ABSTRACT
Background: Music therapy is increasingly examined in randomized controlled trials (RCTs) and shows potential in treating post-traumatic stress disorder (PTSD).
Objective: This systematic review and meta-analysis critically evaluates the current clinical evidence supporting the efficacy and acceptability of music therapy for PTSD.
Method: RCTs comparing music therapy in addition to care as usual (CAU) versus either CAU alone or CAU combined with standard psychotherapy/pharmacotherapy for PTSD were retrieved from major English – and Chinese-language databases. Standardized mean differences (SMDs) for post-treatment PTSD symptom scores and risk differences (RDs) for retention rates upon treatment completion were calculated to assess the efficacy and acceptability of music therapy, respectively. The Cochrane risk of bias (RoB) tool 2.0 and the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) were used to assess the RoB of included studies and certainty of the evidence, respectively.
Results: Nine studies, incorporating 527 PTSD patients, were included, all with high RoB. The post-treatment PTSD symptom scores were significantly lower in the music therapy group than the inactive control group (SMD = −1.64, P < .001), but comparable between the music therapy group and the active control group (SMD = −0.28, P = .330). The retention rates did not differ significantly between the music therapy group and both control groups (RD = 0.03, P = .769; RD = 0.16, P = .829). The GRADE rated certainty level of evidence as low.
Conclusions: Although meta-analytic findings suggest that music therapy is effective in reducing post-traumatic symptoms in individuals with PTSD, with its therapeutic effect comparable to that of standard psychotherapy, the low level of certainty limits its generalizability. More methodologically stringent studies are warranted to strengthen the clinical evidence for the efficacy and acceptability of music therapy for PTSD.
KEYWORDS: Post-traumatic stress disorder, music therapy, efficacy, acceptability, meta-analysis
HIGHLIGHTS
This systematic review critically appraised the existing methodologically rigorous evidence for the efficacy and acceptability of music therapy for post-traumatic stress disorder (PTSD).
The post-treatment PTSD symptom scores were significantly lower in the music therapy group than the inactive control group and comparable between the music therapy group and the active control group.
The post-treatment retention rates did not differ significantly between the music therapy group and both the inactive and active control groups.
Abstract
Antecedentes: La musicoterapia se examina cada vez más en ensayos controlados aleatorios (ECA) y muestra potencial en el tratamiento del trastorno de estrés postraumático (TEPT).
Objetivo: Esta revisión sistemática y metanálisis evalúa críticamente la evidencia clínica actual que respalda la eficacia y aceptabilidad de la musicoterapia para el trastorno de estrés postraumático.
Método: Los ECA que compararon musicoterapia además de la atención habitual (CAU) versus CAU sola o CAU combinada con psicoterapia/farmacoterapia estándar para el trastorno de estrés postraumático se recuperaron de las principales bases de datos en inglés y chino. Se calcularon las diferencias de medias estandarizadas (DME) para las puntuaciones de los síntomas de TEPT post-tratamiento y las diferencias de riesgo (DR) para las tasas de retención al finalizar el tratamiento para evaluar la eficacia y aceptabilidad de la musicoterapia, respectivamente. Se utilizaron la herramienta Cochrane de riesgo de sesgo (RoB) 2.0 y la Clasificación de recomendaciones, evaluación, desarrollo y evaluaciones (GRADE) para evaluar el RoB de los estudios incluidos y la certeza de la evidencia, respectivamente.
Resultados: Se incluyeron nueve estudios que incorporaron 527 pacientes con PTSD, todos con RoB alto. Las puntuaciones de los síntomas de PTSD posteriores al tratamiento fueron significativamente más bajas en el grupo de musicoterapia que en el grupo de control inactivo (SMD = −1.64, P < .001), pero comparables entre el grupo de musicoterapia y el grupo de control activo (SMD = −0.28, P = .330). Las tasas de retención no difirieron significativamente entre el grupo de musicoterapia y ambos grupos de control (RD = 0.03, P = .769; RD = 0.16, P = .829). GRADE calificó el nivel de certeza de la evidencia como bajo.
Conclusiones: Aunque los hallazgos metanalíticos sugieren que la musicoterapia es eficaz para reducir los síntomas postraumáticos en personas con trastorno de estrés postraumático, con un efecto terapéutico comparable al de la psicoterapia estándar, el bajo nivel de certeza limita su generalización. Se necesitan estudios metodológicamente más estrictos para fortalecer la evidencia clínica sobre la eficacia y aceptabilidad de la musicoterapia para el trastorno de estrés postraumático.
PALABRAS CLAVE: Trastorno de estrés postraumático, musicoterapia, eficacia, aceptabilidad, meta-análisis
Abstract
背景:随机对照试验(RCTs)越来越多地应用于音乐疗法效果的考察,并显示出治疗创伤后应激障碍(PTSD)的潜力。
目的:该系统综述和荟萃分析对现有的音乐疗法治疗 PTSD临床证据进行了批判性评价。
方法:从主要的英文和中文数据库中检索了将音乐疗法加入到常规治疗(CAU)中,并将其与单独的 CAU 或与标准心理治疗/药物治疗结合的 CAU 进行比较的 RCTs。为了评估音乐疗法的疗效和可接受性,我们计算了治疗末的 PTSD 症状评分的标准化均差(SMDs)和治疗完成后的患者保留率的风险差异(RDs)。使用 Cochrane偏倚风险(RoB)工具 2.0 和推荐意见分级的评估、制订及评价(GEADE)来分别评估纳入的研究的 RoB 和证据的确定性。
结果: 9项研究纳入研究, 包括527 名 PTSD 患者,所有的研究的 RoB 都很高。音乐疗法组的治疗后 PTSD 症状评分显著低于阴性对照组 (SMD = −1.64, P < .001),但是与阳性对照组相似 (SMD = −0.28, P = .330)。音乐疗法组和两个对照组的保留率差异不显著 (RD = 0.03, P = .769; RD = 0.16, P = .829)。GRADE评估证据的确定性级别为低。
结论:尽管本研究结果显示音乐疗法缓解 PTSD 患者的创伤后应激症状有效,其疗效与标准心理疗法相当,但该研究发现的可推广性却受限于其低级别的证据确定性。有必要开展更多的方法学严谨设计的研究,以增强音乐疗法对 PTSD 的疗效和可接受性的临床证据。
关键词: 创伤后应激障碍, 音乐疗法, 疗效, 可接受性, 荟萃分析
1. Introduction
Post-traumatic stress disorder (PTSD) is a severe, often long-lasting, and impairing mental disorder associated with adverse health consequences, including mental and physical morbidity, reduced quality of life, increased suicide risk, and higher healthcare burden (Clark et al., 2023; Kim et al., 2021; von der Warth et al., 2020; Xiong et al., 2021; Zhao et al., 2023). It is prevalent globally, with the World Health Organization World Mental Health Survey reporting cross-national lifetime prevalence rates of 3.9% among the general population and 5.6% among individuals exposed to traumatic events (Koenen et al., 2017).
Trauma-focused psychotherapy is strongly recommended as the primary treatment for PTSD, with selective serotonin reuptake inhibitors (SSRIs) conditionally recommended as alternative first-line options when psychotherapy is not readily available or not preferred (Cipriani et al., 2018; Hamblen et al., 2019; Mavranezouli et al., 2020; Merz et al., 2019; Stein, 2023). However, exposure-based psychotherapies may be challenging due to the retelling and confronting of traumatic events, leading to poor retention (Varker et al., 2021). Dropout rates of 22% to 30% have been observed in trauma-focused therapies such as cognitive processing therapy, prolonged exposure therapy, and group cognitive behaviour treatment (CBT) (Lewis et al., 2020). Similarly, SSRIs raise concerns due to lower response rates and high treatment discontinuation rates (Cipriani et al., 2018). As such, switching, combination, and augmentation strategies are suggested to improve the treatment response. Nevertheless, due to inadequate related clinical research, the recommendation levels of these treatment strategies remain very low or uncertain in available clinical guidelines (Hamblen et al., 2019).
