Abstract
The impact of air pollution and climate change on mental health has recently raised strong concerns. However, a comprehensive overview analyzing the existing evidence while addressing relevant biases is lacking. This umbrella review systematically searched the PubMed/Medline, Scopus and PsycINFO databases (up to June 26, 2023) for any systematic review with meta‐analysis investigating the association of air pollution or climate change with mental health outcomes. We used the R metaumbrella package to calculate and stratify the credibility of the evidence according to criteria (i.e., convincing, highly suggestive, suggestive, or weak) that address several biases, complemented by sensitivity analyses. We included 32 systematic reviews with meta‐analysis that examined 284 individual studies and 237 associations of exposures to air pollution or climate change hazards and mental health outcomes. Most associations (n=195, 82.3%) involved air pollution, while the rest (n=42, 17.7%) regarded climate change hazards (mostly focusing on temperature: n=35, 14.8%). Mental health outcomes in most associations (n=185, 78.1%) involved mental disorders, followed by suicidal behavior (n=29, 12.4%), access to mental health care services (n=9, 3.7%), mental disorders‐related symptomatology (n=8, 3.3%), and multiple categories together (n=6, 2.5%). Twelve associations (5.0%) achieved convincing (class I) or highly suggestive (class II) evidence. Regarding exposures to air pollution, there was convincing (class I) evidence for the association between long‐term exposure to solvents and a higher incidence of dementia or cognitive impairment (odds ratio, OR=1.139), and highly suggestive (class II) evidence for the association between long‐term exposure to some pollutants and higher risk for cognitive disorders (higher incidence of dementia with high vs. low levels of carbon monoxide, CO: OR=1.587; higher incidence of vascular dementia per 1 μg/m3 increase of nitrogen oxides, NOx: hazard ratio, HR=1.004). There was also highly suggestive (class II) evidence for the association between exposure to airborne particulate matter with diameter ≤10 μm (PM10) during the second trimester of pregnancy and the incidence of post‐partum depression (OR=1.023 per 1 μg/m3 increase); and for the association between short‐term exposure to sulfur dioxide (SO2) and schizophrenia relapse (risk ratio, RR=1.005 and 1.004 per 1 μg/m3 increase, respectively 5 and 7 days after exposure). Regarding climate change hazards, there was highly suggestive (class II) evidence for the association between short‐term exposure to increased temperature and suicide‐ or mental disorders‐related mortality (RR=1.024), suicidal behavior (RR=1.012), and hospital access (i.e., hospitalization or emergency department visits) due to suicidal behavior or mental disorders (RR=1.011) or mental disorders only (RR=1.009) (RR values per 1°C increase). There was also highly suggestive (class II) evidence for the association between short‐term exposure to increased apparent temperature (i.e., the temperature equivalent perceived by humans) and suicidal behavior (RR=1.01 per 1°C increase). Finally, there was highly suggestive (class II) evidence for the association between the temporal proximity of cyclone exposure and severity of symptoms of post‐traumatic stress disorder (r=0.275). Although most of the above associations were small in magnitude, they extend to the entire world population, and are therefore likely to have a substantial impact. This umbrella review classifies and quantifies for the first time the global negative impacts that air pollution and climate change can exert on mental health, identifying evidence‐based targets that can inform future research and population health actions.
Keywords: Air pollution, climate change, mental health, temperature, dementia, cognitive disorders, post‐partum depression, suicide, schizophrenia, post‐traumatic stress disorder
Air pollution, increasing temperatures, and extreme changes in weather patterns represent intertwined elements of a severe global crisis destined to worsen without a fast and radical action 1 , 2 . They pose a significant physical health threat, leading to an increased risk and/or exacerbation of a variety of diseases, including infectious, allergic, metabolic, neoplastic, respiratory and cardiovascular ones 3 .
They also impact mental health, although this relationship has received attention only in more recent years 4 . For example, exposure to air pollution has been associated with a higher risk for cognitive disorders 5 , and temperature rise has been found to be related to an increased suicide risk 6 . Extreme weather events such as cyclones, floods or wildfires can foster traumatic experiences, leading to post‐traumatic stress disorder (PTSD) in exposed populations 7 .
While these environmental exposures can directly affect individuals' mental health, they also appear to exert indirect influences. For example, climate change can affect economic stability, food security, community well‐being and physical health, or accelerate migration and conflict, which are themselves key drivers of mental health 8 , 9 .
The direct and indirect impacts of environmental changes on mental health are so concerning, particularly for young generations, that new words have been coined: solastalgia (i.e., the distress caused by the transformation and degradation of one's home environment) 10 , ecological grief (i.e., grief concerning ecological loss) 11 , and eco‐anxiety (i.e., anxiety related to a changing and uncertain environment) 12 .
At a scientific level, the associations between these environmental exposures and mental health outcomes have been extensively addressed, leading to an exponential number of publications and, eventually, several systematic reviewse.g.,5,6,13. However, findings often conflict across primary studies. For example, one study 14 found a significant association between long‐term exposure to airborne particulate matter (PM) and the diagnosis of depression, while another study 15 did not detect this association using a much larger sample. Similarly, while short‐term exposure to an increasing temperature has been reported to elevate mortality related to suicide 16 , this association was not replicated in another study 17 . Similar inconsistencies are even present between different systematic reviews with meta‐analysis. For example, while a systematic review with meta‐analysis did not identify an overall association between exposure to PM ≤2.5 μm in diameter (PM2.5) and depression 18 , another one confirmed it13.
These contrasting findings may be partially due to different sample sizes 19 , small‐study effects, reporting biases, large heterogeneity, and inconsistent definition and measuring of relevant exposures. In this context, the existence, direction and magnitude of associations between these environmental exposures and mental health outcomes remain uncertain. The resulting unclear level of evidence and reliable targets hinder further research and prevent population health actions aimed to mitigate the impact of these exposures on mental health.
The present work aims to fill these gaps by providing a comprehensive umbrella review to systematically examine and classify the evidence associating air pollution and climate change with mental health outcomes globally. To this end, a standardization of units of measurement was performed, and the R metaumbrella package was used to calculate and stratify the credibility of the evidence according to criteria that address several biases.
The evidence‐based classification provided by this umbrella review is designed to support sound recommendations for the next generation of research and population‐level approaches addressing the impact of air pollution and climate change on mental health.
METHODS
We conducted the present umbrella review according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) 20 , and pre‐registered its protocol at https://osf.io/rgjdp/?view_only=d60ab9238c714014ae148acde5e55ad2.
Search strategy
We systematically searched the PubMed/Medline, Scopus and PsycINFO databases from inception to June 26, 2023. The search strategy included terms related to air pollution and climate change and to mental health outcomes (see supplementary information). We hand‐searched the references of each included review, textbooks, and other materials to identify potential additional systematic reviews with meta‐analysis not captured by the original search string.
Exposures and outcomes
Air pollution and climate change were pragmatically operation‐alized according to the definitions provided in each systematic review with meta‐analysis. They were referred to the general population, unless specifically mentioned (e.g., air pollution during pregnancy).
Mental health outcomes included: a) mental disorders grouped into ICD‐10 diagnostic blocks: organic mental disorders; mental and behavioral disorders due to psychoactive substance use; schizophrenia, schizotypal and delusional disorders; mood (affective) disorders; neurotic, stress‐related and somatoform disorders; behavioral syndromes associated with psychological disturbances and physical factors; disorders of adult personality and behavior; mental retardation; disorders of psychological development; and behavioral and emotional disorders with onset usually occurring in childhood and adolescence; b) mental disorders‐related symptomatology (e.g., symptoms or manifestations associated with a mental disorder, such as depressive or anxiety symptoms); c) suicidal behavior; d) access to mental health care services.
Inclusion and exclusion criteria
We considered eligible for inclusion any systematic review with meta‐analysis including observational studies (both cross‐sectional and longitudinal), that: a) investigated the association of either air pollution or climate change, or both, with any mental health outcome (as defined above); and b) compared exposed vs. non‐exposed populations, or populations at different levels of exposure. Each association had to be based on at least two individual studies to be eligible for inclusion.
