Abstract
Objective
During the first year of the COVID-19 pandemic, most of the Centers for Disease Control and Prevention (CDC)’s National Breast and Cervical Cancer Early Detection Program (NBCCEDP) funded programs (recipients) experienced significant declines in breast and cervical cancer screening volume. However, 6 recipients maintained breast and/or cervical cancer screening volume during July–December 2020 despite their states' high COVID-19 test percent positivity. We led a qualitative multi-case study to explore these recipients' actions that may have contributed to screening volume maintenance.
Methods
We conducted 22 key informant interviews with recipients, screening provider sites, and partner organizations. Interviews explored organizational and operational changes; screening barriers; actions taken to help maintain screening volume; and support for provider sites to continue screening. We documented contextual factors that may have influenced these actions, including program structures; clinic capacity; and state COVID-19 policies.
Results
Thematic analysis revealed crosscutting themes at the recipient, provider site, and partner levels. Recipients made changes to administrative processes to reduce burden on provider sites and delivered tailored technical assistance to support safe screening. Provider sites modified clinic protocols to increase patient safety, enhanced patient reminders for upcoming appointments, and increased patient education on the importance of timely screening during the pandemic. Partners worked with provider sites to identify and reduce patients' structural barriers to screening.
Conclusion
Study findings provide lessons learned to inform emergency preparedness-focused planning and operations, as well as routine operations for NBCCEDP recipient programs, other cancer screening initiatives, primary care clinics, and chronic disease prevention programs.
Keywords MeSH terms): Early detection of cancer; Uterine cervical neoplasms/prevention & control; Breast neoplasms/prevention & control; COVID-19; Centers for disease control and prevention, US; Chronic disease; Pandemics; Emergencies; Adult; Female
Highlights
-
•
The National Breast and Cervical Cancer Early Detection Program's screening volume declined during the COVID-19 pandemic.
-
•
However, six funding recipients maintained breast and/or cervical cancer screening volume during periods of high COVID-19.
-
•
These recipients changed processes to reduce provider site burden and delivered technical assistance on safe screening.
-
•
Provider sites modified clinic protocols to increase patient safety and education and enhance patient reminders.
-
•
Other partners worked with provider sites to identify and reduce patients' structural barriers to screening.
1. Introduction
The onset of the COVID-19 pandemic had a significant impact on health care utilization in the United States (US), with fewer people receiving care to prevent or detect chronic diseases, including cancer screening [1]. Screening is an effective strategy for prevention and early detection of breast and cervical cancer, substantially reducing cancer incidence and mortality [2,3]. However, cancer screening was significantly disrupted by the pandemic, resulting in an approximately 94 % decrease in both breast and cervical cancer screening during January–April 2020, as well as delayed diagnoses and treatment initiation [4,5]. In March 2020, institutions began postponing or canceling elective medical care, including screenings, to reduce the risk of COVID-19 transmission and reserve medical resources for COVID-19 patients [6]. Screening service delivery was also impacted by state-level stay-at-home policies, patients’ fear of COVID-19 exposure at medical sites, and other COVID-19-related barriers (e.g., lack of transportation, employment, and childcare) [7].
Researchers assessed not only the national impact of the COVID-19 pandemic, but its effect on screening within the Centers for Disease Control and Prevention (CDC)’s National Breast and Cervical Cancer Early Detection Program (NBCCEDP) [8]. The NBCCEDP funds all 50 state health departments the District of Columbia, 13 tribes or tribal organizations, 2 US territories, and 5 US-Affiliated Pacific Islands to provide breast and cervical cancer screening, diagnostic testing, and treatment referral to women in their jurisdictions who have low incomes and are under- or uninsured [9]. In April 2020, breast and cervical cancer screening volume among NBCCEDP funded programs (hereafter “recipients”) declined by 87 % and 84 %, respectively, compared with the previous 5-year average [8]. Subsequent research, examining the time frame during July–December 2020, revealed that 6 recipients successfully maintained their pre-COVID-19 breast and/or cervical cancer screening volume during their state-level periods of high COVID-19 test percent positivityi (hereafter “high COVID-19”) [10].
This paper describes results from a qualitative multi-case study exploring actions taken by these 6 recipients, their provider sites, and other partners (e.g., community-based organizations that promote and/or support the program), which may have contributed to recipients' ability to maintain their screening volume during July–December 2020 despite high rates of COVID-19. Our findings can be useful to NBCCEDP recipients, primary care clinics, other cancer screening initiatives, and chronic disease prevention programs by informing planning and operations during future public health emergencies.
