Abstract
Borderline personality disorder (BPD) and alcohol use disorder frequently co-occur, yet we know relatively little about risk processes underlying this association. Previous research with nonclinical samples has highlighted how drinking motives may link personality characteristics with heavy alcohol use and problems. The present study substantively extends previous research by examining if drinkers with BPD had higher levels of alcohol use problems compared with drinkers without BPD and similar levels of alcohol use involvement. Multiple domains of impulsivity and affective instability were examined as dimensional markers of risk that may increase alcohol problems for individuals with BPD. Furthermore, multiple domains of drinking motives were examined as potential mediators accounting for the association between BPD and alcohol-related problems. Participants were 81 current drinkers (n = 39 with a current diagnosis of BPD). Results indicated that those with BPD endorsed more alcohol problems compared with non-BPD drinkers, F(1, 77) = 22.26, p < .001. These findings remained after accounting for multiple domains of impulsivity and affective instability. The indirect effects of coping and conformity-related drinking motives partially accounted for the relation between BPD and alcohol problems. Research examining differential response to alcohol for individuals with BPD is needed to directly test if acute alcohol consumption is particularly effective at reducing negative affect for adults with BPD. Offering alternative methods of managing uncomfortable or painful states and/or fitting in with others socially may represent particularly important targets for intervention efforts that decrease these reasons for drinking.
Keywords: borderline personality disorder, alcohol use disorder, substance use, coping, drinking motives
Borderline personality disorder (BPD) and alcohol use disorder (AUD) co-occur at a striking rate (Ball, Tennen, Poling, Kranzler, & Rounsaville, 1997; Grant, Stinson, Dawson, Chou, & Ruan, 2005; Sher & Trull, 2002; Skodol, Oldham, & Gallaher, 1999; Trull et al., 2018). Data from the National Epidemiologic Survey on Alcohol and Related Conditions indicate that 58.3% of individuals with a lifetime diagnosis of BPD also endorse lifetime AUD. In this same study, 9.8% to 14.7% of those with lifetime AUD report past or current comorbid BPD. Rates of comorbidity are similarly elevated among clinical samples diagnosed with BPD, with some researchers finding that up to 65% of individuals experience both conditions (Trull et al., 2018; Trull, Sher, Minks-Brown, Durbin, & Burr, 2000; Zanarini et al., 1998). Previous research has shown a transactional process. BPD traits predict future alcohol problems (Stepp, Trull, & Sher, 2005) and onset of AUD (Walter et al., 2009), and increases in alcohol use frequency also exacerbate BPD symptoms (Lazarus, Beardslee, Pedersen, & Stepp, 2017). Each of these disorders is profoundly impairing in isolation—and, when combined, are associated with incrementally poorer prognosis and outcomes (Chen, Brown, Lo, & Linehan, 2007; Links, Heslegrave, Mitton, van Reekum, & Patrick, 1995; Miller, Abrams, Dulit, & Fyer, 1993; Morgenstern, Langenbucher, Labouvie, & Miller, 1997). Understanding why BPD and alcohol problems frequently co-occur is necessary to decrease the disproportionate public health burden for these individuals.
Research examining common factors underlying alcohol problems and BPD point to impulsivity/behavioral undercontrol and emotional lability/negative affectivity as key features contributing to each condition (Bornovalova, Lejuez, Daughters, Rosenthal, & Lynch, 2005; Coffey, Schumacher, Baschnagel, Hawk, & Holloman, 2011; Littlefield, Sher, & Wood, 2010; Sher, Trull, Bartholow, & Vieth, 1999; Stevens, Blanchard, & Littlefield, 2018). For example, individuals with BPD who drink show higher within-person variability in negative affect compared with those who do not drink (Jahng et al., 2011).
Etiological models highlight the combination of trait impulsivity and negative affectivity as genetically influenced predisposing factors for BPD and alcohol use problems (Axelrod, Perepletchikova, Holtzman, & Sinha, 2011; Crowell, Beauchaine, & Linehan, 2009; Trull et al., 2000). Although these trait-level vulnerabilities confer increased risk, important intermediate processes may function to potentiate severe alcohol use problems, BPD, and their co-occurrence. For example, specific environmental characteristics, social factors, and cognitive–behavioral processes are likely to heighten a vulnerable individual’s risk for developing these conditions (Crowell et al., 2009; Lane, Carpenter, Sher, & Trull, 2016).
Drinking motives are one set of factors that appear to mediate relations between personality characteristics, self-regulation, affective instability, and alcohol use (Cooper, 1994; Cooper, Kuntsche, Levitt, Barber, & Wolf, 2016; Littlefield et al., 2010; Martins, Bartholow, Cooper, Von Gunten, & Wood, 2018) and thus, may be particularly relevant to examine among drinkers with BPD. Drinking motives capture the various functions alcohol use can serve, and thereby aid in pinpointing why and under what circumstances people choose to drink (Cooper et al., 2016; Sher et al., 1999; Tragesser, Sher, Trull, & Park, 2007). For example, an individual may be motivated to use alcohol in an attempt to regulate or cope with aversive affective states, enhance positive affective states, conform with others, and/or for sociability (Cooper, 1994). Drinking motives are hypothesized to represent proximal mechanisms through which more distal factors, such as personality traits, operate (Sher et al., 1999).
Consistent with this theory, researchers have found drinking to cope and to get “high” or “drunk” (drinking for enhancement) mediate the relation between broad personality traits (e.g., neuroticism) and drinking problems (Littlefield et al., 2010). Although trait-level vulnerabilities may be difficult to modify, understanding drinking motives could directly inform targeted intervention efforts for alcohol use. As outlined above, trait impulsivity and negative affectivity are individual-level differences that may predispose a person to both BPD and AUD. Each of these factors are linked to drinking motives (see Vest, Murphy, & Tragesser, 2018). Researchers have observed relations between enhancement-based drinking motives and BPD-related traits such as sensation seeking, low inhibitory control, and behavioral impulsivity (Adams, Kaiser, Lynam, Charnigo, & Milich, 2012). Individuals with BPD also frequently score high on measures of neuroticism (Kendler, Myers, & Reichborn-Kjennerud, 2011), which, in turn, is often linked to coping motives (Cooper, Agocha, & Sheldon, 2000; Littlefield et al., 2010; Loose, Acier, & El-Baalbaki, 2018; Stewart & Devine, 2000).
