Summary
Background
Stigma exacerbates power imbalances and societal disparities, significantly impacting diverse identities and health conditions, particularly for low and middle-income countries (LMICs). Though crucial for dismantling harmful stereotypes, and enhancing healthcare utilisation, existing research on anti-stigma interventions is limited with its condition-focused approach. We aimed to thoroughly evaluate peer-reviewed and non-peer-reviewed literature for a comprehensive review of anti-stigma interventions for diverse identities and all health conditions in LMICs.
Methods
This review systematically explored peer-reviewed and non-peer-reviewed literature, in ten electronic databases up to January 30, 2024, covering all anti-stigma interventions across various stigmatised identities and health conditions in LMICs. Quality assessment for this systematic review was conducted as per Cochrane Collaboration's suggested inclusions. The review was registered with PROSPERO (Registration: 2017 CRD42017064283).
Findings
Systematic synthesis of the 192 included studies highlights regional imbalances, while providing valuable insights on robustness and reliability of anti-stigma research. Most studies used quasi-experimental design, and most centred on HIV/AIDS or mental health related stigma, with very little work on other issues. Certain high-population LMICs had no/little representation.
Interpretation
The interventions targeted diverse segments of populations and consequently yielded a multitude of stigma-related outcomes. However, despite the heterogeneity of studies, most reported positive outcomes underscoring the effectiveness of existing interventions to reduce stigma.
Funding
This study is supported by the UK Medical Research Council Indigo Partnership (MR/R023697/1) award.
Keywords: Stigma, Low-income countries, Lower-middle income countries, LMICs, Upper-middle income countries, Intervention, Systematic review
Research in context.
Evidence before this study
Low and middle-income countries (LMICs) face intensified stigma effects due to limited resources, inadequate personnel, and political backing. However, much of the existing research on anti-stigma interventions uses narrow search strategies, limits the focus on peer-reviewed publications or on specific conditions, without looking at commonalities and intersectionality. To address this, we conducted a comprehensive systematic review, searching ten peer-reviewed and non-peer-reviewed databases up to January 30th, 2024, using an extensive range of search terms and identified 192 studies from six WHO regions.
Added value of this study
In this study, we present a comprehensive review of the most updated evidence from 192 studies from lower and middle income countries (LMICs), encompassing anti-stigma interventions across a wide spectrum and includes all stigmatised issues, identities, and conditions. While the findings highlight lack of representation in some countries and a higher focus on HIV/AIDS and mental health, they also underscore the effectiveness of existing interventions to reduce stigma.
Implications of all the available evidence
In alignment with the Lancet Commission on ending stigma and discrimination, findings of the current review highlight the need for culturally, socially and contextually relevant co-designed interventions in LMICs and to focus on key ingredients, invest in capacity building in resource-poor settings and provide training and support to local researchers to build sustainable research capacity.
Introduction
Stigma, defined as the co-occurrence of stereotyping, separating, status loss, and discrimination in the context of power inequities,1 impacts individuals with a wide range of health conditions (e.g., HIV, mental illnesses) and identities (e.g., racial and sexual minorities). When taking all stigmatised identities and conditions into account, stigma affects a large segment of the population at any given time, and most people are stigmatised at some point in their lives. Stigma has been increasingly recognised as a fundamental cause of health disparities,2 given that it drives mortality and morbidity through a wide range of mechanisms. These include limited access to structural resources,3 social isolation,4 maladaptive emotion regulation and coping,5 and stress exposure.6 The impacts of stigma7,8 are exacerbated in low-income and-middle-income countries (LMICs) because of the scarcity of funding, insufficient human resources, and lack of political support to address stigma and introduce appropriate anti-stigma interventions for optimal health and social outcomes.9, 10, 11, 12 Moreover, most research on stigma tends to adopt a condition-specific approach without examining the common features and mechanisms underlying stigmatised conditions.13 This approach misses the opportunity to understand and address stigma in a more comprehensive way, while also hindering the exploration of important concepts such as intersectionality.14,15
Three recent papers have systematically reviewed the literature broadly (i.e., not focused on a single condition) on health-related stigma reduction interventions in LMICs. Focusing on stigma related to health conditions, Rao et al.16 emphasised the importance of addressing stigma at multiple socio-ecological levels (i.e., individual, interpersonal, community, and structural)17 and limited their review to those interventions that target more than one level. Also focusing on stigma related to health conditions, Kemp et al.18 surveyed stigma reduction interventions that assessed at least one implementation outcome (e.g., feasibility, acceptability, cost), with the goal of understanding the potential for implementing anti-stigma programs in LMICs. Most recently, Hartog et al.19 synthesised stigma reduction interventions that specifically target children in LMICs and compared these to adult-focused interventions, with a specific focus on interventions that had a primary objective of reducing stigma (i.e., including “stigma” in the article title). Taken together, these reviews showed that most of the stigma reduction interventions in LMICs were based in Sub-Saharan Africa, addressed HIV-related stigma, and utilised education-based strategies. They also showed that, while a majority of the reviewed studies reported a decline in at least one stigma-related outcome, effect sizes varied widely in magnitude or were often not reported. Further, there were few randomised controlled trials (RCTs) and no systematic examination of implementation outcomes, suggesting that more rigorous research is needed in this area.20
The literature also highlights two important knowledge gaps in our understanding of stigma reduction interventions in LMICs. First, all three reviews cited above included only studies that have been published in peer-reviewed journals. Inclusion of grey literature (i.e., non-peer reviewed studies) in systematic reviews is essential, as doing so has been shown to minimise the potential effects of publication bias and lead to more accurate effect size estimates in meta-analyses.21,22 Second, to our knowledge, Hartog et al.19 represent the only systematic review to date that does not restrict its focus to interventions addressing health-related stigmas, though its scope might have been limited by the authors’ narrow search strategy. Specifically, their decision to only include those interventions with the primary objective of reducing stigma might have missed interventions designed for other purposes, given that disease prevention interventions and awareness raising programs often contain stigma measures as secondary outcomes. Further, their exclusive use of the term “stigma” (without also including synonyms such as “prejudice” and “discrimination”) made it less likely for the review to capture interventions that target attitudes towards women and racial/ethnic minority groups, as “stigma” is more commonly used to characterise the social devaluation of health conditions.23 In order to paint a more complete picture of the existing stigma reduction interventions in LMICs, our objectives were to systematically examine peer-reviewed and non-peer reviewed literature on all health-related stigma reduction interventions addressing all stigmatised identities and health conditions in LMICs.