The World Federation of Music Therapy (WFMT) defines music therapy as the professional application of music and its elements in medical, educational, and daily settings. It aims to enhance the quality of life and promote physical, social, communicative, emotional, intellectual, and spiritual health and well-being for individuals, groups, families, or communities seeking improvement (Haase, 2012). Numerous studies have elucidated the social, cognitive, and neurobiological mechanisms underlying therapeutic music, including but not limited to emotion regulation, stress reduction, mood enhancement, relationship building, and distraction from discomfort (Landis-Shack et al., 2017). Consequently, music has been widely employed as a valuable therapeutic tool, offering relief for a range of physical and mental health problems. Systematic reviews and meta-analyses have confirmed its effectiveness in managing conditions such as pain, hypertension, anxiety, serious mental illnesses, stress, dementia, depression, and insomnia (Aalbers et al., 2017; Cao & Zhang, 2023; de Witte et al., 2022; Feng et al., 2018; He et al., 2023; Isaacs et al., 2022; Lee et al., 2023; Zhang et al., 2017). Over the past decade, music therapy has emerged as an alternative and less linguistically intensive treatment modality for individuals suffering from PTSD. Empirical research has demonstrated its promising efficacy and favourable feasibility in alleviating PTSD symptoms as well as comorbid depressive, anxiety, and insomnia symptoms in individuals with PTSD (Blanaru et al., 2012; Hirschberg et al., 2020; Landis-Shack et al., 2017; Lee et al., 2018; Macfarlane et al., 2019; Ophir & Jacoby, 2020). Nevertheless, it is worth noting that the majority of existing studies exploring the efficacy of music therapy primarily consist of single-arm clinical trials or qualitative studies. These studies typically involve small sample sizes and participants with specific characteristics, making them prone to reporting positive findings. As a result, there is a high risk of bias (RoB) and an overestimation of the true treatment effect size of music therapy for PTSD.
In recent years, there has been a growing body of randomized controlled trials (RCTs) investigating the efficacy of music therapy as a complementary intervention for PTSD. However, we have not found any systematic reviews of RCTs conducted thus far that establish rigorous clinical evidence regarding the efficacy and acceptability of music therapy for PTSD. To fill this knowledge gap, we conducted a systematic review and meta-analysis of RCTs specifically comparing music therapy with appropriate control conditions for PTSD. The objective of our study is to critically appraise the existing clinical evidence supporting music therapy and facilitate its clinical implications.
2. Methods
This systematic review was reported according to the PRISMA guideline. The first and second authors independently conducted literature search, inclusion of eligible studies, data extraction, RoB assessment, and certainty assessment of the available clinical evidence. Any disagreements were resolved through discussion and consensus with the corresponding author.
2.1. Search strategies
We searched international databases (Cochrane, PubMed, Embase, and PsycInfo) as well as Chinese databases (CNKI, Wanfangdata, and VIP Info) from their respective inception dates until November 4, 2023. The search keywords used were (post-traumatic stress OR trauma* OR PTSD) AND (music* OR song* OR improvis*). Additionally, the reference lists of eligible studies and relevant reviews were manually searched to identify any additional studies.
2.2. Inclusion and exclusion criteria
The inclusion criteria for eligible studies were determined based on the PICOS acronym. The participants were limited to patients with PTSD. The interventions were music therapy in addition to care as usual (CAU) versus either CAU alone or CAU combined with standard psychotherapy/pharmacotherapy. The efficacy outcome measure was PTSD symptom severity scores at the end of treatment. The acceptability outcome was assessed by the retention rate, which represents the percentage of participants who remained in the treatment arm until its completion. Only RCTs with available efficacy or acceptability data were considered for inclusion. In addition, if two or more studies used the same sample, only the study with the most complete data or the one published earliest was included. Studies that had no data suitable for meta-analysis, qualitatively analyzed the treatment efficacy of music therapy, or did not evaluate efficacy outcomes using standard scales were excluded.
While the involvement of a music therapist could significantly enhance the therapeutic process, according to the WFMT definition of music therapy (Haase, 2012), it's not a strict requirement for conducting music therapy. As a result, we also considered ‘listening to music’ as a subtype of music therapy, provided that it was administered in medical settings.
2.3. Data extraction
Data extracted from included studies included first author, publication year, diagnostic criteria of PTSD, details of interventions in both the experimental and control groups, sample sizes, and outcome measures (mean ± standard deviation).
2.4. RoB of included studies
The Cochrane risk-of-bias tool, version 2 (RoB 2), was used to assess the RoB of included RCTs (Sterne et al., 2019). This tool evaluates bias across five methodological domains: bias arising from the randomization process, bias due to deviations from intended interventions, bias due to missing outcome data, bias in the measurement of the outcome, and bias in the selection of the reported result. Each domain offers response options of low RoB, some concerns, and high RoB. Based on the judgments for all domains, an overall level of RoB (low, some, or high) was determined using a predefined algorithm outlined in the Cochrane Handbook (Higgins et al., 2023).
2.5. Certainty of overall evidence
The framework of Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) was used to grade the certainty of the body of evidence from the included studies by evaluating the five GRADE domains: RoB, imprecision, inconsistency, indirectness, and publication bias (Guyatt et al., 2008). By applying the rules of rating down and up in the GRADE approach, the certainty of clinical evidence of music therapy for PTSD was rated as high, moderate, low, or very low.
2.6. Statistical analysis
The meta-analysis was conducted to combine standardized mean differences (SMDs) and their 95% confidence intervals (CIs) for post-treatment scores of PTSD symptoms, as well as risk differences (RDs) and their 95%CIs for retention rates between the experimental and control groups. Forest plots were used to present the SMDs, RDs, and their overall estimates. The random-effect model was employed in the presence of heterogeneity (I2 > 50% or P < .10 for Q statistics); otherwise, the fixed-effect model was used. Given the clinical heterogeneity in the interventions of the control group, the meta-analysis was performed based on the type of controls: inactive (i.e. CAU alone or waitlist plus CAU) and active (i.e. psychotherapy plus CAU). In this study, the SMD was on par with the effect size measure, Hedges’ g, where absolute values ranging between 0.20 and 0.49, 0.50 and 0.79, and anything above 0.80 represented small, medium, and large treatment effect sizes, respectively (Luo et al., 2021; Xu et al., 2022; Zhong et al., 2019).
Sources of heterogeneity in the pooled SMDs were examined by using subgroup analyses according to potential categorical moderators such as study country, form of music therapy (music listening only or music therapist-led), and treatment duration. The fail-safe numbers (FSNs) were calculated to test the publication bias for P = .05 and P = .01, given that the number of included studies was less than ten. A two-sided P-value of less than 0.05 was considered statistically significant. All analyses were conducted using R 4.1.2 (R Development Core Team; Vienna, Austria).
