Abstract
Endocannabinoids (eCBs), among which N-arachidonoylethanolamine (AEA) and 2-arachidonoylglycerol (2-AG) are the most biologically active members, are polyunsaturated lipids able to bind cannabinoid, vanilloid and peroxisome proliferator-activated receptors. Depending on the target engaged, these bioactive mediators can regulate different signalling pathways, at both central and peripheral levels. The biological action of eCBs is tightly controlled by a plethora of metabolic enzymes which, together with the molecular targets of these substances, form the so-called “endocannabinoid system”. The ability of eCBs to control manifold peripheral functions has received a great deal of attention, especially in the light of their widespread distribution in the body. In particular, eCBs are important regulators in blood, where they modulate haematopoiesis, platelet aggregation and apoptosis, as well as chemokine release and migration of immunocompetent cells. Here, we shall review the current knowledge on the pathophysiological roles of eCBs in blood. We shall also discuss the involvement of eCBs in those disorders affecting the haematological system, including cancer and inflammation. Knowledge gained to date underlines a fundamental role of the eCB system in blood, thus suggesting that it may represent a therapeutic promise for a broad range of diseases involving impaired hematopoietic cell functions.
Keywords: Bioactive lipids, Haematopoiesis, Leukocytes, Platelets, Cancer, Blood diseases
The endocannabinoid (eCB) system
The endocannabinoid (eCB) system includes: (1) a group of bioactive lipids released from membrane phospholipid precursors, named eCBs, (2) their metabolic enzymes, and (3) their target receptors [1, 2]. Briefly, these components, depicted in Table 1, will be described later.
Table 1.
The main elements of the eCB system
| Member | Description | Function | References |
|---|---|---|---|
| Bioactive lipids | |||
| AEA | Derivatives of ω6 PUFA | They bind CB receptors, and act in the central nervous system and in the periphery | [1, 2] |
| 2-AG | |||
| 2-AGE | |||
| Virodhamine | |||
| NADA | |||
| EPEA | Derivatives of ω3 PUFA | ||
| DHEA | |||
| PEA | eCB-like compounds | They do not bind CB receptors, but potentiate eCB function | [3] |
| OEA | |||
| Metabolic proteins | |||
| EMT | Trans-membrane transporter | Responsible for AEA (and possibly for the other eCBs) transport | [9] |
| NAPE-PLD | Biosynthetic enzymes | Responsible for AEA synthesis | [4, 5] |
| ABHD4 | |||
| PLC | |||
| DAGL | Responsible for 2-AG synthesis | ||
| FAAH-1 | Hydrolytic enzymes | Responsible for AEA hydrolysis | [4, 10] |
| FAAH-2 | |||
| NAAA | |||
| MAGL | Responsible for 2-AG hydrolysis | ||
| ABHD6 | |||
| ABHD12 | |||
| Target receptors | |||
| CB1 | Cannabinoid receptors | Main targets of eCBs | [12–14, 16] |
| CB2 | |||
| GPR55 | Novel target of eCBs | ||
| TRPV1 | Vanilloid receptor | Target of AEA and congeners | [19, 20] |
| PPAR α and γ | Peroxisome proliferator-activated receptors | Targets of eCBs | [21] |
AEA arachidonoylethanolamine, 2-AG 2-arachidonoylglycerol, 2-AGE 2-arachidonoylglycerylether, NADA N-arachidonoyldopamine, EPEA N-eicosapentaenoylethanolamine, DHEA N-docosahexaenoylethanolamine, PEA N-palmitoylethanolamine, OEA N-oleoylethanolamine, EMT endocannabinoid membrane transporter, NAPE-PLD N-acyl-phosphatidylethanolamines-hydrolyzing phospholipase D, ABHD serine a/b-hydrolase, PLC phospholipase C, DAGL diacylglycerol lipase, FAAH fatty acid amide hydrolase, NAAA N-acylethanolamine-hydrolyzing acid amidase, MAGL monoacylglycerol lipase, CB cannabinoid, TRPV1 transient receptor potential vanilloid 1, PPAR peroxisome proliferator-activated receptor, PUFA polyunsaturated fatty acid
The eCB family includes amides, esters and ethers of long-chain polyunsaturated fatty acids (PUFAs), among which the best characterized members are N-arachidonoylethanolamine (anandamide, AEA) and 2-arachidonoylglycerol (2-AG), both derivatives of arachidonic acid [1]. Beside eCBs, our body synthesizes eCB-like compounds [including N-palmitoylethanolamine (PEA) and N-oleoylethanolamine (OEA)] that exert their effect without binding cannabinoid receptors, and potentiate eCB function by inhibiting their degradation [3].
Both AEA and 2-AG are produced “on demand” through multiple biosynthetic pathways, which reflect the variety of physiological stimuli (including neuronal activity, glucocorticoids, insulin and cytokines) able to mobilize these eCBs [4–8]. The in–out and out–in movement of eCBs across the plasma membrane is a not yet fully elucidated process and several hypotheses have been proposed: (1) passive diffusion, (2) facilitated transport via a specific carrier called eCB membrane transporter (EMT), and (3) caveolae-mediated endocytosis [9]. The biological activity of eCBs is ended by hydrolysis catalysed by multiple enzymes or isozymes; the main hydrolases responsible for AEA breakdown into arachidonic acid and ethanolamine are fatty acid amide hydrolase- (FAAH-) 1 and 2 and N-acylethanolamine-hydrolyzing acid amidase (NAAA), while 2-AG is converted to fatty acid and glycerol by monoacylglycerol lipase (MAGL), FAAH, a/b-hydrolases (ABHD) 6 and 12 [4, 10]. Finally, both AEA and 2-AG can originate oxidative derivatives, by the action of lipoxygenases, cyclooxygenase-2 and cytochrome P450 (Fig. 1) [11].
Fig. 1.
Oxidative metabolism of AEA (a) and 2-AG (b). 12-LOX 12-lipoxygenase, COX-2 cyclooxygenase-2, cytP 450 cytochrome P450, 12-HAEA 12-hydroxyeicosatetraenoylethanolamide, PGE 2 -EA prostaglandin E2-ethanolamide, 5,6-EET-EA 5,6-epoxyeicosatrienoic acid-ethanolamide, 12-HETE-G 12-hydroxyeicosatetraenoyl-glycerylester, PGE 2 -GE prostaglandin E2-glycerilester, 5,6-GEET 5,6-glycerated epoxyeicosatrienoic acid
The different signalling pathways activated by AEA and 2-AG strictly depend on the specific receptor engaged. To date, three G protein-coupled receptors (GPRs) have been shown to bind eCBs: (1) type-1 (CB1) cannabinoid receptor highly expressed in brain, but also in lung, liver and kidney, as well as in T lymphocytes and platelets [12–14], (2) type-2 (CB2) receptor, mainly present in the immune system and in haematopoietic cells [12, 15], and (3) GPR55, ubiquitously expressed and involved in modulation of processes related to cardiovascular system and inflammation [16–18]. AEA, but not 2-AG, is also an agonist of the transient receptor potential vanilloid 1 (TRPV1) channel, expressed in primary sensory neurons and peripheral cells; by activating TRPV1, AEA triggers pro-apoptotic signalling pathways, and exerts a physiological control of brain functions [19, 20]. Additional targets of eCBs are the peroxisome proliferator-activated receptors (PPARs) α and γ, through which eCBs regulate adipocyte differentiation, lipid and glucose metabolism, as well as inflammatory responses [21].
In the next sections, we will describe the knowledge gained so far on the role of eCB system in generation and function of haematological cells. Without seeking to be exhaustive, we will focus on few selected examples of blood physiology and pathology.
The eCB system and haematopoiesis
Haematopoiesis is a complex and highly ordered differentiation and self-renewal process, through which blood cells are produced from haematopoietic stem cells (HSCs), a population of multipotent cells residing in bone marrow of adult mammals [22]. HSC retention in bone marrow niches (homing) or mobilization is allowed by specific transcription factors, cytokines [including stromal-derived factor-1 (SDF-1)] and growth factors [including interleukin-3 (IL-3), granulocyte–macrophage colony-stimulating factor (GM-CSF), granulocyte colony-stimulating factor (G-CSF), erythropoietin, and macrophage colony-stimulating factor (M-CSF)] [23–25].
eCBs can be counted among factors governing hematopoietic stem cell biology. Stromal cells, in fact, release significant amounts of eCBs (whose levels also increase during inflammation), which exert distinct effects on HSC differentiation and migration, alone or in synergy with classical growth factors [26–28]; eCB effects on clonal cell expansion and mobilization are mainly achieved through activation of CB2 receptor, highly expressed in human and murine HSCs (Table 2) [26, 27, 29–32]. Not only eCBs (and especially 2-AG) control HSC self-renewal and proliferation, but they are also involved in lineage commitment and differentiation of distinct cell populations. Studies performed in our laboratories indicated that 2-AG was able to drive a bipotential cell line (expressing surface antigens of both erythroid and megakaryocytic phenotypes) towards megakaryocytic differentiation; the eCB, indeed, enhanced expression of megakaryocyte/platelet surface antigens (including β3 integrin subunit and glycoprotein VI), while it reduced the expression of erythroid markers, such as glycophorin A [33]. We recently found that 2-AG was also able to complete megakaryocytic differentiation, by stimulating platelet generation and release, thus potentially having clinical efficacy to counteract thrombocytopenia-associated diseases [34]. Noticeably, we observed that cells drop down the synthesis of this lipid mediator at the end of differentiation, thus indicating that they are able to self-regulate 2-AG levels, and thus pro-differentiating stimuli [33, 34].
Table 2.
Effects of CB2 agonists on haematopoiesis
| Compound | Clonal expansion | Migration | References |
|---|---|---|---|
| AEA | + | − | [27, 29] |
| 2-AG | + | + | [27, 30, 31] |
| PEA | − | + | [27] |
| AM1241 | = | + | [26] |
+, stimulation; −, inhibition; =, no effect
Although further work is needed, the finding that eCBs can be listed among key drivers of hematopoiesis might broaden the field of investigation; targeting the eCB actions should be helpful to manage bone marrow failure and blood cell loss occurring in several pathological conditions.
The eCB system and blood cells
Erythrocytes
To date, only a few data are available on erythrocytes. Using human red blood cell ghosts, Bojesen and Hansen [35] demonstrated that AEA quickly (within seconds) crosses erythrocyte membranes via a saturable mechanism that does not require ATP. At concentrations higher than those found in circulating plasma of healthy individuals, AEA is oxygenated by cyclooxygenase and generates PGE2, with profound effects on erythrocyte survival. Indeed, PGE2 activates Ca2+-permeable channels, thus triggering Ca2+-sensitive K+ channels, water loss and cell shrinkage, accompanied by phosphatidylserine exposure and engulfment of erythrocytes by macrophages [36]. Such an effect may have therapeutical implications, as suggested by Bobbala and colleagues [37]. Indeed, AEA enhances cell death and decreases in vitro parasitaemia of Plasmodium falciparum-infected human erythrocytes, while in vivo administration blunts parasitaemia and enhances survival of Plasmodium berghei-infected mice (Fig. 2). Overall, by exerting a direct toxic effect on the pathogen and by enhancing cell death and rapid clearance of infected erythrocytes, AEA counteracts the lethal course of the disease [37].
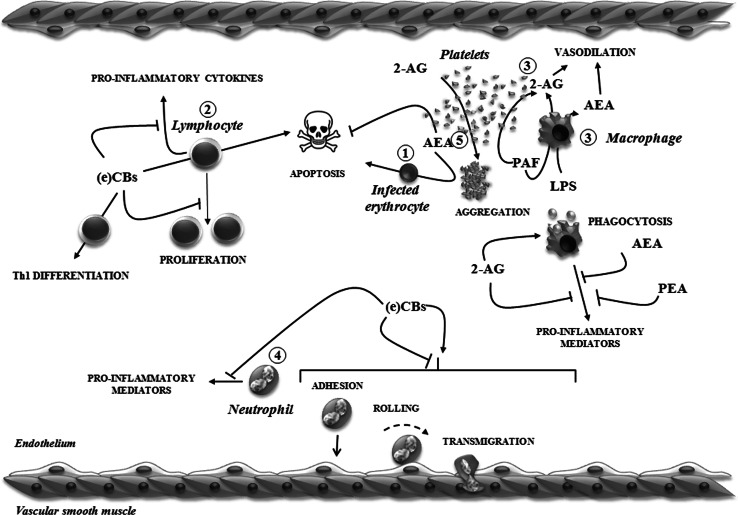
Fig. 2.
