Abstract
Simple Summary
The effectiveness of chemical control of Aedes (Ae.) aegypti is threatened by the increasing frequency of insecticide resistance. This study aimed to determine, in two cities of Benin, the insecticide resistance profiles of Ae. aegypti, the presence of detoxification enzymes, and the frequency of kdr mutations. Ae. aegypti eggs were collected in the study areas using gravid Aedes traps (GATs). Centers for Disease Control and Prevention (CDC) bottle bioassays were used to assess the susceptibility status of adult female Ae. aegypti, followed by kdr screening using allele-specific PCR. The activity levels of key detoxification enzymes were measured among individual, unexposed, and un-engorged adult female Ae. aegypti. In both study sites, Ae. aegypti was resistant to the pyrethroids deltamethrin and permethrin, but susceptible to the carbamate bendiocarb. Significant over-expression of glutathione-S-transferases and under-expression of α and β esterases were observed in these vector populations. Three kdr mutations (F1534C, S989P, and V1016G) were possibly present in resistant Ae. aegypti at high frequencies, including the simultaneous occurrence of all three mutations in individual mosquitoes. Study findings will be used to inform prospective vector control strategies in Benin.
Abstract
Epidemics of arboviruses in general, and dengue fever in particular, are an increasing threat in areas where Aedes (Ae.) aegypti is present. The effectiveness of chemical control of Ae. aegypti is jeopardized by the increasing frequency of insecticide resistance. The aim of this study was to determine the susceptibility status of Ae. aegypti to public health insecticides and assess the underlying mechanisms driving insecticide resistance. Ae. aegypti eggs were collected in two study sites in the vicinity of houses for two weeks using gravid Aedes traps (GATs). After rearing the mosquitoes to adulthood, female Ae. aegypti were exposed to diagnostic doses of permethrin, deltamethrin and bendiocarb, using Centers for Disease Control and Prevention (CDC) bottle bioassays. Unexposed, un-engorged female Ae. aegypti were tested individually for mixed-function oxidase (MFO), glutathione-S-transferase (GST) and α and β esterase activities. Finally, allele-specific PCR (AS-PCR) was used to detect possible kdr mutations (F1534C, S989P, and V1016G) in the voltage-gated sodium channel gene in insecticide-exposed Ae. aegypti. Most traps were oviposition positive; 93.2% and 97% of traps contained Ae. aegypti eggs in the 10ème arrondissement of Cotonou and in Godomey-Togoudo, respectively. Insecticide bioassays detected resistance to permethrin and deltamethrin in both study sites and complete susceptibility to bendiocarb. By comparison to the insecticide-susceptible Rockefeller strain, field Ae. aegypti populations had significantly higher levels of GSTs and significantly lower levels of α and β esterases; there was no significant difference between levels of MFOs. AS-PCR genotyping revealed the possible presence of 3 kdr mutations (F1534C, S989P, and V1016G) at high frequencies; 80.9% (228/282) of the Ae. aegypti tested had at least 1 mutation, while the simultaneous presence of all 3 kdr mutations was identified in 13 resistant individuals. Study findings demonstrated phenotypic pyrethroid resistance, the over-expression of key detoxification enzymes, and the possible presence of several kdr mutations in Ae. aegypti populations, emphasizing the urgent need to implement vector control strategies targeting arbovirus vector species in Benin.
Keywords: Aedes aegypti, pyrethroid resistance, kdr mutations, detoxification enzymes, 10ème arrondissement of Cotonou, Godomey-Togoudo, Benin
1. Introduction
Aedes (Ae.) aegypti mosquitoes are the main vector species of dengue viruses worldwide. The number of dengue fever cases reported to the World Health Organization (WHO) has increased dramatically by more than eightfold over the previous twenty years, from 505,430 cases in 2000 to over 2.4 million cases in 2010 and 5.2 million cases in 2019 [1]. Ae. aegypti is present in Benin and proliferating globally due to the development of trade, rapid urbanization, and high frequency of international travel [2]. Between 2010 and 2019, dengue fever cases have been diagnosed in Benin, resulting in at least one death [2].
In the absence of effective vaccines and available treatments, vector control remains the main strategy for dengue virus prevention. Vector control relies on the use of insecticides, such as pyrethroids, for house spraying and personal protection [3]. As a result of the strong selection pressures exerted using insecticides in agricultural practices and malaria control, including pyrethroid-only long-lasting insecticidal nets (LLINs) and indoor residual spraying (IRS) with pyrethroids, insecticide resistance among Ae. aegypti populations is common and widespread worldwide. According to the WHO, insecticide resistance is defined as “the ability of mosquitoes to survive exposure to a standard dose of insecticide; this ability may result from physiological or behavioral adaptation” [4]. Two of the main mechanisms underlying insecticide resistance in mosquitoes are alterations in the insecticide target site, including knock-down resistance (kdr) mutations in the voltage-gated sodium channel (vgsc) gene and increased metabolic activity [5,6]. Metabolic resistance to pyrethroids may be mediated by glutathione-S-transferases (GSTs), esterases, and mixed-function oxidases (MFOs) [7,8,9].
