Abstract
The suboptimal performance of rotavirus (RV) vaccines in developing countries and in animals necessitates further research on the development of novel therapeutics and control strategies. To initiate infection, RV interacts with cell-surface O-glycans, including histo-blood group antigens (HBGAs). We have previously demonstrated that certain non-pathogenic bacteria express HBGA- like substances (HBGA+) capable of binding RV particles in vitro. We hypothesized that HBGA+ bacteria can bind RV particles in the gut lumen protecting against RV species A (RVA), B (RVB), and C (RVC) infection in vivo. In this study, germ-free piglets were colonized with HBGA+ or HBGA- bacterial cocktail and infected with RVA/RVB/RVC of different genotypes. Diarrhea severity, virus shedding, immunoglobulin A (IgA) Ab titers, and cytokine levels were evaluated. Overall, colonization with HBGA+ bacteria resulted in reduced diarrhea severity and virus shedding compared to the HBGA- bacteria. Consistent with our hypothesis, the reduced severity of RV disease and infection was not associated with significant alterations in immune responses. Additionally, colonization with HBGA+ bacteria conferred beneficial effects irrespective of the piglet HBGA phenotype. These findings are the first experimental evidence that probiotic performance in vivo can be improved by including HBGA+ bacteria, providing decoy epitopes for broader/more consistent protection against diverse RVs.
Keywords: probiotics, rotavirus infection, histo-blood group antigens, glycans, diarrhea, shedding
1. Introduction
Rotavirus (RV) is the major causative agent of acute gastroenteritis and is associated with an increased risk of secondary bacterial infections in children and young animals globally [1]. In children younger than 5 years of age, severe RV-induced diarrhea may lead to hospitalization and even death [2,3]. RV mainly targets the mature terminally differentiated intestinal epithelial cells (IECs), primarily of the ileum and jejunum [4,5]. Among a variety of RV receptors, cellular glycans have been shown to play a major role as attachment sites [5]. Specifically, histo-blood group antigens (HBGAs), including the antigens of the ABO blood group system, have been shown to play a critical role in determining RV species/genotype-specific binding and disease [5,6,7,8]. O and A but not B have been described for pigs (AO system) [9,10]. This is determined by the presence of only two alleles, A and O, in the porcine ABO gene [11,12], resulting in the existence of four phenotypes: A, Aweak, O, and “H-A-” [10]. Based on reactivity with “anti-A” and “anti-H” antibodies, pigs can be H−A+ (A phenotype), H+A+ (Aweak phenotype), H+A− (O phenotype), and H−A- (H−A- phenotype) [12]. Our previous studies have demonstrated that the piglet HBGA phenotype affects RVA/RVC replication levels in vitro (in porcine ileal enteroids) [6,7]. This underscores the importance of considering the AO phenotype as an important factor influencing RV replication in vivo.
Before reaching its principal target, IECs, RV must penetrate the mucus layer, which protects IECs against enteric pathogens, including RV [13], and provides a niche for intestinal commensals [14]. There is growing evidence that several members of non-pathogenic bacteria produce glycans recognized by human HBGA-specific monoclonal antibodies [15,16,17,18,19]. Thus, while cellular HBGAs aid RV attachment, bacterial HBGAs might act as decoy epitopes, preventing RV attachment to the IECs. Our recent study has demonstrated the ability of some Gram-positive and Gram-negative non-pathogenic bacteria to express a variety of HBGAs and bind RV of different species (RVA/RVC) and genotypes in a genotype-specific manner [16,20], suggesting the potential role of these bacteria as decoy receptors for RV (Table S1). However, the impact of these HBGA-expressing bacteria on RV infection and disease in vivo remains unknown.
While probiotic supplementation is generally beneficial in terms of the overall performance of livestock animals [21], feed conversion efficiency, and in reducing post-weaning diarrhea in pigs [21,22], it does not always meet producer expectations mostly due to the inconsistent outcomes [23,24,25,26]. This is likely due to variable dosages and types of probiotics used, animal diet, and age. While most studies on the impact of probiotics demonstrate immune-mediated decreases in viral shedding and clinical disease severity [20,27,28,29], the data on the role of direct bacteria–RV interactions are limited. We hypothesized that colonization of germ-free (GF) piglets with HBGA expressing (HBGA+) vs. non-expressing (HBGA-) bacteria would lead to decreased replication of RV, resulting in reduced diarrhea severity and virus shedding after virus inoculation, and that these beneficial effects will be independent of the probiotic-induced immunomodulation. Thus, the goal of this study was to evaluate the protective effects of HBGA+ vs. HBGA- bacteria against RVA, RVB, and RVC infection in vivo.
2. Materials and Methods
2.1. Commensal Bacteria
We used two commensal facultative anaerobic bacteria (L. brevis, S. bovis) and four obligate anaerobes (B. adolescentis, B. longum, B. thetaiotaomicron, and C. clostridioforme) previously isolated from the gut of healthy pigs (kindly provided by Dr. David Francis, South Dakota State University, Brookings, SD, USA). An additional facultative anaerobe, E. coli G58 (kindly provided by Dr. Carlton Gyles, University of Guelph, Guelph, ON, Canada) was also included in this study. All strains were cultured under aerobic (E. coli G58) and anaerobic conditions (S. bovis, B. thetaiotaomicron, B. adolescentis, L. brevis, C. clostridioforme, B. longum); the latter were generated using the GasPakTM EZ Anaerobe Container System Sachets (BD, Franklin Lakes, NJ, USA). All bacteria were enumerated as described previously [30]. Selected media and growth conditions for preparing bacterial cultures were reported previously [16].
2.2. Rotaviruses
Intestinal contents of GF piglets containing rotavirus A (RVA): Wa G1P[8] [31], RV0084 G9P[13] [32], Gottfried G4P[6] [33], OSU G5P[7]; rotavirus B (RVB): Ohio [34] (non-typed); and rotavirus C (RVC): Cowden G1P[1] [35]; RV0104 G3P[18]; RV0143 G6P[5] [32], were used to orally inoculate piglets at a dose of 1 × 106 fluorescent focus units (FFU).
2.3. Animal Experiments
All our animal experiments were approved by the Institutional Animal Care and Use Committee (IACUC) at Ohio State University (protocols #2009A0146, #2010A00000088). Near-term sows (Landrace × Yorkshire × Duroc crossbred) were purchased from the Ohio State University swine center facility/Shoup Brothers Farm LTD, Orville, OH, USA. GF piglets were derived by cesarean section and maintained as described previously [36]. On the 2nd day of life, rectal swabs were taken from all the piglets, and sterility was confirmed by culturing of rectal swabs in blood agar plates and thioglycolate broth culture. The presence of bacteria in the intestine vs. GF conditions has been shown to play a crucial role in nutrient absorption [37], immune system development [38], glycosylation profiles, and maintaining intestinal epithelial cell integrity [39], thus impacting immune responses to pathogens, including RV [40,41,42]. Therefore, to evaluate the anti-RV properties of the HBGA+ bacterial cocktail, instead of using non-colonized piglets, we used the HBGA- bacterial cocktail as a control. Five- to seven-day-old GF piglets were supplemented for 5 consecutive days with one of the commensal bacteria cocktails (1 × 105 colony-forming units, CFU, of each strain per pig) containing (1) HBGA-expressing bacteria (HBGA+): Escherichia coli G-58, Bifidobacterium adolescentis, Bacteroides thetaiotaomicron, Streptococcus bovis, and Clostridium clostridioforme; (2) HBGA-non-expressing bacteria (HBGA-): Lactobacillus brevis and Bifidobacterium longum. The HBGA expression profiles of the bacterial strains used in this study were evaluated in our previous study [16]. On day 5 of supplementation, rectal swabs were collected for enumeration of fecal bacterial shedding [30] in the colonized pigs. Additionally, the presence of each bacterial strain was confirmed using PCR, as described previously [43] (primers [44,45,46,47,48,49] are listed in Table S2). On day 5 of supplementation, all piglets were inoculated with individual RVA/RVB/RVC strains at a dose of 1 × 106 FFU/piglet. After the RV challenge, rectal swabs were collected daily to assess RV shedding and diarrhea severity, as previously described [50]. Blood samples were collected on days 0, 3, 7, and 11 post-infection (dpi) to evaluate the IgA Ab titers and canonical innate and pro-inflammatory cytokine responses to RV infection. An innate immune response early-response cytokine IFN-α was evaluated at dpi 0 and dpi 3, while TNF-α, IL-10, and IL-22 were assessed at dpi 0 and dpi 11 to capture the late phase of the immune response [51,52,53]. All piglets were euthanized at dpi 11, and small and large intestinal contents (SIC and LIC) were collected, resuspended at a 1:1 ratio in MEM with a protease inhibitor cocktail containing 250 µg/mL of trypsin inhibitor and 50 µg/mL of leupeptin (Sigma, Saint Louis, MO, USA), and stored at −70 °C to evaluate the local IgA response. Ileum sections were collected to determine porcine HBGA phenotype.