Methods
This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines24 and was registered with PROSPERO International Prospective Register of Systematic Reviews (PROSPERO 2017 CRD42017064283). Our team included authors with experience and expertise in stigma research and in developing, implementing, and evaluating anti-stigma interventions and guidelines to ensure the review's relevance and contextual insight for data interpretation.
Search strategy
Ten electronic databases were systematically searched in English up to January 30, 2024: Medline, PsycInfo, the Cochrane Library, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), the Social Science Citation Index (SSCI) were used for peer-reviewed literature, while, Latin American and Caribbean Health Sciences Literature (LILACS), Scileo, Global Health, OpenGrey, and Bielefeld Academic Search Engine (BASE) Search were included to focus on a broader range of literature, including grey literature from various disciplines. A comprehensive set of search terms relating to different types of stigma targeted interventions, and study design were used in each database, as well as subject headings specific to each database (Supplementary Table S2). The Boolean operators “AND” and “OR” were used to combine terms. No limits were set with regards to year of publication or language. Experts in the field were identified from studies included in the initial search and from the authors’ knowledge and were contacted for further recommendations of relevant articles. Reference lists of relevant systematic reviews were searched for additional articles. The methods are reported in line with the PRISMA guidelines.
Inclusion and exclusion criteria
Studies were considered eligible for inclusion if they met all of the following a priori criteria: (1) the impact of an intervention on stigma (characterised in terms of knowledge, attitudes, and behaviour,25,26 as supported by existing literature and aligning with recognised evaluation frameworks for evaluating anti-stigma interventions)26,27 was evaluated; and (2) the setting was a low- or middle-income country defined by World Bank classification for the year of publication. No restrictions were based on the type of stigma targeted or the type of intervention that was used as long as stigma was included as a primary or secondary outcome in the intervention evaluation. The review included published, unpublished or non-peer reviewed research across several quantitative study designs to summarise anti-stigma interventions: Randomised and non-randomised controlled trials, controlled and uncontrolled pre-post, controlled post only and observational studies. Qualitative studies were excluded; however, studies were not excluded based on their country of origin, the language of publication or low quality assessment. Studies were included if a translated version could be accessed or a collaborator with appropriate language skills could be found (Supplementary Table S3).
Study selection and data extraction
Endnote28 and the Covidence29 tools were used to remove duplicate studies and to conduct screening. After databases had been searched and duplicates removed, eleven reviewers (DG, EB, TM, SN, SEL, GH, MS, NV, PCG, NF, CM, LP, TB and YS) participated in the screening and selection process. For reliability purposes, four sets of 400 references each were initially selected for the preliminary step of double screening. All reviewers then discussed issues raised, and refined and clarified inclusion and exclusion criteria together. In the second stage, each reviewer re-screened the initial abstracts in light of the group discussion and then screened the remaining abstracts. As inter-rater reliability was greater than 85%, the remaining records were then screened individually. Three reviewers (GH, TM and SN) identified those studies that were conducted in LMIC settings, followed by the other reviewers who then reviewed full text reports of potentially relevant studies. Reviewers then abstracted study and intervention characteristics on a shared spreadsheet using a pre-piloted data extraction form. At the study level, information was extracted on: (i) study design (including aims, design, sample size, length of follow-up periods); (ii) participant characteristics; (iii) study location; (iv) type of condition/focus of intervention; (v) intervention details (including: content and aims of intervention, lead agency, training provided, type of facilitators, mode of delivery [face-to-face, internet], format [one-to-one or group], frequency and duration of delivery); (vi) details of control/comparison conditions; (vii) timing of assessment; and (vii) results of the study.
Quality assessment
Quality assessment for this systematic review was conducted as per Cochrane Collaboration's suggested inclusions: how the study was designed, conducted, analysed, interpreted, and reported to avoid systematic errors. The Rigour and quality of studies were therefore comprehensively assessed using the ‘Evidence for Policy and Practice Information and Co-ordinating Centre’ method due to its comprehensive assessment of various study designs and its reliability.30 The criteria of assessment included: (i) aims clearly stated, (ii) design appropriate to the stated objectives, (iii) justification given for sample size, (iv) evidence provided of reliability or validity of measures used, (v) statistics accurately reported, and (vi) sample selection relatively unbiased.31 As it was a comprehensive quality assessment as per Cochrane Collaboration's suggested inclusions, a separate risk of bias assessment was not conducted.
The risk of publication bias arises when only published studies are included in systematic reviews, leading to the possibility of an overestimation of intervention effectiveness. Our systematic review attempted to mitigate this bias by including grey literature32,33 and hence avoiding the effects of selective publication and providing a more balanced understanding of the evidence. Consequently, a separate assessment of publication bias was not undertaken.32
Statistical analysis and synthesis
The categories of interventions were developed based on the types of interventions evaluated in the included studies and outcomes are presented according to these categories. Each study was further characterised according to: nature of intervention, stigma-related outcomes assessed, duration of follow-up and effectiveness for stigma reduction. We also looked at which studies assessed some type of behavioural outcome.20 If studies reported inconsistent results across the sample or at follow-ups, we labelled the intervention as having mixed results for that outcome.
Due to heterogeneity of the study designs, interventions, and outcomes of the included studies, SWiM (Synthesis Without Meta-analysis) reporting guidelines were used to present data synthesis using descriptive vote counting and grouping the included studies.34,35 Vote counting compared the number of studies in which a particular outcome improved, with the number of studies in which that outcome did not improve, based only on the direction of effect. However, magnitude of the effect was not measured and reported due to diversity of the designs, interventions, and outcomes of the included studies. Additionally, we produced a standard binary metric (benefit or mixed results), which was used to calculate a proportion, 95% CI (binomial exact calculation) and p-value (binomial probability test) to show the evidence for each intervention category's effectiveness across outcome measures.
Ethics
Due to the nature of the research, the present study did not require informed consent or approval by the local Ethics Committees.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. All the authors had full access to data, and all authors (TM, GH, KW, SN, NV, PG, DG, MS, TB, NF, CM, LP, EB, CL, GT and SEL) were responsible for the decision to submit the manuscript.