Despite consistent empirical support for relations between core BPD features, alcohol use, and drinking motives, few studies have directly examined BPD and drinking motives. In a study of college students, Tragesser and colleagues (2007) found coping motives partially accounted for the cross-sectional association between Cluster B personality disorder symptoms and AUD, whereas enhancement motives mediated the association between Cluster B personality disorder symptoms and prospective AUD five years later. Vest and colleagues (2018) recently examined associations between BPD features and motives for substance use cross-sectionally within an undergraduate sample. Although few participants endorsed BPD symptoms, they found coping motives exhibited the strongest relation with BPD features across alcohol, cannabis, and prescription opioid usage—particularly among women. Conformity motives were also related to alcohol and cannabis use and associated with BPD features. However, enhancement motives were not related to BPD features and alcohol use.
Finally, Chugani and colleagues (2018) found support for two mechanistic pathways linking BPD symptoms and alcohol-related problems in a community sample of 18-year-old women. First, an affective pathway linked BPD symptoms to alcohol-related problems through affective instability and coping motives for alcohol use. Second, the authors found a sensation seeking pathway whereby sensation seeking and enhancement motives for alcohol use mediated the association between BPD symptoms and alcohol-related problems. These findings highlight the possibility of both a positive reinforcement pathway and a negative reinforcement pathway increasing risk for alcohol problems. However, the generalizability of study results is limited to young women in a community setting, with generally low BPD symptoms and alcohol-related problems. Additionally, Koob’s dark side of addiction model (Koob, 2013) would indicate that, over time, positive rewards of heavy drinking lessen and motivation will shift toward avoidance of negative affect and withdrawal symptoms as AUD develops and becomes more severe. Given that Chugani and colleagues (2018) focused on 18-year-olds, it is possible that the positive reinforcement pathway would become less pronounced (and the negative reinforcement pathway more pronounced) in older samples that have progressed into latter stages of addiction. Furthermore, the study only examined two domains of drinking motives. Taken together, existing studies point to coping motives as most consistently related to BPD features, yet further research on drinking motives among individuals who meet diagnostic threshold for this disorder is sorely needed.
Drinking motives have not been explored among individuals who meet full diagnostic criteria for BPD. Additionally, research has not systematically accounted for shared core features of BPD and problem drinking to understand if specific underlying features like affective instability and impulsivity are driving the previously observed associations between BPD and alcohol misuse. Lastly, although research has shown individuals with BPD and alcohol misuse experience worse prognoses than those without BPD (Chen et al., 2007; Links et al., 1995; Miller et al., 1993; Morgenstern et al., 1997), previous research has not accounted for potential differences in actual alcohol use frequency and consumption. It is currently unclear whether drinkers with BPD simply drink more often and/or in higher volumes or whether they are more likely to experience problems when they drink. Understanding if individuals with BPD experience more alcohol problems even at comparable levels of alcohol use is needed. This will illuminate if identification of in-the-drinking-event treatment targets would be beneficial.
The current study addresses these important gaps in the literature by examining alcohol problems and drinking motives in a sample of drinkers with and without a diagnosis of BPD. We hypothesized that individuals with BPD would experience more alcohol problems compared with those without BPD, even at similar rates of alcohol consumption. Second, we hypothesized that individuals with BPD would have higher levels of drinking to cope than individuals without BPD and that this would partially account for the association between BPD and alcohol problems. We also examined enhancement, conformity, and sociability motives to test the specificity of this pathway. However, we did not hold a priori hypotheses about these reasons for drinking. Finally, it is currently unclear whether BPD is related to alcohol problems over and above dimensions of affective instability and impulsivity, key constructs related to both BPD and alcohol problems. Therefore, we examined the effect of including impulsivity and affective instability on our hypothesized associations between (a) BPD and alcohol problems and (b) BPD and drinking motives.
Method
Participants
The current study is part of a larger alcohol administration research protocol. Participants were recruited from the community (posted fliers, Craigslist advertisements, and word of mouth) and previous research registries. A phone screen was conducted with potential participants to determine initial eligibility. Participants were required to report drinking alcohol in the past month (“current drinker”) and having consumed the equivalent amount of alcohol in the past 6 months as would be administered in the laboratory.1 We excluded those abstaining from alcohol, reporting past head injury with loss of consciousness >5 min, currently pregnant or breastfeeding, weighing over 250 pounds, or currently taking medication (selective serotonin reuptake inhibitors and serotonin-norepinephrine reuptake inhibitors were allowed) for which the use of alcohol is contraindicated. Participants were also asked the McLean Screening Instrument for BPD (Zanarini et al., 2003). BPD participants were required to answer “yes” to six or more of the 10 BPD screener questions (e.g., “have you been extremely moody?”) to be considered for enrollment into the BPD sample. During enrollment into the study, participants with and without BPD were matched on self-reported past 30-day drinking behavior from the screener to reduce differences in acute tolerance that could affect alcohol response.
Participants were 81 current drinkers (n = 39 with a current diagnosis of BPD). The sample was 67.9% female with a mean age of 24.2 (age range 21–30 years, SD = 2.5). The majority of participants identified as White/European American (71.6%); 19.8% identified as Black/African American; 8.7% identified as Asian or another race. Twenty-one percent of participants reported an annual household income of under $10,000; an additional 28.4% reported $24,000 or less, and 27.2% reported $39,000 or less (the remaining 23.4% reported earning between $40,000 and over $100,000 annually).
Study Design
Study procedures were approved by the University of Pittsburgh Institutional Review Board. All participants completed an interview session to ascertain Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, diagnoses (American Psychiatric Association, 2013). Participants were required to have five or more current BPD symptoms as determined by a semistructured clinical interview (described below) to be enrolled in the BPD group. Participants in the non-BPD group were required to have two or fewer BPD symptoms and to not meet diagnostic criteria for any additional personality disorders. We did not exclude participants from either group for other comorbid psychopathology, with the exception of meeting diagnostic criteria for psychotic disorders or bipolar disorders at the time of the interview. During this interview session, participants also completed a demographics questionnaire and reported on five domains of impulsivity. Participants were then scheduled to complete a within-subjects alcohol administration protocol and were randomized to first complete either a nonalcohol beverage session or an alcohol session within ~ 1 week of the interview session (findings to be published elsewhere). Participants completed the other beverage session ~ 1 week after the first visit. Upon completion of the nonalcohol beverage session, participants completed a questionnaire battery. The current study uses the data collected in this self-report assessment. Participants were compensated with $75.00 for completion of the interview session, $150.00 for completion of the alcohol session, and $75.00 for the nonalcohol beverage session.
Measures
Borderline personality disorder (BPD = 1, non-BPD = 0).
