Abstract
Background
Working in the nursing profession is hazardous, and nurses report poor health. Risk factors associated with poor health outcomes have been documented. However, the extent of literature exploring the prevalence of health conditions among American nurses that may be attributable to their work has not been examined.
Method
A scoping review following the Joanna Briggs Institute recommendations was conducted of peer-reviewed quantitative studies to answer the question: What are health conditions experienced by American nurses that may be attributable to their work as nurses?
Results
Thirty articles met the inclusion criteria. Due to the methods used in many articles, studies of the prevalence of health conditions among the nursing population were lacking. Health conditions studied broke into six categories: (a) work-related injuries and hazards; (b) unhealthy lifestyles; (c) mental health conditions; (d) burnout; (e) fatigue, sleep, and migraines; and (f) reproductive health. The role of work in the health conditions studied varied from an immediate impact on health (e.g., a needlestick or injury) to a cumulative impact (e.g., scheduling or workplace demands). Within the work demands, the physical environment; physical, emotional, and cognitive demands of work; and shiftwork were all frequently identified as antecedents that could be further explored and addressed to improve nurse health.
Conclusions
Healthcare systems should seek to address the hazards and exposures that may be linked to health conditions in the nursing workforce. Understanding and mitigating the impact of the pandemic and nursing work on the workforce's health is crucial to the solvency of the workforce. Occupational health practitioners should assess for workplace hazards and exposures.
Keywords: Nurse, health condition, scoping review, incidence/prevalence, occupational health and safety, workforce
Introduction
Nurses are the single largest group of healthcare professionals in the United States. Their contribution to population health includes, but is not limited to: health promotion, illness prevention, alleviation of suffering, and protection of patients (American Nurses Association, n.d.). The U.S. Bureau of Labor (2022) projects 194,500 additional nurses will be needed annually between 2020 and 2030. To address the shortage, multiple levers need to be pulled by policymakers, including expanding the pipeline of those entering the workforce and improving retention of those in the workforce (Drennan & Ross, 2019). Factors in nurse retention include macro-level health systems, the healthcare facility, individual nurse factors, and living conditions (Efendi et al., 2019). In the United States, the pipeline of nurses entering the workforce has increased; however, the healthcare work environment has been labeled as “hazardous” by the Occupational Safety and Health Administration (2013), and nurse retention continues to be an issue. Globally, the COVID-19 pandemic has only exacerbated these workforce issues. Nurses who report work-related disabilities and illnesses and experience high demands, burnout, and dissatisfaction with schedule and staffing were more likely to leave the profession of nursing rather than turn over to a different nursing position (Mazurenko et al., 2015). The United States Bureau of Labor Statistics (2018) reported that nurses experienced higher incidences of work injury and illness rates (104.2 cases per 10,000 workers) than the rate for all occupations (91.7 cases per 10,000 workers). Additionally, over 50% of American nurses report suboptimal mental and physical health (Mazurek Melnyk et al., 2018). Therefore, improving the health, well-being, and safety of nurses may improve nurse retention, combat the shortage, and improve their health. However, there is currently a lack of understanding of specific health conditions that nurses experience at higher rates that may be related to their nursing work that can be addressed through changes to the work environment and interventions. To develop interventions to address health conditions related to nurses’ work, researchers, clinicians, and healthcare system leaders need to understand what health conditions nurses are experiencing at higher rates than the general population that may be attributable to their occupation. Therefore, this review asks the question: What are health conditions experienced by American nurses that may be attributable to their work as nurses? A scoping review design with a systematic search strategy was chosen to conduct a preliminary assessment of the potential size and scope of available research literature on this topic (Grant & Booth, 2009).
Nurses are exposed to a variety of hazards due to the demands of their work; examples include safety, chemical, biological, and mental health hazards at work (Mitchell, 2020). Safety hazards of nursing work may include risks such as lifting injuries from moving patients, handling of equipment, slips or falls, and patient violence. Examples of biological and chemical risks include medication administration (e.g., antineoplastic medications), procedures (e.g., needlesticks injury or radiation from radiography), or transmissible illnesses (e.g., COVID-19). In addition, stress experienced at work can negatively affect health; by its nature, nursing work is “stressful” (Cox et al., 1996). This can be compounded by shiftwork common in many nursing positions, which can negatively impact nurses and their patient care (Admi et al., 2008). Therefore, this scoping review aimed to explore health conditions among American nurses that may be attributable to their work.
Method
A scoping review design was chosen to conduct a preliminary assessment of the potential size and scope of available research literature on this topic (Grant & Booth, 2009). The scoping review recommendations by Joanna Briggs Institute (Peters et al., 2021) guided this review process, and the systematic and reporting were guided by PRISMA extension for scoping reviews (PRISMA-ScR; Tricco et al., 2018).
Search Strategy
A comprehensive search was designed using a series of free text terms and subject headings and performed by a medical librarian (MS) in the CINAHL Plus with Full Text (EBSCOHost, 1937–present) and PubMed databases on 26 August 2019. Results were deduplicated in EndNote X9 software and uploaded into Covidence (2020) for screening and analysis of the title and abstract. Then a full-text examination and risk of bias assessment was completed. Team members performed a norming exercise prior to screening to ensure consistency. Two independent reviewers screened each article, with any discrepancies resolved by discussion and a tiebreaker as needed. The search was updated using the same databases and strategies on 7 April 2021, and results were added to the report. The reference lists of study reports included in the systematic review were carefully examined for additional citations; 19 articles were added for screening after reference list searching was completed. Study data were extracted in Covidence using a data template developed in Extraction 1.0. The initial search strategy was developed in PubMed and adapted to CINAHL (see Table 1 for strategy). No date limits or other filters were used in either database.
Table 1.
Search Strategy.
| PubMed and CINAHL search strategies |
| PubMed search strategy |
| (“Nursing/statistics and numerical data”[Mesh] OR “Nursing Staff/statistics and numerical data”[Mesh] OR “Nurses/statistics and numerical data”[Mesh]) |
| AND |
| (“Diseases Category”[Mesh] OR “Mental Disorders”[Mesh] OR “Accidents, Occupational”[Mesh] OR “Behavioral Symptoms”[Mesh] OR “Occupational Diseases”[Mesh] OR “Occupational Exposure”[Mesh] OR “work related”[Title/Abstract] OR work-related[Title/Abstract]) |
| AND |
| English[lang] |
| NOT |
| (“Africa”[Mesh] OR “Asia”[Mesh] OR “Europe”[Mesh] OR “Oceania”[Mesh]) |
| CINAHL search strategy |
| (MH “Nurses+/SN”) |
| AND |
| (MH “Disease+”) OR (MH “Mental Disorders+”) OR (MH “Behavioral |
| Symptoms+”) OR (MH “Accidents, Occupational+”) OR (MH “Occupational |
| Exposure”) OR (MH “Occupational Diseases+”) OR TI (“work related” OR work related) OR AB (“work related” OR work-related) |
| NOT |
| (MH “Africa+”) OR (MH “Asia+”) OR (MH “Europe+”) OR (MH “Australia+”) OR (MH “Pacific Islands+”) |
Inclusion and Exclusion Criteria
The inclusion criteria were a study population of U.S. registered nurses employed at the time of the study, a focus on the prevalence of a health condition, and the use of a quantitative research methodology. Exclusion criteria were any type of intervention study, not working RN sample, non-U.S. sample, not a peer-reviewed publication, no prevalence data, not quantitative, non-English language publication, or lack statistical support as the rationale for sample size. Note that the year of publication was not included in the inclusion criteria as the researchers sought to capture the breadth of work on this topic. A significant source of research on nurses’ health within the United States is the Nurses’ Health Study (NHS, 2016) (and subsequent Nurses’ Health Study II) which are longitudinal cohort studies that have recruited primarily nurses (n = 280,000+) to investigate the risk factors for chronic disease in women in the United States. The NHS 3 is the next wave of the study and recruits from the United States and Canada. However, as occupational factors are not the primary focus and nurses outside of the United States were recruited for subsequent cohorts, many of these articles did not meet this review's criteria.
