Abstract
BACKGROUND:
This narrative review aims to explore the current state and future perspective of artificial intelligence (AI) in respiratory care. The objective is to provide insights into the potential impact of AI in this field.
METHODS:
A comprehensive analysis of relevant literature and research studies was conducted to examine the applications of AI in respiratory care and identify areas of advancement. The analysis included studies on remote monitoring, early detection, smart ventilation systems, and collaborative decision-making.
RESULTS:
The obtained results highlight the transformative potential of AI in respiratory care. AI algorithms have shown promising capabilities in enabling tailored treatment plans based on patient-specific data. Remote monitoring using AI-powered devices allows for real-time feedback to health-care providers, enhancing patient care. AI algorithms have also demonstrated the ability to detect respiratory conditions at an early stage, leading to timely interventions and improved outcomes. Moreover, AI can optimize mechanical ventilation through continuous monitoring, enhancing patient comfort and reducing complications. Collaborative AI systems have the potential to augment the expertise of health-care professionals, leading to more accurate diagnoses and effective treatment strategies.
CONCLUSION:
By improving diagnosis, AI has the potential to revolutionize respiratory care, treatment planning, and patient monitoring. While challenges and ethical considerations remain, the transformative impact of AI in this domain cannot be overstated. By leveraging the advancements and insights from this narrative review, health-care professionals and researchers can continue to harness the power of AI to improve patient outcomes and enhance respiratory care practices.
IMPROVEMENTS:
Based on the findings, future research should focus on refining AI algorithms to enhance their accuracy, reliability, and interpretability. In addition, attention should be given to addressing ethical considerations, ensuring data privacy, and establishing regulatory frameworks to govern the responsible implementation of AI in respiratory care.
Keywords: Algorithm, artificial intelligence, datasets, diagnostics, machine learning, patient monitoring, pulmonary medicine, respiratory care, robotics, treatment planning
Threat to validity: Before delving into the background and related work, it is important to address the potential threats to the validity of this narrative review. While efforts were made to ensure a comprehensive search and inclusion of relevant literature, the possibility of omitting certain studies or sources cannot be completely eliminated. In addition, the interpretation and synthesis of the included literature may be subject to individual biases.
To mitigate these threats, a systematic approach was adopted to identify relevant literature. Multiple databases, including PubMed, Scopus, and IEEE, were searched using the following search strings: “artificial intelligence (AI),” “respiratory care,” “diagnostics,” “treatment planning,” and “patient monitoring.” In addition, citation tracking and manual screening of reference lists were performed to identify any additional relevant studies. Despite these efforts, it is important to acknowledge the limitations inherent in the literature search process.
Following the consideration of potential threats to validity, this section provides a comprehensive background on the applications and advancements of AI in the field of respiratory care. It explores the existing literature, research, and developments in AI technology that have been applied to respiratory diagnostics, treatment planning, and patient monitoring.
Millions of people worldwide, including children, adults, and the elderly, are impacted by respiratory disorders, which are a primary cause of morbidity and mortality globally.[1] Respiratory disorders require specialized knowledge and access to cutting-edge technologies for monitoring and treatment.[2] However, given the rapid development of AI, there is a growing interest in its potential uses in respiratory care, such as precise diagnosis, individualized treatment strategies, and improved patient outcomes. By enabling precise diagnosis, individualized treatment strategies, and improved patient outcomes, AI has the potential to revolutionize respiratory medicine.[3]
The field of computer science known as AI, focuses on creating intelligent machines that can carry out tasks that ordinarily need human intelligence. In order to analyze, it makes use of statistical models and algorithms, such as decision trees, support vector machines (SVMs), and neural networks.[4]
The diagnosis and monitoring of respiratory disorders is one of the main applications of AI in respiratory care. Traditional diagnostic techniques frequently rely on the subjective symptom interpretation, physical examinations, and imaging testing. To deliver a more precise and effective diagnosis, AI algorithms may examine enormous amounts of patient data, including medical images, physiological factors, and patient history. AI-enabled software, for instance, can examine medical images such as computed tomography (CT) scans or chest X-rays to look for early indications of lung cancer or other respiratory diseases. AI can assist medical personnel with diagnosing patients more quickly and accurately, enabling prompt interventions and better patient outcomes.[5]
AI also has the potential to transform respiratory monitoring in patients with respiratory disorders such as asthma, chronic obstructive pulmonary disease (COPD), and cystic fibrosis used to need constant observation in a hospital setting. However, as wearable technology has developed, it is now possible to remotely monitor respiratory parameters with the help of AI algorithms. These gadgets, such as smartwatches or portable spirometers, can gather real-time data on a variety of characteristics, including respiratory rate, oxygen saturation (SpO2) levels, and cough frequency. The data can be used to track the progression of a disease, identify early warning signs of an exacerbation, and personalize treatment plans.[6]
AI has the potential to revolutionize respiratory care treatment and therapy in addition to diagnosis and monitoring. AI technologies can be very helpful for personalized medicine, a growing discipline that customizes treatment strategies for particular patients. AI algorithms can analyze patient data to identify patterns that may indicate whether the patient is more likely to respond to a particular treatment. They can also use these data to predict how a patient will respond to a treatment over time including genetic data, medical history, and response to treatment.
This individualized strategy may result in better treatment outcomes, fewer side effects, and higher patient quality of life.[7]
AI can also help optimize ventilation strategies for patients who require mechanical ventilation. Ventilation settings often need to be adjusted continuously based on the patient's condition and response to therapy. AI systems can analyze patient data, such as respiratory metrics, blood gas levels, and lung mechanics, to make recommendations for ventilator changes in real time. This continuous feedback loop can help health-care providers improve patient outcomes, reduce complications, and optimize ventilation techniques.[8]
The collection and analysis of sensitive patient data increase the risk of data breaches and unauthorized access. It is imperative to establish robust data protection protocols and ensure compliance with privacy regulations to maintain patient trust and confidentiality.[9]
Another challenge is the potential for bias and lack of diversity in AI algorithms. If the training data used to develop AI models is not representative of the diverse population, it can lead to biased predictions and decisions. It is crucial to address these biases and ensure fairness in AI algorithms to avoid exacerbating existing health-care disparities.[10]
Related work
Previous research has made significant contributions to the understanding and implementation of AI in health-care settings. In the context of recommendation systems, the article “A Review of Content-Based and Context-Based Recommendation Systems” by Javed et al.[11] provides valuable insights into the different types of recommendation systems and their applications in health care. This work explores the content-based and context-based approaches and their relevance to personalized respiratory care recommendations.
In the realm of medical data analysis, the article “A Comparative Performance Analysis of Data Resampling Methods on Imbalance Medical Data” by Khushi et al.[12] presents a comprehensive analysis of various data resampling methods for addressing class imbalance in medical datasets. This study's findings can be leveraged to improve the performance and reliability of AI models used in respiratory care, particularly in scenarios where data imbalance is prevalent.
Moreover, the article “Deep Transfer Learning Approaches in Performance Analysis of Brain Tumor Classification Using MRI Images” by Srinivas et al.[13] showcases the application of deep transfer learning techniques in analyzing magnetic resonance imaging images for brain tumor classification. This work provides valuable insights into the performance analysis of deep learning models and their potential application in respiratory diagnostics, particularly in the analysis of medical images such as chest X-rays or CT scans.
By incorporating insights from these articles and the references they provide, this narrative review aims to build upon the existing body of literature on AI in health care and provide a comprehensive overview of its applications in respiratory care.
Limitations of prior work
Prior work in the field has opened the door to investigating the potential of AI in respiratory care. On closer inspection, though, some restrictions have become apparent. For instance, previous research mainly focused on the use of AI in diagnosis but did not provide comparatively a thorough evaluation of its impact on therapy selection. The ethical issues around patient privacy and data security were also not covered that much, despite the fact that it offered insightful information about AI-driven remote monitoring. These constraints, along with others mentioned in multiple books, present areas for further investigation and invention.