Schematic representation of different effects of (e)CBs on blood cells. 1 AEA enhances cell death of infected erythrocytes. 2 (e)CBs exert immunosuppressive effects by inhibiting lymphocyte proliferation and/or inducing apoptosis, as well as inhibiting pro-inflammatory cytokine release. They also control the balance among specific subsets of T cells. 3 Either 2-AG [released from platelet-activating factor (PAF)-stimulated macrophages and platelets] or AEA [produced from lipopolysaccharide (LPS)-stimulated macrophages] induces vasodilation during septic shock. 2-AG also stimulates macrophage phagocytic activity; some eCBs suppress release of pro-inflammatory mediators from activated macrophages. 4 (e)CBs inhibit neutrophil recruitment into inflamed tissues and secretion of pro-inflammatory mediators. Otherwise, they can promote the neutrophil adhesion cascade. 5 2-AG induces platelet aggregation, while AEA prolongs platelet life span. See text for further details
Leukocytes
eCB signalling through CB receptors has been proved to modulate homoeostatic immune balance, affecting the biological activity of all types of white blood cells. The ability of eCBs to influence both humoral and cellular immunity is an ever-increasing area of cannabinoid research; given the complexity of the relationship between eCBs and immune system, we refer to other articles providing a more comprehensive overview [38, 39], here highlighting only some aspects of this topic.
All subsets of lymphocytes express CB receptors, with the CB2 subtype being the most abundant, and expression levels are related to activation state [40]. In addition, message levels are highest in B cells, followed by NK, T8 and T4 cells [41]. B cell proliferation, migration and Ig production are modulated by eCBs, which preferentially act on naïve B cells, thus modulating B cell compartments in spleen and secondary lymphoid tissues [30, 41–44]. Concerning T lymphocytes, eCB generally mediates immunosuppression via at least four different pathways (Fig. 2): (1) inhibition of transcription factors and suppression of cytokine production [45–48], (2) inhibition of proliferation [48], (3) induction of apoptosis [49]; (4) induction of specific subsets of T cells (especially by modulating T helper (Th) 17/T regulatory and Th1/Th2 ratios) [48–51]. In this context, it should be noted that eCB tone is modulated by Th1/Th2 balance: lymphocyte treatment with the Th2 cytokines IL-4 or IL-10 stimulates FAAH expression and activity, whereas the Th1 cytokines IL-12 and interferon (IFN) γ inhibit it [52].
The presence of eCB elements has been documented in both immortalized and primary circulating macrophages, at transcriptional, translational and functional levels. These cells, indeed, possess all proteins to bind and to metabolize both AEA and 2-AG [53–55], although these proteins are differentially regulated upon stimulation. Indeed, RAW264.7 cells and mouse peritoneal macrophages treated with lipopolysaccharide (LPS) show increased AEA levels, due to activation of its biosynthetic enzyme, N-acylphosphatydiletanolamine phospholipase D (NAPE-PLD). Instead, 2-AG cellular levels are unaffected by LPS, although they are sensitive to treatment with platelet-activating factor [56]. These findings indicate that both AEA (produced by activated macrophages) and 2-AG (secreted from activated platelets and macrophages) may be paracrine mediators of endotoxin-induced hypotension [56, 57] (Fig. 2). Several reports documented inhibition of macrophage functions by eCBs. AEA has been proven to inhibit (1) macrophage-mediated killing of tumour necrosis factor α (TNFα)-sensitive murine fibroblasts [58], (2) NO production by LPS-activated mouse peritoneal macrophages [59] and (3) release of pro-inflammatory cytokines (TNFα, IL-4, -6, -8, IFNγ) by human monocytes [60]. PEA shows inhibitory effects similar to those of AEA, except for a lack of effect on monocyte-dependent TNFα production and lymphocyte-dependent IFNγ synthesis [60]. Overall, a selective action of the two eCBs (maybe at receptor level) and a strict dependence on eCB tone [60] might account for these observations. 2-AG has been shown to inhibit TNFα secretion from LPS-treated mouse macrophages [61], as well as NO, PGE2 and IL-6 release from J774 macrophages through CB2 activation [62]. Unlike AEA, 2-AG seems to play an essential role in the recruitment of inflammatory and immunocompetent cells. Indeed, upon 2-AG treatment, undifferentiated HL-60 cells, as well as HL-60 cells differentiated into macrophage-like cells, showed enhanced IL-8 and macrophage-chemotactic protein 1 (MCP-1) production [63], paralleled by actin polymerization and extension of pseudopods [64]. Furthermore, differentiated HL-60 cells showed enhanced phagocytosis of opsonized zymosan in the presence of 2-AG; CB2 receptor, phosphoinositide 3kinase (PI3K) and extracellular signal-related kinase (ERK) were suggested to be involved in these effects [65] (Fig. 2). Once activated by invading microorganisms, immunocompetent cells led to elevated 2-AG levels in inflamed tissues, therefore it is tempting to speculate that 2-AG may stimulate (in an autocrine and/or paracrine fashion) the phagocytic activity of other types of inflammatory cells, thus contributing to self-defence mechanisms against infection.
Finally, our group has recently demonstrated an oxLDL-dependent modulation of the eCB system in primary human macrophage-derived lipid-loaden foam cells. Indeed, foam cells showed: (1) increased FAAH activity, (2) triplicated AEA levels, (3) doubled CB1/CB2 binding activity, (4) reduced TRPV1 binding activity [55]. These data, together with the finding that selective activation of CB2 receptor reduced cellular oxLDL uptake and cytokine (namely, TNFα, IL-12 and IL-10) release by human macrophages [55], seem to speak in favour of a crucial role for the eCB system during foam cell formation.
Data on eCBs and granulocytes are quite few or controversial, and mainly concern neutrophils. Once activated by a gradient of chemotactic factors [e.g. the bacterial product formyl-Met-Leu-Phe (fMLP), and host-derived products, like IL-8 and leukotriene B4 (LTB4)], neutrophils are the first inflammatory cells that rapidly migrate and infiltrate tissues, to phagocyte and destroy disease-producing pathogens [66]. Despite the numerous studies, yet it is not well defined the role that eCBs play in neutrophil function, since conflicting results have been obtained. Controversial literature data may be explained, at least in part, by different experimental paradigms simultaneously supporting direct and indirect effects. Indeed, Balenga and co-workers [67] showed that l-α-lysophosphatidylinositol (LPI), the natural GPR55 agonist, stimulated cytoskeleton remodelling, as well as neutrophil polarization and migration, with a possible cooperation between GPR55 and CB2 receptors, while McHugh and colleagues [68] reported a GPR55-mediated inhibition of migration. Moreover, CB2 activation has been shown to prevent neutrophil release of matrix metalloprotease-9 (MMP-9) both in vivo and in vitro [69]; conversely, 2-AG stimulates chemotaxis, myeloperoxidase release, ERK1/2 phosphorylation and Ca2+ mobilization in freshly isolated human neutrophils, via de novo biosynthesis of LTB4 [70].
eCBs can also interfere in the crosstalk between leukocytes and endothelial cells, in response to chemotactic stimuli released from inflamed endothelium (Fig. 2). For example, 2-AG upregulates the expression of selectins in human endothelial cells, which release TNF-α able to recruit lymphocytes and stimulate their rolling activity, thus allowing a coordinated action between the two cell types [71]. On the contrary, several findings pointed out the negative role played by CB2 receptors on interactions between endothelial and inflammatory cells: indeed, activation of CB2 receptor by specific agonists has been shown to decrease the amount of trans-migrating neutrophils in both myocardial and hepatic ischemia–reperfusion models [72, 73]. CB2 activation also reduces the number of neutrophils in ischemic brain, and inhibits their migration induced by CXCL2, as well as their adhesion to brain endothelial cells; therefore, selective CB2 activation may play a protective role against neuroinflammation, by suppressing leukocyte-blood brain barrier interactions [74, 75]. Targeting endothelial CB2 receptor has been suggested to represent a novel strategy for treatment of atherosclerosis, as it attenuates inflammatory responses in in vitro human coronary artery endothelial cells, as well as in isolated aortas and vascular endothelium [76]. Finally, CB2 activation may be useful to limit the progression of HIV-1 infection in the central nervous system, by inhibiting viral replication in infiltrating monocytes/macrophages [77].
Platelets
Among blood cells, platelets represent an important source of circulating eCBs, especially of 2-AG, which may participate in several pathophysiological responses. First evidence for the production of eCBs was presented by Varga and co-workers [57], who demonstrated that rat platelets contained significant amounts of 2-AG, that increased after in vitro exposure to an inflammatory stimulus. In the same year, Edgemond and colleagues [78] reported that human platelets were able to incorporate AEA and oxygenate it at the 12 position via the lipoxygenase pathway, thus producing the oxygenated derivative 12(S)-HAEA. The latter compound was able to bind both CB1 and CB2 receptors and to inhibit FAAH activity, thus prolonging AEA lifetime in the bloodstream. Later on, our group and others provided further biochemical evidence of eCB metabolism and their role in platelet physiology [79–82]. It is now widely accepted that platelets are able to metabolize both AEA and 2-AG, thus controlling their biological activity within the cardiovascular system.
AEA and 2-AG do not act as interchangeable mediators, but they are endowed with distinct biological functions, especially in megakaryocyte/platelet biology (Fig. 2). Although both eCBs can be involved in platelet activation [83], nonetheless only 2-AG is a true agonist of human platelets [84], while AEA more likely acts as a co-agonist, synergizing with classical inducers, such as collagen, ADP and thrombin. Indeed, 2-AG activates platelets at micromolar concentrations, by eliciting common metabolic responses (including increase in cytosolic calcium, inositol-1,4,5-trisphosphate and thromboxane A2, and decrease in cyclic AMP), through a p38MAPK/cPLA2-dependent mechanism [85, 86]. Activation induced by 2-AG is also accompanied by shape change, resulting from rearrangement of actin cytoskeleton: in the presence of 2-AG, changes in the G/F (i.e. monomeric/polymeric) actin ratio within platelet cytoplasm could be seen, leading to increased formation of actin filaments and cell protrusions [84]. In platelets, 2-AG also increases activity of endothelial nitric oxide synthase (eNOS), by promoting eNOS Ser1177 phosphorylation by protein kinase C, and Thr495 dephosphorylation via a mechanism involving the Ser/Thr protein phosphatase 1 [87] (Fig. 3a).
Fig. 3.
The “Yin-Yang” role of 2-AG and AEA in platelets. a Role of 2-AG as migrating factor. 2-AG activates platelets in a CB1/CB2 dependent manner, (1) by increasing cytosolic Ca2+, IP3 and TXA2 and decreasing cAMP, and (2) by stimulating eNOS activity. 2-AG might also be taken up by platelets and hydrolyzed by MAGL into AA, which, in turn, is oxidized by COX-1 to TXA2. b Role of AEA as survival factor. AEA enhances platelet life span (1) by activating the survival kinase Akt, which regulates, through phosphorylation of Bad, the interactions among pro- and anti-apoptotic members of Bcl-2 family, and (2) by stimulating eNOS activity. NO might also stimulate AEA uptake, thus modulating its action. See text for further details. AA arachidonic acid, CBR cannabinoid receptor, eNOS endothelial nitric oxide synthase, cAMP cyclic AMP, COX-1 cyclooxygenase-1, IP 3 inositol-1,4,5-trisphosphate, NO nitric oxide, MAGL monoacylglycerol lipase, TXA 2 thromboxane A2, PKC protein kinase C, PP1 protein phosphatase 1
Unlike 2-AG, AEA activates platelets at millimolar concentrations and at micromolar concentrations is effective only in the presence of other physiological agonists [79]. Therefore, the role of AEA is other than platelet activation and aggregation. Indeed, we demonstrated that AEA in blood may be one of the factors required for platelet survival; we reported that this eCB was able to prolong platelet life span by modulating the Akt-dependent phosphorylation of Bad, thus preventing its binding to Bcl-xL, and hence its pro-apoptotic activity [88]. Furthermore, by the same PI3K/Akt signalling pathway, AEA stimulates eNOS activity, thus increasing platelet nitric oxide (NO) and cyclic GMP basal levels [89] (Fig. 3b). The AEA-mediated NO increase may contribute to platelet survival and account for beneficial effects produced by this eCB, including vasodilatation [89, 90]. Keeping in mind that NO enhances AEA uptake (Fig. 3b) [91], an autocrine loop may be established, to remove AEA from extracellular space, thus limiting abnormal thrombus formation [79].