Risk of Bias and Data Extraction
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines were used to report the risk of bias and transparency of the studies in the review (Cuschieri, 2019). The STROBE guidelines were not used to assess the quality of studies, nor was it used to exclude studies from the systematic review. The risk of bias was determined by assessing the title/abstract (Q1), background (Q2), objectives (Q3), methods (Q4-12), results (Q13–17), discussion (Q18–20), and funding information (Q21). Reported bias was scored as either having a low (L), high (H), or unclear (?) risk of bias for each study by two readers, and conflicts were discussed until a consensus was achieved (Table 2). Data were extracted by the first reader and confirmed by the second reader into Excel, where the following categories were filled in for each article: (a) author and year, (b) study design, (c) year data collected, (d) condition studied, (e) sample size, and (f) findings. Health conditions studied were thematically grouped by the first author and agreed upon by the whole team. The data extraction can be found in Table 3.
Table 2.
Risk of Bias Assessment.
| Study | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Q14 | Q15 | Q16 | Q17 | Q18 | Q19 | Q20 | Q21 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| McAbee et al. (1993) | H | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | ? | L |
| Shortridge et al. (1995) | L | L | L | L | L | L | L | L | ? | L | L | L | L | L | L | L | L | H | L | ? | L |
| Jason et al. (1998) | L | ? | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L |
| Durham et al. (1998) | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | H | L | H |
| Trinkoff and Storr (1998) | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L |
| Trinkoff et al. (1999) | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | ? | ? |
| Trinkoff et al. (2001) | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | H | L |
| Trinkoff et al. (2002) | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | H | L | L | L |
| Gerberich et al. (2004) | L | L | ? | L | L | L | L | ? | L | L | L | L | L | L | L | L | L | L | L | ? | ? |
| Clarke (2007) | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | ? | L |
| Feskanich et al. (2009) | L | L | L | L | L | H | L | H | L | L | L | L | L | L | L | L | L | L | L | H | L |
| Rodriguez-Acosta et al. (2009) | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | H | L | ? | L |
| Olds and Clarke (2010) | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L |
| McHugh et al. (2011) | L | L | L | L | ? | H | L | L | L | L | L | ? | L | L | L | L | L | L | L | L | L |
| Han et al. (2011) | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | ? | ? |
| Perhats et al. (2012) | L | L | L | L | L | L | L | L | L | L | L | L | L | H | L | L | L | L | L | L | ? |
| Han et al. (2012) | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | ? | L |
| Monroe et al. (2013) | L | L | L | L | L | L | H | L | L | L | L | L | L | H | Y | Y | Y | Y | Y | Y | Y |
| Lee et al. (2015) | L | L | L | L | L | L | L | H | L | L | L | L | L | L | L | L | L | L | L | L | L |
| Unruh and Asi (2018) | L | L | L | L | L | H | L | L | L | L | L | L | L | L | L | H | L | L | L | H | L |
| Dyrbye et al. (2019) | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L |
| Davidson et al. (2020) | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L |
| Patrician et al. (2020) | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L |
| Vogus et al. (2020) | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L |
| Kim et al. (2021) | L | L | L | L | L | H | L | L | H | H | L | L | L | L | L | L | L | L | L | H | L |
| Melnyk et al. (2018) | L | L | L | L | L | L | L | L | ? | L | L | L | L | L | L | L | L | L | L | ? | ? |
| Kunert et al. (2007) | L | L | H | L | H | H | L | L | L | L | L | L | H | L | L | L | L | L | L | L | H |
| Davidson et al. (2019) | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | H |
Note. Critical appraisal assessment was completed with L = low,= missing or unclear, and H = high.
Table 3.
Description of the Included Studies.
| Author, year | Study design | Year data collected | Condition studied | Sample size | Findings |
|---|---|---|---|---|---|
| McAbee et al. (1993) | Retrospective cross-sectional study | Not explicitly stated | Reproductive health | n = 663 | There may be an effect of radiation and other nursing occupational hazards on stillbirths and miscarriages. |
| Shortridge et al. (1995) | Cross-sectional correlational study | 1986 | Reproductive health | n = 1,458 | The study indicated that may be an association between nurse occupational exposure to antineoplastic medications and menstrual dysfunction. |
| Jason et al. (1998) | Questionnaire | 1991 | Fatigue, sleep, and migraines | n = 3,400 | Nurses in the study had a prevalence rate of 1,088 per 100,000 and a lifetime prevalence of 1,265 per 100,000 for chronic fatigue syndrome (CFS) which may indicate that prevalence rates for CFS may be higher for nurses possibly due to them being in a high-risk group for occupational stressors (i.e., shift work, exposure to viruses, accidents, etc.) |
| Durham et al. (1998) | Cross-sectional; survey | 1991 | Fatigue, sleep, and migraines | n = 2,949 | 17% of nurses in sample had migraines and nurses who had migraines had significantly lower work productivity and quality of life than those nurses compared to nurses with nonmigraine/nonsevere headaches. |
| Trinkoff and Storr (1998) | Cross-sectional study | 1994 | Unhealthy lifestyles | n = 4,438 | The combined prevalence of substance use in the past year was 32% with 16% reporting binge drinking, 14% reporting cigarette smoking, 7% reporting prescription-type drugs and 4% reporting marijuana/cocaine use. |
| Trinkoff et al. (1999) | Cross-sectional survey | 1994 | Unhealthy lifestyles | n = 3,917 | Nurses who reported easier perceived availability, who administered drugs daily, and with poor to nonexistent workplace controls, each had almost twice the odds of prescription-type drug use. |
| Trinkoff et al. (2001) | Cross-sectional survey | 1994–1995 | Fatigue, sleep, and migraines | n = 3,727 | 7% of nurses reported that they daily or always got less sleep than they thought they should. |
| Trinkoff et al. (2002) | Cross-sectional survey | 1999–2000 | Work-related injuries and hazards | n = 1,163 | Within the last year, 45.8%, 35.1%, and 47.0% of nurses had neck, shoulder, or back musculoskeletal problems respectively. |
