Abstract
Aims
Previous studies have indicated a poorer survival among women following out-of-hospital cardiac arrest (OHCA), but the mechanisms explaining this difference remain largely uncertain.
This study aimed to assess the survival after OHCA among women and men and explore the role of potential mediators, such as resuscitation characteristics, prior comorbidity, and socioeconomic factors.
Methods and results
This was a population-based cohort study including emergency medical service-treated OHCA reported to the Swedish Registry for Cardiopulmonary Resuscitation in 2010–2020, linked to nationwide Swedish healthcare registries. The relative risks (RR) of 30-day survival were compared among women and men, and a mediation analysis was performed to investigate the importance of potential mediators. Total of 43 226 OHCAs were included, of which 14 249 (33.0%) were women. Women were older and had a lower proportion of shockable initial rhythm. The crude 30-day survival among women was 6.2% compared to 10.7% for men [RR 0.58, 95% confidence interval (CI) = 0.54–0.62]. Stepwise adjustment for shockable initial rhythm attenuated the association to RR 0.85 (95% CI = 0.79–0.91). Further adjustments for age and resuscitation factors attenuated the survival difference to null (RR 0.98; 95% CI = 0.92–1.05). Mediation analysis showed that shockable initial rhythm explained ∼50% of the negative association of female sex on survival. Older age and lower disposable income were the second and third most important variables, respectively.
Conclusion
Women have a lower crude 30-day survival following OHCA compared to men. The poor prognosis is largely explained by a lower proportion of shockable initial rhythm, older age at presentation, and lower income.
Keywords: OHCA, SCD, Sex, Gender, Ventricular arrhythmia, Women’s health
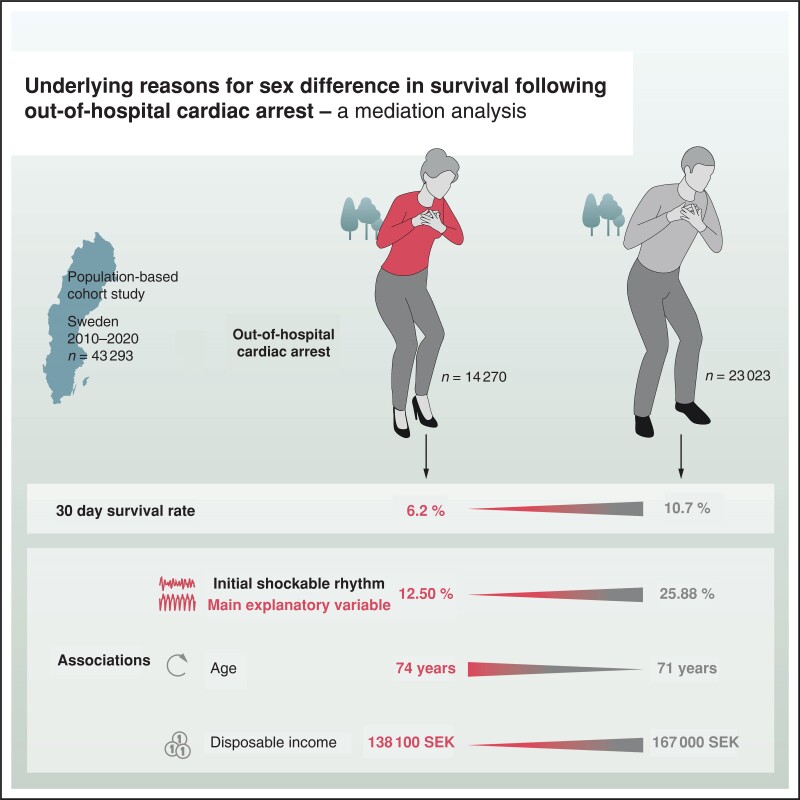
Graphical Abstract
Graphical Abstract.
Introduction
Out-of-hospital cardiac arrest (OHCA) affects around 340 000 persons in Europe each year.1 Survival after OHCA is poor, ∼7–11%, where women appear to have a particularly poor prognosis.2–5 The poor prognosis in women may, however, be attributed to a female predisposition to factors associated with mortality, including lower rate of initial shockable rhythm [ventricular tachycardia (VT) or ventricular fibrillation (VF)], older age, and higher comorbidity burden.6–11 A recent systematic review and meta-analysis of 30 studies and 1 068 788 patients with OHCA found survival to discharge to be comparable among men and women (OR 1.03, 95% confidence interval (CI) 0.95–1.12) after adjustment of prognostic factors, although heterogeneity among included studies was high.5
However, even if there is no difference in survival after adjustments, it is less clear which mediators or confounders are unevenly distributed and how they explain the difference in crude survival. Hence, a mediation analysis could shed more light on this matter.
This study set out to assess sex-specific 30-day survival after OHCA among men and women by using a population-based nationwide registry of OHCA patients in Sweden.
Additionally, we sought to explore the role and magnitude of potential mediators between sex and survival using multiple mediation analysis. The method seeks to identify variables that intervene in the causal relationship between sex and survival. The mediation analysis includes traditional resuscitation characteristics, prior comorbidity, and socioeconomic factors such as level of education and income.
Methods
Study design
This was an observational registry-based nationwide cohort study of OHCA in Sweden, treated by emergency medical services (EMS) and reported to the Swedish Registry for cardiopulmonary resuscitation (SRCR).
Study setting and data sources
Sweden has a population of 10.5 million and covers an area of 407 000 km2.12 In cases of OHCA, most EMS systems have a response of two ambulances providing advanced life support.
All EMS services in Sweden report to SRCR. The criterion for inclusion in the registry is OHCA in which cardiopulmonary resuscitation (CPR) and/or defibrillation is performed by a lay responder or paramedic. The SRCR is a national quality registry founded in 1990. Data collection complies with the Utstein template for most variables and outcomes.13 There is a national web-based procedure for OHCA registration.
