Abstract
Objective
To assess the effectiveness of a teacher led intervention to improve teenagers' knowledge about emergency contraception.
Design
Cluster randomised controlled trial.
Setting
24 mixed sex, state secondary schools in Avon, south west England.
Participants
1974 boys and 1820 girls in year 10 (14-15 year olds).
Intervention
Teachers gave a single lesson on emergency contraception to year 10 pupils. The teachers had previously received in-service training on giving the lesson. The pupils were actively involved during the lesson.
Main outcome measures
Questionnaires distributed to pupils at baseline and six months after the intervention assessed their knowledge of the correct time limits for hormonal emergency contraception and for use of the intrauterine device as emergency contraception, the proportion of pupils who were not virgins, the proportion who had used emergency contraception, and the pupils' intention to use emergency contraception in the future.
Results
The proportion of pupils knowing the correct time limits for both types of emergency contraception was significantly higher in the intervention group than in the control group at six months' follow up (hormonal contraception: proportion of boys 15.9% higher (95% confidence interval 6.5% to 25.3%), girls 20.4% (10.4% to 30.4%); intrauterine device used as emergency contraception: boys 4.2% (0.7% to 7.7%), girls 10.7% (0.4% to 21.0%). The number of pupils needed to be taught for one more pupil to know the correct time limits was six for boys and five for girls. The intervention and control groups did not differ in the proportion of pupils who were not virgins, in the proportion who had used emergency contraception, and in the proportion intending to use emergency contraception in the future.
Conclusions
The intervention significantly improved the proportion of boys and girls knowing the correct time limits for both types of emergency contraception. The intervention did not change the pupils' sexual activity or use of emergency contraception.
What is already known on this topic
Use of condoms as a sole method of contraception is increasing
Emergency contraception—either hormonal or the intrauterine device used as emergency contraception—can be used when condoms or other methods fail or are not used
Awareness of emergency contraception in school pupils is high, but knowledge of specific details, such as the time period within which it can be used, is poor
What this study adds
A single lesson on emergency contraception given by teachers who had previously been trained improves the proportion of pupils aware of the correct time limits for use of both types of emergency contraception
Such a lesson does not increase sexual activity or use of emergency contraception
Introduction
In recent decades in England the age at which first sexual intercourse is reported as having occurred has declined steadily.1 The conception rate among teenagers under 18 years old in England is among the highest in the developed world. Reducing this rate by a half by 2010 is a government priority.2 Use of contraception has increased, including an increase since the 1980s in the use of condoms as the sole method of contraception, but it is generally accepted that much sex remains unprotected.3 Emergency contraception can be used when sex is unprotected or when other methods fail, for example when condoms split.
Emergency contraception is a safe, effective, and cheap way to prevent pregnancy.4–6 Appropriate use of emergency contraception could prevent up to 75% of unplanned pregnancies.7 Awareness of emergency contraception among school age pupils is high, but knowledge of specific details, such as timing, is poor.8
Most people first acquire information on sexual matters from school.9 In the United Kingdom most sex education in schools is provided by teachers, although sex education is not a compulsory part of the curriculum. Pupils want sex education from teachers whom they trust and whom they perceive to be unembarrassed.10 Results of a survey in secondary schools in Avon show that, although most teachers believe it is their responsibility to teach about emergency contraception, there are gaps in teachers' knowledge.11 Of 87 coordinators of the personal, social, and health education part of the curriculum, 31 did not know the correct 72 hour time limit for use of hormonal emergency contraception.
This study evaluated whether a teacher led lesson on emergency contraception could increase the proportion of pupils aware of the correct time limits for hormonal emergency contraception and use of the intrauterine device for emergency contraception. The teachers were trained before the lesson, which they gave to year 10 pupils (14-15 years old). The pupils were actively involved in the different components of the lesson.
Participants and methods
Recruitment
Head teachers of all mixed sex, state secondary schools in the four local education authorities in the county of Avon were sent a letter in May 1999 inviting their school to participate in the study. We asked for reasons for declining to take part.
Consent for the study was elicited from the head teacher, as the “gatekeeper” of the cluster; the director of education in each of the four education authorities; parents, in the form of a letter from the head teacher, with an opt out slip to return should they not want their child to take part in the study; and pupils, at the time of delivery of the questionnaires. The relevant ethics committees approved the study.
