Abstract
Audience
The targeted audience for this simulation is Emergency Medicine (EM) residents. Medical students, advanced practice providers, and staff physicians could all also find educational merit in this scenario.
Background
Cardiovascular disease is the leading cause of death in the United States according to the CDC.1 Coronary artery disease caused 375,000 deaths 2021 alone, and about 5% of all adult patients have a prior history of coronary artery disease.2 Furthermore, chest pain itself is a common chief complaint encountered in the ED, with nearly 8 million visits annually occurring throughout the United States, with 10–20% of those patients ultimately being diagnosed with an acute coronary syndrome3, including ST-elevation myocardial infarction (STEMI). Given this, it is essential that EM residents are well prepared to care for all patients presenting with chest pain, regardless of the acute care or emergency setting.
Throughout their training, most EM residents typically learn and evaluate patients at a large tertiary or quaternary medical center with 24-hour catheterization laboratory availability. For patients presenting with electrocardiogram (EKG) findings consistent with STEMI, the standard of care is for the patient to undergo cardiac catheterization and stent placement within 90 minutes of arrival. Unfortunately, only half of patients living in rural areas have a cardiac catheterization-capable facility available to them within a 60-minute driving radius, making it difficult for those patients to undergo cardiac catheterization within the desired time frame.4 These patients remain candidates for thrombolytic therapy, but given infrequent opportunities to learn about and deploy thrombolytic agents during residency training, graduating EM residents may be unfamiliar with indications, dosing, and contraindications before they begin practice. Furthermore, the recent EM workforce data suggests that although there may be an oversupply of 8,000 emergency physicians by 2030, robust practice opportunities for emergency physicians remain in rural settings.5 Although historically EM graduates have not selected rural areas for practice, with only approximately 8% of emergency physicians practicing in rural areas,6 it is likely that given the opportunities present and perceived saturation in many non-rural settings, more EM graduates will pursue practice in a rural setting. With these changing practice dynamics in mind, this simulation provides the opportunity for residents and medical students to experience the management of a STEMI in the rural setting, with a focus upon the indications, contraindications, dosing, and disposition of a patient receiving thrombolytics.
Educational Objectives
By the end of this simulation, learners will be able to:
Diagnose ST elevation myocardial infarction accurately and initiate thrombolysis in the rural setting without timely access to cardiac catheterization.
Engage the simulated patient in a shared decision-making conversation, clearly outlying the benefits and risks of thrombolysis.
Identify the indications and contraindications for thrombolysis in ST elevation myocardial infarction.
Arrange for transfer to a tertiary care center following completion of thrombolysis.
Educational Methods
This scenario is a simulated encounter in a rural emergency department setting requiring the diagnosis of a STEMI, a discussion with the patient regarding the risks and benefits of thrombolysis prior to administration, administration of thrombolysis, and transfer of patient to a higher level of care.
Research Methods
The educational content of this simulation as a teaching instrument was evaluated by the learner utilizing an internally developed survey after case completion. This survey was reviewed for precision of language and assessment of learning objectives by our simulation faculty and other members of our West Virginia University Emergency Medicine Department of Medical Education. The learner was asked to specify any prior experience with rural STEMI management as well as quantify via a five-point Likert Scale, where 1 = very uncomfortable and 5 = very comfortable, their level of comfort with thrombolysis before and after the scenario as well as their comfort with having a shared decision-making conversation with patients with regards to thrombolysis. Learners were also asked to rank the helpfulness of this simulation in preparing them for administering thrombolytics for STEMI in a rural setting on a five-point Likert scale, where 1 = not helpful and 5 =very helpful. An open response section was also provided to allow learners the opportunity to comment directly on any aspect of the simulation.
Results
Data was collected anonymously from 16 PGY1-3 resident learners via surveys with a 100% response rate. Overall, the feedback received regarding the simulation was positive. There was a low average comfort level with administering thrombolytics and having a shared decision-making conversation regarding administering thrombolytics. There was a high average rating of the helpfulness of this simulation in preparing residents for this conversation as well as managing STEMIs in a rural setting. Subjective comments regarding the simulation were universally positive.
