Abstract
Acute stroke care begins before hospital arrival, and several prehospital factors are critical in influencing overall patient care and poststroke outcomes. This topical review provides an overview of the state of the science on prehospital components of stroke systems of care and how emergency medical services systems may interact in the system to support acute stroke care. Topics include layperson recognition of stroke, prehospital transport strategies, networked stroke care, systems for data integration and real-time feedback, and inequities that exist within and among systems.
Keywords: delivery of healthcare, emergency medical services, stroke, stroke center
Care for the acute stroke patient begins in the prehospital setting. Recognition of stroke symptoms, activation of emergency medical services (EMS), EMS practitioner stroke identification, and subsequent decision-making by EMS are critical. Well-functioning prehospital stroke care is integral to the overall stroke system of care.
This article is the first in a 2-part topical review series on the current state of prehospital stroke care. We provide an overview of the prehospital components of the stroke system of care primarily through the lens of the United States system, which is in many ways more fragmented than in places with centralized systems of planning. Nevertheless, the key principles are largely universal in the priority to design or improve systems of care with an aim of getting the right patient to the right location at the right time. The second, companion review includes more detailed discussions of on-scene prehospital evaluation and management of the patient with suspected stroke.
SYMPTOM RECOGNITION AND ACCESSING EMERGENCY MEDICAL CARE
Layperson Stroke Recognition
Recognition of stroke symptoms is a critical first step in the stroke chain of survival (Figure). Delays in recognition lead to delays in care seeking and contribute to reduced treatment efficacy1 and ineligibility.2–4 Early symptom recognition along with EMS activation contribute to reduced prehospital delays, and more timely, higher-quality care.1,5–7
Figure. Stroke chain of survival within a systems of care framework.
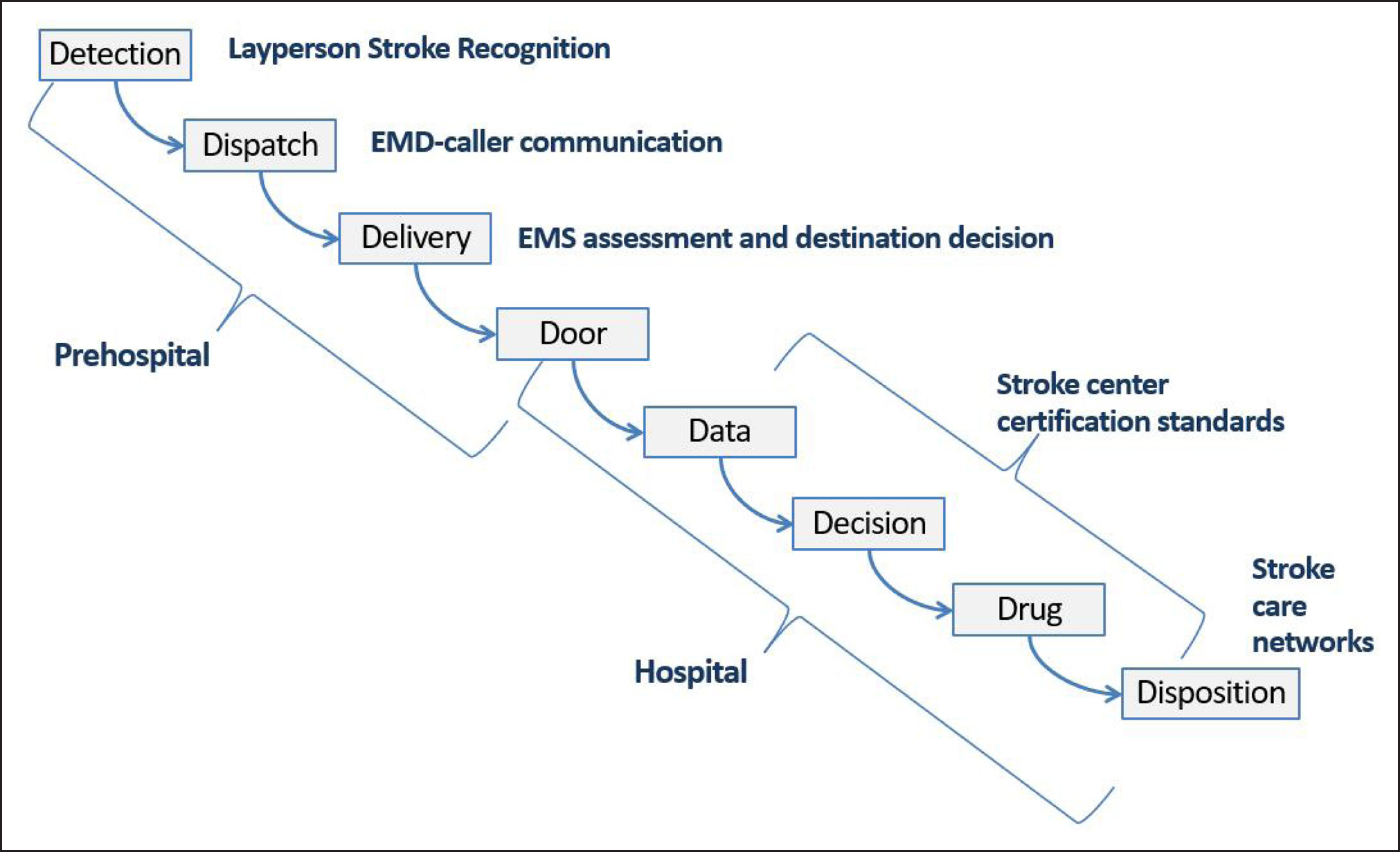
EMD indicates emergency medical dispatcher; and EMS, emergency medical services.
However, the utilization of EMS by patients with stroke in the United States is suboptimal. Between 36% and 42% of stroke patients do not arrive by EMS,6,8,9 and utilization is decreasing over time.9 Use of EMS by stroke patients also varies by subpopulation, with lower use among persons of color, younger patients, and men.6,8,9
To address this, stroke awareness campaigns such as BE FAST and FAST have worked to improve symptom recognition while emphasizing rapid EMS response, including the multilingual equity-oriented approach of the Massachusetts Department of Public Health.10 Other innovative strategies include school-based programs such as Hip-Hop Stroke.11
Yet there is evidence that the decision to make an emergency call (ie, 9-1-1 in the United States) is complex, and stroke knowledge alone is insufficient.4,12,13 For example, fear induced by stroke symptoms may impact decision-making,14 as can patients’ perception of the seriousness of stroke symptoms.6,9,15–17 Systemic factors experienced by marginalized populations such as poverty, racism, and adverse social determinants of health likely present additional barriers.18 A study of Black populations indicated that distrust of the medical community and concern that EMS would not come to their stigmatized neighborhood impacted the decision.14 Concern about the cost of ambulance transport is another barrier, which likely disproportionably impacts populations experiencing poverty.14,16,19
Many public awareness campaigns strive to capitalize on the key role of bystanders in symptom recognition and the decision to call 9-1-1.16 Youth bystanders in particular have described motivation to call 9-1-1 due to perceived responsibility for the person’s wellbeing.14 Future work to address systemic barriers will be important to increase EMS utilization by patients with stroke, and studies leveraging qualitative or community-based participatory research methodologies may be particularly valuable.4,14,20
Accessing Emergency Medical Care During the 9-1-1 Call
The next key link in the stroke chain of survival occurs at the first point of contact between laypersons and medical personnel during an emergency call.21 A call-taker/emergency medical dispatcher has a compressed time frame to gather critical logistical information (ie, address of the emergency), elucidate the type of emergency, and dispatch the appropriate responding unit.22 The American Heart Association recommends this occur within 1 minute.23,24
Accurate emergency medical dispatcher recognition can have critical downstream effects for acute stroke patients. It has been associated with quicker on-scene times by responding paramedics, greater likelihood of transport to a stroke center, higher rate of and faster thrombolysis administration at the receiving emergency department.6,25–29
Yet the sensitivity of emergency medical dispatcher recognition is low, ranging from 41% to 83%, with most studies reporting a sensitivity of approximately 50%, particularly when emergency medical dispatchers do not have structured protocols to assist with stroke recognition.29–40 The cause of this low sensitivity is likely multi-factorial, but an important potential causative factor is the language used by layperson callers to describe stroke. Laypersons often use inconsistent language when describing acute stroke, sometimes even using words that connote acute, time-sensitive conditions other than stroke.40 The combination of distracting terms and the ultra-compressed time frame of the 9-1-1 call contribute to increased uncertainty for the emergency medical dispatcher and downstream delays in stroke recognition.
