Abstract
Introduction
To examine the impact of the COVID-19 pandemic on mortality, we estimated excess all-cause mortality in 24 countries for 2020 and 2021, overall and stratified by sex and age.
Methods
Total, age-specific and sex-specific weekly all-cause mortality was collected for 2015–2021 and excess mortality for 2020 and 2021 was calculated by comparing weekly 2020 and 2021 age-standardised mortality rates against expected mortality, estimated based on historical data (2015–2019), accounting for seasonality, and long-term and short-term trends. Age-specific weekly excess mortality was similarly calculated using crude mortality rates. The association of country and pandemic-related variables with excess mortality was investigated using simple and multilevel regression models.
Results
Excess cumulative mortality for both 2020 and 2021 was found in Austria, Brazil, Belgium, Cyprus, England and Wales, Estonia, France, Georgia, Greece, Israel, Italy, Kazakhstan, Mauritius, Northern Ireland, Norway, Peru, Poland, Slovenia, Spain, Sweden, Ukraine, and the USA. Australia and Denmark experienced excess mortality only in 2021. Mauritius demonstrated a statistically significant decrease in all-cause mortality during both years. Weekly incidence of COVID-19 was significantly positively associated with excess mortality for both years, but the positive association was attenuated in 2021 as percentage of the population fully vaccinated increased. Stringency index of control measures was positively and negatively associated with excess mortality in 2020 and 2021, respectively.
Conclusion
This study provides evidence of substantial excess mortality in most countries investigated during the first 2 years of the pandemic and suggests that COVID-19 incidence, stringency of control measures and vaccination rates interacted in determining the magnitude of excess mortality.
Keywords: COVID-19, Public Health, Vaccines, Control strategies, Epidemiology
WHAT IS ALREADY KNOWN ON THIS TOPIC
A limited number of studies, focusing on more than one country, have investigated sex-specific and age-specific COVID-19 excess mortality for the whole of 2020 and 2021, and they evidenced substantial excess mortality in the majority of included countries. There is a paucity of studies investigating drivers of excess mortality across countries.
WHAT THIS STUDY ADDS
Most of the countries studied had excess all-cause mortality, which was particularly higher among men and among people in the older age groups (65+ or 70+). Further, this study indicates that reported COVID-19 incidence, stringency of control measures and vaccination rates interact in determining the magnitude of excess mortality.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
The results can serve as evidence of the need to strengthen health resilience in the most affected countries, sex and age groups. They also provide quantification on the effectiveness of public health interventions and control measures used during the COVID-19 pandemic to lessen its impact on mortality.
Introduction
In late 2019, the first cases of SARS-CoV-2 were reported in Wuhan, China. Since then, the causative agent of COVID-19 has rapidly spread worldwide, causing dreadful disruptions.1 COVID-19 vaccines were developed with an incredible speed and the first vaccine was administered outside of a clinical trial setting in England on 8 December 2020.2 3 However, up to May 2023, more than 3.5 million COVID-19-related deaths have been recorded since the delivery of the first vaccine.4 5
The impact of the pandemic on mortality is not fully captured in national published COVID-19 mortality estimates.6–9 This might be due to a number of reasons including the limited testing capacity which led to undercounting,10 11 the improper attribution of deaths as COVID-19 deaths instead of deaths from other causes, a delay in the processing of death certificates which created a lag in data,7 12 and the disruption of the healthcare systems, including disruptions of pathology testing13 and delays in health-seeking behaviour. The latter was provoked not only by the COVID-19-related anxiety but also by the lack of hospital resources for non-COVID-19 emergencies, since ambulances and intensive care beds had been mostly used for COVID-19 patients, at the expense of other patients, leading consequently to a large healthcare burden, with patients with life-threading diseases (eg, myocardial infarction patients) not being hospitalised.14
It is challenging to obtain accurate estimates of the death toll of the pandemic. The misclassification of unrelated deaths as COVID-19 deaths, as well as the undercounting of COVID-19-related mortality due to the limited availability of testing, can result in inaccurate estimation of the true COVID-19-related mortality.15 16 These methodological challenges in reporting of COVID-19 deaths are also not comparable across countries as different countries use different definitions and processes to count COVID-19 deaths, and these often vary over time.
A reasonable way to overcome the above challenges is to estimate the excess all-cause mortality at country level, by comparing the observed to the expected number of deaths during a specified time period.17–19 As discussed in Demetriou et al,15 the expected number of deaths can be predicted using historical data and time series analyses accounting for seasonality and other secular trends.
Many studies have investigated COVID-19 excess mortality.9 20–22 However, most focused on single countries or world regions during the first months of the pandemic. They also used publicly available data that were often provisional at the time of analysis. The frequency of updates also influenced the consistency of data.7 15 20 The one study that estimated excess mortality due to the COVID-19 pandemic for both the whole years 2020 and 2021 in 191 countries and territories could not provide estimations by sex and age group.22 However, several studies incorporating data from more than one country have investigated sex-specific and age-specific excess mortality for the whole of 2020 and 2021, and they evidenced substantial excess mortality in the majority of included countries.15 23 24 Understanding the impact of stringency of control measures and of vaccination on the toll of the pandemic at a global level is imperative given the variability of governmental responses and differences in vaccination access and uptake across populations. One study quantified the global impact of the first COVID-19 vaccinations and determined that the death toll was underestimated or overestimated in many countries, compromising the estimates of vaccine effectiveness.3
An international consortium, the COVID-19 MORtality (C-MOR) Consortium, consisting of more than 50 countries across 6 continents was established to investigate the mortality impact of the COVID-19 pandemic.15 16 The consortium encompasses countries worldwide without restriction and focuses all analyses on data from national primary sources. The current analysis estimates overall, sex-specific and age-specific excess all-cause mortality in the 24 countries where age--stratified and sex-stratified data were available, and investigates correlates of overall excess all-cause mortality during the whole of 2020 and 2021.
Methods
Data acquisition
In this study, we examined the mortality data from 24 countries or regions participating in the international consortium that have collected and provided data.25 The participating countries or regions include Australia, Austria, Brazil, Belgium, Cyprus, Denmark, England and Wales, Estonia, France, Georgia, Greece, Israel, Italy, Kazakhstan, Mauritius, Northern Ireland, Norway, Peru, Poland, Slovenia, Spain, Sweden, Ukraine, and the USA. Total, sex-specific and age-specific weekly all-cause mortality for 2015–2021 was collected from national vital statistics databases, made either publicly available or with restricted access (online supplemental table S1).25 Depending on the country, all-cause mortality was reported by either ISO week, starting on Monday; Epi week, starting on Sunday or other national counting week system.
bmjgh-2023-013018supp001.pdf (4.5MB, pdf)
Data were assembled between June and September 2022, that is, several months after the end of the study period, to allow for reporting delays7 14 and enough time for data consolidation by reporting authorities to improve data quality.26
Statistical analysis
Mortality rates
For the calculation of mortality rates, total, age-specific and sex-specific mid-year population estimates for the participating countries were obtained from the World Bank,27 except for the UK nations for which population data from the Office for National Statistics28 was extracted separately for England and Wales, Scotland and the Northern Ireland, and for Cyprus for which Eurostat data29 was used to include only the population in the Republic of Cyprus government-controlled area.
Crude mortality rates (CMRs) were calculated for the total population and sex-specific groups using equation (1)
| (1) |
where denotes the number of deaths in all age groups in year and week , denotes the mid-year population for year and denotes the number of weeks in the year.