Randomisation
To ensure that the control and intervention groups were balanced with respect to factors likely to influence the outcome, we used a minimisation strategy in randomising schools to the groups.12 These factors were the percentage of pupils entitled to free school meals, size of year group, whether sex education was taught by a tutor or specialised team of teachers, and whether sex education was taught mainly in year 9 or in year 10. For size of year group and the percentage of pupils entitled to free school meals, the respective binary variable indicated whether the school was above or below the median. Allocation of schools to the groups, which occurred after all schools were recruited to the study, was determined by a sequential minimisation protocol. The order in which schools were minimised was determined by computer generated random numbers. Teachers and pupils were not blind to allocation.
Intervention
The aims of the in-service training of the teachers were to improve their knowledge about emergency contraception, to examine myths about the method (box), and to develop skills for use in a lesson for year 10 pupils on emergency contraception. The two hour training session was given by one of the authors (AG, who is trained in family planning) to teachers involved in delivering sex education at each school. Costs of extra staff to cover teachers taken out of lessons for the training were reimbursed. The proposed lesson to the pupils was demonstrated to the teachers during the training session. The lesson was taken from a resource produced for schools by Brook Advisory Centres.13 This was the only resource available at the time that included materials for the delivery of a lesson on emergency contraception. We chose year 10 for the intervention because a survey we did of schools in Avon indicated that most schools covered contraception by the end of this year.
Myths about emergency contraception discussed with teachers during the in-service training
“Morning after” means you can use the pill up to 12 hours after unprotected sex
You can use emergency contraception only once in a lifetime
If you are under 16 and you get emergency contraception from your GP, your GP has to ask permission from your parents
You have to pay for emergency contraception
You can only get emergency contraception from a specialist family planning clinic
Hormonal emergency contraception is a “mega” dose of hormone that works by poisoning you
Hormonal emergency contraception is the only method of contraception that can be used after sex
Emergency contraception always prevents pregnancy
Contraception after unprotected sex is really the same as having an abortion
Hormonal emergency contraception always makes you vomit
The content and delivery of the in-service training of teachers and the delivery by teachers of the lesson to pupils were piloted in one school in the area in the summer term of 1999. The pilot included two “active learning” methods (the involvement of pupils in experiential activities): a scenario activity and a role play, which have been shown in a review of the effectiveness of sex education to be the most effective teaching methods.14 The scenario chosen for the pilot involved a male lead role, because research has shown that boys tend to feel excluded from sex education lessons.15 However, our observation of the lesson, and focus group discussions with pupils who took part in the pilot, showed that the pupils saw the male lead as unrealistic, and so we changed the scenario to that of a young woman having unprotected sex while drunk on a Friday night (box). Furthermore, the role play was removed, as pupils found it difficult to actively engage with the activity (as shown by previous research16), and was replaced by a quiz on emergency contraception from the same resource.
The scenario and quiz
The scenario used in the study was entitled “A weekend away.” It tells the story of Lorraine, who joins friends at the bus stop on Monday morning on her way to school. She had been at a disco on Friday night and met Mike, someone she had previously fancied. After drinking and dancing all evening she possibly had sex in the early hours of Saturday morning on the way home from the disco. She does not know what to do and is obviously very upset.
After the scenario was given, groups of four pupils (two boys and two girls) discussed a series of questions about Lorraine's possible courses of action, including emergency contraception, and how her friends could help her. Each group then completed a quiz on emergency contraception. The questions in the quiz were:
What is emergency contraception?
Is the service confidential?
Is it free?
When can it be used?
How soon must it be used?
Where can people get it?
How effective is it?
How does it work?
What are the advantages?
What are the disadvantages?
Will there be a check up three weeks later?
Any other questions?
The pupils were given a booklet with the answers after completing the quiz.
Evaluation of the intervention
The outcome data comprised the pupils' answers to a confidential, self completed questionnaire administered at baseline and to a similar follow up questionnaire six months later. The questionnaires included questions used in a previous study by one of the authors (AG) and in a concurrent study in Scotland.8,16 In schools in the intervention group, the teachers were trained and the pupils were given the lesson within two weeks of the baseline questionnaire. Schools in the control group received the intervention after the follow up questionnaire was completed. All the schools continued to deliver their usual sex education programme. The study was completed in the academic year 1999-2000.