2. Methods
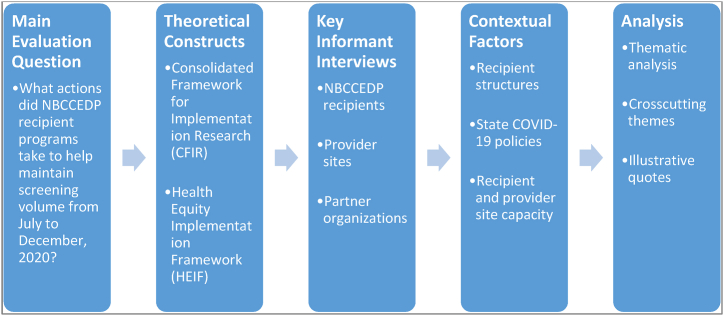
We used an exploratory, qualitative multi-case study evaluation design including key informant interviews. Case study designs recognize the complexity of program implementation in variable contexts and can be particularly effective when examining programs with unique outcomes in unpredictable environments [11]. In our methodological approach (Fig. 1), each NBCCEDP funded program, or recipient, was examined as a unique case.
Fig. 1.
Methodological Approach. Note: Color not essential for figure in print. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
2.1. Site selection
Recipients. We purposefully sampled the 6 NBCCEDP recipients that maintained breast and/or cervical cancer screening despite high COVID-19 during July–December 2020 [10]. Recipients included Arkansas BreastCare, Iowa Care for Yourself, Kansas Early Detection Works, Nevada Women’s Health Connection, South Carolina Best Chance Network, and Tennessee Breast and Cervical Screening Program. Two recipients maintained breast and cervical cancer screening, 3 maintained cervical only, and 1 maintained breast only.
Provider sites. Provider sites are defined as primary care or other clinic sites delivering clinical services, and facilities offering breast screening and diagnostic testing [9,12]. The number of provider sites in each recipient program ranged from 90 to 382. Screening volume varied across provider sites; therefore, we first conducted a rank analysis comparing site-specific screening and diagnostic data from July to December 2020 to the previous 5-year average for those months. We then interviewed representatives from 1 to 2 provider sites from each recipient program that ranked high compared to the other provider sites.
Partners. We defined partners as local organizations providing substantial support to the recipient and/or provider sites to help maintain screening volume during the study period. Partner services included: grassroots community outreach; patient navigation; and maintaining screening provider networks to ensure patient access to care. We interviewed representatives from 1–2partners per recipient based on their or their provider sites' recommendations.
2.2. Guiding frameworks
The Consolidated Framework for Implementation Research (CFIR) and the Health Equity Implementation Framework (HEIF), both part of implementation science, guided our approach. CFIR is one of the most used frameworks for examining contextual factors, barriers, and facilitators that influence program implementation to explain what works, where, and why [13,14]. HEIF merges implementation science with health care disparities science, allowing researchers to better understand how health equity determinants affect program implementation at multiple levels [15]. We aligned relevant constructs with our evaluation questions to structure data collection by respondent role (Table 1).
Table 1.
Evaluation questions aligned with CFIR and HEIF constructs.
| Evaluation Question | Aligned Theoretical Constructs & Definitions | Respondent Role |
|---|---|---|
| What actions did programs take to help maintain screening volume during this 6-month period? |
Process: Planninga The degree to which a scheme or method of behavior—and tasks for implementing an intervention—are developed in advance, and the quality of those schemes or methods. Process: Executinga Carrying out or accomplishing the implementation according to plan. |
Recipient Provider Site Partner |
| What facilitators helped provider sites maintain breast and/or cervical cancer screening volume during this 6-month period? |
Outer Setting: External Policies and Incentives* External strategies to spread interventions, including policy and regulations (governmental or other central entity), external mandates, recommendations and guidelines, pay-for-performance, collaboratives, and public or benchmark reporting. Inner Setting: Structural Characteristicsa The social architecture, age, maturity, and size of an organization. |
Provider Site |
| What barriers threatened provider sites' ability to maintain breast and/or cervical cancer screening volume during this 6-month period? |
Outer Setting: External Policies and Incentivesa Inner Setting: Structural Characteristicsa Recipients: Patient Factorsb Patient beliefs, preferences for treatment, culture and community strengths or limitations, health literacy, and biology. Recipients: Provider Factorsb Health care provider knowledge about a vulnerable group, attitudes or bias toward that group, and competing demands. |
Provider Site |
| How did recipient programs' structures and operations change during the 6-month period? |
Inner Setting: Structural Characteristicsa Process: Executinga Intervention Characteristics: Adaptabilitya Degree to which an intervention can be adapted, tailored, refined, or reinvented to meet local needs. |
Recipient |
| How did provider site structure and operations change during this 6-month period? |
Process: Executinga Intervention Characteristics: Adaptabilitya Process: Championsa People who dedicate themselves to supporting, marketing, or ‘driving through an implementation,’ thus overcoming indifference or resistance that the intervention may provoke in an organization. Inner Setting: Leadership Engagementa Commitment, involvement, and accountability of leaders and managers with the implementation. |
Provider Site |
| What support was provided to recipients and provider sites to help maintain screening volume during this 6-month period? |
Inner Setting: Networks and Communicationsa The nature and quality of webs of social networks and the nature and quality of formal and informal communications within an organization. Readiness for Implementation: Available Resourcesa The level of resources dedicated for implementation and ongoing operations, including money, training, education, physical space, and time. |
Recipient Provider Site Partner |
| What was the reach of these programs during this 6-month period? |
Outer Setting: Patient Needs and Resourcesa Extent to which patient needs, as well as barriers and facilitators to meet those needs, are accurately known and prioritized by the organization. Process: Executinga Recipients: Patient Factorsb Recipients: Provider Factorsb |
Recipient Provider Site |
CFIR construct.
