Abstract
Research using psychophysiological methods holds great promise for refining clinical assessment, identifying risk factors, and informing treatment. Unfortunately, unique methodological features of existing approaches limit inclusive research participation and, consequently, generalizability. This brief overview and commentary provides a snapshot of the current state of representation in clinical psychophysiology, with a focus on the forms and consequences of ongoing exclusion of Black participants. We illustrate issues of inequity and exclusion that are unique to clinical psychophysiology, considering intersections among social constructions of Blackness and biased design of current technology used to measure electroencephalography, skin conductance, and other signals. We then highlight work by groups dedicated to quantifying and addressing these limitations. We discuss the need for reflection and input from a wider variety of stakeholders to develop and refine new technologies, given the risk of further widening disparities. Finally, we provide broad recommendations for clinical psychophysiology research.
Clinical psychological science, like other fields of psychology, is beginning to reckon with historical and ongoing inequities, especially those related to race and racism. Race is socially constructed based on perceptions of physical traits, such as skin color, hair, and facial features, and has been imbued with oppressive power (racism) through the creation and maintenance of a sociopolitical hierarchy (American Psychological Association [APA], 2021a,b). Racism and other intersecting systems of oppression (e.g., sexism, homophobia, ableism, classism, xenophobia) are intertwined with clinical psychological theory and practice (APA, 2021a; for a review, see Roberts et al., 2020).
This overview and commentary aims to expand on recent work examining racial inequities within a subfield of clinical psychological science that rests at the interface between body, brain, and mind: clinical psychophysiology. Psychophysiological methods hold great promise for refining assessment, identifying risk factors, and informing treatment (Hajcak et al., 2019). Clinical psychophysiological research can bridge neurological and behavioral units of analysis, provide a medium for cross-species translation, and parse relevant mechanisms in clinical trials. This approach is a core priority of mental health research funding agencies, as exemplified by the National Institute of Mental Health (NIMH) Research Domain Criteria (RDoC; Hajcak & Patrick, 2015; Insel, 2015; Patrick & Hajcak, 2016). Research questions catalyzed by the continued “neuroscientification of psychology” have increased demand for psychophysiological approaches, particularly within clinical psychology (Haslam et al., 2021). Furthermore, clinical psychophysiology continues to gain ground as the proliferation of more affordable and easy-to-use psychophysiological equipment makes these approaches more accessible to researchers (Kaye et al., 2016; Wilson, 2010).
Clinical psychophysiology is subject to the same issues of racial inequity that plague other subfields of psychology. Systematic reviews have shown mistrust in researchers to be a key barrier to participation of minoritized communities (George et al., 2014; Schmotzer, 2012). Although historical harm by the research and medical community has caused distrust and hesitance to participate in research among individuals with marginalized identities (Kennedy et al., 2007), some analysis suggest they are often as equally willing to participate in research when equitably recruited (Fisher & Kalbaugh, 2011; Wendler et al., 2005). Still, both historically and currently, psychopathology research participant samples have been dominated by individuals with privileged identities, particularly White, college-educated, cisgender people (Fisher & Kalbaugh, 2011; Gatzke-Kopp, 2016; Roberts et al., 2020; Wendler et al., 2005). Because of long-standing systems of racial oppression, biased representation has been made invisible, and findings are generalized as if they were drawn from representative samples (Helms, 1993; Helms et al., 2006). As one example, a classic and well-replicated finding in clinical psychophysiology is that pre-pulse inhibition — the dampened neural response to a strong sensory stimulus when it is preceded by a weak sensory stimulus — is reduced in individuals with or at high risk for schizophrenia (Li et al., 2021; Swerdlow et al., 2014). This finding, considered a key biomarker of schizophrenia (Donati et al., 2020), is derived from studies of predominantly White participants, but the results are presumed to apply universally — even though schizophrenia is diagnosed up to two to four times more often in Black individuals than White (Jones & Gray, 1986; Olbert et al., 2018; Schwartz & Blankenship, 2014). Given complex issues surrounding racially biased diagnostic practices that may contribute to these figures, it remains to be seen whether this biomarker applies equally well across less homogeneous groups (Martinez, 2021).
Importantly, however, psychophysiology broadly, and clinical psychophysiology specifically, also introduces unique forms of systemic bias that prove especially threatening to sample representativeness and, as a result, generalizability of findings. For example, electroencephalography (EEG) and electrodermal analysis (EDA) depend on technology originally developed for, and refined with, light skin and thin, straight hair (see Webb et al., 2022). As we will discuss, individuals with darker skin and/or curly, tightly coiled, dense, or voluminous hair are systematically disqualified at disproportionate rates from clinical psychophysiology research using these methods. These phenotypic characteristics, subject to discrimination because of technical limitations in clinical psychophysiology research (i.e., “phenotypic bias”; Webb et al., 2022), are often observed in those racialized as Black, who are additionally subject to other forms of racial discrimination in clinical psychology more broadly. This intersection between forms of oppression in research — one that may be particularly glaring in clinical psychophysiology — results in unrepresentative samples and biased generalizations. As we will discuss, recent advances in psychophysiological technology risk increasing this inequity in clinical psychophysiology as well as other related subfields of psychology (e.g., cognitive neuroscience).
Clinical and other psychophysiology researchers have a duty to publish robust, generalizable results. This duty is especially important given that studies including psychophysiological measures may be perceived by the public as particularly believable and trustworthy (Gatzke-Kopp, 2016; Weisberg et al., 2008). Because results using such measures are seen as more “objective,” they may be used to justify the development and implementation of non-representative assessment tools and intervention approaches that are mistakenly applied universally. Thus, there is a critical and immediate need to address inequities in clinical psychophysiology.
Goals and Scope
The authors of this article represent a range of career stages, cultural identities, and disciplines, including psychology, communication, neuroscience, engineering, private practice, and the hair care industry. Our collective goal is to increase awareness of problems and potential solutions in addressing diversity, equity, and inclusion in all psychophysiology research, using examples from clinical psychophysiology. To that end, this commentary focuses on issues of racial representation, particularly the systemic exclusion of Black research participants, in our subfield’s study samples, recognizing that this is only one piece of a larger conversation with implications for multiple groups. First, we highlight recent efforts to quantify racial and ethnic representativeness in clinical psychophysiology samples broadly and present results from a new literature review of three prominent academic journals. We then explore how phenotypic discrimination against dark skin and curly, tightly coiled hair in clinical psychophysiology research intersects with anti-Black racism to contribute to sustained inequities and exclusion. In doing so, we emphasize that the problem of underrepresentation in psychophysiological research lies in the limitations of current equipment, rather than the individuals whose phenotypic characteristics are not yet equitably served by psychophysiological technologies. Perhaps most importantly, we call attention to recent and burgeoning work on this topic, including snapshots of new data from groups led by researchers of color who are taking steps to increase inclusivity in this field. To conclude, we provide broad recommendations to help clinical psychophysiologists contribute to a more equitable clinical psychological science.
The State of Racial/Ethnic Representativeness in Clinical Psychophysiology: A Preliminary Literature Review
In pursuing reform in clinical psychophysiology, a foundational step is to quantify existing issues with study sample composition, including the degree to which participants of color — particularly Black individuals — are excluded from this research. However, most researchers using psychophysiology measures simply do not report such demographics for their final sample. In the introduction to a special issue on diversity and representation in Psychophysiology, the flagship journal of the Society for Psychophysiological Research, Gatzke-Kopp (2016) noted that greater than 85% of Psychophysiology articles in the preceding three years were missing a description of racial demographics. To our knowledge, this single statistic is the only existing quantification of the broad state of representativeness in psychophysiology research.
In an effort to develop a more nuanced picture over the last quarter century, we conducted a preliminary literature review of articles from Psychophysiology, which exclusively publishes research using such methods, and two prestigious clinical psychology journals that often publish articles using psychophysiological methods: Journal of Psychopathology and Clinical Science (JPCS; formerly Journal of Abnormal Psychology), and Clinical Psychological Science (CPS). To balance coverage and efficiency, we used sparse sampling by reviewing and coding the main text and supplemental materials of every article published in Psychophysiology during 1997–2000, 2007–2010, and 2017–2020. We also identified articles from the same three time periods in JPCS and the latest time period in CPS (as CPS was established in 2013) that contained psychophysiology measures by searching in APAPsycNet and SAGE Journals and cross-referencing with PubMed for any of several psychophysiology-related terms derived from the Psychophysiology articles found (e.g., “skin conductance,” “electrophysiology”; see Supplemental Materials for search terms). All articles were coded for article type (e.g., empirical report, literature review), region of sample recrutiment (U.S. versus non-U.S.), reported sample demographics (including sex, gender, race, ethnicity), and psychophysiological methods used. Here, we describe the proportion of articles that reported racial and/or ethnic sample composition, and among the articles that did so and used U.S.-based samples, summarize the racial and/or ethnic demographics provided (see Figures 1–3).
Figure 1.