2.4. Rotavirus Fecal Shedding
Cell culture immunofluorescence (CCIF) assay was used to quantify RVA as previously described [54]. The final RV titers were calculated and expressed as the reciprocal of the highest dilution showing positive fluorescing cells. To detect/quantify RVC and RVB, real-time RT-PCR was used as previously described [55,56] (primers are listed in Table S2).
2.5. Rotavirus A-Specific Antibody (Ab) ELISA Assay
Cell-culture-adapted RVA OSU G5P[7] and Wa G1P[8] strains were used to inoculate MA-104 cells, as described previously [57]. Infected cells were frozen/thawed 3 times, and after centrifugation, the supernatant was used as an antigen for IgA Ab ELISA (mock-infected MA-104 cells were used as a control). RV IgA ELISA was performed as described previously [58]. The RVA-specific IgA Ab titers were expressed as the reciprocal of the highest dilution that had a corrected optical density (OD)450 value (sample OD450 in the RVA antigen-coated well minus sample OD450 in the mock antigen-coated well) greater than the cut-off value (the mean + three standard deviations of negative control samples).
2.6. RVC ELISA
Ninety-six-well plates (Nunc Maxisorp, Thermo Scientific Pierce, Rockford, IL, USA) were coated with lysates (normalized for total protein content) of High-Five cells (Mock) or High-Five cells infected with the recombinant baculovirus containing the VP6 gene of RVC G1P[1] diluted 1:50 in carbonate–bicarbonate (coating) buffer (pH 9.6). After overnight incubation at 4 °C, the plates were rinsed twice with PBS containing 0.05% Tween-20 (PBST) and blocked with PBST containing 2% non-fat dry milk, and then incubated at 37 °C for 1 h. After rinsing the plates 5 times with PBST, seven 3-fold dilutions of serum samples (starting at 1:5) were added to both Mock/VP6-coated plates and incubated at 37 °C for 1 h. The plates were rinsed 5 times with PBST, and the secondary antibody, horseradish peroxidase-conjugated goat anti-porcine IgA antibody (Bio-Rad, Hercules, CA, USA), was added and incubated at 37 °C for 1 h. Then, the plates were rinsed 5 times with PBST, developed with TMB 2-Component Microwell Peroxidase Substrate Kit, and stopped with TMB Stop Solution (both from SeraCare Life Sciences Inc. Milford, MA, USA), and the OD values were read at 450 nm using SoftMax Pro 7.1 (Molecular Devices, LLC., San Jose, CA, USA). The antibody titers were determined as described previously [57].
2.7. Cytokine ELISA
Porcine TNF-α, INF-α, IL-10, and IL-22 ELISA kits were used as described in the manufacturer’s recommendations (Thermo Scientific Pierce, Rockford, IL, USA).
2.8. HBGA Immunohistochemistry
To determine porcine HBGA phenotype, formalin-fixed ileal sections [59] were stained with HBGA-A- or -H-specific mouse monoclonal antibodies (mAb) (Biolegend, San Diego, CA, USA) as described previously [6].
2.9. Statistical Analysis
All statistical analyses were performed using GraphPad Prism version 8 (GraphPad Software, Inc., La Jolla, CA, USA). The mean duration of diarrhea and fecal RV shedding post-challenge were analyzed using an unpaired t-test. Log-transformed RV-specific IgA Ab antibodies were analyzed using two-way ANOVA followed by Duncan’s multiple range test. The area under the curve (AUC) analysis was conducted to compare diarrhea severity and shedding among the groups [60]. A Kruskal–Wallis rank sum test was then performed to compare the total AUC values between the groups. Differences were considered significant at p ≤ 0.05.
3. Results
3.1. HBGA-Expressing Bacteria (HBGA+) Cocktail Reduces Diarrhea Severity and Virus Shedding
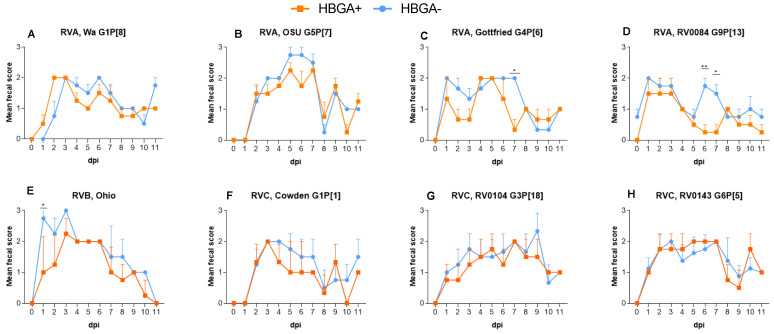
The presence of individual strains of both HBGA+ and HBGA− bacterial cocktails in rectal swabs was confirmed by using species-specific primers in PCR analysis. Total aerobic bacterial counts in piglets colonized with HBGA− vs. HBGA+ bacteria did not differ, while the numbers of anaerobic bacteria were significantly higher in the piglets colonized with HBGA− bacteria (Figure S1, p < 0.05). Diarrhea onset after infection with RVA (G5P[7], G4P[6]), RVC G3P[18], and RVB strains was significantly delayed in the HBGA+ vs. HBGA− piglets (Table 1). Further, the RV-induced diarrhea lasted significantly longer in the piglets colonized with HBGA− bacteria, in groups infected with RVA G4P[6] and RVB strains (Table 1, p < 0.05). In addition, piglets colonized with HBGA+ bacteria displayed a significant reduction in the mean cumulative fecal score (Table 1, p < 0.05), in the RVB-infected piglets. A significantly lower AUC value was noted in the piglets colonized with the HBGA+ bacterial cocktail after infection with RVA G4P[6], G9P[13], and RVB (Table 1, p < 0.05). Further, statistically significant decreases in diarrhea severity were noted at dpi 1 for the RVB-infected piglets (Figure 1E, p < 0.05); at dpi 6 for the RVA G9P[13]-infected piglets (Figure 1D, p < 0.01), and at dpi 7 for the RVA G4P[6]- and G9P[13]-infected piglets (Figure 1C,D, p < 0.05).
Table 1.
