Abstract
Background and Objectives
This population-based analysis characterizes the relative frequency of migraine-related stigma and its cross-sectional relationship to migraine outcomes. We hypothesized that migraine-related stigma would be inversely associated with favorable migraine outcomes across headache day categories.
Methods
OVERCOME (US) is a web-based observational study that annually recruited a demographically representative US sample and then identified people with active migraine using a validated migraine diagnostic questionnaire. It also assessed how frequently respondents experienced migraine-related stigma using a novel 12-item questionnaire (Migraine-Related Stigma, MiRS) that contained 2 factors; feeling that others viewed migraine as being used for Secondary Gain (8 items, α = 0.92) and feeling that others were Minimizing disease Burden (4 items, α = 0.86). We defined 5 groups: (1) MiRS-Both (Secondary Gain and Minimizing Burden often/very often; (2) MiRS-SG (Secondary Gain often/very often); (3) MiRS-MB (Minimizing Burden often/very often); (4) MiRS-Rarely/Sometimes; (5) MiRS-Never. Using MiRS group as the independent variable, we modeled its cross-sectional relationship to disability (Migraine Disability Assessment, MIDAS), interictal burden (Migraine Interictal Burden Scale-4), and migraine-specific quality of life (Migraine Specific Quality of Life v2.1 Role Function-Restrictive) while controlling for sociodemographics, clinical features, and monthly headache day categories.
Results
Among this population-based sample with active migraine (n = 59,001), mean age was 41.3 years and respondents predominantly identified as female (74.9%) and as White (70.1%). Among respondents, 41.1% reported experiencing, on average, ≥4 monthly headache days and 31.7% experienced migraine-related stigma often/very often; the proportion experiencing migraine-related stigma often/very often increased from 25.5% among those with <4 monthly headache days to 47.5% among those with ≥15 monthly headache days. The risk for increased disability (MIDAS score) was significant for each MiRS group compared with the MiRS-Never group; the risk more than doubled for the MiRS-Both group (rate ratio 2.68, 95% CI 2.56–2.80). For disability, interictal burden, and migraine-specific quality of life, increased migraine-related stigma was associated with increased disease burden across all monthly headache day categories.
Discussion
OVERCOME (US) found that 31.7% of people with migraine experienced migraine-related stigma often/very often and was associated with more disability, greater interictal burden, and reduced quality of life.
Introduction
Migraine is a common, complex, chronic neurobiological disease.1 It is the second leading cause of years lived with disability worldwide.2 The burden of migraine occurs during and between attacks and negatively affects an individual's ability to optimally function in their life roles.1,3 Those living with migraine may experience reduced participation in family activities, impaired social functioning, and reduced workplace productivity.4,5
Another potential negative repercussion of living with migraine arises from migraine-related stigma. Stigma involves discrediting/devaluing attitudes toward an individual or group based on them possessing an attribute viewed as deviating from social norms.6,7 Disease-related stigma occurs in many diseases,7 and there is indication that it could be especially relevant for those living with migraine.8-10 Stigma may arise when others express their stigmatizing attitudes through words or behaviors6,11,12 or when the person with the disease recognizes negative stereotypes about the disease and experiences shame (for having the disease), fear (of experiencing stigma from others), or other negative emotions.11,12 Stigma has been linked to poor outcomes for other diseases13-15; findings from focus groups and tertiary care settings16,17 suggest migraine-related stigma may be associated with poorer outcomes.10,16
There are no population-based data assessing how often people with migraine experience migraine-related stigma and how stigma is associated with migraine outcomes. The ObserVational survey of the Epidemiology, tReatment and Care Of MigrainE (OVERCOME) (US) study provides an ideal setting for addressing these gaps. The study recruited demographically representative samples of the US population and then identified individuals with active migraine. A key objective of OVERCOME (US) was to characterize how often people with migraine experience migraine-related stigma and its relationship to migraine outcomes. Given migraine's concealability and the study's interest in evaluating how often people experience migraine-related stigmatizing attitudes/words/behaviors from others, the investigators determined that existing measures6 did not sufficiently capture specific aspects of migraine-related stigma. Accordingly we created a set of questions to specifically assess migraine-related stigma. It was hypothesized that experiencing migraine-related stigma more often would be associated with poorer outcomes (disability, interictal burden, and migraine-specific quality of life) across levels of headache frequency.
Methods
Study Design
OVERCOME (US) is a prospective, multicohort, longitudinal, web-based survey conducted in a US consumer panel using quota sampling to establish a demographically representative (by geographic region, age, race, sex, and race nested within sex) sample (eMethods, links.lww.com/WNL/D342).18
The current analyses focus on pooled data from baseline surveys conducted in 2018, 2019, and 2020. Study inclusion criteria were (1) age 18 years or older, (2) US resident, (3) online survey panel member, (4) internet access, and (5) ability to read/write English. Individuals who passed the demographic screener and reported active headache(s) in the past 12 months completed the validated American Migraine Study/American Migraine Prevalence and Prevention Study migraine diagnostic questionnaire19,20 (which uses ICHD-3 criteria as the basis for the questions within the questionnaire)21 and were asked about a history of a medical diagnosis of migraine. Individuals meeting criteria for migraine had to answer questions related to the impact, consultation, and treatment of migraine. For the current analyses, only those meeting migraine criteria according to the diagnostic questionnaire were included.
Standard Protocol Approvals, Registrations, and Patient Consents
The study was approved by the Sterling Institutional Review Board (IRB ID #6425-001). Random panel participants were emailed invitations to participate in an online general health survey. Interested respondents voluntarily provided electronic informed consent and received honoraria in the form of survey panel points.
Measures
Migraine-Related Stigma
We assessed how often individuals with migraine felt that they had experienced migraine-related stigma using the Migraine-Related Stigma (MiRS) questionnaire. The questions were developed based on our review of existing stigma scales and literature,14,16 expert clinician input, and focus groups among people with migraine. Details of MiRS development are presented elsewhere.22 In brief, the question stem for each item was “How often have you felt that others viewed your migraine or severe headache attacks,” for example, “…as a way to get attention.” eTable 1 (links.lww.com/WNL/D342) includes all 12 MiRS questions. There were 5 frequency-denominated response options (“never,” scored as 0; “rarely,” scored as 1; “sometimes,” scored as 2; “often,” scored as 3; “very often,” scored as 4). Previous factor assessment22 suggested 2 MiRS factors. One factor (Cronbach's α = 0.92) contained 8 items assessing how frequently the respondent felt that others viewed migraine was being used to obtain or avoid something and was labeled “Secondary Gain.” The second factor (Cronbach's α = 0.86) contained 4 items assessing how frequently the respondent felt that others minimized the burden of their migraine disease and was labeled “Minimizing Burden.” Because both MiRS-Secondary Gain scores (range 0–32) and MiRS-Minimizing Burden (range 0–16) had 0-inflated distributions, scores were categorized by how often the respondent experienced each aspect of migraine-related stigma. Secondary Gain categories were 0 = never, 1–8 = rarely, 9–16 = sometimes, 17–24 = often, 25–32 = very often; Minimizing Burden categories were: 0 = never, 1–4 = rarely, 5–8 = sometimes, 9–12 = often, 13–16 = very often). We used these categorizations to determine a respondent's assignment into 1 of 5 overall MiRS groups: (1) MiRS-Both (Secondary Gain and Minimizing Burden often/very often); (2) MiRS-Secondary Gain often/very often; (3) MiRS-Minimizing Burden often/very often; (4) MiRS-Rarely/Sometimes; and (5) MiRS-Never (eFigure 1).
Migraine Disability Assessment
Migraine-related disability was measured using the 5-item Migraine Disability Assessment (MIDAS), 23 which quantifies the number of days an individual missed/had reduced productivity at work/home/social events over the preceding 3 months. For the current article, total number (score) of disability days and validated disability category (0–5 = little/none; 6–10 = mild; 11–20 = moderate; ≥21 = severe) were used.
Migraine Interictal Burden Scale-4
The interictal burden of migraine (i.e., burden of migraine between attacks) during the previous 4 weeks was measured using the 4-item Migraine Interictal Burden Scale-4 (MIBS-4).3,24 Each item contains 5 responses ranging from “never” (scored as 0) to “most or all of the time” (scored as 4) with scores ranging from 0 to 16. For the current article, the total score and interictal burden category (0 = none; 1–2 = mild; 3–4 = moderate; ≥5 = severe)3 were used.
