Abstract
LEAD LEVELS IN NORTH AMERICAN CHILDREN AND ADULTS have declined in the past 3 decades, but lead persists in the environment in lead paint, old plumbing and contaminated soil. There are also a number of occupations and hobbies that carry a high risk of lead exposure. There is no evidence for a threshold below which lead has no adverse health effects. Blood lead levels previously considered safe are now known to cause subtle, chronic health effects. The health effects of lead exposure include developmental neurotoxicity, reproductive dysfunction and toxicity to the kidneys, blood and endocrine systems. Most lead exposures are preventable, and diagnosing lead poisoning is relatively simple compared with diagnosing health effects of exposures to other environmental toxins. Accurate assessment of lead poisoning requires specific knowledge of the sources, high-risk groups and relevant laboratory tests. In this article we review the multiple, systemic toxic effects of lead and provide current information on groups at risk, prevention, diagnosis and clinical treatment. We illustrate how the CH2OPD2 mnemonic (Community, Home, Hobbies, Occupation, Personal habits, Diet and Drugs) and specific screening questions are useful tools for physicians to quickly obtain an environmental exposure history and identify patients at high risk of lead exposure. By applying effective primary prevention, case-finding and treatment interventions for lead exposure, both the individual patient and the larger community reap the benefits of better health.
Case
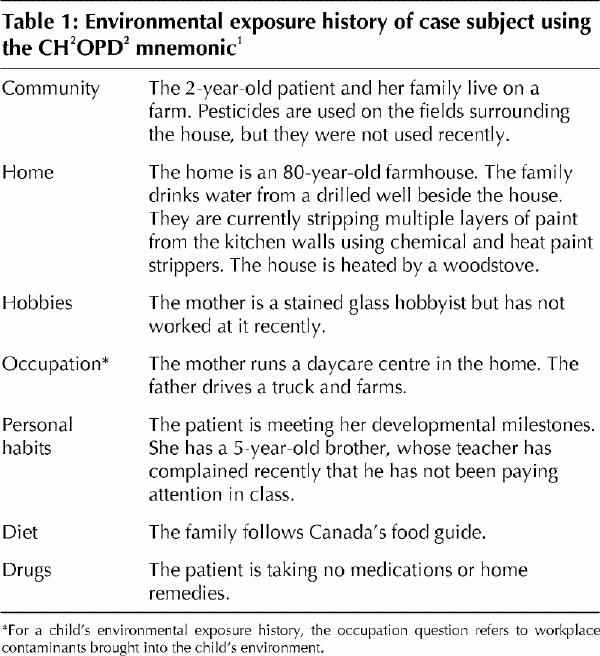
A previously healthy 2-year-old girl and her mother visit their family physician because of the daughter's 2-month history of intermittent complaints of a mild “tummy ache.” There is no associated vomiting, weight loss, or change in appetite, bowels or diet. There are no abnormal findings on physical examination. When asked about symptom onset the mother reports that it began shortly after the family started to renovate their kitchen. They live in an old farmhouse on the outskirts of town and drink water from a drilled well on the property. The physician decides to take an environmental exposure history using the CH2OPD2 mnemonic (Community, Home, Hobbies, Occupation, Personal habits, Diet and Drugs; for children, the occupation question refers to workplace contaminants brought into the child's environment).1 The child's exposure history (Table 1) reveals several potential sources of lead exposure, including the old paint removed during the kitchen renovation and lead paint peeling from other areas of the house, contamination of drinking water from lead solder in old plumbing, lead solder used by the mother for her stained glass hobby, and residual lead, from leaded gasoline and deteriorating paint from buildings, in the soil near the house and barn. The physician decides to have blood lead levels measured in all 4 family members.
Table 1
Questions surrounding this case: Is the family at risk of health effects from lead exposure? Who else might be at risk? Are other laboratory tests indicated? Where can the physician get advice on the significance of the family's blood lead levels? How should this case of lead exposure be treated?