Sample size and study outcomes
The primary outcome was the proportion of pupils able to identify correctly the 72 hour limit for use of hormonal emergency contraception. To detect a difference of 18% between the intervention and control groups with 80% power and a level of significance of P<0.05 (two tailed test), 11 schools were required in each group. This assumed an intention to treat analysis, an absentee rate of 15%, and an intra-cluster correlation coefficient of 0.05, and that at baseline 26% of the girls would know the correct 72 hour time limit for use of hormonal emergency contraception (data derived from previous research8). Secondary outcomes were knowledge of the correct time limit (five days) for the use of the intrauterine device as emergency contraception, the proportion of pupils who weren't virgins, the proportion of pupils who had used emergency contraception, and the pupils' intention to use emergency contraception in the future.
Analysis of data
A regression analysis, weighted for schools rather than individuals, was used to analyse primary and secondary outcomes separately for boys and girls. The analysis was adjusted for baseline score and the four factors used in the minimisation strategy.17
We did a sensitivity analysis of the primary outcome to ascertain the influence of absent pupils on the findings. The number of pupils needed to be taught for one more pupil to know the correct time limit was calculated as the reciprocal of the difference between the groups in the proportion of pupils knowing the time limit, obtained from the adjusted analysis and rounded to the nearest whole number. We used Stata version 6.0 (StataCorp, College Station, TX, 1999) for the analyses.
Results
Participants
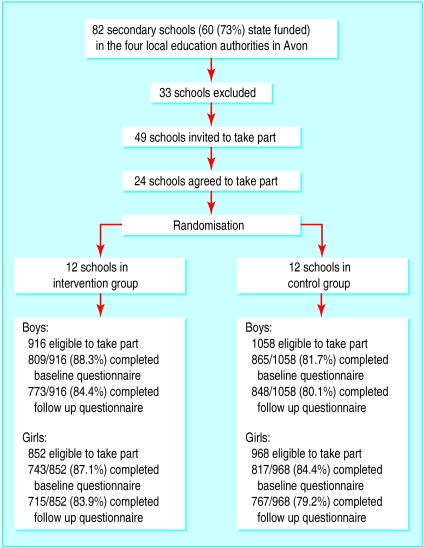
Of the 82 secondary schools in the four local education authorities in Avon, 49 were eligible to take part in the study, and 24 were recruited. Table 1 gives the reasons for exclusion, and table 2 gives the reasons schools gave for declining to take part in the study. A total of 1974 boys and 1820 girls were eligible to take part in the study.
Table 1.
Reasons why schools were excluded from the study (n=33)
| Reason | No of schools |
|---|---|
| Private school | 22 |
| Single sex state school | 4 |
| Pilot school (mixed sex state school) | 1 |
| Mixed sex state school with no sex education until year 11 | 1 |
| Mixed sex state school in which sex education is taught in small groups throughout the year* | 3 |
| Mixed sex state school that closed before the study began | 2 |
Excluded because at any one time pupils in a particular year group would be at different stages of sex education.
Table 2.
Reasons why schools declined to take part (n=25)
| Reason | No of schools |
|---|---|
| Preferred not to (no specific reason given) | 9 |
| School moving or key teacher on long term sick leave | 6 |
| Religious reasons | 4 |
| Research fatigue | 2 |
| Too busy | 2 |
| Sex education led by a nurse | 1 |
| Declined after discussion with governors | 1 |
Nine pupils in the intervention group and 24 pupils in the control group were withdrawn from the study by their parents. Pupils were able to leave their questionnaires blank; 18 boys and two girls did so. A researcher who was blind to allocation to group assessed whether questionnaires were spoilt. Forty four boys and no girls had spoilt questionnaires; these were removed from further analysis. No schools dropped out of the study. Numbers of pupils who completed the study are given in the figure, which shows the flow of pupils and schools though the study.