The EMS crew involved complete a form for each case of OHCA, including information about age, location and probable cause of the arrest, and a standardized report of the resuscitation procedure such as intervention times, bystander CPR, defibrillation, medical treatment, and status at the first contact. The cardiac arrest aetiology is based on the judgement made by the EMS crew, and not confirmed by autopsy findings or further clinical data.
In ambulances with manual defibrillators, the first recorded rhythm is defined as VT, VF pulseless electric activity, or asystole. For automated external defibrillators, the first rhythm is defined as shockable (VT/VF) or non-shockable (pulseless electric activity or asystole). Immediate outcome is reported by the EMS crew as dead on scene, dead in the emergency room, or admitted alive to hospital.
Approximately 75% of patients with OHCA in whom CPR is started are reported prospectively by the EMS crews to the registry, and the rest are reported retrospectively from medical charts.
The registry has been described in more detail elsewhere.14 To explore the role of potential mediators that could explain sex differences in survival, data from the SRCR were linked with data from the National Patient Registry (NPR) to obtain information on comorbidities, and with Statistics Sweden to obtain data on sociodemographic factors. Linkage between SRCR, NPR, and Statistic Sweden was done using the Swedish personal ID number.
The NPR is a nationwide registry run by the Swedish National Board of Health and Welfare. National Patient Registry covers data on diagnoses and surgical procedure codes from hospitals and specialist clinics. The registry also includes outpatient visits from private and public healthcare providers. Primary care, however, is not covered by the NPR. All admissions, both inpatient and outpatient, are registered with International Classification of Diseases (ICD)-10 codes.
The NPR was launched in 1964 and had completed inpatient coverage from 1986. Hospital based outpatient care was added in 2001. The current coverage is estimated to be 99%. The NPR has been validated and the positive predictive value (PPV) for a diagnosis in the register has been estimated to be around 85–95%.15
Ethics
In the SRCR, patients who survive to 3 months are informed that they have been reported to the register and are given the opportunity to withdraw from further participation.
Ethical approval for this study was obtained by the Swedish ethical review authority (dnr 2022-02905-0). The need for informed consent was waived.
Inclusion and exclusion criteria
All consecutive EMS-treated OHCAs reported to the SRCR between 1 January 2010, and 7 March 2020, were included. This specific end-date was chosen because it was the date of the first admitted patient to intensive care unit due to Covid-19 in Sweden.
Exclusion criteria were OHCAs younger than 18 years since causes of OHCA among children and adolescents are markedly different. Patients with missing data on personal identification number, i.e. unknown ID or non-residents were also excluded since follow-up and linkage to other registries was not possible for this group. Out-of-hospital cardiac arrests not treated with CPR by the EMS (usually sure signs of death) are not included since they are not registered in SRCR. Finally, patients with missing data on sex (exposure) were also excluded.
In order to compare bystander treatment and delays to CPR and EMS arrival, patients with cardiac arrest witnessed by the EMS were also excluded.
Exposure and outcome: Exposure was female sex as reported by the EMS. Primary outcome was 30-day survival and secondary outcome was 1-day survival after OHCA.
Data collection
For all included OHCA, data on resuscitation characteristics were collected from SRCR. Data include patient characteristics such as sex (exposure) and resuscitation characteristics such as most probable cause of the arrest (medical vs. non-medical), location, bystander CPR, witness status, time intervals, and shockable initial rhythm. Return of spontaneous circulation was not included in the analysis, since it is a poorly defined variable in the registry. Instead, 1-day survival was used. From the NPR ICD-diagnoses before the index date of the cardiac arrest were collected. All ICD-diagnoses with a prevalence above 5% in the study population were considered potentially relevant and included in the model. Finally, socioeconomic variables were collected from Statistics Sweden, including disposable income per consumption unit (measured from the total family disposable income)16 and the highest level of completed education (categorized as primary, secondary, post-secondary ≤2 years, and post-secondary ≥3 years). We used median disposable income, presented in Swedish Kronor (SEK) where 1 SEK corresponds to ∼0088 € (16 May 2023).
Data on primary and secondary outcomes (30-day and 1-day survival) was obtained through linkage with the Swedish Population Registry.
Statistical analysis
Baseline characteristics are presented as numbers and proportions for categorical variables and medians (10th, 90th percentile) for continuous variables. Baseline difference between men and women was assessed using standardized mean difference (SMD). Values below 0.1 were considered well-balanced. Adjusted relative risks (RR) with 95% CIs were calculated using a modified Poisson regression.17
The modified Poisson regression17 is used to estimate relative risk (RR) and uses a Poisson regression on binomial data and a sandwich estimation to shrink the error of the estimated relative risk.
In the Poisson regression analyses each variable was added in a new model (a total of 35 models). The order of variables added into the models was determined using the variable importance (mean decrease in accuracy) from a random forest model including all potential explanatory variables. Missing data was handled using multiple imputation by chained equations. Missing was assumed to be missing at random. Ten datasets were imputed and the results from each dataset were pooled using Rubins’s rules.
To further investigate the importance of potential mediators we performed a mediation analysis using the multiple mediation analysis (mma) package.18 The mma package uses multiple logistic regression analyses to assess the relative importance for each variable. Since the purpose of the mediation analysis was to explore the relative importance of all mediators, all variables from the Poisson regression analysis were included as potential mediators. Variables associated with both sex (as an outcome variable) and 30-day survival (as an outcome variable) respectively were kept in the model (P-values < 0.1, was used as a threshold).
Finally, sensitivity analyses with VT/VF as outcome among women and a stratified analysis to explore changes in main determinants over time was performed. All analyses were performed using R version 4.1.3 (R project for Statistical computing, Vienna, Austria).