Migraine-Specific Quality of Life Questionnaire v2.1 Role-Function Restrictive
The functional impact of migraine on social and work-related activities over the previous 4 weeks was measured using the 7-item Migraine-Specific Quality of Life Questionnaire v2.1 Role-Function Restrictive (MSQ-RFR) scale.25,26 Each item contains 6 response options ranging from 1 (“none of the time”) to 6 (“all of the time”). The raw score is transformed to a score of 0–100 with higher scores indicating better role function.
eTable 2 (links.lww.com/WNL/D342) includes the full list of sociodemographic and clinical characteristics included for the current analyses. This included age, sex at birth; race (individuals selected all that applied among multiple options; categories used for analytic purposes were White only, Black only, and “Other Races,” which combined non-White only and non-Black only categories given the small percentages within those categories that precluded meaningful comparisons); ethnicity (Hispanic, Latino/Spanish origin); rural-urban residence (the first 3 digits of the respondent's zip code were used to classify rural/urban); geographic region (based on current state of residence); highest level of education (college degree or higher were combined); current employment status (employed full-time or part-time were combined); income (total annual household income before taxes); current health insurance status (any current insurance type was considered “yes”); marital status (married or living with a partner were combined); children (younger than 18 years) living at home (≥1 were classified as “yes”); body mass index (BMI; categories used were underweight/normal, overweight, obese); total comorbidities (respondents indicated yes/no for 26 comorbidities); Patient Health Questionnaire-4 (PHQ-4) total score27 (4 items with total score ranging from 0 to 12 where higher scores reflect more frequently experienced symptoms of key components of anxiety and depression); monthly headache day frequency (calculated as the average over the previous 3 months); and questions concerning how frequently the respondent hid migraine at work or from family/friends.
Statistical Analysis
Mean and SDs were summarized for continuous or ordinal interval variables; percentages were reported for categorical variables. The association between MiRS group and sociodemographics, clinical characteristics, monthly headache day frequency, and patient-reported outcomes was assessed using bivariate analyses (1-way analysis of variance for continuous variables, χ2 test for categorical variables). All tests were 2-sided, and p-values <0.05 were considered statistically significant. Given the large sample size, standardized mean difference (SMD) was used in addition to p-values to compare select sociodemographics between MiRS groups. SMD values of <0.2 indicated no difference, 0.2–0.49 a small difference, 0.5–0.79 a moderate difference, and ≥0.8 represented a large difference. MIDAS score, MIBS-4 score, and MSQ-RFR score were each modeled using a negative binomial regression with log link to accommodate skewness of the distribution of the outcome measures. The covariates used in the model were monthly headache day frequency, age, sex, race, ethnicity, rural-urban commuting area, geographic region, education, income, marital status, having nonadult children, health insurance, employment status, BMI, total self-reported comorbidities, and PHQ-4 total score. The results were expressed as the ratio of the covariate-adjusted estimated mean for a MiRS group relative to the model estimated mean for the MiRS-Never group and are presented as rate ratios (RRs; the ratios involve a rate because the outcome measures were assessed for a period common to all respondents) with 95% CIs. The negative binomial regression models (with and without the 5 MiRS groups as an independent variable) were used to generate estimated (predicted) values (MIDAS score, MIBS-4 score, MSQ-RFR score) for each patient, given the values of their covariates, and the average of those values for each outcome was plotted against monthly headache-day frequency. All statistical analyses were conducted using SAS version 9.4 (Proc FACTOR for the factor analysis and Proc GENMOD for the negative binomial regression).
Data Availability
Lilly will provide access to anonymized individual participant data collected during the study. The data will be available to request on vivli.org after the study team has completed analyses and publications. Access will be provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data sharing agreement. After a proposal is approved, data and documents, including the study protocol, will need to be provided in a secure data sharing environment. For details on submitting a request, see the instructions provided at vivli.org.
Results
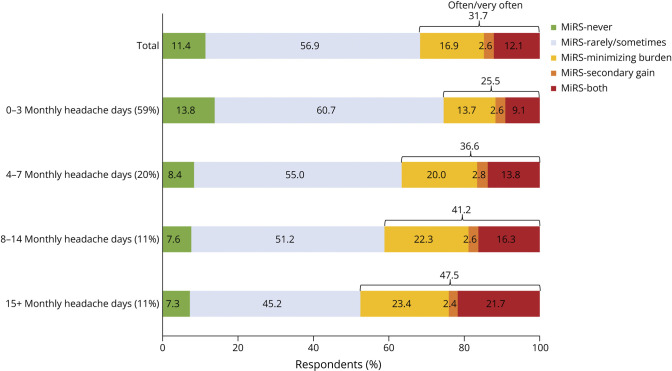
A total of 290,162 individuals responded to the invitation, consented to participate, were eligible, completed the demographic screener, and made up the demographically representative sample of US adults. The OVERCOME (US) baseline migraine cohort consisted of 59,001 individuals with active migraine (eFigure 2, links.lww.com/WNL/D342). Table 1 shows the sample mean age was 41.3 (SD 14.6) years, and the sample predominantly identified as female (74.9%) (44,179/59,001); 10.9% (6,411/59,001) identified as Hispanic, 7.7% (4,560/59,001) as Black, and 70.1% (41,390/59,001) as White. Table 2 shows that 41.0% (24,225/59,001) reported experiencing 4 or more monthly headache days on average over the previous 3 months, a majority (53.8%) (31,730/59,001) reported at least moderate interictal burden (MIBS-4), 44.4% (26,203/59,001) reported at least moderate disability (MIDAS), and MSQ-RFR scores were, on average, 53.9 (SD 23.9). eFigure 3 shows the MiRS Secondary Gain and Minimizing Burden distributions. Figure 1 shows that in this sample, 31.7% (18,708/59,001) reported experiencing MiRS-Secondary Gain and/or MiRS-Minimizing Burden often/very often and shows that the proportion of individuals experiencing at least 1 form of migraine-related stigma often/very often increased from 25.4% in the 0–3 monthly headache day group to 47.5% in the ≥15 monthly headache day group.
Table 1.