| Gerberich et al. (2004) | Comprehensive surveys | 1998 | Work-related injuries and hazards | n = 2,975 | The adjusted rates of physical assaults experienced by nurses per 100 persons were 12.0 and 38.5 per 100 persons for nonphysical violence. |
| Kunert et al. (2007) | Cross-sectional descriptive study | not stated | Fatigue, sleep, and migraines | n = 190 | Night shift nurses perceive a considerably higher level of fatigue and had poorer sleep quality than day shift nurses. |
| Clarke (2007) | Cross-sectional | 1999 | Work-related injuries and hazards | n = 11,516 | Nurses who worked in organizations that were considered “best in class” were 34% less likely to experience needlestick injuries, indicating that nurses’ work environments may be key predictors of needlestick injuries. |
| Feskanich et al. (2009) | Prospective observational study | 1988–2000 | Fatigue, sleep, and migraines | n = 38,062 | Rotating night shift assignments, for prolonged periods, may be a contributing factor to hip and risk fractures. |
| Rodriguez-Acosta et al. (2009) | Retrospective cohort study | 1997–2004 | Work-related injuries and hazards | n = 5,082 | Work-related injuries differ between aides and nurses due to differences in their injury risk profiles and injury outcomes. |
| Olds and Clarke (2010) | Secondary analysis of anonymous surveys | 1999 | Work-related injuries and hazards | n = 11,516 | All adverse events and error variables looked at in this study were significantly related to working more than 40 hr in an average week. |
| McHugh et al. (2011) | Cross-sectional study | 2006–2007 | Burnout | n = 68,724 | Findings show higher job dissatisfaction and burnout among nurses performing patient care in hospitals and nursing homes than in other jobs or settings. |
| Han et al. (2011) | Cross-sectional study | 2002–2003 | Unhealthy lifestyles | n = 2103 | 55% of the nurses in sample were overweight and 27.1% were obese. |
| Neff et al. (2011) | Cross-sectional study | 2007 | Burnout | n = 10951 | 33.8% of nurses working in hospitals, 24.0% working in home health and 27.7% working in nursing homes were burned out. |
| Stimpfel et al. (2012) | Cross-sectional balanced stratified sampling design study | 2005–2008 | Burnout | n = 22,275 | Identified a significant relationship between longer shift lengths and nurse reports of burnout and job dissatisfaction. |
| Perhats et al. (2012) | Cross-sectional survey design | 2009 | Work-related injuries and hazards | n = 2,294 | Found that the three factors that were related to the occurrence of a nonviolence-related workplace injury included: (a) hospitals having safe patient handling policies and programs, (b) access to decontamination and postexposure treatment, and (c) emergency nurses’ perception of staffing in their emergency department. |
| Han et al. (2012) | Cross-sectional study | 2002–2003 | Unhealthy lifestyles | n = 1724 | Nurses with unfavorable work schedules, on average, were younger, had less education, slept less, had more restless sleep, were caregivers for dependents, and their heathy behaviors (exercise sleep) were inversely associated with obesity. |
| Monroe et al. (2013) | Secondary data analyses | 2008–2010 | Unhealthy lifestyles | n = 17,085 | The estimated prevalence of nurses with identified substance-use problems in 2009 was 5.1 per 1000 nurses. |
| Lee et al. (2015) | Cross-sectional stratified design | 2013 | Work-related injuries and hazards | n = 396 | Nurses whose facilities had lift teams, ceiling lifts reported less back and shoulder pain respectively. |
| Melnyk et al. (2018) | Cross-sectional; descriptive study | 2016–2017 | Mental health | n = 1,790 | Nurses had suboptimal health with 54% reporting suboptimal physical health and mental health. A substantial proportion of nurses reported some degree of depression (32.8%), anxiety (51.97%), or stress (38.7%). |
| Unruh and Asi (2018) | Cross-sectional design survey | Not stated | Work-related injuries and hazards | n = 414 | Previous healthcare experience and working longer in the nursing profession were related to higher odds of injury. |
| Davidson et al. (2019) | Descriptive, retrospective longitudinal analysis study | 2015 | Mental health | n = 205 nurse suicides in dataset of 14,774 total suicides | The estimated suicide rate for female nurses was 11.4 per 100,000 while the suicide rate for male nurses was 29.3 per 100,000. |
| Dyrbye et al. (2019) | Multivariable analysis of a cross-sectional survey data | 2017 | Burnout | n = 7,077 | Nurses have a similar risk for burnout as other U.S. workers but are less satisfied with their work–life integration (work hours) than other professions. |
| Davidson et al. (2020) | Descriptive retrospective longitudinal analysis | 2005–2016 | Mental health | n = 1,824 | Nurses are at a greater risk for suicide than the general population. Job problems as well as mental health history were identified as leading factors. Female nurses most often used pharmacological poisoning while male nurses most often used firearms, then pharmacological poisoning. |
| Patrician et al. (2020) | Cross-sectional study of NVDRS data | Data from 2015 but collected 2020 | Mental health | n = 128 RN suicide deaths | The estimated suicide rate for female nurses was 11.4 per 100,000 while the suicide rate for male nurses was 29.3 per 100,000 |
| Vogus et al. (2020) | Cross-sectional analysis of survey data | Not explicitly stated | Burnout | n = 603 | Adverse events have negative consequences affecting nurse burnout, especially when the nurse identifies with their workgroup and has a strong safety climate mitigated by the leaders within their unit. |
| Kim et al. (2021) | Online cross-sectional study | 2020 | Mental health | n = 320 | Higher levels of stress and depression among nurses than was previously reported before COVID-19. |
Results
Description of Sample
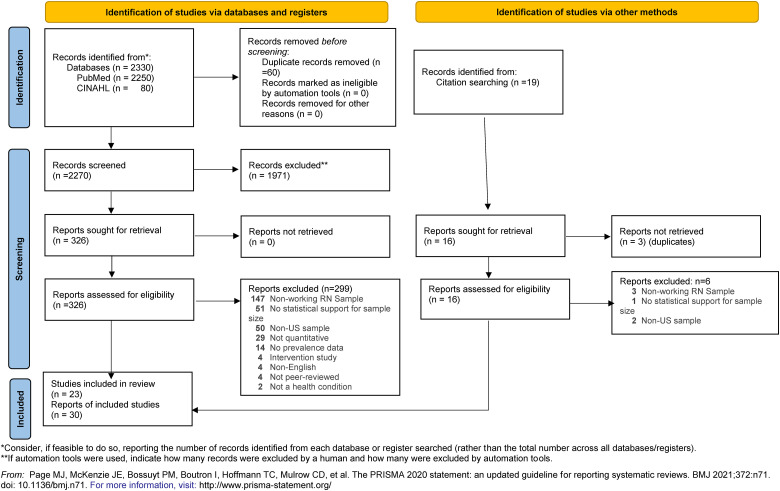
A total of 30 articles were determined to meet inclusion criteria and were included in this scoping review (see Figure 1 for PRISMA). The years of publication that met inclusion criteria ranged from 1992 to 2021. Correlative descriptive design was most often used (n = 26). Sample sizes varied between 190 and 68,488 participants. Additionally, studies that included healthcare providers beyond nurses (e.g., nursing assistants) where nurses were described separately in the analysis also met inclusion criteria.