Kdr mutations have been studied in Ae. aegypti extensively; these mutations confer cross-resistance to pyrethroids and DDT by altering the structure of the vgsc, thus decreasing binding affinity of target insecticides [10]. Several kdr mutations have been identified in Ae. aegypti populations worldwide, including V1016I, V410L, S989P, I1011V, V1016G, I1011M, and F1534C [10,11,12,13]. In Africa, F1534C, V1016I, V410L, and S989P have been associated with pyrethroid resistance in Ae. aegypti. The presence of kdr has been reported in countries near to Benin, such as Burkina Faso, Nigeria, and Ghana [14,15,16,17].
The emergence and re-emergence of dengue fever epidemics requires effective vector control responses, including monitoring of vector population insecticide susceptibility. To date, there is a considerable paucity of insecticide resistance information for Ae. aegypti populations in Benin.
2. Materials and Methods
2.1. Study Sites and Mosquito Sampling
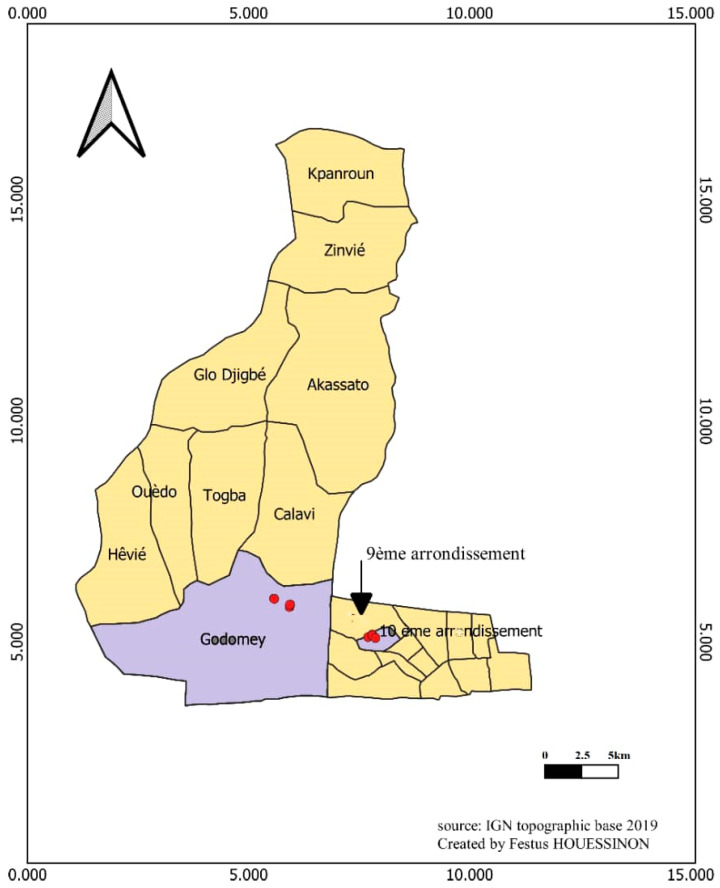
Adult Ae. aegypti mosquitoes were reared from eggs collected over a 2-week period in the 10ème arrondissement of Cotonou and in Godomey-Togoudo, Abomey-Calavi from 31 December 2021 (Figure 1). This collection period coincided with the dry season, which is a period characterized by a scarcity of Aedes breeding sites. During this sampling period, a total of 73 gravid Aedes traps were set in the 10ème arrondissement of Cotonou and 74 in Godomey-Togoudo. The traps used are black plastic pots that can contain half a liter of water, in which wooden egg-laying supports have been immersed. The traps were hung on the box or wall with a nail and a wire. The egg carriers were removed from each trap after 7 days, eggs were counted and then hatched according to standard insectary rearing procedures for Aedes species. A dipper was used to visually count the number of larvae per bowl. Larval hatching rate was measured by dividing the number of larvae by the total number of immersed eggs ×100. Emergent adults were counted by aspiration. Adult emergence rate was measured by dividing the number of emerged adults by the total number of larvae ×100.
Figure 1.
Map of trapping sites in Cotonou and Godomey-Togoudo, Benin. The dots correspond to different traps sites.
2.2. Aedes Morphological Identification
Adult Ae. aegypti for insecticide resistance bioassays were identified using Fontenille’s taxonomic keys [18]. Ae. aegypti and other Aedes were distinguished by characteristic white stripes on their legs. Then, the thorax was used to differentiate the two species; Ae. aegypti has two thin white median lines with a lyre pattern, whereas Ae. albopictus has only one distinct white central line.
2.3. Insecticide Resistance Bioassays
Insecticide resistance profiles for Ae. aegypti field populations were measured using Centers for Disease Control and Prevention (CDC) bottle bioassays [19]. Two-to-five-day-old female Ae. aegypti mosquitoes were exposed to diagnostic doses of deltamethrin (10 µg/bottle), permethrin (15 µg/bottle), and bendiocarb (12.5 µg/bottle) in Wheaton 250 mL bottles, alongside an acetone-treated control bottle. In each bioassay, 10–25 unfed mosquitoes were introduced into each bottle and knock-down was scored every 15 min until all were dead, or up to two hours had elapsed; data were reported for the diagnostic time of 30 min for all insecticides. Approximately 100 mosquitoes (in 3–4 bottle bioassays) were tested per insecticide dose.
2.4. Measurement of Detoxification Enzyme Activity
Biochemical tests were performed to quantify the activity of families of detoxification enzymes, including non-specific esterases (α and β esterases), mixed-function oxidases (MFOs), glutathione S-transferases (GSTs) and total proteins in 3–5-day old female Ae. aegypti mosquitoes; a total of 80 non-insecticide exposed mosquitoes were tested per study site, in parallel with the Rockfeller susceptible strain of Ae. aegypti as a control [20].
