27 May 2022).
bmjopen-2023-078361supp001.pdf (464.1KB, pdf)
The phrase ‘ultrasound scar thickness measurement’ was used to conduct additional searches in (1) Google Scholar and (2) Google to identify original studies in grey literature, and studies not identified in database searches. Title and abstract searches in Google Scholar and Google were limited to the first 200 results.39
Record selection
Following deduplication, six reviewers screened records using Covidence (Veritas Health Innovation, Melbourne, Australia; available at www.covidence.org) for eligibility according to the inclusion criteria (table 1). Both peer-reviewed journal articles and abstracts were included to ensure that all the available and most recent methodological information was obtained.40 Data collected from peer-reviewed journal articles were considered the primary source of data, with information from abstracts used to confirm or extend the journal data. The inclusion of abstracts will assist future authors to further investigate the information presented as full texts may become available. During both title and abstract and full-text screening, one researcher (BM) screened all records as a single reviewer, while other researchers (MS, TM, TR, BD and ZT) screened records as a second reviewer. Conflicts were resolved through discussion between at least two authors to reach agreement. A third author was used as a tiebreaker where agreement could not be reached.
Table 1.
Inclusion and exclusion criteria for studies included in the scoping review
| Inclusion | Exclusion |
|
|
Charting the data
The data extraction table was developed in Microsoft Excel and piloted by two authors (BM and ZT) through independent extraction and comparison of data from two records. The table was then modified to include the scar characteristics (eg, fibrosis, oedema) measured, measurer/assessor training, the number of measurements taken and funding sources (online supplemental table 1). Full-text data extraction was completed by four authors (BM, MS, TM and ZT). An additional author (BD) independently extracted data from five randomly selected records, which was compared with data extracted by other authors. Minimal differences between data extracted by the independent author and that by other authors were observed, thus further independent extraction was not performed. As is typical in scoping reviews, the certainty or quality of evidence was not appraised.38
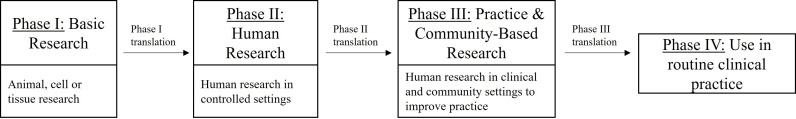
The research-to-practice pipeline published by the Australian Government Department of Health and Aged Care Medical Research Future Fund (figure 1) was used to categorise each included record based on their stated aims into one of the four phases.36 Studies related to phase I of this pipeline, basic research, were only included in this review when data on scar or skin thickness pertained to human participants (table 1). Phase II of this pipeline included randomised controlled trials, while phase III included pragmatic and observational studies conducted outside randomised controlled trials. The final phase of this pipeline (phase IV) indicates initiatives used in routine clinical practice.
Figure 1.
Research to clinical practice pipeline.
Where clinical (eg, treatment satisfaction, scar symptoms), health service (eg, efficiency, safety, effectiveness, equity, patient-centredness and timeliness) and implementation (eg, acceptability, adoption, appropriateness, fidelity, cost, penetration and sustainability) outcomes were addressed, they were reported and defined according to Proctor et al.41 For example, in the context of this scoping review, acceptability is defined as the level to which ultrasound is palatable among stakeholders (eg, assessors), appropriateness is the perceived fit of ultrasound within regular clinical practice and fidelity is the degree to which ultrasound is used in the way it was initially described.41 Measurement instrument-specific feasibility outcomes defined by Prinsen et al 42 are reported in the current review. These outcomes included ease of administration, standardisation, completion time, instrument cost and availability and ease of score calculation.42 Reliability and measurement error were defined according to COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) tools.43 44 Measurements with an intraclass correlation coefficient (ICC) of 0.7 or greater were considered reliable.44 Measurement error was assessed by comparing the reported SEM with the reported smallest detectable change (SDC). Where the reported measurement error was smaller than the reported smallest detectable change, it was interpreted as indicating real change or variance can be detected, and that change or variance is not a result of error.44
Patient and public involvement
There was no patient and/or public involvement in the design, conduct, reporting or dissemination of information in this scoping review.
Results
Electronic database searches identified 9309 records. After removal of 3703 duplicate records, the titles and abstracts of 5606 records were screened for relevance according to the inclusion criteria (table 1). Following full-text screening, 104 records proceeded to data extraction. Searches in Google and Google Scholar identified an additional 14 records, providing a total of 118 records for data extraction. Search and screening results are presented according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) flow diagram (online supplemental figure 1).45
Record characteristics
Of the 118 records included in this review, 82 were journal articles (69%) and 36 were abstracts (31%) (table 2), representing a total of 5213 participants (range 1–438; mode 20 participants per record). Adults aged 18 years and older were the most highly represented age group reported in articles (n=43 articles; 52% of articles),17 26 29 46–85 while most abstracts did not report the age group measured (n=25 abstracts; 69% of abstracts).86–110 The most common scar type measured was burn scars in both journal articles (n=43 articles; 52% of articles),17 22–24 27 47 57–59 61 62 64–67 71–75 81 82 84 111–130 and abstracts (n=23 abstracts; 64% of abstracts)28 30 86–88 91–94 96 98 102–106 131–135 (table 2). Most identified articles used ultrasound measurement of scar thickness as part of research initiatives, and were categorised as either phase II (n=50 articles; 61% of articles)17 22 26 31 46–49 51–56 61 63–65 67 69–71 74–76 78 81 83 84 111 112 114 115 117 124–127 129 130 136–145 or phase III (n=30 articles; 37% of articles).23 24 27 29 50 57–60 62 66 68 72 73 77 79 80 82 85 116 118 120–123 128 146–149 on the research-to-practice pipeline.36 Phase II was also the most common phase represented by abstracts (n=21; 58% of abstracts), 86 88 91 93 95 97 99–104 106–108 131–134 150 151 followed by phase III (n=15 abstracts; 42% of abstracts).28 30 87 89 90 94 96 98 105 109 110 135 152–154 Phase IV was addressed by two articles (2% of articles)113 119 and one abstract (2% of abstracts),92 which used ultrasound to measure treatment response to an intervention already used in routine clinical practice, including compression garments113 119 and CO2 fractional laser.92 No records pertained to phase I.
Table 2.
Summary of characteristics of records included in this review*
| Characteristic | Category | Number of records (translational pipeline phase II)† | Number of records (translational pipeline phase III)† | Number of records (translational pipeline phase IV)† |
| Journal articles | ||||
| Funding source | Commercial | 2 | 1 | 1 |
| Non-commercial | 23 | 13 | 0 | |
| Commercial and non-commercial | 2 | 1 | 1 | |
| No funding | 6 | 3 | 0 | |
| Not reported | 16 | 12 | 0 | |
| Population type | Adult | 27 | 16 | 0 |
| Paediatric | 6 | 4 | 0 | |
| Paediatric and adult | 13 | 7 | 2 | |
| Not reported | 3 | 3 | 0 | |
| Scar aetiology | Burn | 22 | 18 | 1 |
| Surgical‡ | 5 | 2 | 0 | |
| Mixed | 10 | 3 | 0 | |
| Not specified | 12 | 7 | 0 | |
| Abstracts | ||||
| Funding source | Commercial | 0 | 0 | 0 |
| Non-commercial | 3 | 1 | 0 | |
| Commercial and non-commercial | 0 | 0 | 0 | |
| No funding | 0 | 0 | 0 | |
| Not reported | 17 | 14 | 1 | |
| Population type | Adult | 1 | 2 | 0 |
| Paediatric | 0 | 3 | 0 | |
| Paediatric and adult | 4 | 1 | 0 | |
| Not reported | 15 | 9 | 1 | |
| Scar aetiology | Burn | 12 | 10 | 1 |
| Surgical‡ | 1 | 2 | 0 | |
| Mixed | 2 | 1 | 0 | |
| Not specified | 5 | 2 | 0 | |
Paediatric: measurement of patients under the age of 18 years; adult: measurement of patients aged 18 years or older; burn: scars caused by thermal, chemical or friction injury; surgical: scars caused by surgical procedures (including biopsies); mixed: scars of included record were of mixed origin (eg, burn and acne).
*A breakdown of each characteristic per record is presented in online supplemental table 2.
†Stage in the research to clinical practice translational pipeline, as defined by the Australian Government Department of Health and Aged Care.36
‡Type of surgery defined in online supplemental table 2.
Methods used to measure traumatic cutaneous scar thickness
B-mode, including high-frequency B-mode ultrasound (ie, ≥20 MHz) was the most commonly reported ultrasound type in the included articles (n=56; 68% of articles),17 22–24 26 29 31 46–49 53 54 56 57 59 60 64 65 67 69–78 80–82 84 85 111 112 114 116–118 120 122 123 126–130 138 139 141 142 144–146 149 while most abstracts did not report the type of ultrasound used (n=22; 61% of abstracts)86 87 92–98 101 103 105 106 108 131–134 150–153 (table 3). Specialised B-mode ultrasound devices, including the tissue ultrasound palpation system (TUPS; a B-mode ultrasound transducer in-series with a load cell to allow measured compression of the skin),68 99 100 124 and colour Doppler ultrasound,52 149 were used in six records (table 3).
Table 3.
Summary of measurement methods used in included record*
| Characteristic | Parameters | Number of records |
| Journal articles | ||
| Ultrasound type | B-mode | 24 |
| Mid-range | 2 | |
| High-frequency | 29 | |
| Other | 4 | |
| Not reported | 22 | |
| Measurement parameters | Epidermal | 0 |
| Dermal | 4 | |
| Epidermal and dermal | 2 | |
| Combined epidermal and dermal | 32 | |
| Other | 3 | |
| Not reported | 40 | |
| Scar characteristic measured | Fibrosis | 27 |
| Oedema | 1 | |
| Fibrosis and oedema | 10 | |
| Other | 1 | |
| Not reported | 42 | |
| Abstracts | ||
| Ultrasound type | B-mode | 3 |
| Mid-range | 0 | |
| High-frequency | 9 | |
| Other | 3 | |
| Not reported | 21 | |
| Measurement parameters | Epidermal | 0 |
| Dermal | 1 | |
| Epidermal and dermal | 4 | |
| Combined epidermal and dermal | 1 | |
| Other | 1 | |
| Not reported | 29 | |
| Scar characteristic measured | Fibrosis | 2 |
| Oedema | 0 | |
| Fibrosis and oedema | 0 | |
| Other | 0 | |
| Not reported | 34 | |
B-mode ultrasound (<20 MHz); high-frequency: high-frequency B-mode ultrasound (>20 MHz); other: fields are expanded with additional detail in online supplemental table 3.