The Structured Interview for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Personality Disorders (SIDP-IV; Pfolh, Blum, & Zimmerman, 1997) was completed to confirm the presence/absence of BPD and other personality disorders. Participants in the BPD sample were required to endorse five or more symptoms at a 2 (present—criterion is clearly present for most of the past 5 years [i.e., present at least 50% of the time during the past 5 years]) or 3 (strongly present—criterion is associated with subjective distress or some impairment in social or occupational functioning or intimate relationships).2 The non-BPD sample was required to have two or fewer BPD symptoms and not meet diagnostic threshold for any personality disorders. All interviews were conducted by bachelors- and masters-level research assistants who underwent standardized training led by the one of the study’s principal investigators (an expert in personality disorders) and her postdoctoral scholar. The training involved attending a session on administration of the SID-P and rating a standardized set of five training cases to consensus before conducting interviews. Ongoing supervision was implemented on a monthly basis to ensure accurate diagnosis. The postdoctoral scholar reviewed interview data and supervised ongoing coding reliability meetings. Ten percent of cases were viewed and rated by the interviewers and the supervisor. Scores were compared and analyzed to determine reliability ratings. Agreement for BPD was 0.96.
Demographics.
Participants reported their sex (male = 32.1%, female = 67.9%; coded as 1 = male, 2 = female) and age. Additionally, participants identified their race via self-report (1 = White, 2 = non-White). These demographic variables were included as covariates in analyses.
Drinking motives.
Reasons for drinking were assessed with the widely used Drinking Motives Questionnaire Revised (Cooper, 1994; Kuntsche, Knibbe, Gmel, & Engels, 2006). The Drinking Motives Questionnaire is a 20-item Likert-style (1 = almost never/never to 4 = almost always) questionnaire that assesses four distinct domains of motives (five items/domain): Social (e.g., “to be sociable”), Coping (e.g., “to forget your worries”), Enhancement (e.g., “to get high”), and Conformity (e.g., “to be liked”). In the current study, reliability for the four factors ranged from acceptable to high (α = .78 for Sociability; α = .79 for Coping; α = .80 for Enhancement; α = .81 for Conformity).
Frequency of alcohol use and typical quantity of drinks per occasion.
Alcohol use in the past 12 months and in the past 30 days were assessed with a modified Substance Use Questionnaire (Molina & Pelham, 2003), which includes questions about alcohol use adapted from existing measures (Jessor, Donovan, & Costa, 1989; National Household Survey on Drug Abuse, 1992). The current study utilized typical past year alcohol frequency and past month quantity of drinks per occasion to describe the sample’s drinking behavior.
Alcohol problems.
The 23-item Rutgers Alcohol Problems Inventory (response options: 0 = none or not in the past year to 3 = more than five times) was used to assess past year alcohol problems (e.g., neglected your responsibilities; had withdrawal symptoms, that is, felt sick because you stopped or cut down on drinking). The Rutgers Alcohol Problems Inventory has been shown to have good reliability and has been used with both clinical and nonclinical adolescent and young adult samples (e.g., Dick, Aliev, F., Viken, R., Kaprio, J., & Rose, 2011; Levy & Earleywine, 2003; White & Labouvie, 1989). Individual drinking problem items endorsed in the past year were dichotomized (yes/no) and summed to create an alcohol problems score used in current analyses (range 0–22; M = 4.31; SD = 4.45; skewness: 0.30; kurtosis = −1.05). This score captures the number of distinct drinking-related problems endorsed over the previous year.
Substantive covariates.
Impulsivity.
Five impulsivity facets were assessed using the 59-item Urgency, Premeditation (lack of), Perseverance (lack of), Sensation Seeking, Positive Urgency, Impulsive Behavior Scale (UPPS-P; Cyders et al., 2007; Whiteside & Lynam, 2001): Lack of Planning (11 items: α = .86; e.g., “My thinking is usually careful and purposeful”), Sensation Seeking (12 items: α = .90; e.g., “I generally seek new and exciting experiences and sensations”), Negative Urgency (12 items: α = .94; e.g., “In the heat of an argument, I will often say things that I later regret”), Positive Urgency (14 items: α = .96; e.g., “When I am really excited, I tend not to think of the consequences of my actions”), and Lack of Perseverance (10 items: α = .89; e.g., “I generally like to see things through to the end”). Response options ranged from 1 (agree strongly) to 4 (disagree strongly). All responses were coded so that higher numbers meant higher impulsivity.
Affective instability.
The Personality Assessment Inventory Affective subscale (Morey, 1991) was used to measure affective instability. This subscale contains six items scored on a 4-point scale (0 = false, not at all true to 3 = very true) that are summed to create an affective instability index. Internal reliability for this scale was good within the current sample (α = .80).
Results
There were no significant differences between the BPD and non-BPD groups on demographic variables such as age, F(1, 79) = 2.69, p = .11, race, F(1, 79) = 3.31, p = .07, and income, F(1, 79) = 1.41, p = .24; see Table 1. We next examined group differences in alcohol use patterns, drinking motives, affective instability, and impulsivity with an analysis of variance (see Table 2). As hypothesized, participants in the BPD group experienced a significantly higher number of different alcohol-related problems over the previous year, F(1, 77) = 22.26, p < .001. They reported an average of 12 different problems (range = 1–22, SD = 6), whereas those in the non-BPD group reported an average of 6.4 (range = 0–18, SD = 4.4). Importantly, although the groups differed on the number of alcohol problems they experienced as a result of drinking, they did not differ in alcohol use involvement (see Table 2). For example, both groups reported an average of 7.2 drinks on a typical day when they consumed alcohol (BPD group range = 3–9, SD = 1.5; non-BPD group range = 5–10, SD = 1.4). Consistent with previous research, those in the BPD group also reported more affective instability, and higher scores on three domains of impulsivity (negative urgency, lack of perseverance, and positive urgency) compared with individuals without BPD. Significant group differences also emerged for two of the four domains of alcohol use motives—drinking to cope, F(1, 77) = 13.28, p > .001, and drinking for conformity, F(1, 77) = 6.09, p = .02. Those with BPD reported higher levels of both drinking to cope and conformity motives compared with the non-BPD group.
Table 1.
Demographic Characteristics of the Sample
| Variable | Non-BPD group (n = 42) | BPD group (n = 39) |
|---|---|---|
| M (SD)/n | M (SD)/n | |
| Age | 23.79 (2.38) | 24.69 (2.59) |
| Sex | ||
| Male | 13 (31%) | 13 (33.3%) |
| Female | 29 (69%) | 26 (66.6%) |
| Race | ||
| Caucasian | 31 (73.8%) | 27 (69.2%) |
| African American | 6 (14.3%) | 10 (25.6%) |
| Asian | 3 (7.1%) | 2 (5.1%) |
| Pacific Islander/Native Hawaiian | — | — |
| American Indian/Alaskan Native | — | — |
| Other | 2 (4.8%) | — |
| Ethnicity | ||
| Hispanic | 1 (2.4%) | — |
| Non-Hispanic | 41 (97.6%) | 39 (100%) |
| Education level | ||
| No high school diploma or GED | 1 (2.4%) | 0 (0%) |
| High school graduate or GED | 3 (7.1%) | 5 (12.8%) |
| Some college | 17 (40.5%) | 20 (51.3%) |
| College graduate | 9 (21.4%) | 11 (28.2%) |
| Postcollege education | 12 (28.6%) | 3 (7.7%) |
| Estimated household income | ||
| >$10,000 | 8 (19%) | 9 (23.1%) |
| $10,000-$24,000 | 9 (21.4%) | 14 (35.9%) |
| $25,000-$39,000 | 13 (31%) | 9 (23.1%) |
| $40,000-$54,000 | 3 (7.1%) | 1 (2.6%) |
| $55,000-$75,000 | 2 (4.8%) | 2 (5.1%) |
| $76,000-$100,000 | 3 (7.1%) | 1 (2.6%) |
| <$100,000 | 4 (9.5%) | 3 (7.7%) |
Note. BPD = borderline personality disorder; GED = general equivalency diploma.
