Abstract
Background
Pegylated interferon (peginterferon) plus ribavirin is the recommended treatment for patients with chronic hepatitis C, but systematic assessment of the effect of this treatment compared with interferon plus ribavirin is needed.
Objectives
To systematically evaluate the benefits and harms of peginterferon plus ribavirin versus interferon plus ribavirin for patients with chronic hepatitis C.
Search methods
We searched the Cochrane Hepato‐Biliary Group Controlled Trials Register, the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE, Science Citation Index‐Expanded, and LILACS. We also searched conference abstracts, journals, and grey literature. The last searches were conducted in September 2013.
Selection criteria
We included randomised clinical trials comparing peginterferon plus ribavirin versus interferon plus ribavirin with or without co‐intervention(s) (e.g., other antiviral drugs) for chronic hepatitis C. Quasi‐randomised and observational studies retrieved through the searches for randomised clinical trials were also considered for reports of harms. Our primary outcomes were liver‐related morbidity, all‐cause mortality, serious adverse events, adverse events leading to treatment discontinuation, other adverse events, and quality of life. Our secondary outcome was sustained virological response in serum, that is, undetectable hepatitis C virus RNA in serum by sensitive tests six months after the end of treatment.
Data collection and analysis
Two review authors independently used a standardised data collection form. We meta‐analysed data with both fixed‐effect and random‐effects models. For each outcome, we calculated the odds ratio (OR) (for liver‐related morbidity or all‐cause mortality) or the risk ratio (RR) along with 95% confidence interval (CI) based on intention‐to‐treat analysis. We used domains of the trials to assess the risk of systematic errors (bias) and trial sequential analyses to assess the risk of random errors (play of chance).
For each outcome, we calculated the RR with 95% CI based on intention‐to‐treat analysis. Effects of interventions on outcomes were assessed according to GRADE.
Main results
We included 27 randomised trials with 5938 participants. All trials had high risk of bias. We considered that the risk of bias did not impact on the quality of evidence for liver‐related mortality and adverse event outcomes, but it did for virological response. All trials compared peginterferon alpha‐2a or peginterferon alpha‐2b plus ribavirin versus interferon plus ribavirin for participants with chronic hepatitis C. Three trials administered co‐interventions (amantadine hydrochloride 200 mg daily to both intervention groups), and 24 trials were conducted without co‐interventions. The effect observed between the two intervention groups regarding liver‐related morbidity plus all‐cause mortality (5/907 (0.55%) versus 4/882 (0.45%) was imprecise: OR 1.14 ( 95% CI 0.38 to 3.42; five trials; low quality of evidence), as was the risk of adverse events leading to treatment discontinuation (332/2692 (12.3%) versus 409/2176 (18.8%); RR 0.86, 95% CI 0.68 to 1.09; 15 trials; low quality of evidence) or regarding adverse events leading to treatment discontinuation (332/2692 (12.3%) versus 409/2176 (18.8%); RR 0.86, 95% CI 0.66 to 1.12; 17 trials; low quality of evidence). However, peginterferon plus ribavirin versus interferon plus ribavirin significantly increased the risk of neutropenia (332/2202 (15.1%) versus 117/1653 (7.1%); RR 2.15, 95% CI 1.76 to 2.61; 13 trials), thrombocytopenia (65/1113 (5.8%) versus 23/1082 (2.1%); RR 2.63, 95% CI 1.68 to 4.11; 10 trials), arthralgia (517/1740 (29.7%) versus 282/1194 (23.6%); RR 1.19, 95% CI 1.05 to 1.35; four trials), injection site reaction (627/1168 (53.7%) versus 186/649 (28.7%); RR 1.71, 95% CI 1.50 to 1.93; four trials), and nausea (606/1784 (34.0%) versus 354/1239 (28.6%); RR 1.13, 95% CI 1.01 to 1.26; four trials). The most frequent adverse event was fatigue, which occurred in 57% of participants (2024/3608). No significant difference was noted between peginterferon plus ribavirin versus interferon plus ribavirin in terms of fatigue (1177/2062 (57.1%) versus 847/1546 (54.8%); RR 1.01, 95% CI 0.96 to 1.07; 12 trials). No significant differences were reported between the two treatment groups regarding anaemia, headache, rigours, myalgia, pyrexia, weight loss, asthenia, depression, insomnia, irritability, alopecia, pruritus, skin rash, thyroid malfunction, decreased appetite, or diarrhoea. We were unable to identify any data on quality of life. Peginterferon plus ribavirin versus interferon plus ribavirin seemed to significantly increase the number of participants achieving sustained virological response (1673/3300 participants (50.7%) versus 1081/2804 patients (36.7%); RR 1.39, 95% CI 1.25 to 1.56; I2 = 64%; 27 trials; very low quality of evidence). However, the risk of bias in the 13/27 (48.1%) trials reporting on this outcome was high and was considered only 'lower' in the remainder. Because the conventional meta‐analysis did not reach its required information size (n = 14,486 participants), we used trial sequential analysis to control for risks of random errors. Again, in this analysis, the estimated effect was statistically significant in favour of peginterferon. Subgroup analyses according to risk of bias, viral genotype, baseline viral load, past treatment history, and type of intervention yielded similarly significant results favouring peginterferon over interferon on the outcome of sustained virological response.
Authors' conclusions
Peginterferon plus ribavirin versus interferon plus ribavirin seems to significantly increase the proportion of patients with sustained virological response, as well as the risk of certain adverse events. However, we have insufficient evidence to recommend or reject peginterferon plus ribavirin for liver‐related morbidity plus all‐cause mortality compared with interferon plus ribavirin. The clinical consequences of achieved sustained virological response are unknown, as sustained virological response is still an unvalidated surrogate outcome. We found no evidence of the potential benefits on quality of life in patients with achieved sustained virological response. Further high‐quality research is likely to have an important impact on our confidence in the estimate of patient‐relevant outcomes and is likely to change our estimates.There is very low quality evidence that peginterferon plus ribavirin increases the proportion of patients with sustained virological response in comparison with interferon plus ribavirin. There is evidence that it also increases the risk of certain adverse events.
Keywords: Humans; Amantadine; Amantadine/therapeutic use; Antiviral Agents; Antiviral Agents/therapeutic use; Drug Therapy, Combination; Drug Therapy, Combination/methods; Hepatitis C, Chronic; Hepatitis C, Chronic/drug therapy; Hepatitis C, Chronic/mortality; Interferon alpha‐2; Interferon‐alpha; Interferon‐alpha/therapeutic use; Interferons; Interferons/therapeutic use; Polyethylene Glycols; Polyethylene Glycols/therapeutic use; Randomized Controlled Trials as Topic; Recombinant Proteins; Recombinant Proteins/therapeutic use; Ribavirin; Ribavirin/therapeutic use
Plain language summary
Peginterferon plus ribavirin is more effective than interferon plus ribavirin in clearing hepatitis C virus
Importance of the review/background on the condition
Hepatitis C is a disease of the liver caused by the hepatitis C virus. Globally, an estimated 170 million people are chronically infected with the hepatitis C virus. Chronic hepatitis C can cause liver damage in the form of inflammation and scarring of the liver (cirrhosis). Liver damage can lead to liver failure and other complications, including liver cancer. The goal of treatment of chronic hepatitis C is to prevent complications of hepatitis C infection; this could possibly be achieved by clearing the virus from the blood of the patient (sustained virological response, that is, undetectable hepatitis C virus RNA in serum by sensitivity testing six months after the end of treatment). However, we still need to understand whether the sustained virological response outcome induced by antiviral treatment has any association with patient‐relevant and clinically relevant outcomes. A combination of weekly injections of peginterferon and oral ribavirin represents the current standard of care.
Main findings of the review
The review identified and included 27 randomised clinical trials comparing peginterferon plus ribavirin versus interferon plus ribavirin in patients with chronic hepatitis C. All trials had high risk of bias, that is, overestimation of benefits and underestimation of harms. If we disregard bias from lack of blinding and industry support, then 14 trials were considered to have a lower risk of bias. All trials were able to inform on clearing virus from blood six months after the end of treatment (sustained virological response). We could not be certain that peginterferon plus ribavirin has an effect on liver‐related morbidity plus all‐cause mortality when compared with interferon plus ribavirin. Because so few events occurred, we cannot exclude major beneficial or detrimental effects. This review shows that peginterferon plus ribavirin compared with interferon plus ribavirin significantly increases the number of patients with sustained virological response (50.2% compared with 38.5%), but we do not yet know about any patient‐relevant outcomes.
Adverse effects
Peginterferon plus ribavirin compared with interferon plus ribavirin significantly increased the risk of adverse events such as neutropenia (lack of white blood cells in the blood), thrombocytopenia (lack of blood platelets in the blood), arthralgia (joint pain), injection site reaction, and nausea, but adverse events leading to treatment discontinuation remained comparable for both treatments (12.3% versus 18.7%). Data about the influence of treatment on quality of life are insufficient.
Limitations of the review
This effect on virological response seems robust to analysis controlling for the risk of random errors ('play of chance'), but it may be due to the fact that all trials were considered at high risk of bias. Furthermore, we still need to have proof that sustained virological response induced by antiviral treatment has any association with patient‐relevant and clinically relevant outcomes.
Summary of findings
Summary of findings for the main comparison. Peginterferon plus ribavirin versus non‐pegylated interferon plus ribavirin for chronic hepatitis C.
| Peginterferon plus ribavirin versus non‐pegylated interferon plus ribavirin for chronic hepatitis C | ||||||
| Patient or population: patients with chronic hepatitis C. Settings: mainly outpatients. Intervention: peginterferon. Comparison: non‐pegylated. | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Non‐pegylated | Peginterferon | |||||
| Liver‐related morbidity plus all‐cause mortality | Five per 1000 | Six per 1000 (two to 17) | OR 1.14 (0.38 to 3.42) | 1789 (five studies) | ⊕⊕⊝⊝ low1 | |
| Adverse events leading to treatment discontinuation | 207 per 1000 | 178 per 1000 (141 to 226) | RR 0.86 (0.68 to 1.09) | 4571 (15 studies) | ⊕⊕⊝⊝ low2,3 | |
| Sustained virological response | 386 per 1000 | 537 per 1000 (482 to 602) | RR 1.39 (1.25 to 1.56) | 6104 (27 studies) | ⊕⊝⊝⊝4,5 very low | All trials had high risks of bias. Only an unvalidated surrogate outcome. |
| *The basis for the assumed risk (e.g., the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Low due to imprecision and indirectness wide confidence interval. The meta‐analysis included only nine events.
2Low due to imprecision and indirectness.The proportions of observed adverse events differ substantially across trials, and the direction of effect is heterogeneous. However, because the event rate is still relatively low across trials, all of the included trials may be subject to considerable random error, thus explaining the apparent heterogeneity in the direction of estimates. 3The observed treatment effects differ in both direction and magnitude, but most confidence intervals have considerable overlap. Low due to indirectness.
4Sustained virological response does not seem to be a valid surrogate marker for assessing hepatitis C virus treatment efficacy of interferon treatment. Very low due to high risk of bias in all trials and imprecision and indirectness due to surrogate 5Only randomised clinical trials were included.
Background
Description of the condition
Globally, an estimated 170 million people are chronically infected with hepatitis C virus, and three to four million persons are infected each year (WHO 1999). In most patients, hepatitis C infection is asymptomatic in the initial phase. Hepatitis C infection generally is first recognised in the chronic phase (Hodgson 2003). Around 85% of patients who become infected with hepatitis C fail to clear the virus and become chronic carriers. A number of these individuals are reported to develop cirrhosis over a period of approximately 20 to 25 years (Seeff 2002; Seeff 2009). Patients with advanced fibrosis or cirrhosis develop liver complications such as hepatocellular carcinoma at the annual rate of approximately 2% to 4% (Benvegnu 2001; Fattovich 2002). Chronic hepatitis C is the single most common indication for liver transplantation (OPTN 2008). Chronic hepatitis C is expected to become a greater burden during the next decades.
Hepatitis C virus is an enveloped RNA virus that constitutes the genus Hepacivirus within the Flaviviridae family (van Regenmortel 2000; Penin 2004). Hepatitis C virus is divided into six genotypes, which differ from each other by up to 30% in the nucleotide sequence (Rosenberg 2001). Furthermore, hepatitis C virus genotypes differ by geographic region (Davis 1999). Although a genotype does not predict the outcome of the infection, it does predict the likelihood of virological response to treatment and in many cases determines the duration of treatment (Manns 2001; Fried 2002; Hadziyannis 2004).
Description of the intervention
The goal of treatment of chronic hepatitis C is to prevent complications of hepatitis C infection; this is principally sought by eradication of the infection (Ghany 2009). Accordingly, treatment is aimed at achieving a virological response, defined as the absence of hepatitis C virus RNA in serum by sensitive testssix months after the end of treatment (sustained virological response). It is not known whether this outcome bears any relevance to the patient regarding mortality, morbidity, or quality of life (Gluud 2007).
How the intervention might work
Interferons work through complicated cellular mechanisms, leading to a reduction of viral load in patients with chronic hepatitis C. Monotherapy with interferon produces sustained virological response in less than 20% of study participants (Myers 2002). The introduction of combination therapy with interferon plus ribavirin was considered a major advance because of its increased effect on sustained virological response. Combination therapy produces sustained virological response in approximately 40% of previously untreated participants, that is, participants who were previously naive to antiviral drugs (Brok 2009a). A combination of weekly subcutaneous injections of long‐acting peginterferon alpha plus oral ribavirin has achieved the highest overall sustained virological response of 56% of participants (Ghany 2009). This represents the current standard of treatment according to the guidelines of the American Association for the Study of Liver Diseases (Ghany 2009) and the European Association for the Study of the Liver (EASL 2012).
Pegylation involves the addition of polyethylene glycol molecules to the interferon molecule, thus altering metabolism, decreasing renal clearance, and increasing the half‐life of the peginterferon molecule in the circulation, thereby necessitating fewer doses (Reddy 2001). Currently, two licenced products of peginterferon are available: peginterferon alpha‐2a (Pegasys®, Roche), which consists of a 40‐kDa branched pegylated chain linked to the interferon molecule (Bailon 2001), and peginterferon alpha‐2b (Peg‐Intron®, Merck Corporation), which consists of a 12‐kDa linear pegylated chain linked to the interferon molecule (Glue 2000). The two forms of peginterferon differ substantially in terms of chemical and structural characteristics, as well as pharmacokinetic and pharmacodynamic properties (Foster 2004; Awad 2010; Hauser 2014). In the present systematic review, we consider peginterferon alpha‐2a and peginterferon alpha‐2b as a single intervention, but in a subgroup analysis, we analyse them separately.
Why it is important to do this review
Previous reviews, including narrative reviews, meta‐analyses, and health technology assessments, have compared pegylated interferon versus interferon given with or without co‐interventions (Chander 2002; Zaman 2003; Khuroo 2004; Shepherd 2005; Siebert 2005). The overall conclusion of these review authors was that the combination of pegylated interferon plus ribavirin was more efficient than interferon plus ribavirin in obtaining sustained virological response. However, these reviews relied on a sparse number of included trials. Intervention research for hepatitis C is high‐paced, and new trials have emerged since these reviews were completed. This Cochrane systematic review aimed to include and critically assess evidence obtained through extensive searches for randomised clinical trials.
Objectives
To systematically evaluate the benefits and harms of peginterferon plus ribavirin versus interferon plus ribavirin for patients with chronic hepatitis C.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised clinical trials, irrespective of language, publication status, sample size, or year of publication, for assessment of benefits and harms. We also included for assessment of harms quasi‐randomised studies and observational studies that were identified during our searches for randomised trials.
Types of participants
We included patients with chronic hepatitis C. The diagnosis was based on the presence of hepatitis C virus RNA for longer than six months, or the presence of hepatitis C virus RNA plus elevated transaminases in the blood for longer than six months, or histological evidence of chronic hepatitis C. Based on history of previous antiviral treatment, included patients were classified as treatment‐naive (not previously treated with antiviral drugs), relapsers (patients with a transient response to previous treatment), or non‐responders (patients without response to previous treatment). Patients who had undergone liver transplantation and patients with hepatitis B or human immunodeficiency virus coinfection were excluded.
Types of interventions
This review included randomised clinical trials comparing peginterferon alpha‐2a or peginterferon alpha‐2b plus ribavirin versus interferon plus ribavirin for participants with chronic hepatitis C. Trials were included regardless of the type, the dose, or the duration of the interventions. Cointerventions were permitted if they were received by and applied equally to all intervention groups.
Types of outcome measures
Primary outcomes
Liver‐related morbidity plus all‐cause mortality: number of participants who developed cirrhosis, ascites, variceal bleeding, hepatic encephalopathy, or hepatocellular carcinoma, or who died.
-
Adverse events leading to treatment discontinuation.
Numbers and types of adverse events, defined as participants with any untoward medical occurrence not necessarily having a causal relationship to the treatment. We reported separately on adverse events that led to treatment discontinuation and those that did not lead to treatment discontinuation. We defined a serious adverse event according to the guidelines of the International Conference on Harmonisation (ICH‐GCP 1997) as any event that leads to death, is life threatening, requires in‐patient hospitalisation or prolongation of existing hospitalisation, or results in persistent or significant disability, as well as any important medical event that may have jeopardised the participant or required an intervention to prevent it. All other adverse events were considered non‐serious.
Other adverse events: haematological effects, fatigue, flu‐like symptoms, psychiatric symptoms, dermatological symptoms, thyroid malfunction, gastrointestinal symptoms (other than liver related).
Quality of life.
Secondary outcomes
Sustained virological response: number of participants with undetectable hepatitis C virus RNA in serum by sensitive tests six months after the end of treatment.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Hepato‐Biliary Group Controlled Trials Register (Gluud 2013), the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE, Science Citation Index‐Expanded (Royle 2003), and LILACS, using the search strategies and time spans given in Appendix 1. The searches were conducted until September 2013.
Searching other resources
We identified further trials by searching national and topic‐specific databases, bibliographies, conference abstracts, journals, and grey literature. Furthermore, we reviewed the reference lists of the included trials and contacted the principal authors of the identified trials.
Data collection and analysis
We performed the review and meta‐analyses according to the recommendations of The Cochrane Collaboration (Higgins 2011) and the Cochrane Hepato‐Biliary Group Module (Gluud 2013). The analyses were performed using Review Manager 5.2 (RevMan 2012) and Trial Sequential Analysis version 0.9 (CTU 2011; Thorlund 2011).
Selection of studies
We listed the identified trials, and two of the review authors (GH and TA) independently assessed their fulfilment of the inclusion criteria. We listed the excluded trials along with the reasons for exclusion. Disagreements were resolved by discussion and were arbitrated with a third review author (CG).
Data extraction and management
A standardised template or data collection form was used to extract data regarding source identification, eligibility, methods, participants, interventions, outcomes, and results obtained from published reports or by contact with the study authors. Two review authors (GH and TA) extracted all the data independently. Disagreements were resolved by discussion and were arbitrated with a third review author (CG). Any further information required of the original authors was requested by written correspondence, and any relevant information obtained in this manner was included in the review.
Assessment of risk of bias in included studies
Methodological quality was defined as the level of confidence that the design and the report of the randomised clinical trial would restrict bias in the comparison of interventions (Moher 1998). According to empirical evidence (Schulz 1995; Moher 1998; Kjaergard 2001; Wood 2008; Lundh 2012; Savovic 2012; Savovic 2012a), the methodological quality of the trials, hence the risk of bias, was based on the following.
Sequence generation
Low risk of bias: Sequence generation was achieved by using computer random number generation or a random number table. Drawing lots, tossing a coin, shuffling cards, and throwing dice are adequate if performed by an independent person not otherwise involved in the trial.
Uncertain risk of bias: The method of sequence generation was not specified.
High risk of bias: The sequence generation method was not random.
Allocation concealment
Low risk of bias: The participant allocations could not have been foreseen in advance of, or during, enrolment. Allocation was controlled by a central and independent randomisation unit. The allocation sequence was unknown to the investigators (e.g., if the allocation sequence was hidden in sequentially numbered, opaque, and sealed envelopes).
Uncertain risk of bias: The method used to conceal the allocation was not described so that intervention allocations may have been foreseen in advance of, or during, enrolment.
High risk of bias: The allocation sequence was likely to be known to the investigators who assigned the participants.
Blinding of outcome assessors
Low risk of bias: Blinding was performed adequately, or assessment of outcomes was not likely to be influenced by lack of blinding.
Uncertain risk of bias: Information was insufficient to permit assessment of whether blinding was likely to induce bias for the results.
High risk of bias: No blinding or incomplete blinding was performed, and assessment of outcomes was likely to be influenced by lack of blinding.
Incomplete outcome data
Low risk of bias: Missing data were unlikely to make treatment effects depart from plausible values. Sufficient methods, such as multiple imputation, were employed in handling missing data.
Uncertain risk of bias: Information was insufficient to permit assessment of whether missing data in combination with the method used to handle missing data were likely to induce bias for the results.
High risk of bias: The results were likely to be biased as the result of missing data.
Selective outcome reporting
Low risk of bias: All outcomes were predefined and reported, or all clinically relevant and reasonably expected outcomes were reported.
Uncertain risk of bias: It is unclear whether all predefined and clinically relevant and reasonably expected outcomes were reported.
High risk of bias: One or more clinically relevant and reasonably expected outcomes were not reported, and data on these outcomes were likely to have been recorded.
Other sources of bias
Low risk of bias: The trial appears to be free of other components (e.g., academic bias) that could put it at risk of bias.
Uncertain risk of bias: The trial may or may not be free of other components that could put it at risk of bias.
High risk of bias: Other factors in the trial could put it at risk of bias (e.g., authors have conducted trials on the same topic).
The risk of bias of the trials was assessed independently by two review authors, and disagreements were resolved by discussion and were arbitrated with a third review author. Trials with adequate sequence generation and allocation concealment and free of incomplete outcome data and selective outcome reporting were considered trials with lower risk of bias, as we expected all or most trials to be unblinded and to have obtained industry support.
Measures of treatment effect
Dichotomous data
Dichotomous data were expressed as risk ratios (RRs) and risk differences (RDs) with 95% confidence intervals (CIs). Furthermore, the number needed to treat for an additional beneficial outcome was derived from the RD in meta‐analyses in which the 95% CI did not include zero. Rare events (morbidity and mortality) were estimated by using the odds ratio (OR) as a measure of effect.
Dealing with missing data
We planned to perform all analyses according to the intention‐to‐treat method, including all participants, irrespective of compliance or follow‐up. However, we performed analyses according to the intention‐to‐treat method only for dichotomous outcomes. For continuous outcomes, we performed available case analyses and included data only on those whose results were known. Regarding the primary outcome measures, we planned to include participants with incomplete or missing data in the sensitivity analyses by imputing them according to the two scenarios described below (Hollis 1999; Gluud 2013).
'Best‐worst' case scenario analyses: Participants with missing outcomes are considered successes in the experimental group and failures in the control group. The denominator will include all participants in the trial.
'Worst‐best' case scenario analyses: Participants with missing outcomes data are considered failures in the experimental group and successes in the control group. The denominator will include all participants in the trial.
As very few data were available, we decided not to conduct these extreme case scenario analyses. When sufficient data become available in the future, we will conduct such analyses.
