Abstract
Neuroinfections rank among the top ten leading causes of child mortality globally, even in high-income countries. The crucial determinants for successful treatment lie in the timing and swiftness of diagnosis. Although viruses constitute the majority of infectious neuropathologies, diagnosing and treating viral neuroinfections remains challenging. Despite technological advancements, the etiology of the disease remains undetermined in over half of cases. The identification of the pathogen becomes more difficult when the infection is caused by atypical pathogens or multiple pathogens simultaneously. Furthermore, the modern surge in global passenger traffic has led to an increase in cases of infections caused by pathogens not endemic to local areas. This review aims to systematize and summarize information on neuroinvasive viral pathogens, encompassing their geographic distribution and transmission routes. Emphasis is placed on rare pathogens and cases involving atypical pathogens, aiming to offer a comprehensive and structured catalog of viral agents with neurovirulence potential.
Keywords: viral neuropathogens, neuroinfections, CNS infections, rare cases, zoonotic infections, vector-borne infections
1. Introduction
Neuroinfections is the common name for a polyetiological group of infectious pathologies of the central and peripheral nervous system (CNS and PNS, respectively), characterized by the predominant localization of the infectious agent in certain structural and anatomical areas of the nervous system, and a wide range of clinical manifestations. Meningitis, encephalitis, and myelitis are among the most severe diseases throughout the world [1,2,3,4,5,6].
According to a long-term study of The Global Burden of Disease IHME project [7], despite a downward trend in the global number of deaths observed between 1990 and 2016, the number of reported cases of meningitis worldwide during the same period, on average, increased from 2.50 million to 2.82 million [4,8]. According to data published by a public health organization, Meningitis Research Foundation [9], the total number of estimated cases of meningitis for 2019 worldwide among all age groups was 2.51 million, with a total number of deaths of 236 thousand [10]. However, it is important to note that in this instance, the model for calculating the number of deaths encompasses all causes of meningitis, not solely infectious ones. Furthermore, when compared to mortality estimates for specific infectious causes of death and all causes of death combined, inconsistencies were observed between models in global estimates of mortality from meningitis/encephalitis and neonatal sepsis [3]. The burden is notably heavy in low- and middle-income countries, where prevalent infections like HIV and its related opportunistic infections, Dengue fever, malaria, and various others are widespread, affecting billions of people and often leading to neurological complications [11]. Developing countries experience the greatest burden of meningitis, including 26 countries in the so-called African meningitis belt [3,4] and 4 countries located beyond its borders (India, Pakistan, Afghanistan, and China) [4].
The epidemiological well-being of the child population is of particular concern. Meningitis is one of the ten leading causes of death in children under 14 years of age, even in high-income countries [8]. According to estimates, about 3% of the total number of deaths among children under 5 years of age were caused by meningitis [4]. The diagnosis of aseptic meningitis in children, especially newborns, is difficult; symptoms of the disease in newborns are often subtle and reflect symptoms observed with other infections [4]. Despite differences in the ecological [4,12] and socioeconomic status of the regions of residence [4], age [8], and other factors influencing epidemiology, with different approaches to accounting and building statistical models [3,4,13], there is consensus on the high burden of disease [8], where meningitis ranks second or third in importance among infectious syndromes [3], with the mortality rate reaching 70% without proper treatment [4,8].
The etiology of encephalitis is identified in less than half of cases, both in developed and developing countries, partly due to the lack of standardized approaches to diagnosis [2,6]. Globally, between 1990 and 2019, there was an estimated 12% increase in encephalitis cases, from 1.3 million to 1.4 million, with a total of 89,900 deaths in 2019 [1]. The global incidence of acute encephalitis in adults is estimated to range from 3.5 to 7.5 cases per 100,000 people [14]. The overall incidence among the child population is 16 cases per 100,000 people, but the highest incidence is recorded in children under 1 year of age—8.7 cases [14]; moreover, according to some estimates, approximately one third of cases of childhood encephalitis can be prevented by vaccination [1].
Depending on the ecological and climatic conditions of individual geographical areas, in the etiological structure of encephalitis, there is a predominance of some groups of pathogens over others. For example, tick-borne encephalitis (TBE), transmitted by tick bites, is a serious problem primarily in Europe and then in Asia. However, climate change is gradually leading to an expansion of the habitat of ticks (in general, this also applies to other arthropods), which has allowed tick-borne encephalitis to appear in previously unaffected areas and cause an increase in the number of new cases of encephalitis [1,15].
Inflammatory diseases that are associated with damage to the gray and/or white matter of the spinal cord, such as myelitis of an infectious origin, primarily caused by pathogens of a viral, and then bacterial and other origin [16]. The best-known etiological agent is poliovirus. Poliomyelitis is a severe, highly contagious disease of viral etiology, caused by polio enteroviruses. It is characterized by general paralysis, including respiratory muscles and impaired motor functions, and its mortality rate is 5–10% [17]. Children under 5 years of age are most at risk. However, according to WHO, since 1988, the number of cases of wild poliovirus has decreased by more than 99% [17,18] through immunization programs.
Another variant of myelitis caused by non-polio viruses (in the broad sense, i.e., not only non-polio enteroviruses) is acute flaccid myelitis (AFM) [5,18,19,20]. In case of AFM, damage to the gray matter of the spinal cord is observed, paralysis in the acute phase of the disease, and motor deficit subsequently [5,18,19,20].
To date, there is no systematic tracking of the incidence of the disease, but there are data reflecting the approximate frequency: for example, in the United States, the incidence among children under 15 years of age is estimated at 1.4 cases per 100,000 population per year [18]. In 2014, according to the CDC, there were more than 500 cases [19]. Outbreaks of disease with symptoms consistent with AFM have also been reported in East Asia and Australia, and other regions around the world [5,19].
In most cases, especially without proper treatment, infections caused by neurotropic and neuroinvasive pathogens can rapidly progress and lead to secondary severe conditions, in particular, stroke, epilepsy, and hydrocephalus; subsequently cause neurological deficits and impaired cognitive functions; and be associated with a high risk of death [4,21,22].
Inflammatory processes in the organs of the nervous system can be caused by a wide range of representatives of viruses, bacteria, fungi, protozoa, and helminths [22,23], and in some cases even achlorophyllic algae [24,25], although such cases are much less common [4,22,26]. The early identification of the causative agent is critical for prescribing appropriate etiotropic therapy and informing the patient about subsequent clinical intervention [22]. Often, patients who do not have a diagnosis are treated empirically with broad-spectrum antibiotics [22,27,28]. This, in turn, increases the risk of adverse side effects [29]: the individual reaction of the patient’s body to the drug due to the cumulative effect, even with a normal tolerability of the drug in minimal therapeutic doses [30,31]. And moreover, it generally affects the resistance of pathogens to antimicrobial drugs [27,32].
The key factors determining a positive treatment outcome are the time and speed of diagnosis. Traditional nonspecific diagnostic methods have their own number of advantages and, at the same time, limitations. Therefore, for example, one of the “gold standards” for diagnosing patients with suspected neuroinfection is the analysis of cerebrospinal fluid. Non-specific methods of testing cerebrospinal fluid, including cytochemical analysis and culture on nutrient media, may, in some cases, give a false negative result [33,34,35]. Pathogen-specific methods for detecting pathogens, including a reaction to determine antibodies that indirectly indicate the presence of infection, or the direct detection of nucleic acids using PCR in biomaterial, require the clinician to select the specific pathogen being studied. In some cases, the arsenal of test systems used is limited to widespread pathogens; however, when a rare pathogen is involved in the pathological process, or in the case of combined infections (co- and mixed infections), difficulties arise in determining its taxonomic affiliation [29,36]. Simultaneous analysis with a set of tests is often used, but this significantly increases the diagnostic time to determine the cause of the disease and the final diagnosis [22].
As mentioned earlier, viruses account for the majority of neuropathologies of infectious origin [2,37]; for example, in developed countries, the vast majority of cases of primary encephalitis are caused by viruses [16]. Viral neuroinfections are of great importance due to the ability to occur in a latent form; their ability to activate in case of exacerbation of other infections and/or against the background of chronic diseases, thereby worsening the current condition of the patient; the potential impact on the severity and development of fatal neurodegenerative diseases such as Alzheimer’s disease or Parkinson’s disease [38,39], multiple sclerosis, and amyotrophic lateral sclerosis [40,41]; the development of pathological autoimmune reactions, including those aimed at the central nervous system [42,43]; and long-term physical and cognitive complications [44,45]. Viruses can cause neurological disease directly by infecting and damaging neurons, or indirectly by stimulating an immune response that alters host cell function [46]. Several factors, including neuroinvasiveness, neurotropism, neurovirulence, and immune responses of infected hosts, determine the spectrum and severity of virus-induced neurological signs and symptoms [46,47,48].
Viral lesions of the central nervous system—perinatal, infant and childhood—can lead to the disruption of the development of the nervous system, including the brain, during the formation period [47], or to the development of serious pathologies, including lethal ones, as occurs with congenital infection with lymphocytic choriomeningitis virus [49]. Today, more than 100 types of viruses are known, for which a connection with the development of diseases of the peripheral and central nervous system has been determined [48]. However, the etiology of a significant part of cases remains unclear due to the lack of available diagnostic tests. For some viral pathogens, their role in the development of acute disease and their long-term effect on the nervous system remains unclear. Examples of such controversial diseases are the forgotten lethargic encephalitis (Economo’s disease) [50,51,52], Vilyui encephalomyelitis [53,54], and diseases presumably caused by Betatorqueviruses or Cyclovirus genus, sometimes found in biosamples from patients [55,56].
Raising awareness of the etiological structure, particularly concerning rare emerging neurotropic/neuroinvasive viral pathogens, is crucial for enhancing diagnostic capabilities in the realm of infections within this nosology. In this review, we systematized and summarized information about currently known neurotropic viral pathogens and their routes of transmission. Special attention was paid to rare pathogens and cases of infection with atypical pathogens reported in the literature, in order to present the most comprehensive and structured list of viral agents with neuroinvasive potential. This review primarily examines the etiological structure of infectious neuropathologies such as meningitis, encephalitis, and myelitis.
For the convenience of readers, we divided the viral pathogens discussed into the following three groups: (1) viruses whose transmission is predominantly/always carried out with the participation of invertebrate vectors (vector-borne infections); or (2) involves primarily direct contact with a virus-reservoir animal; (3) and common viruses, the transmission of which is predominantly maintained within the human population, from person to person, without the participation of intermediate host vectors. However, it should be noted that the third group of viruses also included representatives of the genera Mamastrovirus, Betacoronavirus, Alphainfluenzavirus, Betainfluenzavirus, and Lentivirus, due to their successful establishment in the population and the possibility of transmission from human to human, despite their active circulation between various vertebrates, and/or confirmed zoonotic origin. Within each group, viral pathogens are considered at the level of species and species variants (subspecies and serotypes), grouped by families and genera, and listed in alphabetical order. At the end of each section, we provided summary tables containing structured information about all pathogens discussed in the section.
2. Vector-Borne Viral Neuropathogens
Viruses transmitted by invertebrates are called arboviruses from the words “arthropod-borne”. To date, more than 500 arboviruses have been described, of which about 50 are veterinary-significant, and about 100 are considered potentially pathogenic for humans [57]. The transmission of arboviruses to humans is primarily carried out by ticks and bloodsucking insects of the Diptera order.
2.1. Tick-Borne Viral Neuropathogens
Ticks are obligate hematophagous ectoparasites [58]. The two main families of ticks, Argasidae (soft ticks) and Ixodidae (hard ticks), differ in their ecology and impact on human health [59], in that hard ticks transmit more diseases than soft ticks.
Most viruses that cause neuroinflammation are concentrated within the family Flaviviridae. The population living in the habitats of vectors experiences the greatest risk of infection with tick-borne viruses. For example, the Center for Disease Control and Prevention reported [60] more than doubling of tick-borne disease cases in the United States—accounting for more than 75% of all vector-borne disease reports. Outside the United States, tick-borne pathogens are responsible for the majority of vector-borne diseases in temperate Eurasia [59].
Flaviviridae. Tick-borne flaviviruses are currently divided into two groups: the group of viruses transmitted by mammalian ticks and the group of viruses transmitted by seabird ticks [61]. Tick-borne encephalitis is one of the leading causes of seasonal morbidity in endemic areas [62]. The clinical course of tick-borne infections can range from asymptomatic to severe or fatal.
The well-known arbovirus tick-borne encephalitis virus (TBEV) (Table 1, Figure 1b) (previously known as Russian spring and summer encephalitis (RSSE) virus), is widespread throughout different Eurasian geographical zones from Japan to northern Europe, include new endemic areas, for example, South Korea and the Netherlands [63]. Infection with TBEV in humans occurs after the bite of a tick carrying the virus. However, in addition to direct transmission, TBEV can also be transmitted in a food-borne way such as through raw milk [64], if the animal was infected after a bite. The main vectors of TBEV are Dermacentor reticulatus, Ixodes persulcatus, and Ixodes ricinus ticks. TBEV possesses high neurotropicity, and with the development of a severe form of illness, severe neurological syndromes may occur, including meningitis, encephalitis, and acute flaccid paralysis.
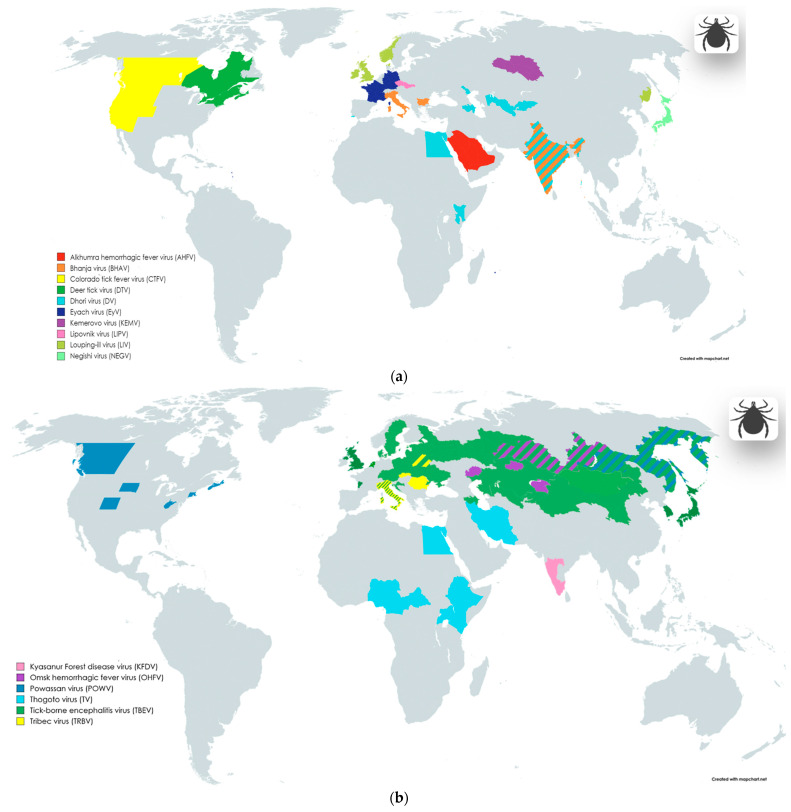
Figure 1.