Results
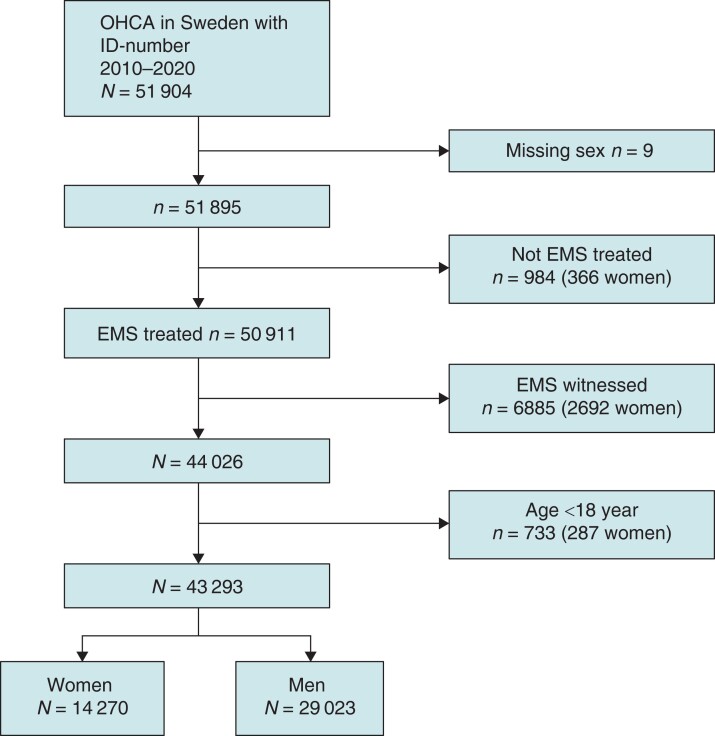
Between 1 January 2010 and 7 March 2020, 51,904 OHCA patients with a Swedish personal ID number were registered into the SRCR. After exclusion of patients not treated with CPR by EMS (n = 984), EMS witnessed cases (n = 6885), patients under the age of 18 (n = 733) and those with missing sex (n = 9) a total of 43 293 patients were included in the final analytical sample, of which 14 270 were women (33%) and 29 023 were men (67%) (Figure 1).
Figure 1.
Flow chart of included patients. EMS, Emergency medical services; OHCA, out-of-hospital cardiac arrest.
Baseline patient and resuscitation characteristics are presented in Table 1. Women, compared to men, were older (median age 74 years vs. 71 years among men, SMD = 0.211), suffered the OHCA at home to a larger extent (82.6 vs. 69.8%, SMD = 0.335), had a lower proportion shockable initial rhythm (12.5 vs. 25.8%, SMD = 0.343) and had a lower disposable income (138 100 SEK vs. 167 000 SEK, SMD = 0.199). Women had a lower proportion defibrillated by a public defibrillator (0.7 vs. 1.7%) or by first responders (1.6 vs. 3.3%). Crude survival to 30-days was also lower among women, 6.2 vs. 10.7% for males.
Table 1.
Baseline characteristics
| Women | Men | SMD | Missing | |
|---|---|---|---|---|
| n | 14 270 | 29 023 | ||
| Patient characteristics | ||||
| Age, years, median [IQR] | 74.0 [63.0, 84.0] | 71.0 [60.0, 80.0] | 0.211 | 0.0 |
| Age category, n (%) | 0.230 | 0.0 | ||
| 1. 18–39 | 804 (5.6) | 2082 (7.2) | ||
| 2. 40–59 | 1945 (13.6) | 4866 (16.8) | ||
| 3. 60–79 | 6261 (43.9) | 14 426 (49.7) | ||
| 4. 80+ | 5260 (36.9) | 7649 (26.4) | ||
| Resuscitation characteristics | ||||
| Witnessed, n (%) | 8122 (58.2) | 17 382 (61.3) | 0.064 | 2.2 |
| Location of cardiac arrest, n (%) | 0.335 | 0.2 | ||
| 1 At home | 11 752 (82.6) | 20 197 (69.7) | ||
| 2 Public location | 1410 (9.9) | 6221 (21.5) | ||
| 3 Other (nursing home, etc.) | 1071 (7.5) | 2545 (8.8) | ||
| Time from call to EMS arrival, minutes, median [IQR] | 9.0 [6.0, 14.0] | 9.0 [6.0, 15.0] | 0.022 | 7.5 |
| VT/VF, n (%) | 1744 (12.5) | 7316 (25.8) | 0.343 | 2.3 |
| Bystander CPR, n (%) | 8697 (62.1) | 17651 (61.8) | 0.006 | 1.7 |
| Bystander defibrillation, n (%) | 100 (0.7) | 472 (1.7) | 0.087 | 1.7 |
| First responder CPR, n (%) | 3274 (23.7) | 7273 (25.8) | 0.048 | 3.0 |
| First responder defibrillation, n (%) | 214 (1.6) | 926 (3.3) | 0.113 | 3.0 |
| Medical aetiology, n (%) | 12 262 (91.3) | 24 945 (90.8) | 0.018 | 5.5 |
| Socioeconomic factors | ||||
| Disposable income, SEK, median [IQR] | 138 100 [111,400, 167,900] | 167 000 [132,700, 240,900] | 0.199 | 7.8 |
| Educational level, n (%) | 0.074 | 7.8 | ||
| 1 Primary school | 5668 (42.9) | 10 545 (39.4) | ||
| 2 Secondary school | 5142 (39.0) | 1,0931 (40.9) | ||
| 3 Post-secondary ≤2y | 934 (7.1) | 2162 (8.1) | ||
| 4 Post-secondary ≥3y | 1455 (11.0) | 3097 (11.6) | ||
| Crude survival | ||||
| 30-day survival (%) | 879 (6.2) | 3097 (10.7) | 0.163 | 0.0 |
CPR, cardiopulmonary resuscitation; EMS, emergency medical services (ambulance and first responders); IQR, interquartile range; SEK, Swedish kronor; SMD, standardized mean difference; VT/VF, ventricular fibrillation/ventricular tachycardia.
