Abstract
This review article examines the utility of artificial intelligence (AI) in anesthesia, with a focus on recent developments and future directions in the field. A total of 19,300 articles were available on the given topic after searching in the above mentioned databases, and after choosing the custom range of years from 2015 to 2023 as an inclusion component, only 12,100 remained. 5,720 articles remained after eliminating non-full text. Eighteen papers were identified to meet the inclusion criteria for the review after applying the inclusion and exclusion criteria. The applications of AI in anesthesia after studying the articles were in favor of the use of AI as it enhanced or equaled human judgment in drug dose decision and reduced mortality by early detection. Two studies tried to formulate prediction models, current techniques, and limitations of AI; ten studies are mainly focused on pain and complications such as hypotension, with a P value of <0.05; three studies tried to formulate patient outcomes with the help of AI; and three studies are mainly focusing on how drug dose delivery is calculated (median: 1.1% ± 0.5) safely and given to the patients with applications of AI. In conclusion, the use of AI in anesthesia has the potential to revolutionize the field and improve patient outcomes. AI algorithms can accurately predict patient outcomes and anesthesia dosing, as well as monitor patients during surgery in real time. These technologies can help anesthesiologists make more informed decisions, increase efficiency, and reduce costs. However, the implementation of AI in anesthesia also presents challenges, such as the need to address issues of bias and privacy. As the field continues to evolve, it will be important to carefully consider the ethical implications of AI in anesthesia and ensure that these technologies are used in a responsible and transparent manner.
Keywords: Anesthesia, applications, artificial intelligence
Introduction
Artificial intelligence (AI) is a field of computer science that focuses on creating systems or machines capable of performing tasks that typically require human intelligence. These tasks include reasoning, problem-solving, learning from data, understanding natural language, and making decisions.[1,2] AI systems use algorithms and computational models to simulate human cognitive functions, enabling them to analyze large datasets, recognize patterns, and make predictions or recommendations. AI is a rapidly evolving technology that can transform healthcare delivery. Machine learning (ML), fuzzy logic, and neural networks are the methods used to train the model and obtain the desired output, which performs complex calculations and mimics the function of the brain.[3,4,5] In the field of anesthesia, AI has the potential to improve patient outcomes, reduce healthcare costs, and enhance the efficiency of anesthesia care delivery. The use of AI in anesthesia is still in its infancy, but there is growing interest in exploring its potential applications.[5,6]
AI in anesthesia can help treat physicians and surgeons in multiple areas, such as patient monitoring; artificial software analyzes multiple streams of data, such as electrocardiogram (ECG) signals, blood pressure readings, and respiratory rate, to detect changes that may be indicative of an adverse event and alert treating physicians, allowing for swift and appropriate intervention.[7,8,9] AI can also be used to optimize the delivery of anesthetic agents based on patient characteristics and surgical requirements; the algorithms take into account several factors such as patient age, weight, medical history, and comorbidities, as well as the type and duration of surgery, to determine the optimal anesthetic plan. This can help ensure that patients receive safe and effective anesthesia care while minimizing the risk of adverse events.[10,11] AI algorithms can analyze patient data to predict the risk of postoperative complications such as respiratory failure, acute kidney injury, or delirium.[12,13,14] This can help anesthesia providers identify patients requiring additional monitoring or interventions and tailor their care accordingly by recommending the optimal anesthetic plan based on patient characteristics and surgical requirements. AI algorithms can recommend the appropriate anesthetic agent, dosage, and delivery method based on patient age, weight, medical history, and comorbidities. This can help to standardize anesthesia care and reduce the risk of human error.[15]
While the use of AI in anesthesia holds great promise, this technology has challenges and limitations. These include the need for high-quality data, the potential for bias and error, and the ethical and regulatory considerations that must be addressed. As AI continues to evolve, we will likely see further advancements in anesthesia care that leverage the power of this technology. Instead of replacing human judgment, anesthesiology should prioritize the doctor–patient connection and be utilized to aid physicians in making decisions.[16]
This review aims to provide an overview of the field’s current state, including the various ways in which AI is being used in anesthesia, the benefits and limitations of this technology, and future directions for research and development.
