Abstract
The field of pancreas development has markedly expanded over the last decade, significantly advancing our understanding of the molecular mechanisms that control pancreas organogenesis. This growth has been fueled, in part, by the need to generate new therapeutic approaches for the treatment of diabetes. The creation of sophisticated genetic tools in mice has been instrumental in this progress. Genetic manipulation involving activation or inactivation of genes within specific cell types has allowed the identification of many transcription factors (TFs) that play critical roles in the organogenesis of the pancreas. Interestingly, many of these TFs act at multiple stages of pancreatic development, and adult organ function or repair. Interaction with other TFs, extrinsic signals, and epigenetic regulation are among the mechanisms by which TFs may play context-dependent roles during pancreas organogenesis. Many of the pancreatic TFs directly regulate each other and their own expression. These combinatorial interactions generate very specific gene regulatory networks that can define the different cell lineages and types in the developing pancreas. Here, we review recent progress made in understanding the role of pancreatic TFs in mouse pancreas formation. We also summarize our current knowledge of human pancreas development and discuss developmental pancreatic TFs that have been associated with human pancreatic diseases.
Keywords: Embryonic pancreas, Transcriptional regulation, Multipotent pancreatic progenitor cells, GATA factors
Pancreas development overview
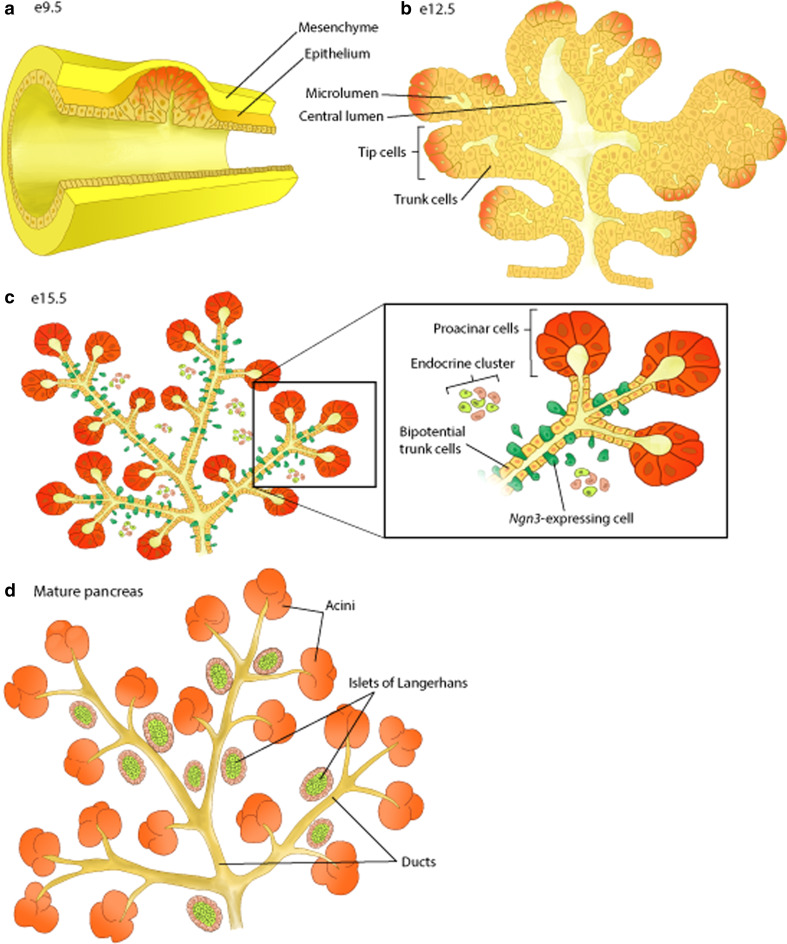
The mammalian pancreas is a mixed exocrine and endocrine organ that plays a critical role in glucose homeostasis and nutrient digestion. The exocrine compartment consists of acinar cells that produce and secrete digestive enzymes into networks of ductal cells. The endocrine portion is comprised of at least five distinct hormone-producing cell types organized into the islets of Langerhans. These include glucagon-producing α-cells, insulin-producing β-cells, somatostatin-producing δ-cells, pancreatic polypeptide-producing PP-cells, and ghrelin-producing ε-cells. The pancreas, like the other organs of the gastrointestinal tract, is derived from the endodermal germ layer during gastrulation. The morphological processes involved in the development of the pancreas have been well characterized in mice. The pancreas arises from two independent primordia (dorsal and ventral) of the foregut epithelium around 8.5–9 days of gestation (e8.5–9) in the mouse [1]. The pancreatic epithelium invades the surrounding mesenchyme and subsequently expands and branches, forming a multilayered, stratified epithelium (Fig. 1). This early pancreatic epithelium contains multipotent pancreatic progenitor cells (MPCs) with the potential to give rise to all pancreatic cell types. Around e11.5–e12.5, the dorsal and ventral buds fuse when stomach and duodenum move during the rotation of the gut. At this time, a dramatic morphogenetic reorganization begins in the pancreatic epithelium that appears to be intimately connected to the formation of two distinct cellular domains. The epithelial “tips” of the branching epithelium contain MPCs while the “trunk” region harbors cells that will give rise to islet and ductal cells [2]. By e13.5, “tip” cells lose their multipotency and become acinar progenitor cells. This marks the beginning of the period known as the “secondary transition” (e13.5–e15.5), in which extensive endocrine and exocrine cell differentiation occurs. After the secondary transition, the differentiated pancreatic cells undergo further growth and differentiation. This period is marked by the extensive proliferation of acinar cells and the organization of endocrine cells into clusters. During postnatal development, endocrine cells coalesce, forming the distinctive islet architecture. The embryonic formation of the pancreas is controlled by precisely timed signaling events, which determine the chronology of activation and repression of transcriptional networks. The signaling pathways that mediate pancreatic development have been reviewed recently in a comprehensive manner [3–8] and will only be briefly discussed throughout the subsequent sections of the present review.
Fig. 1.
Overview of pancreatic organogenesis in mice. a Formation of the pancreatic bud starts at approximately embryonic day (E) 9.5. b At E12.5, the pancreatic epithelium undergoes a marked process of expansion and branching. Segregation of tip (proacinar) and trunk (ductal/endocrine) domains begins. c At e14.5, cells located at the tips of the pancreatic epithelium differentiate into acinar cells. Ngn3-expressing endocrine precursors delaminate and migrate away from the trunk epithelium to form endocrine clusters. d In the mature pancreas, three cell types are found: acinar, ductal, and endocrine cells. Endocrine cells form clusters termed islets of Langerhans
Transcriptional regulation of major morphogenetic processes in pancreas development
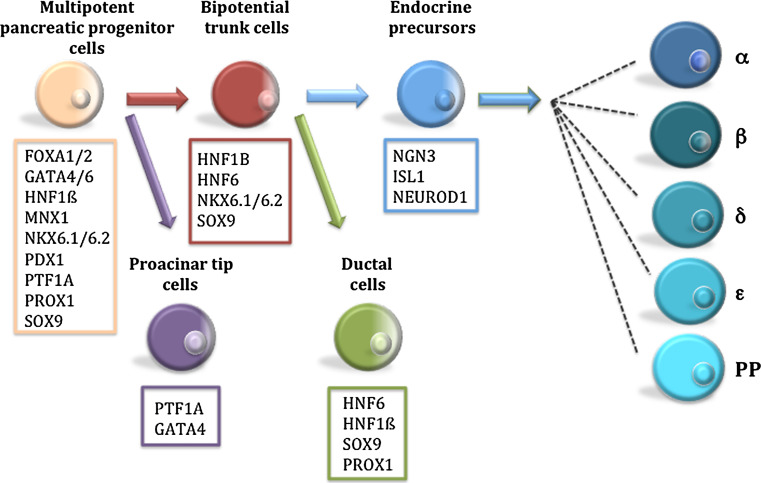
In recent years, the number of TFs that have been implicated in pancreas formation has grown significantly. The purpose of this review is to summarize recent data regarding the TFs mediating pancreas formation. It does not aim to provide an exhaustive compilation of these TFs. Indeed, any attempt to generate a comprehensive list of TFs expressed during pancreas development would be futile, particularly given the vast array of information publicly available from gene expression profiling studies. Rather, we highlight TFs with recently discovered roles in pancreas organogenesis. For purposes of simplicity, we divide the development of the pancreas into four major stages: pancreas specification, pancreatic budding and formation of the multipotent progenitor cell (MPC) population, onset of exocrine and islet development, and endocrine and exocrine differentiation. We will review the specific functions of TFs at each of these developmental stages (Fig. 2). Emphasis will be placed on TFs involved in MPC formation due to the significant advances made in this area in recent years. We also attempt to incorporate information on how TFs are regulated by embryonic signaling pathways at the different developmental stages.
Fig. 2.
Key transcription factors governing lineage decisions during pancreas development
Specification of pancreas in the developing foregut endoderm
After the early patterning of the endoderm, factors secreted from the surrounding mesoderm establish the different organ domains in the primitive gut tube (see [9] for a comprehensive review). Each pancreatic bud receives distinct signals from their adjacent mesodermal tissues. Thus, signals secreted from the lateral plate mesoderm (retinoic acid) and notochord (fibroblast growth factor 2, FGF2, and activin) are essential for the development of the dorsal pancreas while FGF and bone morphogenetic protein (BMP) signaling from the cardiac mesoderm control liver/ventral pancreas fate specification (ventral pancreas being the default program). These signals activate transcription factors specific to each organ domain (for a review, see [10]).
The pancreatic domain in the primitive gut tube is defined by the overlapping expression of Pdx1 (pancreatic and duodenal homeobox 1) and Ptf1a (pancreas-specific transcription factor 1a) [11, 12]. PDX1 and PTF1A are arguably the most important (and most intensely studied) TFs in pancreatic development and both perform multiples roles at different stages of pancreas formation and in the adult organ. Pdx1 is first expressed in the primitive gut tube at e8.5, prior to any apparent morphological changes, thus demarcating the prepancreatic endoderm. However, by e10.5, Pdx1 is also expressed in the posterior stomach, duodenum, and bile duct [13–15]. Pdx1 expression becomes restricted mostly to endocrine cells just before birth in the pancreas [13, 14, 16]. At these stages, Pdx1 expression is also observed in epithelium and Brunner’s glands of the duodenum and pyloric glands of the distal stomach [13, 14, 16, 17]. Ptf1a is first expressed in the pancreatic epithelium at e9.5. By e13.5, its expression is restricted to acinar precursor cells. In contrast to Pdx1, Ptf1a expression is exclusive to the pancreas during development [12]. Interestingly, although Pdx1 and Ptf1a are expressed early in the prepancreatic endoderm and play critical roles in pancreatic development, their function is not critical for pancreas specification. Both Pdx1 and Ptf1a null mice display pancreas agenesis [12, 14, 18]. However, a pancreatic rudiment is still present, indicating that activation of the pancreatic genetic program can occur in the absence of either TF. Based on the specific expression pattern of Pdx1 and Ptf1 in the developing foregut, it has been hypothesized that their combined expression determines the commitment toward a pancreatic fate [19]. However, a recent study has shown that an early pancreatic bud is still formed in mice with simultaneous inactivation of Pdx1 and Ptf1a [20].
Considerable effort has been devoted to the elucidation of the TF mechanisms controlling Pdx1 expression during the early stages of pancreas specification. Several conserved regulatory regions in the Pdx1 promoter have been identified. Areas I–III direct Pdx1 expression in the early pancreas [21, 22], areas I and II impart endocrine expression, and area III confers transient, specific ß-cell expression [23]. Earlier work identified HNF6 and FOXA2 as direct regulators of Pdx1 expression through binding to areas I–III, but these TFs do not appear to be necessary for early pancreas formation [24, 25]. More recently, a redundant role for two members of the GATA family of TFs, GATA4 and GATA6, in activating Pdx1 expression has been reported. Double Gata4/Gata6 mutant mice exhibit severe pancreas agenesis and Pdx1 expression is reduced in multipotent pancreatic progenitors [26, 27] (discussed below). Furthermore, studies with transgenic mice identified two conserved GATA sites in area III of the Pdx1 regulatory sequence [26], a region required for Pdx1 expression in the early pancreatic bud. However, depletion of Gata4 and Gata6 in the early endoderm (prior to pancreas formation) does not impair initial formation of the pancreatic bud [27]. These results indicate that GATA4 and GATA6 function are not required for initial pancreas specification. Other TFs with a role in pancreas formation, such as motor neuron and pancreas homeobox 1 (Mnx1), hematopoietically expressed Homeobox (Hhex), hepatocyte nuclear factor-1-beta (Hnf1b), and the SRY-box containing HMG transcription factor Sox17, are also expressed in the endoderm before Pdx1. It has not been determined whether any of these can directly regulate Pdx1 expression, however. Strikingly, these TFs whose expression precedes Pdx1 activation are widely expressed in the early endoderm [10]. How these TFs might activate the expression of Pdx1 specifically in the prepancreatic endoderm remains unclear. However, it is likely that they act in a cooperative manner, perhaps with additional, undiscovered endodermal TFs. Indeed, the emerging picture in the field is that foregut organ specification is not achieved by activation of individual, organ-specific TFs, but rather through a particular combination of TFs [10]. Evidence for this hypothesis was provided in a recent study that performed a dynamic expression survey of 15 TFs important for endodermal organ formation in the developing foregut [28]. This analysis identified over a dozen specific domains of TFs expression that correspond to different organs of the gastrointestinal system. Another good example of how combinations of TFs can specify different lineages in the endoderm was presented in the recent study by Spence and colleagues [29]. These authors showed that combined expression of Pdx1 and Sox17, a master regulator of endoderm formation [30], define the pancreatobiliary boundary in the ventral posterior foregut. Deletion of Sox17 at e8.5 results in the loss of biliary structures and ectopic pancreas formation in the common duct, whereas Sox17 overexpression suppresses pancreas formation and induces ectopic biliary tissue [29]. Additional research is required to comprehensively establish the combinatorial patterns of TFs that define the pancreatic domain in early endoderm.
Although the key TFs that pattern the foregut endoderm have been identified, much remains to be learned about how these TFs transduce mesodermal signals into specific gene expression programs. For example, a number of secreted factors, including RA and VEGF, are known to influence Pdx1 expression [8, 31]. However, little is known about how these signals are actually translated into Pdx1-activation in the early endoderm. This is an important focus for future investigation; the knowledge generated will undoubtedly contribute to optimization of current protocols to generate insulin-producing cells from embryonic stem cells (ESC). Epigenetic mechanisms might also play an important role in pancreas fate choice during endoderm development. A recent study has found distinct histone modifications at liver and pancreas regulatory elements in the early foregut endoderm [32]. Furthermore, deletion in the foregut endoderm of the histone methyltransferase, Ezh2, leads to a marked expansion of the ventral pancreatic bud at the expense of liver bud development [32]. These results indicate that histone modifiers dictate the fate choice for liver or ventral pancreas induction. It would be interesting to determine whether a similar epigenetic mechanism also controls dorsal pancreas induction.