Results
Overview
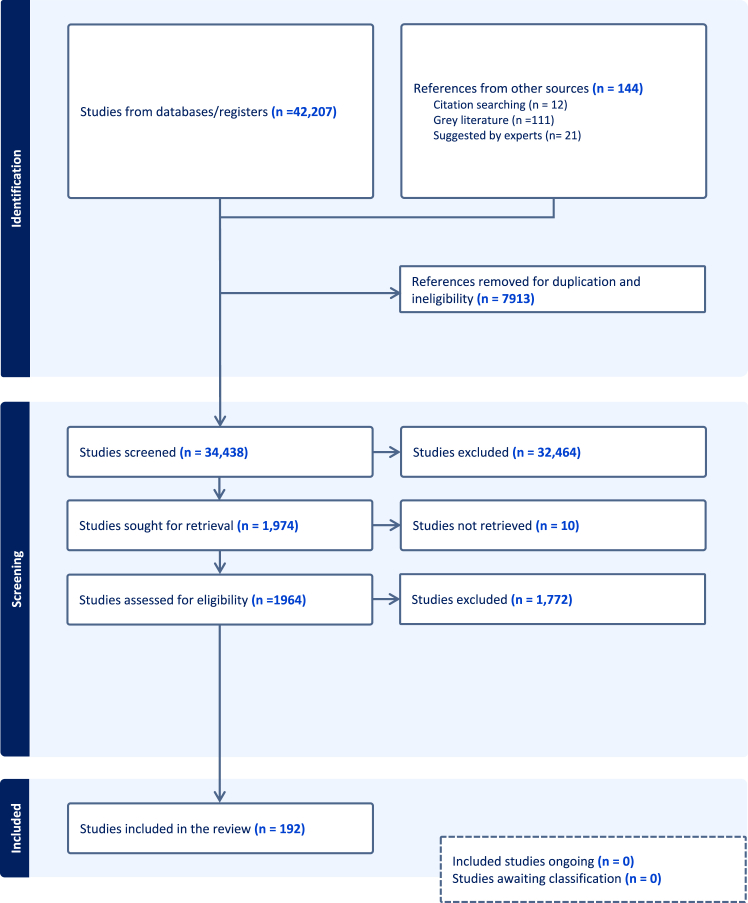
A total of 42,207 studies were identified from the database search; a further 144 references were located from expert recommendations, grey literature, and reference checking. After removal of duplicates, 34,438 studies were screened according to inclusion criteria and the full texts of 1974 studies from LMIC settings were retrieved to make a final decision on eligibility. 192 studies were found to be eligible for inclusion and were included (Fig. 1). All included studies are referenced in the Supplementary Material (Supplementary Table S4).
Fig. 1.
PRISMA diagram legend: reports the number of studies identified by the search strategy, the number of studies excluded and included during the screening process, and the final number of studies included in the systematic review. This is a coloured figure with separate bars identifying 3 stages of the Prisma diagram.
Setting and population characteristics
The setting and population characteristics of included studies are outlined in Table 1. The majority of studies were conducted in countries in the African (n = 92, 47.9%) and Western Pacific (n = 38, 19.8%) WHO regions, with China (n = 27), India (n = 20) and South Africa (n = 20) being the countries most represented. Most studies were from lower middle-income (n = 97, 50.5%), followed by upper middle-income (n = 74, 38.5%) and low-income (n = 38, 19.8%) countries (some included studies were conducted across multiple countries, and WHO regions and belonged to different income groups). Only a few studies (18.6%) were from before 2009, showing an increase in the published literature over the last decade, especially in lower middle-income countries.
Table 1.
Setting and population characteristics.a
| Characteristic | N = 192a | %a |
|---|---|---|
| World Health Organisation (WHO) Region and Country | ||
| Africa | 92 | 47.9 |
| Americas | 32 | 16.6 |
| Eastern Mediterranean | 10 | 5.2 |
| Europe | 8 | 4.1 |
| Southeast Asia | 33 | 17.2 |
| Western Pacific | 38 | 19.8 |
| Country income group | ||
| Low | 38 | 19.8 |
| Lower-Middle | 97 | 50.5 |
| Upper-Middle | 74 | 38.5 |
| Stigma context | ||
| Alcohol and drug use | 6 | 3.1 |
| Disabilities | 6 | 3.1 |
| Ethnicity/Race/Religion | 11 | 5.7 |
| Gender, Sexuality &Women's healthb | 12 | 6.3 |
| HIV/AIDSc | 104 | 54.2 |
| Leprosy | 4 | 2.1 |
| Mental health | 46 | 24.0 |
| Tuberculosis | 4 | 2.1 |
| COVID 19d | 1 | 0.5 |
| Target populatione | ||
| Caregivers of people living with stigmatised conditions | 11 | 5.7 |
| Children and adolescents | 25 | 13.0 |
| College and university students | 12 | 6.3 |
| Criminal justice professionals | 2 | 1.0 |
| Community leaders | 4 | 2.1 |
| General population | 50 | 26.0 |
| Health professionals | 58 | 30.2 |
| High risk groupsf | 12 | 6.3 |
| People living with stigmatised conditions | 23 | 12.0 |
| Academic researchers | 1 | 0.5 |
| Survivors and perpetrators of genocide | 2 | 1.0 |
| Teachers | 7 | 3.6 |
Some included studies were conducted in multiple countries and WHO regions, and which belonged to different income groups, or addressed more than one stigma contexts. Therefore, not all counts and percentages will add up to 100%.
Women's health includes studies on FGM, female birth attendants etc.
Human Immunodeficiency Virus (HIV) and Acquired Immune Deficiency Syndrome (AIDS).
Coronavirus Disease 2019.
Some studies had more than one target population group.
Included: sex workers, market vendors, the military.
The primary outcome in about two-thirds of the studies (n = 124, 64.6%) was evaluating the effects of interventions on stigma. In the remaining studies (n = 68, 35.4%), stigma was a secondary outcome, and the primary outcome/focus was usually either a change in factual knowledge about a health condition, a reduction in health risk behaviour (e.g., increased condom use), or improving symptoms of the health condition (i.e., psychoeducation to improve symptoms) with stigma reduction as a secondary outcome. The largest group of studies focused on stigma related to HIV/AIDS (n = 104, 54.2%) followed by mental health (n = 46, 24.0%), with a range of other health conditions and stigmatised characteristics, such as ethnicity, race or religious issues (n = 11, 5.7%), and or sex, gender, sexuality and women's health issues (n = 12, 6.3%). The most common target groups were: health professionals (n = 58, 30.2%), the general population (n = 50, 26.0%), children and adolescents (n = 25, 13.0%), or people living with the targeted stigmatised conditions (n = 23, 12.0%).