Future research and implementation of initiatives to support emergency medical dispatchers in accurate stroke recognition have been proposed as a target for stroke systems of care optimization and may be used as a model for identifying other time-sensitive conditions during the 9-1-1 call.40–45 Although such interventions would be expected to improve all EMS systems, those with mobile stroke units may be particularly positively impacted by high-fidelity stroke dispatch, enabling the treatment of more patients with true strokes and ultimately increasing mobile stroke units cost-effectiveness.45–47
STRUCTURAL COMPONENTS IN PREHOSPITAL STROKE SYSTEMS OF CARE
Stroke Center Certification
Stroke center certification is critical to standardizing the recognition of hospital capabilities within stroke systems of care. Third-party certification information, with uniform standards, may be incorporated into prehospital protocols to ensure appropriate, rapid transport for patients with suspected stroke. This ensures patients are treated at a hospital with the ability to provide indicated therapies such as thrombolysis, endovascular thrombectomy (EVT), clipping of intracranial aneurysms, or other acute interventions for hemorrhagic stroke. This also enables the design of strong stroke systems of care for a specific geographic region. Certification of stroke centers by independent organizations is an American Heart Association Level 1B recommendation.1 Agencies providing stroke center certification include Joint Commission, Det Norske Veritas, Healthcare Facilities Accreditation Program, Center for Improvement in Healthcare Quality, and state-based certifiers.48–50
There are 4 established levels of certification: Acute Stroke Ready Hospital, Primary, Thrombectomy-Capable, and Comprehensive Stroke Centers.48,49,51–53 Each has unique components to fulfill particular diagnostic and treatment needs within the system.49,51–53 Acute Stroke Ready Hospitals are often located in rural settings and function primarily to assess and stabilize patients (including the administration of intravenous thrombolytics) prior to transfer to a higher level of care according to patient needs.49,51,52
There is some evidence suggesting that even among primary stroke centers, quality of care varies between sites and by certifying organization.50 Further differences exist between certified stroke centers and nonstroke centers; hospitals certified as stroke centers tend to be located in higher income service areas, have higher profit margins, and are less likely to be located in rural areas, demonstrating the impact of economic characteristics of patient populations on certification.54,55 Finally, globally, stroke center certification is more established in high-income countries and regions compared with low- and middle-income countries.56,57
Integration of Prehospital and Hospital Data
Timely feedback is a vital part of continuously improving diagnostic skills and treatment decisions; yet this is uncommonly and inconsistently delivered to frontline EMS practitioners.58 Lack of feedback may lead to miscalibration with EMS practitioners over- or under-estimating the accuracy of their decisions. Up to one-in-three strokes diagnosed in the emergency department were unrecognized prehospital.59,60 Differences between prehospital and hospital diagnoses are understandably common but can lead to further diagnostic errors.61 Prehospital recognition is a necessary first step before prenotification of the receiving emergency department. Error may lead to delays in door-to-imaging or treatment times, and translate to worse patient outcomes.25 Analyses suggest that few EMS encounters are fully concordant with guideline recommendations.62
Hospital-directed feedback increases prehospital compliance with guideline-concordant care, including documentation of a prehospital stroke assessment and last known well time.63 Unfortunately, such processes are uncommon and tend to be resource intensive. Yet health information technology and automated linkage of EMS and hospital data may provide an opportunity for more large-scale improvement efforts related to stroke systems of care.64 Although the practice is not yet a widespread standard, routine linkage of EMS data with hospital data is increasing. Several methods for prehospital and hospital data linkage exist, including health information exchanges, specialized registries, and system interface software from electronic patient care record vendors.65–67 Currently, many data linkage efforts are performed retrospectively and are research-focused, rather than a source of real-time feedback for EMS practitioners. Establishing real-time, bidirectional data exchange could serve as a key strategy to provide EMS practitioners with the feedback they desire, improve patient care, and even help mitigate the effects of work-related burnout.68,69 Local projects have demonstrated the feasibility and benefits of automated real-time bidirectional exchange, allowing front-line EMS practitioners direct access to outcome data.70,71 This may also be of value for the emergency department and in-hospital care of the patient with stroke by ensuring timely access to key information collected by EMS.72,73 Certified hospitals should lead in this work.
Yet data linkage alone will not generate action and improvement. Prehospital and hospital feedback systems should systematically combine linked data with input from clinical and administrative leaders on both sides of the feedback loop to interpret findings and identify points for system-wide improvement.64 This multi-dimensional approach for health information technology-supported feedback systems involving data linkage technology and a culture of information sharing supports the development and evolution of collaborative, integrated approaches to stroke systems of care.
PATIENT MOVEMENT WITHIN A STROKE SYSTEM OF CARE
Transport Destination
A critical goal in the configuration of stroke systems of care is in enabling rapid reperfusion therapies for eligible patients.4,74 Since 2015, with overwhelming evidence of the benefit of EVT for large vessel occlusion stroke, the organization of EMS transport protocols has become more complex. Prehospital routing decisions must now consider whether to bypass closer facilities with thrombolysis capabilities for EVT-capable centers.75
Several observational studies and meta-analyses including EVT-treated patients suggested that direct transport to a thrombectomy-capable center was associated with better functional outcomes, likely due to reducing transfer-related delays in EVT.76–78 To date, the only randomized clinical trial comparing transportation to a Thrombectomy-Capable Centers/Comprehensive Stroke Centers versus the closest local stroke center was the RACECAT trial (Transfer to the Closest Local Stroke Center vs Direct Transfer to Endovascular Stroke Center of Acute Stroke Patients With Suspected Large Vessel Occlusion in the Catalan Territory), performed in Catalonia, Spain. Patients with a prehospital Rapid Arterial oCclusion Evaluation (RACE) scale of 5 or greater had no significant difference in 3-month neurological outcomes between the 2 transport paradigms.79 However, external validity of this study may be limited, as the study region has a highly coordinated and effective stroke care network. Sixty percent of AIS patients received thrombolysis at the local center, and flow was very efficient. Times were extremely fast in both paradigms, even in transferred patients (median door-to-needle time 33 minutes, door-in door-out time 78 minutes, and a difference of only 56 minutes in total time from onset-to-EVT between the 2 groups).
High-quality randomized clinical trial data from other stroke systems with geographical and logistical differences are lacking.80 In fact, observational data from other regions with directed transport protocols but different efficiencies than Catalonia are less clear, with some suggesting improved outcomes for direct-transport patients.81–85 Mathematical modeling suggests that the preferred destination is more complex and may be dependent on system-specific factors, such as differences in transport time and when receiving emergency departments are less efficient.86,87 It is likely that optimal prehospital routing decisions are highly dependent on particular characteristics of individual patients, EMS agencies, and receiving hospital efficiencies. Recent recommendations have acknowledged such nuance in routing recommendations.88
Lastly, with the notable exception of RACECAT, prior studies have largely included only patients with confirmed large vessel occlusion who were EVT-eligible on arrival at the EVT-capable center. In the vast majority of prehospital systems (ie, those without mobile stroke units), accurately distinguishing true stroke from mimic is limited, let alone identifying large vessel occlusion. Ideally, screening tools would identify thrombectomy candidates and discriminate between patients who may benefit from transport to Comprehensive Stroke Centers despite longer times versus those who may experience a dilution of treatment benefit, lose the opportunity for thrombolysis (eg, patients without large vessel occlusion), or even potentially introduce harm (eg, certain hemorrhagic stroke patients). However, the positive predictive value of available prehospital stroke severity screening for large vessel occlusion is, at best, 50%.89 Further, prehospital stroke severity screens have limited ability to discriminate between types of severe stroke (ie, large vessel occlusion or hemorrhagic stroke); more data are required to inform optimal screening and transport. Ultimately, prehospital evaluation tools that allow for more precise, even personalized, decision-making may be needed.90 Additionally, technology-based solutions incorporating artificial intelligence or complex algorithms may improve the reliability of appropriate prehospital transport.80
Network Approach to Prehospital Stroke Systems of Care
The structural configuration of the healthcare system underlies the nature and configuration of stroke systems of care.4,91 This includes how patients are transported to emergency departments and between hospitals, where hospitals and resources are located, how health systems interact with their surrounding communities, and the existence of policies that reinforce or ameliorate legacies of segregation and inequitable access.92 The stroke system of care is thus interconnected and interdependent, and requires tools that enable sophisticated analyses of systems with many interacting components.93 Approaches from network science provide a valuable set of tools for studying and improving the prehospital stroke system.94 Such analyses are useful for describing structural relationships in organizational networks95 and may uncover prehospital transport patterns and network structure that underlies connections between EMS, prehospital systems, emergency departments, and hospitals to which patients are transported. For example, network methods have been used to study the influence of hospital characteristics on interhospital transfer destinations when patients with stroke are transferred between hospitals, demonstrating the influence of hospital affiliation on destination choice, even to a greater extent than hospital stroke center certification or reputation.96 Similar analyses in the prehospital setting may inform prehospital transport policy. For example, in the United States, some EMS systems and many mobile stroke units are operated by hospital systems, which raises the potential concern for preferential transport of patients to destinations within that hospital system. Network approaches may be valuable to study these patterns and examine the extent to which preferential transport benefits patients versus hospital systems.