Discussion
The management of STEMI in the rural emergency department differs significantly from the environment in which many EM residents train. As a leading cause of death in the United States, STEMI management is a vital component of EM resident education. Although the concept of thrombolysis in the rural setting is discussed, the opportunity for real-world experience in its execution is often limited despite many graduates ultimately working in rural emergency departments. This simulation sought to provide a realistic patient encounter to promote familiarity and comfort in the identification, patient discussion and execution of thrombolysis in the treatment of a STEMI. The educational content was shown to be effective via learner survey completion.
USER GUIDE
| List of Resources: | |
|---|---|
| Abstract | 55 |
| User Guide | 58 |
| Instructor Materials | 59 |
| Operator Materials | 68 |
| Debriefing and Evaluation Pearls | 70 |
| Simulation Assessment | 72 |
Learner Audience:
Medical Students, Interns, Junior Residents, Senior Residents, APPs and Clinical Faculty
Time Required for Implementation:
Instructor Preparation: Instructors will typically require 20–30 minutes to familiarize themselves with the case, including critical actions and debriefing objectives
Time for case: 10–15 minutes
Time for debriefing: 10–20 minutes
Recommended Number of Learners per Instructor:
3–4
Topics:
Thrombolysis, ST-elevation myocardial infarction, STEMI, myocardial infarction, MI, rural, heart attack, simulation.
Objectives:
By the end of this simulation, learners will be able to:
Diagnose ST elevation myocardial infarction accurately and initiate thrombolysis in the rural setting without timely access to cardiac catheterization.
Engage the simulated patient in a shared decision-making conversation, clearly outlying the benefits and risks of thrombolysis.
Identify the indications and contraindications for thrombolysis in ST elevation myocardial infarction.
Arrange for transfer to a tertiary care center after administration of thrombolytics.
Linked objectives and methods
This format allows the learner to quantify their comfortability with rural STEMI management as a direct consequence of this simulation. The goal of this case is for the learners to immerse themselves in the experience and respond as they would in this important and increasingly common clinical scenario. The case requires the learner to first identify a STEMI in a patient presenting with chest pain and then recognize the treatment limitations of their rural setting before determining the appropriate treatment option of thrombolysis (Objective 1). Once acknowledged as clinically indicated, the learner must then discuss the associated risks and benefits of thrombolysis with the patient while exploring for any contraindications (Objective 2 and 3). Finally, the learner must organize and execute the timely disposition of the patient to the appropriate level of care (Objective 4). This will require simulated contact and consultation with a cardiologist at a facility equipped for urgent percutaneous interventions. By simulation completion, the learner will have navigated all aspects of the clinical scenario from identification to disposition, gaining confidence and experience managing an important patient population.
Learner responsible content (optional)
No pre-session content is required. Our preferred method of implementation is during our regularly scheduled monthly simulation sessions, during which the learners are blinded to the scenario they will be exposed to. This blinding simulates the real-world uncertainty of patient encounters.
Recommended pre-reading for instructor
Instructors should familiarize themselves with the American College of Cardiology/American Heart Association STEMI guidelines.7
Results and tips for successful implementation
This simulation is successfully implemented when the learners approach the case as a real-world encounter and are asked to articulate their thought process as they move through critical actions. The educator should allow the learner to make mistakes and redirect as needed by real-time patient decompensation and subtle hints. The learner should be tasked to assume the role of an isolated attending physician, as is often the case in the rural setting. Learners can be additionally challenged enhanced by realistic variables proposed by the educator such as inclement weather affecting air transport, post-lytic induced dysrhythmias, or persistent hypotension from inferior MI.