Age-specific mortality rates (ASpMRs) were calculated using equation (2)
| (2) |
where denotes the number of deaths in the age group in year and week , denotes the mid-year population of age group in year , and denotes the number of weeks in the year.
Weekly (directly) age-standardised mortality rates (ASMRs) were calculated as a weighted average of the ASMRs using the equation 3 as previously described,15 where, index denotes the aggregate age groups (see online supplemental table S2) and the standard population weights correspond to the proportion of population in the age interval in the WHO World Standard Population 2000–2025.30
| (3) |
The aggregate age groups created for each country, based on the provided age-specific all-cause mortality data, are presented in online supplemental table S2, followed by the equations used for the age standardisation.
Excess mortality
Total, and sex-specific, weekly excess mortality for 2020 and 2021 was calculated by comparing weekly 2020 and 2021 ASMR (per 100 000 population) against a baseline mortality (expected weekly ASMR in 2020 and 2021, respectively), estimated based on historical data (2015–2019) accounting for seasonality, and long-term and short-term trends, as previously described.15 31–33 The regression model is specified in online supplemental material. Similarly, age-specific weekly excess mortality for 2020 and 2021 was calculated by comparing weekly 2020 and 2021 CMR (per 100 000 population) against a baseline mortality (expected weekly CMR in 2020 and 2021, respectively), estimated based on historical data (2015–2019).
The regression models were built on complete weeks and truncated weeks were excluded. Truncated weeks are usually a result of the different death counts observed around Christmas and New Year,34 and these included week 53 (applicable for Australia, Austria, Brazil, Belgium, Cyprus, Denmark, Estonia, France, Georgia, Greece, Israel, Italy, Norway, Peru, Poland, Spain, Sweden, Ukraine and the USA), weeks 1 and 52 for England and Wales, weeks 1 and 53 for Kazakhstan and Mauritius, weeks 51 and 52 for Northern Ireland, and weeks 52 and 53 for Slovenia. For all countries, observed and expected weekly mortality rates for 2020 and 2021 were each summed up to week 52, except for England and Wales (weeks 2–51), Kazakhstan and Mauritius (weeks 2–52), Northern Ireland (up to week 50) and Slovenia (up to week 51). Sex-specific excess mortality for 2020 and 2021 could not be calculated for Northern Ireland due to the lack of sex-specific all-cause mortality data, and thus Northern Ireland was not included in this analysis. Also, sex-specific weekly all-cause mortality for Peru was collected from 2017 to 2021.
The weekly results of the observed versus expected mortality rates are presented graphically using z-scores [(number of observed deaths–expected mortality)/SD of the residuals]. Z-scores ranging from −2 and +2 are considered ‘normal’, while a z-score >4 is considered a substantial increase.35 36
Subsequently, the cumulative expected 2020 and 2021 mortality rates were subtracted from the respective cumulative observed 2020 and 2021 mortality rates to obtain estimates of excess mortality separately for the years 2020 and 2021. The statistical significance of the excess mortality rate was determined using the 95% confidence intervals (CIs) estimated by the model.
P-score, defined as the ratio of the cumulative excess to the cumulative expected mortality, expressed as a percentage, was calculated for both years 2020 and 2021, for the total, male and female population, as well as for the age groups <65, 65+, <70 and 70+.
Ecological analysis of correlates of excess mortality
In an attempt to identify correlates of excess mortality in the participating countries (ecological analysis), a database of twenty country-level sociodemographic variables (reported yearly) and three pandemic-related variables (reported weekly), was built using publicly available sources as outlined in online supplemental table S3. The variables collected were variables previously investigated in association with excess mortality during the COVID-19 pandemic in published research37 and included: (1) population-related variables (population density, population median age, percentage of population aged 65+ years, life expectancy, hypertension, diabetes and obesity prevalence, and air pollution (PM2.5 concentration)); (2) government and economy-related variables (gross domestic products (GDP), Human development index (HDI), Inequality-adjusted HDI (IHDI), Gini index, Government Effectiveness index and government revenue); (3) health resource variables (hospital beds per thousand population, total medical doctors and total nursing personnel (per 10 000 population), universal health coverage (UHC), completeness of vital registration system and Healthcare Access and Quality Index (HAQ)) and (4) pandemic-related variables (weekly incidence of COVID-19 per 1000 population, stringency index of government control measures (with a 3-week lag) and percentage of people fully vaccinated (with a 3-week lag)). Mauritius was excluded from this analysis due to the lack of recent data from reliable sources.
Initially, the association between each of these variables and excess mortality z-score was examined across countries, for 2020 and 2021 combined, using a linear regression model. A strong association was observed between completeness of vital registration systems and excess mortality (β=−0.42, p<0.001) suggesting that level of completeness may be biasing the excess mortality results. Therefore, countries with a completeness of <90%, namely Kazakhstan and Peru, were excluded from this and subsequent analyses. Then, three multivariable models were built using (1) population variables, (2) economic and government-related variables and (3) healthcare resource variables, as indicated in online supplemental table S3. Multicollinearity was examined within each class of variables, and among the collinear variables the ones that returned the best model fit were retained. The retained variables for each model, all with a variance inflation factor of less than 10, were rescaled to a mean of 0 and an SD of 1.
Following, the pandemic-related variables were examined using multilevel models, with country as a random effect, the pandemic-related variables as fixed effects, and with the method of restricted (residual) maximum likelihood. Two separate multilevel models were run, one for 2020 (excluding vaccination) and one for 2021. Interactions between the pandemic-related variables were also examined for each year. In all models above, weeks with z-scores larger than 15 were excluded as outliers, based on bag plots, and the normality of the z-scores outcome variable was examined (online supplemental figures S1–S3).
Lastly, the associations between stringency of control measures (3-week lag) during 2020–2021 and percentage of population fully vaccinated (3-week lag) during 2021 with excess mortality z-scores were investigated in regression models with time-varying exposure against excess mortality, adjusting for weekly COVID-19 incidence. A separate model was run for each country and the time-varying coefficients were illustratively compared with the static regression model coefficients. All analyses were performed using R Statistical Software, V.4.2.2 (The R Foundation for Statistical Computing, Vienna, Austria).
Patient and public involvement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Results
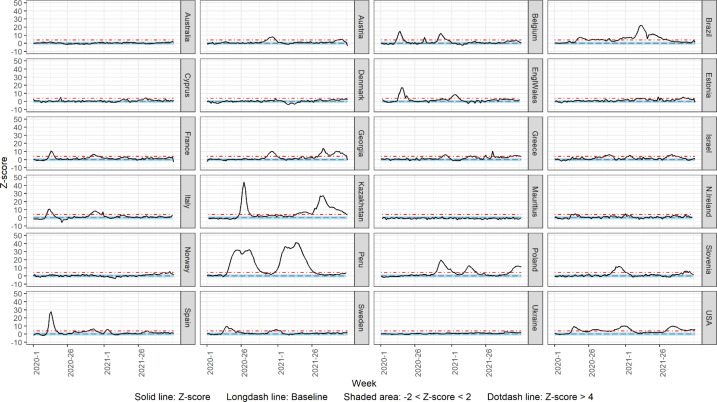
Weekly comparisons-total population and by sex in 2020 and 2021
In 2020, 18 countries showed a substantial increase in the ASMR ranging from 1 to 29 weeks, while in 2021, 17 countries showed a substantial increase in the ASMR ranging from 1 to 37 weeks. Figure 1 shows the weekly ASMR z-score over time from week 1 2020 to week 52 2021. The countries that showed a substantial increase (>4 z-scores) in the ASMR over time from week 1 2020 to week 52 2020 for the total population include Peru (29 weeks), the USA (26 weeks), Brazil (25 weeks), Belgium and Italy (14 weeks), Sweden (13 weeks), Poland (12 weeks), France and Spain (11 weeks), Slovenia (9 weeks), Georgia, England and Wales and Kazakhstan (8 weeks), Austria (7 weeks), Israel (6 weeks), Greece (4 weeks), Northern Ireland (2 weeks) and Cyprus (1 week). In 2021, the countries that showed a substantial increase in the ASMR over time from week 1 2021 to week 52 2021 for the total population include Kazakhstan (37 weeks), Brazil (32 weeks), Peru and the USA (28 weeks), Poland and Georgia (23 weeks), Greece (14 weeks), Israel (10 weeks), Slovenia (7 weeks), Estonia (6 weeks), England and Wales (5 weeks), Austria (4 weeks), Norway and Sweden (3 weeks), Cyprus and Spain (2 weeks) and Belgium and Northern Ireland (1 week). In contrast, Australia, Denmark, Mauritius and Ukraine did not display substantial excess mortality for any week during either year. Norway and Estonia did not show substantial excess mortality for any week during 2020, and we did not find any substantial excess mortality for any week during 2021 for France and Italy.