Schools eligible to take part in the study were similar to all state secondary schools in Avon when compared on factors important to the primary outcome. Schools declining to take part in the study were less likely, compared with schools agreeing to take part, to teach sex education to younger year groups or to use a specialised team of teachers (table 3). Schools in the control group had larger year groups and more specialist teams teaching sex education than schools receiving the intervention (table 4).
Table 3.
Baseline characteristics of state secondary schools in England and Avon and schools in the study
| Characteristic | Schools in England (n=3177) | Schools in Avon (n=60) | Schools eligible to take part in study (n=49) | Schools that declined to take part in study (n=25) | Schools that participated in study (n=24) |
|---|---|---|---|---|---|
| Median % of pupils entitled to free school meals | 12.7 | 12.9 | 13.0 | 13.2 | 12.9 |
| % of pupils obtaining five or more A-C grades in GCSEs | 47.9 | 43.0 | 42.5 | 42.2 | 43.0 |
| Median No of pupils in a year group | 162 | 156 | 158 | 160 | 156 |
| No (%) of schools in which contraception is taught mainly in year 9 | N/A | 9 (15) | 7 (14) | 3 (12) | 12 (50) |
| No (%) of schools with team led sex education | N/A | 28 (47) | 23 (47) | 8 (32) | 14 (58) |
Table 4.
Baseline comparison between intervention and control groups of school level variables. Values are numbers of schools
| Variable | Intervention | Control |
|---|---|---|
| % of pupils entitled to free school meals: | ||
| ⩽12.9% | 6 | 7 |
| >12.9% | 6 | 5 |
| No of pupils in year group: | ||
| ⩽180 | 8 | 3 |
| >180 | 4 | 9 |
| Contraception taught mainly in: | ||
| Year 9 | 7 | 5 |
| Year 10 | 5 | 7 |
| Sex education taught by: | ||
| Specialist team of teachers | 6 | 8 |
| Tutors | 6 | 4 |
Effect of the intervention on the primary outcome
Tables 5 and 6 show the results of the intervention on the proportions of pupils knowing the correct time limit for hormonal emergency contraception. At six months' follow up the proportion of pupils in the intervention group who knew the correct time limit was significantly higher than the proportion in the control group (boys 15.9% higher (95% confidence interval 6.5% to 25.3%, P<0.01), girls 20.4% higher (10.4% to 30.4%, P<0.01)). To examine the effect of absent pupils on the results, we did a sensitivity analysis assuming that all absent pupils at both baseline and follow up in both groups did not know the correct time limit for hormonal emergency contraception. The results show that the intervention effect remained (boys 14.8% higher (6.6% to 23.0%, P<0.01), girls 19.8% higher (12.0% to 27.6%, P<0.01). The number of pupils needed to be taught for one more pupil to know the correct time limit was six for boys (1/0.159=6.29) and five for girls (1/0.204=4.90).
Table 5.
Percentages (numbers) of pupils at baseline and six months' follow up knowing the correct time limit for hormonal emergency contraception, before and after sensitivity analysis*
| Baseline
|
Follow up
|
||||
|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | ||
| Before sensitivity analysis | |||||
| Boys | 9.3 (75/809) | 11.9 (103/865) | 31.8 (233/733) | 15.9 (135/848) | |
| Girls | 26.2 (195/743) | 31.6 (258/817) | 54.8 (392/715) | 39.2 (301/767) | |
| After sensitivity analysis | |||||
| Boys | 8.2 (75/916) | 9.7 (103/1058) | 25.4 (233/916) | 12.8 (135/1058) | |
| Girls | 20.1 (195/968) | 30.3 (258/852) | 40.5 (392/968) | 35.3 (301/852) | |
Assumes that all pupils who were absent at both baseline and follow up did not know the correct time limit.
Table 6.
Weighted regression analysis* of difference between intervention and control groups in the proportion of pupils knowing the correct time limit for hormonal emergency contraception. Values are differences between the proportions (%) in the two groups (95% confidence interval)
| Increase of intervention group over control group (P<0.01 for all)
|
||
|---|---|---|
| Unadjusted | Adjusted† | |
| Before sensitivity analysis‡ | ||
| Boys | 12.9 (4.8 to 21.0) | 15.9 (6.5 to 25.3) |
| Girls | 15.8 (6.2 to 25.3) | 20.4 (10.4 to 30.4) |
| After sensitivity analysis‡ | ||
| Boys | 11.8 (4.1 to 19.5) | 14.8 (6.6 to 23.0) |
| Girls | 15.0 (5.8 to 24.1) | 19.8 (12.0 to 27.6) |
Weighted for schools rather than individuals, using methods described by Donner and Klar.17
Adjusted for baseline results, percentage of pupils entitled to free school meals, size of year group, whether sex education was taught by a tutor or a specialised team of teachers, and whether sex education was taught mainly in year 9 or 10.