Table 2.
Differences in Alcohol Use Patterns, Drinking Motives, Affective Instability, and Impulsivity Among BPD and Non-BPD Participants
| Variable | Non-BPD group | BPD group | ANOVA | |
|---|---|---|---|---|
| M (SD) | M (SD) | F (df1, df2) | P | |
| BPD symptom count | 0.88 (0.71) | 5.82 (0.97) | F (1, 79) = 649.22 | <.001 |
| Drinking motives | ||||
| Sociability | 3.16 (0.54) | 3.11 (0.60) | F (1, 77) = 0.16 | .69 |
| Coping | 1.99 (0.57) | 2.52 (0.72) | F (1, 77) = 13.28 | <.001 |
| Enhancement | 2.70 (0.63) | 2.78 (0.66) | F (1, 77) = 0.36 | .55 |
| Conformity | 1.45 (0.50) | 1.78 (0.68) | F (1, 77) = 6.09 | .02 |
| Affective instability | 1.96 (0.54) | 2.92 (0.93) | F (1, 77) = 64.23 | <.001 |
| Number of different alcohol-related problems over the past year | 6.42 (4.36) | 11.95 (5.99) | F (1, 77) = 22.26 | <.001 |
| Number of drinks on a typical drinking day over the past year | 7.21 (1.40) | 7.29 (1.41) | F (1, 71) = 0.001 | .98 |
| Number of drinking days in the past month | 10.0 (6.53) | 11.24 (7.13) | F (1, 77) = 0.65 | .42 |
| UPPS | ||||
| Negative urgency | 1.93 (0.59) | 2.79 (0.72) | F (1, 79) = 35.15 | <.001 |
| Lack of premeditation | 1.81 (0.49) | 1.94 (0.49) | F (1, 79) = 1.28 | .26 |
| Lack of perseverance | 1.74 (0.51) | 2.18 (0.65) | F (1, 79) = 11.22 | .001 |
| Sensation seeking | 2.84 (0.68) | 2.62 (0.72) | F (1, 79) = 1.97 | .16 |
| Positive urgency | 1.55 (0.53) | 2.14 (0.76) | F (1, 79) = 16.91 | <.001 |
Note. BPD = borderline personality disorder; ANOVA = analysis of variance; UPPS = Urgency, Premeditation (lack of), Perseverance (lack of), Sensation Seeking, Positive Urgency, Impulsive Behavior Scale (UPPS-P).
We next conducted a linear regression with coping and conformity motives predicting reported alcohol problems. We accounted for participant sex, race, and mean centered age in this analysis and all subsequent analyses. Both coping and conformity motives were significant predictors of alcohol problems (p < .001 and p = .01, respectively). Coping and conformity motives accounted for ~ 37.5% of the variance in alcohol-related problems above and beyond the effects of covariates (R2= 0.37), F(2, 76) = 22.36, p < .001.
We next conducted a parallel mediation analysis using ordinary least squares path analysis via the PROCESS macro for SPSS Version 3.1 (Hayes, 2017). Given the results of our regression analyses, we investigated the relations between BPD and number of participants’ distinct drinking problems over the previous year via coping (M1) and conformity motives (M2; see Figure 1). Results indicated that BPD remains directly related to drinking problems (c’ = 3.42; ). Individuals in the BPD group endorsed an average of 3.42 additional drinking problems over the previous year compared with those in the non-BPD group. As hypothesized, BPD also indirectly related to drinking problems through its effect on drinking to cope motives. A bootstrap confidence interval for the indirect effect of drinking to cope (a1b1 =0.32) based on 5,000 bootstrap samples was entirely above zero (0.14 to 0.55). Drinking for conformity also partially accounted for the relation between BPD and drinking problems (a2b2 = 0.11) as the confidence interval based on 5,000 bootstrap samples was entirely above zero (0.004 to 0.27); the point estimate of the difference between these specific indirect effects was 0.21 and a 95% confidence interval straddles 0 [−0.05, 0.49]. Thus, the indirect effects of coping and conformity were not significantly different from each other.
Figure 1.
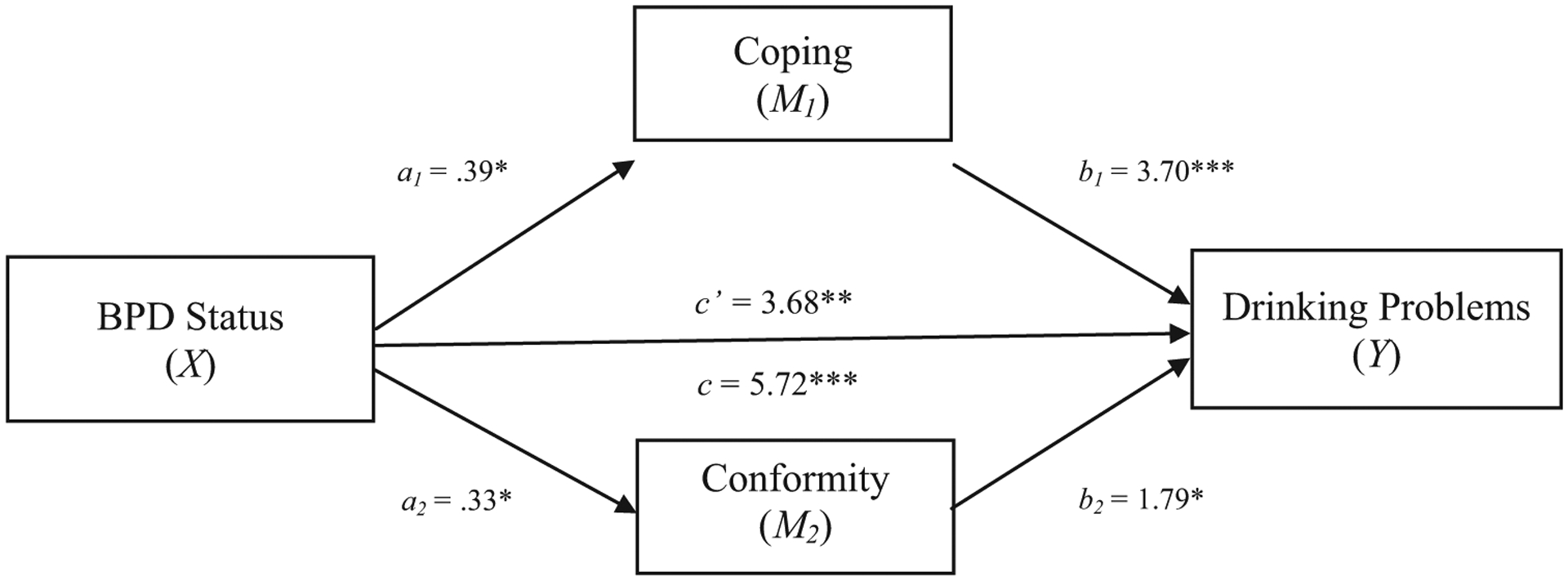
Parallel mediation using the mediating effect of two motivations for drinking (coping and conformity/social pressure) in the relation between BPD status and number of different drinking-related problems experienced over the previous year. We controlled for participant age, race, sex, and number of drinking days over the past month. Notes: an is the effect of BPD on drinking motive dimensions; participants without BPD are coded as 0 and participants with BPD as 1; bn is effect of drinking motive dimensions on number of drinking problems; c’ is direct effect of BPD status on drinking problems; and c is the total effect of BPD status on drinking problems using partially standardized coefficients.4 * p < .05; ** p < .01; *** p < .001.