Figure 1.
Weekly z-score of age-standardised all-cause mortality rate for total population for 2020 and 2021.
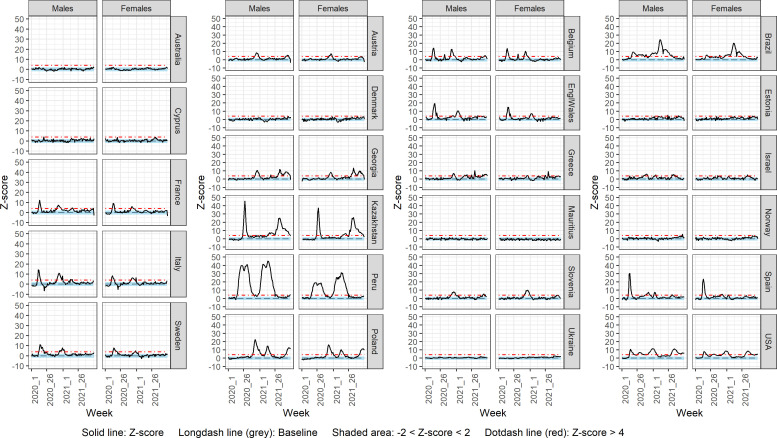
Sex-specific weekly ASMR z-scores over 2020 and 2021 are shown for each country in figure 2 for males and females, respectively. The countries that showed a substantial increase (>4 z-scores) in the ASMR over 2020 for the male population include Austria, Belgium, Brazil, Cyprus, England and Wales, France, Georgia, Greece, Israel, Italy, Kazakhstan, Peru, Poland, Slovenia, Spain, Sweden, and the USA. The excess mortality duration between countries in 2020 varied between 1 and 33 weeks for 2020. The same countries, besides Cyprus, showed a substantial increase in the ASMR over 2021 for the male population, with the addition of Norway and Estonia. The excess mortality duration between countries varied between 1 and 39 weeks in 2021 for 2021. Australia, Denmark, Mauritius and Ukraine did not display substantial excess mortality in males for any week during the years 2020 and 2021. Norway and Estonia did not display substantial excess mortality in males for any week during 2020, while Cyprus did not display substantial excess mortality for any week during 2021.
Figure 2.
Weekly z-score of age-standardised all-cause mortality rate by sex for 2020 and 2021.
In 2020, the countries that showed a substantial increase in the ASMR over time for the female population included Austria, Belgium, Brazil, England and Wales, France, Georgia, Greece, Israel, Italy, Kazakhstan, Peru, Poland, Slovenia, Spain, Sweden, and the USA. The excess mortality duration between countries varied between 2 and 24 weeks for 2020. The same countries, besides Belgium, France, Italy and Sweden, showed a substantial increase in the ASMR over time during 2021 for the female population as well, with the addition of Estonia. The excess mortality duration between countries varied between 1 and 32 weeks for 2021. Australia, Cyprus, Denmark, Mauritius, Norway and Ukraine did not display substantial excess mortality in females for any week during both years 2020 and 2021. Estonia did not display substantial excess mortality in females for any week during 2020, while Belgium, France, Italy and Sweden did not display substantial excess mortality for any week during 2021.
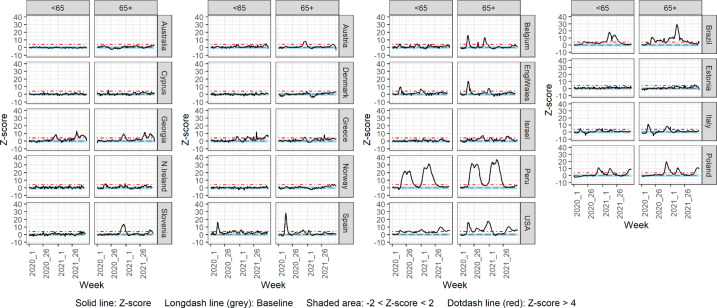
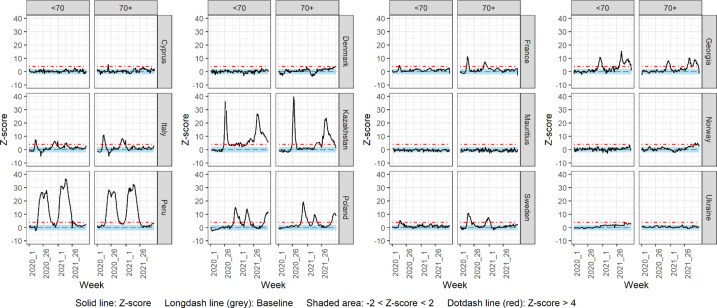
Weekly comparisons by age group for total population in 2020 and 2021
Figures 3 and 4 show the weekly mortality rate z-score over time in 2020 and 2021 for ages <65, 65+, <70 and 70+ years for the total population. The countries that showed a substantial increase in the weekly mortality rate over 2020 for the younger age group investigated include Austria, Belgium, Brazil, England and Wales, Georgia, Greece, Italy, Peru, Poland, Spain, and the USA (age group <65), and France, Georgia, Italy, Kazakhstan, Peru, Poland, and Sweden (age group <70). In 2021, apart from France and Sweden, these countries also showed a substantial increase in the weekly mortality rate for the younger age groups, with the addition of Slovenia.
Figure 3.
Weekly z-score of all-cause mortality rate for age groups <65 and 65+ for 2020 and 2021.
Figure 4.
Weekly z-score of all-cause mortality rate for age groups <70 and 70+ for 2020 and 2021.