Contributions of the current work
To address the gaps in the body of literature, this research paper offers a number of original contributions that can help to advance the understanding of “AI in Respiratory Care.” The present study emphasizes the potential of AI algorithms to support medical professionals in treatment planning and decision-making processes in addition to exploring their diagnostic capabilities. By filling in this gap, it will provide a more thorough understanding of AI's function in respiratory care.
Contributions
This narrative review will make the following key contributions:
Comprehensive overview
This review offers a comprehensive understanding of the potential benefits and impact of AI technology. It consolidates research findings and current practices to present a holistic view of the role of AI in respiratory care.
Ethical considerations
In addition to highlighting the advantages of AI, this review also addresses the ethical considerations associated with its implementation in respiratory care. It explores issues related to patient privacy, data security, and the responsible use of AI algorithms. By shedding light on these ethical concerns, this review aims to promote the responsible and ethical integration of AI in respiratory care practices.
Future opportunities
Recognizing the dynamic nature of AI technology, this review identifies future directions and opportunities for AI in respiratory care. It explores emerging trends and discusses the potential for AI to enhance electronic health records and health-care delivery systems. By outlining future opportunities, this review aims to inspire further research and innovation in the field of AI in respiratory care.
Rational for this Review Article
This review article aims to provide an objective overview of the current state and future prospects of AI in respiratory care. Through a systematic analysis of existing literature, research studies, and technological advancements, this paper intends to examine the application of AI in respiratory care. Specifically, the focus will be on AI-assisted diagnosis, monitoring, and treatment of respiratory conditions. Furthermore, this review will critically evaluate the potential benefits, limitations, and challenges associated with the integration of AI technologies into respiratory care practices.
Aims and objectives
To provide a comprehensive overview of the current state of AI applications in respiratory care, with a focus on AI-assisted diagnosis, monitoring, and treatment
To explore the potential benefits and limitations of AI in respiratory care, including AI-assisted diagnosis, monitoring, and treatment
To assess the clinical impact of AI technologies in respiratory disease management and patient outcomes
To discuss the future perspective and potential areas of research and development for AI in respiratory care.
By achieving these aims and objectives, the review article will contribute to the knowledge base surrounding AI in respiratory care, inform clinical practice, guide future research efforts, and facilitate the responsible and beneficial implementation of AI technologies in this critical field.
Methods
Literature search strategy
Systematic literature search was conducted with the help of electronic databases, such as PubMed, Scopus, and Web of Science, using relevant keywords such as “artificial intelligence,” “respiratory care,” and associated terms.
Inclusion criteria
Studies published within the last 15 years to ensure the inclusion of recent advancements in AI technology including review articles, original research papers, and meta-analyses to gather a comprehensive understanding of the current landscape were included.
Retrieved articles were screened based on predefined inclusion and exclusion criteria.
Articles specifically discussing AI applications in respiratory care, encompassing diagnosis, monitoring, and treatment were included.
Results
Relevant information from the selected articles, including study design, AI techniques used, and relevant outcomes were assessed and key findings were extracted. The extracted data were organized into the below-discussed appropriate categories or themes to facilitate further analysis.
Respiratory care spectrum
Respiratory care involves a wide range of services and is administered in a variety of locations to meet the individual requirements of patients [Table 1]. When contemplating the possible integration of technology such as AI, it is essential to analyze the many domains of respiratory care. These services are provided in a variety of venues, including hospitals, clinics, residences, and distant areas. In hospital settings, respiratory care providers play a critical role in treating acute respiratory problems by giving mechanical ventilation and drugs and monitoring patients’ respiratory state. They engage with diverse teams to maximize patient outcomes and provide comprehensive treatment. In addition, the adoption of AI in respiratory care has the potential to improve diagnostic precision, individualized treatment methods, and remote monitoring capabilities in each of these domains. For instance, AI algorithms may examine patient data, such as medical pictures and physiological parameters, in order to aid in the exact diagnosis and early identification of respiratory disorders. AI technology can allow remote monitoring and offer real-time data analysis to follow illness development and tailor therapy in home-based respiratory care. In addition, the integration of AI with telehealth platforms may offer remote evaluations, consultations, and treatment changes in distant places where access to specialist health-care services may be restricted. It can enhance patient outcomes and assure complete treatment throughout the whole spectrum of respiratory health by taking into account the specific demands and settings of respiratory care, as well as the potential advantages of AI and other technologies.
Table 1.
Different aspects of respiratory care and their corresponding interventions and strategies
| Spectrum of respiratory care | Description | Reference |
|---|---|---|
| Prevention and health promotion | Public health campaigns, education, and occupational health measures to prevent respiratory conditions | [14] |
| Screening and early detection | Routine screenings, spirometry tests, and imaging studies to identify respiratory conditions at an early stage | [15] |
| Diagnostic evaluation | Comprehensive medical history, physical examinations, pulmonary function tests, sleep studies, and genetic testing | [16] |
| Medical management and treatment | Pharmacological interventions, oxygen therapy, pulmonary rehabilitation, allergy management, and personalized treatment plans | [17] |
| Intensive care and critical care | Invasive and noninvasive mechanical ventilation, continuous monitoring, ECMO, and prediction models for risk stratification | [18] |
| Home-based respiratory care | Home oxygen therapy, home mechanical ventilation, patient education, telehealth, remote monitoring, and predictive analytics | [19] |
| Palliative and end-of-life care | Symptom management, advance care planning, hospice care, and palliative care algorithms | [20] |
| Rehabilitation and support services | Respiratory therapy programs, smoking cessation, patient education, digital health tools, and predictive modeling | [21] |
ECMO=Extracorporeal membrane oxygenation
Current challenges in respiratory care
Respiratory care poses numerous challenges for health-care professionals, which can impact patient outcomes and quality of life. One of the primary challenges in respiratory care is the accurate and timely diagnosis of respiratory conditions. Many respiratory diseases, such as COPD or asthma, share similar symptoms, which can be difficult to differentiate. This diagnostic ambiguity can lead to delays in initiating appropriate treatment strategies and potentially compromise patient outcomes. Furthermore, the interpretation of diagnostic tests, such as pulmonary function tests or imaging studies, is subjective and result interpretation can vary among health-care professionals.[22] This subjectivity poses an additional challenge to achieving consistent and accurate diagnoses. In addition to diagnosis, another challenge in respiratory care is the effective monitoring of patients with respiratory conditions. Traditional methods of monitoring, such as spirometry or peak flow measurements, often require patients to visit health-care facilities, which can be inconvenient and time-consuming. This limitation can hinder the regular monitoring of patients and the prompt identification of exacerbations or changes in disease progression. Moreover, the manual interpretation of monitoring data can be prone to human error, limiting the accuracy of assessments.[23] Treatment adherence is also a challenge in chronic respiratory conditions. Many patients struggle to adhere to complex treatment regimens, which can involve the use of multiple inhalers, medications, or devices. Poor treatment adherence can lead to suboptimal control of symptoms, disease exacerbations, and increased health-care utilization.[24] AI algorithms can analyze vast amounts of patient data, including clinical records, imaging studies, and real-time monitoring data, to provide accurate and timely diagnoses. Furthermore, AI-powered monitoring systems can enable remote patient monitoring, allowing for continuous assessment and early detection of changes in disease status.[25]
Artificial intelligence in the prevention of respiratory diseases
Predictive modeling for respiratory disease risk
AI has shown considerable potential in the domain of predictive modeling for assessing the risk of respiratory diseases. Bhowmik and Most[26] proposed an innovative spatiotemporal ML framework that integrates convolutional and recurrent neural networks. This framework aims to forecast the likelihood of respiratory disease exacerbations, specifically COPD, by identifying real-time respiratory events and monitoring local environmental and meteorological information. This technology offers a novel approach for the timely detection of exacerbations, which has the potential to decrease hospitalization rates and mitigate medical expenses. In a separate investigation,[27] emphasized the application of clinical decision support systems (CDSS) in the timely identification of respiratory ailments, such as asthma and COVID-19, employing diverse ML methodologies, including artificial neural networks, SVM, and other approaches. This technique facilitates the early detection of diseases for medical professionals and provides guidance for future advancements in CDSS.
