Abstract
Late-onset sepsis continues to be a significant cause of morbidity and mortality in very low-birth-weight infants. Earlier detection of infection with heart rate variability monitoring through the use of the HeRO monitor has been shown to reduce mortality rate by 22%. This article reviews how HeRO is used to assist in earlier diagnosis and treatment of infection.
Keywords: heart rate variability, infection, neonate, prematurity, sepsis, very low birth weight
INTRODUCTION: HeRO MONITOR FOR SEPSIS DETECTION AND MORTALITY REDUCTION
Late-onset sepsis (LOS) is a leading cause of death among very-low-birth-weight (VLBW, <1500g) infants, and early detection and treatment will lead to better outcomes in many cases. Heart rate characteristics monitoring with the HeRO (Heart Rate Observation) monitor was developed to detect sepsis in its early stages,1–3 and the use of the monitor reduced mortality rates by 22% in a large, multi-center, randomized, clinical trial of 3003 VLBW infants.4 Nurses are the frontline caregivers in the NICU and need to know about the HeRO monitor to maximize its usefulness. In this review, we provide a general overview of neonatal sepsis, explain how abnormal heart rate characteristics occur in sepsis, describe development of the HeRO monitor, and give practical suggestions on how to use the HeRO score to make important decisions in the care of patients in the neonatal intensive care unit (NICU).
SEPSIS INCIDENCE, RISKS, AND SIGNS IN VLBW INFANTS
Although the incidence of sepsis is declining with increased attention to hand and central catheter hygiene, preterm VLBW infants will always be vulnerable to life-threatening infections. In a survey of nearly 7000 VLBW infants in the National Institutes of Child Health and Development Neonatal Research Network centers from 1998 to 2000, 21% of infants who survived longer than 3 days had at least 1 episode of blood culture-positive sepsis (late-onset septicemia >3 days of age; late-onset sepsis [LOS]).5 Infants with LOS had a mortality rate that was more than twice as high as those without sepsis, and survivors had a higher rate of neurodevelopmental impairment.6,7 The estimated cost of each episode of LOS in VLBW infants is $10,000.8