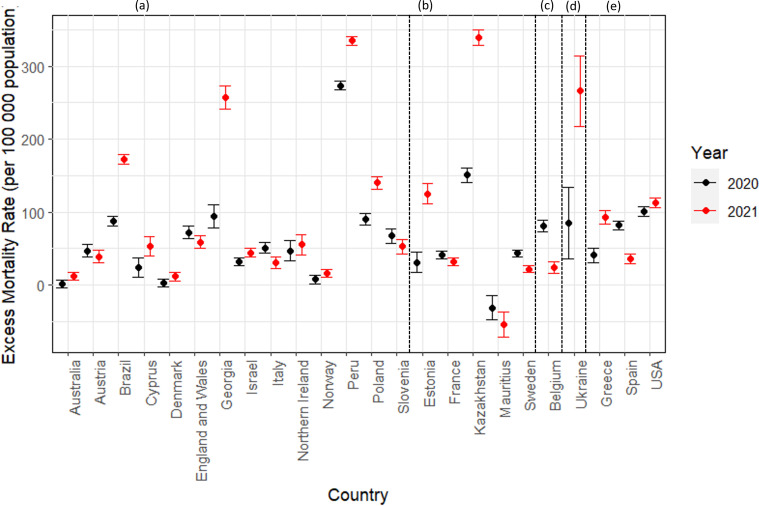
Cumulative excess mortality in 2020 and 2021
Figure 5 shows the comparison of the cumulative excess all-cause mortality for 2020 and 2021. Online supplemental tables S4 and S5 show the cumulative observed and expected all-cause ASMRs for each year, 2020 and 2021, respectively. Online supplemental table S6 shows the cumulative observed and expected all-cause ASMRs for both 2020 and 2021 together.
Figure 5.
Cumulative excess age-standardised mortality rate for total population for 2020 and 2021. Plot letters correspond to the age groups in which countries have provided data, and therefore, the age groups used for age standardisation: (A) age groups <15, 15–44, 45–64, 65+; (B) age groups <20, 20–49, 50–69, 70+; (C) age groups <45, 45–64, 65+; (D) age groups <20, 20–69, 70+; (E) age groups <15, 15–64, 65+.
All participating countries, with the exception of Australia, Denmark and Mauritius, presented statistically significant excess cumulative mortality rates during 2020. On the other hand, Mauritius revealed a statistically significant decrease in yearly all-cause mortality rate, while Australia and Denmark showed no statistically significant differences in all-cause mortality rate in 2020. During 2021, all countries included in this analysis, except for Mauritius, reported statistically significant excess cumulative mortality rates. Mauritius demonstrated a statistically significant decrease in yearly all-cause mortality rate during both years 2020 and 2021.
Online supplemental tables S7 and S8 report the yearly cumulative mortality rate differences (observed - expected) by sex for 2020 and 2021, respectively. For the male population, all countries demonstrated statistically significant excess cumulative mortality rates during 2020 and 2021, except for Australia in 2020, Denmark in 2020, and Mauritius in both years. For the female population, with the exception of Australia, Denmark, Norway and Ukraine, all countries demonstrated statistically significant excess cumulative mortality rates during 2020. In 2021, excess all-cause mortality was observed in all countries except Belgium and Mauritius.
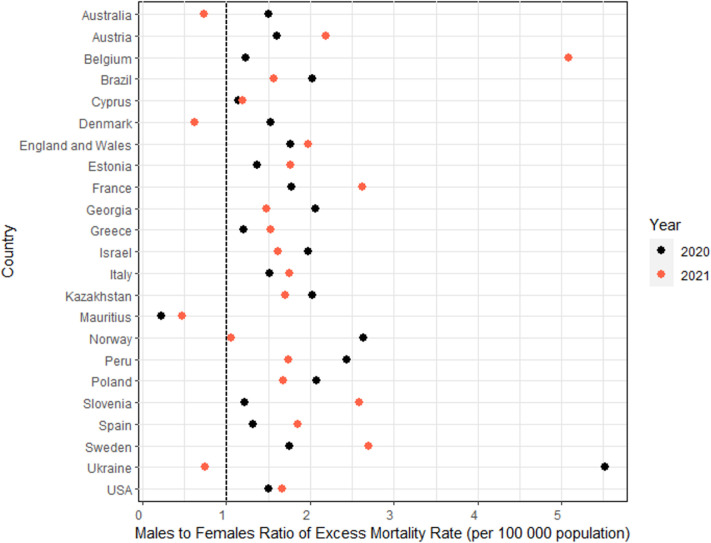
Figure 6 and online supplemental table S9 show the male to female cumulative excess ASMR ratios for 2020 and 2021. Females were more affected than males in Mauritius only in 2020, and in Australia, Denmark, Mauritius and Ukraine in 2021. Cumulative excess all-cause mortality for males and females during 2020 and 2021 are shown in online supplemental figures S4 and S5.
Figure 6.
Males to females cumulative excess age-standardised mortality rate ratio for 2020 and 2021.
Online supplemental tables S10 and S11 demonstrate the cumulative CMR differences (observed - expected) by age group for the years 2020 and 2021, respectively. Age-specific differences in all-cause mortality for the whole years 2020 and 2021 were observed in the majority of the countries included in the present study. However, the differences were higher in the older age groups; 65+ and 70+ than those in the younger age groups for both years. During 2020, only Australia observed no statistically significant differences in all-cause mortality for any of the age groups, and Denmark demonstrated statistically significant cumulative CMR difference only in the 70+ age group. Norway and Israel demonstrated statistically significant increase in the cumulative CMR difference in the older groups only. Mauritius demonstrated statistically significant decrease in the cumulative CMR difference in the <70 age group, and significant increase in the 70+ age group.
During 2021, all the countries observed statistically significant increases in cumulative CMR difference in the 65+ age group. In the <65 age group, all countries showed statistically significant increase in cumulative CMR difference, except for Australia, Denmark and Norway. Also, in the 70+age group, all countries observed statistically significant increases in cumulative CMR difference, except for Mauritius that showed a statistically significant decrease. In the <70 age group, the following countries observed statistically significant increases in cumulative CMR difference: Cyprus, France, Georgia, Italy, Kazakhstan, Norway, Peru, Sweden and Ukraine. Mauritius and Poland demonstrated statistically significant decrease in the cumulative CMR difference in the <70 age group.
Ecological analysis of correlates of excess mortality
The univariable regression results for each of the 20 investigated variables are included in table 1 and the distribution of these variables across countries is shown in online supplemental table S12. In the multivariable model of population-related variables, median population age and life expectancy were removed due to collinearity. Of the remaining variables, hypertension prevalence (β=0.54, p<0.001), diabetes prevalence (β=0.43, p<0.001) and obesity prevalence (β=0.35, p<0.001) were positively associated with excess mortality (table 1). In the multivariable model of government and economy-related variable, GDP, IHDI and government effectiveness were removed due to collinearity between them and the retained HDI. Of the retained variables, HDI (β=−0.28, p<0.001) was negatively associated with excess mortality, whereas, GINI index (β=0.66, p<0.001) was positively associated. Lastly, of the healthcare resource-related variables, UHC was removed due to collinearity with HAQ. Of the included variables hospital beds per 1000 population (β=−0.26, p<0.001) and HAQ (β=−0.67, p<0.001) were both negatively associated with excess mortality, whereas completeness of vital registration systems (β=0.13, p=0.023) was significantly positively associated with excess mortality. Total medical and nursing personnel were not significantly associated with excess mortality (table 1).
Table 1.