Diarrhea in piglets orally inoculated with virulent RVs.
| N | Mean Days to Diarrhea Onset 1 | Mean Diarrhea Duration (Days) 2 | Mean Cumulative Fecal Score 3 | AUC 4 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| RV Strains | HBGA+ | HBGA− | HBGA+ | HBGA− | HBGA+ | HBGA− | HBGA+ | HBGA− | HBGA+ | HBGA− |
| Wa G1P[8] | 4 | 4 | 2.0 | 2.8 | 3.3 | 4.8 | 13.0 | 13.8 | 12.50 | 12.88 |
| OSU G5P[7] | 4 | 4 | 3.3 | 2.5 | 5.5 | 6.0 | 15.0 | 17.0 | 14.38 | 16.50 |
| Gottfried G4P[6] | 3 | 3 | 2.0 | 1.0 | 3.3 | 5.7 | 11.7 | 15.3 | 11.17 | 14.83 |
| RV0084 G9P[13] | 4 | 4 | 1.0 | 1.0 | 2.3 | 3.8 | 8.8 | 13.8 | 8.625 | 13.75 |
| RVB Ohio | 4 | 4 | 2.0 | 1.0 | 5.3 | 7.3 | 13.5 | 19.0 | 13.50 | 19.00 |
| Cowden G1P[1] | 4 | 4 | 2.7 | 2.8 | 2.7 | 4.5 | 10.3 | 13.5 | 9.833 | 12.75 |
| RV0104 G3P[18] | 4 | 4 | 4.5 | 3.8 | 3.8 | 5.3 | 14.3 | 16.3 | 13.75 | 15.83 |
| RV0143 G6P[5] | 4 | 8 | 2.3 | 2.1 | 6.0 | 5.3 | 16.3 | 16.0 | 15.75 | 15.50 |
1 Diarrhea onset is defined as the number of days between the virus inoculation and the first manifestation of diarrhea (e.g., fecal consistency score of ≥2). 2 Duration of diarrhea is defined as the number of days that the fecal consistency score was ≥2. Fecal diarrhea was scored as follows: 0, normal; 1, pasty; 2, semiliquid; 3, liquid. 3 Mean cumulative fecal score [(sum of fecal consistency score for 11 days postinoculation)/N], where N is the number of pigs receiving the inoculation. Means in the same row were analyzed by unpaired t-test. 4 Area under the curve (AUC) was calculated using the area under the curve analysis function in the Prism software. A Kruskal–Wallis rank sum test was then performed to compare the total AUC between the groups. Significant differences (bold) are indicated as calculated by an unpaired t-test.
Figure 1.
Diarrhea in piglets following RVA (A–D), RVB (E), and RVC (F–H) inoculation. Individual RV strains were used to inoculate (1 × 106 FFU) piglets after 5 consecutive days of supplementation with HBGA+ or HBGA- bacteria. Fecal consistency was scored as follows: 0, normal; 1, pasty; 2, semiliquid; 3, liquid; and diarrhea was considered as a score of ≥2. The error bars represent the standard deviations; significant differences (* p < 0.05, ** p < 0.01) are indicated as calculated by two-way ANOVA followed by Duncan’s multiple comparisons test.
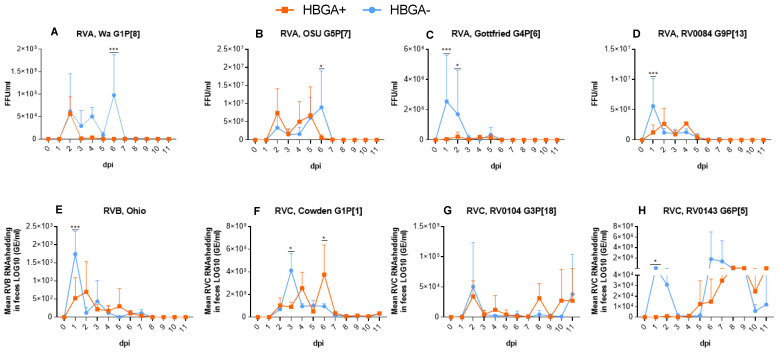
Consistent with the clinical data, we observed a significantly delayed onset of virus shedding in the piglets colonized with HBGA+ bacteria after infection with RVC strains G6P[5] and G3P[18] (Table 2, p < 0.05) compared to the piglets colonized with HBGA− bacteria. In addition, HBGA+-inoculated piglets had a significantly shortened duration of virus shedding in piglets infected with RVA G1P[8] and RVC G6P[5] (Table 2, p < 0.05). Significantly lower viral shedding titers in this group were observed on dpi 1 after infection with RVA G4P[6], G9P[13], RVB (Figure 2C–E, p < 0.001), and RVC G6P[5] (Figure 2H, p < 0.05); on dpi 2 after infection with RVA G4P[6] (Figure 2C, p < 0.05); and at dpi 6 after infection with RVA G5P[7] and RVC G1P[1] (Figure 2B,F, p < 0.05).
Table 2.
Virus shedding in piglets orally inoculated with virulent RVs.
| N | Mean Days to Shedding Onset | Mean Shedding Duration (Days) | Avg Peak Titer (FFU/mL) | AUC 1 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| RV Strains | HBGA+ | HBGA− | HBGA+ | HBGA− | HBGA+ | HBGA− | HBGA+ | HBGA− | HBGA+ | HBGA− |
| Wa G1P[8] | 4 | 4 | 2.0 | 2.0 | 6.3 | 8.5 | 5.58 × 104 | 6.14 × 104 | 6.04 × 104 | 2.50 × 105 |
| OSU G5P[7] | 4 | 4 | 2.0 | 2.0 | 6.8 | 6.5 | 7.41 × 106 | 9.01 × 106 | 2.16 × 107 | 2.18 × 107 |
| Gottfried G4P[6] | 3 | 3 | 2.0 | 1.7 | 4.7 | 5.7 | 6.63 × 105 | 4.83 × 106 | 6.62 × 105 | 4.82 × 106 |
| RV0084 G9P[13] | 4 | 4 | 1.3 | 1.0 | 7.5 | 8.3 | 8.02 × 106 | 9.85 × 106 | 8.04 × 106 | 9.87 × 106 |
| RVB Ohio | 4 | 4 | 1.0 | 1.0 | 7.0 | 7.0 | 7.00 × 102 | 1.74 × 103 | 2.07 × 103 | 2.64 × 103 |
| Cowden G1P[1] | 4 | 4 | 2.0 | 2.0 | 10.0 | 10.0 | 3.76 × 105 | 4.12 × 105 | 9.60 × 105 | 8.29 × 105 |
| RV0104 G3P[18] | 4 | 4 | 2.0 | 1.0 | 9.8 | 10.3 | 5.07 × 104 | 3.94 × 104 | 1.32 × 105 | 9.23 × 104 |
| RV0143 G6P[5] | 4 | 8 | 3.5 | 1.1 | 8.0 | 10.5 | 1.60 × 105 | 1.83 × 106 | 3.97 × 105 | 3.53 × 106 |
Means in the same row were analyzed by unpaired t-test. 1 Area under the curve (AUC) was calculated using the area under the curve analysis function in the Prism software. A Kruskal–Wallis rank sum test was then performed to compare the total AUC between the groups. Significant differences (bold) are indicated as calculated by an unpaired t-test.
Figure 2.
Mean virus shedding titers in piglets following RVA (A–D), RVB (E), and RVC (F–H) inoculation. Individual RV strains were used to colonize (1 × 106 FFU) piglets after 5 consecutive days of supplementation with HBGA+ or HBGA− bacteria. The error bars represent the standard deviations; significant differences (* p < 0.05, *** p < 0.001) are indicated as calculated by two-way ANOVA followed by Duncan’s multiple comparisons test.