Sociodemographics by MiRS Group (n = 59,001),a as a Percentage of All Respondents
| MiRS group | Minimizing burden/secondary gain/both often/very often (N = 18,708; 31.7%) | SMD Minimizing burden/secondary gain/both often/very often vs never | ||||||
| Never (N = 6,715; 11.4%) | Rarely/sometimes (N = 33,578; 56.9%) | Minimizing burden Often/very often (N = 9,987; 16.9%) |
Secondary gain Often/very often (N = 1,556; 2.6%) |
Both often/very often (N = 7,165; 12.1%) | Total (N = 59,001) | |||
| Age, y, mean (SD)b | 44.7 (15.3) | 42.5 (14.8) | 40.0 (14.1) | 35.3 (11.7) | 35.9 (11.9) | 41.3 (14.6) | 38.0 (13.3) | 0.46 |
| Sex at birth, n (%)b | ||||||||
| Female | 5,208 (77.6) | 24,920 (74.2) | 7,803 (78.1) | 1,003 (64.5) | 5,244 (73.2) | 44,178 (74.9) | 14,050 (75.1) | 0.06 |
| Male | 1,507 (22.4) | 8,658 (25.8) | 2,184 (21.9) | 553 (35.5) | 1,921 (26.8) | 14,823 (25.1) | 4,658 (24.9) | 0.06 |
| Live in metropolitan area, n (% yes)b | 5,605 (83.5) | 28,008 (83.4) | 8,206 (82.2) | 1,324 (85.1) | 5,844 (81.6) | 48,987 (83.0) | 15,374 (82.2) | 0.03 |
| Geographic region, n (%)b | ||||||||
| Northeast | 1,278 (19.0) | 6,072 (18.1) | 1,637 (16.4) | 275 (17.7) | 1,102 (15.4) | 10,364 (17.6) | 3,014 (16.1) | 0.08 |
| Midwest | 1,461 (21.8) | 7,678 (22.9) | 2,285 (22.9) | 352 (22.6) | 1,556 (21.7) | 13,332 (22.6) | 4,193 (22.4) | 0.02 |
| South | 2,650 (39.5) | 13,152 (39.2) | 4,026 (40.3) | 638 (41.0) | 3,011 (42.0) | 23,477 (39.8) | 7,675 (41.0) | 0.03 |
| West | 1,326 (19.7) | 6,676 (19.9) | 2,039 (20.4) | 291 (18.7) | 1,496 (20.9) | 11,828 (20.0) | 3,826 (20.5) | 0.02 |
| Ethnicity, n (% Hispanic, Latino/Spanish)b | 532 (7.9) | 3,469 (10.3) | 1,074 (10.8) | 284 (18.3) | 1,052 (14.7) | 6,411 (10.9) | 2,410 (12.9) | 0.16 |
| Race, n (%)b | ||||||||
| White only | 4,956 (73.8) | 23,782 (70.8) | 7,083 (70.9) | 898 (57.7) | 4,668 (65.2) | 41,387 (70.1) | 12,649 (67.6) | 0.14 |
| Black only | 564 (8.4) | 2,677 (8.0) | 688 (6.9) | 139 (8.9) | 492 (6.9) | 4,560 (7.7) | 1,319 (7.1) | 0.05 |
| Other races | 1,195 (17.8) | 7,119 (21.2) | 2,216 (22.2) | 519 (33.4) | 2,005 (28.0) | 13,054 (22.1) | 4,740 (25.3) | 0.18 |
| Education, n (% college graduate)b | 2,386 (35.5) | 11,924 (35.5) | 3,229 (32.3) | 534 (34.3) | 2,377 (33.2) | 20,450 (34.7) | 6,140 (32.8) | 0.06 |
| Employment status, n (% full-time/part-time)b | 3,696 (55.0) | 19,313 (57.5) | 5,328 (53.3) | 966 (62.1) | 4,203 (58.7) | 33,506 (56.8) | 10,497 (56.1) | 0.02 |
| Annual household income, n (% <$50,000)b | 3,097 (46.1) | 16,473 (49.1) | 5,265 (52.7) | 801 (51.5) | 3,930 (54.8) | 29,566 (50.1) | 9,996 (53.4) | 0.15 |
| Health insurance, n (% yes)b | 5,725 (85.3) | 28,796 (85.8) | 8,448 (84.6) | 1,268 (81.5) | 5,999 (83.7) | 50,236 (85.1) | 15,715 (84.0) | 0.03 |
| Married/living with partner, n (% yes)b | 3,821 (56.9) | 18,579 (55.3) | 5,388 (54.0) | 796 (51.2) | 3,914 (54.6) | 32,498 (55.1) | 10,098 (54.0) | 0.06 |
| Children younger than 18 y, n (% yes)b | 2,426 (36.1) | 14,062 (41.9) | 4,457 (46.4) | 864 (55.5) | 3,914 (54.6) | 25,723 (43.9) | 9,235 (49.4) | 0.27 |
Abbreviations: MiRS = Migraine-Related Stigma; SMD = standardized mean difference.
Minimizing burden/secondary gain/both often/very often column reflects the mean (SD) or percentage when combining the individual columns of minimizing burden often/very often, secondary gain often/very often, and both often/very often.
See eTable 2 (links.lww.com/WNL/D342) for full variable description.
All comparisons were significant p < 0.001.
Table 2.
Migraine-Related Characteristics/Outcomes and Clinical Characteristics by MiRS Group (n = 59,001),a as a Percentage of All Respondents
| MiRS group | Minimizing burden/secondary gain/both often/very often (N = 18,708; 31.7%) | SMD Minimizing burden/secondary gain/both often/very often vs never |
||||||
| Never (N = 6,715; 11.4%) | Rarely/sometimes (N = 33,578; 56.9%) | Minimizing burden Often/very often (N = 9,987; 16.9%) |
Secondary gain Often/very often (N = 1,556; 2.6%) |
Both often/very often (N = 7,165; 12.1%) | Total (N = 59,001) | |||
| Migraine-related characteristics/outcomes | ||||||||
| Monthly headache days, n (%)b | ||||||||
| 0–3 | 4,807 (71.6) | 21,112 (62.9) | 4,779 (47.9) | 914 (58.7) | 3,164 (44.2) | 34,776 (58.9) | 8,857 (47.3) | 0.51 |
| 4–7 | 966 (14.4) | 6,363 (18.9) | 2,312 (23.2) | 327 (21.0) | 1,592 (22.2) | 11,560 (19.6) | 4,231 (22.6) | 0.21 |
| 8–14 | 479 (7.1) | 3,218 (9.6) | 1,400 (14.0) | 164 (10.5) | 1,022 (14.3) | 6,283 (10.6) | 2,586 (13.8) | 0.22 |
| 15+ | 463 (6.9) | 2,885 (8.6) | 1,496 (15.0) | 151 (9.7) | 1,387 (19.4) | 6,382 (10.8) | 3,034 (16.2) | 0.29 |
| MIDAS, n (%)b | ||||||||
| Little or no disability (score = 0–5) | 4,703 (70.0) | 14,819 (44.1) | 2,241 (22.4) | 307 (19.7) | 848 (11.8) | 22,918 (38.8) | 3,396 (18.2) | 1.23 |
| Mild disability (score = 6–10) | 767 (11.4) | 6,201 (18.5) | 1,714 (17.2) | 248 (15.9) | 950 (13.3) | 9,880 (16.7) | 2,912 (15.6) | 0.12 |
| Moderate disability (score = 11–20) | 582 (8.7) | 5,794 (17.3) | 2,213 (22.2) | 376 (24.2) | 1,545 (21.6) | 10,510 (17.8) | 4,134 (22.1) | 0.38 |
| Severe disability (score = 21+) | 663 (9.9) | 6,764 (20.1) | 3,819 (38.2) | 625 (40.2) | 3,822 (53.3) | 15,693 (26.6) | 8,266 (44.2) | 0.84 |
| MIBS-4, n (%)b | ||||||||
| No interictal burden (score = 0) | 4,224 (62.9) | 10,998 (32.8) | 1,839 (18.4) | 69 (4.4) | 339 (4.7) | 17,469 (29.6) | 2,247 (12.0) | 1.24 |
| Mild interictal burden (score = 1–2) | 1,088 (16.2) | 6,481 (19.3) | 1,736 (17.4) | 88 (5.7) | 409 (5.7) | 9,802 (16.6) | 2,233 (11.9) | 0.12 |
| Moderate interictal burden (score = 3–4) | 648 (9.6) | 5,328 (15.9) | 1,804 (18.1) | 119 (7.6) | 707 (9.9) | 8,606 (14.6) | 2,630 (14.1) | 0.14 |
| Severe interictal burden (score = 5+) | 755 (11.2) | 10,771 (32.1) | 4,608 (46.1) | 1,280 (82.3) | 5,710 (79.7) | 23,124 (39.2) | 11,598 (62.0) | 1.24 |
| MSQ-RFR, mean (SD) | 68.7 (24.5) | 58.0 (21.8) | 45.5 (21.7) | 43.2 (18.8) | 34.8 (20.2) | 53.9 (23.9) | 41.2 (21.5) | 1.20 |
| Clinical characteristics | ||||||||
| BMI group, n (%)b | ||||||||
| Underweight/normal | 2,284 (34.0) | 11,699 (34.8) | 3,400 (34.0) | 600 (38.6) | 2,524 (35.2) | 20,507 (34.8) | 6,524 (34.9) | 0.02 |
| Overweight | 1,859 (27.7) | 9,115 (27.1) | 2,564 (25.7) | 374 (24.0) | 1,740 (24.3) | 15,652 (26.5) | 4,678 (25.0) | 0.06 |
| Obese | 2,141 (31.9) | 11,118 (33.1) | 3,642 (36.5) | 481 (30.9) | 2,549 (35.6) | 19,931 (33.8) | 6,672 (35.7) | 0.08 |
| No answer | 431 (6.4) | 1,646 (4.9) | 381 (3.8) | 101 (6.5) | 352 (4.9) | 2,911 (4.9) | 834 (4.5) | 0.09 |
| Total comorbidities, mean (SD)b | 3.0 (2.7) | 3.6 (2.9) | 4.2 (3.1) | 4.6 (3.6) | 5.1 (3.4) | 3.8 (3.1) | 4.6 (3.3) | 0.52 |
| PHQ-4, mean (SD)b | 2.6 (3.1) | 3.9 (3.2) | 5.4 (3.4) | 6.1 (3.1) | 7.0 (3.3) | 4.5 (3.5) | 6.1 (3.4) | 1.00 |
Abbreviations: BMI = body mass index; MIDAS = Migraine Disability Assessment; MIBS-4 = Migraine Interictal Burden Scale-4; MiRS = Migraine-Related Stigma; MSQ-RFR = Migraine Specific Quality of Life v2.1 Role Function-Restrictive; SMD = standardized mean difference.