Country-level sociodemographic determinants of excess mortality*
| Unadjusted model on scaled data | Adjusted model on scaled data—population-related variables† | Adjusted model on scaled data—government and economy-related variables‡ | Adjusted model on scaled data—health resources-related variables§ | ||||||
| Regression coefficient | P value | R2=0.101 | R2=0.106 | R2=0.089 | |||||
| Regression coefficient | P value | Regression coefficient | P value | Regression coefficient | P value | ||||
| Population variables | Population density | −0.11 | 0.0565 | 0.07 | 0.414 | ||||
| Median age | −0.34 | <0.001 | |||||||
| Percentage of population more than 65 years old | −0.46 | <0.001 | −0.07 | 0.280 | |||||
| Life expectancy | −0.52 | <0.001 | |||||||
| Hypertension | 0.42 | <0.001 | 0.54 | <0.001 | |||||
| Diabetes | 0.62 | <0.001 | 0.43 | <0.001 | |||||
| Obesity | 0.38 | <0.001 | 0.35 | <0.001 | |||||
| PM2.5 (air pollution) | 0.32 | <0.001 | 0.07 | 0.433 | |||||
| Government and economy | Gross domestic products (GDP) | −0.33 | <0.001 | ||||||
| Human Development Index (HDI) | −0.53 | <0.001 | −0.28 | <0.001 | |||||
| Inequality-adjusted Human Development Index (IHDI) | −0.71 | <0.001 | |||||||
| Gini index | 0.79 | <0.001 | 0.66 | <0.001 | |||||
| Government Effectiveness | −0.55 | <0.001 | |||||||
| Government revenue | −0.58 | <0.001 | −0.06 | 0.439 | |||||
| Health resources | Hospital beds per thousand population | −0.20 | 0.008 | −0.26 | <0.001 | ||||
| Total medical doctors (per 10 000 population) | −0.04 | 0.511 | −0.03 | 0.606 | |||||
| Total nursing personnel (per 10 000 population) | −0.37 | <0.001 | 0.04 | 0.541 | |||||
| Universal health coverage | −0.48 | <0.001 | |||||||
| Completeness of vital registration | 0.02 | 0.75 | 0.13 | 0.023 | |||||
| Healthcare Access and Quality Index (HAQ) | −0.62 | <0.001 | −0.67 | <0.001 | |||||
Bold fonts indicate statistically significant p-values, at an alpha level of 0.05.
*Kazakhstan and Peru were excluded from this analysis due to a completeness of vital registration systems of <90% which affects excess mortality estimates.
†Life expectancy removed from model due to collinearity (r≥0.60) with hypertension and median age due to collinearity (r≥0.94) with proportion of population 65+.
‡GDP, IHDI and government effectiveness were removed from model due to collinearity (r≥0.90) between them and with HDI.
§Universal health coverage removed from model due to collinearity (r≥0.80) with HAQ.
Across all models, 1 SD increase in Gini, diabetes and hypertension prevalence produced the strongest positive effect estimates, whereas HAQ and HDI had the strongest negative effect estimates. Nevertheless, the R2 values of the predictive models were low (0.101, 0.106 and 0.089, respectively) suggesting the influence of additional predictors.
In the year-specific models built for examining the influence of pandemic-related variables, the random effect of country introduced variation in the model, with an intraclass correlation coefficients of 0.24 for 2020 and 0.38 for 2021 (table 2). In the mixed model including 2020 weeks only, weekly incidence of reported COVID-19 cases (β=0.75, p<0.001) and stringency of control measures (β=0.312, p<0.001) were positively associated with excess mortality z-scores, given a zero (average) value for the other variable. For higher values of stringency of control measures, the influence of the weekly incidence of reported COVID-19 cases on excess mortality was decreased, but this was of borderline significance (βinteraction=-0.18, p=0.050).
Table 2.
Multilevel model results on the ability of pandemic-related variables to predict excess mortality (z-scores) during 2020 and 2021
| Predictors | 2020* | 2021* | ||||
| Estimates | 95% CI | P value | Estimates | 95% CI | P value | |
| (Intercept) | 1.90 | 1.32 to 2.49 | <0.001 | 1.94 | 1.26 to 2.62 | <0.001 |
| Weekly incidence of COVID-19 (3-week lag) | 0.75 | 0.54 to 0.96 | <0.001 | 0.59 | 0.40 to 0.78 | <0.001 |
| Stringency of control measures (3-week lag) | 0.31 | 0.15 to 0.47 | <0.001 | −0.39 | −0.61 to −0.17 | <0.001 |
| Weekly incidence of COVID-19×stringency of control measures (interaction) | −0.18 | −0.35 to 0.00 | 0.050 | |||
| No of fully vaccinated per 100 population (3-week lag) | 0.08 | −0.13 to 0.29 | 0.449 | |||
| Weekly incidence of COVID-19×No of fully vaccinated per 100 population (interaction) | −0.21 | −0.32 to −0.10 | <0.001 | |||
| Random effects | 2020 | 2021 | ||||
| σ2 | 5.41 | 3.90 | ||||
| ICC | 0.24 | 0.38 | ||||
| N data$location | 21 | 21 | ||||
| Observations | 910 | 1074 | ||||
| Marginal R2/conditional R2 | 0.083 / 0.305 | 0.070 / 0.428 | ||||
*For each year, the model included all listed but not shaded variables. Kazakhstan and Peru were excluded from this analysis due to a completeness of vital registration systems of <90% which affects excess mortality estimates.
ICC, intraclass correlation coefficient.
In the model including 2021 weeks only, weekly incidence of reported COVID-19 cases (β=0.59, p<0.001) was again positively associated with excess mortality, whereas stringency of control measures (β=−0.39, p<0.001) was inversely associated, given zero (average) values for all other variables in the model (table 2). The number of people fully vaccinated per 100 population was not independently associated with excess mortality (β=0.08, p=0.449), however, it interacted significantly with weekly incidence of reported COVID-19 cases so that a 1 SD increase in vaccination rates attenuated the positive relationship between weekly incidence of reported COVID-19 cases and excess mortality from 0.59 to 0.38 (βinteraction=-0.210, p<0.001).
Lastly, the results of the time-varying models for stringency of control measures and the effect of vaccination on the excess mortality in each country are presented and described in online supplemental figures S6–S26. Overall, the results indicate that in each country a different pattern of associations was observed with substantial fluctuations in the coefficients across the time period of investigation for both variables.
Discussion
Summary of findings
The present study estimated total, sex-specific and age-specific excess all-cause mortality in 24 countries during the years 2020 and 2021. The majority of investigated countries showed significant excess mortality during at least 1 week of 2020 and 1 week of 2021, with varying duration. Australia, Denmark, Mauritius and Ukraine did not display excess mortality for any week during both years 2020 and 2021, while Norway did not display excess mortality during 2020, and France and Italy during 2021. Moreover, excess mortality was higher for people aged 65+ years and 70+ years than in younger age groups (<65 and <70) in most countries.