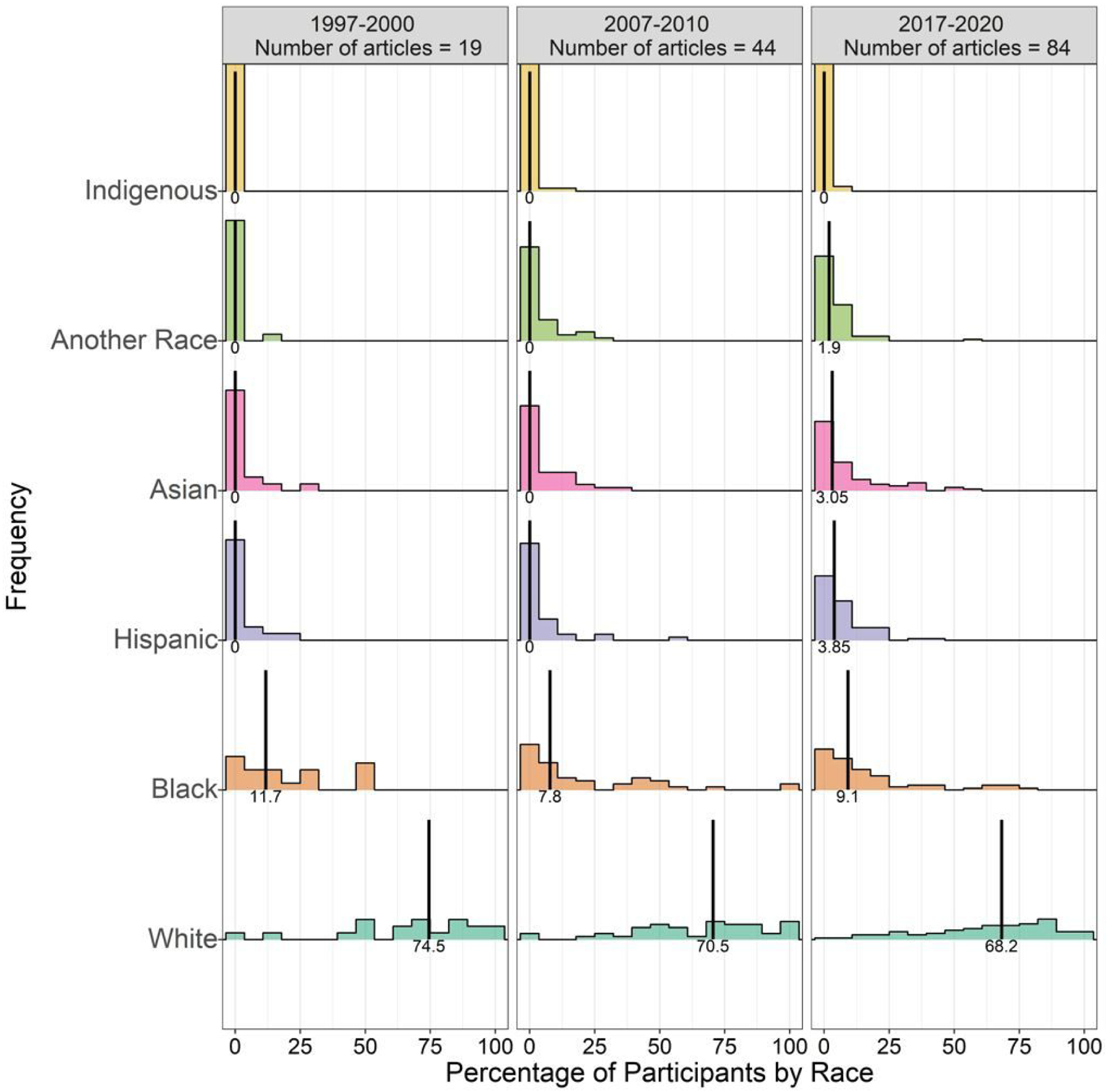
Participant demographics among the 13.8% of Psychophysiology articles that reported sample race and ethnicity.
Vertical black lines refer to the median percentage of each race/ethnicity across included articles. Of note, medians are presented due to the clear overdispersion of percentage of races and ethnicities; medians will often not sum to 100%. ‘Another Race’ includes all races not included in the listed categories, including biracial/multiracial individuals.
Figure 3.
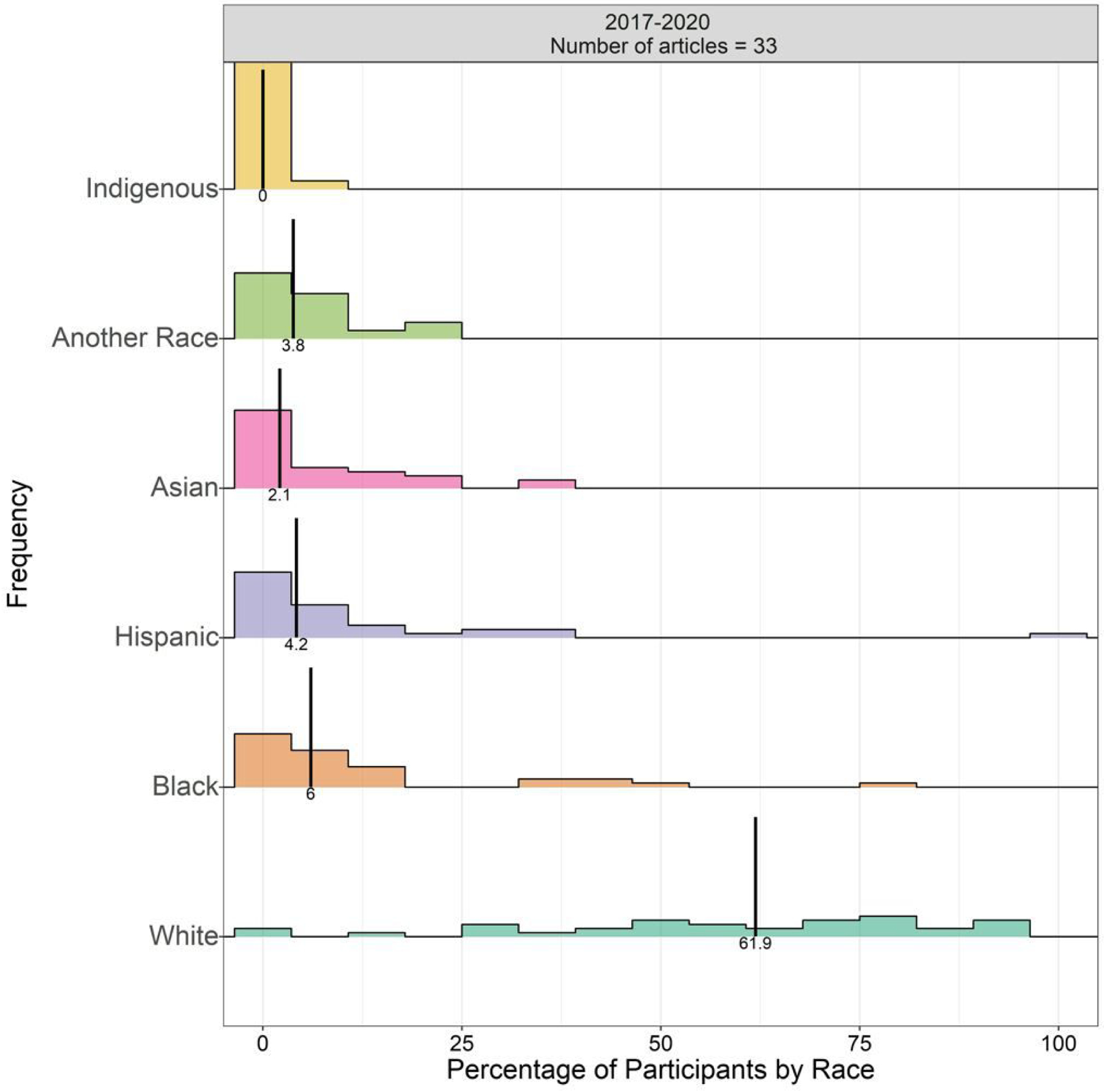
Participant demographics among the 74.5% of Clinical Psychological Science (CPS) articles that reported sample race and ethnicity.
Vertical black lines refer to the median percentage of each race/ethnicity across included articles. Of note, medians are presented due to the clear overdispersion of percentage of races and ethnicities; medians will often not sum to 100%. ‘Another Race’ includes all races not included in the listed categories, including biracial/multiracial individuals.
Out of 1480 articles in Psychophysiology across all three time periods, we screened out “ineligible” articles that did not include empirical samples (e.g., commentaries, literature reviews), leaving 1315 articles. Of these, only 182 (13.8%) included a description of the sample’s race and/or ethnicity. Reporting of race and/or ethnicity increased in 2017–2020 (17.7%) compared to 2007–2010 (12.1%) and 1997–2000 (8.0%). Though reporting of race and/or ethnicity has clearly improved following Psychophysiology’s special issue that strongly encouraged and emphasized the importance of doing so (Gatzke-Kopp, 2016), it remains inadequate, likely because it is still not explicitly required by the journal.
Out of 978 articles from the targeted time frame in JPCS, 161 included at least one psychophysiology term, of which 38 were deemed ineligible, mirroring the criteria for Psychophysiology (e.g., lacking an empirical sample or missing psychophysiological measurements), resulting in 123 articles for analysis. Among these, 62 (50.4%) included a description of sample race and/or ethnicity. Reporting of race and/or ethnicity improved across years (in 1997–2000: 29.0%; 2007–2010: 58.5%; 2017–2020: 56.9%), yet, like Psychophysiology, needs continued improvement. As an American Psychological Association journal, JPCS officially follows the Journal Articles Reporting Standards (JARS; Kofalt, 2018) which include clear guidelines for demographics reporting across all article types. However, this reporting does not appear to be enforced by the journal.
Out of 155 articles from the 2017–2020 time frame reviewed in CPS, 87 included at least one psychophysiology term, of which 36 were deemed ineligible, resulting in 51 articles for analysis. Among these, 38 (74.5%) included a description of sample race and/or ethnicity. Reporting of race and/or ethnicity in CPS appears relatively frequent, with a high likelihood of continuous improvement with the implementation of new authorship guidelines. Under new editorship in 2021, CPS began explicitly requiring reporting of participant demographics including race and ethnicity.