Baseline prior comorbidities are presented in Table 2. Notable differences were seen in chronic ischaemic heart disease (14.9% among women vs. 24.4% among men, SMD = 0.239), atrial fibrillation (17.4% among women vs. 22.7% among men, SMD 0.133), previous acute myocardial infarction (10.7% among women vs. 15.1% among men, SMD = 0.131), chronic obstructive pulmonary disease (COPD) (14.8% among women vs. 10.3% among men, SMD = 0.136), anxiety disorders (14.5% among women vs. 9.5% among men, SMD = 0.155), dementia (10.2% among women vs. 6.3% among men, SMD = 0.142), and delusional/mood disorders (17.3% among women vs. 10.9% among men, SMD = 0.184).
Table 2.
Comorbidities prior to the event
| Women | Men | SMD | |
|---|---|---|---|
| n | 14 270 | 29 023 | |
| Anxiety disorders | 2075 (14.5) | 2763 (9.5) | 0.155 |
| Aortic valve disorder | 793 (5.6) | 1793 (6.2) | 0.026 |
| Atrial fibrillation | 2475 (17.3) | 6575 (22.7) | 0.133 |
| Arthrosis | 2615 (18.3) | 3994 (13.8) | 0.125 |
| Chronic ischaemic heart disease | 2126 (14.9) | 7061 (24.3) | 0.239 |
| Chronic obstructive pulmonary disease | 2110 (14.8) | 2991 (10.3) | 0.136 |
| Diabetes mellitus type 1 | 928 (6.5) | 2129 (7.3) | 0.033 |
| Diabetes mellitus type 2 | 2510 (17.6) | 5651 (19.5) | 0.048 |
| Delusional/mood disorders | 2465 (17.3) | 3161 (10.9) | 0.184 |
| Dementia | 1451 (10.2) | 1819 (6.3) | 0.142 |
| Heart failure | 3029 (21.2) | 7079 (24.4) | 0.075 |
| Hypertension | 6616 (46.4) | 12 572 (43.4) | 0.061 |
| Kidney disease | 1214 (8.5) | 3029 (10.4) | 0.066 |
| Late effects of cerebrovascular disease | 948 (6.7) | 2042 (7.0) | 0.016 |
| Myocardial infarction | 1526 (10.7) | 4372 (15.1) | 0.131 |
| Stroke | 1229 (8.6) | 2537 (8.7) | 0.005 |
| Substance abuse disorder | 1944 (13.6) | 4472 (15.4) | 0.051 |
Values are n (%).SMD, standardized mean difference.
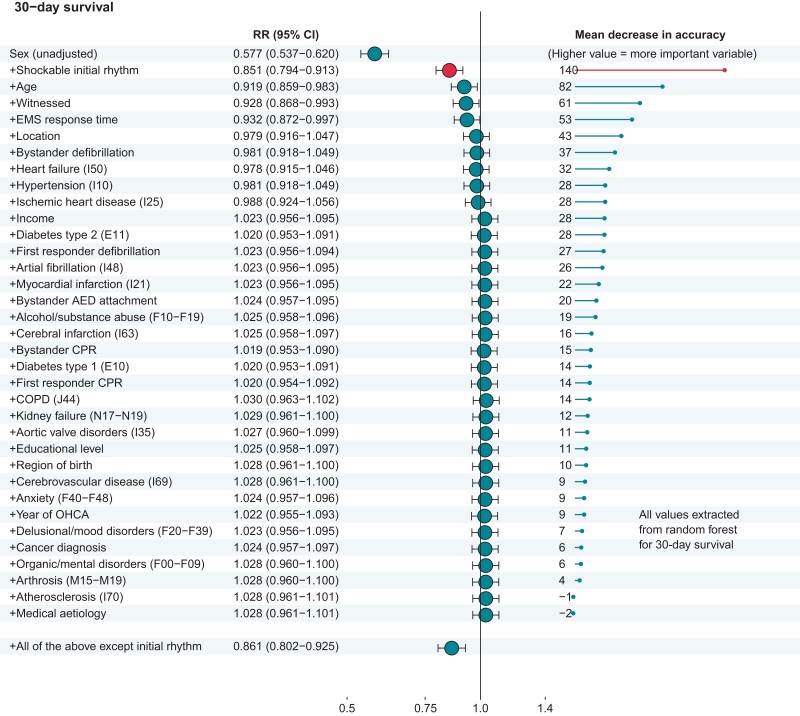
Figure 2 shows the results of the regression analyses. The crude association for female sex and 30-day survival was RR = 0.577 (95% CI 0.537–0.620). After adjustment for initial rhythm the association weakens to RR = 0.851 (95% CI = 0.794–0.913). Further adjustment for age, witness status, EMS response time and location reduces the association to RR = 0.979 (95% CI = 0.916–1.047). After adding heart failure, hypertension, ischaemic heart disease, and disposable income, the estimate favours female sex (RR = 1.023, 95% CI = 0.956–1.095). If all variables except initial rhythm were added the association between female sex and 30-day survival was still negative (RR = 0.861, 95% CI = 0.802–0.925).
Figure 2.
Association between female sex and 30-day survival post-OHCA. Male sex comparison. Results from regression analyses. AED, automated external defibrillator; COPD, chronic obstructive pulmonary disease; CPR, cardiopulmonary resuscitation; EMS, Emergency medical services; OHCA, out-of-hospital cardiac arrest; RR, relative risks.
The crude association between female sex and 1-day survival was RR = 0.855 (95% CI 0.822–0.888) (see Supplementary material online, Figure S1). Stepwise adjustment for initial rhythm attenuated the survival difference between sexes to null (RR = 1.033; 95% CI 0.994–1.073).