To some extent lead is one of the small success stories of environmental health. The association of lead poisoning with cognitive impairment is well established2 and has resulted in the removal of lead from gasoline, paint and food cans. Despite these preventive measures, however, silent, low-level lead exposure continues to present a problem for many communities and populations. In 1997, data from the US National Health and Nutrition Examination Surveys showed that 4.4% of children in the United States had elevated blood lead levels.3 Black children living in older housing, children living in metropolitan areas with populations of 1 million or more and poor children living in older housing were at highest risk of exposure.3
In Canada children living near a point-source smelter in the South Riverdale area of Toronto were tested in 1973 and found to have an unusually high mean lead level (1.34 μmol/L).4 Canada's Federal–Provincial Committee on Environmental and Occupational Health suggested in 1994 that 5%–10% of Canadian children living in urban areas have blood lead levels exceeding 0.48 μmol/L, even though they are not exposed to point sources.5 The Ontario government estimated in 1994 that 4% of children in the province still had blood lead levels above 0.48 μmol/L;6 a 1992 study found that the mean level in Ontario children had fallen from 0.91 μmol/L in 1972 to 0.29 μmol/L in 1988.7 A study of Vancouver children using blood lead levels collected in 1989 found that 8% had elevated levels (mean 0.29 μmol/L).8 A later study of the children living in Trail, BC, the site of a lead and zinc smelter, demonstrated that 50% had an elevated blood lead level.9
Sources of lead and health effects
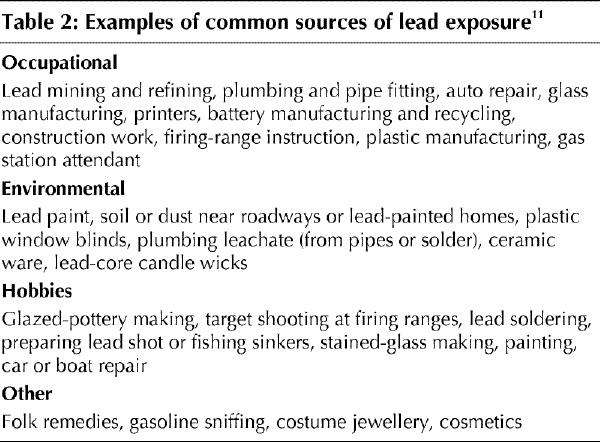
Examples of common sources of lead exposure are listed in Table 2. Sources in the community may include a nearby lead smelter or battery recycling plant. Common sources in and around the home include interior lead paint if the home was built before 1950, contaminated soil from vehicle exhaust before 1990 or from chalking of exterior paint, and lead solder from plumbing installed before 1989. Consumer products as diverse as plastic window blinds, candle wicks, costume jewellery10 and children's knapsacks have been found to contain unacceptably high lead levels. Additional common sources include hobbies using lead (e.g., stained glass and home furniture refinishing), occupational exposure of parents, and alternative medicines and home remedies (e.g., azarcon for infant colic, and the folk remedies ghasard, greta and paylooah).4,11
Table 2
In adults 20%–70% of ingested lead and nearly 100% of inhaled lead enters the blood.11 Children aged 9 months to 3 years are more vulnerable because they absorb lead 5–10 times more effectively than adults and have greater exposure because of their exploratory behaviour and frequent hand-to-mouth activity.4 Other high-risk groups include pregnant women and their fetuses4,11,12 and occupationally exposed workers and artisans and their families.4,13,14,15
Lead toxicity affects the hematologic, renal and neurologic systems. Most physicians know that lead exposure is in the differential diagnosis of microcytic anemia; lead inhibits heme synthesis and increases the rate of erythrocyte destruction.11 It is less well known that chronic, low-level lead exposure also results in glomerular and tubulointerstitial changes that lead to glycosuria, proteinuria, chronic renal failure and hypertension.13,16 A longitudinal study of renal function and lead levels in middle-aged and elderly people showed that a 10-fold increase in blood lead level predicted a decline in renal function equivalent to that caused by 20 years of aging.16 The neurotoxic effects of lead are perhaps the best known and studied.2,11,12,17 Lead disrupts the main structural components of the blood–brain barrier through primary injury of astrocytes and secondary damage to endothelial microvasculature.17 Electrophysiological studies have shown decreased auditory sensitivity and visuomotor performance in children exposed to lead, as well as increased latency in brain auditory-evoked potentials. In the brain, lead-induced damage occurs preferentially in the prefrontal cerebral cortex, hippocampus and cerebellum.17 Some of the characteristic clinical features of lead exposure — distractibility, attention deficits and memory problems2,11,12,18,19 — are consistent with injury to these anatomical areas. Recent, compelling evidence from rat studies showed a dose-dependent relation between lead exposure and decreased gene and protein expression of N-methyl-D-aspartate receptor subunits in the hippocampus, which resulted in deficits of memory, synaptic plasticity and spatial learning in a water maze.20