Pancreatic budding and formation of the MPC population
Following bud formation, the pancreatic epithelium significantly expands and branches. A detailed description of the pancreatic branching process has recently been reported [33, 34]. These studies have provided a novel mechanism for pancreatic branching, which involves transient epithelial stratification and partial loss of cell polarity, de novo tubulogenesis, as well as microlumen formation and fusion. The early pancreatic bud (e9.5–e12.5) is mainly comprised of undifferentiated cells, known as multipotent pancreatic progenitor cells (MPCs). However, whether MPCs at these early stages represent a homogeneous population remains to be determined. Single cell transcript analysis and colocalization experiments with progenitor markers do, indeed, suggest MPC heterogeneity as early as e10.5 [11, 35, 36]. Clonogenic assays of MPCs, such as those recently described by Sugiyama and colleagues [37], combined with a comprehensive molecular characterization of MPCs, will help shed light on this issue. Lineage-tracing studies have demonstrated that MPCs retain the potential to give rise to all three pancreatic lineages until e12.5 [2, 12, 38–41]. However, a similar study has challenged this notion, as lineage analysis of cells expressing the TF Sox9 (discussed below) were shown to contribute to acinar, ductal and endocrine cell compartments between e13.5 and birth [42]. Although this study suggests that MPCs might exist in the fetal pancreas beyond e12.5, experiments using conditional ablation of progenitor cells have demonstrated that the final pancreas size is determined by the number of MPCs present between e9.5 and e12.5 [43]. Thus, this period is a critical developmental window for progenitor expansion and significant efforts have been made to identify mesenchymal factors that control this process. These include, among others, Notch, FGF, and Wnt signaling pathways. Notch signaling inhibits differentiation of the MPC population whereas FGF signaling (namely the FGF10/FGFR2b ligand-receptor pair) [44] and Wnt signaling promote the expansion of the progenitor pool [45, 46].
The number of TFs shown to be critical for MPC formation has grown considerably in the last few years. These include PDX1, PTF1A, SOX9, FOXA1/2, PROX1, MNX1, ONECUT1, HNF1β, and GATA4/6. Next, we will review the roles of these TFs in the formation and maintenance of MPCs, highlighting the reported interactions.
PDX1
As described above, germ-line inactivation of Pdx1 causes pancreas agenesis. Initial budding of the pancreas is seen in these mutants, but growth of the pancreatic epithelium is arrested around e10.5 [14, 15, 18]. These observations, along with experiments involving temporally controlled inactivation of Pdx1 during pancreatic development [47, 48], indicate that PDX1 is necessary for epithelial growth and branching morphogenesis. How PDX1 regulates progenitor expansion remains poorly understood, but it might involve regulation of other TFs known to be involved in MPC formation and maintenance. In agreement with this notion, microarray analyses performed on e10.5 Pdx1 mutant embryos found downregulation of several TFs expressed in MPCs, including Nkx6.1 and Ptf1a [49]. In addition, a modest decrease in Sox9 expression has been observed in Pdx1 mutant mice [50]. However, whether PDX1 directly regulates these TFs has not yet been confirmed. It is remarkable that few direct PDX1 targets at this stage have been described. Two recent studies have identified a direct regulation of Gata4, Foxa2, and Hnf1b by PDX1 at early stages of pancreas formation. Experiments performed in transgenic mice have shown that PDX/HOX sites in an enhancer of the TF Gata4 are required for enhancer function in vivo at e10.5 [51]. Chromatin immunoprecipitation (ChIP) assays using chromatin from wild-type pancreata at later stages of pancreatic development (e13.5) have demonstrated that PDX1 directly occupies sequences in both Hnf1b and Foxa2 genes [52]. Interestingly, and as discussed in the earlier section about pancreas specification, many of the TFs expressed in MPCs including FOXA2, GATA4, HNF6, and PTF1A also directly regulate Pdx1 expression in the early pancreatic bud.
PTF1A
Loss of Ptf1a results in pancreas agenesis although a rudimentary dorsal bud is present. Lineage-tracing experiments have shown that Ptf1a-deficient cells adopt an intestinal or common bile duct fate [12]. These results suggest that PTF1A is essential for the commitment and proliferation of pancreatic progenitors. It has been suggested that FGF10 signaling from the mesenchyme cells maintains Ptf1a expression in the dorsal pancreatic bud [53] but the underlying mechanism is unclear. PTF1A is the only bHLH TF that requires a third DNA-binding subunit for transcriptional activity called RBP-J [54]. The formation of the complex PTF1A-RBP-J is essential for proper pancreatic development. Mutations in one of the motifs of PTF1A that impairs the incorporation of RBPJ (but not the Rbpj homolog Rbpjl that appears to act with PTF1A in later stages of exocrine cell development) into the complex causes pancreatic phenotypes similar to those observed in Ptf1a null mice [55]. Notably, RBPJ function in the PTF1A complex is independent of its role as the effector of Notch signaling [54]. A recent study has identified a significant number of direct targets of PTF1A in pancreatic progenitors [56]. Remarkably, several of these targets are TFs that are also expressed in the MPC population such as Pdx1 (confirming previous results [22]), Nkx6.1, Hnf6, and Mnx1. It is also important to note that Ptf1a maintains its own expression during pancreatic development [57].
SOX9
Sox9, a member of the SRY/HMG box family, is expressed in the Pdx1 domain from e9.5 [58, 59]. Lineage-tracing experiments have shown that at this stage Sox9-expressing cells give rise to all pancreatic cell types [58]. During the secondary transition, Sox9 expression becomes restricted to the trunk ductal/endocrine progenitor domain. At later stages of pancreas development, Sox9 expression is maintained in ductal cells. Conditional inactivation of Sox9 in the Pdx1 domain results in severe pancreatic hypoplasia [58] due to both diminished MPC proliferation and increased MPC cell death. In addition to MPC proliferation and survival, SOX9 is required to maintain MPC identity through a mechanism mediated by mesenchymal FGF signaling [50]. SOX9 regulates fibroblast growth factor receptor 2b (Fgfr2b) expression in the pancreatic epithelium, which is required to transduce mesenchymal FGF10 signals. In turn, FGF10 is required to maintain expression of Sox9 and Fgfr2b. Thus, SOX9 and FGF10-FGFGR2b form a feed-forward loop in the MPC population that maintains pancreas identity. Disruption of this loop results in activation of the liver developmental program in the pancreatic epithelium [50]. SOX9 directly regulates the expression of other TFs expressed in MPCs, such as Hnf1b, Hnf6, and FoxA2 suggesting a central role for SOX9 in the transcriptional network controlling MPC formation and maintenance [59].
GATA factors
The GATA transcription factor family is composed of six zinc finger TFs that play important roles in the specification and differentiation of multiple cell types [60–62]. All members of the GATA family recognize the motif WGATAR in the regulatory sequences of the target genes. In the mouse embryo, the expression pattern of Gata4 and Gata6 overlaps in the foregut endoderm, including the prepancreatic endoderm [61]. As embryonic development proceeds, Gata4 and Gata6 expression become mutually exclusive. Gata4 is expressed in acinar cells, whereas Gata6 expression is restricted to endocrine islets [63]. Earlier work performed in Gata4 and Gata6 tetraploid embryos, has suggested a role for these TFs in ventral bud formation. More recently, two studies have established a critical regulatory role for GATA4 and GATA6 in pancreas formation. While the inactivation of either Gata4 or Gata6 does not impair pancreas formation, inactivation of both Gata4 and Gata6 in the pancreatic progenitor domain leads to pancreatic agenesis, indicating a functional redundancy for these TFs during pancreas formation [26, 27]. Gata4/Gata6 mutant embryos exhibit defects in MPC proliferation and branching morphogenesis. Furthermore, cell commitment toward endocrine and exocrine lineages is also severely impaired. As discussed in the previous section, GATA factors directly regulate Pdx1 expression [26]. Therefore, it is possible that some of the defects observed in Gata4/Gata6 pancreata might be due to diminished Pdx1 expression. It would be interesting to determine whether GATA factors also directly regulate the expression of other TFs critical for the formation of the MPC population.
HNF1β
Hnf1b is expressed in the foregut endoderm prior to Pdx1 (E8) [64]. During the secondary restriction, its expression is restricted to the epithelial trunk domain. At later stages, Hnf1b expression is observed only in the exocrine ducts [65, 66]. Lineage-tracing studies have shown that Hnf1b-expressing cells can give rise to all three pancreatic lineages until e13.5 [39]. Hnf1b mutants display a severely reduced dorsal pancreatic bud combined with complete absence of the ventral bud, a phenotype reminiscent of that observed in Ptf1a mutants. Indeed, Ptf1a is not expressed in the Hnf1b pancreatic bud rudiment, suggesting that PTF1A is downstream of HNF1β [66].
HNF6
Hnf6 is first expressed at e8.5 in the foregut-midgut region of the endoderm. It is broadly expressed within the pancreatic epithelium at early stages of pancreas formation, but becomes restricted to ductal and acinar cells prior to birth [65, 67]. Global Hnf6 null mice exhibit pancreas hypoplasia with reduced Pdx1 expression [24]. More recently, it was reported that inactivation of the Hnf6 gene in Pdx1 expression domain mice results in defects in pancreatic epithelial branching and growth [67]. HNF1β regulates Hnf6 expression in the prepancreatic endoderm, which has led to the hypothesis that the sequential activation of Hnf1b, Hnf6, and Pdx1 in the endoderm might control the generation of pancreatic progenitors [68].
MNX1
The Motor neuron and pancreas homeobox protein (Mnx1) is expressed throughout the primitive gut endoderm at e8 [69, 70]. Mnx1 forms a transient dorsal–ventral gradient at e9.5 [28]. This Mnx1 expression rapidly disappears from the pancreatic epithelium by e12.5 [71]. Interestingly, Mnx1 later becomes expressed in adult ß-cells [69, 70]. Mnx1-deficient embryos display agenesis of the dorsal pancreas, whereas the ventral bud is normally formed.
PROX1
The Prospero-related homeobox transcription factor1 (Prox1) is expressed in the prepancreatic endoderm. It is broadly expressed in the early pancreatic progenitor domain but becomes restricted to ductal and endocrine cells by e15.5 [72]. Prox1 mutant embryos exhibit premature acinar cell differentiation and defects in pancreatic epithelial branching [73]. It has been proposed that PROX1 controls the expansion of tip progenitors in the early developing pancreas [73].
FOXA factors
The forkhead box A1 and A2 proteins (FOXA1 and FOXA2), two winged-helix TFs, are expressed in the pancreatic primordium prior to pancreas morphogenesis and persists in all pancreatic cell types throughout development and adulthood [25, 74]. FOXA1 and FOXA2 play redundant roles in early pancreas development. Individual inactivation of these TFs does not have a major impact on pancreas formation. However, conditional ablation of both Foxa1 and Foxa2 in the pancreatic progenitor domain leads to severe pancreatic hypoplasia [74]. These defects might be due to loss of Pdx1 expression in MPCs. ChIP and ChIP sequencing (ChIPSeq) experiments performed in fetal pancreas have demonstrated that FOXA1 and FOXA2 are the essential transcription factors required for early Pdx1 expression.
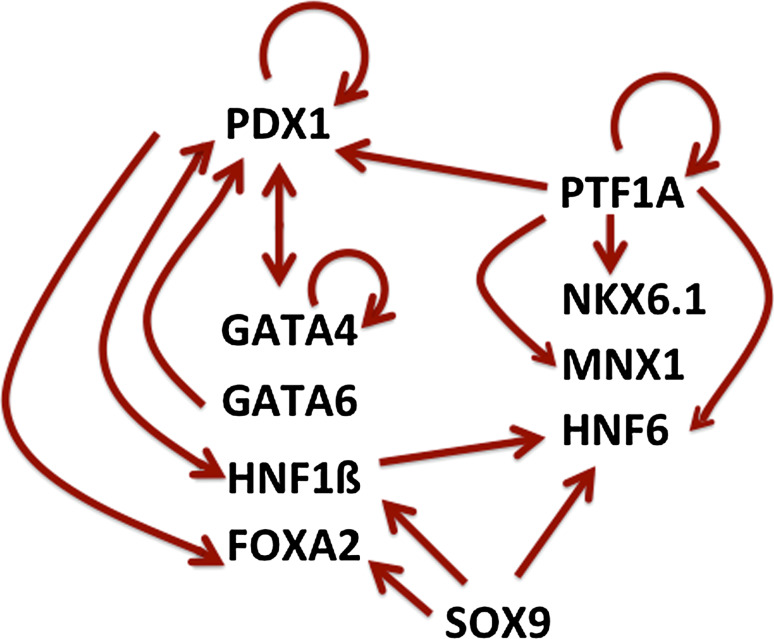
The studies summarized above have revealed a significant number of TFs with critical roles in MPC formation and maintenance. Many of the pancreatic TFs directly regulate each other and their own expression, suggesting that they form a specific cross-regulatory network during early pancreas formation (Fig. 3) [7, 59, 75, 76]. Future studies focused on the identification and characterization of TFs target genes and signal inputs, as well as computational approaches to integrate such knowledge, should significantly advance our understanding of how pancreatic progenitor formation is regulated.
Fig. 3.
Transcriptional regulatory interactions between TFs in multipotent pancreatic progenitors (MPCs). Only direct interactions are included
Onset of exocrine and islet development
Between e12.5 and e15.5, the pancreatic epithelium undergoes a significant process of expansion, branching and differentiation. Concomitantly, a massive wave of endocrine and acinar cell differentiation, known as the secondary transition, begins [77]. During these stages, the epithelium is separated into tip and trunk domains that generate acinar progenitor cells, and ductal/endocrine progenitor cells, respectively [2, 39, 42]. These domains are also defined by the specific expression of TFs. Ptf1a is expressed exclusively in the tip cells whereas Sox9, Hnf1b, and Nkx6.1 are expressed in the trunk domain [2, 36, 39, 42, 78]. Recent work has begun to shed light on the molecular mechanisms that establish this lineage allocation. PTF1A and the NKX6 factors (NKX6.1 and NKX6.2) mutually antagonize each other to specify an exocrine or ductal/endocrine fate [36]. The interaction might be mediated by direct transcriptional repression of Ptf1a by Nkx6 proteins. Notch signaling pathway might mediate this process. Activation of Notch signaling in MPCs promotes a ductal/endocrine progenitor fate [36, 79, 80]. Conversely, Notch signaling attenuation in the early pancreatic epithelium results in an increase in proacinar tip cells [80, 81] and diminished expression of trunk-specific TFs such as Nkx6.1 and Sox9 [80]. Interestingly, Nkx6.1 appears to be a direct target of Notch signaling, suggesting that this pathway might act initially on NKX6.1 during tip-trunk patterning [80]. An exciting recent discovery is the link between epithelial tubulogenesis and cell specification. Inactivation of the Rho-GTPase Cdc42 in pancreatic progenitors disrupted the developing epithelial structure that led to a perturbed tip-trunk compartmentalization and an increase in acinar cell differentiation at the expense of endocrine fate [33]. It is not yet clear how defects in tubulogenesis affect pancreatic cell fate. However, it has been suggested that it might be related to the fact that tip and trunk domains are exposed to different microenvironments during pancreatic development, with tip cells in close proximity to extracellular matrix components. Two relevant recent studies have reported that endothelial cells are preferentially positioned close to the trunk cells of the epithelium [82, 83]. In agreement with this spatial organization of endothelial cells in the pancreatic epithelium, endothelial cells have been shown to limit acinar differentiation, perhaps by repressing the expression of Ptf1a [82, 83]. During the secondary transition, scattered individual cells within the trunk transiently express the master regulator of endocrine formation, neurogenin 3, (Ngn3) and differentiate into the endocrine lineage. Endocrine progenitor cells delaminate from the ductal epithelium and form clusters, where they continue to differentiate. Little is known about the mechanisms governing endocrine delamination, migration, and aggregation. Epithelial-to-mesenchymal transition (EMT) might be involved in endocrine delamination [84, 85], although conclusive evidence remains elusive. More recently, Grg3 (Groucho-related gene 3), a member of the Groucho/TLE family of co-repressors, has been implicated in endocrine delamination [86]. GRG3 appears to promote delamination of endocrine cells by suppressing E-cadherin gene expression. Interestingly, NGN3 is required for Grg3 expression suggesting a possible interaction between NGN3 and GRG3. These observations are consistent with recent research describing a role for NGN3 in endocrine delamination [87–89]. E-cadherin function might also be important for endocrine migration. Current evidence suggests that RAC1, a member of the Rho family of small GTPases, acts as a key regulator of endocrine cell migration by modulating E-cadherin-mediated cell–cell adhesion [90]. Clearly, this is an area of research that merits further investigation.