We next conducted a series of mediation models to explore whether the relation between BPD and alcohol-related problems via coping and conformity motives would remain significant when also accounting for affective instability and impulsivity. Earlier analyses indicated our groups differed on indices of affective instability, and three types of impulsivity. Thus, we examined affective instability, urgency (positive and negative urgency were included in the same model), and lack of perseverance in three separate models to parse out which dimensional constructs might be underlying the association between BPD and alcohol problems. When including affective instability as a covariate, the direct effect of BPD group on drinking problems remained significant (c’ = 3.00; ). However, the indirect effects of coping and conformity were no longer significant (a1b1 =0.05,[−0.20, 0.32]; a2b2 = 0.11, CI [−0.01, 0.31]). When including negative and positive urgency as covariates, the direct effect of BPD group again remained directly related to drinking problems (c’ = 3.48; ). In this urgency model, coping motives mediated the relation between BPD group and alcohol problems. A bootstrap confidence interval for the indirect effect of drinking to cope (a1b1 = 0.22) based on 5,000 bootstrap samples was entirely above zero (0.02 to 0.46). However, conformity no longer mediated the relation between BPD group and drinking problems.
Finally, we investigated the effects of including the impulsivity domain capturing lack of perseverance (e.g., ability to finish tasks). The resulting model revealed the direct effect of BPD group remained directly related to drinking problems (c’ = 3.68; ), and both the indirect effect of coping and conformity were significant. A bootstrap confidence interval for the indirect effect of drinking to cope (a1b1 = 0.25) based on 5,000 bootstrap samples was entirely above zero (0.04 to 0.48), as was the indirect effect of drinking for conformity (a2b2 = 0.10) with a confidence interval ranging from 0.003 to 0.27.
Discussion
Previous research has consistently demonstrated that individuals with BPD are at increased risk for experiencing alcohol problems relative to individuals without BPD. Identifying malleable treatment targets that could decrease this risk is needed, especially in light of the poorer outcomes for individuals with this comorbidity (Goldstein, 2004; Links et al., 1995). In the current study, we significantly expanded on existing literature by (a) comparing alcohol problems among drinkers with and without BPD who have comparable levels of alcohol use, (b) testing four domains of drinking motives as potential pathways linking BPD and alcohol-related problems, and (c) evaluating these associations above and beyond other core dimensional contributors to BPD/alcohol problems (affective instability and impulsivity).
Interestingly, although participants across both groups reported similar patterns of drinking behavior (endorsing comparable rates of drinking days [frequency] over the previous year and identical rates of alcoholic beverage consumption on typical drinking days), those with BPD experienced significantly more problems associated with their alcohol use. Thus, those with BPD appear to be at higher risk when they drink. Our results indicate processes that unfold while an individual with BPD is consuming alcohol may disproportionately increase risk in this population. Additional research is needed to explore why this might be the case. Perhaps those with BPD are more likely to become disinhibited when drinking, drink when particularly dysregulated, or drink in chaotic/unsafe environments where the consequences for excessive use are particularly severe. Ecological momentary assessment data demonstrate that individuals with BPD consume alcohol more rapidly than community individuals during a drinking episode and that rate of consumption is associated with subjective stimulation, increased positive affect (enhancement effects), and reduced negative affect (drinking to cope; Carpenter et al., 2017). Interpersonal dysregulation is a core feature of BPD (APA, 2013) and may interact with drinking behavior to exacerbate interpersonal conflict and subsequent emotion dysregulation. Research testing BPD participants’ acute response to alcohol across various social settings may be particularly beneficial in understanding these poor drinking-related outcomes.
In line with results from college and community samples with low BPD symptom endorsement (Tragesser et al., 2007),3 we found that drinking to cope with negative mood and drinking to fit in with peers or in social settings (conformity motives) partially accounted for the association between BPD and alcohol problems. BPD is characterized by severe difficulties with interpersonal relationships and emotional functioning (APA, 2013). Individuals with BPD have heightened emotional sensitivity, increased stress reactivity, and attentional bias to cues of social threat rejection (Linehan, 1993; Smeijers, Rinck, Bulten, van den Heuvel, & Verkes, 2017; Winter, Koplin, Schmahl, Bohus, & Lis, 2016). Leading theories suggest impulsive behavior and the use of maladaptive coping methods often arise in response to emotion dysregulation among those with BPD (Linehan, 1993; Selby & Joiner, 2009). Although research on conformity motives has less consistently shown associations with alcohol compared with coping motives, it may be more relevant for individuals with higher levels of anxiety sensitivity and/or self-consciousness (Cooper et al., 2016). Previous research demonstrates that those with BPD are more likely to drink in response to cravings in a variety of social contexts (e.g., while at work, when with romantic partners, children, and coworkers; Lane et al., 2016)—consistent with literature showing conformity motives are related to avoidance of social embarrassment. Our results support the possibility that individuals with BPD are drinking alcohol to reduce social discomfort.