Immaturity of the preterm immune system increases the risk for life-threatening infections.9 Decreased barrier function such as permeable skin and mucous membranes, and immature inflammatory responses and complement, limit the ability to contain infection at the site of entry. Invasive plastic tubes and catheters, although essential for keeping VLBW infants alive, allow colonization and infection with bacteria and fungi. Once pathogens enter the preterm infant’s bloodstream, the immaturity of the infant’s innate and adaptive immune functions increases the likelihood that the infection will progress to overwhelming sepsis.
Sepsis is difficult to diagnose in its early stages when VLBW infants have subtle, nonspecific signs that could be caused by sepsis or other developmental or pathophysiologic processes.10 Signs may include lethargy, decreased tone, increased apnea and bradycardia, feeding intolerance, temperature and glucose instability, and respiratory distress. As sepsis progresses, infants may develop shock, coagulopathy, and multiorgan system failure, leading to death.11 Despite advances in NICU care, sepsis-associated mortality among VLBW infants remains unacceptably high at approximately 20%.5
Detecting sepsis early, before the infant gets terribly sick, is a difficult task. Once subtle signs are identified, laboratory tests may be obtained to assess whether the symptoms are caused by sepsis. The complete blood cell count may show a high or low white blood cell number, increased immature neutrophil forms, or low platelets. Acute-phase reactants such as C-reactive protein and procalcitonin, may rise during infection.12 Point-of-care testing may show hyper- or hypoglycemia or metabolic acidosis. Clinicians may use some or all of these tests to help make decisions about starting or stopping antibiotics while awaiting results of cultures. Although blood culture is the gold standard for the diagnosis of sepsis, the false-negative rate may be high when low sample volumes are obtained in neonates.13
Finding a way to detect sepsis earlier, before an infant has clinical deterioration prompting testing and treatment, would be a better solution to improving outcomes. One way to do this is through monitoring for physiologic changes that occur in the early phase of sepsis, and one such change is in heart rate characteristics.14,15
HEART RATE CHARACTERISTICS IN LATE-ONSET SEPTICEMIA
In the healthy state, there is beat-to-beat variability in the heart rate, with numerous small accelerations and decelerations regulated by the autonomic nervous system. The sympathetic system is responsible for accelerations and the parasympathetic system for decelerations. Various pathologic processes are associated with decreased heart rate variability, including sepsis, acute brain injury, and cardiac disease.16 In neonatal sepsis, decreased