Figure 1:
PRISMA 2020 flow diagram.
Risk of Bias
The risk of bias assessment highlighted the strengths and limitations of each study (see Table 2). High-risk bias was typically found in the methods section by inadequately describing participants and addressing potential sources of bias, the discussion section addressing limitations and generalizability, and funding sources for studies. Several studies also needed to be clarified in the method section addressing potential bias, the discussion section with generalizability, and funding sources. Despite the limitations, seven of the 30 studies had a low risk of bias overall.
Synthesis of Health Conditions Studied
The health conditions studied broke down into six thematic categories (listed in order by the number of articles in each category): (a) work-related injuries and hazards (eight articles); (b) unhealthy lifestyles (five articles); (c) mental health conditions (five articles); (d) burnout (five articles); (e) fatigue, sleep, and migraines (five articles); and (f) reproductive health (two articles). Durham et al. (1998) collected and reported comorbidity data on nurses in their sample. In their sample of 2,926 RNs from North Carolina, 25.39% reported allergies, 25% reported headaches, 18% reported migraines, 16.85% reported anemia, 12.17% reported arthritis, and 11.83% reported high blood pressure. This was the only article that included this type of data.
The workplace injuries and hazards category included articles on work-related violence; needlesticks; musculoskeletal injuries and pain; occupational injuries and illnesses broadly; and latex allergies. What differentiated these conditions from others in this review is the focus on acute injury or conditions that occurred at work compared to some of the other health conditions studied due to cumulative exposure. In a sample of over 11,500 nurses from Pennsylvania studied by Clarke (2007) and Olds and Clarke (2010), 9.6% reported a sharps injury in the prior year. Clarke (2007) found that that number was lower for nurses working in hospitals with favorable work environments (7.2%) and higher for nurses who had performed venipuncture during the last shift (with a 42% increase in risk). Rodriguez-Acosta et al. (2009) studied rates of injuries resulting in both no-lost work time and work time lost among nurses and aides. Among nurses, the work unit was the most significantly associated work-related factor in injury. Those working in critical care and psychiatric units had the highest risk for no-lost time injuries and those in orthopedic and rehabilitation units had a higher risk of lost work time injuries. Perhats et al. (2012) explored nonviolence-related work injuries among emergency room nurses (n = 2,294). Nineteen percent of respondents reported experiencing an injury in the last year with the majority (72%) being related to patient handling. In comparison, Lee et al. (2015) found an incidence of work-related musculoskeletal injuries among RNs in California (n = 220) to be 69% with symptom areas being lower back 54%, neck 41%, shoulders 34%, and hands/wrists 26%. Trinkoff et al. (2002) found similar rates of back (47%), neck (46%), and shoulder (35%) musculoskeletal problems in their sample of 1,163 nurses. Unruh and Asi (2018) studied work injuries among new graduate nurses in Florida (n = 414). Respondents reported that the most frequent injuries were verbal violence (70%), bruises and contusions (49%) followed by physical violence (25%). Gerberich et al. (2004) used the Minnesota Nurses’ Study survey and found a total of 352 out of 2975 (adjusted rate of 12.0 per 100 persons) of nurses reported work-related violence with 1,134 out of 2,975 nurse respondents (adjusted rate of 38.5 per 100 persons) reporting nonphysical violence in the past year. Overall, nursing work demands were associated with a higher risk of needlestick; and verbal and physical violence at work was the most frequent workplace injury type.
Unhealthy lifestyles among nurses included articles on the prevalence of smoking, obesity, unhealthy lifestyles and type 2 diabetes among nurses. Trinkoff and Storr (1998) explored nurse substance use rates and found the prevalence of past-year substance use for all substances combined was 32% in a sample of 4,438, with nurses in oncology reporting the highest prevalence of use, and binge drinking (16%) being the most commonly reported substance. Trinkoff et al. (1999) found that perceived availability, frequency of administration, and degree of workplace control over storage and dispensing of substances were associated with increased use. Monroe et al. (2013) study found rates of nurses enrolled in substance abuse monitoring programs and getting treatment were lower than the general population (0.51% vs. 1.0%). Similarly, Han, Trinkoff, Storr, Geiger-Brown, Johnson, and Park's studies (Han et al., 2011, 2012) explored nurse obesity in the Nurses’ Worklife and Health Study dataset (n = 2,624 total in dataset) 55% of nurses were overweight or obese, and obesity was significantly related to work stress, unfavorable work schedules, and work demands. Overall, studies in this category found that over 50% of nurses were overweight or obese and that work schedule, stress and/or demands were associated factors for overweight/obesity and some nurses used substances.
Mental health conditions included articles related to suicide, mental health overall, depression and self-harm. Nurse suicide was the focus of three articles which were all published between 2019 and 2020, possibly signifying a new focus in research on nurse health. Suicide rates among RNs varied from 13 per 100,000 (Patrician, 2020) to 13.9 per 100,000 (Davidson, 2019), and in a longitudinal analysis, Davidson (2020) found a greater risk of suicide among nurses than the general population (female IRR 1.395, 95% confidence interval [CI] 1.323, 1.470, p < .001; male IRR 1.205, 95% CI 1.083, 1.338, p < .001). However, in a study comparing suicide rates and methods between the nursing population and the general population using the 2014 National Violent Death Reporting System Dataset, Davidson (2019) found both male and female nurses had higher rates than their same-gendered general population counterparts (11.97/100,000 vs. 7.58/100,000 for females and 39.8/100,000 vs. 28.2/100,000 for males). Additionally, female nurses were more likely to use pharmacologic poisoning, specifically the use of opioids and benzodiazepines, than other methods than females in the general American population (Davidson, 2019, 2020). Davidson (2020) also found job problems, mental health history and leaving a suicide note were more common among nurse suicide deaths than other suicides. Kim (2021) and Melnyk et al. (2018) both explored rates of stress, anxiety and depression among nurses. Kim (2021) surveyed new nurses (n = 320) and found 43% had moderate to severe anxiety and 26% were depressed, while Melnyk et al. (2018) in a survey of 1,790 nurses identified some level of stress (38.7%), depression (32.8%), and anxiety (51.97%).