STROKE IN LIMITED RESOURCED SETTING
Prehospital systems of care for stroke in resource-limited settings, such as in rural communities, face additional sets of challenges in providing timely, high-quality care. In general, access to acute stroke care has increased substantially over time, though over one-third of the US population remains over 60 minutes from a Thrombectomy-Capable or Comprehensive Stroke Centers by ground transport.1 Rural patients are also less likely to call 9-1-1 and be transported by EMS.6 Even with prompt activation, EMS response times for rural patients often exceed the <8-minute goal set by the American Heart Association.1,97,98 Transport times may also be extended, and median transport times are significantly longer in frontier areas.97
The feasibility of EMS transport to a stroke center also varies in rural areas, and the existence of direct-transport protocols is variable.99,100 Current recommendations are that rural EMS consider the transport of patients with suspected stroke, particularly those with suspected large vessel occlusion, to the closest facility capable of administering thrombolysis if the transport time to a Thrombectomy-Capable or Comprehensive Stroke Centers would exceed a reasonable threshold (eg, 60 minutes).88 In rural and limited-resourced areas, transport times by ground may greatly exceed that threshold, requiring eventual inter-facility transfer after initial local assessment and treatment. Recently, there has been a paradigm shift in bringing care to the patient rather than the patient to care. For example, some rural areas, especially outside the United States, have established mobile stroke units to increase access to thrombolysis,101–103 transported endovascular specialists to outlying hospitals,104,105 or developed methods for telestroke consultations during EMS transport.106
Aeromedical transport is another alternative in rural settings to provide rapid transport to higher-level care from the scene. About 90% of EMS personnel reported access to at least 1 helicopter EMS service and 86% had the authority to request a helicopter EMS scene response,107 though stroke is an infrequent use.108 Advantages of air transport for stroke are unclear, and the cost effectiveness of using helicopter EMS resources depends on travel distance and time since last seen well.109,110 Overtriage and transport of stroke mimics is also common,111,112 leading to “low value” helicopter EMS activations. When accounting for response time, a helicopter may not save time if ground transport can commence quickly.113,114 Finally, clinical outcomes may not differ substantially among patients transported by air compared with ground.110 The best use of helicopter EMS resources for acute stroke in resource-limited settings remains unclear.
Workforce capabilities and call volumes may also affect acute stroke care in resource-limited settings. Rural areas more commonly rely on volunteer EMS personnel and are less likely to have advanced life support care available.115,116 The ongoing challenges with EMS workforce shortages and stability in the United States are even more pronounced in rural areas.117–119 Thus, particular consideration is needed regarding constraints of the local EMS system and workforce, and its implications for staffing of ambulances and availability to respond to community needs.
INEQUITIES IN PREHOSPITAL STROKE CARE
In 2022, the NINDS Brain Attack Coalition convened to explore inequities and potential solutions across the stroke care continuum.106 Priority areas were developed through subject matter expertise and a critical assessment of the literature. Experts across the country were invited to identify solutions along 4 domains: (1) geography, (2) policies and regulations, (3) economics and healthcare resources, and (4) demographics (race, ethnicity, and gender). The following is a brief overview of ideas generated from the discussions with a focus on the prehospital setting.
Geography
Geographic disparities in access to high-quality prehospital stroke care are linked to differences in access to stroke centers, which may adversely affect patient outcomes.120 Rural–urban differences in prehospital stroke care have been linked to the limited frequency at which strokes are seen by rural EMS providers, long drive times, and inconsistent wireless connectivity.51,74,108,111 Disparities in stroke mortality are heightened in rural areas, US territories, and across Native peoples’ reservations, as access to nearby hospitals with stroke expertise is limited.51,74,109,110 Successful and efficient prehospital stroke management may benefit from more research on the impact of regionalized stroke center networks, standardization of screening tools, routing protocols, and the use of telestroke to facilitate ambulance-based assessments.88 Incorporating these factors in a geographically mindful way may facilitate collaboration and decrease geographic disparities.
Policies and Regulations
The regulation of EMS in the United States occurs largely at state and local levels. Federal entities, such as the National Highway and Transportation Safety Administration, the Federal Interagency Committee on EMS, and the National EMS Advisory Council, also provide guidance and coordination among regional EMS entities.23,88 As a result of this tiered system of regulation, coordination of policies is variable, even within states. Fragmentation of policies may result in differential access to high-quality EMS care for patients.1,51 Thus, a better understanding of how standardization of polices and regulations that support reducing disparities in prehospital stroke care is warranted. Areas to explore may include policies related to EMS reimbursement based on the complexity of assessment and destination decision-making for strokes; culturally-informed EMS stroke education and training; and systematic EMS data collection linked to patient outcomes that support the creation of meaningful metrics to promote equity in stroke care quality improvement.1,51
Economics and Healthcare Resources
Prehospital care systems are often interdependent with hospital systems, and both may reflect the underlying economic basis associated with the communities that they serve.65,66 Variability in the economic base of communities may also be associated with disparities in stroke care and outcomes.112 Low-resourced and historically marginalized communities may have different barriers to activating EMS and reduced access to trained healthcare professionals specialized in stroke care.51 Improved understanding of underlying economic drivers of healthcare resource allocation, EMS reimbursement, and work-force solutions that target professionals that commit to treating patients in underserved areas may impact disparities across the continuum.
Demographics
Sociodemographic differences in utilization of EMS transport among hospitalized stroke patients have been consistently documented.8 Multiple community and prehospital-related factors may contribute to the downstream demographic disparities in stroke treatment rates related to sex/gender, race, ethnicity, socioeconomic status, and insurance status.51,113–115 These sociodemographic disparities contribute to inequitable access to emergency care, which in turn results in disparities in access to efficient stroke diagnosis and treatment for members of disenfranchised communities, even in geographic areas with adequate stroke resources. Priority areas that may reduce sociodemographic disparities in the prehospital stroke setting include (1) the development of a high-quality, systematic, and comprehensive national data set that may be used at the community level to provide information for targeted interventions and (2) an expansion of programs to enhance public education about stroke identification and acute management, especially for populations and/or regions where disparities exist.
SUMMARY AND CONCLUSIONS
Optimal prehospital care of stroke patients is imperative for downstream high-quality care in the emergency department and in-hospital, ultimately resulting in improved patient outcomes. Ongoing investment is needed in processes to improve symptom recognition and communication, develop additional evidence to inform routing destination decisions, processes for data integration for enabling feedback as a component of continual quality improvement and strategies for ensuring equitable access to high-quality acute stroke care for all patients.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Disclosures
Dr. Zachrison reports grants from Agency for Healthcare Research and Quality, National Institute of Neurological Disorders and Stroke, CRICO, the American College of Emergency Physicians and the MGH Executive Committee on Research, employment by Partners Healthcare and Boston Bruins, and compensation from Wolters Kluwer Health, Inc, for other services. Dr. Madsen reports grants from NIH Clinical Center. Dr. Crowe reports employment by ESO. Dr. Jauch reports compensation from Medical Malpractice for expert witness services and compensation from Genentech for consultant services. Dr. Adeoye reports compensation from NICO Corporation for data and safety monitoring services and service as Chief Medical Officer for sense diagnostics. Dr. Richards reports compensation from Prehospital Guidelines Consortium for consultant services.
Contributor Information
Kori S. Zachrison, Department of Emergency Medicine, Massachusetts General Hospital, Boston, MA.