Assessment of heterogeneity
Heterogeneity was explored by the Chi2 test, and the quantity of heterogeneity was measured by the I2 statistic (Higgins 2002;Higgins 2011). Sources of heterogeneity were assessed by subgroup analyses and meta‐regression when possible. Subgroup analyses were carried out only when data from at least two trials were available for each subgroup. Meta‐regression was carried out only for meta‐analyses that included more than 10 trials. Whether sensitivity analyses needed to be performed was determined during the review process.
Assessment of reporting biases
Different types of reporting biases (e.g., publication bias, time lag bias, outcome reporting bias) were handled according to the recommendations of The Cochrane Collaboration (Higgins 2011). For dichotomous outcomes with intervention effects measured as odds ratios, the arcsine test proposed by Rücker 2008 was used to test for funnel plot asymmetry. Nevertheless, asymmetrical funnel plots are not necessarily caused by publication bias, and publication bias does not necessarily cause asymmetry in a funnel plot (Egger 1997).
Data synthesis
Meta‐analysis For all analyses, we used both random‐effects (DerSimonian 1986) and fixed‐effect models (DeMets 1987). Because of underlying assumptive differences, results from the random‐effects model and from the fixed‐effect model may differ to a non‐ignorable extent. In case such discrepancies were observed, P values were ignored, and results were interpreted according to the implications of the subgroup and heterogeneity analyses according to confidence intervals of the two models. Trial sequential analysis Random errors may play an important role in the evaluation of cumulative meta‐analyses as the result of sparse data and multiplicity from repetitive testing of accumulating data. To assess the reliability of inferences from our meta‐analysis on sustained virological response, we calculated the diversity‐adjusted required information size (DARIS). We defined DARIS as the required sample size for the meta‐analysis to detect a 10% relative risk reduction in sustained virological response, assuming an average outcome proportion of 50% in the control group, a diversity observed in the meta‐analysis, and statistical error levels of alpha = 5% and beta = 10% (90% power). Meta‐analyses conducted before they surpassed the DARIS are considered analogous to interim analyses in a single randomised trial, and thus they necessitate adjustment of the threshold for statistical significance to maintain the predetermined maximum risk of obtaining a false positive (set to alpha = 5% in our analysis). Therefore, we substituted the conventional 5% threshold for statistical significance with those of Lan‐DeMets trial sequential monitoring boundaries (Bangalore 2008; Brok 2008; Wetterslev 2008; Brok 2009; Thorlund 2009, Wetterslev 2009; Thorlund 2010). To minimise the risk of random errors, we used trial sequential analysis (CTU 2011; Thorlund 2011). On the basis of the required information size and the risk for type I (5%) and type II (10% or 20%) errors, trial sequential monitoring boundaries were constructed (Wetterslev 2008; CTU 2011; Thorlund 2011). These boundaries determine the statistical inference that one may draw regarding the cumulative meta‐analysis that has not reached the required information size. If the cumulative Z‐score crosses a trial sequential monitoring boundary before the required information size is reached in a cumulative meta‐analysis, firm evidence may have been established, and further trials may be superfluous, provided that systematic errors can be excluded. On the other hand, if the monitoring boundaries are not surpassed, it is most probably necessary to continue doing further trials to detect or reject a certain intervention effect. We used as default a type I error of 5%, a type II error of 10%, and adjusted information size for heterogeneity with diversity, unless otherwise stated (Wetterslev 2008; Wetterslev 2009; CTU 2011; Thorlund 2011). Posthoc, we also challenged the trial sequential analysis on sustained virological response by a type I error of 1%.
Subgroup analysis and investigation of heterogeneity
The following subgroup analyses were considered and performed when feasible.
Risk of bias: trials assessed to have low risk of bias compared to trials with high risk of bias.
Participants: trials with treatment‐naive participants compared to trials with relapsers or non‐responders.
Genotype: comparisons of trials with participants infected with different hepatitis C virus genotypes.
Baseline viral load: trials assessed as having high or low risk of viral load on the basis of 800,000 IU (˜ four million copies/mL) threshold.
Type of peginterferon: trials with peginterferon alpha‐2a compared to trials with peginterferon alpha‐2b.
We performed a test of interaction between subgroups within each of the five categories. We performed tests of interaction only between subgroups that both included at least three trials.
Sensitivity analysis
Suitable sensitivity analyses were identified during the review process. For example, if zero‐event trials occurred, we employed a number of different continuity corrections according to the sensitivity analysis proposed by Bradburn 2006 using the TSA programme (CTU 2011; Thorlund 2011). We also carried out a sensitivity analysis from which we excluded trials that provided triple therapy with amantadine.
Summary of findings table
To minimise wrong interpretations of our findings and recommendations, we planned to rate the available evidence for all outcomes following the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) guidelines in order to prepare a Summary of Findings (SoFs) table (Guyatt 2008). A SoFs table consists of three parts: information about the review, a summary of the statistical results, and the grade of the quality of evidence. The quality assessment comprises three parts: the number of studies, the types of studies (randomised or observational), and the factors that affect the quality of the evidence (see below).
Factors that affect the quality of the evidence
| Decrease quality | Increase quality |
| Risk of bias | Large magnitude of effect |
| Inconsistency of results | Demonstrated effect reduced by all plausible confounding |
| Indirectness of evidence | Dose‐response gradient |
| Imprecision | |
| Publication bias |
Results
Description of studies
Results of the search
We identified a total of 8089 references through electronic searches until September 2013. The Cochrane Hepato‐Biliary Group Controlled Trials Register identified 923 references. We excluded 2459 duplicates and 3346 clearly irrelevant references by reading abstracts. Accordingly, 2284 references were retrieved for further assessment. We excluded 2225 references because they were not randomised clinical trials or because interventions or participants did not meet our inclusion criteria. Fifty‐nine references describing a total of 27 randomised clinical trials fulfilled our inclusion criteria (see the Characteristics of included studies table) (Manns 2001; Cariti 2002; Fried 2002; Hinrichsen 2002; Esmat 2003; Shobokshi 2003; Thakeb 2003; Al‐Faleh 2004; Bruno 2004; Fargion 2004; Izumi 2004; Derbala 2005; Dollinger 2005; Lee 2005; Mangia 2005; Napoli 2005; PRETTY 2005; Scotto 2005; Tsubota 2005; Derbala 2006; Wakil 2006; Rahman 2007a; Rahman 2007b; Sjögren 2007; Horsmans 2008; Roffi 2008; Nevens 2010). Accordingly, several of the trials were published multiple times. Seventeen trials were published as full‐paper articles, and 10 trials were published in abstract form only.
Included studies
Participants
A total of 5938 participants were randomly assigned in the 27 trials. The number of participants in each trial ranged from 40 to 1530. Twenty‐three trials included treatment‐naive participants, and four trials included non‐responders or relapsers. In 10 trials, all participants were infected with hepatitis C virus genotype one. In two trials, all participants were infected with genotype two or three. In seven trials, all participants were infected with genotype four. In eight trials, participants infected with different genotypes were included.
Experimental interventions
The type of peginterferon was alpha‐2a (nine trials) or alpha‐2b (18 trials).
The dose of peginterferon alpha‐2a was 180 μg/wk (Cariti 2002; Fried 2002; Shobokshi 2003; Thakeb 2003; Fargion 2004; Mangia 2005; PRETTY 2005; Derbala 2006; Nevens 2010).
The dose of peginterferon alpha‐2b was 1.0 μg/kg/wk (Hinrichsen 2002; Esmat 2003; Al‐Faleh 2004) or 1.5 μg/kg/wk (Manns 2001; Izumi 2004; Derbala 2005; Dollinger 2005; Lee 2005; Napoli 2005; Scotto 2005; Tsubota 2005; Wakil 2006; Rahman 2007a; Rahman 2007b; Sjögren 2007). In the Manns 2001 trial, a third intervention group was given peginterferon alpha‐2b 1.5 μg/kg/wk for four weeks, followed by 0.5 μg/kg/wk for an additional 44 weeks. In the Roffi 2008 trial, participants were given peginterferon alpha‐2b 1.0 μg/kg/wk for four weeks, followed by 0.5 μg/kg/wk for an additional two weeks.
Control interventions
The type of interferon was alpha‐2a (eight trials), alpha‐2b (14 trials), consensus interferon (four trials), or leucocyte interferon‐alpha (one trial).
The dose of interferon alpha‐2a was 3 MU (Thakeb 2003; Mangia 2005;Derbala 2006), 4.5 MU (Shobokshi 2003), or 6 MU (Cariti 2002; PRETTY 2005), given thrice weekly. In the Fargion 2004 trial, participants were given interferon alpha‐2a 6 MU daily for four weeks, then 3 MU daily for an additional 20 weeks, and then 3 MU thrice weekly for an additional 24 weeks. In the Nevens 2010 trial, participants were given interferon alpha‐2a at a dose of 6 MU for eight weeks, and then 3 MU for an additional 40 weeks.
The dose of interferon alpha‐2b was 3 MU (Manns 2001; Fried 2002; Hinrichsen 2002; Esmat 2003; Al‐Faleh 2004; Lee 2005; Scotto 2005; Wakil 2006), 5 MU (Wakil 2006), or 6 MU (Bruno 2004; Derbala 2005; Scotto 2005), given thrice weekly. In one trial (Izumi 2004), interferon alpha‐2b was given daily at a dose of 3 MU for the first two weeks, and then thrice weekly for an additional 46 weeks. In the Tsubota 2005 trial, interferon alpha‐2b was given daily at a dose of 6 MU for the first two weeks, and then thrice weekly for an additional 46 weeks. In the Bruno 2004 trial, peginterferon alpha‐2b 100 µg was given to participants weighing 65 kg or more, and 80 µg to those weighing less than 65 kg, for the first eight weeks, followed by a fixed dose of 50 µg for the next 40 weeks.
The dose of consensus interferon was 9 µg (Rahman 2007a; Rahman 2007b) or 15 µg (Sjögren 2007) for 48 weeks. In the Dollinger 2005 trial, consensus interferon was given at a dose of 18 µg/d for six weeks followed by 9 µg/d for 42 weeks.
In the Rahman 2007a trial, consensus interferon was given at a dose of 27 to 18 µg once a day for 12 weeks followed by 9 µg once a day for 36 weeks.The dose of leucocyte interferon‐alpha was 6 MIU daily (Napoli 2005).
Two trials (Shobokshi 2003; Horsmans 2008) included three intervention groups. In the first trial (Shobokshi 2003), group one was given peginterferon alpha‐2a 180 µg plus ribavirin 800 mg for 48 weeks (n = 60); group two was given peginterferon alpha‐2a 180 µg (n = 60); and group three was given interferon alpha‐2a 4.5 MU plus ribavirin 800 mg for 48 weeks (n = 60). In the second trial (Horsmans 2008), group one was given daily interferon alpha‐2b at a dose of 4 MIU for participants weighing more than 65 kg, and 0.06 MIU/kg for those weighing 65 kg or less; group two was given interferon alpha‐2b three times a week at a dose of 3 MIU; and group three was given peginterferon alpha‐2b at a dose of 100 mcg/wk for participants weighing more than 65 kg, and 1.5 mcg/kg/d for participants weighing 65 kg or less. Participants were followed up for 24 weeks after the end of treatment.
Cointerventions in both intervention groups
The dose of ribavirin was 600 mg, 800 mg, 1000 mg, or 1200 mg daily, based on body weight. Three trials also administered amantadine hydrochloride 200 mg daily to both intervention groups (Fargion 2004; Mangia 2005; PRETTY 2005).
Excluded studies
Seven publications were excluded for the reasons shown in the Characteristics of excluded studies table (APRICOT 2004; Asahina 2004; Gromova 2004; Laguno 2004; RIBAVIC 2004; ACTG 2005; Ali 2010).
Risk of bias in included studies
The risk of bias was unclearly reported in a considerable number of included trials, hence giving them a high risk of bias (Figure 1; Figure 2). Fourteen trials reported adequate sequence generation (generation of the allocation sequence ) (e.g., computer‐generated random numbers, table of random numbers, minimisation). Fourteen trials used adequate allocation concealment (e.g., central independent unit, sealed opaque envelopes). None of the trials were blinded. It is unclear to what extent the outcome assessors or the participants were blinded; therefore, a risk of bias might be present in the registration of subjective outcome measures (e.g., diagnosis of complications, adverse events). Only one trial had adequate blinding for the outcome assessors for sustained virological response (Sjögren 2007). Nineteen trials addressed incomplete outcome data adequately. Protocols were not available for any of the included trials, but most trials reported on the primary outcomes of our review. Several trials had possible vested interest bias (Manns 2001; Fried 2002; Shobokshi 2003; Al‐Faleh 2004; Bruno 2004; Dollinger 2005; Lee 2005; Mangia 2005; Horsmans 2008), and in the remainder, the risk of vested interest bias was unclear. The risk of bias was high in all of the trials from one or more domains.
1.
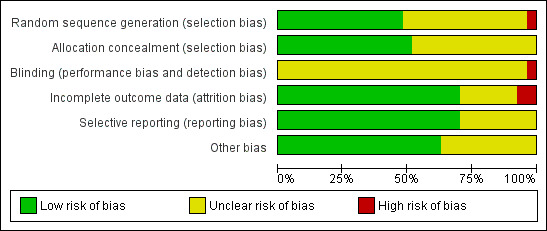
Methodological quality graph: review authors' judgements about all methodological quality items presented as percentages across all included studies.
2.
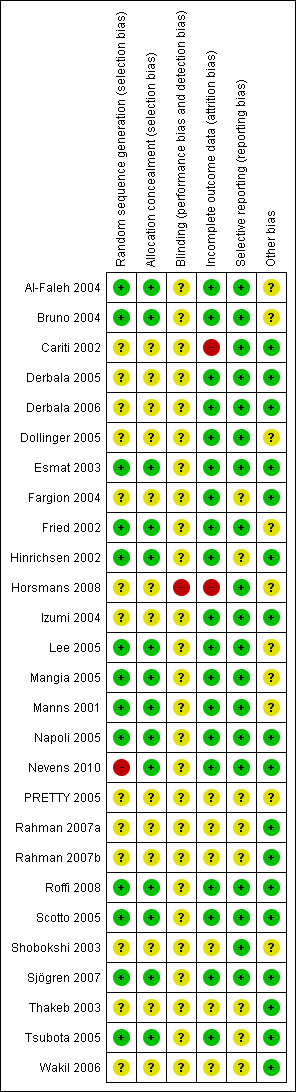
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Disregarding the risk of bias from lack of blinding and vested interests, we considered 14/27 trials (51.9%) as having a lower risk of bias according to the following domains: generation of the allocation sequence, allocation concealment, incomplete outcome reporting, and selective outcome reporting.
Effects of interventions
See: Table 1
Liver‐related morbidity plus all‐cause mortality
Four deaths (suicide (suspected drug overdose), ruptured oesophageal varices, traffic‐related, and unexplained) on peginterferon plus ribavirin versus three deaths (following surgery for colon cancer, hypertensive heart disease, and brain tumour) on interferon plus ribavirin were reported (Analysis 1.1). Two participants developed hepatocellular carcinoma, one on each intervention. No significant difference in liver‐related morbidity or all‐cause mortality was noted between participants receiving peginterferon plus ribavirin versus interferon plus ribavirin (Peto OR 1.14, 95% CI 0.38 to 3.42; five trials).
1.1. Analysis.
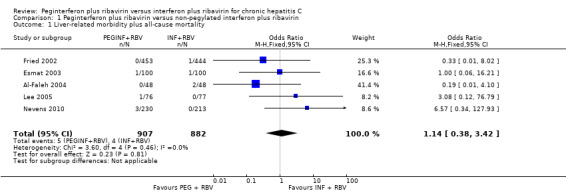
Comparison 1 Peginterferon plus ribavirin versus non‐pegylated interferon plus ribavirin, Outcome 1 Liver‐related morbidity plus all‐cause mortality.
Adverse events
Data from 17 trials yielded a non‐significant difference regarding adverse events leading to treatment discontinuation of peginterferon plus ribavirin when compared with interferon plus ribavirin (332/2692 (12.3%) versus 409/2176 (18.8%); RR 0.86, 95% CI 0.66 to 1.12; 17 trials). When RR was used as the association measure of intervention effect, the Cochrane homogeneity test statistic yielded a P value of 0.003, and the heterogeneity was I2 = 56% (Analysis 1.2). Funnel plot visual inspection did not reveal significant evidence of publication bias (Figure 3). Peginterferon plus ribavirin compared with interferon plus ribavirin significantly increased the risk of neutropenia (RR 2.15, 95% CI 1.76 to 2.61; 13 trials) (Analysis 2.1), thrombocytopenia (RR 2.63, 95% CI 1.68 to 4.11; 10 trials) (Analysis 2.1), arthralgia (RR 1.19, 95% CI 1.05 to 1.35; four trials) (Analysis 2.4), injection site reaction (RR 1.71, 95% CI 1.50 to 1.93; four trials) (Analysis 2.4; Figure 1), or nausea (RR 1.13, 95% CI 1.01 to 1.26; four trials) (Analysis 2.6). The most frequent adverse event was fatigue, which overall occurred in 57% (2024/3608). No significant difference was seen between the effects of peginterferon plus ribavirin versus interferon plus ribavirin on fatigue (RR 1.01, 95% CI 0.96 to 1.07; 10 trials) (Analysis 2.2). No significant differences were noted between the two interventions regarding anaemia (Analysis 2.1), headache, rigours, myalgia, pyrexia, weight loss, asthenia (Analysis 2.4), depression, insomnia, irritability (Analysis 2.3), alopecia, pruritus, skin rash (Analysis 2.4), thyroid malfunction (Analysis 2.5), or regarding decreased appetite and diarrhoea (Analysis 2.6).
1.2. Analysis.
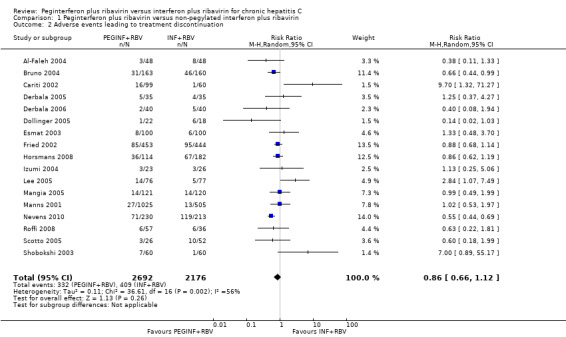
Comparison 1 Peginterferon plus ribavirin versus non‐pegylated interferon plus ribavirin, Outcome 2 Adverse events leading to treatment discontinuation.
3.
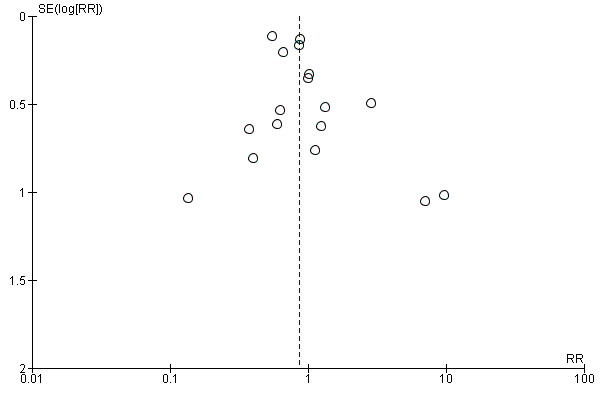
Funnel plot of comparison: peginterferon plus ribavirin versus non‐pegylated interferon plus ribavirin, outcome: 1.2 Adverse events leading to treatment discontinuation.
2.1. Analysis.
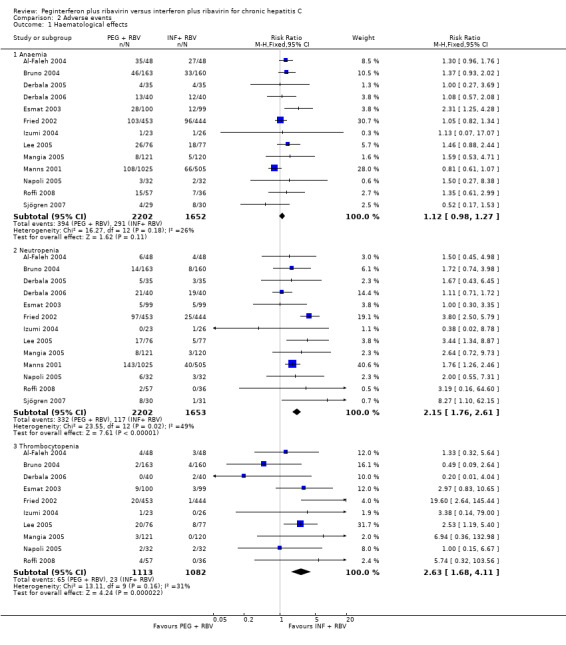
Comparison 2 Adverse events, Outcome 1 Haematological effects.
2.4. Analysis.
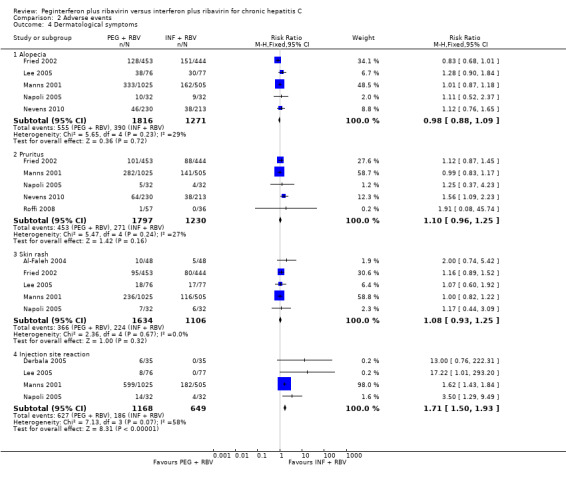
Comparison 2 Adverse events, Outcome 4 Dermatological symptoms.
2.6. Analysis.
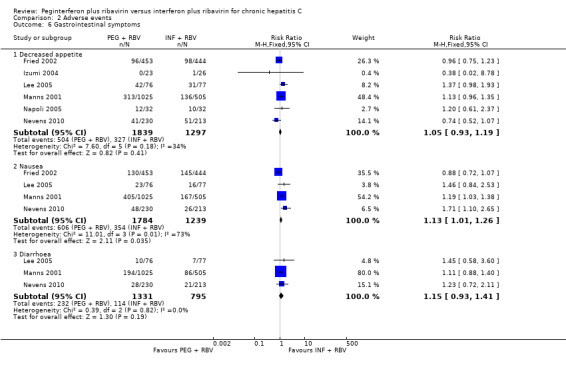
Comparison 2 Adverse events, Outcome 6 Gastrointestinal symptoms.
