Abstract
Proper treatment of developmental disabilities requires health workers to have adequate knowledge of etiology and referral procedures. There is a dearth of research on knowledge of developmental disabilities among health workers in Ghana. The purpose of this study was to document knowledge about developmental disorders, causes, and referral procedures among health workers. Researchers used a successive free-listing method to interview 37 health workers. Developmental disabilities which present with physical symptoms were the most salient disorders identified among health workers, while learning disabilities and attention deficit disorder were largely overlooked. The most commonly listed developmental disabilities were cerebral palsy, Down syndrome, and autism spectrum disorder. Respondents had limited knowledge about the causes of and referral resources for developmental disabilities. Results show the need for continuing medical education, public awareness, and enhanced resources to support the identification and care of children with developmental disabilities in Ghana.
Keywords: autism spectrum disorder, cerebral palsy, attention deficit hyperactivity disorder, developmental disability, Down syndrome, language and learning disorders, intellectual disabilities
Introduction
Developmental disabilities significantly impair functionality in a wide range of areas including cognition, language, vision, hearing, movement, and learning (American Psychiatric Association 2013, Bakare et al. 2019, Fjermestad et al. 2021). These disabilities are associated with lifelong impairments, reduced quality of life for affected children and their families, high treatment costs, and increased burden on health and educational facilities (Russell et al. 1999). Adverse effects may be felt more strongly in low- and middle-income countries (LMICs) like Ghana because of limited access to health facilities and health professionals (Lasater et al. 2017, Bakare et al. 2015, 2019), and limited knowledge among both parents (Philip et al. 2021), and health workers (Bakare et al. 2015, Eseigbe et al. 2015, Hayat et al. 2019).
Like many other LMICs, the array of social and health services publicly available to children with developmental disorders is limited in Ghana. For instance, although Ghana boasts a physiotherapy unit in all its regional hospitals, staff shortages are common. Other specialized services such as neurodevelopmental clinics are concentrated in pediatric hospitals with low capacity. Private specialized hospitals and schools have risen as key sources of support, but remain largely inaccessible to children with developmental disabilities, the vast majority of whom come from impoverished families.
In addition to the challenge of allocating insufficient resources, medical professionals must be well-equipped to appropriately recognize and manage developmental disorders (Short and Schopler 1988, Rogers and DiLalla 1990, Zwaigenbaum et al. 2015). This includes having knowledge about etiology, symptoms, the course of the disability, and referral procedures (Eseigbe et al. 2015). Inability of health workers to recognize, treat, and properly refer those with developmental disabilities severely limits effective intervention, prevention, and management practices (Agrawal et al. 2012).
Neurodevelopmental disabilities are a specific subtype of developmental disability which occur as a result of abnormal brain development and include conditions such as Down syndrome, autism, and cerebral palsy among others (American Psychiatric Association (2013). These disorders have distinct clinical relevance due to significant difficulties with their diagnosis and treatment in sub-saharan Africa (Achilike and Achilike 2016, Donald et al. 2015, Ruparelia et al. 2016).The World Health Organization describes neurodevelopmental disorders as an interaction between the child, any impairment to their body structure and the function, as well as the people who relate to him/her (World Health Organization (WHO) 1997). This implies that neurodevelopmental impairment has three components - level of functioning of the body or body part, the whole person, and the whole person within a social context. Therefore, the causes of and the language to describe neurodevelopmental disabilities may vary by social and cultural context. In LMICs, the typical causes are reported to be genetic, intrauterine growth retardation, asphyxia at birth, malnutrition, metabolic abnormalities and infectious diseases (Grantham-McGregor et al. 2007). There are other augmenting factors which include poverty, lack of healthcare, famine, maternal health, stigma and orphanhood (Bakare et al. 2019, Tilahun et al. 2016). These factors in themselves are not causes but they contribute to the severity of neurodevelopmental disorders.
The prevalence of developmental disabilities, including those that are neurodevelopmental in nature, has been increasing worldwide, and the increase is disproportionately centered in developing countries like Ghana (Bornstein and Hendricks 2013, Hartley and Newton 2009). Despite rising incidence, research on the subject of health worker knowledge about these conditions in sub-Saharan Africa is scarce (Abubakar et al. 2016, Eseigbe et al. 2015, Wireko-Gyebi and Ashiagbor 2018). Available research has focused on the prevalence of neurodevelopmental disabilities within the hospital-setting, and frequently reports on their clinical manifestations (Ae-Ngibise et al. 2015, Commey 1995, Dickson et al. 2020, Nyame and Biritwum 1997). Autism in particular has received the most widespread attention from researchers in west Africa, and yet, to date, there is only one reported study evaluating the knowledge of healthcare workers about autism in Ghana (Wireko-Gyebi and Ashiagbor 2018). In addition, the assessment of knowledge about most developmental disabilities (and particularly neurodevelopmental disabilities) among healthcare workers relies on tools standardized among western healthcare workers, and is not reflective of how these disabilities are conceptualized within the cultural context of LMICs in Africa (Adeosun et al. 2015, Harrison et al. 2017, Johnson et al. 2019). With poor capacity to accurately evaluate the extent and nature of knowledge gaps about developmental disabilities, efforts to promote targeted awareness campaigns among health workers in west Africa have been hampered (Bakare et al. 2009).
To our knowledge, the information needs of health workers and their culturally significant understandings of developmental disabilities (and neurodevelopmental disabilities in particular) has yet to be investigated in Ghana. It is vital to assess if and where knowledge gaps exist, given the impact of knowledge on the quality of healthcare delivery (Agrawal et al. 2012). Therefore, the aims of this study are to characterize the common understandings about developmental disabilities and the knowledge of resources among healthcare workers in Accra Ghana. Compared to other knowledge-related studies, this study has the unique potential to improve cultural competency among researchers and global stakeholders by exposing the language and associations that have been culturally constructed by Ghanaian health workers in reference to developmental disabilities. Moreover, the results of this study can be used to inform interventions which aim to improve awareness and accurate knowledge of developmental disabilities among health workers in Ghana and other LMICs. This exploratory study answers the research question: how are developmental disabilities defined locally, and what do health workers know about the etiology of and referral services for these disabilities?
Methods
In this study, we examined the knowledge base about developmental disabilities among different categories of health workers in an urban location in Ghana. This work distinguishes itself from other knowledge-related studies because it does not attempt to evaluate the knowledge of LMIC healthcare workers through closed-ended assessments based on western medical culture and western understandings of developmental disabilities. Rather, an open-ended free-listing technique was utilized to capture unique patterns in the Ghanaian knowledge base of developmental disabilities. We examined the accuracy of health workers’ knowledge and the sources of their information.