3.2. There Was No Evidence That the Protective Effect of HBGA+ Bacteria Was Immune-Mediated
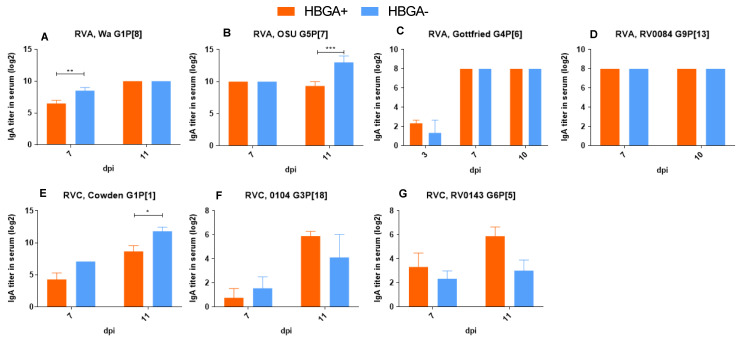
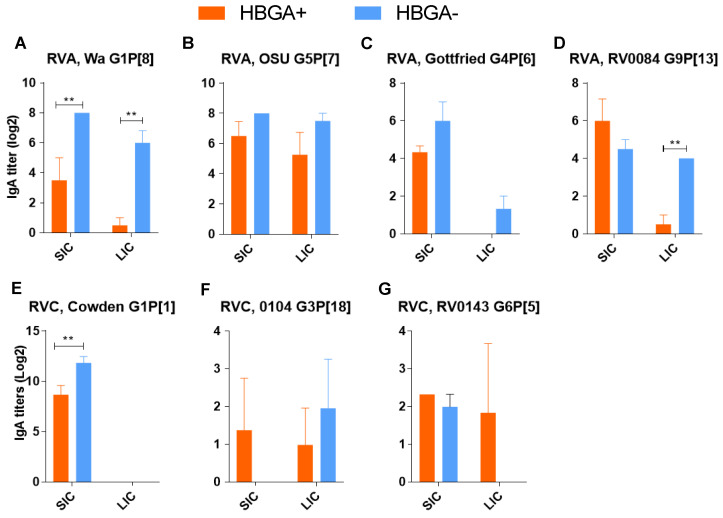
To confirm that the observed protective effect of HBGA+ bacteria on RV infections was not associated with bacteria-mediated immunomodulation, we evaluated the local (intestinal content) and systemic (serum) RV-specific IgA Ab responses. Data on the mean RVA/RVC-specific IgA Ab titers in the blood (Figure 3) and intestinal contents (Figure 4) revealed that colonization with HBGA+ bacteria did not result in significantly higher IgA Ab titers (compared to piglets colonized with HBGA− bacteria) after infection with RVA/RVC strains. In addition, significantly lower IgA Ab titers in the blood of HBGA+ bacteria-colonized piglets were observed after infection with RVA G1P[8] (Figure 3A, p < 0.01), RVA G5P[7] (Figure 3B, p < 0.001), and RVC G1P[1] (Figure 3E, p < 0.05). This coincided with significantly lower IgA Ab titers in the intestinal contents of the piglets colonized with HBGA+ bacteria after infection with RVA G1P[8] and G9P[13] (Figure 4A,D, p < 0.01).
Figure 3.
IgA Ab titers in blood samples collected on dpi 0, 3, 7, 11 following RVA (A–D), and RVC (E–G) infection. ELISA IgA Ab titers were analyzed using two-way ANOVA followed by Duncan’s multiple comparisons test (* p < 0.05, ** p < 0.01, *** p < 0.001).
Figure 4.
IgA Ab titers in piglet small/large intestinal content (SIC/LIC) samples collected at necropsy 11 days after RVA (A–D), and RVC (E–G) infection. ELISA IgG Ab titers were analyzed using two-way ANOVA followed by Duncan’s multiple comparisons test (** p < 0.01).
We also evaluated the cytokine profiles in blood samples collected before (dpi 0) and after (dpi 3) virus inoculation (Figures S2 and S3). In piglets colonized with HBGA- bacteria, we observed a higher IFN-α concentration compared to those colonized with HBGA+ bacteria after infection with RVA G5P[7] (Figure S2B, p < 0.05). The TNF-α concentrations were higher following RVC G3P[18] infection in the piglets colonized with HBGA+ vs. HBGA− bacteria (Figure S3G, p < 0.05). However, the rest of the data on TNF-α and IL-22/IL-10 responses did not allow for discrimination between piglets colonized with HBGA+ vs. HBGA- bacterial cocktails.
3.3. The Protective Effect of HBGA+ Bacteria Did Not Vary with the Piglet HBGA Phenotype
Although previous studies suggested that the host HBGA phenotype plays an important role in RV infection and evolution [61,62], there are no in vivo data for porcine RVs [6,7]. Here, we aimed to establish whether the protective effect of the bacterial cocktail was independent of the piglet HBGA phenotype. In our study, the data for piglets with the Astrong (A+H−) and Aweak (A+H+) phenotypes were combined and compared with the O phenotype (A−H+). Our analysis demonstrated that there were no significant differences in diarrhea severity and virus shedding associated with the A+ vs. A− phenotypes (Table S3). This indicates that the protective effect of HBGA+ bacteria on RV infection was not affected by piglet HBGA phenotype.
4. Discussion
The tripartite RV–host–commensal bacteria interactions have been demonstrated to have profound impacts on RV infection and disease [13,18,63]. In addition to the known mechanisms of protection, such as immunomodulation [64], metabolic and enzymatic support [65], and improved barrier function [66] utilized by probiotics, studies have shown that certain non-pathogenic bacteria possess the ability to directly bind certain viruses [67], including RVs [13,68]. For RVs, this phenomenon has been shown to be associated with the ability of bacteria to express structures similar to what RV uses as attachment sites on IECs, such as HBGAs [16]. However, there is no consensus opinion on the significance of these interactions in vivo [13,69,70]. The current study aimed to evaluate whether direct binding of RV by HBGA+ bacteria is associated with reduced or enhanced RV infection and disease.
Our current data suggest that HBGA+ bacteria improved protection against RVA, RVB, and RVC infection compared to HBGA- bacteria [16]. Although several studies have shown that the presence of bacterial HBGA-like structures enhanced viral replication [71,72], our study demonstrated that the direct binding of RV virions may represent an additional mechanism of antiviral protection conferred by probiotic/commensal bacteria. These contrasting findings may be attributed to the use of in vitro models (cell culture) in other studies, which lack a key component of the RV–host–bacteria interactions, the mucus, and, thus, may not be physiologically relevant. While RV binding by bacteria can facilitate RV particle delivery to target cells in vitro, the intestinal mucus in the gut may significantly restrict direct contact between bacteria and IECs [73,74], thus limiting the ability of bacteria to serve as a “Trojan horse” for viruses.
There are multiple studies on the use of probiotics against RV infection in which the beneficial/protective effects of certain bacteria are linked to the immunomodulatory effects of bacteria [75,76,77,78]. Our findings indicated that in most cases, the IgA Ab titers and IFN-α concentrations following RV infection were either similar or lower in the piglets colonized with HBGA+ bacteria. This suggests that the beneficial effect of HBGA+ bacteria was not associated with improved immune responses. In contrast, increased IgA Ab titers and cytokine concentrations in most cases could be associated with increased virus replication in the piglets colonized with HBGA- bacteria.