heart rate variability is often accompanied by transient decelerations in the heart rate, as shown in Figure 1.17–19 Figure 2 displays a multipatient view of the current HeRO score and 5-day trend. These heart rate abnormalities are similar to those seen in fetuses in the setting of poor perfusion, asphyxia, and chorioamnionitis.20,21 In some preterm infants, abnormal heart rate characteristics of decreased variability and decelerations occur hours or even days before clinicians suspect that the infant is septic. After following heart rate patterns and correlating them with cases of sepsis in more than 300 VLBW NICU patients, researchers at the University of Virginia developed a noninvasive continuous heart rate characteristics (HRC) monitoring system to assess risk for impending sepsis.2 The HeRO monitor (Medical Predictive Sciences, Charlottesville, VA) takes electrocardiogram data from standard NICU bedside monitors and, using a mathematical formula that includes measures of variability and decelerations, displays a number, the HRC index, or HeRO score. The score was developed using multivariable logistic regression3,19,22 as the fold increased risk a baby will deteriorate from sepsis in the next 24 hours. It was developed at the University of Virginia NICU and then validated in more than 300 VLBW infants at the Wake Forest University NICU. A HeRO score of 1 indicates low-risk for infection, whereas a score of >2 indicates a 2-fold higher chance that the infant will be diagnosed with sepsis within 24 hours, a score of 3, a 3-fold increased risk, and so on. The HeRO score was shown to add to clinical signs and laboratory tests for the diagnosis of late-onset sepsis in preterm infants.22,23
FIGURE 1.
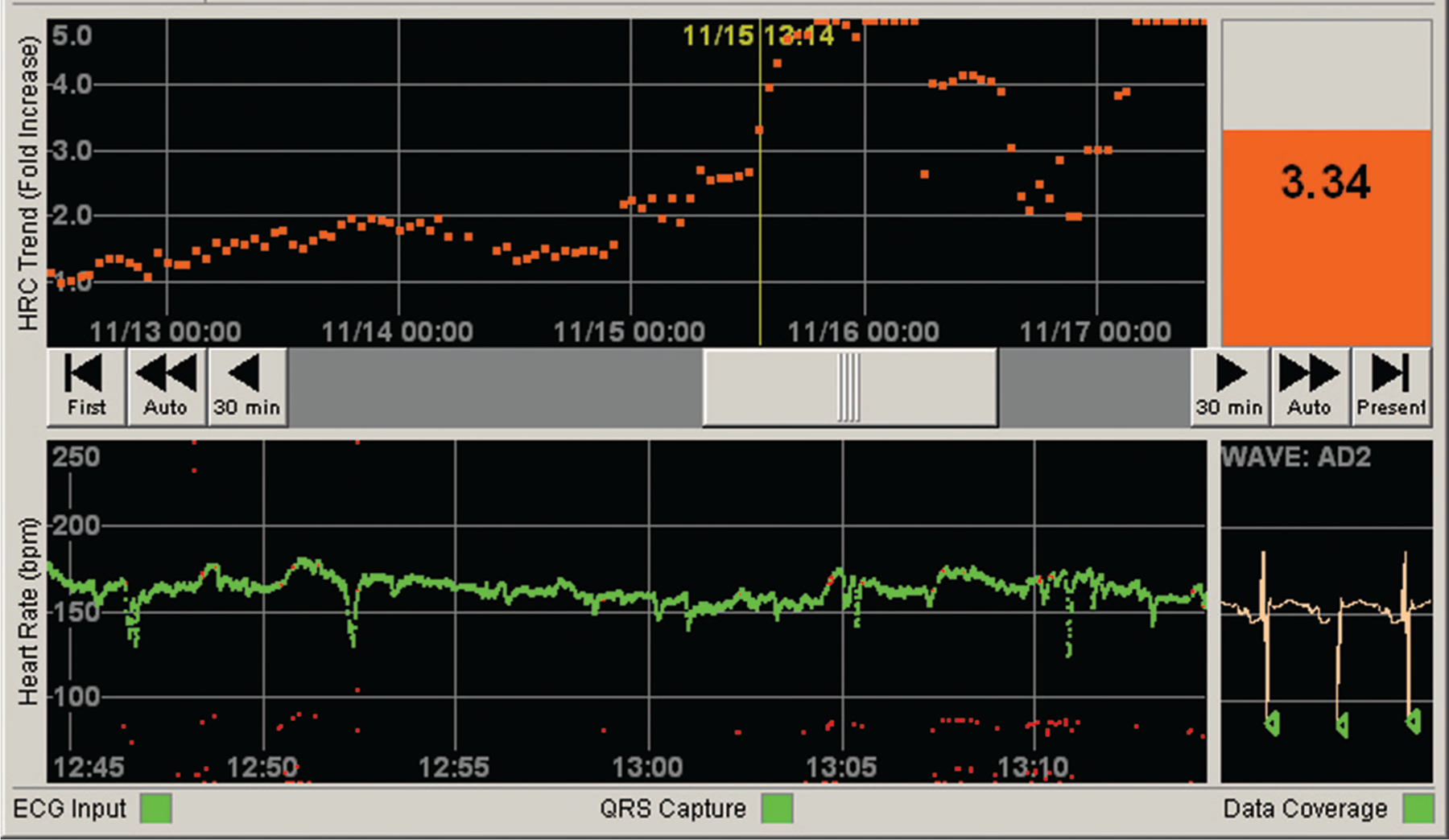
HeRO (Heart Rate Observation) monitor screen shot from an infant with sepsis. The top tracing shows the trend in the HeRO score over the last 5 days. The bottom tracing shows the last 30 minutes of heart rate. Clinicians can see the current HeRO score displayed at the top right, compare it with the previous 5-day trend, and scroll through to see 30-min heart rate (HR) tracings. In this case, the HeRO score had risen from a baseline of 1 to 2 for several days, eventually reaching a peak of >5. At the time indicated by the vertical line, the HeRO score was 3.34 and rising, and the 30-min HR tracing shows an abnormal pattern of few accelerations and numerous decelerations. The infant was diagnosed with Klebsiella septicemia (positive blood and urine cultures).
FIGURE 2.