Artificial intelligence for respiratory care education and public health
The use of AI beyond the domain of illness prediction and encompasses areas such as education and public health. In a cross-sectional research conducted by,[28] it was shown that those aspiring to become medical professionals have the perception that AI has the potential to serve as an assistive tool, aiding in the acquisition of knowledge, mitigating mistakes, and improving the overall quality of patient health care. Nevertheless, the individuals voiced apprehensions about possible negative consequences, including the depreciation of the medical field and erosion of trust. They underscored the need for restructuring educational programs to adequately prepare upcoming doctors in using AI applications with proficiency and efficacy. In their recent study, Fisher and Rosella[29] delineated six primary areas of focus that are crucial for the effective integration of AI inside public health institutions. These objectives include current data governance, the allocation of resources toward the enhancement of data infrastructure, and the resolution of talent deficiencies, among other significant factors. According to the findings of Morgenstern et al. (Fisher and Rosella, 2022), professionals express a measured sense of optimism about the potential effects of AI in the field of public health. Specifically, they highlight its potential for enhancing disease surveillance. However, these experts also note the existence of several obstacles and concerns, such as insufficient regulation and a scarcity of accessible expertise in this domain.
Artificial intelligence for respiratory occupational health measures
AI's role in occupational respiratory health measures is under active exploration. Tran, Kwo, and Nguyen[30] suggested that AI can match trained clinicians’ precision under specific conditions, particularly in processing big data, and could contribute to the greater implementation of precision medicine. While the role of AI in a clinical setting is still being debated, it appears to increase objectivity through its correlational methodology. Hence, if its strengths and weaknesses are appropriately accounted for, AI has the potential to enhance health-care access and improve care quality.
Artificial intelligence-driven diagnosis and monitoring
ML algorithms can play a vital role in respiratory care by analyzing large volumes of data and identifying patterns that can assist in diagnosis, treatment, and monitoring. For instance, Zeng et al. (Giri et al., 2021) developed a ML model that effectively predicted exacerbations in patients with COPD. By analyzing a range of patient data, such as symptoms, vital signs, and environmental factors, the model could enable early intervention and prevent exacerbations. Similarly, Giri et al. utilized ML techniques to improve the accuracy of spirometry interpretation, aiding in the diagnosis and assessment of lung function.[31]
Natural language processing (NLP) is another AI technology that can benefit respiratory care. NLP algorithms have the capability to extract meaningful information from unstructured clinical notes, reports, and literature. This enables automated analysis and synthesis of vast amounts of textual data, providing valuable insights.[32]
AI-driven diagnosis and monitoring in respiratory care is an emerging field that aims to improve the detection and treatment of respiratory diseases using smart wearable devices and real-time data analysis.[33] AI systems can collect and classify biosignals such as cough, body temperature, and airflow, and provide accurate and timely diagnosis of respiratory illnesses, such as COVID-19, asthma, and COPD (Chen et al., 2021; Zhang et al., 2022). AI systems can also monitor the patient's condition and provide feedback and guidance for self-management and treatment adherence. AI-driven diagnosis and monitoring in respiratory care has the potential to reduce the burden on health-care systems, improve patient outcomes, and enhance the quality of life for respiratory patients.
Artificial intelligence-enabled treatment and interventions
One area where AI shows promise is in optimizing treatment plans for respiratory conditions. AI algorithms can analyze large datasets, including patient demographics, clinical records, and treatment outcomes, to identify patterns and factors that influence treatment response. By personalizing treatment plans, AI can help health-care professionals make informed decisions and enhance therapeutic efficacy.[34]
AI can also assist in therapeutic interventions by providing real-time guidance and feedback. For instance, AI-powered inhaler devices can monitor inhalation technique, provide instruction on proper device usage, and offer feedback to patients. This can help individuals with respiratory conditions achieve better medication delivery, leading to improved symptom control and disease management.[35]
Personalization of care is another area where AI can make a significant impact. By analyzing patient data, AI algorithms can identify patient-specific risk factors, predict disease progression, and tailor treatment plans accordingly. Personalized approach can help health-care professionals proactively intervene, prevent complications, and optimize patient outcomes.[36]
While AI-enabled treatment and intervention hold great potential, it is crucial to address challenges such as data privacy, algorithm bias, and ethical considerations to ensure the safe and effective implementation of AI technologies in respiratory care.
Clinical applications
Real-world examples and success stories demonstrate the potential of AI in transforming respiratory care. Several research papers and case studies highlight the successful implementation of AI technologies in clinical settings, showcasing the positive impact on patient care and outcomes.
One notable application of AI is in the diagnosis of respiratory conditions. For instance, Wang et al. presented a paper where a deep learning model accurately detected and classified lung nodules in CT scans. The AI algorithm demonstrated high sensitivity and specificity, aiding radiologists in making accurate diagnoses and facilitating timely intervention. This study showcases the potential of AI to enhance diagnostic accuracy and efficiency.[37]
Another significant research paper focuses on the use of AI in respiratory monitoring. Manoni et al. presented a paper where a wearable device equipped with AI algorithms continuously monitored respiratory patterns and identified abnormal breathing events in patients with sleep apnea. The AI technology enabled early detection of respiratory disturbances, allowing for timely intervention and improved patient outcomes. This research paper highlights the potential of AI-enabled monitoring systems in enhancing patient care and management.[38]
In addition, AI has been employed in the optimization of treatment plans for respiratory conditions. For example, Tsang et al. presented a research paper where AI algorithms analyzed patient data to personalize medication dosages for individuals with asthma. The AI-driven approach resulted in improved symptom control and enhanced treatment outcomes. This study showcases how AI can optimize treatment strategies and personalize care for respiratory patients.[39]
These research papers provide valuable insights into the successful implementation of AI technologies in respiratory care. They demonstrate the potential of AI to improve diagnostic accuracy, enhance monitoring capabilities, and optimize treatment plans. However, further research and larger-scale studies are needed to evaluate the long-term impact and cost-effectiveness of AI in respiratory care.
Breath-evaluating algorithms, smart inhalers, and wearable equipment are at the forefront of respiratory care. Pulmonary diseases such as lung cancer, pulmonary fibrosis, and asthma account for 70% of the pulmonary diseases globally. However, AI-driven technological advancements are making it easier for pulmonary specialists to diagnose diseases, and patients to administer self-care.
Brisbane-based ResApp is a global leader in audio-based evaluation of respiratory health that assesses the sound of a cough through ML/AI to identify different respiratory diseases such as pneumonia. These AI-driven smart apps utilize special algorithms that work on smartphones, without the need of any additional hardware system. These algorithms are built into smartphone apps that have been approved as medical devices and used by telehealth companies, clinics, and pharmaceutical companies globally.[40]
Wearable devices and biosensors
Wearable biomedical sensors are devices that can measure physiological and environmental parameters and be worn by the patient without restricting their mobility or daily activities. These devices can monitor:
Physiological parameters such as respiratory rate, heart rate, SpO2, lung sounds, lung motion, and electrocardiogram.[41]
Environmental parameters such as air temperature, humidity, allergen and pollutant concentration, and ozone level.[42]
Wearable sensors can also track the patient's physical activity, which is related to health outcomes such as disease morbidity, hospitalization, and mortality.[43] Table 2 lists examples on the technology.
Table 2.