*A full summary of each included record is available in online supplemental table 3.
B-mode, brightness mode.
The type of scar and skin thickness measurement (ie, thickness of the dermis, epidermis or combined epidermal and dermal measurement) was reported in 39 records (33%) (table 3). Where reported, combined measurement of epidermal and dermal thickness was the most common method used in articles (n=32; 76% of articles reporting skin measurement type).17 22–24 27 29 50 53 56–58 60 64–66 70 72–77 80–82 114 116 118 122 126 127 130 139 146 148 Separate epidermal and/or dermal thickness measurements were reported in seven journal articles (17% of articles reporting skin thickness measurement type).26 47 48 52 53 71 118 Of these records, two authors provided a rationale for this decision: each skin layer provided different information on the scar;26 or responded differently to treatment.67 71 Most abstracts did not report the type of skin measurement used (n=30; 83% of abstracts).28 30 91–101 103–110 131–134 150–154
Three articles (4% of articles)47 110 111 and one abstract (3% of abstracts)28 directly reported that fibrosis was the scar characteristic targeted by the measurement. One of these records also quantified hair follicle density to assess the difference between scared and unscarred skin.47 An additional 25 articles (30% of articles)17 46 52 53 56 63–65 67 70 79 80 83 84 112 120 123 125–127 140 142 145 148 149 155 and 1 abstract (3% of abstracts)110 made indirect reference (ie, within the introduction or discussion) to the measurement of fibrosis. Ten journal articles (12%) made indirect reference to the measurement of both oedema and fibrosis,31 54 55 71 74 76–78 138 144 and one record made indirect reference to the measurement of oedema.59
Additional objective and/or subjective measurement methods were employed alongside ultrasound measurement in 72 articles (88% of articles)17 22 24 26 29 31 46–53 55–57 60–70 72–81 83–85 111–122 124–130 136–142 144 145 147–149 and 31 abstracts (86% of abstracts)86 88 89 91–95 97–110 131–134 150 151 153 154 (online supplemental table 4). All three phase IV studies investigating routine clinical practice used additional measurements.92 113 119 The additional objective measurements used in included records were elastography (elasticity), cutometric assessment (pliability) and Doppler ultrasound (vascularity). The additional subjective measurements were conducted using clinician-based rating scales (eg, Vancouver Scar Scale (VSS) or modified VSS) or patient-reported outcome measures (PROMs). The VSS was used in 35 articles (43% of articles)17 31 46 47 49 50 52 55 57 61–64 66–70 73 85 111 112 114 116 118 121 124 128 130 136–138 140–142 and 11 abstracts (31% of abstracts).88 91 92 98–100 107 134 150 151 153 PROMs were used in 27 articles (33% of articles) and 11 abstracts (31% of abstracts).46 53 56 57 60 72–75 85 91 94 97 101–106 111 112 114 115 117 118 120 122 129 131–133 138 140 141 148 150 151 153 154 Of the records that reported using PROMs, the most commonly used was the patient report of the Patient and Observer Scar Assessment Scale (POSAS), used in 17 articles (63% of articles reporting use of PROMs)17 22 46 50 53 61 62 64 76 77 79 114 121 125–127 147 and 8 abstracts (73% of abstracts reporting use of PROMs)91 93 102 104 106 132 153 (online supplemental table 4). In most cases, additional measurement methods were used to supplement ultrasound thickness measurements as research outcomes. In some records (n=16; 14% of records), however, ultrasound was compared with histology, POSAS, dermoscopy, VSS and modified VSS, clinical assessment, modified Seattle Scar Scale, high-definition optical coherence tomography, three-dimensional (3D) camera, immunohistochemistry and immunohistomorphometry.17 24 26 29 31 50 51 64 73 77 86 95 110 120 124 149 Where the effectiveness of ultrasound was judged against other methods, it was only found to be inadequate against histology.26 86
Methods used to relocate the scar for repeated measurements were reported in 34 records (29%) (online supplemental table 3). The most common relocation method was tracing the outline or boundaries of the scar on a transparent or translucent sheet (n=14 articles; 35% of articles reporting scar relocation),23 49 65 74 81 115 116 120 124 125 153 occasionally including prominent or bony landmarks close to the scar.23 24 72 73 123 Photographs (n=10 articles; 25% of articles reporting relocation and n=1 abstract) and linear measurements from defined points or anatomical landmarks on or around the scar (n=4 articles; 10% of articles reporting relocation) were also used for scar relocation. The ‘worst’ or ‘thickest’ part of the scar, as determined by patients or assessors, was chosen as the measurement site in 14 journal articles (35% of journal articles reporting relocation)23 31 52 54 57 61 62 67 126 127 138 141 148 155 and 1 abstract.105
Measurement of unscarred skin, either contralateral or adjacent to the scar, was performed in 32 articles (39% of articles)17 22–24 27 29 46–48 50 51 53 56–60 64 72 73 80 81 85 114 118 120–122 128 145 146 148 and 7 abstracts (19% of abstracts).28 94 95 150 151 153 154 These measurements were primarily used as controls or comparators to scar measurements (n=27, 69% of records reporting unscarred skin measurement).17 22 23 28 29 47 48 51 53 56–60 64 67 73 80 85 95 118 120 122 128 146 148 153 154 Additionally, four records (10% of records reporting unscarred skin measurement) evaluating treatment efficacy measured both unaffected skin thickness and the thickness of a ‘control’ or untreated scar.46 74 94 114 All instances where additional ultrasound measurements were taken of unscarred skin or untreated scars were reported as part of research initiatives aligning with phases II and III of the research-to-practice pipeline (figure 1).36
Reliability and measurement error
Reliability was calculated for both scarred and unscarred skin in 13 articles (16% of articles) and 2 abstracts (5% of abstracts), and was generally considered acceptable (online supplemental table 5). This included inter-rater reliability (n=5; 4% of articles),54 64 73 120 137 intra-rater reliability (n=3; 4% of journal articles)22 23 65 and both inter-rater and intra-rater reliability (n=7; 6%; including two abstracts).17 24 57 82 87 105 124 The ICC was the most commonly reported reliability statistic (n=10; 8% of records, including one abstract),17 24 57 64 65 73 82 87 120 124 where it was reported for both scar and unscarred skin measurements in four articles (5% of articles).17 24 57 73 The reported combined thickness (ie, epidermal and dermal) ICCs for inter-rater reliability of scarred skin ranged from 0.82 to 0.985, while the inter-rater ICC for the measurement of unscarred skin ranged from 0.33 to 0.98, with one of the four records reporting an ICC below the threshold value of 0.7 (ICC=0.33)24 and one record simply reported that the inter-rater ICC for scarred skin was ‘acceptable to high’.64 The reported intra-rater reliability for combined thickness measurements of scarred skin ranged from 0.89 to 0.983, and for unscarred skin ranged from 0.61 to 0.982, with one record reporting an ICC below the threshold of 0.7 (ICC=0.61).24 One record reported both the inter-rater and intra-rater ICCs for individual epidermal (inter-rater ICC=0.297; intra-rater ICC=0.809) and dermal (inter-rater ICC=0.991; intra-rater ICC=0.991) scar thickness measurement.87 Four articles (5% of articles) reporting reliability used Pearson’s R, an undisclosed method, or description (eg, high), as detailed in online supplemental table 2.22 54 105 137
Measurement error for inter-rater and intra-rater reliability of combined, epidermal or dermal thickness was reported in four articles (5% of articles) and one abstract using SEM. The inter-rater SEM for the combined epidermal and dermal thickness of scarred skin ranged from 0.11 to 0.5 mm, and the intra-rater SEMs ranged from 0.18 to 0.52 mm. Individual records reported SEM values for unscarred skin, and separate epidermal and dermal measurements, available in online supplemental table 5.17 23 24 82 87 Only one record reported calculation of the SDC. In that record, the inter-rater and intra-rater SDC was calculated for both scarred and unscarred skin. The scarred skin SDCs were 1.4 mm (inter-rater) and 0.6 mm (intra-rater), and unscarred skin SDCs were 0.8 mm (inter-rater) and 0.5 mm (intra-rater).24 The reported SEMs were all close to or below the largest SDC value reported. This finding may indicate that ultrasound can detect true variance in scar thickness above measurement error for traumatic scar and skin thickness.
Of the records that reported reliability and measurement error, measurements were taken by practitioners with varying clinical expertise and roles within the treating team. These included therapists, nurses, and doctors, sometimes under the supervision of trained radiologists. One record reported that 3 assessors received 3 hours of training, and conducted 10 assessments using the study protocol before the study began.57
Clinical, health service, implementation and feasibility outcomes
No record specifically investigated clinical, health service, implementation or feasibility outcomes of ultrasound as a measurement-based care initiative. Ultrasound was used to assess the clinical outcomes of scar treatment initiatives in all included records. Clinical, health service, implementation and feasibility outcomes related to ultrasound measurement were, however, reported in 53 journal articles17 22–24 26 27 31 46–48 50 51 54 56–61 63–66 69–75 77 80 82 113–116 119 120 122–124 128 129 138 142–144 148 149 155 and 14 abstracts28 86 87 89 90 95 96 102 105 107 109 110 152 153 that focused on scar treatments.