Although the relevance of eCBs as (co-)agonists of human platelets is now widely accepted, the role of CB receptors, as well as the mechanism of action, is controversial [92]. Our group and others [80, 85, 86, 93] showed that 2-AG-triggered aggregation is CB1/CB2-dependent (Fig. 3a), because it was reversed by CB1 and CB2 antagonists. Coherently, in unstimulated whole blood, the CB1 antagonist rimonabant decreased P-selectin and glycoprotein IIb/IIIa surface expression (thus reducing fibrinogen binding), and thrombin-induced platelet aggregation [86]. In contrast, Braud and colleagues [81] reported that, in rabbit platelets, AEA-induced aggregation was completely prevented by inhibition of cyclooxygenase-1 and FAAH activity, and so did Keown and co-workers [92], thus supporting that eCB action occurs via release of arachidonic acid. This hypothesis has recently been sustained also by Brantl and colleagues [94], who found that 2-AG and virodhamine (but not AEA) induced human platelet aggregation in their physiological milieu, i.e. blood and plasma, as well as shape change, aggregation and ATP secretion in platelet-rich plasma, through a MAGL-dependent mechanism leading to arachidonic acid release and its subsequent metabolism to thromboxane A2 by cyclooxygenase-1/thromboxane synthase (Fig. 3a). As we recently assessed [95], differences in experimental approaches might account for discrepancies among data concerning eCB effects on platelets. Moreover, taking into account that: (1) eCBs are metabolized by specific biosynthetic and degradative enzymes [4, 10] that control their activity at both central and peripheral levels, including in platelets [79–82]; and (2) inhibitors employed by Brantl’s group [94] to inhibit cyclooxygenase and MAGL activities have been used at significantly high concentrations, it is too simplistic to consider eCBs as a simple source of arachidonic acid, rather than true platelet (co)-agonists. Indeed, if arachidonic acid was the main player of eCB signalling, one might predict that AEA is also effective, since platelets promptly cleave it into arachidonic acid [79]. But, besides the recent study from De Angelis’ group [96] that reported an AEA-dependent inhibition of platelet aggregation and α-granule release by collagen, it is well recognized that AEA is unactive as platelet agonist [79, 80, 94]. In this context, it should also be underlined that 2-AG itself is a substrate of cyclooxygenases and lipoxygenases (see Fig. 1), being converted in biologically active oxygenated derivatives [11]. Hence, the effect of acetylsalicylic acid (inhibitor of cyclooxygenase activity) reported by Brantl’s group [94] might reflect blockade of 2-AG oxidation rather inhibition of the conversion of 2-AG-derived arachidonic acid into thromboxane A2. In conclusion, the effects of such inhibitors should be interpreted with caution and more work has to be done to unravel the molecular details of eCBs–platelet interactions.
Incidentally, human platelets express authentic CB1 and CB2 receptors, as we have recently demonstrated [14]. By analysing protein levels, cellular localization and functionality, we provided direct experimental evidence that both receptor subtypes are expressed in highly purified human platelets; however, they are predominantly confined inside platelets, thus explaining why only a small portion of CB1 and CB2 might be detected in preparations of plasma membranes [14].
Further studies are clearly warranted, especially considering the clinical potential of CB2 agonism or CB1 antagonism as additional therapeutic targets to reduce cardiovascular risk, where cyclooxygenase inhibitors cannot be chosen.
The eCB system in blood cell cancer
Oncogenesis, proliferation, migration and apoptosis of tumour cells are connected, in some way, to an altered eCB tone [97, 98]. However, it is not clear the exact role of eCBs in cancer-related events, neither it is known whether alterations in eCB system are one of the cancer-promoting factors or rather a consequence of generalized altered metabolism. Indeed, the ability of eCBs to activate more than one molecular target allows to trigger different (and sometimes opposite) signalling pathways, so that protective or oncogenic effects may vary according to the type of cancer, and to the activated receptor (CB1 versus TRPV1) [99].
Overexpression of CB receptors has been reported in different blood cancer types (Table 3). Increased CB2 levels have been found in human myeloid leukaemia cell lines, in human blasts from acute myeloid leukaemia (AML), and in certain non-Hodgkin’s B and T lymphomas [100–102]. Moreover, the finding that the majority of non-Hodgkin’s B lymphomas [101], as well as of Hodgkin’s lymphomas [103], also have increased levels of CB1 receptor strongly suggests the involvement of this receptor in tumorigenesis.
Table 3.
Alterations of blood eCB system in pathological conditions
| Pathology | Up-regulation | Down-regulation | Agonist | Effect | References |
|---|---|---|---|---|---|
| Blood cancer | |||||
| Acute myeloid leukaemia | CB2 | [100] | |||
| Non-Hodgkin’s B lymphoma | CB1, CB2 | WIN55212-2, Met-AEA, rimonabant | ↑Cell death, ↓ proliferation | [101, 104–107] | |
| Non-Hodgkin’s T lymphoma | CB2 | [102] | |||
| Hodgkin’s lymphoma | CB1 | [103] | |||
| Neurological diseases | |||||
| Huntington’s disease | AEA | FAAH | [136] | ||
| Multiple sclerosis | AEA, CB2 NAPE-PLD | FAAH | [137–139] | ||
| Parkinson’s disease | AEA | FAAH | [135, 143] | ||
| Alzheimer disease | FAAH | [144] | |||
| Migraine | FAAH, EMT | AEA | [150] | ||
| Chronic/medication-overuse headache | FAAH, EMT AEA, 2-AG | [151, 153] | |||
| Psychiatric disorders | |||||
| Attention-deficit/hyperactivity disorder | AEA | FAAH | [145] | ||
| Depression | AEA, 2-AG | [146] | |||
| Schizophrenia | Cannabidiol | ↑ AEA, improvement of symptoms | [147] | ||
An interesting finding is that CB2 receptor acts as a protooncogene involved in leukemic transformation in AML, while it plays a protective role against abnormal cell growth in certain B cell malignancies (Table 3) [30, 31, 100]. In mantle cell lymphoma, Gustafsson and co-workers [101, 104, 105] demonstrated that CB2 pharmacological activation (by WIN55212-2 or Met-AEA) reduces cell proliferation via CB-dependent ceramide accumulation and p38-dependent activation of caspase-3. As demonstrated by Wasik and co-workers [106], other mechanisms, including CB-independent cytoplasmic vacuolation, may induce cell death in certain types of primary mantle cell lymphoma. Mantle cell lymphoma proliferation can be blocked also by rimonabant (a CB1 antagonist/inverse agonist), thus suggesting that more complex mechanisms underlying CB-dependent cell growth inhibition exist [101]. Similarly, rimonabant has been shown to regulate proliferation of other types of blood cancers, where it induces cell cycle arrest or cell death responses (e.g. inhibition of PI3K/Akt pathway, phosphatydilserine exposure and dissipation of mitochondrial membrane potential) depending on the cell type considered [107].
Finally, it should also be underlined that pharmacological targeting of CB receptors might represent a novel therapeutic approach to restore blood cell functions compromised by chemo- and radiation therapies. Following sublethal irradiation, haematopoietic recovery is significantly enhanced in mice treated with AM1241 (a CB2 agonist), via inhibition of apoptosis and promotion of cell cycle entry of HSCs, while it is impaired in CB2 knockout mice [26].
The eCB system in inflammatory diseases
The ability of eCBs to modulate immunocompetent cells is receiving growing interest in scientific community, especially in the light of the impact on inflammatory diseases. Indeed, tissue-specific dysregulated eCB tone, resulting from altered expression of CB receptors and/or eCB metabolizing enzymes, has been reported in numerous pathological conditions. As the pathological role of the eCB system in inflammatory pathologies has been summarized in more detail elsewhere [38, 108], here we reported only few selected examples (Table 3).
(e)CBs have been shown to reduce inflammatory hyperalgesia, either in animals or humans [109–112]. In this context, it should be recalled that FAAH modulates the eCB tone, in vivo; this finding is supported by the evidence that, in λ-carrageenin treated rats, increased FAAH expression (paralleled by decreased AEA, 2-AG and PEA concentrations and enhanced CB1 and CB2 receptor expression) was associated to granuloma formation, while its pharmacological blockade reduced TNFα release and granuloma-dependent angiogenesis [113].
In inflammatory bowel disease (IBD), inflamed mucosa has low AEA levels, as a result of decreased biosynthesis and increased degradation [114]. Accordingly, the not-hydrolysable analogue Met-AEA drops off the release of pro-inflammatory cytokines (IFN-γ, IL-17 and TNF-α) from inflamed mucosa of IBD patients [114], thus suggesting that activation of CB receptors may be useful for treatment of the disease; indeed, pharmacological elevation of eCB content attenuates colitis symptoms in wild-type mice, but not in CB−/−1 and CB−/−2 littermates [115]. Accordingly, activation of CB2 receptor: (1) reduces the number of neutrophils, mast, CD4+, NK and T cells, in intestinal lamina propria and mesenteric lymph nodes of IL-10−/− mice (which spontaneously develop chronic colitis at 12 weeks of age) [116]; (2) reduces the number of macrophages and IFNγ-expressing cells in dextran sodium sulphate-treated mice (which are affected by acute colitis) [117]. Conversely, we found that human inflamed IBD mucosa expressed more CB1 than uninflamed mucosa without changes in CB2 content [114]. Differences in species (humans versus mice), as well as in IBD experimental models, might underlie these discrepancies. Another interesting finding is that, in celiac disease, AEA seems to act as a pro-inflammatory compound: active celiac subjects show high levels of CB receptors, as well as of AEA (and PEA) in their mucosa (due to increased NAPE-PLD activity), which return to basal levels with a gluten-free diet [118–120].
eCB signalling appears to be also involved in immune responses associated to atherogenesis and its clinical manifestations, although its exact role is quite controversial. In atherosclerosis-prone apolipoprotein E-deficient (ApoE−/−) mice, CB2 stimulation reduces both infiltrating neutrophils and intraplaque MMP-9 levels, thus restraining plaque susceptibility to rupture [69]; coherently, leukocyte infiltration in atherosclerotic plaques increases in double knocked out mice for ApoE and CB2 receptor or in irradiated ApoE−/− mice reconstituted with CB−/−2 bone marrow [121]. On the contrary, Willecke and co-workers [122] reported that neither genetic deficiency nor activation of CB2 receptor was able to modulate atherogenesis in low-density lipoprotein receptor knockout mice, while Lenglet’s group [123] showed that in ApoE−/− mice feeding high-cholesterol diet, pharmacological and genetic ablation of FAAH enhanced neutrophil recruitment. Accordingly, FAAH deletion exacerbated myocardial injury by increasing myocardial neutrophil infiltration [124].
An interesting finding with pharmacological implications is that, in primary peritoneal and immortalized macrophages, oxidized low-density lipoproteins increase eCB tone; subsequent activation of CB receptor triggers cholesterol accumulation in macrophages, by up-modulating expression of CD36 receptor (responsible for cholesterol influx), and by down-modulating expression of ATP-binding cassette protein A1 (responsible for cholesterol efflux) [125]. Accordingly, patients with coronary artery disease show enhanced serum levels of eCBs (including AEA, 2-AG, PEA and OEA), which might increase the risk of atherosclerotic plaque rupture, via promotion of neutrophil recruitment and activity [126].
Systemic and local inflammation is also deeply connected to ischemic stroke [127–129]. Using different experimental models, it has been shown that CB2 activation limits cerebral infarct size, via attenuation of chemokine signalling, inflammatory cell infiltration, oxidative/nitrosative stress and/or cell death [130]. Furthermore, treatment of transient focal ischemic mice with selective CB2 receptor agonists, before and after reperfusion, both prevents and reduces leukocyte migration, thus improving infarct outcome and motor function [74, 131, 132]. In a mouse model of liver ischemia/reperfusion injury, JWH133 protects against damage, by decreasing inflammatory cell infiltration, tissue and serum TNFα, MIP-1a/CCL3 and MIP-2/CXCL2 levels, as well as ICAM-1 expression [133]. It has also been hypothesized that receptors other than CB2 might represent promising therapeutic approaches for ischemia-induced inflammation, since CBD attenuates TNFα production in Kupffer cells (resident macrophages of the liver), along with ICAM-1 expression and leukocyte adhesion to human sinusoidal endothelium [134].
Blood eCB system as a mirror of neurological diseases
In recent years, an increasing number of experimental observations have indicated that peripheral blood cells might represent a novel, non-invasive diagnostic tool of several neurological disorders, as dysregulation of their activity often mirrors central dysfunctions (Table 3).
In particular, patients suffering from distinct neurological diseases show alterations of the eCB system in their lymphocytes or/and platelets [135]. This is the case of peripheral lymphocytes from Huntington’s disease patients that have a remarkable decrease of FAAH activity and increase of endogenous AEA levels compared to healthy subjects, with no changes in other elements of the eCB system [136]. Similarly, AEA (but not 2-AG) levels are higher in peripheral lymphocytes of relapsing multiple sclerosis (MS) patients; in this case, increased blood AEA content depends on increased synthesis by NAPE-PLD and reduced degradation by FAAH, and mirrors increased AEA levels found in the cerebrospinal fluid [137]. AEA levels are increased in active MS lesions [138], coherently CB2 receptor, absent in inactive plaques, is expressed in macrophages showing recent phagocytic activity, as well as in perivascular T lymphocytes [139]. Accordingly, T and B cells from MS patients had significantly high CB1 and CB2 expression, respectively [140].
It has been recently proposed that AEA may limit immune response associated to MS and, thus, protect brain from neuroinflammation, by restoring cytokine balance in microglia, via a CB2-dependent mechanism [141, 142]. This hypothesis is supported by the evidence that AEA (but not 2-AG) levels were significantly elevated in B, T and NK cells prior interferon therapy and returned to values comparable to healthy subjects following 1 year of treatment [140]. Incidentally, we have shown that AEA has distinct immunomodulatory effects on human myeloid and plasmacytoid dendritic cells from healthy and MS individuals. AEA modulates cytokine production and Th-1/Th-17 commitment in both healthy dendritic cells and MS myeloid dendritic cells, while it has no effect at all in MS plasmacytoid dendritic cells. Such a lack of effect depends on increased FAAH expression in MS plasmacytoid dendritic cells [55]. This finding, together with the evidence that the expression of FAAH was unchanged in MS B, T and NK cells [140] seems to speak in favour of a specific regulation of FAAH activity in distinct blood cells.