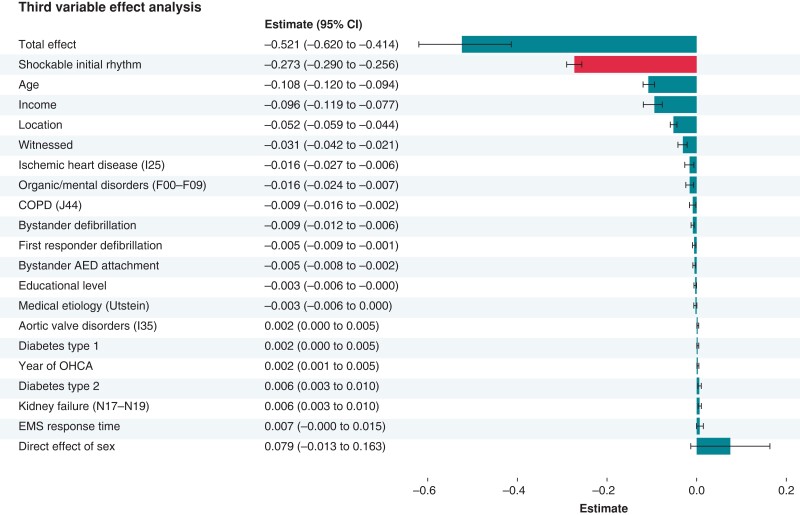
Figure 3 shows the results from the third-variable effect analysis, where most variables were potential mediators. The total effect of female sex is negative (−0.521). The variable with the largest relative effect was shockable initial rhythm which explains ∼50% of the negative association between female sex and 30-day OHCA survival. Age and disposable income were the second and third most important variables, respectively, followed by location and witnessed status. The rest of the variables explain only minor parts of the association seen between female sex and 30-day survival after OHCA. The direct effect of sex after adjustments is slightly positive but did not reach statistical significance (0.079, 95% CI = −0.013–0.163).
Figure 3.
Results from third-variable effect (mediation) analysis. Third-variable effect refers to the effect transmitted by a variable that intervene in the relationship between an exposure and a response variable. The direct effect of sex in the last row is the effect of sex when all mediating factors are accounted for. AED, automated external defibrillator; COPD, chronic obstructive pulmonary disease; EMS, Emergency medical services; OHCA, out-of-hospital cardiac arrest.
To further explore the difference in VT/VF at presentation we performed a sensitivity analysis with VT/VF as an outcome. Female sex was associated with lower chance of VT/VF at presentation despite adjustment for all covariables, RR 0.65 (95% CI 0.62–0.68) (see Supplementary material online, Figure S2).
Finally, a supplementary analysis was performed to explore how the main determinants, shockable rhythm, age, and income had evolved over time (see Supplementary material online, Table S1). The proportion of patients with shockable rhythm decreased, and age and disposable income increased for both men and women.
Discussion
The main finding of this nationwide study was that female sex was associated with a lower chance of surviving OHCA. The survival difference between sexes was mainly explained by a significantly lower rate of shockable initial rhythm among women at presentation. Other important explanatory factors of the lower survival rate among women were older age and socioeconomic factors such as disposable income. There was no difference in early treatment such as bystander CPR or EMS response time intervals. Previously known comorbidities explained only a very small portion of the sex difference in survival.
Explanation of the results
Shockable initial rhythm
In our study, women had a significantly lower rate of VT/VF at presentation compared to men. This is in line with other studies that have shown that female sex is independently associated with lower odds of shockable initial rhythm at OHCA presentation.11,19,20 The presence of VT/VF is one of the strongest independent predictors of a favourable outcome after OHCA, with a chance of survival up to 10 times higher than patients presenting with a non-shockable initial rhythm.21 Shockable initial rhythm is associated with shorter duration of so-called no-flow time, i.e. the time with no organ perfusion measured from the time of the collapse to the initiation of CPR.22 A non-shockable initial rhythm could thus be a late manifestation of an untreated non-perfusing ventricular rhythm, such as pulseless VT or VF, that has deteriorated into asystole. Therefore, one possible explanation for a lower rate of VT/VF among women could be patient’s delay or bystander delay, of which the latter has been described earlier.11,23 Hence, the best way to increase overall survival is probably related to the first links of the chain of survival, i.e. early recognition, call for help and short response times.24 Importantly, in our study, there was no significant difference in EMS response time, i.e. the time between the call for an ambulance and the arrival of the ambulance. Moreover, it was no significant difference in bystander CPR between men and women and thus, we believe these factors cannot explain the difference in presenting rhythm (see Supplementary material online, Figure S2). On the other hand, we found that men were more likely to be defibrillated by a public automated external defibrillator (AED) or by a first responder such as fire-fighters. This could be linked to the lower proportion of shockable rhythm among women but also the higher proportion of OHCA in public locations among men, where early defibrillation can occur sooner. The time between collapse and ambulance call was not available for the present study. It remains unclear whether there is a longer delay between collapse to call among women, and the fact that women more often suffered cardiac arrest at home could support a longer delay between collapse and ambulance call.
Ischaemic heart disease is more likely to be a causative factor for OHCA in patients presenting with shockable, compared to non-shockable initial rhythm.25 Hence, the lower rate of VT/VF among women with OHCA might be explained by the fact that women who suffer from sudden cardiac arrest have a lower prevalence of underlying structural heart disease or left ventricular dysfunction than men.7,26–29 Furthermore, female survivors after sudden cardiac arrest are less likely to have underlying coronary artery disease compared to men.30 In the present study we tried to take this into account by adjusting for prior comorbidity such as previous diagnoses of cardiovascular and pulmonary disease, however, the difference in VT/VF between sexes remained and is thus not entirely explained by previous known comorbidities. This is in line with a previous study by van Dongen et al. 31 found that comorbidities only modestly explained the lower odds of shockable initial rhythm among women with OHCA. It is important to note that in the present study the exact aetiology of the cardiac arrest remains unknown, thus, sex differences in the underlying cause of the event could still be a possible explanatory factor.