HEIF construct.
2.3. Data collection
To inform data collection, we compiled (prior to interviews) NBCCEDP and publicly available data to capture contextual factors that may have influenced recipients' ability to maintain screening volume. Sources included NBCCEDP data reports (e.g., annual survey, quarterly progress reports), CDC COVID Data Tracker [16], and Kaiser Family Foundation state COVID-19 data and policy actions database [17].
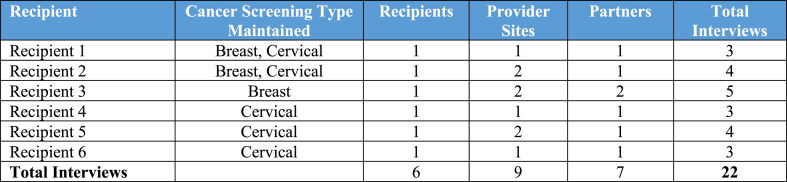
During April–December 2022, we conducted 22 interviews with representatives from 6 recipients, 9 provider sites, and 7 partners (Table 2). Interviews lasted 45–60 min and explored respondent role; organizational and operational changes; barriers and facilitators to maintaining screening; actions to help maintain screening levels; and support provided or received to continue screening. Each interview was conducted by an interviewer and notetaker. We obtained verbal consent from each respondent. All interviews were audio recorded, and detailed notes were captured and analyzed. CDC’s Institutional Review Board determined this study did not constitute human subjects research.
Table 2.
Total Number of Interviews Conducted Among Recipients, Provider Sites, and Partners.
2.4. Analysis
We used rapid qualitative analysis (RQA) to identify emerging themes across recipient programs. RQA is an effective, efficient method for identifying relevant themes using systematic approaches other than line-by-line coding of verbatim transcripts [18,19]. We used highly structured tools (e.g., detailed notetaking template; analysis matrix) to ensure systematic analysis. A primary and secondary analyst were designated for each respondent’s data. The primary analyst reviewed interview responses across respondent types and developed program-specific theme tables with illustrative quotes. The secondary analyst reviewed theme tables and met with the primary analyst to reach consensus on themes. All analysts met to identify and refine crosscutting themes, defined as having relevance across 2 or more recipients and supported by 2 or more respondent types. We considered contextual data to further enhance our understanding of crosscutting themes.
3. Results
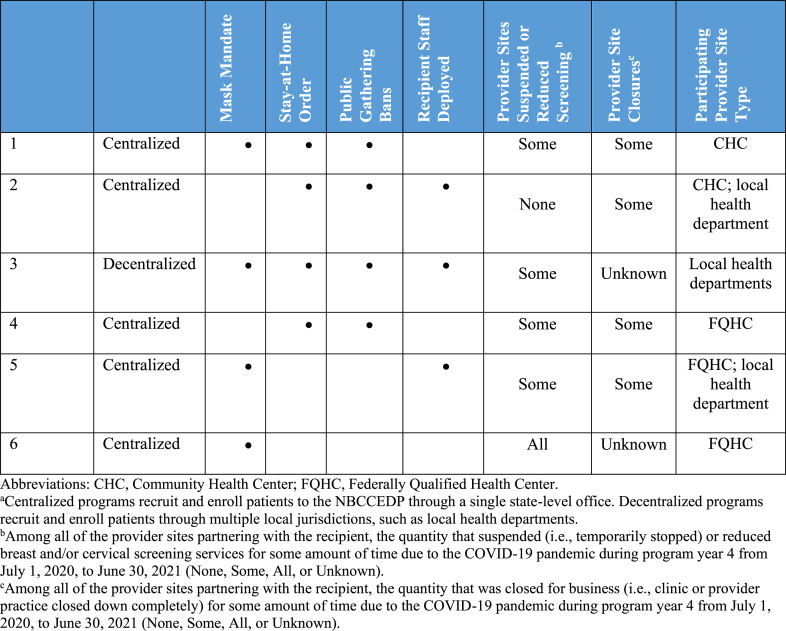
We considered 8 contextual factors that may have influenced screening volume maintenance for 1 or more months during the study period (Table 3). These factors related to the external environments within which recipients operated (i.e., state COVID-19 policies including mask mandates, stay-at-home orders, public gathering bans) and internal operations (i.e., recipient program structures; recipient and provider site capacity such as staff deployments, suspended or reduced screening, and provider site types and closures) that may have influenced program activities.