Methodology
The methodology for the research review article on the utility of AI in anesthesia involved a comprehensive literature search of various databases, including PubMed and Google Scholar. The search was conducted using a combination of keywords such as “AI,” “anesthesia,” “patient monitoring,” “drug dosing,” and “decision-making.” MK and ST retrieved and screened all the records, and any concerns were resolved through discussion and a third reviewer, SJ.[17]
The Population, Intervention, Comparison, Outcomes, and Study (PICOS) used for the review are as follows:
The proper dosage of medication administered to a patient undergoing anesthesia during surgery is essential to a safe and successful anesthetic experience. Drug dosages have typically been decided by human judgment, based on the training and experience of the anesthesiologist. However, there may be a change in the way medication dosages are determined and given as a result of the incorporation of AI into medical procedures.[18]
A major development in medical technology is the incorporation of AI into surgical patient monitoring. There are a number of possible advantages and factors to take into account when comparing AI-based monitoring to conventional human monitoring in terms of patient outcomes.[19]
Exclusion criteria
There are some specific standards that specify which subjects or studies are not taken into account within the parameters of the research, and they are found in manuscripts on the application of AI in anesthesia and were excluded from the study. Studies or applications of AI that were not directly related to the field of anesthesia were excluded. Studies conducted on animals or experiments that do not have direct implications for human anesthesia practices were not involved. Studies that primarily involve patient populations not typically associated with anesthesia, such as pediatric, high-risk, vulnerable patients, and obstetric populations, if the focus is on adult general anesthesia, were excluded. The studies conducted focusing on outdated or obsolete AI technologies that are no longer relevant to current anesthesia practices were not included.[20]
Inclusion criteria
The inclusion criteria for the manuscript are as follows: The studies that have included the use of anesthetic drugs are involved. Also, participants who received general anesthesia techniques are only included. Patients posted for elective surgery are included in the given study.
Screening and data extraction
Two independent reviewers, MK and ST, conducted duplicate title and abstract screening and full-text review to identify eligible studies. Two reviewers completed data extraction independently and in duplicate, and a third reviewer, SJ, verified the data. All disagreements were resolved by the group consensus.
We extracted the following information:
Characteristics of the enrolled population at the baseline and summary of the eligible trials, including study ID (last name of first author or publication year), study arms, region, mean age, surgery type, type of anesthesia, conversion of anesthesia, a dose of the drug, type of AI, P value of increased efficiency, P value of post-op complications, area under the curve (AUC) of the studies, inclusion and exclusion criteria of eligible studies, primary endpoints, and conclusions.[21,22]
Outcomes: efficiency of AI and reduced postoperational complications.
Domains of the Cochrane random risk-of-bias assessment tool for randomized controlled trials (RCTs) and prospective studies.[23]
Quality assessment
We use standardized critical appraisal instruments from Joanna Briggs Institute for critical appraisal Tool assessment, as appropriate for methodological quality. Any disagreements that arose were resolved through discussion. The essential results of the appraisal are reported in narrative format and tables in an additional supplement and are not mentioned in this review. Regardless of their methodological quality, all studies were included in data extraction and synthesis.[24,25]
Literature search
Nineteen thousand three hundred articles were available on a given topic after searching the databases mentioned above, and after choosing the custom range of years from 2015–2023 as an inclusion component, only 12,100 remained. Five thousand seven hundred twenty articles remained after eliminating non-full text. After applying the inclusion and exclusion criteria, 18 papers were identified to meet the inclusion criteria for the review. As shown in Figure 1 which shows how the data is collected after slecting inclusion component.
Figure 1.