Examples of wearable sensors for respiratory diseases
| Device | Description | Application | Reference examples |
|---|---|---|---|
| Pulse oximeter | Measures light absorption through an electronic processor and a pair of small light-emitting diodes | Evaluates and manages acute apnea in primary and secondary care; measures SpO2 continuously and sends personalised alerts based on smart algorithms that detect signs of disease decline in COPD patients; monitors self-isolated patients and detects early deterioration of the pulmonary function during the pandemic | [46] [47] [48] |
| Air quality monitor | Measures outdoor and indoor air quality and other environmental data | Correlates individual environmental exposure to health response for understanding impacts of ozone on chronic asthma conditions; creates maps of air quality on cell phones via Bluetooth or Wi-Fi | [40] [49] [42] |
| Wristband and chest patch | Measures heart valve sounds, lung motions, and ECGs using acoustics and biopotentials | Delivers a quick digital diagnosis of lung health status; monitors cardiovascular and respiratory activities simultaneously | [50] [51] |
SpO2=Oxygen saturation, COPD=Chronic obstructive pulmonary disease, ECGs=Electrocardiograms
Recent developments in the field of AI and wearable technology have facilitated the real-time monitoring of patients’ health, enabling the detection of various health conditions such as stress, respiratory problems associated with COVID-19, and other pertinent medical issues. Previous studies have shown the successful use of AI algorithms in the analysis of biosignals obtained from wearable sensors, resulting in the correct identification of stress.[44] The research demonstrated that the use of ML methods enabled the successful identification of stress based on biosignals, achieving a notable degree of accuracy. These findings provide support for the future development of noninvasive wearable devices that can identify and manage stress at an early stage.
In a similar manner,[45] have developed a wearable stethoscope that utilizes an AI system to provide instantaneous monitoring of lung sounds and automated identification of wheezing. The lung sound monitoring patch used in this investigation demonstrated the capability to monitor respiratory function and discern between typical and atypical breathing patterns. In long-term clinical applications, the AI-based counter has shown a remarkable ability to recognize aberrant breathing episodes, including wheezing occurrences, with an accuracy rate of over 80%.
The use of wearable technology has also been investigated in the surveillance of respiratory rate and SpO2 in individuals affected by COVID-19. According to a systematic review conducted by,[52] wearable devices have shown usefulness in continuous monitoring. However, more investigation involving real patients is required to ascertain the efficiency and efficacy of this technology.
In a study conducted by,[44] the use of AI in the analysis of data obtained from wearable devices was highlighted as a means to detect and identify stress. The findings of the research indicate that ML algorithms demonstrated a notable level of accuracy in the detection of stress based on biosignals. In a similar vein,[53] conducted a meticulously designed, longitudinal clinical trial to investigate the efficacy of wearable sensors in the timely identification and monitoring of viral respiratory tract infections.
In a recent research conducted by,[45] the efficacy of a wearable stethoscope in providing precise real-time monitoring of lung sounds and automated identification of wheezing using an AI algorithm was proven. The research findings indicate that the adventitious breathing event counter, which utilizes AI, had a discernment rate of 80% for various events, particularly those associated with wheeze, when used in long-term clinical settings.
These studies underscore the promise of wearable technology and AI in the field of health care, namely in the monitoring of respiratory health and stress levels. Further investigation is required to ascertain the efficacy of these technologies in practical contexts.
Smart inhalers
The use of AI in health care has created new opportunities for enhancing patient care, notably in the treatment of chronic respiratory diseases. One example of an AI application is inhaler usage, where it has shown promise in improving patient adherence, technique, and overall disease treatment.
AI systems have been utilized to identify and monitor medication self-administration mistakes, which pose a substantial issue in respiratory illness treatment.[54] These systems may identify when patients use their inhalers and assess whether they follow the proper procedures for utilizing these devices, hence enhancing drug safety with minimum overhead for patients and health-care providers.
Furthermore, Amiko Respiro Sense, a linked technology, has been used as an add-on attachment to inhaler devices to record clinical and real-world adherence data, which is critical for guiding treatment regimens and enhancing patient inhaler technique.[55] This technique can estimate important metrics of inhaler use and lung health with an accuracy of 90% or higher for all of these respiratory parameters.
Investigated the viability of innovative electronic adherence monitoring devices in terms of use, acceptability to patients and health-care professionals, and accuracy in a mixed-method research.[56] They discovered that devices that could record both actuation and inhalation were the most desired and useful in clinical practice. However, the research also emphasized the need of patient-centricity when selecting a device, since there is no “one size fits all.”
Finally,[57] found six consumer-directed mobile health (mHealth) applications that communicate with inhalers for asthma treatment in a cross-sectional study. These applications not only improve provider contact and act as a logbook, but they also employ alerts, reminders, or alarms to remind users of inhaler doses. Some even include direct pharmacy access for refill requests and AI to forecast future asthma exacerbations. The study does, however, encourage further research on the results and usage of these applications in order for health-care practitioners to make evidence-based recommendations.
The usage of AI inhalers is a promising field of study that might have a substantial influence on the treatment of respiratory disorders. However, further study is required to properly understand its influence on patient outcomes and its inclusion into ordinary clinical practice.
The use of artificial intelligence in spirometry
Spirometry, an essential instrument in the field of respiratory care, assumes a critical role in the evaluation of pulmonary function and the identification of diverse pulmonary ailments. The use of AI methodologies in spirometry has shown considerable promise in enhancing precision, productivity, and analysis of outcomes.
A qualitative research conducted by[58] has examined the problems and possibilities associated with the resumption of spirometry services during the COVID-19 epidemic. The research indicates that the use of AI decision support software has promise in facilitating the evaluation and analysis of spirometry outcomes for the purpose of assessing their quality. The integration of AI algorithms into spirometry has the potential to raise the precision, diminish variability, and elevate the overall quality of spirometry services. The validation of AI software plays a critical role in fostering trust and confidence among physicians and commissioners.
The use of AI has seen a growing prevalence in the domain of Interstitial lung disease (ILDs), with its application extending to spirometry as well.[59] These applications include the examination of spirometry data in order to provide automated interpretation and decision assistance. AI algorithms have the potential to assist in the diagnosis and categorization of interstitial lung diseases (ILDs) by effectively recognizing patterns and anomalies in spirometry readings.
The health-care industry has seen a significant transformation with the incorporation of the Internet of medical things (IoMT) and AI, leading to advancements in several areas such as spirometry.[60] The integration of IoMT devices with AI algorithms facilitates the remote monitoring and instantaneous analysis of spirometry data. AI algorithms have the capability to evaluate the efficacy of spirometry maneuvers, provide immediate feedback to patients, and aid health-care professionals in the interpretation of the obtained findings.
The discipline of spirometry in pediatric pulmonology has been significantly impacted by the integration of AI techniques, as noted by.[61] AI systems have the capability to analyze spirometry data in pediatric populations, hence facilitating precise interpretation and assisting in the identification of respiratory disorders. The aforementioned algorithms possess the capability to discern patterns, recognize anomalies, and aid in the process of decision-making, hence augmenting the comprehensive care of pediatric pulmonary disorders.
The use of AI into spirometry offers a multitude of benefits. AI algorithms have the capability to automate the process of interpreting and analyzing spirometry data, resulting in a reduction of subjectivity and variability. Spirometry maneuvers may be used to identify trends, anomalies, and quality difficulties. In addition, they provide immediate input to patients and aid health-care personnel in rendering precise diagnoses and therapy determinations.
In general, the use of AI in the field of spirometry offers a range of advantages, including enhanced precision, efficacy, and interpretation of outcomes. AI systems have the potential to assist in the detection and categorization of lung disorders by using spirometry data. In addition, they have the capability to aid in the evaluation of quality, provide immediate feedback, and improve the overall administration of respiratory ailments.
Digital stethoscope
The use of conventional stethoscopes for the purpose of auscultating lung sounds has significant importance in the process of diagnosing and distinguishing various pulmonary ailments. Nevertheless, the subjective interpretation of these auditory signals and the dependence on the personal expertise of health-care professionals impose constraints on the efficacy of stethoscopes in the context of clinical use. The introduction of electronic stethoscopes has significantly transformed the discipline of pulmonology via the augmentation of precision and dependability in the practice of lung auscultation.[62]
A meta-analysis was conducted by[63] which aimed to understand the power of combining digital pulmonary auscultation with computer-based algorithms. This study indicated that the specificity and sensitivity of identifying the abnormal pulmonary sounds using computer-based algorithms were 85% and 80%, respectively.