Endocrine cell specification begins with the induction of the bHLH (basic helix loop helix) TF NGN3. Ngn3 expression is first observed at e9.5. Its expression peaks during the secondary transition and markedly decreases during later stages of pancreatic development [91]. NGN3 is essential for endocrine cell formation. Ngn3 null mice lack all endocrine cell types, but display normal exocrine development [92]. Furthermore, overexpression of Ngn3 under the Pdx1 promoter results in premature differentiation of MPCs and increases the formation of endocrine cells [93, 94]. Consistent with these results, lineage-tracing studies have demonstrated that all pancreatic endocrine cells derive from Ngn3-positive progenitor cells [38]. In addition, achieving high NGN3 levels has been shown to be critical for allocation of endocrine cell fate [95]. NGN3 activation is directly regulated by a complex cross-regulatory TF network that includes FOXA2, GLIS3, HNF1β, HNF6, and PDX1 and SOX9 [52, 59, 76, 96–98]. Although the key TFs that regulate Ngn3 expression in pancreatic progenitors have been identified in recent years, the mechanistic details of how this TF network activates Ngn3 expression in specific cells within the trunk domain have not been fully elucidated. The Notch pathway appears to play a key role in this process by a classical mechanism of lateral inhibition [93, 99]. Endocrine progenitors induce the production of Notch ligands. Notch signaling activates the target gene, Hes1, in neighboring cells, which directly downregulates Ngn3 expression [100]. Consequently, these cells are maintained as undifferentiated progenitors. This mechanism helps to ensure the proper balance between proliferation and differentiation in ductal/endocrine trunk progenitors. However, recent studies have challenged this lateral inhibition model, suggesting further complexities in Notch-mediated regulation of endocrine differentiation [101–104]. It has been proposed that Ngn3 activation is governed by a gradient of Notch activity in the pancreatic epithelium. SOX9 appears to play a key role in this process [101]. Epigenetic mechanisms might also play a key role in the regulation of endocrine progenitor selection: histone modifications, such as acetylation, alter endocrine cell fate allocation in embryonic pancreas [105]. Another particularly exciting discovery is that planar cell polarity controls endocrine differentiation from pancreatic progenitor cells [106]. These studies have provided new insight into the intrinsic mechanisms that govern endocrine commitment. We can expect to see more studies focused on the interaction between these cell-intrinsic mechanisms and the endocrine-specific transcriptional network in the next few years. In particular, elucidation of the mechanism that allows TFs to work in concert with chromatin modifiers to direct endocrine differentiation is an important area of investigation.
Ngn3-expressing precursors can give rise to the five different endocrine cell lineages. Ngn3-expressing cells are postmitotic and lineage-tracing studies have determined that they are allocated to a single endocrine cell lineage. Therefore, Ngn3-expressing cells are unipotent endocrine precursors [107]. At present, it is not understood how Ngn3-expressing precursors are instructed to specific islet cell fates. However, elegant studies by Johansson et al. [94] have shown that the timing of Ngn3 activation in precursors cells can determine the endocrine cell type generated. For example, Ngn3 expression induced during early pancreas development promotes the formation of α-cells. The induction of Ngn3 expression from e11.5 onward favored the generation of β- and PP-cells. From e14.5 onward, Ngn3-expressing cells become competent to generate δ-cells, whereas the competence to produce α-cells markedly diminishes.
NGN3 induces the endocrine developmental program by directly activating the expression of TFs necessary for endocrine differentiation, including Neurod1, Pax4, Insm1, Rfx6, Nkx2.2, and Myt1 [76, 108–115]. It is likely that the list of TFs directly regulated by NGN3 and presumably with a potential role in endocrine formation will increase in the future. Microarray analysis of Ngn3 mutant mice, as well as gene expression profiling studies performed in Ngn3-expressing cells, have already yielded a long list of TFs that might potentially be regulated by NGN3 [115–119].
Endocrine and exocrine differentiation
Endocrine cells
A remarkable number of TFs that are required for different aspects of endocrine development, including cell differentiation, survival, maturation and endocrine subtype allocation development have been identified (see [7, 120] for comprehensive reviews). Here, we highlight TFs with recently discovered roles in endocrine formation.
Among the NGN3 regulated TFs, NEUROD1 and INSM1 appear to occupy relevant positions in the hierarchy of endocrine development. Mutant embryos deficient in these TFs exhibit reduced numbers of all endocrine cell types (although not to the degree observed in Ngn3 mutant mice) [121, 122], consistent with defects in early endocrine formation. Similar defects in islet formation have recently been described in mice lacking Regulatory X-box binding 6 (Rfx6) and the LIM homeodomain protein Islet1 (Isl1) [114, 115, 123]. Although RFX6 and ISL1 appear to act downstream of NGN3 [92, 115], direct regulation of these TFs by NGN3 has not been reported. Rfx6 is broadly expressed in the gut endoderm including the nascent pancreatic bud at e9.0 [114, 115]. From e10.5, Rfx6 expression in the pancreas is found only in endocrine progenitor cells. Rfx6 expression is maintained in all adult islet cell types [114, 115]. Rfx6 mutant mice display a dramatic reduction of all endocrine cell types with the exception of PP-cells [114]. This is not related to loss of endocrine progenitors, because Ngn3 remains normally expressed. Indeed, endocrine cells are present in the Rfx6 pancreata, but they do not appear to express hormone genes or other mature markers. These results indicate that Rfx6 is required for the differentiation of endocrine cell types (with the exception of PP-cells). ISL1 is required for the differentiation, proliferation and survival of endocrine cells after the secondary transition [123]. A second level of transcriptional control during endocrine formation involves the specification of individual endocrine cell types. A number of TFs whose inactivation causes differential loss of endocrine cell types have been described, including Pax4, Arx and NKX-homeodomain factors. Three NKX genes are expressed during pancreas development, Nkx2.2, Nkx6.1 and Nkx6.2. These TFs are broadly expressed in the MPC compartment during early pancreatic development. However, the role of the NKX factors in MPCs formation and maintenance is, at present unclear, since they are dispensable for early pancreas development [124–126]. Nkx6.1 and its paralog Nkx6.2 show some degree of functional redundancy during endocrine formation. Nkx6.1/Nkx6.2 double mutants exhibit reduced numbers of α- and β-cells. However, only β-cells are affected in Nkx6.1 mutant mice, while Nkx6.2 mice do not show any apparent pancreatic defects [126]. Nkx2.2 null mice display a total loss of β-cells and decreased numbers of α- and PP-cells [124]. Interestingly, a significant increase in ghrelin-producing ε-cells is observed indicating a switch in lineage specification [127]. NKX2.2 genetically interacts with other TFs to regulate the specification of endocrine cell lineages. Simultaneous inactivation of NeuroD1 and Nkx2.2 restores α- and PP-cell, but not β-cell formation and decreases the number of ε-cells [128]. NKX2.2 differentially regulates NeuroD1 in progenitor cells to specify different cell lineages. Thus, activation of NeuroD1 by NKX2.2 is necessary for β-cell formation, while NKX2.2 must repress NeuroD1 to allow proper allocation of the α-cell lineage [129]. NKX2.2 also interacts with aristaless-related homeobox x-linked (Arx) in the regulation of the PP-cell lineage [130]. Pax4 mutant mice display a phenotype similar to Nkx2.2 mice (reduced β- and δ-cell numbers and increased α- and ε-cells), although it is unclear whether a genetic interaction between these TFs exists [127]. Recent studies have provided insight into the mechanisms regulating the fate choice between the α- and β-cell lineage (see [131] for an detailed review on this subject). The opposing activities of PAX4, an important β-cell differentiation TF, and ARX, a key factor in α-cell specification, appear to play a key role in this process. Both Pax4 and Arx are initially expressed in Ngn3-expressing progenitor cells [132, 133]. During endocrine differentiation, Pax4 and Arx expression becomes restricted to β- and α-cell lineages, respectively. Pax4 inactivation results in the loss of β- and δ-cells and a corresponding increase in α-cell number [133] while deficiency in Arx leads to a complete loss of α-cells, concomitant with an increase in β- and δ-cells [132]. Ectopic expression of Pax4 and Arx in endocrine progenitor cells induces β- and α-cell formation, respectively [134, 135]. Thus, Pax4 promotes β- and δ-cell fate, while Arx promotes the α-cell fate at the expense of β- and δ-cell fate. The antagonistic interaction between these TFs might be mediated by reciprocal transcriptional repression [134, 135]. A similar antagonistic relationship between NKX6.1 and ARX function might also participate in α- versus β-cell lineage commitment [136]. Misexpression of Nxk6.1 in endocrine progenitor cells promotes β-cell formation at the expense of α-cell lineage [136] while ectopic expression of Arx results in the opposite alteration, as discussed previously. Conversely, inactivation of Nkx6.1 in endocrine precursors switches β-cells to different endocrine lineages. The underlying molecular mechanism by which Nkx6.1 regulates α- and β-cell fate allocation might involve the direct transcriptional repression of the Arx gene through competition with the Arx activator ISL1, as suggested by in vitro studies [136]. PDX1 might also act as a regulator of α- and β-cell lineage commitment. Enforced Pdx1 expression in endocrine progenitors induces a slight increase in β-cell formation, which is accompanied by a decrease in α-cell numbers [98]. These results are consistent with the expansion of α-cell number observed in mice with specific ablation of Pdx1 in embryonic β-cells [137]. However, it is important to note that in this study, lineage-tracing experiments indicated that α-cells did not arise from β-cells. Once endocrine cell fate has been established, additional TFs are required for terminal cell differentiation and maintenance of cell function. A significant number of TFs involved in this process have been described, including FOXA2, GLIS3, ISL1, MAFA, MAFB, NEUROD1, PAX6, RFX3 and PDX1 (see [7, 120] for detailed reviews). Here it is important to note that maintenance of endocrine cell identity requires not only the activation of genes specific for that particular cell lineage, but also the repression of genes. This is best illustrated in a recent study that inactivated Nkx2.2 specifically in β-cells [138]. Loss of Nxx2.2 causes a β-to-α cell transdifferentiation due to derepression of the α-cell regulator Arx, proving that the repressor activities of NKX2.2 are required for maintaining β-cell identity.
The studies summarized above have revealed significant developmental plasticity among the different endocrine cell types as a consequence of forced expression of lineage-specific TFs. Recent studies have suggested that epigenetic mechanisms such as DNA methylation might play a role in the regulation of cell plasticity in endocrine cells [138, 139]. These results might be particularly relevant in light of reports characterizing α-to-β cell reprogramming in adult stages [140] and the suggestion that reprogramming strategies might lead to novel sources of β-cells for diabetes therapies.
Acinar cells
PTF1A is the master regulator of acinar cell differentiation [141, 142]. As discussed above, PTF1A forms a complex with the subunit RBPJ during early pancreas development. PTF1A initiates acinar differentiation by a mechanism that involves the replacement of the subunit RBPJ by RBPJL [142]. The PTF1A-RBP-JL complex appears to directly activate the expression of acinar-specific genes, such as secretory proteins, as suggested by Chip-Seq and gene profiling experiments [142]. Interestingly, PDX1 also seems to be required for exocrine differentiation. Pdx1 inactivation from e13.5 results in the formation of immature acini [48]. These results indicate that while PDX1 is not required for acinar cell specification, it is needed to complete the final steps of acinar differentiation. Recent studies have suggested that GATA factors might also play a role in exocrine formation. As discussed above, Gata6 is coexpressed with Gata4 in the early pancreatic epithelium. At later stages, Gata4 expression is observed only in acinar cells, whereas Gata6 expression is restricted to endocrine cells [26, 143]. Inactivation of either Gata4 or Gata6 does not have a major impact on acinar cell formation. A minor defect in acinar architecture is observed in Gata4 neonatal mice, but these phenotypes are resolved postnatally [27]. However, mice lacking both alleles of Gata4, but retaining one Gata6 allele display severe acinar cell loss. The architecture of remaining acini was disorganized, but cell differentiation appears unaffected [26, 27]. Interestingly, mice lacking both alleles of Gata6, but retaining one Gata4 allele, do not exhibit any apparent exocrine defects. In other words, one allele of Gata4, but not Gata6, was sufficient for normal acinar formation. These results indicate that GATA6 is more critical than GATA4 in supporting exocrine pancreas development. These results appear to be at odds with the lack of expression of Gata6 in the exocrine lineage during late pancreas development. A possible explanation is that the exocrine phenotypes in Gata4 homozygous, Gata6 heterozygous mice are due to defects in acinar cell lineage allocation during early pancreas development. However, in support of a role for GATA6 in acinar cell development, a recent study has described that GATA6 is required for maintenance of cell identity in adult acinar cells [144]. Inactivation of Gata4 and Gata6, individually as well as in combination, within the acinar lineage is required to conclusively establish whether GATA4 or GATA6 are necessary for exocrine formation. Mist1 and Nr5a2 are two TFs that are specifically expressed during acinar differentiation. Although these TFs are dispensable for the embryonic development of the acinar lineage, they are critical for postnatal maturation and adult homeostasis of acinar cells [145, 146]. Importantly, NR5A2 cooperates with the PTF1A-RBJL complex in activating acinar-specific gene expression in adult stages [147]. Several other TFs highly expressed in the acinar lineage have been reported, but their roles in acinar formation have not been determined (see [148] for a comprehensive list of these TFs).