The clinical outcome of patient satisfaction related to ultrasound measurement was only reported in one journal article. While patient satisfaction was not directly measured in that record, a proxy measure of satisfaction was reported by the authors stating that no paediatric patient or their caregiver refused ultrasound measurement once the purpose was explained.24
Timeliness was the only reported health service outcome, reported as the time required to take ultrasound measurements. Where reported in three journal articles, this was short, taking between 1 and 5 minutes.24 27 122
The most common implementation outcomes reported in the identified records were fidelity, acceptability and appropriateness. Fidelity to the measurement method was reported through the use of experienced or trained assessors (n=6 journal articles; n=1 abstract),24 57 58 87 142 144 148 and/or using the same assessor/s for all measurement sessions (n=5 journal articles; 6% of included journal articles).24 61 138 144 148 Differences between intended and actual measurement methods were not discussed. The training and/or experience of the assessors was discussed in 24 records (23 journal articles and 1 abstract),17 23 24 27 51 56–59 63–66 71 73 115 116 120 123 124 138 144 149 153 where measurements were either taken by a clinician (n=13; 54% of records reporting training),17 23 24 58 59 64–67 71 120 124 141 members of the research team (n=6; 25% of records reporting training)57 63 73 115 123 144 or by specialist sonographers and/or radiologists (n=5, including 1 abstract; 21% of records reporting training).56 116 138 149 153 Only one record reported on fidelity in the context of routine clinical practice. In this instance, ultrasound was conducted in the Department of Radiology, however the role or training of the staff was not reported.119
The acceptability and appropriateness of the ultrasound methods used in individual records were generally based on author’s opinion and outlined in the discussion. Acceptability was reported in 26 records (23 journal articles and 3 abstracts),17 22–24 26–28 31 57 64 70 74 75 77 80 82 86 96 116 119 120 122 124 143 149 155 including for paediatric populations, where one record reported potential difficulty in measuring this population,22 contrasting that which reported that measurement was acceptable to both children and their caregivers.24 One record reported acceptability where the intervention being analysed by ultrasound was already part of routine clinical practice. In this instance, the authors referenced additional publications which stated that ultrasound had an accuracy of 0.5 mm, which was judged by the authors to be sufficient for assessment of scar thickness.24 27 119 122 Potential difficulty was identified in the measurement of open wounds,24 and traditionally hard-to-reach areas (such as the axillae or groin).22
The appropriateness of the ultrasound methods was reported in 35 journal articles (43% of included journal articles)22 24 26 27 31 46–48 50 54 57 60 61 64–66 69 72–75 77 80 82 113 114 116 119 120 122 124 128 148 149 155 and 11 abstracts (31% of included abstracts),86 87 89 90 95 102 105 107 109 110 152 where it was generally addressed in the discussion. Of these records, two (4% of records reporting appropriateness) determined that ultrasound was not appropriate for scar measurement. The first stated that it was too inaccurate and complex86; and the second, which reported on initiatives within routine clinical practice, determined that the minimum resolution of the Diasonography ultrasonic scanner (Nuclear Enterprises, Edinburgh, UK) precluded its use in scars thinner than 3 mm.113
The feasibility of ultrasound was reported in 12 journal articles (15% of included journal articles).22 24 26 46 57 70 80 119 120 124 129 Five records considered ultrasound not feasible for scar measurements. The rationale presented included high-frequency 20 MHz ultrasound having an inadequate penetration depth26 57; and ultrasound measurement and training of investigators requiring too much time (as reported in one record in phase IV of the research-to-practice pipeline).22 119 120 Another factor identified as precluding feasibility was the inability to consistently relocate the measurement site.24 Conversely, one record reported ultrasound to be feasible in combination with VSS measurement,70 and another stated that ultrasound was able to distinguish between subcutaneous fat and muscle, which was interpreted by the authors of that record to mean that skin thickness measurements were accurate.129 The majority (n=11; 92%) of the records reporting feasibility were research initiatives in phase II or phase III of the research to practice pipeline. One record examined feasibility in the context of routine clinical practice (ie, phase IV; figure 1),119 where it was determined that ultrasound was not suitable for use in their 12-year longitudinal study due to changes in staff, equipment and software over such a long time period, which introduced additional variables to the measurement process that were impossible to control.119
Factors influencing ultrasound images and measurement methods
The only factor that was reported to influence the imaging and measurement methods was the measurement of scars with open wounds. This was reported in one record, which determined that ultrasound and ultrasound gel was unsuitable in this instance. The authors of that record suggested the use of a flexible transparent plastic wrap, which is placed over the measurement area prior to measurement with ultrasound.24
Reported strengths and limitations of the measurement methods
The safety, practicality, objectivity, versatility, reliability and non-invasive nature of ultrasound were all reported as strengths of the measurement method.22 27–29 47 50 57 61 64 77 78 80 82 87 89 95 96 105 107 109 119 123 124 129 139 148 When compared with other subjective (eg, VSS) or clinical (eg, 3D camera) measurement methods, ultrasound was viewed as the superior measurement method of scar and skin thickness, due to its improved accuracy, greater sensitivity to change and objectivity.24 64 73 116 120 The ability of ultrasound to differentiate between scarred and unscarred skin was also highlighted (n=4; 3%),47 60 72 122 as was the versatility of ultrasound in its ability to measure a variety of anatomical areas and be used with child participants (ie, <18 years) (n=2; 2%).22 149
The poor correlation between ultrasound and histological thickness measurements,86 and the established inverse relationship between ultrasound penetration depth and the resolution of superficial structures were identified as limitations of ultrasound in the measurement of scar thickness.26 27 77 80 89 113 149 This may be an evidence gap worth exploring in more depth. One record, reporting on a longitudinal study that was conducted over 12 years, reported that the continuous development of ultrasound software and hardware over that time limited the usefulness of ultrasound.119 Despite being reported elsewhere as acceptable (ie, between 1 and 5 min24 27 122), one record reported that the time-consuming nature of measurement and the requirement for assessors to be trained in the operation of, and techniques required for, ultrasonography was a limitation of the method.120 Methodologically, concerns were raised around the pressure caused by application of the ultrasound transducer to the skin, and how that may influence thickness measurement.61 62 123 124 The size of the transducer head relative to the size of scars was also considered a potential limitation, as multiple measurements are required for quantification of larger scars.57 Finally, it was recognised that there may be a difference between changes to the scar that can be measured by ultrasound, and what is felt and/or experienced by the patient.75 80 126 127 It was suggested that changes that are detectable by ultrasound may be smaller than those able to be detected by patients. In patients with burn scars, a minimum change in scar thickness of between 1 and 6 mm measured by ultrasound, has been reported to be required before a patient may report noticing any difference to their scar thickness.24 75 While further research is required to allow generalisation of these findings to other scar aetiologies, this indicates that a holistic approach to scar thickness using the patient’s opinion as well as objective measurement through ultrasound may be beneficial.
Guidelines or frameworks used to guide the measurement methods
No records reported using any guidelines or frameworks to inform their measurement methods. One record used suggestions from The American Wound Healing Society to support the measurement of contralateral, unscarred skin thickness on the same individual as a control or comparator.75
Methodological considerations
Based on the ultrasound methods and outcomes identified in this review, a list of methodological considerations have been compiled (online supplemental table 6). These are intended to guide the decision-making and methodological reporting of researchers and/or clinicians undertaking scar or skin thickness ultrasound measurement.
Discussion
This review mapped the methods used in the published literature to measure traumatic scar thickness using ultrasound across the research-to-practice translational pipeline. No record reported their methods with sufficient detail to allow them to be independently replicated. Overall, there was a lack of consistent rationale underpinning which skin layers (ie, epidermis, dermis and combined) were measured, and little consideration was given to the training and experience required by assessors. The included records mainly aligned with the second and third phases of the research-to-practice pipeline (figure 1), with only three records (two articles and one abstract) reporting the use of ultrasound in routine clinical practice (phase IV).92 113 119 The paucity of records aligning with phase IV studies (use in clinical practice) suggests a translational gap from research to regular clinical practice. There are two likely explanations for this: (1) that ultrasound is most commonly used as an outcome measure for research initiatives and is not regularly used to evaluate care once treatments are implemented into routine clinical practice or (2) that use of ultrasound in routine clinical practice is not reported or evaluated, as routine clinical practice is rarely published.
Searching of grey literature was conducted in an attempt to identify clinical practice documents, however none were located. Surveys of health service departments may be the best method of identifying ultrasound methods used in regular clinical practice as part of future research. While some records reported using additional subjective and objective measurement methods in addition to ultrasound, none used these methods to determine the criterion validity of the ultrasound for scar thickness measurement. This is another evidence gap that should be addressed.
While efforts have been made to standardise ultrasound measurement procedures elsewhere in dermatology (including tumours, cancers, vascular anomalies and systemic sclerosis34 35), this same effort has not yet extended to the measurement of traumatic scarring. Methodological standardisation has the potential to increase confidence in the use of ultrasound as the basis of measurement-based care initiatives for clinical decision-making, allowing patient care and scar treatments to be tailored towards individual needs.62 147 156 Standardising the core methodological components of ultrasound measurement of scar thickness, or at the very least, creating a standardised framework for methodological decision-making, may support implementation of ultrasound measurement into routine clinical practice, supported by strategies to overcome barriers to implementation at local sites.157
This review identified novel insights into the identification of the composition of cutaneous scars using ultrasound, and highlighted the apparent lack of consistent understanding of, or rationale behind, what scar thickness characteristics were being measured. Fibrosis is generally understood to be the primary cause of scar thickness through the deposition of excessive extracellular matrix proteins such as collagen.158 159 This has been confirmed through histological analysis, which has shown the presence of excess collagen and other extracellular matrix proteins in the dermis of hypertrophic scars.160 161 An additional method for assessing the effects of scarring on the dermis, as identified by one record in this review,47 is through quantification of the presence and density of hair follicles. This quantification may serve as a method of differentiation between scarred and physiological skin, and may also serve as a measure of skin function.47 What is less understood, and perhaps largely overlooked, is the function of the epidermis in scar thickness. In the one record identified in this review that directly reports the measurement of the epidermis, the authors noted that the measurement quantified the presence of oedema.55 This was further supported by two records that noted that the epidermis and dermis responded differently to treatment,67 71 indicating that there is likely a difference in the composition of the scar between these skin layers. Cutaneous oedema has been observed using high-frequency ultrasound in other pathologies, including atopic dermatitis and skin ageing, where it is characterised by the presence of a subepidermal low echogenic band, a hyperechoic band at the dermoepidermal junction.162 Understanding the interplay between epidermal oedema, dermal fibrosis and the presence and density of hair follicles may result in an increased understanding of the mechanisms and treatment responses of cutaneous scarring. With better understanding, more targeted scar treatments that inform a greater understanding of scar responsivity may arise.