We excluded: a) any publication other than systematic reviews with meta‐analysis, including systematic reviews without meta‐analysis, and meta‐analyses that did not follow a systematic search procedure; b) systematic reviews with meta‐analysis including only interventional studies; c) systematic reviews with meta‐analysis including only studies providing prevalence data in a single group; d) systematic reviews with meta‐analysis including only pre‐post studies; e) systematic reviews with meta‐analysis that were not related to our research question; f) grey literature (i.e., publications that did not undergo a peer review process, such as doctoral theses and conference abstracts); g) systematic reviews with meta‐analysis that were retracted after publication; h) systematic reviews with meta‐analysis reporting the same associations of other systematic reviews with meta‐analysis that were more comprehensive or recent; i) systematic reviews with meta‐analysis that did not provide sufficient data to conduct the umbrella review.
Selection of systematic reviews with meta‐analysis and data extraction
Three authors (MDP, VO, GF) independently assessed systematic reviews with meta‐analysis of potential interest at the title, abstract and full‐text levels. Any disagreement was resolved by consensus, and another author (JR, PFP) was consulted when an agreement could not be reached. The same three authors independently extracted information from the included reviews.
At a single systematic review with meta‐analysis level, we recorded the first author, publication year, number of included individual studies, type of exposure, type of mental health outcome, and type of effect size considered – i.e., odds ratio (OR), hazard ratio (HR), or risk ratio (RR). For time‐dependent exposures (i.e., long‐term and short‐term ones), we recorded the time frame considered for each specific association. Long‐term exposures were considered to be those lasting months or years, while short‐term exposures were those lasting days or weeks (generally less than 30 days).
At an individual study level, we recorded the first author, publication year, study design, any measure useful to calculate the effect size, and dependencies in the data (multiple outcomes from the same group, or multiple groups in a study).
Quality of evidence
We used A Measurement Tool To Assess Systematic Reviews (AMSTAR‐2) 21 to assess the quality of the included systematic reviews with meta‐analysis. We classified methodological quality as “high” (no critical weakness and no more than one non‐critical weakness); “moderate” (no critical weakness but more than one non‐critical weaknesses); “low” (one critical weakness); and “critically low” (more than one critical weaknesses) 21 .
Statistical analyses
During the early phase of data collection, we noticed that the included systematic reviews with meta‐analysis investigated the associations between air pollution or climate change exposures and mental health outcomes either continuously (e.g., suicide mortality increases per each 5°C increase in temperature) or binarily (e.g., differences in dementia incidence between individuals highly exposed and those not, or little, exposed to solvents). Systematic reviews with meta‐analysis investigating continuous associations were heterogeneous with regards to the exposure intervals used to report the results. To overcome this problem, we converted all intervals to one unit in the International System of Units (e.g., change per 1°C increase or change per 1 μg/m3 increase). This was performed by dividing the logarithm of the RR or OR by the number of international system units 22 . When a review analyzed continuous and binary data together, we meta‐analyzed the individual studies providing continuous data separately from those providing binary data.
We assessed the credibility of the associations according to recognized international criteria 23 , 24 , 25 , 26 . Specifically, we classified each association as convincing (class I), highly suggestive (class II), suggestive (class III), or weak (class IV). If an association was not significant, we classified it as such. Class I requires more than 1,000 cases, p<10−6, no evidence of small‐study effects or excess of significance bias, prediction interval not including the null value, the largest study nominally significant, and not large heterogeneity (i.e., I2< 50%). Class II requires more than 1,000 cases, p<10−6, and the largest study nominally significant. Class III requires more than 1,000 cases and p<10−3. Class IV only requires p<0.05.
We conducted a sensitivity analysis that included only longitudinal studies, to test the impact of the study design on the findings and ensure that, in the associations, the air pollution and climate change exposures reliably preceded the mental health outcomes.
We performed a complementary analysis by inferring the increase in the rates of selected mental health outcomes (i.e., those that were found to be associated with temperature increase with class I or II evidence) as a function of the earth yearly average land temperature anomaly. We retrieved the earth yearly average land temperature from 1750 to 2022 from Berkeley Earth (https://berkeleyearth.org), and calculated the earth yearly land temperature anomaly by subtracting from the observed 1800‐2022 land temperature the mean land temperature in the pre‐industrial period (i.e., from 1750 to 1799).
We used the corresponding RR derived from the umbrella review to make these inferences. For instance, if a mental health outcome had RR=1.01 per 1°C increase and the land temperature anomaly in a given year was 1°, we inferred 1% increase that year.
We estimated the yearly land temperature increase rate in the last decades and projected this rate up to 2050 (i.e., assuming that the land temperature anomaly will increase the same amount each year). Up to 2022, we derived the confidence intervals (CIs) of the inferred increase in mental health outcomes directly from the CIs of the present umbrella review. CIs from 2023 to 2050 were estimated via Monte‐Carlo simulations of the combination of our CIs with the prediction intervals of land temperature anomaly.
We performed all umbrella calculations with the R package metaumbrella 27 , which was developed by our group and first applied in a previous publication in this journal 23 . This is the first comprehensive package that allows conducting umbrella reviews by automatically performing all the necessary calculations and subsequently classifying the credibility of the evidence.
RESULTS
Literature search and studies identified
We identified 3,582 references. After duplicate removal, we screened 2,421 at the title and abstract level and 132 at the full‐text level. A final set of 32 systematic reviews with meta‐analysis 5 , 6 , 13 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , encompassing 284 individual studies (231 longitudinal and 53 cross‐sectional), were included in the umbrella review (see Figure 1 and Table 1). The excluded studies are detailed in the supplementary information.
Figure 1.

PRISMA flow chart
Table 1.
Characteristics of the systematic reviews with meta‐analysis included in the umbrella review
| Studies included | Sample size | Associations included | Exposure | Mental health outcome | |
|---|---|---|---|---|---|
| Abolhasani et al 28 | 4 | 86,516,610 | 1 | Air pollution | Hospitalization due to dementia |
| Borroni et al 13 | 39 | 4,659,344 | 12 | Air pollution | Depression |
| Braithwaite et al 31 | 4 | 34,451 | 1 | Air pollution | Suicidal behavior (mortality) |
| Cheng et al 33 | 19 | 40,217,872 | 2 | Air pollution | Dementia, vascular dementia |
| Chun et al 34 | 4 | 91,363 | 1 | Air pollution | Autism spectrum disorder |
| Bernardina Dalla et al 35 | 11 | 95,607 | 5 | Air pollution | ADHD |
| Davoudi et al 36 | 9 | 1,532,847 | 13 | Air pollution | Suicidal behavior (mortality) |
| Dhiman et al 37 | 4 | 578,383 | 1 | Air pollution | Alzheimer's disease |
| Dutheil et al 38 | 26 | 748,247 | 14 | Air pollution | Autism spectrum disorder |
| Flores‐Pajot et al 39 | 4 | 141,061 | 9 | Air pollution | Autism spectrum disorder |
| Fu et al 40 | 15 | 218,487 | 2 | Air pollution | Autism spectrum disorder, mild cognitive impairment |
| Fu et al 5 | 8 | 13,528,702 | 2 | Air pollution | Alzheimer's disease |
| Gong et al 41 | 14 | 77,053,755 | 4 | Air pollution | Alzheimer's disease, dementia, vascular dementia |
| Li et al 44 | 9 | 70,214 | 1 | Air pollution | Depression |
| Lin et al 45 | 17 | 645,663 | 10 | Air pollution | ADHD, autism spectrum disorder |
| Liu et al 46 | 27 | 1,009,799 | 4 | Air pollution | Autism spectrum disorder |
| Pourhoseini et al 48 | 3 | 31,587 | 20 | Air pollution | Post‐partum depression |
| Song et al 49 | 13 | 27,055 | 40 | Air pollution | Schizophrenia |
| Tang et al 50 | 12 | 13,158,086 | 3 | Air pollution | Alzheimer's disease, dementia, vascular dementia |
| Trushna et al 51 | 9 | 445,562 | 4 | Air pollution | Anxiety disorders, psychological stress |
| Wilker et al 52 | 12 | 16,357,675 | 2 | Air pollution | Dementia |
| Yu et al 53 | 10 | 2,703,941 | 2 | Air pollution | Cognitive impairment, dementia |
| Zeng et al 54 | 12 | 289,066 | 11 | Air pollution | Depression, depressive symptoms |
| Zhang et al 55 | 5 | 102,925 | 3 | Air pollution | ADHD |
| Zhao et al 56 | 52 | 80,986,923 | 23 | Air pollution | Alzheimer's disease, cognitive impairment, dementia, vascular dementia |
| Beaglehole et al 29 | 2 | 1,144 | 2 | Landslides, wildfires | Mental disorders, psychological distress |
| Bonde et al 30 | 4 | 2,702 | 1 | Cyclones, floods, tsunami | Depression |
| Chan et al 32 | 8 | 2,934 | 1 | Cyclones | PTSD symptoms |
| Frangione et al 6 | 20 | 3,021,622 | 7 | Precipitation, temperature | Suicidal behavior (mortality or attempts) |
| Li et al 43 | 32 | 8,179,080 | 15 | Barometric pressure, sunshine duration, temperature | Mental disorders; mood disorders; neurotic, stress‐related and somatoform disorders; schizophrenia |
| Liu et al 47 | 30 | 3,159,423 | 14 | Temperature | Mental disorders, organic mental disorders, schizophrenia, substance‐related mental disorders, suicidal behavior (mortality), hospital access |
| Heo et al 42 | 29 | 2,635,678 | 7 | Air pollution, temperature | Suicidal behavior (mortality, attempts or ideation, or self‐harm) |
ADHD – attention‐deficit/hyperactivity disorder, PTSD – post‐traumatic stress disorder
The individual studies included samples from the US (n=74), China (n=41), the UK (n=21), South Korea (n=20), Canada (n=19), Taiwan (n=13), Germany (n=12), The Netherlands (n=11), Spain (n=11), Sweden (n=11), France (n=8), Australia (n=6), Italy (n=6), Hong Kong (n=4), Japan (n=4), Denmark (n=3), Finland (n=3), Iran (n=3), Israel (n=3), Norway (n=3), Belgium (n=2), Brazil (n=2), India (n=2), Mexico (n=2), New Zealand (n=2), Poland (n=2), Portugal (n=2), Austria (n=1), Bangladesh (n=1), Colombia (n=1), Ghana (n=1), Greece (n=1), Greenland (n=1), Kazakhstan (n=1), Nigeria (n=1), Slovakia (n=1), South Africa (n=1), Sri Lanka (n=1), Switzerland (n=1), Turkey (n=1) and Vietnam (n=1). These samples do not sum to 284 because an individual study may have included multiple samples from different countries.