This simulation was presented to EM resident physicians of all levels in a 3-year program with 30 residents as part of a standard monthly simulation curriculum. An anonymous electronic survey was distributed after the simulation for learner feedback. Data was collected anonymously from 16 PGY1-3 resident learners via surveys with a 100% response rate. Overall, the feedback received regarding the simulation was positive. Interestingly, only 1 in 16 (6%) of surveyed residents had ever administered thrombolytics for STEMI in the clinical setting. On a 1–5 Likert scale where 1 = very uncomfortable and 5 = very comfortable, learners reported low comfort levels with administering thrombolytics to treat STEMIs prior to completing the simulation, with an average of 2.4 and a standard deviation of 0.9. Comfortability with shared decision making regarding thrombolytic administration was evaluated with the same Likert scale, and learner comfort was higher with thrombolytic administration, with an average of 3.3 and a standard deviation of 1.2. Learners were asked to rank the helpfulness of this simulation in preparing them for administering thrombolytics for STEMI in a rural setting on a Likert scale where 1 = not helpful and 5 =very helpful. Overall, learners found the simulation very helpful with an average score of 4.6 with a standard deviation of 0.7. Finally, with regards to how the simulation helped residents feel comfortable with having a shared decision-making conversation centered on thrombolytic administration, residents felt that the simulated scenario was very helpful overall with a post-simulation score of 4.6 with a standard deviation of 0.6. Comments in the open response section were universally positive. Below are some sampled comments from learners:
“This was an excellent simulation. We are often involved in care of stroke patients who receive TPA, but I have never been the one to have the informed consent conversation with families or patients. Therefore, I did not feel comfortable with the correct way to have the conversation and the correct risk and benefit information to provide to them. Great work!”
“Very helpful to have community setting/low resource simulation."
“I thought this SIM was good in that 1. It made you need to filter out extraneous information. 2. It made you “pull the trigger” on ordering thrombolytics to a patient. 3. We reviewed shared decision-making discussions/importance!”
Supplementary Information
INSTRUCTOR MATERIALS
Case Title: Managing STEMIs without a Catheterization Lab: A Simulated Scenario to Improve Emergency Clinician Recognition and Execution of Thrombolysis in the Setting of Rural STEMI Management
Case Description & Diagnosis (short synopsis): This is a simulated clinical scenario. An emergency medicine physician working in a rural setting is presented with a middle-aged man with no known cardiac history presenting with chest pain. The learner is first challenged to correctly identify the patient as having an acute STEMI. The learner must then assess the capabilities of their institution before correctly articulating thrombolysis as the indicated treatment prior to transport. A detailed risks/benefits discussion must then be had with the patient before initiating treatment. Failure to identify the STEMI or lack of timely initiation of thrombolysis will result in acute decompensation of the patient. The learner will have successfully completed the scenario when the patient’s clinical status has improved, and the patient is appropriately designated for transportation to higher level of care and cardiac catheterization. Post-case debriefing should highlight the objectives of the case and allow the learner to ask questions while the teaching points of the case are discussed.
Equipment or Props Needed:
High fidelity manikin capable of voice and vital sign findings to represent the STEMI patient. Ready-made printouts of lab findings, x-rays, and vital sign changes in response to delay of treatment enhances the simulation. A standardized patient could also be implemented.
Actors Needed:
A confederate playing the role of the nurse will be needed to facilitate interactions and help advance the case. A confederate will also be needed to voice the manikin and input vital sign changes as necessary into the manikin software. The case could be deployed utilizing a standardized patient in lieu of a manikin, in which case a confederate would be needed to play the role of the STEMI patient.