2.2. Analysis.
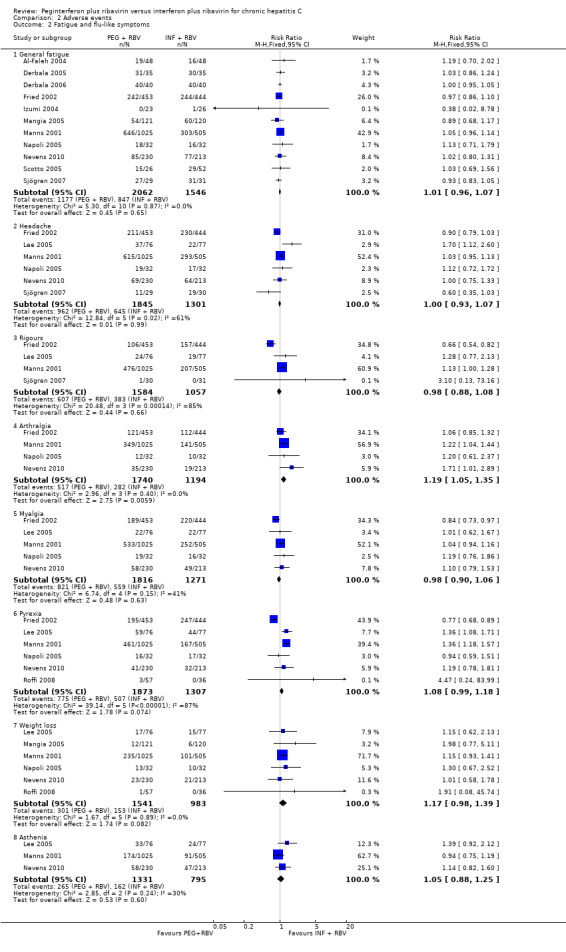
Comparison 2 Adverse events, Outcome 2 Fatigue and flu‐like symptoms.
2.3. Analysis.
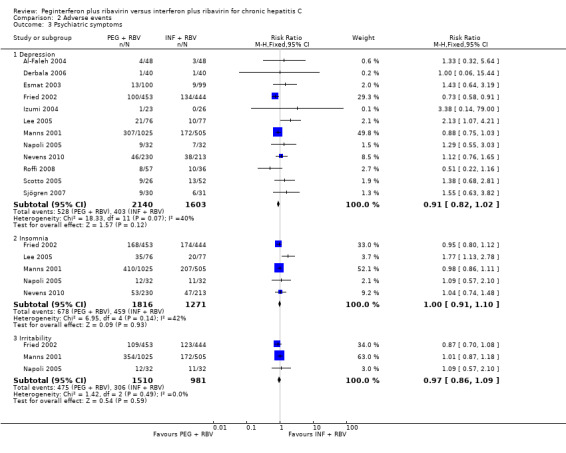
Comparison 2 Adverse events, Outcome 3 Psychiatric symptoms.
2.5. Analysis.
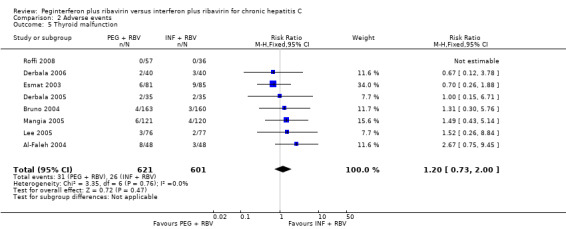
Comparison 2 Adverse events, Outcome 5 Thyroid malfunction.
Quality of life
Only one trial reported quality of life in the Methods section (Hinrichsen 2002). This trial is published only as an abstract, and we could not find the data in the Results section. We contacted the study authors to ask for further information, but no answer has been received.
Sustained virological response
Peginterferon plus ribavirin seems to significantly increase the number of participants achieving sustained virological response compared with interferon plus ribavirin (1673/3300 (50.7%) versus 1081/2804 (38.6%); RR 1.39, 95% CI 1. 25 to 1.56; I2 = 64%; 27 trials) (Analysis 1.3; Figure 4). When RR was used as the measure of effect, the Cochran homogeneity test statistic yielded a P value less than 0.00001 and the heterogeneity was I2 = 64%. The estimated number needed to treat for an additional beneficial outcome to achieve an extra participant with sustained virological response is seven participants (95% CI 5 to 10 participants) with peginterferon plus ribavirin versus interferon plus ribavirin. Funnel plot visual inspection did not reveal significant risk of publication bias (Figure 5).
1.3. Analysis.
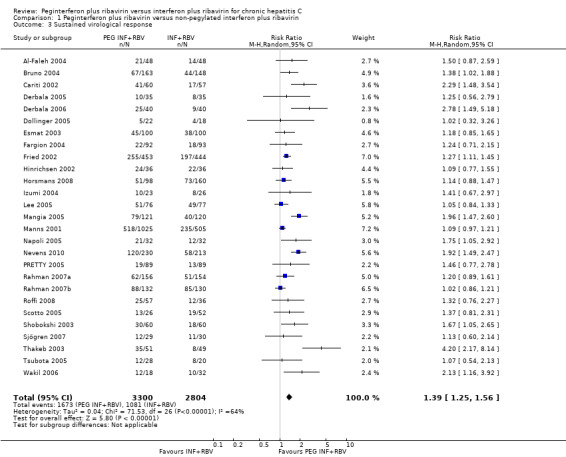
Comparison 1 Peginterferon plus ribavirin versus non‐pegylated interferon plus ribavirin, Outcome 3 Sustained virological response.
4.
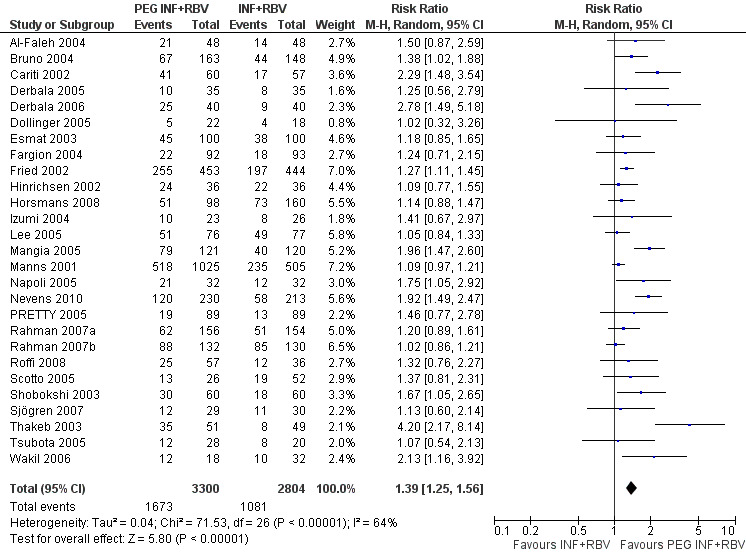
Forest plot of comparison: pegylated interferon plus ribavirin versus interferon plus ribavirin, outcome: 1.1 Sustained virological response.
5.
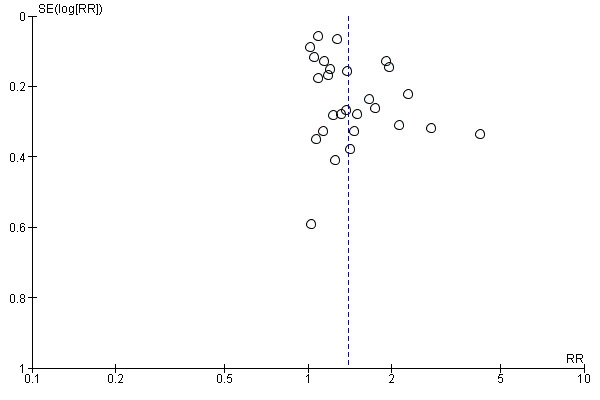
Funnel plot of comparison: pegylated interferon plus ribavirin versus interferon plus ribavirin, outcome: 1.1 Sustained virological response.
Because this meta‐analysis did not reach its required information size of 14,486 participants based on the assumption of a maximum type I error of 5%, we used a trial sequential analysis to assess the statistical significance. Based on the assumption of a maximum type I error of 1%, the required information size was 20,513 participants. Again, the estimated effects were statistically significant in favour of peginterferon plus ribavirin (Figure 6; Figure 7).
6.
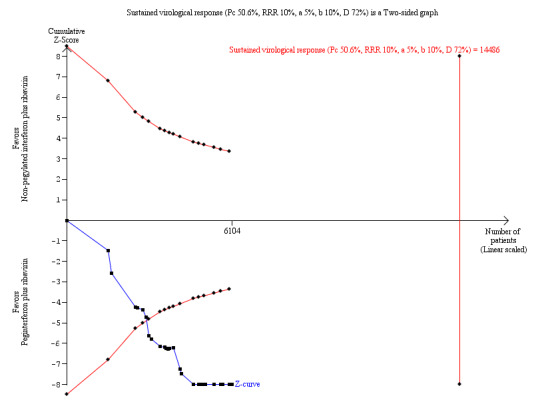
Trial sequential analysis (TSA): pegylated interferon plus ribavirin versus interferon plus ribavirin ‐ sustained virological response. Lan‐DeMets statistical monitoring boundaries for assessing statistical significance regarding sustained virological response to pegylated interferon plus ribavirin versus interferon plus ribavirin. The diversity‐adjusted required information size of n = 14,486 was calculated based on an event proportion of 50.6% of participants in the interferon‐treated group (Pc) with a risk ratio (RR) reduction of 10% in pegylated interferon group; an alpha (a, type I error) of 5%, a beta (b, type II error) of 10%, and the observed diversity D = 72%. The solid blue curve presents the cumulative meta‐analysis test Z‐score and the inward sloping red curves present the adjusted threshold for statistical significance according to the two‐sided Lan‐DeMets trial sequential boundaries. The cumulative Z‐score crosses the boundaries for superiority, and this corresponds with superiority of pegylated interferon.
7.
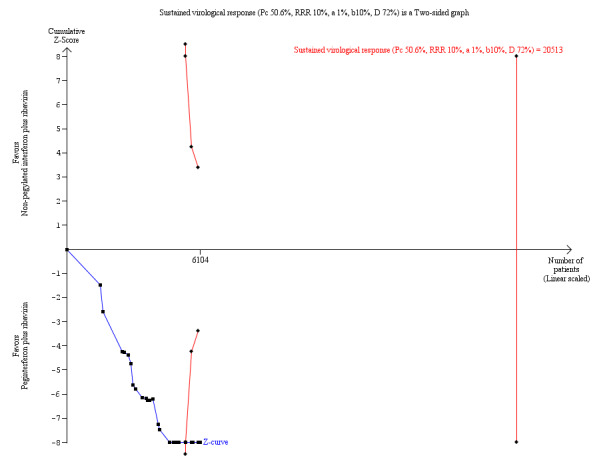
Trial sequential analysis (TSA): pegylated interferon plus ribavirin versus interferon plus ribavirin ‐ sustained virological response. Lan‐DeMets statistical monitoring boundaries for assessing statistical significance regarding sustained virological response to pegylated interferon plus ribavirin versus interferon plus ribavirin. The diversity‐adjusted required information size of n = 20,513 was calculated based on an event proportion of 50.6% of participants in the interferon‐treated group (Pc) with a risk ratio (RR) reduction of 10% in the pegylated interferon group; an alpha (a, type I error) of 1%, a beta (b, type II error) of 10%, and the observed diversity D = 72%. The solid blue curve presents the cumulative meta‐analysis test Z‐score and the inward sloping red curves present the adjusted threshold for statistical significance according to the two‐sided Lan‐DeMets trial sequential monitoring boundaries. The cumulative Z‐score crosses the boundaries for superiority, and this corresponds with the superiority of pegylated interferon.
Subgroup analyses showed pronounced differences in comparative treatment effects according to the genotype of the virus (Analysis 3.3). Data from 16 trials (Manns 2001; Cariti 2002; Fried 2002; Bruno 2004; Izumi 2004; Dollinger 2005; Lee 2005; Mangia 2005; Napoli 2005; PRETTY 2005; Scotto 2005; Tsubota 2005; Rahman 2007a; Sjögren 2007; Roffi 2008; Nevens 2010) for genotype one yielded RR 1.47, 95% CI 1.27 to 1.70, when the random‐effects model was used. Data from nine trials (Manns 2001; Fried 2002; Hinrichsen 2002; Fargion 2004; Mangia 2005; Napoli 2005; Rahman 2007b; Horsmans 2008; Roffi 2008) for genotype two or three yielded RR 1.10, 95% CI 1.03 to 1.19, when the random‐effects model was used. Data from nine trials (Manns 2001; Fried 2002; Esmat 2003; Shobokshi 2003; Thakeb 2003; Al‐Faleh 2004; Derbala 2005; Derbala 2006; Wakil 2006) for genotype four yielded RR 1.76, 95% CI 1.30 to 2.39, when the random‐effects model was used. These differences were substantiated by tests of interaction that yielded statistically significant differences between genotype one and genotype two or three (P value < 0.002) and between genotype two or three and genotype four (P value < 0.029).
3.3. Analysis.
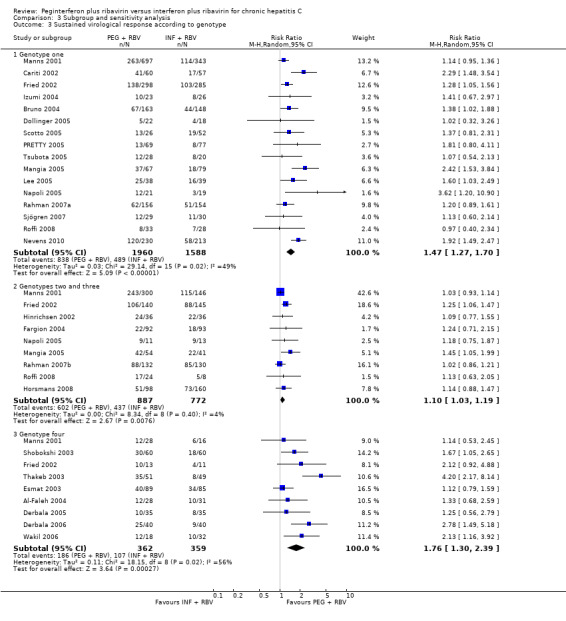
Comparison 3 Subgroup and sensitivity analysis, Outcome 3 Sustained virological response according to genotype.
Subgroup analyses showed a pronounced difference in comparative treatment effects by type of peginterferon (Analysis 3.5; Analysis 3.6). Data from nine trials (Cariti 2002; Fried 2002; Shobokshi 2003; Thakeb 2003; Fargion 2004; Mangia 2005; PRETTY 2005; Derbala 2006; Nevens 2010) assessing peginterferon alpha‐2a yielded RR 1.85 (95% CI 1.46 to 2.35) by using the random‐effects model. Data from 18 trials (Manns 2001; Hinrichsen 2002; Esmat 2003; Al‐Faleh 2004; Bruno 2004; Izumi 2004; Derbala 2005; Dollinger 2005; Lee 2005; Napoli 2005; Scotto 2005; Tsubota 2005; Wakil 2006; Rahman 2007a; Rahman 2007b; Sjögren 2007; Horsmans 2008; Roffi 2008) assessing peginterferon alpha‐2b yielded RR 1.14, 95% CI 1.06 to 1.22, when the random‐effects model was used. These differences were substantiated by tests of interaction that yielded statistically significant differences between peginterferon alpha‐2a plus ribavirin and peginterferon alpha‐2b plus ribavirin (P < 0.001).
3.5. Analysis.
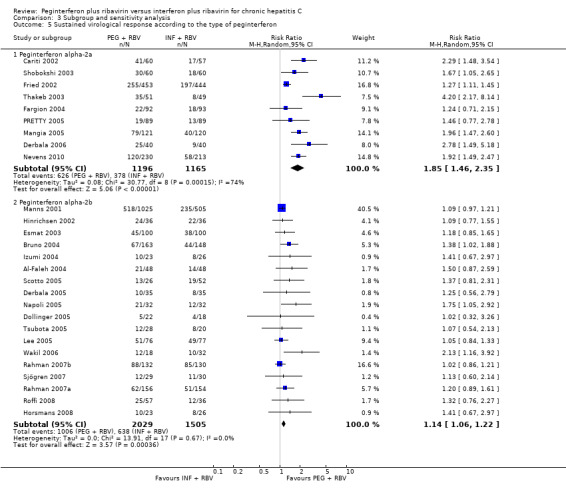
Comparison 3 Subgroup and sensitivity analysis, Outcome 5 Sustained virological response according to the type of peginterferon.
3.6. Analysis.
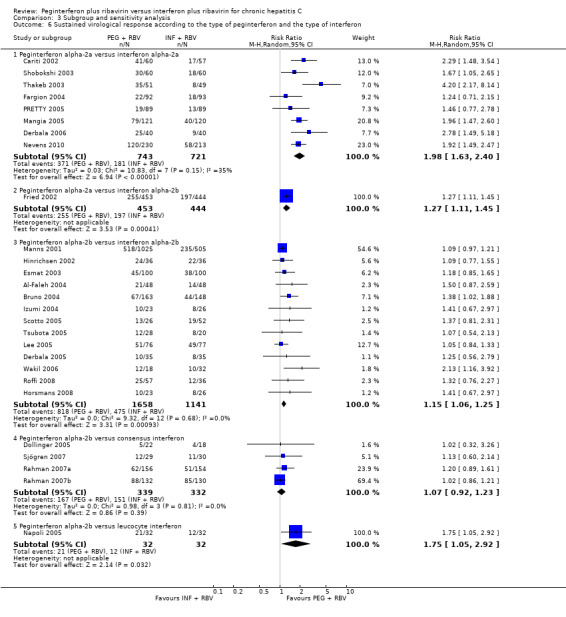
Comparison 3 Subgroup and sensitivity analysis, Outcome 6 Sustained virological response according to the type of peginterferon and the type of interferon.
Subgroup analyses on risk of bias (Analysis 3.1), treatment history (Analysis 3.2), and baseline viral load (Analysis 3.4) using RR as the measure of effect yielded similar results favouring peginterferon over interferon. Tests of interactions of the latter subgroup analyses were non‐significant.
3.1. Analysis.
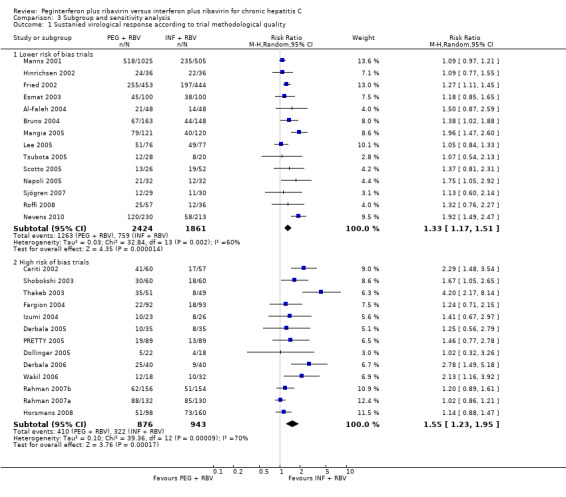
Comparison 3 Subgroup and sensitivity analysis, Outcome 1 Sustanied virological response according to trial methodological quality.
3.2. Analysis.
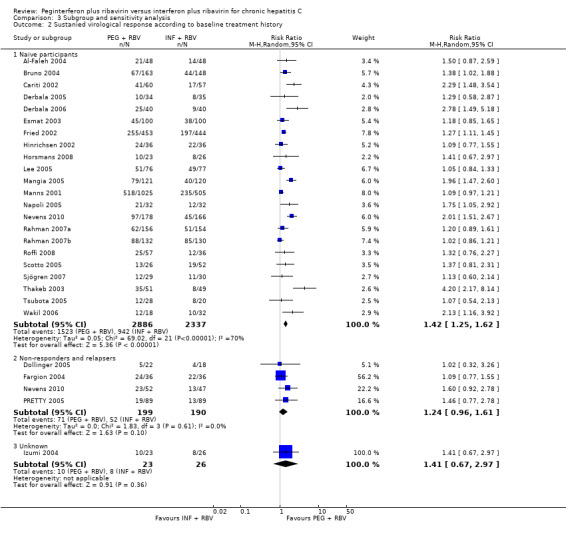
Comparison 3 Subgroup and sensitivity analysis, Outcome 2 Sustanied virological response according to baseline treatment history.
3.4. Analysis.
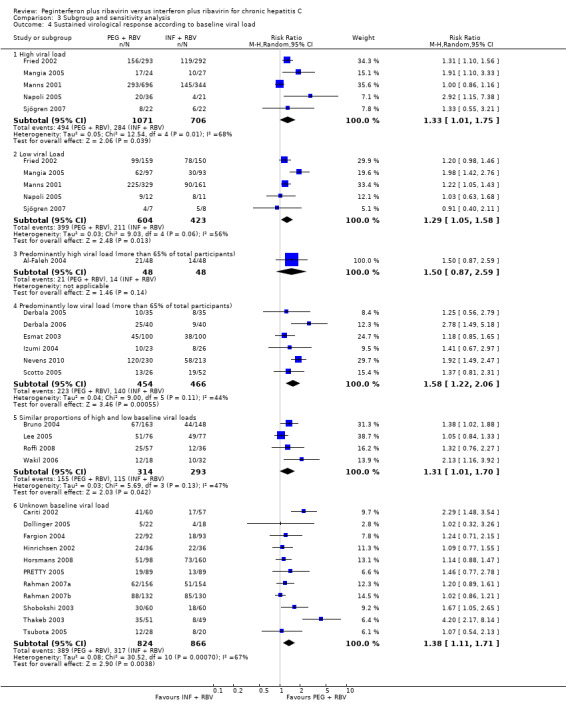
Comparison 3 Subgroup and sensitivity analysis, Outcome 4 Sustained virological response according to baseline viral load.
A sensitivity analysis from which we excluded the three trials in which amantadine was used as triple therapy in both the peginterferon plus ribavirin group and the interferon plus ribavirin group yielded similar significant results favouring peginterferon (Analysis 3.7).
3.7. Analysis.
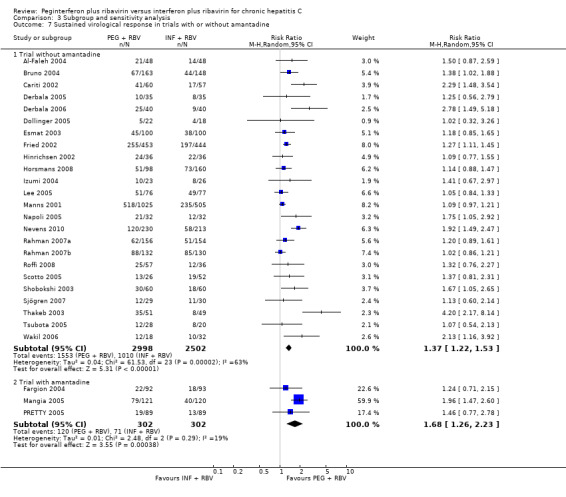
Comparison 3 Subgroup and sensitivity analysis, Outcome 7 Sustained virological response in trials with or without amantadine.
Summary of findings table
We prepared a Summary of Findings (SoFs) table for all outcomes but one, ie, quality of life (Table 1). The SoFs table presents that we can have low confidence in the current evidence on harms measured as morbidity plus mortality and adverse events leading to treatment discontinuation. The meta‐analysis on morbidity plus mortality showed a very serious imprecision because only nine events were included in the meta‐analysis with five trials. In the meta‐analysis on adverse events, serious discrepancies across trials and lack of precision were evident. The proportions of observed adverse events differ substantially across the trials, and the direction of effect is heterogeneous. However, because the event proportion is still relatively low across the trials, all included trials may be subject to a considerable risk of random errors, thus explaining the apparent heterogeneity in direction of estimates. The observed treatment effects differ in magnitude as well, but most confidence intervals show considerable overlap. In addition, we can have a very low confidence in the current evidence on treatment benefits measured as sustained virological response.