Ductal cells
The molecular mechanisms involved in ductal specification and development are poorly understood. This is somewhat surprising considering that these cells have received extensive attention due to their potential involvement in adult pancreatic regeneration, as well as pathologies like pancreatitis and cancer [149]. An increasing number of TFs that are expressed in the ductal lineage during late pancreas formation and adult stages have been described in recent years, including SOX9, HES1, HNf1β, HNF6, and PROX1. Some of these TFs might play a role in ductal development. Inactivation of Hnf6 or Sox9 results in ductal cyst formation [67, 101, 150]. The underlying mechanism might be (partly) related to the lack of primary cilia in Hnf6- and Sox9-deficient ductal cells [67, 101, 150]. Primary cilia have been demonstrated to be necessary for proper pancreatic duct organization [151, 152]. More recently, a role for PROX1 in ductal development has also been reported [73]. Mutant mice deficient in Prox1 display increased ductal proliferation and altered duct morphogenesis. Interestingly, Hnf6 mutants exhibit decreased Prox1 expression. The interactions between HNF6, HNf1β, and PROX1 suggest that they might form a transcriptional network involved in ductal development. It is important to note that in all of these genetic studies, TFs have been inactivated during early pancreas formation, and thus, it remains entirely possible that some of the ductal phenotypes are consequence of early effects on pancreatic development rather than defects in ductal differentiation. Conditional inactivation of these factors in the ductal lineage should determine their precise role in pancreatic duct formation. Recently, a microarray analysis of pancreatic ductal cells at both later stages of embryonic development and neonatal stages has been published [153]. The authors report an increase in expression of several TFs, including Prox1, Hnf1B and Hhex in neonatal ducts. Detailed analysis of this microarray data might help to elucidate the regulatory mechanisms involved in ductal differentiation.
Human pancreas development
Our current knowledge of human pancreatic development is mainly derived from histological studies. These studies are limited by the difficulty in obtaining high-quality fetal human tissues, especially at early stages of pancreas development. Despite these challenges, the information obtained from these studies indicates that the morphogenesis events of pancreas development are largely conserved between human and mouse. Furthermore, all the key regulators of pancreas formation are expressed in human fetal pancreatic development [154–159]. In this section. we briefly review the expression pattern of key developmental TFs in human pancreas development highlighting key differences between mouse and human. In addition, we will discuss genetic studies that have identified mutations in genes encoding TFs that have been linked to human pancreatic disorders.
During embryonic development, the human pancreas forms from a dorsal and a ventral evagination of the primitive gut epithelium. The dorsal pancreatic bud is first evident on day 26 post-conception (dpc), while the ventral pancreas buds over the next few days. The pancreatic buds fuse by 56 dpc [154]. Thus, pancreas formation in human is initiated at an equivalent stage to that in mouse. Human endocrine differentiation occurs during the first trimester of gestation and β-cells can be detected as early as 8 weeks post-conception (wpc). Scattered α- and δ-cells are observed a week later [154–158]. Thus, it appears that the beginning of endocrine differentiation is slightly delayed in human compared to mouse. This might be related to the apparent lack of the first wave of endocrine cell formation that is observed in mouse [159]. Interestingly, despite this delayed endocrine differentiation, clustering of endocrine cells into islet-like structures occurs comparatively earlier in human embryos. Endocrine cell clusters are observed around 11–14 wpc [154, 157, 158] in human islet-like structures that are formed just prior to birth in mouse. Another significant disparity between human and mouse endocrine development is that a single, prolonged period of endocrine cell formation appears to exist in humans [157, 159, 160]. Protoacinar structures emerge by 14 wpc [157, 159]. Further pancreatic expansion and growth occur during the rest of the gestation period. Adult human and mouse islets are markedly different, both in terms of islet architecture and cell composition [161–163]. Thus, human islets contain fewer β-cells and more α- and δ-cells than mouse islets [161]. In mouse, β-cells are located at the core of islets while non-β-cells are found in the periphery. In contrast, β-cells are intermingled with α and δ cells in adult human islets. The unique cellular arrangement of adult human islets may have important effects on islet function [162]. Interestingly, human fetal islet architecture resembles that found in adult mouse islets with non-β-cells found in the periphery of islets [158]. It has been suggested that after 21 wpc, human fetal islets undergo a reorganization process that results in the establishment of the characteristic cell organization of adult human islets with intermingled β- and α-cells [158].
Several studies have analyzed the expression of key TFs in developing human fetal pancreas [154–159, 164]. These studies have revealed that TFs expression patterns are generally similar in human and mouse pancreas development (see [159] for a detailed description). This has led to hypothesize that the same key regulatory TFs might govern human and mouse pancreas formation. However, some notable differences exist. For example, PDX1 expression appears slightly later in human pancreatic development, when dorsal foregut is separated from the notochord and aorta [159]. Another significant difference is that NKX2.2 is not expressed in early human pancreatic progenitors prior to endocrine formation [159]. Also, a single phase of NGN3 expression is observed in human embryonic pancreata [159, 160]. However, NGN3 expression in the developing human pancreas is prolonged [157, 160], consistent with the described extensive phase of endocrine cell differentiation. Interestingly, differences between endocrine TFs expression in mouse and human have also been found in adult stages. MAFB expression is observed in human β-cells, whereas it is absent in mouse β-cells [165, 166].
Although informative, these histological studies only provide a limited snapshot of the specific developmental stage and therefore cannot indicate whether the transcriptional regulatory mechanisms governing pancreas development are conserved between human and mouse. Thus, there is an urgent need for longitudinal and functional studies on human pancreas development (for an excellent discussion on this issue, see [167]). Ex vivo culture of human fetal pancreas (mainly late fetal stages) have been used for decades to dynamically investigate human pancreatic differentiation. More recently, the Scharfmann’s group has developed models of xenografts of early human fetal pancreas under the kidney and the epimysium of the thigh muscle [160, 168]. These fetal xenografts develop properly into a functional endocrine pancreas allowing detailed examination of human pancreas development. These studies have validated the expression pattern of key TFs, such as PDX1, NKX2.2, and NGN3, during human pancreas development obtained from earlier immunohistochemical analysis [160]. Protocols have been established to efficiently generate endocrine cells from human embryonic stem cells (hESCs) and induced pluripotent stem cells (hPSCs) as a potential source of β-cells for replacement therapies in type 1 diabetes. The most efficient protocols utilize signals known to regulate embryonic pancreas formation in vivo (reviewed in [6, 169, 170]). In addition to their potential therapeutic applications, these stem-cell-based strategies offer a valuable in vitro model for the study of human pancreatic development. Thus, expression of major developmental TFs during the differentiation process has revealed an expression pattern consistent with embryonic pancreas formation in mouse [171–173]. Of note, cells simultaneously expressing PDX1, SOX9, PTF1A, GATA4, and NKX6.1 have been observed during intermediate stages that might correspond to mouse MPCs. Genetic tools including gene targeting and virus-mediated gene transfer have recently begun to be applied to human fetal grafts and hESCs [160, 174]. Widespread application of genetic methodologies in these ex vivo and in vitro models might provide additional, powerful experimental lines of investigation, including lineage-tracing and gain-/loss-of-function studies to investigate the role of TFs in human pancreatic development.
Genetic studies linking human pancreatic disorders to mutations in developmentally relevant transcription factors provide further support to the notion that regulatory developmental programs are conserved between human and mouse (Table 1). Thus, homozygous mutations in PDX1 and PTF1A lead to pancreatic agenesis in human [175, 176]. Homozygous mutations in GLIS3, NEUROD1, and RFX6 have been associated with permanent neonatal diabetes [114, 177, 178]. Compound heterozygous mutations in NGN3 have also been linked to permanent neonatal diabetes [179]. These results are consistent with the reported function of these TFs in mouse. However, human genetic studies have also revealed apparent differences in the roles of several developmental TFs between mouse and human. Perhaps the best-known examples are some of the TFs linked to Maturity-onset diabetes of the young (MODY). MODY is a form of monogenic diabetes caused by mutations in an autosomal dominant gene. Heterozygous loss-of-function mutations in the TFs hepatocyte nuclear factors HNF1A (MODY3), HNF1B (MODY5), and HNF4A (MODY1), cause diabetes in human but not in mouse (although homozygosity does) [180–182]. Why haploinsufficiency of these TFS cause diabetes in human but not in mouse is not completely understood but it has been suggested that the extended period of endocrine cell differentiation in human might make this process more sensitive to changes in gene dosage [183]. Differential functions for ARX in human and mouse pancreas development have been suggested based on the analysis of pancreatic tissue of patients with mutations in ARX linked to X-linked lissencephaly with abnormal genitalia (XLAG) [184]. Defects in pancreatic α-cell formation were observed in these patients, in agreement with the described role of ARX in mouse pancreas development. However, acinar abnormalities were also observed in the pancreata of XLAG patients suggesting that ARX contributes not only to endocrine development, but also to exocrine development of the human pancreas [185]. The regulatory function of GATA factors appears to constitute a major disparity between human and mouse transcriptional developmental program. Hattersley and colleagues [186] have recently shown that mutations in GATA6 are the most common cause of human pancreas agenesis, accounting for approximately 50 % of the cases. An exome sequence analyses of a cohort of patients with neonatal diabetes associated with pancreatic agenesis or severe pancreatic hypoplasia has revealed that 15 of 27 patients exhibit loss of function mutations in GATA6. Interestingly, these de novo mutations were found in heterozygotes, highlighting the important role of GATA6 in human pancreas development. More recently, a study of a larger cohort of patients by the same group has confirmed the high prevalence of pancreatic agenesis associated with mutations in GATA6 [187]. Remarkably, four patients with heterozygous GATA6 mutations developed diabetes without exocrine sufficiency at adult stages. A more extensive study of families carrying mutations in GATA6 is necessary to establish the prevalence of mutations in GATA6 as a cause of monogenic diabetes in adults. This human data is in stark contrast to the results obtained in Gata4 and Gata6 mutant mice. As discussed earlier, single inactivation of Gata4 or Gata6 in mouse does not result in any major pancreatic abnormalities. Indeed, three or four Gata alleles need to be eliminated to cause a severe pancreatic phenotype [26, 27]. The discrepancy in phenotypes is not completely understood but it is important to note that Gata6 is expressed in other mesodermal and endodermal tissues during mouse embryonic development. If that is also the case in human embryonic development, mutations in GATA6 might affect these mesodermal and endodermal tissues potentially interfering with pancreas development. Alternatively, differences in the pancreatic genetic program between species might account for this discrepancy. The spatiotemporal pattern of GATA6 expression during human pancreas development has not been reported. Thus, it remains to be determined whether GATA4 and GATA6 expression overlap and are functionally redundant in early human pancreatic formation. To this end, a detailed report of GATA4 expression in human pancreas development was recently published [159]. Interestingly, GATA4 is strongly expressed during early human pancreas budding, consistent with the observed expression in mouse. However, GATA4 expression appears to rapidly decrease in the early human pancreatic progenitor domain (defined by simultaneous expression of PDX1, PTF1A, SOX9 and NKX6.1) [159], thus making this stage potentially more sensitive to reductions in GATA6 gene dosage.
Table 1.
Transcription factors linked to human pancreatic disorders
| Gene | Name | Pancreatic abnormalities |
|---|---|---|
| ARX | Aristaless-related homeobox | Hemizygous male: partial loss of endocrine and exocrine cells [185] |
| FOXP3 | Forkhead box P 3 | Hemizygous male: permanent diabetes [188] |
| GATA6 | Gata binding protein 6 | Heterozygous: neonatal diabetes, pancreatic agenesis [186]. Adult-onset diabetes [187] |
| GLIS3 | Glis family zinc finger 3 | Homozygous: neonatal diabetes [178] |
| HNF1Α | Hepatocyte nuclear factor 1α | Heterozygous: MODY3 [182] |
| HNF1B | Hepatocyte nuclear factor 1ß | Heterozygous: MODY5 [181] |
| HNF4Α | Hepatocyte nuclear factor 4α | Heterozygous: MODY1 [180] |
| MNX1 | Motor neuron and pancreas homeobox 1 | Homozygous: permanent neonatal diabetes [189] |
| NEUROD1 | Neurogenin differentiation factor 1 | Heterozygous: MODY6 [190]. Homozygous: neonatal diabetes [177] |
| NGN3 | Neurogenin 3 | Homozygous (hypomorphic mutation): diabetes [191, 192]. Biallelic mutations: permanent neonatal diabetes [179] |
| PAX4 | Paired box 4 | Heterozygous: MODY9 [193] |
| PDX1 | Pancreatic and duodenal homeobox 1 | Homozygous: congenital pancreatic agenesis [175]. Heterozygous: MODY4 [194] |
| PTF1A | Pancreatic-specific transcription factor 1A | Homozygous: pancreatic agenesis [176] |
| RFX6 | Regulatory factor X6 | Homozygous: neonatal diabetes and pancreatic hypoplasia [114] |
| SOX9 | Sex determine region Y (SRY)-box 9 | Heterozygous: pancreatic abnormalities [195] |
In summary, human genetic studies have revealed significant distinctions between human and mouse pancreas development. This highlights the need for experimental studies in human tissue to fully elucidate the roles of TFs in pancreas formation. The generation of PSCs form patients harboring mutations in genes encoding TFs, coupled with in vitro production of functional β-cells, will facilitate studies aimed at understanding the regulatory mechanisms that govern human pancreas development.
Concluding remarks
Genetic studies in mice have led to the discovery of a vast number of TFs that participate in pancreas organogenesis. Functional genomics assays have made it possible to determine gene expression profiles and to identify transcription factor-binding sites on a genome-wide scale. These studies have revealed the complexity of the transcriptional interactions and networks underlying pancreatic differentiation. Although our understanding of the transcription factors and the genetic regulatory networks they form in pancreatic development has greatly increased over the last decade, some key gaps in our knowledge need to be filled before a comprehensive model of transcriptional pathways during pancreas formation can be built. Functional integration of TFs with the extrinsic signaling pathways that regulate the multiple steps of pancreatic organogenesis, in particular, is poorly understood. Similarly, more information is needed about how pancreatic lineage-specific transcription factors interact with the epigenetic machinery to drive pancreatic cell differentiation. Also, more studies on human tissue are required since differences between mouse and human pancreas development might exist. We can expect that the identification of new TFs with roles in pancreas formation, together with the advent of more sensitive functional genomics tools and the emerging field of epigenetics, will lead to a greater understanding of the transcriptional networks that operate in pancreas organogenesis over the next few years.
Acknowledgments
The authors apologize to the investigators whose work could not be to cited due to space limitations. We are indebted to Alvaro Flores for his fine artwork in Fig. 1. D.A.C. is supported by grants from the Spanish Ministry of Science and Innovation (SAF2008-02469 and SAF2011-26805) and the Andalusian Regional Ministry of Health. B.S. is supported by ISCIII (cofinanced by FEDER: Red TerCel-Grant RD06/0010/0025; Grant PI10/00964), Consejería de Innovación Ciencia y Empresa, Junta de Andalucía (CTS-6505), Ministry of Health and Consumer Affairs (Advanced Therapies Program Grant TRA-120) and European Union (BIOREG SOE3/P1/E750, confinanced by FEDER). A.R. is supported by a grant from ISCIII co-funded by Fondos FEDER (PI11/01125).