Stimulus Inventory:
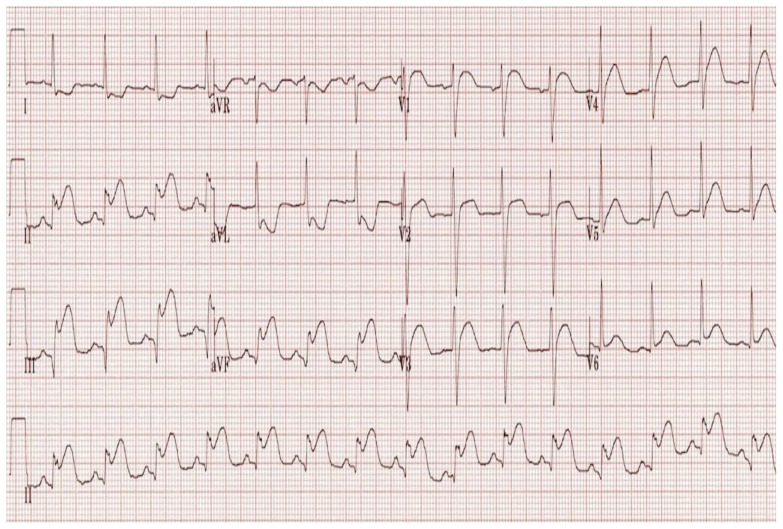
| #1 | Electrocardiogram (ECG) |
| #2 | Complete blood count (CBC) |
| #3 | Basic metabolic panel (BMP) |
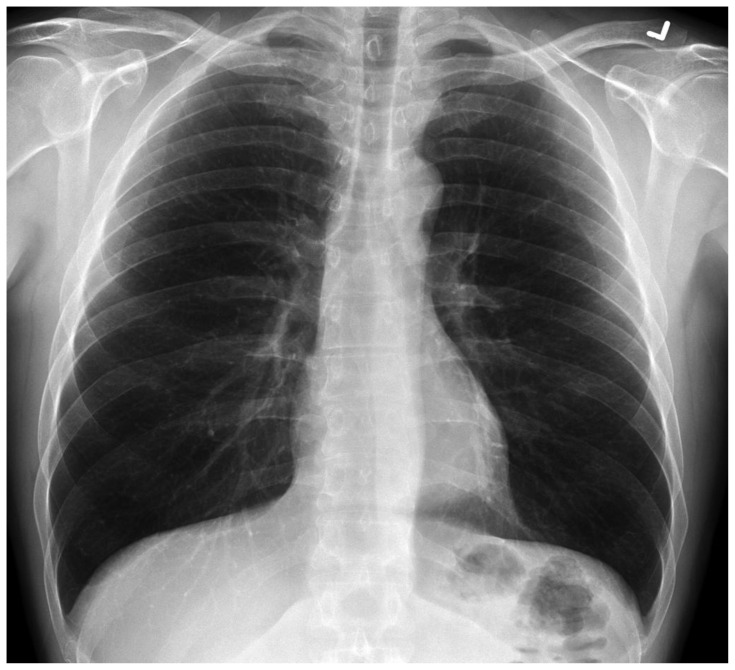
| #4 | Chest radiograph (CXR) |
| #5 | Troponin |
Background and brief information: The learner is asked to assume the role of an attending physician in a resource-limited, rural ED where a middle-aged man presents with chest pain and electrocardiographic evidence of a STEMI. If the STEMI is not recognized and thrombolysis is not initiated in a timely manner, the patient will decompensate and require emergent intervention.
Initial presentation: Nursing introduces the patient and the history of present illness (HPI) is presented by the patient. The patient is a 58-year-old man complaining of a three-day history of intermittent chest pain which acutely worsened today while eating and has been constant for the past three hours. The discomfort is described as “an elephant sitting on my chest” and associated with dyspnea and nausea. Of note, the patient indicates that he was in a low energy motor vehicle collision without airbag deployment one week ago and has been diffusely sore since that time but did not seek medical intervention. The patient indicates that he does not regularly visit a physician and is on no medications at the present time. He is a half pack per day smoker and does not drink or use illicit drugs. The patient will look uncomfortable upon exam, but there are no other pertinent exam findings.
How the scene unfolds: The learner should quickly diagnose the patient with an inferior STEMI via a promptly obtained EKG (stimulus 1). Lab work, if obtained, will demonstrate a significantly elevated troponin (stimulus 5). Chest x-ray will be unremarkable (stimulus 4). Failure to promptly recognize and treat the STEMI via indicated thrombolysis will result in patient decompensation with worsened chest discomfort, hypotension, worsening tachycardia and oxygen saturation. The learner(s) must have a shared decision-making conversation with the patient regarding thrombolysis during which the patient will express concerns regarding his recent motor vehicle collision. Shared decision making should result in the decision to pursue thrombolysis. Post lysis, the patient will express improving symptoms and vital signs will stabilize. The patient should then be arranged for transfer to a percutaneous coronary intervention (PCI) capable facility.