Individual mosquitoes were ground in 200 µL of distilled water using sterile pestles, after which the lysate was centrifuged at 14,000 rpm for two minutes. For non-specific esterases, we used 2 substrates: α-naphthyl acetate and β-naphthyl acetate. Each plate was calibrated with the products of the esterase-substrate reaction (α-naphthyl acetate or β-naphthyl acetate). The reaction consisted of hydrolysis of α-naphthyl (or β-naphthyl) acetate by esterase with the formation of α-(or β)-naphthol with Fast Garnett Salt. This assay involved determining the quantity of α-(or β)-naphthol formed as a function of time. For each esterase plate, 10 µL of mosquito lysate was added in duplicate. Then, the standard curves of α or β naphthol were generated with Gen5 software (version 2.0) to determine each well concentration. To each well, 10 µL of supernatant or standards and 90 µL of Phosphate Saline Buffer (PBS) pH 6.5 + 1% triton ×100 was added. The plate was then incubated at 25 °C for 10 min, after which 100 µL of working solution (500 µL α-naphthyl acetate or β-naphthyl (0.03 M) + 2.5 mL PBS buffer (pH mL 6.5) + 7 mL H2O), was added to each well and the plate was again incubated at 25 °C for 30 min. Finally, 100 µL of 3 mM of a solution of Fast Garnett Salt dissolved in 10 mL distilled water was added to each well and the plate was incubated at 25 °C for 10 min. Plate absorbance values were read on an ELx808 spectrophotometer at 550 nm. The standard curve fitted a straight line: DO = ax + b where x is the quantity of α- or β-naphthol in the well. Using this formula with the optical density (OD) of the sample we calculated the amount of α- or β-naphthol produced by 10 µL of mosquito supernatant for 30 min. Esterase activity of each mosquito was expressed as µmol α- or β-naphthol produced/min/mg protein and calculated according to the following: α- or β-naphthol in µmol per mL/amount of protein in mg per mL/30.
For MFOs, 20 µL of mosquito lysate was added to 2 wells (technical duplicate) of a 96-well ELISA plate. Then, the standards curve of cytochrome C was generated with Gen5 software to determine the each well concentration. The first 2 columns are reserved for the H2O control and the standard range. For each duplicate of 20 µL of supernatant, 80 µL of 0.0625M Potassium Phosphate Buffer (KHPO4; pH 7.2) was added; then, 200 µL of working solution (1.6 mM of 3,3,5,5-tetramethylbenzidine dihydrochloride was dissolved in 5 mL ethanol and 15 mL of 0.25 M sodium acetate buffer pH 5.0). After adding 25 µL of 3% hydrogen peroxide, the plate was incubated for 30 min, and plate absorbance values were read on an ELx808 spectrophotometer at 630 nm. The standard curve was fitted to a second-degree curve: OD = ax2 +bx + c, where x is the amount of P450 equivalent units in the homogenates. Using this formula with the ODs of the samples, we calculated the quantity of “P450 equivalent units” (in nmol) produced by 20 µL of supernatant. This transformation was usually performed automatically by the software supplied with the spectrophotometer. The oxidase activity of each mosquito in nmol P450 equivalent units/mg protein is as follows: (nmol P450 equivalent units for 20 µL supernatant/2 mg protein in 10 µL supernatant).
For GSTs, to each duplicate of 10 µL supernatant we added 200 µL of working solution: (10 mM GSH prepared in 0.1 M phosphate buffer, pH 6.5-, and 3-mM Di chloronitrobenzene dissolve in methanol). For each microtiter plate, 2 blanks with 10 µL of distilled water + 200 µL of working solution was added and the absorbance was measured at 340 nm for 5 min. The GST activity for individual mosquitos was calculated as μmol GSH conjugated/min/mg protein using known extinction coefficients: (Milli DO × 0.21)/(5.76 × 1000)/(amount of protein in mg in 10 µL of supernatant.
For total protein, 10 µL of supernatant was added to 2 wells (technical duplicate) of 96-well ELISA plate. Then, the standards curve of Bovine Serum Albumin (BSA) was generated with Gen5 software to determine the each well concentration. We added 200 µL of working solution (19 mL bicinchoninic Acid Solution + 380 mL Copper (II) Sulfate Solution) as described by the manufacturer. The plate was incubated for 30 min at room temperature, after which the OD was read as an end point at 595 nm.
2.5. Ae. aegypti kdr Genotyping
After grinding each mosquito in 200 μL of 2% CTAB, samples were then incubated at 65 °C for 5 min. Thereafter, 200 μL of chloroform was added and each sample was centrifuged at 12,000 rpm for 5 min at room temperature after mixing by inversion at least 10 times. The supernatant was mixed with 200 μL of isopropanol and centrifuged at 12,000 rpm at room temperature for 10 min. The DNA pellet was washed in 200 μL of 70% ethanol by centrifugation for 5 min at 12,000 rpm. The DNA pellet was dried at room temperature and re-suspended in 140 μL of sterile H2O.