References
- 1.Pictet RL, Clark WR, Williams RH, Rutter WJ. An ultrastructural analysis of the developing embryonic pancreas. Dev Biol. 1972;29(4):436–467. doi: 10.1016/0012-1606(72)90083-8. [DOI] [PubMed] [Google Scholar]
- 2.Zhou Q, Law AC, Rajagopal J, Anderson WJ, Gray PA, Melton DA. A multipotent progenitor domain guides pancreatic organogenesis. Dev Cell. 2007;13(1):103–114. doi: 10.1016/j.devcel.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 3.Gittes GK. Developmental biology of the pancreas: a comprehensive review. Dev Biol. 2009;326(1):4–35. doi: 10.1016/j.ydbio.2008.10.024. [DOI] [PubMed] [Google Scholar]
- 4.Serup P. Signaling pathways regulating murine pancreatic development. Semin Cell Dev Biol. 2012;23(6):663–672. doi: 10.1016/j.semcdb.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 5.Seymour PA, Sander M. Historical perspective: beginnings of the beta-cell: current perspectives in beta-cell development. Diabetes. 2011;60(2):364–376. doi: 10.2337/db10-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guo T, Hebrok M. Stem cells to pancreatic beta-cells: new sources for diabetes cell therapy. Endocr Rev. 2009;30(3):214–227. doi: 10.1210/er.2009-0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan FC, Wright C. Pancreas organogenesis: from bud to plexus to gland. Dev Dyn. 2011;240(3):530–565. doi: 10.1002/dvdy.22584. [DOI] [PubMed] [Google Scholar]
- 8.Lammert E, Cleaver O, Melton D. Induction of pancreatic differentiation by signals from blood vessels. Science. 2001;V294(N5542):564–567. doi: 10.1126/science.1064344. [DOI] [PubMed] [Google Scholar]
- 9.McCracken KW, Wells JM. Molecular pathways controlling pancreas induction. Semin Cell Dev Biol. 2012;23(6):656–662. doi: 10.1016/j.semcdb.2012.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zorn AM, Wells JM. Vertebrate endoderm development and organ formation. Annu Rev Cell Dev Biol. 2009;25:221–251. doi: 10.1146/annurev.cellbio.042308.113344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chiang MK, Melton DA. Single-cell transcript analysis of pancreas development. Dev Cell. 2003;4(3):383–393. doi: 10.1016/s1534-5807(03)00035-2. [DOI] [PubMed] [Google Scholar]
- 12.Kawaguchi Y, Cooper B, Gannon M, Ray M, MacDonald RJ, Wright CV. The role of the transcriptional regulator Ptf1a in converting intestinal to pancreatic progenitors. Nat Genet. 2002;32(1):128–134. doi: 10.1038/ng959. [DOI] [PubMed] [Google Scholar]
- 13.Guz Y, Montminy MR, Stein R, Leonard J, Gamer LW, Wright CVE, Teitelman G. Expression of murine STF-1, a putative insulin gene transcription factor, in β cells of pancreas, duodenal epithelium and pancreatic exocrine and endocrine progenitors during ontogeny. Development. 1995;121:149–161. doi: 10.1242/dev.121.1.11. [DOI] [PubMed] [Google Scholar]
- 14.Offield MF, Jetton TL, Labosky PA, Ray M, Stein R, Magnuson MA, Hogan BLM, Wright CVE. PDX-1 is required for pancreatic outgrowth and differentiation of the rostral duodenum. Development. 1996;122:983–995. doi: 10.1242/dev.122.3.983. [DOI] [PubMed] [Google Scholar]
- 15.Jonsson J, Carlsson L, Edlund T, Edlund H. Insulin-promoter-factor 1 is required for pancreas development in mice. Nature. 1994;371:606–609. doi: 10.1038/371606a0. [DOI] [PubMed] [Google Scholar]
- 16.Stoffers DA, Heller RS, Miller CP, Habener JF. Developmental expression of the homeodomain protein IDX-1 in mice transgenic for an IDX-1 promoter/lacZ transcriptional reporter. Endocrinology. 1999;140(11):5374–5381. doi: 10.1210/endo.140.11.7122. [DOI] [PubMed] [Google Scholar]
- 17.Larsson LI, Madsen OD, Serup P, Jonsson J, Edlund H. Pancreatic-duodenal homeobox 1 -role in gastric endocrine patterning. Mech Dev. 1996;60(2):175–184. doi: 10.1016/s0925-4773(96)00609-0. [DOI] [PubMed] [Google Scholar]
- 18.Ahlgren U, Jonsson J, Edlund H. The morphogenesis of the pancreatic mesenchyme is uncoupled from that of the pancreatic epithelium in IPF1/PDX1- deficient mice. Development. 1996;122:1409–1416. doi: 10.1242/dev.122.5.1409. [DOI] [PubMed] [Google Scholar]
- 19.Jonas JC, Bensellam M, Duprez J, Elouil H, Guiot Y, Pascal SM. Glucose regulation of islet stress responses and beta-cell failure in type 2 diabetes. Diabetes Obes Metab. 2009;11(Suppl 4):65–81. doi: 10.1111/j.1463-1326.2009.01112.x. [DOI] [PubMed] [Google Scholar]
- 20.Burlison JS, Long Q, Fujitani Y, Wright CV, Magnuson MA. Pdx-1 and Ptf1a concurrently determine fate specification of pancreatic multipotent progenitor cells. Dev Biol. 2008;316(1):74–86. doi: 10.1016/j.ydbio.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gannon M, Gamer LW, Wright CV. Regulatory regions driving developmental and tissue-specific expression of the essential pancreatic gene pdx1. Dev Biol. 2001;238(1):185–201. doi: 10.1006/dbio.2001.0359. [DOI] [PubMed] [Google Scholar]
- 22.Wiebe PO, Kormish JD, Roper VT, Fujitani Y, Alston NI, Zaret KS, Wright CV, Stein RW, Gannon M. Ptf1a binds to and activates area III, a highly conserved region of the Pdx1 promoter that mediates early pancreas-wide Pdx1 expression. Mol Cell Biol. 2007;27(11):4093–4104. doi: 10.1128/MCB.01978-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gannon M, Herrera PL, Wright CV. Mosaic Cre-mediated recombination in pancreas using the pdx-1 enhancer/promoter. Genesis. 2000;26(2):143–144. doi: 10.1002/(sici)1526-968x(200002)26:2<143::aid-gene13>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 24.Jacquemin P, Lemaigre FP, Rousseau GG. The Onecut transcription factor HNF-6 (OC-1) is required for timely specification of the pancreas and acts upstream of Pdx-1 in the specification cascade. Dev Biol. 2003;258(1):105–116. doi: 10.1016/s0012-1606(03)00115-5. [DOI] [PubMed] [Google Scholar]
- 25.Lee CS, Sund NJ, Behr R, Herrera PL, Kaestner KH. Foxa2 is required for the differentiation of pancreatic alpha-cells. Dev Biol. 2005;278(2):484–495. doi: 10.1016/j.ydbio.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 26.Carrasco M, Delgado I, Soria B, Martin F, Rojas A. GATA4 and GATA6 control mouse pancreas organogenesis. J Clin Investig. 2012;122(10):3504–3515. doi: 10.1172/JCI63240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xuan S, Borok MJ, Decker KJ, Battle MA, Duncan SA, Hale MA, Macdonald RJ, Sussel L. Pancreas-specific deletion of mouse Gata4 and Gata6 causes pancreatic agenesis. J Clin Investig. 2012;122(10):3516–3528. doi: 10.1172/JCI63352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sherwood RI, Chen TY, Melton DA. Transcriptional dynamics of endodermal organ formation. Dev Dyn. 2009;238(1):29–42. doi: 10.1002/dvdy.21810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Spence JR, Lange AW, Lin SC, Kaestner KH, Lowy AM, Kim I, Whitsett JA, Wells JM. Sox17 regulates organ lineage segregation of ventral foregut progenitor cells. Dev Cell. 2009;17(1):62–74. doi: 10.1016/j.devcel.2009.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kanai-Azuma M, Kanai Y, Gad JM, Tajima Y, Taya C, Kurohmaru M, Sanai Y, Yonekawa H, Yazaki K, Tam PP, Hayashi Y. Depletion of definitive gut endoderm in Sox17-null mutant mice. Development. 2002;129(10):2367–2379. doi: 10.1242/dev.129.10.2367. [DOI] [PubMed] [Google Scholar]
- 31.Pan FC, Bankaitis ED, Boyer D, Xu X, Van de Casteele M, Magnuson MA, Heimberg H, Wright CV. Spatiotemporal patterns of multipotentiality in Ptf1a-expressing cells during pancreas organogenesis and injury-induced facultative restoration. Development. 2013;140(4):751–764. doi: 10.1242/dev.090159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xu CR, Cole PA, Meyers DJ, Kormish J, Dent S, Zaret KS. Chromatin “prepattern” and histone modifiers in a fate choice for liver and pancreas. Science. 2011;332(6032):963–966. doi: 10.1126/science.1202845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kesavan G, Sand FW, Greiner TU, Johansson JK, Kobberup S, Wu X, Brakebusch C, Semb H. Cdc42-mediated tubulogenesis controls cell specification. Cell. 2009;139(4):791–801. doi: 10.1016/j.cell.2009.08.049. [DOI] [PubMed] [Google Scholar]
- 34.Villasenor A, Chong DC, Henkemeyer M, Cleaver O. Epithelial dynamics of pancreatic branching morphogenesis. Development. 2010;137(24):4295–4305. doi: 10.1242/dev.052993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kopp JL, von Figura G, Mayes E, Liu FF, Dubois CL, Morris JPt, Pan FC, Akiyama H, Wright CV, Jensen K, Hebrok M, Sander M. Identification of Sox9-dependent acinar-to-ductal reprogramming as the principal mechanism for initiation of pancreatic ductal adenocarcinoma. Cancer Cell. 2012;22(6):737–750. doi: 10.1016/j.ccr.2012.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schaffer AE, Freude KK, Nelson SB, Sander M. Nkx6 transcription factors and Ptf1a function as antagonistic lineage determinants in multipotent pancreatic progenitors. Dev Cell. 2010;18(6):1022–1029. doi: 10.1016/j.devcel.2010.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sugiyama T, Benitez CM, Ghodasara A, Liu L, McLean GW, Lee J, Blauwkamp TA, Nusse R, Wright CV, Gu G, Kim SK. Reconstituting pancreas development from purified progenitor cells reveals genes essential for islet differentiation. Proc Natl Acad Sci USA. 2013;110(31):12691–12696. doi: 10.1073/pnas.1304507110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gu G, Dubauskaite J, Melton DA. Direct evidence for the pancreatic lineage: NGN3+ cells are islet progenitors and are distinct from duct progenitors. Development. 2002;129(10):2447–2457. doi: 10.1242/dev.129.10.2447. [DOI] [PubMed] [Google Scholar]
- 39.Solar M, Cardalda C, Houbracken I, Martin M, Maestro MA, De Medts N, Xu X, Grau V, Heimberg H, Bouwens L, Ferrer J. Pancreatic exocrine duct cells give rise to insulin-producing beta cells during embryogenesis but not after birth. Dev Cell. 2009;17(6):849–860. doi: 10.1016/j.devcel.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 40.Kopinke D, Murtaugh LC. Exocrine-to-endocrine differentiation is detectable only prior to birth in the uninjured mouse pancreas. BMC Dev Biol. 2010;10:38. doi: 10.1186/1471-213X-10-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kopinke D, Brailsford M, Shea JE, Leavitt R, Scaife CL, Murtaugh LC. Lineage tracing reveals the dynamic contribution of Hes1+ cells to the developing and adult pancreas. Development. 2011;138(3):431–441. doi: 10.1242/dev.053843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kopp JL, Dubois CL, Schaffer AE, Hao E, Shih HP, Seymour PA, Ma J, Sander M. Sox9+ ductal cells are multipotent progenitors throughout development but do not produce new endocrine cells in the normal or injured adult pancreas. Development. 2011;138(4):653–665. doi: 10.1242/dev.056499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stanger BZ, Tanaka AJ, Melton DA. Organ size is limited by the number of embryonic progenitor cells in the pancreas but not the liver. Nature. 2007;445(7130):886–891. doi: 10.1038/nature05537. [DOI] [PubMed] [Google Scholar]
- 44.Bhushan A, Itoh N, Kato S, Thiery JP, Czernichow P, Bellusci S, Scharfmann R. Fgf10 is essential for maintaining the proliferative capacity of epithelial progenitor cells during early pancreatic organogenesis. Development. 2001;128(24):5109–5117. doi: 10.1242/dev.128.24.5109. [DOI] [PubMed] [Google Scholar]
- 45.Murtaugh LC, Law AC, Dor Y, Melton DA. Beta-catenin is essential for pancreatic acinar but not islet development. Development. 2005;132(21):4663–4674. doi: 10.1242/dev.02063. [DOI] [PubMed] [Google Scholar]
- 46.Wells JM, Esni F, Boivin GP, Aronow BJ, Stuart W, Combs C, Sklenka A, Leach SD, Lowy AM. Wnt/beta-catenin signaling is required for development of the exocrine pancreas. BMC Dev Biol. 2007;7:4. doi: 10.1186/1471-213X-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Holland AM, Hale MA, Kagami H, Hammer RE, MacDonald RJ. Experimental control of pancreatic development and maintenance. Proc Natl Acad Sci USA. 2002;99(19):12236–12241. doi: 10.1073/pnas.192255099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hale MA, Kagami H, Shi L, Holland AM, Elsasser HP, Hammer RE, MacDonald RJ. The homeodomain protein PDX1 is required at mid-pancreatic development for the formation of the exocrine pancreas. Dev Biol. 2005;286(1):225–237. doi: 10.1016/j.ydbio.2005.07.026. [DOI] [PubMed] [Google Scholar]
- 49.Svensson P, Williams C, Lundeberg J, Ryden P, Bergqvist I, Edlund H. Gene array identification of Ipf1/Pdx1-/- regulated genes in pancreatic progenitor cells. BMC Dev Biol. 2007;7:129. doi: 10.1186/1471-213X-7-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Seymour PA, Shih HP, Patel NA, Freude KK, Xie R, Lim CJ, Sander M. A Sox9/Fgf feed-forward loop maintains pancreatic organ identity. Development. 2012;139(18):3363–3372. doi: 10.1242/dev.078733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rojas A, Schachterle W, Xu SM, Black BL. An endoderm-specific transcriptional enhancer from the mouse Gata4 gene requires GATA and homeodomain protein-binding sites for function in vivo. Dev Dyn. 2009;238(10):2588–2598. doi: 10.1002/dvdy.22091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Oliver-Krasinski JM, Kasner MT, Yang J, Crutchlow MF, Rustgi AK, Kaestner KH, Stoffers DA. The diabetes gene Pdx1 regulates the transcriptional network of pancreatic endocrine progenitor cells in mice. J Clin Invest. 2009;119(7):1888–1898. doi: 10.1172/JCI37028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jacquemin P, Yoshitomi H, Kashima Y, Rousseau GG, Lemaigre FP, Zaret KS. An endothelial-mesenchymal relay pathway regulates early phases of pancreas development. Dev Biol. 2006;290(1):189–199. doi: 10.1016/j.ydbio.2005.11.023. [DOI] [PubMed] [Google Scholar]