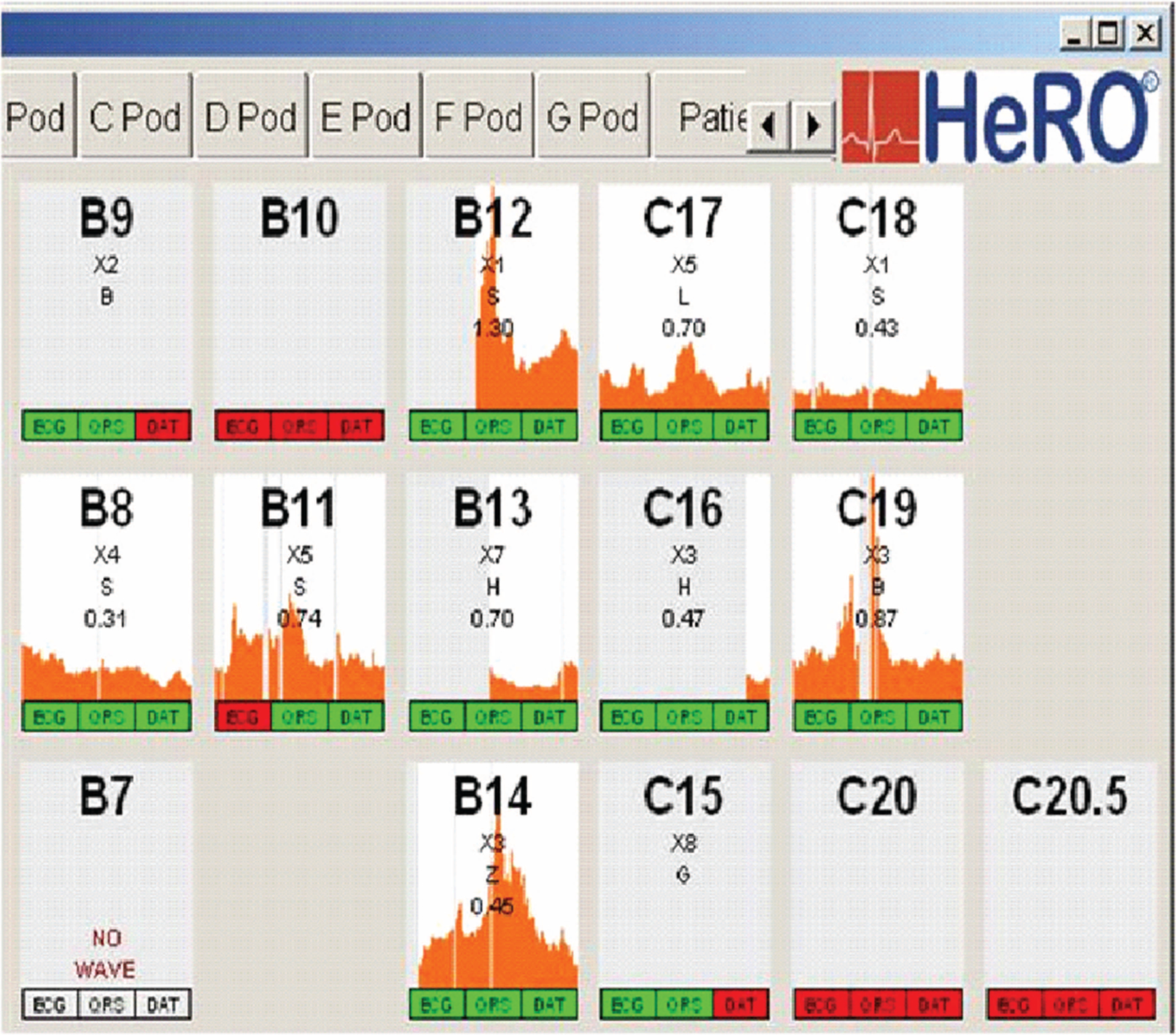
Multipatient view of HeRO (Heart Rate Observation) monitor. Shown are HeRO scores for infants in 2 sections of a neonatal intensive care unit. The orange shading indicates the height of the HeRO score for the previous 5 days. The bottom number in each patient panel indicates the current HeRO score, which is updated every hour on the basis of heart rate variability and decelerations over the previous 12 hours. By clicking on a specific bed number, the individual patient HeRO screen shown in Figure 1 may be viewed.
The important question of whether the HRC monitor improves patient outcomes was tested in a randomized, controlled trial of 3003 VLBW infants in 9 NICUs in the United States.4 The study group had the HeRO score monitored and displayed to the healthcare team. The control group had the score monitored but not displayed. Clinicians were educated on how the HeRO score was developed and were encouraged to evaluate a baby when the score was rising. There was no required intervention for any particular score; instead, clinicians were encouraged to use clinical judgment for decisions about cultures and antibiotics. This trial was sponsored by the National Institutes of Health and was the largest, randomized, clinical trial ever published in VLBW infants. The outcome was a 22% relative decrease in mortality rate in the infants whose HeRO score was displayed to clinicians (10.2% in control nondisplay infants vs 8.1% in infants whose HeRO score was displayed; P = .04). The number needed to monitor was 48 VLBW infants or 23 extremely low birth weight (ELBW) (<1000 g) infants for each life saved. There was a small increase in the number of blood cultures sent and antibiotics given in the HeRO monitor display group.