Victoria M. Nielsen, Massachusetts Department of Public Health, Boston, MA.
Natalia Perez de la Ossa, Department of Neurology, Stroke Unit, Hospital Universitari Germans Trias I Pujol, Badalona, Spain and Stroke Programme, Catalan Health Department, Agency for Health Quality and Assessment of Catalonia, Barcelona, Spain.
Tracy E. Madsen, Department of Emergency Medicine, Warren Alpert Medical School of Brown University, Providence, RI.
Rebecca E. Cash, Department of Emergency Medicine, Massachusetts General Hospital, Boston, MA.
Remle P. Crowe, ESO, Inc, Austin, TX.
Erika C. Odom, Division for Heart Disease and Stroke Prevention, Centers for Disease Control and Prevention, Atlanta, GA.
Edward C. Jauch, Department of Research, University of North Carolina Health Sciences at Mountain Area Health Education Center, Asheville, NC.
Opeolu M. Adeoye, Department of Emergency Medicine, Washington University School of Medicine, St. Louis, MO.
Christopher T. Richards, Division of EMS, Department of Emergency Medicine, University of Cincinnati College of Medicine, Cincinnati, OH.
REFERENCES
- 1.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke a guideline for healthcare professionals from the American Heart Association/American Stroke A. Stroke 2019;50:E344–E418. doi: 10.1161/STR.0000000000000211 [DOI] [PubMed] [Google Scholar]
- 2.Moser DK, Kimble LP, Alberts MJ, Alonzo A, Croft JB, Dracup K, Evenson KR, Go AS, Hand MM, Kothari RU, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on Cardiovascular Nursing and Stroke Council. J Cardiovasc Nur. 2007;22:326–343. doi: 10.1097/01.jcn.0000278963.28619.4a [DOI] [PubMed] [Google Scholar]
- 3.Higashida R, Alberts MJ, Alexander DN, Crocco TJ, Demaerschalk BM, Derdeyn CP, Goldstein LB, Jauch EC, Mayer SA, Meltzer NM, et al. ; American Heart Association Advocacy Coordinating Committee. Interactions within stroke systems of care: a policy statement from the American Heart Association/American Stroke Association. Stroke. 2013;44:2961–2984. doi: 10.1161/STR.0b013e3182a6d2b2 [DOI] [PubMed] [Google Scholar]
- 4.Adeoye O, Nyström KV, Yavagal DR, Luciano J, Nogueira RG, Zorowitz RD, Khalessi AA, Bushnell C, Barsan WG, Panagos P, et al. Recommendations for the establishment of stroke systems of care: a 2019 update: a policy statement from the American Stroke Association. Stroke 2019;50:e187–e210. doi: 10.1161/STR.0000000000000173 [DOI] [PubMed] [Google Scholar]
- 5.Patel MD, Rose KM, O’Brien EC, Rosamond WD. Prehospital notification by emergency medical services reduces delays in stroke evaluation: findings from the North Carolina stroke care collaborative. Stroke. 2011;42:2263–2268. doi: 10.1161/STROKEAHA.110.605857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ekundayo OJ, Saver JL, Fonarow GC, Schwamm LH, Xian Y, Zhao X, Hernandez AF, Peterson ED, Cheng EM. Patterns of emergency medical services use and its association with timely stroke treatment findings from Get with the Guidelines-Stroke. Circ Cardiovasc Qual Outcomes. 2013;6:262–269. doi: 10.1161/CIRCOUTCOMES.113.000089 [DOI] [PubMed] [Google Scholar]
- 7.Nielsen VM, DeJoie-Stanton C, Song G, Christie A, Guo J, Zachrison KS. The Association between presentation by EMS and EMS prenotification with receipt of intravenous tissue-type plasminogen activator in a state implementing stroke systems of care. Prehosp Emerg Care. 2020;24:319–325. doi: 10.1080/10903127.2019.1662862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mochari-Greenberger H, Xian Y, Hellkamp AS, Schulte PJ, Bhatt DL, Fonarow GC, Saver JL, Reeves MJ, Schwamm LH, Smith EE. Racial/ethnic and sex differences in emergency medical services transport among hospitalized us stroke patients: analysis of the national get with the guidelines-stroke registry. J Am Heart Assoc. 2015;4:e002099. doi: 10.1161/JAHA.115.002099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Asaithambi G, Tong X, Lakshminarayan K, Coleman King SM, George MG, Odom EC. Emergency medical services utilization for acute stroke care: analysis of the paul coverdell national acute stroke program, 2014–2019. Prehosp Emerg Care. 2022;26:326–332. doi: 10.1080/10903127.2021.1877856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stroke (Stroke Heroes Act FAST): Massachusetts Health Promotion Clearinghouse [Internet]. [cited 2019 Mar 17]; Available from: https://massclearinghouse.ehs.state.ma.us/category/HDSP.html [Google Scholar]
- 11.Williams O, Quinn ELH, Teresi J, Eimicke JP, Kong J, Ogedegbe G, Noble J. Improving community stroke preparedness in the hhs (hip-hop stroke) randomized clinical trial. Stroke. 2018;49:972–979. doi: 10.1161/STROKEAHA.117.019861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fussman C, Rafferty AP, Lyon-Callo S, Morgenstern LB, Reeves MJ. Lack of association between stroke symptom knowledge and intent to call 911: A population-based survey. Stroke. 2010;41:1501–1507. doi: 10.1161/STROKEAHA.110.578195 [DOI] [PubMed] [Google Scholar]
- 13.Denti L, Caminiti C, Scoditti U, Zini A, Malferrari G, Zedde ML, Guidetti D, Baratti M, Vaghi L, Montanari E, et al. Impact on prehospital delay of a stroke preparedness campaign a SW-RCT (Stepped-Wedge Cluster Randomized Controlled Trial). Stroke. 2017;48:3316–3322. doi: 10.1161/STROKEAHA.117.018135 [DOI] [PubMed] [Google Scholar]
- 14.Skolarus LE, Murphy JB, Zimmerman MA, Bailey S, Fowlkes S, Brown DL, Lisabeth LD, Greenberg E, Morgenstern LB. Individual and community determinants of calling 911 for stroke among African Americans in an urban community. Circ Cardiovasc Qual Outcomes. 2013;6:278–283. doi: 10.1161/CIRCOUTCOMES.111.000017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mandelzweig L, Goldbourt U, Boyko V, Tanne D. Perceptual, social, and behavioral factors associated with delays in seeking medical care in patients with symptoms of acute stroke. Stroke. 2006;37:1248–1253. doi: 10.1161/01.STR.0000217200.61167.39 [DOI] [PubMed] [Google Scholar]
- 16.Xirasagar S, Tsai MH, Heidari K, Hardin JW, Wu Y, Wronski R, Hurley D, Jauch EC, Sen S. Why acute ischemic stroke patients in the United States use or do not use emergency medical services transport? Findings of an inpatient survey. BMC Health Serv Res. 2019;19:1–11. doi: 10.1186/s12913-019-4741-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iversen AB, Blauenfeldt RA, Johnsen SP, Sandal BF, Christensen B, Andersen G, Christensen MB. Understanding the seriousness of a stroke is essential for appropriate help-seeking and early arrival at a stroke centre: a cross-sectional study of stroke patients and their bystanders. Eur Stroke J. 2020;5:351–361. doi: 10.1177/2396987320945834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eisenstein AR, Song S, Mason M, Kandula NR, Richards C, Aggarwal NT, Prabhakaran SK. A community-partnered approach to inform a culturally relevant health promotion intervention for stroke. Health Educ Behav. 2018;45:697–705. doi: 10.1177/1090198117752787 [DOI] [PubMed] [Google Scholar]