The epidemiologic evidence of the link between low-level lead exposure early in life and later deficits in intellectual and school performance is strong. In 1987 Bellinger and associates12 conducted a prospective study involving 249 newborns to assess the relation between prenatal lead exposure and early cognitive development. At every age tested, the subjects with high prenatal exposure (umbilical cord blood lead level >> 0.48 μmol/L) scored lower on the Bayley scale of infant mental development than did infants with lower prenatal exposure. In 1990 Needleman and colleagues2 conducted an 11-year follow-up study of 132 young adults first studied as primary schoolchildren. They discovered that those with high dentine lead levels (>> 20 ppm) at 6–7 years of age were at a considerably higher risk of dropping out of school (adjusted odds ratio [OR] 7.4, 95% confidence interval [CI] 1.4–40.7) or of having a reading disability (OR 5.8, 95% CI 1.7–19.7) than subjects with low dentine lead levels (< 10 ppm) at that age. In 1996 Needleman and collaborators18 followed 7-year-old boys for 4 years and found an association between bone lead levels and delinquent behaviour. The subjects with high lead levels were more likely than those with low levels to have attention problems, aggressiveness, and antisocial and delinquent behaviour; raters of behaviour were blinded to the boys' lead levels. Another large, longitudinal study, reported in 1997, found that 16% of boys who had high dentine lead levels at age 6–8 years were reading below the 12-year-old level at ages 16–18 (p < 0.001).19 These studies controlled for a large number of potentially confounding sociodemographic, familial and environmental factors.
In isolation, each of these studies demonstrates merely an association between lead levels and impaired mental development. However, the volume and consistency of the epidemiological evidence and the strength of the prospective, longitudinal study designs, in conjunction with evidence supporting the biologic plausability of the neurotoxicity of lead,17,20 provides persuasive evidence that low-level lead exposure results in persistent impairment of learning and other complex cognitive tasks.
Screening for lead exposure
There are 2 main populations at risk of adverse health effects from lead exposure: children aged 9 months to 3 years and people living near point sources of lead pollution. Physicians should be aware of these point sources, such as those in the well-known cases of Trail, BC, and the South Riverdale area of Toronto.4,7,15 Information on such “hot spots” should be available from the local public health department.
Finding children with high lead levels is a more complex clinical problem. Because the early signs of lead poisoning in children manifest as subtle neurobehavioural changes that affect social interaction, physicians should consider screening for lead exposure children who present with growth failure, behavioural disorders, hearing loss, speech, language or attention deficits, developmental delay, microcytic anemia or sleep problems.21 Adults presenting with glycosuria,13 unexplained neurological symptoms such as tremor, attention deficit disorder, unexplained arthralgias or headaches, or a history of occupational or hobby exposures may also require screening.4,11
In Canada neither universal nor targeted screening for lead exposure has been practised,22 even though the estimated prevalence of elevated lead levels among children is comparable to that among children in the United States (4%–5%).3,5,6 In 1998 the US Centers for Disease Control and Prevention (CDC) issued new guidelines, adopted by the American Academy of Pediatrics,11,21 that endorse universal screening in areas where 27% or more of the housing was built before 1950 and in populations in which the proportion of 1- and 2-year-old children with elevated blood lead levels is 12% or higher. Applying these criteria to the Canadian situation, 1991 census data indicated that 20% of housing in Canada was built before 1946,4 and in 2000 the Canada Mortgage and Housing Corporation estimated that 15% of housing in Canada was built before 1950 (Virginia Salares, Canada Mortgage and Housing Corporation: personal communication, 2000). Nationally these levels are below the threshold for universal screening, but in some inner-city practices in areas with high levels of both poverty and old housing, the CDC criteria are met and universal screening may be appropriate. For example, 1991 census data revealed that 47% of dwellings in the former City of Toronto were built before 1946, as compared with 20% in Ontario as a whole.23
For children living in lower-risk areas, the CDC recommends “targeted screening based on risk-assessment during specified pediatric visits.” 21 A comparison study on the cost-effectiveness of lead screening strategies in the United States suggests that risk assessment followed by a blood lead test in high-risk children is the least expensive strategy.24 In clinical practice, this risk assessment can be done by asking parents 4 questions that target common, specific sources of lead exposure (see box on preceding page).