Minimizing burden/secondary gain/both often/very often column reflects the mean (SD) or percentage when combining the individual columns of minimizing burden often/very often, secondary gain often/very often, and both often/very often.
See eTable 2 (links.lww.com/WNL/D342) for full variable description.
All comparisons were significant p < 0.001.
Figure 1. MiRS Group by Monthly Headache Day Category (n = 59,001).
MiRS = Migraine-Related Stigma.
Sociodemographic and Clinical Measures
Nearly all sociodemographic and clinical measures differed significantly among MiRS groups (Tables 1 and 2). Of note, respondents reporting MiRS-MB/MiRS-SG/MiRS-Both often/very often (vs MiRS-Never) were younger age (38.0 vs 44.7 years, SMD 0.46), more likely to have children younger than 18 years (49.4% vs 36.1%, SMD 0.27), more monthly headache days (e.g., 15+ monthly headache days 16.2% vs 6.9%, SMD 0.29), more severe migraine-related disability (e.g., Severe MIDAS, 44.2% vs 9.9%, SMD 0.84), higher interictal burden (Severe MIBS-4 62.0% vs 11.2%, SMD 1.24), lower quality of life (MSQ-RFR 41.2 vs, 68.7, SMD 1.2), more comorbidities (4.6 vs 3.0, SMD 0.52), and higher PHQ-4 scores (6.1 vs 2.6, SMD 1.0) (Table 2). As a percentage of respondents of specific groups, MiRS-MB/MiRS-SG/MiRS-Both often/very often was not associated with any specific sociodemographic factor (eTable 3, links.lww.com/WNL/D342). Although most (60.3%, 35,583/59,001) respondents' BMI classified them as overweight/obese, there was not a consistent pattern concerning weight and experiencing more frequent migraine-related stigma (Table 2).
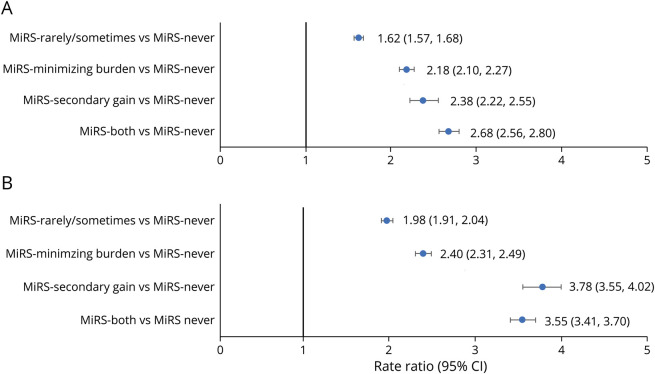
Relationship of MIDAS to MiRS
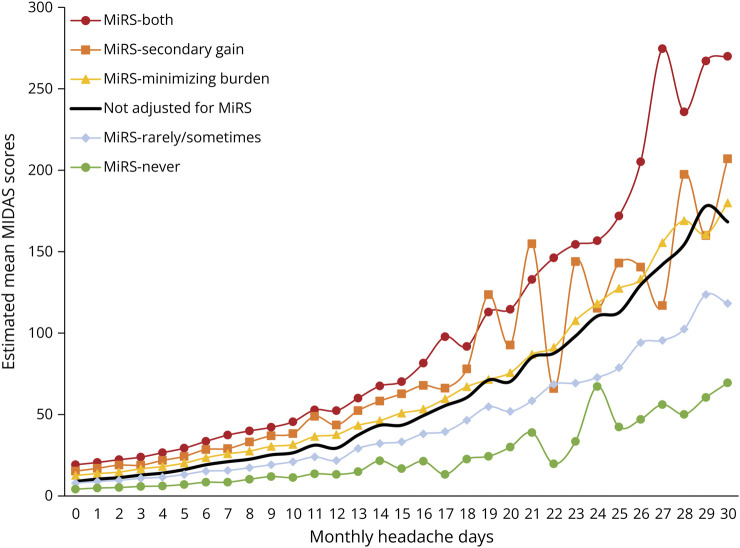
The percentage of individuals with at least moderate disability was higher for those experiencing MiRS often/very often (eFigure 4, links.lww.com/WNL/D342); 74.9% of the MiRS-Both group had moderate or severe disability compared with just 18.6% of the MiRS-Never group. After accounting for sociodemographics, clinical characteristics, and monthly headache days associated with MIDAS total score (eTable 4), the risk of disability was significantly increased for each MiRS group compared with the MiRS-Never group (Figure 2A). For example, the risk more than doubled for the MiRS-Both group (RR 2.68, 95% CI 2.56–2.80) in comparison with the MiRS-Never group. Figure 3 shows estimated MIDAS score increases as stigma and monthly headache days increase. At each monthly headache day, the highest estimated MIDAS score was within the MiRS-Both group and lowest was within the MiRS-Never group.
Figure 2. Likelihood of Increased Migraine-Related Disability and Interictal Burden by MiRS Group.
(A) Likelihood of increased migraine-related disability (MIDAS, rate ratios) by MiRS group (n = 59,001). (B) Likelihood of increased migraine interictal burden (MIBS score) by MiRS group (n = 59,001). Values reflect rate ratio and 95% CI. MIDAS = Migraine Disability Assessment; MIBS-4 = Migraine Interictal Burden Scale; MiRS = Migraine-Related Stigma.
Figure 3. Estimated Mean MIDAS Scores Across Monthly Headache Days (n = 59,001).
The negative binomial regression model was run adjusting for age, sex, race (White, Black, Other Races), ethnicity (Hispanic, Latino/Spanish), metropolitan/micropolitan/rural residence, geographic region (northeast, midwest, south, west), education (high school degree or less, some college, college graduate), marital status (married or living with a partner vs no), children younger than 18 years living at home (yes vs no), income, health insurance (yes vs no), employment (full time, part-time, homemaker, retired, other), BMI (normal/underweight, overweight, obese), sum of self-reported comorbidities (0–26 total), PHQ-4 total score (range 0–12), and monthly headache day frequency. BMI = body mass index; MIDAS = Migraine Disability Assessment; MiRS = Migraine-Related Stigma; PHQ-4 = Patient Health Questionnaire.
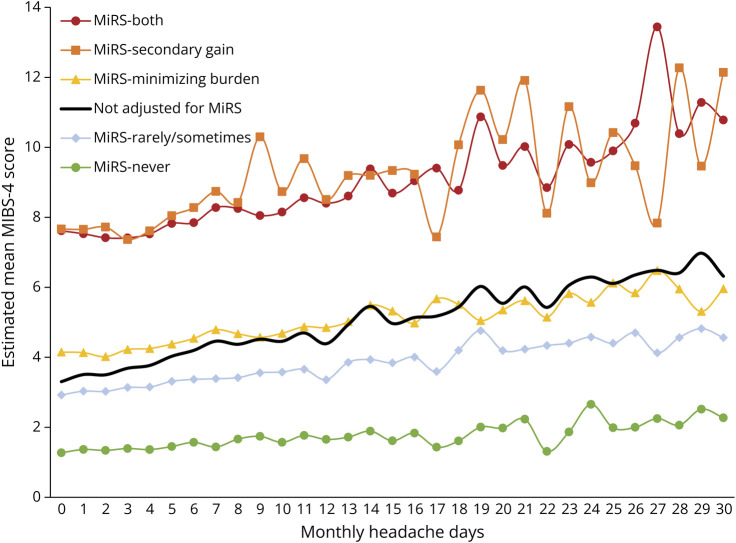
Relationship of MIBS-4 to MiRS
The percentage of individuals with at least moderate interictal burden was higher for those experiencing MiRS often/very often (eFigure 5, links.lww.com/WNL/D342); 79.7% of the MiRS-Both group had severe interictal burden compared with 11.2% of the MiRS-Never group. After accounting for sociodemographics, clinical characteristics, and monthly headache day frequency associated with MIBS-4 total score (eTable 5), the risk of increased burden of migraine between attacks was significant for each MiRS group compared with the MiRS-Never group (Figure 2B), and the risk more than tripled for the MiRS-Both group (RR 3.55, 95% CI 3.41–3.70). The highest estimated MIBS-4 score at nearly every monthly headache day was similar for the MiRS-Secondary Gain and MiRS-Both groups, and lowest at each monthly headache day was within the MiRS-Never group (Figure 4). The estimated MIBS-4 score difference was relatively consistent across monthly headache days.