Our findings have important clinical and prevention implications. Drinking to cope with negative mood and to socially conform each reflect motivations for using alcohol related to removal of an aversive stimuli. The pathways through coping and conformity motives were no longer significant when affective instability was included in our model. This points to the potential importance of reducing affective instability to lower the motivation to drink to cope or to fit in for this population. Offering alternative methods of managing uncomfortable or painful states and/or fitting in with others socially may represent particularly important targets for intervention efforts that decrease these reasons for drinking. Available treatments for alcohol misuse and BPD such as dialectical behavior therapy offer skills designed for tolerating distress and building emotion regulation skills (Linehan, 1993). However, conformity-related needs may be less directly addressed. Focusing on these deficits could ultimately reduce alcohol problems.
Additionally, promising research shows that reasons for drinking are malleable with intervention. Providing feedback to challenge drinking to cope with negative mood is effective for reducing these motives over a 2-month period (Blevins & Stephens, 2016). This type of targeted feedback may be especially important for individuals with BPD, as these individuals display elevated levels of drinking to cope (the drinking motive most consistently shown to predict alcohol problems; Littlefield et al., 2010). Future research is needed to determine whether streamlining interventions to focus on negative reinforcement targets facilitate reductions in alcohol use more rapidly or effectively than whole-program implementation for BPD. It is possible that frontloading skills to address coping and conformity motives may function to increase client commitment to treatment and more rapidly reduce problem drinking.
Importantly, our study is the first to demonstrate that the association between BPD and alcohol problems remains even when accounting for three domains of impulsivity and affective instability. These findings suggest that other symptoms of BPD (e.g., interpersonal difficulties, chronic emptiness, identity disturbance) are also notably contributing to alcohol problems. Research is needed to directly test this possibility. Focusing solely on affect regulation or delaying decision making may overlook important contributors to alcohol problems in this population.
This study has both notable strengths and limitations. Our sample was unique in that we ascertained participants who met criteria for BPD, included a community sample with a range of psychiatric illness who engaged in the same level of alcohol use as our BPD sample, and included semistructured interview to determine BPD as opposed to relying solely on self-report questionnaires (as has been done in other studies). Although well characterized, our sample was relatively homogenous with regard to race and ethnicity and potentially underpowered to detect some effects. Our BPD sample also demonstrated higher levels of psychopathology compared with our non-BPD sample. Although we accounted for dimensional measures of affective instability and impulsivity, our sample was too small to allow for in-depth exploration of multiple comorbidities that could be driving results (e.g., elevated levels of depression). We used a BPD-specific measure of affective lability, whereas our impulsivity instrument captured domains of impulsivity more broadly. Future studies should utilize a non–BPD-specific affective lability scale to ensure results remain consistent.
Additionally, the data we present are cross-sectional in nature, and thus, we cannot make claims of causality for our effects. Furthermore, motivations to use alcohol may be subject to change, and longitudinal research is needed to assess the stability of the patterns we observed. Real-time analyses of reasons for drinking are needed to unpack if drinking to cope predicts specific drinking episodes that end in problems (e.g., arguing) more often than occasions when an individual is drinking to celebrate or fit in socially. Lastly, we did not assess motives to use other substance use besides alcohol. Future research focused on understanding if reasons for using drugs, such as marijuana, are similar as what was found for alcohol is needed.
Findings from the current study contribute substantively to existing literature and increase our understanding of why individuals with BPD may be particularly at risk for experiencing alcohol problems. The present study demonstrated that drinkers with BPD may be especially vulnerable to negative outcomes associated with their alcohol use compared with individuals without BPD—even at similar levels of alcohol involvement. These findings point to the importance of future research examining experiences that occur while individuals with BPD are drinking as opposed to focusing on decisions to drink. This association remained even when indices of impulsivity and affective instability were included in our models. Thus, BPD as a heterogeneous disorder appears to explain more of the variance in alcohol use problems above and beyond affective instability and impulsivity, core shared features of BPD and heavy drinking. This study also bolstered support for the role of coping motives as an important pathway contributing to alcohol problems for individuals with BPD. However, coping was no longer a significant mediator with affective instability included in our model. This finding may indicate affective instability is driving elevated coping motives for individuals with BPD and is consistent with previous research documenting that these individuals often use ineffective coping strategies when emotionally distressed (Linehan, 1993). These findings highlight the importance of assessing reasons for drinking among individuals with BPD and for increased research on experiences while drinking for this vulnerable population.
Acknowledgments
This research and the efforts of the authors were supported by grants from the National Institute on Alcohol Abuse and Alcoholism (R21 AA023180; Multiple Principal Investigators: Stephanie D. Stepp and Sarah L. Pedersen).
Footnotes
Laboratory dosing was calculated using participants’ age (for males), sex assigned at birth, height, and weight to determine the alcohol amount needed to achieve a breath alcohol concentration (BrAC) of 0.08%.
To meet criteria for impulsivity, two endorsements of impulsive behaviors from a list (which included getting drunk and getting high) at threshold levels were required (e.g., 10+ times a year). Many participants endorsed getting drunk and high. However, if these were the only impulsive behaviors endorsed, a third behavior was required to meet criteria. Thus, impulsivity wasn’t conflated with alcohol and substance use.
It is notable that results are consistent across samples with a range of BPD symptom severity. Consistency among those with BPD features and full BPD diagnosis lend support to the utility of dimensional perspectives of personality pathology (Hopwood et al., 2018).
The use of standardized effects are not recommended when X is a dichotomous variable (see Hayes, 2017).
Contributor Information
Erin A. Kaufman, Department of Psychology, University of Western Ontario;
Jessica Perez, Department of Psychology, University of Vermont;.
Sophie Lazarus, Department of Psychiatry and Behavioral Health, The Ohio State University Wexner Medical Center;.
Stephanie D. Stepp, Department of Psychiatry, University of Pittsburgh School of Medicine.
Sarah L. Pedersen, Department of Psychiatry, University of Pittsburgh School of Medicine.