Box 1.
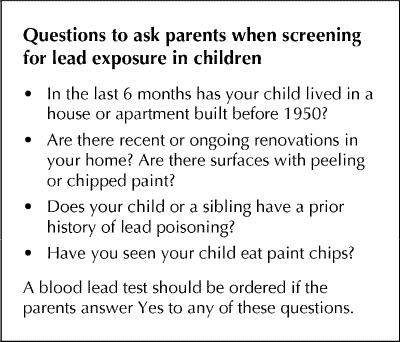
The first question reflects the fact that the age of the housing is now considered the single most important environmental marker of lead poisoning in a community.25 The 4 questions were validated in a large study (n = 4678) and were found to have a sensitivity of 75% and a specificity of 49% for detecting a blood lead level greater than 0.48 μmol/L.26 A smaller study using similar questions found a sensitivity and specificity of 75% and 39% for detecting the same blood lead level.27 Both studies showed better sensitivities for detecting higher levels.
Only a blood level is a valid and reliable measure of current lead exposure.28 Summer, when lead exposure tends to peak, is a good time to test children's levels.29 The half-life of lead in blood is 30 days, so a blood level is useful if the exposure occurred within 3 months. If the exposure occurred beyond that time, a zinc protoporphyrin test (half-life 68 days) may be helpful.11 However, this test has no significant correlation with blood lead levels, and false-positive results can occur in children with iron deficiency anemia.30 Measuring lead levels in urine is not recommended for screening,31,32 and neither is measuring lead levels in hair samples, which has a reported sensitivity of only 57%.33
The blood lead level should be less than 0.50 μmol/L, with adverse health effects likely occurring at greater levels. Levels between 0.30 and 0.50 μmol/L are above the Canadian average5,6 and should prompt a detailed exposure history and search for environmental sources of lead exposure. Any blood level of 0.50 μmol/L or higher requires repeat measurement immediately and in 3–6 months; in some cases immediate referral or treatment is also required. Table 3 summarizes the actions required by primary care physicians according to the severity of lead poisoning. Removing the child from further exposure and cleaning up the environment to eliminate the source of exposure are the main approaches to treatment. A calcium-rich diet or calcium supplements may be useful to prevent the release of lead from bone, which would accompany calcium deficiency. The negative effects of calcium deficiency are especially relevant for children and pregnant or lactating women.11 For children with a blood lead level between 0.50 and 0.75 μmol/L, a thorough exposure history and environmental clean-up are indicated (physicians may wish to use the more comprehensive environmental exposure history forms developed by the Environmental Health Clinic of Sunnybrook & Women's College Health Sciences Centre to identify sources of lead exposure [information on where to find these forms appears at the end of the article]). The primary care physician should contact the local public health department with the exposure information, which can be used by the public health official to recommend an appropriate home remediation program. This may include removal or covering of lead-based paints, cleaning and vacuuming the home repeatedly using a special fine vacuum filter (HEPA filter) and taking steps to reduce lead in drinking water. Occasionally, community-wide soil contamination must be remediated by large-scale removal of soil.4
Table 3
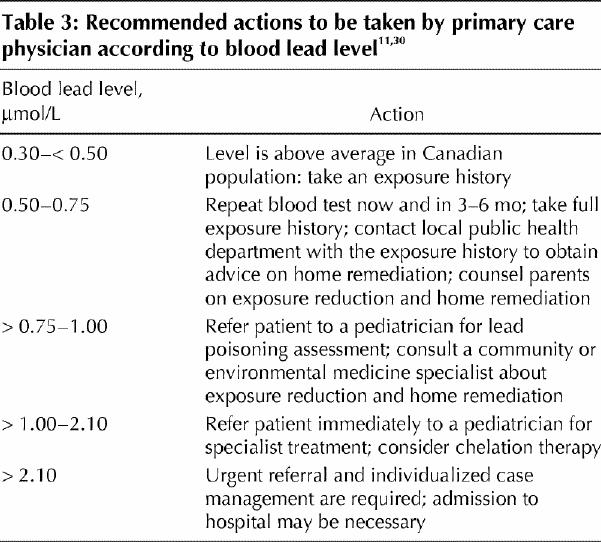