Recently, a prototype of a digital stethoscopic system using ML methods is proposed by.[64] The prototype used real-time diagnosis of cardiac abnormalities. The system consists of three subsystems: a portable digital subsystem for capturing and digitizing phonocardiographic sounds, a decision-making subsystem for classifying sounds as normal or abnormal using ML techniques, and a display subsystem for visualizing the results. The proposed system demonstrates high accuracy in diagnosing cardiac abnormalities, with 93.5% accuracy for normal heart sounds and 93.25% accuracy for abnormal heart sounds. In addition, the system offers the advantage of faster examination, with results obtained within 15 s.
Furthermore,[65] research work presented the development of an electronic stethoscope interfaced with Raspberry Pi 4B (Raspberry Pi 4B is a compact, single-board computer that offers a range of features and capabilities, making it suitable for various projects and applications [Wikipedia Contributors; 2023]) and a CNN-based deep learning model (a CNN-based deep learning model refers to a convolutional neural network that is specifically designed for image and pattern recognition tasks, utilizing multiple layers of interconnected nodes to extract relevant features and make predictions)[66] for accurate prediction of valvular heart diseases. The system under consideration encompasses an electronic stethoscope equipped with Bluetooth technology and a convolutional neural network (CNN) model that has been developed. This system has demonstrated a remarkable accuracy rate of 99.35% in the identification of abnormal heart sounds. Consequently, it presents itself as an affordable and easily transportable solution for the initial assessment of valvular diseases. This is particularly advantageous in regions where access to comprehensive medical resources is limited. At another settings and needs, researchers did not find a difference between conventional or electronic stethoscope for the detection of pediatric congenital heart disease preoperatively.[2] In contrast to the results of Roy et al.,[65] this may be explained not just by the requirements and population examined but also by the hardware and software used.
Ethical considerations and challenges
The incorporation of AI inside the health-care sector, namely in the domain of respiratory care, has significant promise for transforming the discipline via the augmentation of precision, productivity, and patient welfare. Nevertheless, in conjunction with the auspicious progressions in AI, there exist ethical deliberations and obstacles that want meticulous attention and resolution.[67] This discourse aims to examine the ethical implications and obstacles linked to the integration of AI in the domain of respiratory care, including many levels of analysis: AI in a broader context, AI within the health-care sector, and AI specifically within the realm of respiratory care [Figure 1].
Figure 1.
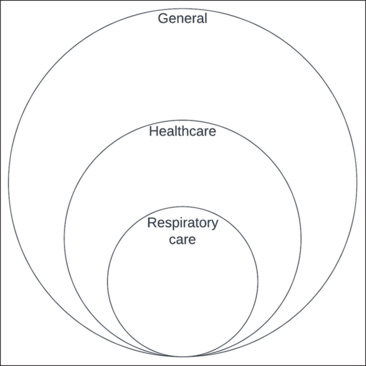
Ethical challenges of artificial intelligence development and uses. The size of the areas does not represent size effect but rather relationship. AI = Artificial intelligence
General ethical concerns of artificial intelligence technology
The advent of AI technologies has engendered salient ethical considerations pertaining to matters of data privacy, discrimination, transparency, prejudice, accountability, and more (DG, 2020; Marr, 2023; Nzenwata et al., 2023).[68] AI systems possess vast capabilities for aggregating and storing substantial corpora of data, thus begetting apprehensions regarding the protection and security of such data. The potential exists for this amalgamated data to be leveraged for tracking individuals’ movements, surveilling their health statuses, and even prognosticating future medical vulnerabilities (Centers for Disease Control and Prevention, 2022).[69] Moreover, in situations where AI systems are trained on biased data sets, the propagation of prejudices is possible, culminating in inequitable or discriminatory outcomes such as the preclusion of employment opportunities or credit extension.[70] Ensuring transparency in AI systems is of profound importance, as it enables individuals to comprehend the decision-making processes, thereby fostering trust in the impartiality of said systems. Furthermore, instituting accountability mechanisms is critical to guarantee that human agents are held responsible for the determinations made by AI systems, particularly when such judgments engender pernicious ramifications for human well-being.
Ethical concerns of artificial intelligence technology in health care
In the health-care sector, the use of AI technology introduces additional ethical concerns. One major concern is the potential impact on patient–provider relationships. The integration of AI systems in health care could potentially replace or displace health-care workers, which may negatively affect the interpersonal connection and trust between patients and providers.[71] Another concern is the risk of medical errors. As AI systems are still being developed, there is a possibility of errors that could compromise patient safety and well-being.[72] In addition, the cost of AI technology is a significant concern. The high expenses associated with implementing and maintaining AI systems could limit access to health care for certain individuals or communities, exacerbating existing health-care disparities (Celi et al., 2022).[73]
Ethical concerns of artificial intelligence technology in respiratory care
In the field of respiratory care, specific ethical concerns arise when AI technology is used. One concern is the accuracy of AI-based respiratory diagnosis. While AI systems have shown promising results, they may not yet be as accurate as human doctors in diagnosing respiratory diseases.[74] This raises concerns about potential misdiagnosis and inappropriate treatment decisions. Another concern is the impact on patient autonomy. AI systems, if given decision-making power, could make decisions about patient care without the individual's consent, which could violate patient autonomy and pose ethical challenges. Furthermore, the security of respiratory data is a crucial concern.[75] Respiratory data are sensitive and should be protected from unauthorized access. The potential vulnerability of AI systems to hacking or data breaches could lead to the disclosure of patient data and compromise privacy.
Addressing these ethical concerns is paramount to ensure the safe and ethical use of AI technology in the health-care sector, including respiratory care.
The resolution of these ethical problems and difficulties requires the collective effort and cooperation of health-care practitioners, researchers, policymakers, and ethicists. The establishment of comprehensive standards, rules, and training programs may play a pivotal role in promoting the appropriate and ethical integration of AI technology within the domain of respiratory care. The ongoing surveillance and assessment of AI systems are vital in order to detect and resolve ethical dilemmas promptly. This practice guarantees that the incorporation of AI technology remains consistent with ethical standards and prioritizes patient-centered care.
Vulnerability of deep learning models to adversarial attacks in respiratory care
In recent years, the vulnerability of deep learning models to adversarial attacks has garnered significant attention across various domains. Adversarial attacks involve manipulating input data in such a way that it can deceive the model's predictions, leading to potential security risks and compromised performance. This issue is not limited to malware detection but also extends to the field of respiratory care, where deep learning models are being used for diagnostics and decision-making. Addressing the challenge of adversarial attacks is crucial to ensure the robustness and reliability of AI models in respiratory care.
The recent paper by Kamran et al.[76] “A Novel Method for Improving the Robustness of Deep Learning-based Malware Detectors against Adversarial Attacks” proposes a method that could be adapted and applied to respiratory care AI systems. According to this paper, the method focuses on generating adversarial examples during the training phase and integrating them into the training dataset. By exposing the model to these adversarial examples, it enhances the model's ability to recognize and resist potential adversarial attacks at inference time. This approach can potentially improve the robustness and generalizability of deep learning models in respiratory diagnostics, treatment planning, and patient monitoring, minimizing the risk of manipulated input data leading to incorrect predictions or compromised patient care.
Study Limitations
While this narrative review provides valuable insights into the applications and potential benefits of AI in respiratory care, it is important to acknowledge certain limitations inherent in the current approach.
Generalizability of findings
The study findings presented in this review are based on the available literature and research studies within the scope of the presently available literature search. However, it is crucial to recognize that the applicability and generalizability of these findings may vary across different health-care settings, regions, and patient populations. Further research and studies are needed to validate and refine the conclusions drawn from this review in diverse health-care contexts.
Data quality and availability
The success and effectiveness of AI algorithms in respiratory care heavily rely on the quality and availability of data. However, the availability of high-quality, standardized, and annotated datasets in respiratory care may be limited. The lack of diverse and representative datasets can impact the performance and generalizability of AI models. Future efforts should focus on addressing data quality issues, promoting data-sharing initiatives, and ensuring the diversity and representativeness of datasets used in AI development for respiratory care.
Ethical considerations and bias
This review touches upon the ethical considerations associated with AI implementation in respiratory care, such as patient privacy.