Table 3.
Contextual Factors by Recipient. Abbreviations: CHC, Community Health Center; FQHC, Federally Qualified Health Center. aCentralized programs recruit and enroll patients to the NBCCEDP through a single state-level office. Decentralized programs recruit and enroll patients through multiple local jurisdictions, such as local health departments. bAmong all of the provider sites partnering with the recipient, the quantity that suspended (i.e., temporarily stopped) or reduced breast and/or cervical screening services for some amount of time due to the COVID-19 pandemic during program year 4 from July 1, 2020, to June 30, 2021 (None, Some, All, or Unknown). cAmong all of the provider sites partnering with the recipient, the quantity that was closed for business (i.e., clinic or provider practice closed down completely) for some amount of time due to the COVID-19 pandemic during program year 4 from July 1, 2020, to June 30, 2021 (None, Some, All, or Unknown).
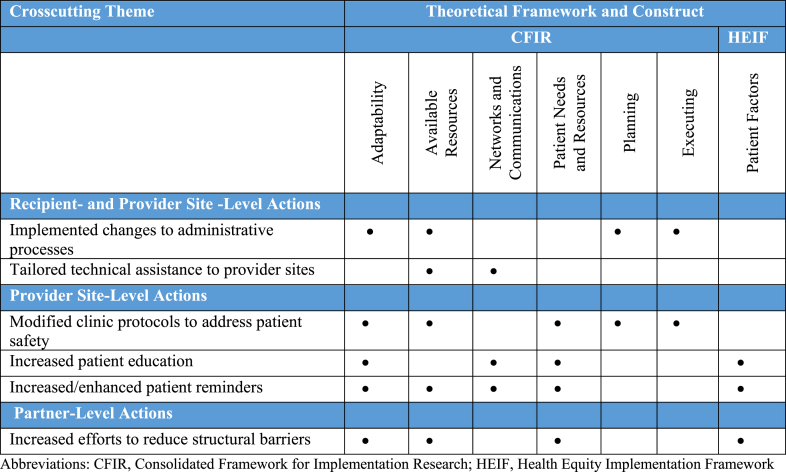
Six crosscutting themes, representing actions to support breast and/or cervical cancer screening during the study period, emerged from interviews. Table 4 organizes themes by respondent type and aligned with relevant CFIR and HEIF constructs.
Table 4.
Overview of Crosscutting Themes by CFIR and HEIF Construct. Abbreviations: CFIR, Consolidated Framework for Implementation Research; HEIF, Health Equity Implementation Framework.
3.1. Recipient- and provider site-level actions
3.1.1. Implemented changes to administrative processes
Five recipients adapted their program’s administrative processes to reduce burden on state-level staff and provider sites. Respondents described actions to alleviate barriers to securing or using annual funding, such as helping sites complete continuation applications so clinic staff could devote more time to providing patient care; transferring unspent funds into mini-grants for provider sites' use towards screening promotion; issuing additional funds to provider sites to support continued clinic operations; and consolidating recipient staff roles to increase efficiencies and simplify patient enrollment processes (e.g., combining billing and data specialist roles to conduct 1 patient application review vs 2).
Several respondents discussed eliminating barriers to NBCCEDP enrollment. One respondent revised their patient enrollment process to enable direct enrollment by designated provider site staff (e.g., program coordinator) instead of requiring referral submission and approval by the recipient. Another respondent reported partnering with mammography sites to enroll new patients and provide screening during the initial visit. A provider site respondent highlighted this important change: “Being able to provide services same day and not having to have them come back made a big difference, lessened barriers to transportation; they didn’t have to go anywhere else for it because they were already there.” Another respondent noted removing a requirement to re-enroll patients every 6 months, which allowed patients due for screening to get an appointment quickly with less administrative burden.