All children with a blood lead level greater than 0.75 μmol/L should be referred to a pediatrician knowledgeable in treating lead poisoning. The primary care physician should consult a community or environmental medicine specialist, who may further investigate likely sources of lead exposure and identify specific populations who may be at high risk. Levels above 1.00 μmol/L always require immediate action and referral. Levels above 2.10 μmol/L require urgent management and possible admission of the child to hospital.30 Very few children require chelation therapy.11 Lead mobilization tests with a chelating drug are no longer performed and may be dangerous.11
Prevention
There is no evidence for a threshold below which lead has no adverse effects. The precautionary principle when applied to lead exposure means that any reduction in exposure is beneficial to health. In addition to identifying people with elevated blood lead levels, physicians play an important role in educating all patients to minimize their exposure to lead. This has important economic consequences because of the well-established negative relation between lead levels and intelligence quotient (IQ) and adult earning power.34 In the United States calculations of the societal costs of cognitive impairment caused by lead have shown that an economic benefit of $2.5 billion per annual birth cohort would accrue from reducing population lead levels in children by only 0.05 μmol/L.34 It has also been calculated that an average drop of 5 points in IQ across the population would double the number of people with an IQ below 70.35
Physicians can receive advice about reducing lead exposure and home remediation from the local public health department. The Canada Mortgage and Housing Corporation booklet Lead in Your Home is also a useful handout for patients.36 The comparable US document is another excellent resource.37 The module on lead toxicity of the Agency for Toxic Substances and Disease Registry11 and the resource manual on the health risks from lead and their prevention from Toronto Public Health4 have excellent practical information and are recommended as quick office references.
Lead paint should be covered over with latex paint or removed with chemical stripper using appropriate personal protection, including gloves and a respirator. Removal by heat stripping or sanding mobilizes the lead and increases exposure. The local public health department can offer advice on the safest way to deal with old lead paints.
To reduce lead in drinking and cooking water, use only the cold water tap and run the water for 30–60 seconds or until the water is as cold as it gets. An inexpensive reverse osmosis filter (e.g., Brita) is also effective in removing lead from drinking water. Hobbyists, such as stained-glass workers, can reduce personal and family exposure to lead by wearing gloves and respirators, washing hands after working with lead and ensuring that their work area is well-ventilated, frequently vacuumed and off-limits to children in the house.
The questions answered
Is the family at risk of health effects from lead exposure? Who else might be at risk?
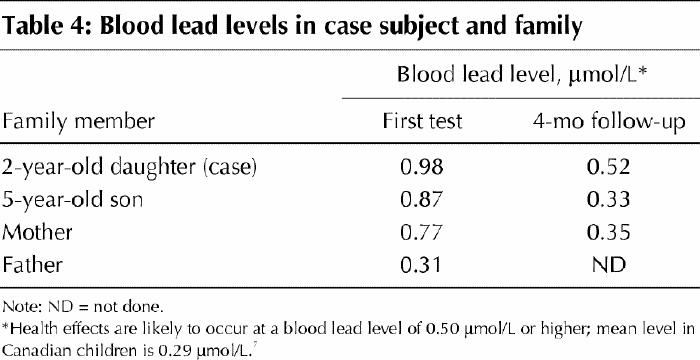
In the case described earlier the mother and both children are found to have blood lead levels that may be associated with adverse health effects (Table 4). The children in the home daycare are also at risk.