3. Results
3.1. Characteristics of included studies
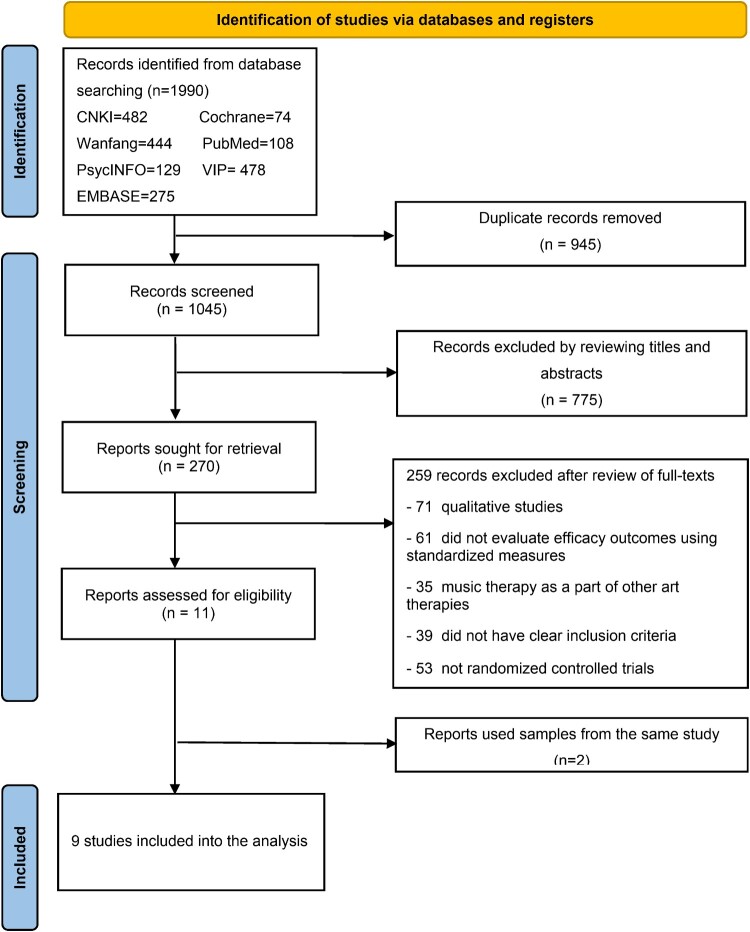
Initially, 1016 studies were identified, and eventually, nine studies incorporating 527 PTSD patients (271 in the experimental group and 256 in the control group) were included (Beck et al., 2021; Carr et al., 2012; Du et al., 2019; Gao & Chen, 2018; Li et al., 2023; Pezzin et al., 2018; Pourmovahed et al., 2021; Rudstam et al., 2022; Zhang et al., 2022) (Figure 1). The traumatic events encountered by individuals with PTSD varied considerably across the nine studies. In six of the studies, participants only experienced a specific type of trauma: breast cancer, wars, spinal cord injury, premature neonates’ ICU hospitalization, multiple injuries, and acute stroke. The remaining three studies included participants who had experienced a range of traumas, including torture, rape, false imprisonment, and emotional abuse (Beck et al., 2021; Carr et al., 2012; Rudstam et al., 2022).
Figure 1.
PRISMA flowchart of inclusion of studies for the meta-analysis.
The music intervention in six studies was led and supervised by music therapists, either individually or in group settings. In contrast, the music intervention in the remaining three studies solely involved music listening without the involvement of music therapists (Gao & Chen, 2018; Li et al., 2023; Pourmovahed et al., 2021). The interventions in control groups of two studies were active, both CAU plus standard psychotherapy (Beck et al., 2021; Li et al., 2023) while the interventions in control groups of the remaining seven studies were inactive, CAU alone or CAU plus waitlist. Detailed characteristics of the nine included studies are shown in Table 1.
Table 1.
Characteristics of randomized controlled trials included for the meta-analysis of music therapy for post-traumatic stress disorder (PTSD).
| Study | Participants | Diagnostic criteria of PTSD | Experimental intervention | Control intervention | Details of music therapy | Music prescription | Numbers of participants in the experimental vs. control groups | Efficacy outcome measure |
|---|---|---|---|---|---|---|---|---|
| Carr et al. (2012) | PTSD patients who did not respond to CBT in United Kindom | DSM-IV | Group music therapy + pharmacotherapy | Waitlist + pharmacotherapy | Group psychodynamic music therapy, a combination of active and receptive activities, led by music therapists, 10 weekly one-hour sessions over a period of 2.5 months | Participants engaged in free music improvisation using a wide range of musical instruments. Therapists provided improvised instrumental support, and the musical instruments were specifically selected for their ease of accessibility. | 8 (M/F: 3/5, mean age: 34 years) vs. 8 (M/F: 4/4, mean age: 44 years) | Post-treatment IES-R score |
| Gao & Chen (2018) | Patients with breast cancer receiving chemotherapy who developed PTSD in China | NR | Listening to music + CAU | CAU | Group listening to Gregorian hymns and Mozart music, 80 daily sessions over a period of 2.5 months | Recordings of Gregorian hymns and Mozart music were used. The music was selected by patients’ treating physicians. | 40 (M/F: 0/40, mean age: NR) vs. 40 (M/F: 0/40, mean age: NR) | Post-treatment PTSD-SS score |
| Pezzin et al. (2018)* | Veterans with PTSD in United States | ICD-9CM | Active, music-instruction intervention + CAU | Waitlist + CAU | Individual and group music instruction, led by professional music teachers, six weekly one-hour sessions over a period of 1.5 months | Participants were provided guitars and offered personal and group instructions on playing the guitar. | 25 (M/F: 22/3, mean age: 49.8 years) vs. 15 (M/F: 14/1, mean age: 53.8 years) | Post-treatment PCL-C score |
| Du et al. (2019) | Patients with spinal cord injury who developed PTSD in China | DSM-V | Music therapy + CAU | CAU | Individual receptive music therapy, led by music therapists, 12 biweekly 50-minute sessions over a period of three months | Recordings of Bandari light music were played to induce muscle relaxation, and soft, beautiful, cheerful, and lively music was utilized for music-guided imagery. The selection criteria for the music were not specified. | 27 (M/F: 21/6, mean age: 35.6 years) vs. 27 (M/F: 20/7, mean age: 34.3 years) | Post-treatment PTSD-SS score |
| Beck et al. (2021) | Refugees with PTSD in Denmark | ICD-10 and DSM-IV | Trauma-focused music and imagery + pharmacotherapy (if needed) | Standard psychotherapy + pharmacotherapy (if needed) | Individual trauma-focused music and imagery, led by music therapists, 16 weekly one-hour sessions over a period of 4 months | Recordings of music were utilized, with pieces selected from the Guided Imagery and Music repertoire that included classical music, light classical music, film music, and meditative music. Pieces from the participant’s own musical tradition were also incorporated. The therapists chose the music after consultation with the patient. | 39 (M/F: 22/17, mean age: 42 years) vs. 35 (M/F: 21/14, mean age: 42 years) | Post-treatment HTQ-IV score |
| Pourmovahed et al. (2021) | Mothers of premature neonates hospitalized in NICU who developed PTSD in Iran | NR | Listening to the non-verbal music + CAU | CAU | Group listening to the non-verbal music, 14 daily 20-minute sessions over a period of two weeks | Sound recordings of rain, sea, and nature, characterized by a slow, gentle, and soothing rhythm, were used. The selection criteria for the music were not specified. | 23 (M/F: 0/23, mean age: 28.1 years) vs. 22 (M/F: 0/22, mean age: 28.0 years) | Post treatment PPQ score |