References
- Adams ZW, Kaiser AJ, Lynam DR, Charnigo RJ, & Milich R (2012). Drinking motives as mediators of the impulsivity-substance use relation: Pathways for negative urgency, lack of premeditation, and sensation seeking. Addictive Behaviors, 37, 848–855. 10.1016/j.addbeh.2012.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Axelrod SR, Perepletchikova F, Holtzman K, & Sinha R (2011). Emotion regulation and substance use frequency in women with substance dependence and borderline personality disorder receiving dialectical behavior therapy. The American Journal of Drug and Alcohol Abuse, 37, 37–42. 10.3109/00952990.2010.535582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball SA, Tennen H, Poling JC, Kranzler HR, & Rounsaville BJ (1997). Personality, temperament, and character dimensions and the DSM–IV personality disorders in substance abusers. Journal of Abnormal Psychology, 106, 545–553. 10.1037/0021-843X.106.4.545 [DOI] [PubMed] [Google Scholar]
- Blevins CE, & Stephens RS (2016). The impact of motives-related feedback on drinking to cope among college students. Addictive Behaviors, 58, 68–73. 10.1016/j.addbeh.2016.02.024 [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Lejuez CW, Daughters SB, Rosenthal MZ, & Lynch TR (2005). Impulsivity as a common process across borderline personality and substance use disorders. Clinical Psychology Review, 25, 790–812. 10.1016/j.cpr.2005.05.005 [DOI] [PubMed] [Google Scholar]
- Carpenter RW, Trela CJ, Lane SP, Wood PK, Piasecki TM, & Trull TJ (2017). Elevated rate of alcohol consumption in borderline personality disorder patients in daily life. Psychopharmacology, 234, 3395–3406. 10.1007/s00213-017-4727-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen EY, Brown MZ, Lo TTY, & Linehan MM (2007). Sexually transmitted disease rates and high-risk sexual behaviors in borderline personality disorder versus borderline personality disorder with substance use disorder. Journal of Nervous and Mental Disease, 195, 125–129. 10.1097/01.nmd.0000254745.35582.f6 [DOI] [PubMed] [Google Scholar]
- Chugani CD, Byrd AL, Pedersen SL, Chung T, Hipwell AE, & Stepp SD (2018). Affective and sensation-seeking pathways linking borderline personality disorder symptoms and alcohol-related problems in young women. Journal Of Personality Disorders. Advance online publication. 10.1521/pedi_2018_32_389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey SF, Schumacher JA, Baschnagel JS, Hawk LW, & Holloman G (2011). Impulsivity and risk-taking in borderline personality disorder with and without substance use disorders. Personality Disorders, 2, 128–141. 10.1037/a0020574 [DOI] [PubMed] [Google Scholar]
- Cooper ML (1994). Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment, 6, 117–128. 10.1037/1040-3590.6.2.117 [DOI] [Google Scholar]
- Cooper ML, Agocha VB, & Sheldon MS (2000). A motivational perspective on risky behaviors: The role of personality and affect regulatory processes. Journal of Personality, 68, 1059–1088. 10.1111/1467-6494.00126 [DOI] [PubMed] [Google Scholar]
- Cooper ML, Kuntsche E, Levitt A, Barber LL, & Wolf S (2016). Motivational models of substance use: A review of theory and research on motives for using alcohol, marijuana, and tobacco. In Sher KJ (Ed.), The Oxford handbook of substance use and substance use disorders (Vol. 1, pp. 375–421). New York, NY: Oxford University Press. [Google Scholar]
- Crowell SE, Beauchaine TP, & Linehan MM (2009). A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychological Bulletin, 135, 495–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Smith GT, Spillane NS, Fischer S, Annus AM, & Peterson C (2007). Integration of impulsivity and positive mood to predict risky behavior: Development and validation of a measure of positive urgency. Psychological Assessment, 19, 107–118. 10.1037/1040-3590.19.1.107 [DOI] [PubMed] [Google Scholar]
- Dick DM, Aliev F, Viken R, Kaprio J, & Rose RJ (2011). Rutgers Alcohol Problem Index scores at age 18 predict alcohol dependence diagnoses 7 years later. Alcoholism: Clinical and Experimental Research, 35, 1011–1014. 10.1111/j.1530-0277.2010.01432.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein EG (2004). Substance abusers with borderline disorders. In Straussner SLA(Ed.), Clinical work with substance-abusing clients (2nd ed., pp. 370–391). New York, NY: Guilford Press. [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, & Ruan WJ (2005). Co-occurrence of DSM–IV personality disorders in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Comprehensive Psychiatry, 46, 1–5. 10.1016/j.comppsych.2004.07.019 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (2nd ed.). New York, NY: Guilford Press. [Google Scholar]
- Hopwood CJ, Kotov R, Krueger RF, Watson D, Widiger TA, Althoff RR,… Zimmermann J (2018). The time has come for dimensional personality disorder diagnosis. Personality and Mental Health, 12, 82–86. 10.1002/pmh.1408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahng S, Solhan MB, Tomko RL, Wood PK, Piasecki TM, & Trull TJ (2011). Affect and alcohol use: An ecological momentary assessment study of outpatients with borderline personality disorder. Journal of Abnormal Psychology, 120, 572–584. 10.1037/a0024686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jessor R, Donovan JE, & Costa FM (1989). Health Behavior Questionnaire. Boulder, CO: Institute of Behavioral Science, University of Colorado. [Google Scholar]
- Kendler KS, Myers J, & Reichborn-Kjennerud T (2011). Borderline personality disorder traits and their relationship with dimensions of normative personality: A web-based cohort and twin study. Acta Psychiatrica Scandinavica, 123, 349–359. 10.1111/j.1600-0447.2010.01653.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF (2013). Negative reinforcement in drug addiction: The darkness within. Current Opinion in Neurobiology, 23, 559–563. 10.1016/j.conb.2013.03.011 [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, & Engels R (2006). Replication and Validation of the Drinking Motive Questionnaire Revised (DMQ-R, Cooper, 1994) among adolescents in Switzerland. European Addiction Research, 12, 161–168. 10.1159/000092118 [DOI] [PubMed] [Google Scholar]
- Lane SP, Carpenter RW, Sher KJ, & Trull TJ (2016). Alcohol craving and consumption in borderline personality disorder: When, where, and with whom. Clinical Psychological Science, 4, 775–792. 10.1177/2167702615616132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus SA, Beardslee J, Pedersen SL, & Stepp SD (2017). A within-person analysis of the association between borderline personality disorder and alcohol use in adolescents. Journal of Abnormal Child Psychology, 45, 1157–1167. 10.1007/s10802-016-0225-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy B, & Earleywine M (2003). Reinforcement expectancies for studying predict drinking problems among college students: Approaching drinking from an expectancies choice perspectives. Addictive Behaviors, 28, 551–559. 10.1016/S0306-4603(01)00250-7 [DOI] [PubMed] [Google Scholar]