Geographical distribution of tick-borne infections, including areas of endemic and imported cases involving nervous system symptoms. The division into blocks (a,b) was implemented to enhance the visualization of data on the maps; information about the taxonomic groups located on each block is provided in the legend within the pictures, as well as in the main text alongside the first mention of the corresponding virus. Maps were created with the Map Chart online map-making tool (https://www.mapchart.net/index.html, accessed on 7 May 2024); Graphic objects were created with the BioRender online science illustration making tool (https://www.biorender.com/, accessed on 7 May 2024). The images may contain slight inaccuracies in depicting the boundaries of virus distribution areas due to the limitation of the map scale and the choice of scientific sources utilized to create these illustrations.
Negishi virus (NEGV) (Table 1, Figure 1a) and Louping ill virus (LIV) (Table 1, Figure 1a) are similar to each other and closely related variants of the TBEV virus, forming part of the “tick-borne encephalitis (TBE) serocomplex”, as noted in some papers [65,66].
The distribution area of Negishi virus (NEGV) covers Japan and the adjacent territories of China and the Republic of Korea [61,62,63,64]. The virus was first isolated from the cerebrospinal fluid of a patient in Japan (Tokyo area) in 1948, during an outbreak of Japanese encephalitis [61,62,63,64]. The carriers of NEGV in the territories of Japan, China, and the Republic of Korea are mainly considered ixodid ticks [61,62,63,64]. The exact association and incidence of NEGV encephalitis are difficult to estimate, but awareness is necessary.
The main region of distribution of Louping-ill virus (LIV) are the areas of the British Isles, particularly Scotland, Cumbria, Wales, Devon, and Ireland [67,68]. However, a closely related LIV variant was also discovered in the Far East of Russia [69]. LIV mainly affects small domestic animals such as sheep and goats; manifestations of the disease in animals include fatal encephalomyelitis and other severe lesions of nervous tissue [66,67,68]. Cases of morbidity in humans have been reported extremely rarely (about 30–45 cases are known, including one with a fatal outcome [67,70]), and people involved in tending livestock and grazing are mainly at risk. In humans, rare manifestations of the disease may include encephalitis and similar conditions [67,68].
Alkhumra hemorrhagic fever virus (AHFV) (Table 1, Figure 1a) can also be transmitted to humans through soft tick (Ornithodoros savignyi or “Sand tampan”) and hard tick (Hyalomma dromedarii) bites [71]; however, the possibility of transmission of the virus through mosquito bites and in a food-borne way has also been reported. The Middle East region is recognized as the predominant area for the spread of the virus and its vector [71,72]; AHFV was first isolated from a patient in Mecca (Saudi Arabia), in the mid-1990s [71]. Symptoms of the disease include fever and headache; severe complications are represented by hemorrhagic manifestations and encephalitis, and the mortality rate of the disease is about 20–25% [72,73,74].
Kyasanur Forest disease virus (KFDV) (Table 1, Figure 1a) was discovered in the 1950s in the state of Karnataka in southern India [73]. In addition to various rodents and birds, susceptible organisms in the wild are monkeys [73]. The infection of humans and animals occurs mainly through the bites of Haemaphysalis ticks. However, the detection of the virus among Ixodes, argas, Ornithodoros, Hyalomma, Dermacentor, and Rhipicephalus ticks has also been reported [73]. Domestic animals such as cows are also bitten [73]. Over time, the number of states in India where outbreaks were recorded among the local population increased [73,75]. In recent decades, an increase in the number of cases has been reported; for example, between 2003 and 2012, a total of more than 3 thousand human cases were reported in Karnataka (of which 28 cases were fatal) [73,75]. Direct person-to-person transmission has not yet been reported. The main manifestation of the disease is fever, sometimes with hemorrhagic and neurological manifestations [73,75]. Approximately 20% of cases have severe symptoms with hemorrhagic and neurological symptoms (including encephalitis) [73,75].
Locally distributed Omsk hemorrhagic fever virus (OHFV) (Table 1, Figure 1b) is also an important pathogen. The main region of the distribution of OHFV are the Western Siberia parts of Russia [76,77]; however, a group of researchers recently presented a publication that reported the first case of detection of OHFV outside Russia—in the territories of Kazakhstan [78], including areas non-adjacent to Western Siberia. The discovery of a new distribution area for OHFV may be associated with the migration of the main vertebrate hosts—muskrat (Ondathra zibethicus) or water vole (Arvicola amphibius Syn. Arvicola terrestris) [78,79]. The main arthropod hosts of the virus are the ixodid ticks Dermacentor marginatus and Dermacentor reticulatus [76,79]. In addition, OHFV has been isolated from Aedes and Mansonia mosquito genera, but their role as vectors is minor [76]. The dynamics of incidence since the discovery of OHFV has changed in different periods, with the largest number of cases recorded in the period from 1945 to 1972 [77]. Symptoms of the disease include fever and hemorrhagic manifestations, but a third of patients may develop pneumonia, meningitis, kidney damage, or a combination of manifestations [76].
Powassan virus (POWV) (Table 1, Figure 1b) is considered an endemic pathogen in North America, causing encephalitis, but several cases of infection with this virus have also been reported in Russia [80,81]. Related to POWV, deer tick virus (DTV) (Table 1, Figure 1a) is also recognized as a rare but important agent of neuroinfections. The virus was first isolated from the ixodid tick Ixodes scapularis in 1997 in North America. The work of Tavakoli et al. [82] describes a case of necrotizing meningoencephalitis with a fatal outcome in an adult patient.
Orthomyxoviridae. Two closely related members of this family belonging to the genus Thogotovirus are also viruses transmitted by tick bites. Dhori virus (DV) (Table 1, Figure 1a) and Thogoto virus (TV) (Table 1, Figure 1b) remain relatively poorly studied, but have been reported to cause a range of clinical manifestations, from self-limited febrile state to meningoencephalitis and encephalitis [83,84].
Dhori virus (DV) was originally isolated from Hyalomma dromedarii camel ticks in Dhori state, India [84]. In addition to India, the virus has also been detected in carriers in the Astrakhan region of Russia, in southern Portugal, Central Asia, Kenya, etc. Dhori virus was also found in mosquitoes; a number of authors do not exclude the possibility of transmission of this pathogen from human to human [84].
Thogoto virus (TV) was first isolated from Boophilus decoloratus and Rhipicephalus spp. ticks, collected from cattle in the Thogoto Forest in Nairobi, Kenya, in 1960. In Europe, this virus was discovered a few years later in Sicily in 1969. Reports of human cases included bilateral optic neuritis and a case of fatal meningoencephalitis associated with hepatitis [84].
Phenuiviridae are a large family of RNA-containing arboviruses, pathogenic for humans and animals, currently including 19 recognized genera and more than 100 species [85]. Phenuiviruses have a wide geographic distribution, and the range of competent vectors includes ticks and dipterous insects [85].
A representative of the family, Bhanja virus (BHAV) [79,84,86,87] (Table 1, Figure 1a) (Bandavirus) was first isolated from Haemaphysalis intermedia ticks in Banjanagar, India, in 1954 [84]. The virus is now known to be transmitted by ixodid ticks of several genera such as Amblyomma, Boophilus, Dermacentor, Haemaphysalis, and Rhipicephalus. The prevalence of BHAV ticks is not limited to India. In competent hosts, the virus is found in areas with warm climates and steppe vegetation, in Central Asia, Europe (in regions of Italy and Bulgaria), Africa, and several regions of Southeast Asia [84]. In humans, BHAV causes a febrile illness, sometimes with meningoencephalitis or encephalitis, photophobia, vomiting, and paresis.
Sedoreoviridae. The genus Orbivirus of the family contains more than 100 subspecies, classified into 14 serogroups, infecting a wide range of arthropod and vertebrate hosts [88,89]. Most members of this genus infect vertebrates but not humans, although transmission to humans is thought to be possible. Recognized vectors involved in the transmission of these viruses include a wide range of invertebrate intermediate hosts, such as mosquitoes, midges, and ticks [88,89].
For humans, three species of orbiviruses pose a danger as etiological agents of neuroinflammation, namely, Kemerovo virus (KEMV) (Table 1, Figure 1a), Lipovnik virus (LIPV) (Table 1, Figure 1a), and Tribec virus (TRBV) (Table 1, Figure 1b), common in Russia and Eastern Europe [88,89].
Ticks of the genus Ixodes in Russia (Western Siberia is an endemic region) transmit Kemerovo virus (KEMV). This virus has also been detected in migrating birds (Phoenicurus phoenicurus) in Egypt, and in Hyalomma anatolicum ticks in Uzbekistan, which indicates a more complex and widespread distribution of the pathogen [88,89,90]. In humans, KEMV infection is associated with the development of aseptic meningitis, meningoencephalitis, and encephalitis [88,89,90].
Lipovnik virus (LIPV) is also common in Ixodes ricinus ticks. Presumably, competent amplification hosts are various wild forest rodents living in the territories of Slovakia and the Czech Republic. In case of an unfavorable outcome, after being bitten by an infected tick, a person also develops aseptic meningitis, meningoencephalitis, or encephalitis [58,88,89,90].
Tribec virus (TRBV) is transmitted by ixodid ticks in the territories of Slovakia, Moldova, Romania, Belarus, and Italy. Amplification hosts are small wild rodents: the virus has so far been found in voles and hares. The virus has also been detected in migrating birds and domestic goats. Infection occurs after a tick bite, and can subsequently lead to meningitis, meningoencephalitis, or encephalitis, as is the case with the KEMV and LIPV viruses [58,88,89,90].
Spinareoviridae. Colorado tick fever virus (CTFV) (Table 1, Figure 1a) and Eyach virus (EyV) (Table 1, Figure 1a), belonging to the genus Coltivirus, have been described as agents that cause febrile illnesses and neuroinfections.
The range of vectors of the Colorado tick fever virus include forest hard ticks of the Dermacentor genus, Haemaphysalis leporispalustris species, and Ixodes genus, and the soft tick Otobius lagophilus [52,84,91,92,93]. The main regions of distribution of these viruses are North America for CTFV [84] and Europe for EYAV [94,95]. In addition to direct transmission through a tick bite, CTFV may also be transmitted from person to person, through blood transfusion, or congenitally through maternal infection [94]. Severe manifestations of CTFV infection may include aseptic meningitis, encephalitis, and meningoencephalitis [52,84,96].
Eyach virus was isolated from Ixodes ricinus and Ixodes ventalloi, and the clinical manifestations of the infection include meningoencephalitis [58,59,84,94,95].
Table 1.
List of tick-borne viral pathogens of neuroinflammation.