| Zhang et al. (2022) | Patients with multiple injuries who developed PTSD in China | NR | Mindfulness training with soothing music + CAU | CAU | Individual mindfulness training with soothing music, daily 30-minute sessions | Recordings of soothing and gentle Chinese classical music were played. The music was selected based on expert consultations with clinical and music professionals, as well as the patient's preferences. | 53 (M/F: 30/23, mean age: 36.1 years) vs. 52 (M/F: 28/24, mean age: 35.3 years) | Post-treatment PCL-C score |
| Li et al. (2023) | Patients with acute ischemic stroke who developed PTSD in China | DSM-V | Five-element music from Traditional Chinese Medicine + CAU | CBT + CAU | Individually listening to five-element music, 20 daily 30-minute sessions over a period of one month | Recordings of the five-element music from Traditional Chinese Medicine were used. The selection of music was based on the patient’ preference. | 34 (M/F: 16/18, mean age: 59.3 years) vs. 34 (M/F: 15/19, mean age: 58.5 years) | Post-treatment PCL-C score |
| Rudstam et al. (2022) | Women referred for treatment of PTSD/CPTSD in Sweden | DSM-V and ICD-11 | Trauma-focused group music and imagery + pharmacological treatments (if needed) | Waitlist + pharmacological treatments (if needed) | Group trauma-focused receptive music and imagery, 12 weekly 2.5-hour sessions over a period of 4 months | Recordings, predominantly of classical music from the western tradition, were utilized. These selections were drawn from the Bonny Method of Guided Imagery and Music repertoire. The choice of music was based on therapists’ professional assessments of each group's capacity to handle varying music intensities, while ensuring optimal arousal levels. | 22 (M/F: 0/22, mean age: 45.2 years) vs. 23 (M/F: 0/23, mean age: 42.2 years) | Post-treatment PCL-5 score |
Note: CBT, Cognitive Behavioral Therapy; NIUC, Neonatal Intensive Care Unit; CPTSD, complex PTSD; DSM, Diagnostic & Statistical Manual of Mental Disorders; ICD, International Classification of Diseases; NR, not reported; CAU, Care as usual; M/F, male/female; IES-R, Impact of Event Scale-Revised; PTSD-SS, PTSD Self-rating Scale; PCL-C, PTSD Checklist-Civilian Version; HTQ-IV, Harvard Trauma Questionnaire, section IV; PPQ, Perinatal PTSD Questionnaire; PCL-5, PTSD Checklist for DSM-5. *In Pezzin et al.'s 2018 study, the experimental group underwent music therapy for six weeks, while the control group was only observed for four weeks. To ascertain the average PCL-C score of the control group at six weeks, we first determined the weekly change in mean PCL-C score. Then we calculated the mean PCL-C score at six weeks by using the formula: baseline mean PCL-C score – (6 * change in mean PCL-C score per week). The standard deviation (SD) of the PCL-C score at six weeks was directly obtained from the SD at the fourth week.
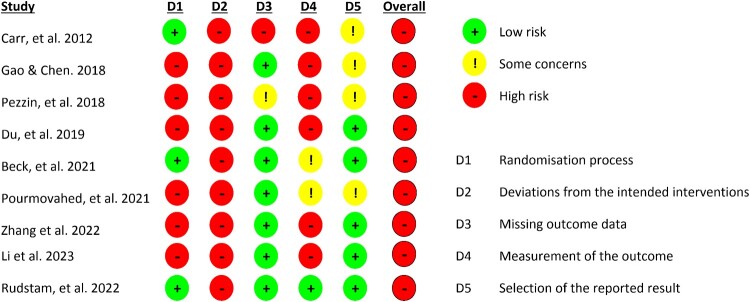
3.2. RoB of included studies
Figure 2 illustrates that all nine included studies had a high RoB. Deviations from the intended interventions were the most common source of bias (n = 9), followed by issues with the randomization process (n = 6) and outcome measurement (n = 6).
Figure 2.
Risk of bias assessment of included studies according to the Cochrane risk-of-bias tool 2.0.
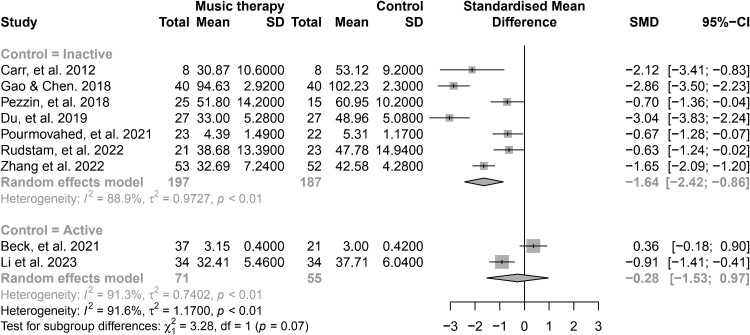
3.3. Meta-analysis of post-treatment PTSD symptom scores and publication bias
Figure 3 shows that the post-treatment PTSD symptom scores were significantly lower in the music therapy group compared to the inactive control group (SMD = −1.64, P < .001). However, the scores were comparable between the music therapy group and the active control group (SMD = −0.28, P = .330). The FSNs for meta-analysis of music therapy versus inactive control groups were 707 (P = .05) and 347 (P = .01), respectively.
Figure 3.
Forest plot of standardized mean differences in post-treatment post-traumatic stress symptom scores: comparing music therapy with inactive and active control groups.
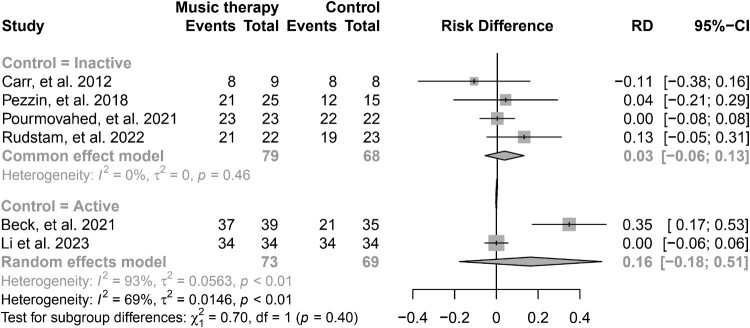
3.4. Meta-analysis of post-treatment retention rates
Figure 4 illustrates that the post-treatment retention rates did not significantly differ between the music therapy group and both the inactive and active control groups (RD = 0.03, P = .769; RD = 0.16, P = .829).
Figure 4.
Forest plot of risk differences in post-treatment retention rates: comparing music therapy with inactive and active control groups.
3.5. Sources of heterogeneity in meta-analysis of efficacy of music therapy vs. inactive control groups
Two sources of heterogeneity were found in the subgroup analysis (Table 2). The pooled SMDs significantly varied across studies using different diagnostic criteria for PTSD. The highest value was found in those using the Diagnostic and Statistical Manual (DSM) criteria (SMD = −2.78), while the lowest value emerged in studies using both the DSM and International Classification of Diseases (ICD) criteria (SMD = −0.63). Further, the pooled SMDs were statistically higher in studies that administered music therapy for two to four months (SMD = −2.83) compared to those that administered music therapy for less than two months (SMD = −0.95).
Table 2.