Additionally, lymphocytes from Parkinson’s disease patients, whose cerebrospinal fluid contains high AEA levels [143], have FAAH expression and activity significantly lower than that found in healthy controls, thus indicating that enzyme dysfunction might represent a compensatory mechanism, also occurring at striatal level, aimed at compensating central dopamine deficiency [135]. Peripheral blood mononuclear cells of subjects with late-onset Alzheimer disease (AD) show increased FAAH activity, as a result of epigenetic regulation, identifying FAAH as a new potential biomarker for AD in easily accessible peripheral cells [144].
Alterations in the eCB system of immune cells have also been observed in psychiatric disorders. Decreased AEA hydrolysis (but not synthesis) has been found in lymphocytes derived from patients affected by attention-deficit/hyperactivity disorder, the most commonly diagnosed neurodevelopmental disorder in childhood [145]. Serum levels of both AEA and 2-AG also increase and correlate with blood pressure in women diagnosed with depression [146]. The relevance of blood eCBs tone has recently been sustained by a double-blind, randomized clinical trial, where cannabidiol treatment was shown to increase serum AEA levels that were correlated with clinical improvement of schizophrenia symptoms [147]. Moreover, CB2 gene expression appears to be significantly upregulated in peripheral blood mononuclear cells from autistic children [148], with a specific increase of NAPE-PLD/FAAH expression ratio in their macrophages [149].
Also platelet eCB system has been shown to be altered in patients with some neurological disorders. This is the case of patients with migraine, whose platelets show altered serotonin concentration, which correlates with chronification of headache [150]. Platelets from female (but not male) patients with migraine without aura have increased activity of both FAAH and EMT, with no difference in the expression of CB receptors [150]. Such an observation may explain the prevalence of migraine in women, as increased degradation of platelet AEA, and thus lower blood AEA content, may contribute to reduce pain threshold [150]. Instead, platelets from chronic migraine (CM) and medication-overuse headache (MOH) subjects show reduced EMT and FAAH levels, compared to either controls or episodic migraine group, without differences in gender [151]. We recently identified a relationship between altered platelet FAAH activity and reduction in facilitation of pain processing in MOH subjects; this could represent the consequence of a mechanism devoted to acutely reduce eCB degradation upon pain [152]. Finally, decreased plasma AEA and 2-AG levels (especially in females) have also been reported in CM and MOH patients [153]. Interestingly, alterations of the eCB tone seem to reflect those of serotonin, as a correlation between the levels of this neurotransmitter and 2-AG has been found, particularly in MOH patients [153], hence supporting validity of platelets as models for neuronal pathophysiology.
Therapeutic exploitation
The wide pharmacopoeia of CB receptor ligands (including agonists, antagonists and inverse agonists) has offered the incentive for developing meaningful therapeutic approaches in a plethora of pathologies affecting humans due to inflammatory, immunological and oncological disorders [108, 154–156].
The only therapeutically relevant CB receptor ligands currently in use are Δ9-tetra-hydrocannabinol (Δ9-THC), its synthetic forms and closely related compounds (154). Sativex is a vaporized delivery system for purified Δ9-THC that has obtained approval status for treatment of neuropathic pain and spasticity in multiple sclerosis; Dronabinol, a synthetic Δ9-THC, is usually employed for treatment of neuropathic pain in multiple sclerosis, anorexia in AIDS and nausea and vomiting in cancer chemotherapy; Nabilone, a derivatized synthetic Δ9-THC, has been approved in UK, Canada and Mexico for cancer patients [154]. Sanofi-Synthelabo has developed CB receptor antagonists to be used in the clinic: initially approved for therapeutic use, the CB1 antagonist SR141716A (Rimonabant, Accomplia) has been withdrawn because of serious concerns to the safety [157].
The immunosuppressive potency of eCBs, together with their ability to negatively impact the release of pro-inflammatory mediators, has allowed testing the eCB-based drugs in inflammatory experimental models and even in some human diseases [158, 159]. For example, inhaled Δ9-THC can restrain airway or gastrointestinal inflammation, suggesting its clinical application for treatment of asthma, inflammatory Bowel and Crohn’s diseases. Despite the body of evidences from pre-clinical studies, successful randomized trials are very few and, till now, it is difficult to translate the basic data in therapeutic interventions, because of several factors, including chemically labile structures, poor bioavailability, severe side effects, and failure to arrest disease progression.
Several aspects may account for this gap between in vitro and in vivo experimental data and clinical translation. First, currently available receptor agonists are not totally specific, so that, at high doses, agonists of one receptor may activate the other type of receptor, especially when the levels of CB1 and CB2 expression are considerably different [108]. This should be taken into account, considering that in many immunocytes, CB2 activation exerts suppressive effects, while CB1 activation is mainly responsible for the pro-inflammatory action of eCBs [160]. Another cause is that eCBs may exert different effects depending on specific steps of the disease. For example, CB agonists appear to be effective at early stages, while losing their efficacy at later time points, as it is the case of sepsis immunopathogenesis [158]: during the early hyper-inflammatory response, modulation of CB2 receptor is helpful to dampen down the uncontrolled over-activation of the innate immune system, but in later stages of sepsis immune-suppression occurs and, therefore, modulation of the eCB system is needed to enhance the inflammatory response.
Finally, potential side effects of eCB therapeutics, including those affecting the neurological (mood alterations, depression, psychosis) and/or cardiovascular (hypotension, ischemia, stroke, inflammation) systems should also be considered [161–164]. Given their immunoactivity, profound phenotypic changes may indeed occur after continued eCB exposure; increases in TNFα, IFNγ and IL-2 levels have been found in Dronabinol-treated patients [165], and marijuana users have experienced decrease in NK cell numbers, reduction of IL-2 levels, and increase in pro-inflammatory cytokines IL-10 and TGF1 [166]. Therefore, it is conceivable that, in the long term, therapeutic eCBs may have immunological side effects, including increased susceptibility to infectious agents, dysregulated production of cytokines, and alterations in cell-mediated immunity. This should be considered when eCB-based drugs are thought for treating diseases (such as AIDS, anorexia, cancer, obesity) where immune responses are impaired, so that prolonged exposure to eCBs has the potential to worsen an already compromised immune system.
Conclusions and future perspectives
Since the discovery of the eCB system in the early 1990s, an ever-growing body of literature data has helped to better define its role in haematopoiesis and bone marrow function, as well as in platelet and leukocyte pathophysiology. Moreover, the evidence that the eCB system (and particularly CB2 receptor) is dysregulated in several blood cancers and pathologies characterized by abnormal inflammatory responses, clearly supports that it should be considered a therapeutic target to prevent (and even treat) blood-related disorders. Nonetheless, the complexity of the eCB system requires special caution in drawing eCB therapeutic applications, as activation of these pathways may either represent a compensatory response to a specific insult (thus slowing progression of the disease) or may be pathogenic (thus exacerbating symptoms). A typical example of eCB system complexity is offered by platelets that may store eCBs, may be arachidonate reservoirs, or may release the oxygenated eCB derivatives to activate other cells; this multi-faced aspect requires being very careful in the therapeutic application of eCBs, to optimize benefits and minimize risks.
An interesting finding is that several elements of blood eCB system appear to follow the same alterations observed in some neurological disorders, thus leading to the challenging hypothesis that blood eCB system might be a central nervous system mirror, suitable for novel, non-invasive diagnostic strategies for brain diseases. Due to the complexity of neurological disorders, it is very difficult to have perfect and accessible biomarkers useful for measuring the progress of neurological disorders or the effects of treatment. Therefore, it is wished to better clarify the role of eCB system in these diseases to have effective therapeutic targets.
Acknowledgments
We wish to thank all colleagues who have contributed over the years to our studies on endocannabinoids in blood cell biology. Financial support from Ministero dell’Istruzione, dell’Università e della Ricerca (PRIN 2009 to L.A., PRIN 2010–2011 to M.M.), and by Fondazione TERCAS (Grant 2009–2012 to M.M.).