Figure 4. Estimated Mean MIBS-4 Scores Across Monthly Headache Days (n = 59,001).
The negative binomial regression model was run adjusting for age, sex, race (White, Black, Other Races), ethnicity (Hispanic, Latino/Spanish), metropolitan/micropolitan/rural residence, geographic region (northeast, midwest, south, west), education (high school degree or less, some college, college graduate), marital status (married or living with a partner vs no), children younger than 18 years living at home (yes vs no), income, health insurance (yes vs no), employment (full-time, part-time, homemaker, retired, other), BMI category (normal/underweight, overweight, obese), sum of self-reported comorbidities (0–26 total), PHQ-4 total score (range 0–12), and monthly headache day frequency. BMI = body mass index; MIBS-4 = Migraine Interictal Burden Scale-4; MiRS = Migraine-Related Stigma; PHQ-4 = Patient Health Questionnaire.
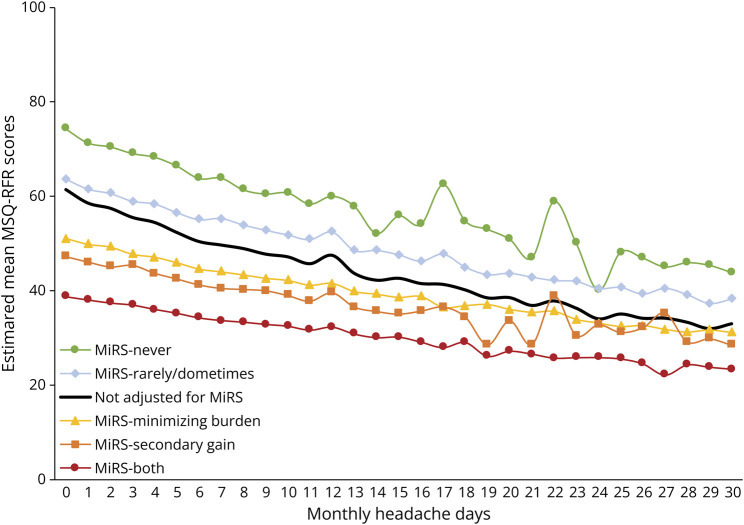
Relationship of MSQ-RFR to MiRS
The individual's quality of life/ability to function in life roles was poorer because individuals experienced MiRS more frequently (Table 2). After accounting for sociodemographics, clinical characteristics, and monthly headache day frequency associated with MSQ-RFR (eTable 6, links.lww.com/WNL/D342), the likelihood of experiencing better MSQ-RFR was significantly less for each MiRS group compared with the MiRS-Never group; MiRS-Rarely/Sometimes (RR 0.90, 95% CI 0.89–0.91), MiRS-Minimizing Burden (RR 0.77, 95% CI 0.75–0.78), MiRS-Secondary Gain (RR 0.74, 95% CI 0.71–0.76), MiRS-Both (RR 0.63, 95% CI 0.61–0.64). The poorest estimated role function–related quality of life score at every monthly headache day was within the MiRS-Both group and best nearly every day within the MiRS-Never group (Figure 5). The estimated MSQ-RFR score difference decreased as monthly headache day frequency increased.
Figure 5. Estimated Functional Impact of Migraine (MSQ-RFR Score) Across Monthly Headache Days (n = 59,001).
The negative binomial regression model was run adjusting for age, sex, race (White, Black, Other Races), ethnicity (Hispanic, Latino/Spanish), metropolitan/micropolitan/rural residence, geographic region (northeast, midwest, south, west), education (high school degree or less, some college, college graduate), marital status (married or living with a partner vs no), children younger than 18 years living at home (yes vs no), income, health insurance (yes vs no), employment (full-time, part-time, homemaker, retired, other), BMI (normal/underweight, overweight, obese), sum of self-reported comorbidities (0–26 total), PHQ-4 total score (range 0–12), and monthly headache day frequency. BMI = body mass index; MSQ-RFR = Migraine Specific Quality of Life v2.1 Role Function-Restrictive; MiRS = Migraine-Related Stigma; PHQ-4 = Patient Health Questionnaire.
Discussion
OVERCOME (US) is the first population-based examination of migraine-related stigma. We evaluated nearly 60,000 adults living with migraine in the United States, selected to be representative of the US population, across the full spectrum of headache frequency. The MiRS questionnaire was developed and validated for this project.22 MiRS includes 2 psychometrically robust subscales and has high internal consistency, reliability, and strong external validity, based on the association of MiRS group with previously validated patient-reported outcomes. The Secondary Gain subscale primarily reflects the respondents' feeling that others viewed them as using migraine to obtain something undeserved (e.g., attention, medication) or evade responsibilities (e.g., work/family/social commitments). The Minimizing Burden factor primarily reflects the respondents' feeling that others viewed migraine pain, symptoms, and burden as unworthy. That is, Secondary Gain may be thought of stigma toward an individual with a disease, whereas Minimizing Burden may be thought of stigma toward a disease that an individual is living with. Though correlated (r = 0.66), these factors reflect distinct aspects of stigma. Importantly, the current analysis demonstrated that migraine-related stigma is associated with increased disability, greater burden between attacks, and reduced quality of life in the role function domain.
Nearly one-third (31.7%) of respondents reported that they experience at least 1 type of migraine-related stigma often or very often; 14.8% experienced secondary gain stigma often/very often, and 29.1% reported others minimizing their disease burden often/very often. Moreover, those with 8–14 (41.2%) or ≥15 (47.5%) monthly headache days were more likely to report at least 1 form of stigma often/very often than those with <4 monthly headache days (25.5%). Providers may want to be alert to stigma as a contributor to disease burden for patients with migraine presenting with frequent monthly headache days, particularly in light of a recent clinic-based study finding correlations between stigma (measured by Stigma Scale for Chronic Illnesses 8-item version) and MIDAS.10,16,17 However, the finding that 25.5% of those with <4 monthly headache days were experiencing migraine-related stigma often/very often is a reminder that considering monthly headache day frequency alone may be inadequate when assessing the full impact of migraine or the presence of stigma.
Disease-related stigma is common among other diseases considered concealable or invisible (e.g., chronic pain, mental health14,28,29) in that they cannot be objectively detected by medical tests (e.g., blood tests, EEG, or MRI) or by externally observable clinical signs. Concealable diseases often elicit societal stereotypes (aka, “public stigma”).28,30 For example, people with invisible diseases may be viewed as less able to cope with pain and/or the stressors of daily life. Indeed, minimizing burden was the more commonly reported aspect of migraine-related stigma in this study. As many as 90% of all people experience headache in their lifetime, and 16% experience headache on any given day; most people with headaches do not experience high levels of disability.31 People with less severe headache might develop stigmatizing attitudes toward those with a more severe and disabling form of headache.3,4 Those who experience migraine interictal burden may be especially prone to experiencing stigma because people typically seem completely well between attacks and are expected to function normally. People with interictal burden may have lingering symptoms as well as anxiety and fear of making plans and commitments. Because lifestyle factors can contribute to migraine control, people with migraine may blame themselves or be blamed by others if work stress, sleep dysregulation, missed meals, alcohol consumption, or other factors contribute to headache onset. Because migraine is not externally visible and has significant impact on role function,19,20 it is not surprising that societal stereotypes about migraine may promote the view that migraine is being used to avoid responsibilities and/or not participate in life roles/functions.32 Although one might propose that exposure and direct interactions between people without migraine with people with migraine could be an effective antidote to these stereotypes, studies of a nonmigraine cohort of OVERCOME (US) suggest those who know multiple people with migraine tend to hold more stigmatizing attitudes toward people with migraine.32 Moreover, there is evidence that migraine is considered a nonprestigious neurologic disease among physicians,33,34 and it is possible that a provider's attitude toward migraine could lead them to devalue the treatment needs of the individual presenting with burdensome migraine.