Our study has several limitations related to the inability to control all the aspects of the bacteria–RV interactions between the two different bacterial cocktails. First, in this study, we utilized a different number of bacterial strains in probiotic cocktails (five in the HBGA+ and two in the HBGA−). However, our previous study demonstrated that an increased number of probiotics in treatment does not result in superior anti-RV protection compared to an individual probiotic treatment [20]. In our current study, both HBGA+ and HBGA- bacteria colonized GF piglets effectively, with higher total bacterial counts observed in piglets colonized with HBGA- bacteria, which could be due to the individual growing characteristics of bacterial strains. This indicates that the higher number of bacterial strains used in the HBGA+ bacterial cocktail did not result in a higher bacterial load in the colonized piglets. Next, while we did not have any evidence that the protective effect of the HBGA+ probiotic cocktail was immune-mediated, there are other bacteria-mediated effects on the host and RV infection that were not evaluated in this study. For example, bacteria can regulate the mucus composition by stimulating the production or degradation of mucin-type glycans, altering the ability of mucus to provide decoy epitopes for RV attachment. Several probiotics have been shown to up- (Lactobacilli) and down-regulate (Bifidobacteria and Streptococci) mucin secretion [79]. In addition, B. thetaiotaomicron, which was used in this study as a component of the HBGA+ bacterial cocktail, was previously shown to stimulate mucin secretion in vitro [80]. In addition, various commensal bacteria, including B. thetaiotaomicron and B. longum were shown to produce sialidases, a group of enzymes responsible for sialic acid removal and mucin degradation, thus affecting the protective role of the intestinal mucus [81,82]. Thus, more studies are needed to dissect the roles of individual/combined HBGA+ bacteria in RV infection.
Nevertheless, this is the first study that evaluated a probiotic cocktail broadly protective against genetically distinct RVA, RVB, and RVC strains and demonstrated the role of the HBGA-mediated interactions in this protection in vivo. Thus, our data provide a proof-of-concept that probiotic/commensal bacteria can act as decoy receptors reducing the severity of RV infection and disease in vivo. Further studies are needed to validate the feasibility of this concept in conventional animals.
5. Conclusions
In conclusion, we demonstrated the ability of the HBGA+ bacteria to reduce species A, B, and C RV infection in vivo. This may represent a novel mechanism for protection against RV-associated diarrhea. However, the protective effects of the HBGA+ bacteria in conventional animals, where HBGA+ bacteria would need to compete with already established microbiota, remain to be evaluated. In addition, other aspects of RV–host–bacteria interactions, such as enzymatic and metabolic alterations associated with the HBGA+ bacterial cocktail and their effects on IEC integrity, must be further investigated.
Acknowledgments
We gratefully acknowledge the technical assistance of Molly Raque, Ronna Wood, Juliette Hanson, Sara Tallmadge, Megan Strother, Alfred Mainga, and Yusheng Guo. This study was supported by a grant from the IDRC, 109053 (Anastasia N. Vlasova, PI, and Linda J. Saif, co-PI).
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/v16050660/s1, Table S1: Data on the ability of individual HBGA+ and HBGA- bacterial strains to bind virulent RVs; Figure S1: Fecal probiotic bacterial shedding from probiotic colonized piglets. An asterisk indicates a significant difference (p < 0.05) in fecal probiotic counts among treatment groups; Figure S2: IFN-α concentrations in piglet blood samples collected on dpi 0 and dpi 3 following RVA (A–D), RVB (E), and RVC (F–H) infection. Significant differences (* p < 0.05) are indicated as calculated by two-way ANOVA followed by Sidak’s multiple comparisons test; Figure S3: TNF-α concentrations in piglet blood samples collected on dpi 0 and 11 following RVA (A–D), RVB (E), and RVC (F–H) infection. Significant differences (* p < 0.05) are indicated as calculated by two-way ANOVA followed by Duncan’s multiple comparisons test; Table S2: Primers used in this study; Table S3: Diarrhea and virus shedding in gnotobiotic piglets after oral inoculation with virulent RVs.
Author Contributions
Conceptualization, A.N.V.; methodology, S.A.R. and A.N.V.; formal analysis, S.A.R.; investigation, S.A.R.; technical support, J.O.A., M.K.K. and M.C.; resources, A.N.V.; writing—original draft preparation, S.A.R.; revised draft writing, review, and editing, A.N.V., J.O.A. and S.A.R.; critical review, A.N.V. and L.J.S.; visualization, S.A.R.; supervision, A.N.V.; project administration, A.N.V.; funding acquisition, A.N.V. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
All our animal experiments were approved by the Institutional Animal Care and Use Committee (IACUC) at Ohio State University) (protocol #2009A0146, approved on 10 December 2021 and #2010A00000088 approved on 23 February 2021).
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
Author J.O.A is employed by the company Givax. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
This work was supported by the International Development Research Centre (IDRC, Canada), grant number 109053, to Dr. Vlasova and Dr. Vlasova’s startup funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Grimprel E., Rodrigo C., Desselberger U. Rotavirus Disease: Impact of Coinfections. Pediatr. Infect. Dis. J. 2008;27:S3. doi: 10.1097/INF.0b013e31815eedfa. [DOI] [PubMed] [Google Scholar]
- 2.Ma L., El Khoury A.C., Itzler R.F. The Burden of Rotavirus Hospitalizations Among Medicaid and Non-Medicaid Children Younger Than 5 Years Old. Am. J. Public Health. 2009;99((Suppl. S2)):S398–S404. doi: 10.2105/AJPH.2008.148494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Du Y., Chen C., Zhang X., Yan D., Jiang D., Liu X., Yang M., Ding C., Lan L., Hecht R., et al. Global burden and trends of rotavirus infection-associated deaths from 1990 to 2019: An observational trend study. Virol. J. 2022;19:166. doi: 10.1186/s12985-022-01898-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ishizuka T., Kanmani P., Kobayashi H., Miyazaki A., Soma J., Suda Y., Aso H., Nochi T., Iwabuchi N., Xiao J.Z., et al. Immunobiotic Bifidobacteria Strains Modulate Rotavirus Immune Response in Porcine Intestinal Epitheliocytes via Pattern Recognition Receptor Signaling. PLoS ONE. 2016;11:e0152416. doi: 10.1371/journal.pone.0152416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Amimo J.O., Raev S.A., Chepngeno J., Mainga A.O., Guo Y., Saif L., Vlasova A.N. Rotavirus Interactions with Host Intestinal Epithelial Cells. Front. Immunol. 2021;12:793841. doi: 10.3389/fimmu.2021.793841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guo Y., Candelero-Rueda R.A., Saif L.J., Vlasova A.N. Infection of porcine small intestinal enteroids with human and pig rotavirus A strains reveals contrasting roles for histo-blood group antigens and terminal sialic acids. PLoS Pathog. 2021;17:e1009237. doi: 10.1371/journal.ppat.1009237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guo Y., Raev S., Kick M.K., Raque M., Saif L.J., Vlasova A.N. Rotavirus C Replication in Porcine Intestinal Enteroids Reveals Roles for Cellular Cholesterol and Sialic Acids. [(accessed on 15 September 2022)];Viruses. 2022 14:1825. doi: 10.3390/v14081825. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9416568/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hu L., Crawford S.E., Czako R., Cortes-Penfield N.W., Smith D.F., Le Pendu J., Estes M.K., Prasad B.V. Cell attachment protein VP8* of a human rotavirus specifically interacts with A-type histo-blood group antigen. Nature. 2012;485:256–259. doi: 10.1038/nature10996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martínez-Alarcón L., Ramis G., Majado M.J., Quereda J.J., Herrero-Medrano J.M., Ríos A., Ramírez P., Muñoz A. ABO and RH1 Blood Group Phenotyping in Pigs (Sus scrofa) Using Microtyping Cards. Transplant. Proc. 2010;42:2146–2148. doi: 10.1016/j.transproceed.2010.05.105. [DOI] [PubMed] [Google Scholar]