- 19.Seo M, Begley C, Langabeer JR, DelliFraine JL. Barriers and disparities in emergency medical services 911 calls for stroke symptoms in the United States adult population: 2009 BRFSS survey. West J Emerg Med. 2014;15:251–259. doi: 10.5811/westjem.2013.9.18584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Skolarus LE, Zimmerman MA, Murphy J, Brown DL, Kerber KA, Bailey S, Fowlkes S, Morgenstern LB. Community-based participatory research: a new approach to engaging community members to rapidly call 911 for stroke. Stroke. 2011;42:1862–1866. doi: 10.1161/STROKEAHA.110.609495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jauch EC, Cucchiara B, Adeoye O, Meurer W, Brice J, Chan YYF, Gentile N, Hazinski MF. Part 11: adult stroke. Circulation. 2010;122:S818–S828. doi: 10.1161/CIRCULATIONAHA.110.971044 [DOI] [PubMed] [Google Scholar]
- 22.Clawson JJ, Sinclair R. The emotional content and cooperation score in emergency medical dispatching. Prehospital emergency care. 2001;5:29–35. doi: 10.1080/10903120190940290 [DOI] [PubMed] [Google Scholar]
- 23.Acker JE, Pancioli AM, Crocco TJ, Eckstein MK, Jauch EC, Larrabee H, Meltzer NM, Mergendahl WC, Munn JW, Prentiss SM, et al. ; American Heart Association. Implementation strategies for emergency medical services within stroke systems of care: a policy statement from the American Heart Association/American Stroke Association Expert Panel on Emergency Medical Services Systems and the Stroke Council. Stroke. 2007;38:3097–3115. doi: 10.1161/STROKEAHA.107.186094 [DOI] [PubMed] [Google Scholar]
- 24.Jauch EC, Saver JL, Adams HP, Bruno A, Connors JJB, Demaerschalk BM, Khatri P, McMullan PW, Qureshi AI, Rosenfield K, et al. ; American Heart Association Stroke Council. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:870–947. doi: 10.1161/STR.0b013e318284056a [DOI] [PubMed] [Google Scholar]
- 25.Abboud ME, Band R, Jia J, Pajerowski W, David G, Guo M, Mechem CC, Messé SR, Carr BG, Mullen MT. Recognition of stroke by EMS is associated with improvement in emergency department quality measures. Prehosp Emerg Care. 2016;20:729–736. doi: 10.1080/10903127.2016.1182602 [DOI] [PubMed] [Google Scholar]
- 26.Abdullah AR, Smith EE, Biddinger PD, Kalenderian D, Schwamm LH. Advance hospital notification by EMS in acute stroke is associated with shorter door-to-computed tomography time and increased likelihood of administration of tissue-plasminogen activator. Prehosp Emerg Care. 2009;12:426–431. doi: 10.1080/10903120802290828 [DOI] [PubMed] [Google Scholar]
- 27.Messe SR, Khatri P, Reeves MJ, Smith EE, Saver JL, Bhatt DL, Grau-Sepulveda MV, Cox M, Peterson ED, Fonarow GC, et al. Why are acute ischemic stroke patients not receiving IV tPA? Results from a national registry. Neurology. 2016;87:1565–1574. doi: 10.1212/WNL.0000000000003198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prabhakaran S, O’Neill K, Stein-Spencer L, Walter J, Alberts MJ. Prehospital triage to primary stroke centers and rate of stroke thrombolysis. JAMA Neurol. 2013;70:1126–1132. doi: 10.1001/jamaneurol.2013.293 [DOI] [PubMed] [Google Scholar]
- 29.Eliakundu AL, Cadilhac DA, Kim J, Kilkenny MF, Bagot KL, Andrew E, Cox S, Bladin CF, Stephenson M, Pesavento L, et al. Determining the sensitivity of emergency dispatcher and paramedic diagnosis of stroke: statewide registry linkage study. J Am Coll Emerg Physicians Open. 2022;3:e12750. doi: 10.1002/emp2.12750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buck BH, Starkman S, Eckstein M, Kidwell CS, Haines J, Huang R, Colby D, Saver JL. Dispatcher recognition of stroke using the national academy medical priority dispatch system. Stroke. 2009;40:2027–2030. doi: 10.1161/STROKEAHA.108.545574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Caceres JA, Adil MM, Jadhav V, Chaudhry SA, Pawar S, Rodriguez GJ, Suri MFK, Qureshi AI. Diagnosis of stroke by emergency medical dispatchers and its impact on the prehospital care of patients. J Stroke Cerebrovasc Dis. 2013;22:e610–e614. doi: 10.1016/j.jstrokecerebrovasdis.2013.07.039 [DOI] [PubMed] [Google Scholar]
- 32.Ellison SR, Gratton MC, Schwab RA, Ma OJ. Prehospital dispatch assessment of stroke. Mo Med 2004;101:64–66. [PubMed] [Google Scholar]
- 33.Jia J, Band R, Abboud ME, Pajerowski W, Guo M, David G, Mechem CC, Messé SR, Carr BG, Mullen MT. Accuracy of emergency medical services dispatcher and crew diagnosis of stroke in clinical practice. Front Neurol. 2017;8:466. doi: 10.3389/fneur.2017.00466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krebes S, Ebinger M, Baumann AM, Kellner PA, Rozanski M, Doepp F, Sobesky J, Gensecke T, Leidel BA, Malzahn U, et al. Development and validation of a dispatcher identification algorithm for stroke emergencies. Stroke. 2012;43:776–781. doi: 10.1161/STROKEAHA.111.634980 [DOI] [PubMed] [Google Scholar]
- 35.Oostema JA, Carle T, Talia N, Reeves M. Dispatcher stroke recognition using a stroke screening tool: a systematic review. Cerebrovasc Dis. 2016;42:370–377. doi: 10.1159/000447459 [DOI] [PubMed] [Google Scholar]
- 36.Porteous GH, Corry MD, Smith WS. Emergency medical services dispatcher identification of stroke and transient ischemic attack. Prehosp Emerg Care. 2009;3:211–216. doi: 10.1080/10903129908958939 [DOI] [PubMed] [Google Scholar]
- 37.Ramanujam P, Guluma KZ, Castillo EM, Chacon M, Jensen MB, Patel E, Linnick W, Dunford J. Accuracy of stroke recognition by emergency medical dispatchers and paramedics—San Diego experience. Prehosp Emerg Care. 2009;12:307–313. doi: 10.1080/10903120802099526 [DOI] [PubMed] [Google Scholar]
- 38.Reginella R, Crocco T, Tadros A, Shackleford A, Davis S. Predictors of stroke during 9-1-1 calls: opportunities for improving EMS response. Prehosp Emerg Care. 2009;10:369–373. doi: 10.1080/10903120600725850 [DOI] [PubMed] [Google Scholar]
- 39.Rosamond WD, Evenson KR, Schroeder EB, Morris DL, Johnson AM, Brice JH. Calling emergency medical services for acute stroke: a study of 9-1-1 tapes. Prehosp Emerg Care. 2009;9:19–23. doi: 10.1080/10903120590891985 [DOI] [PubMed] [Google Scholar]
- 40.Richards CT, Wang B, Markul E, Albarran F, Rottman D, Aggarwal NT, Lindeman P, Stein-Spencer L, Weber JM, Pearlman KS, et al. Identifying key words in 9-1-1 calls for stroke: a mixed methods approach. Prehosp Emerg Care. 2017;21:761–766. doi: 10.1080/10903127.2017.1332124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bache KG, Grotta JC. Improving stroke treatment and outcomes with mobile stroke units. JAMA. 2021;325:441–442. doi: 10.1001/jama.2020.25832 [DOI] [PubMed] [Google Scholar]
- 42.Fassbender K, Merzou F, Lesmeister M, Walter S, Grunwald IQ, Ragoschke-Schumm A, Bertsch T, Grotta JR. Impact of mobile stroke units. J Neurol Neurosurg Psychiatry. 2021;92:815. doi: 10.1136/jnnp-2020-324005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Navi BB, Audebert HJ, Alexandrov AW, Cadilhac DA, Grotta JC; PRESTO (Prehospital Stroke Treatment Organization) Writing Group. Mobile stroke units: evidence, gaps, and next steps. Stroke 2022;53:2103–2113. doi: 10.1161/STROKEAHA.121.037376 [DOI] [PubMed] [Google Scholar]
- 44.Grotta JC, Yamal J-M, Parker SA, Rajan SS, Gonzales NR, Jones WJ, Alexandrov AW, Navi BB, Nour M, Spokoyny I, et al. Prospective, multicenter, controlled trial of mobile stroke units. N Engl J Med. 2021;385:971–981. doi: 10.1056/NEJMoa2103879. [DOI] [PubMed] [Google Scholar]
- 45.Ebinger M, Siegerink B, Kunz A, Wendt M, Weber JE, Schwabauer E, Geisler F, Freitag E, Lange J, Behrens J, et al. ; Berlin_PRehospital Or Usual Delivery in Stroke Care (B_PROUD) Study Group. Association between dispatch of mobile stroke units and functional outcomes among patients with acute ischemic stroke in Berlin. JAMA. 2021;325:454–466. doi: 10.1001/jama.2020.26345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Grotta JC, Yamal J-M, Parker SA, Rajan SS, Gonzales NR, Jones WJ, Alexandrov AW, Navi BB, Nour M, Spokoyny I, et al. Prospective, multicenter, controlled trial of mobile stroke units. N Engl J Med. 2021;385:971–981. doi: 10.1056/NEJMoa2103879 [DOI] [PubMed] [Google Scholar]