HeRO MONITOR: WHAT NICU CLINICIANS NEED TO KNOW
The HeRO monitor is now used in many NICUs in the Unites States to aid in the detection of sepsis. It was cleared by the US Food and Drug Administration in 2003 for monitoring heart rate characteristics and was approved for use in Europe in 2012. Nurses providing direct care to infants should regularly observe and record each infant’s HeRO score and report rising scores to physicians and nurse practitioners. There are no alarms on the monitor, and it is essential that caregivers pay attention to the score, together with standard observations of patient status such as physical examination, vital signs, and laboratory values. An example of the HeRO monitor showing abnormal heart rate characteristics in a VLBW infant with sepsis is shown in Figure 1.
WHAT CONDITIONS OTHER THAN SEPSIS CAUSE AN ELEVATED HeRO SCORE?
The HeRO monitor was developed to detect sepsis, and an acute increase in the HeRO score may be associated with either blood culture-positive or clinical sepsis or other infectious conditions such as urinary tract infection. Necrotizing enterocolitis can also cause a rise in the HeRO score. In many cases, the score starts to rise before there is clinical suspicion of illness.14
Noninfectious disease states can be associated with abnormally low heart rate variability or transient heart rate decelerations, leading to an increased HeRO score. Infants with severe intraventricular hemorrhage, for example, may have intermittent spikes in their score in the first month after birth. Babies with severe chronic lung disease may have chronically or intermittently elevated HeRO scores, and acute respiratory decompensation including severe apnea, hypoxia, or respiratory acidosis may cause a spike in the score.15 For infants with chronically or frequently elevated scores, diagnosis of sepsis presents a challenge. The relative change in the score over the infant’s usual baseline should be considered together with other clinical and laboratory indicators to determine whether a sepsis workup and antibiotics are indicated.
Most medications commonly used in the NICU do not affect the HeRO score, with the exception of dexamethasone, anticholinergics, and muscle relaxants. Dexamethasone improves heart rate variability and lowers the HeRO score, likely in part because of anti-inflammatory effects.24 Atropine and other anti-cholinergic drugs dramatically depress heart rate variability, and muscle relaxants (paralytics) and other anesthetic agents can also decrease variability and lead to an acute rise in the HeRO score. Surgical procedures usually lead to a transient elevation in the HeRO score, which may be because of anesthetic agents or because of tissue trauma or systemic inflammation.25
CLINICAL APPROACH TO AN INFANT WITH A RISING HeRO SCORE
The most important point is to consider the patient first. If a baby is looking or acting septic, cultures should be obtained and antibiotics given regardless of the HeRO score. On the contrary, even in the absence of any clinical signs, a rise of the HeRO score more than 1–2 points over the infant’s baseline without another explanation should raise the suspicion for sepsis. In between these 1–2 scenarios, if the HeRO score is only slightly elevated over baseline (eg, 1 point) and all other indicators are normal and reassuring, close observation for clinical signs or for continued rise in the HeRO score may be the best course of action. It is important to use clinical judgment and, when appropriate, to obtain adjunct tests for making decisions about therapy, since overuse of antibiotics can be detrimental. The Table outlines a course of action when a baby’s HeRO score is rising.
TABLE.
What to Do When the HeRO (Heart Rate Observation) Score Is Increasing
|
HeRO IN ACTION: CASE STUDIES
Baby H is a 30-week infant now 2 weeks old. She is on room air and just reached full enteral feedings and had her central catheter removed. She develops a slightly low temperature of 36°C but looks well on examination and is not acting sick. The nurse notifies the nurse practitioner of the temperature and observes that the HeRO score has increased from 0.8 to 1.9 over the past 12 hours. Blood and urine cultures are sent and antibiotics started. The blood culture yields coagulase-negative Staphylococcus and the baby is treated with vancomycin and does well.