Discussion
Summary of main results
A major obstacle to treatment and patient compliance is the association of combined antiviral therapy with frequent and sometimes serious adverse events. Timely recognition of adverse events has a crucial role in the continuation of antiviral therapy with a hope for successful virological treatment results. In clinical trials, approximately 10% to 15% of participants discontinue peginterferon and ribavirin therapy because of adverse effects; in clinical practice, the rate of treatment discontinuation has been reported as substantially higher (Sulkowski 2011). The adverse effects of combined antiviral therapy are numerous and can be observed in many organ systems. The most common adverse effects are haematological, dermatological, neurological, immunological, gastrointestinal, pulmonary, cardiovascular, and ocular (Sulkowski 2011). We are lacking data on direct comparisons of different types of interferons. Among the most frequent adverse effects is myelosuppression. Neutrophil count decreases by an average of 34% (Soza 2002), and mean platelet drop is around 42% (Roomer 2010). Regarding haemoglobin levels, more than 50% of participants experienced a decrease in haemoglobin to around 30 g/L. Women are more prone to experiencing a haemoglobin level less than 100 g/L (Sulkowski 2004). Many of those adverse effects usually require only adjustment of antiviral therapy. In some patients, application of growth factors is needed because of haematological disturbances. Psychiatric disturbances and mood alterations associated with long‐term interferon therapy are well described. In some trials (Constant 2005), mood alterations occurred in 32% of participants, and significant depressive symptoms were noted in 21% to 58% of participants (Raison 2005). Retinopathy associated with pegylated interferon therapy has been reported in 21% of participants, but the vast majority of participants recovered without cessation of treatment (Lim 2010). Among the rare adverse events that could be linked to combined antiviral therapy are some potentially fatal disorders that are usually reported as case reports. Pulmonary complications such as pneumonitis and pulmonary hypertension are rare but require early detection and premature cessation of antiviral therapy (Kumar 2002; Dhillon 2010; Slavenburg 2010). In one trial, mortality secondary to pneumonitis was seen exclusively with peginterferon alpha‐2b (Slavenburg 2010).
In this systematic review, we have summarised the available evidence from randomised clinical trials comparing peginterferon alpha versus interferon alpha, both given in combination with ribavirin. Because of the high risk of bias in the trials, our results seem to suggest that the combination of peginterferon plus ribavirin is associated with a moderate or low beneficial effect on sustained virological response when compared with interferon plus ribavirin. Our results show that evidence on liver‐related morbidity plus all‐cause mortality is sparse, and that the meta‐analysis is underpowered to detect any difference in risk of liver‐related morbidity plus all‐cause mortality. However, regarding adverse events, the two regimens seem to differ significantly, with interferon plus ribavirin causing less harm than peginterferon plus ribavirin.
Both peginterferon alpha‐2a and peginterferon alpha‐2b plus ribavirin were superior in terms of sustained virological response when compared with interferon plus ribavirin for participants with chronic hepatitis. Our subgroup analyses demonstrated that peginterferon alpha‐2a was associated with a significantly higher sustained virological response than peginterferon alpha‐2b versus interferon. This indirect observation is in harmony with our previous observations from head‐to‐head trials that peginterferon alpha‐2a leads to sustained virological response in a greater number of participants than is seen with peginterferon alpha‐2b (Awad 2010; Hauser 2014).
Overall completeness and applicability of evidence
The Summary of Findings table that we have prepared reveals that, in generalwe can have only low confidence in the current evidence on harms measured as liver‐related morbidity plus all‐cause mortality, and adverse events or adverse events leading to treatment discontinuation. In addition, we can have very low confidence in the current evidence on treatment benefits measured as sustained virological response (Table 1). All trials had high risks of bias. If we disregarded bias due to lack of blinding and due to vested interests, about half of the trials could be considered trials with a lower risk of bias. Our sensitivity analyses, however, showed no important influence of bias risk on our estimates of intervention effects. This may be due to the fact that we were unable to identify trials with a lower risk of bias. In our study, trials that adequately reported on the methodology of trial performance are large trials that dominate the pooled estimates of effect. Therefore, it is less likely that the pooled estimates are biased. In the meta‐analysis for sustained virological response, no serious inconsistencies were seen across trials, and the meta‐analyses crossed the Lan‐DeMets monitoring boundary, leaving out any random error. The only trial with blinded assessment of sustained virological response showed no significant differences between the two interventions but suffered from the fact that it was very small (Sjögren 2007). Subgroup analyses for sustained virological response showed a pronounced difference in comparative treatment effects by genotype and type of peginterferon. Data from 16 trials for genotype one yielded RR 1.5, 95% CI 1.3 to 1.7. Data from nine trials for genotype two or three yielded RR 1.1, 95% CI 1.0 to 1.2. Data from nine trials for genotype four yielded RR 1.8, 95% CI 1.3 to 2.4. These differences were substantiated by tests of interaction that yielded statistically significant differences between genotype one and genotype two or three (P value 0.0002) and between genotype two or three and genotype four (P value 0.029). The larger effects of peginterferons versus interferons on sustained virological response were observed in participants infected with genotype one and genotype four, whereas the difference between peginterferon and interferon was least for participants infected with genotype two or three. Moreover, peginterferon alpha‐2a plus ribavirin seemed significantly more effective than peginterferon alpha‐2b plus ribavirin when compared with interferon plus ribavirin in subgroup analyses. Data from nine trials for peginterferon alpha‐2a yielded RR 1.9, 95% CI 1.5 to 2.4. Data from 18 trials for peginterferon alpha‐2b yielded only RR 1.1, 95% CI 1.1 to 1.2. These differences were substantiated by tests of interaction that yielded statistically significant differences between peginterferon alpha‐2a plus ribavirin and peginterferon alpha‐2b plus ribavirin trials (P < 0.0001). This is in accordance with our previous observations based on head‐to‐head randomised clinical trials comparing peginterferon alpha‐2a versus peginterferon alpha‐2b (Awad 2010; Hauser 2014). All other tests of interaction regarding risk of bias (lower risk of bias compared with high risk of bias), treatment history, and baseline viral load yielded non‐significant results. We found three trials that used amantadine cointervention, four trials that used consensus interferon, and one trial that used leucocyte interferon. However, the paucity of evidence precludes any firm conclusions on effects of triple therapy regimens with the use of amantadine, leucocyte interferon, or consensus interferon. Our analyses strengthen the evidence that peginterferon plus ribavirin increases sustained virological response for participants with chronic hepatitis C, irrespective of genotype, previous antiviral status, or viral load, and with or without amantadine as cointervention.
Quality of the evidence
The methodological quality was unclearly reported in a considerable number of included trials. Only 14 of the 27 trials (51.9%) reported adequate randomisation and allocation concealment. Most trial reports described unclearly blinded outcome assessment. These aspects may be essential in minimising the risks of selection, performance, and ascertainment bias in individual trials (Schulz 1995; Moher 1998; Kjaergard 2001; Wood 2008; Lundh 2012; Savovic 2012; Savovic 2012a). However, we found no significant association between methodological quality and trial results (Analysis 3.1).These findings may support the robustness of our results but do not exclude the possibility of bias, especially as we could not assess risk of bias from blinding and vested interests. Industry support is known to significantly bias trial results (Lundh 2012). Regarding blinding, only one trial assessed sustained virological response with blinding and found no significant effect of pegylated interferon versus interferon (Sjögren 2007). However, this trial was small, and the confidence interval was accordingly wide (Sjögren 2007).
Selective outcome reporting was difficult to assess in this review. None of the included trials was adequately registered or had its protocol publicly available before trial completion (Krleza‐Jeric 2005; WHO 2009). It is hoped that the initiation of the World Health Organization International Clinical Trials Registry Platform will facilitate such assessments for future trials (WHO 2009). Another limitation in this review was insufficient design and reporting. Investigators of future trials therefore are well advised to adhere to the guidelines of Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) (Chan 2013) and the Consolidated Standards for Reporting of Trials (CONSORT) (Moher 2012) to improve the quality of trials.
In general, we can have only low confidence in the current evidence on harms measured as morbidity plus mortality and adverse events leading to discontinuation, whereas we can have moderate confidence in the current evidence on treatment benefits measured as sustained virological response (Table 1). In the meta‐analysis for morbidity plus mortality, very serious imprecision was evident because only nine events were included in the meta‐analysis from five trials (Fried 2002; Esmat 2003; Al‐Faleh 2004; Lee 2005; Nevens 2010). In the meta‐analysis on adverse events, serious discrepancies across trials and lack of precision were noted. The proportions of observed adverse events differ substantially across trials, and the direction of effect is heterogeneous. However, because the event rate is still relatively low across trials, all of the included trials may be subject to considerable random error, thus explaining the apparent heterogeneity in direction of estimates. The observed treatment effects differ in magnitude as well, but most confidence intervals show considerable overlap. In the meta‐analysis for sustained virological response, no serious inconsistencies across studies were evident, and the meta‐analyses showed adequate precision (i.e., the TSA alpha‐spending monitoring boundary for benefit was crossed, favouring pegylated interferon). Nonetheless, we had some concerns regarding bias (which was high in all trials) and indirectness, as all included randomised clinical trials had virological response as the predominant measure of benefit. Many of the trials measured sustained virological response, which is currently the commonly used surrogate outcome measure of benefit. Recent large cohort studies show a positive correlation between the presence of viraemia and mortality (Adeel 2009; Hirofumi 2009). However, it is important to remember that sustained virological response still is only a putative (unvalidated) surrogate outcome for the patient‐relevant intervention effects of antivirals (Gluud 2007; Koretz 2013; Gurusamy 2013). Because randomised clinical trials need to inform clinical practice, clinical outcomes such as risk of liver failure, hepatocellular carcinoma, mortality, and quality of life would be of greater interest to patients and clinicians. Such measures nevertheless require a follow‐up of maybe up to five years. Currently, no randomised clinical trials assessing the two pegylated interferons are of such long duration.
Potential biases in the review process
The included meta‐analyses had a seemingly reasonable mix of small and large studies, yielding fairly consistent results, thus causing little concern about the presence of publication bias.
The strengths of this Cochrane Hepato‐Biliary Group systematic review are that it builds on a peer‐reviewed published protocol, uses extensive searches until recently (Appendix 1), considers risks of systematic errors (‘bias’) (Schulz 1995; Moher 1998; Kjaergard 2001; Wood 2008; Lundh 2012; Savovic 2012; Savovic 2012a), and considers risks of random errors (‘play of chance’) by adjusting the threshold for statistical significance according to the information and strength of evidence present in the cumulative meta‐analysis (Brok 2008; Wetterslev 2008; Brok 2009; Thorlund 2009, Wetterslev 2009; Thorlund 2010). Furthermore, to avoid publication and ascertainment bias, we included trials regardless of publication status and language, and all data were abstracted independently by at least two review authors to avoid information bias. However, our review has potential limitations that may lower our confidence in the estimates of intervention effect. First, we are aware of possible inclusion bias in excluding special patient groups (hepatitis B virus, human immunodeficiency virus, cancer, and liver‐transplanted patients). Future systematic reviews should assess the intervention effects of antivirals in these patient groups. Second, a possible limitation of our review is the lack of availability of full reports of all included trials. Ten of the 27 included trials were available only as abstracts. However, including these abstracts in our systematic review may likely be a strength rather than a limitation. By including abstracts, we are looking at the complete available body of evidence. By excluding abstracts, we would have been looking only at a subset defined through present‐day publication mechanisms, favouring trials that show beneficial effects. This would considerably increase the likelihood of publication bias. Third, in general, adverse events were reported insufficiently. Most of the participants treated with peginterferon alpha or interferon alpha experience one or more adverse effects (e.g., influenza‐like symptoms, depression, neutropenia, thrombocytopenia). The proportions of observed adverse events differed greatly across trials, and the direction of effect was heterogeneous.
Agreements and disagreements with other studies or reviews
By comparing our results with those of the other meta‐analyses, we have found two main differences. Our searches of the literature were much more detailed than searches previously conducted. In previous meta‐analyses, authors usually did not perform grey literature searches and did not include meeting abstracts. Some authors excluded trials that were not published in English or used just two databases (Chander 2002; Zaman 2003), performed only cost‐effectives analysis (Shepherd 2005; Siebert 2005), or evaluated only one genotype (Khuroo 2004; Aljumah 2013). Second, we performed several sensitivity analyses to ensure the robustness of the results of our systematic review; this procedure is lacking in previously published meta‐analyses. Moreover, our number of included trials is much higher than the number included in the meta‐analyses mentioned above. Fourth, we considered risk of bias. Fifth, we also took precautions to interpret the statistical inference according to the strength of the evidence. In this vein, we constructed adjusted thresholds for statistical significance by using TSA.
Authors' conclusions
Implications for practice.
Moderate evidence shows that pegylated interferon plus ribavirin compared with interferon plus ribavirin increases sustained virological response for patients with chronic hepatitis C, irrespective of genotype, previous antiviral status, or viral load, and with or without amantadine as cointervention. However, evidence is insufficient with regard to the risk of liver‐related morbidity plus all‐cause mortality, adverse events, and quality of life. Therefore, in their best interest, patients must be informed and involved in the decision to treat and with what to treat. Once started, treatment should be monitored carefully to minimise the risk of harm for patients.
Implications for research.
We can have very low confidence in the current evidence on treatment benefits measured as sustained virological response; thus, further research may not change our confidence in the estimate of effect. However, we lack knowledge about the clinical consequences of obtaining sustained virological response through antiviral treatment. We have only low confidence in the current evidence on harms measured as morbidity and mortality and adverse events leading to discontinuation; thus, further research is very likely to have an important impact on our confidence in the estimates of effect and is likely to change the estimates. Although we did not find differences regarding adverse events leading to treatment discontinuation between peginterferon plus ribavirin when compared with interferon plus ribavirin, an obvious trend was noted toward more adverse events among patients treated with pegylated interferons. Randomised clinical trials are needed to confirm or refute the effect of peginterferon plus ribavirin treatment in non‐responders and relapsers. Longer follow‐up assessment on existing trials and research on the long‐term association between sustained virological response and liver‐related morbidity and all‐cause mortality seem warranted. Future trials ought to assess quality of life as well. Future trials should be designed according to the SPIRIT guidelines (Chan 2013) and reported according to the CONSORT guidelines (www.consort‐statement.org) (Moher 2012).
Acknowledgements
Thanks to Marija Simin for drafting the previous version of this systematic review. Thanks to Sarah Klingenberg for advising on and conducting the search strategy. Thanks to Esmat GH, Lee SD, Izumi N, Mangia A, Napoli N, Nevens F, and Tsubota A who provided us with additional information regarding their trials.
Peer reviewers: Jalal Poorolajal, Iran. Contact editors: Bodil Als‐Nielsen, Denmark; Ronald Koretz, USA.
Appendices
Appendix 1. Search strategies
| Database | Search date | Search strategy |
| The Cochrane Hepato‐Biliary Group Controlled Trials Register | September 2013 | (interferon alfa or interferon alpha or intron A or roferon A or pegylated interferon‐2a or pegylated interferon‐2b or pegasus or pegasys or pegintron or viraferonPeg or peginterferon or peg‐ifn) AND (ribavirin OR riba OR copegus OR rebetol OR ribasphere OR vilona OR virazole) AND (hepatitis C OR hep C OR HCV) |
| The Cochrane Central Register of Controlled Trials (CENTRAL) | Issue 8, 2013 | #1 MeSH descriptor: [Interferon‐alpha] explode all trees #2 interferon al*a or intron or roferon or pegylated interferon‐2a or pegylated interferon‐2b or pegas*s or pegintron or viraferonpeg or peginterferon or peg‐ifn #3 #1 or #2 #4 MeSH descriptor: [Ribavirin] explode all trees #5 ribavirin or riba or copegus or rebetol or ribasphere or vilona or virazole #6 #4 or #5 #7 MeSH descriptor: [Hepatitis C, Chronic] explode all trees #8 hepatitis c or hep c or hcv #9 #7 or #8 #10 #3 and #6 and #9 |
| MEDLINE (Ovid SP) | 1946 to September 2013 |
1. exp Interferon‐alpha/ 2. (interferon al$a or intron or roferon or pegylated interferon‐2a or pegylated interferon‐2b or pegas$s or pegintron or viraferonpeg or peginterferon or peg‐ifn).mp. [mp=protocol supplementary concept, rare disease supplementary concept, title, original title, abstract, name of substance word, subject heading word, unique identifier] 3. 1 or 2 4. exp Ribavirin/ 5. (ribavirin or riba or copegus or rebetol or ribasphere or vilona or virazole).mp. [mp=protocol supplementary concept, rare disease supplementary concept, title, original title, abstract, name of substance word, subject heading word, unique identifier] 6. 4 or 5 7. exp Hepatitis C, Chronic/ 8. (hepatitis c or hep c or hcv).mp. [mp=protocol supplementary concept, rare disease supplementary concept, title, original title, abstract, name of substance word, subject heading word, unique identifier] 9. 7 or 8 10. 3 and 6 and 9 11. (random* or blind* or placebo* or meta‐analysis).mp. [mp=protocol supplementary concept, rare disease supplementary concept, title, original title, abstract, name of substance word, subject heading word, unique identifier] 12. 10 and 11 |
| EMBASE (Ovid SP) | 1974 to September 2013 |
1. exp Alpha Interferon/ 2. exp peginterferon/ or exp peginterferon alpha2a/ or exp peginterferon alpha2b/ or exp recombinant alpha2a interferon/ or exp recombinant alpha2b interferon/ 3. (interferon al$a or intron or roferon or pegylated interferon‐2a or pegylated interferon‐2b or pegas$s or pegintron or viraferonpeg or peginterferon or peg‐ifn).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword] 4. 1 or 2 or 3 5. exp Ribavirin/ 6. (ribavirin or riba or copegus or rebetol or ribasphere or vilona or virazole).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword] 7. 6 or 5 8. exp Hepatitis C/ 9. (hepatitis c or hep c or hcv).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword] 10. 8 or 9 11. 4 and 7 and 10 12. (random* or blind* or placebo* or meta‐analysis).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword] 13. 11 and 12 |
| Science Citation Index‐Expanded | 1900 to September 2013 | #6 #5 AND #4 #5 TS=(random* or blind* or placebo* or meta‐analysis) #4 #3 AND #2 AND #1 #3 TS=(chronic hepatitis c) #2 TS=(ribavirin OR riba OR copegus OR rebetol OR ribasphere OR vilona OR virazole) #1 TS=(interferon al*a or intron or roferon or pegylated interferon‐2a or pegylated interferon‐2b or pegas*s or pegintron or viraferonpeg or peginterferon or peg‐ifn) |
| LILACS | 1980 to September 2013 | interferon AND ribavirin AND hepatitis C |
Data and analyses
Comparison 1. Peginterferon plus ribavirin versus non‐pegylated interferon plus ribavirin.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Liver‐related morbidity plus all‐cause mortality | 5 | 1789 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.38, 3.42] |
| 2 Adverse events leading to treatment discontinuation | 17 | 4868 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.66, 1.12] |
| 3 Sustained virological response | 27 | 6104 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [1.25, 1.56] |
Comparison 2. Adverse events.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Haematological effects | 13 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Anaemia | 13 | 3854 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.98, 1.27] |
| 1.2 Neutropenia | 13 | 3855 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.15 [1.76, 2.61] |
| 1.3 Thrombocytopenia | 10 | 2195 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.63 [1.68, 4.11] |
| 2 Fatigue and flu‐like symptoms | 13 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 General fatigue | 11 | 3608 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.96, 1.07] |
| 2.2 Headache | 6 | 3146 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.93, 1.07] |
| 2.3 Rigours | 4 | 2641 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.88, 1.08] |
| 2.4 Arthralgia | 4 | 2934 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [1.05, 1.35] |
| 2.5 Myalgia | 5 | 3087 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.90, 1.06] |
| 2.6 Pyrexia | 6 | 3180 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.99, 1.18] |
| 2.7 Weight loss | 6 | 2524 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.98, 1.39] |
| 2.8 Asthenia | 3 | 2126 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.88, 1.25] |
| 3 Psychiatric symptoms | 12 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Depression | 12 | 3743 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.82, 1.02] |
| 3.2 Insomnia | 5 | 3087 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.91, 1.10] |
| 3.3 Irritability | 3 | 2491 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.86, 1.09] |
| 4 Dermatological symptoms | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Alopecia | 5 | 3087 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.88, 1.09] |
| 4.2 Pruritus | 5 | 3027 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.96, 1.25] |
| 4.3 Skin rash | 5 | 2740 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.93, 1.25] |
| 4.4 Injection site reaction | 4 | 1817 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.71 [1.50, 1.93] |
| 5 Thyroid malfunction | 8 | 1222 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.73, 2.00] |
| 6 Gastrointestinal symptoms | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Decreased appetite | 6 | 3136 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.93, 1.19] |
| 6.2 Nausea | 4 | 3023 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [1.01, 1.26] |
| 6.3 Diarrhoea | 3 | 2126 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.93, 1.41] |
Comparison 3. Subgroup and sensitivity analysis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Sustanied virological response according to trial methodological quality | 27 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Lower risk of bias trials | 14 | 4285 | Risk Ratio (M‐H, Random, 95% CI) | 1.33 [1.17, 1.51] |
| 1.2 High risk of bias trials | 13 | 1819 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [1.23, 1.95] |
| 2 Sustanied virological response according to baseline treatment history | 26 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Naive participants | 22 | 5223 | Risk Ratio (M‐H, Random, 95% CI) | 1.42 [1.25, 1.62] |
| 2.2 Non‐responders and relapsers | 4 | 389 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.96, 1.61] |
| 2.3 Unknown | 1 | 49 | Risk Ratio (M‐H, Random, 95% CI) | 1.41 [0.67, 2.97] |
| 3 Sustained virological response according to genotype | 27 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 Genotype one | 16 | 3548 | Risk Ratio (M‐H, Random, 95% CI) | 1.47 [1.27, 1.70] |
| 3.2 Genotypes two and three | 9 | 1659 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [1.03, 1.19] |
| 3.3 Genotype four | 9 | 721 | Risk Ratio (M‐H, Random, 95% CI) | 1.76 [1.30, 2.39] |
| 4 Sustained virological response according to baseline viral load | 27 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 High viral load | 5 | 1777 | Risk Ratio (M‐H, Random, 95% CI) | 1.33 [1.01, 1.75] |
| 4.2 Low viral Load | 5 | 1027 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [1.05, 1.58] |
| 4.3 Predominantly high viral load (more than 65% of total participants) | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 1.5 [0.87, 2.59] |
| 4.4 Predominantly low viral load (more than 65% of total participants) | 6 | 920 | Risk Ratio (M‐H, Random, 95% CI) | 1.58 [1.22, 2.06] |
| 4.5 Similar proportions of high and low baseline viral loads | 4 | 607 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [1.01, 1.70] |
| 4.6 Unknown baseline viral load | 11 | 1690 | Risk Ratio (M‐H, Random, 95% CI) | 1.38 [1.11, 1.71] |
| 5 Sustained virological response according to the type of peginterferon | 27 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 Peginterferon alpha‐2a | 9 | 2361 | Risk Ratio (M‐H, Random, 95% CI) | 1.85 [1.46, 2.35] |
| 5.2 Peginterferon alpha‐2b | 18 | 3534 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [1.06, 1.22] |
| 6 Sustained virological response according to the type of peginterferon and the type of interferon | 27 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 Peginterferon alpha‐2a versus interferon alpha‐2a | 8 | 1464 | Risk Ratio (M‐H, Random, 95% CI) | 1.98 [1.63, 2.40] |
| 6.2 Peginterferon alpha‐2a versus interferon alpha‐2b | 1 | 897 | Risk Ratio (M‐H, Random, 95% CI) | 1.27 [1.11, 1.45] |
| 6.3 Peginterferon alpha‐2b versus interferon alpha‐2b | 13 | 2799 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [1.06, 1.25] |
| 6.4 Peginterferon alpha‐2b versus consensus interferon | 4 | 671 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.92, 1.23] |
| 6.5 Peginterferon alpha‐2b versus leucocyte interferon | 1 | 64 | Risk Ratio (M‐H, Random, 95% CI) | 1.75 [1.05, 2.92] |
| 7 Sustained virological response in trials with or without amantadine | 27 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 Trial without amantadine | 24 | 5500 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [1.22, 1.53] |
| 7.2 Trial with amantadine | 3 | 604 | Risk Ratio (M‐H, Random, 95% CI) | 1.68 [1.26, 2.23] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Al‐Faleh 2004.
| Methods | Randomised clinical trial with two parallel‐group design. Sample size calculation: performed, 48 participants estimated for each group. Intention‐to‐treat analysis: used. Participants who discontinued treatment or were lost to follow‐up were classified as non‐responders. |
|
| Participants | Country: Saudi Arabia. Number of participants randomly assigned: 96; 54 men and 42 women. All participants were treatment‐naive. Genotype: four. Inclusion criteria.