Setting and participants
Data for this qualitative study was collected in the Greater Accra Region, the most densely populated region of Ghana. Thirty-seven health workers were recruited from two government hospitals in this region: a pediatric hospital with specialized services for children with developmental disabilities (including physical therapy and nutrition support), and a secondary-level hospital that provides general pediatric care. Cases of developmental disabilities from secondary-level hospitals are usually referred to specialist hospitals within the Greater Accra Region. The two hospitals under study were selected in conjunction with the Ghana Health Service based on their large patient volume.
Participants included nurses, pediatricians, general medical officers, physician assistants, and midwives. Selection of participants was based on the following inclusion criteria: (1) provides health services for children (2) is employed as a health worker in the Greater Accra region (3) informed consent attained. A simple random sampling method was used to select sixty potential participants from a list of eligible hospital employees. Thirty-seven of these health workers consented to participate in the study.
Participating hospitals and descriptive statistics of participants in the study are provided in Table 1. The mean age of participants was 37.5 years, and ranged from 26 to 59 years. Close to 89% (n = 33) of participants were female and about 59% (n = 22) worked as nurses. Most respondents had between 5 and 10 years of experience working in the hospital setting. Less than 20% (n = 7) of participants knew of a close family member, friend, or neighbor with a developmental delay or disability. About 41% (n = 15) of participants had ever worked in a psychiatric unit before occupying their current positions.
Table 1.
Demographic characteristics of study participants (n = 37).
| Characteristic | N (%) |
|---|---|
| Hospital | |
| Princess Marie Louise Children’s Hospital | 19 (51%) |
| Achimota hospital | 18 (49%) |
| Gender | |
| Male | 4 (11%) |
| Female | 33 (89%) |
| Age (years) | |
| 26–35 | 23 (62%) |
| 36–49 | 3 (8%) |
| >50 | 9 (24%) |
| No response | 2 (5%) |
| Occupation | |
| Medical officer | 3 (8%) |
| Pediatrician | 2 (5%) |
| Nurse | 22 (59%) |
| Midwife | 4 (11%) |
| Physician assistant | 4 (11%) |
| Other | 2 (5%) |
| Years of experience | |
| 5–10 | 18 (49%) |
| 11–20 | 3 (8%) |
| >20 | 4 (11%) |
| Unavailable | 12 (32%) |
Measures
This qualitative study drew on a methodology used in ethnography called free-listing. This technique is a structured, qualitative method in which participants are asked to provide a list of items pertaining to a particular cultural domain of interest (in this case, developmental disabilities) (Brewer 2002, Quinlan 2005, Ryan et al. 2000). Free-listing is useful for understanding how a population of interest defines the domain of interest based on the frequency of items on the list, the terminology used, the length and variability of list items, and omitted items (Ryan et al. 2000). This method has been utilized in previous health-related studies to assess and examine knowledge among groups of interest about specific illnesses (e.g. Lasater et al. 2017, Ahorlu et al. 2007). Free-listing is particularly useful for this study since it allows participants to provide information that is uniquely relevant to their knowledge base and culture (an emic perspective), rather than information based on the presumptions of the researcher (an etic perspective).
Free-listing is similar in rigor and reliability to the structured in-depth interview, prompting participants to respond to focused yet open-ended questions with the ultimate goal of exhausting their personal knowledge in a particular subject area (Quinlan 2005). In analysis, free-listing offers researchers the opportunity to examine language and common recurring associations suggesting prominent attitudes and beliefs. This method of analysis is similar to inductive coding methods used regularly in qualitative research. In addition, the opportunity to ask follow-up questions and probe for additional information enhance the reliability of this method.
Selected participants completed a face-to-face, 10–15 min free-listing interview and background questionnaire which included demographic information on gender, age, occupation, and years of experience. All data collection was done in a private setting at the respective health facilities of each health worker.
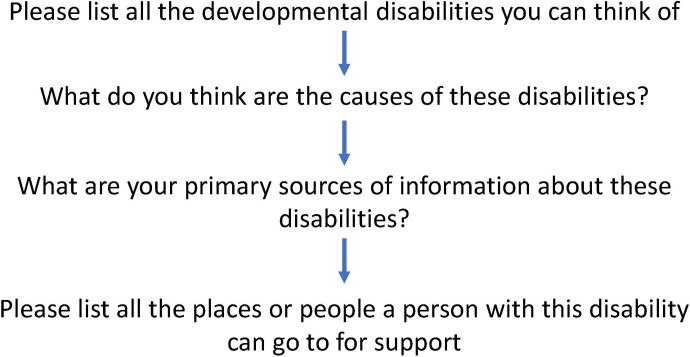
The type and flow of questions participants were asked are presented in Figure 1. Participants were asked to create multiple free-lists in succession, all linked together by their responses to the first list they created. Participants were asked: ‘Please list every developmental disability you can think of’. For each developmental disorder listed by participants, they were asked to list places and people they could refer someone with that disability to, causes of that disability, and their primary sources of information about the disability. Both the responses and the order of the responses were recorded by a research associate. The data collection procedure and tools were pilot tested and refined before use.
Figure 1.
Interview script for successive free-listing.
Data collection was done by research associates who were non-health workers. They received a week-long training on qualitative research, ethics, and data collection techniques, including free-listing. They were trained and supervised by 1) a PhD-level, qualitative, social scientist, 2) a clinical psychologist, and 3) a senior-level medical officer. The social scientist on the team monitored the quality of the interviews by observing and reviewing randomly selected interviews.
Analysis
We used Anthropac (Version 1.0), a cultural domain analysis software (Borgatti et al. 1996) to analyze the free-list data. Responses (items) were tabulated and evaluated for frequency, average rank, and saliency (Borgatti et al. 1996). Frequency measures how often each item is listed across participant responses. The average rank refers to the mean position of each item (i.e. the order in which it appears on a free-list) across participants. Common items that define a domain appear earlier on a free-list than uncommon ones. Lastly, saliency is a statistic (ranging from 0 to 1, where 0 = least salient, and 1 = most salient) that is calculated based on the frequency and average rank of items (Borgatti et al. 1996). The most salient items are listed earlier and appear more often on free-lists. In addition to these indices, the research team searched for patterns in the responses to identify gaps in knowledge and care of developmental disorders. In this study, individually listed items were identified as developmental disabilities or non-developmental disabilities according to DSM-5 listings and criteria.
Ethical considerations
The study was approved by the Ghana Health Services Ethical Review Committee [#GHS-ERC 08/08/16]]. Participants were not given monetary compensation. Written informed consent was taken from each participant.
Results
Results of free-listing responses
All participants were able to list at least one developmental disorder. A complete list of the disabilities recorded by participants is organized by frequency, average rank, and overall salience in Table 2. Several participants listed mongolism and Trisomy 21 as developmental disabilities. These responses were recorded and analyzed as separate responses from Down syndrome.