Baby R is a 24-week infant now 4 months old with a complicated NICU course including severe chronic lung disease, necrotizing enterocolitis, and short bowel syndrome requiring parenteral nutrition via a central venous catheter. He has had chronically high and spiky HeRO scores in the past, but his recent baseline is less than 2. He develops worsening respiratory distress and acidosis requiring increased ventilator rate. The nurse alerts the nurse practitioner that the HeRO score has increased to 3.2. After discussion with the medical team, a decision is made to send cultures and start antibiotics. The cultures are negative, the clinical course, chest radiographs, and ancillary tests are not felt to be suggestive of sepsis or pneumonia, the HeRO score declines, and antibiotics are discontinued after 48 hours.
Baby C is a 27-week infant, now 3 weeks old, on full feeds and caffeine. He typically has about 3 apnea events requiring intervention per day, but today the nurse indicates on rounds that he had 6 documented apnea events in the last 24 hours. A discussion ensues about whether this increase in apnea is real or simply represents differences in documentation from 1 day to the next. If there truly is more apnea, does the baby need more caffeine, or could this be an early sign of sepsis? The nurse reports that the HeRO score remains low (<1.5 over the last 24 hours). The team decides to watch the baby closely and not send tests or start antibiotics unless the clinical condition or HeRO score worsens.
CONCLUSION
Sepsis continues to be a serious threat to the life and well-being of VLBW infants. Determining which NICU patients are becoming septic on any given day is difficult, if not impossible, through routine observation of the baby and the vital signs. The HeRO monitor provides a continuous, noninvasive way of identifying pathologic patterns in heart rate and can alert clinicians to subtle physiologic changes in the early phase of sepsis. Reduced mortality was demonstrated with HeRO monitoring, and this mortality reduction was greatest in infants with late-onset sepsis. It is critical that nurses understand how to appropriately use this important new technology to optimize the care of preterm infants, reduce mortality rate, and send babies home healthier.
Footnotes
The authors declare no conflict of interest or financial relationship with the HeRO monitor.
References
- 1.Griffin MP, Moorman JR. Toward the early diagnosis of neonatal sepsis and sepsis-like illness using novel heart rate analysis. Pediatrics. 2001;107(1):97–104. [DOI] [PubMed] [Google Scholar]
- 2.Griffin MP, O’Shea TM, Bissonette EA, Harrell FE Jr, Lake DE, Moorman JR. Abnormal heart rate characteristics preceding neonatal sepsis and sepsis-like illness. Pediatr Res 2003;53(6):920–926. [DOI] [PubMed] [Google Scholar]
- 3.Griffin MP, Lake DE, Bissonette EA, Harrell FE Jr, O’Shea TM, Moorman JR. Heart rate characteristics: novel physiomarkers to predict neonatal infection and death. Pediatrics. 2005;116(5):1070–1074. [DOI] [PubMed] [Google Scholar]
- 4.Moorman JR, Carlo WA, Kattwinkel J, et al. Mortality reduction by heart rate characteristic monitoring in very low birth weight neonates: a randomized trial. J Pediatr 2011;159(6):900.e1–906.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stoll BJ, Hansen N, Fanaroff AA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics. 2002;110(2 Pt 1):285–291. [DOI] [PubMed] [Google Scholar]
- 6.Stoll BJ, Hansen NI, Adams-Chapman I, et al. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA 2004;292(19):2357–2365. [DOI] [PubMed] [Google Scholar]