Future Directions: Embracing the Potential of Artificial Intelligence in Respiratory Care
Looking ahead, there are several key areas where AI can play a transformative role:
Personalized medicine
One exciting future direction is the development of AI algorithms that can analyze vast amounts of patient data, including medical history, genetic information, and real-time physiological data. By leveraging this wealth of information, AI systems can provide personalized treatment plans and recommendations, tailored to each individual's unique needs. This has the potential to optimize patient outcomes and improve overall respiratory care.
Remote monitoring and telemedicine
With the increasing adoption of telemedicine, AI can enhance remote monitoring capabilities for respiratory patients. AI-powered devices can collect data on lung function, oxygen levels, and other vital parameters, providing real-time feedback to health-care providers and enabling timely interventions. This can be especially beneficial for patients in rural or underserved areas, allowing them to access quality respiratory care without the need for frequent hospital visits.
Early detection and diagnosis
AI algorithms have the ability to analyze large datasets and identify subtle patterns that may indicate the early onset of respiratory diseases. By leveraging ML, AI can assist health-care professionals in detecting respiratory conditions at an early stage when treatment options are more effective. This early detection can lead to better outcomes and potentially save lives.
Smart ventilation systems
AI has the potential to optimize mechanical ventilation in critically ill patients. By continuously monitoring patient data, including respiratory patterns, blood gas levels, and lung mechanics, AI algorithms can adjust ventilation parameters in real time, ensuring optimal support for the patient's respiratory system. This can improve patient comfort, reduce complications, and potentially shorten the duration of mechanical ventilation.
Collaborative artificial intelligence systems
In the future, we can expect to see AI systems that not only analyze data but also collaborate with health-care professionals. These systems can serve as reliable clinical decision-support tools, providing insights and recommendations based on the analysis of patient data. Through this collaboration, AI can augment the expertise of respiratory care professionals, leading to more accurate diagnoses and more effective treatment strategies.
It is important to note that as these future directions unfold, ethical considerations, data privacy, and the need for regulatory oversight will be vital to ensure the responsible and safe implementation of AI in respiratory care.
By embracing these future directions, we can tap into the full potential of AI, revolutionizing the way respiratory care is delivered and ultimately improving patient outcomes.
Conclusion
This narrative review has shed light on the transformative role of AI in respiratory care. Based on the analysis of various studies and advancements in the field, several critical results have emerged.
AI has demonstrated remarkable potential in respiratory diagnostics. Through image recognition and ML algorithms, AI systems have shown high accuracy in diagnosing respiratory conditions from medical images such as chest X-rays or CT scans. This development holds significant promise for improving the speed and accuracy of diagnosis, enabling health-care professionals to make informed decisions and provide timely interventions
AI has contributed to personalized treatment planning in respiratory care. By analyzing patient history, symptoms, and response to therapies, AI algorithms can assist in developing tailored treatment plans. This development has the potential to optimize patient outcomes by ensuring customized and effective interventions
AI-based monitoring and early detection systems have emerged as invaluable tools in respiratory care. These systems enable continuous monitoring of respiratory patients, allowing for early detection of deterioration and prompt interventions. By leveraging wearable devices and smart technologies, AI facilitates remote patient monitoring, reducing the burden on health-care facilities and enhancing patient comfort, the integration of AI technologies with electronic health records holds promise for seamless data analysis, decision support, and improved health-care delivery.
The main contributions of this narrative review:
Comprehensive overview: This review provides a comprehensive understanding of the applications and potential benefits of AI in respiratory care. By synthesizing research findings and exploring current practices, it offers valuable insights into the transformative potential of AI technology
Ethical considerations: The review addresses the ethical implications associated with AI implementation in respiratory care, including patient privacy, data security, and algorithm biases. By highlighting these considerations, it encourages responsible and ethical integration of AI in respiratory care practices
Future opportunities: By identifying emerging trends and future opportunities, such as AI integration with electronic health records, this review stimulates further research and innovation in the field of AI in respiratory care.
Finally, by improving diagnosis, AI has the potential to revolutionize respiratory care, treatment planning, and patient monitoring. While challenges and ethical considerations remain, the transformative impact of AI in this domain cannot be overstated. By leveraging the advancements and insights from this narrative review, health-care professionals and researchers can continue to harness the power of AI to improve patient outcomes and enhance respiratory care practices.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
I am extremely grateful to Professor Dr. Awad for her valuable feedback and reviews. In addition, I deeply appreciate Dr. Safug for his extensive knowledge and expertise. Finally, I must not overlook expressing my gratitude toward my team at Azeer Company, who provided unwavering support throughout the completion of this review.
References
- 1.Soriano JB, Kendrick PJ, Paulson KR, Gupta V, Abrams EM, Adedoyin RA, et al. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir Med. 2020;8:585–96. doi: 10.1016/S2213-2600(20)30105-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahuja AS. The impact of artificial intelligence in medicine on the future role of the physician. https://doi.org/10.7717/peerj.7702. Peer J. 2019;7:e7702. doi: 10.7717/peerj.7702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Collins C, Dennehy D, Conboy K, Mikalef P. Artificial intelligence in information systems research: A systematic literature review and research agenda. International Journal of Information Management. 2021;60:102383. [Google Scholar]
- 4.Stokes K, Castaldo R, Federici C, Pagliara S, Maccaro A, Cappuccio F, et al. The use of artificial intelligence systems in diagnosis of pneumonia via signs and symptoms: A systematic review. Biomedical Signal Processing and Control. 2022;72:103325. [Google Scholar]
- 5.Li X, Zhou H-P, Zhou Z-J, Du N, Zhong E-H, Zhai K, et al. Artificial intelligence-powered remote monitoring of patients with chronic obstructive pulmonary disease. Chinese Medical Journal. 2021;134:1546–8. doi: 10.1097/CM9.0000000000001529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. https://doi.org/10.7861/futurehosp.6-2-94. Future Healthc J. 2019;6:94–98. doi: 10.7861/futurehosp.6-2-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liao KM, Ko SC, Liu CF, Cheng KC, Chen CM, Sung MI, et al. Development of an interactive ai system for the optimal timing prediction of successful weaning from mechanical ventilation for patients in respiratory care centers. Diagnostics. 2022;12:975. doi: 10.3390/diagnostics12040975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gerke S, Minssen T, Cohen G. In Artificial intelligence in healthcare. Elsevier; 2020. Ethical and legal challenges of artificial intelligence-driven healthcare; pp. 295–336. [Google Scholar]