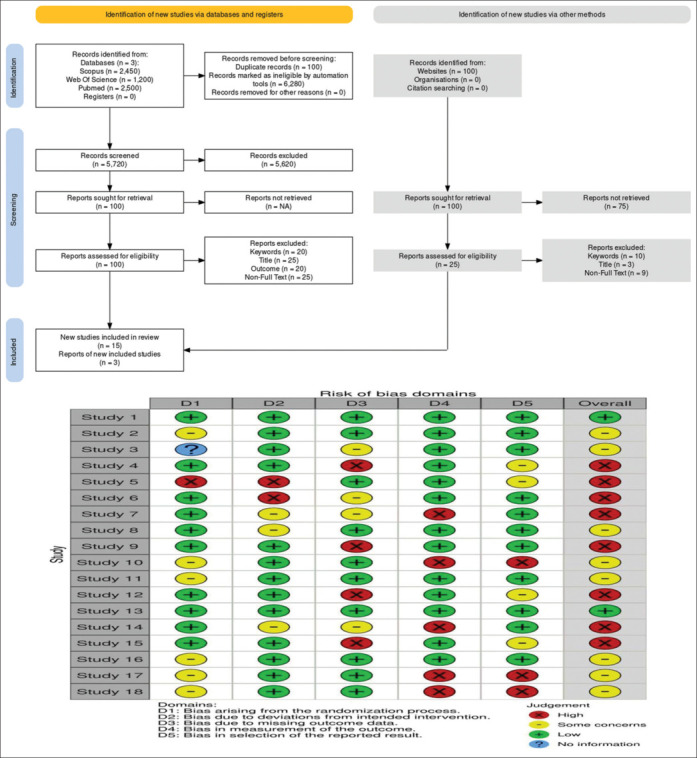
Flowchart outlining how studies were chosen to be part of the review (Cochrane Method)
Summary of included studies
The total number of included patients from 18 studies was
The study arms included atracurium + vecuronium, vecuronium + rocuronium, rocuronium + mivacurium, and AI + control. The most commonly reported outcome was the efficiency of AI. All study characteristics are shown in Table 1.[25,26]
Baseline characteristics of the included population
The primary chemotherapy type was anthracycline. The main cancer type in our included studies was breast cancer.[27,28] The follow-up duration ranged from 6 to 12 months, with 12 months being the most common. Table 1 shows the summary of the included studies.
A thorough literature search across several databases, including PubMed and Google Scholar, was part of the methodology for the research review article on the utility of AI in anesthesia. The selected articles were reviewed, and the relevant information was extracted and summarized. The information extracted included the study design, sample size, AI algorithms used, and outcomes measured.[29,30,31]
The information extracted from the articles was synthesized and organized into themes related to the application of AI in anesthesia. The themes included patient monitoring, drug dosing, decision-making, and limitations and challenges of AI in anesthesia.[32,33]
The review’s findings were analyzed and presented in a narrative format, highlighting the essential findings and recommendations for applying AI in anesthesia. The limitations of the studies were also discussed, and areas for future research were identified.
In addition to the literature search, expert opinions from anesthesiologists and AI specialists were sought to provide additional insights into AI’s potential utility in anesthesia and identify areas where further research is needed.[26,34,35,36]
Results
Clinical application of AI in patient outcomes
The use of AI in anesthesia has been a topic of growing interest in recent years, with several articles addressing the current state of AI in anesthesia and the potential benefits and challenges of incorporating AI into anesthesia care; V Mihir (2022) conducted a questionnaire-based feedback on the support of ML to anesthesiologists, and the anesthesiologist reported that the efficiency of peak glucose level estimation rose from 79.0 ± 13.7% without the assistance of ML to 84.7 ± 11.5% (P < 0.001) when they were provided with ML estimates, and opioid estimation increased from 18% to 42% with the help of ML. Wag Hao conducted another study validating multi-data analysis on artificial neural network (ANN) to predict long-term pain outcomes after microvascular decompression (MVD) in patients with trigeminal neuralgia (TN). The model trained could predict long-term pain with an efficiency of 95.2% and an AUC of 0.862.