- 47.Gyrd-Hansen D, Rose Olsen K, Bollweg K, Kronborg C, Ebinger M, Audebert HJ. Cost-effectiveness estimate of prehospital thrombolysis. Neurology. 2015;84:1090–1097. doi: 10.1212/WNL.0000000000001366 [DOI] [PubMed] [Google Scholar]
- 48.Stroke Certification | The Joint Commission. Accessed January 14, 2020. https://www.jointcommission.org/accreditation-andcertification/certification/certifications-by-setting/hospital-certifications/stroke-certification/. [Google Scholar]
- 49.Waldman A, Tadi P, Rawal AR. Stroke center certification. J Neurosci Nurs. 2021;38:399–402. [PubMed] [Google Scholar]
- 50.Man S, Cox M, Patel P, Smith EE, Reeves MJ, Saver JL, Bhatt DL, Xian Y, Schwamm LH, Fonarow GC. Differences in acute ischemic stroke quality of care and outcomes by primary stroke center certification organization. Stroke. 2017;48:412–419. doi: 10.1161/STROKEAHA.116.014426 [DOI] [PubMed] [Google Scholar]
- 51.Alberts MJ, Wechsler LR, Lee Jensen ME, Latchaw RE, Crocco TJ, George MG, Baranski J, Bass RR, Ruff RL, Huang J, et al. Formation and function of acute stroke-ready hospitals within a stroke system of care recommendations from the brain attack coalition. Stroke. 2013;44:3382–3393. doi: 10.1161/STROKEAHA.113.002285 [DOI] [PubMed] [Google Scholar]
- 52.Alberts MJ, Latchaw RE, Jagoda A, Wechsler LR, Crocco T, George MG, Connolly ES, Mancini B, Prudhomme S, Gress D, et al. ; Brain Attack Coalition. Revised and updated recommendations for the establishment of primary stroke centers. Stroke 2011;42:2651–2665. doi: 10.1161/STROKEAHA.111.615336 [DOI] [PubMed] [Google Scholar]
- 53.Alberts MJ, Latchaw RE, Selman WR, Shephard T, Hadley MN, Brass LM, Koroshetz W, Marler JR, Booss J, Zorowitz RD, et al. ; Brain Attack Coalition. Recommendations for comprehensive stroke centers: a consensus statement from the Brain Attack Coalition. Stroke 2005;36:1597–1616. doi: 10.1161/01.STR.0000170622.07210.b4 [DOI] [PubMed] [Google Scholar]
- 54.Shen YC, Chen G, Hsia RY. Community and hospital factors associated with stroke center certification in the United States, 2009 to 2017. JAMA Netw Open. 2019;2:e197855–e197855. doi: 10.1001/jamanetworkopen.2019.7855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shen Y-C, Sarkar N, Hsia RY. Structural inequities for historically underserved communities in the adoption of stroke certification in the United States. JAMA Neurol 2022;79:777–786. doi: 10.1001/jamaneurol.2022.1621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Novarro-Escudero N, Moon YJ, Olmedo A, Ferguson T, Caballero I, Onodera E, Effio E, Klein LM, Zink EK, Johnson B, et al. Organization and implementation of a stroke center in panamá, a model for implementation of stroke centers in low and middle income countries. Front Neurol. 2021;12:684775. doi: 10.3389/fneur.2021.684775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Waje-Andreassen U, Nabavi DG, Engelter ST, Dippel DWJ, Jenkinson D, Skoda O, Zini A, Orken DN, Staikov I, Lyrer P. European Stroke Organisation certification of stroke units and stroke centres. Eur Stroke J. 2018;3:220–226. doi: 10.1177/2396987318778971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cash RE, Crowe RP, Rodriguez SA, Panchal AR. Disparities in feedback provision to emergency medical services professionals. Prehosp Emerg Care. 2017;21:773–781. doi: 10.1080/10903127.2017.1328547 [DOI] [PubMed] [Google Scholar]
- 59.Brichko L, Jennings P, Bain C, Smith K, Mitra B. Selecting cases for feedback to pre-hospital clinicians – a pilot study. Aust Health Rev. 2016;40:306–310. doi: 10.1071/AH15079 [DOI] [PubMed] [Google Scholar]
- 60.Oostema JA, Chassee T, Baer W, Edberg A, Reeves MJ. A brief educational intervention improves emergency medical services stroke recognition. Stroke. 2019;50:1193–1200. doi: 10.1161/STROKEAHA.118.023885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Meyer AND, Payne VL, Meeks DW, Rao R, Singh H. Physicians’ diagnostic accuracy, confidence, and resource requests: a vignette study. JAMA Intern Med. 2013;173:1952–1958. doi: 10.1001/jamainternmed.2013.10081 [DOI] [PubMed] [Google Scholar]
- 62.Dylla L, Rice JD, Poisson SN, Monte AA, Higgins HM, Ginde AA, Herson PS. Analysis of stroke care among 2019–2020 National emergency medical services information system encounters. J Stroke Cerebrovasc Dis. 2022;31:106278. doi: 10.1016/j.jstrokecerebrovasdis.2021.106278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Choi B, Tsai D, McGillivray CG, Amedee C, Sarafin JA, Silver B. Hospital-directed feedback to emergency medical services improves prehospital performance. Stroke. 2014;45:2137–2140. doi: 10.1161/STROKEAHA.114.005679 [DOI] [PubMed] [Google Scholar]
- 64.Cifra CL, Sittig DF, Singh H. Bridging the feedback gap: a sociotechnical approach to informing clinicians of patients’ subsequent clinical course and outcomes. BMJ Qual Saf. 2021;30:591–597. doi: 10.1136/bmjqs-2020-012464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mears GD, Rosamond WD, Lohmeier C, Murphy C, O’Brien E, Asimos AW, Brice JH. A link to improve stroke patient care: a successful linkage between a statewide emergency medical services data system and a stroke registry. Acad Emerg Med. 2010;17:1398–1404. doi: 10.1111/j.1553-2712.2010.00925.x [DOI] [PubMed] [Google Scholar]
- 66.Martin TJ, Ranney ML, Dorroh J, Asselin N, Sarkar IN. Health information exchange in emergency medical services. Appl Clin Inform. 2018;9:884–891. doi: 10.1055/s-0038-1676041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Isenberg DL, Henry KA, Sigal A, Deaner T, Nomura JT, Murphy KA, Cooney D, Wojcik S, Brandler ES, Kuc A, et al. Optimizing prehospital stroke systems of care-reacting to changing paradigms (OPUS-REACH): a pragmatic registry of large vessel occlusion stroke patients to create evidence-based stroke systems of care and eliminate disparities in access to stroke care. BMC Neurol. 2022;22:132. doi: 10.1186/s12883-022-02653-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Li T, Munder SP, Chaudhry A, Madan R, Gribko M, Arora R. Emergency medical services providers’ knowledge, practices, and barriers to stroke management. Open Access Emerg Med. 2019;11:297–303. doi: 10.2147/OAEM.S228240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Crowe RP, Fernandez AR, Pepe PE, Cash RE, Rivard MK, Wronski R, Anderson SE, Hogan TH, Andridge RR, Panchal AR, et al. The association of job demands and resources with burnout among emergency medical services professionals. J Am Coll Emerg Physicians Open. 2020;1:6–16. doi: 10.1002/emp2.12014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Michigan Links Hospital and Emergency Medical Services Data | cdc.gov. Accessed August 23, 2022. https://www.cdc.gov/dhdsp/programs/success_MI.htm. [Google Scholar]
- 71.Linking Patient Data from Emergency Dispatch to Hospital Discharge – JEMS: EMS, Emergency Medical Services – Training, Paramedic, EMT News. Accessed August 23, 2022. https://www.jems.com/operations/linking-patient-data-from-emergency-dispatch-to-hospital-discharge/. [Google Scholar]