For more advanced learners, several additional complications could be added. Inclement weather could impede patient transport. The patient could suffer a post-lytic induced dysrhythmia, such as ventricular tachycardia, requiring additional actions like cardioversion. The patient could suffer from persistent hypotension from the inferior MI and require additional resuscitation.
Critical actions:
Identify the patient’s chest pain as being the result of an acute STEMI.
Assess the limited capability of their institution and articulate the indication for thrombolysis.
Have a shared decision-making conversation with the patient regarding the risks and benefits of treatment, resulting in lysis.
Ensure patient stabilization prior to transfer to the appropriate level of care.
Case Title: A Simulated Scenario to Improve Emergency Clinician Competence and Confidence in Rural STEMI Management
Chief Complaint: Chest pain
| Vitals: | Heart Rate (HR) 102 | Blood Pressure (BP) 150/75 |
| Respiratory Rate (RR) 15 | Temperature (T) 98.7°F | |
| Oxygen Saturation (O2Sat) 100% on room air | ||
General Appearance: Diaphoretic
Primary Survey:
Airway: Patent, clear voice
Breathing: Clear breath sounds bilateral, unlabored
Circulation: Intact central and peripheral pulses
History:
History of present illness: Patient reports a three-day history of intermittent chest pain. Today the symptoms acutely worsened while eating and have become severe and constant. Pain is described as an “elephant sitting on my chest.” Patient reports also feeling mild shortness of breath and nausea. Patient will describe being in a low mechanism motor vehicle collision approximately one week ago. Patient has been ambulatory since the incident and did not seek medical care. No loss of consciousness. No airbag deployment.
Past medical history: None – patient admits to “never going to the doctor”
Past surgical history: None
medications: None
Allergies: None
Social history: Smokes one half ppd “for decades.” No drinking or drug use
Family history: Father died of “some heart condition”
Secondary Survey/Physical Examination:
General Appearance: Diaphoretic
-
HEENT
○ Head: within normal limits
○ Eyes: within normal limits
○ Ears: within normal limits
○ Nose: within normal limits
○ Throat/oropharynx: within normal limits
Neck: within normal limits
Heart: within normal limits
Lungs: within normal limits
Abdominal/GI: within normal limits
Genitourinary: deferred/within normal limits
Rectal: deferred/within normal limits
Extremities: within normal limits
Neuro: within normal limits
Skin: diaphoretic
Lymph: within normal limits
Psych: within normal limits
Electrocardiogram
Buttner R, Burns E. Inferior STEMI Example #3. In: Life in the Fast Lane.
https://litfl.com/inferior-stemi-ecg-library/. Published March 21, 2023. Accessed March 15, 2024. CC BY-NC-SA 4.0 DEED
| Complete blood count (CBC) | |
| White blood count (WBC) | 16.0 × 1000/mm3 |
| Hemoglobin (Hgb) | 14.1 g/dL |
| Hematocrit (HCT) | 41% |
| Platelet (Plt) | 450 × 1000/mm3 |
| Basic metabolic panel (BMP) | |
| Sodium | 134 mEq/L |
| Potassium | 3.4 mEq/L |
| Chloride | 105 mEq/L |
| Bicarbonate (HCO3) | 18 mEq/L |
| Blood Urea Nitrogen (BUN) | 5 mg/dL |
| Creatinine (Cr) | 0.8 mg/dL |
| Troponin | 124,071 ng/L |
| Coagulation Studies | |
| Partial thromboplastin time | 29 seconds |
| International normalized ratio | 1.2 |
Chest X-ray
Gaillard F. Normal Chest X-ray. In: Radiopaedia.