Burnout is defined by the World Health Organization (2019) as “a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed.” It is characterized by three dimensions: (a) feelings of energy depletion or exhaustion; (b) increased mental distance from one's job, or feelings of negativism or cynicism related to one's job; and (c) reduced professional efficacy.” The articles in this review used the Maslach Burnout Inventory (MBI) (Dyrbye, 2019; McHugh et al., 2011; Neff et al., 2011; Stimpfel et al., 2012; Vogus, 2020) to measure burnout. McHugh et al. (2011) in a survey (n = 68,724) found that there was a difference in the level of burnout based on work setting with 34% of nurses working in hospitals, 37% of nurses working in nursing homes, and 22% of nurses working in other settings reporting feeling burned out as determined by higher scores than average for healthcare workers on the emotional exhaustion subscale of the MBI. Using the same dataset, Stimpfel et al. (2012) explored the relationship between nurse burnout and shift length and found that nurses working longer shifts had higher burnout (56% reporting burnout of those worked >13 hr shifts in comparison to 20% of those working 8–9 hr shifts). Neff et al. (2011) also explored nurse burnout levels across work settings using the emotional exhaustion subscale of the MBI in a survey of nurses (n = 10,832), finding that 33.8% of nurses working in hospitals, 24.0% of those working in home health, 27.7% of those working in nursing homes and 20.8% of those in other settings were burned out. However, Dyrbye (2019) found that 38.4% of nurses (n = 7,077) in their sample had at least one symptom of burnout on the MBI and there were significant associations between increased age (for each year older, odds ratio [OR] 0.98, 95% CI [0.98–0.99), alongside professional factors like size of the hospital (referent: 100 beds or less; 101–250 beds, OR 1.22, 95% CI [0.94–1.59]; 251 beds or more, OR 1.63, 95% CI [1.23–2.15]; overall p-value = .001) and work hours (referent: 6 hr or less; 6–8 hr, OR 2.98, 95% CI [0.36–24.85]; 8–10 hr, OR 3.37, 95% CI [0.41–27.86]; more than 10 hr, OR 4.52, 95% CI [0.55–37.13]; overall p = .002). Interestingly, the studies related factors like staffing, benefits, practice environment, safety climate, and work-life integration to burnout. Articles in this category also often related burnout to nurse job satisfaction and intent to leave, patient satisfaction and quality of care, adverse events, and workability. Overall, most studies found about a third of respondents were burned out and that nurses who work in hospital and nursing home settings and worked longer shifts were more burned out.
Fatigue, sleep, and migraines included articles that covered chronic fatigue syndrome, inadequate sleep, and sleep quality, the relationship between fatigue, shift length and timing, mood, and osteoporosis, and migraines. Jason et al. (1998) estimated the prevalence of chronic fatigue syndrome among nurses to be 1,088 per 100,000 based on the findings of their two-phase study. In Trinkoff et al. (2001)'s longitudinal survey study of RNs (n = 3,727), 7% of nurses reported that they “daily or always got less sleep than they thought they should” and that there was a dose–response relationship wherein nurses reported higher physical demands of work the likelihood of inadequate sleep increased (OR, 1.96; 95% CI [1.41–2.72]). This relationship was unexplained by lifestyle factors, demographics, and work-schedule characteristics. Kunert et al. (2007) examined differences in fatigue levels and sleep quality among day and night shift nurses and found that night shift nurses reported higher daily fatigue and poorer sleep quality. Migraines were studied by Durham et al. (1998) and were reported by 18% of the sample (n = 2926) while 25% reported headaches. Feskanich et al. (2009) used the NHS to explore the role of working over 20 years of nightshift on bone fracture risk and found there was a significantly increased risk of wrist and hip fractures (RR = 1.37, 95% CI [1.04–1.80]).
Studies describing reproductive health conditions explored the relationships between nurses who administered antineoplastic medications and miscarriages, menstrual cycles, the prevalence of fecundity, and adverse reproductive outcomes. McAbee et al. (1993) compared adverse reproductive outcomes and occupational exposures between nonnurses, oncology nurses, and non-oncology nurses and found an association between administration of radiation and chemotherapeutic agents with stillbirths and miscarriages (OR = 3.78, 95% CI [1.12–12.78], p = .03). Shortridge et al. (1995) in a survey of oncology and non-oncology nurses (n = 1,458 total) found that nurses who reported handling antineoplastic medications had higher odds of menstrual dysfunction among nurses between 30 and 45. Studies found a reproductive health impact of administering antineoplastic medications and radiation on pregnancy outcomes and menstrual dysfunction. These studies both focused on reproductive health consequences for nurses due to antineoplastic medication administration.
Discussion
This review aimed to identify any health conditions that were more prevalent among nurses that may be related to work factors that should be the target of work interventions and work system changes. Studies looked at incidents at work that had an immediate impact on health (e.g., a needlestick or injury), others looked at cumulative impact (e.g., scheduling or demands), and some have an unclear antecedent or an antecedent that could come from personal and work factors (e.g., the incidence of suicide or substance use). Within the work environment, physical, emotional, and cognitive demands of work, including shiftwork, were all frequently identified as antecedents that could be further explored and addressed to improve nurse health.
The physical demands of nursing work and the work environment precede many workplace injuries and conditions common among nurses during and after cumulative shift impact. In the United States, nurses often work 12-hr shifts or more, often cluster shifts 3 days in a row (Stimpfel et al., 2012). Articles in this review linked the physical demands, including shiftwork, and work environment of nursing work to inadequate sleep, violence, sharps injuries, burnout, risk of developing hip and wrist fractures, reproductive health challenges, obesity, and diabetes (Feskanich et al., 2009; Han et al., 2012; McAbee et al., 1993; Shan et al., 2018; Shortridge et al., 1995; Stimpfel et al., 2012; Trinkoff et al., 2001; Unruh & Asi, 2018). These findings are supported by other reviews of studies that have linked the demands of nursing and the work environment to consequences for nurses in addition to consequences for patient care and organizations (Dall'Ora et al., 2016; Lake et al., 2019). The National Academy of Medicine (2020) recommends addressing the work system issues linked to decreased clinician well-being and burnout. There are also recommendations to address scheduling shiftwork to maximize time for recovery and these include decreasing rotating schedules and shift length (American Nurses Association, 2014). Organizations can use these recommendations to begin to address some of the occupational factors related to nurse health conditions.
Nurses care for patients and their family members at some of the most difficult times in their lives and often in work environments that are toxic. While nurses are incredibly resilient, they also report negative coping strategies, including some of the unhealthy lifestyle choices studied above (Jordan et al., 2016). This review found that some nurses do struggle with mental health conditions, including higher rates of suicide (Davidson et al., 2019, 2020; Dyrbye, 2019; Kim, 2021; Mazurek Melnyk et al., 2018; McHugh et al., 2011; Patrician et al., 2020). The COVID-19 Pandemic is an additional strain on healthcare providers in the United States and around the globe and rates of mental health conditions have increased (Vizheh et al., 2020). However, there continues to be a stigma among healthcare professionals seeking mental health services, and in the United States, some healthcare professional licensing bodies maintain that reporting a mental health illness is grounds for not being licensed or being monitored (Bernstein & Gold, 2020). Changing the culture around seeking help and these licensing rules are important steps before the mental health of providers can be addressed.