Abbreviations
- 2-AG
2-Arachidonoylglycerol
- Met-AEA
2-methylarachidonyl-(2′-fluoroethyl)amide
- ABHD
a/b-hydrolase
- AML
Acute myeloid leukaemia
- ApoE
Apolipoprotein E
- CB
Cannabinoid
- CM
Chronic migraine
- eCB
Endocannabinoid
- EMT
eCB membrane transporter
- eNOS
Endothelial nitric oxide synthase
- ERK
Extracellular signal-related kinase
- FAAH
Fatty acid amide hydrolase
- fMLP
Formyl-Met-Leu-Phe
- G-CSF
Granulocyte-colony-stimulating factor
- GM-CSF
Granulocyte-macrophage colony-stimulating factor
- HETE-G
Hydroxyeicosatetraenoyl glycerylester
- (S)-HAEA
Hydroxyeicosatetraenoylethanolamide
- IBD
Inflammatory bowel disease
- IFNγ
Interferon γ
- IL
Interleukin
- LTB4
Leukotriene B4
- LPS
Lipopolysaccharide
- MCP-1
Macrophage-chemotactic protein 1
- MMP-9
Matrix metalloprotease-9
- MOH
Medication-overuse headache
- MAGL
Monoacylglyceride lipase
- MS
Multiple sclerosis
- NAPE-PLD
N-acylphosphatydiletanolamine phospholipase D
- anandamide, AEA
N-arachidonoylethanolamine
- NK
Natural killer
- NO
Nitric oxide
- PEA
N-palmitoylethanolamine
- OEA
N-oleoylethanolamine
- PPARs
Peroxisome proliferator-activated receptors
- PI3 K
Phosphoinositide 3kinase
- PGE2
Prostaglandin E2
- Th
T helper
- TRPV1
Transient receptor potential vanilloid 1
- TNFα
Tumour necrosis factor α
- CB1
Type-1 cannabinoid receptor
- CB2
Type-2 cannabinoid receptor
Footnotes
M. Maccarrone and M. V. Catani are equal senior authors.
References
- 1.Fonseca BM, Costa MA, Almada M, Correia-da-Silva G, Teixeira NA. Endogenous cannabinoids revisited: a biochemistry perspective. Prostaglandins Other Lipid Mediat. 2013;102–103:13–30. doi: 10.1016/j.prostaglandins.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 2.Bisogno T, Maccarrone M. Endocannabinoid signaling and its regulation by nutrients. BioFactors. 2014;40:373–380. doi: 10.1002/biof.1167. [DOI] [PubMed] [Google Scholar]
- 3.Hansen HS. Palmitoylethanolamide and other anandamide congeners. Proposed role in the diseased brain. Exp Neurol. 2010;224:48–55. doi: 10.1016/j.expneurol.2010.03.022. [DOI] [PubMed] [Google Scholar]
- 4.Ueda N, Tsuboi K, Uyama T. Metabolism of endocannabinoids and related N-acylethanolamines: canonical and alternative pathways. FEBS J. 2013;280:1874–1894. doi: 10.1111/febs.12152. [DOI] [PubMed] [Google Scholar]
- 5.Piomelli D. More surprises lying ahead. The endocannabinoids keep us guessing. Neuropharmacology. 2014;76:228–234. doi: 10.1016/j.neuropharm.2013.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giuffrida A, Parsons LH, Kerr TM, Rodríguez de Fonseca F, Navarro M, Piomelli D. Dopamine activation of endogenous cannabinoid signaling in dorsal striatum. Nat Neurosci. 1999;2:358–363. doi: 10.1038/7268. [DOI] [PubMed] [Google Scholar]
- 7.Malcher-Lopes R, Di S, Marcheselli VS, Weng FJ, Stuart CT, Bazan NG, Tasker JG. Opposing crosstalk between leptin and glucocorticoids rapidly modulates synaptic excitation via endocannabinoid release. J Neurosci. 2006;26:6643–6650. doi: 10.1523/JNEUROSCI.5126-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silvestri C, Di Marzo V. The endocannabinoid system in energy homeostasis and the etiopathology of metabolic disorders. Cell Metab. 2013;17:475–490. doi: 10.1016/j.cmet.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 9.Fowler CJ. Transport of endocannabinoids across the plasma membrane and within the cell. FEBS J. 2013;280:1895–1904. doi: 10.1111/febs.12212. [DOI] [PubMed] [Google Scholar]
- 10.Maccarrone M, Dainese E, Oddi S. Intracellular trafficking of anandamide: new concepts for signalling. Trends Biochem Sci. 2010;35:601–608. doi: 10.1016/j.tibs.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 11.Rouzer CA, Marnett LJ. Endocannabinoid oxygenation by cyclooxygenases, lipoxygenases, and cytochromes P450: cross-talk between the eicosanoid and endocannabinoid signalling pathways. Chem Rev. 2011;111:5899–5921. doi: 10.1021/cr2002799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pertwee RG, Howlett AC, Abood ME, Alexander SP, Di Marzo V, Elphick MR, Greasley PJ, Hansen HS, Kunos G, Mackie K, Mechoulam R, Ross RA. International Union of Basic and Clinical Pharmacology. LXXIX. Cannabinoid receptors and their ligands: beyond CB1 and CB2 . Pharmacol Rev. 2010;62:588–631. doi: 10.1124/pr.110.003004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Howlett AC, Blume LC, Dalton GD. CB(1) cannabinoid receptors and their associated proteins. Curr Med Chem. 2010;17:1382–1393. doi: 10.2174/092986710790980023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Catani MV, Gasperi V, Catanzaro G, Baldassarri S, Bertoni A, Sinigaglia F, Avigliano L, Maccarrone M. Human platelets express authentic CB1 and CB2 receptors. Curr Neurovasc Res. 2010;7:311–318. doi: 10.2174/156720210793180774. [DOI] [PubMed] [Google Scholar]
- 15.Viscomi MT, Oddi S, Latini L, Pasquariello N, Florenzano F, Bernardi G, Molinari M, Maccarrone M. Selective CB2 receptor agonism protects central neurons from remote axotomy-induced apoptosis through the PI3 K/Akt pathway. J Neurosci. 2009;29:4564–4570. doi: 10.1523/JNEUROSCI.0786-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gasperi V, Dainese E, Oddi S, Sabatucci A, Maccarrone M. GPR55 and its interaction with membrane lipids: comparison with other endocannabinoid-binding receptors. Curr Med Chem. 2013;20:64–78. [PubMed] [Google Scholar]
- 17.Ryberg E, Larsson N, Sjogren S, Hjorth S, Hermansson NO, Leonova J, Elebring T, Nilsson K, Drmota T, Greasley PJ. The orphan receptor GPR55 is a novel cannabinoid receptor. Br J Pharmacol. 2007;152:1092–1101. doi: 10.1038/sj.bjp.0707460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lauckner JE, Jensen JB, Chen HY, Lu HC, Hille B, Mackie K. GPR55 is a cannabinoid receptor that increases intracellular calcium and inhibits M current. Proc Natl Acad Sci USA. 2008;105:2699–2704. doi: 10.1073/pnas.0711278105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maccarrone M, Lorenzon T, Bari M, Melino G, Finazzi-Agro A. Anandamide induces apoptosis in human cells via vanilloid receptors. Evidence for a protective role of cannabinoid receptors. J Biol Chem. 2000;275:31938–31945. doi: 10.1074/jbc.M005722200. [DOI] [PubMed] [Google Scholar]
- 20.Di Marzo V, De Petrocellis L. Endocannabinoids as regulators of transient receptor potential (TRP) channels: a further opportunity to develop new endocannabinoid-based therapeutic drugs. Curr Med Chem. 2010;17:1430–1449. doi: 10.2174/092986710790980078. [DOI] [PubMed] [Google Scholar]
- 21.Pistis M, Melis M. From surface to nuclear receptors: the endocannabinoid family extends its assets. Curr Med Chem. 2010;17:1450–1467. doi: 10.2174/092986710790980014. [DOI] [PubMed] [Google Scholar]
- 22.Cao H, Oteiza A, Nilsson SK. Understanding the role of the microenvironment during definitive hemopoietic development. Exp Hematol. 2013;41:761–768. doi: 10.1016/j.exphem.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 23.Anthony BA, Link DC. Regulation of hematopoietic stem cells by bone marrow stromal cells. Trends Immunol. 2014;35:32–37. doi: 10.1016/j.it.2013.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Massberg SP, Schaerli I, Knezevic-Maramica I, Köllnberger M, Tubo N, Moseman EA, Huff IV, Junt T, Wagers AJ, Mazo IB, von Andrian UH. Immunosurveillance by hematopoietic progenitor cells trafficking through blood, lymph, and peripheral tissues. Cell. 2007;131:994–1008. doi: 10.1016/j.cell.2007.09.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Granick JL, Simon SI, Borjesson DL. Hematopoietic stem and progenitor cells as effectors in innate immunity. Bone Marrow Res. 2012;2012:165107–165115. doi: 10.1155/2012/165107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jiang S, Fu Y, Avraham HK. Regulation of hematopoietic stem cell trafficking and mobilization by the endocannabinoid system. Transfusion. 2011;51:65S–71S. doi: 10.1111/j.1537-2995.2011.03368.x. [DOI] [PubMed] [Google Scholar]
- 27.Patinkin D, Milman G, Breuer A, Fride E, Mechoulam R. Endocannabinoids as positive or negative factors in hematopoietic cell migration and differentiation. Eur J Pharmacol. 2008;595:1–6. doi: 10.1016/j.ejphar.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 28.Galve-Roperh I, Chiurchiù V, Díaz-Alonso J, Bari M, Guzmán M, Maccarrone M. Cannabinoid receptor signaling in progenitor/stem cell proliferation and differentiation. Prog Lipid Res. 2013;52:633–650. doi: 10.1016/j.plipres.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 29.Valk P, Verbakel S, Vankan Y, Hol S, Mancham S, Ploemacher R, Mayen A, Löwenberg B, Delwel R. Anandamide, a natural ligand for the peripheral cannabinoid receptor is a novel synergistic growth factor for hematopoietic cells. Blood. 1997;90:1448–1457. [PubMed] [Google Scholar]
- 30.Jordà MA, Verbakel SE, Valk PJ, Vankan-Berkhoudt YV, Maccarrone M, Finazzi-Agrò A, Löwenberg B, Delwel R. Hematopoietic cells expressing the peripheral cannabinoid receptor migrate in response to the endocannabinoid 2-arachidonoylglycerol. Blood. 2002;99:2786–2793. doi: 10.1182/blood.v99.8.2786. [DOI] [PubMed] [Google Scholar]
- 31.Jordà MA, Löwenberg B, Delwel R. The peripheral cannabinoid receptor Cb2, a novel oncoprotein, induces a reversible block in neutrophilic differentiation. Blood. 2003;101:1336–1343. doi: 10.1182/blood-2002-07-2034. [DOI] [PubMed] [Google Scholar]
- 32.Hoggat J, Pelus LM. Eicosanoid regulation of hematopoiesis and hematopoietic stem and progenitor trafficking. Leukemia. 2010;24:1993–2002. doi: 10.1038/leu.2010.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Catani MV, Fezza F, Baldassarri S, Gasperi V, Bertoni A, Pasquariello N, Finazzi-Agrò A, Sinigaglia F, Avigliano L, Maccarrone M. Expression of the endocannabinoid system in the bi-potential HEL cell line: commitment to the megakaryoblastic lineage by 2-arachidonoylglycerol. J Mol Med (Berl) 2009;87:65–74. doi: 10.1007/s00109-008-0406-3. [DOI] [PubMed] [Google Scholar]
- 34.Gasperi V, Avigliano L, Evangelista D, Oddi S, Chiurchiù V, Lanuti M, Maccarrone M, Catani MV (2014) 2-Arachidonoylglycerol enhances platelet formation from human megakaryoblasts. Cell Cycle In press [DOI] [PMC free article] [PubMed]
- 35.Bojesen IN, Hansen HS. Membrane transport of anandamide through resealed human red cell membranes. J Lipid Res. 2005;46:1652–1659. doi: 10.1194/jlr.M400498-JLR200. [DOI] [PubMed] [Google Scholar]
- 36.Bentzen PJ, Lang F. Effect of anandamide on erythrocyte survival. Cell Physiol Biochem. 2007;20:1033–1042. doi: 10.1159/000110714. [DOI] [PubMed] [Google Scholar]
- 37.Bobbala D, Alesutan I, Föller M, Huber SM, Lang F. Effect of anandamide in plasmodium berghei infected mice. Cell Physiol Biochem. 2010;26:355–362. doi: 10.1159/000320559. [DOI] [PubMed] [Google Scholar]
- 38.Witkamp R, Meijerink J. The endocannabinoid system: an emerging key player in inflammation. Curr Opin Clin Nutr Metab Care. 2014;17:130–138. doi: 10.1097/MCO.0000000000000027. [DOI] [PubMed] [Google Scholar]
- 39.Constantinescu CS (ed) (2010) Immunobiol. Special Issue Cannabinoids Immunol 215:587–672 [DOI] [PubMed]
- 40.Coopman K, Smith LD, Wright KL, Ward SG. Temporal variation in CB2R levels following T lymphocyte activation: evidence that cannabinoids modulate CXCL12-induced chemotaxis. Int Immunopharmacol. 2007;7:360–371. doi: 10.1016/j.intimp.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 41.Bouaboula M, Rinaldi M, Carayon P, Carillon C, Delpech B, Shire D, Le Fur G, Casellas P. Cannabinoid-receptor expression in human leukocytes. Eur J Biochem. 1993;214:173–180. doi: 10.1111/j.1432-1033.1993.tb17910.x. [DOI] [PubMed] [Google Scholar]
- 42.Ziring D, Wei B, Velazquez P, Schrage M, Buckley NE, Braun J. Formation of B and T cell subsets require the cannabinoid receptor CB2. Immunogenetics. 2006;58:714–725. doi: 10.1007/s00251-006-0138-x. [DOI] [PubMed] [Google Scholar]
- 43.Tanikawa T, Kurohane K, Imai Y. Induction of preferential chemotaxis of unstimulated B-lymphocytes by 2-arachidonoylglycerol in immunized mice. Microbiol Immunol. 2007;51:1013–1019. doi: 10.1111/j.1348-0421.2007.tb03985.x. [DOI] [PubMed] [Google Scholar]