Design characteristics
The design characteristics of included studies are outlined in Table 2. Many of the studies (56.8%) used a quasi-experimental design, while 34.3% and 8.9% used RCTs and non-experimental designs respectively. About two-thirds of studies (n = 131, 68.2%) conducted only one follow up assessment.
Table 2.
Study design characteristics.
| Characteristic | N = 192 | % |
|---|---|---|
| Design | ||
| Cluster Randomised Controlled Trial (RCT) | 31 | 16.1 |
| Individual Randomised Controlled Trial (RCT) | 35 | 18.2 |
| Quasi-Experimentala | 109 | 56.8 |
| Non-Experimentalb | 17 | 8.9 |
| Timing of first follow-Upc, d | ||
| Immediate | 67 | 34.9 |
| Short | 18 | 9.4 |
| Medium | 60 | 31.3 |
| Long | 38 | 19.8 |
| Not described | 10 | 5.2 |
| Timing of subsequent follow-Ups | ||
| Short | 11 | 5.7 |
| Medium | 21 | 11.0 |
| Long | 29 | 15.1 |
| Not described | 131 | 68.2 |
Quasi-experimental: non-randomised research design where a control/pre/post group or variable was chosen by researchers.
Non-experimental: research design focusing solely on observation, interaction and interpretation, without any control on predictor variable or subjects.
Follow up was determined to be immediate if it took place immediately after the intervention concluded; short term if below 1 month; medium term if between 1 and 6 months; long term if over 6 months.
Some included studies had two different first follow-up times for intervention and control groups. Therefore, not all counts and percentages will add up to 100%.
Intervention characteristics
Intervention characteristics are outlined in Table 3. Almost all interventions had an educational component (n = 168, 87.5%) but only about one-third incorporated social contact with a person living with the stigmatised health condition or characteristic (n = 75, 39.1%). Social contact can be defined as contact between people with and without experience of mental disorders.26,36,37 The type of contact included varied between meeting a person in real life, to virtual, or guided imagining of interactions. A small number of interventions provided increased access or outreach for services (n = 25, 13.0%). A few studies provided booster sessions that took place after the initial intervention (n = 15, 7.7%).
Table 3.
Intervention characteristics.
| Intervention characteristic | N = 192 | % |
|---|---|---|
| Nature of interventionsa | ||
| Educational | 168 | 87.5 |
| Social contact | 75 | 39.1 |
| Increased access to services | 25 | 13.0 |
| Counselling/mentoring/case management | 11 | 5.7 |
| Social activism | 11 | 5.7 |
| Not described | 3 | 1.7 |
| Booster session | ||
| Yes | 15 | 7.7 |
87 (45.3%) studies used more than one type of intervention and therefore not all counts and percentages will add up to 100%.
Outcomes
Table 4 presents information on the direction of effects in the included studies. Most studies showed statistically significant positive effects on reducing stigma (n = 158, 82.2%), with a few showing increases in stigma (n = 3, 1.6%) or no significant effect (n = 27, 14.1%). In one study, it was not possible to state a direction of effect due to the lack of a pre-post comparison.
Table 4.
Change in stigma outcomes according to study characteristics.
| Intervention characteristic | Negative effect n (%) | No significant effect n (%) | Positive effect n (%) | Mixed effect n (%) | NAˆ n (%) |
|---|---|---|---|---|---|
| All studies (n = 192) | 3 (1.6) | 27 (14.1) | 158 (82.2) | 3 (1.6) | 1 (0.5) |
| Educational | |||||
| Yes (n = 168) | 3 (1.8) | 22 (13.1) | 139 (82.7) | 3 (1.8) | 1 (0.6) |
| No (n = 21) | 0 (0.0) | 4 (19.0) | 17 (81.0) | 0 (0.0) | 0 (0.0) |
| Not described (n = 3) | 0 (0.0) | 2 (66.7) | 1 (33.3) | 0 (0.0) | 0 (0.0) |
| Contact | |||||
| Yes (n = 75) | 0 (0.0) | 7 (9.3) | 67 (89.3) | 1 (1.3) | 0 (0.0) |
| No (n = 114) | 3 (2.6) | 15 (13.2) | 92 (80.7) | 3 (2.6) | 1 (0.9) |
| Not described (n = 3) | 0 (0.0) | 2 (66.7) | 1 (33.3) | 0 (0.0) | 0 (0.0) |
| Increased access to service | |||||
| Yes (n = 25) | 1 (4.0) | 4 (16.0) | 20 (80.0) | 0 (0.0) | 0 (0.0) |
| No (n = 164) | 2 (1.2) | 22 (13.4) | 136 (83.0) | 3 (1.8) | 1 (0.6) |
| Not described (n = 3) | 0 (0.0) | 2 (66.7) | 1 (33.3) | 0 (0.0) | 0 (0.0) |
| Booster | |||||
| Yes (n = 15) | 0 (0.0) | 1 (6.7) | 13 (86.7) | 1 (6.7) | 0 (0.0) |
| No (n = 170) | 2 (1.2) | 23 (13.5) | 141 (82.9) | 3 (1.8) | 1 (0.6) |
| Not described (n = 7) | 1 (14.3) | 1 (14.3) | 5 (71.4) | 0 (0.0) | 0 (0.0) |
| Behavioural outcome measures | |||||
| Yes (n = 61) | 2 (3.3) | 6 (9.9) | 51 (83.6) | 1 (1.6) | 1 (1.6) |
| Length of follow-up | |||||
| Medium-term follow-up (>1 and ≤ 6 months) | |||||
| Yes (n = 62) | 2 (3.2) | 8 (12.9) | 52 (83.9) | 0 (0.0) | 0 (0.0) |
| Long-term follow-up (>6 months) | |||||
| Yes (n = 40) | 0 (0.0) | 8 (20.0) | 32 (80.0) | 0 (0.0) | 0 (0.0) |
There was no association between nature of intervention and change in stigma outcomes. A higher proportion of studies that included a booster component had a positive impact compared to those that did not (90.0% versus 82.5%), however, this was not statistically significant, (p = 0.418).
Some studies (61/192) explored the impact of anti-stigma interventions on behaviour. Of these studies, 51 (83.6%) found a positive impact of the intervention. The stigma targeted in these sixty one studies were HIV/AIDS (n = 24, 12.5%), mental health (n = 22, 11.5%), leprosy (n = 1, 0.5%), tuberculosis (n = 4, 2.1%), ethnicity (n = 2, 0.4%) and gender/sexuality (n = 5, 2.6%) and COVID 19 (n = 1, (0.5%). Forty percent (n = 70) of studies used validated measures when measuring the main stigma outcome. See Table 4 for further information.