Implications for Practice
As Drennan and Ross (2019) state improving retention is an important lever in expanding the nursing pipeline that organizations can address. A survey of critical care nurses by the American Association of Critical-Care Nurses (2021; n = 6,000) found that two-third of critical care nurses considered leaving due to the pandemic, and a study of frontline nurses in Alabama found that turnover intention is correlated with COVID-19 occupational-related factors, for example, personal health risk as a factor, patient assignment acuity, and their personal protective equipment (Cole et al., 2021). Globally, studies of turnover intention due to COVID-19 in other countries have found there has been an impact of COVID-19 on nurse turnover intention (Labrague & de Los Santos, 2021). Turnover impacts staffing which has negative consequences for nurse and patient outcomes (Aiken et al., 2018; Shin et al., 2018). Subsequently, when patient and nurse outcomes suffer, organizations can incur significant financial impacts in terms of reimbursement for patient care. Therefore, organizational leaders should prioritize improving the work environment and addressing issues related to care demands and lack of resources. This may be done through policy advocacy. The policy implications of work-related health conditions among American nurses encompass key areas such as enforcing workplace safety regulations, addressing staffing levels and workload, prioritizing mental health support, enhancing training and education, establishing robust reporting and surveillance systems, ensuring fair compensation and benefits, promoting nurses’ advocacy and representation, allocating research funding for workplace health, and considering telehealth and flexible work arrangements (NASEM, 2020). Through the greater advocacy of these policies, the aim is to create a supportive and safe environment for nurses, ultimately improving the quality of patient care and the overall healthcare system through collaboration across stakeholders and organizations.
Strengths and Limitations
Some limitations need to be considered; specifically, criteria and search strategy, and the limitations of the designs of studies included in this review's ability to address prevalence. The search strategy is limited to English and this review's focus is on the United States. More to be learned from work in other countries. The decision to focus solely on the United States was made because of the unique healthcare system aspects and culture. It is possible that exploring this literature with a more global perspective would yield different results on the prevalence of health conditions among nurses that may be linked to work conditions. However, those findings would need to be reviewed for country-specific context as nursing varies greatly around the globe. Only the two most common databases (CINAHL and PubMed) were used in the search. Additional databases may have produced more literature; however, these databases are the most used in nursing and allied health research. Another limitation is that a scoping review was performed rather than a meta-analysis or systematic review due to the exploratory nature of this review's research question. Given the wide breadth of conditions and designs used, these kinds of reviews would not be feasible. The aim of this scoping review was to identify articles with a focus on the prevalence of health conditions among registered nurses. However, many studies were excluded because they included additional data for participants such as healthcare providers, advanced practice registered nurses, unlicensed health aids or lack of data on whether those in the sample were working as nurses (e.g., Nurses’ Health Study). Studies that did include a working registered nurse sample that could not be extracted independently were excluded. The sampling strategies of many of the studies meant that the prevalence of the health conditions studied could not be extracted. The strengths of this review are the systematic search and screening strategy.
Conclusions
This review sought to explore the prevalence of health conditions among U.S. working nurses and to determine whether these are due to work conditions that could be targeted by interventions to the work environment. We found that there are not many studies that explore the prevalence of health conditions among nurses and the potential role of their work in the development of those conditions. This is a gap in the existing literature that should be filled by future systematic population studies. Other countries that have cohort studies of nurses, like the Korean NHS, include occupational factors in their regular surveys, so they can explore the impact of work as a nurse on health conditions (Kim et al., 2017). This is something that can be addressed in future NHS survey time points. In the wake of the COVID-19 pandemic, the ramifications of the pandemic on nurse health are still only starting to be realized. The pandemic put additional strain on the already strained healthcare system and nursing workforce, yet little has been done to address it. Policy work should focus on minimizing job demands that contribute to poor nurse health and well-being (e.g., burnout, staffing shortages, and work demands) while increasing job resources (e.g., mental health services and individual-level stress reduction interventions). Understanding and mitigating the impact of the pandemic and nursing work overall on the health of the nursing workforce is crucial to the solvency of the workforce and nurses’ health.
Acknowledgments
We would like to acknowledge Mary Anne Vandegrift for her assistance with some abstract screening. A poster presentation on this scoping review was presented at the 55th Annual Communicating Nursing Research Conference, “Justice, Equity, Diversity, and Inclusion (JEDI): Creating a Nursing Force for Change,” held in Portland, Oregon from April 6–9 2022. An abstract was published in Communicating Nursing Research Volume 22, Western Institute of Nursing (2022).
Footnotes
Author Contributions: JGR conceived of the idea for the review; JGR brought the team together to do the review; JGR, KMD, CB, and MS created a plan for the article search collection, analysis, and writing; MS ran the search; JGR, KMD, CB, AN, CP, and PKV completed title, abstract, full-text review, data extraction, and assessed rigor of included articles; JGR, KMD, CB, AN, CP, PKV, and MS each drafted sections of the manuscript and tables and edited the manuscript.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Jessica G. Rainbow https://orcid.org/0000-0002-5415-6049
Christine Platt https://orcid.org/0000-0002-9122-942X
References
- Admi H., Tzischinsky O., Epstein R., Herer P., Lavie P. (2008). Shift work in nursing: Is it really a risk factor for nurses’ health and patients’ safety? Nursing Economics, 26(4), 250. [PubMed] [Google Scholar]
- Aiken L. H., Cerón C., Simonetti M., Lake E. T., Galiano A., Garbarini A., Soto P., Bravo D., Smith H. L. (2018). Hospital nurse staffing and patient outcomes. Revista Médica Clínica Las Condes, 29(3), 322–327. 10.1016/j.rmclc.2018.04.011 [DOI] [Google Scholar]
- American Nurses Association. (2014). Addressing nurse fatigue to promote patient safety and health: Joint responsibilities of registered nurses and employers to reduce risks ANA position statement .
- American Nurses Association. (n.d.). What is nursing? https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/ .
- Bernstein S. A., Gold J. A. (2020). Mental health on the frontlines: Before, during, and after COVID-19. Missouri Medicine, 117(5), 421–425. [PMC free article] [PubMed] [Google Scholar]
- Bureau of Labor Statistics U.S. Department of Labor. Occupational Outlook Handbook, Registered Nurses. Retrieved April 19 2022 from https://www.bls.gov/ooh/healthcare/registered-nurses.htm.
- Clarke S. P. (2007). Hospital work environments, nurse characteristics, and sharps injuries. American Journal of Infection Control, 35(5), 302–309. 10.1016/j.ajic.2006.07.014 [DOI] [PubMed] [Google Scholar]
- Cole A., Ali H., Ahmed A., Hamasha M., Jordan S. (2021). Identifying patterns of turnover intention among Alabama frontline nurses in hospital settings during the COVID-19 pandemic. Journal of Multidisciplinary Healthcare, 14, 1783–1794. 10.2147/JMDH.S308397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covidence systematic review software. In. Veritas Health Innovation. www.covidence.org.