Table 2.
All free-listed listed developmental disabilities.
| Developmental disability | Frequency (%) | Average rank | Salience |
|---|---|---|---|
| Down syndrome | 43.2 | 2.00 | 0.327 |
| Autism spectrum disorder | 40.5 | 1.80 | 0.309 |
| Cerebral palsy | 37.8 | 1.93 | 0.278 |
| Talipes | 10.8 | 2.00 | 0.083 |
| Cleft Palate | 8.10 | 1.00 | 0.081 |
| Extra digits | 8.10 | 4.67 | 0.021 |
| Spina Bifida | 8.10 | 2.00 | 0.052 |
| Delayed language development | 5.40 | 1.00 | 0.054 |
| Intellectual disability | 5.40 | 3.00 | 0.025 |
| Hydrocephalus | 5.40 | 4.00 | 0.024 |
| Subnormality | 2.70 | 1.00 | 0.027 |
| Slurred Speech | 2.70 | 6.00 | 0.005 |
| Neonatal Sepsis | 2.70 | 5.00 | 0.009 |
| Neonatal Jaundice | 2.70 | 4.00 | 0.014 |
| Poor vision | 2.70 | 2.00 | 0.014 |
| Blindness | 2.70 | 3.00 | 0.014 |
| Microcephaly | 2.70 | 6.00 | 0.010 |
| Unresponsive to bright colors and moving objects | 2.70 | 2.00 | 0.014 |
| Cushing syndrome | 2.70 | 2.00 | 0.023 |
| Deaf and Dumb | 2.70 | 4.00 | 0.007 |
| Accident to the head/brain | 2.70 | 2.00 | 0.018 |
| Asthma | 2.70 | 3.00 | 0.009 |
| Bilirubin encephalopathy | 2.70 | 2.00 | 0.018 |
| Hole in the heart | 2.70 | 3.00 | 0.009 |
| Genetics | 2.70 | 3.00 | 0.009 |
| Hyperactive disorder | 2.70 | 4.00 | 0.007 |
| Incompatibility problem | 2.70 | 5.00 | 0.014 |
| Delayed cognition | 2.70 | 2.00 | 0.014 |
| Delayed sitting | 2.70 | 1.00 | 0.027 |
| Delayed crawling | 2.70 | 1.00 | 0.027 |
| Fetal alcohol syndrome | 2.70 | 2.00 | 0.014 |
| Delayed walking | 2.70 | 2.00 | 0.014 |
| Hydrocephalus | 5.40 | 4.00 | 0.024 |
| Subnormality | 2.70 | 1.00 | 0.027 |
| Birth asphyxia | 2.70 | 1.00 | 0.027 |
| Infection | 2.7 | 3.00 | 0.009 |
| Kwashiorkor | 5.4 | 3.00 | 0.025 |
| Marasmus | 2.7 | 2.00 | 0.020 |
| Developmental Disability | Frequency | Average Rank | Salience |
| Rabies | 2.7 | 2.00 | 0.018 |
| Mongoloid | 2.7 | 1.00 | 0.027 |
| Seizure disorder | 2.7 | 3.00 | 0.014 |
| Convulsion | 5.4 | 1.00 | 0.054 |
| Malnutrition | 2.7 | 4.00 | 0.007 |
| Epilepsy | 2.7 | 2.00 | 0.018 |
| Scabies | 2.7 | 3.00 | 0.009 |
Down Syndrome, autism spectrum disorder (ASD), and cerebral palsy were the top three most listed developmental disabilities. Besides ASD, all of the top seven most commonly listed developmental disorders are characterized by some physical symptom, such as unusual anatomical features or motor dysfunction. Approximately 5% of participants mentioned other categories of developmental disabilities such as language and learning disabilities and intellectual disabilities. Less than 3% of participants mentioned ADHD, vision impairment, hearing loss, fetal alcohol syndrome, or delays in cognition, sitting, or walking.
More than one-third of participants incorrectly listed epilepsy disorders, infectious diseases, and/or nutritional disorders as developmental disabilities (see Table 3). Epilepsy disorders and nutritional disorders such as kwashiorkor, malnutrition, and marasmus were mentioned by 11% of participants. Other diseases such as malaria, bronchopneumonia, and scabies were mentioned by over 16% of participants.
Table 3.
Other conditions incorrectly listed by occupation.
| Incorrect free-listing | Occupation | N (%) | Items listed |
|---|---|---|---|
| Epilepsy | seizure disorder, convulsions, epilepsy | ||
| All participants | 5 (100%) | ||
| Prescribers | 0 (0%) | ||
| Nurse | 3 (60%) | ||
| Midwife | 0 (0%) | ||
| Physician Assistant | 0 (0%) | ||
| Other | 2 (40%) | ||
| Nutritional disorders | kwashiorkor, malnutrition, marasmus | ||
| All participants | 5 (100%) | ||
| Prescribers | 0 (0) | ||
| Nurse | 5 (100%) | ||
| Midwife | 0 (0%) | ||
| Physician Assistant | 0 (0%) | ||
| Other | 0 (0%) | ||
| Infectious diseases | scabies, bronchopneumonia, infection, malaria, rabies | ||
| All participants | 6 (100%) | ||
| Prescribers | 1 (17%) | ||
| Nurse | 5 (83%) | ||
| Midwife | 0 (0%) | ||
| Physician Assistant | 0 (0%) | ||
| Other | 0 (0%) | ||
| Other | Birth asphyxia, genetics, incompatibility | ||
| All participants | 3 (100%) | ||
| Prescribers | 1 (33%) | ||
| Nurse | 0 (0%) | ||
| Midwife | 0 (0%) | ||
| Physician Assistant | 2 (66%) | ||
| Other | 0 (0%) |
Variations in free-listing responses by age and occupation
In Tables 4 and 5, the list of developmental disabilities by age and occupation of participants are presented. Younger participants (ages 26–35) were most likely to include Down syndrome and ASD on their list, whereas older participants (50+ years) were most likely to list Down syndrome and cerebral palsy. Across the different age groups, cerebral palsy and ASD were always listed, and cerebral palsy consistently ranked among the top three most salient disabilities. Disabilities characterized by physical indicators such as cleft palate and spina bifida were the most salient type of disabilities listed across all age groups, particularly among older participants. Younger participants were the only group of health workers to list intellectual disabilities (n = 2) and ADHD (n = 1) as developmental disabilities. They were also more likely to incorrectly list infectious diseases as developmental disabilities compared to older participants.
Table 4.