| Family | Genus | Species/ Acronym(s) |
Common Names or Subspecies/ Acronym(s) |
Genome | Host-Source, Vector, Transmission |
Geographic Distribution |
NS Pathology | Reference |
|---|---|---|---|---|---|---|---|---|
| (Sub)Species Complex/ Acronym(s) | ||||||||
|
Flaviviridae
Flaviviridae |
Orthoflavivirus |
Orthoflavivirus
encephalitidis |
Tick-borne encephalitis virus/ TBEV |
ssRNA(+) |
Hs: Sylvatic birds, rodents, domestic ruminants V: Hard ticks (Dermacentor reticulatus, Ixodes persulcatus, Ixodes ricinus) T: With tick bites—primarily; Food-borne way (raw milk and dairy products); SOT—rare cases. |
Highly endemic regions: China (Inner Mongolia, Northwestern parts of China), Russia, Belarus, Ukraine, Croatia, Poland, Baltic countries, Czech Republic, Southern Germany, Austria, Sweden New endemic areas: France (Bordeaux region), Italy, Japan, Netherlands, England, South Korea, Mongolia, Denmark, Kazakhstan, Kyrgyzstan, Armenia, Azerbaijan, Uzbekistan |
Meningitis, encephalitis, Meningoencephalitis, encephalitis, meningitis, poliomyelitis like flaccid paralysis, polyradiculoneuritis | [46,62,63,79,97,98,99,100,101,102] |
| Negishi virus 1/ NEGV |
ssRNA(+) |
Hs: Small mammals (large Japanese field mouse—Apodemus speciosus; small Japanese field mouse—Apodemus argenteus; grey red-backed vole—Myodes rufocanus; brown rat—Rattus norvegicus)—presumably V: Hard ticks (Ixodes ovatus—presumably) T: With tick bites |
Japan | Encephalitis | [52,103,104] | |||
| Orthoflavivirus loupingi | Louping-ill virus/ LIV |
ssRNA(+) |
Hs: Sheep, goats, domestic sheep dog, yellow-necked mouse (Apodemus sylvaticus), common shrew (Sorex araneus), mountain hare (Lepus timidus), red grouse (Lagopus lagopus scoticus) V: Hard ticks (Ixodes ricinus) T: With tick bites—primarily; Food-borne way (raw milk); Contact with contaminated animal blood; Laboratory-acquired infection. |
England, Scotland, Ireland, Norway, Denmark (Bornholm), Russian Federation (Primorsky Krai) | Encephalitis | [52,67,69] | ||
|
Orthoflavivirus
kyasanurense |
Alkhumra hemorrhagic fever virus/ AHFV |
ssRNA(+) |
Hs: Camels, sheep V: Hard ticks (Hyalomma dromedarii), soft ticks (Ornithodoros savignyi) T: With tick bites—primarily; Food-borne way (raw milk); Contact with contaminated animal blood. |
Highly endemic regions: Saudi Arabia, Egypt |
Encephalitis | [72,73,74] | ||
| Kyasanur Forest disease virus/ KFDV |
ssRNA(+) |
Hs: Black-faced langur (genus Semnopithecus), red-faced bonnet macaque (Macaca radiate); forest rats, shrews, white-bellied rat (Niviventer niviventer), squirrels, bats (Rhinolophus rouxi), ground-dwelling birds, Indian crested porcupines (Hystrix indic) V: Hard ticks (Haemophysalis spinigera) T: With tick bites |
India (Goa, Karnataka, Kerela, Maharashtra, Tamilnadu states) | Encephalitis, aseptic meningitis-like picture | [73,75] | |||
|
Orthoflavivirus
omskense |
Omsk hemorrhagic fever virus/ OHFV |
ssRNA(+) |
Hs: Muskrats (Ondatra zibethicus), water vole (Arvicola terrestris); other local species of rodents V: Hard ticks (Dermacentor reticulatus, Dermacentor marginatus—primarily; Ixodes persulcatus, Ixodes apronophorus—rarely) T: With tick bites—primarily; Contact with blood and raw muskrat leather-material—rarely. |
Highly endemic regions: Russia (Kurgan, Omsk, Tyumen, Novosibirsk regions); Kazakhstan (Almaty region (human CSF sample), Akmola region (ticks), West Kazakhstan (rodents)) |
Encephalitic symptoms (continuous headache and meningism) |
[76,78,79] | ||
|
Orthoflavivirus
powassanense |
Powassan virus/ POWV |
ssRNA(+) |
Hs: Woodchuck (Mormota monax)—main reservoir; skunk (Mephitis mephitis); sylvatic wild rodents; carnivores V: Hard ticks Dermacentor andersoni—Colorado; Haemaphysalis neumanni—Primorsky Krai, Russia T: With tick bites |
Highly endemic regions: Russia (Far East); US (Colorado, Connecticut, Massachusetts, South Dakota, West Virginia); Canada (Alberta, British Columbia, Nova Scotia) |
Meningitis, encephalitis, encephalomeningitis | [79,80,104,105,106,107] | ||
| Deer tick virus/ DTV |
ssRNA(+) |
Hs: White-footed mouse (Peromyscus leucopus)—main reservoir; sylvatic wild rodents; carnivores V: Hard ticks (Dermacentor andersoni, Ixodes scapularis) T: With tick bites |
North US (Hudson Valley, Nantucket Island, Prudence Island); Canada | Encephalitis, meningopolio-encephalitis, meningopoliomyelitis | [82,106,107] | |||
| Orthomyxoviridae | Thogotovirus |
Thogotovirus
dhoriense |
Dhori virus/ DV |
ssRNA(−) |
Hs: Banded mongooses (Mungos mungo); wild and domestic rodents; domestic ruminants V: Hard ticks (Amblyomma gemma, Hyalomma marginatum, Hyalomma dromedarii); may be transmitted by mosquitoes (Anopheles hyrcanus, Aedes caspius, Culex hortensis) T: With tick bites |
Focally endemic worldwide spread in natural boskematic foci; Southern Portugal, Egypt, Astrakhan (Volga delta), Kenya (eastern and northeastern provinces), India, Armenia, Azerbaijan, Kirghizia, Uzbekistan | Meningoencephalitis, encephalitis-like reaction, encephalitis |
[83,84] |
| Thogotovirus thogotoense | Thogoto virus/ TV |
ssRNA(−) | Hs: Cattle, camels V: Hard ticks (Amblyomma variegatum, Hyalomma anatolicum, Hyalomma eruncatum, Rhipicephalus appendiculatus, Rhipicephalus evertsi, Rhipicephalus sanguineus) T: With tick bites |
Nigeria, Kenya, Uganda, Ethiopia, Cameroon, Central Africa, Egypt, Iran | Bilateral optic neuritis, fatal meningoencephalitis |
[84] | ||
| Phenuiviridae | Bandavirus |
Bandavirus
bhanjanagarense |
Bhanja virus/ BHAV |
ssRNA(+/−) |
Hs: Cattle, sheep, goats V: Hard ticks (Amblyomma variegatum, Boophilus annulatus, Boophilus decoloratus, Boophilus geigyi, Dermacentor marginatus, Haemaphysalis salctata, Rhipicephalus bursa, Rhipicephalus appendiculatus, etc.) T: With tick bites |
Focally endemic worldwide spread in natural boskematic foci; Europe (Italy, Bulgaria); India |
Meningoencephalitis, encephalitis, paresis | [79,84,86,87] |
| Sedoreoviridae | Orbivirus |
Great Island virus/ GIV |
Kemerovo virus 1/ KEMV |
dsRNA |
Hs: Migrating bird (redstarts—Phoenicurus phoenicurus, in Egypt) V: Hard ticks (Ixodes persulcatus—Russia; Hyalomma anatolicum—Uzbekistan) T: With tick bites |
Highly endemic region: Western Siberia (Kemerovo region) Egypt (from migratory birds) |
Aseptic meningitis, meningoencephalitis, encephalitis | [88,89,90] |
| Lipovnik virus 1/ LIPV |
dsRNA |
Hs: Sylvatic rodents? V: Hard ticks (Ixodes ricinus) T: With tick bites |
Slovakia, Czech Republic | Aseptic meningitis, meningoencephalitis, encephalitis | [58,88,89,90] | |||
| Tribec virus 1/ TRBV |
dsRNA |
Hs: Rodents (bank vole—Clethrionomys glareolus; pine vole—Microtus pinetorum; hare—Lepus europeus); goats; birds (European starling—Sturnus vulgaris; common chaffinch—Fringilla coelebs) V: Hard ticks (Ixodes ricinus – Czechoslovakia, Moldova; Haemaphisalis punctate –Romania) T: With tick bites |
Slovakia, Moldova, Romania, Italy, Belarus | Aseptic meningitis, meningoencephalitis, encephalitis | [58,88,89,90] | |||
| Spinareoviridae | Coltivirus |
Colorado tick
fever coltivirus |
Colorado tick fever virus/ CTFV |
dsRNA |
Hs: Golden-mantled ground squirrels (Callospermophilus lateralis); chipmunks (Tamias spp.) V: Wood hard tick (Dermacentor andersoni); also hard ticks (Dermacentor albopictus, Dermacentor arumapertus, Dermacentor occidentalis, Haemaphysalis leporispalustris, Ixodes sculptus, Ixodes spinipalpis); also soft ticks (Otobius lagophilus) T: With tick bites; with blood transfusion (from infected humans) |
Highly endemic region: Western parts of North US; Canada (Alberta, British Columbia) |
Aseptic meningitis, encephalitis, meningoencephalitis | [52,84,96] |
| Eyach coltivirus | Eyach virus/ EyV |
dsRNA |
Hs: European rabbit (Oryctolagus cunniculus) V: Hard ticks (Ixodes ricinus, Ixodes ventalloi) T: With tick bites |
Germany, France | Meningoencephalitis | [58,59,84,94,95] | ||
Taxonomic and trivial names are given according to the reports of the International Committee on Taxonomy of Viruses (ICTV) https://ictv.global/msl and https://ictv.global/vmr (versions from 2022/2023); 1 Commonly accepted alternative names not given in the reports of the International Committee on Taxonomy of Viruses (ICTV) (see above); SOT—Solid organ transplantation.
2.2. Mosquito- and Midge-Borne Viral Neuropathogens
Diptera, such as mosquitoes and midges, are even more effective agents of arbovirus transmission. The dynamics of distribution are influenced by many factors, but given the rapid climate change and anthropogenic influences, there is a risk of expansion of the original habitats of vectors, including dipterans, for example, through the inclusion of new intermediate hosts such as rodents [108] or birds [79].
Flaviviridae. Bussuquara virus (BSQV) (Table 2, Figure 2c), Iguape virus (IGUV) (Table 2, Figure 2c), and Cacipacoré virus (CPCV) (Table 2, Figure 2a) are mainly transmitted to humans through the bites of infected Aedes mosquitoes in endemic regions of Brazil. Like other viruses classified in the genus, CPCV, BSQV, and IGUV have important medical significance as pathogens capable of causing, in addition to fever, severe manifestations including encephalitis [109,110]. The causative agent of Dengue fever, Dengue virus (DENV) (Table 2, Figure 2c) is transmitted through the bites of mosquitoes of the genus Aedes spp. The greatest burden of disease from DENV is experienced by populations living in tropical and subtropical regions (the number of human cases of infection is estimated to range from 100 to 400 million) [111]. DENV usually occurs in a mild or asymptomatic form, but in some cases, the disease can progress to hemorrhagic fever and cause encephalopathy, polyneuritis, cerebellitis, etc.
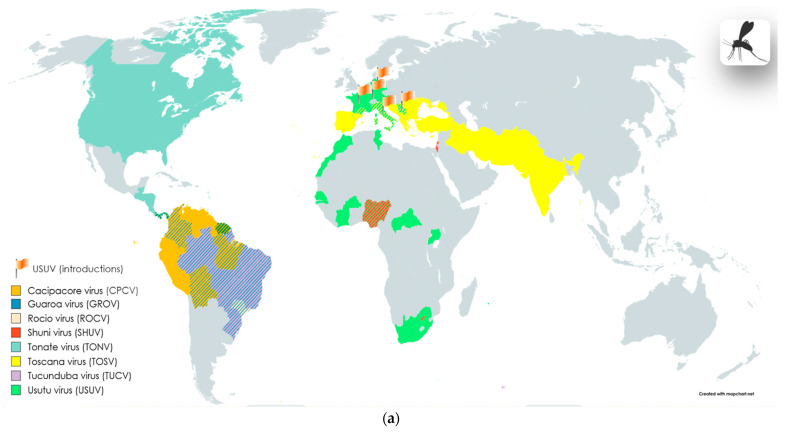
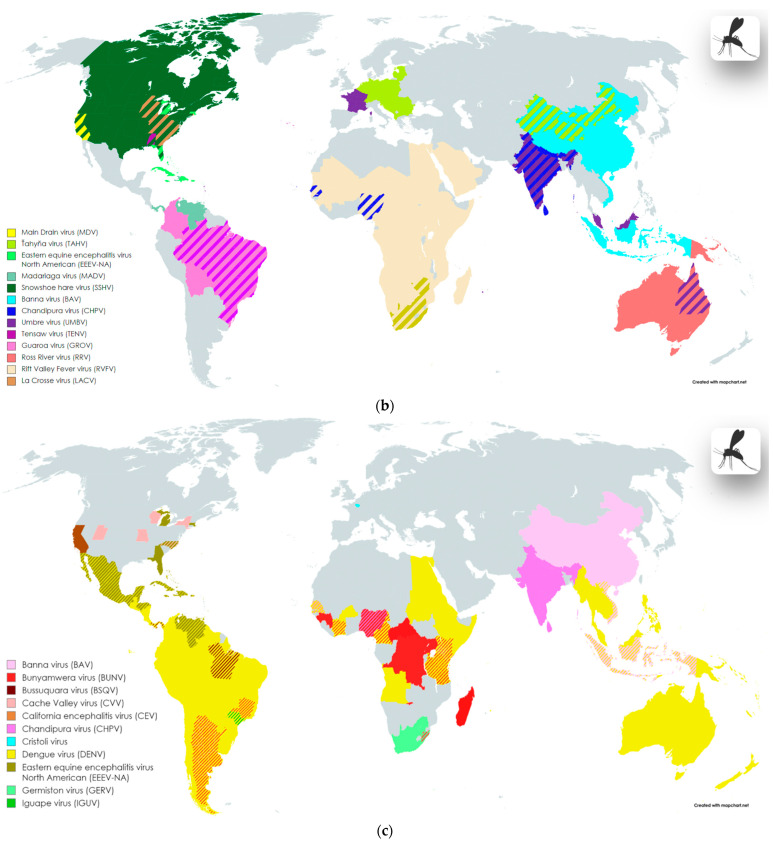
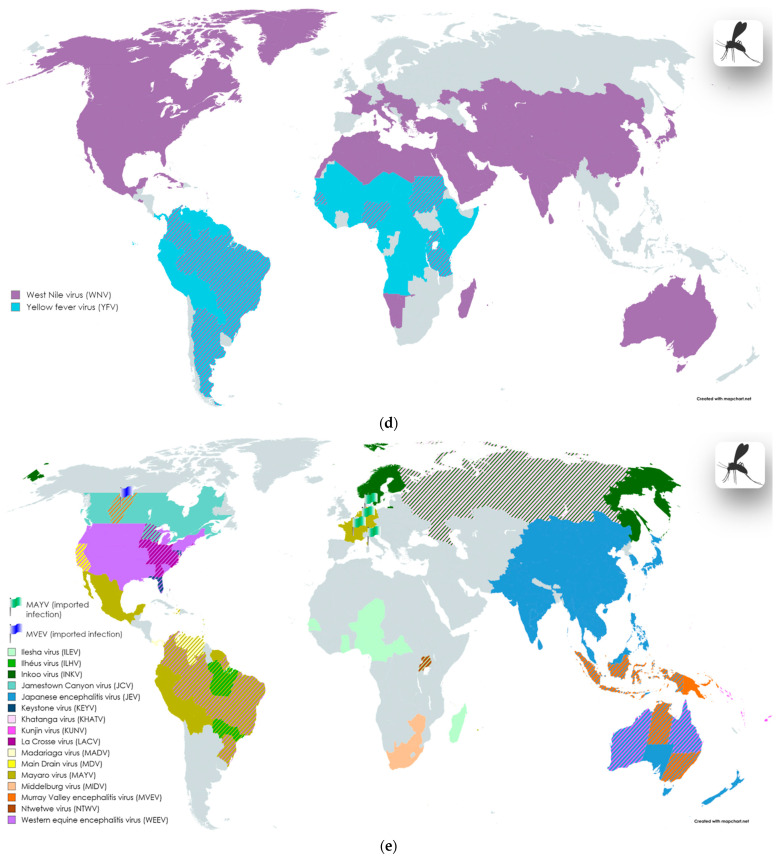
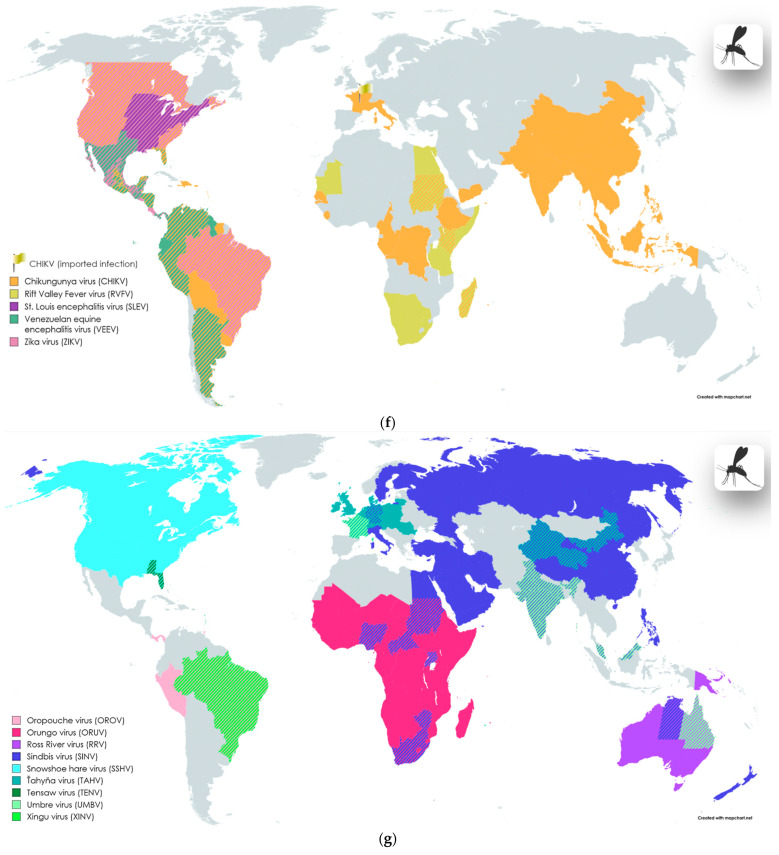
Figure 2.