An allele-specific PCR (AS-PCR) was used to detect the presence of S989P, V1016G, and F1534C kdr mutations [12]. Each individual mosquito was tested by AS-PCR twice, the first PCR used a primer specific to the susceptible wild-type and the second PCR used a primer specific to the mutant. The primers used for the genotyping were the following: S989PF:5′AATGATATTAACAAAATTGCGC3′ and S989PR:5′GCACGCCTCTAATATTGATGC; V1016GF:5′GCCACCGTAGTGATAGGAAATC3′ and V1016GVal-R:5′CGGGTTAAGTTTCGTTTAGTAGC3′; and F1534CF:5′GGAGAACTACACGTGGGAGAAC3′and F1534CR:5′CGCCACTGAAATTGAGAATAGC3′.
Each reaction was carried out in a final volume of 25 µL containing 1X Eurogentec Taq buffer (Kaneka Eurogentec, Liège, Belgium), 1.5mM MgCl2, 400 µm of each dNTP 25 pmol forward primer, 25 pmol reverse primer, 25 pmol sensitive or mutant primer, and 1 unit of Eurogentec Taq polymerase (Kaneka Eurogentec, Liège, Belgium). PCR conditions were as follows: 1 cycle at 94 °C for 3 min, then 35 cycles of 94 °C for 30 s, 60 °C (for F1534C and V1016G) or 62 °C (for S989P) for 30 s and 72 °C for 1 min, followed by one cycle at 72 °C for 7 min.
PCR products were separated by electrophoresis in a 2% agarose gel, stained with ethidium bromide. PCR amplicon sizes for the detection of kdr mutations were 240 bp (S989P), 284 bp (F1534C), or 348 bp (V1016G). Non-allele-specific external primers produced bands of 594 bp (S989P), 517 bp (F1534C), or 592 bp (V1016G). No-template controls (NTCs) were run in parallel for all assays as negative controls. Laboratory susceptible specimens (Rockfeller) were used as positive controls.
2.6. Data Analysis
Global Positioning System (GPS) coordinates of the gravid Aedes traps were recorded using the OSM Tracker for Android application. Insecticide susceptibility test results were recorded and analyzed using Microsoft Excel 2016. All biochemical data were saved after reading on a computer connected to the plate reader. Transformations from the various right-hand equations to determine the quantity of the final product were performed automatically by the software (GeneS.1) supplied with the spectrophotometer. Statistical analyses were also performed using GraphPad-Prism 5 software (version 5.00, San Diego, CA, USA). The Mann–Whitney test was chosen for comparison between Rockefeller (susceptible strain), and field mosquitoes. Statistical significance was determined if p < 0.05. Statistical analyses were conducted in Stata/SE 17.0, including Pearson’s Chi-squared test to investigate deviations from Hardy–Weinberg equilibrium.
3. Results
3.1. Mosquito Sampling
A total of 147 gravid Aedes traps were used in the 2 study areas, of which 142 were positive (i.e., female Aedes oviposited in them); yielding an attractiveness rate of 97%. The total number of eggs obtained was 15,844; 8846 eggs in the 10ème arrondissement of Cotonou, and 6998 eggs in Godomey-Togoudo.
Of the 8846 eggs obtained in the 10ème arrondissement of Cotonou, 3154 hatched (35.7%) and 1240 adult Aedes mosquitoes emerged (39.3%). Of the 6998 eggs obtained in Godomey-Togoudo, 4918 eggs hatched (70.3%) and 2486 adult Aedes mosquitoes emerged (50.5%).
Of the 3726 total mosquitoes that emerged, 3723 were Ae. aegypti (>99%), while 3 were Ae. albopictus (<1%). One of the three Ae. albopictus came from the 10ème arrondissement of Cotonou, and the others from Godomey-Togoudo.
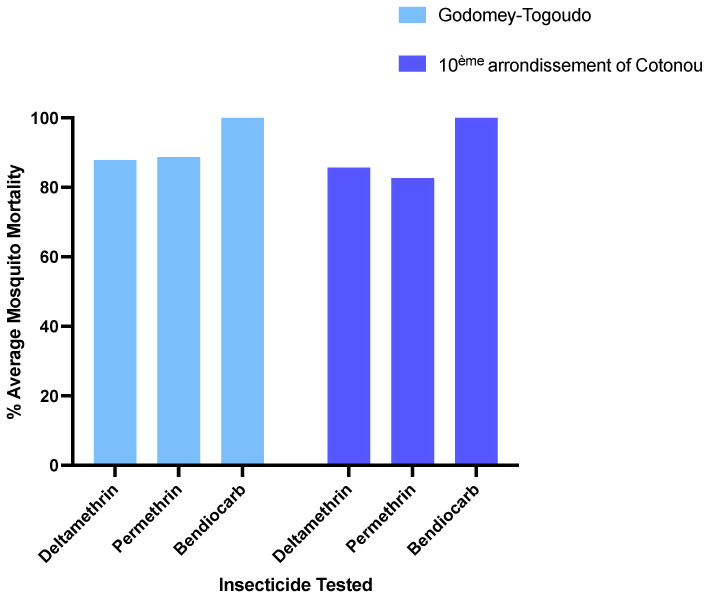
3.2. Insecticide Resistance Profiles
Resistance to permethrin and deltamethrin was evident in both populations of Ae. aegypti. Mosquito mortality was 85.7% and 82.7%, following exposure to the diagnostic dose of deltamethrin or permethrin after 30 min, respectively, in the 10ème arrondissement of Cotonou (Figure 2). Similarly, in Godomey-Togoudo, mortality was 87.9% and 88.8% with deltamethrin and permethrin, respectively. By comparison, complete susceptibility to bendiocarb was observed in both vector populations (100% mortality) (Figure 2).