- 44.Muppidi JR, Arnon TI, Bronevetsky Y, Veerapen N, Tanaka M, Besra GS, Cyster JG. Cannabinoid receptor 2 positions and retains marginal zone B cells within the splenic marginal zone. J Exp Med. 2011;208:1941–1948. doi: 10.1084/jem.20111083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sancho R, Macho A, de La Vega L, Calzado MA, Fiebich BL, Appendino G, Muñoz E. Immunosuppressive activity of endovanilloids: N-arachidonoyl-dopamine inhibits activation of the NF-kB, NFAT, and activator protein 1 signalling pathways. J Immunol. 2004;172:2341–2351. doi: 10.4049/jimmunol.172.4.2341. [DOI] [PubMed] [Google Scholar]
- 46.Kaplan BL, Ouyang Y, Herring A, Yea SS, Razdan R, Kaminski NE. Inhibition of leukocyte function and interleukin-2 gene expression by 2-methylarachidonyl-(2 V-fluoroethyl)amide, a stable congener of the endogenous cannabinoid receptor ligand anandamide. Toxicol Appl Pharmacol. 2005;205:107–115. doi: 10.1016/j.taap.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 47.Rockwell CE, Raman P, Kaplan BL, Kaminski NE. A COX-2 metabolite of the endogenous cannabinoid, 2-arachidonyl glycerol, mediates suppression of IL-2 secretion in activated Jurkat T cells. Biochem Pharmacol. 2008;76:353–361. doi: 10.1016/j.bcp.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 48.Cencioni MT, Chiurchiù V, Catanzaro G, Borsellino G, Bernardi G, Battistini L, Maccarrone M. Anandamide suppresses proliferation and cytokine release from primary human T-lymphocytes mainly via CB2 receptors. PLoS ONE. 2010;5:e8688. doi: 10.1371/journal.pone.0008688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nagarkatti P, Pandey R, Rieder SA, Hegde VL, Nagarkatti M. Cannabinoids as novel anti-inflammatory drugs. Future Med Chem. 2009;1:1333–1349. doi: 10.4155/fmc.09.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Maestroni GJ. The endogenous cannabinoid 2-arachidonoyl glycerol as in vivo chemoattractant for dendritic cells and adjuvant for Th1 response to a soluble protein. FASEB J. 2004;18:1914–1916. doi: 10.1096/fj.04-2190fje. [DOI] [PubMed] [Google Scholar]
- 51.Ribeiro A, Ferraz-de-Paula V, Pinheiro ML, Sakai M, Costa-Pinto FA, Palermo-Neto J. Anandamide prior to sensitization increases cell-mediated immunity in mice. Int Immunopharmacol. 2010;10:431–439. doi: 10.1016/j.intimp.2009.12.017. [DOI] [PubMed] [Google Scholar]
- 52.Maccarrone M, Valensise H, Bari M, Lazzarin N, Romanini C, Finazzi-Agrò A. Progesterone up-regulates anandamide hydrolase in human lymphocytes: role of cytokines and implications for fertility. J Immunol. 2001;166:7183–7189. doi: 10.4049/jimmunol.166.12.7183. [DOI] [PubMed] [Google Scholar]
- 53.Kuwae T, Shiota Y, Schmid PC, Krebsbach R, Schmid HH. Biosynthesis and turnover of anandamide and other N-acylethanolamines in peritoneal macrophages. FEBS Lett. 1999;459:123–127. doi: 10.1016/s0014-5793(99)01226-0. [DOI] [PubMed] [Google Scholar]
- 54.Di Marzo V, Bisogno T, De Petrocellis L, Melck D, Orlando P, Wagner JA, Kunos G. Biosynthesis and inactivation of the endocannabinoid 2-arachidonoylglycerol in circulating and tumoral macrophages. Eur J Biochem. 1999;264:258–267. doi: 10.1046/j.1432-1327.1999.00631.x. [DOI] [PubMed] [Google Scholar]
- 55.Chiurchiù V, Cencioni MT, Bisicchia E, De Bardi M, Gasperini C, Borsellino G, Centonze D, Battistini L, Maccarrone M. Distinct modulation of human myeloid and plasmacytoid dendritic cells by anandamide in multiple sclerosis. Ann Neurol. 2013;73:626–636. doi: 10.1002/ana.23875. [DOI] [PubMed] [Google Scholar]
- 56.Liu J, Batkai S, Pacher P, Harvey-White J, Wagner JA, Cravatt BF, Gao B, Kunos G. Lipopolysaccharide induces anandamide synthesis in macrophages via CD14/MAPK/phosphoinositide 3-kinase/NF-kappaB independently of platelet-activating factor. J Biol Chem. 2003;278:45034–45039. doi: 10.1074/jbc.M306062200. [DOI] [PubMed] [Google Scholar]
- 57.Varga K, Wagner JA, Bridgen DT, Kunos G. Platelet- and macrophage-derived endogenous cannabinoids are involved in endotoxin-induced hypotension. FASEB J. 1998;12:1035–1044. doi: 10.1096/fasebj.12.11.1035. [DOI] [PubMed] [Google Scholar]
- 58.Cabral GA, Toney DM, Fischer-Stenger K, Harrison MP, Marciano-Cabral F. Anandamide inhibits macrophage-mediated killing of tumor necrosis factor-sensitive cells. Life Sci. 1995;56:2065–2072. doi: 10.1016/0024-3205(95)00190-h. [DOI] [PubMed] [Google Scholar]
- 59.Coffey RG, Yamamoto Y, Snella E, Pross S. Tetrahydrocannabinol inhibition of macrophage nitric oxide production. Biochem Pharmacol. 1996;52:743–751. doi: 10.1016/0006-2952(96)00356-5. [DOI] [PubMed] [Google Scholar]
- 60.Berdyshev EV, Boichot E, Germain N, Allain N, Anger JP, Lagente V. Influence of fatty acid ethanolamides and delta9-tetrahydrocannabinol on cytokine and arachidonate release by mononuclear cells. Eur J Pharmacol. 1997;330:231–240. doi: 10.1016/s0014-2999(97)01007-8. [DOI] [PubMed] [Google Scholar]
- 61.Gallily R, Breuer A, Mechoulam R. 2-Arachidonylglycerol, an endogenous cannabinoid, inhibits tumor necrosis factor-alpha production in murine macrophages, and in mice. Eur J Pharmacol. 2000;406:R5–R7. doi: 10.1016/s0014-2999(00)00653-1. [DOI] [PubMed] [Google Scholar]
- 62.Chang YH, Lee ST, Lin WW. Effects of cannabinoids on LPS-stimulated inflammatory mediator release from macrophages: involvement of eicosanoids. J Cell Biochem. 2001;81:715–723. doi: 10.1002/jcb.1103. [DOI] [PubMed] [Google Scholar]
- 63.Kishimoto S, Kobayashi Y, Oka S, Gokoh M, Waku K, Sugiura T. 2-Arachidonoylglycerol, an endogenous cannabinoid receptor ligand, induces accelerated production of chemokines in HL-60 cells. J Biochem. 2004;135:517–524. doi: 10.1093/jb/mvh063. [DOI] [PubMed] [Google Scholar]
- 64.Gokoh M, Kishimoto S, Oka S, Mori M, Waku K, Ishima Y, Sugiura T. 2-arachidonoylglycerol, an endogenous cannabinoid receptor ligand, induces rapid actin polymerization in HL-60 cells differentiated into macrophage-like cells. Biochem J. 2005;386:583–589. doi: 10.1042/BJ20041163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gokoh M, Kishimoto S, Oka S, Sugiura T. 2-Arachidonoylglycerol enhances the phagocytosis of opsonized zymosan by HL-60 cells differentiated into macrophage-like cells. Biol Pharm Bull. 2007;30:1199–1205. doi: 10.1248/bpb.30.1199. [DOI] [PubMed] [Google Scholar]
- 66.Hayashi R, Miyazaki M, Osada S, Kawasaki H, Fujita I, Hamasaki Y, Kodama H. A formyl peptide substituted with a conformationally constrained phenylalanine residue evokes a selective immune response in human neutrophils. Bioorg Med Chem. 2013;21:668–675. doi: 10.1016/j.bmc.2012.11.046. [DOI] [PubMed] [Google Scholar]
- 67.Balenga NA, Aflaki E, Kargl J, Platzer W, Schröder R, Blättermann S, Kostenis E, Brown AJ, Heinemann A, Waldhoer M. GPR55 regulates cannabinoid 2 receptor-mediated responses in human neutrophils. Cell Res. 2011;21:1452–1469. doi: 10.1038/cr.2011.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.McHugh D, Tanner C, Mechoulam R, Pertwee RG, Ross RA. Inhibition of human neutrophil chemotaxis by endogenous cannabinoids and phytocannabinoids: evidence for a site distinct from CB1 and CB2. Mol Pharmacol. 2008;73:441–450. doi: 10.1124/mol.107.041863. [DOI] [PubMed] [Google Scholar]
- 69.Montecucco F, Di Marzo V, da Silva RF, Vuilleumier N, Capettini L, Lenglet S, Pagano S, Piscitelli F, Quintao S, Bertolotto M, Pelli G, Galan K, Pilet L, Kuzmanovic K, Burger F, Pane B, Spinella G, Braunersreuther V, Gayet-Ageron A, Pende A, Viviani GL, Palombo D, Dallegri F, Roux-Lombard P, Santos RA, Stergiopulos N, Steffens S, Mach F. The activation of the cannabinoid receptor type 2 reduces neutrophilic protease-mediated vulnerability in atherosclerotic plaques. Eur Heart J. 2012;33:846–856. doi: 10.1093/eurheartj/ehr449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chouinard F, Lefebvre JS, Navarro P, Bouchard L, Ferland C, Lalancette-Hébert M, Marsolais D, Laviolette M, Flamand N. The endocannabinoid 2-arachidonoyl-glycerol activates human neutrophils: critical role of its hydrolysis and de novo leukotriene B4 biosynthesis. J Immunol. 2011;186:3188–3196. doi: 10.4049/jimmunol.1002853. [DOI] [PubMed] [Google Scholar]
- 71.Gasperi V, Evangelista D, Chiurchiù V, Florenzano F, Savini I, Oddi S, Avigliano L, Catani MV, Maccarrone M. 2-Arachidonoylglycerol modulates human endothelial cell/leukocyte interactions by controlling selectin expression through CB1 and CB2 receptors. Int J Biochem Cell Biol. 2014;51:79–88. doi: 10.1016/j.biocel.2014.03.028. [DOI] [PubMed] [Google Scholar]
- 72.Di Filippo C, Rossi F, Rossi S, D’Amico M. Cannabinoid CB2 receptor activation reduces mouse myocardial ischemia–reperfusion injury: involvement of cytokine/chemokines and PMN. J Leukoc Biol. 2004;75:453–459. doi: 10.1189/jlb.0703303. [DOI] [PubMed] [Google Scholar]
- 73.Rajesh M, Pan H, Mukhopadhyay P, Bátkai S, Osei-Hyiaman D, Haskó G, Liaudet L, Gao B, Pacher P. Cannabinoid-2 receptor agonist HU-308 protects against hepatic ischemia/reperfusion injury by attenuating oxidative stress, inflammatory response, and apoptosis. J Leukoc Biol. 2007;82:1382–1389. doi: 10.1189/jlb.0307180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Murikinati S, Juttler E, Keinert T, Ridder DA, Muhammad S, Waibler Z, Ledent C, Zimmer A, Kalinke U, Schwaninger M. Activation of cannabinoid 2 receptors protects against cerebral ischemia by inhibiting neutrophil recruitment. FASEB J. 2010;24:788–798. doi: 10.1096/fj.09-141275. [DOI] [PubMed] [Google Scholar]
- 75.Rom S, Zuluaga-Ramirez V, Dykstra H, Reichenbach NL, Pacher P, Persidsky Y. Selective activation of cannabinoid receptor 2 in leukocytes suppresses their engagement of the brain endothelium and protects the blood-brain barrier. Am J Pathol. 2013;183:1548–1558. doi: 10.1016/j.ajpath.2013.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rajesh M, Mukhopadhyay P, Bátkai S, Haskó G, Liaudet L, Huffman JW, Csiszar A, Ungvari Z, Mackie K, Chatterjee S, Pacher P. CB2-receptor stimulation attenuates TNF-alpha-induced human endothelial cell activation, transendothelial migration of monocytes, and monocyte-endothelial adhesion. Am J Physiol Heart Circ Physiol. 2007;293:H2210–H2218. doi: 10.1152/ajpheart.00688.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ramirez SH, Reichenbach NL, Fan S, Rom S, Merkel SF, Wang X, Ho WZ, Persidsky Y. Attenuation of HIV-1 replication in macrophages by cannabinoid receptor 2 agonists. J Leukoc Biol. 2013;93:801–810. doi: 10.1189/jlb.1012523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Edgemond WS, Hillard CJ, Falck JR, Kearn CS, Campbell WB. Human platelets and polymorphonuclear leukocytes synthesize oxygenated derivatives of arachidonylethanolamide (anandamide): their affinities for cannabinoid receptors and pathways of inactivation. Mol Pharmacol. 1998;54:180–188. doi: 10.1124/mol.54.1.180. [DOI] [PubMed] [Google Scholar]
- 79.Maccarrone M, Bari M, Menichelli A, Del Principe D, Finazzi AA. Anandamide activates human platelets through a pathway independent of the arachidonate cascade. FEBS Lett. 1999;447:277–282. doi: 10.1016/s0014-5793(99)00308-7. [DOI] [PubMed] [Google Scholar]
- 80.Maccarrone M, Bari M, Menichelli A, Giuliani E, Del Principe D, Finazzi-Agrò A. Human platelets bind and degrade 2-arachidonoylglycerol, which activates these cells through a cannabinoid receptor. Eur J Biochem. 2001;268:819–825. doi: 10.1046/j.1432-1327.2001.01942.x. [DOI] [PubMed] [Google Scholar]
- 81.Braud S, Bon C, Touqui L, Mounier C. Activation of rabbit blood platelets by anandamide through its cleavage into arachidonic acid. FEBS Lett. 2000;471:12–16. doi: 10.1016/s0014-5793(00)01359-4. [DOI] [PubMed] [Google Scholar]
- 82.Gkini E, Anagnostopoulos D, Mavri-Vavayianni M, Siafaka-Kapadai A. Metabolism of 2-acylglycerol in rabbit and human platelets. Involvement of monoacylglycerol lipase and fatty acid amide hydrolase. Platelets. 2009;20:376–385. doi: 10.1080/09537100903121813. [DOI] [PubMed] [Google Scholar]
- 83.Maccarrone M, Del Principe D, Finazzi-Agrò A. Endocannabinoids: new physiological (co-)agonists of human platelets. Thromb Haemost. 2002;88:165–166. [PubMed] [Google Scholar]