Excess of cumulative ASMRs was reported in all countries analysed in 2020 and/or 2021, except for Australia and Mauritius. Denmark showed no statistically significant differences in all-cause mortality rate in 2020 and Mauritius demonstrated a statistically significant decrease in yearly all-cause mortality rate during both years. The highest estimated excess mortality rate for 2020 was 273 deaths per 100 000 population in Peru, while the highest estimated excess mortality rate for 2021 was 338.7 deaths per 100 000 population in Kazakhstan. These findings are in accordance with those reported elsewhere, regardless of the use of different methodologies and data sources.22 24 38 39 More specifically, Nepomuceno et al, using a combination of different methodologies, demonstrated that Italy, the USA, Slovenia and countries of the UK were the most heavily affected in terms of ASMRs.40 Additionally, Karlinsky and Kobak estimated excess deaths by using data from the World Mortality Dataset until the end of 2020 or the first half of 2021, and showed that Peru, Brazil, the USA, Italy and countries of the UK were the most affected.41 COVID-19 Excess Mortality Collaborators (2022) have also identified Italy, Greece, Norway, Spain, Sweden and the USA as having a high excess of all-cause deaths.22
The cumulative excess for all-cause mortality for the total population in 2020 was higher than in 2021 in Austria, Belgium, England and Wales, France, Italy, Mauritius, Slovenia, and Spain. This may be due to the COVID-19 vaccination programmes that have been shown to reduce at least COVID-19-related mortality,3 42 or due to the time of different waves as in the case of Belgium where a second wave arrived in late 2020 rather than early 2021.43 The same scenario applies to both female and male populations, with the exception of Slovenia where for females the cumulative excess for all-cause mortality was higher in 2021 than in 2020. These results align with other published results. The Our World in Data also shows that in France, Belgium, Italy and Spain, excess mortality in 2020 was higher than in 2021.44
In the yearly cumulative comparison, increases or decreases in all-cause mortality were similar between sexes in both years except for Mauritius (statistically significant decrease only in females in 2020), Norway (statistically significant increase only in males in 2020), Ukraine (statistically significant increase only in males in 2020) and Belgium (statistically significant increase only in males in 2021). Moreover, males were more affected than females in terms of cumulative excess ASMR, with the exception of Australia and Mauritius in 2020, and Australia, Denmark, Mauritius and Ukraine in 2021. Many studies have previously reported the male predominance in excess mortality in most countries.15 24 45–47 This may be due to a number of factors, such as occupation and lifestyle factors, or differences in comorbidities between males and females that may rise the possibility of SARS-CoV-2 exposure among males than females.24
The observed pattern of weekly excess mortality in the countries included in the current study demonstrates that some countries experienced substantial excess mortality during the first half of the year but not later, for both 2020 and 2021 (Kazakhstan, Peru, Spain in 2020, Brazil in 2021), while other countries did so during the second half of the year but not earlier (Austria, Georgia, Greece, Israel in 2020 and 2021). Similar peaks in excess mortality for the participating countries were reported elsewhere.22 24 41 44
Of the country-level sociodemographic variables investigated, hypertension, diabetes and obesity prevalence, as well as Gini index were positively associated with increased excess mortality, whereas HDI, hospital beds per 1000 population and HAQ were inversely associated with excess mortality as also shown elsewhere.22 48–54 Interestingly, completeness of vital registration and excess mortality were significantly positively associated when the multivariable model was restricted to countries with higher than 90% of completeness. Below that completeness level, multiple factors unique to under resourced health system settings are likely to influence the death rate, and deaths recording, and as a result the observed relationship with excess deaths is likely underestimated and biased. Therefore, interpretation of results from countries with less than 90% of completeness in their vital registrations should be treated with caution, as the observed mortality rates may underestimate the true excess mortality.
In the multilevel models investigating pandemic-related variables, the random effect of country explains a substantial proportion of the variability in the outcome, highlighting that different countries had a different experience with respect to the determinants of excess mortality. It is also important to highlight that in these models, the coefficients returned are an average of the experience of the included countries. Weekly reported incidence of COVID-19 significantly increased excess mortality during both years. Seroprevalence was also shown to be associated with excess mortality elsewhere.22 During 2020, contrary to expectations,16 the stringency of control measures was positively associated with excess mortality, whereas, during 2021, those countries that retained strict control measures experienced less excess mortality. In the time-varying models that investigated the effects of stringency on excess mortality, across 2020–2021, in each country independently, substantial fluctuations are evident in the observed coefficients suggesting that it might not be the overall stringency of measures, but specific policies that had a greater benefit in mitigating excess mortality in each country. Nevertheless, for most countries, despite the fluctuations, the coefficients were in the negative range for most of the duration of the 2 years indicating an overall protective effect of the stringency of control measures.
In the multilevel model for 2021, no significant association was observed between vaccination rates and excess mortality, despite a clear and significant trend between maximum achieved vaccination coverage and cumulative excess mortality, across countries, in 2021 (online supplemental figure S27). This non-significant association is likely attributed to the different experience of each country in terms of the prioritising older and vulnerable populations in vaccine distribution and to the variability of the development level of participating countries since high-income countries tended to have greater vaccine access, and managed to cover larger proportions of their older and at-risk populations. Conversely, lower-income and middle-income countries, such as Georgia and Ukraine, experienced delays in achieving sufficient vaccination coverage compared with high-income countries. Consequently, substantial benefits may not have been reflected during 2021. Similarly, as seen in online supplemental figures S6–S27, for many countries, sharp increases in vaccine coverage coincided with the increasing prevalence of the more virulent Delta variant (between July and November 2021), something that could be masking beneficial effects of vaccination. Vaccinations did benefit excess mortality through interaction with weekly incidence of reported COVID-19 cases; in countries and weeks with higher than average vaccination rates, increases in incidence of COVID-19 did not lead to as high excess mortality as compared with countries and weeks with average vaccination rates.
Despite the variable experience of countries, the time-varying models for vaccination display some common features between countries. Several countries (Austria, Belgium, Denmark, England and Wales, France, Israel, Northern Ireland, Norway, and Sweden) had negative coefficients for the association between vaccination coverage and excess mortality, during the first weeks of vaccine introduction, suggesting that the first wave of vaccinations that, in most countries prioritised older and vulnerable portions of the population, managed to mitigate excess mortality. For most of these countries, the coefficients of the association then increased to zero or even positive numbers. In fact, Australia, Austria, Belgium, Denmark, England and Wales, Norway, Poland, Slovenia, and Northern Ireland experienced positive coefficients during the second half of 2021, which could be explained by waning effectiveness of the first vaccinations, as well as by the rise in prevalence of the Delta variant. On the other hand, Brazil, Cyprus, Georgia, Greece and Italy all started with positive coefficients that declined as vaccination coverage increased. The reasons for the different experiences in these latter countries remain to be investigated.
Strengths and limitations
To the best of our knowledge, the present study belongs to a small group of studies that attempted to investigate total, sex-specific and age-specific excess mortality for multiple countries for the whole years 2020 and 2021, using national data sources for mortality estimates. This is also one of the few studies presenting mortality estimates for Kazakhstan and Mauritius.15 22 The model used for the estimation of excess mortality, also used in our previous work,15 was shown to produce estimates with the least bias compared with an array of methodologies.39 40 In addition, investigating excess mortality by age group and applying age standardisation in the calculation of total and sex-specific excess mortality is a critical advantage as it was previously shown that the age stratification has an impact on excess death calculations.55 56 Lastly, this is one of few existing studies that investigated several correlates of excess mortality in the participating countries.37 57 One of the limitations of our study is that participating countries did not use consistent age groupings to calculate age-specific all-cause mortality. Therefore, age-standardised results are not entirely comparable between countries and direct comparisons between countries cannot be applied. Thus, the magnitude of excess mortality for 2020 and 2021 should not be used as a measure of comparison of impact between countries; rather as an indicator of the COVID-19 impact on all-cause mortality in each country, as previously discussed.15 Another limitation is the ecological nature of the investigation of determinants of excess mortality since correlations at population level may be proxies for other factors that directly relate to excess deaths or the reporting of deaths. With numerous and strong correlations between the investigated variables, any findings should only be taken to indicate association rather than causation. Lastly, even though the reference period and the data collection for Ukraine predate the start of the war, we cannot preclude that updates to the data may have been adversely impacted by the disastrous war.