The sensitivity analysis assumes that all pupils who were absent at both baseline and follow up did not know the correct time limit.
Secondary outcomes
Table 7 shows the effect of the intervention on the secondary outcomes. The proportion of pupils knowing the correct time limit for use of the intrauterine device as emergency contraception was significantly higher in the intervention group than in the control group (boys 4.2% higher (0.7% to 7.7%, P=0.02), girls 10.7% higher (0.4% to 21.0%, P=0.04). The proportion of pupils who were not virgins did not differ significantly between the groups, and of these pupils the proportion who said they had used emergency contraception did not differ significantly between the groups. There was no difference between the groups in the proportion of pupils intending to use emergency contraception in the future.
Table 7.
Percentages (numbers*) of pupils in secondary outcomes at baseline and at six months' follow up
|
Baseline
|
Follow up
|
Weighted regression analysis of difference between groups†
|
||||||
|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Difference (%) | 95% CI | |||
| Pupils knowing correct time limit for use of the intrauterine device as emergency contraception | ||||||||
| Boys | 2.2 (17/783) | 3.7 (31/845) | 7.1 (54/756) | 3.5 (29/836) | 4.2 | 0.7 to 7.7 (P=0.02) | ||
| Girls | 4.6 (33/724) | 5.1 (41/802) | 21.1 (150/711) | 9.9 (74/751) | 10.7 | 0.4 to 21.0 (P=0.04) | ||
| Pupils who were not virgins | ||||||||
| Boys | 19.1 (149/781) | 19.3 (158/819) | 26.6 (198/744) | 26.0 (212/816) | −0.3 | −6.2 to 5.6 (P=0.9) | ||
| Girls | 20.5 (148/722) | 23.0 (184/800) | 28.5 (199/699) | 29.5 (240/747) | 0.8 | −7.2 to 8.7 (P=0.8) | ||
| Pupils who were not virgins who said they had used emergency contraception | ||||||||
| Boys‡ | 18.8 (27/144) | 24.2 (36/149) | 20.1 (38/189) | 15.6 (33/211) | −0.1 | −8.9 to 8.7 (P=1.0) | ||
| Girls | 29.0 (42/145) | 29.1 (51/175) | 32.3 (63/195) | 35.9 (79/220) | −8.0 | −20.8 to 4.7 (P=0.2) | ||
| Pupils intending to use emergency contraception in the future when contraception not used during intercourse§ | ||||||||
| Boys | N/A | N/A | 83.1 (629/757) | 83.7 (689/823) | N/A | N/A | ||
| Girls | N/A | N/A | 87.6 (621/709) | 86.9 (652/750) | N/A | N/A | ||
Denominators exclude pupils not responding to that question.
Weighted for schools rather than individuals, using methods described by Donner and Klar,17 and adjusted for baseline results, percentage of pupils entitled to free school meals, size of year group, whether sex education was taught by a tutor or a specialised team of teachers, and whether sex education was taught mainly in year 9 or 10.
Boys' responses are likely to be less reliable than the girls', as girls will have accessed emergency contraception themselves.
Question not asked at baseline.
Discussion
A single lesson to pupils given by teachers who had previously been instructed by a general practitioner significantly increased the proportion of boys and girls knowing the correct time limit for hormonal emergency contraception, compared with a control group who did not receive the lesson until after the study. The lesson also increased the proportion of pupils knowing the correct time limit for use of the intrauterine device as emergency contraception.
Design of the study
Reviews of interventions in sexual health education aimed at young people concluded that the design of such evaluations needed to be improved so that evidence of the effectiveness of different interventions could be generated.14,18 We believe our evaluation to be rigorously designed, with a defined focus and clear objectives. The lesson was developed by an organisation that is well known for providing resources that are appropriate for particular age groups and that use active learning rather than didactic teaching methods. The in-service training and the lesson were piloted and amended to ensure their relevance for, respectively, teachers and year 10 pupils.