Geographic distribution of mosquito- and midge-borne infections, including areas of endemic and imported cases involving nervous system symptoms. The division into blocks (a–g) was implemented to enhance the visualization of data on the maps; information about the taxonomic groups located on each block is provided in the legend within the pictures, as well as in the main text alongside the first mention of the corresponding virus; imported cases are marked with flags. Maps were created with the Map Chart online map-making tool (https://www.mapchart.net/index.html, accessed on 7 May 2024); graphic objects were created with the BioRender online science illustration making tool (https://www.biorender.com/, accessed on 7 May 2024). The images may contain slight inaccuracies in depicting the boundaries of virus distribution areas due to the limitation of the map scale and the choice of scientific sources utilized to create these illustrations.
Yellow fever virus (YFV) (Table 2, Figure 2d) circulates in a cycle between non-human primates and mosquitoes of the genera Aedes, Haemagogus, and Sabethes [112,113,114,115,116,117,118]. The transmission of the virus to humans and non-human primates occurs after the bite of an infected insect, but also, in some regions of Africa, cases of transmission through the bites of the Amblyomma variegatum tick have been reported [112,113,114,115,116,117,118]. The main regions where the virus spreads are Africa and South America. In some cases, Yellow fever virus infection may be characterized by systemic damage, including the liver, kidneys, and nerve tissue. Nervous system complications of yellow fever include encephalitis (including YFV vaccine-associated encephalitis), ADEM, and meningitis [112,113,114,115,116,117,118].
Ilheus virus (ILHV) and Rocio virus (ROCV) are important etiological agents of encephalitis in South America. Ilheus virus (ILHV) Table 2, Figure 2e) has been reported to cause severe febrile illness, and cases of encephalitis have been reported in Central and South America and Trinidad [109]. Rocio virus (ROCV) (Table 2, Figure 2a) is associated with a large outbreak of epidemic encephalitis in the 1970s, recorded in southeast Brazil [109]. ROCV is transmitted by mosquitoes of the genus Ochleratus from the reservoir host—Zonotrichia capensis sparrows; however, the complete epidemiological cycle of this virus is not precisely defined [119].
Japanese encephalitis virus (JEV) (Table 2, Figure 2e) is transmitted through the bite of Culex spp. The endemic area for the spread of the virus is the Asia–Pacific region. The virus circulation cycle is associated with wild waterfowl and domestic animals [120]. According to the WHO, the annual number of cases of the disease reaches 70 thousand, and the mortality rate is estimated at 20–30% [120].
St. Louis encephalitis virus (SLEV) (Table 2, Figure 2f) is common in the United States. The transmission cycle of the virus includes wild and domestic birds, and mosquitoes of the Culex genus as vectors [121,122,123,124]. Murray Valley encephalitis virus (MVEV) (Table 2, Figure 2e) is endemic to the territories of Australia and Oceania. The virus transmission cycle includes a variety of animals and waterfowl [125,126,127,128]. West Nile virus (WNV) (Table 2, Figure 2d) is transmitted by Culex spp. mosquito bites, and the reservoirs of the virus are mainly wild birds. The neuroinvasive form of the infection is the most severe form of the disease; more often, the infection in humans may be asymptomatic or manifest in a mild form [129,130,131,132].
Kunjin virus (KUNV) (Table 2, Figure 2e) is found in Australia and Oceania, like MVEV, severe manifestations of this rare infection can include encephalitis [133,134]. Usutu virus (USUV) (Table 2, Figure 2a) is distributed throughout the African continent, but has also been detected in European countries. The transmission cycle of the virus includes small insectivorous bats, rodents, and shrews; the virus is transmitted by Culex annulirostris mosquitoes [135,136,137,138].
Zika virus (ZIKV) (Table 2, Figure 2f) is transmitted to humans by Aedes aegypti and Aedes albopictus mosquito bites. For a long time, it was believed that the spread of the Zika virus was limited, but since 2015, the number of cases of this virus has sharply increased in a number of countries [139,140]. Outbreaks have been reported in Brazil and Central and North America. Infections were associated with significant increases in the incidence of microcephaly and Guillain–Barré syndrome in outbreak regions [139,140]. Evidence suggests that ZIKV may exhibit a higher affinity for placental cells compared to other flaviviruses [141]. Infants exposed to ZIKV during prenatal development, even without structural brain pathologies, may still experience neurological sequelae and developmental delays [142]. Currently, there is compelling evidence linking ZIKV to the aforementioned pathologies; however, further investigation of this phenomenon is warranted.
Peribunyaviridae. Representatives of the genus Orthobunyavirus, assigned to this family, include a wide range of arboviruses, including those transmitted by dipteran insects. This review included 17 species associated with CNS lesions. CNS diseases associated with orthobunyaviruses can be divided into two types: congenital and postnatal. In humans, the most common postnatal diseases of the central nervous system are meningitis and encephalitis [143]. Ortabunyaviruses are widely represented in endemic regions around the world, and are not only limited to regions with warm climates, i.e., they do not only refer to tropical pathogens [79,143].
Bunyamwera virus (BUNV) (Table 2, Figure 2c) was first isolated in 1943 from Aedes mosquitoes in Uganda [144,145]. In the 1950s, the virus was detected in KwaZulu-Natal in a sample from an adult male with severe headache, neck stiffness, and fever. Another study conducted in the same area revealed a 54% seropositivity rate among adults [144]. The predominant vectors of the spread are mosquitoes; however, Binder et al. reported the detection of BUNV in ixodid ticks [146]. Nowadays, several African countries are considered as endemic areas [145]; however, detections of the virus have also been reported outside Africa, in Brazil and Argentina [145,146]. In 2013, BUNV was first isolated from horses with neurological symptoms and a fatal outcome in Argentina [145]. In humans, BUNV predominantly causes mild illness characterized by febrile symptoms, and the onset of severe symptoms is common in children [145]. But in immunocompromised patients, BUNV infection can progress to encephalitis and meningitis [144,145]. Other mammals are also susceptible to infection, including domestic ruminants, in which infection results in severe symptoms such as spontaneous abortion and fetal defects [145]; antibodies to the virus have also been detected in a number of waterfowl in the KwaZulu-Natal province of South Africa [144].
Germiston virus (GERV) (Table 2, Figure 2c) is transmitted through the bites of Culex mosquitoes. In rare cases, infection is also possible through contact with infected tissues. The region of virus circulation is reportedly represented by Africa, in particular, the South Africa region. Complications of the disease after infection with this virus can manifest as meningoencephalitis and encephalitis [79,143,144,147].
Xingu virus (XINV) (Table 2, Figure 2g) was discovered in Brazil, and the natural vectors of the virus are mosquitoes (as for many other viruses in the Orthobunyavirus genus) [79,148]. Xingu is a member of the Bunyamwera serogroup [79,148]. The incidence of this virus is expected to be limited to very rare sporadic cases. A fatal case of Xingu disease was reported in which the patient presented with fever, headache, and jaundice [148]. However, the patient was also seropositive for hepatitis B, which in turn makes it difficult to remember the role of the virus in the development of the disease [148]. Additionally, there is a mention of the manifestation of infection with meningoencephalitis [79].
Cache Valley virus (CVV) (Table 2, Figure 2c) is reportedly circulating in several states in the United States; the main vectors of the virus are mosquitoes of the genus Culex. In humans, the manifestations of infection can include brain lesions (meningitis, meningoencephalitis, and encephalitis) [149,150,151,152].
California encephalitis virus (CEV) (Table 2, Figure 2c), Jamestown Canyon virus (JEV) (Table 2, Figure 2e), Keystone virus (KEYV) (Table 2, Figure 2e), Main Drain virus (MDV) (Table 2, Figure 2e), snowshoe hare virus (SSHV) Table 2, Figure 2b), La Crosse virus (LACV), (Table 2, Figure 2b) and Tensaw virus (TENV) (Table 2, Figure 2b) as well as Cache Valley virus, are also endemic to the United States and Canada. All of these viruses are transmitted to susceptible mammals through mosquito and midge (for Main Drain virus [66,143]) bites. However, for Tensaw virus, cases of intrauterine transmission have been documented, leading to the subsequent development of brain pathologies in the fetus. The clinical manifestations of infection with these viruses in humans include meningitis, encephalitis, and meningoencephalitis (see Table 2).
Cristoli virus (Table 2, Figure 2c), recently identified in France, was obtained from a patient with fatal encephalitis and an immunosuppressed status [153]. Mosquitoes are currently the suspected vectors of the virus [153]. Cristoli virus is closely related to Umbre virus, a member of the Turlock serogroup not previously associated with human disease [153]. The authors of the work [153] describing this clinical case suggested that Cristoli virus is endemic in France.
Khatanga virus (KHATV) (Table 2, Figure 2e) was found in the territory of the Russian Federation, in both the European part and Siberia. Amplification hosts include various wild sylvatic animals and, in some cases, domestic animals [79,154,155]. KHATV transmission occurs through the bites of blood-sucking insects of the genera Aedes, Culiseta, Culex, and Anopheles. Infection in humans may be accompanied, in particular, by encephalitis.
Inkoo virus (INKV) (Table 2, Figure 2e) is spread in the Russian Federation and Northern European countries, and transmitted by the bites of Aedes mosquitoes. In humans, INKV infection can cause encephalitis and other complications of the nervous system [52,79,156,157,158,159].
Ťahyňa virus (TAHV) (Table 2, Figure 2b,g) was found in Central Europe and China (Xinjiang, Qinghai, and Inner Mongolia). TAHV infection can cause meningitis, meningoencephalitis, encephalomyelitis, and encephalitis [79,160,161,162,163,164,165,166].
Oropouche virus (OROV) (Table 2, Figure 2g) is distributed in Latin America and is considered one of the most important arboviruses causing febrile illness in humans [167,168]. Reported cases of Oropouche fever have occurred in Brazil, Panama, Peru, and Trinidad and Tobago [167,168]. Oropouche fever occurs mainly during the rainy season, which is associated with an increase in the number of the main vectors of the virus belonging to the genera Culex and Aedes [167,168]. It is also noted that in addition to the spread of the virus between the vector and a susceptible host (pale-throated sloths, non-human primates, and birds) in the sylvatic cycle, the virus is well transmitted in the urban cycle between already infected people with the participation of the Culicoides paraensis vector [167,168]. There have been cases of CNS lesions occurring in patients; however, some of these patients already had concomitant diseases, including neurocysticercosis [168]. In total, during the entire observation period, fewer than 10 sporadic cases of central nervous system damage due to OROV infection were recorded in medical practice [168].
Tucunduba virus (TUCV) (Table 2, Figure 2a) and Guaroa virus (GROV) (Table 2, Figure 2a,b) are also common in Latin America. GROV transmission occurs through the bites of Anopheles mosquitoes [143,169], and TUCV is transmitted by mosquitoes of the genera Culex, Wyeomia, Sabethes, Psorophora, Limatus, and Trichoprosopon [170]. Complications in the nervous system can manifest as meningoencephalitis [170] and paresis [143,169].
Shuni virus (SHUV) (Table 2, Figure 2a) is transmitted by mosquitoes and Cullicoides midges; the virus is distributed in the territories of South Africa (Gauteng Province), Israel, and Nigeria; in some cases, complications of the disease may include meningitis and encephalitis [66,171].
Ntwetwe virus (NTWV) (Table 2, Figure 2e) and Ilesha virus (ILEV) (Table 2, Figure 2e) also circulate in Africa. The circulation area of ILEV includes the territories of Cameroon, Central African Republic, Nigeria, Senegal, Uganda, Madagascar, Ghana, and Niger [144,172]. Clinical manifestations of the disease in the nervous system can include meningitis [144,172]. NTWV was found in Uganda in patients with fatal encephalopathy and encephalitis [143,173].
Umbre virus (UMBV) (Table 2, Figure 2b,g) was first discovered in mosquitoes (Culex genus) in India in the 1950s [174]. Further research was able to detect viruses similar to UMBV in Australia, Malaysia, and the south of France [174]. Two clinical cases of patients with encephalitis and weakened immunity caused by UMBV (found in biomaterial) were reported, potentially exposing its neuroinvasive potential [174].
Phenuiviridae. As reported above, representatives of this family are transmitted not only by ticks. Between mosquito- and sandfly-borne Phenuiviruses, the following pathogens are well known: Rift Valley fever virus (RVFV) and sandfly fever viruses (SFVs).
Rift Valley fever virus (RVFV) (Table 2, Figure 2b,f) is the causative agent of the febrile disease of the same name, most often found in African countries [139,175]. However, outside the African continent, cases have been reported in Europe, Asia, and the USA [139]. The main route of transmission of the virus to humans is through the bites of Culex mosquitoes; the transmission of the virus is also possible through contact with the blood and other biological material of infected domestic animals, for example, cows, goats, and buffalo [139]. The direct transmission (human-to-human) of the virus has not been recorded [139]. In animals, the virus causes severe disease, while in most humans, it is either asymptomatic or has mild febrile manifestations [139]. However, in approximately 10% of patients, the disease may present with bleeding and encephalitis [139].
The Sandfly fever group of viruses includes sandfly fever Sicilian virus (SFSV), sandfly fever Naples virus (SFNV), and Toscana virus (TOSV) (Table 2, Figure 2a), associated with human febrile diseases. The endemic region of distribution of these viruses includes Italy, France, Spain, Slovenia, Turkey, Portugal, and Greece [176,177,178]. In other countries, such as Sweden, cases of infection have also been reported. The transmission of these viruses occurs through the bites of the virus-competent phlebotomine midges Phlebotomus perniciosus and Phlebotomus perfiliewi [176,177,178]. In humans, the infection mainly causes a mild febrile illness with neurological damage (aseptic meningitis or encephalitis), sometimes with complete recovery. Other common symptoms are leukopenia, neck stiffness, a decreased level of consciousness, tremors, and paresis [176,177,178].
Rhabdoviridae. Chandipura virus (CHPV) (Table 2, Figure 2b,c) is an important cause of morbidity, primarily in India. However, apart from India, to date, CHPV has also been detected in Bhutan, Nepal, Sri Lanka, and African countries (Nigeria and Senegal) [179]. The virus was first discovered during a fever outbreak in 1965 in Nagpur, Maharashtra. The transmission cycle of CHPV involves mosquitoes, which are thought to carry the virus continuously in endemic regions [179]. The presence of neutralizing antibodies to CHPV in the blood of pigs, buffalo, cattle, goats, and sheep indicates the constant circulation of the virus in the regions of distribution. CHPV is the causative agent of acute encephalitis, especially among children under 15 years of age [179]. A critical feature of the infection is the sudden onset of clinical symptoms, including neurological complications (within 24 h) and a high mortality [179].
Sedoreoviridae. Arboviruses Orungo virus (ORUV) and Banna virus (BAV) are rare causative agents of febrile diseases, and, in some cases, with complications in the nervous system. Orungo virus (ORUV) (Table 2, Figure 2g) is transmitted by Aedes spp., Culex spp., and Anopheles spp. in regions of sub-Saharan Africa. Manifestations of infection in humans include acute fever and headaches. One case of encephalitis in a child, with convulsions and flaccid paralysis, has also been reported [88]. For Banna virus (BAV) (Table 2, Figure 2b,c), the vectors are Culex spp. and presumably other types of mosquitoes. There are reports in the literature of BAV infection in humans, manifested in flu-like symptoms, myalgia, fever, and encephalitis [180].