- 10.Smith D.M., Newhouse M., Naziruddin B., Kresie L. Blood groups and transfusions in pigs. Xenotransplantation. 2006;13:186–194. doi: 10.1111/j.1399-3089.2006.00299.x. [DOI] [PubMed] [Google Scholar]
- 11.Bolner M., Bertolini F., Bovo S., Schiavo G., Fontanesi L. Investigation of ABO Gene Variants across More Than 60 Pig Breeds and Populations and Other Suidae Species Using Whole-Genome Sequencing Datasets. Animals. 2023;14:5. doi: 10.3390/ani14010005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hampton C., Dehghanpir S., Armstrong C., Scully C., Baker R.E., Mitchell M. Prevalence of AO blood group and level of agreement for AO blood-typing methods in pet pigs from Louisiana. J. Vet. Emerg. Crit. Care. 2023;33:549–558. doi: 10.1111/vec.13266. [DOI] [PubMed] [Google Scholar]
- 13.Raev S.A., Amimo J.O., Saif L.J., Vlasova A.N. Intestinal mucin-type O-glycans: The major players in the host-bacteria-rotavirus interactions. Gut Microbes. 2023;15:2197833. doi: 10.1080/19490976.2023.2197833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li H., Limenitakis J.P., Fuhrer T., Geuking M.B., Lawson M.A., Wyss M., Brugiroux S., Keller I., Macpherson J.A., Rupp S., et al. The outer mucus layer hosts a distinct intestinal microbial niche. Nat. Commun. 2015;6:8292. doi: 10.1038/ncomms9292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miura T., Sano D., Suenaga A., Yoshimura T., Fuzawa M., Nakagomi T., Nakagomi O., Okabe S. Histo-Blood Group Antigen-Like Substances of Human Enteric Bacteria as Specific Adsorbents for Human Noroviruses. J. Virol. 2013;87:9441–9451. doi: 10.1128/JVI.01060-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raev S., Omwando A., Guo Y., Raque M., Amimo J., Saif L., Vlasova A. Glycan-mediated interactions between bacteria, rotavirus and the host cells provide an additional mechanism of antiviral defence. Benef. Microbes. 2022;13:383–395. doi: 10.3920/BM2022.0026. [DOI] [PubMed] [Google Scholar]
- 17.Comstock L.E., Kasper D.L. Bacterial Glycans: Key Mediators of Diverse Host Immune Responses. Cell. 2006;126:847–850. doi: 10.1016/j.cell.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 18.Gozalbo-Rovira R., Rubio-Del-Campo A., Santiso-Bellón C., Vila-Vicent S., Buesa J., Delgado S., Molinero N., Margolles A., Yebra M.J., Collado M.C., et al. Interaction of Intestinal Bacteria with Human Rotavirus during Infection in Children. Int. J. Mol. Sci. 2021;22:1010. doi: 10.3390/ijms22031010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Almand E.A., Moore M.D., Jaykus L.A. Characterization of human norovirus binding to gut-associated bacterial ligands. BMC Res. Notes. 2019;12:607. doi: 10.1186/s13104-019-4669-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kandasamy S., Vlasova A.N., Fischer D., Kumar A., Chattha K.S., Rauf A., Shao L., Langel S.N., Rajashekara G., Saif L.J. Differential Effects of Escherichia coli Nissle and Lactobacillus rhamnosus Strain GG on Human Rotavirus Binding, Infection, and B Cell Immunity. J. Immunol. 2016;196:1780–1789. doi: 10.4049/jimmunol.1501705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liao S.F., Nyachoti M. Using probiotics to improve swine gut health and nutrient utilization. Anim. Nutr. 2017;3:331–343. doi: 10.1016/j.aninu.2017.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhao P.Y., Kim I.H. Effect of direct-fed microbial on growth performance, nutrient digestibility, fecal noxious gas emission, fecal microbial flora and diarrhea score in weanling pigs. Anim. Feed Sci. Technol. 2015;200:86–92. doi: 10.1016/j.anifeedsci.2014.12.010. [DOI] [Google Scholar]
- 23.Bekaert H., Moermans R., Eeckhout W. Effect of a live yeast culture in diets of weanling piglets on performances and fre-quency of diarrhoea. Anim. Res. 1996;45:369–376. doi: 10.1051/animres:19960409. [DOI] [Google Scholar]
- 24.Harper A.F., Kornegay E.T., Bryant K.L., Thomas H.R. Efficacy of virginiamycin and a commercially-available lactobacillus probiotic in swine diets. Anim. Feed Sci. Technol. 1983;8:69–76. doi: 10.1016/0377-8401(83)90044-5. [DOI] [Google Scholar]
- 25.Jeong J., Kim J.K., Lee S., Kim I. Evaluation of Bacillus subtilis and Lactobacillus acidophilus probiotic supplementation on reproductive performance and noxious gas emission in sows. Ann. Anim. Sci. 2015;15:699–710. doi: 10.1515/aoas-2015-0018. [DOI] [Google Scholar]
- 26.Walsh M., Saddoris K., Sholly D., Hinson R., Sutton A., Applegate T., Richert B., Radcliffe J. The effects of direct fed microbials delivered through the feed and/or in a bolus at weaning on growth performance and gut health. Livest. Sci. 2007;108:254–257. doi: 10.1016/j.livsci.2007.01.051. [DOI] [Google Scholar]
- 27.Das S., Gupta P.K., Das R.R. Efficacy and Safety of Saccharomyces boulardii in Acute Rotavirus Diarrhea: Double Blind Randomized Controlled Trial from a Developing Country. J. Trop. Pediatr. 2016;62:464–470. doi: 10.1093/tropej/fmw032. [DOI] [PubMed] [Google Scholar]
- 28.Lee D.K., Park J.E., Kim M.J., Seo J.G., Lee J.H., Ha N.J. Probiotic bacteria, B. longum and L. acidophilus inhibit infection by rotavirus in vitro and decrease the duration of diarrhea in pediatric patients. Clin. Res. Hepatol. Gastroenterol. 2015;39:237–244. doi: 10.1016/j.clinre.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 29.Maragkoudakis P.A., Chingwaru W., Gradisnik L., Tsakalidou E., Cencic A. Lactic acid bacteria efficiently protect human and animal intestinal epithelial and immune cells from enteric virus infection. Int. J. Food Microbiol. 2010;141((Suppl. S1)):S91–S97. doi: 10.1016/j.ijfoodmicro.2009.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huang H.C., Vlasova A.N., Kumar A., Kandasamy S., Fischer D.D., Deblais L., Paim F.C., Langel S.N., Alhamo M.A., Rauf A., et al. Effect of antibiotic, probiotic, and human rotavirus infection on colonisation dynamics of defined commensal microbiota in a gnotobiotic pig model. Benef. Microbes. 2018;9:71–86. doi: 10.3920/BM2016.0225. [DOI] [PubMed] [Google Scholar]
- 31.Wyatt R.G., James W.D., Bohl E.H., Theil K.W., Saif L.J., Kalica A.R., Greenberg H.B., Kapikian A.Z., Chanock R.M. Human rotavirus type 2: Cultivation in vitro. Science. 1980;207:189–191. doi: 10.1126/science.6243190. [DOI] [PubMed] [Google Scholar]