Exclusion criteria.
|
|
| Interventions | Participants were randomly assigned to two groups.
Participants were followed up for 24 weeks after the end of treatment. |
|
| Outcomes | Primary outcomes were biochemical and virological responses at the end of treatment and at the end of follow‐up. Other outcomes reported are adverse events. Limit for hepatitis C virus RNA detection was 3200 copies/mL. |
|
| Notes | Author contacted for additional information, but no reply received. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: randomly generated numbers by a computer program. |
| Allocation concealment (selection bias) | Low risk | Quote: performed in a central unit and were distributed in opaque sealed envelopes to individual centres. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: It is mentioned only that the pathologists were blinded to the treatment allocation of the participant. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | It is clearly stated that treatment was discontinued in three and eight participants in peginterferon plus ribavirin and interferon plus ribavirin groups. Intention‐to‐treat analysis was used when participants who discontinued treatment or were lost to follow‐up were classified as non‐responders. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Unclear risk | Conflict of interest bias might be present. The study was supported in part by a grant from Schering‐Plough, Saudi Arabia. |
Bruno 2004.
| Methods | Randomised clinical trial with two parallel‐group design. Sample size calculation: performed, 151 participants estimated for each group. Intention‐to‐treat analysis: not used, although stated. |
|
| Participants | Country: Italy. Number of participants randomly assigned: 323; 194 men and 117 women, and 12 excluded from analyses. All participants were treatment‐naive. All participants were infected with HCV genotype one. Inclusion criteria.
Exclusion criteria.
|
|
| Interventions | Participants were randomly assigned to two groups.
For both groups, ribavirin was given at a dose of 1000 mg for participants weighting 75 kg or less and 1200 mg for those weighing more than 75 kg. Participants were withdrawn from treatment if they did not achieve a virological response that was defined as undetectable serum HCV RNA by PCR 24 weeks after starting treatment. |
|
| Outcomes | Primary outcome was sustained virological response, defined as the absence of detectable HCV RNA by PCR 24 weeks after the end of treatment. Other outcomes reported are end of treatment biochemical and virological response, sustained biochemical response, and frequency of discontinuations and dose reductions with causes. Limit for hepatitis C virus RNA detection was 50 IU/mL. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: computer‐generated scheme. Patients were stratified according to centre and randomised in blocks of four to the peginterferon plus ribavirin or interferon plus ribavirin group. |
| Allocation concealment (selection bias) | Low risk | Comment: central randomisation centre. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: It is mentioned only that the slides of liver biopsy specimens were coded and read by a single pathologist, who was unaware of clinical data. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: The number of participants lost to follow‐up is mentioned. Treatment was discontinued in 31 and 46 participants in peginterferon plus ribavirin and interferon plus ribavirin groups. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Unclear risk | Comment: Conflict of interest bias might be present. Schering‐Plough Italy supplied peginterferon alpha‐2b, and the other drugs were provided by the National Health System. |
Cariti 2002.
| Methods | Study design: randomised clinical trial. Inclusion criteria: biopsy proven chronic hepatitis C, persistently elevated ALT, HCV RNA positive. |
|
| Participants | Country: Italy. Total number (sample size): 117. Age: 46.7 group A; 43.7 group B. Sex (male): group A 73%, group B 76%. Genotype: one. Previous HCV treatment: naive. |
|
| Interventions | Group A.
Group B.
|
|
| Outcomes | Sustained virological response. | |
| Notes | Abstract form, study authors were contacted, but we received no reply. It is not clear whether Intention‐to‐treat analysis was used when participants discontinued treatment or were lost to follow‐up. The trial included 150 participants, but data from only 117 are available. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "patients where randomised". Comments: Method used to perform sequence generation is not mentioned. |
| Allocation concealment (selection bias) | Unclear risk | Comment: Method of allocation concealment is not mentioned. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: It is mentioned only that the pathologists were blinded to the treatment allocation of the participant. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: It is not clear whether Intention‐to‐treat analysis was used when participants discontinued treatment or were lost to follow‐up. The trial included 150 participants, but the data from only 117 are available. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Low risk | Comment: The trial seems to be free of other sources of bias. |
Derbala 2005.
| Methods | Study design: randomised clinical trial. | |
| Participants | Country: Egypt. Total number (sample size): 70. Age, years: 42.6 group A; 38.7 group B. Sex (male): group A 27, group B 26. Genotype: four. Previous HCV treatment: naive. Inclusion criteria: biopsy proven chronic hepatitis C, persistently elevated ALT, HCV RNA positive. |
|
| Interventions | Group A: 35 participants
Group B: 35 participants.
Ribavirin was given to both groups at a weight‐based dose ranging from 800 mg to 1000 mg.
|
|
| Outcomes | Sustained virological response. Adverse events. |
|
| Notes | Abstract only, no data about inclusion and exclusion criteria are provided. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comments: Method used to perform sequence generation is not mentioned. |
| Allocation concealment (selection bias) | Unclear risk | Comment: Method of allocation concealment is not mentioned. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: It is not mentioned whether outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: The number and reasons for participant dropout were clearly specified. Intention‐to‐treat analysis did not change the estimates for sustained virological response. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Low risk | Comment: The trial seems to be free of other sources of bias. |
Derbala 2006.
| Methods | Study design: randomised clinical trial. | |
| Participants | Country: Egypt. Total number: 73 (seven participants did not continue the treatment). Age, years: 45.5. Sex (male): 31% to 33%. Comorbidity: bilharziasis. Genotype: four. Previous HCV treatment: naïve. Inclusion criteria: chronic active hepatitis C as evidenced by the following.
Exclusion criteria.
|
|
| Interventions | Group A (n = 38).
Group B (n = 35).
|
|
| Outcomes | Primary outcomes: end of treatment response, sustained virological response, adverse events. | |
| Notes | Published article. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comments: Method used to perform sequence generation is not mentioned. |
| Allocation concealment (selection bias) | Unclear risk | Comments: Allocation concealment is not mentioned. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comments: Blinding to the outcome assessor is not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: Incomplete outcome data were addressed adequately. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Low risk | Comment: The trial seems to be free of other sources of bias. |
Dollinger 2005.
| Methods | Study design: randomised multicentre trial. ITT analysis: performed. Sample size calculation: not mentioned. |
|
| Participants | Country: Germany. Total number (sample size): 40. Age: not mentioned. Sex (male): not mentioned. Comorbidity: not mentioned. Genotype: one‐b. Previous HCV treatment: non‐responders to previous combination treatment with IFN and RBV. Inclusion criteria: chronic hepatitis C diagnosed by the following.
|
|
| Interventions | Group A (n = 22).
Group B (n = 18).
|
|
| Outcomes | Early response rate (24 weeks of treatment); end‐of‐treatment response rate (52 weeks of treatment); sustained response rate (six months after treatment); adverse events. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comments: Method of sequence generation is not mentioned. |
| Allocation concealment (selection bias) | Unclear risk | Comments: Allocation concealment is not mentioned. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comments: Blinding to outcome assessors is not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: Incomplete outcome data were addressed adequately. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Unclear risk | Quote: "The study was supported by a grant of Yamanouchi and Essexpharma, Germany". Comments: The study may contain conflict of interest risk of bias. |
Esmat 2003.
| Methods | Randomised clinical trial with two parallel‐group design. Sample size calculation: unclear, not described. Intention‐to‐treat analysis: used. |
|
| Participants | Country: Egypt. Number of participants randomly assigned: 200; 158 men and 42 women. All participants were treatment‐naive. Mean inflammatory histological activity index score was 7/18 ± 2 and fibrosis stage 2.7/6 ± 1.3 in both arms. 90% of participants were infected with HCV genotype four. Inclusion and exclusion criteria: none stated. |
|
| Interventions | Participants were randomly assigned to two groups:
If HCV RNA was detectable at week 24, the treatment was stopped. Participants were followed‐up for an additional 24 weeks after the end of treatment. |
|
| Outcomes | Primary outcome was HCV RNA status at week 72 (end of follow‐up). Other outcomes reported were end of treatment virological response and adverse events. Limit for hepatitis C virus RNA detection was 50 copies/mL. |
|
| Notes | The report is abstract. Abstract only, no data about inclusion and exclusion criteria are provided. Additional data were obtained through personal communication with the study author. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: A computer programme randomly allocated participants to one of the two treatment groups in blocks of 10. |
| Allocation concealment (selection bias) | Low risk | Comment: The group assignment was concealed in opaque sealed envelopes that were not opened until all study entry criteria were met. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: Participants were not blinded; however, it is mentioned whether outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: The number of participants lost to follow‐up is stated. 67 participants discontinued treatment in peginterferon plus ribavirin group and 69 in interferon plus ribavirin group. Intention‐to‐treat analysis was employed. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Low risk | Comments: The trial seem to be free of other sources of bias. |
Fargion 2004.
| Methods | Randomised clinical trial with two parallel‐group design. Samlpe size calculation: not described. |
|
| Participants | Country: Italy. Number of participants randomly assigned: 185. All participants were non‐responders to previous interferon plus ribavirin treatment. Inclusion and exclusion criteria: none stated. |
|
| Interventions | Participants were randomly assigned to two groups.
Participants with detectable HCV RNA after 24 weeks of treatment were considered non‐responders and therapy discontinued. Participants were followed‐up for 24 weeks after the end of treatment. |
|
| Outcomes | Primary outcome was sustained virological response, defined as undetectable HCV RNA 24 weeks after the end of treatment. Other outcome reported was end of treatment virological response. |
|
| Notes | The report is abstract; because the study has not been published yet, no data about inclusion and exclusion criteria are provided. Data were extracted from the primary reference and the previous abstract: Fargion S et al. End of treatment and sustained response to peginterferon alfa‐2a (40 kD) (Pegasys) plus ribavirin (RBV) (Copegus) and amantadine (AMA), and to induction therapy with interferon (IFN) alfa‐2A (Roferon‐A) plus RBV and AMA in INF/RBV non‐responders with chronic hepatitis C (CHC) [AASLD abstract]. Hepatology 2003;38(4, Suppl 1):733A. Number of participants in each group is not reported, so we provisionally divided the total number of participants by two. Study author contacted for additional information, but no data were obtained. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comments: Method of sequence generation is not mentioned. |
| Allocation concealment (selection bias) | Unclear risk | Comments: Allocation concealment is not mentioned. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comments: Blinding to outcome assessors is not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: No post randomisation dropouts were reported. |
| Selective reporting (reporting bias) | Unclear risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Low risk | Comments: The trial seem to be free of other sources of bias. |
Fried 2002.
| Methods | Randomised clinical trial with three‐group design. Sample size calculation: unclear, not described. Intention‐to‐treat analysis: not used, although stated (28 participants who were randomly assigned and did not receive allocated intervention were excluded from analyses). All participants who received at least one dose of study medication were included in all efficacy analyses, and if they had undergone at least one safety assessment after baseline, they were included in the safety analysis. All participants with follow‐up of less than 20 weeks were considered to have had no response to treatment. |
|
| Participants | Country: 81 centres worldwide. Number of participants randomly assigned: 1149; 800 men and 321 women, and 28 excluded from analyses. All participants were treatment‐naive. Genotype: one. Inclusion criteria.
Exclusion criteria.
|
|
| Interventions | Participants were randomly assigned to three groups.
For two arms, ribavirin was given at a dose of 1000 mg for participants weighing 75 kg or less and 1200 mg for those weighing more than 75 kg. Participants were withdrawn from treatment if they continued to have viraemia at week 24, if they missed four consecutive doses, or at the discretion of the investigator. Participants were followed for 24 weeks after the end of treatment. |
|
| Outcomes | Primary outcome was sustained virological response, defined as the absence of detectable HCV RNA at the end of follow‐up according to a PCR assay. Other outcomes reported are end of treatment virological response, incidence of treatment discontinuation, dose modification, and adverse events. Limit for hepatitis C virus RNA detection was 50 IU/mL (100 copies/mL). |
|
| Notes | The study was designed by the sponsor in collaboration with expert hepatologists. Data were collected by the Pegasys International Study Group. Data analysis was performed by the sponsor and the authors of the report; the authors had full access to the data, and the decision to publish was not limited by the sponsor. Data were extracted from the primary reference and Hassanein T, et al. The impact of peginterferon alfa‐2a plus ribavirin combination therapy on health‐related quality of life in chronic hepatitis C. Journal of Hepatology 2004;40:675‐81. Study author contacted for additional information, but no reply obtained. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comments: Sequence generation was performed by a computer programme. |
| Allocation concealment (selection bias) | Low risk | Comments: Central allocation concealment. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comments:Method of blinding was not described. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: No postrandomisation dropouts were reported. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Unclear risk | The trial was sponsored by Roche. Designed by the sponsor in collaboration with expert hepatologists. Data were collected by the Pegasys International Study Group. Data analysis was performed by the sponsor and the authors of the report; the authors had full access to the data, and the decision to publish was not limited by the sponsor. This trial may contain conflict of interest bias. |
Hinrichsen 2002.
| Methods | Randomised clinical trial with two‐group design. Samlpe size calculation: unclear, not described. Intention‐to‐treat analysis: used. |
|
| Participants | Country: Germany. Number of participants randomly assigned: 72; 41 men and 31 women. All participants were treatment‐naive. All participants were infected with HCV genotype two and three. Inclusion and exclusion criteria: none stated. |
|
| Interventions | Participants were randomly assigned to two groups.
|
|
| Outcomes | Primary outcomes were sustained and end of treatment virological responses. Other outcome reported is quality of life. Limit for hepatitis C virus RNA detection was 50 IU/mL. |
|
| Notes | The report is abstract; because the study has not been published yet, no data about inclusion and exclusion criteria are provided. Study author contacted for additional information, but no data obtained. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comments: Method used to perform sequence generation is not mentioned. |
| Allocation concealment (selection bias) | Low risk | Comments: Allocation concealment is not mentioned. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comments: Blinding is not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: The trial seems to have addressed incomplete outcome data adequately. |
| Selective reporting (reporting bias) | Unclear risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Low risk | Comment: The trial seems to be free of other sources of bias. |
Horsmans 2008.
| Methods | Study design: multi‐centre, controlled randomised trial comparing three groups. ITT analysis: performed. |
|
| Participants | Country: Belgium. Total number (sample size): 258 (initially 336, but 78 had not commenced treatment). Age, years (STD) : 45, 46, and 45. Sex (male, number): 63, 62, and 36. Genotype: one, two, and three. Previous HCV treatment: naive. Inclusion criteria: chronic hepatitis C diagnosed by the following.
Exclusion criteria.
|
|
| Interventions | Group 1 (n = 101).
Group 2 (n = 98).
Group 3 (n = 59).
|
|
| Outcomes | End of treatment response; sustained virological response; adverse events. | |
| Notes | Inconsistency in the figures across the study report is evident: total number (sample size): 258 (initially 336, but 78 had not commenced treatment). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comments: Method of sequence generation is not mentioned. Randomisation process is not well described. |
| Allocation concealment (selection bias) | Unclear risk | Comments: The allocation concealment process is not mentioned. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Coments: open‐label trial. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: 78 participants had not commenced treatment; it is not clear whether the trial adhered to the intention‐to‐treat analysis. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Unclear risk | All medication was provided by Schering‐Plough. |
Izumi 2004.
| Methods | Randomised clinical trial with two parallel‐group design. Sample size calculation: unclear, not described. Intention‐to‐treat analysis: unclear, not described. |
|
| Participants | Country: Japan. Number of participants randomly assigned: 49; 23 men and 26 women. 63% of participants were treatment‐naive and 37% were retreated. None of the participants had cirrhosis. All participants were infected with HCV genotype one. Limit for hepatitis C virus RNA detection was 10 copies/mL. Mean HCV RNA levels (kIU/mL) were 720 in peginterferon plus ribavirin group and 640 in interferon plus ribavirin group. Inclusion criteria.
Exclusion criteria.
|
|
| Interventions | Participants were randomly assigned to two groups.
Both arms received ribavirin 600 mg for participants who weighed less than 60 kg, 800 mg for participants who weighed between 60 and 80 kg, and 1000 mg for participants who weighed more than 80 kg. |
|
| Outcomes | Primary outcome was HCV RNA dynamics. No other outcomes were reported. |
|
| Notes | Data were obtained through personal communication with the study author. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comments: Method used to perform sequence generation is not mentioned. |
| Allocation concealment (selection bias) | Unclear risk | Comments: Allocation concealment is not mentioned. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comments: Blinding to outcome assessors is not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: Incomplete outcome data were addressed adequately. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Low risk | Comments: The trial seems to be free of other sources of bias. |
Lee 2005.
| Methods | Randomised clinical trial with two parallel‐group design. Sample size calculation: performed, 70 participants estimated for each group. Intention‐to‐treat analysis: used (14 and five participants discontinued treatment in peginterferon plus ribavirin and interferon plus ribavirin groups). |
|
| Participants | Country: Taiwan. Number of participants randomly assigned: 153; 105 men and 48 women. All participants were treatment‐naive. Genotype: one, two, three, four. Inclusion criteria.
Exclusion criteria.
|
|
| Interventions | Participants were randomly assigned to two arms.
The dose of ribavirin was based on body weight (1000 mg for weight 75 kg, and 1200 mg for weight greater than 75 kg). Participants were treated for 24 weeks and were followed for another 24 weeks after the end of treatment. |
|
| Outcomes | Primary outcomes were biochemical response, virological response, which was defined as the persistent disappearance of serum HCV RNA, and degree of histological improvement. Other outcomes reported are adverse events. Limit for hepatitis C virus RNA detection was 50 IU/mL. |
|
| Notes | The trial was supported by research grants from Schering‐Plough Limited, Taiwan. Additional data were obtained through personal communication with the study author. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comments: Sequence generation was performed by a computer programme. |
| Allocation concealment (selection bias) | Low risk | Comments: Central allocation concealment. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: It is mentioned only that the liver histology was analysed by a single pathologist, who was unaware of the participant's identity, treatment regimen, response or timing of the biopsy relative to treatment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: Incomplete outcome data were addressed adequately. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Unclear risk | Comment: The trial was supported by research grants from Schering‐Plough Limited, Taiwan. The study may have conflict of interest bias. |
Mangia 2005.
| Methods | Randomised clinical trial with three parallel‐group design. Sample size calculation: performed, 118 participants estimated for each group. Intention‐to‐treat analysis: used. Participants who discontinued treatment or were lost during follow‐up were considered to be virological non‐responders (i.e., no sustained virological response). 39 participants discontinued treatment in peginterferon plus ribavirin plus amantadine group, 46 in interferon plus ribavirin plus amantadine group, and 54 in interferon plus ribavirin group. |
|
| Participants | Country: Italy. Number of participants randomly assigned: 362; 215 men and 147 women. All participants were treatment‐naive. Genotype: one, two, three. Mean HCV RNA levels (UI/mL × 1000) were 2817 ± 4318. 618 in peginterferon plus ribavirin plus amantadine group and 1998 ± 2255. 631 in interferon plus ribavirin plus amantadine group. Inclusion criteria.
Exclusion criteria.
|
|
| Interventions | Participants were randomly assigned to three groups.
All participants received ribavirin 1000 mg (body weight less than 75 kg) or 1200 mg (body weight greater than 75 kg). Participaants were evaluated for virological response at 24 weeks of treatment. Therapy was continued only in participants with undetectable HCV RNA at this time. |
|
| Outcomes | Primary outcome was sustained virological response, defined as undetectable HCV RNA 24 weeks after the end of treatment (study week 72). Other outcomes reported included end of treatment virological response, sustained and end of treatment biochemical responses, and adverse events. Limit for hepatitis C virus RNA detection was 50 copies/mL. |
|
| Notes | The study was conducted by the Al‐liver Study Group. Data were extracted from the primary reference, and additional data were obtained through personal communication with the study author. Dose reductions are reported only if they were greater than 20% of the prescribed drugs and for longer than 20% of the prescribed duration. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comments: Sequence generation was performed by a computer programme. |
| Allocation concealment (selection bias) | Low risk | Comments: Central allocation concealment. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: It is mentioned only that the liver histology was analysed by a single pathologist, who was unaware of the participant's identity, treatment regimen, response, or timing of the biopsy relative to treatment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: Incomplete outcome data were addressed adequately. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Unclear risk | Comment: No conflict of interest statement was provided. |
Manns 2001.
| Methods | Randomised clinical trial with three parallel‐group design. Sample size calculation: performed. This study was designed to include 525 participants per group. Intention‐to‐treat analysis: used. As prospectively specified in the protocol, all safety and efficacy analyses, except for changes from baseline in the histological scores, were based on all participants who received at least one dose of study medication. Participants who were missing HCV RNA values during follow‐up were classified as non‐responders. Analyses of changes from baseline in histological scores were based on participants who had both a pretreatment and a post‐treatment biopsy sample. 72 participants discontinued treatment in higher‐dose peginterferon plus ribavirin group, 67 in lower‐dose peginterferon plus ribavirin group, and 66 in interferon plus ribavirin group. |
|
| Participants | Country: 62 centres in Europe, Canada, Argentina, and the USA. Number of participants randomly assigned: 1530; 1003 men and 527 women. All participants were treatment‐naive. Genotype: one, two, three. Geometric mean HCV RNA levels (copies/mL × 1,000,000) were 2.7 in both peginterferon plus ribavirin arms, and 2.8 in interferon plus ribavirin group. Limit for hepatitis C virus RNA detection was 100 copies/mL. Inclusion criteria.