Several provider sites relaxed scheduling parameters, allowing scheduling for sick and well visits at any time (vs designated time slots) and triple-booking appointments to account for no-shows.
3.1.2. Provided tailored technical assistance to provider sites
Five recipients reported offering tailored technical assistance (TA) to provider sites to help maintain screening. TA focused on each provider sites' individual challenges (e.g., electronic health record optimization, contract management, and implementing safe screening guidelines). One recipient described:
We just worked with them [provider sites]. I hate to say it because it’s overstated, but we were all in it together. We were all trying to get through it and continue addressing the breast and cervical screening needs of [state]. (Recipient respondent)
Recipients also shared general screening and chronic disease prevention messaging from their state health department and lessons learned across provider sites to facilitate peer learning.
3.2. Provider-site level actions
3.2.1. Modified clinic protocols to address patient safety
Four provider sites reported using safety measures to protect patients and clinic staff from COVID-19 transmission and reduce patient fears of in-person clinic visits. Respondents described provider sites' policies requiring COVID-19 mitigation strategies, including masks and other personal protective equipment for patients and staff; social distancing in clinic waiting areas and on mobile mammography vans; sanitization and/or disinfecting protocols; air filtration system installation; and separate waiting rooms, treatment areas, and entrances/exits for suspected COVID-19 patients. Two provider sites offered COVID-19 safety protocol training to ensure staff were confident implementing safe screening guidelines and communicating safety protocols to patients. One respondent emphasized sites’ focus on helping patients feel safe visiting the clinic for screening:
I feel like at that time we were pushing really hard to say, it's okay, you need to get this [screening] done and we will protect you when you're here. We will do everything we can to make you safe when you come in to get your screening test. So, I feel like that's probably the best that we could have done. And it's what we did, and our numbers show that we were able to continue screening. (Partner respondent)
One provider site discussed the importance of social distancing in mobile mammography vans to screen patients who feared entering the clinic:
… the idea of going into a brick-and-mortar building, sitting in a waiting area with all these other people, not knowing who's been exposed, who currently is … sick. That's what helped promote the idea of the mobile van. Knowing that you're the only woman on that van at the time that you go, there's no waiting area. (Provider site respondent)
Respondents reported minimizing in-person contact through remote completion of certain intake processes before appointments. Provider sites screened patients for COVID-19 symptoms via phone and advised symptomatic patients not to visit the clinic; obtained patients’ verbal consent to receive medical services via phone instead of in person; gathered patient health information via phone to shorten patient intake; and implemented a text-based system for appointment check-in to minimize the number of patients in the waiting room.
Several provider sites delivered non-screening-related services in the clinic parking lot or in patient vehicles whenever possible to reduce COVID-19 exposure risk and to alleviate patients’ fears about entering the clinic.
3.2.2. Enhanced patient reminders
Four provider sites discussed enhancing patient reminders to help maintain screening, including updating patient reminder protocols to increase the number of attempts to reach patients and/or using more methods to deliver patient reminders (e.g., phone calls and text reminders vs texts only). One respondent stressed the importance of increased attempts to deliver reminders:
I said [to call center staff], “I don’t care what you have to do, but get them in here,” and we did, and it started to pick up a little bit … The only thing that works is being persistent and continuously making those calls. (Provider site respondent)
Another respondent changed their call center phone number from a 1–800 number to a local number to promote familiarity to patients, which carried no costs and resulted in more successful contact attempts.
Sites also reported enhancing patient reminder content with information about what to expect during their visit, including describing the clinic’s COVID-19 safety measures and confirming co-payment coverage.
3.2.3. Increased patient education
Four provider sites increased patient education on the importance of staying up to date with cancer screening during the COVID-19 pandemic and the rationale behind the clinics' COVID-19 safety measures. Some sites disseminated educational information through social media or “on-hold” messages that patients heard when they called the provider site. One respondent described their “Rack Card,” a pamphlet for patients that corrected COVID-19 myths with accurate facts.
3.3. Partner-level actions
3.3.1. Increased efforts to reduce patients' structural barriers
Four partners reported using their existing knowledge of the communities served and working closely with provider sites to identify and reduce patients' barriers to care. One respondent stated: “I think it’s just keeping very open communication on both ends—both the provider end and the patient end—so we can identify barriers and work on eliminating them.” Another respondent highlighted the essential role of care coordinators familiar with the community served for understanding and addressing patients' barriers: “[Care coordinators] assisted those providers in breaking down the barrier of fear for patients, which I honestly think was the biggest thing that was stopping patients from getting their services at that time.”