- 84.Malorni W, Bari M, Straface E, Battista N, Matarrese P, Finazzi-Agrò A, Del Principe D, Maccarrone M. Morphological evidence that 2-arachidonoylglycerol is a true agonist of human platelets. Thromb Haemost. 2004;92:1159–1161. [PubMed] [Google Scholar]
- 85.Baldassarri S, Bertoni A, Bagarotti A, Sarasso C, Zanfa M, Catani MV, Avigliano L, Maccarrone M, Torti M, Sinigaglia F. The endocannabinoid 2-arachidonoylglycerol activates human platelets through non-CB1/CB2 receptors. J Thromb Haemost. 2008;6:1772–1779. doi: 10.1111/j.1538-7836.2008.03093.x. [DOI] [PubMed] [Google Scholar]
- 86.Signorello MG, Giacobbe E, Leoncini G. Activation by 2-arachidonoylglycerol of platelet p38MAPK/cPLA2 pathway. J Cell Biochem. 2011;112:2794–2802. doi: 10.1002/jcb.23194. [DOI] [PubMed] [Google Scholar]
- 87.Signorello MG, Giacobbe E, Segantin A, Avigliano L, Sinigaglia F, Maccarrone M, Leoncini G. Activation of human platelets by 2-arachidonoylglycerol: role of PKC in NO/cGMP pathway modulation. Curr Neurovasc Res. 2011;8:200–209. doi: 10.2174/156720211796558041. [DOI] [PubMed] [Google Scholar]
- 88.Catani MV, Gasperi V, Evangelista D, Finazzi Agrò A, Avigliano L, Maccarrone M. Anandamide extends platelets survival through CB(1)-dependent Akt signalling. Cell Mol Life Sci. 2010;67:601–610. doi: 10.1007/s00018-009-0198-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Signorello MG, Giacobbe E, Passalacqua M, Leoncini G. The anandamide effect on NO/cGMP pathway in human platelets. J Cell Biochem. 2011;112:924–932. doi: 10.1002/jcb.23008. [DOI] [PubMed] [Google Scholar]
- 90.Kunos G, Jarai Z, Batkai S, Goparaju SK, Ishac EJ, Liu J, Wang L, Wagner JA. Endocannabinoids as cardiovascular modulators. Chem Phys Lipids. 2000;108:159–168. doi: 10.1016/s0009-3084(00)00194-8. [DOI] [PubMed] [Google Scholar]
- 91.Maccarrone M, Bari M, Lorenzon T, Bisogno T, Di Marzo V, Finazzi-Agrò A. Anandamide uptake by human endothelial cells and its regulation by nitric oxide. J Biol Chem. 2000;275:13484–13492. doi: 10.1074/jbc.275.18.13484. [DOI] [PubMed] [Google Scholar]
- 92.Keown OP, Winterburn TJ, Wainwright CL, Macrury SM, Neilson I, Barrett F, Leslie SJ, Megson IL. 2-arachidonyl glycerol activates platelets via conversion to arachidonic acid and not by direct activation of cannabinoid receptors. Br J Clin Pharmacol. 2010;70:180–188. doi: 10.1111/j.1365-2125.2010.03697.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Schäfer A, Pfrang J, Neumüller J, Fiedler S, Ertl G, Bauersachs J. The cannabinoid receptor-1 antagonist rimonabant inhibits platelet activation and reduces pro-inflammatory chemokines and leukocytes in Zucker rats. Br J Pharmacol. 2008;154:1047–1054. doi: 10.1038/bjp.2008.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Brantl SA, Khandoga AL, Siess W. Mechanism of platelet activation induced by endocannabinoids in blood and plasma. Platelets. 2014;25:151–161. doi: 10.3109/09537104.2013.803530. [DOI] [PubMed] [Google Scholar]
- 95.Maccarrone M. Activation of platelets by endocannabinoids: distinct agonists or arachidonate reservoirs? Platelets. 2014;25:463–464. doi: 10.3109/09537104.2013.833599. [DOI] [PubMed] [Google Scholar]
- 96.De Angelis V, Koekman AC, Weeterings C, Roest M, de Groot PG, Herczenik E, Maas C. Endocannabinoids control platelet activation and limit aggregate formation under flow. PLoS One. 2014;9:e108282. doi: 10.1371/journal.pone.0108282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Guindon J, Hohmann AG. The endocannabinoid system and cancer: therapeutic implication. Br J Pharmacol. 2011;163:1447–1463. doi: 10.1111/j.1476-5381.2011.01327.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Pisanti S, Picardi P, D’Alessandro A, Laezza C, Bifulco M. The endocannabinoid signaling system in cancer. Trends Pharmacol Sci. 2013;34:273–282. doi: 10.1016/j.tips.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 99.Maccarrone M. Endocannabinoid signaling in cancer: a rather complex puzzle. Trends Pharmacol Sci. 2013;34:426–427. doi: 10.1016/j.tips.2013.06.006. [DOI] [PubMed] [Google Scholar]
- 100.Jordà M, Rayman N, Tas M, Verbakel SE, Battista N, van Lom K, Löwenberg B, Maccarrone M, Delwel R. The peripheral cannabinoid receptor Cb2, frequently expressed on AML blasts, either induces a neutrophilic differentiation block or confers abnormal migration properties in a ligand-dependent manner. Blood. 2004;104:526–534. doi: 10.1182/blood-2003-12-4357. [DOI] [PubMed] [Google Scholar]
- 101.Gustafsson K, Wang X, Severa D, Eriksson M, Kimby E, Merup M, Christensson B, Flygare J, Sander B. Expression of cannabinoid receptors type 1 and type 2 in non-Hodgkin lymphoma: growth inhibition by receptor activation. Int J Cancer. 2008;123:1025–1033. doi: 10.1002/ijc.23584. [DOI] [PubMed] [Google Scholar]
- 102.Rayman N, Lam KH, Van Leeuwen J, Mulder AH, Budel LM, Löwenberg B, Sonneveld P, Delwel R. The expression of the peripheral cannabinoid receptor on cells of the immune system and non-Hodgkin’s lymphomas. Leuk Lymphoma. 2007;48:1389–1399. doi: 10.1080/10428190701377030. [DOI] [PubMed] [Google Scholar]
- 103.Benz AH, Renné C, Maronde E, Koch M, Grabiec U, Kallendrusch S, Rengstl B, Newrzela S, Hartmann S, Hansmann ML, Dehghani F. Expression and functional relevance of cannabinoid receptor 1 in Hodgkin lymphoma. PLoS One. 2013;8:e81675. doi: 10.1371/journal.pone.0081675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Gustafsson K, Christensson B, Sander B, Flygare J. Cannabinoid receptor-mediated apoptosis induced by R(+)-methanandamide and Win 55,212–2 is associated with ceramide accumulation and p38 activation in mantle cell lymphoma. Mol Pharmacol. 2006;70:1612–1620. doi: 10.1124/mol.106.025981. [DOI] [PubMed] [Google Scholar]
- 105.Gustafsson K, Sander B, Bielawski J, Hannun YA, Flygare J. Potentiation of cannabinoid-induced cytotoxicity in mantle cell lymphoma through modulation of ceramide metabolism. Mol Cancer Res. 2009;7:1086–1098. doi: 10.1158/1541-7786.MCR-08-0361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wasik AM, Almestrand S, Wang X, Hultenby K, Dackland ÅL, Andersson P, Kimby E, Christensson B, Sander B. WIN55,212-2 induces cytoplasmic vacuolation in apoptosis-resistant MCL cells. Cell Death Dis. 2011;2:e225. doi: 10.1038/cddis.2011.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gallotta D, Nigro P, Cotugno R, Gazzerro P, Bifulco M, Belisario MA. Rimonabant-induced apoptosis in leukemia cell lines: activation of caspase-dependent and -independent pathways. Biochem Pharmacol. 2010;80:370–380. doi: 10.1016/j.bcp.2010.04.023. [DOI] [PubMed] [Google Scholar]
- 108.Pacher P, Kunos G. Modulating the endocannabinoid system in human health and disease–successes and failures. FEBS J. 2013;280:1918–1943. doi: 10.1111/febs.12260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Skaper SD, Facci L. Mast cell-glia axis in neuroinflammation and therapeutic potential of the anandamide congener palmitoylethanolamide. Philos Trans R Soc Lond B Biol Sci. 2012;367:3312–3325. doi: 10.1098/rstb.2011.0391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zogopoulos P, Vasileiou I, Patsouris E, Theocharis SE. The role of endocannabinoids in pain modulation. Fundam Clin Pharmacol. 2013;27:64–80. doi: 10.1111/fcp.12008. [DOI] [PubMed] [Google Scholar]
- 111.Farquhar-Smith WP, Rice AS. A novel neuroimmune mechanism in cannabinoid-mediated attenuation of nerve growth factor-induced hyperalgesia. Anesthesiology. 2003;99:1391–1401. doi: 10.1097/00000542-200312000-00024. [DOI] [PubMed] [Google Scholar]
- 112.De Filippis D, Luongo L, Cipriano M, Palazzo E, Cinelli MP, de Novellis V, Maione S, Iuvone T. Palmitoylethanolamide reduces granuloma-induced hyperalgesia by modulation of mast cell activation in rats. Mol Pain. 2011;7:3–12. doi: 10.1186/1744-8069-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Endocannabinoid Research Group, De Filippis D, D’Amico A, Cipriano M, Petrosino S, Orlando P, Di Marzo V, Iuvone T Levels of endocannabinoids and palmitoylethanolamide and their pharmacological manipulation in chronic granulomatous inflammation in rats. Pharmacol Res. 2010;61:321–328. doi: 10.1016/j.phrs.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 114.Di Sabatino A, Battista N, Biancheri P, Rapino C, Rovedatti L, Astarita G, Vanoli A, Dainese E, Guerci M, Piomelli D, Pender SL, MacDonald TT, Maccarrone M, Corazza GR. The endogenous cannabinoid system in the gut of patients with inflammatory bowel disease. Mucosal Immunol. 2011;4:574–583. doi: 10.1038/mi.2011.18. [DOI] [PubMed] [Google Scholar]
- 115.Storr MA, Keenan CM, Emmerdinger D, Zhang H, Yüce B, Sibaev A, Massa F, Buckley NE, Lutz B, Göke B, Brand S, Patel KD, Sharkey KA. Targeting endocannabinoid degradation protects against experimental colitis in mice: involvement of CB1 and CB2 receptors. J Mol Med. 2008;86:925–936. doi: 10.1007/s00109-008-0359-6. [DOI] [PubMed] [Google Scholar]
- 116.Singh UP, Singh NP, Singh B, Price RL, Nagarkatti M, Nagarkatti PS. Cannabinoid receptor-2 (CB2) agonist ameliorates colitis in IL-10(−/−) mice by attenuating the activation of T cells and promoting their apoptosis. Toxicol Appl Pharmacol. 2012;258:256–267. doi: 10.1016/j.taap.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kimball ES, Schneider CR, Wallace NH, Hornby PJ. Agonists of cannabinoid receptor 1 and 2 inhibit experimental colitis induced by oil of mustard and by dextran sulfate sodium. Am J Physiol Gastrointest Liver Physiol. 2006;291:G364–G371. doi: 10.1152/ajpgi.00407.2005. [DOI] [PubMed] [Google Scholar]
- 118.D’Argenio G, Petrosino S, Gianfrani C, Valenti M, Scaglione G, Grandone I, Nigam S, Sorrentini I, Mazzarella G, Di Marzo V. Overactivity of the intestinal endocannabinoid system in celiac disease and in methotrexate-treated rats. J Mol Med (Berl) 2007;85:523–530. doi: 10.1007/s00109-007-0192-3. [DOI] [PubMed] [Google Scholar]
- 119.Battista N, Di Sabatino A, Di Tommaso M, Biancheri P, Rapino C, Vidali F, Papadia C, Montana C, Pasini A, Lanzini A, Villanacci V, Corazza GR, Maccarrone M. Abnormal anandamide metabolism in celiac disease. J Nutr Biochem. 2012;23:1245–1248. doi: 10.1016/j.jnutbio.2011.06.017. [DOI] [PubMed] [Google Scholar]
- 120.Battista N, Di Sabatino A, Di Tommaso M, Biancheri P, Rapino C, Giuffrida P, Papadia C, Montana C, Pasini A, Vanoli A, Lanzarotto F, Villanacci V, Corazza GR, Maccarrone M. Altered expression of type-1 and type-2 cannabinoid receptors in celiac disease. PLoS One. 2013;8:e62078. doi: 10.1371/journal.pone.0062078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hoyer FF, Steinmetz M, Zimmer S, Becker A, Lütjohann D, Buchalla R, Zimmer A, Nickenig G. Atheroprotection via cannabinoid receptor-2 is mediated by circulating and vascular cells in vivo. J Mol Cell Cardiol. 2011;51:1007–1014. doi: 10.1016/j.yjmcc.2011.08.008. [DOI] [PubMed] [Google Scholar]
- 122.Willecke F, Zeschky K, Ortiz Rodriguez A, Colberg C, Auwärter V, Kneisel S, Hutter M, Lozhkin A, Hoppe N, Wolf D, von zur Mühlen C, Moser M, Hilgendorf Hilgendorf, Bode C, Zirlik A. Cannabinoid receptor 2 signaling does not modulate atherogenesis in mice. PLoS One. 2011;6:e19405. doi: 10.1371/journal.pone.0019405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Lenglet S, Thomas A, Soehnlein O, Montecucco F, Burger F, Pelli G, Galan K, Cravatt B, Staub C, Steffens S. Fatty acid amide hydrolase deficiency enhances intraplaque neutrophil recruitment in atherosclerotic mice. Arterioscler Thromb Vasc Biol. 2013;33:215–223. doi: 10.1161/ATVBAHA.112.300275. [DOI] [PubMed] [Google Scholar]
- 124.Mukhopadhyay P, Horváth B, Rajesh M, Matsumoto S, Saito K, Bátkai S, Patel V, Tanchian G, Gao RY, Cravatt BF, Haskó G, Pacher P. Fatty acid amide hydrolase is a key regulator of endocannabinoid-induced myocardial tissue injury. Free Radic Biol Med. 2011;50:179–195. doi: 10.1016/j.freeradbiomed.2010.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Jiang LS, Pu J, Han ZH, Hu LH, He B. Role of activated endocannabinoid system in regulation of cellular cholesterol metabolism in macrophages. Cardiovasc Res. 2009;81:805–813. doi: 10.1093/cvr/cvn344. [DOI] [PubMed] [Google Scholar]