When viewed across psychophysiology measures, these early results suggest that the prevalence of racial/ethnic demographic reporting in clinical psychophysiology articles is beginning to increase but varies across journals and remains low in general. Given substantial variability in the number of psychophysiology articles per journal, differences in reporting rates between journals should be interpreted very cautiously. We speculate, however, that articles in a methods-focused journal such as Psychophysiology may more often focus on assumed “basic” or “universal” mechanisms and processes than articles in clinical psychology journals (i.e., JPCS, CPS) that may more often focus on clinically relevant mechanisms or applied processes that tend to be studied with greater consideration of the relevance of demographics such as racial or ethnic differences.
For those articles reporting racial and ethnic demographic data, we undertook informal analyses of the representativeness of their samples. Given our focus in this article on race and racism in the unique context of the United States (Ledgerwood et al., 2002), we restricted these analyses to U.S. samples. Such samples were identified based on the location of the Institutional Review Board of record, explicitly stated region of recruitment in the Method section, and location of author affiliations. These inclusion criteria resulted in inclusion ns of 147 articles from Psychophysiology, 56 from JCPS, and 33 from CPS. The demographics of these studies are depicted in Figures 1 through 3. In general, when demographics were reported, minoritized racial identities tended to be underrepresented compared to White participants. Of note, no article in any of the three journals reported phenotypic descriptions such as skin color, hair texture, etc., leading to a reliance on socially constructed categories of race.
The true representation of minoritized participants in research samples is likely to be even lower than these data suggest. There was a small proportion of articles reporting race and ethnicity; as such, these likely had a greater proportion of non-White populations than the broader literature (which often does not report racial demographics). It is possible that authors who report descriptions of race and ethnicity are more likely to recruit more diverse samples, and in many cases are conducting research specifically focused on demographic differences, thus necessarily increasing the diversity of their samples. The potential reasons for exclusion of minoritized participants may also vary by specific psychophysiology measure (see Supplemental Figures 1 – 3 for visualization of data for specific commonly used measures) and are discussed in greater depth below.
EEG: Recent Progress and Areas for Further Study
Of all clinical psychophysiology measures, issues of equity in EEG appear to have gained the most attention and, consequently, steps towards progress. For researchers collecting EEG data, the problem is clear: Current EEG equipment is not designed for participants with curly, tightly coiled, dense, or otherwise voluminous hair.
EEG measures neuronally generated electrical signals on the scalp. As currently designed, this technology depends on contact, between the electrode and scalp, either direct or through a conductive medium (e.g., saline gel); any impedance introduces noise into the signal and degrades data quality (Luck, 2014; see Choy et al., 2021). Protocols for applying EEG caps prescribe simply moving strands of hair aside (Farrens et al., 2020), but this step presumes the participant has thin, straight hair that can be easily moved away from the intended scalp location. Moreover, in clinical psychophysiology research, electrodes are typically embedded in a cloth cap, which imposes a further assumption that participants’ hair, when moved, will not push the cap so far away from the scalp as to impede scalp-electrode contact. Systems that rely on a chemical gel needed to bridge the scalp to the electrode require more gel for participants with curly, tightly coiled, dense or otherwise voluminous hair. Larger amounts of gel can be detrimental for higher density electrode montages (i.e., those with 64 channels and higher) as gel bridging between electrodes commonly produces signal artifacts. These technical limitations, based on manufacturer assumptions about participant hair, make scalp preparation for EEG more time-consuming, burdensome, and disruptive for individuals with curly, tightly coiled, dense, or voluminous hair.
For participants with these hair types, scalp preparation is sometimes terminated prematurely, but even when it is successfully completed, typical EEG equipment often produces noisy data for these individuals that is then excluded in post-processing (Choy et al., 2021; Etienne et al., 2020). When data are included from participants with curly, tightly coiled hair, signals are often attenuated due to these technical limitations, risking the illusion that their neural responses are blunted when compared to those with thinner, straighter hair (Etienne et al., 2020). Furthermore, some EEG researchers screen out potential participants with, for example, weaves, dreadlocks, or braids — all of which are typical hairstyles in the Black community — due to their perception that it will be difficult or impossible to secure the electrodes closely enough to the scalp to achieve an adequate level of contact (Choy et al., 2021). Importantly, curly, tightly coiled, dense, and voluminous hair is more prevalent among individuals of, for example, African, African American, and Caribbean ancestry (Loussouarn et al., 2007), who are more likely to be socially coded as Black. In these ways, such individuals are subject to not only phenotypic discrimination through the shortcomings of EEG equipment, but also the myriad ways racism influences psychological research in general (e.g., the pervasive provision of cultural explanations for behavior of non-White individuals in contrast to psychological explanations for White behavior; Causadias et al., 2018).
Despite these issues, which are obvious to many in the field, quantification of the magnitude of the problem with representation in EEG is sparse. Choy and colleagues (2021) conducted a “proof of concept” survey of EEG research articles across two months in 2019, finding that only 5 of 81 articles (6.2%) reported that their sample included Black participants, though it was not stated how many of these articles reported any demographic information at all. Recognizing the need for more data, the Biomechanics, Rehabilitation, and Interdisciplinary Neuroscience (BRaIN) Lab at the University of Central Florida designed a detailed assessment of current practices in the field as part of their EEG Hair Project. This ongoing survey, available for participation at https://hellobrainlab.com/research/eeg-hair-project/, asks EEG researchers and participants about their own identities, EEG research experience, and perceptions about the influence of hair and other factors on participation in EEG studies.
As of this writing, more than 200 researchers have responded, with half (~49%) reporting having recorded EEG data from fewer than five Black- or African American-identified participants and the next highest percentage (~13%) reporting having recorded data from only 6 to 10 such participants. A majority (~71%) reported having excluded fewer than five participants with curly, tightly coiled, dense, or voluminous hair, but ~3% acknowledged excluding over 50 such participants. These results, though highly preliminary, suggest that most researchers lack experience working with research participants with these hair types, and at least a small proportion of labs enroll but exclude them from analyses with regularity. These preliminary data suggest that the underrepresentation of Black participants across clinical EEG studies may be more attributable to initial under-recruitment than post-enrollment exclusion for data quality issues, at least in most labs.
The survey also asked about approaches to recording EEG from individuals with curly, tightly coiled, dense, or voluminous hair. Some researchers mentioned insightful solutions like flexible scheduling so data collection could occur just before salon appointments. Other responses highlighted the continuing demand for accessible solutions, with researchers noting that they “never found a solution” or simply “hope for the best” during data collection. Several respondents voiced an interest in specific training on collecting EEG from participants with often-excluded hair types.
Final results from the EEG Hair Project will deepen our understanding of the true magnitude of the problem, as well as details about where in the pipeline (e.g., recruitment, data retention) the exclusion occurs. In the meantime, some researchers have initiated efforts to address these issues. For example, in the first project of its kind, Etienne et al. (2020) developed electrode casings that preferentially work on curly, tightly coiled, and dense hair. Their “Sèvo” product resembles a hair barrette containing a traditional electrode; these clips are then secured between cornrows that are braided in alignment with traditional EEG electrode layouts. The clips specifically harness the quantity and thickness of curly, tightly coiled hair to stabilize the electrode against the scalp at the specified site, thus celebrating these textures and empowering participants. Early trials of these electrodes suggest that they increase electrode-to-scalp contact and improve data quality for individuals with curly, tightly coiled, dense, or otherwise voluminous hair; future research is needed to determine if such improvements extend to all hair types (Etienne et al., 2020; Kwasa et al., 2021).
Until such technology is refined and adopted by EEG hardware manufacturers, other practices can be implemented using existing equipment to obtain higher-quality data from participants with this hair type. For example, though presented in the context of hardware improvements, the braiding technique highlighted by Etienne et al. (2020) is a valuable approach to increase standard electrode contact. This technique does not interfere with the standardized placement of electrodes, but it adds ~15–20 minutes of preparation time, depending on the size of the head and the coarseness of the hair. Given that hair-braiding is a culturally familiar process, and that scape preparation is already often paired with other research tasks such as questionnaire completion, the relative costs of this extra time burden for some participants may be outweighed by the relative benefits of circumventing standard approaches could prevent them from participating. Still, any approach that may systemically add time or other burden to a specific group of participants should be carefully considered equity and research integrity perspectives. More detailed guidance for hair preparation based on specific hair types — with multidisciplinary input including a hair stylist with expertise in curly, tightly coiled hair — can be found in A Guide to Hair Preparation for EEG Studies (Richardson, et al., 2021).
New organizations such as Black in Neuro and SPARK Society are doing important work to raise awareness about systemic racism in brain sciences and empower researchers of color, including compiling educational and career resources online (blackinneuro.com; sparksociety.org). Black in Neuro also hosts an annual #BlackinNeuro Week comprising panels, webinars, and other events discussing the existing biases in neuroscience, celebrating and encouraging researchers of color, and providing a call to action for others in the field. These organizations form the foundation of a necessary and overdue paradigm shift in awareness of inequity in clinical psychophysiology and related fields.
EDA: Initial Stirrings and Room for Growth
As inequity in EEG research gains greater attention, thanks to the efforts of advocacy groups, bias within EDA measurements was largely ignored until very recently. EDA has historically been considered a “gold standard” psychophysiology measure of arousal and is often used to assess conditioned biological responses to a previously neutral stimulus that has been paired with an aversive stimulus (e.g., a mild electric shock; Fullana et al., 2020; Harnett et al., 2019; Kredlow et al., 2017; Rauch et al., 2012). These “fear learning” paradigms and associated fear extinction processes serve as laboratory models of fear and anxiety. This work establishes an empirical basis for clinical treatments such as prolonged exposure therapy for post-traumatic stress disorder (PTSD).