Several respondents mentioned meeting patients’ increased transportation needs. Several partners provided gas cards; funds for public transportation or taxis; and rideshare services to help patients travel to the clinic. A few partners worked to maintain a strong network of screening providers to facilitate patient access to local providers. Respondents also increased promotion of partner-led mobile mammography events, which patients without transportation could access more easily.
Several partners worked with provider sites to reduce other patient barriers to screening, such as added language translation services to ensure effective communication with patients. One respondent described their organization’s initiative “Miles and Minutes,” which provided patients with a cellular phone and pre-paid minutes to ensure stable communication before and after visits. Partners also increased efforts to address patients' basic housing and food security needs.
4. Discussion
The 6 NBCCEDPs in this study operated within unique contexts that influenced the ability to maintain cancer screening volume. During the study period, all recipients experienced clinic closures and/or suspension or reduction of screening services among some of their clinics; however, these provider sites were operating and therefore were able to provide in-person routine screening services. While we did not identify themes that were unique to maintaining either breast or cervical screening volume, findings demonstrate the value of recipients, provider sites, and partners working collaboratively to mitigate the impact of the COVID-19 pandemic and continue screening. This study benefitted from use of relevant CFIR and HEIF constructs to help frame our examination of individual programs’ characteristics and actions while identifying crosscutting themes.
Recipients and provider sites largely focused on simplifying administrative processes, thereby reducing burden on frontline provider site staff overwhelmed by pandemic-related demands. These adjustments highlight the importance of adaptability within a public health initiative. Adaptability is a key characteristic of a resilient health system, allowing the system to respond to emergent challenges with organizational and management changes that increase efficiency and productivity [20]. Programs nimbly adjusted: staff assignments; funding allocation-related practices; NBCCEDP referral and enrollment processes; and scheduling parameters to help provider sites continue screening. During public health emergencies, state-level cancer screening programs and other chronic disease prevention initiatives may benefit from promoting adaptability in administrative structures and processes (e.g., develop flexible protocols that minimize steps for patient enrollment).
During the study period, many people feared contracting COVID-19 during health care visits. Therefore, it was essential to minimize patients' exposure risk, to calm fears of COVID-19 transmission. Provider sites focused on increasing support to help patients feel safe when entering the clinic. Enhanced patient reminders, a strategy proven effective in increasing breast and cervical cancer screening prevalence [21,22], included expanding the types and numbers of reminders as well as the information and support for patients prior to their appointments. Our findings demonstrate the lengths that provider sites went to in ensuring that patients understood clinic safety protocols and felt safe entering the clinic. This was partly due to highly passionate and dedicated staff who carried out increased duties. Previous research has noted the ability of clinic staff to overcome COVID-19-related capacity limitations by remaining flexible and being creative to reach patients [8]. Future research can explore how provider sites could shift resources towards these increased efforts despite reduced capacity.
Partners—whose role in supporting screening efforts ranged from grassroots promotion and patient recruitment to directly facilitating screening services—used their knowledge, relationships, and experience in communities to address patient factors related to social determinants of health (SDOH) by addressing barriers (transportation, language, finances) to screening. Research shows that patients with SDOH-related factors resulting in poor health outcomes (e.g., inadequate or no health insurance and/or a low income) are less likely to seek cancer screening [4]. Additional stressors caused by the COVID-19 pandemic (e.g., job loss, caring for ill family members) may have further exacerbated cancer disparities among patients already experiencing health inequities [4,23]. Given an existing focus on achieving health equity in breast and cervical cancer screening, NBCCEDP recipients and their partners were well positioned to work together to build on existing practices that identify and reduce patients’ barriers to care. This ongoing focus on health equity is a programmatic strength and may benefit other health programs addressing SDOH in future public health emergencies.
Despite both recipients and provider sites being asked to reflect on TA they provided or received, TA was discussed much more among recipients compared to provider sites. There are a few possible explanations for this unexpected finding. Provider sites already maintaining screening volume may not have requested individualized support from recipients, and broad TA efforts across all sites may not have resonated with these provider sites if general guidance was unneeded. Alternatively, provider sites may not have identified recipients' support activities as TA, given differing terms and environments between the 2 respondent types. Additional research may explore optimal strategies for identifying and responding to the TA needs of provider sites during strained times, especially among those unable to maintain screening volume.
Of note, these 6 programs implemented both permanent adaptations to increase efficiency and temporary solutions to continue providing high-quality patient care. Lessons learned from this study include the importance of considering both short- and long-term solutions to increase efficiency and support patient care when facing significant unexpected challenges. Researchers may choose to explore both short- and long-term TA needs and preferences, and promising strategies for state screening programs to best support clinics in dedicating time and resources to screening promotion and completion. Future program planning may emphasize strengthening and sustaining those adaptations that prove effective in helping maintain or increase screening volume over time.