- 126.Quercioli A, Pataky Z, Vincenti G, Makoundou V, Di Marzo V, Montecucco F, Carballo S, Thomas A, Staub C, Steffens S, Seimbille Y, Golay A, Ratib O, Harsch E, Mach F, Schindler TH. Elevated endocannabinoid plasma levels are associated with coronary circulatory dysfunction in obesity. Eur Heart J. 2011;32:1369–1378. doi: 10.1093/eurheartj/ehr029. [DOI] [PubMed] [Google Scholar]
- 127.Wang Q, Tang XN, Yenari MA. The inflammatory response in stroke. J Neuroimmunol. 2007;184:53–68. doi: 10.1016/j.jneuroim.2006.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Swardfager W, Winer DA, Herrmann N, Winer S, Lanctôt KL. Interleukin-17 in post-stroke neurodegeneration. Neurosci Biobehav Rev. 2013;37:436–447. doi: 10.1016/j.neubiorev.2013.01.021. [DOI] [PubMed] [Google Scholar]
- 129.van der Spuy WJ, Pretorius E. Interrelation between inflammation, thrombosis, and neuroprotection in cerebral ischemia. Rev Neurosci. 2012;23:269–278. doi: 10.1515/revneuro-2012-0028. [DOI] [PubMed] [Google Scholar]
- 130.Zarruk JG, Fernandez-Lopez D, Garcia-Yebenes I, García-Gutiérrez MS, Vivancos J, Nombela F, Torres M, Burguete MC, Manzanares J, Lizasoain I, Moro MA. Cannabinoid type 2 receptor activation downregulates stroke-induced classic and alternative brain macrophage/microglial activation concomitant to neuroprotection. Stroke. 2012;43:211–219. doi: 10.1161/STROKEAHA.111.631044. [DOI] [PubMed] [Google Scholar]
- 131.Zhang M, Martin BR, Adler MW, Razdan RK, Jallo JI, Tuma RF. Cannabinoid CB(2) receptor activation decreases cerebral infarction in a mouse focal ischemia/reperfusion model. J Cereb Blood Flow Metab. 2007;27:1387–1396. doi: 10.1038/sj.jcbfm.9600447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Zhang M, Adler MW, Abood ME, Ganea D, Jallo J, Tuma RF. CB2 receptor activation attenuates microcirculatory dysfunction during cerebral ischemic/reperfusion injury. Microvasc Res. 2009;78:86–94. doi: 10.1016/j.mvr.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Batkai S, Osei-Hyiaman D, Pan H, El-Assal O, Rajesh M, Mukhopadhyay P, Hong F, Harvey-White J, Jafri A, Haskó G, Huffman JW, Gao B, Kunos G, Pacher P. Cannabinoid-2 receptor mediates protection against hepatic ischemia/reperfusion injury. FASEB J. 2007;21:1788–1800. doi: 10.1096/fj.06-7451com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Mukhopadhyay P, Rajesh M, Horváth B, Bátkai S, Park O, Tanchian G, Gao RY, Patel V, Wink DA, Liaudet L, Haskó G, Mechoulam R, Pacher P. Cannabidiol protects against hepatic ischemia/reperfusion injury by attenuating inflammatory signalling and response, oxidative/nitrative stress, and cell death. Free Radic Biol Med. 2011;50:1368–1381. doi: 10.1016/j.freeradbiomed.2011.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Centonze D, Battistini L, Maccarrone M. The endocannabinoid system in peripheral lymphocytes as a mirror of neuroinflammatory diseases. Curr Pharm Des. 2008;14:2342–2370. doi: 10.2174/138161208785740018. [DOI] [PubMed] [Google Scholar]
- 136.Battista N, Bari M, Tarditi A, Mariotti C, Bachoud-Lévi AC, Zuccato C, Finazzi-Agrò A, Genitrini S, Peschanski M, Di Donato S, Cattaneo E, Maccarrone M. Severe deficiency of the fatty acid amide hydrolase (FAAH) activity segregates with the Huntington’s disease mutation in peripheral lymphocytes. Neurobiol Dis. 2007;27:108–116. doi: 10.1016/j.nbd.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 137.Centonze D, Bari M, Rossi S, Prosperetti C, Furlan R, Fezza F, De Chiara V, Battistini L, Bernardi G, Bernardini S, Martino G, Maccarrone M. The endocannabinoid system is dysregulated in multiple sclerosis and in experimental autoimmune encephalomyelitis. Brain. 2007;130:2543–2553. doi: 10.1093/brain/awm160. [DOI] [PubMed] [Google Scholar]
- 138.Eljaschewitsch E, Witting A, Mawrin C, Lee T, Schmidt PM, Wolf S, Hoertnagl H, Raine CS, Schneider-Stock R, Nitsch R, Ullrich O. The endocannabinoid anandamide protects neurons during CNS inflammation by induction of MKP-1 in microglial cells. Neuron. 2006;49:67–79. doi: 10.1016/j.neuron.2005.11.027. [DOI] [PubMed] [Google Scholar]
- 139.Benito C, Romero JP, Tolón RM, Clemente D, Docagne F, Hillard CJ, Guaza C, Romero J. Cannabinoid CB1 and CB2 receptors and fatty acid amide hydrolase are specific markers of plaque cell subtypes in human multiple sclerosis. J Neurosci. 2007;27:2396–2402. doi: 10.1523/JNEUROSCI.4814-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Sánchez López AJ, Román-Vega L, Ramil Tojeiro E, Giuffrida A, García-Merino A. Regulation of cannabinoid receptor gene expression and endocannabinoid levels in lymphocyte subsets by IFN-β: a longitudinal study in multiple sclerosis patients. Clin Exp Immunol. 2015;179:119–127. doi: 10.1111/cei.12443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Hernangómez M, Mestre L, Correa FG, Loría F, Mecha M, Iñigo PM, Docagne F, Williams RO, Borrell J, Guaza C. CD200-CD200R1 interaction contributes to neuroprotective effects of anandamide on experimentally induced inflammation. Glia. 2012;60:1437–1450. doi: 10.1002/glia.22366. [DOI] [PubMed] [Google Scholar]
- 142.Correa F, Hernangómez-Herrero M, Mestre L, Loría F, Docagne F, Guaza C. The endocannabinoid anandamide downregulates IL-23 and IL-12 subunits in a viral model of multiple sclerosis: evidence for a cross-talk between IL-12p70/IL-23 axis and IL-10 in microglial cells. Brain Behav Immun. 2011;25:736–749. doi: 10.1016/j.bbi.2011.01.020. [DOI] [PubMed] [Google Scholar]
- 143.Pisani A, Fezza F, Galati S, Battista N, Napolitano S, Finazzi-Agrò A, Bernardi G, Brusa L, Pierantozzi M, Stanzione P, Maccarrone M. High endogenous cannabinoid levels in the cerebrospinal fluid of untreated Parkinson’s disease patients. Ann Neurol. 2005;57:777–779. doi: 10.1002/ana.20462. [DOI] [PubMed] [Google Scholar]
- 144.D’Addario C, Di Francesco A, Arosio BC, Dell’Osso B, Bari M, Galimberti D, Scarpini E, Altamura AC, Mari D, Maccarrone M. Epigenetic regulation of fatty acid amide hydrolase in Alzheimer disease. PLoS One. 2012;7:e39186. doi: 10.1371/journal.pone.0039186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Centonze D, Bari M, Di Michele B, Rossi S, Gasperi V, Pasini A, Battista N, Bernardi G, Curatolo P, Maccarrone M. Altered anandamide degradation in attention-deficit/hyperactivity disorder. Neurology. 2009;72:1526–1527. doi: 10.1212/WNL.0b013e3181a2e8f6. [DOI] [PubMed] [Google Scholar]
- 146.Ho WSV, Hill MN, Miller GE, Gorzalka BB, Hillard CJ. Serum contents of endocannabinoids are correlated with blood pressure in depressed women. Lipids Health Dis. 2012;11:32–41. doi: 10.1186/1476-511X-11-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Leweke FM, Piomelli D, Pahlisch F, Muhl D, Gerth CW, Hoyer C, Klosterkötter J, Hellmich M, Koethe D. Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Transl Psychiatry. 2012;2:e94. doi: 10.1038/tp.2012.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Siniscalco D, Sapone A, Giordano C, Cirillo A, de Magistris L, Rossi F, Fasano A, Bradstreet JJ, Maione S, Antonucci N. Cannabinoid receptor type 2, but not type 1, is up-regulated in peripheral blood mononuclear cells of children affected by autistic disorders. J Autism Dev Disord. 2013;11:2686–2695. doi: 10.1007/s10803-013-1824-9. [DOI] [PubMed] [Google Scholar]
- 149.Siniscalco D, Bradstreet JJ, Cirillo A, Antonucci N. The in vitro GcMAF effects on endocannabinoid system transcriptionomics, receptor formation, and cell activity of autism-derived macrophages. J Neuroinflammation. 2014;11:78–89. doi: 10.1186/1742-2094-11-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Cupini LM, Bari M, Battista N, Argiro G, Finazzi-Agro A, Calabresi P, Maccarrone M. Biochemical changes in endocannabinoid system are expressed in platelets of female but not male migraineurs. Cephalalgia. 2006;26:277–281. doi: 10.1111/j.1468-2982.2005.01031.x. [DOI] [PubMed] [Google Scholar]
- 151.Cupini LM, Costa C, Sarchielli P, Bari M, Battista N, Eusebi P, Calabresi P, Maccarrone M. Degradation of endocannabinoids in chronic migraine and medication overuse headache. Neurobiol Dis. 2008;30:186–189. doi: 10.1016/j.nbd.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 152.Perrotta A, Arce-Leal N, Tassorelli C, Gasperi V, Sances G, Blandini F, Serrao M, Bolla M, Pierelli F, Nappi G, Maccarrone M, Sandrini G. Acute reduction of anandamide-hydrolase (FAAH) activity is coupled with a reduction of nociceptive pathways facilitation in medication-overuse headache subjects after withdrawal treatment. Headache. 2012;52:1350–1361. doi: 10.1111/j.1526-4610.2012.02170.x. [DOI] [PubMed] [Google Scholar]
- 153.Rossi C, Pini LA, Cupini ML, Calabresi P, Sarchielli P. Endocannabinoids in platelets of chronic migraine patients and medication-overuse headache patients: relation with serotonin levels. Eur J Clin Pharmacol. 2008;64:1–8. doi: 10.1007/s00228-007-0391-4. [DOI] [PubMed] [Google Scholar]
- 154.Greineisen WE, Turner H. Immunoactive effects of cannabinoids: considerations for the therapeutic use of cannabinoid receptor agonists and antagonists. Int Immunopharmacol. 2010;10:547–555. doi: 10.1016/j.intimp.2010.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Cridge BJ, Rosengren RJ. Critical appraisal of the potential use of cannabinoids in cancer management. Cancer Manag Res. 2013;5:301–313. doi: 10.2147/CMAR.S36105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Steffens S, Pacher P. Targeting cannabinoid receptor CB(2) in cardiovascular disorders: promises and controversies. Br J Pharmacol. 2012;167:313–323. doi: 10.1111/j.1476-5381.2012.02042.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Fulp A, Bortoff K, Seltzman H, Zhang Y, Mathews J, Snyder R, Fennell T, Maitra R. Design and synthesis of cannabinoid receptor 1 antagonists for peripheral selectivity. J Med Chem. 2012;55:2820–2834. doi: 10.1021/jm201731z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Sardinha J, Kelly ME, Zhou J, Lehmann C. Experimental cannabinoid 2receptor-mediated immune modulation in sepsis. Mediators Inflamm. 2014;2014:978678. doi: 10.1155/2014/978678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Barutta F, Piscitelli F, Pinach S, Bruno G, Gambino R, Rastaldi MP, Salvidio G, Di Marzo V, Cavallo Perin P, Gruden G. Protective role of cannabinoid receptor type 2 in a mouse model of diabetic nephropathy. Diabetes. 2011;60:2386–2396. doi: 10.2337/db10-1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Samson MT, Small-Howard A, Shimoda LM, Koblan-Huberson M, Stokes AJ, Turner H. Differential roles of CB1 and CB2 cannabinoid receptors in mast cells. J Immunol. 2003;170:4953–4962. doi: 10.4049/jimmunol.170.10.4953. [DOI] [PubMed] [Google Scholar]
- 161.Sewell RA, Ranganathan M, D’Souza DC. Cannabinoids and psychosis. Int Rev Psychiatry. 2000;21:152–162. doi: 10.1080/09540260902782802. [DOI] [PubMed] [Google Scholar]
- 162.Hall W, Degenhardt L. Cannabis use and the risk of developing a psychotic disorder. World Psychiatry. 2008;7:68–71. doi: 10.1002/j.2051-5545.2008.tb00158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Pratap B, Korniyenko A. Toxic effects of marijuana on the cardiovascular system. Cardiovasc Toxicol. 2012;12:143–148. doi: 10.1007/s12012-011-9150-y. [DOI] [PubMed] [Google Scholar]
- 164.Mir A, Obafemi A, Young A, Kane C. Myocardial infarction associated with use of the synthetic cannabinoid K2. Pediatrics. 2011;128:e1622–e1627. doi: 10.1542/peds.2010-3823. [DOI] [PubMed] [Google Scholar]
- 165.Abrams DI, Hilton JF, Leiser RJ, Shade SB, Elbeik TA, Aweeka FT, Benowitz NL, Bredt BM, Kosel B, Aberg JA, Deeks SG, Mitchell TF, Mulligan K, Bacchetti P, McCune JM, Schambelan M. Short-term effects of cannabinoids in patients with HIV-1 infection: a randomized, placebo-controlled clinical trial. Ann Intern Med. 2003;139:258–266. doi: 10.7326/0003-4819-139-4-200308190-00008. [DOI] [PubMed] [Google Scholar]
- 166.Pacifici R, Zuccaro P, Pichini S, Roset PN, Poudevida S, Farrè M, Segura J, De la Torre R. Modulation of the immune system in cannabis users. JAMA. 2003;289:1929–1931. doi: 10.1001/jama.289.15.1929-b. [DOI] [PubMed] [Google Scholar]