https://radiopaedia.org/cases/normal-chest-x-ray. Accessed March 15, 2024. CC BY-NC-SA 3.0 DEED
OPERATOR MATERIALS
| Minute (state) | Participant action/ trigger | Patient status (simulator response) & operator prompts | Monitor display (vital signs) |
|---|---|---|---|
| 0:00 (Baseline) | Learner performs primary survey, obtains HPI, performs secondary survey. | Patient is diaphoretic and clutching his chest. | T 98.7° F HR 102 BP 150/75 RR 15 O2 100% |
| 3:00 | Learner orders labs and requests ECG. | If labs and ECG not ordered, patient will complain of worsened pain and nurse will prompt the learner. | T 98.7° F HR 115 BP 160/85 RR 17 O2 100% |
| 4:00 | ECG, labs and CXR available. Learner reads ECG. |
Patient continues to complain of chest pain, but condition the same. If STEMI is recognized, proceed to 5:00A. If STEMI is not recognized, advance to 5:00B. |
T 98.7° F HR 117 BP 166/87 RR 21 O2 100% |
| 5:00A | Learner recognizes STEMI and recognizes lack of prompt availability of cath lab. | If learner simply orders lytics without a discussion, the patient prompts them by mentioning their recent MVC. The concerned nurse can prompt further shared decision making and review of the indications and contraindications prior to administration. If learner does not order lysis and simply tries to transfer the patient or other therapies, advance to 10:00B. |
T 98.7° F HR 117 BP 166/87 RR 21 O2 100% |
| 5:00B | Learner fails to identify STEMI or indication for lysis. | Chest pain worsens. Patient has runs of ventricular tachycardia, and nurse asks learner what was on the ECG. If learner recognizes STEMI, proceed to 5:00A. If learner continues to fail to recognize STEMI, continue to prompt but then eventually proceed to 10:00B. |
T 98.7° F HR 130 BP 85/30 RR 25 O2 87% |
| ~10:00A | Learner orders lysis. | Patient reports improvement of symptoms. | T 98.7° F HR 90 BP 130/80 RR 15 O2 100% |
| ~10:00B | Learner fails to order lysis or has yet to recognize STEMI even with prompting. | Patient will have persistent ventricular tachycardia and eventually suffer a cardiac arrest that will not be reversible until learner recognizes the need for thrombolytic therapy. | T 98.7° F HR 217 BP 67/palp RR 32 O2 82% |
| ~12:00 | Learner requests admission or transportation to a higher level of care. | If learner tries to admit patient without transfer for heart catheterization, prompt from local admitting physician or nurse to transfer. | T 98.7° F HR 90 BP 130/80 RR 15 O2 100% |
| Case Completion: ~15:00 | Alternatively: Additional complications for advanced learners. | Consider post-lytic rhythm change, inclement weather barring transport, or persistent hypotension. | T 98.7° F HR 90 BP 130/80 RR 15 O2 100% |
Diagnosis:
Interior wall STEMI
Disposition:
Transportation to a cath lab equipped facility
DEBRIEFING AND EVALUATION PEARLS
Rural STEMI Management
Thrombolysis of STEMI patients is an important tool of the emergency clinician. As emergency physicians may be faced with a need to choose increasingly rural practice sites,6 they will need to confidently administer thrombolysis to appropriate STEMI patients.7 Upon completion of this scenario, the learner should be more familiar and comfortable in the indication, discussion, execution, and disposition of the rural STEMI patient requiring lysis. Learners should finish the case and the debriefing with confidence in discussing the mortality benefits of lytic therapy in treating STEMI7 against the low (0.5–1% risk of intracranial hemorrhage) risks associated with lytic administration in the absence of contraindication.8 Absolute contraindications to thrombolytic treatment are9:
Recent intracranial hemorrhage
Known cerebrovascular lesion, like arteriovenous malformation (AVM), or known intracranial mass
Ischemic stroke within three months
Possible aortic dissection
Active bleeding
Significant head injury or facial trauma within three months
Recent intracranial or spinal surgery
Severe uncontrolled hypertension.