Subgroup analysis of the source of heterogeneity in meta-analysis of randomized controlled trials comparing efficacy of music therapy with inactive control groups.
| Characteristics | Number of studies | Sample size | Heterogeneity [I2], % (P) | Standardized Mean Difference (95%CI) | Q | P | |
|---|---|---|---|---|---|---|---|
| Experimental group | Control group | ||||||
| Participants | |||||||
| Medically ill patients | 4 | 143 | 141 | 96.1(<0.001) | −2.04(−3.11,−0.96) | ||
| Psychiatric patients | 2 | 29 | 31 | 76.2(0.040) | −1.26(−2.70,0.18) | ||
| Veterans | 1 | 25 | 15 | Not applicable | −0.70(−1.36,−0.04) | 4.37 | 0.113 |
| Sample | |||||||
| Males + females | 4 | 113 | 102 | 85.1(<0.001) | −1.84(−2.82,−0.85) | ||
| Females only | 3 | 84 | 85 | 93.8(<0.001) | −1.39(−2.83,0.06) | 0.26 | 0.612 |
| Mean age | |||||||
| < 40 years | 4 | 111 | 109 | 86.5(<0.001) | −1.83(−2.83,−0.83) | ||
| > 40 years | 3 | 86 | 78 | 93.6(<0.001) | −1.40(−2.84,0.04) | 0.23 | 0.630 |
| Diagnostic criteria of PTSD | |||||||
| DSM | 2 | 35 | 35 | 28.7(0.240) | −2.78(−3.46,−2.10) | ||
| DSM + ICD | 1 | 21 | 23 | Not applicable | −0.63(−1.24,−0.02) | ||
| Not reported | 3 | 116 | 114 | 91.8(<0.001) | −1.72(−2.95,−0.50) | ||
| ICD | 1 | 25 | 15 | Not applicable | −0.70(−1.36,−0.04) | 18.60 | <0.001 |
| Music therapy | |||||||
| Led by music therapists | 4 | 81 | 73 | 89.1(<0.001) | −1.58(−2.75,−0.40) | ||
| Music listening only | 3 | 116 | 114 | 91.8(<0.001) | −1.72(−2.95,−0.50) | 0.030 | 0.866 |
| Treatment duration | |||||||
| 2–4 months | 3 | 75 | 75 | 0.0(0.49) | −2.83(−3.29,−2.36) | ||
| <2 months | 4 | 122 | 112 | 73.6(0.038) | −0.95(−1.47,−0.42) | 27.79 | <0.001 |
| Treatment frequency | |||||||
| Daily | 3 | 116 | 114 | 92.3(<0.001) | −1.72(−2.95,−0.50) | ||
| Weekly or biweekly | 4 | 81 | 73 | 89.1(<0.001) | −1.58(−2.75,−0.40) | 0.030 | 0.866 |
| Intervention of the control group | |||||||
| Care as usual alone | 4 | 143 | 141 | 91.1(<0.001) | −2.04(−3.11,−0.96) | ||
| Waitlist + care as usual | 3 | 54 | 46 | 54.7(0.110) | −0.95(−1.63,−0.26) | 2.79 | 0.095 |
Note: DSM, Diagnostic & Statistical Manual of Mental Disorders; ICD, International Classification of Diseases; NR, not reported
3.6. Certainty of the evidence for the efficacy of music therapy for PTSD
We initially classified the level of certainty for the efficacy of music therapy as high. However, due to substantial RoB, high heterogeneity, clinical diversity in the music therapy among included studies, and a relatively small overall sample size in this meta-analysis, we downgraded the certainty by four levels. However, given the large effect size of music therapy's efficacy for PTSD symptoms, and the dose–response relationship – evident through a higher treatment effect size in studies with a longer treatment duration (as indicated in the subgroup analysis) – we upgraded the certainty by two levels. We ultimately concluded with a low level of certainty regarding the evidence.
4. Discussion
The foremost clinical contribution of this meta-analysis is its role as the inaugural critical appraisal of the existing methodologically rigorous evidence, specifically, RCTs, for the effectiveness and acceptability of music therapy for PTSD. The main findings include the large (SMD = −1.64, P < .001) and comparable (SMD = −0.28, P = .330) treatment effects of music therapy for PTSD compared to CAU and CAU plus standard psychotherapy respectively, as well as the similar retention rates in the music therapy group when compared to both the CAU group (RD = 0.03, P = .769) and the CAU plus standard psychotherapy group (RD = 0.16, P = .829). The diagnostic criteria for PTSD that were adopted in the included studies were found to be a significant moderator of the treatment effect. In particular, studies using both DSM and ICD criteria revealed the smallest effect. Moreover, we identified a correlation between the duration of music therapy and effectiveness – with longer therapy duration linked to a larger treatment effect. After taking the five quality domains of clinical evidence into consideration, the GRADE approach assessed the certainty of the evidence for music therapy's efficacy in treating PTSD as low.
The therapeutic effects of music therapy for PTSD involve mechanisms from social, cognitive, and neurobiological realms (Landis-Shack et al., 2017). For example, music is frequently used as a grounding method in psychotherapy to manage the emotional turmoil linked with PTSD patients’ intrusive or unsettling reminders (Carr et al., 2012; Cheng et al., 2023). Furthermore, researchers propose that certain forms of music therapy, like group music making, can bolster social connections and alleviate isolation, consequently enhancing emotional well-being and reducing avoidant behaviours (Chen et al., 2022; Clifford et al., 2022; Ho et al., 2011). Experimental studies indicate that music can elevate the production of dopamine and endorphins, lower cortisol levels, and increase cerebral blood flow to areas correlated with pleasing behaviours, consequently attenuating fear, sadness, co-occurring depression and anxiety, and over-arousal and amplifying experiences of pleasure and reward (Bodner et al., 2001; Boso et al., 2006; Okyay & Ucar, 2023). Importantly, the music interventions in some of the included studies were not pure music therapy. They were embedded with procedures or techniques from psychotherapies such as music-guided muscle relaxation, emotion-regulation, and mindfulness. It is highly likely that the addition of psychotherapy techniques could have enhanced the treatment efficacy of music. In this meta-analysis, we identified a large therapeutic effect of music therapy for PTSD, reaching the level of standard psychotherapy. We speculate that this effect is likely due to a combination of the aforementioned social, cognitive, and neurobiological mechanisms as well as the embedded psychotherapy techniques.
A potential advantage of music therapy compared to trauma-focused psychotherapy is its lower attrition rate upon treatment completion (Beck et al., 2021). However, this meta-analysis only found a slightly higher retention rate in the music therapy group compared to the standard psychotherapy group, a difference that lacked statistical significance. As only two of the studies included in our analysis were psychotherapy-controlled, the suggested benefit of a lower attrition rate in music therapy needs further validation from future research.
Perhaps patients who meet both DSM and ICD criteria for PTSD have more complex clinical symptomatology and longer disease duration, making them more difficult to treat. For instance, DSM-IV's diagnosis of PTSD requires the presence of clinically significant distress or functional impairment, which ICD-10 doesn't necessitate. While DSM-IV considers both avoidance and numbing symptoms, ICD-10 only requires avoidance symptoms. Moreover, DSM-IV mandates that PTSD symptoms persist for at least one month, whereas ICD-10 emphasizes the commencement of symptoms within six months of the traumatic event and their persistence, without specifying a minimum duration (Stein et al., 2014). This could explain why studies adopting both diagnostic criteria tend to have the smallest treatment effect in this meta-analysis. A previously published meta-analysis of music therapy for serious mental illnesses revealed that patients who underwent only a few sessions showed minor improvements, but those who participated in longer or more frequent sessions experienced significantly greater benefits (Gold et al., 2009). In line with this dose–response relationship, our meta-analysis found a positive correlation between the effect of music therapy and its duration.