Kirby et al state that active learning activities help pupils personalise information.14 Teachers need to feel confident enough to deliver such lessons. This “one off” intervention was limited in its ability to develop such teaching skills. However, our observations of a number of lessons in the course of the study led us to believe that active rather than didactic methods were used. There were some differences between the intervention and control groups at baseline. This did not, however, result in bias, because there were no real differences between the results of the adjusted and unadjusted analyses.
Analyses were done at the level of schools rather than individuals for two reasons: the intervention was delivered to clusters of pupils (schools), and the pilot lesson showed that pupils felt more confident completing the questionnaires without individual identification codes.
Our intervention showed no evidence of changed sexual behaviour—whether increased sexual activity or greater use of emergency contraception. It was important for us to show this lack of effect, in view of the ongoing debate on the effects of sex education and the argument that promoting the use of contraception encourages sexual activity.19
The schools in the study were similar to state schools in England generally in terms of standard measures of deprivation and academic attainment, but sex education in our schools was more likely than in schools nationally to be team led, which may reduce the generalisability of the findings. However, this method of teaching may become more common, after a recent report from the Office for Standards in Teaching encouraged the use of teams.20 Even in the schools that already had this good practice, pupils' understanding of emergency contraception improved.
Usefulness of the intervention
Lack of awareness of correct time limits for use of emergency contraception is not the only factor preventing its use. It is likely that concerns about the safety of emergency contraception also act as a deterrent. Women seeking emergency contraception, as well as personal, social, and health education teachers, have been shown to have concerns of this nature.11,21 Of 87 teachers in a survey undertaken in the study area, only 45 agreed with the statement “Using emergency contraception is safe.”11
There is now some evidence that hormonal emergency contraception is more effective the sooner it is used after unprotected sexual intercourse.5 However, it remains effective—and is licensed for use—up to 72 hours after sex. Our study was undertaken before emergency contraception was made available over the counter.
An interesting question is whether the intervention effect lasts: whether the outcome is sustained over a longer period than six months, and how frequently the in service training would need to be repeated in order to continue to be effective.
Limitations of the study
The main limitation is that we did not include an evaluation of health gains, as advocated by previous reviews.14,18 None of the randomised controlled trials in a recent review of research into the primary prevention of pregnancy among adolescents showed any benefit in health based outcomes.22 Also, our sample size was too small to show a reduction in the rate of conceptions.
The change in the pupils' knowledge may not translate to a change in behaviour, as so many other factors undoubtedly play a role. However, educating teenagers on the time limits for use of emergency contraception after unprotected sex is more likely to have an impact on behaviour than, say, encouragement to use a condom.
Figure.
Flow of schools and pupils through the study
Acknowledgments
We thank the participating pupils and teachers; Jill Newman for data management; Andrea Litva for conducting the focus groups with pupils in the pilot school; and Nona Dawson, David Pearson, and Hilary Cooling (the members of the steering committee for the project) for their advice and support. We acknowledge the MRC Social and Public Health Sciences Unit, 4 Lilybank Gardens, Glasgow G12 8RZ, for the use of the SHARE questionnaire.
Footnotes
Funding: AG is funded by a NHS R&D S&W Studentship and by a grant from the Royal College of General Practitioners' Scientific Foundation Board. LM is funded by the Health Promotion Division of the National Assembly for Wales. The views expressed in this paper are those of the authors and not necessarily those of the funding bodies.
Competing interests: Schering Health Care provided, free of charge, samples of emergency contraception (hormonal and the intrauterine device) used in the lesson. AG has received fees from Schering Health Care for speaking at educational events.