EDA involves administering small amounts of electrical current, usually to a participant’s hand, and measuring subtle changes in electrical impedance caused by variations in the sweat response that accompanies arousal. Detecting these impedance changes is difficult for multiple reasons, and participant data is often discarded due to what is deemed too small of a response (i.e., “non-responsiveness”). In addition, participants can be labeled “non-learners” when differences are hard to detect between their response to a conditioned stimulus and a neutral stimulus, also leading to discarded data.
We propose that instead of labeling these individuals as non-responders or non-learners, we interrogate the inherent biases in EDA measurement. In particular, individuals who identify as African American or Black can appear to have lower skin conductance levels and smaller conditioned responses than non-African American/Black individuals (Davis & Cowles, 1989; Janes et al., 1976; Johnson & Landon, 1965). As a result, Black participants are more likely than White participants to have their data discarded — something shown clearly in a review of fear conditioning samples (Kredlow et al., 2017). Unlike EEG, whether EDA signals for Black participants are smaller solely due to technological limitations or additional sources of bias is unclear. Early research identified phenotypic factors that could affect EDA measurement fidelity, including number of active sweat glands (Boucsein, 1992; Kawahata & Adams, 1961; cf. Thomson, 1954; Wesley & Maibach, 2003), thickness of the upper layer of the skin (Berardesca & Maibach, 2003; Johnson & Corah, 1963; Weigand et al., 1974), electrolyte content of sweat (Johnson & Landon, 1965), skin resistance (Johnson & Corah, 1963; Juniper & Dykman, 1967), and skin temperature (Thomson, 1954). The majority of these studies on phenotypic factors were conducted in an era when research commonly relied on arbitrary social categories of race rather than thoughtful experimental design accounting for phenotypic differences between individuals. Unwarranted assumptions about biological differences between races (i.e., racial essentialism) risk exacerbating harmful disparities, akin to the harms imposed by societal belief in phrenology and eugenics. For example, Black individuals receive less treatment for pain because of erroneous assumptions about a shared racial biology that confers higher pain tolerance than White individuals possess (Hoffman et al., 2016).
Thus far, phenotypic factors have not been clearly demonstrated to account for racial differences in EDA. If they do, EDA technology should be made more robust to such phenotypic variation. Until then, skin conductance data must be interpreted thoughtfully, accounting for all possible contributors to differences (e.g., Carter et al., 2021; Harnett et al., 2019). Although the harmful implications of discarding individuals’ EDA data have been touched upon previously (Lonsdorf et al., 2019), direct and clear attention to this equity issue has come only very recently (Webb et al., 2022).
Other Measures and New Technology: A Caution About the Future of Clinical Psychophysiology
Though EEG and EDA provide compelling and accessible examples of how psychophysiological approaches can lack inclusivity, especially for Black individuals, such problems extend beyond these measures and demographics. For example, the eye-blink startle response measured with electromyography (EMG) is a translational measure widely used in studies touting direct clinical implications (Braff, 2010; Grillon & Baas, 2003), particularly in testing psychopharmacological therapeutics (Grillon & Ernst, 2020; Kaye et al., 2017). As with EDA, it is common practice to exclude participants with “small” general startle reactivity at baseline, often using arbitrary criteria, as smaller or harder-to-detect signals are associated with noisier data (Blumenthal et al., 2005; Bradford et al., 2014, 2015). As recent studies suggest that individuals identifying as Hispanic, Asian, or Black exhibit decreased general startle reactivity compared to White participants (Correa et al., 2021; Hasenkamp et al., 2008; Nelson et al., 2014), future work must ensure that those with marginalized social identities and/or phenotypic characteristics are not disproportionately excluded.
As psychophysiological technology advances, our field is at risk of magnifying bias embedded in these systems. Particularly worrisome is the rapidly advancing field of biomedical optics, which leverages the scattering and absorption properties of light within human tissue to infer underlying anatomy and function. Measurements by biomedical optical devices are influenced by the concentration of melanin (Mustafa et al., 2017; Sardar et al., 2001), the light-absorbing chromophore that gives skin its pigment. Thus far, optical studies do not typically report skin color and often use small samples of exclusively light-skinned participants. This technical limitation may skew interpretation of data from participants with darker skin, and the resulting issues of equity have not yet been discussed.
In one example of the use of optical technologies in clinical psychophysiological research, increasing interest in measuring psychophysiology outside of the lab has led to the adoption of consumer-facing mobile devices for research purposes. Commonly used heart rate sensors, such as “fitness trackers” and “smart watches,” rely on light-based technology that is not currently optimized for darker pigmented (melanated) skin. These embedded biases have been highlighted multiple times in the popular press (Krisch & Schwartz, 2015; Rabin, 2020; Tayag, 2020) but are only just beginning to be taken seriously by researchers (e.g., Shcherbina et al., 2017) and industry.
Just as mobile heart rate monitoring brings potential for increased bias, so do other optical technologies designed to be more affordable alternatives to their research-grade counterparts. For example, functional near-infrared spectroscopy (fNIRS) has been touted as a portable and affordable alternative to functional magnetic resonance imaging (fMRI). However, it has been known by NIRS experts for years that the technology does not work as well on darker skin (Wassenaar & Van den Brand., 2005). In addition, fNIRS requires good scalp contact, similar to EEG, but the suitability of current designs for diverse hair types has not been adequately discussed. It is an open secret in the field that fNIRS works best on fair skin, and thin, blond (unpigmented) hair. In response, Meta Reality Labs recently funded six research groups to develop inclusive optical and other psychophysiology technology (Meta Research, 2021).
Interpreting Demographic Differences in Clinical Psychophysiological Research
Thus far, we have largely focused on how psychophysiological technology is not currently optimized for phenotypic variations that map onto minoritized racial and ethnic groups. These technical limitations often lead to discriminatory exclusion of data from individuals with already marginalized identities. In the relatively rare cases when samples contain adequate representation of phenotypic and identity-based diversity, some differences have been demonstrated between racial groups. For example, as noted above, a blunted startle response has been observed for Black participants relative to White participants in some studies (e.g., Hasenkamp et al., 2008). Findings of this kind could be misinterpreted as reflecting true biological differences between racial groups, thus (erroneously) reifying the notion that race is physical. This is especially likely because of the privileged nature of psychophysiological findings, which are commonly viewed as more objective than other psychological research (Gatzke-Kopp, 2016; Weisberg et al., 2008). However, race is a social construction and must be differentiated from the phenotypic variations that only partially overlap with perceived racial categories (APA, 2021b). We have discussed how observed psychophysiological differences among racial groups (e.g., Black versus White) could be attributable, at least in part, to limitations of psychophysiological technologies when working with phenotypic characteristics that are often observed in a given racial/ethnic group (e.g., dense, voluminous, curly hair versus thin, straight hair). However, it is crucial not to dismiss all observed differences as spurious consequences of technical limitations. Other factors, such as lived experience of racial discrimination, are likely to contribute to real differences in psychophysiology across identity groups, in tandem with these phenotypic influences.
Lessons for how to conceptualize these issues in clinical psychophysiology can be learned from cultural neuroscience. This field emerged in response to the presumed universality of the relationships among brain and behavior, regardless of cultural identity, in most neuroscience research (Chiao & Ambady, 2007). Importantly, cultural neuroscience is concerned with the interactional and multilevel influences of nuanced sociocultural and phenotypic factors. Cultural neuroscience was founded with ideas reminiscent of intersectionality (Crenshaw, 1989), a framework that “approaches conceptualizing the human experience through understanding multiple social identities and how they function in contextualized systems of inequality” (Grzanka, 2020, p. 249).
Cultural neuroscience provides a medium for interpreting racial and ethnic differences in psychophysiology. The body is intricately intertwined with other facets of human psychology, such that lived experience influences physiological functions. For example, minority stress has downstream impacts on stress reactivity (Forrester et al., 2019; Huebner et al., 2021; Ruiz et al., 2018). Language differences are also associated with brain structure and function (see Kim & Sasaki, 2014). Further, these social factors can interact with genetic differences — which contribute to phenotypic characteristics rather than explicitly to social categories of race — to produce observed physiological variability (Sasaki & Kim, 2017). Disentangling the influence of factors such as lived experience, language, and culture from the limitations of current psychophysiological measures is immensely challenging and will depend, in large part, on improvements in psychological science broadly.
In the meantime, one step may be to conduct post-hoc analyses to test whether demographics account for variance in psychophysiological responses (Webb et al., 2022), but making such inferences is impossible without adequate representation of each demographic in such samples. Even with adequate representation, psychophysiology studies must continue to increase their typical sample sizes, which are often statistically underpowered for the detection of even medium-sized focal effects — much less the post-hoc assessment of potentially small demographic differences (Correa et al., 2021). Another potential approach is to exclude as little data as possible by including data from participants with even the smallest signals. Researchers could then include participants’ general or baseline response as a covariate in statistical analysis to account for increased noise caused by shortcomings of the equipment (Bradford et al., 2014, 2015). However, researchers must be careful when attempting to “control for”‘ differences they believe are caused by bias in psychophysiological equipment, as doing so may inadvertently parse out meaningful demographic variance of interest if it correlates with nuisance variance caused by equipment bias (Miller & Chapman, 2001). Finally, another approach to disentangling demographic differences attributable to technical issues with diverse phenotypes versus cultural differences of interest is to include multiple measures of social identity and lived experience. These decisions should be made in accordance with theory (see, e.g., Mereish & Miranda, 2021). For example, if differences in EEG between Black and White participants are theorized to reflect minority stress, the study should explicitly measure minority stress as well as key covariates such as self-reported hair texture, rather than relying on a single racial categorization as a proxy for both these potential mechanisms of physiological difference. Clearly, addressing these issues will require continued methodological and statistical work from a variety of stakeholders prioritizing social justice appropriately.