Another important, but potential limiting factor for the use of ultrasound to measure scar thickness raised in this review is the training and/or experience required of assessors, and the ramifications this likely has on the reliability of measurements and interpretation.163 This review identified 24 records where assessor experience was discussed, however none made any recommendations on the optimal training and/or experience. Identifying the training requirements of assessors may prove an important step towards more widespread implementation of reliable ultrasound scar thickness measurement in research trials and as the basis for measurement-based care in routine clinical practice.164 A panel of dermatological and ultrasound experts has previously recommended that a physician with a minimum of 300 examinations per year should hold responsibility for ultrasound measurements.34 It has also been suggested that training existing members of clinical teams and standardising measurement method/s may be the most effective way to achieve minimum reliability standards under clinical conditions. This could allow measurement to be reliably conducted within an outpatient clinic setting by a number of healthcare providers, assisting workflow by negating the requirement for patients to wait for an experienced radiographer.24 164 In the current review, reliability estimates were generally acceptable but were tested under research conditions. The diverse experience and expertise of assessors, where reported for the reliability estimates, means that the acceptable reliability results should be generalisable to most clinical teams, as therapists, doctors and nurses were all included. The cumulative sample size of all reliability studies also supports this generalisation; however, each team should perform their own reliability estimates before conducting ultrasound thickness measurements.
Study limitations
Only articles available in English or with an English abstract were considered for inclusion and data extraction, which may have resulted in the omission of eligible information. Data extraction was completed on the English abstracts of two non-English articles that were available electronically, however the non-English articles themselves were not available to the authors, and thus could not be analysed. Based on the number of records included in this review, however, it is unlikely that this would have impacted the review findings. It is acknowledged that methods reported in included abstracts may not be fully reproducible, due to their brevity. Thus, findings were reported separately to articles. An additional limitation was that authors of included records were not contacted to provide clarification or further information, as this was not feasible given the number of results identified. It should also be acknowledged that the included records were not designed to align with the specific aims of this review, which likely explains some of the lack of reporting on outcomes of interest in our review, particularly clinical, health service and implementation outcomes. Furthermore, as this review relied on published information (including grey literature), routine practices employed within organisations may not have been considered and unpublished industry sponsored reports may not have been identified.
It is also important to consider the limitations of ultrasound itself for the holistic quantification of cutaneous scarring. Ultrasound transducers are generally small, meaning that it is difficult to assess the entirety of a scar, necessitating multiple measurements.165 Additionally, thickness is often not the only scar parameter of clinical or research interest. It has therefore been recommended that multimodal measurement techniques are employed, which include both subjective and objective measurements.166 167 However, use of these methods may be challenging in routine clinical practice, due to the length of time and training required. Thus, feasibility and implementation outcomes are of importance in evaluating measurement-based care initiatives involving ultrasound alone or multimodal measurement tools in scar care practice—a field in its infancy based on this review.
Future directions
It is intended that the results of this review will be used to inform the creation of a Delphi consensus study, leading to the formation of a guideline for the measurement of traumatic scar thickness using ultrasound. This guideline can then be used by researchers and clinicians to standardise the measurement of scars. In preparation for this study, we have provided a list of methodological considerations for assessors or practitioners when planning to conduct scar thickness measurements with ultrasound (online supplemental table 6). Future research could also investigate aspects that were beyond the scope of this review including factors influencing the implementation of ultrasound-based care initiatives, strategies to support implementation and how research-based initiatives could be applied in practice. Further studies are needed that compare SDCs with SEMs to interpret reliability estimates to confirm our interpretation that ultrasound may have the ability to detect true change or variance in scar thickness above measurement error, which was based on the SDC reported by a single study. Our interpretation is supported by mostly acceptable reliability estimates of ultrasound thickness for other cutaneous conditions.168 169 Additional investigations should also be conducted to determine the criterion validity of ultrasound as a measure for scar thickness.
Supplementary Material
Acknowledgments
The authors would like to thank David Honeyman, Faculty of Medicine librarian at The University of Queensland for his assistance in the development of the search strategy, and execution of the database searches for this review.
Footnotes
@BrandonMeikle5, @tyack_z
Contributors: BM and ZT conceived the project after identifying this area as a knowledge gap in existing literature. BM developed the research questions and study methodology, conducted the literature search, screened all articles and extracted data. Record screening and data extraction was completed by BM, MS, TM and TR, with additional extraction completed by BD to assess consistency. MS, TM, TR and RMK provided advice to BM on the clinical implications of ultrasound measurement. MS, RMK and ZT contributed to the supervision of BM as a PhD student. BM drafted the paper, and ZT and MS provided critical appraisal of the drafted manuscript, with further advice provided by TM, TR, BD and RMK. BM acts as guarantor for all work conducted and reported in this manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1. Jagdeo J, Shumaker PR. Traumatic scarring. JAMA Dermatol 2017;153:364. 10.1001/jamadermatol.2016.5232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lawrence JW, Mason ST, Schomer K, et al. Epidemiology and impact of scarring after burn injury: a systematic review of the literature. J Burn Care Res 2012;33:136–46. 10.1097/BCR.0b013e3182374452 [DOI] [PubMed] [Google Scholar]
- 3. Bayat A, McGrouther DA, Ferguson MWJ. Skin scarring. BMJ 2003;326:88–92. 10.1136/bmj.326.7380.88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lee HJ, Jang YJ. Recent understandings of biology, prophylaxis and treatment strategies for hypertrophic scars and keloids. Int J Mol Sci 2018;19:711. 10.3390/ijms19030711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rabello FB, Souza CD, Farina Júnior JA. Update on hypertrophic scar treatment. Clinics (Sao Paulo) 2014;69:565–73. 10.6061/clinics/2014(08)11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. English RS, Shenefelt PD. Keloids and hypertrophic scars. Dermatol Surg 1999;25:631–8. 10.1046/j.1524-4725.1999.98257.x [DOI] [PubMed] [Google Scholar]
- 7. Niessen FB, Spauwen PH, Schalkwijk J, et al. On the nature of hypertrophic scars and keloids: a review. Plast Reconstr Surg 1999;104:1435–58. 10.1097/00006534-199910000-00031 [DOI] [PubMed] [Google Scholar]
- 8. Simons M, Price N, Kimble R, et al. Patient experiences of burn scars in adults and children and development of a health-related quality of life conceptual model: a qualitative study. Burns 2016;42:620–32. 10.1016/j.burns.2015.11.012 [DOI] [PubMed] [Google Scholar]
- 9. Tyack Z, Ziviani J, Kimble R, et al. Measuring the impact of burn scarring on health-related quality of life: development and preliminary content validation of the brisbane burn scar impact profile (BBSIP) for children and adults. Burns 2015;41:1405–19. 10.1016/j.burns.2015.05.021 [DOI] [PubMed] [Google Scholar]
- 10. Sullivan T, Smith J, Kermode J, et al. Rating the burn scar. J Burn Care Rehabil 1990;11:256–60. 10.1097/00004630-199005000-00014 [DOI] [PubMed] [Google Scholar]
- 11. Draaijers LJ, Tempelman FRH, Botman YAM, et al. The patient and observer scar assessment scale: a reliable and feasible tool for scar evaluation. Plast Reconstr Surg 2004;113:1960–5. 10.1097/01.prs.0000122207.28773.56 [DOI] [PubMed] [Google Scholar]
- 12. Tyack Z, Wasiak J, Spinks A, et al. A guide to choosing a burn scar rating scale for clinical or research use. Burns 2013;39:1341–50. 10.1016/j.burns.2013.04.021 [DOI] [PubMed] [Google Scholar]