Quality assessment
Forty eight percent studies met either three (n = 36) or four (n = 56) of the six quality assessment criteria (Table 5). Of the studies that met all six criteria (n = 35), the majority were from the upper middle-income group, employed a quasi-experimental design, and had health professionals as their target group. Twenty-five studies were judged to have met fewer than three items and were of very low quality. The majority of studies did not provide justification for sample size or were not able to show that reliable and valid measures were used. Only 60% of the studies appeared to recruit samples that had a relatively low risk of bias and were likely to be generalisable to a wider population. No studies were excluded because of their quality.
Table 5.
Quality assessment of included studies (N = 192).
| Quality criteria | Yes |
No |
Unclear |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Were aims clearly stated? | 171 (89.1) | 21 (10.9) | 0 |
| Were designs appropriate for the stated objectives? | 172 (89.6) | 19 (9.9) | 1 (0.5) |
| Was a justification for sample size given? | 76 (39.6) | 116 (60.4) | 0 |
| Was evidence on reliability and validity of measures provided? | 83 (43.2) | 109 (56.8) | 0 |
| Were statistics reported accurately? | 164 (85.4) | 27 (14.1) | 1 (0.5) |
| Was the sample selection relatively unbiased? | 116 (60.4) | 67 (34.9) | 9 (4.7) |
Discussion
We set out to conduct a systematic review of anti-stigma intervention studies in LMICs using a comprehensive search strategy. This included both published and unpublished studies, and studies for which stigma reduction was a primary or secondary aim. The findings of this review highlight the effectiveness of various types of anti-stigma interventions across different conditions and identities.
We identified a total of 192 studies, a significantly larger number than those included in prior reviews.16,18,19 Moreover, whereas prior reviews16,18,19 identified relatively few RCTs in LMIC contexts, 34.3% of the studies included in this review were RCTs. We found that the primary outcome of most studies was to assess the effect of interventions on stigma, with the majority (>78%) of the studies focusing on HIV/AIDS and mental health using a quasi-experimental design. Specifically, a majority of the studies focused on stigma related to HIV/AIDS, took place in African or Western Pacific countries, and were published after 2009. These trends reflect the prioritisation of HIV-related work in global health spending,38,39 and an increased urgency in the research community towards developing stigma reduction interventions in the past decade. A significant proportion of studies where stigma was a secondary outcome were also successful in improving stigma related knowledge, attitude or behaviours. For instance, an intervention where the main focus was on teaching school students about HIV/AIDS and its prevention, also resulted in improved knowledge and attitude towards people with AIDS.40 This finding reflects on the importance of integrating stigma as a secondary outcome in different interventions so as to adopt a holistic approach, to leverage and maximise existing programs, resources and infrastructure. This becomes especially important in the context of LMICs, as we continue to gradually dismantle stereotypes, while also focusing on a wide variety of health and other issues.
The process for conducting this review involved complex parameters, as it included various stigmatised conditions and identities (HIV/AIDS, mental health, ethnicity, sexuality etc) and also entailed a wide array of anti-stigma interventions, spanning from interventions aimed at enhancing knowledge, modifying behaviour, shaping attitudes, to improving healthcare practices. These interventions were implemented by diverse stakeholders, including governmental bodies at local or higher levels, non-governmental organisations (NGOs), and researchers. Moreover, the interventions targeted diverse segments of the population, ranging from healthcare professionals, students, teachers and caregivers to individuals who personally experience stigma. Consequently, the interventions yielded a multitude of outcomes related to stigma, which in turn affected the health, livelihoods, as well as the social and economic dimensions of those impacted by stigma.
While the breadth of this review makes it difficult to explore the underlying mechanisms involved in stigma reduction, we identified several common strategies employed across a range of stigmatised conditions. These strategies include education, contact, social activism and increasing access to services and support. Despite the heterogeneity of studies included in our review which makes it difficult to compare the effectiveness of these strategies, it is notable that most studies (>82%) reported positive outcomes. This suggests that these strategies have a promising potential to reduce stigma in global settings, and that they may also be relevant for conditions and identities which were less represented in our review (e.g., tuberculosis, polio, sexuality). Indeed, apart from HIV/AIDS and mental health, there is very little work on other conditions or issues. We only found eight studies on tuberculosis and leprosy, and no studies were found for some other highly stigmatised health issues like polio where stigma may be impacting eradication attempts and reduction in morbidity.41,42 This is a major gap in current anti-stigma research. Furthermore, we found that many interventions were informed by social psychological theories in some way. In particular more than one-third of studies included some type of social contact, drawing on seminal works like Allport's’ Contact Theory,43 and also other theoretical frameworks such as Social Cognitive Theory,44 Attribution Theory,45 Stereotype Content Model46 and Social Identity Theory.47 These theories have been instrumental in advancing our understanding of stigma and facilitating the development of effective interventions.48,49
Another notable finding was how some regions and countries are overrepresented in research, whilst many high-population LMICs had no or very little representation. Although alarming, this can be attributed to a combination of interrelated factors. One significant factor is more pronounced scarcity of resources and funding allocations for research in some countries, compared to others. For instance, China and South Africa (upper middle-income countries) have made significant investments in research and have established international research collaborations, while Bangladesh (also an upper middle-income country) has limited infrastructure. Hence, many LMICs face competing priorities such as addressing immediate public health challenges and resource constraints, diverting attention and resources away from stigma-related research.10,11 Insufficient research infrastructure, including dedicated institutions and trained researchers focused on stigma research, further contributes to the gap in anti-stigma studies, within the LMICs.9,12 Moreover, development and implementation of effective anti-stigma interventions require cultural sensitivity and adaptation to ensure their effectiveness in specific populations,50 which can be challenging due to disparities in health, economic inequities and inequalities in LMICs.51
The findings of this review also provide valuable insights into the robustness and reliability of anti-stigma research and highlights the varying quality. RCTs were adopted by 34.3% studies, with almost 50% conducted in upper-middle income countries and few in low and low-middle income countries, highlighting the issue of feasibility and resource allocation to conduct good quality RCTs in low-resource settings. Most studies (>56%) employed a quasi-experimental design. However, for large-scale population-based anti-stigma interventions, quasi-experimental studies could be a preferred design as identifying unaffected control groups for RCTs could be challenging in resource-poor settings. Future studies, however, could be strengthened by employing stronger quasi-experimental designs including matched control groups or multiple baseline assessment points, or employing mixed methods where contextual information along with quantitative data can facilitate an inclusive, community engaged approach with strong participation that strengthens the validity and relevance of findings.