Figure 2.
Susceptibility of Ae. aegypti to diagnostic doses of three insecticides in Godomey-Togoudo and the 10ème arrondissement of Cotonou.
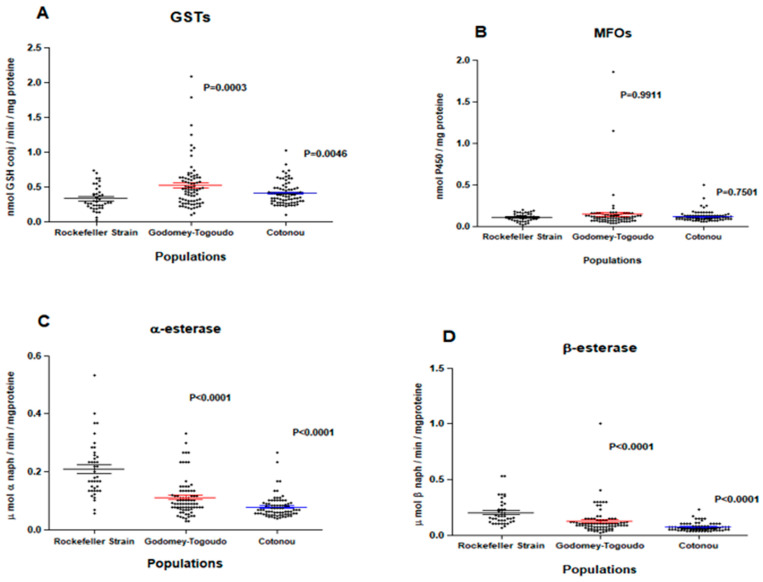
3.3. Expression of Detoxification Enzymes
Field insecticide-resistant Ae. aegypti populations had significantly higher median levels of GSTs compared to the insecticide-susceptible Rockefeller reference strain in Godomey-Togoudo (p = 0.0003) and in the 10ème arrondissement of Cotonou (p = 0.0046) (Figure 3A). By comparison, field Ae. aegypti did not differ in their expression levels of MFOs, compared to the susceptible strain (Figure 3B) and had significantly lower median levels of non-specific esterases (α and β esterases) (Figure 3C,D).
Figure 3.
Expression levels of glutathione-S-transferases (A), mixed-function oxidases (B), α (C) and β (D) esterases among Ae. aegypti Rockefeller strain (insecticide-susceptible) and two insecticide-resistant Ae. aegypti field populations collected from Godomey-Togoudo and in the 10ème arrondissement of Cotonou. Medians for each group are represented by solid-colored lines, accompanied by 95% confidence intervals.
3.4. kdr Mutation Screening
Three kdr mutations (S989P, V1016G, and F1534C) were identified in 82.9% (262/316) of pyrethroid-resistant Ae. aegypti from both study sites (Table 1). Among bioassay survivors, S989P was present in the highest frequencies (0.88 to 0.92). This mutation was under significant selection in both the 10ème arrondissement of Cotonou and Godomey-Togoudo (χ2 = 4.32; p = 0.038; and χ2 = 4.40; p = 0.036; Table 1). F1534C ranged in frequency from 0.69 to 0.70 in Ae. aegypti which survived pyrethroid exposure, with significant deviations from the Hardy–Weinberg equilibrium in both study sites (χ2 = 1.61; p = 0.033 and χ2 = 4.62; p = 0.0024, in the 10ème arrondissement of Cotonou and Godomey-Togoudo, respectively). V1016G ranged in frequency from 0.62 to 0.73, with no evidence for ongoing selection in either site (Table 1). We identified 13 insecticide-resistant Ae. aegypti with the simultaneous presence of all 3 kdr mutations.
Table 1.
kdr mutation (S989P, V1016G, and F1534C) allele frequencies in Benin.
| kdr Mutation | Study Site | # Mosquitoes Tested | Homozygote Mutation (RR) | Heterozygote Mutation (RS) | Homozygote Wild Type (SS) | Allele Frequency | χ2 Test | p-Value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dead | Alive | Dead | Alive | Dead | Alive | R | S | |||||||||
| Dead | Alive | Dead | Alive | Dead | Alive | Dead | Alive | |||||||||
| S989P | 10ème arrondissement of Cotonou | 24 | 0 | 9 | 9 | 3 | 3 | 0 | 0.38 | 0.88 | 0.62 | 0.12 | 4.32 | 0.245 | 0.038 | 0.621 |
| Godomey-Togoudo | 54 | 15 | 21 | 8 | 4 | 6 | 0 | 0.66 | 0.92 | 0.34 | 0.08 | 4.40 | 0.189 | 0.036 | 0.664 | |
| F1534C | 10ème arrondissement of Cotonou | 78 | 33 | 15 | 12 | 9 | 5 | 4 | 0.78 | 0.70 | 0.22 | 0.30 | 4.52 | 1.61 | 0.033 | 0.204 |
| Godomey-Togoudo | 111 | 31 | 23 | 21 | 12 | 17 | 7 | 0.60 | 0.69 | 0.40 | 0.31 | 9.20 | 4.62 | 0.0024 | 0.032 | |
| V1016G | 10ème arrondissement of Cotonou | 33 | 5 | 7 | 5 | 7 | 6 | 3 | 0.47 | 0.62 | 0.53 | 0.38 | 2.22 | 0.279 | 0.136 | 0.597 |
| Godomey-Togoudo | 16 | 1 | 8 | 1 | 3 | 1 | 2 | 0.50 | 0.73 | 0.50 | 0.27 | 0.333 | 2.22 | 0.564 | 0.136 | |
#: number.