- 32.Amimo J.O., Vlasova A.N., Saif L.J. Detection and genetic diversity of porcine group A rotaviruses in historic (2004) and recent (2011 and 2012) swine fecal samples in Ohio: Predominance of the G9P[13] genotype in nursing piglets. J. Clin. Microbiol. 2013;51:1142–1151. doi: 10.1128/JCM.03193-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bohl E.H., Theil K.W., Saif L.J. Isolation and serotyping of porcine rotaviruses and antigenic comparison with other rotaviruses. J. Clin. Microbiol. 1984;19:105. doi: 10.1128/jcm.19.2.105-111.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Theil K.W., Saif L.J., Moorhead P.D., Whitmoyer R.E. Porcine rotavirus-like virus (group B rotavirus): Characterization and pathogenicity for gnotobiotic pigs. J. Clin. Microbiol. 1985;21:340–345. doi: 10.1128/jcm.21.3.340-345.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tsunemitsu H., Saif L.J., Jiang B.M., Shimizu M., Hiro M., Yamaguchi H., Ishiyama T., Hirai T. Isolation, characterization, and serial propagation of a bovine group C rotavirus in a monkey kidney cell line (MA104) J. Clin. Microbiol. 1991;29:2609–2613. doi: 10.1128/jcm.29.11.2609-2613.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Meyer R.C., Bohl E.H., Kohler E.M. Procurement and Maintenance of Germ-Free Swine for Microbiological Investigations. Appl. Microbiol. 1964;12:295–300. doi: 10.1128/am.12.4.295-300.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Krajmalnik-Brown R., Ilhan Z.E., Kang D.W., DiBaise J.K. Effects of Gut Microbes on Nutrient Absorption and Energy Regulation. Nutr. Clin. Pract. 2012;27:201–214. doi: 10.1177/0884533611436116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wu H.J., Wu E. The role of gut microbiota in immune homeostasis and autoimmunity. Gut Microbes. 2012;3:4–14. doi: 10.4161/gmic.19320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kayama H., Takeda K. Manipulation of epithelial integrity and mucosal immunity by host and microbiota-derived metabolites. Eur. J. Immunol. 2020;50:921–931. doi: 10.1002/eji.201948478. [DOI] [PubMed] [Google Scholar]
- 40.Johansson M.E., Jakobsson H.E., Holmén-Larsson J., Schütte A., Ermund A., Rodríguez-Piñeiro A.M., Arike L., Wising C., Svensson F., Bäckhed F., et al. Normalization of Host Intestinal Mucus Layers Requires Long-Term Microbial Colonization. Cell Host Microbe. 2015;18:582–592. doi: 10.1016/j.chom.2015.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Engevik M.A., Banks L.D., Engevik K.A., Chang-Graham A.L., Perry J.L., Hutchinson D.S., Ajami N.J., Petrosino J.F., Hyser J.M. Rotavirus infection induces glycan availability to promote ileum-specific changes in the microbiome aiding rotavirus virulence. Gut Microbes. 2020;11:1324–1347. doi: 10.1080/19490976.2020.1754714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ghosh S., Whitley C.S., Haribabu B., Jala V.R. Regulation of Intestinal Barrier Function by Microbial Metabolites. Cell. Mol. Gastroenterol. Hepatol. 2021;11:1463–1482. doi: 10.1016/j.jcmgh.2021.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Helmy Y.A., Closs G., Jung K., Kathayat D., Vlasova A., Rajashekara G. Effect of Probiotic E. coli Nissle 1917 Supplementation on the Growth Performance, Immune Responses, Intestinal Morphology, and Gut Microbes of Campylobacter jejuni Infected Chickens. Infect. Immun. 2022;90:e00337-22. doi: 10.1128/iai.00337-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhu W., Wei Z., Xu N., Yang F., Yoon I., Chung Y., Liu J., Wang J. Effects of Saccharomyces cerevisiae fermentation products on performance and rumen fermentation and microbiota in dairy cows fed a diet containing low quality forage. J. Anim. Sci. Biotechnol. 2017;8:36. doi: 10.1186/s40104-017-0167-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Whitaker W.R., Shepherd E.S., Sonnenburg J.L. Tunable expression tools enable single-cell strain distinction in the gut microbiome. Cell. 2017;169:538. doi: 10.1016/j.cell.2017.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bartosch S., Fite A., Macfarlane G.T., McMurdo M.E.T. Characterization of Bacterial Communities in Feces from Healthy Elderly Volunteers and Hospitalized Elderly Patients by Using Real-Time PCR and Effects of Antibiotic Treatment on the Fecal Microbiota. Appl. Environ. Microbiol. 2004;70:3575–3581. doi: 10.1128/AEM.70.6.3575-3581.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Monteagudo L.V., Benito A.A., Lázaro-Gaspar S., Arnal J.L., Martin-Jurado D., Menjon R., Quílez J. Occurrence of Rotavirus A Genotypes and Other Enteric Pathogens in Diarrheic Suckling Piglets from Spanish Swine Farms. Animals. 2022;12:251. doi: 10.3390/ani12030251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Robert H., Gabriel V., Fontagné-Faucher C. Biodiversity of lactic acid bacteria in French wheat sourdough as determined by molecular characterization using species-specific PCR. Int. J. Food Microbiol. 2009;135:53–59. doi: 10.1016/j.ijfoodmicro.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 49.Zeng W., Wu J., Xie H., Xu H., Liang D., He Q., Yang X., Liu C., Gong J., Zhang Q., et al. Enteral nutrition promotes the remission of colitis by gut bacteria-mediated histidine biosynthesis. [(accessed on 8 March 2024)];eBioMedicine. 2024 100:104959. doi: 10.1016/j.ebiom.2023.104959. Available online: https://www.thelancet.com/journals/ebiom/article/PIIS2352-3964(23)00525-X/fulltext. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yuan L., Kang S.Y., Ward L.A., To T.L., Saif L.J. Antibody-Secreting Cell Responses and Protective Immunity Assessed in Gnotobiotic Pigs Inoculated Orally or Intramuscularly with Inactivated Human Rotavirus. J. Virol. 1998;72:330–338. doi: 10.1128/JVI.72.1.330-338.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hakim M.S., Ding S., Chen S., Yin Y., Su J., van der Woude C.J., Fuhler G.M., Peppelenbosch M.P., Pan Q., Wang W. TNF-α exerts potent anti-rotavirus effects via the activation of classical NF-κB pathway. Virus Res. 2018;253:28–37. doi: 10.1016/j.virusres.2018.05.022. [DOI] [PubMed] [Google Scholar]
- 52.Jiang B., Snipes-Magaldi L., Dennehy P., Keyserling H., Holman R.C., Bresee J., Gentsch J., Glass R.I. Cytokines as Mediators for or Effectors against Rotavirus Disease in Children. Clin. Vaccine Immunol. 2003;10:995–1001. doi: 10.1128/CDLI.10.6.995-1001.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kumar D., Shepherd F.K., Springer N.L., Mwangi W., Marthaler D.G. Rotavirus Infection in Swine: Genotypic Diversity, Immune Responses, and Role of Gut Microbiome in Rotavirus Immunity. Pathogens. 2022;11:1078. doi: 10.3390/pathogens11101078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bohl E.H., Saif L.J., Theil K.W., Agnes A.G., Cross R.F. Porcine pararotavirus: Detection, differentiation from rotavirus, and pathogenesis in gnotobiotic pigs. J. Clin. Microbiol. 1982;15:312–319. doi: 10.1128/jcm.15.2.312-319.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chepngeno J., Diaz A., Paim F.C., Saif L.J., Vlasova A.N. Rotavirus C: Prevalence in suckling piglets and development of virus-like particles to assess the influence of maternal immunity on the disease development. Vet. Res. 2019;50:84. doi: 10.1186/s13567-019-0705-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Marthaler D., Homwong N., Rossow K., Culhane M., Goyal S., Collins J., Matthijnssens J., Ciarlet M. Rapid detection and high occurrence of porcine rotavirus A, B, and C by RT-qPCR in diagnostic samples. J. Virol. Methods. 2014;209:30–34. doi: 10.1016/j.jviromet.2014.08.018. [DOI] [PubMed] [Google Scholar]