- 54.Beres TM, Masui T, Swift GH, Shi L, Henke RM, MacDonald RJ. PTF1 is an organ-specific and Notch-independent basic helix-loop-helix complex containing the mammalian Suppressor of Hairless (RBP-J) or its paralogue, RBP-L. Mol Cell Biol. 2006;26(1):117–130. doi: 10.1128/MCB.26.1.117-130.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Masui T, Long Q, Beres TM, Magnuson MA, MacDonald RJ. Early pancreatic development requires the vertebrate Suppressor of Hairless (RBPJ) in the PTF1 bHLH complex. Genes Dev. 2007;21(20):2629–2643. doi: 10.1101/gad.1575207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thompson N, Gesina E, Scheinert P, Bucher P, Grapin-Botton A. RNA profiling and chromatin immunoprecipitation-sequencing reveal that PTF1a stabilizes pancreas progenitor identity via the control of MNX1/HLXB9 and a network of other transcription factors. Mol Cell Biol. 2012;32(6):1189–1199. doi: 10.1128/MCB.06318-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Masui T, Swift GH, Hale MA, Meredith DM, Johnson JE, Macdonald RJ. Transcriptional autoregulation controls pancreatic Ptf1a expression during development and adulthood. Mol Cell Biol. 2008;28(17):5458–5468. doi: 10.1128/MCB.00549-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Seymour PA, Freude KK, Tran MN, Mayes EE, Jensen J, Kist R, Scherer G, Sander M. From the Cover: SOX9 is required for maintenance of the pancreatic progenitor cell pool. Proc Natl Acad Sci USA. 2007;104(6):1865–1870. doi: 10.1073/pnas.0609217104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lynn FC, Smith SB, Wilson ME, Yang KY, Nekrep N, German MS. Sox9 coordinates a transcriptional network in pancreatic progenitor cells. Proc Natl Acad Sci USA. 2007;104(25):10500–10505. doi: 10.1073/pnas.0704054104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Arceci RJ, King AA, Simon MC, Orkin SH, Wilson DB. Mouse GATA-4: a retinoic acid-inducible GATA-binding transcription factor expressed in endodermally derived tissues and heart. Mol Cell Biol. 1993;13(4):2235–2246. doi: 10.1128/mcb.13.4.2235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Molkentin JD. The zinc finger-containing transcription factors GATA-4, -5, and -6. Ubiquitously expressed regulators of tissue-specific gene expression. J Biol Chem. 2000;275(50):38949–38952. doi: 10.1074/jbc.R000029200. [DOI] [PubMed] [Google Scholar]
- 62.Patient RK, McGhee JD. The GATA family (vertebrates and invertebrates) Curr Opin Genet Dev. 2002;12(4):416–422. doi: 10.1016/s0959-437x(02)00319-2. [DOI] [PubMed] [Google Scholar]
- 63.Ketola I, Otonkoski T, Pulkkinen MA, Niemi H, Palgi J, Jacobsen CM, Wilson DB, Heikinheimo M. Transcription factor GATA-6 is expressed in the endocrine and GATA-4 in the exocrine pancreas. Mol Cell Endocrinol. 2004;226(1–2):51–57. doi: 10.1016/j.mce.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 64.Coffinier C, Thepot D, Babinet C, Yaniv M, Barra J. Essential role for the homeoprotein vHNF1/HNF1beta in visceral endoderm differentiation. Development. 1999;126(21):4785–4794. doi: 10.1242/dev.126.21.4785. [DOI] [PubMed] [Google Scholar]
- 65.Maestro MA, Boj SF, Luco RF, Pierreux CE, Cabedo J, Servitja JM, German MS, Rousseau GG, Lemaigre FP, Ferrer J. Hnf6 and Tcf2 (MODY5) are linked in a gene network operating in a precursor cell domain of the embryonic pancreas. Hum Mol Genet. 2003;12(24):3307–3314. doi: 10.1093/hmg/ddg355. [DOI] [PubMed] [Google Scholar]
- 66.Haumaitre C, Barbacci E, Jenny M, Ott MO, Gradwohl G, Cereghini S. Lack of TCF2/vHNF1 in mice leads to pancreas agenesis. Proc Natl Acad Sci USA. 2005;102(5):1490–1495. doi: 10.1073/pnas.0405776102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhang H, Ables ET, Pope CF, Washington MK, Hipkens S, Means AL, Path G, Seufert J, Costa RH, Leiter AB, Magnuson MA, Gannon M. Multiple, temporal-specific roles for HNF6 in pancreatic endocrine and ductal differentiation. Mech Dev. 2009;126(11–12):958–973. doi: 10.1016/j.mod.2009.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Poll AV, Pierreux CE, Lokmane L, Haumaitre C, Achouri Y, Jacquemin P, Rousseau GG, Cereghini S, Lemaigre FP. A vHNF1/TCF2-HNF6 cascade regulates the transcription factor network that controls generation of pancreatic precursor cells. Diabetes. 2006;55(1):61–69. [PubMed] [Google Scholar]
- 69.Li H, Arber S, Jessell TM, Edlund H. Selective agenesis of the dorsal pancreas in mice lacking homeobox gene Hlxb9. Nat Genet. 1999;23(1):67–70. doi: 10.1038/12669. [DOI] [PubMed] [Google Scholar]
- 70.Harrison KA, Thaler J, Pfaff SL, Gu H, Kehrl JH. Pancreas dorsal lobe agenesis and abnormal islets of Langerhans in Hlxb9-deficient mice. Nat Genet. 1999;23(1):71–75. doi: 10.1038/12674. [DOI] [PubMed] [Google Scholar]
- 71.Jorgensen MC, Ahnfelt-Ronne J, Hald J, Madsen OD, Serup P, Hecksher-Sorensen J. An illustrated review of early pancreas development in the mouse. Endocr Rev. 2007;28(6):685–705. doi: 10.1210/er.2007-0016. [DOI] [PubMed] [Google Scholar]
- 72.Wang J, Kilic G, Aydin M, Burke Z, Oliver G, Sosa-Pineda B. Prox1 activity controls pancreas morphogenesis and participates in the production of “secondary transition” pancreatic endocrine cells. Dev Biol. 2005;286(1):182–194. doi: 10.1016/j.ydbio.2005.07.021. [DOI] [PubMed] [Google Scholar]
- 73.Westmoreland JJ, Kilic G, Sartain C, Sirma S, Blain J, Rehg J, Harvey N, Sosa-Pineda B. Pancreas-specific deletion of Prox1 affects development and disrupts homeostasis of the exocrine pancreas. Gastroenterology. 2012;142(4):999–1009. doi: 10.1053/j.gastro.2011.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gao N, LeLay J, Vatamaniuk MZ, Rieck S, Friedman JR, Kaestner KH. Dynamic regulation of Pdx1 enhancers by Foxa1 and Foxa2 is essential for pancreas development. Genes Dev. 2008;22(24):3435–3448. doi: 10.1101/gad.1752608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Servitja JM, Ferrer J. Transcriptional networks controlling pancreatic development and beta cell function. Diabetologia. 2004;47(4):597–613. doi: 10.1007/s00125-004-1368-9. [DOI] [PubMed] [Google Scholar]
- 76.Arda HE, Benitez CM, Kim SK. Gene regulatory networks governing pancreas development. Dev Cell. 2013;25(1):5–13. doi: 10.1016/j.devcel.2013.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pictet R, Rutter WJ. Development of the embryonic endocrine pancreas. In: Greep RO, Astwood EB, Steiner DF, Freinkel N, Geiger SR, editors. Handbook of physiology. Washington, DC: American Physiological Society; 1972. pp. 25–76. [Google Scholar]
- 78.Hald J, Sprinkel AE, Ray M, Serup P, Wright C, Madsen OD. Generation and characterization of Ptf1a antiserum and localization of Ptf1a in relation to Nkx6.1 and Pdx1 during the earliest stages of mouse pancreas development. J Histochem Cytochem. 2008;56(6):587–595. doi: 10.1369/jhc.2008.950675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Murtaugh LC, Stanger BZ, Kwan KM, Melton DA. Notch signaling controls multiple steps of pancreatic differentiation. Proc Natl Acad Sci USA. 2003;100(25):14920–14925. doi: 10.1073/pnas.2436557100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Afelik S, Qu X, Hasrouni E, Bukys MA, Deering T, Nieuwoudt S, Rogers W, Macdonald RJ, Jensen J. Notch-mediated patterning and cell fate allocation of pancreatic progenitor cells. Development. 2012;139(10):1744–1753. doi: 10.1242/dev.075804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Horn S, Kobberup S, Jorgensen MC, Kalisz M, Klein T, Kageyama R, Gegg M, Lickert H, Lindner J, Magnuson MA, Kong YY, Serup P, Ahnfelt-Ronne J, Jensen JN. Mind bomb 1 is required for pancreatic beta-cell formation. Proc Natl Acad Sci USA. 2012;109(19):7356–7361. doi: 10.1073/pnas.1203605109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Magenheim J, Ilovich O, Lazarus A, Klochendler A, Ziv O, Werman R, Hija A, Cleaver O, Mishani E, Keshet E, Dor Y. Blood vessels restrain pancreas branching, differentiation and growth. Development. 2011;138(21):4743–4752. doi: 10.1242/dev.066548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pierreux CE, Cordi S, Hick AC, Achouri Y, Ruiz de Almodovar C, Prevot PP, Courtoy PJ, Carmeliet P, Lemaigre FP. Epithelial: endothelial cross-talk regulates exocrine differentiation in developing pancreas. Dev Biol. 2010;347(1):216–227. doi: 10.1016/j.ydbio.2010.08.024. [DOI] [PubMed] [Google Scholar]
- 84.Rukstalis JM, Habener JF. Snail2, a mediator of epithelial-mesenchymal transitions, expressed in progenitor cells of the developing endocrine pancreas. Gene Expr Patterns. 2007;7(4):471–479. doi: 10.1016/j.modgep.2006.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cole L, Anderson M, Antin PB, Limesand SW. One process for pancreatic beta-cell coalescence into islets involves an epithelial-mesenchymal transition. J Endocrinol. 2009;203(1):19–31. doi: 10.1677/JOE-09-0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Metzger DE, Gasperowicz M, Otto F, Cross JC, Gradwohl G, Zaret KS. The transcriptional co-repressor Grg3/Tle3 promotes pancreatic endocrine progenitor delamination and beta-cell differentiation. Development. 2012;139(8):1447–1456. doi: 10.1242/dev.072892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Magenheim J, Klein AM, Stanger BZ, Ashery-Padan R, Sosa-Pineda B, Gu G, Dor Y. Ngn3(+) endocrine progenitor cells control the fate and morphogenesis of pancreatic ductal epithelium. Dev Biol. 2011;359(1):26–36. doi: 10.1016/j.ydbio.2011.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Beucher A, Martin M, Spenle C, Poulet M, Collin C, Gradwohl G. Competence of failed endocrine progenitors to give rise to acinar but not ductal cells is restricted to early pancreas development. Dev Biol. 2012;361(2):277–285. doi: 10.1016/j.ydbio.2011.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gouzi M, Kim YH, Katsumoto K, Johansson K, Grapin-Botton A. Neurogenin3 initiates stepwise delamination of differentiating endocrine cells during pancreas development. Dev Dyn. 2011;240(3):589–604. doi: 10.1002/dvdy.22544. [DOI] [PubMed] [Google Scholar]
- 90.Greiner TU, Kesavan G, Stahlberg A, Semb H. Rac1 regulates pancreatic islet morphogenesis. BMC Dev Biol. 2009;9:2. doi: 10.1186/1471-213X-9-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Schwitzgebel VM, Scheel DW, Conners JR, Kalamaras J, Lee JE, Anderson DJ, Sussel L, Johnson JD, German MS. Expression of neurogenin3 reveals an islet cell precursor population in the pancreas. Development. 2000;127(16):3533–3542. doi: 10.1242/dev.127.16.3533. [DOI] [PubMed] [Google Scholar]
- 92.Gradwohl G, Dierich A, LeMeur M, Guillemot F. Neurogenin3 is required for the development of the four endocrine cell lineages of the pancreas. Proc Natl Acad Sci USA. 2000;97(4):1607–1611. doi: 10.1073/pnas.97.4.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Apelqvist A, Li H, Sommer L, Beatus P, Anderson DJ, Honjo T, Hrabe de Angelis M, Lendahl U, Edlund H. Notch signalling controls pancreatic cell differentiation. Nature. 1999;400(6747):877–881. doi: 10.1038/23716. [DOI] [PubMed] [Google Scholar]
- 94.Johansson KA, Dursun U, Jordan N, Gu G, Beermann F, Gradwohl G, Grapin-Botton A. Temporal control of neurogenin3 activity in pancreas progenitors reveals competence windows for the generation of different endocrine cell types. Dev Cell. 2007;12(3):457–465. doi: 10.1016/j.devcel.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 95.Wang S, Yan J, Anderson DA, Xu Y, Kanal MC, Cao Z, Wright CV, Gu G. Neurog3 gene dosage regulates allocation of endocrine and exocrine cell fates in the developing mouse pancreas. Dev Biol. 2010;339(1):26–37. doi: 10.1016/j.ydbio.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ejarque M, Cervantes S, Pujadas G, Tutusaus A, Sanchez L, Gasa R. Neurogenin3 cooperates with Foxa2 to autoactivate its own expression. J Biol Chem. 2013;288(17):11705–11717. doi: 10.1074/jbc.M112.388173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lee JC, Smith SB, Watada H, Lin J, Scheel D, Wang J, Mirmira RG, German MS. Regulation of the pancreatic pro-endocrine gene neurogenin3. Diabetes. 2001;50(5):928–936. doi: 10.2337/diabetes.50.5.928. [DOI] [PubMed] [Google Scholar]
- 98.Yang YP, Thorel F, Boyer DF, Herrera PL, Wright CV. Context-specific alpha- to-beta-cell reprogramming by forced Pdx1 expression. Genes Dev. 2011;25(16):1680–1685. doi: 10.1101/gad.16875711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jensen J, Pedersen EE, Galante P, Hald J, Heller RS, Ishibashi M, Kageyama R, Guillemot F, Serup P, Madsen OD. Control of endodermal endocrine development by Hes-1. Nat Genet. 2000;24(1):36–44. doi: 10.1038/71657. [DOI] [PubMed] [Google Scholar]
- 100.Jensen J, Heller RS, Funder-Nielsen T, Pedersen EE, Lindsell C, Weinmaster G, Madsen OD, Serup P. Independent development of pancreatic alpha- and beta-cells from neurogenin3-expressing precursors: a role for the notch pathway in repression of premature differentiation. Diabetes. 2000;49(2):163–176. doi: 10.2337/diabetes.49.2.163. [DOI] [PubMed] [Google Scholar]