4. Discussion
To deploy appropriate control strategies targeting arbovirus vectors, it is crucial to understand the distribution of key mosquito species, their bionomics and insecticide resistance profiles. Study findings report Ae. aegypti in the 10ème arrondissement of Cotonou and Godomey-Togoudo during the dry season, which might be explained by climate change, transport development, and increasing urbanization. Both populations of Ae. aegypti were characterized by pyrethroid resistance (to deltamethrin and permethrin), but complete susceptibility to bendiocarb. Pyrethroid resistance in these populations is not expected, given that insecticide treatment specifically targeting Ae. aegypti in Benin is rare; rather, it may have been driven by several alternate factors. It is possible that insecticidal interventions used to control other vector species, e.g., LLINs, IRS, or household mosquito repellents targeting Anopheles vectors of malaria, may have exerted indirect selection pressure on Ae. aegypti for the evolution of pyrethroid resistance. Furthermore, water contamination caused by pesticides used for agricultural practices may have also played a role in the development of resistance.
Regarding insecticide resistance mechanisms, Ae. aegypti populations were characterized by over-expression of GSTs and a slight, but non-significant, increase in the activity of MFOs. It is likely that over-expression of both types of metabolic enzymes could confer pyrethroid resistance in these populations. Further investigation is warranted of molecular mechanisms involving point mutations in the GSTe2 gene, which may be contributing to pyrethroid resistance in Ae. aegypti in Benin. By comparison, under expression of non-specific esterases (α and β esterases) observed in these same populations may explain the strong sensitivity to bendiocarb; therefore, this insecticide has the potential to be used in both areas to suppress Ae. aegypti population densities.
Several mutations at nine different loci in Ae. aegypti have been identified, which are implicated in reduced insecticide susceptibility. Of these, F1534C, S989P, and V1016I are widely reported kdr mutations and have been associated with DDT and pyrethroid resistance [13,14,15,16]. In this study, AS-PCR genotyping revealed the presence of S989P, F1534C, and V1016G mutations in both populations of Ae. aegypti in Benin; 82.9% of genotyped mosquitoes carried at least one mutation. The frequencies of S989P in both study sites (63% and 78%) were much higher compared to that observed in Nigeria (7%) [16]. Paradoxically the high mutation frequencies identified in this study were accompanied by only a moderate amount of phenotypic pyrethroid resistance. It is possible that the high fitness cost associated with these mutations may be adversely impacting mosquito survival [21].
To our knowledge, this is the first report of V1016G in Africa, and this is the first time all three kdr mutations have been detected in Ae. aegypti in Benin. This presence of the V1016G gene mutation in West Africa represents a further expansion of the geographic range of this mutation and is an important finding. However, it would be necessary to confirm this mutation in positive samples using Sanger sequencing; this is a limitation of this study.
We identified 13 insecticide-resistant Ae. aegypti with the simultaneous presence of all three kdr mutations. The co-occurrence of two or three kdr mutations has been previously reported in China, Nigeria and Malaysia, which resulted in highly intense pyrethroid resistance [12,16,22,23]. Other kdr mutations, T1520I and F1534L, have also been found in Ae. aegypti; however, the S989P/V1016G/F1534C mutation is the most widespread, followed by S989P/V1016V and V1016G/F1534C. A quadruple mutation, S989P/V1016G/T1520I/F1534C, was also identified in 2022 in Myanmar in Ae. aegypti [24]. High prevalence of the F1534C mutation has been reported previously, but intense phenotypic resistance to pyrethroids is only found when accompanied by the V1016I mutation or V1016G, S989P, and/or V410L mutations [24,25]. Recent work has also highlighted specific profiles of metabolic gene overexpression associated with resistance to pyrethroids and organophosphates in Ae. aegypti popula-tions from two localities in Puerto Rico [26]. In this study, the detection of multiple kdr mutations and overexpressed detoxification enzymes in the major dengue virus vector Ae. aegypti is concerning and cautions against the use of pyrethroids in arbovirus control programs in Benin. In this part of West Africa, additional surveillance activities are needed to further investigate other co-occurring molecular and metabolic insecticide resistance mechanisms, as well as to assess the susceptibility of these Ae. aegypti populations to alternate pyrethroids (e.g., alpha-cypermethrin, cyfluthrin, or lambda-cyhalothrin), with or without synergists (e.g., piperonyl butoxide), or other classes of insecticides (e.g., organophosphates, neonicotinoids, pyrroles etc.) to identify efficacious insecticidal control measures. In addition to these vector control tools, information education communication and behavior change communication (IEC/BCC) initiatives are needed to encourage local community members to properly dispose of stagnant water sources, which act as potential Aedes breeding sites, and to promote the use personal protective measures (including the use of topical repellents and wearing of long clothing) to prevent mosquito bites. In the event of a dengue fever epidemic, the Ministry of Health in Benin is cautioned against relying exclusively on pyrethroids for vector control; combination and/or rotation of insecticides with different active ingredients may be required to suppress populations of pyrethroid-resistant Ae. aegypti.