Exclusion criteria.
|
|
| Interventions | Participants were randomly assigned to three groups.
In the two arms receiving 1000 mg to 1200 mg of ribavirin, the dose was adjusted according to body weight (1000 mg for weight below 75 kg and 1200 mg for weight 75 kg or more). Both drugs were started and stopped at the same time. Participants were followed‐up for 24 weeks after the end of treatment. |
|
| Outcomes | Primary outcome was sustained virological response, defined as undetectable HCV RNA in serum at the end of follow‐up. Other outcomes reported included end of treatment virological response, sustained and end of treatment biochemical responses, histological response, and rates of discontinuation of treatment, dose reductions, and adverse events. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: computer generated. Eligible participants were randomly assigned the three study treatments in equal proportions, stratified by HCV genotype (one versus others) and the presence or absence of cirrhosis. The randomisation schedule, balanced within each country participating in the study, used a block size of three for each stratum and was generated by the study sponsor (Schering Plough Research Institute). |
| Allocation concealment (selection bias) | Low risk | Comment: Randomisation of participants to treatment was done by an independent central randomisation centre (Information Management Systems, Silver Springs, MD, USA). When a participant was found to be eligible for participation in the study, the study site sent a fax to the randomisation centre documenting the participant's eligibility; the centre sent a return fax with the participant's treatment assignment and identification number for the study. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: It is mentioned only that the liver histology was analysed by a single pathologist, who was unaware of the participant's identity, treatment regimen, response, or timing of the biopsy relative to treatment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: As prospectively specified in the protocol, all safety and efficacy analyses, except for changes from baseline in histological scores, were based on all participants who received at least one dose of study medication. Participants who were missing HCV RNA values during follow‐up were classified as non‐responders. Analyses of changes from baseline in histological scores were based on participants who had both a pretreatment and a post‐treatment biopsy sample. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Unclear risk | Comment: The study may contain conflict of interest bias. The study was supported by research grants from Schering Plough Research Institute, Kenilworth, NJ, and by clinical research centre grants from Massachusetts General Hospital, Scripps Clinic, and University of Florida. Study authors received grants from Schering Corp as part of their participation in current clinical trials. The study was conducted by International Hepatitis Interventional Therapy Group. |
Napoli 2005.
| Methods | Randomised clinical trial with two‐group design. Sample size calculation: unclear, not described. Intention‐to‐treat analysis: used. |
|
| Participants | Country: Italy. Number of participants randomly assigned: 64; 45 men and 19 women. All participants were treatment‐naive. Inclusion criteria.
Exclusion criteria.
|
|
| Interventions | Participants were randomly assigned to two arms:
Dose of ribavirin depended on pretreatment body weight: 800 mg for weight less than 60 kg; 1000 mg for weight greater than and equal to 60 kg and less than 75 kg; 1200 mg for weight greater than and equal to 75 kg. Duration of treatment was 48 weeks for participants infected with HCV genotype one and 24 weeks for participants infected with genotypes two and three. |
|
| Outcomes | Primary outcomes were end of treatment and sustained virological responses, defined as the absence of detectable HCV‐RNA in the serum at the end of treatment and at week 24 of post‐treatment follow‐up. Other outcomes reported are adverse events and dose reductions. Limit for hepatitis C virus RNA detection was 3200 copies/mL. |
|
| Notes | The study was supported by grants from Ministero dell Universita e della Ricerca Scientifica e Tecnologica, Rome, Italy. Additional data were obtained through personal communication with the study author. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comments: Sequence generation was performed by a computer programme. |
| Allocation concealment (selection bias) | Low risk | Comments: central allocation concealment. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comments: Blinding is not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: Incomplete outcome data were addressed adequately. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Low risk | Comment: The study seems to be free of other sources of bias. |
Nevens 2010.
| Methods | Randomised clinical trial with two parallel‐group design. Sample size calculation: unclear, not described. Intention‐to‐treat analysis: used. All participants who received at least one dose of study medication were included in the analysis (ITT/e = exposed). Participants without measurements at the end of the 24‐week untreated follow‐up period were considered as non‐responders. |
|
| Participants | Country: Belgium. Number of participants randomly assigned: 443; 241 men and 202 women. 78% of participants were treatment‐naive and 22% were relapsers. Inclusion criteria.
Exclusion criteria: none stated. |
|
| Interventions | Participants were randomly assigned to two groups.
Participants were followed‐up for 24 weeks after the end of treatment. |
|
| Outcomes | Primary outcome was sustained virological response, defined as undetectable HCV RNA at the end of follow‐up. Other outcomes reported are sustained biochemical response and adverse events. Limit for hepatitis C virus RNA detection was 50 IU/mL. |
|
| Notes | Follow‐up: 71 and 119 participants discontinued treatment in peginterferon plus ribavirin and interferon plus ribavirin groups. Additional data were obtained through personal communication with the study author. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: “Randomisation was stratified according to pre‐treatment status (treatment naïve versus relapse) and presence of cirrhosis”. |
| Allocation concealment (selection bias) | Low risk | Comment: no data about allocation concealment. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comment: open‐label study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: Incomplete outcome data were addressed adequately. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Low risk | Comment: The study seems to be free of other sources of bias. |
PRETTY 2005.
| Methods | Randomised clinical trial with two‐group design. Sample size calculation: unclear, not described. Intention‐to‐treat analysis: unclear, not described. |
|
| Participants | Country: Italy. Number of participants randomly assigned: 178; 119 men and 59 women. Genotype: one, two, three. All participants were non‐responders to previous interferon plus ribavirin treatment. Inclusion and exclusion criteria: none stated. |
|
| Interventions | Participants were randomly assigned to two arms:
|
|
| Outcomes | Primary outcomes were biochemical and virological responses. Other outcome reported was dose reduction. |
|
| Notes | The report is abstract; because the study has not been published yet, no data about inclusion and exclusion criteria were provided. We calculated sustained virological response based on reported proportions of participants because no absolute numbers of participants with sustained virological response were reported. Number of participants in each group is not reported, so we provisionally divided the total number of participants by two. Study author contacted for additional informations, but no reply obtained. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comments: Method used to perform sequence generation is not mentioned. |
| Allocation concealment (selection bias) | Unclear risk | Comments: Allocation concealment is not mentioned. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comments: Blinding to outcome assessors is not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: Information was insufficient to permit assessment of whether missing data in combination with the method used to handle missing data were likely to induce bias on the results. |
| Selective reporting (reporting bias) | Unclear risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Unclear risk | Comment: It was not possible to assess whether the trial was free of other sources of bias. |
Rahman 2007a.
| Methods | Study design: randomised controlled trial. ITT analysis: yes. Sample size calculation: not mentioned. |
|
| Participants | Country: not known. Total number (sample size): 310. Genotype: one. Previous HCV treatment: naive. Inclusion criteria: chronic hepatitis C infection. Exclusion criteria: not mentioned. |
|
| Interventions | Group 1: peginterferon alpha‐2b induction plus ribavirin.
Group 2: peginterferon alpha‐2b standard plus ribavirin.
Group 3: CIFN induction plus ribavirin.
Group 4: CIFN plus ribavirin.
|
|
| Outcomes | Sustained virological response. Adverse events. |
|
| Notes | Only published abstract; no data about inclusion and exclusion criteria were provided. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comments: Method used to perform sequence generation is not mentioned. |
| Allocation concealment (selection bias) | Unclear risk | Comments: Allocation concealment is not mentioned. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comments: Blinding to outcome assessors is not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: Information was insufficient to permit assessment of whether missing data in combination with the method used to handle missing data were likely to induce bias on the results. |
| Selective reporting (reporting bias) | Unclear risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Low risk | Comment: The trial seems to be free of other sources of bias. |
Rahman 2007b.
| Methods | Study design: randomised clinical trial. ITT analysis: yes. Sample size calculation: not mentioned. |
|
| Participants | Country: not known. Total number (sample size): 262. Genotype: two, three. Previous HCV treatment: naive. Inclusion criteria: chronic hepatitis C infection. Exclusion criteria: not mentioned. |
|
| Interventions | Group 1: peginterferon alpha‐2b plus ribavirin.
Group 2: consensus interferon plus ribavirin.
|
|
| Outcomes | Sustained virological response. Adverse events. |
|
| Notes | Only published abstract; no data about inclusion and exclusion criteria provided. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comments: Method used to perform sequence generation is not mentioned. |
| Allocation concealment (selection bias) | Unclear risk | Comments: Allocation concealment is not mentioned. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comments: Blinding to outcome assessors is not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: Information was insufficient to permit assessment of whether missing data in combination with the method used to handle missing data were likely to induce bias on the results. |
| Selective reporting (reporting bias) | Unclear risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Low risk | Comment: The trial seems to be free of other sources of bias. |
Roffi 2008.
| Methods | Randomised clinical trial with two parallel‐group design. Sample size calculation: yes. Intention‐to‐treat analysis: yes. |
|
| Participants | Country: Italy. Number of participants randomly assigned: 91; 64 men and 27 women. Participant status regarding previous antiviral therapy not described. Genotype: one, two, three All participants had bridging fibrosis or cirrhosis. Inclusion criteria.
Exclusion criteria.
|
|
| Interventions | Participants were randomly assigned to two groups (n = 93):
Ribavirin
Participants were followed‐up for 48 weeks after the end of treatment. |
|
| Outcomes | Primary outcomes were end of treatment and sustained virological responses. Other outcome reported is treatment discontinuation. |
|
| Notes | Follow‐up: Six and five participants discontinued treatment in peginterferon plus ribavirin and interferon plus ribavirin groups. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comments: Sequence generation was performed by a computer programme. |
| Allocation concealment (selection bias) | Low risk | Comments: central allocation concealment. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comments: It is mentioned only that the pathologists reviewed the biopsy specimens in a blinded manner. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: Incomplete outcome data were addressed adequately. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Low risk | Comment: The study seems to be free of other sources of bias. |
Scotto 2005.
| Methods | Randomised clinical trial with three parallel‐group design. Sample size calculation: not described. Intention‐to‐treat analysis: used. |
|
| Participants | Country: Italy. Number of participants randomly assigned: 78; 36 men and 42 women. All participants were treatment‐naive. All participants were infected with HCV genotype one‐b. Mean histological activity index score was 13.7 ± 2.9 in peginterferon plus ribavirin group, 13.7 ± 3.8 in lower‐dose interferon plus ribavirin group, and 13.9 ± 3.2 in higher‐dose interferon plus ribavirin group. Inclusion criteria.
Exclusion criteria.
|
|
| Interventions | Participants were randomly assigned to three groups.:
All participants also received ribavirin at 800 to 1000 to 1200 mg according to body weight (less than 65 kg, 65 to 85 kg, and more than 85 kg). Participants were followed up for 24 weeks after the end of treatment. |
|
| Outcomes | Primary outcomes were early, end of treatment, and sustained biochemical and virological responses. Other outcomes reported are histological changes, adverse events, and treatment discontinuations. |
|
| Notes | Follow‐up: Three participants discontinued treatment in peginterferon plus ribavirin group, four in lower‐dose interferon plus ribavirin group, and eight in higher‐dose interferon plus ribavirin group. Study author contacted for additional information, but no reply obtained. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: Randomisation was performed using a matrix of casual numbers, which generated the random allocation sequence table. |
| Allocation concealment (selection bias) | Low risk | Comments: central allocation concealment. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comments: Blinding to the outcome assessor is not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: Incomplete outcome data were addressed adequately. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Low risk | Comment: The study seems to be free of other sources of bias. |
Shobokshi 2003.
| Methods | Randomised clinical trial with three parallel‐group design. Sample size calculation: unclear, not described. Intention‐to‐treat analysis: unclear, not described. |
|
| Participants | Country: Saudi Arabia. Number of participants randomly assigned: 180; 119 men and 61 women. Participant status regarding previous antiviral therapy not described. Histological activity index (22) mean was 6.9 in peginterferon plus ribavirin group and 8.1 in interferon plus ribavirin group. All participants were infected with HCV genotype four. Mean HCV RNA levels (UI/mL) were 459,590 in peginterferon plus ribavirin group and 411,028 in interferon plus ribavirin group. Inclusion and exclusion criteria: none stated. |
|
| Interventions | Participants were randomly assigned in three groups to receive the following.
Participants were followed up for 24 weeks after the end of treatment. |
|
| Outcomes | Primary outcomes were sustained and end of treatment virological responses. Other outcomes reported are sustained and end of treatment biochemical responses. |
|
| Notes | The report is abstract because the study has not been published yet. The study was conducted by MOH PEG‐IFN Clinical Trial Group. Data were extracted from the primary reference and abstracts: Shobokshi, et al. Peginterferon alfa‐2a (40KDA) as a monotherapy or in combination with ribavirin significantly improves end of treatment response rate in hepatitis C virus genotype 4 chronic active hepatitis patients. Saudi Medical Journal 2003;24(Suppl 2):S92‐3; and Shobokshi et al. Early virological response at week 12 has positive predictive value for end of treatment response for hepatitis C virus genotype 4 chronic active hepatitis cases treated with combination therapy of peginterferon plus ribavirin. Saudi Medical Journal 2003;24(Suppl 2):S92‐3. Follow‐up: Seven participants discontinued treatment in peginterferon plus ribavirin group, four in peginterferon group, and one in interferon plus ribavirin group. Study author contacted for additional information, but no reply obtained. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Method of sequence generation was not mentioned. |
| Allocation concealment (selection bias) | Unclear risk | Comments: Allocation concealment is not mentioned. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comments: Blinding to the outcome assessor is not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: Information was insufficient to permit assessment of whether missing data in combination with the method used to handle missing data were likely to induce bias on the results. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Unclear risk | Comment: The trial may have conflict of interest bias. |
Sjögren 2007.
| Methods | Randomised clinical trial with two parallel‐group design. Intention‐to‐treat analysis: used. |
|
| Participants | Country: USA. Number of participants randomly assigned: 59. All participants are treatment‐naive. All participants are infected with HCV genotype one. Inclusion criteria: HCV RNA positive patients with liver biopsy compatible with chronic HCV infection Exclusion criteria: minimum haemoglobin 12g/L for women and 13g/L for men, WBC < 3x103/mm3, Neutrophil count < 1,5x103/mm3, platelet count < 75x103/mm3, prothrombin time > 2 sec above the upper limit of normal, severe psychiatric conditions, other causes of liver disease than HCV infection |
|
| Interventions | Participants are randomly assigned to two groups.
Treatment is planned for 48 weeks if serum HCV RNA is undetectable at week 24; otherwise, drugs are to be discontinued. |
|
| Outcomes | Primary outcome is sustained virological response, which will be determined at week 72. Other outcomes reported include end of treatment virological response and adverse events. |
|
| Notes | An ongoing study with interim results. No new publications regarding this data. Study author contacted for additional information, but no reply obtained. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomised using a computerized system". |
| Allocation concealment (selection bias) | Low risk | Comments: central allocation concealment. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Quote: "HCV RNA and HCV genotype were tested at a central laboratory". However, it is not clear whether adverse event outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: Incomplete outcome data were addressed adequately. |
| Selective reporting (reporting bias) | Low risk | Comment: All clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Low risk | Comment: The trial seems to be free of other sources of bias. |
Thakeb 2003.
| Methods | Study design: randomised clinical trial. ITT analysis: performed. |
|
| Participants | Country: not known. Total number (sample size): 100. Genotype: four. Previous HCV treatment. |
|
| Interventions | Group A (n = 51).
Group B (n = 49).
Ribavirin.
|
|
| Outcomes | Sustained virological response. Adverse events. |
|
| Notes | Published abstract only; no data about inclusion and exclusion criteria were provided. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comments: Method of sequence generation is not mentioned. |
| Allocation concealment (selection bias) | Unclear risk | Comments: Method of allocation concealment is not mentioned. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comments: It is not mentioned whether outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: Information was insufficient to permit assessment of whether missing data in combination with the method used to handle missing data were likely to induce bias on the results. |
| Selective reporting (reporting bias) | Unclear risk | Comment: It is unclear whether all predefined and clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Low risk | Comment: The study seems to be free of other sources of bias. |
Tsubota 2005.
| Methods | Randomised clinical trial with two parallel‐group design. Sample size calculation: not described. Intention‐to‐treat analysis: used. |
|
| Participants | Country: Japan. Number of participants randomly assigned: 48; 31 men and 17 women. All participants were treatment‐naive. None of the participants had cirrhosis. All participants were infected with HCV genotype one. Mean HCV RNA levels (kIU/mL) were 540 (120 to 2100) in peginterferon plus ribavirin group and 700 (250 to 2800) in interferon plus ribavirin group. Inclusion criteria.
Exclusion criteria.
|
|
| Interventions | Participants were randomly assigned to two groups.
For both treatment groups, ribavirin at the total dose of 600 mg to 1000 mg was administered for 48 weeks; the dose was adjusted according to body weight (600 mg for weight 60 kg or less, 800 mg for weight 60 kg to 80 kg, and 1000 mg for weight 80 kg to 100 kg). Both non‐pegylated peginterferon and ribavirin were concurrently initiated. Treatment was provided for 48 weeks, with a subsequent 24‐weeks follow‐up period. |
|
| Outcomes | Primary outcome was viral kinetics. Other outcomes reported include biochemical and virological responses. Limit for hepatitis C virus RNA detection was 50 IU/mL. |
|
| Notes | Additional data were obtained through personal communication with the study author. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: Randomisation was achieved through computer‐generated random numbers. |
| Allocation concealment (selection bias) | Low risk | Comment: Randomisation of eligible participants to treatment was carried out by an independent randomisation centre. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comments: It is not mentioned whether outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: Incomplete outcome data were addressed adequately. |
| Selective reporting (reporting bias) | Unclear risk | Comment: It is unclear whether all predefined and clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Low risk | Comment: The study seems to be free of other sources of bias. |
Wakil 2006.
| Methods | Study design: randomised trial. ITT analysis: not mentioned. |
|
| Participants | County: Egypt. Total number (sample size): 50. Age, years: 38.24 ± 8.56. Sex (male): not stated. Genotype: four. Previous HCV treatment: naive. Inclusion criteria: treatment‐naive chronic hepatitis C patients. Exclusion criteria: not mentioned. |
|
| Interventions | Group 1 (n = 18).
Group 2 (n = 17).
Group 3 (n = 15).
All three groups were given weight‐based ribavirin (1000 mg to 1200 mg). |
|
| Outcomes | Sustanied virological response. Adverse events. |
|
| Notes | Published abstract only; no data about inclusion and exclusion criteria were provided. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comments: Method of sequence generation is not mentioned. |
| Allocation concealment (selection bias) | Unclear risk | Comments: Method of allocation concealment is not mentioned. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Comments: It is not mentioned whether outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: Information was insufficient to permit assessment of whether missing data in combination with the method used to handle missing data were likely to induce bias on the results. |
| Selective reporting (reporting bias) | Unclear risk | Comment: It is unclear whether all predefined and clinically relevant and reasonably expected outcomes were reported. |
| Other bias | Low risk | Comment: The study seems to be free of other sources of bias. |
ALT = alanine aminotransferase. CIFN = consensus interferon. HCV = hepatitis C virus. HIV = human immunodeficiency virus. IFN = interferon. ITT = intention‐to‐treat analysis. MU = mega units. PCR = polymerase chain reaction. PEG IFN = pegylated interferon. WBC = white blood cells.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| ACTG 2005 | Randomised clinical trial in HIV co‐infected participants. |
| Ali 2010 | Not a randomised clinical trial. |
| APRICOT 2004 | Randomised clinical trial in HIV co‐infected participants. |
| Asahina 2004 | Not reported whether the trial was randomised. First study author contacted for additional information, but no reply obtained. |
| Gromova 2004 | Pilot study. |
| Laguno 2004 | Randomised clinical trial in HIV co‐infected participants. |
| RIBAVIC 2004 | Randomised clinical trial in HIV co‐infected participants. |
Differences between protocol and review
We redefined risk of bias subgroup analysis as an analysis between trials that are assessed to be at low or high risk of bias instead of trials that are assessed to be at low, unclear, or high risk of bias. This is in accordance with the recommendation from the Cochrane Handbook for Systematic Reviews of interventions (Higgins 2011) and previous research on the topic (Wood 2008; Savovic 2012; Savovic 2012a).
We changed the outcome measure 'failure of sustained virological response' to 'sustained virological response'.
We changed the sequence of outcomes in accordance with recommendations of the Cochrane Handbook for Systematic Reviews of interventions (Higgins 2011).
A Summary of findings table was planned at the review stage as guidelines about rating quality of evidence were issued after the protocol was published.
Outcomes of the protocol were as follows:
Serum (or plasma) sustained virological response: number of participants with undetectable hepatitis C virus RNA in serum by sensitivity testing six months after the end of treatment.
Liver‐related morbidity plus all‐cause mortality: number of participants who developed cirrhosis, ascites, variceal bleeding, hepatic encephalopathy, or hepatocellular carcinoma, or who died.
Adverse events: numbers and types of adverse events, defined as participants with any untoward medical occurrence not necessarily having a causal relationship to the treatment. We will report separately on adverse events that led to treatment discontinuation and those that did not lead to treatment discontinuation. A serious adverse event is defined according to the guidelines of the International Conference on Harmonisation (ICH‐GCP 1997) as any event that leads to death, is life threatening, requires in‐patient hospitalisation or prolongation of existing hospitalisation, or results in persistent or significant disability, as well as any important medical event that may have jeopardised the participant or required intervention to prevent it. All other adverse events will be considered non‐serious.
Updated outcomes became the following:
Primary outcomes
Liver‐related morbidity plus all‐cause mortality: number of participants who developed cirrhosis, ascites, variceal bleeding, hepatic encephalopathy, or hepatocellular carcinoma, or who died.
Adverse events leading to treatment discontinuation.
Other adverse events: haematological effects, fatigue and flu‐like symptoms, psychiatric symptoms, dermatological symptoms, thyroid malfunction, gastrointestinal symptoms (other than liver related).
Quality of life.
Secondary outcome
Sustained virological response: number of participants with undetectable hepatitis C virus RNA in serum by sensitivity testing six months after the end of treatment.
In our protocol, we included baseline imbalance and early stopping as potential bias components. According to updated guidelines from The Cochrane Collaboration, these two domains should no longer be used (Gluud 2013).
Contributions of authors
Goran Hauser performed the literature search, performed data extraction, assessed the risk of bias in included trials, performed statistical analyses in RevMan including TSA, contributed to the interpretation of results, presented a Summary of Findings table, and drafted the review. Tahany Awad performed the literature search, performed data extraction, assessed the risk of bias in included trials, performed statistical analyses in RevMan, and contributed to the interpretation of results. Jesper Brok performed data extraction, assessed the risk of bias in included trials, contributed to the interpretation of results, and revised the review. Kristian Thorlund assessed the risk of bias associated with incomplete outcome data, performed statistical analyses in RevMan including TSA, contributed to the interpretation of results, and revised the review. Davor Stimac, Mahasen Mabrouk, Christian Gluud, and Lise Lotte Gluud acted as arbitrators for disagreements in data extraction and the bias risk assessment, contributed to the interpretation of results, and revised the review. All authors approved of the review.