Commonly listed developmental disabilities by age.
| Age group (years) | Most commonly listed disabilities | Frequency (%) | Average rank | Salience |
|---|---|---|---|---|
| 26–35 | ||||
| Autism | 43.5 | 1.7 | 0.341 | |
| Down syndrome | 39.1 | 1.89 | 0.293 | |
| Cerebral palsy | 39.1 | 1.78 | 0.293 | |
| Mongolism | 8.7 | 2.50 | 0.040 | |
| Mental retardation | 8.7 | 3.00 | 0.040 | |
| 36–49 | ||||
| Cerebral palsy | 66.7 | 2.50 | 0.444 | |
| Autism | 66.7 | 2.00 | 0.444 | |
| Neonatal jaundice | 33.3 | 4.00 | 0.167 | |
| Neonatal sepsis | 33.3 | 5.00 | 0.111 | |
| Slurred speech | 33.3 | 6.00 | 0.056 | |
| >50 | ||||
| Down syndrome | 44.4 | 2.75 | 0.306 | |
| Cerebral palsy | 33.3 | 2.00 | 0.245 | |
| Cleft palate | 33.3 | 1.00 | 0.333 | |
| Spina Bifida | 22.2 | 2.00 | 0.139 | |
| Poor vision | 11.1 | 2.00 | 0.056 |
Table 5.
Commonly listed developmental disabilities by occupation.
| Correct free-listed developmental disabilities | Frequency (%) | Average rank | Salience |
|---|---|---|---|
| Prescribers | |||
| Down Syndrome | 60% | 2 | 0.367 |
| Cerebral Palsy | 60% | 1.67 | 0.467 |
| Autism | 60% | 2.33 | 0.33 |
| Spina Bifida | 20% | 2 | 0.133 |
| Delayed Language Development | 20% | 1 | 0.2 |
| Nurse | |||
| Down Syndrome | 47.4% | 1.44 | 0.399 |
| Autism | 47.4% | 1.44 | 0.412 |
| Nurse | |||
| Cerebral Palsy | 36.8% | 1.71 | 0.268 |
| Mental Retardation | 10.5% | 3 | 0.048 |
| Fetal Alcohol Syndrome | 5.3% | 2 | 0.026 |
| Midwife | |||
| Talipes | 75% | 1.67 | 0.583 |
| Extra Digits | 50% | 3 | 0.167 |
| Autism | 50% | 1 | 0.5 |
| Hole in Heart | 25% | 3 | 0.083 |
| Down Syndrome | 25% | 1 | 0.25 |
| Cerebral Palsy | 25% | 2 | 0.167 |
| Physician assistant | |||
| Cerebral Palsy | 66.7% | 1.5 | 0.611 |
| Cleft Palate | 66.7% | 1 | 0.667 |
| Extra Digits | 33.3% | 6 | 0.056 |
| Microcephalus | 33.3% | 4 | 0.167 |
| Spina Bifida | 33.3% | 2 | 0.25 |
| Other | |||
| Down Syndrome | 100% | 2 | .667 |
| Hyperactive Disorder | 100% | 3 | .333 |
| Cerebral Palsy | 100% | 1 | 1.00 |
| Incorrect free-listed developmental disabilities | |||
| Prescribers | |||
| Birth Asphyxia | 50% | 1 | 0.5 |
| Infection | 50% | 2 | 0.25 |
| Hydrocephalus | 50% | 1 | 0.5 |
| Nurse | |||
| Mongolism | 25% | 2 | 0.167 |
| Kwashiorkor | 25% | 1 | 0.25 |
| Mongoloid | 12.5% | 1 | 0.125 |
| Marasmus | 12.5% | 2 | 0.083 |
| Rabies | 12.5% | 2 | 0.083 |
| Physician assistant | |||
| Hydrocephalus | 50% | 1 | 0.5 |
| Incompatibility Problem (RH Blood) | 50% | 2 | 0.25 |
| Subnormality | 50% | 1 | 0.5 |
| Genetics | 50% | 3 | 0.167 |
| Accident to heart/brain | 50% | 2 | 0.333 |
| Other | |||
| Seizure disorder | 50 | 1 | 0.50 |
| Convulsion | 50 | 1 | 0.50 |
Disabilities characterized by physical indicators were also the most salient types of disabilities listed across every occupation - and among midwives, this was the only type of disability listed. Down syndrome and/or cerebral palsy were the most commonly listed developmental disabilities across all occupations except for midwives who were most likely to list talipes (club foot). Among the different professions, nurses and pediatricians were the only groups of participants to mention language and learning disorders. Nurses listed a number of disabilities which were not mentioned by participants of any other occupations, including fetal alcohol syndrome, deafness, and blindness. During interviews, nurses were also more likely to describe specific symptoms of developmental disabilities (for example, quote: ‘[the child is] unresponsive to bright colors and moving objects’) while other health workers provided lists of developmental disabilities without additional descriptions.
The length of each free-list across all occupations also varied, ranging from 1 to 8 items, with physician assistants listing the most disabilities (mean = 4 disabilities) and pediatricians and midwives listing the least (mean = 2.5 disabilities).
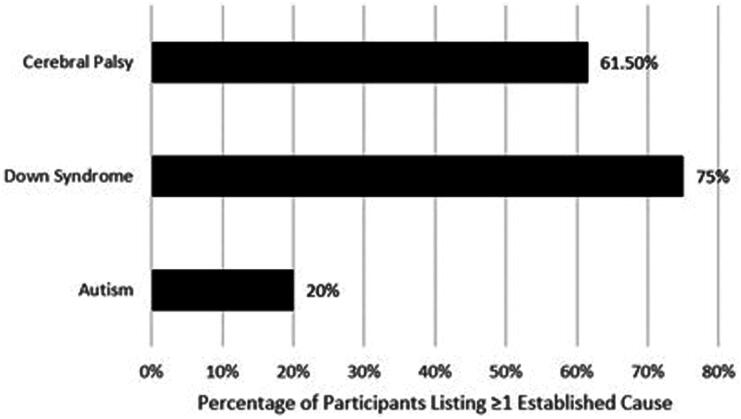
Knowledge of causes of autism spectrum disorder, cerebral palsy, and down syndrome
Those who listed ASD, cerebral palsy, and/or Down syndrome as developmental disabilities were asked to state the etiology. Participants whose responses matched established causes of cerebral palsy, Down syndrome, and ASD are recorded in Figure 2. In this study, to ascertain the accuracy of responses, established causes of developmental disorders were identified from several national organizations, including the National Center on Birth Defects and Developmental Disabilities, the National Institute of Child Health and Human Development, and the DSM-5. Established causes were cross-referenced across international literature for consensus. The established causes of cerebral palsy include injury or damage to the brain, resulting from infections (e.g. meningitis, encephalitis), complications at birth (e.g. birth asphyxia), and/or problems with blood flow (e.g. stroke, sickle cell disease, maldeveloped blood vessels) (MacLennan et al. 2015). The established cause of Down syndrome is an error in cell division arising from an extra copy of chromosome 21 (Korenberg et al. 1990). While there is no official single cause or group of causes for ASD, researchers generally agree that ASD is a problem of abnormal neurodevelopment (Ratajczak 2011). For this study, researchers recorded the number of participants who mentioned any of these established causes.