Togaviridae. Many important pathogens of humans and animals are included in the genus Alphavirus, including viruses transmitted by mosquito bites: Eastern equine encephalitis virus North American (EEEV-NA), Venezuelan equine encephalitis virus (VEEV), Western equine encephalitis virus (WEEV), and Chikungunya virus (CHIKV). Madariaga virus (MADV) (Table 2, Figure 2b,e) [181,182,183,184], Mayaro virus (MAYV) (Table 2, Figure 2e) [103,185,186], Middelburg virus (MIDV) (Table 2, Figure 2e) [187,188], Ross River virus (RRV) (Table 2, Figure 2b,g) [189,190], Sindbis virus (SINV) (Table 2, Figure 2g) [70,158,159,181,191], and Tonate virus (TONV) (Table 2, Figure 2a) [192,193] are recognized as relatively rare but important causative agents of neuroinfections in humans, including encephalitis and aseptic meningitis. The geographic distribution of these viruses is currently limited to the tropical regions of South and Central America, with the exception of RRV (New Guinea and Australia), MIDV (South Africa and Zimbabwe), and SINV. The latter has been repeatedly discovered in various regions of the globe with very different climatic conditions: in African countries, Australia, Europe, Russia, and Asian countries.
Chikungunya virus (CHIKV) (Table 2, Figure 2f) was first described after a series of outbreaks in India and South Asia in the 1960s. The virus is endemic to tropical and subtropical regions. The transmission of the virus is mainly carried out by Aedes aegypti and Aedes albopictus [129,139]. Chikungunya fever, in addition to cases where complications in the nervous system are observed, such as encephalitis and convulsions, is also manifested in a rash, headache, and severe polyarthralgia [129,139].
Eastern equine encephalitis virus North American (EEEV-NA) (Table 2, Figure 2b,c), Venezuelan equine encephalitis virus (VEEV) (Table 2, Figure 2f), and Western equine encephalitis virus (WEEV) (Table 2, Figure 2e) are distributed in South and North America. All three viruses actively circulate in the vector cycle, which includes wild birds, rodents, and mosquitoes. Transmission to humans occurs through Culex and Aedes mosquito bites. Although the disease caused by these viruses is self-limiting, neurological complications can include severe encephalitis, with a mortality rate of 30 to 75% in humans.
Table 2.
List of mosquito- and midge-borne viral agents of neuroinflammation.
| Family | Genus | Species | Common Names or Subspecies/ Acronym(s) |
Genome | Host-Source, Vector, Transmission |
Geographic Distribution |
NS Pathology | Reference |
|---|---|---|---|---|---|---|---|---|
| (Sub)Species complex/ Acronym(s) | ||||||||
| Flaviviridae | Orthoflavivirus |
Orthoflavivirus
aroaense |
Bussuquara virus/ BSQV |
ssRNA(+) |
Hs: Non-human primates, rodents, wild birds V: Mosquitoes (Culex spp.) T: With mosquito bites |
Brazil (Pará state), Panama |
Encephalitis | [110,129] |
| Iguape virus/ IGUV |
ssRNA(+) |
Hs: Wild birds V: Mosquitoes (Aedes spp.) T: With mosquito bites |
Brazil (Sao Paulo state) | Encephalitis | [109,110,194] | |||
|
Orthoflavivirus
cacipacoreense |
Cacipacoré virus/ CPCV |
ssRNA(+) |
Hs: Wild birds (Formicarius analis) V: Mosquitoes (Culex spp.) T: With mosquito bites |
Brazil (Pará and Rondônia states), Amazon region | Encephalitis | [129] | ||
|
Orthoflavivirus
denguei |
Dengue virus/ DENV |
ssRNA(+) |
Hs: Non-human primates (macaques—Macaca spp.; Surilis—Presbytis spp.) V: Mosquitoes (Aedes aegypti, Aedes albopictus, Aedes scutellaris, Aedes polynesiensis; Aedes furcifer, Aedes vittatus, Aedes tailori, Aedes luteocephalus—equatorial parts of Africa) T: With mosquito bites; Human-to-human contact (breastfeeding); Congenital infection. |
Focally worldwide spread; High treat: Africa (Sudan, Egypt, Eritrea, Djibouti, Ethiopia, Kenya, Somalia, Tanzania, Mauritius, Mozambique, Seychelles, Angola, Cameroon, Burkina Faso, Côte d’Ivoire, Senegal); the Caribbean basin, Central America, South America, southeastern Asia, Oceania |
Encephalitis, meningitis, meningoencephalitis, encephalomyelitis, acute cerebellitis, polyneuritis, encephalopathy, Parkinsonian symptoms |
[79,195,196,197,198,199,200,201,202] | ||
|
Orthoflavivirus
flavi |
Yellow fever virus/ YFV |
ssRNA(+) |
Hs: Non-human primates V: Mosquitoes (Aedes spp., Haemagogus spp., Sabethes spp.); ticks (Amblyomma variegatum)—in Africa, extremely rare T: With mosquito bites; With tick bites. |
Endemic regions: West Africa (Benin, Burkina Faso, Cape Verde, Côte d’Ivoire, Equatorial Guinea, Gambia, Ghana, Guinea, Guinea-Bissau, Liberia, Mali, Mauritania, Niger, Nigeria, Sao Tome and Principe, Senegal, Sierra Leone, Togo); Central Africa (Angola, Burundi, Cameroon, Central African Republic, Chad, Democratic Republic of the Congo, Gabon, Rwanda); East Africa (Ethiopia, Kenya, Somalia, Sudan, Tanzania, Uganda); Panama; South America (Argentina, Bolivia, Brazil, Colombia, Ecuador, Guyana, French Guyana, Paraguay, Peru, Suriname, Trinidad and Tobago, Venezuela) |
Encephalitis, YFV vaccine-associated encephalitis, ADEM, Guillain–Barré syndrome, meningitis, meningoencephalitis | [112,113,114,115,116,117,118] |
||
|
Orthoflavivirus
ilheusense |
Ilhéus virus/ ILHV |
ssRNA(+) |
Hs: Wild birds V: Mosquitoes (Aedes spp., Psorophora spp.) T: With mosquito bites |
Brazil (Pará and São Paulo states, Pantanal region) | Encephalitis | [129] | ||
| Rocio virus/ ROCV |
ssRNA(+) |
Hs: Rufous-collared sparrow (Zonotrichia capensis) V: Mosquitoes (Ochleratus spp., Psorofora ferox; specific antibodies: double-collared seedeater (Sporophila caerulescen); creamy-bellied thrush (Turdus amaurochalinus); equines; water buffalo (Bubalus bubalis); marsupials T: With mosquito bites |
Southeast Brazil (Sao Paulo state—endemic region); Other regions of virus circulation: Goiás state, Rio de Janeiro state, Mato Grosso do Sul state, Paraíba state, Mato Grosso state |
Encephalitis, meningoencephalitis, meningitis |
[119,133,203] | |||
|
Orthoflavivirus
japonicum |
Japanese encephalitis virus/ JEV |
ssRNA(+) |
Hs: Wild aquatic birds, domestic birds, domestic pigs V: Mosquitoes (Main vectors—Culex tritaeniorhynchus, Culex vishnui, Culex gelidus) T: With mosquito bites |
Focally worldwide spread; Asia–Pacific region, Southeast Asia, Australia |
Encephalitis, meningoencephalitis, meningitis | [120,204,205,206,207,208] | ||
|
Orthoflavivirus
louisense |
St. Louis encephalitis virus/ SLEV |
ssRNA(+) |
Hs: Sylvatic, peridomestic, and urban birds (sparrows—Passer sp.; pigeons—Columba sp.; blue jay—Cyanocitta cristata; robins—Turdus sp.) V: Mosquitoes (Culex tarsalis, Culex pipiens, Culex quinquefasciatus) T: With mosquito bites |
United States (Eastern and Central states) | Encephalitis, meningoencephalitis, meningitis | [121,122,123,124] | ||
|
Orthoflavivirus
murrayense |
Murray Valley encephalitis virus/ MVEV |
ssRNA(+) |
Hs: Wild animals: marsupials (kangaroos; agile wallabies—Notamacropus agilis); rabbits (Leporidae); rodents; wild birds—Galahs (Cacatuidae); water birds (rufous night heron—Nycticorax caledonicus; Pacific black duck—Anas superciliosa); domestic animals and birds V: Mosquitoes (Culex annulirostris, Culex sitiens) T: With mosquito bites |
Australia (Western Australia, Northern Territory, New South Wales, Victoria); Papua New Guinea; Indonesia; Canada (Alberta)—imported infection | Encephalitis | [125,126,127,128] | ||
|
Orthoflavivirus
nilense |
West Nile virus/ WNV |
ssRNA(+) |
Hs: Wild birds, domestic animals (horses, sheep), alligators, lake frog (Rana ridibunda—competent reservoir (Russia)) V: Mosquitoed (Culex spp.) T: With mosquito bites; Human-to-human transmission (organ transplantation, blood transfusion, placental route) |
Endemic region: East Africa (Uganda) Many cases: North America, Brazil, Middle East, Europe, Asia, Regions of Africa Worldwide spread |
Meningitis, encephalitis, poliomyelitis | [129,130,131,132,209,210] | ||
| Kunjin virus/ KUNV |
ssRNA(+) |
Hs: Wild birds, domestic animals (horses, sheep), alligators V: Mosquitoes (Culex annulirostris) T: With mosquito bites |
Australia (tropical north regions), Oceania | Encephalitis | [133,134] | |||
|
Orthoflavivirus
usutuense |
Usutu virus/ USUV |
ssRNA(+) |
Hs: Wild passerine birds, insectivorous microbats (Pipistrellus sp.), equines, rodents, shrews V: Mosquitoes (Culex spp., Aedes spp., Mansonia spp., Anopheles spp.) T: With mosquito bites |
Africa (South Africa, Central African Republic, Senegal, Côte d’Ivoire, Nigeria, Uganda, Burkina Faso, Tunisia, Morocco); Europe (introductions: France, Germany, Italy, Austria, Serbia) | Encephalitis, meningoencephalitis | [135,136,137,138] | ||
|
Orthoflavivirus
zikaense |
Zika virus/ ZIKV |
ssRNA(+) |
Hs: Non-human primates V: Mosquitoes (Aedes spp.) T: With mosquito bites; Human-to-human transmission (organ transplantation, blood transfusion, placental route); Contact with infected fomites. |
Brazil, Central and North America | Guillain–Barré syndrome, fetal microcephaly, myelitis, meningoencephalitis | [139,140,141,211] | ||
| Peribunyaviridae | Orthobunyavirus |
Orthobunyavirus
bunyamweraense |
Bunyamwera virus/ BUNV |
ssRNA(−) |
Hs: Wild waterfowls V: Mosquitoes (Aedes circumluteolus); hard ticks (Amblyomma dubitatum, Amblyomma sculptum)—presumably T: With mosquito bites; With tick bites—presumably |
Uganda, Tanzania, Mozambique, Nigeria, Guinea, South Africa (KwaZulu-Natal province), Democratic Republic of Congo, Botswana, Namibia (Caprivi region), Senegal, Ivory Cost, Cameroon, Central African Republic, Kenya, Madagascar; Argentina, Brazil (Minas Gerais (ticks)) | Encephalitis, meningitis | [144,145,146] |
| Germiston virus/ GERV |
ssRNA(−) |
Hs: Wild animals (virus isolation); domestic animals (antibody detection) V: Mosquitoes (Culex theileri, Culex rubinotus) T: With mosquito bites; Direct contact with infected tissue and fomites |
Africa; South Africa region | Encephalitis, meningoencephalitis (both sporadic cases; laboratory work infection); mental confusion | [79,143,144,147] | |||
| Xingu virus/ XINV |
ssRNA(−) |
Hs: Not identified V: Mosquitoes T: With mosquito bites—presumably |
South America (Brazil) | Encephalitis/meningoencephalitis (both sporadic cases) | [79,148] | |||
|
Orthobunyavirus
cacheense |
Cache Valley virus/ CVV |
ssRNA(−) |
Hs: Domestic ruminants (equines, cattle); deer V: Mosquitoes (Culex spp.) T: With mosquito bites |
US (Utah, North Carolina, Missouri, Wisconsin, New York) | Encephalitis, meningoencephalitis, meningitis | [149,150,151,152] | ||
| Cristoli virus 1 | – | ssRNA(−) |
Hs: Not identified V: Mosquito—presumably T: With mosquito bites—presumably |
France (Île-de-France region, including Paris) | Encephalitis | [153] | ||
|
Orthobunyavirus
encephalitidis |
California encephalitis virus/ CEV |
ssRNA(−) |
Hs: Equines V: Mosquitoes T: With mosquito bites |
US (California) | Encephalitis | [79,212] | ||
|
Orthobunyavirus
guaroaense |
Guaroa virus/ GROV |
ssRNA(−) |
Hs: Mosquitoes (Anopheles (Kerteszia) neivai) V: Mosquitoes—presumably T: With mosquito bites—presumably |
Brazil, Colombia, Panama, Bolivia | Paresis | [143,169] | ||
|
Orthobunyavirus
ileshaense |
Ilesha virus/ ILEV |
ssRNA(−) |
Hs: – V: Mosquitoes (Anopheles gambiae) T: With mosquito bites |
Cameroon, Central African Republic, Nigeria, Senegal, Uganda; Madagascar (virus isolation from infected persons); Ghana and Niger (antibody from infected persons) | Meningoencephalitis | [144,172] | ||
|
Orthobunyavirus
jamestownense |
Jamestown Canyon virus/ JCV |
ssRNA(−) |
Hs: White-tailed deer (Odocoileus virginianus), moose (Alces alces), elk (Cervus elaphus), bison (Bison bison) V: Mosquitoes (Culiseta inornata, Aedes spp., Anopheles spp.) T: With mosquito bites |