- Cox T., Griffiths A., Cox S. (1996). Work-related stress in nursing: Controlling the risk to health. International Labour Office Geneva. [Google Scholar]
- Cuschieri S. (2019). The STROBE guidelines. Saudi Journal of Anaesthesia, 13(Suppl 1), S31–S34. 10.4103/sja.SJA_543_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dall'Ora C., Ball J., Recio-Saucedo A., Griffiths P. (2016). Characteristics of shift work and their impact on employee performance and wellbeing: A literature review. International Journal of Nursing Studies, 57, 12–27. 10.1016/j.ijnurstu.2016.01.007 [DOI] [PubMed] [Google Scholar]
- Davidson J. E., Proudfoot J., Lee K., Terterian G., Zisook S. (2020). A longitudinal analysis of nurse suicide in the United States (2005-2016) with recommendations for action. Worldviews on Evidence-Based Nursing, 17(1), 6–15. 10.1111/wvn.12419 [DOI] [PubMed] [Google Scholar]
- Davidson J. E., Proudfoot J., Lee K., Zisook S. (2019). Nurse suicide in the United States: Analysis of the center for disease control 2014 national violent death reporting system dataset. Archives of Psychiatric Nursing, 33(5), 16–21. 10.1016/j.apnu.2019.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drennan V. M., Ross F. (2019). Global nurse shortages—the facts, the impact and action for change. British Medical Bulletin, 130(1), 25–37. 10.1093/bmb/ldz014 [DOI] [PubMed] [Google Scholar]
- Durham C. F., Alden K. R., Dalton J. A., Carlson J., Miller D. W., Englebardt S. P., Neelon V. J. (1998). Quality of life and productivity in nurses reporting migraine. Headache: The Journal of Head and Face Pain, 38(6), 427–435. https://headachejournal.onlinelibrary.wiley.com/doi/abs/10.1046/j.1526-4610.1998.3806427.x?sid=nlm%3Apubmed https://doi.org/10.1046/j.1526-4610.1998.3806427.x [DOI] [PubMed] [Google Scholar]
- Dyrbye L. N., West C. P., Johnson P. O., Cipriano P. F., Beatty D. E., Peterson C., Shanafelt T. (2019). Burnout and satisfaction with work-life integration among nurses. Journal of Occupational and Environmental Medicine, 61(8), 689–698. 10.1097/jom.0000000000001637 [DOI] [PubMed] [Google Scholar]
- Efendi F., Kurniati A., Bushy A., Gunawan J. (2019). Concept analysis of nurse retention. Nursing & Health Sciences, 21(4), 422–427. 10.1111/nhs.12629 [DOI] [PubMed] [Google Scholar]
- Feskanich D., Hankinson S. E., Schernhammer E. S. (2009). Nightshift work and fracture risk: The nurses’ health study. Osteoporosis International, 20(4), 537–542. 10.1007/s00198-008-0729-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerberich S. G., Church T. R., McGovern P. M., Hansen H. E., Nachreiner N. M., Geisser M. S., Ryan A. D., Mongin S. J., Watt G. D. (2004). An epidemiological study of the magnitude and consequences of work related violence: The Minnesota Nurses’ study. Occupational and Environmental Medicine, 61(6), 495–503. 10.1136/oem.2003.007294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant M. J., Booth A. (2009). A typology of reviews: An analysis of 14 review types and associated methodologies. Health Information & Libraries Journal, 26, 91–108. 10.1111/j.1471-1842.2009.00848.x [DOI] [PubMed] [Google Scholar]
- Han K., Trinkoff A. M., Storr C. L., Geiger-Brown J. (2011). Job stress and work schedules in relation to nurse obesity. JONA: The Journal of Nursing Administration, 41(11), 488–495. 10.1097/NNA.0b013e3182346fff [DOI] [PubMed] [Google Scholar]
- Han K., Trinkoff A. M., Storr C. L., Geiger-Brown J., Johnson K. L., Park S. (2012). Comparison of job stress and obesity in nurses with favorable and unfavorable work schedules. Journal of Occupational & Environmental Medicine, 54(8), 928–932. 10.1097/JOM.0b013e31825b1bfc [DOI] [PubMed] [Google Scholar]
- Jason L. A., Wagner L., Rosenthal S., Goodlatte J., Lipkin D., Papernik M., Plioplys S., Plioplys A. V. (1998). Estimating the prevalence of chronic fatigue syndrome among nurses. The American Journal of Medicine, 105(3a), 91s–93s. 10.1016/s0002-9343(98)00159-4 [DOI] [PubMed] [Google Scholar]
- Jordan T. R., Khubchandani J., Wiblishauser M. (2016). The impact of perceived stress and coping adequacy on the health of nurses: A pilot investigation. Nursing Research and Practice, 2016, 1–11. https://doi.org/10.1155/2016/5843256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim O., Ahn Y., Lee H. Y., Jang H. J., Kim S., Lee J. E., Jung H., Cho E., Lim J. Y., Kim M. J., Willett W. C., Chavarro J. E., Park H. Y. (2017). The Korea nurses’ health study: A prospective cohort study. Journal of Women's Health, 26(8), 892–899. 10.1089/jwh.2016.6048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. C., Quiban C., Sloan C., Montejano A. (2021). Predictors of poor mental health among nurses during COVID-19 pandemic. Nursing Open, 8(2), 900–907. 10.1002/nop2.697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunert K., King M. L., Kolkhorst F. W. (2007). Fatigue and sleep quality in nurses. Journal of Psychosocial Nursing and Mental Health Services, 45(8), 30–37. 10.3928/02793695-20070801-07 [DOI] [PubMed] [Google Scholar]
- Labrague L. J., de Los Santos J. A. A. (2021). Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. Journal of Nursing Management, 29(3), 395–403. 10.1111/jonm.13168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake E. T., Sanders J., Duan R., Riman K. A., Schoenauer K. M., Chen Y. (2019). A meta-analysis of the associations between the nurse work environment in hospitals and 4 sets of outcomes. Medical Care, 57(5), 353. 10.1097/MLR.0000000000001109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S. J., Lee J. H., Gershon R. R. (2015). Musculoskeletal symptoms in nurses in the early implementation phase of California's safe patient handling legislation. Research in Nursing & Health, 38(3), 183–193. 10.1002/nur.21657 [DOI] [PubMed] [Google Scholar]
- Mazurek Melnyk B., Orsolini L., Tan A., Arslanian-Engoren C., D'Eramo Melkus G., Dunbar-Jacob J., Hill Rice V., Millan A., Dunbar S. B., Braun L. T., Wilbur J., Chyun D. A., Gawlik K., Lewis L. M. (2018). A national study links nurses’ physical and mental health to medical errors and perceived worksite wellness. Journal of Occupational & Environmental Medicine, 60, 126–131. 10.1097/JOM.0000000000001198 [DOI] [PubMed] [Google Scholar]
- Mazurenko O., Gupte G., Shan G. (2015). Analyzing U.S. nurse turnover: Are nurses leaving their jobs or the profession itself? Journal of Hospital Administration, 4(4), 48–56. 10.5430/jha.v4n4p48 [DOI] [Google Scholar]
- McAbee R. R., Gallucci B. J., Checkoway H. (1993). Adverse reproductive outcomes and occupational exposures among nurses: An investigation of multiple hazardous exposures. AAOHN Journal, 41(3), 110–119. 10.1177/216507999304100301 [DOI] [PubMed] [Google Scholar]
- McHugh M. D., Kutney-Lee A., Cimiotti J. P., Sloane D. M., Aiken L. H. (2011). Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Affairs, 30(2), 202–210. 10.1377/hlthaff.2010.0100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melnyk B. M., Orsolini L., Tan A., Arslanian-Engoren C., Melkus G. D., Dunbar-Jacob J., Rice V. H., Millan A., Dunbar S. B., Braun L. T., Wilbur J., Chyun D. A., Gawlik K., Lewis L. M. (2018). A national study links nurses’ physical and mental health to medical errors and perceived worksite wellness. Journal of Occupational & Environmental Medicine, 60(2), 126–131. 10.1097/jom.0000000000001198 [DOI] [PubMed] [Google Scholar]
- Mitchell A. H. (2020). Preventing occupational exposures to infectious disease in health care: A practical guide (1st 2020. ed.). Springer. [Google Scholar]
- Monroe T. B., Kenaga H., Dietrich M. S., Carter M. A., Cowan R. L. (2013). The prevalence of employed nurses identified or enrolled in substance use monitoring programs. Nursing Research, 62(1), 10–15. 10.1097/NNR.0b013e31826ba3ca [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, E., and Medicine. (2020). Strategies to support the health and well-being of clinicians during the COVID-19 outbreak. https://nam.edu/initiatives/clinician-resilience-and-well-being/clinician-well-being-strategies-during-covid-19/.