Figure 2.
Participants whose responses matched established etiology for cerebral palsy, Down’s syndrome, and autism.
Most respondents who listed Down syndrome correctly listed genetics or chromosomal abnormality as the cause of this disability, and over 60% of respondents who listed cerebral palsy correctly listed birth asphyxia or brain infection as causes. In addition, approximately 23% of participants were able to list more than one established cause of cerebral palsy. Other causes of Down syndrome and cerebral palsy mentioned by health workers include: genetics of parents, alcohol/drug use by mothers during pregnancy, and prolonged labor. Many respondents who listed Down syndrome listed ‘old age of parents’ as a cause. Only 20% of participants who listed ASD were able to identify that this disability is a neurological condition and/or a condition with no established causes. The most frequently mentioned causes of ASD were genetics and alcohol/drug use by mothers during pregnancy. A full list of causes listed by participants for ASD, cerebral palsy, and Down syndrome is exhibited in Table 6.
Table 6.
List of participant responses for causes of autism, cerebral palsy, and Down syndrome.
| ASD | Cerebral palsy | Down syndrome | |
|---|---|---|---|
| Participant-Listed Causes | N | N | N |
| Genetic Defect | 5 | 1 | 10 |
| Alcohol/drug use by mother during pregnancy | 3 | 2 | 2 |
| Don’t know | 3 | 0 | 0 |
| Old age of parents | 2 | 0 | 7 |
| Inadequate oxygen to the brain | 1 | 0 | 0 |
| Prolonged labor | 1 | 2 | 0 |
| Infection during pregnancy | 1 | 2 | 0 |
| Neurological (unspecified) | 1 | 0 | 0 |
| Unknown | 2 | 2 | 0 |
| Jaundice | 0 | 4 | 0 |
| Birth Asphyxia | 0 | 7 | 0 |
| Insult in birth/prenatal/postnatal | 0 | 2 | 0 |
| Chromosomal Abnormality | 0 | 2 | 2 |
| Underlying disorders | 0 | 1 | 0 |
Commonly listed sources of knowledge
Participants indicated experience on the job (68%), professional school (62%), and the media (35%) as their top sources of information about developmental disabilities (see Table 7). For participants who cited media as a source of information, television and internet were the most common sources of knowledge. About 22% of participants indicated that they used medical journals as a source of information while 10% listed medical books. Less than 10% of participants mentioned learning about developmental disabilities from seminars, workshops, lectures or from their colleagues or people outside of the hospital.
Table 7.
Percentage of participants citing relevant sources of information on developmental disabilities.
| All developmental disabilities | Autism | Down syndrome | Cerebral palsy | |
|---|---|---|---|---|
| Source of information | % | % | % | % |
| Media | 35 | 53 | 37.5 | 28.6 |
| On the job | 68 | 53 | 43.8 | 57 |
| Journals | 22 | 20 | 31.3 | 21.4 |
| Books | 10 | 6.7 | 12.5 | 21.4 |
| Professional school | 62 | 53 | 68.8 | 57 |
For the most commonly listed developmental disabilities – Down syndrome, ASD, and Cerebral palsy – experience on the job and professional school training were the most frequently cited sources of knowledge. For ASD, the media was also an especially important source of information, ranking at the same level as professional school and experience on the job as a relevant resource for health workers. For Down syndrome, participants emphasized the media (especially the Internet) as a top resource as well, but participants also mentioned medical journals more often as a resource for learning about Down syndrome than they did autism or cerebral palsy. Sources of knowledge about cerebral palsy were mainly limited to experience on the job and professional school, with <30% of participants citing any other source of knowledge.
Referral knowledge
Few (<15%) health workers listed a specific school or care center specially equipped to care for children with developmental disabilities within the Greater Accra region. A slightly higher proportion of health workers (22%) were able to list a specific hospital or clinic that could provide specialized care for those with developmental disabilities in the Accra region. Korle Bu Teaching Hospital, the national teaching hospital situated in Accra, was mentioned most frequently as the preferred site of referral for developmental problems.
Discussion
This study is the first analysis to determine the salience of multiple developmental disabilities, as well as known etiologies, sources of knowledge, and referral sources among health workers in Ghana. The foremost finding from this study is that developmental disabilities which present with physical symptoms tended to be the most salient disabilities among health workers, while other types of common disabilities, such as learning disabilities or attention deficit disorder were largely overlooked. The prevalence of ADHD among children in Ghana is unknown, however, studies in different regions of the country suggest a range from 1.64% (Kusi-Mensah et al. 2019) to 12.8% (Afeti and Nyarko 2017). The prevalence of intellectual disability is estimated to be 2–3% (Ghana Statistical Service (GSS) et al. 2015). Though prevalence data for cerebral palsy and Down syndrome is scarce, both disabilities are currently estimated to impact <1% of the Ghanaian population (Gladstone 2010, Inclusion Ghana 2011).Thus, despite the relatively wider prevalence of ADHD and intellectual disabilities, they were notably less salient among health workers. This finding is consistent with previous studies which suggest that ADHD is not yet a ‘culturally established category in Ghana’ (Bergey and Filipe 2018), and lacks formalized procedures for diagnosis and treatment. Similarly, previous studies have also highlighted that lack of awareness and stigmatization of intellectual disabilities are common within the medical community (Oti-Boadi 2017). Lack of cultural awareness of ADHD and intellectual disabilities as diagnostic categories may explain their low salience among health workers and highlights the value placed on treating disabilities which can be readily seen rather than those inconspicuous to the eye.
It should be noted that autism spectrum disorder, the only highly salient developmental disability not characterized by physical indicators, has received widespread media attention in Ghana in recent years. This trend is largely due to the rise of autism advocacy organizations such as the Autism Awareness Care and Training (AACT) organization, and the Autism Society of Ghana, as well as the implementation of the Inclusive Education Policy in 2016 (Sarkodie 2018). This is consistent with our finding that the media is among the most common sources of information about autism among health workers. Public awareness has spawned a flurry of research, education, and training which may explain the high salience of the disorder among health workers. It might be suggested that similar awareness campaigns for ADHD and intellectual disabilities may increase the salience of these disabilities among health workers.