The theory of music therapy highlights the crucial role that qualified music therapists play in its administration, including assessing patients’ needs, planning treatment goals, preparing for sessions, and monitoring progression (Odell-Miller, 2016). Nevertheless, results from the subgroup analysis based on the involvement of a music therapist demonstrated similar treatment effects of music therapy for PTSD between studies that provided therapist-led therapy and those that only involved music-listening (Table 2). Given the small number and sample sizes of the included studies, this finding does not sufficiently refute the role of professional music therapists in delivering music therapy. Instead, it suggests that listening to therapeutic music is a beneficial alternative music therapy strategy for PTSD in healthcare settings where qualified music therapists are not available, or when patients cannot afford therapist-guided therapy.
The large FSNs, 707 and 347 for statistical significance levels of 0.05 and 0.01, respectively, in this study, suggest greater confidence in the robustness of the meta-analytic results of studies with inactive control groups.
Unlike RCTs for medications, implementing a placebo intervention to mimic the active treatment in RCTs for music therapy is very challenging. As a result, all the studies included in this meta-analysis exhibited a high RoB because of possible deviations from intended interventions. Additionally, the majority were affected by high RoB due to issues in the randomization process and outcome measurement. As a consequence, in this meta-analysis, the level of certainty in the available evidence regarding the efficacy of music therapy for PTSD was rated as low. Hence, it's essential to conduct more methodologically rigorous RCTs with active control groups to solidify the evidence for music therapy as a treatment for PTSD.
This study has several limitations. Music therapy can be highly structured and substantially varied across different instruments, mediums, methods of expression, and dosing parameters. The first major limitation of this study lies in the significant clinical heterogeneity of music therapy regimes among the included studies. This heterogeneity makes it challenging to generalize the current findings, as it prevents us from recommending an optimal music therapy method. Factors contributing to this difficulty include the selection of the instrument, the frequency and duration of treatment, the involvement of a qualified music therapist, and the incorporation of music therapy into psychotherapy. Secondly, physically ill patients with PTSD were overrepresented, making up over 50% of the entire patient sample in the included studies. As indicated in Table 2, the pooled SMD did not show statistical significance in psychiatric patients, though it was significant in physically ill patients. As a result, it remains undetermined if the current findings can be generalized to PTSD patients in psychiatric care settings. Thirdly, despite the inclusion of nine studies, the total sample of PTSD patients was still relatively small (n = 527), especially concerning studies that featured active control groups (n = 142). Fourthly, this meta-analysis examined the efficacy of music therapy for PTSD upon completion of treatment only. Due to inadequate data for long-term efficacy in the included studies, it remains unclear whether and for how long the treatment effects of music therapy would persist.
Findings from the present meta-analysis suggest that music therapy is effective in reducing post-traumatic symptoms in individuals with PTSD, yet the low certainty level of the evidence limits their generalizability. Nevertheless, these promising findings still indicate that music therapy deserves consideration and further research in the context of clinical management for patients with PTSD. Due to an inadequate number of studies, more empirical research is needed to examine the advantage of the lower attrition rate associated with music therapy. Given the aforementioned limitations, we strongly recommend the development of standardized music therapy protocols and the conducting of more methodologically stringent studies to determine the effectiveness of music therapy. Based on the studies reviewed in this study, several important considerations need to be addressed when developing standardized music therapy protocols. These include the involvement of music therapists, number of sessions, duration and frequency of intervention, the criteria for selecting therapeutic music that is culturally adaptable, the choice of musical instruments, and the integration of psychotherapies into the music therapy programme.
Funding Statement
This work was supported by National Natural Science Foundation of China (grant number: 71774060), 2015 Irma and Paul Milstein Program for Senior Health Awards from the Milstein Medical Asian American Partnership Foundation, the Young Top Talent Programme in Public Health from Health Commission of Hubei Province (PI: Zhong BL), and Wuhan Health and Family Planning Commission (grant number: WX17Q30; WG16A02; WG14C24). The funding source listed had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data supporting the results and analyses presented are available within this paper.
References
- Aalbers, S., Fusar-Poli, L., Freeman, R. E., Spreen, M., Ket, J. C., Vink, A. C, Maratos, A., Crawford, M., Chen, X. J., & Gold, C. (2017). Music therapy for depression. Cochrane Database of Systematic Reviews, 11(11), CD004517. 10.1002/14651858.CD004517.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, B. D., Meyer, S. L., Simonsen, E., Søgaard, U., Petersen, I., Arnfred, S. M. H., Tellier, T., & Moe, T. (2021). Music therapy was noninferior to verbal standard treatment of traumatized refugees in mental health care: Results from a randomized clinical trial. European Journal of Psychotraumatology, 12(1), 1930960. 10.1080/20008198.2021.1930960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanaru, M., Bloch, B., Vadas, L., Arnon, Z., Ziv, N., Kremer, I., & Haimov, I. (2012). The effects of music relaxation and muscle relaxation techniques on sleep quality and emotional measures among individuals with posttraumatic stress disorder. Mental Illness, 4(2), e13–e65. 10.4081/mi.2012.e13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodner, M., Muftuler, L. T., Nalcioglu, O., & Shaw, G. L. (2001). FMRI study relevant to the mozart effect: Brain areas involved in spatial-temporal reasoning. Neurological Research, 23(7), 683–690. 10.1179/016164101101199108 [DOI] [PubMed] [Google Scholar]
- Boso, M., Politi, P., Barale, F., & Enzo, E. (2006). Neurophysiology and neurobiology of the musical experience. Functional Neurology, 21(4), 187–191. [PubMed] [Google Scholar]
- Cao, M., & Zhang, Z. (2023). Adjuvant music therapy for patients with hypertension: A meta-analysis and systematic review. BMC Complementary Medicine and Therapies, 23(1), 110. 10.1186/s12906-023-03929-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr, C., d'Ardenne, P., Sloboda, A., Scott, C., Wang, D., & Priebe, S. (2012). Group music therapy for patients with persistent post-traumatic stress disorder–an exploratory randomized controlled trial with mixed methods evaluation. Psychology and Psychotherapy: Theory, Research and Practice, 85(2), 179–202. 10.1111/j.2044-8341.2011.02026.x [DOI] [PubMed] [Google Scholar]