- 101.Shih HP, Kopp JL, Sandhu M, Dubois CL, Seymour PA, Grapin-Botton A, Sander M. A Notch-dependent molecular circuitry initiates pancreatic endocrine and ductal cell differentiation. Development. 2012;139(14):2488–2499. doi: 10.1242/dev.078634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Golson ML, Le Lay J, Gao N, Bramswig N, Loomes KM, Oakey R, May CL, White P, Kaestner KH. Jagged1 is a competitive inhibitor of Notch signaling in the embryonic pancreas. Mech Dev. 2009;126(8–9):687–699. doi: 10.1016/j.mod.2009.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cras-Meneur C, Li L, Kopan R, Permutt MA. Presenilins, Notch dose control the fate of pancreatic endocrine progenitors during a narrow developmental window. Genes Dev. 2009;23(17):2088–2101. doi: 10.1101/gad.1800209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ahnfelt-Ronne J, Jorgensen MC, Klinck R, Jensen JN, Fuchtbauer EM, Deering T, MacDonald RJ, Wright CV, Madsen OD, Serup P. Ptf1a-mediated control of Dll1 reveals an alternative to the lateral inhibition mechanism. Development. 2012;139(1):33–45. doi: 10.1242/dev.071761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Haumaitre C, Lenoir O, Scharfmann R. Histone deacetylase inhibitors modify pancreatic cell fate determination and amplify endocrine progenitors. Mol Cell Biol. 2008;28(20):6373–6383. doi: 10.1128/MCB.00413-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Cortijo C, Gouzi M, Tissir F, Grapin-Botton A. Planar cell polarity controls pancreatic beta cell differentiation and glucose homeostasis. Cell Rep. 2012;2(6):1593–1606. doi: 10.1016/j.celrep.2012.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Desgraz R, Herrera PL. Pancreatic neurogenin 3-expressing cells are unipotent islet precursors. Development. 2009;136(21):3567–3574. doi: 10.1242/dev.039214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Smith SB, Gasa R, Watada H, Wang J, Griffen SC, German MS. Neurogenin3 and hepatic nuclear factor 1 cooperate in activating pancreatic expression of Pax4. J Biol Chem. 2003;278(40):38254–38259. doi: 10.1074/jbc.M302229200. [DOI] [PubMed] [Google Scholar]
- 109.Mellitzer G, Bonne S, Luco RF, Van De Casteele M, Lenne-Samuel N, Collombat P, Mansouri A, Lee J, Lan M, Pipeleers D, Nielsen FC, Ferrer J, Gradwohl G, Heimberg H. IA1 is NGN3-dependent and essential for differentiation of the endocrine pancreas. EMBO J. 2006;25(6):1344–1352. doi: 10.1038/sj.emboj.7601011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Huang HP, Liu M, El-Hodiri HM, Chu K, Jamrich M, Tsai MJ. Regulation of the pancreatic islet-specific gene BETA2 (neuroD) by neurogenin 3. Mol Cell Biol. 2000;20(9):3292–3307. doi: 10.1128/mcb.20.9.3292-3307.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Watada H, Scheel DW, Leung J, German MS. Distinct gene expression programs function in progenitor and mature islet cells. J Biol Chem. 2003;278(19):17130–17140. doi: 10.1074/jbc.M213196200. [DOI] [PubMed] [Google Scholar]
- 112.Gasa R, Mrejen C, Leachman N, Otten M, Barnes M, Wang J, Chakrabarti S, Mirmira R, German M. Proendocrine genes coordinate the pancreatic islet differentiation program in vitro. Proc Natl Acad Sci USA. 2004;101(36):13245–13250. doi: 10.1073/pnas.0405301101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Wang S, Hecksher-Sorensen J, Xu Y, Zhao A, Dor Y, Rosenberg L, Serup P, Gu G. Myt1 and Ngn3 form a feed-forward expression loop to promote endocrine islet cell differentiation. Dev Biol. 2008;317(2):531–540. doi: 10.1016/j.ydbio.2008.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Smith SB, Qu HQ, Taleb N, Kishimoto NY, Scheel DW, Lu Y, Patch AM, Grabs R, Wang J, Lynn FC, Miyatsuka T, Mitchell J, Seerke R, Desir J, Vanden Eijnden S, Abramowicz M, Kacet N, Weill J, Renard ME, Gentile M, Hansen I, Dewar K, Hattersley AT, Wang R, Wilson ME, Johnson JD, Polychronakos C, German MS. Rfx6 directs islet formation and insulin production in mice and humans. Nature. 2010;463(7282):775–780. doi: 10.1038/nature08748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Soyer J, Flasse L, Raffelsberger W, Beucher A, Orvain C, Peers B, Ravassard P, Vermot J, Voz ML, Mellitzer G, Gradwohl G. Rfx6 is an Ngn3-dependent winged helix transcription factor required for pancreatic islet cell development. Development. 2010;137(2):203–212. doi: 10.1242/dev.041673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Petri A, Ahnfelt-Ronne J, Frederiksen KS, Edwards DG, Madsen D, Serup P, Fleckner J, Heller RS. The effect of neurogenin3 deficiency on pancreatic gene expression in embryonic mice. J Mol Endocrinol. 2006;37(2):301–316. doi: 10.1677/jme.1.02096. [DOI] [PubMed] [Google Scholar]
- 117.Gu G, Wells JM, Dombkowski D, Preffer F, Aronow B, Melton DA. Global expression analysis of gene regulatory pathways during endocrine pancreatic development. Development. 2004;131(1):165–179. doi: 10.1242/dev.00921. [DOI] [PubMed] [Google Scholar]
- 118.White P, May CL, Lamounier RN, Brestelli JE, Kaestner KH. Defining pancreatic endocrine precursors and their descendants. Diabetes. 2008;57(3):654–668. doi: 10.2337/db07-1362. [DOI] [PubMed] [Google Scholar]
- 119.Juhl K, Sarkar SA, Wong R, Jensen J, Hutton JC. Mouse pancreatic endocrine cell transcriptome defined in the embryonic Ngn3-null mouse. Diabetes. 2008;57(10):2755–2761. doi: 10.2337/db07-1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Oliver-Krasinski JM, Stoffers DA. On the origin of the beta cell. Genes Dev. 2008;22(15):1998–2021. doi: 10.1101/gad.1670808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Gierl MS, Karoulias N, Wende H, Strehle M, Birchmeier C. The zinc-finger factor Insm1 (IA-1) is essential for the development of pancreatic beta cells and intestinal endocrine cells. Genes Dev. 2006;20(17):2465–2478. doi: 10.1101/gad.381806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Naya FJ, Huang HP, Qiu Y, Mutoh H, DeMayo FJ, Leiter AB, Tsai MJ. Diabetes, defective pancreatic morphogenesis, and abnormal enteroendocrine differentiation in BETA2/neuroD-deficient mice. Genes Dev. 1997;11(18):2323–2334. doi: 10.1101/gad.11.18.2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Du A, Hunter CS, Murray J, Noble D, Cai CL, Evans SM, Stein R, May CL. Islet-1 is required for the maturation, proliferation, and survival of the endocrine pancreas. Diabetes. 2009;58(9):2059–2069. doi: 10.2337/db08-0987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Sussel L, Kalamaras J, Hartigan-O’Connor DJ, Meneses JJ, Pedersen RA, Rubenstein JL, German MS. Mice lacking the homeodomain transcription factor Nkx2.2 have diabetes due to arrested differentiation of pancreatic beta cells. Development. 1998;125(12):2213–2221. doi: 10.1242/dev.125.12.2213. [DOI] [PubMed] [Google Scholar]
- 125.Sander M, Sussel L, Conners J, Scheel D, Kalamaras J, Dela Cruz F, Schwitzgebel V, Hayes-Jordan A, German M. Homeobox gene Nkx6.1 lies downstream of Nkx2.2 in the major pathway of ß-cell formation in the pancreas. Development. 2000;127(24):5533–5540. doi: 10.1242/dev.127.24.5533. [DOI] [PubMed] [Google Scholar]
- 126.Henseleit KD, Nelson SB, Kuhlbrodt K, Hennings JC, Ericson J, Sander M. NKX6 transcription factor activity is required for alpha- and beta-cell development in the pancreas. Development. 2005;132(13):3139–3149. doi: 10.1242/dev.01875. [DOI] [PubMed] [Google Scholar]
- 127.Prado CL, Pugh-Bernard AE, Elghazi L, Sosa-Pineda B, Sussel L. Ghrelin cells replace insulin-producing beta cells in two mouse models of pancreas development. Proc Natl Acad Sci USA. 2004;101(9):2924–2929. doi: 10.1073/pnas.0308604100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Chao CS, Loomis ZL, Lee JE, Sussel L. Genetic identification of a novel NeuroD1 function in the early differentiation of islet alpha, PP and epsilon cells. Dev Biol. 2007;312(2):523–532. doi: 10.1016/j.ydbio.2007.09.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Mastracci TL, Anderson KR, Papizan JB, Sussel L. Regulation of Neurod1 contributes to the lineage potential of Neurogenin3+ endocrine precursor cells in the pancreas. PLoS Genet. 2013;9(2):e1003278. doi: 10.1371/journal.pgen.1003278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Mastracci TL, Wilcox CL, Arnes L, Panea C, Golden JA, May CL, Sussel L. Nkx2.2 and Arx genetically interact to regulate pancreatic endocrine cell development and endocrine hormone expression. Dev Biol. 2011;359(1):1–11. doi: 10.1016/j.ydbio.2011.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Bramswig NC, Kaestner KH. Transcriptional regulation of alpha-cell differentiation. Diabetes Obes Metab. 2011;13(Suppl 1):13–20. doi: 10.1111/j.1463-1326.2011.01440.x. [DOI] [PubMed] [Google Scholar]
- 132.Collombat P, Mansouri A, Hecksher-Sorensen J, Serup P, Krull J, Gradwohl G, Gruss P. Opposing actions of Arx and Pax4 in endocrine pancreas development. Genes Dev. 2003;17(20):2591–2603. doi: 10.1101/gad.269003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Sosa-Pineda B, Chowdhury K, Torres M, Oliver G, Gruss P. The Pax4 gene is essential for differentiation of insulin-producing β cells in the mammalian pancreas. Nature. 1997;386:399–402. doi: 10.1038/386399a0. [DOI] [PubMed] [Google Scholar]
- 134.Collombat P, Xu X, Ravassard P, Sosa-Pineda B, Dussaud S, Billestrup N, Madsen OD, Serup P, Heimberg H, Mansouri A. The ectopic expression of Pax4 in the mouse pancreas converts progenitor cells into alpha and subsequently beta cells. Cell. 2009;138(3):449–462. doi: 10.1016/j.cell.2009.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Collombat P, Hecksher-Sorensen J, Krull J, Berger J, Riedel D, Herrera PL, Serup P, Mansouri A. Embryonic endocrine pancreas and mature beta cells acquire alpha and PP cell phenotypes upon Arx misexpression. J Clin Invest. 2007;117(4):961–970. doi: 10.1172/JCI29115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Schaffer AE, Taylor BL, Benthuysen JR, Liu J, Thorel F, Yuan W, Jiao Y, Kaestner KH, Herrera PL, Magnuson MA, May CL, Sander M. Nkx6.1 controls a gene regulatory network required for establishing and maintaining pancreatic Beta cell identity. PLoS Genet. 2013;9(1):e1003274. doi: 10.1371/journal.pgen.1003274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Gannon M, Ables ET, Crawford L, Lowe D, Offield MF, Magnuson MA, Wright CV. pdx-1 function is specifically required in embryonic beta cells to generate appropriate numbers of endocrine cell types and maintain glucose homeostasis. Dev Biol. 2008;314(2):406–417. doi: 10.1016/j.ydbio.2007.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Papizan JB, Singer RA, Tschen SI, Dhawan S, Friel JM, Hipkens SB, Magnuson MA, Bhushan A, Sussel L. Nkx2.2 repressor complex regulates islet beta-cell specification and prevents beta-to-alpha-cell reprogramming. Genes Dev. 2011;25(21):2291–2305. doi: 10.1101/gad.173039.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Dhawan S, Georgia S, Tschen SI, Fan G, Bhushan A. Pancreatic beta cell identity is maintained by DNA methylation-mediated repression of Arx. Dev Cell. 2011;20(4):419–429. doi: 10.1016/j.devcel.2011.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Thorel F, Nepote V, Avril I, Kohno K, Desgraz R, Chera S, Herrera PL. Conversion of adult pancreatic alpha-cells to beta-cells after extreme beta-cell loss. Nature. 2010;464(7292):1149–1154. doi: 10.1038/nature08894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Esni F, Ghosh B, Biankin AV, Lin JW, Albert MA, Yu X, MacDonald RJ, Civin CI, Real FX, Pack MA, Ball DW, Leach SD. Notch inhibits Ptf1 function and acinar cell differentiation in developing mouse and zebrafish pancreas. Development. 2004;131(17):4213–4224. doi: 10.1242/dev.01280. [DOI] [PubMed] [Google Scholar]
- 142.Masui T, Swift GH, Deering T, Shen C, Coats WS, Long Q, Elsasser HP, Magnuson MA, MacDonald RJ. Replacement of Rbpj with Rbpjl in the PTF1 complex controls the final maturation of pancreatic acinar cells. Gastroenterology. 2010;139(1):270–280. doi: 10.1053/j.gastro.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Decker K, Goldman DC, Grasch CL, Sussel L. Gata6 is an important regulator of mouse pancreas development. Dev Biol. 2006;298(2):415–429. doi: 10.1016/j.ydbio.2006.06.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Martinelli P, Canamero M, Del Pozo N, Madriles F, Zapata A, Real FX. Gata6 is required for complete acinar differentiation and maintenance of the exocrine pancreas in adult mice. Gut. 2012 doi: 10.1136/gutjnl-2012-303328. [DOI] [PubMed] [Google Scholar]
- 145.von Figura G, Morris JPt, Wright CV, Hebrok M. Nr5a2 maintains acinar cell differentiation and constrains oncogenic Kras-mediated pancreatic neoplastic initiation. Gut. 2013 doi: 10.1136/gutjnl-2012-304287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Pin CL, Rukstalis JM, Johnson C, Konieczny SF. The bHLH transcription factor Mist1 is required to maintain exocrine pancreas cell organization and acinar cell identity. J Cell Biol. 2001;155(4):519–530. doi: 10.1083/jcb.200105060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Holmstrom SR, Deering T, Swift GH, Poelwijk FJ, Mangelsdorf DJ, Kliewer SA, MacDonald RJ. LRH-1 and PTF1-L coregulate an exocrine pancreas-specific transcriptional network for digestive function. Genes Dev. 2011;25(16):1674–1679. doi: 10.1101/gad.16860911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.MacDonald RJ, Swift GH, Real FX. Transcriptional control of acinar development and homeostasis. Prog Mol Biol Transl Sci. 2010;97:1–40. doi: 10.1016/B978-0-12-385233-5.00001-5. [DOI] [PubMed] [Google Scholar]