Characteristics of included systematic reviews with meta‐analysis
Of the systematic reviews with meta‐analysis, 25 focused on the mental health impact of air pollution 5 , 13 , 31 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 44 , 45 , 46 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 ; six on the impact of climate change hazards 6 , 29 , 30 , 32 , 43 , 47 ; and one on both 42 .
Mental health outcomes included mental disorders 5 , 13 , 30 , 33 , 34 , 35 , 37 , 38 , 39 , 40 , 41 , 44 , 45 , 46 , 48 , 49 , 50 , 52 , 53 , 55 , 56 ; suicidal behavior 6 , 31 , 36 , 42 ; mental disorders‐related symptomatology 32 ; access to mental health care services 28 , both mental disorders and mental disorders‐related symptomatology 29 , 51 , 54 ; and mental disorders, suicidal behavior, and access to mental health care services 47 .
Associations of air pollution or climate change exposures and mental health outcomes
We included and analyzed 237 associations of exposures to air pollution or climate change hazards and mental health outcomes. Of these associations, 195 (82.3%) concerned air pollution, and 42 (17.7%) involved climate change hazards.
The associations concerning air pollution focused, in decreasing order of frequency, on PM2.5 (n=40, 16.9%), airborne particular matter ≤10 μm in diameter (PM10) (n=35, 14.8%), nitrogen dioxide (NO2) (n=32, 13.6%), ozone (O3) (n=22, 9.3%), sulfur dioxide (SO2) (n=17, 7.2%), carbon monoxide (CO) (n=11, 4.6%), PM coarse (n=8, 3.4%), nitrogen oxides (NOx) (n=6, 2.5%), solvents (n=5, 2.1%), pesticides (n=3, 1.3%), metals (n=2, 0.8%), solid fuels (n=1, 0.4%), diesel PM (n=1, 0.4%), polycyclic aromatic hydrocarbons (n=1, 0.4%), or multiple pollutants together (n=11, 4.6%).
The associations concerning climate change hazards focused on temperature (n=35, 14.8%), barometric pressure (n=1, 0.4%), cyclones (n=1, 0.4%), precipitation (n=1, 0.4%), sunshine duration (n=1, 0.4%), or multiple hazards together (n=3, 1.3%).
Regarding mental health outcomes, associations focused, in decreasing order of frequency, on mental disorders (n=185, 78.1%), suicidal behavior (n=29, 12.4%), access to mental health care services (n=9, 3.7%), mental disorders‐related symptomatology (n=8, 3.3%), or multiple categories together (n=6, 2.5%).
Associations involving mental disorders encompassed organic mental disorders (n=42, 17.7%); schizophrenia (n=42, 17.7%); autism spectrum disorder (n=38, 16%); mood disorders (n=36, 15.3%); attention‐deficit/hyperactivity disorder (n=9, 3.8%); neurotic, stress‐related and somatoform disorders (n=5, 2.1%); substance‐related mental disorders (n=1, 0.4%); and multiple mental disorders together (n=12, 5.1%).
Suicidal behavior encompassed suicide mortality (n=15, 6.4%); suicide mortality, attempts or ideation, or self‐harm (n=7, 3.0%); and suicide mortality or attempts (n=7, 3.0%). Mental disorders‐related symptomatology encompassed depressive symptoms (n=5, 2.1%), psychological distress (n=2, 0.8%), and PTSD symptoms (n=1, 0.4%). Access to mental health care services encompassed hospital access (i.e., hospitalization or emergency department visits) (n=8, 3.3%) and hospitalization only (n=1, 0.4%) for specific mental conditions.
Convincing (class I) and highly suggestive (class II) associations
Among the 237 associations included in the umbrella review, one (0.4%) reached a convincing level of credibility (class I), and eleven (4.6%) reached a highly suggestive level of credibility (class II) (see Table 2).
Table 2.
Convincing (class I) and highly suggestive (class II) associations
| Exposure | Mental health outcome | Estimate (95% CIs) | p | N | I2 | PIs | SSE/ESB | LS | Class | |
|---|---|---|---|---|---|---|---|---|---|---|
| Solvents (high vs. low exposure, long‐term) | Incidence of dementia or cognitive impairment | OR=1.139 (1.090‐1.191) | <10−6 | 19,379 | 41% | SIG | No/No | Yes | I | |
| CO (high vs. low levels, long‐term) | Incidence of dementia | OR=1.587 (1.389‐1.812) | <10−6 | 2,629 | 0% | NS | No/No | Yes | II | |
| NOX (1 μg/m3 increase, long‐term) | Incidence of vascular dementia | HR=1.004 (1.003‐1.005) | <10−6 | 7,608 | 0% | ‐ | ‐/‐ | Yes | II | |
| PM10 (1 μg/m3 increase, during second trimester of pregnancy) | Incidence of post‐partum depression | OR=1.023 (1.014‐1.033) | <10−6 | 2,211 | 36% | ‐ | ‐/‐ | Yes | II | |
| SO2 (1 μg/m3 increase, short‐term) | Relapse of schizophrenia | 5 days after exposure | RR=1.005 (1.004‐1.006) | <10−6 | 8,682 | 0% | ‐ | ‐/‐ | Yes | II |
| 7 days after exposure | RR=1.004 (1.003‐1.005) | <10−6 | 8,682 | 0% | ‐ | ‐/‐ | Yes | II | ||
| Temperature (1°C increase, short‐term) | Suicide‐ or mental disorders‐related mortality | RR=1.024 (1.015‐1.033) | <10−6 | 1,559,502 | 75% | NS | Yes/Yes | Yes | II | |
| Suicidal behavior (mortality, attempts or ideation, or self‐harm) | RR=1.012 (1.011‐1.014) | <10−6 | 2,260,123 | 70% | SIG | No/No | Yes | II | ||
| Hospital access due to suicidal behavior or mental disorders | RR=1.011 (1.008‐1.015) | <10−6 | 1,052,237 | 86% | NS | Yes/Yes | Yes | II | ||
| Hospital access due to mental disorders only | RR=1.009 (1.006‐1.012) | <10−6 | 640,651 | 78% | NS | Yes/Yes | Yes | II | ||
| Mean apparent temperature (1°C increase, short‐term) | Suicidal behavior (mortality or attempts) | RR=1.010 (1.009‐1.011) | <10−6 | 323,163 | 0% | ‐ | ‐/‐ | Yes | II | |
| Cyclone exposure (temporal proximity) | PTSD symptoms severity | r=0.275 (0.189‐0.357) | <10−6 | ≥1,000 | 75% | SIG | No/No | Yes | II | |
CO – carbon monoxide, PM10 – airborne particulate matter with diameter ≤10 μm, NOx – nitrogen oxides, SO2 – sulfur dioxide, PTSD – post‐traumatic stress disorder, OR – odds ratio, HR – hazard ratio, RR – risk ratio, PIs – prediction intervals, SSE – small study effect, ESB – excess significant bias, LS – largest study with significant effect, SIG – significant, NS – not significant
The only class I association was that between long‐term exposure to solvents and a higher incidence of dementia or cognitive impairment (OR=1.139; 95% CI: 1.090‐1.191).