Table 4
Are other laboratory tests indicated?
Further tests, including a complete blood count and renal function test, would be appropriate for the family's 2 children. The girl is found to have a mean corpuscular volume of 80 fL.
Where can the physician get advice on the significance of the family's blood lead levels?
The physician should contact the local public health unit about the significance of the lead levels. The health unit can also provide detailed information on cleaning up the home. A pediatrician with experience in managing lead poisoning should be consulted regarding the girl, and a community medicine specialist (e.g., the medical officer of health) or an environmental health specialist could help assess the sources and extent of the lead exposure.
How should this case of lead exposure be treated?
The parents should be advised to remove the children from the house immediately while clean-up is done. All surfaces should be scrubbed with a general all-purpose cleaner twice and then weekly and the house vacuumed thoroughly. (Trisodium phosphate [TSP] is no longer recommended for clean-up; more recent advice on lead remediation suggests that a general all-purpose cleaner is just as effective as TSP in cleaning up lead dust in the home.37)
The children's follow-up blood lead levels measured 2 years later were still above average (data not shown), which suggests continuing exposure, perhaps in the drinking water. The physician should advise the parents to have their drinking water tested for lead and to replace the plumbing or use a reverse osmosis filter if the lead level is elevated.
Additional resources .
For physicians
· Contaminant profiles: lead. In: The health and environment handbook for health professionals. Ottawa: Health Canada; 1998. p. 1-7. Available: tel 613 954-5995; fax 613 941-5366; www.hc-sc.gc.ca/ehp/ehd/catalogue/bch_pubs/98ehd211/98ehd211.htm (accessed 2002 Apr 8).
· Rolnick SJ, Nordin J, Cherney LM. A comparison of costs of universal versus targeted lead screening for young children. Environ Res 1999;80(1):84-91.
· Silbergeld EK. Preventing lead poisoning in children. Annu Rev Public Health 1997;18:187-210.
For patients
· Lead in your home. Ottawa: Canada Mortgage and Housing Corporation and Health Canada; 1997. Cat no NH15-168/1997E. Available: tel (toll free) 800 668-2642; (pdf format) www.hc-sc.gc.ca/ehp/ehd/catalogue/bch_pubs/leadhome/booklet.pdf (accessed 2002 Apr 8).
Articles to date in this series .
Weir E. Identifying and managing adverse environmental health effects: a new series. CMAJ 2002;166(8):1041-3.
Marshall L, Weir E, Abelsohn A, Sanborn MD. Identifying and managing adverse environmental health effects: 1. Taking an exposure history. CMAJ 2002;166(8):1049-55.
Abelsohn A, Stieb D, Sanborn MD, Weir E. Identifying and managing adverse environmental health effects: 2. Outdoor air pollution. CMAJ 2002;166(9):1161-7.
Footnotes
[A detailed exposure history questionnaire is available on the Ontario College of Family Physicians Web site (www.cfpc.ca/ocfp/index.html — click on “Exposure History Sheets in MS Word” in the scrolling menu located in the middle of the page). The different components (Community, Home and Hobbies, Occupation, Personal habits, Diet and Drugs) can be printed on coloured paper for easy identification in patient charts. The questionnaire may be given to a patient to complete at home and bring to the next appointment for review and interpretation.]
This article has been peer reviewed.
Contributors: Dr. Sanborn conceived of and drafted the article. Drs. Campbell, Abelsohn and Weir contributed substantially to the conception and design of the article and to the acquisition of data. All authors contributed to the revising of the manuscript and approved the final version.
Competing interests: None declared.