- 9.Norori N, Hu Q, Aellen FM, Faraci FD, Tzovara A. Addressing bias in big data and AI for health care: A call for open science. Patterns, 2021;2:100347. doi: 10.1016/j.patter.2021.100347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Honkoop P, Usmani O, Bonini M. The current and future role of technology in respiratory care. Pulmonary Therapy. 2022;8:167–79. doi: 10.1007/s41030-022-00191-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Javed U, Shaukat KA. Hameed I, Iqbal F, Mahboob Alam T, Luo S. A Review of Content-Based and Context-Based Recommendation Systems. https://doi.org/10.3991/ijet.v16i03.18851 International Journal of Emerging Technologies in Learning (iJET) 2021;16:274–306. [Google Scholar]
- 12.Khushi M, Shaukat K, Alam TM, Hameed IA, Uddin S, Luo S, et al. “A Comparative Performance Analysis of Data Resampling Methods on Imbalance Medical Data,”. in IEEE Access. 2021;9:109960–109975. doi: 10.1109/ACCESS.2021.3102399. [Google Scholar]
- 13.Srinivas C, Nandini Prasad KS, Zakariah M, Alothaibi YA, Shaukat K, Partibane B, et al. Deep Transfer Learning Approaches in Performance Analysis of Brain Tumor Classification Using MRI Images. J Healthc Eng. 2022;2022:3264367. doi: 10.1155/2022/3264367. doi: 10.1155/2022/3264367. PMID: 35299683; PMCID: PMC8923754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Banatvala N, Akselrod S, Webb D, Sladden T, Hipgrave D, Schneidman M. Actions needed to prevent noncommunicable diseases and improve mental health. Bull World Health Organ. 2019;97:75–75A. doi: 10.2471/BLT.18.228700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Qaseem A, Wilt TJ, Weinberger SE, Hanania NA, Criner G, van der Molen T, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155:179–91. doi: 10.7326/0003-4819-155-3-201108020-00008. [DOI] [PubMed] [Google Scholar]
- 16.Ponce MC SA, Sharma S. Pulmonary Function Tests. Https://www.ncbi.nlm.nih.gov/books/NBK482339/ 2022 [PubMed] [Google Scholar]
- 17.Reddel HK, Bacharier LB, Bateman ED, Brightling CE, Brusselle GG, Buhl R, et al. Global Initiative for Asthma Strategy 2021: executive summary and rationale for key changes. Am J Respir Crit Care Med. 2022;205:17–35. doi: 10.1164/rccm.202109-2205PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goligher EC, Ferguson ND, Brochard LJ. Clinical challenges in mechanical ventilation. The Lancet. 2016;387:1856–66. doi: 10.1016/S0140-6736(16)30176-3. [DOI] [PubMed] [Google Scholar]
- 19.McKim DA, Avendano M, Abdool S, Côté F, Duguid N, Fraser J, et al. Home mechanical ventilation: a Canadian Thoracic Society clinical practice guideline. Canadian Respiratory Journal. 2011;18:197–215. doi: 10.1155/2011/139769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rocker GM, Simpson AC, Horton R. Palliative care in advanced lung disease: the challenge of integrating palliation into everyday care. Chest. 2015;148:801–809. doi: 10.1378/chest.14-2593. [DOI] [PubMed] [Google Scholar]
- 21.Zwerink M, Brusse-Keizer M, van der Valk PD, Zielhuis GA, Monninkhof EM, van der Palen J, et al. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2014;(3):CD002990. doi: 10.1002/14651858.CD002990.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Graham BL, Steenbruggen I, Miller MR, Barjaktarevic IZ, Cooper BG, Hall GL, et al. Standardization of spirometry 2019 update. An official American thoracic society and European respiratory society technical statement. Am J Respir Crit Care Med. 2019;200:e70–e88.. doi: 10.1164/rccm.201908-1590ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Restrepo RD, Alvarez MT, Wittnebel LD, Sorenson H, Wettstein R, Vines DL, et al. Medication adherence issues in patients treated for COPD. International journal of chronic obstructive pulmonary disease. 2008;3:371–84. doi: 10.2147/copd.s3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J. 2019;6:94–8. doi: 10.7861/futurehosp.6-2-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zeng S, Arjomandi M, Tong Y, Liao ZC, Luo G. Developing a machine learning model to predict severe chronic obstructive pulmonary disease exacerbations: retrospective cohort study. J Med Internet Res. 2022;24:e28953. doi: 10.2196/28953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bhowmik RT, Most SP. A Personalized Respiratory Disease Exacerbation Prediction Technique Based on a Novel Spatio-Temporal Machine Learning Architecture and Local Environmental Sensor Networks. Electronics. 2022;11:2562. [Google Scholar]
- 27.Ali SW, Asif M, Zia MYI, Rashid M, Syed SA, Nava E. CDSS for Early Recognition of Respiratory Diseases based on AI Techniques: A Systematic Review. Wireless Personal Communications. 2023:1–23. [Google Scholar]
- 28.Civaner MM, Uncu Y, Bulut F, Chalil EG, Tatli A. Artificial intelligence in medical education: A cross-sectional needs assessment. BMC Med Educ. 2022;22:772. doi: 10.1186/s12909-022-03852-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fisher S, Rosella LC. Priorities for successful use of artificial intelligence by public health organizations: a literature review. BMC Public Health. 2022;22:2146. doi: 10.1186/s12889-022-14422-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tran D, Kwo E, Nguyen E. Current state and future potential of AI in occupational respiratory medicine. Current Opinion in Pulmonary Medicine. 2022;28:139–43. doi: 10.1097/MCP.0000000000000852. [DOI] [PubMed] [Google Scholar]
- 31.Juhn Y, Liu H. Artificial intelligence approaches using natural language processing to advance EHR-based clinical research. J Allergy Clin Immunol. 2020;145:463–9. doi: 10.1016/j.jaci.2019.12.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Khemasuwan D, Sorensen JS, Colt HG. Artificial intelligence in pulmonary medicine: computer vision, predictive model and COVID-19. Eur Respir Rev. 2020;29:200181. doi: 10.1183/16000617.0181-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Belkacem AN, Ouhbi S, Lakas A, Benkhelifa E, Chen C. End-to-end AI-based point-of-care diagnosis system for classifying respiratory illnesses and early detection of COVID-19: A theoretical framework. Front Med (Lausanne) 2021;8:585578. doi: 10.3389/fmed.2021.585578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cataldo D, Hanon S, Peché RV, Schuermans DJ, Degryse JM, De Wulf IA, et al. How to choose the right inhaler using a patient-centric approach? Adv Ther. 2022;39:1149–63. doi: 10.1007/s12325-021-02034-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Johnson KB, Wei WQ, Weeraratne D, Frisse ME, Misulis K, Rhee K, et al. Precision medicine, AI, and the future of personalized health care. Clin Transl Sci. 2021;14:86–93. doi: 10.1111/cts.12884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang H, Zhu H, Ding L. Accurate classification of lung nodules on CT images using the TransUnet. Front Public Health. 2022;10:1060798. doi: 10.3389/fpubh.2022.1060798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Manoni A, Loreti F, Radicioni V, Pellegrino D, Della Torre L, Gumiero A, et al. A new wearable system for home sleep apnea testing, screening, and classification. Sensors (Basel) 2020;20:7014. doi: 10.3390/s20247014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tsang KC, Pinnock H, Wilson AM, Shah SA. Application of machine learning algorithms for asthma management with mHealth: a clinical review. J Asthma Allergy. 2022;15:855–873. doi: 10.2147/JAA.S285742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. Pharmacy and Therapeutics. 2014;39:356–364. [PMC free article] [PubMed] [Google Scholar]
- 40.Aliverti A. Wearable technology: role in respiratory health and disease. Breathe. 2017;13:e27–e36.. doi: 10.1183/20734735.008417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cinel G, Tarim EA, Tekin HC. Wearable respiratory rate sensor technology for diagnosis of sleep apnea. 2020 Medical Technologies Congress (TIPTEKNO) 2020 DOI: 10.1109/TIPTEKNO50054.2020.9299255. [Google Scholar]
- 42.Salamone F, Masullo M, Sibilio S. Wearable devices for environmental monitoring in the built environment: a systematic review. Sensors, 2021;21:4727. doi: 10.3390/s21144727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.JeyaJothi ES, Anitha J, Rani S, Tiwari B. A comprehensive review: computational models for obstructive sleep apnea detection in biomedical applications. Biomed Res Int. 2022:7242667. doi: 10.1155/2022/7242667. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 44.D’Alpaos B. AI for health: Using AI to identify stress from wearable devices data Politecnico di Torino] 2023 [Google Scholar]
- 45.Lee SH, Lee KR, Kim T, Im S, Lee YJ, Jeong S, et al. Research Square Platform LLC; 2023. A wearable stethoscope for accurate real-time lung sound monitoring and automatic wheezing detection based on an AI algorithm. doi.org/10.21203/rs.3.rs-2844027/v1. [Google Scholar]