Age
Older age was the second most important explanatory variable to the lower survival rate among women seen in our study. Older age is known to be associated with poorer survival following OHCA. However, age has been found to be a much weaker predictor of survival than other factors such as initial rhythm, which is in line with our results.32 Furthermore, survival rates among elderly with favourable resuscitation characteristics are reported to be 10% or higher and have improved over the last years.33,34 Therefore, age alone cannot explain the difference in survival rates between men and women post-OHCA.
Treatment
We found no difference in bystander CPR and witness status between men and women. This is encouraging since several studies have reported the opposite.8,11,23 The results of our study is in line with a recent study published by Ok Ahn et al. 35 who found that women and men received bystander CPR to the same extent. They also found that the association between bystander CPR and survival was weaker in women than in men, which raises the question if the quality of the CPR that women receive is inferior to CPR given to men. With the present study’s result at hand, a potential hypothesis for this finding is that CPR given to women is less effective because of their underlying non-shockable rhythm, rather than the quality of the CPR itself. For the present study, we did not have information on CPR quality.
We observed that women had a lower chance of surviving their in-hospital stay than men, but they also had a higher survival rate to 1 day after admission than 30 days post-OHCA. This suggests that women have a higher in-hospital mortality than men. For the present study, we did not have information on in-hospital treatment, but there is evidence that post-resuscitation care differs between sexes, where women undergo coronary angiography and targeted temperature management therapy to a lesser extent than men.8 Whether these factors can explain lower in-hospital survival rate among women in our study remains unclear. Initial rhythm may also impact in-hospital treatment, as VT/VF is commonly associated with ischaemic heart disease OHCA patients with shockable initial rhythm may undergo coronary angiography to a greater extent than patients presenting with non-shockable rhythm.
Comorbidity
Women with OHCA had a higher rate of psychiatric disorders and a lower rate of ischaemic heart disease than men in our study. These are both factors that could affect the presenting rhythm, since ischaemic heart disease increases the risk of VT/VF, whereas antipsychotic drugs have been found to be independently associated with a non-shockable initial rhythm.36,37 Moreover, COPD was more prevalent among women and is also associated with non-shockable cardiac arrest according to previous studies.11,37
Socioeconomic factors
The third most important variable to explain the sex difference in survival in our study was disposable income. This is in line with previous studies on socioeconomic status, where low socioeconomic status was associated with increased risk of OHCA, decreased chance to receive bystander CPR and poorer survival.38 The difference in incidence and mortality probably reflects differences in coronary heart disease risk factors, comorbidity burden, and health literacy.
In our study, women suffered from OHCA at home to a larger extent than men, which is in line with previous studies.8,11 This is a factor associated with poorer prognosis independent of age, bystander CPR, witnessed status, presenting rhythm, and time intervals.39,40 Furthermore, the use of public-access defibrillators at home is extremely rare.41 Being at home at the time of the event could also be a proxy for activity level or frailty.
Strengths and limitations
The main strength of this study was the large study population and its nationwide coverage. To our knowledge this was the first mediation analysis trying to specify which parameters that explain sex difference in survival after OHCA. Another strength was that we had information about prior comorbidities before the cardiac arrest, as well as socioeconomic status, both from national registries with excellent coverage. Follow-up was almost complete.
Limitations of the study were that it was an observational study, and therefore carries a risk of residual confounding. We did not have information on time delay from cardiac arrest to call. Neither did we have data on in-hospital treatment, nor information on the true OHCA aetiology in terms of autopsies or cause of death. Also, the study relies on the quality of the data in the registries used and the reporting to the SRCR carries the risk of selection bias or systematic misclassification and has not been completely validated yet.
The use of ICD codes for comorbidity is derived from a nationwide register that capture hospital based inpatient or outpatient care. Therefore, mild forms could be present but treated at the primary health level of care, and not captured in our register. It is possible that pattern of seeking care (primary health level vs. hospital level) differs between sexes. Secondly, access to care and socioeconomic factors could influence seeking patterns. However, the Swedish health care system is publicly financed which may attenuate those differences. We chose to include all diagnoses in NPR with a prevalence over 5%, which is an arbitrary threshold. We reasoned that diagnoses with a lower prevalence, although maybe relevant in the individual case, would not affect overall results.
Finally, the generalizability of these findings to other countries remains uncertain. Studies in other national registries will be required to confirm if these potential mechanisms are more universal or unique to Sweden.
Conclusions
In this nationwide study, women have a lower 30-day survival following OHCA compared to men. The poor prognosis is primarily explained by the absence of shockable initial rhythm, followed by older age at presentation and lower disposable income.
Clinical perspectives
On a population level, women presenting with OHCA are less likely to have traditional risk factors predicting the event, such as ischaemic heart disease. Thus, the lower rate of shockable initial rhythm observed in women could reflect a lower prevalence of underlying structural heart disease or left ventricular dysfunction and point to other causes for OHCA among women. Further research addressing sex-specific preventive measures with regard to sudden cardiac arrest is warranted.
Supplementary Material
Contributor Information
Charlotte Miedel, Department of Clinical Science and Education, Center for Resuscitation Science, Södersjukhuset, Karolinska Institutet, Sjukhusbacken 10, 118 83, Stockholm, Sweden.
Martin Jonsson, Department of Clinical Science and Education, Center for Resuscitation Science, Södersjukhuset, Karolinska Institutet, Sjukhusbacken 10, 118 83, Stockholm, Sweden.
Mariana Dragas, Department of Clinical Science and Education, Center for Resuscitation Science, Södersjukhuset, Karolinska Institutet, Sjukhusbacken 10, 118 83, Stockholm, Sweden.
Therese Djärv, Department of Clinical Science and Education, Center for Resuscitation Science, Södersjukhuset, Karolinska Institutet, Sjukhusbacken 10, 118 83, Stockholm, Sweden; Department of Medicine, Karolinska Institutet, Solna, Sweden.
Per Nordberg, Department of Clinical Science and Education, Center for Resuscitation Science, Södersjukhuset, Karolinska Institutet, Sjukhusbacken 10, 118 83, Stockholm, Sweden.