Sources of support
Internal sources
Copenhagen Trial Unit, Centre for Clinical Intervention Research, Rigshospitalet, Copenhagen University Hospital, Denmark.
External sources
-
ERASMUS project, Other.
- ERASMUS project, Croatia Erasmus staff mobility was organised by the University of Rijeka and realised with the financial support of the European Commission under the auspices of the LLP Erasmus Programme.
Declarations of interest
Tahany Awad acted as an invited speaker for Roche and is now employed by AbbVie.
New
References
References to studies included in this review
Al‐Faleh 2004 {published data only}
- Alfaleh FZ, Hadad Q, Khuroo MS, Aljumah A, Algamedi A, Alashgar H, et al. Peginterferon alpha‐2b plus ribavirin compared with interferon alpha‐2b plus ribavirin for initial treatment of chronic hepatitis C in Saudi patients commonly infected with genotype 4. Liver International 2004;24:568‐74. [DOI] [PubMed] [Google Scholar]
Bruno 2004 {published data only}
- Bruno S, Camma C, Marco V, Rumi M, Vinci M, Camozzi M, et al. Peginterferon alfa‐2b plus ribavirin for naive patients with genotype 1 chronic hepatitis C: a randomized controlled trial. Journal of Hepatology 2004;41:474‐81. [DOI] [PubMed] [Google Scholar]
- Bruno S, Camma C, Marco V, Rumi MG, Vinci M, Camozzi M, et al. Chronic hepatitis C (CH‐C) genotype 1: an independent, multicenter RCT comparing PEG‐IFN alfa‐2b 12 kD plus ribavirin (RBV) and IFN alfa‐2b plus RBV in naive patients. Journal of Hepatology 2003;38(Suppl 2):131‐2. [Google Scholar]
Cariti 2002 {published data only}
- Cariti G, Andreoni M, Calleri G, Manca A, Rosina F, Sartori M, et al. PEG‐INF alpha‐2A (40KD) plus ribavirin (RBV) vs IFN alpha‐2A (ROFERON‐A) in naive patients with chronic hepatitis C (CHC) and genotype 1 [AASLD abstract]. Hepatology 2002;36(4 Pt 2):595A. [Google Scholar]
Derbala 2005 {published data only}
- Derbala M, Amer A, Bener B, Lopez A, Omar M, Ghannam M. Pegylated interferon‐alpha 2b‐ ribavirin combination in Egyptian patients with genotype 4 chronic hepatitis. Journal of Viral Hepatitis 2005;12(4):380‐5. [DOI: 10.1111/j.1365-2893.2005.00604.x] [DOI] [PubMed] [Google Scholar]
Derbala 2006 {published data only}
- Derbala MF, Kaabi SR, Dweik NZ, Pasic F, Butt MT, Yakoob R, et al. Treatment of hepatitis C virus genotype 4 with pegylated interferon alpha 2a:Impact of bilharziasis and fibrosis stage. World Journal of Gastroenterology 2006;12(35):5692‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dollinger 2005 {published data only}
- Dollinger MM, Dridi Y, Lesske J, Behl S, Fleig WE. Efficacy of daily consensus interferon and ribavirin compared to peg‐interferon alpha‐2B and interferon in non‐responders with chronic hepatitis C [AASLD abstract]. Hepatology 2005;42(4 Suppl 1):691‐2. [Google Scholar]
Esmat 2003 {published data only}
- Esmat GH, Abouzied A, Abdel‐Hamid M, Mohamed MK, Zalata K, Raziky MS, et al. Results of a randomized clinical trial of genotype‐4 infected subjects when treated with standard or pegylated interferon alfa‐2b in combination with ribavirin [AASLD abstract]. Hepatology 2003;38(4 Suppl 1):314A‐315A. [Google Scholar]
Fargion 2004 {published data only}
- Fargion S, Borzio M, Cargnel A. End of treatment and sustained response to peginterferon alfa‐2a (40kD) (Pegasys) plus ribavirin (RBV) (Copegus) and amantadine (AMA), and to induction therapy with interferon (IFN) alfa‐2a (Roferon‐A) plus RBV and AMA in IFN/RBV nonresponders with chronic hepatitis C (CHC) [AASLD abstract]. Hepatology 2003;38(4 Suppl 1):733A. [Google Scholar]
- Fargion S, Borzio M, Cargnel A. Peginterferon alfa‐2a (40kD) (Pegasys) plus ribavirin (RBV) and amantadine (AMA) vs induction therapy with interferon alfa‐2a (Roferon‐A) plus RBV and AMA in IFN/RBV nonresponder patients with chronic hepatitis C (CHC). Journal of Hepatology 2003;38(Suppl 2):139‐40. [Google Scholar]
- Fargion S, Borzio M, Cargnel A. Peginterferon alfa‐2a (40kD) (Pegasys) plus ribavirin (RBV) and amantadine (AMA) vs induction therapy with interferon alfa‐2a (Roferon‐A) plus RBV and AMA in IFN/RBV nonresponder patients with chronic hepatitis C (CHC) [AASLD abstract]. Hepatology 2002;36(4 Pt 2):572A. [Google Scholar]
- Fargion S, Borzio M, Maraschi A, Cargnel A. Sustained virological response (SVR) to peginterferon alfa‐2a (40 kD) (Pegasys) plus ribavirin (RBV) and amantadine (AMA) vs induction therapy with interferon alfa‐2a (Roferon‐A) plus RBV and AMA in IFN/RBV non responders (NR) with chronic hepatitis C (CHC). Journal of Hepatology 2004;40(Suppl 1):140. [Google Scholar]
Fried 2002 {published data only}
- Bosques‐Padilla F, Trejo‐Estrada R, Campollo‐Rivas O, Cortez‐Hernandez C, Dehesa‐Violante M, Maldonado‐Garza H, et al. Peginterferon alfa‐2a plus ribavirin for treating chronic hepatitis C virus infection: analysis of Mexican patients included in a multicenter international clinical trial. Annals of Hepatology 2003;2(3):135‐9. [PubMed] [Google Scholar]
- Fried MW, Shiffman ML, Reddy KR, Smith C, Marinos G, Goncales FL Jr, et al. Peginterferon alfa‐2a plus ribavirin for chronic hepatitis C virus infection. New England Journal of Medicine 2002;347(13):975‐82. [DOI] [PubMed] [Google Scholar]
- Hassanein T, Cooksley G, Sulkowski M, Smith C, Marinos G, Lai M‐Y, et al. The impact of peginterferon alfa‐2a plus ribavirin combination therapy on health‐related quality of life in chronic hepatitis C. Journal of Hepatology 2004;40(4):675‐81. [DOI] [PubMed] [Google Scholar]
- Hassanein TI, Cooksley G, Sulkowski M, Smith C, Marinos G, Lai M‐Y, et al. Treatment with 40 kDa peginterferon alfa‐2a (Pegasys) in combination with ribavirin significantly enhances quality of life compared with interferon alfa‐2b plus ribavirin [AASLD abstract]. Hepatology 2001;34(4 Pt 2):243A. [Google Scholar]
- Hassanein TI, Cooksley WGE, Sulkowski M, Smith C, Marinos G, Lai M‐Y, et al. QOL benefits observed as early as week 2 with peginterferon alfa‐2a (40kD) (Pegasys) in combination with ribavirin (RBV) versus interferon alfa‐2b plus RBV [EASL abstract]. Journal of Hepatology 2002;36(1):110. [Google Scholar]
- Herrmann E, Lee J‐H, Marinos G, Modi M, Zeuzem S. Effect of ribavirin on hepatitis C viral kinetics in patients treated with pegylated interferon. Hepatology 2003;37(6):1351‐8. [DOI] [PubMed] [Google Scholar]
- Lutchman G, Hoofnagle JH. Viral kinetics in hepatitis C. Hepatology 2003;37(6):1257‐9. [DOI] [PubMed] [Google Scholar]
- Sullivan SD, Craxi A, Alberti A, Giuliani G, Carli C, Wintfeld N, et al. Cost effectiveness of peginterferon alpha‐2a plus ribavirin versus interferon alpha‐2b plus ribavirin as initial therapy for treatment‐naive chronic hepatitis C. Pharmacoeconomics 2004;22(4):257‐65. [DOI] [PubMed] [Google Scholar]
- Sullivan SD, Green J, Patel KK, Craxi A, Alberti A, Giuliani G, et al. A comparison of cost‐effectiveness of peginterferon alfa‐2a (40kD) (Pegasys) plus ribavirin (Copegus) vs interferon alfa‐2b plus ribavirin as first treatment of chronic hepatitis C (CHC). Journal of Hepatology 2003;38(Suppl 2):174‐5. [Google Scholar]
- Sullivan SD, Jensen DM, Bernstein DE, Hassanein TI, Foster GR, Lee SS, et al. Cost‐effectiveness of combination peginterferon alpha‐2a and ribavirin compared with interferon alpha‐2b and ribavirin in patients with chronic hepatitis C. American Journal of Gastroenterology 2004;99:1490‐6. [DOI] [PubMed] [Google Scholar]
- Zeuzem S, Herrmann E, Lee J‐H, Marinos G, Modi M, Roth WK. Effect of ribavirin on viral kinetics in hepatitis C virus genotype 1 infected patients treated with pegylated interferon alpha2a [AASLD abstract]. Hepatology 2001;34(4 Pt 2):558A. [Google Scholar]
Hinrichsen 2002 {published data only}
- Hinrichsen H, Buggisch P, Nasser S, Foelsch UR. A prospective randomised 24 week trial of peg‐interferon alpha2b plus ribavirin versus standard combination therapy in untreated hepatitis C genotype 2 and 3 patients [AASLD abstract]. Hepatology 2002;36(4 Pt 2):311A. [Google Scholar]
Horsmans 2008 {published data only}
- Horsmans Y, Colle I, Vlierberghe H, Langlet P, Adler M, Bourgeois N, et al. Weekly pegylated Interferon alpha‐2b vs daily interferon a‐2b versus standard regimen of Interferon a‐2b in the treatment of patients with chronic hepatitis C virus infection. Acto Gastro‐Enterologica Belgica 2008;71(3):293‐7. [PubMed] [Google Scholar]
Izumi 2004 {published data only}
- Izumi N, Asahina Y, Kurosaki M, Uchihara M, Nishimura Y, Inoue K, et al. A comparison of the exponential decay slope between PEG‐IFN alfa‐2b/ribavirin and IFN alfa‐2b/ribavirin combination therapy in patients with chronic hepatitis C. Intervirology 2004;47:102‐7. [DOI] [PubMed] [Google Scholar]
Lee 2005 {published data only}
- Lee SD, Yu ML, Cheng PN, Lai MY, Chao YC, Hwang SJ, et al. Comparison of a 6‐month course peginterferon alpha‐2b plus ribavirin and interferon alpha‐2b plus ribavirin in treating Chinese patients with chronic hepatitis C in Taiwan. Journal of Viral Hepatitis 2005;12:283‐91. [DOI] [PubMed] [Google Scholar]
Mangia 2005 {published data only}
- Mangia A, Ricci GL, Persico M, Minerva N, Caretta V, Bacca D, et al. A randomized controlled trial of peginterferon alpha‐2a (40 kD) or interferon alpha‐2a plus ribavirin and amantadine vs interferon alpha‐2a and ribavirin in treatment‐naive patients with chronic hepatitis C. Journal of Viral Hepatitis 2005;12(3):292‐9. [DOI] [PubMed] [Google Scholar]
Manns 2001 {published data only}
- Buti M, Medina M, Casado MA, Wong JB, Fosbrook L, Esteban R. A cost‐effectiveness analysis of peginterferon alfa‐2b plus ribavirin for the treatment of naive patients with chronic hepatitis C. Alimentary Pharmacology & Therapeutics 2003;17:687‐94. [DOI] [PubMed] [Google Scholar]
- Condat B. Peginterferon alpha‐2b plus ribavirin compared with interferon alpha‐2b and ribavirin for the treatment of chronic hepatitis C: A randomized trial. Hepato‐Gastroenterology 2002;9(2):141‐2. [Google Scholar]
- Gish R, Bzowej N, Brooks L, Brass C, Weng W. Treatment with pegylated interferon alfa‐2b in combination with ribavirin improved health‐related quality of life compared with interferon alfa‐2b plus ribavirin in chronic hepatitis C [AASLD abstract]. Hepatology 2002;36(4 Pt 2):582A. [Google Scholar]
- Jen J, Laughlin M, Chung C, Heft S, Affrime MB, Gupta SK, et al. Ribavirin dosing in chronic hepatitis C: application of population pharmacokinetic‐pharmacodynamic models. Clinical Pharmacology and Therapeutics 2002;72(4):349‐61. [DOI] [PubMed] [Google Scholar]
- Manns MP, McHutchison JG, Gordon S, Rustgi V, Shiffman ML, Lee WM, et al. Peginterferon alfa‐2b plus ribavirin compared to interferon alfa‐2b plus ribavirin for the treatment of chronic hepatitis C: 24 week treatment analysis of a multicenter, multinational phase III randomized controlled trial [AASLD abstract]. Hepatology 2000;32(4 Pt 2):297A. [Google Scholar]
- Manns MP, McHutchison JG, Gordon SC, Rustgi VK, Shiffman M, Reindollar R, et al. Peginterferon alfa‐2a plus ribavirin compared with interferon alfa‐2b plus ribavirin for initial treatment of chronic hepatitis C: a randomised trial. Lancet 2001;358:958‐65. [DOI] [PubMed] [Google Scholar]
- McHutchison J, Manns M, Harvey J, Albrecht JK. Adherence to therapy enhances sustained response in chronic hepatitis C patients receiving peg‐interferon alfa‐2b plus ribavirin [abstract]. Journal of Hepatology 2001;34(1):2‐3. [Google Scholar]
- McHutchison JG, Manns M, Patel K, Poynard T, Lindsay KL, Trepo C, et al. Adherence to combination therapy enhances sustained response in genotype‐1‐infected patients with chronic hepatitis C. Gastroenterology 2002;123(4):1061‐9. [DOI] [PubMed] [Google Scholar]
- McHutchison JG, Manns MP, Harvey J, Garaud J‐J, Albrecht J. Adherence to therapy enhances sustained response in chronic hepatitis C patients receiving peginterferon alfa 2b plus ribavirin. Hepatology 2001;34(4 Pt 2):417A. [Google Scholar]
- McHutchison JG, Manns MP, Ling M‐H, Albrecht JK. Peginterferon alfa‐2b plus ribavirin for treatment of chronic hepatitis C: is patient gender a confounding factor for sustained virological response when ribavirin dose is expressed as mg/kg of body weight? [AASLD abstract]. Hepatology 2001;34(4 Pt 2):329A. [Google Scholar]
- Poynard T, McHutchison J, Manns M, Myers RP, Albrecht J. Biochemical markers as surrogate markers of liver fibrosis and activity in patients infected by hepatitis C virus: an example in a randomized trial of pegylated‐interferon alpfa‐2b and ribavirin combination [AASLD abstract]. Hepatology 2002;36(4 Pt 2):351A. [Google Scholar]
- Poynard T, McHutchison J, Manns M, Myers RP, Albrecht J. Biochemical surrogate markers of liver fibrosis and activity in a randomized trial of peginterferon alfa‐2b and ribavirin. Hepatology 2003;38(2):481‐92. [DOI] [PubMed] [Google Scholar]
- Poynard T, Ratziu V, McHutchison J, Manns M, Goodman Z, Zeuzem S, et al. Effect of treatment with peginterferon or interferon alfa‐2b and ribavirin on steatosis in patients infected with hepatitis C. Hepatology 2003;38(1):75‐85. [DOI] [PubMed] [Google Scholar]
- Siebert U, Sroczynski G, Rossol S, Wasem J, Ravens‐Sieberer U, Kurth BM, et al. Cost effectiveness of peginterferon alpha‐2b plus ribavirin versus interferon alpha‐2b plus ribavirin for initial treatment of chronic hepatitis C. Gut 2003;52:425‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong JB, Davis GL, McHutchison JG, Manns MP, Albrecht JK. Economic and clinical effects of evaluating rapid viral response to peginterferon alfa‐2b plus ribavirin for the initial treatment of chronic hepatitis C. American Journal of Gastroenterology 2003;98(11):2354‐62. [DOI] [PubMed] [Google Scholar]
Napoli 2005 {published data only}
- Napoli N, Giannelli G, Parisi CV, Antonaci A, Maddalena G, Antonaci S. Predictive value of early virological response to treatment with different interferon‐based regimens plus ribavirin in patients with chronic hepatitis C. New Microbiologica 2005;28:13‐21. [PubMed] [Google Scholar]
Nevens 2010 {published data only}
- Nevens F, Vlierberghe H, D'Heygere E, Delwaide J, Adler M, Henrion J, et al. A randomised, open‐label, multicenter study evaluating the efficacy of peginterferon alfa‐2a versus interferon alfa‐2a, in combination with ribavirin, in naïve and relapsed chronic hepatitis C patients. Acta Gastroenterologica Belgica 2010;73:223‐8. [PubMed] [Google Scholar]
PRETTY 2005 {published data only}
- Mangia A, Cimino L, Persico M, Demelia L, Rumi M, Spinzi G, et al. Enhanced response to peginterferon‐alpha‐2a‐based triple therapy in previously non‐responsive chronic hepatitis C: final results of PRETTY study. Journal of Hepatology 2005;42(2):200‐1. [Google Scholar]
Rahman 2007a {published data only}
- Rahman F, Schuchmann M, Lohr HF, Link R, Buggisch P, Fuchs M, et al. Daily consensus interferon versus peg‐interferon alfa2b with weight based or 800 mg ribavirin in treatment‐naive patients with chronic hepatitis C genotype 1. Hepatology 2007;46(4 Suppl 1):826A. [Google Scholar]
Rahman 2007b {published data only}
- Rahman F, Schuchmann M, Lohr HF, Link R, Buggisch P, Fuchs M, et al. Daily consensus interferon versus peg‐interferon alfa2b with weight based or 800 mg ribavirin in treatment‐naive patients with chronic hepatitis C genotypes 2 or 3. Hepatology 2007;46(4 Suppl 1):826A. [Google Scholar]
Roffi 2008 {published data only}
- Roffi L, Colloredo G, Poggio P, Fornaciari G, Castagnetti E, Ceriani R, et al. Efficacy and safety of low doses of interferon (IFN) alfa‐2b plus ribavirin (RBV) in advanced HCV related liver disease [AASLD abstract]. Hepatology 2004;40(4 Suppl 1):322A. [Google Scholar]
- Roffi L, Colloredo G, Pioltelli P, Bellati G, Pozzpi M, Parravicini P, et al. Pegylated interferon‐alpha2b plus ribavirin: an efficacious and well‐tolerated treatment regimen for patients with hepatitis C virus related histologically proven cirrhosis. Antiviral Therapy 2008;13(5):663‐73. [PubMed] [Google Scholar]
Scotto 2005 {published data only}
- Scotto G, Fazio V, Palumbo E, Cibelli DC, Saracino A, Angarano G. Treatment of genotype 1b HCV‐related chronic hepatitis: efficacy and toxicity of three different interferon alfa‐2b/ribavirin combined regimens in naive patients. New Microbiologica 2005;28:23‐9. [PubMed] [Google Scholar]
Shobokshi 2003 {published data only}
- Shobokshi A, Serebour FE, Skakni L, Al‐Jasser N, Tantawi AO, Sabah A, et al. Combination therapy of peginterferon alfa‐2a (40kD) (Pegasys(R)) and ribavirin (Copegus(R)) significantly enhance sustained virological and biochemical response rate in chronic hepatitis C genotype 4 patients in Saudi Arabia [AASLD abstract]. Hepatology 2003;38(4 Suppl 1):636A. [Google Scholar]
- Shobokshi O, Serebour F, Skakni L, Tantawi A, Dinish T, Al Quaiz M, et al. Efficacy of pegylated (40kDa) IFN alfa‐2a (Pegasys) plus ribavirin in the treatment of hepatitis C genotype 4 chronic active patients in Saudi Arabia. Journal of Hepatology 2002;36(Suppl 1):129. [Google Scholar]
- Shobokshi O, Serebour FE, Skakni L, Al‐Jaser N, Tantawe AO, Sabah A, et al. Early virological response at week 12 has positive predictive value for end of treatment response for hepatitis C virus genotype 4 chronic active hepatitis cases treated with combination therapy of pegylated interferon plus ribavirin. Saudi Medical Journal 2003;24(Suppl 2):S92‐S93. [Google Scholar]
- Shobokshi O, Serebour FE, Skakni L, Al‐Jaser N, Tantawe AO, Sabah A, et al. Pegylated interferon alfa‐2a (40KDA) as a monotherapy or in combination with ribavirin significantly improves end of treatment response rate in hepatitis C virus genotype 4 chronic active hepatitis patients. Saudi Medical Journal 2003;24(Suppl 2):S92‐S93. [Google Scholar]
Sjögren 2007 {published data only}
- Sjogren MH, Sjogren R, Lyons MF, Ryan M, Santoro J, Smith C, et al. Antiviral response of HCV genotype 1 to consensus interferon and ribavirin versus pegylated interferon and ribavirin. Digestive Diseases and Sciences 2007;52(6):1540‐7. [DOI] [PubMed] [Google Scholar]
Thakeb 2003 {published data only}
- Thakeb FIA, Omar MM, Awady MM, Isshak SY. Randomized controlled trial of peginterferon alfa‐2a plus ribavirin for chronic hepatitis C virus‐genotype 4 among Egyptian patients [AASLD abstract]. Hepatology 2003;38(4 Suppl 1):278A. [Google Scholar]
Tsubota 2005 {published data only}
- Tsubota A, Arase Y, Someya T, Suzuki Y, Suzuki F, Saitoh S, et al. Early viral kinetics and treatment outcome in combination of high‐dose interferon induction vs. pegylated interferon plus ribavirin for naive patients infected with hepatitis C virus of genotype 1b and high viral load. Journal of Medical Virology 2005;75:27‐34. [DOI] [PubMed] [Google Scholar]
Wakil 2006 {published data only}
- Wakil RM, Montasser MF, Mansour MA, Salman TA, El‐Batanony MH, Helail EH, et al. Peginterferon alpha‐2b plus ribavirin versus interferon alpha‐2b plus ribavirin for treatment of chronic hepatitis C in treatment‐naive Egyptian patients. Journal of Clinical Virology 2006;36:S142‐S143. [Google Scholar]
References to studies excluded from this review
ACTG 2005 {published data only}
- Chung RT, Andersen J, Volberding P, Robbins GK, Liu T, Sherman KE, et al. Peginterferon alfa‐2a plus ribavirin versus interferon alfa‐2a plus ribavirin for chronic hepatitis C in HIV‐coinfected persons. New England Journal of Medicine 2004;351(5):451‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman KE, Shire NJ, Rouster SD, Peters MG, Koziel MJ, Chung RT, et al. Viral kinetics in hepatitis C or hepatitis C/human immunodeficiency virus‐infected patients. Gastroenterology 2005;128(2):313‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ali 2010 {published data only}
- Ali S, Nazir G, Khan SA, Iram S, Fatima F. Comparative therapeutic response to pegylated interferon plus ribavirin versus interferon alpha‐2b in chronic hepatitis C patients. Journal of Ayub Medical College 2010;22:127‐30. [PubMed] [Google Scholar]
APRICOT 2004 {published data only}
- Mauss S, Valenti W, DePamphilis J, Duff F, Cupelli L, Passe S, et al. Risk factors for hepatic decompensation in patients with HIV/HCV coinfection and liver cirrhosis during interferon‐based therapy. AIDS 2004;18(13):F21‐F25. [DOI] [PubMed] [Google Scholar]