- Neff D. F., Cimiotti J. P., Heusinger A. S., Aiken L. H. (2011). Nurse reports from the frontlines: Analysis of a statewide nurse survey. Nursing Forum, 46(1), 4–10. 10.1111/j.1744-6198.2010.00201.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurses A. A. o. C.-C. (2021). Hear us out campaign reports nurses’ COVID-19 reality. https://www.aacn.org/newsroom/hear-us-out-campaign-reports-nurses-covid-19-reality.
- Olds D. M., Clarke S. P. (2010). The effect of work hours on adverse events and errors in health care. Journal of Safety Research, 41(2), 153–162. 10.1016/j.jsr.2010.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- OSHA. (2013). Worker Safety in Your Hospital .
- Patrician P. A., Peterson C., McGuinness T. M. (2020). Original research: Suicide among RNs: An analysis of 2015 data from the national violent death reporting system. AJN, American Journal of Nursing, 120(10), 24–28. 10.1097/01.NAJ.0000718624.25806.3f [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrician P. A., Peterson C., McGuinness T. M. (2020). Suicide among RNs: An analysis of 2015 data from the national violent death reporting system. AJN, American Journal of Nursing, 120(10), 24–28. 10.1097/01.NAJ.0000718624.25806.3f [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perhats C., Keough V., Fogarty J., Hughes N. L., Kappelman C. J., Scott M., Moretz J. (2012). Non-violence-related workplace injuries among emergency nurses in the United States: Implications for improving safe practice, safe care. Journal of Emergency Nursing, 38(6), 541–548. 10.1016/j.jen.2011.06.005 [DOI] [PubMed] [Google Scholar]
- Peters M. D. J., Marnie C., Tricco A. C., Pollock D., Munn Z., Alexander L., McInerney P., Godfrey C. M., Khalil H. (2021). Updated methodological guidance for the conduct of scoping reviews. JBI Evidence Implementation, 19(1), 3–10. 10.1097/XEB.0000000000000277 [DOI] [PubMed] [Google Scholar]
- Rodriguez-Acosta R. L., Richardson D. B., Lipscomb H. J., Chen J. C., Dement J. M., Myers D. J., Loomis D. P. (2009). Occupational injuries among aides and nurses in acute care. American Journal of Industrial Medicine, 52(12), 953–964. 10.1002/ajim.20762 [DOI] [PubMed] [Google Scholar]
- Shan Z., Li Y., Zong G., Guo Y., Li J., Manson J. E., Hu F. B., Willett W. C., Schernhammer E. S., Bhupathiraju S. N. (2018). Rotating night shift work and adherence to unhealthy lifestyle in predicting risk of type 2 diabetes: Results from two large US cohorts of female nurses. BMJ, 363, k4641. 10.1136/bmj.k4641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin S., Park J. H., Bae S. H. (2018). Nurse staffing and nurse outcomes: A systematic review and meta-analysis. Nursing Outlook, 66(3), 273–282. 10.1016/j.outlook.2017.12.002 [DOI] [PubMed] [Google Scholar]
- Shortridge L. A., Lemasters G. K., Valanis B., Hertzberg V. (1995). Menstrual cycles in nurses handling antineoplastic drugs. Cancer Nursing, 18(6), 439–444. 10.1097/00002820-199512000-00003 [DOI] [PubMed] [Google Scholar]
- Stimpfel A. W., Sloane D. M., Aiken L. H. (2012). The longer the shifts for hospital nurses, the higher the levels of burnout and patient dissatisfaction. Health Aff (Millwood), 31(11), 2501–2509. 10.1377/hlthaff.2011.1377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Study N. H. (2016). Nurses’ health study. https://nurseshealthstudy.org.
- Tricco A. C., Lillie E., Zarin W., O'Brien K. K., Colquhoun H., Levac D., Moher D., Peters M. D. J., Horsley T., Weeks L., Hempel S., Akl E. A., Chang C., McGowan J., Stewart L., Hartling L., Aldcroft A., Wilson M. G., Garritty C., Straus S. E. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- Trinkoff A. M., Lipscomb J. A., Geiger-Brown J., Brady B. (2002). Musculoskeletal problems of the neck, shoulder, and back and functional consequences in nurses. American Journal of Industrial Medicine, 41(3), 170–178. 10.1002/ajim.10048 [DOI] [PubMed] [Google Scholar]
- Trinkoff A. M., Storr C. L. (1998). Substance use among nurses: Differences between specialties. American Journal of Public Health, 88(4), 581–585. 10.2105/ajph.88.4.581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinkoff A. M., Storr C. L., Lipscomb J. A. (2001). Physically demanding work and inadequate sleep, pain medication use, and absenteeism in registered nurses. Journal of Occupational and Environmental Medicine, 43(4), 355–363. 10.1097/00043764-200104000-00012 [DOI] [PubMed] [Google Scholar]
- Trinkoff A. M., Storr C. L., Wall M. P. (1999). Prescription-type drug misuse and workplace access among nurses. Journal of Addictive Diseases, 18(1), 9–17. https://doi.org/10.1300/J069v18n01_02 [DOI] [PubMed] [Google Scholar]
- United States Bureau of Labor Statistics. (2018). Occupational injuries and illnesses among registered nurses. https://www.bls.gov/opub/mlr/2018/article/occupational-injuries-and-illnesses-among-registered-nurses.htm.
- Unruh L., Asi Y. (2018). Determinants of workplace injuries and violence among newly licensed RNs. Workplace Health & Safety, 66(10), 482–492. 10.1177/2165079918756909 [DOI] [PubMed] [Google Scholar]
- Vizheh M., Qorbani M., Arzaghi S. M., Muhidin S., Javanmard Z., Esmaeili M. (2020). The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. Journal of Diabetes & Metabolic Disorders, 19, 1967–1978. 10.1007/s40200-020-00643-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogus T. J., Ramanujam R., Novikov Z., Venkataramani V., Tangirala S. (2020). Adverse events and burnout: The moderating effects of workgroup identification and safety climate. Medical Care, 58(7), 594–600. 10.1097/mlr.0000000000001341 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2019). QD85 burnout. In 11th Revision of the International Classification of Diseases. http://id.who.int/icd/entity/129180281.