- 13. Gold HM, McGuire AM, Mustoe AT, et al. Updated International clinical recommendations on scar management: part 2 - Algorithms for scar prevention and treatment. Dermatol Surg 2014;40:825–31. 10.1111/dsu.0000000000000050 [DOI] [PubMed] [Google Scholar]
- 14. Jones LL, Calvert M, Moiemen N, et al. Outcomes important to burns patients during scar management and how they compare to the concepts captured in burn-specific patient reported outcome measures. Burns 2017;43:1682–92. 10.1016/j.burns.2017.09.004 [DOI] [PubMed] [Google Scholar]
- 15. McGarry S, Elliott C, McDonald A, et al. Paediatric burns: from the voice of the child. Burns 2014;40:606–15. 10.1016/j.burns.2013.08.031 [DOI] [PubMed] [Google Scholar]
- 16. Bloemen MCT, van der Veer WM, Ulrich MMW, et al. Prevention and curative management of hypertrophic scar formation. Burns 2009;35:463–75. 10.1016/j.burns.2008.07.016 [DOI] [PubMed] [Google Scholar]
- 17. Lee KC, Bamford A, Gardiner F, et al. Investigating the Intra- and inter-rater reliability of a panel of subjective and objective burn scar measurement tools. Burns 2019;45:1311–24. 10.1016/j.burns.2019.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Brusselaers N, Pirayesh A, Hoeksema H, et al. Burn scar assessment: a systematic review of different scar scales. J Surg Res 2010;164:e115–23. 10.1016/j.jss.2010.05.056 [DOI] [PubMed] [Google Scholar]
- 19. Brusselaers N, Pirayesh A, Hoeksema H, et al. Burn scar assessment: a systematic review of objective scar assessment tools. Burns 2010;36:1157–64. 10.1016/j.burns.2010.03.016 [DOI] [PubMed] [Google Scholar]
- 20. Hambleton J, Shakespeare PG, Pratt BJ. The progress of hypertrophic scars monitored by ultrasound measurements of thickness. Burns 1992;18:301–7. 10.1016/0305-4179(92)90151-j [DOI] [PubMed] [Google Scholar]
- 21. van Sonsbeek MAMS, Hutschemaekers GJM, Veerman JW, et al. The results of clinician-focused implementation strategies on uptake and outcomes of measurement-based care (MBC) in general mental health care. BMC Health Serv Res 2023;23. 10.1186/s12913-023-09343-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gee Kee EL, Kimble RM, Cuttle L, et al. Scar outcome of children with partial thickness burns: a 3 and 6 month follow up. Burns 2016;42:97–103. 10.1016/j.burns.2015.06.019 [DOI] [PubMed] [Google Scholar]
- 23. Wang X-Q, Mill J, Kravchuk O, et al. Ultrasound assessed thickness of burn scars in association with laser doppler imaging determined depth of burns in paediatric patients. Burns 2010;36:1254–62. 10.1016/j.burns.2010.05.018 [DOI] [PubMed] [Google Scholar]
- 24. Simons M, Kee EG, Kimble R, et al. Ultrasound is a reproducible and valid tool for measuring scar height in children with burn scars: a cross-sectional study of the psychometric properties and utility of the ultrasound and 3D camera. Burns 2017;43:993–1001. 10.1016/j.burns.2017.01.034 [DOI] [PubMed] [Google Scholar]
- 25. Izzetti R, Vitali S, Aringhieri G, et al. Ultra-high frequency ultrasound, a promising diagnostic technique: review of the literature and single-center experience. Can Assoc Radiol J 2021;72:418–31. 10.1177/0846537120940684 [DOI] [PubMed] [Google Scholar]
- 26. Agabalyan NA, Su S, Sinha S, et al. Comparison between high-frequency ultrasonography and histological assessment reveals weak correlation for measurements of scar tissue thickness. Burns 2017;43:531–8. 10.1016/j.burns.2016.09.008 [DOI] [PubMed] [Google Scholar]
- 27. Kim JD, Oh SJ, Kim SG, et al. Ultrasonographic findings of re-epithelialized skin after partial-thickness burns. Burns Trauma 2018;6:21. 10.1186/s41038-018-0122-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Blome-Eberwein S, Gogal C, Folz C. Assessment of hair density and sub-epidermal tissue in burn scars using high frequency ultrasound. J Burn Care Res 2012;33:S105. 10.1097/BCR.0b013e3182331e09 [DOI] [PubMed] [Google Scholar]
- 29. Ud-Din S, Foden P, Stocking K, et al. Objective assessment of dermal fibrosis in cutaneous scarring, using optical coherence tomography, high‐frequency ultrasound and immunohistomorphometry of human skin. Br J Dermatol 2019;181:722–32. 10.1111/bjd.17739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Du Y-C, Lin C-M, Chen Y-F, et al. Implementation of a burn scar assessment system by ultrasound techniques. Conf Proc IEEE Eng Med Biol Soc 2006;2006:2328–31. 10.1109/IEMBS.2006.260018 [DOI] [PubMed] [Google Scholar]
- 31. Elrefaie AM, Salem RM, Faheem MH. High-resolution ultrasound for keloids and hypertrophic scar assessment. Lasers Med Sci 2020;35:379–85. 10.1007/s10103-019-02830-4 [DOI] [PubMed] [Google Scholar]
- 32. Jasaitiene D, Valiukeviciene S, Linkeviciute G, et al. Principles of high‐frequency ultrasonography for investigation of skin pathology. J Eur Acad Dermatol Venereol 2011;25:375–82. 10.1111/j.1468-3083.2010.03837.x [DOI] [PubMed] [Google Scholar]
- 33. Rodríguez Bandera AI, Sebaratnam DF, Feito Rodríguez M, et al. Cutaneous ultrasound and its utility in pediatric dermatology. part I: lumps, bumps, and inflammatory conditions. Pediatric Dermatology 2020;37:29–39. 10.1111/pde.14033 [DOI] [PubMed] [Google Scholar]
- 34. Wortsman X, Alfageme F, Roustan G, et al. Guidelines for performing dermatologic ultrasound examinations by the DERMUS group. J Ultrasound Med 2016;35:577–80. 10.7863/ultra.15.06046 [DOI] [PubMed] [Google Scholar]
- 35. Vanhaecke A, Cutolo M, Heeman L, et al. High frequency ultrasonography: reliable tool to measure skin fibrosis in SSC? A systematic literature review and additional pilot study. Rheumatology (Oxford) 2021;61:42–52. 10.1093/rheumatology/keab462 [DOI] [PubMed] [Google Scholar]
- 36. Australian Government Department of Health and Aged Care Medical Research Future Fund . Research translation Australia. 2022. Available: https://www.health.gov.au/our-work/medical-research-future-fund/mrff-research-themes/research-translation#what-is-the-research-pipeline
- 37. Meikle B, Kimble RM, Tyack Z. Ultrasound measurements of pathological and physiological skin thickness: a scoping review protocol. BMJ Open 2022;12:e056720. 10.1136/bmjopen-2021-056720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 39. Haddaway NR, Collins AM, Coughlin D, et al. The role of google scholar in evidence reviews and its applicability to grey literature searching. PLoS One 2015;10:e0138237. 10.1371/journal.pone.0138237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Pieper D, Puljak L. Language restrictions in systematic reviews should not be imposed in the search strategy but in the eligibility criteria if necessary. J Clin Epidemiol 2021;132:146–7. 10.1016/j.jclinepi.2020.12.027 [DOI] [PubMed] [Google Scholar]
- 41. Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research Agenda. Adm Policy Ment Health 2011;38:65–76. 10.1007/s10488-010-0319-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Prinsen CAC, Vohra S, Rose MR, et al. “How to select outcome measurement instruments for outcomes included in a "Core Outcome Set" - a practical guideline. Trials 2016;17:449. 10.1186/s13063-016-1555-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Mokkink LB, Boers M, van der Vleuten CPM, et al. COSMIN risk of bias tool to assess the quality of studies on reliability or measurement error of outcome measurement instruments: a delphi study. BMC Med Res Methodol 2020;20:293. 10.1186/s12874-020-01179-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Terwee CB, Bot SDM, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007;60:34–42. 10.1016/j.jclinepi.2006.03.012 [DOI] [PubMed] [Google Scholar]
- 45. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Blome-Eberwein S, Gogal C, Weiss MJ, et al. Prospective evaluation of fractional CO2 laser treatment of mature burn scars. J Burn Care Res 2016;37:379–87. 10.1097/BCR.0000000000000383 [DOI] [PubMed] [Google Scholar]
- 47. Blome-Eberwein SA, Roarabaugh C, Gogal C. Assessment of hair density and sub-epidermal tissue thickness in burn scars using high-definition ultrasound imaging. J Burn Care Res 2020;41:421–6. 10.1093/jbcr/irz191 [DOI] [PubMed] [Google Scholar]
- 48. Cai L, Hu M, Lin L, et al. Evaluation of the efficacy of triamcinolone acetonide in the treatment of keloids by high‐frequency ultrasound. Skin Res Technol 2020;26:489–93. 10.1111/srt.12820 [DOI] [PubMed] [Google Scholar]
- 49. Candy LHY, Cecilia L-T, Ping ZY. Effect of different pressure magnitudes on hypertrophic scar in a Chinese population. Burns 2010;36:1234–41. 10.1016/j.burns.2010.05.008 [DOI] [PubMed] [Google Scholar]
- 50. Chae JK, Kim JH, Kim EJ, et al. Values of a patient and observer scar assessment scale to evaluate the facial skin graft scar. Ann Dermatol 2016;28:615–23. 10.5021/ad.2016.28.5.615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Deng H, Li-Tsang CWP, Li J. Measuring vascularity of hypertrophic scars by dermoscopy: construct validity and predictive ability of scar thickness change. Skin Res Technol 2020;26:369–75. 10.1111/srt.12812 [DOI] [PubMed] [Google Scholar]
- 52. Deng K, Xiao H, Liu X, et al. Strontium-90 brachytherapy following Intralesional triamcinolone and 5-fluorouracil injections for keloid treatment: a randomized controlled trial. PLoS One 2021;16:e0248799. 10.1371/journal.pone.0248799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Deng H, Tan T, Luo G, et al. Vascularity and thickness changes in immature hypertrophic scars treated with a pulsed dye laser. Lasers Surg Med 2021;53:914–21. 10.1002/lsm.23366 [DOI] [PubMed] [Google Scholar]