AI in automation of drug delivery
AI has been proven to help physicians automate drug delivery. A study conducted by Shieh JS (2020) using fuzzy logic, a subset of AI to automate the delivery of neuromuscular blockades, in 10 patients with American Society of Anesthesiologists (ASA) I and II with blockade by rocuronium and mivacurium showed that when the groups were compared, the coefficient of variation in both cases was 36.13 (standard deviation (SD) 9.35)% and 34.03 (SD 10.76)%, showing a good activity by the controller. H Yuh-Jyh (2012) showed that decision tree had better efficiency (80.9% and 73.1%) in predicting patient-controlled analgesia consumption and its readjustment over other learning methods.
Another study conducted by Shamberg G et al. (2022) shows that continuous action deep reinforcement learning outperforms proportional integral derivative model control in the delivery of anesthesia drug, and reinforcement learning produces anesthetic control policies that are interpretable.
AI in pain management
For the management of pain, clinicians prefer the use of guidelines while making clinical decisions. The ASA provides guidelines for pain management. The use of AI has been vastly studied in the last 5 years. A study in this direction was conducted by G. Bochen (2021) on 4674 participants with knee pain, they created a deep learning (DL) algorithm and compared it to the traditional method, and the AUC for both was 0.692 (66.9% sensitivity and 64.1% specificity) and 0.770 (76.7% sensitivity and 70.5% specificity), which shows a higher significance (P < 0.001). Along with this, a combined model was created and the AUC of the model was 0.807 (72.3% sensitivity and 80.9% specificity), which is higher than both traditional and DL models. Jae-Geum Shim conducted another study on the prediction of chronic lower back pain by using a ML algorithm, and he studied 6119 patients, out of whom 1394 had lower back pain. Hence, ML is seen to help the anesthesiologist in the pain management of the patient.
Armin Kiani’s 2020 article “Artificial Intelligence in Anesthesia: Recent Advances and Future Direction” provides an overview of recent advances in AI in anesthesia care, including the use of AI for patient monitoring, decision support, and predictive analytics. Kiani also discusses the potential future directions of AI in anesthesia care, such as the development of closed-loop anesthesia systems.
Michael P. W. Grocott’s 2021 review, “Anesthesia and Artificial Intelligence: A Review,” provides an overview of the current state of AI research in anesthesia, including the use of AI for patient monitoring, decision support, and predictive analytics. Grocott also discusses the potential future directions of AI in anesthesia, such as the use of AI for personalized medicine.
Limitations and future challenges
AI is more prone to bias and relies on associations and relations drawn through its algorithm. There is a risk of racial biases emerging in the healthcare field as the artificial algorithm can make associations based on race. The “statistical bias” in AI could lead to discrimination and is one of the leading questions in the ethical and legal space. Researchers have attempted to identify the desirable and undesirable biases, which may affect the AI ability to produce the best results expected, and the difference in gender, effective treatment for each gender, and well-being of the patients are the desirable bias and unrepresentative samples, and adverse reactions and ineffective treatment are the undesirable bias for AI in health (Cirillo et al., 2020). Another case study showing the bias in medical AI reported that the authors (Gainz et al.) used a cutting-edge algorithm and training sets with a gender balance of 0/100% to examine diagnoses of 12 different thoracic diseases based on chest X-rays. 25% and 50% in women, 25%, 75% and 100% in Men, respectively, as anticipated, diagnostic AI outperformed when diagnosing women in one disease and men in another. However, for some diseases, such as pneumothorax, when used as an example, the diagnostic AI was more effective in men, even though it was initially programmed to diagnose more for women accurately. This difference is emphasized by women and men, even if bias remains.
The algorithm that worked best for women was to diagnose women better than men. If the same algorithm is used for different diseases, in women it performs the worst.