Long‐term exposure to high vs. low CO levels was associated with an increased incidence of dementia (OR=1.587; 95% CI: 1.389‐1.812, class II). Long‐term exposure to NOx increase was associated with a higher incidence of vascular dementia (HR=1.004 per 1 μg/m3, 95% CI: 1.003‐1.005, class II).
An increase in PM10 exposure during the second trimester of pregnancy was associated with an increased risk of developing post‐partum depression (OR=1.023 per 1 μg/m3 increase; 95% CI: 1.014‐1.033, class II). An increase in short‐term exposure to SO2 was associated with a higher risk of relapse of schizophrenia (RR=1.005 per 1 μg/m3, 95% CI: 1.004‐1.006; and RR=1.004 per 1 μg/m3, 95% CI: 1.003‐1.005, respectively 5 and 7 days after exposure; class II).
Short‐term exposure to temperature increase was associated with a higher risk of suicide‐ or mental disorders‐related mortality (RR=1.024 per 1°C increase; 95% CI: 1.015‐1.033, class II). It was also associated with a higher risk of suicidal behavior (RR=1.012 per 1°C increase; 95% CI: 1.011‐1.014, class II), a higher risk of hospital access due to suicidal behavior or mental disorders (RR=1.011 per 1°C increase; 95% CI: 1.008‐1.015, class II), and a higher risk of hospital access due to mental disorders only (RR=1.009 per 1°C increase; 95% CI: 1.006‐1.012, class II).
A short‐term exposure to apparent temperature increase (“apparent” is defined as the temperature equivalent perceived by humans 57 ) was associated with a higher risk of suicidal behavior (RR=1.010 per 1°C increase; 95% CI: 1.009‐1.011, class II).
Higher temporal proximity of cyclone exposure (i.e., fewer months since exposure) was associated with higher severity of PTSD symptoms (r=0.275; 95% CI: 0.189‐0.357, class II).
Sensitivity and complementary analyses
The sensitivity analysis that included only longitudinal studies confirmed all the above class I and class II associations, except that between temporal proximity of cyclone exposure and PTSD severity, which was based on cross‐sectional studies only.
One additional association reached class II evidence in the longitudinal analysis. This was the association between exposure to solid fuels (e.g., biomass, firewood) and a higher incidence of depression (OR=1.27; 95% CI: 1.16‐1.39, previously class III) (see also supplementary information).
Figure 2 shows, according to the above data, how much earth yearly land temperature anomaly (i.e., the increase in land temperature compared to the pre‐industrial period) may have increased the relevant mental health outcomes (e.g., suicide‐ or mental disorders‐related mortality) up to 2022, and the potential increase in the upcoming years. Our estimate indicates that this increased mortality is already ~5% now and will reach ~7% (95% CI: 4.2‐ 9.7) in 2050.
Figure 2.
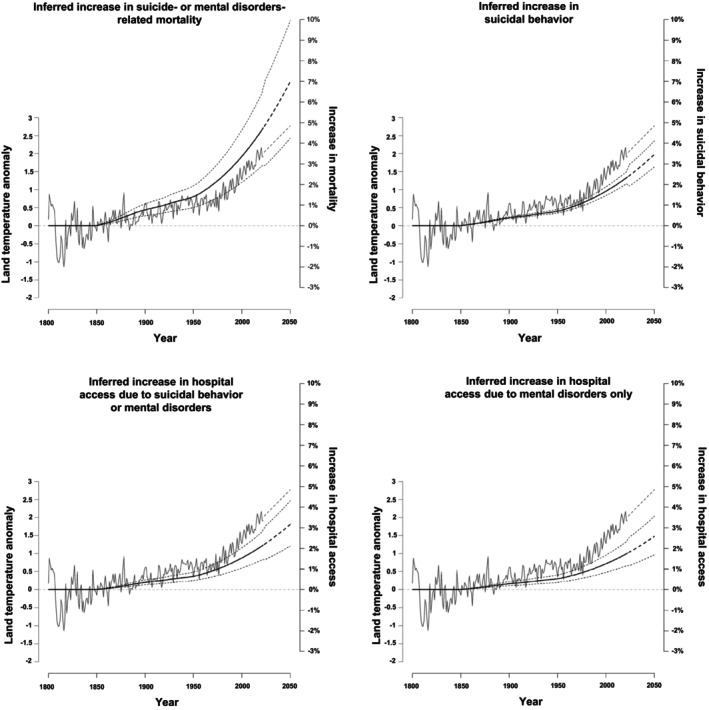
Inferred increase in mental health outcomes associated with temperature anomaly (earth yearly land temperature increase compared to average of pre‐industrial period). The fluctuating line represents the temperature anomaly. The steady line represents the relative risks (RRs) corresponding to temperature anomalies according to the RRs from the umbrella review. The dashed lines represent the confidence intervals derived from the umbrella review up to 2022, and estimated via Monte‐Carlo simulation for 2023‐2050.
Suggestive (class III), weak (class IV), and not significant associations
Among the 237 associations between exposures to air pollution or climate change hazards and mental health outcomes included in this umbrella review, 24 (10.1%) reached a suggestive level of credibility (class III); 65 (27.3%) reached a weak level of credibility (class IV); and 136 (57.6%) were not significant (see also supplementary information).
Quality of included systematic reviews with meta‐analysis
The quality of all the included systematic reviews with meta‐analysis was rated as “low” or “critically low”. Specifically, AMSTAR‐2 item 2 (i.e., presence of protocol) was not satisfied by 14 reviews (43.8%); item 4 (i.e., comprehensive literature search) by 15 reviews (46.9%); item 7 (i.e., list of studies excluded with reasons) by 31 reviews (96.9%); item 9 (i.e., satisfactory assessment of risk of bias) by four reviews (12.5%); item 13 (i.e., taking into account risk of bias in discussion of the results) by 15 reviews (46.9%); and item 15 (i.e., exploring and taking into account publication bias in discussion of results) by 17 reviews (53.1%) (see also supplementary information).
DISCUSSION
The present umbrella review comprehensively summarizes and assesses for the first time the credibility of the existing evidence on the impact of air pollution and climate change on mental health outcomes. Evidence emerged that some of these exposures are associated with mental health outcomes. Higher levels of specific air pollutants were associated with a higher risk of dementia or cognitive impairment (class I), cognitive disorders (class II), post‐partum depression (class II), and schizophrenia relapse (class II). Temperature increase was associated with an increase in suicidal behavior, suicide‐ or mental disorders‐related mortality; and hospital access due to suicidal behavior or mental disorders, or mental disorders only (class II).
A first strength of this umbrella review is the extensive database (284 individual studies) encompassing all continents, including the Global South, and therefore providing a global picture. Furthermore, we included the largest ever set of associations (n=237), systematically appraised with evidence‐based classification criteria that assess existing biases. To provide more stringent evidence, we converted all the exposure intervals to one unit in the International System of Units; applied a sensitivity analysis restricted to longitudinal studies; and conducted a complementary analysis to predict the future impact of associations involving increased temperature. The state‐of‐the‐art umbrella review method was further enhanced by using the metaumbrella package 27 , which facilitates large syntheses across multiple databases and association measures.
The strongest finding of this umbrella review is the convincing (class I) association between higher levels of exposure to solvents and a higher risk of developing dementia or cognitive impairment. Solvents (e.g., toluene, acetone, xylene, hexane, heptane, and ethyl acetate) can release volatile organic compounds into the atmosphere, contributing to the formation of ground‐level O3 and smog 58 . They are also directly toxic to many parts of the body, with symptoms ranging from skin irritation, headaches and blurred vision, to loss of consciousness and death 59 . The solvent most studied at the central nervous system level is toluene, whose adverse effects are manifested with acute encephalopathy and white matter damage, multifocal myelin loss, and macrophage accumulation 60 , 61 .