Those experiencing migraine-related stigma reported higher rates of at least moderate disability (74.9% of those experiencing both Secondary Gain and Minimizing Burden stigma often/very often had a MIDAS score ≥11 vs 18.6% among those never experiencing stigma), severe interictal burden (79.7% of those experiencing both often/very often had a MIBS-4 score ≥5 vs 11.2% among those never experiencing stigma), and poorer quality of life (MSQ-RFR mean score of 34.8 among those experiencing both often/very often vs 68.7 among those never experiencing stigma). In addition, as hypothesized, these findings remained even when accounting for sociodemographics, clinical characteristics, and monthly headache day frequency such that the risk for a higher MIDAS score more than doubled among those experiencing both aspects of stigma often/very often relative to those never experiencing stigma. Similarly, the risk of a higher MIBS-4 score more than tripled when the same groups were contrasted. For all 3 outcomes, the poorest estimated outcomes at every monthly headache day frequency were for those experiencing migraine-related stigma often/very often. The magnitude of these effects is sobering. For example, respondents who experience both minimizing burden and secondary gain migraine-related stigma often/very often and report <5 monthly headache days had lower MSQ-RFR (i.e., worse estimated quality of life) scores (estimated range 36.1–38.8) than those who never experience migraine-related stigma and report >25 monthly headache days (estimated range 43.9–46.9). That is, the social context of migraine may have a greater impact on quality of life than the number of monthly headache days.
This study identified omnibus differences in migraine-related stigma across sociodemographic and clinical characteristics (e.g., age, monthly headache day frequency, MIDAS, MIBS-4, MSQ-RFR, number of comorbidities, PHQ-4) generally consistent with previous findings.8,16,35,36 Consistent with previous studies,10,16,35 we did not identify sex differences in stigma, although it has been argued that migraine is stigmatized, in part, because it is more common in women.37 Perhaps the perception that migraine is a women's disease could increase migraine-related stigma among men without migraine.38 In this study, stigma often/very often was also not associated with race, ethnicity, education, or employment. Additional work is required to understand the interaction of sociodemographic, cultural, and clinical factors with migraine-related stigma. That is, other categorical discriminatory attitudes (e.g., toward race, sex, ethnicity, etc.) undoubtedly can co-occur with migraine-related stigma potentially leading to emergent and unappreciated intersectional effects.
Previous work has shown that experiencing stigma is associated with poorer outcomes across diseases.28,39 This is particularly true for those living with mood/anxiety disorders,14,29,40 common migraine comorbidities.41,42 In this study, we controlled for anxiety and depression (PHQ-4) because previous research has demonstrated an independent and combined impact of these disorders on migraine disability and quality of life.43,44 PHQ-4 scores were highest in the MiRS-Both group in this study. We also did not find that BMI was associated with migraine-related stigma. Furthermore, the relative magnitude of stigma toward migraine may be greater than that toward many comparator diseases35,45; migraine may be the most stigmatized of neurologic diseases.46 Moreover, people with migraine and comorbid disorders are likely simultaneously contending with stigma toward multiple diseases, thereby potentially creating a stigma syndemic47 that may magnify their collective impacts on the individual.
Given the current findings, clinical and public health policy considerations are warranted. The current finding that more frequent monthly headache days was associated with experiencing migraine-related stigma more often provides additional impetus to recommend migraine preventive treatments early in the course of migraine progression. Multiple US population–based studies of migraine have shown a significant clinical care gap in that many people eligible for preventive treatment never receive it or discontinue it.18,20,48 Behavioral interventions indicated for migraine prevention (e.g., cognitive behavioral therapies, mindfulness-based therapies) may provide additional benefit for those experiencing stigma. Moreover, providers can play a role in reducing migraine-related stigma by discussing migraine's impact beyond only assessing the “number of days” of headache pain and associated symptoms during a visit for migraine and ensure that federal Americans with Disabilities Act accommodations and Family and Medical Leave Act benefits are supported across workplaces and IDEA benefits across schools when appropriate.
Although it is possible that migraine prevention may reduce migraine-related stigma, the current cross-sectional study cannot infer any impact of reduction of headache frequency on stigma. It is conceivable that migraine stigma becomes a refractory personal identity once established, comparable with some other diseases (e.g., “survivors” of cancer, “recovering addicts” for substance use disorders). Moreover, hiding the presence of migraine during social interactions may entrench its stigma,40 yet publicly acknowledging and disclosing the myriad impacts of migraine, including with health care providers, may seem daunting. However, it is possible that connecting with others with migraine, including active involvement in advocacy efforts, may unmask and defang enacted migraine-related stigma and stereotypes.
OVERCOME (US) used quota sampling rather than random sampling to create a demographically representative sample. The requirement for internet access and the modest participation rate could lead to differential exclusion of the most severely affected individuals. Requiring individuals be able to read/write English limits the generalizability of results; it is possible that being unable to communicate in English could contribute to experiencing migraine-related stigma. Individuals were required to complete the entire survey to be counted in the cohort, and this may have introduced further participation bias and nonrandom missingness of data. Survey data were self-reported and thus may be susceptible to recall bias.
In the absence of a migraine-specific stigma questionnaire, we developed a novel one using a validation process outlined in the Methods section and in a separate report. Consequently, we cannot directly compare migraine-related stigma with other disease states. In addition, this measure of migraine-related stigma was specifically developed to assess how often people experience migraine-related stigmatizing attitudes/words/behaviors from others; it was not designed to capture the entirety of constructs that surround stigma (e.g., alienation, stereotype endorsement, perceived discrimination, social withdrawal, stigma resistance). Further research is required to determine how the current measure is associated with other measures of stigma.14 Although our 2-factor model is supported psychometrically, alternative scoring procedures are possible. With the exception of the “never” category, scores range within a category (particularly “rarely/sometimes”) indicating some variance in the experience of stigma within categories. The cross-sectional nature of the current analyses limits comments regarding questionnaire reproducibility or inferring potential unidirectional or bidirectional causal relationships between health outcomes and stigma. Longitudinal studies and mechanistic explorations will be next steps to identify opportunities for improving patients' lives by reducing the burden of migraine stigma.
Strategies aimed at mitigating migraine-related stigma at a public health level may yield benefits because stigmatizing attitudes toward those with migraine may collectively lead to inequitable policies of public institutions (structural stigma). For example, migraine has consistently been among the least funded research areas by the NIH, among the most burdensome diseases, despite persistent advocacy efforts to reduce this disparity.8,9 Research examining where and how stigma are most likely to occur may allow for narrowcast messaging for cost-effective allocation of public health resources. Other potential means for changing the public's perception of migraine have been elaborated elsewhere.8,9,37,49
Specific assessment of migraine-related stigma in the workplace could be especially informative,8,16,35,50 including evaluating relationships between migraine-related stigma and presenteeism or seeking workplace accommodations. Research is needed to clarify which sociodemographic, clinical, interpersonal, and previous life experiences of migraine-related loss may be most associated with experiencing migraine-related stigma. Future studies should also evaluate potential migraine-related stigma influences on migraine-related care seeking, diagnosis, and treatment delivery and response.
The current population-based study of nearly 60,000 people with migraine found more than 30% report experiencing migraine-related stigma often or very often, either in the form of others minimizing the burden of migraine or others believing they are using migraine for secondary gain. After controlling for sociodemographics, clinical characteristics, and monthly headache days, this study found experiencing migraine-related stigma more often was associated with increased disability and interictal burden and reduced quality of life across all frequencies of monthly headache days. Scientific, clinical, and public health efforts to better understand and address migraine-related stigma are warranted. In particular, clarifying the mechanisms that link stigma to health outcomes could set the stage for interventions that may reduce the burdens of migraine across the full spectrum of headache frequency.