Other debriefing points: If the learners failed to identify the STEMI in a timely manner, spend some time exploring the frame that led them to view the ECG incorrectly. Ensure adequate discussion of the indications and contraindications to thrombolysis, with specific focus upon how the low mechanism MVC several days prior to does not represent a contraindication to thrombolysis. For more junior learners, the case can be used to facilitate a discussion regarding the frameworks underlying the evaluation of undifferentiated chest pain patients in the ED. Explain the appropriate workup of all chest pain patients and the need for timely ECG interpretation. If the learner allows the patient’s concerns of the low mechanism MVC multiple days ago to interfere with indicated thrombolysis of an acute STEMI, explore barriers the learner may have when executing an appropriate risks/benefits discussion. This discussion should center on the demonstrated mortality benefit of thrombolytics in combination with PCI in patients with acute MI remote from a PCI capable center.8 The learner should have ready recall of the 0.5–1% risk of intracranial hemorrhage as the primary risk in this shared decision-making conversation.8 If the learner has progressed well through the simulation, the educator can provide real-time additional challenges to the learner such as inclement weather affecting transportation, reperfusion dysrhythmias, or hemodynamic instability from inferior MI.
SIMULATION ASSESSMENT
A Simulated Scenario to Improve Emergency Clinician Competence and Confidence in Rural STEMI Management
Learner: _________________________________________
Assessment Timeline
This timeline is to help observers assess their learners. It allows observer to make notes on when learners performed various tasks, which can help guide debriefing discussion.
Critical Actions:
|
0:00 |
Critical Actions:
□ Identify the patient’s chest pain as being the result of an acute STEMI.
□ Assess the limited capability of their institution and articulate the indication for thrombolysis.
□ Have a shared decision-making conversation with the patient regarding the risks and benefits of treatment, resulting in lysis.
□ Ensure patient stabilization prior to transfer to the appropriate level of care.
Summative and formative comments:
Milestones assessment:
| Milestone | Did not achieve level 1 | Level 1 | Level 2 | Level 3 | |
|---|---|---|---|---|---|
| 1 | Emergency Stabilization (PC1) | □ Did not achieve Level 1 |
□ Recognizes abnormal vital signs |
□ Recognizes an unstable patient, requiring intervention Performs primary assessment Discerns data to formulate a diagnostic impression/plan |
□ Manages and prioritizes critical actions in a critically ill patient Reassesses after implementing a stabilizing intervention |
| 2 | Performance of focused history and physical (PC2) | □ Did not achieve Level 1 |
□ Performs a reliable, comprehensive history and physical exam |
□ Performs and communicates a focused history and physical exam based on chief complaint and urgent issues |
□ Prioritizes essential components of history and physical exam given dynamic circumstances |
| 3 | Diagnostic studies (PC3) | □ Did not achieve Level 1 |
□ Determines the necessity of diagnostic studies |
□ Orders appropriate diagnostic studies. Performs appropriate bedside diagnostic studies/procedures |
□ Prioritizes essential testing Interprets results of diagnostic studies Reviews risks, benefits, contraindications, and alternatives to a diagnostic study or procedure |
| 4 | Diagnosis (PC4) | □ Did not achieve Level 1 |
□ Considers a list of potential diagnoses |
□ Considers an appropriate list of potential diagnosis May or may not make correct diagnosis |
□ Makes the appropriate diagnosis Considers other potential diagnoses, avoiding premature closure |
| 5 | Pharmacotherapy (PC5) | □ Did not achieve Level 1 |
□ Asks patient for drug allergies |
□ Selects an medication for therapeutic intervention, consider potential adverse effects |
□ Selects the most appropriate medication and understands mechanism of action, effect, and potential side effects Considers and recognizes drug-drug interactions |