Broad Recommendations for Researchers Using Psychophysiology
Above, we suggested approaches to reduce inequity in EEG and EDA research. Below is a list of broad recommendations that cut across measures. We recognize that inequity in clinical psychophysiology is systemic, and addressing it will require a “top-down” approach with buy-in and action from powerful institutions (e.g., government agencies, funders, university departments). The authors of this article wholeheartedly support the many thoughtful appeals previously made to those with the most power, including calls to address racial disparities in grant funding and earmark funding for equity-focused initiatives (Harnett & Ressler, 2021; Settles et al., 2020). At the same time, many readers of this article will not possess the institutional power to implement such suggestions. Accordingly, we provide actionable recommendations for researchers currently conducting or starting clinical psychophysiological research. These recommendations have the potential to improve inclusiveness by increasing the fidelity of research with not only Black participants, but also a range of others who differ from White individuals in terms of skin color and hair texture (e.g., Latine, South Asian, etc).
1. Review your lab’s current practices.
Recent public and scientific movements have provided a “conversation starter” to identify and address inequities in science. Practically speaking, clinical psychophysiological data collection is slow-moving or even paused due to the ongoing COVID-19 pandemic. These circumstances provide an opportunity for reflection and planning. Recommendations and resources highlighted above and below can provide a starting point. We acknowledge that adjusting recruitment and data collection procedures to increase inclusivity requires substantial time and effort; this undertaking can and should be reported to evaluators as a valuable project during data collection downtime. As funding agencies and academic institutions continue to publicly reinforce their stated commitments to diversity, equity, and inclusion, researchers must remind them to acknowledge (i.e., “count” and potentially reward) this valuable work. Once lab-level policies have been reformed, they should be revisited periodically as best practices evolve.
2. Be transparent in reporting of sample demographics and exclusions.
As attention to diversity in clinical psychophysiology samples grows, researchers may feel hesitant to highlight the lack of diversity in their studies, and even more so to report that they disproportionately excluded individuals based on phenotypic characteristics. As outlined above, significant barriers prevent researchers from collecting adequately representative samples in clinical psychophysiology studies, and unfortunately, lack of diversity is still the norm (Rad et al., 2018). The demographics of final samples and excluded individuals must be reported transparently to aid efforts to quantify the magnitude of these problems and further justify (re)direction of resources towards their solutions. These efforts may be best aided if researchers collect and report not only self-reported race and ethnicity but also phenotypic characteristics such as skin color and hair type which may be more directly tied to the shortcomings of current psychophysiological approaches (e.g., Monk, 2015). Reforms such as fully online journals and exclusion of methods sections from word counts further facilitate the thorough description of sample characteristics. For example, Clinical Psychological Science now requires detailed reporting of participant demographics, or acknowledgment of a lack of such detail as a weakness, consistent with the journal’s designation of diversity and representation as a priority area (Drew, 2020).
3. Bring typically excluded stakeholders to the table.
Consistent with well-established but chronically underfunded approaches such as community-based participatory research (Chen et al., 2012; Ciccarella et al., 2018; Sandoval et al., 2012; Wallerstein & Duran, 2008), researchers can engage stakeholders with diverse demographics characteristics and various lived experiences allowing cultural translation through the expertise of native speakers and community partners. This will help ensure equity in all aspects of a research project. For example, researchers can organize focus groups with Black women to identify potential barriers to participation in EEG research and co-develop solutions. From information gathered during these focus groups, researchers might modify, for example, recruitment and study materials to use more inclusive and equitable content and language that address concerns about how EEG may affect hair or create an inconvenience, especially for individuals with hairstyles that require significant time and financial investment. For instance, recruitment materials might state that the hair gel is water-soluble or, if using dry electrodes, specify that study participation does not involve the use of hair gel. Researchers might also modify their recruitment procedures, such as explicitly offering flexible scheduling to accommodate participants’ individual haircare routines or wash cycles.
Data collection for measures such as EEG can be aided by partnerships with local hair stylists who have expertise in specific hair types. Such partnerships can be facilitated by recruiting trainees with existing connections to their local communities. For example, the BRaIN Lab recruited a local Black hair expert only after successfully recruiting a Black graduate student who inquired with their local network of natural-haired individuals. For researchers privileged enough to be in such a position, start-up or other funds could be earmarked for building these partnerships. Social media (e.g., Twitter; open-membership academic Slack groups) also facilitates connections among typically siloed groups and disciplines. In addition to directly improving representativeness and sociodemographic nuance in ongoing research, these practices would help to address the lack of diversity in authorship of published papers in psychology (Nunes, 2021).
4. Leverage the unique consumer power held by psychophysiology researchers to encourage inclusive change in hardware.
Psychophysiology equipment is highly specialized, and manufacturers are exceptionally responsive to the requests of their small user bases. As a result, researchers have unique leverage to change problematic technical norms in clinical psychophysiology. Authors of this paper have personal experience with their mentors or colleagues requesting modifications to psychophysiology hardware to suit their lab’s specific needs (e.g., the addition of a new cable connection), with these changes implemented in the product’s next standard iteration. Similarly, clinical psychophysiology researchers can advocate for the design and production of new equipment that addresses the pitfalls of current technology outlined above. With the continuing development of methods that ignore diversity in skin color and hair texture, phenotypic discrimination has the potential to become even more severe going forward if these limitations go unaddressed. Researchers must assert abandoning “color-blind” approaches in engineering psychophysiological equipment and hold manufacturers accountable as new technologies emerge.
5. Support existing efforts to improve clinical psychophysiology.
As highlighted above, organizations such as Black In Neuro and SPARK Society are making great strides in increasing awareness of representation issues in clinical psychophysiology for both the general public and scientific communities. Interested researchers can contribute to such societies by joining and/or donating money and resources. Researchers can also participate in efforts such as the EEG Hair Project survey to aid in quantification and understanding of recruitment and exclusion practices. Aside from providing their own insight, one low-cost — but potentially high-impact — way for researchers to support these efforts is to share them in their circles through social media and laboratory or department websites.
Support can also occur at a more local level. While much has been written about the need to recruit scholars with marginalized identities (McCormick-Huhn et al., 2019), there has been less discussion about providing the continued support and systemic restructuring needed to retain those individuals in science (Settles et al., 2020; De Los Reyes & Uddin, 2021). Researchers can work to support these individuals — even when they do not know them personally — by centering and elevating their voices in research (Sukhera & Palaniyappan, 2021). It is also important to adopt and encourage intersectional thinking while combating systemic biases stacked against marginalized researchers and their disciplines (Settles et al., 2020). Although these suggestions are not specific to clinical psychophysiology, the relative specialization of this discipline facilitates awareness of new research by junior scholars with marginalized identities, as well as the ability to network at relevant conferences. Finally, even if a researcher does not independently study issues of marginalization as a core content area, they can offer expertise in a given psychophysiological approach, quantitative modeling, or other specialized areas to such projects, thus contributing to the evolution of the field in a more equitable direction (Uddin & De Los Reyes, 2021).
Concluding Remarks
Clinical psychophysiological research holds great promise for refining assessment, identifying risk factors, and informing treatment. Despite continually increasing adoption of, and enthusiasm for, this approach, critical issues of representation and equity have been neglected. Consequently, the potential for this research to inform psychological interventions that decrease disparities and increase equity in mental health is lost. As anti-racism campaigns for systemic change slowly gain traction, researchers can take steps to increase inclusivity both immediately and over the long term and, in doing so, help ensure a more equitable future for clinical psychophysiology. Stated succinctly, clinical psychological science is at an inflection point: “The time to reimagine our discipline is now” (Ledgerwood et al., 2022, Introduction section, para 7).
Supplementary Material
Figure 2.