Correspondence to: Dr. Margaret D. Sanborn, Chesley Medical Clinic, Box 459, 33 Second St. SE, Chesley ON N0G 1L0; msanborn@sbghc.on.ca
References
- 1.Marshall L, Weir E, Abelsohn A, Sanborn MD. Identifying and managing adverse environmental health effects: 1. Taking an exposure history. CMAJ 2002;166(8):1049-55. Available: www.cmaj.ca/cgi/content/full/166/8/1049. [PMC free article] [PubMed]
- 2.Needleman HL, Schell A, Bellinger D, Leviton A, Allred EN. The long-term effects of exposure to low doses of lead in childhood: an 11-year follow-up report. N Engl J Med 1990,322(2):83-8. [DOI] [PubMed]
- 3.Update: blood lead levels — United States, 1991–1994 [published erratum appears in MMWR Morb Mortal Wkly Rep 1997;46(26):607]. MMWR Morb Mortal Wkly Rep 1997;46(7):141-6. [PubMed]
- 4.Why barns are red: the health risks from lead and their prevention. A resource manual to promote public awareness. Toronto: Metropolitan Toronto Teaching Health Units and the South Riverdale Community Health Centre; 1995. Available: www.city.toronto.on.ca/health/pubs_index.htm#barns (accessed 2002 Apr 9).
- 5.Working Group on Blood Lead Intervention Levels and Strategies. Update of evidence for low-level effects of lead and blood lead intervention levels and strategies. Final report of the working group. Ottawa: Federal-Provincial Committee on Environmental and Occupational Health, Health and Welfare Canada; 1994.
- 6.Fleming S, Ursitti F. Scientific criteria document for multimedia environmental standards development — lead. Toronto: Standards Development Branch, Ontario Ministry of the Environment and Energy; 1994.
- 7.Myres AW, Easson E. Lead in paint: an “old” problem revisited. Environ Health Rev 1992;36:102-4.
- 8.Jin A, Hertzman C, Peck SHS, Lockitch G. Blood lead levels in children aged 24 to 36 months in Vancouver. CMAJ 1995;152(7):1077-86. [PMC free article] [PubMed]
- 9.Hilts SR, Bock S, Oke T, Yates C, Copes R. Effect of intervention on children's blood lead levels. Environ Health Perspect 1998;106(2):79-83. [DOI] [PMC free article] [PubMed]
- 10.Health Canada advises Canadians about potential lead exposure from inexpensive jewellery and candles with lead core wicks [advisory]. Ottawa: Health Canada; 2001 Jan 8. Available: www.hc-sc.gc.ca/english/protection/warnings/2001/2001_02e.htm (accessed 2002 Apr 9).
- 11.Case studies in environmental medicine: lead toxicity. Atlanta (GA): Agency for Toxic Subtances and Disease Registry; 2000. Available: www.atsdr.cdc.gov/HEC/CSEM/lead/index.html (accessed 2002 Apr 9).
- 12.Bellinger D, Leviton A, Rubinovitz M, Needleman H, Waternaux C. Longitudinal analysis of prenatal and postnatal lead exposure and early cognitive development. N Engl J Med 1987;316(1):1037-43. [DOI] [PubMed]
- 13.Loghman-Adham M. Renal effects of environmental and occupational lead exposure. Environ Health Perspect 1997;105(9):928-38. [DOI] [PMC free article] [PubMed]
- 14.Roscoe RJ, Gittleman JL, Deddens JA, Petersen MR, Halperin WE. Blood lead levels among children of lead-exposed workers: a meta-analysis. Am J Ind Med 1999;36(4):475-81. [DOI] [PubMed]
- 15.Neri LC, Johansen H, Hewitt D. Health effects of low level occupational exposure to lead: the Trail, British Columbia study. Arch Environ Health 1983; 38 (3) :180-9. [DOI] [PubMed]
- 16.Kim R, Rotnitzky A, Sparrow D, Weiss ST, Wager C, Hu H. A longitudinal study of low-level lead exposure and impairment of renal function. JAMA 1996; 275(15):1177-81. [PubMed]
- 17.Finkelstein Y, Markowitz ME, Rosen JF. Low-level lead-induced neurotoxicity in children: an update on central nervous system effects. Brain Res Rev 1998;27:168-76. [DOI] [PubMed]
- 18.Needleman H, Riess J, Tobin M, Biesecker G, Greenhouse J. Bone lead levels and delinquent behaviour. JAMA 1996;275(5):363-9. [PubMed]
- 19.Fergusson DM, Horwood J, Lynskey MT. Early dentine lead levels and educational outcomes at 18 years. J Child Psychol Psychiatry 1997;38(4):471-8. [DOI] [PubMed]
- 20.Nihei MK, Desmond NL, McGlothan JL, Kuhlmann AC, Guilarte TR. N-methyl-D-aspartate receptor subunits changes are associated with lead-induced deficits of long-term potentiation and spatial learning. Neuroscience 2000;99:233-42. [DOI] [PubMed]
- 21.American Academy of Pediatrics Committee on Environmental Health. Screening for elevated blood lead levels Pediatrics 1998;101(6):1072-8. [PubMed]
- 22.Levallois P, Gaudreault P, Rhainds M, Weber JP. Is there a need for systematic blood lead screening in Canadian children? Can J Public Health 1994;85(3):167-70. [PubMed]
- 23.Campbell M, Lee-Han H. Self-reported prevalence of lead exposure risk factors: a precursor to the development of a community awareness program. Environ Health Rev 1996;winter:90-111.