The media, professional school training, and on-the-job experience emerged as important sources of information about developmental disabilities for health workers. The media, in particular, ranked highly as a relevant source of information for the most commonly-listed developmental disabilities: autism, and Down syndrome. This, again, suggests that the media may be a fundamental tool for increasing awareness of developmental disabilities among the public, as well as healthcare workers. However, overall, on-the-job experience and professional school training are the most relevant sources of knowledge for health workers. While many existing interventions aim to provide additional clinical training at the hospital level, few resources have been invested at the professional school level. However, our findings highlight the essential role of teaching staff at the university level, who must be encouraged to reinforce curriculum focused on developmental disabilities in early clinical training. This will help serve the information needs of future health professionals in conjunction with on-the-job clinical training. As far as the authors are aware, this study provides the first analysis on the various sources of knowledge for Ghanaian healthcare workers with respect to developmental disabilities. Thus, this study provides valuable evidence for interventionists seeking to use the media, professional schools, and on-the-job experiences as platforms for education or training about developmental disabilities.
Knowledge about referral options for developmentally disabled patients was extremely low. Most health workers (∼80%) were unable to list one specific school, care center, clinic, or hospital specifically equipped to care for children with developmental disabilities. This is likely a reflection of the low availability of such facilities. Though Ghana committed itself to an inclusive education policy in 2003 (which is intended to support improved access to school for disabled children and training programs for teachers (Pekeberg 2012)), none of the over 120 schools in Ghana classified as ‘inclusive’ accommodate students with severe disabilities – this leaves behind students with intellectual disabilities, cerebral palsy, autism, Down syndrome, and even some cases of ADHD (Anthony 2010). In addition, Ghana faces a severe shortage of health workers specialized to care for developmentally disabled patients. In 2010, for example, it was reported that only one doctor in the entirety of Accra was available to diagnose autistic patients (Anthony 2010). This shortage aligns with our findings indicating that health workers had limited or no knowledge about referral options for children with developmental disorders in Accra. While the number of doctors with the expertise in treating neurodevelopmental disorders has improved significantly since 2009 (e.g. via increased training for psychiatrists and psychologists), our results highlight the continued need for more specialized services, as well as increased training and awareness of referral services among health workers (Jacob et al. 2007). Information about referral services may be best distributed during training and on-the-job. Increasing visibility of existing resources is essential for dispelling the common belief among health workers that there simply is no help available.
Though health workers’ knowledge about the etiology of cerebral palsy and Down Syndrome tended to be consistent with the current established causes of these disabilities, health workers also frequently mentioned the behavioral activity of mothers (most notably, alcohol and drug use) as a key cause of Down Syndrome, cerebral palsy, and autism. However, the causal link between parental behavior and disability is currently weak for cerebral palsy and autism spectrum disorder, and not at all established for Down syndrome. While some parental behaviors, particularly drug and alcohol use, appear to increase the risk of developmental disabilities in children, it is important not to mistakenly associate them as causes of these disabilities. It is particularly important in the Ghanaian cultural context - where childhood disability is still widely perceived to be a spiritual punishment or a moral failing on the part of caregivers - to not issue blame to parents for their child’s disability (Agbenyega 2003). Medical personnel can help subvert stigmatizing claims about the origins of these disabilities by emphasizing the role of established genetic and biological factors rather than personal behaviors. Furthermore, future research focused on the stigma surrounding developmental disabilities in Ghana may extend the results of this study by identifying common biases among the health workers tasked with providing care to developmentally disabled children and the teachers or school officials responsible for fulfilling Ghana’s inclusive education policy. This research may reveal important links between how community-held knowledge may interact with the understanding that health professionals have about developmental disabilities, while revealing barriers to the implementation of inclusive education. Lastly, it should be mentioned that the role of language is extremely important in the interpretation of these results. It also has implications for the validity of future surveys designed to measure knowledge on developmental disabilities within the sub-saharan African context. A number of health workers used alternative or archaic names for common developmental disabilities, for example, referring to Down syndrome as mongolism. This term has been largely discontinued among many medical professionals due to its racist implications and is largely perceived as a derogatory term (Rodríguez-Hernández and Montoya 2011). Future investigations may clarify what, if any, derogatory beliefs are associated with usage of this term among Ghanaian health workers. In addition, a number of health workers were unable to list the name of common developmental disabilities, but were able to provide accurate descriptions of the symptoms and causes for these disabilities. For future investigations assessing the knowledge of health workers, researchers should take into consideration how unique medical terminology and conceptions of disability inform the capacity of health workers to identify and correctly impart knowledge about developmental disabilities.
Limitations
Interviews with health workers were limited to non-specialists, particularly nurses. This was, in part, due to the lack of available health workers specializing in the diagnosis and treatment of children with developmental disorders at the time of data collection. Thus, the ability of health workers to respond to questions assessing their knowledge about developmental disabilities is limited by occupation. Researchers endeavored to the best of their ability to conduct interviews in private and quiet locations. In some cases, it was impossible to ensure total privacy and limit distractions due to the professional obligations of some participants. In these cases, the interview environment may have impeded participants’ ability to answer questions due to frequent disturbances. In addition, the first twelve participants were not asked about their years of experience in the field during the background questionnaire given at the beginning of the interview. This missing data did not allow researchers to stratify and analyze results according to years of experience.
Conclusion
Poor knowledge among healthcare workers jeopardizes the provision of quality healthcare for children with developmental disabilities. Findings regarding knowledge of developmental disabilities, symptoms, and known referral sources among a Ghanaian sample suggest the need for continuing medical education and publicity to bring awareness of developmental disabilities (particularly language and learning disabilities) to health workers. Findings also highlight the urgent need for more trained specialized providers to care for children with developmental disabilities. Collating referral sources in the various cities and regions is crucial to support the work of health workers in providing accurate resources for parents. Finally, on a policy and funding level, ensuring that resources are properly allocated to train and educate health workers would be essential to improving quality medical care in this area for both children and their caregivers.
Funding Statement
This work was funded by the National Institute on Minority Health and Health Disparities (DOI: 10.13039/100006545) Grant #5T37MD008655 at Brown University.
Declaration of interest statement
The authors declare no conflict of interest. The funders had no role in the design of the study, in the collection, analysis, or interpretation of data, in the writing of the manuscript, and in the decision to publish the results.