- 54. Dunkin CSJ, Pleat JM, Gillespie PH, et al. Scarring occurs at a critical depth of skin injury: precise measurement in a graduated dermal scratch in human volunteers. Plast Reconstr Surg 2007;119:1722–32. 10.1097/01.prs.0000258829.07399.f0 [DOI] [PubMed] [Google Scholar]
- 55. Fabbrocini G, Marasca C, Ammad S, et al. Assessment of the combined efficacy of needling and the use of silicone gel in the treatment of C-section and other surgical hypertrophic scars and keloids. Adv Skin Wound Care 2016;29:408–11. 10.1097/01.ASW.0000490028.37994.14 [DOI] [PubMed] [Google Scholar]
- 56. Fraccalvieri M, Zingarelli E, Ruka E, et al. Negative pressure wound therapy using gauze and foam: histological, immunohistochemical and ultrasonography morphological analysis of the granulation tissue and scar tissue. Int Wound J 2011;8:355–64. 10.1111/j.1742-481X.2011.00798.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Gankande TU, Duke JM, Danielsen PL, et al. Reliability of scar assessments performed with an integrated skin testing device – the DermaLab combo. Burns 2014;40:1521–9. 10.1016/j.burns.2014.01.025 [DOI] [PubMed] [Google Scholar]
- 58. Huang PW, Lu CW, Liang Liu H. Fitted pressure garment of assessment of scar thickness on third-degree burns through ultrasonic measurement. J Cytol Histol 2017;08. 10.4172/2157-7099.1000488 [DOI] [Google Scholar]
- 59. Huang P-W, Lu C-W, Chu K-T, et al. Assessing thickness of burn scars through ultrasound measurement for patients with arm burns. J Med Biol Eng 2021;41:84–91. 10.1007/s40846-020-00592-x [DOI] [Google Scholar]
- 60. Huang S-Y, Xiang X, Guo R-Q, et al. Quantitative assessment of treatment efficacy in keloids using high-frequency ultrasound and shear wave elastography: a preliminary study. Sci Rep 2020;10:1375. 10.1038/s41598-020-58209-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Issler-Fisher AC, Fisher OM, Haertsch PA, et al. Effectiveness and safety of Ablative fractional CO2 laser for the treatment of burn scars: a case-control study. Burns 2021;47:785–95. 10.1016/j.burns.2020.10.002 [DOI] [PubMed] [Google Scholar]
- 62. Issler-Fisher AC, Fisher OM, Haertsch P, et al. Ablative fractional resurfacing with laser‐facilitated steroid delivery for burn scar management: does the depth of laser penetration matter? Lasers Surg Med 2020;52:149–58. 10.1002/lsm.23166 [DOI] [PubMed] [Google Scholar]
- 63. Joo SY, Lee SY, Cho YS, et al. Clinical utility of extracorporeal shock wave therapy on hypertrophic scars of the hand caused by burn injury: a prospective, randomized, double-blinded study. J Clin Med 2020;9:1376. 10.3390/jcm9051376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Lee KC, Bamford A, Gardiner F, et al. Burns objective scar scale (BOSS): validation of an objective measurement devices based burn scar scale panel. Burns 2020;46:110–20. 10.1016/j.burns.2019.05.008 [DOI] [PubMed] [Google Scholar]
- 65. Li JQ, Li-Tsang CWP, Huang YP, et al. Detection of changes of scar thickness under mechanical loading using ultrasonic measurement. Burns 2013;39:89–97. 10.1016/j.burns.2012.05.009 [DOI] [PubMed] [Google Scholar]
- 66. Li P, Li-Tsang CWP, Deng X, et al. The recovery of post-burn hypertrophic scar in a monitored pressure therapy intervention programme and the timing of intervention. Burns 2018;44:1451–67. 10.1016/j.burns.2018.01.008 [DOI] [PubMed] [Google Scholar]
- 67. Li N, Yang L, Cheng J, et al. Early intervention by Z-plasty combined with fractional CO2 laser therapy as a potential treatment for hypertrophic burn scars. J Plast Reconstr Aesthet Surg 2021;74:3087–93. 10.1016/j.bjps.2021.03.079 [DOI] [PubMed] [Google Scholar]
- 68. Li-Tsang CWP, Lau JCM, Chan CCH. Prevalence of hypertrophic scar formation and its characteristics among the Chinese population. Burns 2005;31:610–6. 10.1016/j.burns.2005.01.022 [DOI] [PubMed] [Google Scholar]
- 69. Li-Tsang CWP, Lau JCM, Choi J, et al. A prospective randomized clinical trial to investigate the effect of silicone GEL sheeting (cica-care) on post-traumatic hypertrophic scar among the Chinese population. Burns 2006;32:678–83. 10.1016/j.burns.2006.01.016 [DOI] [PubMed] [Google Scholar]
- 70. Mamdouh M, Omar GA, Hafiz HSA, et al. Role of vitamin D in treatment of keloid. J Cosmet Dermatol 2022;21:331–6. 10.1111/jocd.14070 [DOI] [PubMed] [Google Scholar]
- 71. Meirte J, Moortgat P, Anthonissen M, et al. Short-term effects of vacuum massage on epidermal and dermal thickness and density in burn scars: an experimental study. Burns Trauma 2016;4:27. 10.1186/s41038-016-0052-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Nedelec B, Correa JA, de Oliveira A, et al. Longitudinal burn scar quantification. Burns 2014;40:1504–12. 10.1016/j.burns.2014.03.002 [DOI] [PubMed] [Google Scholar]
- 73. Nedelec B, Correa JA, Rachelska G, et al. Quantitative measurement of hypertrophic scar: interrater reliability and concurrent validity. J Burn Care Res 2008;29:501–11. 10.1097/BCR.0b013e3181710881 [DOI] [PubMed] [Google Scholar]
- 74. Nedelec B, Couture M-A, Calva V, et al. Randomized controlled trial of the immediate and long-term effect of massage on adult postburn scar. Burns 2019;45:128–39. 10.1016/j.burns.2018.08.018 [DOI] [PubMed] [Google Scholar]
- 75. Nedelec B, LaSalle L, de Oliveira A, et al. Within-patient, single-blinded, randomized controlled clinical trial to evaluate the efficacy of triamcinolone acetonide injections for the treatment of hypertrophic scar in adult burn survivors. J Burn Care Res 2020;41:761–9. 10.1093/jbcr/iraa057 [DOI] [PubMed] [Google Scholar]
- 76. Reinholz M, Guertler A, Schwaiger H, et al. Treatment of keloids using 5‐fluorouracil in combination with crystalline triamcinolone acetonide suspension: evaluating therapeutic effects by using non‐invasive objective measures. J Eur Acad Dermatol Venereol 2020;34:2436–44. 10.1111/jdv.16354 [DOI] [PubMed] [Google Scholar]
- 77. Reinholz M, Schwaiger H, Poetschke J, et al. Objective and subjective treatment evaluation of scars using optical coherence tomography, sonography, photography, and standardised questionnaires. Eur J Dermatol 2017;26:599–608. 10.1684/ejd.2016.2873 [DOI] [PubMed] [Google Scholar]
- 78. Schwaiger H, Reinholz M, Poetschke J, et al. Evaluating the therapeutic success of keloids treated with cryotherapy and intralesional corticosteroids using noninvasive objective measures. Dermatol Surg 2018;44:635–44. 10.1097/DSS.0000000000001427 [DOI] [PubMed] [Google Scholar]
- 79. Soykan EA, Butzelaar L, de Kroon TL, et al. Minimal extracorporeal circulation (MECC) does not result in less hypertrophic scar formation as compared to conventional extracorporeal circulation (CECC) with dexamethasone. Perfusion 2014;29:249–59. 10.1177/0267659113511656 [DOI] [PubMed] [Google Scholar]
- 80. Timar-Banu O, Beauregard H, Tousignant J, et al. Development of noninvasive and quantitative methodologies for the assessment of chronic ulcers and scars in humans. Wound Repair Regen 2001;9:123–32. 10.1046/j.1524-475x.2001.00123.x [DOI] [PubMed] [Google Scholar]
- 81. Van den Kerckhove E, Stappaerts K, Fieuws S, et al. The assessment of erythema and thickness on burn related scars during pressure garment therapy as a preventive measure for hypertrophic scarring. Burns 2005;31:696–702. 10.1016/j.burns.2005.04.014 [DOI] [PubMed] [Google Scholar]
- 82. Van den Kerckhove E, Staes F, Flour M, et al. Reproducibility of repeated measurements on post-burn scars with dermascan C. Skin Res Technol 2003;9:81–4. 10.1034/j.1600-0846.2003.00375.x [DOI] [PubMed] [Google Scholar]
- 83. van der Veer WM, Ferreira JA, de Jong EH, et al. Perioperative conditions affect long-term hypertrophic scar formation. Ann Plast Surg 2010;65:321–5. 10.1097/SAP.0b013e3181c60f88 [DOI] [PubMed] [Google Scholar]
- 84. Wang G-Q, Xia Z-F. Transplantation of epidermis of scar tissue on acellular dermal matrix. Burns 2009;35:352–5. 10.1016/j.burns.2008.06.021 [DOI] [PubMed] [Google Scholar]
- 85. Lee SY, Cho YS, Kim L, et al. The intra-rater reliability and validity of ultrasonography in the evaluation of hypertrophic scars caused by burns. Burns 2023;49:344–52. 10.1016/j.burns.2022.03.016 [DOI] [PubMed] [Google Scholar]
- 86. Agabalyan NA, Su S, Sinha V, et al. Evaluating high frequency ultrasonography for the non-invasive measurement of human scarring. J Burn Care Res 2016;37. 10.1097/01.bcr.0000483036.52429.db [DOI] [Google Scholar]
- 87. Anthonissen M, Meirte J, Moortgat P, et al. Intrarater and interrater reliability of an open 22MHz ultrasound scanning system to assess thickness and density of burn scars. Ann Burns Fire Disasters 2015;28. [Google Scholar]
- 88. Bajouri A, Kajoor AS, Fallah N, et al. Autologous human stromal vascular fraction injection in post-burn hypertrophic scar: a double-blinded placebo-controlled clinical trial. Bioimpacts 2018;8:37–8. 10.15171/bi.2018.S1 [DOI] [Google Scholar]
- 89. Bezugly A. Noninvasive skin pathology evaluation: high-frequency ultrasound imaging and diagnostics. J Dermatol Nurses Assoc 2020;12. [Google Scholar]
- 90. Bezugly A, Potekaev N. In vivo skin morphology monitoring of patients with acne, scars and dermal fillers, with 22 and 75 mhz high frequency ultrasound. J Dermatol 2014;41:4. 10.1111/1346-8138.12685 [DOI] [Google Scholar]