- Chen, W. C., Chen, S. J., & Zhong, B. L. (2022). Sense of alienation and its associations with depressive symptoms and poor sleep quality in older adults who experienced the lockdown in Wuhan, China, during the COVID-19 pandemic. Journal of Geriatric Psychiatry and Neurology, 35(2), 215–222. 10.1177/08919887221078564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng, W. L., Tang, A. C., Tsang, M. C., Wong, L. L., & Korlin, D. (2023). Effect of music breathing, a program based on mindful breathing and music listening therapy for promoting sense of coherence in young people: Study protocol for a randomized controlled trial. Trials, 24(1), 662. 10.1186/s13063-023-07645-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cipriani, A., Williams, T., Nikolakopoulou, A., Salanti, G., Chaimani, A., Ipser, J., Cowen, P. J., Geddes, J. R., & Stein, D. J. (2018). Comparative efficacy and acceptability of pharmacological treatments for post-traumatic stress disorder in adults: A network meta-analysis. Psychological Medicine, 48(12), 1975–1984. 10.1017/S003329171700349X [DOI] [PubMed] [Google Scholar]
- Clark, R., Kuffel, R. L., Neylan, T. C., Maguen, S., Li, Y., Boscardin, W. J., & Byers, A. L. (2023). Posttraumatic stress disorder, suicide, and unintended overdose death in later life: A national cohort study of veterans aged 50 and older. Journal of the American Geriatrics Society, 71(5), 1462–1472. 10.1111/jgs.18199 [DOI] [PubMed] [Google Scholar]
- Clifford, A. M., Bhriain Ni, O., Byrne, S., Cheung, P. S., Louw, Q., Glynn, L., Moss, H., O'Neill, D., Woods, C. B., Sheikhi, A., Gowran, R. J., Maher, C., Kennelly, B., Salsberg, J., & Thabane, L. (2022). Music and movement for health: Protocol for a pragmatic cluster-randomised feasibility pilot trial of an arts-based programme for the health and wellbeing of older adults. HRB Open Research, 5, 42. 10.12688/hrbopenres.13535.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Witte, M., Pinho, A. D. S., Stams, G. J., Moonen, X., Bos, A. E. R., & van Hooren, S. (2022). Music therapy for stress reduction: A systematic review and meta-analysis. Health Psychology Review, 16(1), 134–159. 10.1080/17437199.2020.1846580 [DOI] [PubMed] [Google Scholar]
- Du, N., Shi, X., Cui, S., Wang, Z., Hu, Y., & Tang, J. (2019). The effect of participatory music therapy on the rehabilitation outcomes of post-traumatic stress disorder in patients with spinal cord injury. Chinese Journal of Rehabilitation Medicine, 34(9), 1097–1099. 10.3969/j.issn.1001-1242.2019.09.018 [DOI] [Google Scholar]
- Feng, F., Zhang, Y., Hou, J., Cai, J., Jiang, Q., Li, X., Zhao, Q., Li, B. A. (2018). Can music improve sleep quality in adults with primary insomnia? A systematic review and network meta-analysis. International Journal of Nursing Studies, 77, 189–196. 10.1016/j.ijnurstu.2017.10.011 [DOI] [PubMed] [Google Scholar]
- Gao, J., & Chen, C. (2018). Effect of tomatis sound therapy on post-traumatic stress disorder of patients with breast cancer undergoing chemotherapy. Chinese Journal of Disaster Medicine, 6(4), 213–217. 10.13919/j.issn.2095-6274.2018.04.008 [DOI] [Google Scholar]
- Gold, C., Solli, H. P., Kruger, V., & Lie, S. A. (2009). Dose-response relationship in music therapy for people with serious mental disorders: Systematic review and meta-analysis. Clinical Psychology Review, 29(3), 193–207. 10.1016/j.cpr.2009.01.001 [DOI] [PubMed] [Google Scholar]
- Guyatt, G. H., Oxman, A. D., Vist, G. E., Kunz, R., Falck-Ytter, Y., Alonso-Coello, P., Schünemann, H. J., & GRADE Working Group . (2008). GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ, 336(7650), 924–926. 10.1136/bmj.39489.470347.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haase, U. (2012). Thoughts on WFMT's definition of music therapy. Nordic Journal of Music Therapy, 21(2), 194–195. 10.1080/08098131.2012.678373 [DOI] [Google Scholar]
- Hamblen, J. L., Norman, S. B., Sonis, J. H., Phelps, A. J., Bisson, J. I., Nunes, V. D., Megnin-Viggars, O., Forbes, D., Riggs, D. S. & Schnurr, P. P. (2019). A guide to guidelines for the treatment of posttraumatic stress disorder in adults: An update. Psychotherapy, 56(3), 359–373. 10.1037/pst0000231 [DOI] [PubMed] [Google Scholar]
- He, H., Li, Z., Zhao, X., & Chen, X. (2023). The effect of music therapy on anxiety and pain in patients undergoing prostate biopsy: A systematic review and meta-analysis. Complementary Therapies in Medicine, 72, 102913. 10.1016/j.ctim.2022.102913 [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J., & Welch, V. A. (2023). Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). Cochrane, 2023. www.training.cochrane.org/handbook.
- Hirschberg, R., Sylvia, L. G., Wright, E. C., Gupta, C. T., McCarthy, M. D., Harward, L. K., Goetter, E. M., Boland, H., Tanev, K., & Spencer, T. J. (2020). Collaborative songwriting intervention for veterans with post-traumatic stress disorder. The Journal of Alternative and Complementary Medicine, 26(3), 198–203. 10.1089/acm.2019.0368 [DOI] [PubMed] [Google Scholar]
- Ho, P., Tsao, J. C., Bloch, L., & Zeltzer, L. K. (2011). The impact of group drumming on social-emotional behavior in low-income children. Evidence-Based Complementary and Alternative Medicine, 2011, 250708. 10.1093/ecam/neq072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaacs, A. N., Brooks, H., Lawn, S., Mohammadi, L., Vicary, E., & Sutton, K. (2022). Effectiveness of personal recovery facilitators in adults with schizophrenia and other psychoses: A systematic review of reviews and narrative synthesis. Schizophrenia Research, 246, 132–147. 10.1016/j.schres.2022.06.018 [DOI] [PubMed] [Google Scholar]
- Kim, S., Park, S., & Kim, G. U. (2021). Association of depression, pain, resilience, social support with post-traumatic stress in sexual abuse: A quantile regression approach. Nursing & Health Sciences, 23(3), 611–619. 10.1111/nhs.12815 [DOI] [PubMed] [Google Scholar]
- Koenen, K. C., Ratanatharathorn, A., Ng, L., McLaughlin, K. A., Bromet, E. J., Stein, D. J., Karam, E. G., Ruscio, A. M., Benjet, C., Scott, K., Atwoli, L., Petukhova, M., Lim, C. C. W.Aguilar-Gaxiola, S., Al-Hamzawi, A., Alonso, J., Bunting, B., Ciutan, M., de Girolamo, G., … Kessler R. C. (2017). Posttraumatic stress disorder in the world mental health surveys. Psychological Medicine, 47(13), 2260–2274. 10.1017/S0033291717000708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landis-Shack, N., Heinz, A. J., & Bonn-Miller, M. O. (2017). Music therapy for posttraumatic stress in adults: A theoretical review. Psychomusicology, 27(4), 334–342. 10.1037/pmu0000192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, H. Y., Nam, E. S., Chai, G. J., & Kim, D. M. (2023). Benefits of music intervention on anxiety, pain, and physiologic response in adults undergoing surgery: A systematic review and meta-analysis. Asian Nursing Research, 17(3), 138–149. 10.1016/j.anr.2023.05.002 [DOI] [PubMed] [Google Scholar]
- Lee, W. J., Choi, S. H., Shin, J. E., Oh, C. Y., Ha, N. H., Lee, U. S., Lee, Y. I., Choi, Y., Lee, S., Jang, J. H., Hong, Y. C., & Kang, D. H. (2018). Effects of an online imagery-based treatment program in patients with workplace-related posttraumatic stress disorder: A pilot study. Psychiatry Investigation, 15(11), 1071–1078. 10.30773/pi.2018.09.28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis, C., Roberts, N. P., Gibson, S., & Bisson, J. I. (2020). Dropout from psychological therapies for post-traumatic stress disorder (PTSD) in adults: Systematic review and meta-analysis. European Journal of Psychotraumatology, 11(1), 1709709. 10.1080/20008198.2019.1709709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Z., Liu, L., Zhang, Y., & Li, L. (2023). Effect of Wuyintiaoshen therapy on post? Traumatic stress disorder and sleep quality in patients with acute ischemic stroke. Chinese Nursing Research, 37(4), 577–583. 10.12102/j.issn.1009-6493.2023.04.003 [DOI] [Google Scholar]