Ethical and legal issues must also be considered when integrating AI into health care because patient health is at stake. Research by Gerke et al. (2020) identifies the legal and ethical issues, such as informed consent. This pressing question still requires careful attention as to the extent of responsibility of the physician or cardiologist when teaching the complexities of AI to patients and, in what cases, the principles of consent shall apply, optionally. The black-box nature of the algorithm is worrying because sometimes the mechanism the algorithm uses to trigger an alert is unknown and may not be effective. Security and transparency are also among the emerging issues, as there is a need to train on good quality and large enough data, as well as whether these algorithms should be open to the public for verification because this conflicts with intellectual property rights. The third issue addresses concerns about algorithmic fairness and bias, as the data used for training must be a diverse and faithful representation of the population. Data protection and privacy also play an important role, and many laws relating to protection and privacy are currently in force.[37]
Discussion
-
Decision Support Systems:
Studies focusing on AI-based decision support systems reveal a growing body of literature in this domain. The review suggests that AI algorithms show promise in optimizing drug dosage, predicting patient responses, and aiding clinicians in decision-making. However, the discussion also underscores the need for further research to enhance the interpretability and explainability of these AI models. The “black-box” nature of some systems could challenge anesthesiologists’ acceptance and trust, emphasizing the importance of developing transparent and collaborative decision support tools.
-
Monitoring and Predictive Analytics:
The synthesis of evidence related to AI applications in monitoring and predictive analytics during anesthesia underscores their significant potential. Studies included in the review demonstrate the ability of AI to monitor vital signs, predict adverse events, and identify anomalies in real time. However, the discussion critically evaluates the translational challenges these technologies face, emphasizing data quality, interoperability, and the need for large, diverse datasets. Standardization and collaboration among institutions emerge as crucial factors for successfully integrating AI-driven predictive analytics into routine clinical practice.
-
Personalized Anesthesia Care:
The systematic review delves into the emerging area of personalized medicine in anesthesia, facilitated by AI. It is evident from the synthesized evidence that AI holds promise for tailoring anesthesia interventions to individual patient profiles, optimizing drug regimens, and minimizing adverse effects. However, the discussion also addresses ethical considerations, including data privacy and algorithmic biases. The review calls for further research to address these ethical implications and ensure the responsible implementation of AI-driven personalized anesthesia care.
-
Human–Machine Interaction:
The section on human–machine interaction reveals a growing interest in understanding how anesthesiologists interact with AI systems. The design of user-friendly interfaces and decision support tools is explored in the literature, and the review emphasizes the need for interdisciplinary research involving clinicians, AI experts, and human factor specialists. The discussion critically evaluates AI’s impact on healthcare professionals’ roles and responsibilities, raising essential questions about the optimal balance between AI support and human decision-making in anesthetic practice.
-
Challenges and Future Directions:
This systematic review systematically addresses the challenges faced by integrating AI into anesthetic practice, including standardization issues, ethical considerations, and human–machine interaction complexities. The evidence synthesis highlights the scarcity of high-quality, labeled datasets as a significant challenge and emphasizes the need for ongoing interdisciplinary collaboration between academia and industry. The discussion encourages future research to focus on overcoming these challenges, fostering ethical AI practices, and ensuring the seamless integration of AI into routine anesthetic care.
Usage of AI in Anesthesia
AI has the potential to revolutionize anesthesia care by improving patient outcomes, reducing costs, and enhancing the efficiency of anesthesia delivery. Here are some examples of how AI can be used in anesthesia:
Patient Monitoring: AI can improve patient monitoring in anesthesia care by enabling real-time monitoring of patient vital signs and early detection of potential complications. Here are some examples of how AI is being used in patient monitoring in anesthesia by real-time monitoring of multiple vital signs, predictive analytics for patient outcomes, anomaly detection, patient risk stratification, and automated documentation.[29,31]
Anesthetic Delivery: AI can potentially improve anesthesia delivery by optimizing the dosage and delivery of anesthetic agents based on patient characteristics and surgical requirements. Here are some examples of how AI is being used in anesthesia delivery for personalized anesthetic plans, automated dose adjustment, closed-loop anesthesia delivery systems, and automated drug delivery.[30,37,38]
Predictive Analytics: AI can be used for predictive analytics in anesthesia by analyzing large datasets of patient information to predict patient outcomes and identify patients at increased risk for complications. Here are some examples of how AI is being used in predictive analytics in anesthesia for risk prediction models, real-time risk stratification, outcome prediction, and early warning systems.[25,26,27]
Decision Support: AI can be used for decision support in anesthesia by providing anesthesia providers with recommendations for the optimal anesthetic plan based on patient characteristics and surgical requirements. Here are some examples of how AI is being used in decision support in anesthesia- anesthesia planning, medication selection, intraoperative decision support, and postoperative care.[29,33]
Electronic Medical Record (EMR) Integration: AI can be used for EMR integration in anesthesia by analyzing patient data and integrating it into the EMR system in real time. Here are some examples of how AI is being used for EMR integration in anesthesia- automated documentation, real-time data integration, decision support, and data analytics.