- 91. Blome-Eberwein S, Pagella P, Boorse D, et al. Treatment of hypertrophic burn scars with different laser modalities. Lasers Surg Med 2014;46:6–7. 10.1002/lsm.22229 [DOI] [Google Scholar]
- 92. Cho J, Choi J, Hur J, et al. The effect of Co2 fractional laser (Pixel®) on hypertrophic burn scars. J Burn Care Res 2012;33:S132. 10.1097/BCR.0b013e3182508c98 [DOI] [Google Scholar]
- 93. Cooper LE, Bohan PK, Hatem VD, et al. Analysis of the utility of CO2 and pulse-dye lasers in the treatment of hypertrophic burn scars. J Burn Care Res 2021;42:S28–9. 10.1093/jbcr/irab032.041 [DOI] [Google Scholar]
- 94. Edger-Lacoursière Z, Marois-Pagé E, de Oliveira A, et al. Objective quantification of hypertrophic scar and donor scar between 2 to 7 months post-burn injury. J Burn Care Res 2022;43:S103. 10.1093/jbcr/irac012.165 [DOI] [Google Scholar]
- 95. El-Zawahry MBM, Abdel El-Hameed El-Cheweikh HM, Abd-El-Rahman Ramadan S, et al. Ultrasound biomicroscopy in the diagnosis of skin diseases. Eur J Dermatol 2007;17:469–75. 10.1684/ejd.2007.0261 [DOI] [PubMed] [Google Scholar]
- 96. George R, Siordia H, Buhler J, et al. The use of high frequency ultrasound to monitor treatment of hypertrophic burn scars with fractionated ablative CO2 laser therapy. J Burn Care Res 2019;40:S135. 10.1093/jbcr/irz013.229 [DOI] [Google Scholar]
- 97. Jang KU, Lee JY, Choi JS, et al. 5FU and triamcinolone injection to the hypertrophic scar were compared. Burns 2009;35:S41–2. 10.1016/j.burns.2009.06.166 [DOI] [Google Scholar]
- 98. Li P, Li-Tsang CWP. Clinical effectiveness and intervention timing of smart pressure-monitored suit in the management of post-burn hypertrophic scar: a clinical controlled study with objective assessment. J Burn Care Res 2016;37:S199. 10.1097/01.bcr.0000483036.52429.db [DOI] [Google Scholar]
- 99. Li-Tsang CWP. The effect of a new silicone padding (SPMP) in management of Keloids: case review. J Burn Care Res 2011;32:S169. 10.1097/BCR.0b013e3182109aea [DOI] [Google Scholar]
- 100. Li-Tsang CWP, Feng B-B, Li K-C. Pressure therapy of hypertrophic scars after burns and related research. Zhonghua Shao Shang Za Zh 2010;26:411–5. [PubMed] [Google Scholar]
- 101. Maari C. Randomized, controlled, within-patient, single-blinded pilot study to evaluate the efficacy of the ablative fractional CO2 laser in the treatment of hypertrophic scars in adult burn patients. J Am Acad Dermatol 2017;76:AB212. 10.1016/j.jaad.2017.04.1113 [DOI] [Google Scholar]
- 102. Moortgat P, Vanhullebusch T, Anthonissen M, et al. Tension reducing taping as a mechanotherapy for hypertrophic burn scars: preliminary results from a pilot study. Wound Repair Regen 2020;28:A21. 10.1111/wrr.12772 [DOI] [Google Scholar]
- 103. Nedelec B, Couture M, Calva V, et al. Randomized controlled trial of the immediate and long-term effect of massage on adult postburn scar. J Burn Care Res 2018;39:S57. 10.1093/jbcr/iry006.106 [DOI] [PubMed] [Google Scholar]
- 104. Peters EP, Moortgat P. Electronic micro-needling on mature burn scars: a case series report. Wound Repair Regen 2018;26. 10.26226/morressier.5d1df08574846b60c6f39000 [DOI] [Google Scholar]
- 105. Seo C. Dynamic burn scar elasticity evaluation using ultrasonography. J Burn Care Res 2011;32:S167. 10.1097/BCR.0b013e3182109aea [DOI] [Google Scholar]
- 106. Siwy KG, Lee K, Donelan MB, et al. Fractionated Co2 laser and burn scar contractures: evaluation of post treatment scar function and appearance. J Burn Care Res 2016;37:S202. 10.1097/01.bcr.0000483036.52429.db [DOI] [Google Scholar]
- 107. Tu P, Wang Z-G, Zhang Q-X, et al. High frequency ultrasound in dynamic observation on effect of local injection with diprospan for treating pathological scar. CJIIT 2014;11:217–20. [Google Scholar]
- 108. Ud-Din S, Foden P, Douglas M, et al. A double-blind randomized controlled trial demonstrates for the first time evidence for the role of topical Epigallocatechin-3-Gallate in reducing angiogenesis, inflammation, and skin thickness in human skin Scarring: a noninvasive, morphological and Immu. Wound Repair Regen 2017;25:A3. 10.1111/wrr.12573 [DOI] [Google Scholar]
- 109. Ud-Din S, Foden P, Mazhari M, et al. Histomorphic assessment of noninvasive quantitative imaging in progression of cutaneous healing in human skin: dynamic optical coherence tomography versus high Requency ultrasound. Wound Repair Regen 2017;25:A3–4. 10.1111/wrr.12573 [DOI] [Google Scholar]
- 110. Ud-Din S, Foden P, Samer A, et al. Quantitative index for skin fibrosis: combined optical coherence tomography with ultrasound validated by histology and Immunohistochemisrty. Wound Repair Regen 2018;26:A11–2. 10.1111/wrr.12623 [DOI] [Google Scholar]
- 111. Alsharnoubi J, Mohamed O, Fawzy M. Photobiomodulation effect on children’s scars. Lasers Med Sci 2018;33:497–501. 10.1007/s10103-017-2387-3 [DOI] [PubMed] [Google Scholar]
- 112. Alsharnoubi J, Shoukry K-S, Fawzy MW, et al. Evaluation of scars in children after treatment with low-level laser. Lasers Med Sci 2018;33:1991–5. 10.1007/s10103-018-2572-z [DOI] [PubMed] [Google Scholar]
- 113. Berry RB, Tan OT, Cooke ED, et al. Transcutaneous oxygen tension as an index of maturity in hypertrophic scars treated by compression. Br J Plast Surg 1985;38:163–73. 10.1016/0007-1226(85)90045-1 [DOI] [PubMed] [Google Scholar]
- 114. Blome-Eberwein SA, Roarabaugh C, Gogal C, et al. Exploration of nonsurgical scar modification options: can the irregular surface of matured mesh graft scars be smooted with microdermabrasion? J Burn Care Res 2012;33:e133–40. 10.1097/BCR.0b013e3182331e09 [DOI] [PubMed] [Google Scholar]
- 115. Chan HH, Wong DSY, Ho WS, et al. The use of pulsed dye laser for the prevention and treatment of hypertrophic scars in Chinese persons. Dermatol Surg 2004;30:987–94. 10.1111/j.1524-4725.2004.30303.x [DOI] [PubMed] [Google Scholar]
- 116. Cheng W, Saing H, Zhou H, et al. Ultrasound assessment of scald scars in Asian children receiving pressure garment therapy. J Pediatr Surg 2001;36:466–9. 10.1053/jpsu.2001.21613 [DOI] [PubMed] [Google Scholar]
- 117. Cho YS, Jeon JH, Hong A, et al. The effect of burn rehabilitation massage therapy on hypertrophic scar after burn: a randomized controlled trial. Burns 2014;40:1513–20. 10.1016/j.burns.2014.02.005 [DOI] [PubMed] [Google Scholar]
- 118. Danin A, Georgesco G, Touze AL, et al. Assessment of burned hands reconstructed with integra® by ultrasonography and elastometry. Burns 2012;38:998–1004. 10.1016/j.burns.2012.02.017 [DOI] [PubMed] [Google Scholar]
- 119. Engrav LH, Heimbach DM, Rivara FP, et al. 12-year within-wound study of the effectiveness of custom pressure garment therapy. Burns 2010;36:975–83. 10.1016/j.burns.2010.04.014 [DOI] [PubMed] [Google Scholar]
- 120. Fong SSL, Hung LK, Cheng JCY. The cutometer and ultrasonography in the assessment of postburn hypertrophic scar: a preliminary study. Burns 1997;23 Suppl 1:S12–8. 10.1016/s0305-4179(97)90095-4 [DOI] [PubMed] [Google Scholar]
- 121. Issler-Fisher AC, Fisher OM, Smialkowski AO, et al. Ablative fractional CO2 laser for burn scar reconstruction: an extensive subjective and objective short-term outcome analysis of a prospective treatment cohort. BURNS 2017;43:573–82. 10.1016/j.burns.2016.09.014 [DOI] [PubMed] [Google Scholar]
- 122. Katz SM, Frank DH, Leopold GR, et al. Objective measurement of hypertrophic burn scar: a preliminary study of tonometry and ultrasonography. Ann Plast Surg 1985;14:121–7. 10.1097/00000637-198502000-00005 [DOI] [PubMed] [Google Scholar]
- 123. Kemp Bohan PM, Cooper LE, Lu KN, et al. Fractionated ablative carbon dioxide laser therapy decreases ultrasound thickness of hypertrophic burn scar: a prospective process improvement initiative. Ann Plast Surg 2021;86:273–8. 10.1097/SAP.0000000000002517 [DOI] [PubMed] [Google Scholar]
- 124. Lau JCM, Li-Tsang CWP, Zheng YP. Application of tissue ultrasound palpation system (TUPS) in objective scar evaluation. Burns 2005;31:445–52. 10.1016/j.burns.2004.07.016 [DOI] [PubMed] [Google Scholar]
- 125. Miletta N, Siwy K, Hivnor C, et al. Fractional ablative laser therapy is an effective treatment for hypertrophic burn scars: a prospective study of objective and subjective outcomes. Ann Surg 2021;274:e574–80. 10.1097/SLA.0000000000003576 [DOI] [PubMed] [Google Scholar]
- 126. Wiseman J, Simons M, Kimble R, et al. Effectiveness of topical silicone GEL and pressure garment therapy for burn scar prevention and management in children 12-months postburn: a parallel group randomised controlled trial. Clin Rehabil 2021;35:1126–41. 10.1177/02692155211020351 [DOI] [PubMed] [Google Scholar]
- 127. Wiseman J, Ware RS, Simons M, et al. Effectiveness of topical silicone GEL and pressure garment therapy for burn scar prevention and management in children: a randomized controlled trial. Clin Rehabil 2020;34:120–31. 10.1177/0269215519877516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Wood FM, Currie K, Backman B, et al. Current difficulties and the possible future directions in scar assessment. Burns 1996;22:455–8. 10.1016/0305-4179(95)00168-9 [DOI] [PubMed] [Google Scholar]
- 129. Yim H, Cho YS, Seo CH, et al. The use of alloderm on major burn patients: alloderm prevents post-burn joint contracture. Burns 2010;36:322–8. 10.1016/j.burns.2009.10.018 [DOI] [PubMed] [Google Scholar]