References
- Abubakar, A., Ssewanyana, D. and Newton, C. R.. 2016. A systematic review of research on Autism spectrum disorders in Sub-Saharan Africa. Behavioural Neurology, 2016, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Achilike, B. A. and Achilike, C.. 2016. Identification and diagnosis of ADHD among primary school children in ebonyi state southeast nigeria: implications for effective classroom management/interventions. Journal of Educational Policy and Entrepreneurial Research, 3, 92–102. [Google Scholar]
- Adeosun, I., Ogun, O., Adeyemo, S., Bello, A. and Fatiregun, O.. 2015. The impact of an educational intervention on knowledge of attention-deficit hyperactivity disorder among Primary School Teachers in Lagos Nigeria. Babcock University Medical Journal (BUMJ), 1, 14–20. [Google Scholar]
- Ae-Ngibise, K., Akpalu, B., Ngugi, A. K., Akpalu, A., Agbokey, F., Adjei, P., Punguyire, D., Bottomley, C., Newton, C. R. and Owusu-Agyei, S.. 2015. Prevalence and risk factors for active convulsive epilepsy in Kintampo, Ghana. Pan African Medical Journal, 21, 29. doi: 10.11604/pamj.2015.21.29.6084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Afeti, K. and Nyarko, S. H.. 2017. Prevalence and effect of attention-deficit/hyperactivity disorder on school performance among primary school pupils in the Hohoe Municipality, Ghana. Annals of General Psychiatry, 16,11. doi: 10.1186/s12991-017-0135-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agbenyega, J. 2003. The power of labeling discourse in the construction of disability in Ghana. In A Paper presented at the Australian Association for Research in Education Conference, Newcastle, December. Association of Active Educational Researchers (AARE) (Vol. 16). [Google Scholar]
- Agrawal, P. K., Agrawal, S., Ahmed, S., Darmstadt, G. L., Williams, E. K., Rosen, H. E., Kumar, V., Kiran, U., Ahuja, R.C., Srivastava, V.K., Santosham, M., Black, R.E. and Baqui, A. H.. 2012. Effect of knowledge of community health workers on essential newborn healthcare: A study from rural India. Health Policy and Planning, 27, 115–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahorlu, C. K., Koram, K. A. and Weiss, M. G.. 2007. Children, pregnant women and the culture of malaria in two rural communities of Ghana. Anthropology & Medicine, 14, 167–181. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . 2013. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, D.C.: American Psychiatric Association Publishing. 10.1176/appi.books.9780890425596. [DOI] [Google Scholar]
- Anthony, J. 2010. Access to Education for Students with Autism in Ghana: Implications for EFA(Rep.). 6. <http://unesdoc.unesco.org/images/0018/001865/186588e.pdf>
- Bakare, M. O., Ebigbo, P. O., Agomoh, A. O., Eaton, J., Onyeama, G. M., Okonkwo, K. O., Onwukwe, J.U., Igwe, M.N., Orovwigho, A.O. and Aguocha, C. M.. 2009. Knowledge about childhood Autism and opinionamong healthcare workers on availability of facilities and law caring for the needs and rights of children with childhood Autism and other developmental disorders in Nigeria. BMC Pediatrics, 9, 12–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakare, M. O., Taiwo, O. G., Bello-Mojeed, M. A. and Munir, K. M.. 2019. Autism spectrum disorders in Nigeria: A scoping review of literature and opinion on future research and social policy directions. Journal of Health Care for the Poor and Underserved, 30, 899–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakare, M. O., Tunde-Ayinmode, M. F., Adewuya, A. O., Bello-Mojeed, M. A., Sale, S., James, B. O., Yunusa, M. A., Obindo, J. T., Igwe, M. N., Odinka, P. C., Okafor, C. J., Oshodi, Y. O., Okonoda, K. M., Munir, K. M. and Orovwigho, A. O.. 2015. Recognition of Autism Spectrum Disorder (ASD) symptoms and knowledge about some other aspects of ASD among final year medical students in Nigeria, Sub-Saharan Africa. BMC Research Notes, 8, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergey, M. R. and Filipe, A. M.. 2018. ADHD in Global Context. Global Perspectives on ADHD: Social Dimensions of Diagnosis and Treatment in Sixteen Countries, 1. [Google Scholar]
- Borgatti, S. P., Everett, M. G. and Freeman, L. C.. 1996. UCINET IV: Network analysis software; reference manual. Harvard, MA: Analytic Technologies. [Google Scholar]
- Bornstein, M. H. and Hendricks, C.. 2013. Screening for developmental disabilities in developing countries. Social Science & Medicine (1982), 97, 307–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer, D. D. 2002. Supplementary interviewing techniques to maximize output in free listing tasks. Field Methods, 14, 108–118. [Google Scholar]
- Commey, J. O. 1995. Neurodevelopmental problems in Ghanaian children: Part Convulsive disorder. West African Journal of Medicine, 14, 189–193. [PubMed] [Google Scholar]
- Dickson, E., Osafo, J., Asampong, E. and Kretchy, I.. 2020. Clinical presentation and pattern of neuro-developmental disorders in a health facility in Ghana: Implications for the health and educational sectors. Health Sciences Investigations Journal, 1, 114–120. [Google Scholar]
- Donald, K. A., Kakooza, A. M., Wammanda, R. D., Mallewa, M., Samia, P., Babakir, H., Bearden, D., Majnemer, A., Fehlings, D., Shevell, M., Chugani, H. and Wilmshurst, J. M.. 2015. Pediatric cerebral palsy in Africa. Journal of Child Neurology, 30, 963–971. [DOI] [PubMed] [Google Scholar]
- Eseigbe, E. E., Nuhu, F. T., Sheikh, T. L., Eseigbe, P., Sanni, K. A. and Olisah, V. O.. 2015. Knowledge of childhood Autism and challenges of management among medical doctors in Kaduna State, Northwest Nigeria. Autism Research and Treatment, 2015, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fjermestad, K., Pat, P., Dearozet, S., Vatne, T., Hafting, M. and Jegannathan, B.. 2021. Manual-based group intervention for siblings and parents of children with neurodevelopmental disorders in Cambodia. Journal of Developmental and Physical Disabilities, 33, 839–856. [Google Scholar]
- Ghana Statistical Service (GSS), Ghana Health Service (GHS), and ICF International . 2015. Ghana Demographic and Health Survey 2014. Rockville, MD: GSS, GHS, and ICF International. [Google Scholar]
- Gladstone, M. 2010. A review of the incidence and prevalence, types and aetiology of childhood cerebral palsy in resource-poor settings. Annals of Tropical Paediatrics, 30, 181–196. [DOI] [PubMed] [Google Scholar]
- Grantham-McGregor, S., Cheung, Y. B., Cueto, S., Glewwe, P., Richter, L. and Strupp, B.. 2007. Developmental potential in the first 5 years for children in developing countries. The Lancet, 369, 60–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison, A. J., Slane, M. M., Hoang, L. and Campbell, J. M.. 2017. An international review of Autism knowledge assessment measures. Autism, 21, 262–275. [DOI] [PubMed] [Google Scholar]