Conclusion
In conclusion, the use of AI in anesthesia has the potential to revolutionize the field and improve patient outcomes. AI algorithms can accurately predict patient outcomes and anesthesia dosing, as well as monitor patients during surgery in real time. These technologies can help anesthesiologists make more informed decisions, increase efficiency, and reduce costs. However, the implementation of AI in anesthesia also presents challenges, such as the need to address issues of bias and privacy. As the field continues to evolve, it will be important to carefully consider the ethical implications of AI in anesthesia and ensure that these technologies are used in a responsible the promise of AI in anesthesia is substantial, and it is an exciting time for researchers, clinicians, and patients alike.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bihorac A, Ozrazgat-Baslanti T, Ebadi A, Motaei A, Madkour M, Pardalos PM, et al. MySurgeryRisk: Development and validation of a machine-learning risk algorithm for major complications and death after surgery. Ann Surg. 2019;269:652–62. doi: 10.1097/SLA.0000000000002706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kendale S, Kulkarni P, Rosenberg AD, Wang J. Supervised machine-learning predictive analytics for prediction of post induction hypotension. Anesthesiology. 2018;129:675–88. doi: 10.1097/ALN.0000000000002374. [DOI] [PubMed] [Google Scholar]
- 3.Hao W, Cong C, Yuanfeng D, Ding W, Li J, Yongfeng S, et al. Multidata analysis based on an artificial neural network model for long-term pain outcome and key predictors of microvascular decompression in trigeminal neuralgia. World Neurosurg. 2022;164:e271–9. doi: 10.1016/j.wneu.2022.04.089. [DOI] [PubMed] [Google Scholar]
- 4.Shieh JS, Fan SZ, Chang LW, Liu CC. Hierarchical rule-based monitoring and fuzzy logic control for neuromuscular blocks. J Clin Monit Comput. 2000;16:583–92. doi: 10.1023/a:1012212516100. [DOI] [PubMed] [Google Scholar]
- 5.Hu YJ, Ku TH, Jan RH, Wang K, Tseng YC, Yang SF. Decision tree-based learning to predict patient controlled analgesia consumption and readjustment. BMC Med Inform Decis Mak. 2012;12:131. doi: 10.1186/1472-6947-12-131. doi: 10.1186/1472-6947-12-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schamberg G, Badgeley M, Meschede-Krasa B, Kwon O, Brown EN. Continuous action deep reinforcement learning for propofol dosing during general anesthesia. Artificial Intelligence Med. 2022;123:102227. doi: 10.1016/j.artmed.2021.102227. [DOI] [PubMed] [Google Scholar]
- 7.Hashimoto DA, Witkowski E, Gao L, Meireles O, Rosman G. Artificial intelligence in anesthesiology: Current techniques, clinical applications, and limitations. Anesthesiology. 2020;132:379–94. doi: 10.1097/ALN.0000000000002960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guan B, Liu F, Mizaian AH, Demehri S, Samsonov A, Guermazi A, et al. Deep learning approach to predict pain progression in knee osteoarthritis. Skeletal Radiol. 2021;51:363–73. doi: 10.1007/s00256-021-03773-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shim JG, Ryu KH, Cho EA, Ahn JH, Kim HK, Lee YJ, et al. Machine learning approaches to predict chronic lower back pain in people aged over 50 years. Medicina. 2021;57:1230. doi: 10.3390/medicina57111230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Latifi K, Negaresh M, Nima Javanshir, Safari S. The advent of artificial intelligence in anesthesiology and pain management: A review article. Int J Drug Res Clin. 2023;1:e14–4. [Google Scholar]