- 130. Żądkowski T, Nachulewicz P, Mazgaj M, et al. A new CO2 laser technique for the treatment of pediatric hypertrophic burn scars: an observational study. Medicine (Baltimore) 2016;95:e5168. 10.1097/MD.0000000000005168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Cho J, Jang Y, Hur J, et al. Effectiveness of Emu oil on burn scar. J Burn Care Res 2012;33:S71. 10.1097/BCR.0b013e3182508c98 [DOI] [Google Scholar]
- 132. Comstock J, Sood R. Can mature facial scars benefit from a transparent face mask? J Burn Care Res 2018;39:S219–20. 10.1093/jbcr/iry006.416 [DOI] [Google Scholar]
- 133. Jacobs M, Roggy D, Sood R. A preliminary report of a prospective study evaluating outcomes of burn scars treated with laser therapy. J Burn Care Res 2016;37:S106. 10.1097/01.bcr.0000483036.52429.db [DOI] [Google Scholar]
- 134. Kim SK, Park JM, Jang YH, et al. Management of hypertrophic scar after burn wound using microneedling procedure (dermastamp). Burns 2009;35:S37. 10.1016/j.burns.2009.06.146 [DOI] [Google Scholar]
- 135. Zuccaro J, Kelly C, Perez M, et al. The effectiveness of laser therapy for hypertrophic burn scars in pediatric patients: a prospective investigation. J Burn Care Res 2021;42:S24. [Google Scholar]
- 136. Alshehari A, Wahdan W, Maamoun MI. Comparative study between intralesional steriod injection and silicone sheet versus silicone sheet alone in the treatment of pathologic scars. Arch Balk Med Union 2015;50:364–6. [Google Scholar]
- 137. Chang C-S, Wallace CG, Hsiao Y-C, et al. Botulinum toxin to improve results in cleft lip repair: a double-blinded, randomized, vehicle-controlled clinical trial. PLoS ONE 2014;9:e115690. 10.1371/journal.pone.0115690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Fraccalvieri M, Sarno A, Gasperini S, et al. Can single use negative pressure wound therapy be an alternative method to manage keloid scarring? A preliminary report of a clinical and ultrasound/colour-power-doppler study. Int Wound J 2013;10:340–4. 10.1111/j.1742-481X.2012.00988.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Lacarrubba F, Patania L, Perrotta R, et al. An open-label pilot study to evaluate the efficacy and tolerability of a silicone gel in the treatment of hypertrophic scars using clinical and ultrasound assessments. J Dermatolog Treat 2008;19:50–3. 10.1080/09546630701387009 [DOI] [PubMed] [Google Scholar]
- 140. Li K, Nicoli F, Cui C, et al. Treatment of hypertrophic scars and keloids using an intralesional 1470 nm bare-fibre diode laser: a novel efficient minimally-invasive technique. Sci Rep 2020;10:21694. 10.1038/s41598-020-78738-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Li N, Yang L, Cheng J, et al. A retrospective study to identify the optimal parameters for pulsed dye laser in the treatment of hypertrophic burn scars in Chinese children with fitzpatrick skin types III and IV. Lasers Med Sci 2021;36:1671–9. 10.1007/s10103-021-03252-x [DOI] [PubMed] [Google Scholar]
- 142. Li-Tsang CWP, Zheng YP, Lau JCM. A randomized clinical trial to study the effect of silicone gel dressing and pressure therapy on posttraumatic hypertrophic scars. J Burn Care Res 2010;31:448–57. 10.1097/BCR.0b013e3181db52a7 [DOI] [PubMed] [Google Scholar]
- 143. Nicoletti G, Brenta F, Bleve M, et al. Long‐term in vivo assessment of bioengineered skin substitutes: a clinical study. J Tissue Eng Regen Med 2015;9:460–8. 10.1002/term.1939 [DOI] [PubMed] [Google Scholar]
- 144. Niessen FB, Spauwen PH, Robinson PH, et al. The use of silicone occlusive sheeting (Sil-K) and silicone occlusive gel (epiderm) in the prevention of hypertrophic scar formation. Plast Reconstr Surg 1998;102:1962–72. 10.1097/00006534-199811000-00023 [DOI] [PubMed] [Google Scholar]
- 145. Xuan Z, Liu H, Li C, et al. Wavelet bilateral filter algorithm-based high-frequency ultrasound image analysis on effects of skin scar repair. Sci Program 2021;2021:1–7. 10.1155/2021/9573474 [DOI] [Google Scholar]
- 146. Avetikov DS, Bukhanchenko OP, Skikevich MG, et al. Features of ultrasound diagnostics of postoperative hypertrophic and keloid scars. New Armen Med J 2018;12:43–8. [Google Scholar]
- 147. Ge X, Sun Y, Lin J, et al. Effects of multiple modes of ultrapulse fractional CO2 laser treatment on extensive scarring: a retrospective study. Lasers Med Sci 2022;37:1575–82. 10.1007/s10103-021-03406-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Guo R, Xiang X, Wang L, et al. Quantitative assessment of keloids using ultrasound shear wave elastography. Ultrasound Med Biol 2020;46:1169–78. 10.1016/j.ultrasmedbio.2020.01.010 [DOI] [PubMed] [Google Scholar]
- 149. Lobos N, Wortsman X, Valenzuela F, et al. Color doppler ultrasound assessment of activity in keloids. Dermatol Surg 2017;43:817–25. 10.1097/DSS.0000000000001052 [DOI] [PubMed] [Google Scholar]
- 150. Blome-Eberwein S. Fractional er:glass photothermolysis laser therapy to treat hypertrophic scarring. Lasers Surg Med 2012;44:61. 10.1002/lsm.22023 [DOI] [Google Scholar]
- 151. Blome-Eberwein S, Blaine C, Gogal C, et al. Fractional er:glass photothermolysis laser therapy to treat hypertrophic scarring. J Burn Care Res 2011;32:S95. 10.1097/BCR.0b013e3182109aea [DOI] [Google Scholar]
- 152. Timina I, Sharobaro V, Trykova I. A potential of the high-frequency ultrasonic investigation in the differential diagnostics of scars. Ultraschall Med 2013;34:01. 10.1055/s-0033-1355042 [DOI] [Google Scholar]
- 153. Zuccaro J, Kelly C, Perez M, et al. The effectiveness of laser therapy for hypertrophic burn scars in pediatric patients: a prospective investigation. J Burn Care Res 2021;42:847–56. 10.1093/jbcr/irab090 [DOI] [Google Scholar]
- 154. Zuccaro J, Perez M, Mohanta A, et al. Elastography-based quantification of burn scar stiffness. J Burn Care Res 2019;40:S215. 10.1093/jbcr/irz013.374 [DOI] [Google Scholar]
- 155. Issler-Fisher AC, Fisher OM, Smialkowski AO, et al. Ablative fractional CO2 laser for burn scar reconstruction: an extensive subjective and objective short-term outcome analysis of a prospective treatment cohort. Burns 2017;43:573–82. 10.1016/j.burns.2016.09.014 [DOI] [PubMed] [Google Scholar]
- 156. Jameson JL, Longo DL. Precision medicine — personalized, problematic, and promising. N Engl J Med 2015;372:2229–34. 10.1056/NEJMsb1503104 [DOI] [PubMed] [Google Scholar]
- 157. Robinson T, Bailey C, Morris H, et al. Bridging the research-practice gap in healthcare: a rapid review of research translation centres in England and Australia. Health Res Policy Syst 2020;18:117. 10.1186/s12961-020-00621-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Wynn TA. Cellular and molecular mechanisms of fibrosis. J Pathol 2008;214:199–210. 10.1002/path.2277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Willenborg S, Eming SA. Cellular networks in wound healing. Science 2018;362:891–2. 10.1126/science.aav5542 [DOI] [PubMed] [Google Scholar]
- 160. Kwan P, Desmouliere A, Tredget EE. Molecular and cellular basis of hypertrophic scarring. In: Herndon DN, ed. Total burn care. China: Elsevier, 2018: 455–65. [Google Scholar]
- 161. Hellström M, Hellström S, Engström-Laurent A, et al. The structure of the basement membrane zone differs between keloids, hypertrophic scars and normal skin: a possible background to an impaired function. J Plast Reconstr Aesthet Surg 2014;67:1564–72. 10.1016/j.bjps.2014.06.014 [DOI] [PubMed] [Google Scholar]
- 162. Nicolescu AC, Ionescu S, Ancuta I, et al. Subepidermal low-echogenic band—its utility in clinical practice: a systematic review. Diagnostics (Basel) 2023;13:970. 10.3390/diagnostics13050970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Laverde-Saad A, Simard A, Nassim D, et al. Performance of ultrasound for identifying morphological characteristics and thickness of cutaneous basal cell carcinoma: a systematic review. Dermatology 2022;238:692–710. 10.1159/000520751 [DOI] [PubMed] [Google Scholar]
- 164. Russell FM, Herbert A, Ferre RM, et al. Development and implementation of a point of care ultrasound curriculum at a multi-site institution. Ultrasound J 2021;13:9. 10.1186/s13089-021-00214-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Perry DM, McGrouther DA, Bayat A. Current tools for noninvasive objective assessment of skin scars. Plast Reconstr Surg 2010;126:912–23. 10.1097/PRS.0b013e3181e6046b [DOI] [PubMed] [Google Scholar]
- 166. Powers PS, Sarkar S, Goldgof DB, et al. Scar assessment: current problems and future solutions. J Burn Care Res 1999;20:54–60. 10.1097/00004630-199901001-00011 [DOI] [PubMed] [Google Scholar]
- 167. Nguyen DQA, Potokar T, Price P. A review of current objective and subjective scar assessment tools. J Wound Care 2008;17:101–2. 10.12968/jowc.2008.17.3.28666 [DOI] [PubMed] [Google Scholar]
- 168. Li H, Furst DE, Jin H, et al. High-frequency ultrasound of the skin in systemic sclerosis: an exploratory study to examine correlation with disease activity and to define the minimally detectable difference. Arthritis Res Ther 2018;20:181. 10.1186/s13075-018-1686-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Santiago T, Santos E, Ruaro B, et al. Ultrasound and elastography in the assessment of skin involvement in systemic sclerosis: a systematic literature review focusing on validation and standardization – WSF skin ultrasound group. Semin Arthritis Rheum 2022;52:151954. 10.1016/j.semarthrit.2022.151954 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-078361supp001.pdf (464.1KB, pdf)
Data Availability Statement
No data are available.