- Torriani FJ, Ribeiro RM, Gilbert TL, Schrenk UM, Clauson M, Pacheco DM, et al. Hepatitis C virus (HCV) and human immunodeficiency virus (HIV) dynamics during HCV treatment in HCV/HIV coinfection. Journal of Infectious Diseases 2003;188:1498‐507. [DOI] [PubMed] [Google Scholar]
- Torriani FJ, Rodriguez‐Torres M, Rockstroh JK, Lissen E, Gonzalez‐Garcia J, Lazzarin A, et al. Peginterferon alfa‐2a plus ribavirin for chronic hepatitis C virus infection in HIV‐infected patients. New England Journal of Medicine 2004;351(5):438‐50. [DOI] [PubMed] [Google Scholar]
Asahina 2004 {published data only}
- Asahina Y, Izumi N, Onuki Y, Ueda K, Nishimura Y, Nakanishi H, et al. Enhanced interferon (IFN)‐stimulated gene expression and HCV dynamics in patients treated with pegylated IFN alfa 2b and ribavirin: effect of pharmacokinetic change of IFN and ribavirin. Hepatology 2004;40(4 Suppl 1):338A. [Google Scholar]
Gromova 2004 {published data only}
- Gromova NI, Bogomolov BP. Comparative efficacy of combined treatment with Intron a and Pegintron in combination with ribavirin in patients with chronic hepatitis C. Terapevticheskii Arkhiv 2004;76(2):31‐5. [PubMed] [Google Scholar]
Laguno 2004 {published data only}
- Laguno M, Murillas J, Blanco JL, Martinez E, Miquel R, Sanchez‐Tapias JM, et al. Peginterferon alfa‐2b plus ribavirin compared with interferon alfa‐2b plus ribavirin for treatment of HIV/HCV co‐infected patients. AIDS 2004;18(13):F27‐F36. [DOI] [PubMed] [Google Scholar]
RIBAVIC 2004 {published data only}
- Carrat F, Bani‐Sadr F, Pol S, Rosenthal E, Lunel‐Fabiani F, Benzekri A, et al. Pegylated interferon alfa‐2b vs standard interferon alfa‐2b, plus ribavirin, for chronic hepatitis C in HIV‐infected patients. JAMA 2004;292(23):2839‐48. [DOI] [PubMed] [Google Scholar]
- Lunel F, Pivert A, Payan C. Comparison of HCV RNA and HCV core antigen kinetics in the follow up of a therapeutic protocol in HCV‐HIV co‐infected patients (RIBAVIC). Journal of Hepatology 2004;40(Suppl 1):144‐5. [Google Scholar]
- Pol S, Carrat F, Bani‐Sadr F, Rosenthal E, Lunel F, Morand P, et al. Final results of ANRS HC02‐RIBAVIC: a randomized controlled trial of pegylated‐interferon alfa‐2b plus ribavirin vs interferon alfa‐2b plus ribavirin for the initial treatment of chronic hepatitis C in HIV co‐infected [AASLD abstract]. Hepatology 2004;40(4):315A. [Google Scholar]
- Pol S, Carrat F, Bani‐Sadr F, Rosenthal E, Lunel F, Morand P, et al. Final results of ANRS HC02‐RIBAVIC: a randomized controlled trial of pegylated‐interferon alpha‐2b plus ribavirin vs interferon alpha‐2b plus ribavirin for naive HCV‐HIV co‐infected patients. Journal of Hepatology 2005;42(Suppl 2):10‐1. [Google Scholar]
Additional references
Adeel 2009
- Adeel AB, Xiaoqiang Wang, Charity GM. Effect of hepatitis C virus and its treatment on survival. Hepatology 2009;50(2):387‐92. [DOI] [PubMed] [Google Scholar]
Aljumah 2013
- Aljumah AA, Murad MH. Pegylated versus standard interferon plus ribavirin in chronic hepatitis C genotype 4: a systematic review and meta‐analysis. Hepatology Research 2013;43(12):1255‐63. [DOI: 10.1111/hepr.12084] [DOI] [PubMed] [Google Scholar]
Awad 2010
- Awad T, Thorlund K, Hauser G, Stimac D, Mabrouk M, Gluud C. Peginterferon alpha‐2a is associated with higher sustained virological response than peginterferon alfa‐2b in chronic hepatitis C: systematic review of randomized trials. Hepatology 2010;51:1176‐84. [DOI: 10.1002/hep.23504.] [DOI] [PubMed] [Google Scholar]
Bailon 2001
- Bailon P, Palleroni A, Schaffer CA, Spence CL, Fung W‐J, Porter JE, et al. Rational design of a potent, long‐lasting form of interferon: a 40 kDa branched polyethylene glycol‐conjugated interferon alpha‐2a for the treatment of hepatitis. Bioconjugate Chemistry 2001;12(2):195‐202. [DOI] [PubMed] [Google Scholar]
Bangalore 2008
- Bangalore S, Wetterslev J, Pranesh S, Sawhney S, Gluud C, Messerli F. Perioperative beta blockers in patients having non‐cardiac surgery: a meta‐analysis. Lancet 2008;372(9654):1962‐76. [DOI] [PubMed] [Google Scholar]
Benvegnu 2001
- Benvegnu L, Alberti A. Patterns of hepatocellular carcinoma development in hepatitis B virus and hepatitis C virus‐related cirrhosis. Antiviral Research 2001;52:199‐207. [DOI] [PubMed] [Google Scholar]
Bradburn 2006
- Bradburn MJ, Deeks JJ, Berlin JA, Localio AR. Much ado about nothing: a comparison of the performance of meta‐analytical methods with rare events. Statistics in Medicine 2006;26(1):53‐77. [DOI] [PubMed] [Google Scholar]
Brok 2008
- Brok J, Thorlund K, Gluud C, Wetterslev J. Trial sequential analysis reveals insufficient information size and potentially false positive results in many meta‐analyses. Journal of Clinical Epidemiology 2008;61(8):763‐9. [DOI] [PubMed] [Google Scholar]
Brok 2009
- Brok J, Thorlund K, Gluud C, Wetterslev J. Apparently conclusive meta‐analyses may be inconclusive—trial sequential analysis adjustment for random error risk in conclusive Cochrane neonatal meta‐analyses. International Journal of Epidemiology 2009;38(1):287‐98. [DOI: 10.1093/ije/dyn188] [DOI] [PubMed] [Google Scholar]
Brok 2009a
- Brok J, Gluud LL, Gluud C. Ribavirin plus interferon versus interferon for chronic hepatitis C. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD005445.pub2] [DOI] [PubMed] [Google Scholar]
Chan 2013
- Chan AW, Tetzlaff JM, Gøtzsche PC, Altman DG, Mann H, Berlin JA, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ (Clinical Research Ed.) 2013;8:346:e7586. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chander 2002
- Chander G, Sulkowski MS, Jenckes MW, Torbenson MS, Herlong HF, Bass EB, et al. Treatment of chronic hepatitis C: a systematic review. Hepatology 2002;36(S1):135‐44. [DOI] [PubMed] [Google Scholar]
Constant 2005
- Constant A, Castera L, Dantzer R, Couzigou P, Ledinghen V, Demotes‐Mainard J, et al. Mood alterations during interferon‐alfa therapy in patients with chronic hepatitis C: evidence for an overlap between manic/hypomanic and depressive symptoms. Journal of Clinical Psychiatry 2005;66:105‐23. [DOI] [PubMed] [Google Scholar]
CTU 2011
- Copenhagen Trial Unit. TSA—Trial Sequential Analysis. ctu.dk/tsa/ 2011 (accessed 28 May 2013).
Davis 1999
- Davis GL. Hepatitis C virus genotypes and quasispecies. American Journal of Medicine 1999;107(6B):S21‐S26. [DOI] [PubMed] [Google Scholar]
DeMets 1987
- DeMets DL. Methods of combining randomized clinical trials: strengths and limitations. Statistics in Medicine 1987;6(3):341‐50. [DOI] [PubMed] [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta‐analysis in clinical trials. Controlled Clinical Trials 1986;7(3):177‐88. [DOI] [PubMed] [Google Scholar]
Dhillon 2010
- Dhillon S, Kaker A, Dosanjh A, Japra D, Vanthiel DH. Irreversible pulmonary hypertension associated with the use of interferon alpha for chronic hepatitis C. Digestive Diseases and Sciences 2010;55:1785‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
EASL 2012
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines: management of hepatitis C virus infection. Journal of Hepatology 2011;55:245‐64. [DOI] [PubMed] [Google Scholar]
Fattovich 2002
- Fattovich G, Pantalena M, Zagni I, Realdi G, Schalm SW, Christensen E, European Concerted Action on Viral Hepatitis (EUROHEP). Effect of hepatitis B and C virus infections on the natural history of compensated cirrhosis: a cohort study of 297 patients. American Journal of Gastroenterology 2002;97(11):288‐95. [DOI] [PubMed] [Google Scholar]
Foster 2004
- Foster GR. Pegylated interferons: chemical and clinical differences. Alimentary Pharmacology & Therapeutics 2004;20(8):825‐30. [DOI] [PubMed] [Google Scholar]
Ghany 2009
- Ghany MG, Strader DB, Wright T, Thomas DL, Seeff LB, American Association for the Study of Liver Disease. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology 2009;49(4):1335‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Glue 2000
- Glue P, Fang JWS, Rouzier‐Panis R, Raffanel C, Sabo R, Gupta SK, et al. Pegylated interferon‐[alpha]2b: pharmacokinetics, pharmacodynamics, safety, and preliminary efficacy data. Clinical Pharmacology and Therapeutics 2000;68(5):556‐67. [DOI] [PubMed] [Google Scholar]
Gluud 2007
- Gluud C, Brok J, Gong Y, Koretz RL. Hepatology may have problems with putative surrogate outcome measures. Journal of Hepatology 2007;46(4):734‐42. [DOI] [PubMed] [Google Scholar]
Gluud 2013
- Gluud C, Nikolova D, Klingenberg SL, Alexakis N, Als‐Nielsen B, Colli A, et al. Cochrane Hepato‐Biliary Group. About The Cochrane Collaboration (Cochrane Review Groups (CRGs)). 2013, Issue 12. Art. No.: LIVER.
Gurusamy 2013
- Gurusamy KS, Wilson E, Koretz RL, Allen VB, Davidson BR, Burroughs AK, et al. Is sustained virological response a marker of treatment efficacy in patients with chronic hepatitis C viral infection with no response or relapse to previous antiviral intervention?. PLoS ONE 2013;8(12):e83313. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2008
- Guyatt GH, Oxman AD, Vist G, Kunz R, Falck‐Ytter Y, Alonso‐Coello P, et al. Rating quality of evidence and strength of recommendations GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clinical Research Ed) 2008;336:924‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hadziyannis 2004
- Hadziyannis SJ, Sette H, Morgan TR, Balan V, Diago M, Marcellin P, et al. Peginterferon alfa‐2a (40 kilodaltons) and ribavirin combination therapy in chronic hepatitis C: randomized study of the effect of treatment duration and ribavirin dose. Annals of Internal Medicine 2004;140:346–55. [DOI] [PubMed] [Google Scholar]
Hauser 2014
- Hauser G, Awad T, Thorlund K, Štimac D, Mabrouk M, Gluud C. Peginterferon alpha‐2a versus peginterferon alpha‐2b for chronic hepatitis C (Review). Cochrane Database of Systematic Reviews 2014, Issue 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2002
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 2002;21(11):1539‐58. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Hirofumi 2009
- Uto H, Sherri OS, Hayashi K, Kumagai K, Sasaki F, Kanmura S, et al. Increased rate of death related to presence of viremia among hepatitis C virus antibody‐positive subjects in a community‐based cohort study. Hepatology 2009;50(2):393‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hodgson 2003
- Hodgson HJF. Viral hepatitis—clinical aspects. In: Warrell DA, Cox TM, Firth JD, Benz EJ Jr editor(s). Oxford Textbook of Medicine. 4th Edition. Oxford/ New York: Oxford University Press, 2003. [Google Scholar]
Hollis 1999
- Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ (Clinical Research Ed) 1999;319:670‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
ICH‐GCP 1997
- International Conference on Harmonisation Expert Working Group. International conference on harmonisation of technical requirements for registration of pharmaceuticals for human use. ICH harmonised tripartite guideline. Guideline for good clinical practice CFR & ICH Guidelines. Vol. 1, PA 19063‐2043, USA: Barnett International/PAREXEL, 1997. [Google Scholar]
Khuroo 2004
- Khuroo MS, Khuroo MS, Dahab ST. Meta‐analysis: a randomized trial of peginterferon plus ribavirin for the initial treatment of chronic hepatitis C genotype 4. Alimentary Pharmacology and Therapeutics 2004;20(9):931‐8. [DOI] [PubMed] [Google Scholar]
Kjaergard 2001
- Kjaergard LL, Villumsen J, Gluud C. Reported methodological quality and discrepancies between small and large randomized trials in meta‐analyses. Annals of Internal Medicine 2001;135(11):982‐9. [DOI] [PubMed] [Google Scholar]
Koretz 2013
- Koretz RL, Pleguezuelo M, Arvaniti V, Barrera Baena P, Ciria R, Gurusamy KS. Interferon for interferon nonresponding and relapsing patients with chronic hepatitis C. Cochrane Database of Systematic Reviews 2013, Issue 1. [DOI: 10.1002/14651858.CD003617] [DOI] [PMC free article] [PubMed] [Google Scholar]
Krleza‐Jeric 2005
- Krleza‐Jeric K, Chan AW, Dickersin K, Sim I, Grimshaw J, Gluud C. Principles for international registration of protocol information and results from human trials of health related interventions: Ottawa statement. BMJ (Clinical Research Ed) 2005;330(7497):956‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kumar 2002
- Kumar KS, Russo MW, Borczuk AC, Brown M, Esposito SP, Lobritto SJ, et al. Significant pulmonary toxicity associated with interferon and ribavirin therapy for hepatitis C. American Journal of Gastroenterology 2002;97:2432‐40. [DOI] [PubMed] [Google Scholar]
Lim 2010
- Lim JW, Shin MC. Pegylated‐interferon‐associated retinopathy in chronic hepatitis patients. Ophtalmologica 2010;224:224‐9. [DOI] [PubMed] [Google Scholar]
Lundh 2012
- Lundh A, Sismondo S, Lexchin J, Busuioc OA, Bero L. Industry sponsorship and research outcome. Cochrane Database of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/14651858.MR000033.pub2] [DOI] [PubMed] [Google Scholar]
Moher 1998
- Moher D, Pham B, Jones A, Cook DJ, Jadad AR, Moher M, et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta‐analyses?. Lancet 1998;352:609‐13. [DOI] [PubMed] [Google Scholar]
Moher 2012
- Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. International Journal of Surgery 2012;10:28‐55. [DOI] [PubMed] [Google Scholar]
Myers 2002
- Myers RP, Regimbeau C, Thevenot T, Leroy V, Mathurin P, Opolon P, et al. Interferon for interferon naive patients with chronic hepatitis C. Cochrane Database of Systematic Reviews 2002, Issue 2. [DOI: 10.1002/14651858.CD000370] [DOI] [PMC free article] [PubMed] [Google Scholar]
OPTN 2008
- United Network for Organ Sharing. Chapter IV; Liver and Intestine Transplantation in the United States, 1998‐2007. optn.transplant.hrsa.gov/ar2008/chapter_iv_AR_cd.htm?cp=5 (accessed 27 May 2013).
Penin 2004
Raison 2005
- Raison CL, Demetrashvili M, Capuron L, Miller AH. Neuropsychiatric adverse effects of interferon‐alpha: recognition and management. CNS Drugs 2005;19:105‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reddy 2001
- Reddy KR, Wright TL, Pockros PJ, Shiffman M, Everson G, Reindollar R, et al. Efficacy and safety of pegylated (40‐kd) interferonalpha‐2a compared with interferon alpha‐2a in noncirrhotic patients with chronic hepatitis C. Hepatology 2001;33(2):433–8. [DOI] [PubMed] [Google Scholar]
RevMan 2012 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012.
Roomer 2010
- Roomer R, Hansen BE, Janssen HL, Knegt RJ. Thrombocytopenia and the risk of bleeding during treatment with peginterferon alfa and ribavirin for chronic hepatitis C. Journal of Hepatology 2010;53:455‐9. [DOI] [PubMed] [Google Scholar]
Rosenberg 2001
- Rosenberg S. Recent advances in the molecular biology of hepatitis C virus. Journal of Molecular Biology 2001;313:451‐64. [DOI] [PubMed] [Google Scholar]
Royle 2003
- Royle P, Milne R. Literature searching for randomized controlled trials used in Cochrane reviews: rapid versus exhaustive searches. International Journal of Technology Assessment in Health Care 2003;19(4):591‐603. [DOI] [PubMed] [Google Scholar]
Rücker 2008
- Rücker G, Schwarzer G, Carpenter J. Arcsine test for publication bias in meta‐analyses with binary outcomes. Statistics in Medicine 2008;27:746‐63. [DOI] [PubMed] [Google Scholar]
Savovic 2012
- Savovic J, Jones HE, Altman DG, Harris RJ, Jüni P, Pildal J, et al. Influence of reported study design characteristics on intervention effect estimates from randomized, controlled trials. Health Technology Assessment 2012;16(35):1‐82. [DOI] [PubMed] [Google Scholar]
Savovic 2012a
- Savovic J, Jones HE, Altman DG, Harris RJ, Jüni P, Pildal J, et al. Influence of reported study design characteristics on intervention effect estimates from randomized, controlled trials. Annals of Internal Medicine 2012;157(6):429‐38. [DOI] [PubMed] [Google Scholar]
Schulz 1995
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273(5):408‐12. [DOI] [PubMed] [Google Scholar]
Seeff 2002
Seeff 2009
- Seeff LB. The history of the "natural history" of hepatitis C (1968‐2009). Liver International 2009;29(S1):89‐99. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shepherd 2005
- Shepherd J, Brodin H, Kan FT, Cave CB, Waugh NR, Price A, et al. Clinical‐ and cost‐effectiveness of pegylated interferon alfa in the treatment of chronic hepatitis C: a systematic review and economic evaluation. International Journal of Technology Assessment in Health Care 2005;21(1):47‐54. [DOI] [PubMed] [Google Scholar]
Siebert 2005
- Siebert U, Sroczynski G, German Hepatitis C Model GEHMO Group, HTA Expert Panel on Hepatitis C. Effectiveness and cost‐effectiveness of initial combination therapy with interferon/peginterferon plus ribavirin in patients with chronic hepatitis C in Germany: a health technology assessment commissioned by the German Federal Ministry of Health and Social Security. International Journal of Technology Assessment in Health Care 2005;21(1):55‐65. [DOI] [PubMed] [Google Scholar]
Slavenburg 2010
- Slavenburg S, Heijdra YF, Drenth JP. Pneumonitis as a consequence of (peg)interferon‐ribavirin combination therapy for hepatitis C: a review of the literature. Digestive Diseases and Sciences 2010;55:579‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Soza 2002
- Soza A, Everhart JE, Ghany MG, Doo E, Heller T, Promrat K, et al. Neutropenia during combination therapy of interferon alfa and ribavirin for chronic hepatitis C. Hepatology 2002;36:1273‐9. [DOI] [PubMed] [Google Scholar]
Sulkowski 2004
- Sulkowski MS, Wasserman R, Brooks L, Ball L, Gish R. Changes in haemoglobin during interferon alpha‐2b plus ribavirin combination therapy for chronic hepatitis C virus infection. Journal of Viral Hepatitis 2004;11:243‐50. [DOI] [PubMed] [Google Scholar]
Sulkowski 2011
- Sulkowski MS, Cooper C, Hunyady B, Jia J, Ogurtsov P, Peck‐Radosavljevic M, et al. Management of adverse effects of Peg‐IFN and ribavirin therapy for hepatitis C. Nature Reviews. Gastroenterology & Hepatology 2011;8:212‐23. [DOI] [PubMed] [Google Scholar]
Thorlund 2009
- Thorlund K, Devereaux PJ, Wetterslev J, Guyatt G, Ioannidis JPA, Thabane L, et al. Can trial sequential monitoring boundaries reduce spurious inferences from meta‐analyses?. International Journal of Epidemiology 2009;38(1):276‐86. [DOI: 10.1093/ije/dyn179] [DOI] [PubMed] [Google Scholar]
Thorlund 2010
- Thorlund K, Anema A, Mills E. Interpreting meta‐analysis according to the adequacy of sample size. An example using isoniazid chemoprophylaxis for tuberculosis in purified protein derivative negative HIV‐infected individuals. Clinical Epidemiology 2010;2:57‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thorlund 2011
- Thorlund K, Engstrøm J, Wetterslev J, Brok J, Imberger G, Gluud C. User manual forTrial Sequential Analysis (TSA). ctu.dk/tsa/files/tsa_manual.pdf 2011 (accessed 23 April 2013).
van Regenmortel 2000
- Regenmortel MHV, Fauquet CM, Bishop DHL, Carstens EB, Estes MK, Lemon SM, et al. Virus Taxonomy: The Classification and Nomenclature of Viruses. The Seventh Report of the International Committee on Taxonomy of Viruses. San Diego: Academic Press, 2000:599‐621. [Google Scholar]
Wetterslev 2008
- Wetterslev J, Thorlund K, Brok J, Gluud C. Trial sequential analysis may establish when firm evidence is reached in cumulative meta‐analysis. Journal of Clinical Epidemiology 2008;61(1):64‐75. [DOI] [PubMed] [Google Scholar]
Wetterslev 2009
- Wetterslev J, Thorlund K, Brok J, Gluud C. Estimating required information size by quantifying diversity in random‐effects model meta‐analyses. BMC Medical Research Methodology 2009;9:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 1999
- World Health Organization (WHO). Global surveillance and control of hepatitis C. Journal of Viral Hepatitis 1999;6(1):35‐47. [PubMed] [Google Scholar]
WHO 2009
- WHO. International Clinical Trials Registry Platform (ICTRP). www.who.int/ictrp/en/ (accessed 27 May 2013).
Wood 2008
- Wood L, Egger M, Gluud LL, Schulz KF, Jüni P, Altman GD, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta‐epidemiological study. BMJ (Clinical Research Ed.) 2008;336:601‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zaman 2003
- Zaman A, Fennerty MB, Keeffe EB. Peginterferon vs. standard interferon in the treatment of chronic hepatitis C. Alimentary Pharmacology & Therapeutics 2003;18(7):661‐70. [DOI] [PubMed] [Google Scholar]