- 11.Singh M, Nath G. Artificial intelligence and anesthesia: A narrative review. Saudi J Anaesth. 2022;16:86–93. doi: 10.4103/sja.sja_669_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mathis MR, Kheterpal S, Najarian K. Artificial intelligence for anesthesia: What the practicing clinician needs to know: More than black magic for the art of the dark. Anesthesiology. 2018;129:619–22. doi: 10.1097/ALN.0000000000002384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goldstein JC, Goldstein HV. Artificial intelligence in anesthesiology: What are the missing pieces? J Clin Anesth. 2021;71:110219. doi: 10.1016/j.jclinane.2021.110219. doi: 10.1016/j.jclinane.2021.110219. [DOI] [PubMed] [Google Scholar]
- 14.Bellini V, Rafano Carnà E, Russo M, Di Vincenzo F, Berghenti M, Baciarello M, et al. Artificial intelligence and anesthesia: A narrative review. Ann Transl Med. 2022;10:528. doi: 10.21037/atm-21-7031. doi: 10.21037/atm-21-7031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh M, Nath G. Artificial intelligence and anesthesia: A narrative review. Saudi J Anaesth. 2022;16:86–93. doi: 10.4103/sja.sja_669_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gupta B, Sahay N, Vinod K, Sandhu K, Basireddy HR, Mudiganti RKR. Recent advances in system management, decision support systems, artificial intelligence and computing in anaesthesia. Indian J Anaesth. 2023;67:146–51. doi: 10.4103/ija.ija_974_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Connor CW. Artificial intelligence and machine learning in anesthesiology. Anesthesiology. 2019;131:1346–59. doi: 10.1097/ALN.0000000000002694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhu H. Big data and artificial intelligence modeling for drug discovery. Annu Rev Pharmacol Toxicol. 2020;60:573–89. doi: 10.1146/annurev-pharmtox-010919-023324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wingert T, Lee C, Cannesson M. Machine learning, deep learning, and closed loop devices-anesthesia delivery. Anesthesiol Clin. 2021;39:565–81. doi: 10.1016/j.anclin.2021.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nayarisseri A, Khandelwal R, Tanwar P, Madhavi M, Sharma D, Thakur G, et al. Artificial intelligence, big data and machine learning approaches in precision medicine & drug discovery. Curr Drug Targets. 2021;22:631–55. doi: 10.2174/1389450122999210104205732. [DOI] [PubMed] [Google Scholar]
- 21.Tripathi N, Goshisht MK, Sahu SK, Arora C. Applications of artificial intelligence to drug design and discovery in the big data era: A comprehensive review. Mol Divers. 2021;25:1643–64. doi: 10.1007/s11030-021-10237-z. [DOI] [PubMed] [Google Scholar]
- 22.Bini SA. Artificial intelligence, machine learning, deep learning, and cognitive computing: What do these terms mean and how will they impact health care? J Arthroplasty. 2018;33:2358–61. doi: 10.1016/j.arth.2018.02.067. [DOI] [PubMed] [Google Scholar]
- 23.Meyer JU, Kullik G, Wruck N, Kück K, Manigel J. Advanced technologies and devices for inhalational anesthetic drug dosing. Handb Exp Pharmacol. 2008:451–70. doi: 10.1007/978-3-540-74806-9_21. doi: 10.1007/978-3-540-74806-9_21. [DOI] [PubMed] [Google Scholar]