Conclusion
Our study estimating overall, sex-specific and age-specific excess all-cause mortality in 24 countries, demonstrated that during 2020 and 2021, most of the investigated countries presented excess all-cause mortality compared with what was expected based on the years 2015–2019. Furthermore, looking at the male to female ratio of excess mortality, females were more affected than males only in Australia, Denmark, Mauritius and Ukraine. Also, our findings showed that excess mortality was higher for people aged 65+ years and 70+ years than in younger age groups (<65 and <70) in most countries, but younger age groups were also affected in several countries. These findings can serve as evidence that health resilience needs to be strengthened in those countries and the sex and age groups that were most affected. Lastly, our results support that public health interventions, such as stringency of control measures and vaccinations, directly or indirectly influenced the impact of the pandemic in terms of mortality. Therefore, it is evident that continued tracking of excess all-cause mortality is crucial to accurately estimate the true toll of COVID-19.
Footnotes
Handling editor: Seye Abimbola
@LucyGoldsmith19, @mariochong_up
Contributors: Authors CTP, CAD, SA, AQ, EC, MRRH, SP, TL, AA, JMRL, CMB, CZ, ESS, LHM, JAC, and NLM contributed to 1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, 2) the drafting of the article or revising it critically for important intellectual content, and 3) the final approval of the version to be submitted. Authors JG, MA, NBS, RE, JL, LM, LPG, GD, LK, KA, BBi, TM, GA, FS, KD, NG, CM, MCS, TPH, MC, BL, IE, PAG, BBu, NP, OV, QH, AP and AC contributed to 1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, and 2) the final approval of the version to be submitted.
Funding: This work was supported by the University of Nicosia Medical School (internal funding).
Disclaimer: The funding source did not have any involvement in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. The data underlying this study, beyond what is available in the article and in its online supplemental material, along with statistical analysis codes, are available in a public repository: CTP, CD, SA, AA and MRRH (2023). Dataset and code for 'Magnitude and determinants of excess total, age-specific and sex-specific all-cause mortality in 24 countries worldwide during 2020 and 2021: results on the impact of the COVID-19 pandemic from the C-MOR project' (Data set). Zenodo. https://doi.org/10.5281/zenodo.8414193.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Yang L, Liu S, Liu J, et al. COVID-19: immunopathogenesis and immunotherapeutics. Sig Transduct Target Ther 2020;5:1–8. 10.1038/s41392-020-00243-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. NHS England . Landmark moment as first NHS patient receives COVID-19 vaccination. Available: https://www.england.nhs.uk/2020/12/landmark-moment-as-first-nhs-patient-receives-covid-19-vaccination/ [Accessed 07 Apr 2023].
- 3. Watson OJ, Barnsley G, Toor J, et al. Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect Dis 2022;22:1293–302. 10.1016/S1473-3099(22)00320-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mathieu E, Ritchie H, Rodés-Guirao L, et al. Coronavirus pandemic (COVID-19). Our world in data. 2020. Available: https://ourworldindata.org/coronavirus [Accessed 23 May 2023].
- 5. Organization WH . WHO COVID-19 dashboard. 2020. Available: https://covid19.who.int/ [Accessed 23 May 2023].
- 6. Michelozzi P, de’Donato F, Scortichini M, et al. Erratum: publisher correction to: temporal dynamics in total excess mortality and COVID-19 deaths in Italian cities. BMC Public Health 2020;20:1325. 10.1186/s12889-020-09398-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Félix-Cardoso J, Vasconcelos H, Rodrigues P, et al. Excess mortality during COVID-19 in five European countries and a critique of mortality analysis data. medRxiv 2020. 10.1101/2020.04.28.20083147 [DOI] [Google Scholar]
- 8. Tanne JH. Covid-19: at least two thirds of 225 000 excess deaths in US were due to virus. BMJ 2020;371:m3948. 10.1136/bmj.m3948 [DOI] [PubMed] [Google Scholar]
- 9. Woolf SH, Chapman DA, Sabo RT, et al. Excess deaths from COVID-19 and other causes, March-July 2020. JAMA 2020;324:1562. 10.1001/jama.2020.19545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Arons MM, Hatfield KM, Reddy SC, et al. Presymptomatic SARS-Cov-2 infections and transmission in a skilled nursing facility. N Engl J Med 2020;382:2081–90. 10.1056/NEJMoa2008457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Li R, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid dissemination of novel Coronavirus. Science 2020;368:489–93. 10.1126/science.abb3221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Quast T, Andel R, Gregory S, et al. Years of life lost associated with COVID-19 deaths in the USA during the first 2 years of the pandemic. J Public Health (Oxf) 2022;44:e353–8. 10.1093/pubmed/fdac057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vigliar E, Cepurnaite R, Alcaraz-Mateos E, et al. Global impact of the COVID-19 pandemic on cytopathology practice: results from an international survey of Laboratories in 23 countries. Cancer Cytopathol 2020;128:885–94. 10.1002/cncy.22373 [DOI] [PubMed] [Google Scholar]
- 14. Sofi F, Dinu M, Reboldi G, et al. Worldwide differences of hospitalization for ST-segment elevation myocardial infarction during COVID-19: a systematic review and meta-analysis. Int J Cardiol 2022;347:89–96. 10.1016/j.ijcard.2021.10.156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Demetriou CA, Achilleos S, Quattrocchi A, et al. Impact of the COVID-19 pandemic on total, Sexand age-specific all-Causemortality in 20 countries worldwide during 2020: results from the C-MOR project. Int J Epidemiol 2022;00:1–13. 10.1093/ije/dyac170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Achilleos S, Quattrocchi A, Gabel J, et al. Excess all-cause mortality and COVID-19-related mortality: a temporal analysis in 22 countries, from January until August 2020. Int J Epidemiol 2022;51:35–53. 10.1093/ije/dyab123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Beaney T, Clarke JM, Jain V, et al. Excess mortality: the gold standard in measuring the impact of COVID-19 worldwide? J R Soc Med 2020;113:329–34. 10.1177/0141076820956802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Leon DA, Shkolnikov VM, Smeeth L, et al. COVID-19: a need for real-time monitoring of weekly excess deaths. Lancet 2020;395:e81. 10.1016/S0140-6736(20)30933-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Islam N. Excess deaths” is the best metric for tracking the pandemic. BMJ 2022;376:o285. 10.1136/bmj.o285 [DOI] [PubMed] [Google Scholar]
- 20. Alicandro G, Remuzzi G, La Vecchia C. Italy ’ s first wave of the COVID-19 pandemic has ended: no excess mortality in May. Lancet 2020;396:e27–8. 10.1016/S0140-6736(20)31865-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bustos Sierra N, Bossuyt N, Braeye T, et al. All-cause mortality supports the COVID-19 mortality in Belgium and comparison with major fatal events of the last century. Arch Public Health 2020;78:117. 10.1186/s13690-020-00496-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Collaborators EM. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020-21. Lancet 2022;399:1513–36. 10.1016/S0140-6736(21)02796-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Aburto JM, Schöley J, Kashnitsky I, et al. Quantifying impacts of the COVID-19 pandemic through life-expectancy losses: a population-level study of 29 countries. Int J Epidemiol 2022;51:63–74. 10.1093/ije/dyab207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Islam N, Shkolnikov VM, Acosta RJ, et al. Excess deaths associated with COVID-19 pandemic in 2020: age and sex disaggregated time series analysis in 29 high income countries. BMJ 2021;373:n1137. 10.1136/bmj.n1137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pallari C, Demetriou CA, Achilleos S, et al. Data from: magnitude and determinants of excess total, Age- and sex-specific all-cause mortality in 24 countries worldwide during 2020 and 2021: results on the impact of the COVID-19 pandemic from the C-MOR project. Zenodo Repository 2023. Available: 10.5281/zenodo.8414193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Covid-19 - Inserm-CépiDc. Available: https://opendata.idf.inserm.fr/cepidc/covid-19/ [Accessed 08 Apr 2023].