- 149.Reichert M, Rustgi AK. Pancreatic ductal cells in development, regeneration, and neoplasia. J Clin Investig. 2011;121(12):4572–4578. doi: 10.1172/JCI57131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Pierreux CE, Poll AV, Kemp CR, Clotman F, Maestro MA, Cordi S, Ferrer J, Leyns L, Rousseau GG, Lemaigre FP. The transcription factor hepatocyte nuclear factor-6 controls the development of pancreatic ducts in the mouse. Gastroenterology. 2006;130(2):532–541. doi: 10.1053/j.gastro.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 151.Cano DA, Murcia NS, Pazour GJ, Hebrok M. Orpk mouse model of polycystic kidney disease reveals essential role of primary cilia in pancreatic tissue organization. Development. 2004;131(14):3457–3467. doi: 10.1242/dev.01189. [DOI] [PubMed] [Google Scholar]
- 152.Cano DA, Sekine S, Hebrok M. Primary cilia deletion in pancreatic epithelial cells results in cyst formation and pancreatitis. Gastroenterology. 2006;131(6):1856–1869. doi: 10.1053/j.gastro.2006.10.050. [DOI] [PubMed] [Google Scholar]
- 153.Reichert M, Takano S, von Burstin J, Kim SB, Lee JS, Ihida-Stansbury K, Hahn C, Heeg S, Schneider G, Rhim AD, Stanger BZ, Rustgi AK. The Prrx1 homeodomain transcription factor plays a central role in pancreatic regeneration and carcinogenesis. Genes Dev. 2013;27(3):288–300. doi: 10.1101/gad.204453.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Piper K, Brickwood S, Turnpenny LW, Cameron IT, Ball SG, Wilson DI, Hanley NA. Beta cell differentiation during early human pancreas development. J Endocrinol. 2004;181(1):11–23. doi: 10.1677/joe.0.1810011. [DOI] [PubMed] [Google Scholar]
- 155.Polak M, Bouchareb-Banaei L, Scharfmann R, Czernichow P. Early pattern of differentiation in the human pancreas. Diabetes. 2000;49(2):225–232. doi: 10.2337/diabetes.49.2.225. [DOI] [PubMed] [Google Scholar]
- 156.Lyttle BM, Li J, Krishnamurthy M, Fellows F, Wheeler MB, Goodyer CG, Wang R. Transcription factor expression in the developing human fetal endocrine pancreas. Diabetologia. 2008;51(7):1169–1180. doi: 10.1007/s00125-008-1006-z. [DOI] [PubMed] [Google Scholar]
- 157.Sarkar SA, Kobberup S, Wong R, Lopez AD, Quayum N, Still T, Kutchma A, Jensen JN, Gianani R, Beattie GM, Jensen J, Hayek A, Hutton JC. Global gene expression profiling and histochemical analysis of the developing human fetal pancreas. Diabetologia. 2008;51(2):285–297. doi: 10.1007/s00125-007-0880-0. [DOI] [PubMed] [Google Scholar]
- 158.Jeon J, Correa-Medina M, Ricordi C, Edlund H, Diez JA. Endocrine cell clustering during human pancreas development. J Histochem Cytochem. 2009;57(9):811–824. doi: 10.1369/jhc.2009.953307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Jennings RE, Berry AA, Kirkwood-Wilson R, Roberts NA, Hearn T, Salisbury RJ, Blaylock J, Hanley KP, Hanley NA. Development of the human pancreas from foregut to endocrine commitment. Diabetes. 2013;62(10):3514–3522. doi: 10.2337/db12-1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Capito C, Simon MT, Aiello V, Clark A, Aigrain Y, Ravassard P, Scharfmann R. The mouse muscle as an ectopic permissive site for human pancreatic development. Diabetes. 2013 doi: 10.2337/db13-0554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Brissova M, Fowler MJ, Nicholson WE, Chu A, Hirshberg B, Harlan DM, Powers AC. Assessment of human pancreatic islet architecture and composition by laser scanning confocal microscopy. J Histochem Cytochem. 2005;53(9):1087–1097. doi: 10.1369/jhc.5C6684.2005. [DOI] [PubMed] [Google Scholar]
- 162.Cabrera O, Berman DM, Kenyon NS, Ricordi C, Berggren PO, Caicedo A. The unique cytoarchitecture of human pancreatic islets has implications for islet cell function. Proc Natl Acad Sci USA. 2006;103(7):2334–2339. doi: 10.1073/pnas.0510790103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Bosco D, Armanet M, Morel P, Niclauss N, Sgroi A, Muller YD, Giovannoni L, Parnaud G, Berney T. Unique arrangement of alpha- and beta-cells in human islets of Langerhans. Diabetes. 2010;59(5):1202–1210. doi: 10.2337/db09-1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Riedel MJ, Asadi A, Wang R, Ao Z, Warnock GL, Kieffer TJ. Immunohistochemical characterisation of cells co-producing insulin and glucagon in the developing human pancreas. Diabetologia. 2012;55(2):372–381. doi: 10.1007/s00125-011-2344-9. [DOI] [PubMed] [Google Scholar]
- 165.Dai C, Brissova M, Hang Y, Thompson C, Poffenberger G, Shostak A, Chen Z, Stein R, Powers AC. Islet-enriched gene expression and glucose-induced insulin secretion in human and mouse islets. Diabetologia. 2012;55(3):707–718. doi: 10.1007/s00125-011-2369-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Dorrell C, Schug J, Lin CF, Canaday PS, Fox AJ, Smirnova O, Bonnah R, Streeter PR, Stoeckert CJ, Jr, Kaestner KH, Grompe M. Transcriptomes of the major human pancreatic cell types. Diabetologia. 2011;54(11):2832–2844. doi: 10.1007/s00125-011-2283-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.McKnight KD, Wang P, Kim SK. Deconstructing pancreas development to reconstruct human islets from pluripotent stem cells. Cell Stem Cell. 2010;6(4):300–308. doi: 10.1016/j.stem.2010.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Castaing M, Peault B, Basmaciogullari A, Casal I, Czernichow P, Scharfmann R. Blood glucose normalization upon transplantation of human embryonic pancreas into beta-cell-deficient SCID mice. Diabetologia. 2001;44(11):2066–2076. doi: 10.1007/s001250100012. [DOI] [PubMed] [Google Scholar]
- 169.Mayhew CN, Wells JM. Converting human pluripotent stem cells into beta-cells: recent advances and future challenges. Curr Opin Organ Transplant. 2010;15(1):54–60. doi: 10.1097/MOT.0b013e3283337e1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Nostro MC, Keller G. Generation of beta cells from human pluripotent stem cells: potential for regenerative medicine. Semin Cell Dev Biol. 2012;23(6):701–710. doi: 10.1016/j.semcdb.2012.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Kroon E, Martinson LA, Kadoya K, Bang AG, Kelly OG, Eliazer S, Young H, Richardson M, Smart NG, Cunningham J, Agulnick AD, D’Amour KA, Carpenter MK, Baetge EE. Pancreatic endoderm derived from human embryonic stem cells generates glucose-responsive insulin-secreting cells in vivo. Nat Biotechnol. 2008;26(4):443–452. doi: 10.1038/nbt1393. [DOI] [PubMed] [Google Scholar]
- 172.D'Amour KA, Bang AG, Eliazer S, Kelly OG, Agulnick AD, Smart NG, Moorman MA, Kroon E, Carpenter MK, Baetge EE. Production of pancreatic hormone-expressing endocrine cells from human embryonic stem cells. Nat Biotechnol. 2006;24(11):1392–1401. doi: 10.1038/nbt1259. [DOI] [PubMed] [Google Scholar]
- 173.Xie R, Everett LJ, Lim HW, Patel NA, Schug J, Kroon E, Kelly OG, Wang A, D’Amour KA, Robins AJ, Won KJ, Kaestner KH, Sander M. Dynamic chromatin remodeling mediated by Polycomb proteins orchestrates pancreatic differentiation of human embryonic stem cells. Cell Stem Cell. 2013;12(2):224–237. doi: 10.1016/j.stem.2012.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Wang P, Rodriguez RT, Wang J, Ghodasara A, Kim SK. Targeting SOX17 in human embryonic stem cells creates unique strategies for isolating and analyzing developing endoderm. Cell Stem Cell. 2011;8(3):335–346. doi: 10.1016/j.stem.2011.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Stoffers DA, Zinkin NT, Stanojevic V, Clarke WL, Habener JF. Pancreatic agenesis attributable to a single nucleotide deletion in the human IPF1 gene coding sequence. Nat Genet. 1997;15(1):106–110. doi: 10.1038/ng0197-106. [DOI] [PubMed] [Google Scholar]
- 176.Sellick GS, Barker KT, Stolte-Dijkstra I, Fleischmann C, Coleman RJ, Garrett C, Gloyn AL, Edghill EL, Hattersley AT, Wellauer PK, Goodwin G, Houlston RS. Mutations in PTF1A cause pancreatic and cerebellar agenesis. Nat Genet. 2004;36(12):1301–1305. doi: 10.1038/ng1475. [DOI] [PubMed] [Google Scholar]
- 177.Rubio-Cabezas O, Minton JA, Kantor I, Williams D, Ellard S, Hattersley AT. Homozygous mutations in NEUROD1 are responsible for a novel syndrome of permanent neonatal diabetes and neurological abnormalities. Diabetes. 2010;59(9):2326–2331. doi: 10.2337/db10-0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Senee V, Chelala C, Duchatelet S, Feng D, Blanc H, Cossec JC, Charon C, Nicolino M, Boileau P, Cavener DR, Bougneres P, Taha D, Julier C. Mutations in GLIS3 are responsible for a rare syndrome with neonatal diabetes mellitus and congenital hypothyroidism. Nat Genet. 2006;38(6):682–687. doi: 10.1038/ng1802. [DOI] [PubMed] [Google Scholar]
- 179.Rubio-Cabezas O, Jensen JN, Hodgson MI, Codner E, Ellard S, Serup P, Hattersley AT. Permanent neonatal diabetes and enteric anendocrinosis associated with biallelic mutations in NEUROG3. Diabetes. 2011;60(4):1349–1353. doi: 10.2337/db10-1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Yamagata K, Furuta H, Oda N, Kaisaki PJ, Menzel S, Cox NJ, Fajans SS, Signorini S, Stoffel M, Bell GI. Mutations in the hepatocyte nuclear factor-4alpha gene in maturity-onset diabetes of the young (MODY1) Nature. 1996;384(6608):458–460. doi: 10.1038/384458a0. [DOI] [PubMed] [Google Scholar]
- 181.Horikawa Y, Iwasaki N, Hara M, Furuta H, Hinokio Y, Cockburn BN, Lindner T, Yamagata K, Ogata M, Tomonaga O, Kuroki H, Kasahara T, Iwamoto Y, Bell GI. Mutation in hepatocyte nuclear factor-1 beta gene (TCF2) associated with MODY. Nat Genet. 1997;17(4):384–385. doi: 10.1038/ng1297-384. [DOI] [PubMed] [Google Scholar]
- 182.Yamagata K, Oda N, Kaisaki PJ, Menzel S, Furuta H, Vaxillaire M, Southam L, Cox RD, Lathrop GM, Boriraj VV, Chen X, Cox NJ, Oda Y, Yano H, Le Beau MM, Yamada S, Nishigori H, Takeda J, Fajans SS, Hattersley AT, Iwasaki N, Hansen T, Pedersen O, Polonsky KS, Bell GI, et al. Mutations in the hepatocyte nuclear factor-1alpha gene in maturity-onset diabetes of the young (MODY3) Nature. 1996;384(6608):455–458. doi: 10.1038/384455a0. [DOI] [PubMed] [Google Scholar]
- 183.Rodriguez-Segui S, Akerman I, Ferrer J. GATA believe it: new essential regulators of pancreas development. J Clin Investig. 2012;122(10):3469–3471. doi: 10.1172/JCI65751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Kitamura K, Yanazawa M, Sugiyama N, Miura H, Iizuka-Kogo A, Kusaka M, Omichi K, Suzuki R, Kato-Fukui Y, Kamiirisa K, Matsuo M, Kamijo S, Kasahara M, Yoshioka H, Ogata T, Fukuda T, Kondo I, Kato M, Dobyns WB, Yokoyama M, Morohashi K. Mutation of ARX causes abnormal development of forebrain and testes in mice and X-linked lissencephaly with abnormal genitalia in humans. Nat Genet. 2002;32(3):359–369. doi: 10.1038/ng1009. [DOI] [PubMed] [Google Scholar]
- 185.Itoh M, Takizawa Y, Hanai S, Okazaki S, Miyata R, Inoue T, Akashi T, Hayashi M, Goto Y. Partial loss of pancreas endocrine and exocrine cells of human ARX-null mutation: consideration of pancreas differentiation. Differentiation. 2010;80(2–3):118–122. doi: 10.1016/j.diff.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 186.Lango Allen H, Flanagan SE, Shaw-Smith C, De Franco E, Akerman I, Caswell R, Ferrer J, Hattersley AT, Ellard S. GATA6 haploinsufficiency causes pancreatic agenesis in humans. Nat Genet. 2012;44(1):20–22. doi: 10.1038/ng.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.De Franco E, Shaw-Smith C, Flanagan SE, Shepherd MH, Hattersley AT, Ellard S. GATA6 mutations cause a broad phenotypic spectrum of diabetes from pancreatic agenesis to adult-onset diabetes without exocrine insufficiency. Diabetes. 2013;62(3):993–997. doi: 10.2337/db12-0885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Rubio-Cabezas O, Minton JA, Caswell R, Shield JP, Deiss D, Sumnik Z, Cayssials A, Herr M, Loew A, Lewis V, Ellard S, Hattersley AT. Clinical heterogeneity in patients with FOXP3 mutations presenting with permanent neonatal diabetes. Diabetes Care. 2009;32(1):111–116. doi: 10.2337/dc08-1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Bonnefond A, Vaillant E, Philippe J, Skrobek B, Lobbens S, Yengo L, Huyvaert M, Cave H, Busiah K, Scharfmann R, Polak M, Abdul-Rasoul M, Froguel P, Vaxillaire M. Transcription factor gene MNX1 is a novel cause of permanent neonatal diabetes in a consanguineous family. Diabetes Metab. 2013;39(3):276–280. doi: 10.1016/j.diabet.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 190.Malecki MT, Jhala US, Antonellis A, Fields L, Doria A, Orban T, Saad M, Warram JH, Montminy M, Krolewski AS. Mutations in NEUROD1 are associated with the development of type 2 diabetes mellitus. Nat Genet. 1999;23(3):323–328. doi: 10.1038/15500. [DOI] [PubMed] [Google Scholar]
- 191.Jensen JN, Rosenberg LC, Hecksher-Sorensen J, Serup P. Mutant neurogenin-3 in congenital malabsorptive diarrhea. N Engl J Med. 2007;356(17):1781–1782. doi: 10.1056/NEJMc063247. [DOI] [PubMed] [Google Scholar]
- 192.Wang J, Cortina G, Wu SV, Tran R, Cho JH, Tsai MJ, Bailey TJ, Jamrich M, Ament ME, Treem WR, Hill ID, Vargas JH, Gershman G, Farmer DG, Reyen L, Martin MG. Mutant neurogenin-3 in congenital malabsorptive diarrhea. N Engl J Med. 2006;355(3):270–280. doi: 10.1056/NEJMoa054288. [DOI] [PubMed] [Google Scholar]
- 193.Plengvidhya N, Kooptiwut S, Songtawee N, Doi A, Furuta H, Nishi M, Nanjo K, Tantibhedhyangkul W, Boonyasrisawat W, Yenchitsomanus PT, Doria A, Banchuin N. PAX4 mutations in Thais with maturity onset diabetes of the young. J Clin Endocrinol Metab. 2007;92(7):2821–2826. doi: 10.1210/jc.2006-1927. [DOI] [PubMed] [Google Scholar]
- 194.Stoffers DA, Ferrer J, Clarke WL, Habener JF. Early-onset type-II diabetes mellitus (MODY4) linked to IPF1. Nat Genet. 1997;17(2):138–139. doi: 10.1038/ng1097-138. [DOI] [PubMed] [Google Scholar]
- 195.Piper K, Ball SG, Keeling JW, Mansoor S, Wilson DI, Hanley NA. Novel SOX9 expression during human pancreas development correlates to abnormalities in Campomelic dysplasia. Mech Dev. 2002;116(1–2):223–226. doi: 10.1016/s0925-4773(02)00145-4. [DOI] [PubMed] [Google Scholar]