US (Minnesota, Wisconsin); Canada (British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, Quebec, New Brunswick, Nova Scotia) | Encephalitis, meningoencephalitis, meningitis | [79,185,186,213,214] | ||
| Inkoo virus/ INKV |
ssRNA(−) |
Hs: Wild birds V: Mosquitoes (Aedes spp.) T: With mosquito bites |
Finland, Sweden, Norway, Russia | Asthenoneurologic disturbances, microfocal neurologic symptoms, encephalitis | [52,79,156,157,158,159] | |||
|
Orthobunyavirus
kernense |
Main Drain virus/ MDV |
ssRNA(−) |
Hs: Horses, wild birds, black-tailed jackrabbit (Lepus californicus) V: Mosquitoes (Culicidae)—occasional vector; biting midges (Ceratopogonidae, Culicoides variipennis) T: With mosquito or midge bites |
US (California) | Unspecified CNS disease | [66,143] | ||
|
Orthobunyavirus
keystoneense |
Keystone virus/ KEYV |
ssRNA(−) |
Hs: Squirrels, raccoons, whitetail deer (Odocoileus virginianus) V: Mosquitoes (Aedes spp.) T: With mosquito bites |
US (Florida, coastal regions of the Chesapeake Bay) | Encephalitis, meningitis | [191,215] | ||
|
Orthobunyavirus
khatangaense |
Snowshoe hare virus/ SSHV |
ssRNA(−) |
Hs: Hares, squirrels V: Mosquitoes (Aedes spp.) T: With mosquito bites |
US, Canada | Meningoencephalitis, encephalitis, meningitis | [79,216,217,218,219] | ||
| Khatanga virus; Chatanga virus/ KHATV |
ssRNA(−) |
Hs: Wild sylvatic animals; domestic animals—presumably V: Mosquitoes (Aedes spp., Culiseta spp., Culex spp., Anopheles spp.) T: With mosquito bites |
Russia (European part, western, middle and northeastern Siberia) | Encephalitis | [79,154,155] | |||
|
Orthobunyavirus
lacrosseense |
La Crosse virus/ LACV |
ssRNA(−) |
Hs: Chipmunks, squirrels V: Mosquitoes (Aedes spp.) T: With mosquito bites |
US (Ohio, Wisconsin, Minnesota, Indiana, Illinois, Iowa, North Carolina, Tennessee, West Virginia, Georgia, Virginia, Kentucky, Rhode Island) | Encephalitis | [79,134,139,140] | ||
| Orthobunyavirus oropoucheense | Oropouche virus/ OROV |
ssRNA(−) |
Hs: Pale-throated sloths, non-human primates V: Mosquitoes (Culex spp., Aedes spp.); biting midges (Culicoides) T: With mosquito bites |
Brazil, Panama, Peru, Trinidad and Tobago | Meningitis | [167,168,171] | ||
| Orthobunyavirus shuniense | Shuni virus/ SHUV |
ssRNA(−) |
Hs: Horses, domestic cattle V: Mosquitoes (Culex theileri); Cullicoides midges T: With mosquito and midge bites |
South Africa (Gauteng province), Israel, Nigeria | Encephalitis, meningitis | [66,171] | ||
|
Orthobunyavirus
tahynaense |
Ťahyňa virus/ TAHV |
ssRNA(−) |
Hs: Small wild mammals V: Mosquitoes (Culex spp., Aedes spp.) T: With mosquito bites |
Central Europe; China (Xinjiang, Qinghai, Inner Mongolia) | Meningitis, meningoencephalitis, encephalomyelitis, encephalitis | [79,160,161,162,163,164,165,166] | ||
|
Orthobunyavirus
tensawense |
Tensaw virus/ TENV |
ssRNA(−) |
Hs: Sylvatic rodents, foxes, raccoons, dogs, cows V: Mosquitoes (Aedes vexans, Anopheles crucians, Coquillettidia perturbans, Culex salinarius, Uranotaenia sapphirina) T: With mosquito bites—presumably; Congenital infection. |
US (Alabama, Florida) | Rabies-like symptoms, encephalitis, micro-/macrocephaly |
[143,220] | ||
| Orthobunyavirus umbreense | Umbre virus/ UMBV |
ssRNA(−) |
Hs: Not identified V: Mosquitoes (Culex spp.) T: With mosquito bites—presumably |
India, Australia (Queensland—Umbre-related viruses); Malaysia (Umbre-related domestic avian pathogenic virus); France—presumably | Lethal encephalitis | [174] | ||
|
Orthobunyavirus
wyeomyiae |
Tucunduba virus/ TUCV |
ssRNA(−) |
Hs: – V: Mosquitoes (Culex spp., Wyeomia spp., Sabethes spp., Psorophora spp., Limatus spp., Trichoprosopon spp.) T: With mosquito bites |
Brazil | Meningoencephalitis | [170] | ||
| Ntwetwe virus 1 | Ntwetwe virus 1/ NTWV 1 |
ssRNA(−) |
Hs: – V: Mosquitoes (Anopheles spp.) T: – |
Uganda | Fatal encephalopathy, encephalitis | [143,173] | ||
| Phenuiviridae | Phlebovirus |
Phlebovirus
riftense |
Rift Valley Fever virus/ RVFV |
ssRNA(+/−) |
Hs: Wild and domestic animals V: Mosquitoes (Culex spp.) T: With mosquito bites; Direct contact with contaminated biological fluids. |
Kenya, Tanzania, South Africa, Sudan, Egypt, Madagascar, Somalia, Mauritania, Botswana, Namibia | Meningoencephalitis, encephalitis | [139,175] |
|
Phlebovirus
toscanaense |
Toscana virus/ TOSV |
ssRNA(+/−) |
Hs: – V: Sandflies (Phlebotomus perniciosus, Phlebotomus perfiliewi) T: With sandfly bites |
Italy, Spain, Slovenia, Turkey, Portugal, Greece, Cyprus, Southern France, the Balkans, the Black Sea coast, Iraq, Iran, Pakistan, Afghanistan, India | Meningitis, meningoencephalitis | [176,177,178] | ||
| Rhabdoviridae | Vesiculovirus |
Vesiculovirus
chandipura |
Chandipura virus/ CHPV |
ssRNA(−) |
Hs: Pigs, buffalo, cattle V: Mosquitoes (Phlebotomus spp.) T: With mosquito bites |
India, Bhutan, Nepal, Sri Lanka, Nigeria, Senegal | Encephalitis | [179] |
| Sedoreoviridae | Orbivirus | Orungo virus | Orungo virus/ ORUV |
dsRNA |
Hs: – V: Mosquito (Aedes spp., Culex spp., Anopheles spp.) T: With mosquito bites |
Regions of sub-Saharan Africa | Encephalitis | [88] |
| Seadornavirus | Banna virus | Banna virus/ BAV |
dsRNA |
Hs: Domestic pigs, cattle V: Mosquitoes (Culex tritaeniorhynchus, Culex pipiens pallens, Culex annulus, Culex pseudovishnui, Culex modestus, Anopheles sinensis, Aedes vagus, Aedes albopictus, Aedes vexans, Aedes dorsalis); Midges (Culicoides sp.) T: With mosquito bites |
Indonesia, China, Vietnam | Encephalitis | [180,221,222] | |
| Togaviridae | Alphavirus |
Chikungunya
virus |
Chikungunya virus/ CHIKV |
ssRNA(+) |
V: Mosquitoes (Aedes spp.) T: With mosquito bites |
Africa, Southeastern Asia, Europe (imported infection), North America | Myelitis, encephalitis | [129,139,223] |
|
Eastern equine
encephalitis virus |
Eastern equine encephalitis virus North American/ EEEV-NA |
ssRNA(+) |
Hs: Birds, mammals V: Mosquitoes (Aedes spp., Culex spp., Anopheles spp.) T: With mosquito bites |
North America (Massachusetts, Michigan, Florida, Georgia, North Carolina), the Caribbean region | Encephalitis | [224,225,226] | ||
| Madariaga virus | Madariaga virus; Eastern equine encephalitis virus South American/ MADV; EEEV-SA |
ssRNA(+) |
Hs: Birds, mammals V: Mosquitoes (Aedes spp., Culex spp., Anopheles spp.) T: With mosquito bites |
South America (Panama, Venezuela), Haiti | Encephalitis, encephalomyelitis | [181,182,183,184] | ||
| Mayaro virus | Mayaro virus/ MAYV |
ssRNA(+) |
Hs: Non-human primates, migratory birds V: Mosquitoes (Haemagogus spp.—particularly Haemagogus janthinomys); Culex spp., Mansonia spp., Aedes spp., Psorophora spp., Sabethes spp. T: With mosquito bites |
Europe (Germany, France, Netherlands, Switzerland—imported infection); United states (isolated in non-human primates, migratory birds); Mexico, Trinidad and Tobago, Brazil, Surinam, French Guiana, Venezuela, Haiti, Bolivia, Peru, Ecuador, Colombia (isolated from mosquitoes) | Encephalopathy | [129,227,228] | ||
| Middelburg virus | Middelburg virus/ MIDV |
ssRNA(+) |
Hs: Equines, mice, sheep V: Mosquitoes (Aedes spp.) T: With mosquito bites |
South Africa, Zimbabwe | Meningo-encephalitis | [187,188] | ||
| Ross River virus | Ross River virus/ RRV |
ssRNA(+) |
Hs: Mammals, birds V: Mosquitoes (Culex spp.) T: With mosquito bites |
Australia, Papua New Guinea | Meningitis (rare cases); encephalitis (rare cases) |
[189,190] | ||
| Sindbis virus | Sindbis virus/ SINV |
ssRNA(+) |
Hs: Wild birds (Corvus corone sardonius—hooded crow); rodents; domestic animals V: Mosquitoes (Culex spp., Anopheles spp., Coquillettidia spp., Aedes spp., Ocheleratus spp.); Gamasidae ticks (Ornithonyssus bacoti), Ixodidae ticks (Hyalomma marginatum) T: With arthropod-vector bites |
Africa (endemic regions—Egypt, South Africa, Uganda, Central African Republic, Sudan, Nigeria, and Zimbabwe), Europe (Germany, Sweden, Finland, Italy, Slovakia), Russia, the Middle East, the Philippines, Turkey, Azerbaijan, Israel, India, China, Malaysia, Australia (north regions), New Zealand | Meningitis—presumably | [66,79,192,229,230] | ||
| Tonate virus | Tonate virus; Venezuelan equine encephalitis virus IIIB/ TONV; VEEV-IIIB |
ssRNA(+) |
Hs: Wild birds (Psarocolius decumanus—crested oropendola) V: Mosquitoes (Culex portesi) T: With mosquito bites |
North America, South America (Surinam, French Guiana), Central America | Encephalitis | [192,193] | ||
|
Venezuelan equine
encephalitis virus |
Venezuelan equine encephalitis virus/ VEEV |
ssRNA(+) |
Hs: Wild rodents (cotton mouse—Peromyscus gossypinus; hispid cotton rat—Sigmodon hispidus; spiny rats—Proechimys spp.; Oryzomys spp., Zigodontomys spp., Heteromys spp.), equines, canids, pigs, wild birds, bats V: Mosquitoes (Culex spp., Mansonia spp., Anopheles spp., Aedes spp., Psorophora spp., Sabethes spp., Haemagogus spp., Deinocerites spp.); Ochlerotatus taeniorhynchus T: With mosquito bites |
Costa Rica, Venezuela, Colombia, Belize, Peru, Ecuador, British Guyana, Guatemala, Argentina, Panama, Trinidad, Honduras, El Salvador, Nicaragua, Mexico; United States (Texas, Florida) | Encephalitis, meningitis | [15,52,66,192,231,232,233] | ||
|
Western equine
encephalitis virus |
Western equine encephalitis virus/ WEEV |
ssRNA(+) |
Hs: Wild birds (passerine); wild rodents, horses V: Mosquitoes (Culex tarsalis; Aedes spp.); Ochlerotatus melanimon (California), Aedes dorsalis (Utah, New Mexico), Aedes campestris (New Mexico) T: With mosquito bites |
Brazil, Colombia, United States | Encephalitis, meningitis, encephalomyelitis |
[15,129,233,234] | ||
Taxonomic and trivial names are given according to the reports of the International Committee on Taxonomy of Viruses (ICTV) https://ictv.global/msl and https://ictv.global/vmr (versions from 2022/2023); 1 Commonly accepted alternative names not given in the reports of the International Committee on Taxonomy of Viruses (ICTV) (see above).
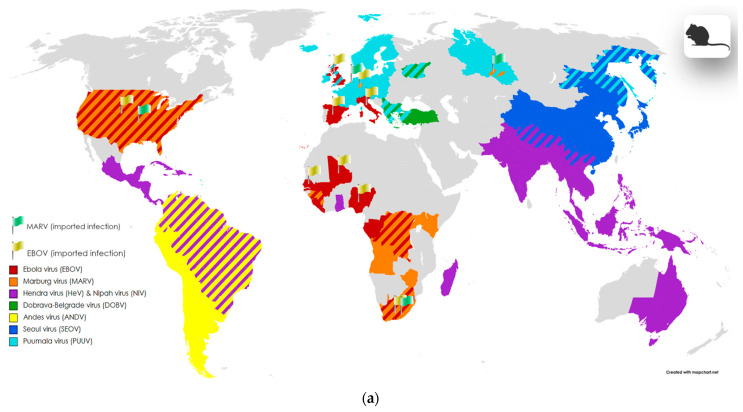
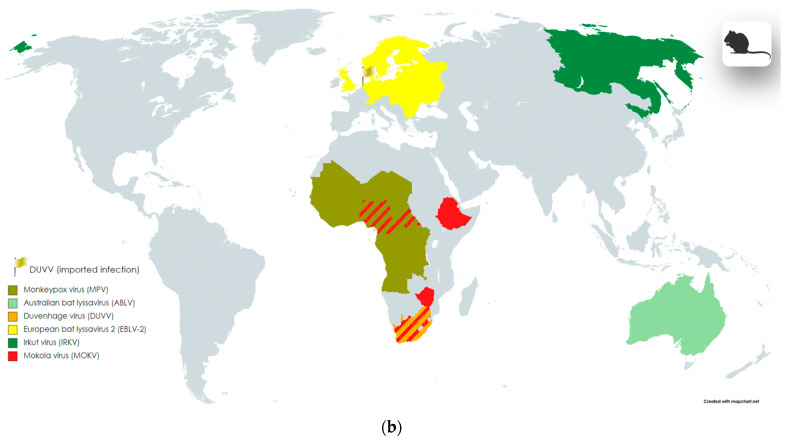
3. Zoonotic Viral Neuropathogens
There are an estimated 2.5 billion cases and 2.7 million deaths associated with zoonotic infections worldwide each year [235]. By some estimates, more than 60% of currently known pathogens affecting humans, and 75% of emerging diseases, are zoonotic [236,237,238]. Of the just over 500 known zoonotic viruses transmitted directly or indirectly, 120 have been identified as capable of causing human disease [236]. It is believed that 10,000 of the 40,000 viruses carried by mammals have zoonotic potential and may pose a threat as causes of epidemics [239].
Among all agents that cause zoonotic diseases, viruses are the most common [133], accounting for more than 65% of pathogens discovered since 1980 [240]. Most of these viruses are RNA-containing, which explains their high variability/lability, and as a result, their ability to exist in a wide range of hosts (unlike DNA viruses, which have greater genetic stability, limiting their range to a range of closely related animal hosts) [133,237]. The most effective carriers of viruses with zoonotic potential among vertebrates are bats and rodents. For example, rodents are reservoirs of about 80 zoonotic viruses [239].
Often, zoonotic viruses are low-pathogenic for their natural hosts (amplification or reservoir hosts), but when the virus enters a new and often “dead-end” host organism, they can manifest themselves as highly virulent agents [241]. It is assumed that, in some cases, the severity and lethality of the pathological process when affected by zoonotic viruses is primarily associated with the immune response of the new host [241].