The main uses of solvents include paints, paint strippers, inks, and dry cleaning, and they continue to pose serious health risks, especially in low‐ and middle‐income countries, where alternatives to these materials are difficult to find for construction and manufacturing processes 62 , 63 . Because of their widespread use, solvent emissions are expected to approximately double by 2030 64 , which is alarming considering their environmental risk 58 and potential impact on climate change 65 .
We also found highly suggestive (class II) evidence for a higher incidence of cognitive disorders with CO and NOX increased exposure. CO is among the main gases that trap heat in the atmosphere (greenhouse gases), making the planet warmer and “thickening the Earth's atmospheric blanket” 66 . It is mainly produced by human activity (e.g., burning fossil fuels, solid waste, chemical reactions) 66 . NOx are gases mainly produced during the combustion of fossil fuels. They are precursors for the formation of O3, which has adverse effects on the environment 67 .
CO and NOx share toxic brain effects with other air pollutants 68 , 69 , including neuroinflammation, neurodegeneration, and cerebral vascular damage 70 . These air pollutants can enter the organism through the respiratory tract 71 . Once in the body, they may activate the inflammatory system and contribute to activation of microglia 72 , oxidative stress, and cell damage or death 73 , 74 . The current findings are therefore consistent with those reported by population‐based cohort studies indicating that living near major roads is associated with a higher incidence of dementia 75 .
It is also worth noticing that the association between CO and dementia did not reach class I evidence because of the prediction intervals that crossed the null value. The package metaumbrella that we used to perform the analyses estimates the prediction intervals through a t‐distribution with k‐2 degrees of freedom 76 . This method provides conservative results compared to other accepted methods, such as constructing prediction intervals using a normal distribution, which would have elevated this association to class I evidence.
Furthermore, we found evidence (class II) that the incidence of post‐partum depression increased with PM10 exposure during the second trimester of pregnancy. PM10 can contain harmful substances (e.g., benzopyrenes, furans, dioxins, and carcinogenic heavy metals) that can be inhaled. These particles are essentially produced by human sources (e.g., fuel combustion, heating, vehicles, biomass burning, and industrial activities), and their detrimental effects on physical health (e.g., the respiratory system) are well established 77 . It is possible that their effect on mental health is mediated by an increase in stress hormone levels 78 .
Indeed, there is some evidence that exposure to these particles increases cortisol levels 79 . These levels tend to be elevated during the second and third trimesters of pregnancy 80 (when there is an increased secretion of corticotropin‐releasing hormone from the placenta) and are associated with the risk of post‐partum depression 81 . Thus, the interplay of these pollutants with the physiological increase in stress hormones may account for the increased incidence of post‐partum depression. Future empirical research is, however, needed to confirm this hypothesis.
We also found evidence (class II) for a higher risk of relapse in patients with schizophrenia shortly (5 to 7 days) after exposure to increased levels of SO2. This is a toxic gas naturally released by volcanic activity and in the production of sulfuric acid. It can also be used as a disinfectant, a refrigerant, a reducing agent, a bleach, and a food preservative. It can modulate climate change processes 82 and has also been associated with increased all‐cause mortality 83 , higher risk of respiratory disease, and increased likelihood of cardiovascular events 84 , including stroke 85 .
However, the mechanism linking short‐term SO2 exposure to physical health outcomes has yet to be established. While it is possible that this exposure induces increased inflammation, potentially exacerbating or triggering new symptoms in individuals with schizophrenia, this remains speculative, and there is no conclusive evidence linking inflammatory markers to relapse in this disorder 86 . While the nature of this association requires further empirical studies, this finding conceptually supports the profound socio‐environmental dimension and origin of schizophrenia, which has been previously appraised by our and other groups 26 , 87 .
Overall, these findings align with the detrimental role of air pollution as a major global environmental and physical health problem, contributing to more than 8 million deaths per year 88 . It is estimated that the world's entire population (99%) breathes air that exceeds the pollution limits recommended by the World Health Organization (WHO) 89 . The current study adds to this evidence by indicating that air pollution has a negative impact also on mental health worldwide.
Innovative policies and initiatives have recently been launched to improve air quality, monitor pollutants, and strengthen cooperation between countries, such as the Forum for International Cooperation on Air Pollution 90 , the Task Force on Techno‐Economic Issues (TFTEI) Clearing House of Control Technologies 91 , and the WHO Air Quality Guidelines 92 . Future upgrades of these policies could consider the associations emerging from this umbrella review as outcome measures to map their global impact on mental health.
The second main finding of this study is the highly suggestive (class II) evidence for an association between temperature increase and several mental health outcomes, such as suicide‐ or mental disorders‐related mortality, suicidal behavior; and hospital access due to suicidal behavior or mental disorders, or mental disorders only. These are core real‐world outcomes of high clinical relevance, and their associations with an increasing temperature may represent an alarming finding.
In recent years, global warming has become one of the highest concerns, particularly for young people 93 . According to the Intergovernmental Panel on Climate Change, the global mean surface temperature in 2011‐2020 was 1.09°C higher than in 1850‐1900 94 . Recent reports revealed that 2023 was the hottest year on record, with global temperatures being close to the Paris Agreement limit of 1.5°C 95 . This finding is even more concerning when considering that temperatures on land rise faster (1.59°C) than those in the ocean (0.88°C), emphasizing the impact on humans 94 . The greenhouse effect caused by specific pollutants is the main driver of temperature increase and global warming 96 .
In this scenario, we demonstrate here that global warming negatively affects mental health. However, despite the huge magnitude of the problem, the biological mechanisms underlying this association remain unknown and likely involve complex multifactorial relationships 97 , 98 , 99 . Some evidence suggests that exposure to hot temperatures may directly affect brain function, with alterations in proper oxygenation and permeability of the blood‐brain barrier. Other studies implicate alterations in neurotransmitters 97 , or suggest that higher temperatures may directly worsen mood, leading people to feel more irritable and stressed, and amplifying symptoms of mental disorders 100 .
There are also numerous indirect effects of global warming on mental health outcomes. For example, in 2022, 84% of refugees and asylum seekers fled from highly climate‐fueled crises and climate‐vulnerable countries (e.g., because of droughts and increases in sea levels), representing “environmental refugees” 101 . Short‐term projections up to 2040 estimate that the average global surface temperature will increase by 0.4‐1°C, and long‐term projections suggest a temperature increase of up to 4.8°C in a high‐emissions scenario 102 . Accordingly, the United Nations’ projections predict that the environmental refugee situation will significantly deteriorate in the future.
To further support these projections and therefore inform future global initiatives that could tackle these issues, we estimated the future increase in suicide‐ or mental disorders‐related mortality associated with the predicted increase in land temperature. We inferred that this increased mortality is already ~5% now (compared with pre‐industrial levels) and will reach ~7% in 2050.
This umbrella review also found evidence (class II) that cyclones are increasing the severity of PTSD. These are large masses of air rotating around an area of low pressure, generally associated with heavy rainfalls, that can cause massive destruction to human populations in their path. In fact, they can cause both physical and psychological damage, interrupting daily routines and forcing dramatic evacuation and sheltering 103 . These events, along with the significant economic loss and adversity experienced in the aftermath, may constitute severe traumatic events associated with the development of PTSD 104 . However, this umbrella review calls for further studies and future confirmation, as the available evidence was not confirmed in sensitivity analyses.
The present work has some limitations. First, as an umbrella review, the evidence presented is limited to that found in systematic reviews with meta‐analysis, not considering associations that have not been meta‐analyzed. Second, the quality of the included systematic reviews with meta‐analysis was generally low, mainly because of inadequate discussion and investigation of sources of heterogeneity, or little transparency in presenting excluded studies. Third, although we evaluated an increase in a given exposure and the corresponding increased risk for a given mental health outcome, we did not assume that a reduction in the same exposure automatically corresponds to a proportional decrease in that risk. Indeed, our evidence does not contradict the fact that, for example, exposure to extreme cold may also worsen mental health outcomes, as described in Northern European countries 105 .
Fourth, although we analyzed specific associations, the exposures considered are not independent in the real world, and tend to co‐occur. Therefore, our results cannot provide information on the interaction and interdependence between different exposures. Fifth, some associations may be spurious or mediated by external factors not included in the analysis, such as the age, sex, or socioeconomic distribution of the population considered. Finally, association does not mean causation. Future research may better investigate associations for which we found no or weak evidence, investigate non‐linear relationships, and explore multiple environmental exposures simultaneously.