Glossary
- BMI
body mass index
- ICHD-3
International Classification of Headache Disorders, 3rd edition
- IRB
Institutional Review Board
- MIBS-4
Migraine Interictal Burden Scale-4
- MIDAS
Migraine Disability Assessment
- MiRS
Migraine-Related Stigma
- MSQ-RFR
Migraine Specific Quality of Life, Role Function-Restrictive
- OVERCOME
ObserVational survey of the Epidemiology, tReatment and Care Of MigrainE
- PHQ-4
Patient Health Questionnaire-4
- RR
rate ratio
- SMD
standardized mean difference
Appendix. Authors
| Name | Location | Contribution |
| Robert E. Shapiro, MD, PhD | Larner College of Medicine, University of Vermont, Burlington | Drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; study concept or design; analysis or interpretation of data |
| Robert A. Nicholson, PhD | Eli Lilly and Company, Indianapolis, IN | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design; analysis or interpretation of data |
| Elizabeth K. Seng, PhD | Yeshiva University, New York, NY | Drafting/revision of the manuscript for content, including medical writing for content; analysis or interpretation of data |
| Dawn C. Buse, PhD | Albert Einstein College of Medicine, Montefiore Medical Center, Bronx, NY | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design; analysis or interpretation of data |
| Michael L. Reed, PhD | Vedanta Research, Chapel Hill, NC | Drafting/revision of the manuscript for content, including medical writing for content; major role in the acquisition of data; study concept or design; analysis or interpretation of data |
| Anthony J. Zagar, MS | Eli Lilly and Company, Indianapolis, IN | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design; analysis or interpretation of data |
| Sait Ashina, MD | Harvard Medical School, Beth Israel Deaconess Medical Center, Boston, MA | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design; analysis or interpretation of data |
| E. Jolanda Muenzel, MD, PhD | Eli Lilly and Company, Indianapolis, IN | Drafting/revision of the manuscript for content, including medical writing for content; analysis or interpretation of data |
| Susan Hutchinson, MD | Orange County Migraine and Headache Center, Irvine, CA | Drafting/revision of the manuscript for content, including medical writing for content; analysis or interpretation of data |
| Eric M. Pearlman, MD, PhD | Eli Lilly and Company, Indianapolis, IN | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design; analysis or interpretation of data |
| Richard B. Lipton, MD | Albert Einstein College of Medicine, Montefiore Medical Center, Bronx, NY | Drafting/revision of the manuscript for content, including medical writing for content; study concept or design; analysis or interpretation of data |
Footnotes
Editorial, page e209192
Study Funding
This study was funded by Eli Lilly & Company, Indianapolis, IN.
Disclosure
R.E. Shapiro serves as consultant, advisory board member, or has received honoraria or research support from Eli Lilly and Company, Lundbeck, and Theranica. R.A. Nicholson is an employee and minor stockholder of Eli Lilly and Company. E.K. Seng has consulted or served on an advisory board for GlaxoSmithKline, Click Therapeutics, and Abbvie and received research funding from the National Institute of Neurological Disorders and Stroke (NS096107 PI: Seng), NCCIH (R01AT011005-01A1 MPIs: Seng and Shallcross), and the Veteran's Health Administration (the Headache Center of Excellence Research and Evaluation Center and VA HSR&D, IRP 20-002 PI: Damush). D.C. Buse has received research support from the FDA and the National Headache Foundation. She serves as consultant, advisory board member, or has received honoraria or research support from AbbVie/Allergan, Amgen, Biohaven, Collegium, Eli Lilly and Company, Lundbeck, Novartis, and Teva. M.L. Reed has received research support from the National Headache Foundation. He serves as consultant, advisory board member, or has received honoraria or research support from Abbvie/Allergan, Amgen, Dr. Reddy's Laboratories (Promius), and Eli Lilly and Company. A.J. Zagar, MS, is an employee and minor stockholder of Eli Lilly and Company. S. Ashina consulting, teaching, honoraria: Allergan, Amgen, Biohaven Pharmaceuticals, Eli Lilly and Company, Impel NeuroPharma, Novartis, Satsuma, Supernus, Percept, and Theranica. E.J. Muenzel is an employee and minor stockholder of Eli Lilly and Company. S. Hutchinson consulting, speaking, honoraria from Alder/Lundbeck, AbbVie/Allergan, Amgen, Biohaven, Currax, electroCore, Eli Lilly and Company, Impel, Novartis, Teva, Theranica, and Upsher-Smith. E.M. Pearlman is an employee and minor stockholder of Eli Lilly and Company. R.B. Lipton has received research support from the NIH, the FDA, and the National Headache Foundation. He serves as consultant, advisory board member, or has received honoraria or research support from AbbVie/Allergan, Amgen, Biohaven, Dr. Reddy's Laboratories (Promius), electroCore, Eli Lilly and Company, GlaxoSmithKline, Lundbeck, Manistee, Novartis, Teva, Vector, and Vedanta Research. He receives royalties from Wolff's Headache, 8th edition (Oxford University Press, 2009) and Informa. He holds stock/options in Biohaven and Manistee. Go to Neurology.org/N for full disclosures.
References
- 1.Burch RC, Buse DC, Lipton RB. Migraine: epidemiology, burden, and comorbidity. Neurol Clin. 2019;37(4):631-649. doi: 10.1016/j.ncl.2019.06.001 [DOI] [PubMed] [Google Scholar]
- 2.Steiner TJ, Stovner LJ, Jensen R, Uluduz D, Katsarava Z; Lifting The Burden: the Global Campaign against Headache. Migraine remains second among the world's causes of disability, and first among young women: findings from GBD2019. J Headache Pain. 2020;21(1):137. doi: 10.1186/s10194-020-01208-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buse DC, Rupnow MFT, Lipton RB. Assessing and managing all aspects of migraine: migraine attacks, migraine-related functional impairment, common comorbidities, and quality of life. Mayo Clin Proc. 2009;84(5):422-435. doi: 10.1016/S0025-6196(11)60561-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buse DC, Fanning KM, Reed ML, et al. Life with migraine: effects on relationships, career, and finances from the Chronic Migraine Epidemiology and Outcomes (CaMEO) study. Headache. 2019;59(8):1286-1299. doi: 10.1111/head.13613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stewart WF, Wood GC, Manack A, Varon SF, Buse DC, Lipton RB. Employment and work impact of chronic migraine and episodic migraine. J Occup Environ Med. 2010;52(1):8-14. doi: 10.1097/JOM.0b013e3181c1dc56 [DOI] [PubMed] [Google Scholar]
- 6.Molina Y, Choi SW, Cella D, Rao D. The Stigma Scale for Chronic Illnesses 8-item version (SSCI-8): development, validation and use across neurological conditions. Int J Behav Med. 2013;20(3):450-460. doi: 10.1007/s12529-012-9243-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goffman E. Stigma and social identity. In: Stigma: Notes on the Management of Spoiled Identity. Prentice-Hall Inc.; 1963. [Google Scholar]
- 8.Parikh SK, Kempner J, Young WB. Stigma and migraine: developing effective interventions. Curr Pain Headache Rep. 2021;25(11):75. doi: 10.1007/s11916-021-00982-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shapiro RE. What will it take to move the needle for headache disorders? An advocacy perspective. Headache. 2020;60(9):2059-2077. doi: 10.1111/head.13913 [DOI] [PubMed] [Google Scholar]
- 10.Seng EK, Shapiro RE, Buse DC, Robbins MS, Lipton RB, Parker A. The unique role of stigma in migraine-related disability and quality of life. Headache. 2022;62(10):1354-1364. doi: 10.1111/head.14401 [DOI] [PubMed] [Google Scholar]
- 11.Jacoby A. Felt versus enacted stigma: a concept revisited. Evidence from a study of people with epilepsy in remission. Soc Sci Med. 1994;38(2):269-274. doi: 10.1016/0277-9536(94)90396-4 [DOI] [PubMed] [Google Scholar]
- 12.Scambler G, Hopkins A. Being epileptic: coming to terms with stigma. Sociol Health Illness. 2008;8(1):26-43. doi: 10.1111/1467-9566.ep11346455 [DOI] [Google Scholar]