Moreover, many included studies had methodological or reporting limitations, such as the lack of validated stigma outcome measures and the justification for the sample size, or the effect size estimates. These limitations affect the validity and generalizability of their findings, as well as the comparability and synthesis of the results across different studies. Therefore, our review emphasises the importance of maintaining methodological rigor and improving data quality and reporting standards in anti-stigma research in LMICs. To achieve this, researchers should consider adopting strong quasi-experimental designs that involve matched control groups or multiple baseline assessment points, or mixed methods that combine quantitative and qualitative data to provide a more comprehensive and contextualised evaluation of intervention effectiveness. By using these alternative designs when RCTs are not feasible, researchers can overcome some of the challenges associated with limited resources while still providing valid and reliable evidence on anti-stigma interventions in LMICs. More than 40% studies scored five or higher (out of six) in quality assessment, indicating the robustness of their approach.
The current systematic review was based on a comprehensive search strategy using terms related to diverse populations and a range of databases for peer-reviewed and non-peer-reviewed (grey) literature. Our review identified a recent increase in relevant non-peer-reviewed (grey literature) materials, including unpublished academic papers, reports, and ongoing research across various fields. These materials reported ongoing research, preliminary findings, as well as significant, marginally significant, or insignificant results. However, a detailed sub-analysis specifically focussing on grey literature was not performed. Additionally, experts within this area were consulted and publications of relevant experts and systematic reviews were hand searched. However, it is possible that, due to the complex and broad nature of the review, some published and grey literature may have been missed.
Our decision to include all studies, regardless of quality, has resulted in broader inclusion which increased the comprehensiveness and genralisability of the review findings. However, this may have resulted in the inclusion of less robust results. As the robustness of research conducted in LMICs improves, subsequent reviews may consider prioritising robustness over breadth of included studies.
Further, because of the broad nature of this review, it was not possible to delve in detail into the underlying mechanisms of the interventions, or to consider, for example, the relative effectiveness/efficacy of stigma reduction interventions for different conditions (e.g., mental health versus HIV versus sexuality). Also, considering the heterogeneity across the studies, and the inclusion of all studies that met the inclusion criteria regardless of their quality, meta-analysis was not conducted in order to avoid any misleading results.52 Conducting sub-group analyses for all the various stigma contexts/types of interventions/target populations was also beyond the objective and scope of this review. Nevertheless, a strength of this review was our ability to identify some commonalities of stigma reduction interventions (e.g., inclusion of educational and contact components) that have demonstrated effectiveness across diverse conditions. Utilising a more integrated approach which acknowledges these commonalities might help overcome the limitations of a siloed, condition-specific response and further acknowledges the intersectionality of many marginalised conditions.
The existing research gap pertaining to certain stigmatised conditions serves as a clear call to action, underscoring the crucial role of policymakers, funding organisations, healthcare providers and researchers in adopting cross-cutting strategies and fostering collaboration to address this global concern.
It is imperative to prioritise fair distribution of global research funding to LMICs, with evidence underscoring the urgent need for action in at least three key areas: i) capacity building to position researchers in LMICs to lead and participate in high impact research, ii) fostering high quality collaborative initiatives to drive research and innovation; and iii) designing sustainable funding models to avoid undermining programs in LMICs due to irregular funding.53 Building capacity is vital for improving the quality of anti-stigma research particularly in areas or conditions with high levels of stigma which are under-represented in the literature. Individual capacity could be built by providing training and support to researchers in LMICs working in these areas to develop their expertise in conducting strong quasi-experimental studies which would enable the development of long-term research capacity, enabling more rigorous and contextually relevant studies. In addition to incorporating anti-stigma projects in existing formal research training at Masters and PhD level, this could include developing user-friendly research training guidelines specifically tailored for anti-stigma research across conditions. Training guidelines could cover research design, methods for improving the quality of data collection and reporting, but also training and support around including social contact elements and assessment of behavioural outcomes. Organisational capacity and a culture of collaboration can be improved by providing sustained funding to anti-stigma interventions to build teams of researchers who have the capacity and funding to conduct high quality research and by fostering collaborations within LMICs. Better collaboration will support sustainable research, reposition researchers from LMICs in the global knowledge economy and eventually lead to independent, stronger health systems.
In addition, work to improve the comparability of anti-stigma research, for example, by developing a core outcome set for anti-stigma interventions54 which are appropriate for use in both LMIC and HIC, will allow us to understand more about what works for whom across contexts and under what circumstances.
Addressing the dearth of anti-stigma research in LMICs requires collaborative efforts among governments, international organisations, and research institutions. Prioritising health stigma reduction is essential, accompanied by the allocation of adequate resources for research infrastructure. Additionally, fostering interdisciplinary collaborations and promoting partnerships with researchers to enhance capacity building and knowledge sharing.55,56
In conclusion, overcoming the barriers to anti-stigma research in LMICs is crucial for advancing stigma reduction efforts and promoting equality, population health and well-being. By prioritising and investing in anti-stigma research, we can drive positive change and improve the lives of diverse marginalised populations in these settings.
Contributors
GH and SEL designed and coordinated the review. GH and TM executed the search strategy. GH, TM, NV, SN, PCG, DG, MS, EB, NF, CM, LP, TB and SEL screened titles and abstracts and full text reports and extracted data. GH, TM, SEL, KW interpreted the findings and prepared the initial draft of the manuscript. All the authors had full access to data, however, TM and SEL were responsible for the verification of the data (including collection, analysis, and interpretation). NV, PCG, MS, EB, CL, SEL and GT provided revision of the manuscript for important intellectual content.
All the authors agreed to submit the manuscript for publication.
Data sharing statement
The data generated during the current study are available in the text and Supplementary material. Further data can be made available from the corresponding author on reasonable request.
Declaration of interests
None to declare.