| 6 | Observation and reassessment (PC6) | □ Did not achieve Level 1 |
□ Reevaluates patient at least one time during case |
□ Reevaluates patient after most therapeutic interventions |
□ Consistently evaluates the effectiveness of therapies at appropriate intervals |
| 7 | Disposition (PC7) | □ Did not achieve Level 1 |
□ Appropriately selects whether to admit or discharge the patient |
□ Appropriately selects whether to admit or discharge Involves the expertise of some of the appropriate specialists |
□ Educates the patient appropriately about their disposition Assigns patient to an appropriate level of care (ICU/Tele/Floor) Involves expertise of all appropriate specialists |
| 9 | General Approach to Procedures (PC9) | □ Did not achieve Level 1 |
□ Identifies pertinent anatomy and physiology for a procedure Uses appropriate Universal Precautions |
□ Obtains informed consent Knows indications, contraindications, anatomic landmarks, equipment, anesthetic and procedural technique, and potential complications for common ED procedures |
□ Determines a back-up strategy if initial attempts are unsuccessful Correctly interprets results of diagnostic procedure |
| 20 | Professional Values (PROF1) | □ Did not achieve Level 1 |
□ Demonstrates caring, honest behavior |
□ Exhibits compassion, respect, sensitivity and responsiveness |
□ Develops alternative care plans when patients’ personal beliefs and decisions preclude standard care |
| 22 | Patient centered communication (ICS1) | □ Did not achieve level 1 |
□ Establishes rapport and demonstrates empathy to patient (and family) Listens effectively |
□ Elicits patient’s reason for seeking health care |
□ Manages patient expectations in a manner that minimizes potential for stress, conflict, and misunderstanding. Effectively communicates with vulnerable populations, (at risk patients and families) |
| 23 | Team management (ICS2) | □ Did not achieve level 1 |
□ Recognizes other members of the patient care team during case (nurse, techs) |
□ Communicates pertinent information to other healthcare colleagues |
□ Communicates a clear, succinct, and appropriate handoff with specialists and other colleagues Communicates effectively with ancillary staff |
References/Suggestions for further reading
- 1.Current multiple cause of death data on CDC Wonder. Centers for Disease Control and Prevention; At https://wonder.cdc.gov/mcd.html. [Google Scholar]
- 2.Tsao CW, Aday AW, Almarzooq ZI, et al. Heart Disease and Stroke Statistics—2023 Update: A Report From the American Heart Association. Circulation. 2023;147:e93– e621. doi: 10.1161/CIR.0000000000001123. [DOI] [PubMed] [Google Scholar]
- 3.Chang AM, Fischman DL, Hollander JE. Evaluation of chest pain and acute coronary syndrome. Cardiology Clin. 2018;36:1–12. doi: 10.1016/j.ccl.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 4.Nallamothu BK, Bates ER, Wang Y. Driving times and distances to hospitals with percutaneous coronary intervention in the United States: implications for prehospital triage of patients with ST-elevation myocardial infarction. Circulation. 2006;113:1189–1195. doi: 10.1161/CIRCULATIONAHA.105.596346. [DOI] [PubMed] [Google Scholar]
- 5.Bennett CL, Clay CE, Espinola JA, et al. United States 2020 emergency medicine resident workforce analysis. Ann Emerg Med. 2022;80:3–11. doi: 10.1016/j.annemergmed.2022.03.007. [DOI] [PubMed] [Google Scholar]
- 6.Marco CA, Courtney DM, Ling LL, et al. The emergency medicine physician workforce: projections for 2030. Ann Emerg Med. 2021;78:726–737. doi: 10.1016/j.annemergmed.2021.05.029. [DOI] [PubMed] [Google Scholar]
- 7.Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145:e18– e114. doi: 10.1161/CIR.0000000000001038. Originally published 9 Dec 2021. At: [DOI] [PubMed] [Google Scholar]
- 8.Tintinalli JE, Ma O, Yealy DM, editors. Tintinalli's Emergency Medicine: A Comprehensive Study Guide. 9ed. McGraw-Hill Education; 2020. [Google Scholar]
- 9.Baig MU, Bodle J. StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2024. Jan, Thrombolytic therapy. Updated 2023 Aug 28. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557411/ [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.