In conclusion, this umbrella review confirms that air pollution and climate change represent intertwined elements of the main global crisis of our time. The study extends the vast list of adverse effects of exposures to air pollution and climate change hazards on physical health by indicating that they are also a threat to global mental health. We quantified for the first time the negative impact that these exposures can exert on mental health worldwide, summarizing evidence‐based associations that can inform future research and population health actions. Notably, while the magnitude of most class I or II associations discussed above is small, they extend to the entire world population, and are therefore likely to have a substantial impact.
Our findings can be used to inform educational and public awareness campaigns on the impact of air pollution and climate change hazards on mental health, and to ensure public participation in programmes and information access on the issue. As we are living in a time that many authors refer to as the “Anthropocene” (i.e., the geological epoch dating from the commencement of significant human impact on earth's ecosystems, including anthropogenic air pollution and climate change 106 ), education is essential to encourage people to change their attitudes and behaviors and make informed decisions.
Widespread literacy on the impact of air pollution and climate change on mental health can empower all people and especially further motivate youth to take action 107 . Being aware of the available evidence and the associated actionable behaviors may also mitigate currently emerging pathological fears (e.g., eco‐anxiety, solastalgia, or ecological grief) 10 , 11 , 12 .
The current findings may also directly inform policy makers and institutions in order to better incorporate mental health as a core outcome in relevant policies. While mental health has recently received more attention in the context of environmental policies, this is still not enough. For example, initiatives such as the Lancet Countdown on Health and Climate Change, which aims to maintain an updatable monitoring system on climate change and human health, recognize that their system is currently limited when it comes to the impact of climate change on mental health 108 . Similarly, the WHO Policy Brief on Mental Health and Climate Change 20222 acknowledged that countries are not sufficiently considering mental health in their response to the climate emergency. Another report produced in the lead‐up to the 2023 Climate Change Conference by the WHO highlighted that mental health considerations remain largely absent from country commitments to meeting the Paris Agreement 109 . We hope that our findings may represent a reference point for the next generation of climate change policies and research.
As the urgency for action on air pollution and climate change increases, researching the specific factors modulating the associations outlined in this umbrella review becomes crucial. Future research should facilitate a closer interdisciplinary cross‐fertilization of environmental research and clinical psychiatry. A pivotal area of future research may include studies addressing the potential benefits of preventive approaches that target environmental exposures to improve physical and mental health outcomes conjointly. This umbrella review provides an initial evidence‐based set of actionable targets that future interventional studies could empirically investigate.
Overall, the evidence‐based associations identified here emphasize the need for collaborative, interdisciplinary efforts to develop and implement strategies that map and mitigate the effects of air pollution and climate change, and proactively protect mental health globally. This umbrella review calls for an urgent population‐level response, inviting policy makers, health professionals, and the public to prioritize and invest in initiatives that address the intersection of air pollution and climate change with mental health, in order to create the conditions for a more resilient and sustainable future.
ACKNOWLEDGEMENTS
This work was supported by NextGenerationEU (NGEU) and funded by the Italian Ministry of University and Research, National Recovery and Resilience Plan, project MNESYS (PE0000006). J. Radua is supported by the Spanish Ministry of Science and Innovation (PI22/00261), the AXA Research Fund, EIT Health, and the CERCA Program. G. Fico's work is supported by a fellowship from “La Caixa” Foundation. E. Vieta is supported by the Spanish Ministry of Science and Innovation (PI21/00787); the Secretaria d'Universitats i Recerca del Departament d'Economia i Coneixement (2021‐SGR‐01358); the CERCA Programme, Generalitat de Catalunya; La Marató‐TV3 Foundation; and the European Union Horizon 2020 Research and Innovation Program (H2020‐EU.3.1.1 and H2020‐EU.3.1.3). J. Radua and M. De Prisco contributed equally to this work. Supplementary information on this study is available at https://imardgroup.com/air_pollution_and_climate_change.
REFERENCES
- 1. Campbell‐Lendrum D, Neville T, Schweizer C et al. Climate change and health: three grand challenges. Nat Med 2023;29:1631‐8. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization . Mental health and climate change: policy brief. Geneva: World Health Organization, 2022. [Google Scholar]
- 3. Abbasi K, Ali P, Barbour V et al. Time to treat the climate and nature crisis as one indivisible global health emergency. BMC Public Health 2023;1:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Massazza A, Teyton A, Charlson F et al. Quantitative methods for climate change and mental health research: current trends and future directions. Lancet Planet Health 2022;6:e613‐27. [DOI] [PubMed] [Google Scholar]
- 5. Fu P, Yung KKL. Air pollution and Alzheimer's disease: a systematic review and meta‐analysis. J Alzheimer's Dis 2020;77:701‐14. [DOI] [PubMed] [Google Scholar]
- 6. Frangione B, Villamizar LAR, Lang JJ et al. Short‐term changes in meteorological conditions and suicide: a systematic review and meta‐analysis. Environ Res 2022;207:112230. [DOI] [PubMed] [Google Scholar]
- 7. Patz JA, Frumkin H, Holloway T et al. Climate change: challenges and opportunities for global health. JAMA 2014;312:1565‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Berry HL, Bowen K, Kjellstrom T. Climate change and mental health: a causal pathways framework. Int J Public Health 2010;55:123‐32. [DOI] [PubMed] [Google Scholar]
- 9. Crandon TJ, Dey C, Scott JG et al. The clinical implications of climate change for mental health. Nat Hum Behav 2022;6:1474‐81. [DOI] [PubMed] [Google Scholar]
- 10. Albrecht G. Solastalgia'. A new concept in health and identity. PAN: Philosophy Activism Nature; 2005;3:41‐55. [Google Scholar]
- 11. Cunsolo A, Harper SL, Minor K et al. Ecological grief and anxiety: the start of a healthy response to climate change? Lancet Planet Health 2020;4:e261‐3. [DOI] [PubMed] [Google Scholar]
- 12. Albrecht G. Chronic environmental change: emerging ‘psychoterratic’ syndromes. In: Weissbecker I (ed). Climate change and human well‐being: global challenges and opportunities. Berlin: Springer, 2011:43‐56. [Google Scholar]
- 13. Borroni E, Pesatori AC, Bollati V et al. Air pollution exposure and depression: a comprehensive updated systematic review and meta‐analysis. Environ Pollut 2022;292:118245. [DOI] [PubMed] [Google Scholar]
- 14. Pelgrims I, Devleesschauwer B, Guyot M et al. Association between urban environment and mental health in Brussels, Belgium. BMC Public Health 2021;21:1‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zijlena WL, Wolf K, Emeny R et al. The association of air pollution and depressed mood in 70,928 individuals from four European cohorts. Int J Hyg Environ Health 2016;219:212‐9. [DOI] [PubMed] [Google Scholar]
- 16. Luan G, Yin P, Wang L et al. Associations between ambient high temperatures and suicide mortality: a multi‐city time‐series study in China. Environ Sci Pollut Res 2019;26:20377‐85. [DOI] [PubMed] [Google Scholar]
- 17. Fernández‐Niño JA, Flórez‐García VA, Astudillo‐García CI et al. Weather and suicide: a decade analysis in the five largest capital cities of Colombia. Int J Environ Res Public Health 2018;15:1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fan S‐J, Heinrich J, Bloom MS et al. Ambient air pollution and depression: a systematic review with meta‐analysis up to 2019. Sci Total Environ 2020;701:134721. [DOI] [PubMed] [Google Scholar]
- 19. De Prisco M, Vieta E. The never‐ending problem: sample size matters. Eur Neuropsychopharmacol 2023;79:17‐8. [DOI] [PubMed] [Google Scholar]
- 20. Page MJ, Moher D, Bossuyt PM et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 2021;372:n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Shea BJ, Reeves BC, Wells G et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non‐randomised studies of healthcare interventions, or both. BMJ 2017;358: j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bureau International des Poids et Mesures . The International System of Units (SI): base units. www.bipm.org.