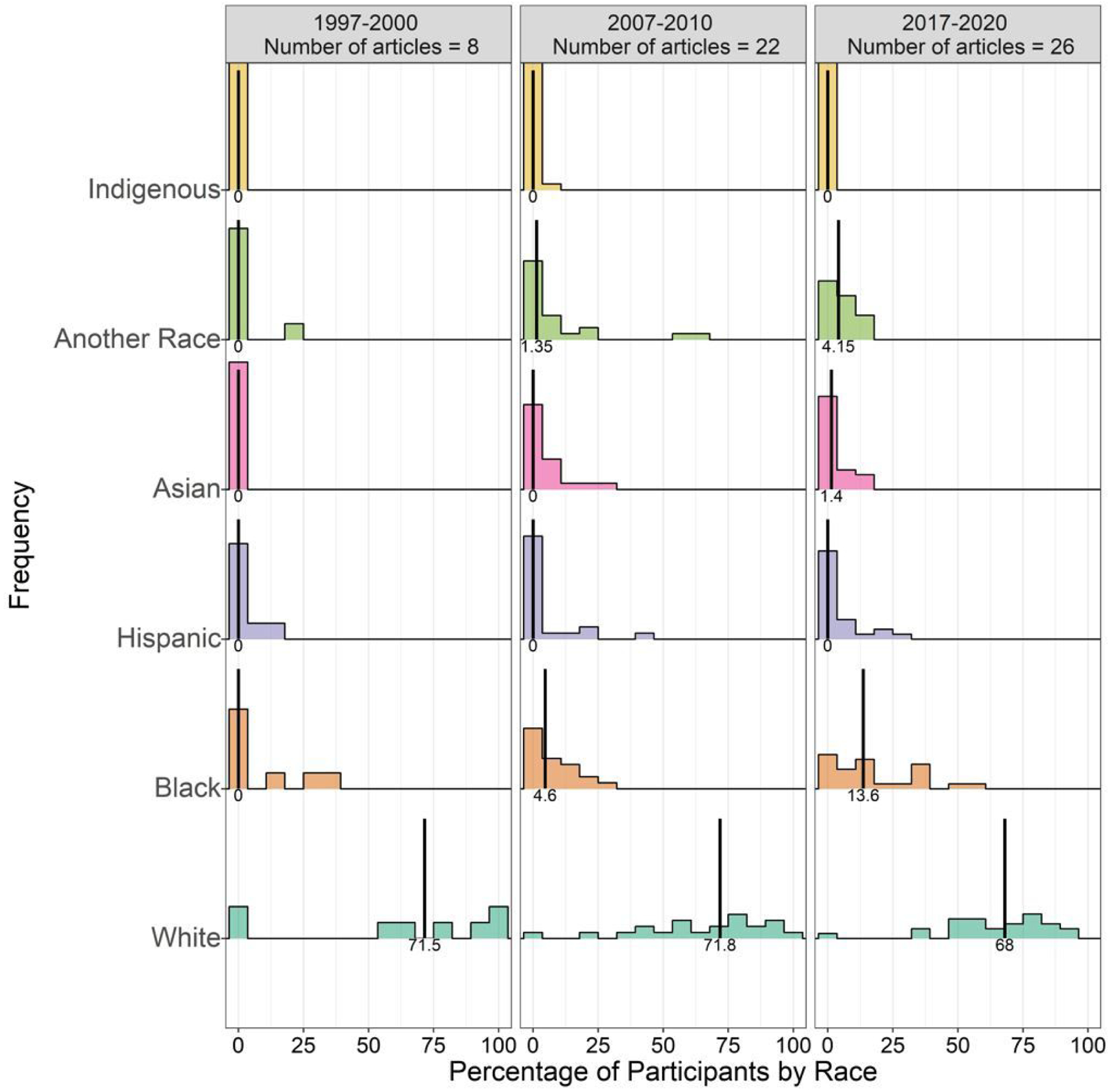
Participant demographics among the 50.4% of Journal of Psychopathology and Clinical Science (JPCS; formerly Journal of Abnormal Psychology) articles that reported sample race and ethnicity.
Vertical black lines refer to the median percentage of each race/ethnicity across included articles. Of note, medians are presented due to the clear overdispersion of percentage of races and ethnicities; medians will often not sum to 100%. ‘Another Race’ includes all races not included in the listed categories, including biracial/multiracial individuals.
Acknowledgments
The authors acknowledge Justin Thomas, Harley Beach, and Danielle Jones at Florida State University and Jackson Cutler, Lindsay Beaman, Nico Doran and Mia Tognoli at Oregon State University for their help collecting literature review data. The authors acknowledge E. K. Webb for early conceptual input and helpful comments on an initial draft. This project was partially supported by NIH 5R01AG054621-05 to HJH, F31MH122096 to ERP, and F99 NS115331 to JK.
References
- American Psychological Association. (2021a). APA resolution on harnessing psychology to combat racism: Adopting a uniform definition and understanding. https://www.apa.org/about/policy/resolution-combat-racism.pdf
- American Psychological Association. (2021b). Inclusive language guidelines. https://www.apa.org/about/apa/equity-diversity-inclusion/language-guidelines.pdf
- Berardesca E, & Maibach H (2003). Ethnic skin: Overview of structure and function. Journal of the American Academy of Dermatology, 48(6, Supplement), S139–S142. 10.1067/mjd.2003.273 [DOI] [PubMed] [Google Scholar]
- Blumenthal TD, Cuthbert BN, Filion DL, Hackley S, Lipp OV, & Van Boxtel A (2005). Committee report: Guidelines for human startle eyeblink electromyographic studies. Psychophysiology, 42(1), 1–15. 10.1111/j.1469-8986.2005.00271.x [DOI] [PubMed] [Google Scholar]
- Bradford DE, Kaye JT, & Curtin JJ (2014). Not just noise: Individual differences in general startle reactivity predict startle response to uncertain and certain threat. Psychophysiology, 51(5), 407–411. 10.1111/psyp.12193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradford DE, Starr MJ, Shackman AJ, & Curtin JJ (2015). Empirically based comparisons of the reliability and validity of common quantification approaches for eyeblink startle potentiation in humans. Psychophysiology, 52(12), 1669–1681. 10.1111/psyp.12545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braff DL (2010). Prepulse inhibition of the startle reflex: A window on the brain in schizophrenia. In Swerdlow NR (Ed.), Behavioral Neurobiology of Schizophrenia and Its Treatment (pp. 349–371). Springer. 10.1007/7854_2010_61 [DOI] [PubMed] [Google Scholar]
- Boucsein W (1992). Electrodermal activity. Springer US. 10.1007/978-1-4614-1126-0 [DOI] [Google Scholar]
- Carter SE, Gibbons FX, & Beach SRH (2021). Measuring the biological embedding of racial trauma among Black Americans utilizing the RDoC approach. Development and Psychopathology, 33(5), 1849–1863. 10.1017/S0954579421001073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Causadias JM, Vitriol JA, & Atkin AL (2018). Do we overemphasize the role of culture in the behavior of racial/ethnic minorities? Evidence of a cultural (mis)attribution bias in American psychology. American Psychologist, 73(3), 243–255. 10.1037/amp0000099 [DOI] [PubMed] [Google Scholar]
- Chiao JY, & Ambady N (2007). Cultural neuroscience: Parsing universality and diversity across levels of analysis. In Kitayama S & Cohen D (Eds.), Handbook of cultural psychology (pp. 237–254). The Guilford Press. [Google Scholar]
- Chen Y-W, Milstein T, Anguiano C, Sandoval J, & Knudsen L (2012). Challenges and benefits of community-based participatory research for environmental justice: A case of collaboratively examining ecocultural struggles. Environmental Communication, 6(3), 403–421. 10.1080/17524032.2012.698291 [DOI] [Google Scholar]
- Choy T, Baker E, & Stavropoulos K (2021). Systemic racism in EEG research: Considerations and potential solutions. Affective Science. 10.1007/s42761-021-00050-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarella A, Staley AC, & Franco AT (2018). Transforming research: Engaging patient advocates at all stages of cancer research. Annals of Translational Medicine, 6(9), 167. 10.21037/atm.2018.04.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw K (1989). Demarginalizing the intersection of race and sex: A Black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum, 1989, Article 8. [Google Scholar]
- Correa KA, Carrillo V, Funkhouser CJ, Shenberger ER, & Shankman SA (2021). Ethnic differences in behavioral and physiological indicators of sensitivity to threat. Journal of Anxiety Disorders, 85, 102508. 10.1016/j.janxdis.2021.102508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis C, & Cowles M (1989). Some sources of variance in skin conductance. Canadian Journal of Psychology, 43(1), 97–103. 10.1037/h0084211 [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, & Uddin LQ (2021). Revising evaluation metrics for graduate admissions and faculty advancement to dismantle privilege. Nature Neuroscience, 24, 755–758. 10.1038/s41593-021-00836-2 [DOI] [PubMed] [Google Scholar]
- Donati FL, D’Agostino A, & Ferrarelli F (2020). Neurocognitive and neurophysiological endophenotypes in schizophrenia: An overview. Biomarkers in Neuropsychiatry, 3, 100017. 10.1016/j.bionps.2020.100017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drew A (2020, October 29). New Clinical Psychological Science editor vows to reflect “incredibly diverse field.” APS Observer. https://www.psychologicalscience.org/observer/new-clinical-psychological-science-editor-vows-to-reflect-incredibly-diverse-field
- Etienne A, Laroia T, Weigle H, Afelin A, Kelly SK, Krishnan A, & Grover P (2020). Novel electrodes for reliable EEG recordings on coarse and curly hair [Preprint]. Bioengineering. 10.1101/2020.02.26.965202 [DOI] [PubMed] [Google Scholar]
- Farrens JL, Simmons AM, Luck SJ, & Kappenman ES (2020). Electroencephalogram (EEG) recording protocol for cognitive and affective human neuroscience research [Preprint]. Protocol Exchange. 10.21203/rs.2.18328/v2 [DOI]
- Fisher JA, & Kalbaugh CA (2011). Challenging assumptions about minority participation in U.S. clinical research. American Journal of Public Health, 101(12), 2217–2222. 10.2105/AJPH.2011.300279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrester SN, Gallo JJ, Whitfield KE, & Thorpe RJ (2019). A framework of minority stress: From physiological manifestations to cognitive outcomes. The Gerontologist, 59(6), 1017–1023. 10.1093/geront/gny104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fullana MA, Dunsmoor JE, Schruers KRJ, Savage HS, Bach DR, & Harrison BJ (2020). Human fear conditioning: From neuroscience to the clinic. Behaviour Research and Therapy, 124, 103538. 10.1016/j.brat.2019.103528 [DOI] [PubMed] [Google Scholar]
- Gatzke-Kopp LM (2016). Diversity and representation: Key issues for psychophysiological science. Psychophysiology, 53(1), 3–13. 10.1111/psyp.12566 [DOI] [PubMed] [Google Scholar]
- George S, Duran N, & Norris K (2014). A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. American Journal of Public Health, 104: 316._e31 10.2105/AJPH.2013.301706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grillon C, & Baas J (2003). A review of the modulation of the startle reflex by affective states and its application in psychiatry. Clinical Neurophysiology, 114(9), 1557–1579. 10.1016/S1388-2457(03)00202-5 [DOI] [PubMed] [Google Scholar]
- Grillon C, & Ernst M (2020). A way forward for anxiolytic drug development: Testing candidate anxiolytics with anxiety-potentiated startle in healthy humans. Neuroscience and Biobehavioral Reviews, 119, 348–354. 10.1016/j.neubiorev.2020.09.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grzanka PR (2020). From buzzword to critical psychology: An invitation to take intersectionality seriously. Women & Therapy, 43(3–4), 244–261. [Google Scholar]
- Hajcak G, & Patrick CJ (2015). Situating psychophysiological science within the Research Domain Criteria (RDoC) framework. International Journal of Psychophysiology, 98(2, Part 2), 223–226. 10.1016/j.ijpsycho.2015.11.001 [DOI] [PubMed] [Google Scholar]