5. Conclusions
This study reports resistance to deltamethrin and permethrin in Ae. aegypti populations, collected from the 10ème arrondissement of Cotonou and Godomey-Togoudo in Abomey-Calavi. Molecular and metabolic mechanisms associated with pyrethroid resistance included the kdr mutations F1534C, S989P, and V1016G, and significant over-expression of certain detoxification enzymes. To our knowledge, this is the first report of V1016G in Africa, and this is the first time all three kdr mutations have been detected in Ae. aegypti in Benin, suggesting alternative vector tools may be required for arbovirus control in this part of West Africa. Study results highlight the importance of strengthening and scaling-up surveillance activities to respond to the control of vector-borne diseases.
Acknowledgments
The findings and conclusions in this manuscript are those of the author(s). We acknowledge the support received from the Manager of the Entomological Research Center of Cotonou (MC Germain Gil Padonou) and his staff in the field and laboratory. We also thank Come Zinsou Koukpo, Arsene Fassinou, Ahouandjinou Juvenal and Agassounon Brunelle for your support.
Author Contributions
Conceptualization: T.F.T., R.O. and M.A.; data collection, T.F.T., R.O., S.D.Z., G.A., G.I. and H.F.; formal analysis, T.F.T., R.O., S.D.Z., G.A., A.S. and L.A.M.; mobilization of funding, T.F.T., G.A., S.D.Z., H.F., G.I. and R.O.; methodology, T.F.T., R.O., M.A., L.A.M. and M.A.; project administration, T.F.T. and R.O.; original draft preparation formal, T.F.T., R.O., L.A.M. and M.A., supervision, T.F.T., R.O. and M.A. All authors have read and agreed to the published version of the manuscript.
Mosquito collections did not directly involve humans, but their living environments and permissions were requested and obtained prior to the placement of the mosquito traps. All individuals included in this section have consented to the acknowledgement.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest regarding the publication of this paper.
Funding Statement
This work was partly funded by Researchers in the Entomological Research Center of Cotonou.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Dengue et Dengue Sévère. [(accessed on 20 January 2022)]. Available online: https://www.who.int/fr/news-room/fact-sheets/detail/dengue-and-severe-dengue.
- 2.Padonou G.G., Ossè R., Salako A.S., Aikpon R., Sovi A., Kpanou C., Sgbaohan HAkadiri Y., Lamine B., Akogbeto C.M. Entomological assessment of the risk of dengue outbreak in Abomey-Calavi Commune, Benin. Trop. Med. Health. 2020;48:20. doi: 10.1186/s41182-020-00207-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Esu E., Lenhart A., Smith L., Horstick O. Effectiveness of peridomestic space spraying with insecticide on dengue transmission; systematic review. Trop. Med. Int. Health. 2010;15:619–631. doi: 10.1111/j.1365-3156.2010.02489.x. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization . Test Procedures for Insecticide Resistance Monitoring in Malaria Vector Mosquitoes. 2nd ed. World Health Organization; Geneva, Switzerland: 2018. [Google Scholar]
- 5.Liu N. Résistance aux insecticides chez les moustiques: Impact, mécanismes et directions de recherche. Ann. Rev. Entomol. 2015;60:537–559. doi: 10.1146/annurev-ento-010814-020828. [DOI] [PubMed] [Google Scholar]
- 6.Brogdon W.G., McAllister J.C. Résistance aux insecticides et lutte antivectorielle. Urgence Infect. Dis. 1998;4:605–613. doi: 10.3201/eid0404.980410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hemingway J., Ranson H. Insecticide resistance in insect vectors of human disease. Annu. Rev. Entomol. 2000;45:371–391. doi: 10.1146/annurev.ento.45.1.371. [DOI] [PubMed] [Google Scholar]
- 8.Flores A.E., Albeldaño-Vázquez W., Salas I.F., Badii M.H., Becerra H.L., Garcia G.P., Fuentes S.L., Brogdon W.G., Black Iv W.C., Beaty B. Elevated α-esterase levels associated with permethrin tolerance in Aedes aegypti (L.) from Baja California, México. Pestic. Biochem. Phys. 2005;82:66–78. doi: 10.1016/j.pestbp.2004.12.007. [DOI] [Google Scholar]
- 9.Bisset J.A., Marin R., Rodriguez M.M., Severson D.W., Ricardo Y., French L., Díaz M., Perez O. Insecticide resistance in two Aedes aegypti (Diptera: Culicidae) strains from Costa Rica. J. Med. Entomol. 2013;50:352–361. doi: 10.1603/ME12064. [DOI] [PubMed] [Google Scholar]