- 23. Dragioti E, Radua J, Solmi M et al. Impact of mental disorders on clinical outcomes of physical diseases: an umbrella review assessing population attributable fraction and generalized impact fraction. World Psychiatry 2023;22:86‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ioannidis JP. Integration of evidence from multiple meta‐analyses: a primer on umbrella reviews, treatment networks and multiple treatments meta‐analyses. CMAJ 2009;181:488‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Machado MO, Veronese N, Sanches M et al. The association of depression and all‐cause and cause‐specific mortality: an umbrella review of systematic reviews and meta‐analyses. BMC Med 2018;16:1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Radua J, Ramella‐Cravaro V, Ioannidis JP et al. What causes psychosis? An umbrella review of risk and protective factors. World Psychiatry 2018;17:49‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gosling CJ, Solanes A, Fusar‐Poli P et al. metaumbrella: the first comprehensive suite to perform data analysis in umbrella reviews with stratification of the evidence. BMJ Ment Health 2023;26:e300534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Abolhasani E, Hachinski V, Ghazaleh N et al. Air pollution and incidence of dementia: a systematic review and meta‐analysis. Neurology 2023;100:e242‐54. [DOI] [PubMed] [Google Scholar]
- 29. Beaglehole B, Mulder RT, Frampton CM et al. Psychological distress and psychiatric disorder after natural disasters: systematic review and meta‐analysis. Br J Psychiatry 2018;213:716‐22. [DOI] [PubMed] [Google Scholar]
- 30. Bonde JP, Utzon‐Frank N, Bertelsen M et al. Risk of depressive disorder following disasters and military deployment: systematic review with meta‐analysis. Br J Psychiatry 2016;208:330‐6. [DOI] [PubMed] [Google Scholar]
- 31. Braithwaite I, Zhang S, Kirkbride JB et al. Air pollution (particulate matter) exposure and associations with depression, anxiety, bipolar, psychosis and suicide risk: a systematic review and meta‐analysis. Environ Health Perspect 2019;127:126002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chan CS, Rhodes JE. Measuring exposure in Hurricane Katrina: a meta‐analysis and an integrative data analysis. PLoS One 2014;9:e92899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cheng S, Jin Y, Dou Y et al. Long‐term particulate matter 2.5 exposure and dementia: a systematic review and meta‐analysis. Public Health 2022;212:33‐41. [DOI] [PubMed] [Google Scholar]
- 34. Chun H, Leung C, Wen SW et al. Maternal exposure to air pollution and risk of autism in children: a systematic review and meta‐analysis. Environ Pollut 2020;256:113307. [DOI] [PubMed] [Google Scholar]
- 35. Bernardina Dalla MD, Ayala CO, Castro FCAQ et al. Environmental pollution and attention deficit hyperactivity disorder: a meta‐analysis of cohort studies. Environ Pollut 2022;315:120351. [DOI] [PubMed] [Google Scholar]
- 36. Davoudi M, Barjasteh‐Askari F, Amini H et al. Association of suicide with short‐term exposure to air pollution at different lag times: a systematic review and meta‐analysis. Sci Total Environ 2021;771:144882. [DOI] [PubMed] [Google Scholar]
- 37. Dhiman V, Trushna T, Raj D et al. Is air pollution associated with increased risk of dementia? A meta‐analysis of epidemiological research. Neurol India 2022;70:1004. [DOI] [PubMed] [Google Scholar]
- 38. Dutheil F, Comptour A, Morlon R et al. Autism spectrum disorder and air pollution: a systematic review and meta‐analysis. Environ Pollut 2021;278:116856. [DOI] [PubMed] [Google Scholar]
- 39. Flores‐Pajot M‐C, Ofner M, Do MT et al. Childhood autism spectrum disorders and exposure to nitrogen dioxide, and particulate matter air pollution: a review and meta‐analysis. Environ Res 2016;151:763‐76. [DOI] [PubMed] [Google Scholar]
- 40. Fu P, Guo X, Cheung FMH et al. The association between PM2.5 exposure and neurological disorders: a systematic review and meta‐analysis. Sci Total Environ 2019;655:1240‐48. [DOI] [PubMed] [Google Scholar]
- 41. Gong Y, Zhang X, Zhao X et al. Global ambient particulate matter pollution and neurodegenerative disorders: a systematic review of literature and meta‐analysis. Environ Sci Pollut Res 2023;30:39418‐30. [DOI] [PubMed] [Google Scholar]
- 42. Heo S, Lee W, Bell ML. Suicide and associations with air pollution and ambient temperature: a systematic review and meta‐analysis. Int J Environ Res Public Health 2021;18:7699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Li D, Zhang Y, Li X et al. Climatic and meteorological exposure and mental and behavioral health: a systematic review and meta‐analysis. Sci Total Environ 2023;892:164435. [DOI] [PubMed] [Google Scholar]
- 44. Li N, Song Q, Su W et al. Exposure to indoor air pollution from solid fuel and its effect on depression: a systematic review and meta‐analysis. Environ Sci Pollut Res 2022;29:49553‐67. [DOI] [PubMed] [Google Scholar]
- 45. Lin L‐Z, Zhan X‐L, Jin C‐Y et al. The epidemiological evidence linking exposure to ambient particulate matter with neurodevelopmental disorders: a systematic review and meta‐analysis. Environ Res 2022;209:112876. [DOI] [PubMed] [Google Scholar]
- 46. Liu H, Ding L, Qu G et al. Particulate matter exposure during pregnancy and infancy and risks of autism spectrum disorder in children: a systematic review and meta‐analysis. Sci Total Environ 2023;855:158830. [DOI] [PubMed] [Google Scholar]
- 47. Liu J, Varghese BM, Hansen A et al. Is there an association between hot weather and poor mental health outcomes? A systematic review and meta‐analysis. Environ Int 2021;153:106533. [DOI] [PubMed] [Google Scholar]
- 48. Pourhoseini SA, Akbary A, Mahmoudi H et al. Association between prenatal period exposure to ambient air pollutants and development of postpartum depression: a systematic review and meta‐analysis. Int J Environ Health Res 2024;34:455‐65. [DOI] [PubMed] [Google Scholar]
- 49. Song R, Liu L, Wei N et al. Short‐term exposure to air pollution is an emerging but neglected risk factor for schizophrenia: a systematic review and meta‐analysis. Sci Total Environ 2023;854:158823. [DOI] [PubMed] [Google Scholar]
- 50. Tang J, Chen A, He F et al. Association of air pollution with dementia: a systematic review with meta‐analysis including new cohort data from China. Environ Res 2022;223:115048. [DOI] [PubMed] [Google Scholar]
- 51. Trushna T, Dhiman V, Raj D et al. Effects of ambient air pollution on psychological stress and anxiety disorder: a systematic review and meta‐analysis of epidemiological evidence. Rev Environ Health 2021;36:501‐21. [DOI] [PubMed] [Google Scholar]
- 52. Wilker EH, Osman M, Weisskopf MG. Ambient air pollution and clinical dementia: systematic review and meta‐analysis. BMJ 2023;381:e071620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Yu X, Zheng L, Jiang W et al. Exposure to air pollution and cognitive impairment risk: a meta‐analysis of longitudinal cohort studies with dose‐response analysis. J Glob Health 2020;10:010417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Zeng Y, Lin R, Liu L et al. Ambient air pollution exposure and risk of depression: a systematic review and meta‐analysis of observational studies. Psychiatry Res 2019;276:69‐78. [DOI] [PubMed] [Google Scholar]
- 55. Zhang M, Wang C, Zhang X et al. Association between exposure to air pollutants and attention‐deficit hyperactivity disorder (ADHD) in children: a systematic review and meta‐analysis. Int J Environ Health Res 2022;32:207‐19. [DOI] [PubMed] [Google Scholar]
- 56. Zhao Y‐L, Qu Y, Ou Y‐N et al. Environmental factors and risks of cognitive impairment and dementia: a systematic review and meta‐analysis. Ageing Res Rev 2021;72:101504. [DOI] [PubMed] [Google Scholar]
- 57. National Weather Service . What is the heat index? www.weather.gov.
- 58. Lewis AC, Hopkins JR, Carslaw DC et al. An increasing role for solvent emissions and implications for future measurements of volatile organic compounds. Philos Trans R Soc A 2020;378:20190328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Joshi DR, Adhikari N. An overview on common organic solvents and their toxicity. J Pharm Res Int 2019;28:1‐18. [Google Scholar]
- 60. Al‐Hajri Z, Del Bigio MR. Brain damage in a large cohort of solvent abusers. Acta Neuropathol 2010;119:435‐45. [DOI] [PubMed] [Google Scholar]
- 61. Filley CM, Halliday W, Kleinschmidt‐DeMasters B. The effects of toluene on the central nervous system. J Neuropathol Exp Neurol 2004;63:1‐12. [DOI] [PubMed] [Google Scholar]
- 62. Dodson RE, Udesky JO, Colton MD et al. Chemical exposures in recently renovated low‐income housing: influence of building materials and occupant activities. Environ Int 2017;109:114‐27. [DOI] [PubMed] [Google Scholar]
- 63. Roose B, Tennyson EM, Meheretu G et al. Local manufacturing of perovskite solar cells, a game‐changer for low‐and lower‐middle income countries? Energy Environ Sci 2022;15:3571‐82. [Google Scholar]
- 64. US Environmental Protection Agency . Global mitigation of non‐CO2 greenhouse gases: solvents. www.epa.gov.