- 46.De Fazio R, Stabile M, De Vittorio M, Velázquez R, Visconti P. An overview of wearable piezoresistive and inertial sensors for respiration rate monitoring. Electronics, 2021;10:2178. [Google Scholar]
- 47.Raza T, Qu L, Khokhar WA, Andrews B, Ali A, Tian M. Progress of wearable and flexible electrochemical biosensors with the aid of conductive nanomaterials. Frontiers in Bioengineering and Biotechnology. 2021;9:761020. doi: 10.3389/fbioe.2021.761020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wong CK, Ho DTY, Tam AR, Zhou M, Lau YM, Tang MOY, et al. Artificial intelligence mobile health platform for early detection of COVID-19 in quarantine subjects using a wearable biosensor: protocol for a randomised controlled trial. BMJ open. 2020;10:e038555. doi: 10.1136/bmjopen-2020-038555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saini J, Dutta M, Marques G. A comprehensive review on indoor air quality monitoring systems for enhanced public health. Sustainable Environment Research. 2020;30:1–12. doi: 10.3390/ijerph17144942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fu W, Li R. Diagnostic performance of a wearing dynamic ECG recorder for atrial fibrillation screening: the HUAMI heart study. BMC Cardiovasc Disord. 2021;21:1–10. doi: 10.1186/s12872-021-02363-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Soon S, Svavarsdottir H, Downey C, Jayne DG. Wearable devices for remote vital signs monitoring in the outpatient setting: An overview of the field. BMJ Innovations. 2020:6. [Google Scholar]
- 52.Takahashi S, Nakazawa E, Ichinohe S, Akabayashi A, Akabayashi A. Wearable technology for monitoring respiratory rate and SpO2 of COVID-19 patients: a systematic review. Diagnostics. 2022;12:2563. doi: 10.3390/diagnostics12102563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hadid A, McDonald EG, Cheng MP, Papenburg J, Libman M, Dixon PC, et al. The WE SENSE study protocol: A controlled, longitudinal clinical trial on the use of wearable sensors for early detection and tracking of viral respiratory tract infections. Contemporary clinical trials. 2023;128:107103. doi: 10.1016/j.cct.2023.107103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhao M, Hoti K, Wang H, Raghu A, Katabi D. Assessment of medication self-administration using artificial intelligence. Nature medicine. 2021;27:727–35. doi: 10.1038/s41591-021-01273-1. [DOI] [PubMed] [Google Scholar]
- 55.Rogueda P, Grinovero M, Ponti L, Purkins G, Croad O. Telehealth ready: Performance of the Amiko Respiro sense connected technology with Merxin DPIs. J Aerosol Med Pulm Drug Delivery. 2019;32:A26–A26. [Google Scholar]
- 56.Makhecha S, Chan A, Pearce C, Jamalzadeh A, Fleming L. Novel electronic adherence monitoring devices in children with asthma: A mixed-methods study. BMJ Open Respiratory Research. 2020;7:e000589. doi: 10.1136/bmjresp-2020-000589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nguyen E, Miao B, Pugliese N, Huang D, Sobieraj DM. Cross-sectional analysis of consumer-facing mHealth apps associated with inhaler monitoring for asthma. J Am Pharm Assoc. 2020;60:e162–e167.. doi: 10.1016/j.japh.2020.05.007. [DOI] [PubMed] [Google Scholar]
- 58.Doe G, Taylor SJC, Topalovic M, Russell R, Evans RA, Maes J, et al. Challenges and opportunities in resuming spirometry services in England post-pandemic with potential to adopt Artificial Intelligence decision support software: A qualitative study. British Journal of General Practice. 2023;73 doi: 10.3399/BJGP.2022.0608. BJGP.2022.0608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Exarchos KP, Gkrepi G, Kostikas K, Gogali A. Recent Advances of Artificial Intelligence Applications in Interstitial Lung Diseases. Diagnostics. 2023;13:2303. doi: 10.3390/diagnostics13132303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nakshbandi G, Moor CC, Wijsenbeek MS. Role of the internet of medical things in care for patients with interstitial lung disease. Curr Opin Pulm Med. 2023;29:285–92. doi: 10.1097/MCP.0000000000000971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Alzayed AA. Application of Artificial Intelligence in Pediatric Pulmonology: Current Scenario and Future Prospective. SVU-International Journal of Medical Sciences, 2023;6:501–510. [Google Scholar]
- 62.Leng S, Tan RS, Chai KTC, Wang C, Ghista D, Zhong L. The electronic stethoscope. Biomedical engineering online. 2015;14:1–37. doi: 10.1186/s12938-015-0056-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gurung A, Scrafford CG, Tielsch JM, Levine OS, Checkley W. Computerized lung sound analysis as diagnostic aid for the detection of abnormal lung sounds: A systematic review and meta-analysis. Respir Med. 2011;105:1396–403. doi: 10.1016/j.rmed.2011.05.007. doi: 10.1016/j.rmed.2011.05.007. Epub 2011 Jun 14. PMID: 21676606; PMCID: PMC3227538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Omarov B, Saparkhojayev N, Shekerbekova S, Akhmetova O, Sakypbekova M, Kamalova G, et al. Artificial Intelligence in Medicine: Real Time Electronic Stethoscope for Heart Diseases Detection. Computers, Materials & Continua. 2022:70. DOI:10.32604/cmc.2022.019246. [Google Scholar]
- 65.Roy TS, Roy JK, Mandal N. Design and development of electronic stethoscope for early screening of valvular heart disease prediction. Biomedical Signal Processing and Control. 2023;86:105086. [Google Scholar]
- 66.LeCun Y, Bengio Y, Hinton G. Deep Learning. http://dx.doi.org/10.1038/nature14539. Nature, 2015;521:436–444. doi: 10.1038/nature14539. [DOI] [PubMed] [Google Scholar]
- 67.Gundersen T, Bærøe K. The Future Ethics of Artificial Intelligence in Medicine: Making Sense of Collaborative Models. https://doi.org/10.1007/s11948-022-00369-2. Science and engineering ethics. 2022;28:17. doi: 10.1007/s11948-022-00369-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.DG E. The ethics of artificial intelligence: Issues and initiatives, EPRS: European Parliamentary Research Service. Belgium. 2023 Retrieved from https://policycommons.net/artifacts/1337278/the-ethics-of-artificial-intelligence/1944981/ on 11 Jan 2024. CID: 20.500.12592/w726c9. [Google Scholar]
- 69.Dumbrava C. Tracking mobile devices to fight coronavirus 2020. https://www.europarl.europa.eu/RegData/etudes/BRIE/2020/649384/EPRS_BRI(2020)649384_EN.pdf. [Last accessed on 2020 May 30] [Google Scholar]
- 70.Marr B. The 15 Biggest Risks Of Artificial Intelligence. Forbes. 2023 Available from: https://www.forbes.com/sites/bernardmarr/2023/06/02/the-15-biggest-risks-of-artificial-intelligence/?sh=77bb81ff2706. [Last retrieved on Aug 19] [Google Scholar]
- 71.Sauerbrei A, Kerasidou A, Lucivero F, Hallowell N. The impact of artificial intelligence on the person-centred, doctor-patient relationship: some problems and solutions. BMC Medical Informatics and Decision Making. 2023;23:1–14. doi: 10.1186/s12911-023-02162-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gregory A, Hern A. AI poses existential threat and risk to health of Millions, experts warn. https://www.theguardian.com/technology/2023/may/10/ai-poses-existential-threat-and-risk-to-health-of-millions-experts-warn The Guardian. 2023 [Google Scholar]
- 73.Celi LA, Cellini J, Charpignon ML, Dee EC, Dernoncourt F, Eber R, et al. Sources of bias in artificial intelligence that perpetuate healthcare disparities—A global review. PLOS Digital Health. 2022;1:e0000022. doi: 10.1371/journal.pdig.0000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kumar Y, Koul A, Singla R, Ijaz MF. Artificial intelligence in disease diagnosis: a systematic literature review, synthesizing framework and future research agenda. https://doi.org/10.1007/s12652-021-03612-z. Journal of Ambient Intelligence and Humanized Computing. 2023;14:8459–486. doi: 10.1007/s12652-021-03612-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lamanna C, Byrne L. Should artificial intelligence augment medical decision making? The case for an autonomy algorithm. AMA J Ethics. 2018;20:902–910. doi: 10.1001/amajethics.2018.902. [DOI] [PubMed] [Google Scholar]
- 76.Kamran S, Luo S, Varadharajan V. A novel method for improving the robustness of deep learning-based malware detectors against adversarial attacks. Eng Appl Artif Intell. 2022;116:105461. ISSN 0952-1976. doi:10.1016/j.engappai.2022.105461. [Google Scholar]