- 57.Arnold M., Patton J.T., McDonald S.M. Culturing, Storage, and Quantification of Rotaviruses. Curr. Protoc. Microbiol. 2009;15:15C-3. doi: 10.1002/9780471729259.mc15c03s15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Parreno V., Hodgins D.C., De Arriba L., Kang S.Y., Yuan L., Ward L.A., To T.L., Saif L.J. Serum and intestinal isotype antibody responses to Wa human rotavirus in gnotobiotic pigs are modulated by maternal antibodies. Pt 6J. Gen. Virol. 1999;80:1417–1428. doi: 10.1099/0022-1317-80-6-1417. [DOI] [PubMed] [Google Scholar]
- 59.Vlasova A.N., Paim F.C., Kandasamy S., Alhamo M.A., Fischer D.D., Langel S.N., Deblais L., Kumar A., Chepngeno J., Shao L., et al. Protein Malnutrition Modifies Innate Immunity and Gene Expression by Intestinal Epithelial Cells and Human Rotavirus Infection in Neonatal Gnotobiotic Pigs. mSphere. 2017;2:e00046-17. doi: 10.1128/mSphere.00046-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chattha K.S., Vlasova A.N., Kandasamy S., Rajashekara G., Saif L.J. Divergent Immunomodulating Effects of Probiotics on T Cell Responses to Oral Attenuated Human Rotavirus Vaccine and Virulent Human Rotavirus Infection in a Neonatal Gnotobiotic Piglet Disease Model. J. Immunol. 2013;191:2446–2456. doi: 10.4049/jimmunol.1300678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liu Y., Huang P., Tan M., Liu Y., Biesiada J., Meller J., Castello A.A., Jiang B., Jiang X. Rotavirus VP8*: Phylogeny, Host Range, and Interaction with Histo-Blood Group Antigens. J. Virol. 2012;86:9899–9910. doi: 10.1128/JVI.00979-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Huang P., Xia M., Tan M., Zhong W., Wei C., Wang L., Morrow A., Jiang X. Spike Protein VP8* of Human Rotavirus Recognizes Histo-Blood Group Antigens in a Type-Specific Manner. [(accessed on 21 January 2022)];J. Virol. 2012 86:4833–4843. doi: 10.1128/JVI.05507-11. Available online: https://journals.asm.org/doi/abs/10.1128/JVI.05507-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kim A.H., Hogarty M.P., Harris V.C., Baldridge M.T. The Complex Interactions between Rotavirus and the Gut Microbiota. Front. Cell. Infect. Microbiol. 2021;10:586751. doi: 10.3389/fcimb.2020.586751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mazziotta C., Tognon M., Martini F., Torreggiani E., Rotondo J.C. Probiotics Mechanism of Action on Immune Cells and Beneficial Effects on Human Health. Cells. 2023;12:184. doi: 10.3390/cells12010184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Indira M., Venkateswarulu T.C., Abraham Peele K., Nazneen Bobby Md Krupanidhi S. Bioactive molecules of probiotic bacteria and their mechanism of action: A review. 3 Biotech. 2019;9:306. doi: 10.1007/s13205-019-1841-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ohland C.L., Macnaughton W.K. Probiotic bacteria and intestinal epithelial barrier function. Am. J. Physiol. Gastrointest. Liver Physiol. 2010;298:G807–G819. doi: 10.1152/ajpgi.00243.2009. [DOI] [PubMed] [Google Scholar]
- 67.Almand E.A., Moore M.D., Jaykus L.A. Virus-Bacteria Interactions: An Emerging Topic in Human Infection. Viruses. 2017;9:58. doi: 10.3390/v9030058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Engevik K., Banks L., Petrosino J., Engevik M., Hyser J. Exploring the interaction between rotavirus and Lactobacillus. [(accessed on 24 October 2023)];FASEB J. 2021 35 doi: 10.1096/fasebj.2021.35.S1.04505. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1096/fasebj.2021.35.S1.04505. [DOI] [Google Scholar]
- 69.Robinson C.M., Jesudhasan P.R., Pfeiffer J.K. Bacterial lipopolysaccharide binding enhances virion stability and promotes environmental fitness of an enteric virus. Cell Host Microbe. 2014;15:36–46. doi: 10.1016/j.chom.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kuss S.K., Best G.T., Etheredge C.A., Pruijssers A.J., Frierson J.M., Hooper L.V., Dermody T.S., Pfeiffer J.K. Intestinal microbiota promote enteric virus replication and systemic pathogenesis. Science. 2011;334:249–252. doi: 10.1126/science.1211057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jones M.K., Watanabe M., Zhu S., Graves C.L., Keyes L.R., Grau K.R., Gonzalez-Hernandez M.B., Iovine N.M., Wobus C.E., Vinjé J., et al. Enteric bacteria promote human and mouse norovirus infection of B cells. Science. 2014;346:755–759. doi: 10.1126/science.1257147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Karst S.M. Identification of a novel cellular target and a co-factor for norovirus infection—B cells & commensal bacteria. Gut Microbes. 2015;6:266–271. doi: 10.1080/19490976.2015.1052211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Johansson M.E.V., Hansson G.C. Immunological aspects of intestinal mucus and mucins. Nat. Rev. Immunol. 2016;16:639–649. doi: 10.1038/nri.2016.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Johansson M.E.V., Phillipson M., Petersson J., Velcich A., Holm L., Hansson G.C. The inner of the two Muc2 mucin-dependent mucus layers in colon is devoid of bacteria. Proc. Natl. Acad. Sci. USA. 2008;105:15064–15069. doi: 10.1073/pnas.0803124105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ahmadi E., Alizadeh-Navaei R., Rezai M.S. Efficacy of probiotic use in acute rotavirus diarrhea in children: A systematic review and meta-analysis. Caspian J. Intern. Med. 2015;6:187–195. [PMC free article] [PubMed] [Google Scholar]
- 76.Gonzalez-Ochoa G., Flores-Mendoza L.K., Icedo-Garcia R., Gomez-Flores R., Tamez-Guerra P. Modulation of rotavirus severe gastroenteritis by the combination of probiotics and prebiotics. Arch. Microbiol. 2017;199:953–961. doi: 10.1007/s00203-017-1400-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Vlasova A.N., Kandasamy S., Chattha K.S., Rajashekara G., Saif L.J. Comparison of probiotic lactobacilli and bifidobacteria effects, immune responses and rotavirus vaccines and infection in different host species. Vet. Immunol. Immunopathol. 2016;172:72–84. doi: 10.1016/j.vetimm.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kandasamy S., Vlasova A.N., Fischer D.D., Chattha K.S., Shao L., Kumar A., Langel S.N., Rauf A., Huang H.-C., Rajashekara G., et al. Unraveling the Differences between Gram-Positive and Gram-Negative Probiotics in Modulating Protective Immunity to Enteric Infections. Front. Immunol. 2017;8:334. doi: 10.3389/fimmu.2017.00334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Caballero-Franco C., Keller K., De Simone C., Chadee K. The VSL#3 probiotic formula induces mucin gene expression and secretion in colonic epithelial cells. Am. J. Physiol.-Gastrointest. Liver Physiol. 2007;292:G315–G322. doi: 10.1152/ajpgi.00265.2006. [DOI] [PubMed] [Google Scholar]
- 80.Varyukhina S., Freitas M., Bardin S., Robillard E., Tavan E., Sapin C., Grill J.-P., Trugnan G. Glycan-modifying bacteria-derived soluble factors from Bacteroides thetaiotaomicron and Lactobacillus casei inhibit rotavirus infection in human intestinal cells. Microbes Infect. 2012;14:273–278. doi: 10.1016/j.micinf.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 81.Odamaki T., Bottacini F., Kato K., Mitsuyama E., Yoshida K., Horigome A., Xiao J.-Z., van Sinderen D. Genomic diversity and distribution of Bifidobacterium longum subsp. longum across the human lifespan. Sci. Rep. 2018;8:85. doi: 10.1038/s41598-017-18391-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Park K.-H., Kim M.-G., Ahn H.-J., Lee D.-H., Kim J.-H., Kim Y.-W., Woo E.-J. Structural and biochemical characterization of the broad substrate specificity of Bacteroides thetaiotaomicron commensal sialidase. Biochim. Biophys. Acta. 2013;1834:1510–1519. doi: 10.1016/j.bbapap.2013.04.028. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are contained within the article.