- 72.Gunderson MR, Florin A, Price M, Reed J. NEMSMA position statement and white paper: process and outcomes data sharing between EMS and receiving hospitals. Prehosp Emerg Care. 2021;25:307–313. doi: 10.1080/10903127.2020.1792017 [DOI] [PubMed] [Google Scholar]
- 73.Goldberg SA, Porat A, Strother CG, Lim NQ, Wijeratne HRS, Sanchez G, Munjal KG. Quantitative analysis of the content of EMS handoff of critically ill and injured patients to the emergency department. Prehosp Emerg Care. 2017;21:14–17. doi: 10.1080/10903127.2016.1194930 [DOI] [PubMed] [Google Scholar]
- 74.Schwamm LH, Pancioli A, Acker JE, Goldstein LB, Zorowitz RD, Shephard TJ, Moyer P, Gorman M, Johnston SC, Duncan PW, et al. ; American Stroke Association’s Task Force on the Development of Stroke Systems. Recommendations for the establishment of stroke systems of care: recommendations from the American Stroke Association’s Task Force on the Development of Stroke Systems. Stroke. 2005;36:690–703. doi: 10.1161/01.STR.0000158165.42884.4F [DOI] [PubMed] [Google Scholar]
- 75.Zachrison KS, Khatri P. Self-driven prehospital triage decisions for suspected stroke – another step closer. JAMA Neurol. 2021;78:146–148. doi: 10.1001/jamaneurol.2020.4425 [DOI] [PubMed] [Google Scholar]
- 76.Ismail M, Armoiry X, Tau N, Zhu F, Sadeh-Gonik U, Piotin M, Blanc R, Mazighi M, Bracard S, Anxionnat R, et al. Mothership versus drip and ship for thrombectomy in patients who had an acute stroke: a systematic review and meta-analysis. J Neurointerv Surg. 2019;11:11–19. doi: 10.1136/neurintsurg-2018-014249 [DOI] [PubMed] [Google Scholar]
- 77.Romoli M, Paciaroni M, Tsivgoulis G, Agostoni EC, Vidale S. Mothership versus drip-and-ship model for mechanical thrombectomy in acute stroke: a systematic review and meta-analysis for clinical and radiological outcomes. J Stroke. 2020;22:317–323. doi: 10.5853/jos.2020.01767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mohamed A, Fatima N, Shuaib A, Saqqur M. Comparison of mothership versus drip-and-ship models in treating patients with acute ischemic stroke: a systematic review and meta-analysis. Int J Stroke.2022;17:141–154. doi: 10.1177/17474930211013285 [DOI] [PubMed] [Google Scholar]
- 79.Perez de la ON, Abilleira S, Jovin TG, Garcia-Tornel A, Jimenez X, Urra X, Cardona P, Cocho D, Purroy F, Serena J, et al. Effect of direct transportation to local stroke center vs thrombectomy-capable center on neurological outcomes in patients with suspected large vessel occlusion stroke in non-urban areas: the RACECAT randomized clinical trial. JAMA. 2022;327:1782–1794. doi: 10.1001/jama.2022.4404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zachrison KS, Schwamm LH. Strategic opportunities to improve stroke systems of care. JAMA. 2022;327:1765–1767. doi: 10.1001/jama.2022.3820 [DOI] [PubMed] [Google Scholar]
- 81.Yu CY, Panagos PD, Kansagra AP. Travel time and distance for bypass and non-bypass routing of stroke patients in the USA. J Neurointerv Surg. 2022;neurintsurg-2022-018787. doi: 10.1136/neurintsurg-2022-018787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rynor H, Levine J, Souchak J, Shashoua N, Ramirez M, Gonzalez IC, Ramos V, Saxena A, Veledar E, Starosciak AK, et al. The effect of a county prehospital FAST-ED initiative on endovascular treatment times. J Stroke Cerebrovasc Dis. 2020;29:105220. doi: 10.1016/j.jstrokecerebrovasdis.2020.105220 [DOI] [PubMed] [Google Scholar]
- 83.Mohamad NF, Hastrup S, Rasmussen M, Andersen MS, Johnsen SP, Andersen G, Simonsen CZ. Bypassing primary stroke centre reduces delay and improves outcomes for patients with large vessel occlusion. Eur Stroke J. 2016;1:85–92. doi: 10.1177/2396987316647857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Jumaa MA, Castonguay AC, Salahuddin H, Shawver J, Saju L, Burgess R, Kung V, Slawski DE, Tietjen G, Lindstrom D, et al. Long-term implementation of a pre-hospital severity scale for EMS triage of acute stroke: a real-world experience. J Neurointerv Surg. 2020;12:19–24. doi: 10.1136/neurintsurg-2019-014997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Jayaraman MV, Hemendinger ML, Baird GL, Yaghi S, Cutting S, Saad A, Siket M, Madsen TE, Williams K, Rhodes J, et al. Field triage for endovascular stroke therapy: a population-based comparison. J Neurointerv Surg. 2020;12:233–239. doi: 10.1136/neurintsurg-2019-015033 [DOI] [PubMed] [Google Scholar]
- 86.Ernst M, Schlemm E, Holodinsky JK, Kamal N, Thomalla G, Fiehler J, Brekenfeld C. Modeling the optimal transportation for acute stroke treatment: the impact of the drip-and-drive paradigm. Stroke. 2019;51:275–281. doi: 10.1161/STROKEAHA.119.027493 [DOI] [PubMed] [Google Scholar]
- 87.Holodinsky JK, Williamson TS, Demchuk AM, Zhao H, Zhu L, Francis MJ, Goyal M, Hill MD, Kamal N. modeling stroke patient transport for all patients with suspected large-vessel occlusion. JAMA Neurol. 2018;75:1477–1486. doi: 10.1001/jamaneurol.2018.2424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jauch EC, Schwamm LH, Panagos PD, Barbazzeni J, Dickson R, Dunne R, Foley J, Fraser JF, Lassers G, Martin-Gill C, et al. ; Prehospital Stroke System of Care Consensus Conference. Recommendations for regional stroke destination plans in rural, suburban, and urban communities from the prehospital stroke system of care consensus conference: a consensus statement from the American Academy of Neurology, American Heart Association/American Stroke Association, American Society of Neuroradiology, National Association of EMS Physicians, National Association of State EMS Officials, Society of NeuroInterventional Surgery, and Society of Vascular and Interventional Neurology: Endorsed by the Neurocritical Care Society. Stroke. 2021;52:e133–e152. doi: 10.1161/STROKEAHA.120.033228 [DOI] [PubMed] [Google Scholar]
- 89.Duvekot MHC, Venema E, Rozeman AD, Moudrous W, Vermeij FH, Biekart M, Lingsma HF, Maasland L, Wijnhoud AD, Mulder LJMM, et al. ; PRESTO Investigators. Comparison of eight prehospital stroke scales to detect intracranial large-vessel occlusion in suspected stroke (PRESTO): a prospective observational study. Lancet Neurol. 2021;20:213–221. doi: 10.1016/S1474-4422(20)30439-7 [DOI] [PubMed] [Google Scholar]
- 90.Ali A, Zachrison KS, Eschenfeldt PC, Schwamm LH, Hur C. Optimization of prehospital triage of patients with suspected ischemic stroke: results of a mathematical model. Stroke. 2018;49:2532–2535. doi: 10.1161/STROKEAHA.118.022041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Magdon-Ismail Z, Benesch C, Cushman JT, Brissette I, Southerland AM, Brandler ES, Sozener CB, Flor S, Hemmitt R, Wales K, et al. ; Upstate New York Stroke Work Groups. Establishing recommendations for stroke systems in the thrombectomy era: the upstate New York stakeholder proceedings. Stroke. 2017;48:2003–2006. doi: 10.1161/STROKEAHA.117.017412 [DOI] [PubMed] [Google Scholar]
- 92.Baciu AB, Rodriguez LJ, Bibbins-Domingo K. Spatial justice and implications for US health care. JAMA Health Forum. 2021;2:e214082. doi: 10.1001/jamahealthforum.2021.4082 [DOI] [PubMed] [Google Scholar]
- 93.Otte E, Rousseau R. Social network analysis: a powerful strategy, also for the information sciences. J Inf Sci. 2002;28:441–453. 10.1177/016555150202800601 [DOI] [Google Scholar]