- Linehan M (1993). Cognitive-behavioral treatment of borderline personality disorder. New York, NY: Guilford Press. [Google Scholar]
- Links PS, Heslegrave RJ, Mitton JE, van Reekum R, & Patrick J (1995). Borderline personality disorder and substance abuse: Consequences of comorbidity. Canadian Journal of Psychiatry, 40, 9–14. 10.1177/070674379504000105 [DOI] [PubMed] [Google Scholar]
- Littlefield AK, Sher KJ, & Wood PK (2010). Do changes in drinking motives mediate the relation between personality change and “maturing out” of problem drinking? Journal of Abnormal Psychology, 119, 93–105. 10.1037/a0017512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loose T, Acier D, & El-Baalbaki G (2018). Drinking motives as mediators between personality traits and alcohol use among young French people. Personality and Individual Differences, 134, 268–274. 10.1016/j.paid.2018.06.036 [DOI] [Google Scholar]
- Martins JS, Bartholow BD, Cooper ML, Von Gunten CD, & Wood PK (2018). Associations between executive functioning, affect-regulation drinking motives, and alcohol use and problems. Psychology of Addictive Behaviors, 32, 16 –28. 10.1037/adb0000324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller FT, Abrams T, Dulit R, & Fyer M (1993). Substance abuse in borderline personality disorder. American Journal of Drug and Alcohol Abuse, 19, 491–497. 10.3109/00952999309001637 [DOI] [PubMed] [Google Scholar]
- Molina BSG, & Pelham WE Jr. (2003). Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. Journal of Abnormal Psychology, 112, 497–507. 10.1037/0021-843X.112.3.497 [DOI] [PubMed] [Google Scholar]
- Morey LC (1991). Personality assessment inventory: Professional manual. Odessa, FL: Psychologcal Assessment Resources. [Google Scholar]
- Morgenstern J, Langenbucher J, Labouvie E, & Miller KJ (1997). The comorbidity of alcoholism and personality disorders in a clinical population: Prevalence rates and relation to alcohol typology variables. Journal of Abnormal Psychology, 106, 74–84. 10.1037/0021-843X.106.1.74 [DOI] [PubMed] [Google Scholar]
- National Household Survey on Drug Abuse (NHSDA). (1992). OMB No. 0930–0110. Washington, DC: U.S. Department of Health and Human Services, Public Health Service, and Alcohol, Drug Abuse and Mental Health Administration, National Institute on Drug Abuse. [Google Scholar]
- Pfolh B, Blum N, & Zimmerman M (1997). Structured Interview for DSM–IV Personality: SIDP–IV. Iowa City, IA: American Psychiatric Press. [Google Scholar]
- Selby EA, & Joiner TE Jr. (2009). Cascades of emotion: The emergence of borderline personality disorder from emotional and behavioral dysregulation. Review of General Psychology, 13, 219–229. 10.1037/a0015687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher KJ, & Trull TJ (2002). Substance use disorder and personality disorder. Current Psychiatry Reports, 4, 25–29. 10.1007/s11920-002-0008-7 [DOI] [PubMed] [Google Scholar]
- Sher KJ, Trull TJ, Bartholow BD, & Vieth A (1999). Personality and alcoholism: Issues, methods, and etiological processes. In Leonard KE& Blane HT (Eds.), Psychological theories of drinking and alcoholism (2nd ed., pp. 54–105). New York, NY: Guilford Press. [Google Scholar]
- Skodol AE, Oldham JM, & Gallaher PE (1999). Axis II comorbidity of substance use disorders among patients referred for treatment of personality disorders. The American Journal of Psychiatry, 156, 733–738. Retrieved from https://ajp.psychiatryonline.org/doi/pdf/10.1176/ajp.156.5.733 [DOI] [PubMed] [Google Scholar]
- Smeijers D, Rinck M, Bulten E, van den Heuvel T, & Verkes RJ (2017). Generalized hostile interpretation bias regarding facial expressions: Characteristic of pathological aggressive behavior. Aggressive Behavior, 43, 386–397. 10.1002/ab.21697 [DOI] [PubMed] [Google Scholar]
- Stepp SD, Trull TJ, & Sher KJ (2005). Borderline personality features predict alcohol use problems. Journal of Personality Disorders, 19, 711–722. 10.1521/pedi.2005.19.6.711 [DOI] [PubMed] [Google Scholar]
- Stevens AK, Blanchard BE, & Littlefield AK (2018). Impulsive dispositions and alcohol: What we know, how we know it, and where to go from here. Borderline Personality Disorder and Emotion Dysregulation, 5, 4. 10.1186/s40479-018-0081-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart SH, & Devine H (2000). Relations between personality and drinking motives in young adults. Personality and Individual Differences, 29, 495–511. 10.1016/S0191-8869(99)00210-X [DOI] [Google Scholar]
- Tragesser SL, Sher KJ, Trull TJ, & Park A (2007). Personality disorder symptoms, drinking motives, and alcohol use and consequences: Cross-sectional and prospective mediation. Experimental and Clinical Psychopharmacology, 15, 282–292. 10.1037/1064-1297.15.3.282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull TJ, Freeman LK, Vebares TJ, Choate AM, Helle AC, & Wycoff AM (2018). Borderline personality disorder and substance use disorders: An updated review. Borderline Personality Disorder and Emotion Dysregulation, 5, 15. 10.1186/s40479-018-0093-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull TJ, Sher KJ, Minks-Brown C, Durbin J, & Burr R (2000). Borderline personality disorder and substance use disorders: A review and integration. Clinical Psychology Review, 20, 235–253. 10.1016/S0272-7358(99)00028-8 [DOI] [PubMed] [Google Scholar]
- Vest NA, Murphy KT, & Tragesser SL (2018). Borderline personality disorder features and drinking, cannabis, and prescription opioid motives: Differential associations across substance and sex. Addictive Behaviors, 87, 46 –54. 10.1016/j.addbeh.2018.06.015 [DOI] [PubMed] [Google Scholar]
- Walter M, Gunderson JG, Zanarini MC, Sanislow CA, Grilo CM, McGlashan TH,… Skodol AE (2009). New onsets of substance use disorders in borderline personality disorder over 7 years of follow-ups: Findings from the collaborative longitudinal personality disorders study. Addiction, 104, 97–103. 10.1111/j.1360-0443.2008.02413.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- White HR, & Labouvie EW (1989). Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol, 50(1), 30–37. 10.15288/jsa.1989.50.30 [DOI] [PubMed] [Google Scholar]
- Whiteside SP, & Lynam DR (2001). The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences, 30, 669–689. 10.1016/S0191-8869(00)00064-7 [DOI] [Google Scholar]
- Winter D, Koplin K, Schmahl C, Bohus M, & Lis S (2016). Evaluation and memory of social events in borderline personality disorder: Effects of valence and self-referential context. Psychiatry Research, 240, 19–25. 10.1016/j.psychres.2016.03.042 [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, & Reynolds V (1998). Axis I comorbidity of borderline personality disorder. American Journal of Psychiatry, 155, 1733–1739. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Vujanovic AA, Parachini EA, Boulanger JL, Frankenburg FR, & Hennen J (2003). A screening measure for BPD: The McLean screening instrument for borderline personality disorder (MSI-BPD). Journal of Personality Disorders, 17, 568–573. [DOI] [PubMed] [Google Scholar]