Araz Rawshani, Department of Molecular and Clinical Medicine, Institute of Medicine, University of Gothenburg, Sahlgrenska Academy, Gothenburg, Sweden.
Andreas Claesson, Department of Clinical Science and Education, Center for Resuscitation Science, Södersjukhuset, Karolinska Institutet, Sjukhusbacken 10, 118 83, Stockholm, Sweden; Department of Molecular and Clinical Medicine, Institute of Medicine, University of Gothenburg, Sahlgrenska Academy, Gothenburg, Sweden.
Sune Forsberg, Department of Clinical Science and Education, Center for Resuscitation Science, Södersjukhuset, Karolinska Institutet, Sjukhusbacken 10, 118 83, Stockholm, Sweden.
Anette Nord, Department of Clinical Science and Education, Center for Resuscitation Science, Södersjukhuset, Karolinska Institutet, Sjukhusbacken 10, 118 83, Stockholm, Sweden.
Johan Herlitz, Department of Clinical Science and Education, Center for Resuscitation Science, Södersjukhuset, Karolinska Institutet, Sjukhusbacken 10, 118 83, Stockholm, Sweden; Prehospen-Centre for Prehospital Research, Faculty of Caring Science, Work-Life and Social Welfare, University of Borås, Borås, Sweden.
Gabriel Riva, Department of Clinical Science and Education, Center for Resuscitation Science, Södersjukhuset, Karolinska Institutet, Sjukhusbacken 10, 118 83, Stockholm, Sweden.
Supplementary material
Supplementary material is available at Europace online.
Funding
G.R. has received research grants from the Region Stockholm (ALF) and the Swedish Heart and Lung Foundation. The funding bodies had no role in the design of this study or decision to submitt for publication.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
- 1. Empana JP, Lerner I, Valentin E, Folke F, Böttiger B, Gislason G et al. Incidence of sudden cardiac death in the European Union. J Am Coll Cardiol 2022;79:1818–27. [DOI] [PubMed] [Google Scholar]
- 2. Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation 2010;81:1479–87. [DOI] [PubMed] [Google Scholar]
- 3. Gräsner JT, Wnent J, Herlitz J, Perkins GD, Lefering R, Tjelmeland I et al. Survival after out-of-hospital cardiac arrest in Europe - results of the EuReCa TWO study. Resuscitation 2020;148:218–26. [DOI] [PubMed] [Google Scholar]
- 4. Chan PS, McNally B, Tang F, Kellermann A. Recent trends in survival from out-of-hospital cardiac arrest in the United States. Circulation 2014;130:1876–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Malik A, Gewarges M, Pezzutti O, Allan KS, Samman A, Akioyamen LE et al. Association between sex and survival after non-traumatic out of hospital cardiac arrest: a systematic review and meta-analysis. Resuscitation 2022;179:172–82. [DOI] [PubMed] [Google Scholar]
- 6. Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 2010;3:63–81. [DOI] [PubMed] [Google Scholar]
- 7. Chugh SS, Uy-Evanado A, Teodorescu C, Reinier K, Mariani R, Gunson K et al. Women have a lower prevalence of structural heart disease as a precursor to sudden cardiac arrest: the ore-SUDS (Oregon Sudden Unexpected Death Study). J Am Coll Cardiol 2009;54:2006–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Feng D, Li C, Yang X, Wang L. Gender differences and survival after an out-of-hospital cardiac arrest: a systematic review and meta-analysis. Intern Emerg Med 2021;16:765–75. [DOI] [PubMed] [Google Scholar]
- 9. Kim C, Fahrenbruch CE, Cobb LA, Eisenberg MS. Out-of-hospital cardiac arrest in men and women. Circulation 2001;104:2699–703. [DOI] [PubMed] [Google Scholar]
- 10. Lampert R, McPherson CA, Clancy JF, Caulin-Glaser TL, Rosenfeld LE, Batsford WP. Gender differences in ventricular arrhythmia recurrence in patients with coronary artery disease and implantable cardioverter-defibrillators. J Am Coll Cardiol 2004;43:2293–9. [DOI] [PubMed] [Google Scholar]
- 11. Blom MT, Oving I, Berdowski J, van Valkengoed IGM, Bardai A, Tan HL. Women have lower chances than men to be resuscitated and survive out-of-hospital cardiac arrest. Eur Heart J 2019;40:3824–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Statistics Sweden . https://www.statistikdatabasen.scb.se/pxweb/sv/ssd/ (1 January 2023, date last accessed).