- 94.Zachrison KS, Dhand A, Schwamm LH, Onnela J-P. A Network Approach to Stroke Systems of Care. Circ Cardiovasc Qual Outcomes. 2019;12:e005526. doi: 10.1161/CIRCOUTCOMES.119.005526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Luke DA, Harris JK. Network analysis in public health: history, methods, and applications. Annu Rev Public Health. 2007;28:69–93. doi: 10.1146/annurev.publhealth.28.021406.144132 [DOI] [PubMed] [Google Scholar]
- 96.Zachrison KS, Amati V, Schwamm LH, Yan Z, Nielsen V, Christie A, Reeves MJ, Sauser JP, Lomi A, Onnela J-P. Influence of hospital characteristics on hospital transfer destinations for patients with stroke. Circ Cardiovasc Qual Outcomes. 2022;15:e008269. doi: 10.1161/CIRCOUTCOMES.121.008269 [DOI] [PubMed] [Google Scholar]
- 97.Cash RE, Boggs KM, Richards CT, Camargo CA, Zachrison KS. Emergency medical service time intervals for patients with suspected stroke in the United States. Stroke. 2022;29:E75–E78. doi: 10.1161/STROKEAHA.121.037509 [DOI] [PubMed] [Google Scholar]
- 98.Schwartz J, Dreyer RP, Murugiah K, Ranasinghe I. Contemporary prehospital emergency medical services response times for suspected stroke in the United States. Prehosp Emerg Care. 2016;20:560–565. doi: 10.3109/10903127.2016.1139219 [DOI] [PubMed] [Google Scholar]
- 99.Chuck CC, Martin TJ, Kalagara R, Madsen TE, Furie KL, Yaghi S, Reznik ME. Statewide emergency medical services protocols for suspected stroke and large vessel occlusion. JAMA Neurol. 2021;78:1404–1406. doi: 10.1001/jamaneurol.2021.3227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Dimitrov N, Koenig W, Bosson N, Song S, Saver JL, Mack WJ, Sanossian N. Variability in criteria for emergency medical services routing of acute stroke patients to designated stroke center hospitals. Western J Emerg Med. 2015;16:743–746. doi: 10.5811/westjem.2015.7.26179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Walter S, Zhao H, Easton D, Bil C, Sauer J, Liu Y, Lesmeister M, Grunwald IQ, Donnan GA, Davis SM, et al. Air-mobile stroke unit for access to stroke treatment in rural regions. Int J Stroke. 2018;13:568–575. doi: 10.1177/1747493018784450 [DOI] [PubMed] [Google Scholar]
- 102.Mathur S, Walter S, Grunwald IQ, Helwig SA, Lesmeister M, Fassbender K. Improving prehospital stroke services in rural and underserved settings with mobile stroke units. Front Neurol. 2019;10:159. doi: 10.3389/fneur.2019.00159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kate MP, Jeerakathil T, Buck BH, Khan K, Nomani AZ, Butt A, Thirunavukkarasu S, Nowacki T, Kalashyan H, Lloret-Villas MI, et al. Pre-hospital triage of suspected acute stroke patients in a mobile stroke unit in the rural Alberta. Sci Rep. 2021;11:4988. doi: 10.1038/s41598-021-84441-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hubert GJ, Kraus F, Maegerlein C, Platen S, Friedrich B, Kain HU, Witton-Davies T, Hubert ND, Zimmer C, Bath PM, et al. The “Flying Intervention Team”: a novel stroke care concept for rural areas. Cerebrovasc Dis. 2021;50:375–382. doi: 10.1159/000514845 [DOI] [PubMed] [Google Scholar]
- 105.Hubert GJ, Hubert ND, Maegerlein C, Kraus F, Wiestler H, Müller-Barna P, Gerdsmeier-Petz W, Degenhart C, Hohenbichler K, Dietrich D, et al. Association between use of a flying intervention team vs patient interhospital transfer and time to endovascular thrombectomy among patients with acute ischemic stroke in nonurban Germany. JAMA. 2022;327:1795–1805. doi: 10.1001/jama.2022.5948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lippman JM, Smith SNC, Mcmurry TL, Sutton ZG, Gunnell BS, Cote J, Perina DG, Cattell-Gordon DC, Rheuban KS, Solenski NJ, et al. Mobile telestroke during ambulance transport is feasible in a rural EMS setting: The iTREAT Study. Telemed J E Health. 2016;22:507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Crowe RP, Levine R, Bentley MA. Prehospital helicopter air ambulances part 1: access, protocols, and utilization. Air Med J. 2015;34:333–336. doi: 10.1016/j.amj.2015.06.004 [DOI] [PubMed] [Google Scholar]
- 108.Hawk A, Marco C, Huang M, Chow B. Helicopter scene response for stroke patients: a 5-year experience. Air Med J. 2016;35:352–354. doi: 10.1016/j.amj.2016.05.007 [DOI] [PubMed] [Google Scholar]
- 109.Silbergleit R, Scott PA, Lowell MJ, Silbergleit R. Cost-effectiveness of helicopter transport of stroke patients for thrombolysis. Acad Emerg Med. 2003;10:966–972. doi: 10.1197/s1069-6563(03)00316-6 [DOI] [PubMed] [Google Scholar]
- 110.Tal S, Mor S. The impact of helicopter emergency medical service on acute ischemic stroke patients: a systematic review. Am J Emerg Med. 2021;42:178–187. doi: 10.1016/j.ajem.2020.02.021 [DOI] [PubMed] [Google Scholar]
- 111.Sequeira D, Martin-Gill C, Kesinger MR, Thompson LR, Jovin TG, Massaro LM, Guyette FX. Characterizing strokes and stroke mimics transported by helicopter emergency medical services. Prehosp Emerg Care. 2016;20:723–728. doi: 10.3109/10903127.2016.1168889 [DOI] [PubMed] [Google Scholar]
- 112.Adcock AK, Minardi J, Findley S, Daniels D, Large M, Power M. Value utilization of emergency medical services air transport in acute ischemic stroke. J Emerg Med. 2020;59:687–692. doi: 10.1016/j.jemermed.2020.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Meuli L, Zimmermann A, Menges AL, Tissi M, Becker S, Albrecht R, Pietsch U. Helicopter emergency medical service for time critical interfacility transfers of patients with cardiovascular emergencies. Scand J Trauma Resusc Emerg Med. 2021;29:1–9. doi: 10.1186/s13049-021-00981-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kunte SA, Anderson D, Brown-Espaillat K, Froehler MT. Total transfer time for ground vs. air transport for interhospital and scene transfers of acute stroke patients. J Stroke Cerebrovasc Dis. 2021;30:105704. doi: 10.1016/j.jstrokecerebrovasdis.2021.105704 [DOI] [PubMed] [Google Scholar]
- 115.Cash RE, Rivard MK, Chrzan K, Mercer CB, Camargo CA, Panchal AR. Comparison of volunteer and paid EMS professionals in the United States. Prehosp Emerg Care. 2021;25:205–212. doi: 10.1080/10903127.2020.1752867 [DOI] [PubMed] [Google Scholar]
- 116.Freeman VA, Slifkin RT, Patterson PD. Recruitment and retention in rural and urban EMS: results from a national survey of local EMS directors. J Public Health Manag Pract. 2009;15:246–252. doi: 10.1097/PHH.0b013e3181a117fc [DOI] [PubMed] [Google Scholar]
- 117.Congressional Letter on the EMS Workforce Shortage – American Ambulance Association. Accessed February 28, 2022. https://ambulance.org/2021/10/04/workforceshortage/. [Google Scholar]
- 118.The Pandemic Exacerbates the “Paramedic Paradox” in Rural America | Kaiser Health News. Accessed July 12, 2022. https://khn.org/news/article/rural-paramedic-pandemic-shortage-montana/. [Google Scholar]
- 119.Results of a survey of New York’s emergency medical service work-force conducted by the New York State Emergency Medical Services Council WHERE ARE THE EMERGENCY MEDICAL RESPONDERS? 2019. Accessed July 12, 2022. https://ubmdems.com/wp-content/uploads/2020/01/Download-2019-NYS-EMS-Workforce-Report.pdf. [Google Scholar]
- 120.Shultis W, Graff R, Chamie C, Hart C, Louangketh P, McNamara M, Okon N, Tirschwell D. Striking rural-urban disparities observed in acute stroke care capacity and services in the pacific northwest: implications and recommendations. Stroke. 2010;41:2278–2282. doi: 10.1161/STROKEAHA.110.594374 [DOI] [PubMed] [Google Scholar]