- Hartley, S. and Newton, C. R. J. C.. 2009. Children with developmental disabilities in the majority of the world. In Neurodevelopmental disabilities: Clinical and scientific foundations. London: Mac Keith Press, pp.70–84. [Google Scholar]
- Hayat, A. A., Meny, A. H., Salahuddin, N., Alnemary, F. M., Ahuja, K. R. and Azeem, M. W.. 2019. Assessment of knowledge about childhood Autism spectrum disorder among healthcare workers in Makkah-Saudi Arabia. Pakistan Journal of Medical Sciences, 35, 951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inclusion Ghana . 2011. Down Syndrome Fact Sheet. Retrieved from http://www.inclusion-ghana.org/resources/factsheets/Down Syndrome Fact Sheet.pdf
- Jacob, K. S., Sharan, P., Mirza, I., Garrido-Cumbrera, M., Seedat, S., Mari, J. J., Sreenivas, V. and Saxena, S.. 2007. Mental health systems in countries: Where are we now? The Lancet, 370, 1061–1077. [DOI] [PubMed] [Google Scholar]
- Johnson, E., Nilsson, S. and Adolfsson, M.. 2019. How pain management for children with cerebral palsy in South African schools complies with up-to-date knowledge. African Journal of Disability, 8, 575–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korenberg, J. R., Kawashima, H., Pulst, S. M., Ikeuchi, T., Ogasawara, N., Yamamoto, K., Schonberg, S. A., West, R., Allen, L. and Magenis, E.. 1990. Molecular definition of a region of chromosome 21 that causes features of the Down syndrome phenotype. American Journal of Human Genetics, 47, 236–246. [PMC free article] [PubMed] [Google Scholar]
- Kusi-Mensah, K., Donnir, G., Wemakor, S., Owusu-Antwi, R. and Omigbodun, O.. 2019. Prevalence and patterns of mental disorders among primary school age children in Ghana: Correlates with academic achievement. Journal of Child & Adolescent Mental Health, 31, 214–223. [DOI] [PubMed] [Google Scholar]
- Lasater, M. E., Beebe, M., Gresh, A., Blomberg, K. and Warren, N.. 2017. Addressing the unmet need for maternal mental health services in low-and middle-income countries: Integrating mental health into maternal health care. Journal of Midwifery & Women’s Health, 62, 657–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLennan, A. H., Thompson, S. C. and Gecz, J.. 2015. Cerebral palsy: Causes, pathways, and the role of genetic variants. American Journal of Obstetrics and Gynecology, 213, 779–788. [DOI] [PubMed] [Google Scholar]
- Nyame, P. K. and Biritwum, R. B.. 1997. Epilepsy: Knowledge, attitude and practice in literate urban population, Accra, Ghana. West African Journal of Medicine, 16, 139–145. [PubMed] [Google Scholar]
- Oti-Boadi, M. 2017. Exploring the lived experiences of mothers of children with intellectual disability in Ghana. SAGE Open, 7, 215824401774557. [Google Scholar]
- Pekeberg, I. M. B. 2012. Inclusive education in Ghana: An analysis of policies and the practices of one mainstream school and one inclusive school in the Greater Accra Region (Master’s thesis). [Google Scholar]
- Philip, M., Ramu, R., Prasannan, R. V., Thomas, M., James, N. and Kathyayani, B. V.. 2021. Mothers’ knowledge of childhood neurodevelopmental disorders: Indian perspective. Journal of Neurosciences in Rural Practice, 12, 165–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinlan, M. 2005. Considerations for collecting free-lists in the field: Examples from ethnobotany. Field Methods, 17, 219–234. [Google Scholar]
- Ratajczak, H. V. 2011. Theoretical aspects of autism: Causes—A review. Journal of Immunotoxicology, 8, 68–79. [DOI] [PubMed] [Google Scholar]
- Rodríguez-Hernández, M. L. and Montoya, E.. 2011. Fifty years of evolution of the term Down's syndrome. The Lancet, 378, 402. [DOI] [PubMed] [Google Scholar]
- Rogers, S. J. and DiLalla, D. L.. 1990. Age of symptom onset in young children with pervasive developmental disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 29, 863–872. [DOI] [PubMed] [Google Scholar]
- Ruparelia, K., Abubakar, A., Badoe, E., Bakare, M., Visser, K., Chugani, D. C., Chugani, H.T., Donald, K.A., Wilmshurst, J.M., Shih, A., Skuse, D. and Newton, C. R.. 2016. Autism spectrum disorders in Africa: Current challenges in identification, assessment, and treatment: A report on the International Child Neurology Association Meeting on ASD in Africa, Ghana, April 3-5, 2014. Journal of Child Neurology, 31, 1018–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell, P. S. S., John, J. K. and Lakshmanan, J. L.. 1999. Family intervention for intellectually disabled children: Randomised controlled trial. The British Journal of Psychiatry : The Journal of Mental Science, 174, 254–258. [DOI] [PubMed] [Google Scholar]
- Ryan, G. W., Nolan, J. M. and Yoder, P. S.. 2000. Successive free listing: Using multiple free lists to generate explanatory models. Field Methods, 12, 83–107. [Google Scholar]
- Sarkodie, E. 2018. Highlights on inclusive education policy in Ghana. International Journal of Advanced Educational Research, 3, 64–68. [Google Scholar]
- Short, A. B. and Schopler, E.. 1988. Factors relating to age of onset in Autism. Journal of Autism and Developmental Disorders, 18, 207–216. [DOI] [PubMed] [Google Scholar]
- Tilahun, D., Hanlon, C., Fekadu, A., Tekola, B., Baheretibeb, Y. and Hoekstra, R. A.. 2016. Stigma, explanatory models and unmet needs of caregivers of children with developmental disorders in a low-income African country: A cross-sectional facility-based survey. BMC Health Services Research, 16, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wireko-Gyebi, S. and Ashiagbor, E.S.. 2018. Comparative study on knowledge about autism spectrum disorder among paediatric and psychiatric nurses in public hospitals in Kumasi, Ghana. Clinical Practice & Epidemiology in Mental Health, 14, 99–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) . 1997. Let's communicate: a handbook for people working with children with communication disorders (No. WHO/RHB/97.1). World Health Organization. [Google Scholar]
- Zwaigenbaum, L., Bauman, M. L., Stone, W. L., Yirmiya, N., Estes, A., Hansen, R. L., McPartland, J.C., Natowicz, M.R., Choueiri, R., Fein, D., Kasari, C., Pierce, K., Buie, T., Carter, A., Davis, P.A., Granpeesheh, D., Mailloux, Z., Newschaffer, C., Robins, D., Roley, S.S., Wagner, S. and Wetherby, A.. 2015. Early identification of Autism spectrum disorder: Recommendations for practice and research. Pediatrics, 136, S10–S40. [DOI] [PMC free article] [PubMed] [Google Scholar]