Arenaviridae. Among the pathogens of this family, viruses of the Mammarenavirus genus are dangerous to humans. Representatives of the genus that are pathogenic for humans, with serious manifestations of infection (though asymptomatic cases have also been noted), most often cause hemorrhagic fever, including in immunocompetent individuals [239,242,243,244]. For example, endemic to regions of West Africa, Mammarenavirus lassaense (Lassa virus, LASV) causes Lassa fever, with a fatality rate that can reach about 69%, and is estimated to infect about 300,000 people annually [242,244].
Mammarenaviruses are divided into Old and New World viruses (the same division is used for Hantaviruses), based on their genetic relationship, geographic distribution, and epidemiological characteristics [243]. The spread of mammarenaviruses is closely related to their reservoir hosts, the vast majority of which belong to the order of rodents, including synanthropic and ubiquitous ones, such as house mice (Mus musculus) [245]. Among other mammals that are reservoirs of these mammarenaviruses, hedgehogs, jerboas, and some arthropods are also noted [246].
The main routes of transmission of viruses from a chronic animal carrier to a dead-end host, a human, are contact with fomites of infected animals and biological fluids, including through airborne droplets; when eating meat; or through trauma—as a result of bites or other damage to the skin [239].
Among the mammarenaviruses that can cause CNS pathologies in humans is Lymphocytic choriomeningitis virus (LCMV) (Table 3). LCMV is a relatively rare but clinically important pathogen (less than 0.5% of viral meningitis cases) [244,247]. The clinical spectrum of acquired LCMV infection is quite wide, from asymptomatic manifestations to those requiring serious medical intervention. In a third of patients, the disease is asymptomatic, but this does not apply to people with compromised immunity nor to cases of perinatal infection [49]. Severe manifestations of congenital infection in humans are meningitis, encephalitis, hydrocephalus, transverse myelitis, cerebellar hypoplasia, focal brain destruction, gyral dysplasia, and fetal death [49]. LCMV is the only known endemic mammarenavirus in Europe [246]. Just like other members of the genus, LCMV circulates within the rodent population, including Mus musculus, where the transmission of the virus from one generation to another occurs, including transplacentally; about 9% of the mouse population are chronic carriers of the virus [49,244,247]. Passive carriage by rodent reservoirs is possible since the virus is not cytolytic [49,247]. A subsequent release of the virus into the environment from a colonized reservoir organism is observed throughout the life of rodents, and does not depend on seasonal factors [49,247]. However, the risk of infection with lymphocytic choriomeningitis virus through contact with animals increases during periods of reproduction and an increase in the number of rodents. The transmission of the virus is possible in several ways: postnatally, through the transplantation of donor organs; upon contact with maternal secretions or blood during maternal viremia (rare cases); and perinatally, i.e., transplacentally [49,244,247].
Filoviridae. Ebola virus (EBOV) (Table 3, Figure 3a) is the causative agent of a severe form of viral hemorrhagic fever in humans. Outbreaks associated with the Ebola virus pose a serious threat to public health due to high case fatality rates of approximately 50% (previously, this ranged from 25 to 90%) [240,248]. The Ebola virus is endemic on the African continent, but there is a risk of possible spread to other territories. EBOV is an initially zoonotic infection that emerged sporadically in the human population and subsequently became transmitted from person to person [248]. The initial reservoirs of the virus are bats and non-human primates [248].
Figure 3.
Geographic distribution of zoonotic (vertebrate) infections, including areas of endemic and imported cases involving nervous system symptoms. The division into blocks (a,b) was implemented to enhance the visualization of data on the maps; information about the taxonomic groups located on each block is provided in the legend within the pictures, as well as in the main text alongside the first mention of the corresponding virus; imported cases are marked with flags. Maps were created with the Map Chart online map-making tool (https://www.mapchart.net/index.html, accessed on 7 May 2024); graphic objects were created with the BioRender online science illustration making tool (https://www.biorender.com/, accessed on 7 May 2024). The images may contain slight inaccuracies in depicting the boundaries of virus distribution areas due to the limitation of the map scale and the choice of scientific sources utilized to create these illustrations.
Marburg virus (MARV) (Table 3, Figure 3a), belonging to the same genus and family as the Ebola virus, is also common among bats and some primates [249]. The clinical manifestations of infection caused by the Marburg virus are similar to those of the Ebola virus: in addition to the symptoms of neuroinfections, hemorrhagic fever, liver failure, and the infection of the spleen and kidney tissues are observed. MARV has been the cause of several outbreaks since its simultaneous discovery and description in 1967 in Marburg, Frankfurt, and Belgrade. However, most MARV outbreaks have occurred in Africa [250].
Hantaviridae. Members of the family contain segmented negative-sense RNA genomes packaged in enveloped virions [251]. Hantavirus infections are natural focal zoonoses, predominantly associated with rodents [252,253]. Old World hantaviruses cause hemorrhagic fever with renal syndrome (HFRS) and are more common in Asia and Europe, while New World hantaviruses are found in the Americas and cause HPS (hemorrhagic pulmonary syndrome). HFRS, caused by Hantaan virus, Dobrava (DOBV) (Table 3, Figure 3a), Saaremaa virus, Seoul virus (SEOV) (Table 3, Figure 3a), and Puumala virus (PUUV) (Table 3, Figure 3a), may have a mortality rate of up to 15%, while HPS, caused by Sin Nombre virus (SNV) and Andes virus (ANDV) (Table 3, Figure 3a), has a mortality rate of up to 40% [254]. In Russia, hantaviruses are among the most common zoonoses [252,253]. Rodents serve as the natural reservoir for almost all known hantaviruses. In Eurasia, transmission is mainly associated with mice, rats, and voles [253]. Like the lymphocytic choriomeningitis virus, the prevalence of hantaviruses is ubiquitous and is associated with the habitats of certain groups of rodents (reservoirs), but some of the representatives of the genus Orthohantaviruses have an endemic distribution pattern [252,255]. Lesions associated with the nervous system, such as meningitis and encephalitis caused by hantavirus infection, are recorded much less frequently than other manifestations of the disease. However, there are data on cases of severe neurological manifestations associated with hantaviruses [256,257,258,259,260,261,262]. For example, in the work of Talamonti et al., a case of encephalitis due to hantavirus pulmonary syndrome caused by Andes virus infections is reported.
Paramyxoviridae. This family also includes regionally endemic chiropteran-associated viruses. Henipaviruses, which include Hendra (HeV) (Table 3, Figure 3a) and Nipah (NiV) (Table 3, Figure 3a) viruses, are relatively new paramyxoviruses of zoonotic origin that infect humans. HeV and NiV may be transmitted through bats, domestic pigs, horses, and from person to person [240,263]. Diseases associated with HeV and NiV viruses can affect a wide range of wild and domestic animals, as well as humans, in which these viruses exhibit a high level of pathogenicity, mainly causing pulmonary or encephalitic disease with an observed mortality of up to 60% and 90% for HeV and NiV, respectively [264]. In humans, the virus is transmitted through airborne droplets or direct contact with an infected person, infectious body fluids, or other secretions. Cases of infection have also been described after drinking date palm sap, because palm trees are a source of food for fruit mice of the family Pteropodidae, which are the natural hosts of the virus. The main areas of spread of the virus are India and Bangladesh. The consequences of viral infection include meningoencephalitis, the inflammation of the walls of blood vessels (systemic vasculitis), and severe respiratory failure [263].
Poxviridae. Monkeypox virus (MPV) (Table 3, Figure 3b) has relatively few reported cases associated with nervous system complications of infection. Monkeypox is thought to rarely cause encephalitis, but Billioux et al. reported several cases of encephalitis in patients of different ages during outbreaks in Africa [265]. Reported clinical manifestations of infection during these outbreaks included encephalitis, ADEM, encephalomyelitis, and demyelinating encephalitis.
Rhabdoviridae. Bats (order Chiroptera) are the primary reservoir hosts for most lyssaviruses, while predators (order Carnivora) maintain rabies virus circulation; evolutionary analysis suggests that all lyssaviruses likely originated from bats [249,266]. Many viruses assigned to the genus are ubiquitous, but for some representatives of the genus, there is limited distribution and different areas of circulation [249,266]. Healthy bat populations may serve as reservoirs for the virus: for example, the prevalence of rabies virus (RABV) in large bat colonies is typically less than 1%, but 70% of bats can produce antiviral antibodies, suggesting that bats may be exposed frequently to allow them to produce immunity in the absence of infection [249].
The well-known neurotropic pathogen rabies virus (RABV) (Table 3) causes the majority of cases of rabies in humans worldwide and can be divided into two lineages: one transmitted primarily by carnivores with a worldwide distribution, and the other transmitted by bats and present only in America [133,249]. The disease caused by this pathogen is endemic in more than 150 countries and causes 40,000–70,000 deaths annually, most of which occur in Asia, Africa, and South America [240]. Human infection most often occurs through bites from sick dogs. Unfortunately, rabies is a disease with a high risk of death when severe clinical signs appear [263]. Cases of virus transmission during organ transplantation and perinatal transmission are also mentioned in the literature [263]. Duvenhage virus (DUVV), Irkut virus (IRKV), Australian bat lyssavirus (ABLV), European bat lyssavirus 2 (EBLV-2), and Mokola virus (MOKV) also cause fatal diseases in humans, including those with central nervous system damage, including encephalitis and meningoencephalitis [267,268,269,270,271]. European bat lyssavirus 2 (EBLV-2) (Table 3, Figure 3b) was discovered in bats in Europe; Irkut virus (IRKV) (Table 3, Figure 3b)—in Eurasia; Duvenhage virus (DUVV) (Table 3, Figure 3b)—in Africa; Australian bat lyssavirus (ABLV) (Table 3, Figure 3b)—in Australia [249]; and Mokola virus (MOKV) (Table 3, Figure 3b) is associated with shrews, rodents, and cats in Africa [267]. Unlike RABV, cases of infection with the viruses listed above are much less common; this is due to the predominance of competent viral hosts in certain endemic areas and, accordingly, the limitation of their spread.
Table 3.
List of zoonotic viral pathogens causing neuroinflammation.
| Family | Genus | Species | Common Names or Subspecies/ Acronym(s) |
Genome | Host-Vector, Transmission |
Geographic Distribution |
NS Pathology | Reference |
|---|---|---|---|---|---|---|---|---|
| Arenaviridae | Mammarenavirus |
Mammarenavirus
choriomeningitidis |
Lymphocytic choriomeningitis virus/ LCMV |
ssRNA(+/−) |
Hv: Predominantly wild and domestic rodents T: With bites; Contact with fomites/blood/nesting materials. |
Worldwide (where rodents are present) | Meningitis, encephalitis, encephalomyelitis, meningoencephalitis, transverse myelitis | [46,49,62,81,247,272,273,274] |
| Filoviridae | Orthoebolavirus |
Orthoebolavirus
zairense |
Ebola virus/ EBOV |
ssRNA(−) |
Hv: Non-human primates; bats; flying foxes; infected human hosts T: With bites; Contact with infectious body fluids of a patient (high risk group—medical workers); Contact with fomites/blood/nesting materials of infected animal hosts. |
Imported infection: Mali, Nigeria, Senegal, Italy, Spain, UK, US, Russia (laboratory infection) Democratic Republic of Congo, Republic of the Congo, Gabon, Liberia, Sierra Leone, Guinea, South Africa |
Meningitis, encephalitis, meningoencephalitis, neurocomplication after system infection | [248,274,275,276] |
| Orthomarburgvirus |
Orthomarburgvirus
marburgense |
Marburg virus/ MARV |
ssRNA(−) |
Hv: Egyptian fruit bat (Rousettus aegyptiacus), Sundevall’s leaf-nosed bat (Hipposideros caffer); non-human primates T: With bites; Contact with infected patients; Contact with fomites/blood/nesting materials of infected animal hosts. |
Imported infection: Germany (Marburg, Frankfurt), Serbia (Belgrade), Russia (Koltsovo), Netherlands (Leiden), US, South Africa Angola, Democratic Republic of Congo, Kenya, Uganda, Zimbabwe, Guinea |
Encephalitis | [112,250,277] | |
| Hantaviridae | Orthohantavirus |
Orthohantavirus
andesense |
Andes virus/ ANDV |
ssRNA(−) |
Hv: Wild and domestic rodents (long-tailed pygmy rice rat (Oligoryzomys longicaudatus)—most common host) T: With bites; Person-to-person transmission between humans (including breastfeeding, household contacts, nosocomial transmission); Contact with fomites/blood/nesting materials of infected animal hosts. |
Highly endemic region: Regions of South America (Argentina, Bolivia, Chile, Uruguay) | Encephalitis | [257,278,279,280] |
|
Orthohantavirus
dobravaense |
Dobrava-Belgrade virus/ DOBV |
ssRNA(−) |
Hv: Rodents (yellow-necked mouse—Apodemus flavicollis; striped field mouse—Apodemus agrarius; Caucasian wood mouse—Apodemus ponticus; Small forest mouse—Apodemus uralensis) T: With bites and scratches; Inhalation of aerosolized droplets; Contact with fomites/blood/nesting materials of infected animal host; Contaminated food. |
Russia (Central Russia, Western Siberia), Europe, Turkey Highly endemic region: Balkans |
Encephalitis | [79,258,281,282] | ||
|
Orthohantavirus
puumalaense |
Puumala virus/ PUUV |
ssRNA(−) |
Hv: Rodents (bank vole—Clethrionomys glareolus) T: With bites and scratches; Inhalation of aerosolized droplets; Contact with fomites/blood/nesting materials of infected animal host; Contaminated food. |
Russia (Central Russia, Western Siberia, Far East), Balkans, Europe (Northern, Western, Central regions) | Encephalitis, encephalomyelitis | [79,259,260,282,283] | ||
|
Orthohantavirus
seoulense |
Seoul virus/ SEOV |
ssRNA(−) |
Hv: Rodents (Norwegian brown rat—Rattus norvegicus; black rat—Rattus rattus) T: With bites and scratches; Inhalation of aerosolized droplets; Contact with fomites/blood/nesting materials of infected animal hosts; Contaminated food. |
Far East of Russia, China, Japan, North and South Korea | Encephalitis | [79,262,282] | ||
| Paramyxoviridae | Henipavirus |
Henipavirus
hendraense |
Hendra virus/ HeV |
ssRNA(−) |
Hv: Infected domestic animals (horses, pigs, dogs, cats); flying fox (fruit bats) (family Pteropidinae—Pteropus alecto, Pteropus poliocephalus, Pteropus scapulatus, Pteropus conspicillatus), etc. T: With bites and scratches; Contact with fomites/blood/nesting materials of infected animal hosts; Food-borne way (with horsemeat, pork, date palm sap or wine, fruits); Human-to-human. |
Southeast Asia (including Singapore, Cambodia, Indonesia, Thailand, Malaysia, Philippines, Bangladesh), Eastern Australia, Ghana, Madagascar, Papua New Guinea, China, India, Latin America | Meningitis, encephalitis | [139,249,284,285,286,287,288] |
|
Henipavirus
nipahense |
Nipah virus/ NiV |
ssRNA(−) |