- 13. Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation 2015;132:1286–300. [DOI] [PubMed] [Google Scholar]
- 14. Strömsöe A, Svensson L, Axelsson ÅB, Göransson K, Todorova L, Herlitz J. Validity of reported data in the Swedish Cardiac Arrest Register in selected parts in Sweden. Resuscitation 2013;84:952–6. [DOI] [PubMed] [Google Scholar]
- 15. Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C et al. External review and validation of the Swedish national inpatient register. BMC Public Health 2011;11:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ludvigsson JF, Svedberg P, Olén O, Bruze G, Neovius M. The longitudinal integrated database for health insurance and labour market studies (LISA) and its use in medical research. Eur J Epidemiol 2019;34:423–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702–6. [DOI] [PubMed] [Google Scholar]
- 18. Yu Q, Wu X, Li B, Scribner RA. Multiple mediation analysis with survival outcomes: with an application to explore racial disparity in breast cancer survival. Stat Med 2019;38:398–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kotini-Shah P, Del Rios M, Khosla S, Pugach O, Vellano K, McNally B et al. Sex differences in outcomes for out-of-hospital cardiac arrest in the United States. Resuscitation 2021;163:6–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Teodorescu C, Reinier K, Dervan C, Uy-Evanado A, Samara M, Mariani R et al. Factors associated with pulseless electric activity versus ventricular fibrillation: the Oregon sudden unexpected death study. Circulation 2010;122:2116–22. [DOI] [PubMed] [Google Scholar]
- 21. Herlitz J, Svensson L, Engdahl J, Silfverstolpe J. Characteristics and outcome in out-of-hospital cardiac arrest when patients are found in a non-shockable rhythm. Resuscitation 2008;76:31–6. [DOI] [PubMed] [Google Scholar]
- 22. Cournoyer A, de Montigny L, Potter BJ, Segal E, Chauny JM, Lamarche Y et al. Can a shockable initial rhythm identify out-of-hospital cardiac arrest patients with a short no-flow time? Resuscitation 2021;158:57–63. [DOI] [PubMed] [Google Scholar]
- 23. Blewer AL, McGovern SK, Schmicker RH, May S, Morrison LJ, Aufderheide TP et al. Gender disparities among adult recipients of bystander cardiopulmonary resuscitation in the public. Circ Cardiovasc Qual Outcomes 2018;11:e004710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Waalewijn RA, Nijpels MA, Tijssen JG, Koster RW. Prevention of deterioration of ventricular fibrillation by basic life support during out-of-hospital cardiac arrest. Resuscitation 2002;54:31–6. [DOI] [PubMed] [Google Scholar]
- 25. Kauppila JP, Hantula A, Kortelainen ML, Pakanen L, Perkiömäki J, Martikainen M et al. Association of initial recorded rhythm and underlying cardiac disease in sudden cardiac arrest. Resuscitation 2018;122:76–8. [DOI] [PubMed] [Google Scholar]
- 26. Kannel WB, Wilson PW, D'Agostino RB, Cobb J. Sudden coronary death in women. Am Heart J 1998;136:205–12. [DOI] [PubMed] [Google Scholar]
- 27. Lerner DJ, Kannel WB. Patterns of coronary heart disease morbidity and mortality in the sexes: a 26-year follow-up of the Framingham population. Am Heart J 1986;111:383–90. [DOI] [PubMed] [Google Scholar]
- 28. Albert CM, Chae CU, Grodstein F, Rose LM, Rexrode KM, Ruskin JN et al. Prospective study of sudden cardiac death among women in the United States. Circulation 2003;107:2096–101. [DOI] [PubMed] [Google Scholar]
- 29. Linde C, Bongiorni MG, Birgersdotter-Green U, Curtis AB, Deisenhofer I, Furokawa T et al. Sex differences in cardiac arrhythmia: a consensus document of the European Heart Rhythm Association, endorsed by the Heart Rhythm Society and Asia Pacific Heart Rhythm Society. Europace 2018;20:1565–1565ao. [DOI] [PubMed] [Google Scholar]
- 30. Albert CM, McGovern BA, Newell JB, Ruskin JN. Sex differences in cardiac arrest survivors. Circulation 1996;93:1170–6. [DOI] [PubMed] [Google Scholar]
- 31. van Dongen LH, Oving I, Dijkema PW, Beesems SG, Blom MT, Tan HL. Sex differences in the association of comorbidity with shockable initial rhythm in out-of-hospital cardiac arrest. Resuscitation 2021;167:173–9. [DOI] [PubMed] [Google Scholar]
- 32. Kim C, Becker L, Eisenberg MS. Out-of-hospital cardiac arrest in octogenarians and nonagenarians. Arch Intern Med 2000;160:3439–43. [DOI] [PubMed] [Google Scholar]
- 33. Libungan B, Lindqvist J, Strömsöe A, Nordberg P, Hollenberg J, Albertsson P et al. Out-of-hospital cardiac arrest in the elderly: a large-scale population-based study. Resuscitation 2015;94:28–32. [DOI] [PubMed] [Google Scholar]
- 34. Kitamura T, Morita S, Kiyohara K, Nishiyama C, Kajino K, Sakai T et al. Trends in survival among elderly patients with out-of-hospital cardiac arrest: a prospective, population-based observation from 1999 to 2011 in Osaka. Resuscitation 2014;85:1432–8. [DOI] [PubMed] [Google Scholar]
- 35. Ok Ahn K, McNally B, Al-Araji R, Cisneros C, Chan PS. Sex differences in the association between bystander CPR and survival for out-of-hospital cardiac arrest. Resuscitation 2022;182:109603. [DOI] [PubMed] [Google Scholar]
- 36. Teodorescu C, Reinier K, Uy-Evanado A, Chugh H, Gunson K, Jui J et al. Antipsychotic drugs are associated with pulseless electrical activity: the Oregon sudden unexpected death study. Heart Rhythm 2013;10:526–30. [DOI] [PubMed] [Google Scholar]
- 37. Granfeldt A, Wissenberg M, Hansen SM, Lippert FK, Lang-Jensen T, Hendriksen OM et al. Clinical predictors of shockable versus non-shockable rhythms in patients with out-of-hospital cardiac arrest. Resuscitation 2016;108:40–7. [DOI] [PubMed] [Google Scholar]
- 38. van Nieuwenhuizen BP, Oving I, Kunst AE, Daams J, Blom MT, Tan HL et al. Socio-economic differences in incidence, bystander cardiopulmonary resuscitation and survival from out-of-hospital cardiac arrest: a systematic review. Resuscitation 2019;141:44–62. [DOI] [PubMed] [Google Scholar]
- 39. Litwin PE, Eisenberg MS, Hallstrom AP, Cummins RO. The location of collapse and its effect on survival from cardiac arrest. Ann Emerg Med 1987;16:787–91. [DOI] [PubMed] [Google Scholar]
- 40. Herlitz J, Eek M, Holmberg M, Engdahl J, Holmberg S. Characteristics and outcome among patients having out of hospital cardiac arrest at home compared with elsewhere. Heart 2002;88:579–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kiyohara K, Nishiyama C, Matsuyama T, Sado J, Kitamura T, Shimamoto T et al. Out-of-Hospital cardiac arrest at home in Japan. Am J Cardiol 2019;123:1060–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.