- Hajcak G, Klawohn J, & Meyer A (2019). The utility of event-related potentials in clinical psychology. Annual Review of Clinical Psychology, 15(1), 71–95. 10.1146/annurev-clinpsy-050718-095457 [DOI] [PubMed] [Google Scholar]
- Harnett NG, Wheelock MD, Wood KH, Goodman AM, Mrug S, Elliott MN, Schuster MA, Tortolero S, & Knight DC (2019). Negative life experiences contribute to racial differences in the neural response to threat. NeuroImage, 202, 116086. 10.1016/j.neuroimage.2019.116086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harnett NG, & Ressler KJ (2021). Structural racism as a proximal cause for race-related differences in psychiatric disorders. American Journal of Psychiatry, 178(7), 579–581. 10.1176/appi.ajp.2021.21050486 [DOI] [PubMed] [Google Scholar]
- Hasenkamp W, Norrholm SD, Green A, Lewison B, Boshoven W, Keyes M, & Duncan E (2008). Differences in startle reflex and prepulse inhibition in European-Americans and African-Americans. Psychophysiology, 45(5), 876–882. 10.1111/j.1469-8986.2008.00680.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslam N, Vylomova E, Murphy SC, & Wilson SJ (2021). The neuroscientification of psychology: The rising prevalence of neuroscientific concepts in psychology from 1965 to 2016. Perspectives on Psychological Science [advance online e-publication]. 10.1177/1745691621991864 [DOI] [PubMed] [Google Scholar]
- Helms JE (1993). I also said, “White racial identity influences White researchers.” The Counseling Psychologist, 21(2), 240–243. 10.1177/0011000093212007 [DOI] [Google Scholar]
- Helms JE, Henze KT, Mascher J, & Satiani A (2006). Ethical issues when White researchers study ALANA and immigrant people and communities. In Trimble J & Fisher C (Eds.), The handbook of ethical research with ethnocultural populations & communities (pp. 300–324). SAGE Publications, Inc. 10.4135/9781412986168.n16 [DOI] [Google Scholar]
- Hoffman KM, Trawalter S, Axt JR, & Oliver MN (2016). Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proceedings of the National Academy of Sciences, 113(16), 4296–4301. 10.1073/pnas.1516047113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huebner DM, McGarrity LA, Perry NS, Spivey LA, & Smith TW (2021). Cardiovascular and cortisol responses to experimentally-induced minority stress. Health Psychology, 40(5), 316–325. 10.1037/hea0001067 [DOI] [PubMed] [Google Scholar]
- Insel TR (2015). The NIMH experimental medicine initiative. World Psychiatry, 14(2), 151–153. 10.1002/wps.20227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janes CL, Worland J, & Stern JA (1976). Skin potential and vasomotor responsiveness of black and white children. Psychophysiology, 13(6), 523–527. 10.1111/j.1469-8986.1976.tb00873.x [DOI] [PubMed] [Google Scholar]
- Jones BE, & Gray BA (1986). Problems in diagnosing schizophrenia and affective disorders among Blacks. Psychiatric Services, 37(1), 61–65. 10.1176/ps.37.1.61 [DOI] [PubMed] [Google Scholar]
- Johnson LC, & Landon M (1965). Eccrine sweat gland activity and racial differences in resting skin conductance. Psychophysiology, 1(4), 322–329. 10.1111/J.1469-8986.1965.TB03264.X [DOI] [PubMed] [Google Scholar]
- Johnson LC, & Corah NL (1963). Racial differences in skin resistance. Science, 139(3556), 766–767. 10.1126/science.139.3556.766 [DOI] [PubMed] [Google Scholar]
- Juniper K, & Dykman RA (1967). Skin resistance, sweat-gland counts, salivary flow, and gastric secretion: Age, race, and sex differences, and intercorrelations. Psychophysiology, 4(2), 216–222. 10.1111/j.1469-8986.1967.tb02759.x [DOI] [PubMed] [Google Scholar]
- Kawahata A, & Adams T (1961). Racial Variations in Sweat Gland Distribution. Proceedings of the Society for Experimental Biology and Medicine, 106(4), 862–865. 10.3181/00379727-106-26501 [DOI] [PubMed] [Google Scholar]
- Kaye JT, Bradford DE, & Curtin JJ (2016). Psychometric properties of startle and corrugator response in NPU, affective picture viewing, and resting state tasks. Psychophysiology, 53(8), 1241–1255. 10.1111/psyp.12663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye JT, Bradford DE, Magruder KP, & Curtin JJ (2017). Probing for neuroadaptations to unpredictable stressors in addiction: Translational methods and emerging evidence. Journal of Studies on Alcohol and Drugs, 78(3), 353–371. 10.15288/jsad.2017.78.353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy BR, Mathis CC, & Woods AK (2007). African Americans and their distrust of the health care system: Healthcare for diverse populations. Journal of Cultural Diversity, 14(2), 56–60. [PubMed] [Google Scholar]
- Kim HS, & Sasaki JY (2014). Cultural neuroscience: Biology of the mind in cultural contexts. Annual Review of Psychology, 65(1), 487–514. 10.1146/annurev-psych-010213-115040 [DOI] [PubMed] [Google Scholar]
- Kofalt D (2018, May 14). The Updated APA Style JARS: Advancing Psychological Research. The APA Style Blog. https://blog.apastyle.org/apastyle/2018/05/the-updated-apa-style-jars-advancing-psychological-research.html
- Kredlow MA, Pineles SL, Inslicht SS, Marin M-F, Milad MR, Otto MW, & Orr SP (2017). Assessment of skin conductance in African American and Non-African American participants in studies of conditioned fear. Psychophysiology, 54(11), 1741–1754. 10.1111/psyp.12909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krisch JA, & Schwartz O (2015, April 29). Science explains why tattoos and dark skin may foil Apple Watch. Vocativ. https://www.vocativ.com/culture/health-culture/tattoos-apple-watch-dark-skin/index.html [Google Scholar]
- Kwasa J, Etienne A, Mensah-Agyekum E, Weigle H, Marmer V, Kelly S, Patterson C, & Grover P (2021, December 3-7). Clinical evaluation of Sèvo systems: Equitable EEG for coarse, curly hair [Poster presentation abstract]. American Epilepsy Society 75th Annual Meeting 2021, Chicago, IL. https://www.aesnet.org/abstractslisting/clinical-evaluation-of-sevo-systems--equitable-eeg-for-coarse--curly-hair [Google Scholar]
- Ledgerwood A, Hudson STJ, Lewis NA, Maddox KB, Pickett CL, Remedios JD, Cheryan S, Diekman AB, Dutra NB, Goh JX, Goodwin SA, Munakata Y, Navarro DJ, Onyeador IN, Srivastava S, & Wilkins CL (2022). The Pandemic as a Portal: Reimagining Psychological Science as Truly Open and Inclusive. Perspectives on Psychological Science. 10.1177/17456916211036654 [DOI] [PubMed] [Google Scholar]
- Li W, Mao Z, Bo Q, Sun Y, Wang Z, & Wang C (2021). Pre-pulse inhibition deficits in individuals at clinical high-risk for psychosis: A systematic review and meta-analysis. Early Intervention in Psychiatry, 15(4), 794–806. 10.1111/eip.13015 [DOI] [PubMed] [Google Scholar]
- Lonsdorf TB, Klingelhöfer-Jens M, Andreatta M, Beckers T, Chalkia A, Gerlicher A, Jentsch VL, Meir Drexler S, Mertens G, Richter J, Sjouwerman R, Wendt J, & Merz CJ (2019). Navigating the garden of forking paths for data exclusions in fear conditioning research. Elife, 8, e52465. 10.7554/eLife.52465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loussouarn G, Garcel A-L, Lozano I, Collaudin C, Porter C, Panhard S, Saint-Léger D, & De La Mettrie R (2007). Worldwide diversity of hair curliness: A new method of assessment. International Journal of Dermatology, 46(s1), 2–6. 10.1111/j.1365-4632.2007.03453.x [DOI] [PubMed] [Google Scholar]
- Luck SJ (2014). An introduction to the event-related potential technique (2nd ed.). MIT Press. [Google Scholar]
- Martinez Emily L. [@_EmilyLMartinez]. (2021, November 2). This is such an important effort, especially for #schizophrenia #EEG researchers (using methods that can systematically exclude data from people of color, in order to study brain processes in a disorder that disproportionately affects these same groups)… We must do better! [Tweet]. Twitter. https://twitter.com/_emilylmartinez/status/1455577081761333249
- McCormick-Huhn K, Warner LR, Settles IH, & Shields SA (2019). What if psychology took intersectionality seriously? Changing how psychologists think about participants. Psychology of Women Quarterly. Advance online publication. 10.1177/0361684319866430 [DOI] [Google Scholar]
- Mereish EH, & Miranda R (2021). A preliminary experimental study of minority stress, startle reactivity, and alcohol use among heavy drinking sexual minority young adults. Substance Use & Misuse, 56(1), 162–168. 10.1080/10826084.2020.1846197 [DOI] [PubMed] [Google Scholar]