Acknowledgements
This study is supported by the UK Medical Research Council Indigo Partnership (MR/R023697/1) award. GT is supported by the National Institute for Health Research (NIHR) Applied Research Collaboration South London at King’s College London NHS Foundation Trust, and by the NIHR Asset Global Health Unit award. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. GT is also supported by the Guy's and St Thomas' Charity for the On Trac project (EFT151101), and by the UK Medical Research Council (UKRI) in relation to the Emilia (MR/S001255/1) and Indigo Partnership (MR/R023697/1) awards. CL is supported by the NIHR ASSET Global Health Unit award. NV is supported by the UK Medical Research Council (UKRI) in relation to the Emilia project (MR/S001255/1). PCG is supported by the UK Medical Research Council (UKRI) in relation the Indigo Partnership (MR/R023697/1) award. DG is supported by the U.S. National Institutes of Health (R01MH120649). MS is supported by the Global Health Research Unit for Neglected Tropical Diseases at the Brighton & Sussex Medical School, which is funded by the National Institute for Health and Care Research (NIHR) (NIHR131996). KW is supported U.S. National Institutes of Health (K01DA045738).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2024.102612.
Appendix A. Supplementary data
References
- 1.Link B.G., Phelan J.C. Conceptualizing stigma. Annu Rev Sociol. 2001;27(1):363–385. [Google Scholar]
- 2.Hatzenbuehler M.L., Phelan J.C., Link B.G. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hatzenbuehler M.L. Structural stigma: research evidence and implications for psychological science. Am Psychol. 2016;71(8):742. doi: 10.1037/amp0000068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pachankis J.E. The psychological implications of concealing a stigma: a cognitive-affective-behavioral model. Psychol Bull. 2007;133(2):328. doi: 10.1037/0033-2909.133.2.328. [DOI] [PubMed] [Google Scholar]
- 5.Hatzenbuehler M.L. How does sexual minority stigma "get under the skin"? A psychological mediation framework. Psychol Bull. 2009;135(5):707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Major B., O'Brien L.T. The social psychology of stigma. Annu Rev Psychol. 2005;56:393–421. doi: 10.1146/annurev.psych.56.091103.070137. [DOI] [PubMed] [Google Scholar]
- 7.Beyrer C. Pushback: the current wave of anti-homosexuality laws and impacts on health. PLoS Med. 2014;11(6):e1001658–e. doi: 10.1371/journal.pmed.1001658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mascayano F., Armijo J.E., Yang L.H. Addressing stigma relating to mental illness in low- and middle-income countries. Front Psychiatry. 2015;6:38. doi: 10.3389/fpsyt.2015.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chisholm D., Flisher A.J., Lund C., et al. Scale up services for mental disorders: a call for action. Lancet. 2007;370(9594):1241–1252. doi: 10.1016/S0140-6736(07)61242-2. [DOI] [PubMed] [Google Scholar]
- 10.Lund C., De Silva M., Plagerson S., et al. Poverty and mental disorders: breaking the cycle in low-income and middle-income countries. Lancet. 2011;378(9801):1502–1514. doi: 10.1016/S0140-6736(11)60754-X. [DOI] [PubMed] [Google Scholar]
- 11.Patel V., Chisholm D., Parikh R., et al. Addressing the burden of mental, neurological, and substance use disorders: key messages from disease control priorities, 3rd edition. Lancet. 2016;387(10028):1672–1685. doi: 10.1016/S0140-6736(15)00390-6. [DOI] [PubMed] [Google Scholar]
- 12.Shidhaye R., Kermode M. Stigma and discrimination as a barrier to mental health service utilization in India. Int Health. 2013;5(1):6–8. doi: 10.1093/inthealth/ihs011. [DOI] [PubMed] [Google Scholar]
- 13.van Brakel W.H., Cataldo J., Grover S., et al. Out of the silos: identifying cross-cutting features of health-related stigma to advance measurement and intervention. BMC Med. 2019;17(1):13. doi: 10.1186/s12916-018-1245-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weiss M.G., Ramakrishna J., Somma D. Health-related stigma: rethinking concepts and interventions. Psychol Health Med. 2006;11(3):277–287. doi: 10.1080/13548500600595053. [DOI] [PubMed] [Google Scholar]
- 15.Scambler G. Health-related stigma. Sociol Health Illn. 2009;31(3):441–455. doi: 10.1111/j.1467-9566.2009.01161.x. [DOI] [PubMed] [Google Scholar]
- 16.Rao D., Elshafei A., Nguyen M., Hatzenbuehler M.L., Frey S., Go V.F. A systematic review of multi-level stigma interventions: state of the science and future directions. BMC Med. 2019;17(1):41. doi: 10.1186/s12916-018-1244-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cook J.E., Purdie-Vaughns V., Meyer I.H., Busch J.T.A. Intervening within and across levels: a multilevel approach to stigma and public health. Soc Sci Med. 2014;103:101–109. doi: 10.1016/j.socscimed.2013.09.023. [DOI] [PubMed] [Google Scholar]
- 18.Kemp C.G., Jarrett B.A., Kwon C.S., et al. Implementation science and stigma reduction interventions in low- and middle-income countries: a systematic review. BMC Med. 2019;17(1):6. doi: 10.1186/s12916-018-1237-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hartog K., Hubbard C.D., Krouwer A.F., Thornicroft G., Kohrt B.A., Jordans M.J.D. Stigma reduction interventions for children and adolescents in low- and middle-income countries: systematic review of intervention strategies. Soc Sci Med. 2020;246 doi: 10.1016/j.socscimed.2019.112749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thornicroft G., Sunkel C., Alikhon Aliev A., et al. The lancet commission on ending stigma and discrimination in mental health. Lancet. 2022;400(10361):1438–1480. doi: 10.1016/S0140-6736(22)01470-2. [DOI] [PubMed] [Google Scholar]
- 21.Hopewell S., McDonald S., Clarke M., Egger M. Grey literature in meta-analyses of randomized trials of health care interventions. Cochrane Database Syst Rev. 2007;2 doi: 10.1002/14651858.MR000010.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McAuley L., Pham B., Tugwell P., Moher D. Does the inclusion of grey literature influence estimates of intervention effectiveness reported in meta-analyses? Lancet. 2000;356(9237):1228–1231. doi: 10.1016/S0140-6736(00)02786-0. [DOI] [PubMed] [Google Scholar]