- 13.Pachankis JE, Hatzenbuehler ML, Wang K, et al. The burden of stigma on health and well-being: a taxonomy of concealment, course, disruptiveness, aesthetics, origin, and peril across 93 stigmas. Pers Soc Psychol Bull. 2018;44(4):451-474. doi: 10.1177/0146167217741313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc Sci Med. 2010;71(12):2150-2161. doi: 10.1016/j.socscimed.2010.09.030 [DOI] [PubMed] [Google Scholar]
- 15.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring). 2009;17(5):941-964. doi: 10.1038/oby.2008.636 [DOI] [PubMed] [Google Scholar]
- 16.Young WB, Park JE, Tian IX, Kempner J. The stigma of migraine. PLoS One. 2013;8(1):e54074. doi: 10.1371/journal.pone.0054074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martínez-Fernández A, Rueda Vega M, Quintas S, et al. Psychosocial repercussion of migraine: is it a stigmatized disease? Neurol Sci. 2020;41(8):2207-2213. doi: 10.1007/s10072-020-04332-6 [DOI] [PubMed] [Google Scholar]
- 18.Lipton RB, Nicholson RA, Reed ML, et al. Diagnosis, consultation, treatment, and impact of migraine in the US: results of the OVERCOME (US) study. Headache. 2022;62(2):122-140. doi: 10.1111/head.14259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache. 2001;41(7):646-657. doi: 10.1046/j.1526-4610.2001.041007646.x [DOI] [PubMed] [Google Scholar]
- 20.Lipton RB, Bigal ME, Diamond M, et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68(5):343-349. doi: 10.1212/01.wnl.0000252808.97649.21 [DOI] [PubMed] [Google Scholar]
- 21.Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38(1):1-211. doi: 10.1177/0333102417738202 [DOI] [PubMed] [Google Scholar]
- 22.Shapiro RE, Nicholson RA, Zagar AJ, et al. Identifying factors pertaining to migraine-related stigma from a novel question set: results of the OVERCOME (US) study (S4.001). Neurology 2022;98(18 suppl):2997. doi: 10.1212/wnl.98.18_supplement.2997 [DOI] [Google Scholar]
- 23.Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the Migraine Disability Assessment (MIDAS) Questionnaire to assess headache-related disability. Neurology. 2001;56(6 suppl 1): S20-S28. doi: 10.1212/wnl.56.suppl_1.s20 [DOI] [PubMed] [Google Scholar]
- 24.Buse D, Bigal MB, Rupnow M, Reed ML, Serrano D, Lipton R. Development and validation of the Migraine Interictal Burden Scale (MIBS): a self-administered instrument for measuring the burden of migraine between attacks. Neurology. 2007;68:A89. [Google Scholar]
- 25.Jhingran P, Osterhaus JT, Miller DW, Lee JT, Kirchdoerfer L. Development and validation of the migraine-specific quality of life questionnaire. Headache. 1998;38(4):295-302. doi: 10.1046/j.1526-4610.1998.3804295.x [DOI] [PubMed] [Google Scholar]
- 26.Speck RM, Shalhoub H, Wyrwich KW, et al. Psychometric validation of the role function restrictive domain of the Migraine Specific Quality-of-Life Questionnaire Version 2.1 electronic patient-reported outcome in patients with episodic and chronic migraine. Headache. 2019;59(5):756-774. doi: 10.1111/head.13497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Löwe B, Wahl I, Rose M, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122(1-2):86-95. doi: 10.1016/j.jad.2009.06.019 [DOI] [PubMed] [Google Scholar]
- 28.De Ruddere L, Craig KD. Understanding stigma and chronic pain: a-state-of-the-art review. Pain. 2016;157(8):1607-1610. doi: 10.1097/j.pain.0000000000000512 [DOI] [PubMed] [Google Scholar]
- 29.Curcio C, Corboy D. Stigma and anxiety disorders: a systematic review. Stigma and Health. 2020;5(2):125-137. doi: 10.1037/sah0000183 [DOI] [Google Scholar]
- 30.Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27(1):363-385. doi: 10.1146/annurev.soc.27.1.363 [DOI] [Google Scholar]
- 31.Stovner LJ, Hagen K, Linde M, Steiner TJ. The global prevalence of headache: an update, with analysis of the influences of methodological factors on prevalence estimates. J Headache Pain 2022;23(1):34. doi: 10.1186/s10194-022-01402-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shapiro RE, Araujo AB, Nicholson RA, et al. Stigmatizing attitudes about migraine by people without migraine: results of the OVERCOME study. Headache. 2019. 59(suppl 1):14-16. [Google Scholar]
- 33.Kristoffersen ES, Winsvold BS, Faiz KW. Prestige of neurological disorders among future neurologists in Norway. Acta Neurol Scand. 2019;139(6):555-558. doi: 10.1111/ane.13087 [DOI] [PubMed] [Google Scholar]
- 34.Robbins MS, Rosen NL. Headache interest in academic neurology leadership: a cross-sectional study. Headache 2018;58(1):102-108. doi: 10.1111/head.13186 [DOI] [PubMed] [Google Scholar]
- 35.Shapiro RE, Lipton R, Reiner P, Reiner PB. EHMTI-0313. Factors influencing stigma towards persons with migraine. J Headache Pain. 2014;15(suppl 1):E36. doi: 10.1186/1129-2377-15-s1-e36 [DOI] [Google Scholar]
- 36.Parikh SK, Young WB. Migraine: stigma in society. Curr Pain Headache Rep. 2019;23(1):8. doi: 10.1007/s11916-019-0743-7 [DOI] [PubMed] [Google Scholar]
- 37.Kempner J. What biology can't do. Headache. 2016;56(6):1047-1052. doi: 10.1111/head.12854 [DOI] [PubMed] [Google Scholar]
- 38.Shapiro RE, Fitz NS, Lipton RB, Reiner PB. Socio-demographic and individual characteristics associated with stigmatizing attitudes towards people with migraine. Headache. 2015;55:259-260. [Google Scholar]
- 39.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813-821. doi: 10.2105/AJPH.2012.301069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, Rüsch N. Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatr Serv 2012;63(10):963-973. doi: 10.1176/appi.ps.201100529 [DOI] [PubMed] [Google Scholar]
- 41.Minen MT, Begasse De Dhaem O, Kroon Van Diest A, et al. Migraine and its psychiatric comorbidities. J Neurol Neurosurg Psychiatry. 2016;87(7):741-749. doi: 10.1136/jnnp-2015-312233 [DOI] [PubMed] [Google Scholar]
- 42.Seng EK, Seng CD. Understanding migraine and psychiatric comorbidity. Curr Opin Neurol. 2016;29(3):309-313. doi: 10.1097/WCO.0000000000000309 [DOI] [PubMed] [Google Scholar]
- 43.Lipton RB, Seng EK, Chu MK, et al. The effect of psychiatric comorbidities on headache-related disability in migraine: results from the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study. Headache. 2020;60(8):1683-1696. doi: 10.1111/head.13914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lipton RB, Hamelsky SW, Kolodner KB, Steiner TJ, Stewart WF. Migraine, quality of life, and depression: a population-based case-control study. Neurology. 2000;55(5):629-635. doi: 10.1212/wnl.55.5.629 [DOI] [PubMed] [Google Scholar]
- 45.Caspermeyer JJ, Sylvester EJ, Drazkowski JF, Watson GL, Sirven JI. Evaluation of stigmatizing language and medical errors in neurology coverage by US newspapers. Mayo Clin Proc 2006;81(3):300-306. doi: 10.4065/81.3.300 [DOI] [PubMed] [Google Scholar]
- 46.Best RK, Arseniev-Koehler A. Stigma's uneven decline. SocArXiv. 2022. Accessed July 1, 2022. osf.io/preprints/socarxiv/7nm9x/. [Google Scholar]
- 47.Singer M, Bulled N, Ostrach B, Mendenhall E. Syndemics and the biosocial conception of health. Lancet. 2017;389(10072):941-950. doi: 10.1016/S0140-6736(17)30003-X [DOI] [PubMed] [Google Scholar]
- 48.Buse DC, Armand CE, Charleston L IV, et al. Barriers to care in episodic and chronic migraine: results from the Chronic Migraine Epidemiology and Outcomes Study. Headache. 2021;61(4):628-641. doi: 10.1111/head.14103 [DOI] [PubMed] [Google Scholar]
- 49.Gvantseladze K, Do TP, Hansen JM, Shapiro RE, Ashina M. The stereotypical image of a person with migraine according to mass media. Headache. 2020;60(7):1465-1471. doi: 10.1111/head.13846 [DOI] [PubMed] [Google Scholar]
- 50.Burton WN, Landy SH, Downs KE, Runken MC. The impact of migraine and the effect of migraine treatment on workplace productivity in the United States and suggestions for future research. Mayo Clin Proc. 2009;84(5):436-445. doi: 10.1016/S0025-6196(11)60562-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Lilly will provide access to anonymized individual participant data collected during the study. The data will be available to request on vivli.org after the study team has completed analyses and publications. Access will be provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data sharing agreement. After a proposal is approved, data and documents, including the study protocol, will need to be provided in a secure data sharing environment. For details on submitting a request, see the instructions provided at vivli.org.