- Luo, W., Zhong, B. L., & Chiu, H. F. (2021). Prevalence of depressive symptoms among Chinese university students amid the COVID-19 pandemic: A systematic review and meta-analysis. Epidemiology and Psychiatric Sciences, 30, e31. 10.1017/S2045796021000202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macfarlane, C., Masthoff, E., & Hakvoort, L. (2019). Short-Term music therapy attention and arousal regulation treatment (SMAART) for prisoners with posttraumatic stress disorder: A feasibility study. Journal of Forensic Psychology Research and Practice, 19(5), 376–392. 10.1080/24732850.2019.1670023 [DOI] [Google Scholar]
- Mavranezouli, I., Megnin-Viggars, O., Daly, C., Dias, S., Welton, N. J., Stockton, S., Bhutani, G., Grey, N., Leach, J., Greenberg, N., Katona, C., El-Leithy, S. & Pilling, S. (2020). Psychological treatments for post-traumatic stress disorder in adults: A network meta-analysis. Psychological Medicine, 50(4), 542–555. 10.1017/S0033291720000070 [DOI] [PubMed] [Google Scholar]
- Merz, J., Schwarzer, G., & Gerger, H. (2019). Comparative efficacy and acceptability of pharmacological, psychotherapeutic, and combination treatments in adults with posttraumatic stress disorder: A network meta-analysis. JAMA Psychiatry, 76(9), 904–913. 10.1001/jamapsychiatry.2019.0951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odell-Miller, H. (2016). The role, function and identity of music therapists in the 21st century, including new research and thinking from a UK perspective. British Journal of Music Therapy, 30(1), 5–12. 10.1177/13594575166395 [DOI] [Google Scholar]
- Okyay, E. K., & Ucar, T. (2023). The effect of emotional freedom technique and music applied to pregnant women who experienced prenatal loss on psychological growth, well-being, and cortisol level: A randomized controlled trial. Archives of Psychiatric Nursing, 45, 101–112. 10.1016/j.apnu.2023.04.027 [DOI] [PubMed] [Google Scholar]
- Ophir, I., & Jacoby, R. (2020). Sparks that became a little light over time": A qualitative investigation of musicking as a means of coping in adults with PTSD. PLoS One, 15(1), e0228050. 10.1371/journal.pone.0228050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pezzin, L. E., Larson, E. R., Lorber, W., McGinley, E. L., & Dillingham, T. R. (2018). Music-instruction intervention for treatment of post-traumatic stress disorder: A randomized pilot study. BMC Psychology, 6(1), 60. 10.1186/s40359-018-0274-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pourmovahed, Z., Yassini Ardekani, S. M., Roozbeh, B., & Ezabad, A. R. (2021). The effect of Non-verbal music on posttraumatic stress disorder in mothers of premature neonates. Iranian Journal of Nursing and Midwifery Research, 26(2), 150–153. 10.4103/ijnmr.IJNMR_37_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudstam, G., Elofsson, U. O. E., Söndergaard, H. P., Bonde, L. O., & Beck, B. D. (2022). Trauma-focused group music and imagery with women suffering from PTSD/complex PTSD: A randomized controlled study. European Journal of Trauma & Dissociation, 6(3), 100277. 10.1016/j.ejtd.2022.100277 [DOI] [Google Scholar]
- Stein, D. J., McLaughlin, K. A., Koenen, K. C., Atwoli, L., Friedman, M. J., Hill, E. D., Maercker, A., Petukhova, M., Shahly, V., van Ommeren, M., Alonso, J., Borges, G., de Girolamo, G., de Jonge, P., Demyttenaere, K., Florescu, S., Karam, Kawakami E. G., N., Matschinger, H., … Kessler, R.C. (2014). DSM-5 and ICD-11 definitions of posttraumatic stress disorder: Investigating “narrow” and “broad” approaches. Depression and Anxiety, 31(6), 494–505. 10.1002/da.22279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein, M. B. (2023). Posttraumatic stress disorder in adults: Treatment overview. In: UpToDate, Post, TW (Ed), UpToDate, Waltham, MA. Retrieved August 21, 2023, from https://www.uptodate.com/contents/posttraumatic-stress-disorder-in-adults-treatment-overview#:~:text=Trauma%2Dfocused%20psychotherapy%20as%20preferred%20treatment%20%E2%80%94%20For%20most%20adults%20diagnosed,SSRI%5D%20or%20serotonin%2Dnorepinephrine%20reuptake
- Sterne, J. A. C., Savovic, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., Cates, C. J., Cheng, H. Y., Corbett, M. S., Eldridge, S.M., Emberson, J. R., Hernán, M. A., Hopewell, S., Hróbjartsson, A., Junqueira, D. R., Jüni, P., Kirkham, J J., Lasserson, T., Li, T., … Higgins, J. P. T. (2019). Rob 2: A revised tool for assessing risk of bias in randomised trials. BMJ, 366, l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- Varker, T., Jones, K. A., Arjmand, H.-A., Hinton, M., Hiles, S. A., Freijah, I., Forbes, D., Kartal, D., Phelps, A., Bryant, R. A., McFarlane, A., Hopwood, M. & O'Donnell, M. (2021). Dropout from guideline-recommended psychological treatments for posttraumatic stress disorder: A systematic review and meta-analysis. Journal of Affective Disorders Reports, 4, 100093. 10.1016/j.jadr.2021.100093 [DOI] [Google Scholar]
- von der Warth, R., Dams, J., Grochtdreis, T., & Konig, H. H. (2020). Economic evaluations and cost analyses in posttraumatic stress disorder: A systematic review. European Journal of Psychotraumatology, 11(1), 1753940. 10.1080/20008198.2020.1753940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong, L. J., Zhong, B. L., Cao, X. J., Xiong, H. G., Huang, M., Ding, J., Li, W. T., Tong, J., Shen, H. Y., Xia, J. H., & Hu, Y. (2021). Possible posttraumatic stress disorder in Chinese frontline healthcare workers who survived COVID-19 6 months after the COVID-19 outbreak: Prevalence, correlates, and symptoms. Translational Psychiatry, 11(1), 374. 10.1038/s41398-021-01503-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu, Y. M., Deng, F., & Zhong, B. L. (2022). Facial emotion identification impairments in Chinese persons living with schizophrenia: A meta-analysis. Frontiers in Psychiatry, 13, 1097350. 10.3389/fpsyt.2022.1097350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, J., Wang, D., & Liu, D. (2022). Observation on the effect of mindfulness soothing music training on patients with multiple injuries combined with post-traumatic stress disorder. Chinese Journal of Convalescent Medicine, 31(5), 525–527. 10.13517/j.cnki.ccm.2022.05.018 [DOI] [Google Scholar]
- Zhang, Y., Cai, J., An, L., Hui, F., Ren, T., Ma, H., & Zhao, Q. (2017). Does music therapy enhance behavioral and cognitive function in elderly dementia patients? A systematic review and meta-analysis. Ageing Research Reviews, 35, 1–11. 10.1016/j.arr.2016.12.003 [DOI] [PubMed] [Google Scholar]
- Zhao, Y. J., Zhang, C., Guo, T., Sha, S., Su, Z., Cheung, T., Jackson, T., An, F. R. & Xiang, Y. T. (2023). Associations between post-traumatic stress symptoms and quality of life among psychiatric healthcare personnel in China during the COVID-19 pandemic: A network approach. Frontiers in Psychiatry, 14, 975443. 10.3389/fpsyt.2023.975443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong, B. L., Xu, Y. M., Xie, W. X., & Li, Y. (2019). Can P300 aid in the differential diagnosis of unipolar disorder versus bipolar disorder depression? A meta-analysis of comparative studies. Journal of Affective Disorders, 245, 219–227. 10.1016/j.jad.2018.11.010 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the results and analyses presented are available within this paper.