- 65. Jimenez‐Gonzalez C. Life cycle considerations of solvents. Curr Opin Green Sustain Chemistry 2019;18:66‐71. [Google Scholar]
- 66. US Environmental Protection Agency . Overview of greenhouse gases. www.epa.gov.
- 67. UK Department for Environment Food & Rural Affairs. National statistics. Nitrogen dioxide (NO2). www.gov.uk.
- 68. Lo C‐P, Chen S‐Y, Lee K‐W et al. Brain injury after acute carbon monoxide poisoning: early and late complications. Am J Roentgenol 2007;189:205‐11. [DOI] [PubMed] [Google Scholar]
- 69. Ridgway P, Nixon T, Leach J‐P. Occupational exposure to organic solvents and long‐term nervous system damage detectable by brain imaging, neurophysiology or histopathology. Food Chem Toxicol 2003;41:153‐87. [DOI] [PubMed] [Google Scholar]
- 70. Block ML, Calderón‐Garcidueñas L. Air pollution: mechanisms of neuroinflammation and CNS disease. Trends Neurosci 2009;32:506‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Jankowska‐Kieltyka M, Roman A, Nalepa I. The air we breathe: air pollution as a prevalent proinflammatory stimulus contributing to neurodegeneration. Front Cell Neurosci 2021;15:647643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Gómez‐Budia M, Konttinen H, Saveleva L et al. Glial smog: interplay between air pollution and astrocyte‐microglia interactions. Neurochem Int 2020;136:104715. [DOI] [PubMed] [Google Scholar]
- 73. Levy RJ. Carbon monoxide pollution and neurodevelopment: a public health concern. Neurotoxicol Teratol 2005;49:31‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Li H, Xin X. Nitrogen dioxide (NO2) pollution as a potential risk factor for developing vascular dementia and its synaptic mechanisms. Chemosphere 2013;92:52‐8. [DOI] [PubMed] [Google Scholar]
- 75. Chen H, Kwong JC, Copes R et al. Living near major roads and the incidence of dementia, Parkinson's disease, and multiple sclerosis: a population‐based cohort study. Lancet 2017;389:718‐26. [DOI] [PubMed] [Google Scholar]
- 76. Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta‐analyses. BMJ 2011;342:d549. [DOI] [PubMed] [Google Scholar]
- 77. Dominski FH, Branco JHL, Buonanno G et al. Effects of air pollution on health: a mapping review of systematic reviews and meta‐analyses. Environ Res 2021;201:111487. [DOI] [PubMed] [Google Scholar]
- 78. Payne JL, Maguire J. Pathophysiological mechanisms implicated in postpartum depression. Front Neuroendocrinol 2019;52:165‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Khamirchi R, Moslem A, Agah J et al. Maternal exposure to air pollution during pregnancy and cortisol level in cord blood. Sci Total Environ 2020;713:136622. [DOI] [PubMed] [Google Scholar]
- 80. Duthie L, Reynolds RM. Changes in the maternal hypothalamic‐pituitary‐adrenal axis in pregnancy and postpartum: influences on maternal and fetal outcomes. Neuroendocrinology 2013;98:106‐15. [DOI] [PubMed] [Google Scholar]
- 81. Yim IS, Glynn LM, Schetter CD et al. Risk of postpartum depressive symptoms with elevated corticotropin‐releasing hormone in human pregnancy. Arch Gen Psychiatry 2009;66:162‐69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Ward PL. Sulfur dioxide initiates global climate change in four ways. Thin Solid Films 2009;517:3188‐203. [Google Scholar]
- 83. Orellano P, Reynoso J, Quaranta N. Short‐term exposure to sulphur dioxide (SO2) and all‐cause and respiratory mortality: a systematic review and meta‐analysis. Environ Int 2021;150:106434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Mustafić H, Jabre P, Caussin C et al. Main air pollutants and myocardial infarction: a systematic review and meta‐analysis. JAMA 2012;307:713‐21. [DOI] [PubMed] [Google Scholar]
- 85. Shen S, Li X, Yuan C et al. Association of short‐term exposure to sulfur dioxide and hospitalization for ischemic and hemorrhagic stroke in Guangzhou, China. BMC Public Health 2020;20:1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Miller BJ, Lemos H, Schooler NR et al. Longitudinal study of inflammation and relapse in schizophrenia. Schizophr Res 2023;252:88‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Arango C, Dragioti E, Solmi M et al. Risk and protective factors for mental disorders beyond genetics: an evidence‐based atlas. World Psychiatry 2021;20:417‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Lelieveld J, Haines A, Burnett R et al. Air pollution deaths attributable to fossil fuels: observational and modelling study. BMJ 2023;383:e077784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. World Health Organization . Air pollution. Geneva: World Health Organization, 2022. [Google Scholar]
- 90. Swedish Environmental Protection Agency . Forum for International Cooperation on Air Pollution. www.naturvardsverket.se.
- 91.Task Force on Techno‐Economic Issues. TFTEI Clearing House of Control Technologies. www.tftei.citepa.org.
- 92. World Health Organization . WHO global air quality guidelines: particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide. Geneva: World Health Organization, 2021. [PubMed] [Google Scholar]
- 93. Marlon J, Rosenthal S, Goldberg M et al. Younger Americans are growing more worried about global warming. New Haven: Yale Program on Climate Change Communication, 2022. [Google Scholar]
- 94. Gulev SK, Thorne PW, Ahn J et al. Changing state of the climate system. In: Masson‐Delmotte V, Zhai P, Pirani A et al. (eds). Climate change 2021: the physical science basis. Cambridge: Cambridge University Press, 2021:287‐422. [Google Scholar]
- 95. Copernicus Climate Change Service . 2023. is the hottest year on record, with global temperature close to the 1.5°C limit. https://climate.copernicus.eu.
- 96. D'Amato G, Akdis C. Global warming, climate change, air pollution and allergies. Allergy 2020;75:2158‐60. [DOI] [PubMed] [Google Scholar]
- 97. Lõhmus M. Possible biological mechanisms linking mental health and heat – a contemplative review. Int J Environ Res Public Health 2018;15:1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Minor K, Bjerre‐Nielsen A, Jonasdottir SS et al. Rising temperatures erode human sleep globally. One Earth 2022;5:534‐49. [Google Scholar]
- 99. Bundo M, Preisig M, Merikangas K et al. How ambient temperature affects mood: an ecological momentary assessment study in Switzerland. Environ Health 2023;22:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Massazza A. Explained: How climate change affects mental health. https://wellcome.org.
- 101. United Nations High Commissioner for Refugees. Climate change and disaster displacement. www.unhcr.org.
- 102. Lee J‐Y, Marotzke J, Bala G et al. Future global climate: scenario‐based projections and near‐term information. In: Masson‐Delmotte V, Zhai P, Pirani A et al (eds). Climate change 2021: the physical science basis. Cambridge: Cambridge University Press, 2021:553‐672. [Google Scholar]
- 103. Espinel Z, Kossin JP, Galea S et al. Forecast: Increasing mental health consequences from Atlantic hurricanes throughout the 21st century. Psychiatr Serv 2019;70:1165‐67. [DOI] [PubMed] [Google Scholar]
- 104. Galea S, Brewin CR, Gruber M et al. Exposure to hurricane‐related stressors and mental illness after Hurricane Katrina. Arch Gen Psychiatry 2007;64:1427‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Ruuhela R, Hiltunen L, Venäläinen A et al. Climate impact on suicide rates in Finland from 1971 to 2003. Int J Biometeorol 2009;53:167‐75. [DOI] [PubMed] [Google Scholar]
- 106. Pavid K. What is the Anthropocene and why does it matter? www.nhm.ac.uk.
- 107. United Nations Climate Actions . Education is key to addressing climate change. www.un.org.
- 108. Romanello M, di Napoli C, Green C et al. The 2023 report of the Lancet Countdown on health and climate change: the imperative for a health‐centred response in a world facing irreversible harms. Lancet 2023;402:2346‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. World Health Organization . 2023 WHO review of health in Nationally Determined Contributions and long‐term strategies: health at the heart of the Paris Agreement. Geneva: World Health Organization, 2023. [Google Scholar]