There are some limitations to acknowledge. First, we are unsure whether the actions of these 6 recipient programs are unique. Because we did not examine other NBCCEDP funded programs that could not maintain screening volume during periods of high COVID-19, it is possible that some may have used similar strategies. Second, to manage the study’s scope, we considered a limited number of contextual factors. However, additional factors likely influenced how these programs maintained screening during the study period. Third, findings reflect a small subset of NBCCEDP recipients and therefore cannot be generalized across NBCCEDP or breast and cervical cancer screening programs overall. Fourth, within each recipient program, we spoke to a small subset of provider sites that may not reflect all actions taken by provider sites statewide.
Using theoretical frameworks focused on implementation and health equity science, this study explored actions taken by select NBCCEDP recipients, provider sites, and partners able to maintain breast and/or cervical cancer screening volume during periods of high COVID-19. Results offer insights into strategies to maintain cancer screening; the importance of recipients, provider sites, and partners collaborating to address pandemic-related challenges; and the need to respond to patients’ varying circumstances to provide high-quality care. Ultimately, many of the observed strategies are not specific to breast or cervical cancer screening and therefore may inform both routine and emergency preparedness-focused planning for chronic disease prevention.
Funding statement
No financial support was received for this study.
Ethics statement
The CDC Institutional Review Board determined that this study did not constitute human subjects research and therefore did not require review. All participants provided informed consent to participate in the study.
This manuscript was not previously published, either in whole or in part, nor have the findings been posted online. No copyrighted materials, surveys, instruments, or tools were used for this study. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Data availability statement
Data associated with this study have not been deposited into a publicly available repository in order to protect participants' confidentiality. Given the named locations and limited potential participants - particularly among recipient sites - respondents may be identifiable even from de-identified transcripts.
CRediT authorship contribution statement
Dara Schlueter: Resources, Methodology, Conceptualization, Formal analysis, Investigation, Supervision, Writing – original draft, Writing – review & editing. Yamisha Bermudez: Writing – review & editing, Writing – original draft, Resources, Methodology, Investigation, Conceptualization, Formal analysis. Karen F. Debrot: Writing – review & editing, Resources, Methodology, Investigation, Formal analysis, Conceptualization. Leslie W. Ross: Formal analysis, Conceptualization, Investigation, Methodology, Resources, Writing – original draft, Writing – review & editing. Manal Masud: Conceptualization, Writing – review & editing. Stephanie Melillo: Writing – review & editing, Conceptualization. Peggy A. Hannon: Writing – review & editing, Conceptualization. Jacqueline W. Miller: Writing – review & editing, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to express appreciation to all the individuals who participated in qualitative interviews for this study, including staff from Arkansas Department of Health, Community Clinic Rogers Medical, Arkansas Cancer Coalition, Iowa Department of Health and Human Services, Black Hawk County Health Department, Polk County Health Department, People Community Health Center, MercyOne Mammography, Kansas Department of Health and Environment, Salina Health Education Foundation, Sedgwick County Health Department Kansas Healthcare Collaborative, Nevada Department of Health and Human Services, Guadalupe Medical Center, Access to Healthcare Network, South Department of Health and Environmental Control, HopeHealth Inc., South Carolina Rural Health Tennessee Department of Health, Johnson City Community Clinic, Knox County Health Department, Church Health. We would also like to thank colleagues in the Division of Cancer Prevention and Control for their insights to inform this study.
Footnotes
Test percent positivity was calculated for each state by dividing the cumulative number of positive COVID-19 tests by the total number of tests performed per month and multiplying that quotient by 100.