- 24.Hornung AL, Hornung CM, Mallow GM, Barajas JN, Rush A, 3rd, Sayari AJ, et al. Artificial intelligence in spine care: Current applications and future utility. Eur Spine J. 2022;31:2057–81. doi: 10.1007/s00586-022-07176-0. [DOI] [PubMed] [Google Scholar]
- 25.Dmitry N. Automation of Anesthesiology-Will artificial intelligence replace clinicians. Int J Anesthetics Anesthesiol. 2022:9. doi: 10.23937/2377-4630/1410147. [Google Scholar]
- 26.Naaz S, Asghar A. Artificial intelligence, nano-technology and genomic medicine: The future of anaesthesia. J Anaesthesiol Clin Pharmacol. 2022;38:11–7. doi: 10.4103/joacp.JOACP_139_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shah N, Arshad A, Mazer MB, Carroll CL, Shein SL, Remy KE. The use of machine learning and artificial intelligence within pediatric critical care. Pediatr Res. 2022;93:405–12. doi: 10.1038/s41390-022-02380-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arora A. Artificial intelligence: A new frontier for anesthesiology training. Br J Anaesth. 2020;125:e407–8. doi: 10.1016/j.bja.2020.06.049. [DOI] [PubMed] [Google Scholar]
- 29.Rajkomar A, Dean J, Kohane I. Machine learning in medicine. N Engl J Med. 2019;380:1347–58. doi: 10.1056/NEJMra1814259. [DOI] [PubMed] [Google Scholar]
- 30.Safran T, Viezel-Mathieu A, Corban J, Kanevsky A, Thibaudeau S, Kanevsky J. Machine learning and melanoma: The future of screening. J Am Acad Dermatol. 2018;78:620–21. doi: 10.1016/j.jaad.2017.09.055. [DOI] [PubMed] [Google Scholar]
- 31.Fernandes MPB, Armengol de la Hoz M, Rangasamy V, Subramaniam B. Machine learning models with preoperative risk factors and intraoperative hypotension parameters predict mortality after cardiac surgery. J Cardiothorac Vasc Anesth. 2021;35:857–65. doi: 10.1053/j.jvca.2020.07.029. [DOI] [PubMed] [Google Scholar]
- 32.Vanhonacker D, Verdonck M, Nogueira Carvalho H. Impact of closed-loop technology, machine learning, and artificial intelligence on patient safety and the future of anesthesia. Curr Anesthesiol Rep. 2022;12:451–60. [Google Scholar]
- 33.Char DS, Burgart A. Machine-learning implementation in clinical anesthesia: Opportunities and challenges. Anesth Analg. 2020;130:1709–12. doi: 10.1213/ANE.0000000000004656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gambus PL, Jaramillo S. Machine learning in anaesthesia: Reactive, proactive… predictive! Br J Anaesth. 2019;123:401–3. doi: 10.1016/j.bja.2019.07.009. [DOI] [PubMed] [Google Scholar]
- 35.Meier JM, Tschoellitsch T. Artificial intelligence and machine learning in patient blood management: A scoping review. Anesth Analg. 2022;135:524–31. doi: 10.1213/ANE.0000000000006047. [DOI] [PubMed] [Google Scholar]
- 36.Miyaguchi N, Takeuchi K, Kashima H, Morita M, Morimatsu H. Predicting anesthetic infusion events using machine learning. Sci Rep. 2021;11:23648. doi: 10.1038/s41598-021-03112-2. doi: 10.1038/s41598-021-03112-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Konar S, Auluck N, Ganesan R, Goyal AK, Kaur T, Sahi M, et al. A non-linear time series based artificial intelligence model to predict outcome in cardiac surgery. Health Technol. 2022;12:1169–81. [Google Scholar]
- 38.Devani RN, Kirubakaran A, Molokhia M. Digital health RCT interventions for cardiovascular disease risk reduction: A systematic review and meta-analysis. Health Technol (Berl) 2022;12:687–700. doi: 10.1007/s12553-022-00651-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