References
- 1.Wellings K, Field J, Johnson A, Wadsworth J. Sexual behaviour in Britain. Harmondsworth: Penguin; 1994. [Google Scholar]
- 2.Social Exclusion Unit. Teenage pregnancy. London: HMSO; 1999. [Google Scholar]
- 3.McEwan J, Wadsworth J, Johnson AM, Wellings K, Field J. Changes in the use of contraceptive methods in England and Wales over two decades: Margaret Bone's surveys and the national survey of sexual attitudes and lifestyles. Br J Fam Plann. 1997;23:5–8. [Google Scholar]
- 4.Vasilakis C, Jick S, Jick H. The risk of venous thromboembolism in users of postcoital contraceptive pills. Contraception. 1999;59:79–83. doi: 10.1016/s0010-7824(99)00011-6. [DOI] [PubMed] [Google Scholar]
- 5.Task Force on Postovulatory Methods of Fertility Regulation. Randomised controlled trial of levonorgestrel versus the Yuzpe regimen of combined oral contraceptives for emergency contraception. Lancet. 1998;352:428–433. [PubMed] [Google Scholar]
- 6.Trussell J, Koenig J, Ellertson C, Stewart F. Preventing unintended pregnancy: the cost-effectiveness of three methods of emergency contraception. Am J Public Health. 1997;87:932–937. doi: 10.2105/ajph.87.6.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trussell J, Rodriguez G, Ellertson C. Updated estimates of the effectiveness of the Yuzpe regimen of emergency contraception. Contraception. 1999;59:147–151. doi: 10.1016/s0010-7824(99)00018-9. [DOI] [PubMed] [Google Scholar]
- 8.Graham A, Green L, Glasier AF. Teenagers' knowledge of emergency contraception: questionnaire survey in south east Scotland. BMJ. 1996;312:1567–1569. doi: 10.1136/bmj.312.7046.1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wellings K, Wadsworth J, Johnson AM, Field J, Whitaker L, Field B. Provision of sex education and early sexual experience: the relation examined. BMJ. 1995;311:417–420. doi: 10.1136/bmj.311.7002.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Allen I. Education in sex and personal relationships. London: Policy Studies Institute; 1987. [Google Scholar]
- 11.Graham A, Dawson N, Moore L. Emergency contraception: a survey of knowledge and attitudes among PSHE co-ordinators in Avon secondary schools. Health Educ J. 2000;59:329–339. [Google Scholar]
- 12.Treasure T, MacRae KD. Minimisation: the platinum standard for trials? BMJ. 1998;317:362–363. doi: 10.1136/bmj.317.7155.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Went D. Understanding contraception. London: Brook Publications; 1998. [Google Scholar]
- 14.Kirby D, Short L, Collins J, Rugg D, Kolbe L, Howard M, et al. School based programs to reduce sexual risk behaviours: a review of effectiveness. Public Health Rep. 1994;109:339–360. [PMC free article] [PubMed] [Google Scholar]
- 15.Let's hear it for the boys! Supporting sex and relationships education for boys and young men. London: National Children's Bureau; 1997. [Google Scholar]
- 16.Wight D, Abraham C. From psycho-social theory to sustainable classroom practice: developing a research-based teacher delivered sex education programme. Health Educ Res. 2000;15:25–38. doi: 10.1093/her/15.1.25. [DOI] [PubMed] [Google Scholar]
- 17.Donner A, Klar N. Design and analysis of cluster randomised controlled trials in health research. London: Arnold; 2000. pp. 87–88. [Google Scholar]
- 18.Oakley A, Fullerton D, Holland J, Arnold S, France-Dawson M, Kelley P, et al. Sexual health education interventions for young people: a methodological review. BMJ. 1995;310:158–162. doi: 10.1136/bmj.310.6973.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stammers T, Ingham R. For and against: doctors should advise adolescents to abstain from sex. BMJ. 2000;321:1520–1522. doi: 10.1136/bmj.321.7275.1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.OFSTED subject reports, 1999-2000: secondary personal, social and health education (PSHE). London: Office for Standards in Teaching; 2001. [Google Scholar]
- 21.Ziebland S, Maxwell K, Greenhall E. “It's a mega dose of hormones, isn't it?” Why women may be reluctant to use emergency contraception. Br J Fam Plann. 1996;22:84–86. [Google Scholar]
- 22.Guyatt GH, DiCenso A, Farewell V, Willan A, Griffith L. Randomised trials versus observational studies in adolescent pregnancy prevention. J Clin Epidemiol. 2000;53:167–174. doi: 10.1016/s0895-4356(99)00160-2. [DOI] [PubMed] [Google Scholar]