- 23.Phelan J.C., Link B.G., Dovidio J.F. Stigma and prejudice: one animal or two? Soc Sci Med. 2008;67(3):358–367. doi: 10.1016/j.socscimed.2008.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372 doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kassam A., Rose D., Sartorius N., Thornicroft G. Stigma: ignorance, prejudice or discrimination? Br J Psychiatry. 2007;190(3):192–193. doi: 10.1192/bjp.bp.106.025791. [DOI] [PubMed] [Google Scholar]
- 26.Thornicroft G., Mehta N., Clement S., et al. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet. 2016;387(10023):1123–1132. doi: 10.1016/S0140-6736(15)00298-6. [DOI] [PubMed] [Google Scholar]
- 27.Evans-Lacko S., Henderson C., Thornicroft G. Public knowledge, attitudes and behaviour regarding people with mental illness in England 2009-2012. Br J Psychiatry Suppl. 2013;55:s51–s57. doi: 10.1192/bjp.bp.112.112979. [DOI] [PubMed] [Google Scholar]
- 28.The EndNote Team . Clarivate; Philadelphia, PA: 2013. Endnote. Endnote 20 ed. [Google Scholar]
- 29.Covidence systematic review software. www.covidence.org
- 30.Oliver S., Harden A., Rees R., et al. An emerging framework for including different types of evidence in systematic reviews for public policy. Evaluation. 2005;11(4):428–446. [Google Scholar]
- 31.Evans-Polce R.J., Castaldelli-Maia J.M., Schomerus G., Evans-Lacko S.E. The downside of tobacco control? Smoking and self-stigma: a systematic review. Soc Sci Med. 2015;145:26–34. doi: 10.1016/j.socscimed.2015.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paez A. Gray literature: an important resource in systematic reviews. J Evid Based Med. 2017;10(3):233–240. doi: 10.1111/jebm.12266. [DOI] [PubMed] [Google Scholar]
- 33.Mahood Q., Van Eerd D., Irvin E. Searching for grey literature for systematic reviews: challenges and benefits. Res Synth Methods. 2014;5(3):221–234. doi: 10.1002/jrsm.1106. [DOI] [PubMed] [Google Scholar]
- 34.McKenzie J.E., Brennan S.E. Cochrane handbook for systematic reviews of interventions. 2019. Synthesizing and presenting findings using other methods; pp. 321–347. [Google Scholar]
- 35.Campbell M., McKenzie J.E., Sowden A., et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368 doi: 10.1136/bmj.l6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pettigrew T.F., Tropp L.R. A meta-analytic test of intergroup contact theory. J Pers Soc Psychol. 2006;90(5):751–783. doi: 10.1037/0022-3514.90.5.751. [DOI] [PubMed] [Google Scholar]
- 37.Pettigrew T.F., Tropp L.R., Wagner U., Christ O. Recent advances in intergroup contact theory. Int J Intercult Relat. 2011;35(3):271–280. [Google Scholar]
- 38.Iemmi V. Philanthropy for global mental health 2000–2015. Global Mental Health. 2020;7:e9. doi: 10.1017/gmh.2020.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Iemmi V. Global collective action in mental health financing: allocation of development assistance for mental health in 142 countries, 2000–2015. Soc Sci Med. 2021;287 doi: 10.1016/j.socscimed.2021.114354. [DOI] [PubMed] [Google Scholar]
- 40.Aplasca M.R.A., Siegel D., Mandel J.S., et al. Results of a model AIDS prevention program for high school students in the Philippines. AIDS. 1995;9(Suppl 1):S7–S13. [PubMed] [Google Scholar]
- 41.Groce N.E., Banks L.M., Stein M.A. Surviving polio in a post-polio world. Soc Sci Med. 2014;107:171–178. doi: 10.1016/j.socscimed.2014.02.024. [DOI] [PubMed] [Google Scholar]
- 42.Vikash R.K., Juriasinghani K., Yang D., Hashmi S. Poliomyelitis (polio) vaccination and associated stigma in Pakistan. Int J Vaccines Vaccin. 2016;2(2) [Google Scholar]
- 43.Allport G.W. Addison-Wesley; Oxford, England: 1954. The nature of prejudice; pp. xviii, 537–xviii. [Google Scholar]
- 44.Bandura A. Social foundations of thought and action: a social cognitive theory. Prentice-Hall, Inc; 1986. Social foundations of thought and action: a social cognitive theory; pp. xiii, 617–xiii. [Google Scholar]
- 45.Hegarty P., Golden A.M. Attributional beliefs about the controllability of stigmatized traits: antecedents or justifications of Prejudice?1. J Appl Soc Psychol. 2008;38(4):1023–1044. [Google Scholar]
- 46.Cuddy A.J.C., Fiske S.T., Kwan V.S.Y., et al. Stereotype content model across cultures: towards universal similarities and some differences. Br J Soc Psychol. 2009;48(1):1–33. doi: 10.1348/014466608X314935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tajfel H. Social identity and intergroup behaviour. Soc Sci Inf. 1974;13(2):65–93. [Google Scholar]
- 48.Corrigan P.W., Rao D. On the self-stigma of mental illness: stages, disclosure, and strategies for change. Can J Psychiatry. 2012;57(8):464–469. doi: 10.1177/070674371205700804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Thornicroft G., Brohan E., Kassam A., Lewis-Holmes E. Reducing stigma and discrimination: candidate interventions. Int J Ment Health Syst. 2008;2(1):3. doi: 10.1186/1752-4458-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kakuma R., Minas H., van Ginneken N., et al. Human resources for mental health care: current situation and strategies for action. Lancet. 2011;378:1654–1663. doi: 10.1016/S0140-6736(11)61093-3. [DOI] [PubMed] [Google Scholar]
- 51.van Deurzen I., Van Oorschot W., van Ingen E. The link between inequality and population health in low and middle income countries: policy myth or social reality? PLoS One. 2014;9(12) doi: 10.1371/journal.pone.0115109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Covidence.org Covidence explains the difference between systematic review & meta-analysis. https://www.covidence.org/blog/the-difference-between-a-systematic-review-and-a-meta-analysis/ Available from:
- 53.Olufadewa I., Adesina M., Ayorinde T. Global health in low-income and middle-income countries: a framework for action. Lancet Global Health. 2021;9(7):e899–e900. doi: 10.1016/S2214-109X(21)00143-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kirkham J.J., Davis K., Altman D.G., et al. Core outcome set-STAndards for development: the COS-STAD recommendations. PLoS Med. 2017;14(11) doi: 10.1371/journal.pmed.1002447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kohn R., Saxena S., Levav I., Saraceno B. The treatment gap in mental health care. Bull World Health Organ. 2004;82(11):858–866. [PMC free article] [PubMed] [Google Scholar]
- 56.Saxena S., Thornicroft G., Knapp M., Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007;370(9590):878–889. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.