- 7.Bassler D, Stoll BJ, Schmidt B, et al. Using a count of neonatal morbidities to predict poor outcome in extremely low birth weight infants: added role of neonatal infection. Pediatrics. 2009;123(1):313–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson TJ, Patel AL, Jegier BJ, Engstrom JL, Meier PP. Cost of morbidities in very low birth weight infants. J Pediatr 2013;162(2):243.e1–249.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cuenca AG, Wynn JL, Moldawer LL, Levy O. Role of innate immunity in neonatal infection. Am J Perinatol 2013;30(2):105–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Short MA. Guide to a systematic physical assessment in the infant with suspected infection and/or sepsis. Adv Neonatal Care. 2004;4(3):141–153; quiz 54–57. [DOI] [PubMed] [Google Scholar]
- 11.Short MA. Linking the sepsis triad of inflammation, coagulation, and suppressed fibrinolysis to infants. Adv Neonatal Care. 2004;4(5):258–273. [DOI] [PubMed] [Google Scholar]
- 12.Benitz WE. Adjunct laboratory tests in the diagnosis of early-onset neonatal sepsis. Clin Perinatol 2010;37(2):421–438. [DOI] [PubMed] [Google Scholar]
- 13.Schelonka RL, Chai MK, Yoder BA, Hensley D, Brockett RM, Ascher DP. Volume of blood required to detect common neonatal pathogens. J Pediatr 1996;129(2):275–278. [DOI] [PubMed] [Google Scholar]
- 14.Fairchild KD. Predictive monitoring for early detection of sepsis in neonatal ICU patients. Curr Opin Pediatr 2013;25(2):172–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fairchild K, Aschner JL. HeRO monitoring to reduce mortality in NICU patients. Res Rep Neonatol 2012;2:65–76. [Google Scholar]
- 16.Buchman TG, Stein PK, Goldstein B. Heart rate variability in critical illness and critical care. Curr Opin Crit Care. 2002;8(4):311–315. [DOI] [PubMed] [Google Scholar]
- 17.Kovatchev BP, Farhy LS, Cao H, Griffin MP, Lake DE, Moorman JR. Sample asymmetry analysis of heart rate characteristics with application to neonatal sepsis and systemic inflammatory response syndrome. Pediatr Res 2003;54(6):892–898. [DOI] [PubMed] [Google Scholar]
- 18.Cao H, Lake DE, Griffin MP, Moorman JR. Increased nonstationarity of neonatal heart rate before the clinical diagnosis of sepsis. Ann Biomed Eng 2004;32(2):233–244. [DOI] [PubMed] [Google Scholar]
- 19.Moorman JR, Lake DE, Griffin MP. Heart rate characteristics monitoring for neonatal sepsis. IEEE Trans Biomed Eng 2006;53(1): 126–132. [DOI] [PubMed] [Google Scholar]
- 20.Lake DE, Griffin MP, Moorman JR. New mathematical thinking about fetal heart rate characteristics. Pediatr Res 2003;53(6):889–890. [DOI] [PubMed] [Google Scholar]
- 21.Cao H, Lake DE, Ferguson JE II, Chisholm CA, Griffin MP, Moorman JR. Toward quantitative fetal heart rate monitoring. IEEE Trans Biomed Eng 2006;53(1):111–118. [DOI] [PubMed] [Google Scholar]
- 22.Griffin MP, Lake DE, Moorman JR. Heart rate characteristics and laboratory tests in neonatal sepsis. Pediatrics. 2005;115(4):937–941. [DOI] [PubMed] [Google Scholar]
- 23.Griffin MP, Lake DE, O’Shea TM, Moorman JR. Heart rate characteristics and clinical signs in neonatal sepsis. Pediatr Res 2007;61(2): 222–227. [DOI] [PubMed] [Google Scholar]
- 24.Griffin MP, Lake D, Siadaty MS, Moorman JR. Dexamethasone increases neonatal heart rate variability. Pediatr Res 2003;53(4):479A.12595598 [Google Scholar]
- 25.Griffin MP, Lake DE, Siadaty MS, Moorman JR. Heart rate characteristics are abnormal after surgery in neonates. Pediatr Res 2003;53(4):31A. [Google Scholar]