References
- 1.Hacker K.A., Briss P.A., Richardson L., Wright J., Petersen R. COVID-19 and chronic disease: the impact now and in the future. Prev. Chronic Dis. 2021;18:E62. doi: 10.5888/pcd18.210086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Curry S.J., Krist A.H., Owens D.K., Barry M.J., Caughey A.B., Davidson K.W., et al. Screening for cervical cancer: US preventive services task force recommendation statement. JAMA. 2018;320(7):674–686. doi: 10.1001/jama.2018.10897. [DOI] [PubMed] [Google Scholar]
- 3.Siu A.L., US Preventive Services Task Force Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 2016;164(4):279–296. doi: 10.7326/M15-2886. [DOI] [PubMed] [Google Scholar]
- 4.Cancino R.S., Su Z., Mesa R., Tomlinson G.E., Wang J. The impact of COVID-19 on cancer screening: challenges and opportunities. JMIR Cancer. 2020;6(2) doi: 10.2196/21697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Center for Medicare and Medicaid Services Non-emergent, elective medical services, and treatment recommendations. 2020. https://www.cms.gov/files/document/cms-non-emergent-elective-medical-recommendations.pdf
- 6.Carethers J.M., Sengupta R., Blakey R., Ribas A., D'Souza G. Disparities in cancer prevention in the COVID-19 era. Cancer Prev. Res. 2020;13(11):893–896. doi: 10.1158/1940-6207.CAPR-20-0447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Epic Health Research Network Delayed cancer screenings. 2020. https://epicresearch.org/articles/delays-in-preventive-cancer-screenings-during-covid-19-pandemic/
- 8.DeGroff A., Miller J., Sharma K., Sun J., Helsel W., Kammerer W., et al. COVID-19 impact on screening test volume through the national breast and cervical cancer early detection program, January-June 2020, in the United States. Prev. Med. 2021;151 doi: 10.1016/j.ypmed.2021.106559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. National Breast and Cervical Cancer Early Detection Program. Accessed May 9, 2023. https://www.cdc.gov/cancer/nbccedp/.
- 10.Bermudez Y., Scott L.C., Beckman M., DeGroff A., Kenney K., Sun J., et al. Geographic examination of COVID-19 test percent positivity and proportional change in cancer screening volume, national breast and cervical cancer early detection program. Prev. Chronic Dis. 2022;19:E59. doi: 10.5888/pcd19.220111. PMID: 36108291; PMCID: PMC9480839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Balbach E.D. California Department of Health Services; 1999. Using Case Studies to Do Program Evaluation.https://www.betterevaluation.org/sites/default/files/ProgramEvaluation.pdf [Google Scholar]
- 12.Tangka F., Kenny K., Miller J., Howard D.H. The eligibility and reach of the national breast and cervical cancer early detection program after implementation of the affordable care act. Cancer Causes Control. 2020;31(5):473–489. doi: 10.1007/s10552-020-01286-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Damschroder L.J., Aron D.C., Keith R.E., Kirsh S.R., Alexander J.A., Lowery J.C. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement. Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Damschroder L.J., Reardon C.M., Widerquist M.A.O., Lowery J. The updated Consolidated Framework for Implementation Research based on user feedback. Implement. Sci. 2022;17:75. doi: 10.1186/s13012-022-01245-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Woodward E.N., Matthieu M.M., Uchendu U.S., Rogal S., Kirchner J.E. The health equity implementation framework: proposal and preliminary study of hepatitis C virus treatment. Implement. Sci. 2019;14:26. doi: 10.1186/s13012-019-0861-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. COVID Data Tracker. Accessed June 8, 2022. https://covid.cdc.gov/covid-data-tracker.
- 17.Kaiser Family Foundation. State COVID-19 Data and Policy Actions. Accessed June 8, 2023 from https://www.kff.org/other/state-indicator/state-actions-to-mitigate-the-spread-of-covid-19/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D.
- 18.Hamilton A. Spotlight on Women’s Health; 2013, December 13. Qualitative Methods In Rapid Turnaround Health Services Research [Cyber Seminar]. VA HSR&D Cyberseminar.https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/video_archive.cfm?SessionID=780 [Google Scholar]
- 19.Gale R.C., Wu J., Erhardt T., Bounthavong M., Reardon C.M., Damschroder L.J., et al. Comparison of rapid vs in-depth qualitative analytic methods from a process evaluation of academic detailing in the Veterans Health Administration. Implement. Sci. 2019;14:11. doi: 10.1186/s13012-019-0853-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kruk M.E., Myers M., Varpilah S.T., Dahn B.T. What is a resilient health system? Lessons from Ebola. Lancet. 2015;385(9980):1910–1912. doi: 10.1016/S0140-6736(15)60755-3. [DOI] [PubMed] [Google Scholar]
- 21.Guide to Community Preventive Services Cancer screening: client reminders – breast cancer. 2010. https://www.thecommunityguide.org/findings/cancer-screening-client-reminders-breast-cancer
- 22.Guide to Community Preventive Services Cancer screening: client reminders – cervical cancer. 2010. https://www.thecommunityguide.org/findings/cancer-screening-client-reminders-cervical-cancer
- 23.Centers for Disease Control and Prevention. Sharp declines in breast and cervical cancer screening [press release]. Accessed July 7, 2023. https://www.cdc.gov/media/releases/2021/p0630-cancer-screenings.html.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data associated with this study have not been deposited into a publicly available repository in order to protect participants' confidentiality. Given the named locations and limited potential participants - particularly among recipient sites - respondents may be identifiable even from de-identified transcripts.