- 10.Hernandez J.R., Longnecker M., Fredregill C.L., Debboun M., Pietrantonio P.V. Kdr genotyping (V1016I, F1534C) of the Nav channel of Aedes aegypti (L.) mosquito populations in Harris County (Houston), Texas, USA, after Permanone 31–66 field tests and its influence on probability of survival. PLoS Negl. Trop. Dis. 2021;15:e0009833. doi: 10.1371/journal.pntd.0009833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moyes C.L., Vontas J., Martins A.J., Ng L.C., Koou S.Y., Dusfour I., Raghavendra K., Pinto J., Corbel V., David J.P., et al. Contemporary status of insecticide resistance in the major Aedes vectors of arboviruses infecting humans. PLoS Negl. Trop. Dis. 2017;11:e0005625. doi: 10.1371/journal.pntd.0005625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li C.X., Kaufman P.E., Xue R.D., Zhao M.H., Wang G., Yan T., Guo X.X., Zhang Y.M., Dong Y.D., Xing D., et al. Relationship between insecticide resistance and kdr mutations in the dengue vector Aedes aegypti in Southern China. Parasites Vectors. 2015;8:325. doi: 10.1186/s13071-015-0933-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kawada H., Oo S.Z.M., Thaung S.K.E., Maung Y.N.M., Thu H.M., Thant K.Z., Minakawa N. Co-occurrence of point mutations in the voltage-gated sodium channel of pyrethroid-resistant Aedes aegypti populations in Myanmar. PLoS Negl. Trop. Dis. 2014;8:e3032. doi: 10.1371/journal.pntd.0003032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kawada H., Higa Y., Futami K., Muranami Y., Kawashima E., Osei J.H., Sakyi K.Y., Dadzie S., de Souza D.K., Appawu M. Discovery of point mutations in the voltag egated sodium channel from African Aedes aegypti populations: Potential phylogenetic reasons for gene introgression. PLoS Negl. Trop. Dis. 2016;10:e0004780. doi: 10.1371/journal.pntd.0004780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sombié A., Saiki E., Yaméogo F., Sakurai T., Shirozu T., Fukumoto S., Sanon A., Weetman D., McCall P., Kanuka H., et al. Fréquences élevées des mutations F1534C et V1016I kdr et association avec la résistance aux pyréthroïdes chez Aedes aegypti de Somgandé (Ouagadougou), Burkina Faso. Trop. Med. Santé. 2019;47:2. doi: 10.1186/s41182-018-0134-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agbohun I.K., Idowu E.T., Oyeniyi T.A., Adeogun A.O., Adesalu K., Nwanya O., Okonkwo F., Oladosu Y., Otubanjo O. First Detection and Co-occurrence of kdr (F1534C and S989P) Mutations in Multiple Insecticides Resistant Aedes aegypti in Nigeria. Preprints. 2021:2021070302. doi: 10.20944/preprints202107.0302.v1. [DOI] [PubMed] [Google Scholar]
- 17.Ayres C.F.J., Seixas G., Borrego S., Marques C., Monteiro I., Marques C.S., Gouveia B., Leal S., Troco A.D., Fortes F., et al. The V410L knockdown resistance mutation occurs in island and continental populations of Aedes aegypti in West and Central Africa. PLoS Negl. Trop. Dis. 2020;14:e0008216. doi: 10.1371/journal.pntd.0008216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fontenille D., Traore-Lamizana M., Diallo M., Thonnon J., Digoutte J.P., Zeller H.G. New vectors of Rift Valley fever in West Africa. Emerg. Infect. Dis. 1998;4:289–293. doi: 10.3201/eid0402.980218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guideline for Evaluating Insecticide Resistance in Vectors Using the CDC Bottle Bioassay. [(accessed on 20 January 2022)]; Available online: https://stacks.cdc.gov/view/cdc/21777/cdc_21777_DS1.pdf.
- 20.Hemingway J. Insecticide Resistance Mechanisms (Field and Laboratory Manual) World Health Organization; Geneva, Switzerland: 1998. pp. 1–39. [Google Scholar]
- 21.Rigby L.M., Rašić G., Peatey C.L., Hugo L.E., Beebe N.W., Devine G.J. Identifying the fitness costs of a pyrethroid-resistant genotype in the major arboviral vector Aedes Aegypti. Parasites Vectors. 2020;13:358. doi: 10.1186/s13071-020-04238-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zuharah W.F., Sufian M. The discovery of a novel knockdown resistance (kdr) mutation A1007G on Aedes aegypti (Diptera: Culicidae) from Malaysia. Sci. Rep. 2021;11:5180. doi: 10.1038/s41598-021-84669-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.AhbiRami R., Ishak I.H., Yahya Z.S., Zuharah W.F. Knockdown resistance (kdr) in dengue vectors, Aedes aegypti and Aedes albopictus from Malaysia: A post-flood risk assessment. Gen. Mol. Biol. 2020;19:gmr18604 [Google Scholar]
- 24.Naw H., Võ T.C., Lê H.G., Kang J.-M., Mya Y.Y., Myint M.K., Kim T.-S., Shin H.-J., Na B.-K. Knockdown Resistance Mutations in the Voltage-Gated Sodium Channel of Aedes aegypti (Diptera: Culicidae) in Myanmar. Insects. 2022;13:322. doi: 10.3390/insects13040322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fan Y., Scott J.G. The F1534C voltage-sensitive sodium channel mutation confers 7- to 16-fold resistance to pyrethroid insecticides in Aedes aegypti. Pest Manag. Sci. 2020;76:2251–2259. doi: 10.1002/ps.5763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Derilus D., Impoinvil L.M., Muturi E.J., McAllister J., Kenney J., Massey S.E., Hemme R., Kothera L., Lenhart A. Comparative Transcriptomic Analysis of Insecticide-Resistant Aedes aegypti from Puerto Rico Reveals Insecticide-Specific Patterns of Gene Expression. Genes. 2023;14:1626. doi: 10.3390/genes14081626. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are contained within the article.