- 27. Population, total | data. Available: https://data.worldbank.org/indicator/SP.POP.TOTL [Accessed 08 Apr 2023].
- 28. National life tables. UK: Office for National Statistics; Available: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/lifeexpectancies/datasets/nationallifetablesunitedkingdomreferencetables [Accessed 08 Apr 2023]. [Google Scholar]
- 29. Database - Eurostat. Available: https://ec.europa.eu/eurostat/web/main/data/database [Accessed 08 Apr 2023].
- 30. Ahmad OB, Boschi-Pinto C, Lopez AD, et al. Age standardization of rates: a new WHO standard. GPE discussion paper series: No31. Geneva: World Heal Organ; 2000. Available: http://www.who.int/healthinfo/paper31.pdf [Google Scholar]
- 31. Farrington CP, Andrews NJ, Beale AD, et al. A statistical algorithm for the early detection of outbreaks of infectious disease. J R Stat Soc Ser A (Stat Soc) 1996;159:547. 10.2307/2983331 [DOI] [Google Scholar]
- 32. Serfling RE. Methods for current statistical analysis of excess pneumonia-influenza deaths. Public Health Rep (1896) 1963;78:494–506. 10.2307/4591848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nielsen J, Krause TG, Mølbak K. Influenza-associated mortality determined from all-cause mortality, Denmark 2010/11-2016/17: the Flumomo model. Influenza Resp Viruses 2018;12:591–604. 10.1111/irv.12564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kontis V, Bennett JE, Rashid T, et al. Magnitude, demographics and dynamics of the effect of the first wave of the COVID-19 pandemic on all-cause mortality in 21 industrialized countries. Nat Med 2020;26:1919–28. 10.1038/s41591-020-1112-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Vestergaard LS, Nielsen J, Richter L, et al. Excess all-cause mortality during the COVID-19 pandemic in Europe – preliminary pooled estimates from the Euromomo network. Euro Surveill 2020;25. 10.2807/1560-7917.ES.2020.25.26.2001214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Nielsen J, Vestergaard LS, Richter L, et al. European all-cause excess and influenza-attributable mortality in the 2017/18 season: should the burden of influenza B be reconsidered. Clin Microbiol Infect 2019;25:1266–76. 10.1016/j.cmi.2019.02.011 [DOI] [PubMed] [Google Scholar]
- 37. Kneebone-Hopkins C, Artemiou A, Demetriou CA. Determinants of excess mortality during the COVID-19 pandemic in 18 countries of the CMOR consortium: christiana demetriou. Eur J Public Health 2022;32. 10.1093/eurpub/ckac129.278 [DOI] [Google Scholar]
- 38. Msemburi W, Karlinsky A, Knutson V, et al. The WHO estimates of excess mortality associated with the COVID-19 pandemic. Nature 2023;613:130–7. 10.1038/s41586-022-05522-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Schöley J. Robustness and bias of European excess death estimates in 2020 under varying model specifications. medRxiv 2021. 10.1101/2021.06.04.21258353 [DOI] [Google Scholar]
- 40. Nepomuceno MR, Klimkin I, Jdanov DA, et al. Sensitivity analysis of excess mortality due to the COVID-19 pandemic. Popul Dev Rev 2022;48:279–302. 10.1111/padr.12475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Karlinsky A, Kobak D. Tracking excess mortality across countries during the COVID-19 pandemic with the world mortality dataset. Elife 2021;10:e69336. 10.7554/eLife.69336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Moghadas SM, Vilches TN, Zhang K, et al. The impact of vaccination on Coronavirus disease 2019 (COVID-19) outbreaks in the United States. Clin Infect Dis 2021;73:2257–64. 10.1093/cid/ciab079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Sciensano . Belgian mortality monitoring. 2023. Available: https://epistat.sciensano.be/momo/ [Accessed 21 Oct 2023].
- 44. Our World in Data . Excess mortality during the Coronavirus pandemic (COVID-19). Available: https://ourworldindata.org/excess-mortality-covid [Accessed 07 Apr 2023].
- 45. Arolas Hp, Acosta E, Casasnovas GL, et al. Global years of life lost to COVID-19. SocArXiv 2020. 10.31219/OSF.IO/GVEAJ [DOI] [Google Scholar]
- 46. Ugarte MP, Achilleos S, Quattrocchi A, et al. Premature mortality attributable to COVID-19: potential years of life lost in 17 countries around the world, January–August 2020. BMC Public Health 2022;22:54. 10.1186/s12889-021-12377-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Peckham H, de Gruijter NM, Raine C, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun 2020;11:6317. 10.1038/s41467-020-19741-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hernandez I, Bakola M, Stuckler D. The impact of air pollution on COVID-19 incidence, severity, and mortality: a systematic review of studies in Europe and North America. Environ Res 2020:1–15. 10.1016/j.envres.2022.114155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Liang LL, Tseng CH, Ho HJ, et al. Covid-19 mortality is negatively associated with test number and government effectiveness. Sci Rep 2020;10:12567. 10.1038/s41598-020-68862-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Wu X, Nethery RC, Sabath MB, et al. Air pollution and COVID-19 mortality in the United States: strengths and limitations of an ecological regression analysis. Sci Adv 2020;6:1–7. 10.1126/sciadv.abd4049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sepulveda ER, Brooker AS. Income inequality and COVID-19 mortality: age-stratified analysis of 22 OECD countries. SSM - Popul Heal 2021;16:100904. 10.1016/j.ssmph.2021.100904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Chang D, Chang X, He Y, et al. The determinants of COVID-19 morbidity and mortality across countries. Sci Rep 2022;12:5888. 10.1038/s41598-022-09783-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Wang H, Paulson KR, Pease SA, et al. Appendix to “estimating excess mortality due to SARS-Cov-2 pandemic: a systematic analysis of COVID-19 mortality, 2020 – 2021". Lancet 2022;6736. 10.1016/S0140-6736(21)02796-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Zhou L, Puthenkalam JJ. Effects of the human development index on COVID-19 mortality rates in high-income countries. Eur J Dev Stud 2022;2:26–31. 10.24018/ejdevelop.2022.2.3.104 [DOI] [Google Scholar]
- 55. Levitt M, Zonta F, Ioannidis JPA. Comparison of pandemic excess mortality in 2020–2021 across different empirical calculations. Environ Res 2022;213:113754. 10.1016/j.envres.2022.113754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. De Nicola G, Kauermann G. An update on excess mortality in the second year of the COVID-19 pandemic in Germany. AStA Wirtsch Sozialstat Arch 2022;16:21–4. 10.1007/s11943-022-00303-9 [DOI] [Google Scholar]
- 57. Excess mortality and vaccination. 2022. Available: https://pandem-ic.com/excess-mortality-and-vaccination/ [Accessed 11 Apr 2023].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2023-013018supp001.pdf (4.5MB, pdf)
Data Availability Statement
Data are available in a public, open access repository. The data underlying this study, beyond what is available in the article and in its online supplemental material, along with statistical analysis codes, are available in a public repository: CTP, CD, SA, AA and MRRH (2023). Dataset and code for 'Magnitude and determinants of excess total, age-specific and sex-specific all-cause mortality in 24 countries worldwide during 2020 and 2021: results on the impact of the COVID-19 pandemic from the C-MOR project' (Data set). Zenodo. https://doi.org/10.5281/zenodo.8414193.