- Meta Research (2021, September 13). Announcing the winners of the 2021 Engineering Approaches to Responsible Neural Interface Design request for proposals. Meta Research. https://research.facebook.com/blog/2021/09/announcing-the-winners-of-the-2021-engineering-approaches-to-responsible-neural-interface-design-request-for-proposals/ [Google Scholar]
- Miller GA, & Chapman JP (2001). Misunderstanding analysis of covariance. Journal of Abnormal Psychology, 110(1), 40–48. 10.1037//0021-843x.110.1.40 [DOI] [PubMed] [Google Scholar]
- Monk EP (2015). The Cost of Color: Skin Color, Discrimination, and Health among African-Americans. American Journal of Sociology, 121(2), 396–444. 10.1086/682162 [DOI] [PubMed] [Google Scholar]
- Mustafa FH, Jones PW, & McEwan AL (2017). Near infrared spectroscopy for body fat sensing in neonates: Quantitative analysis by GAMOS simulations. BioMedical Engineering OnLine, 16(1), 14. 10.1186/s12938-016-0310-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson BD, Bishop JR, Sarapas C, Kittles RA, & Shankman SA (2014). Asians demonstrate reduced sensitivity to unpredictable threat: A preliminary startle investigation using genetic ancestry in a multi-ethnic sample. Emotion, 14(3), 615–623. 10.1037/a0035776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunes L (2021, January 6). Turning the page: Race in research and publishing. APS Observer. https://www.psychologicalscience.org/observer/turning-the-page
- Olbert CM, Nagendra A, & Buck B (2018). Meta-analysis of Black vs. White racial disparity in schizophrenia diagnosis in the United States: Do structured assessments attenuate racial disparities? Journal of Abnormal Psychology, 127(1), 104–115. 10.1037/abn0000309 [DOI] [PubMed] [Google Scholar]
- Patrick CJ, & Hajcak G (2016). Reshaping clinical science: Introduction to the special issue on psychophysiology and the NIMH Research Domain Criteria (RDoC) initiative. Psychophysiology, 53(3), 281–285. 10.1111/psyp.12613 [DOI] [PubMed] [Google Scholar]
- Rabin RC (2020, December 22). Pulse oximeter devices have higher error rate in Black patients. The New York Times. https://www.nytimes.com/2020/12/22/health/oximeters-covid-black-patients.html [Google Scholar]
- Rad MS, Martingano AJ, & Ginges J (2018). Toward a psychology of Homo sapiens: Making psychological science more representative of the human population. Proceedings of the National Academy of Sciences, 115(45), 11401–11405. 10.1073/pnas.1721165115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauch SA, Eftekhari A, & Ruzek JI (2012). Review of exposure therapy: A gold standard for PTSD treatment. Journal of Rehabilitation Research & Development, 49(5), 679–688. 10.1682/jrrd.2011.08.0152 [DOI] [PubMed] [Google Scholar]
- Richardson L, Woodley N, Neuberger L, Sandoval J, & Huang HJ (2021). A guide to hair preparation for EEG studies. https://hellobrainlab.com/research/eeg-hair-project/
- Roberts SO, Bareket-Shavit C, Dollins FA, Goldie PD, & Mortenson E (2020). Racial inequality in psychological research: Trends of the past and recommendations for the future. Perspectives on Psychological Science, 15(6), 1295–1309. 10.1177/1745691620927709 [DOI] [PubMed] [Google Scholar]
- Ruiz JM, Sbarra D, & Steffen PR (2018). Hispanic ethnicity, stress psychophysiology and paradoxical health outcomes: A review with conceptual considerations and a call for research. International Journal of Psychophysiology, 131, 24–29. 10.1016/j.ijpsycho.2018.04.001 [DOI] [PubMed] [Google Scholar]
- Sandoval JA, Lucero J, Oetzel J, Avila M, Belone L, Mau M, Pearson C, Tafoya G, Duran B, Iglesias Rios L, & Wallerstein N (2012). Process and outcome constructs for evaluating community-based participatory research projects: A matrix of existing measures. Health Education Research, 27(4), 680–690. 10.1093/her/cyr087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sardar DK, Mayo ML, & Glickman RD (2001). Optical characterization of melanin. Journal of Biomedical Optics, 6(4), 404–411. 10.1117/1.1411978 [DOI] [PubMed] [Google Scholar]
- Sasaki JY, & Kim HS (2017). Nature, nurture, and their interplay: A review of cultural neuroscience. Journal of Cross-Cultural Psychology, 48(1), 4–22. 10.1177/0022022116680481 [DOI] [Google Scholar]
- Schwartz RC, & Blankenship DM (2014). Racial disparities in psychotic disorder diagnosis: A review of empirical literature. World Journal of Psychiatry, 4(4), 133–140. 10.5498/wjp.v4.i4.133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shcherbina A, Mattsson CM, Waggott D, Salisbury H, Christle JW, Hastie T, Wheeler MT, & Ashley EA (2017). Accuracy in wrist-worn, sensor-based measurements of heart rate and energy expenditure in a diverse cohort. Journal of Personalized Medicine, 7(2), 3. 10.3390/jpm7020003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Settles I, Warner L, Buchanan N, & Jones M (2020). Understanding psychology’s resistance to intersectionality theory using a framework of epistemic exclusion and invisibility. Journal of Social Issues, 76. 10.1111/josi.12403 [DOI] [Google Scholar]
- Schmotzer GL (2012). Barriers and facilitators to participation of minorities in clinical trials. Ethnicity and Disease 22(2):226–30. https://pubmed.ncbi.nlm.nih.gov/22764647/ [PubMed] [Google Scholar]
- Sukhera J, & Palaniyappan L (2021). Walking the walk: Advice for anti-racist academic leaders. Psychiatry Research, 308, 114343. 10.1016/j.psychres.2021.114343 [DOI] [PubMed] [Google Scholar]
- Swerdlow NR, Light GA, Sprock J, Calkins ME, Green MF, Greenwood TA, Gur RE, Gur RC, Lazzeroni LC, Nuechterlein KH, Radant AD, Ray A, Seidman LJ, Siever LJ, Silverman JM, Stone WS, Sugar CA, Tsuang DW, Tsuang MT, … Braff DL (2014). Deficient prepulse inhibition in schizophrenia detected by the multi-site COGS. Schizophrenia Research, 152(2), 503–512. 10.1016/j.schres.2013.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tayag Y (2020, September 18). The final say on pulse oximeters. Medium Coronavirus Blog. https://coronavirus.medium.com/the-final-say-on-pulse-oximeters-8ffa458fbf68
- Thomson ML (1954). A comparison between the number and distribution of functioning eccrine sweat glands in Europeans and Africans. The Journal of Physiology, 123(2), 225–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uddin LQ, & De Los Reyes A (2021). Cultivating allyship through casual mentoring to promote diversity. Trends in Cognitive Science, 25(10), 813–815. 10.1016/j.tics.2021.07.014 [DOI] [PubMed] [Google Scholar]
- Wallerstein N, & Duran B (2008). The theoretical, historical, and practice roots of CBPR. In Minkler M & Wallerstein N, Community-based participatory research for health: From process to outcomes (2nd ed.) (pp. 25–46). 10.13140/RG.2.2.34282.72648 [DOI] [Google Scholar]
- Wassenaar EB, & Van den Brand JGH (2005). Reliability of near-infrared spectroscopy in people with dark skin pigmentation. Journal of Clinical Monitoring and Computing, 19(3), 195–199. [DOI] [PubMed] [Google Scholar]
- Webb EK, Etter JA, & Kwasa JA (2022). Addressing racial and phenotypic bias in human neuroscience methods. Nature Neuroscience, 25(4), 410–414. 10.1038/s41593-022-01046-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weigand DA, Haygood C, & Gaylor JR (1974). Cell layers and density of Negro and Caucasian stratum corneum. The Journal of Investigative Dermatology, 62(6), 563–568. 10.1111/1523-1747.ep12679412 [DOI] [PubMed] [Google Scholar]
- Weisberg DS, Keil FC, Goodstein J, Rawson E, & Gray JR (2008). The Seductive Allure of Neuroscience Explanations. Journal of Cognitive Neuroscience, 20(3), 470–477. 10.1162/jocn.2008.20040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wendler D, Kington R, Madans J, Wye GV, Christ-Schmidt H, Pratt LA, Brawley OW, Gross CP, & Emanuel E (2005). Are racial and ethnic minorities less willing to participate in health research? PLOS Medicine, 3(2), e19. 10.1371/journal.pmed.0030019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesley NO, & Maibach HI (2003). Racial (ethnic) differences in skin properties. American Journal of Clinical Dermatology, 4(12), 843–860. 10.2165/00128071-200304120-00004 [DOI] [PubMed] [Google Scholar]
- Wilson LC (2010, March 1). Psychophysiology: Daunting or doable? APS Observer. https://www.psychologicalscience.org/observer/psychophysiology-daunting-ordoable
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