- 24.Campbell JR, Paris M, Schaffer SJ. A cost comparison of screening strategies for elevated blood lead levels. Arch Pediatr Adolesc Med 1996;150(11):1205-8. [DOI] [PubMed]
- 25.Bailey AJ, Sargent JD, Goodman DC, Freman J, Brown MJ. Poisoned landscapes: the epidemiology of environmental lead exposure in Massachusetts children 1990–1991. Soc Sci Med 1994;39(6):757-66. [DOI] [PubMed]
- 26.Nordin JD, Rolnick S, Griffin JM. Prevalence of excess lead absorption and associated risk factors in children enrolled in a Midwestern health maintenance organization. Pediatrics 1994;93(2):172-7. [PubMed]
- 27.Binns HJ, LeBailly SA, Fingar AR, Saunders S. Blood lead screening in Illinois. Pediatrics 1999;103(1):100-6. [DOI] [PubMed]
- 28.Graziano JH. Validity of lead exposure markers in diagnosis and surveillance Clin Chem 1994;40(7 Pt 2):1387-90. [PubMed]
- 29.Yiin LH, Rhoads GG, Lioy PJ. Seasonal influences on childhood lead exposure. Environ Health Perspect 2000;108(2):177-82. [DOI] [PMC free article] [PubMed]
- 30.Chao J, Kikano GE. Lead poisoning in children. Am Fam Physician 1993;47: 113-20. [PubMed]
- 31.Higashikawa K, Zhang ZW, Shimbo S, Moon CS, Watanabe T, Nakatsuka H, et al. Correlation between concentration in urine and in blood of cadmium and lead among women in Asia. Sci Total Environ 2000;246(2-3):97-107. [DOI] [PubMed]
- 32.Bergdahl IA, Schutz A, Gerhardsson L, Jensen A, Skerfving S. Lead concentrations in human plasma, urine and whole blood. Scand J Work Environ Health 1997;23(5):359-63. [DOI] [PubMed]
- 33.Esteban E, Rubin CH, Jones RL, Noonan G. Hair and blood as substrates for screening children for lead poisoning. Arch Environ Health 1999;54(6):436-40. [DOI] [PubMed]
- 34.Salkever DS. Updated estimates of earnings benefits from from reduced exposure of children to environmental lead. Environ Res 1995;17:1-6. [DOI] [PubMed]
- 35.Rutter M. Raised lead levels and impaired cognitive/behavioural functioning: a review of the evidence. Dev Med Child Neurol Suppl 1980;42:1-26. [PubMed]
- 36.Lead in your home. Ottawa: Canada Mortgage and Housing Corporation and Health Canada; 1997. Cat no NH15-168/1997E. p. 23. Available (pdf format): www.hc-sc.gc.ca/ehp/ehd/catalogue/bch_pubs/leadhome/booklet.pdf (accessed 2002 Apr 8).
- 37.Protect your family from lead in your home. Washington: US Environmental Protection Agency, US Consumer Product Safety Commission, US Department of Housing and Urban Development; 2001. Publ no EPA747-K-99-001. Available (pdf format): www.hud.gov/offices/lead/outreach/leapame.pdf (accessed 2002 Apr 8).