Hv: Infected domestic animals (horses, pigs, dogs, cats); flying fox (fruit bats) (Pteropus giganteus, Pteropus hypomelanus, Pteropus lylei); flying dog (Cynopterus brachyotis); cave nectar bat (Eonycteris spelaea); microbats (Scotophilus kuhlii, Myotis), etc. T: With bites and scratches; Contact with fomites/blood/nesting materials of infected animal hosts; Food-borne way (with horsemeat, pork, date palm sap, fruits); Human-to-human transmission. |
Southeast Asia (including Singapore, Cambodia, Indonesia, Thailand, Malaysia, Philippines, Bangladesh), Eastern Australia, Ghana, Madagascar, Papua New Guinea, China, India, Latin America | Acute encephalitis | [112,249,284,285,286,288,289,290] | ||
| Poxviridae | Orthopoxvirus | Monkeypox virus | Monkeypox virus/ MPV |
dsDNA |
Hv: Non-human primates (mangabey monkeys), Gambian pouched rats, squirrels, prairie dogs T: With bites and scratches; Contact with fomites/blood of infected animal-host; Human-to-human transmission. |
Highly endemic region: Tropical rainforest areas of Central and Western Africa Outbreaks (imported infection): 50 countries (worldwide) |
Encephalitis, ADEM, encephalomyelitis, demyelinating encephalomyelitis | [139,263,265,291,292,293] |
| Rhabdoviridae | Lyssavirus |
Lyssavirus
australis |
Australian bat lyssavirus/ ABLV |
ssRNA(−) |
Hv: Pteropod and insectivorous bat species (black flying fox—Pteropus Alecto; yellow-bellied sheath-tailed bat—Saccolaimus flaviventris) T: With bites and scratches; Contact with fomites (especially saliva)/blood of infected animal hosts. |
Australia (New South Wales, the Northern Territory, Queensland, South Australia, Victoria, Western Australia) | Encephalitic rabies | [266,294,295] |
|
Lyssavirus
duvenhage |
Duvenhage virus/ DUVV |
ssRNA(−) |
Hv: Bats—presumably T: With bites and scratches; Contact with fomites (especially saliva)/blood of infected animal hosts. |
South Africa; Europe (one case of imported infection—Netherlands) | Encephalitic rabies | [266,267,268] | ||
| Lyssavirus helsinki | European bat lyssavirus 2/ EBLV-2 |
ssRNA(−) |
Hv: Insectivorous microbats—Daubenton’s bat (Myotis daubentonii), pond bat (Myotis dasycneme) T: With bites and scratches; Contact with fomites (especially saliva)/blood of infected animal hosts. |
Northeastern Europe, Mediterranean region, Netherlands, Switzerland, United Kingdom, Germany | Rabies-like encephalitis | [266,271,294,296] | ||
| Lyssavirus irkut | Irkut virus/ IRKV |
ssRNA(−) |
Hv: Insectivorous microbats—greater tube-nosed bat (Murina leucogaster); domestic dog T: With bites and scratches; Contact with fomites (especially saliva)/blood of infected animal hosts. |
Russia (Irkutsk region, Far East (Primorsky Krai region, Amur region)); China (Jilin province) |
Encephalitic rabies | [294,297,298] | ||
| Lyssavirus mokola | Mokola virus/ MOKV |
ssRNA(−) |
Hv: Domestic cats, dogs T: With bites and scratches; Contact with fomites (especially saliva)/blood of infected animal hosts. |
Africa (Nigeria, Cameroon, Central African Republic, Ethiopia, Zimbabwe, South Africa) | Encephalitic rabies (human cases very rare) |
[249,294,299] | ||
| Lyssavirus rabies | Rabies virus/ RABV |
ssRNA(−) |
Hv: Vampire bat (Desmodus rotundus), big brown bat (Eptesicus fuscus), Mexican/Brazilian free-tail bat (Tadarida brasiliensis), silver-haired bat (Lasionycteris noctivagens), tri-colored bat (Perimyotis subflavus), carnivores (including domestic synanthrope species) T: With bites and scratches; Contact with fomites (especially saliva)/blood of infected animal hosts. |
Worldwide | Meningoencephalitis, encephalitic rabies |
[46,247,266,300,301,302,303] |
Taxonomic and trivial names are given according to the reports of the International Committee on Taxonomy of Viruses (ICTV) https://ictv.global/msl and https://ictv.global/vmr (versions from 2022/2023); ADEM—Acute disseminated encephalomyelitis.
4. Widespread Viral Neuropathogens
In this section, we included ubiquitous viral pathogens that cause infections primarily not related to the nervous system (with the exception of polio enteroviruses and non-polio enteroviruses). A distinctive feature of these viruses, when compared with previously described pathogens, is their direct route of transmission from person to person, which usually does not include intermediate hosts.
Adenoviridae. Representatives of the family that cause various human diseases belong to the genus Mastadenovirus (Table 4) [304]. Mastadenoviruses are widespread and are detected in patients throughout the year, but the peak of incidence occurs in the winter–spring period [304,305,306]. All groups of the population are susceptible to infection, regardless of gender and age, but among immunocompetent individuals, young children are at greatest risk of infection and the development of severe complications [306,307,308].
The transmission of the virus occurs through contact with an infected person or through the inhalation of an aerosol containing the virus; by the fecal–oral route; or during the reactivation of a latent virus, which can persist in lymphoid and other tissues [304,306]. A rapid spread of the virus occurs in isolated populations through the close contact of virus carriers (including asymptomatic) and susceptible individuals in public places such as schools and health care facilities (nosocomial infection) [305,306].
About 100 variants of adenoviruses are known, with different tropism for tissues and circulating in different regions [304,309]. Adenoviruses typically cause mild infections of the upper or lower respiratory tract, gastrointestinal tract, or conjunctiva [305], but the most severe manifestations of infection, for example, pneumonia or meningitis, are observed in persons with immunosuppression, including drug-induced [304,305]. The spectrum of clinical manifestations of atypical severe infection varies and includes encephalitis, acute disseminated encephalomyelitis, cerebellitis, Guillain–Barré syndrome, acute flaccid myelitis, acute flaccid paralysis, and necrotizing encephalopathy, as well as symptomatic manifestations with status epilepticus [304,305,306,309,310,311].
Astroviridae. Astroviruses are widespread among various vertebrates, including humans. Human mamastroviruses (Table 4) are typical causative agents of acute intestinal infections, next in prevalence after rotaviruses and noroviruses (about 10% of cases), in children under 5 years old and immunocompromised patients [312,313,314,315]. However, recent studies have shown that a number of variants of astroviruses pathogenic for humans can also act as etiological agents of encephalitis and acute flaccid paralysis [313,314], including in immunocompetent persons [313]. Koukou et al. report a clinical case of encephalitis caused by the classic human astrovirus Virginia (HAstV) variant in a previously healthy 16-month-old girl. Also, in the work of Naccache et al., a case of fatal encephalitis in a child with X-linked agammaglobulinemia and a weakened immune system was described, caused by a variant of the human astrovirus Virginia, presumably of zoonotic origin [314].
Coronaviridae. Coronaviruses are found in many vertebrates. Coronaviruses pathogenic to humans (Table 4) (including zoonotic MERS and SARS) are endemic throughout the world and are currently classified into two genera, Alphacoronavirus and Betacoronavirus. The recent SARS-CoV-2 pandemic has significantly increased the interest of the medical and scientific community in the study of respiratory viruses and their potential to cause severe complications. Typically, in humans, coronavirus infection causes respiratory diseases: rhinitis, pharyngitis, bronchitis, and pneumonia [310,316]. However, severe manifestations of infection can also include serious complications in the nervous system. Human coronaviruses have been sensu lato recognized as neurotropic agents causing encephalitis, acute disseminated encephalomyelitis, Guillain–Barré syndrome, acute flaccid myelitis, necrotizing encephalopathy, etc. [310,316]. The mechanisms of penetration of coronaviruses and their interaction with nerve cells require further detailed study. However, already now, various studies and reviews speak about the role of these pathogens, in particular, using the example of SARS-CoV-2 [317,318,319,320].
Flaviviridae. The vast majority of Flaviviridae pathogens that cause diseases of the central nervous system are transmitted through the bites of certain insects and ticks; see Section 2 and Section 3. However, among the pathogens of this family that are transmitted from person to person without the mandatory participation of a carrier, one can note hepatitis C virus (HCV). Hepatitis C virus (HCV) (Table 4) is an important etiological agent of chronic hepatitis. Humans are the primary reservoir of the virus. In addition to its direct role in the development of hepatitis, HCV has also been identified as having a role in the development of other severe systemic concomitant diseases, including encephalitis, myelitis, and encephalomyelitis [38,321,322]. The mechanism of occurrence of CNS lesions during chronic HCV infection is not yet completely clear. But, for example, it has been suggested that during chronic infection, an autoimmune pathogenic mechanism occurs against blood vessels or myelin due to chronic viral antigenic stimulation, as has been observed in several patients with chronic HCV [321].
Matonaviridae. The family includes only one genus, Rubivirus, to which Rubella virus (RuV) (Table 4), the causative agent of rubella, also known as “German measles”, belongs [323]. The transmission of the virus occurs through airborne droplets from person to person. Children are mainly susceptible to infection, and most cases are benign or asymptomatic [323,324]; however, this does not apply to congenital rubella, i.e., with maternal infection [324]. In postnatal infection, rubella virus may be the etiological agent of encephalitis in pediatric patients [81].
Orthoherpesviridae. Herpesviruses (HSV) (Table 4) are ubiquitous, occurring in many vertebrates [325]. In humans, herpesviruses are widely associated with diseases of the nervous system, such as aseptic meningitis, encephalitis, and meningoencephalitis [38,62,110,272,326,327]. After the primary infection, the adult host may develop a lifelong latent infection, and severe manifestations of the infection are observed, as a rule, in the fetus (with maternal infection) or in an organism with a weakened immune system [325]. For example, HSV encephalitis caused by HSV-1 occurs more often in immunocompetent adults, while HSV-2 affects immunocompromised individuals [328]. About 30% of cases of herpes encephalitis are associated with a primary infection (usually in children and teenagers), and 70% of cases are associated with the reactivation of the virus [110]. Also, some studies suggest and demonstrate data on the relationship of herpesviruses with the development of neurodegenerative diseases, such as Alzheimer’s disease and multiple sclerosis [110,327].
Orthomyxoviridae. The family includes ubiquitous viruses of various mammals and birds [329]. Well-characterized pathogens, including in humans, are Influenza A (IAV) (Table 4) and Influenza B viruses (IBV) (Table 4). In humans, influenza viruses mainly cause seasonal respiratory diseases, in some cases with serious complications. All groups of the population are susceptible to infection. It is believed that influenza viruses do not directly affect the central nervous system, but are neurotropic (for some variants) [330,331], and adverse pathological reactions are the result of the immune response to infection (secondary inflammation observed in the central nervous system) [38,332]. At the same time, the work of Popescu et al. describes cases of neurological complications in patients with influenza B virus, including myelitis, encephalitis, and Guillain–Barré syndrome [333]. The neuropathophysiology of influenza-associated neurological complications remains poorly understood but is thought to be related to systemic cytokine release and likely host-specific genetic predisposition [332]. Therefore, vigilance against influenza viruses is necessary in the development of neuropathologies, given the high variability and prevalence of these pathogens.
Paramyxoviridae. This family includes several genera of large heterogeneous enveloped RNA viruses that infect a variety of mammals, reptiles, birds, and fish [334]. Measles virus (measles virus) (Table 4) and human parainfluenza viruses (parainfluenza viruses) (Table 4) are causes of aseptic meningitis in extremely rare cases [335]. The mumps virus, before the widespread introduction of vaccines, was the most common cause of viral meningitis. However, whereas the incidence of mumps has gradually declined in developed countries, the virus continues to be a problem in developing regions [335]. Children are most susceptible to the disease [272]. Parainfluenza viruses, as well as the measles and mumps viruses, are transmitted through contact with a sick person through aerogenic means. The incidence of parainfluenza fluctuates throughout the year, with outbreaks recorded in the autumn and spring periods, in all age groups. In essence, the disease is characterized by damage to the upper respiratory tract; however, extrapulmonary manifestations of infection can manifest as meningitis and meningoencephalitis [336,337].
Parvoviridae. Members of the genera Bocaparvovirus (Table 4), Erythroparvovirus (Table 4), and Tetraparvovirus (Table 4) are associated with a wide range of conditions, including neurological complications [338]. Human parvovirus B19 (B19V), a member of the genus Erythroparvovirus, is believed to cause aseptic viral meningitis relatively rarely [335]. In the paper of Vilmane et al., it was suggested that active parvovirus infection is associated with the development of meningitis and meningoencephalitis. It was shown that the genomic sequences of HBoV1–4 and B19V were present in 52.38% and 16.67% of samples from hospitalized patients with meningitis and meningoencephalitis of unknown etiology [339]. Also, the presence of obvious severe neurological symptoms, such as headache, disorientation, and impaired concentration, was more common in patients with confirmed parvovirus infection, which may likely indicate the connection of these viruses with the effect on the nervous system [339].
Picornaviridae (Table 4) is a family of small icosahedral viruses containing positive-sense single-stranded RNA that cause subclinical infections in humans and animals or conditions ranging from mild fever to severe diseases of the heart, liver, and central nervous system [340]. Human-pathogenic members of the family included in this review, as etiological agents of neurological diseases, belong to the genera Enterovirus, Hepatovirus, and Parechovirus.
Representatives of the Enterovirus genus, are a well-studied ubiquitous pathogens, causing acute intestinal infections in children. Enteroviruses are the most common cause of viral meningitis in patients of any age [273]. In temperate regions, outbreaks, including reported cases of aseptic meningitis, tend to peak during the summer and autumn months, whereas in tropical regions, they occur consistently throughout the year [341]. Enteroviruses CV-B5, E-6, and E-30 are common causes of meningitis outbreaks worldwide [342], as is CVA2 [343]. Enteroviruses are the cause of most cases of viral encephalitis, acute flaccid myelitis [310], and acute flaccid paralysis [344], caused by non-polio variants of Enterovirus C—EV68 [310] and A71 [300], as well as CV-A1, CV-A11, CV-A13, CV-A17, CV-A19—A22, and CV-A24 [45]. It is also noted that infection in children of a young age can lead to delayed nervous development with motor, speech, and cognitive function impairment [45].
Representatives of the genera Hepatovirus (hepatitis A virus) and Parechovirus are also associated with the occurrence of viral meningitis [62,247]. Parechoviral meningoencephalitis is a problem among children under 5 years of age [345,346,347], with children under 6 months of age being at highest risk [347].
Pneumoviridae (Table 4). This is a family of RNA-containing pleomorphic (mainly spherical or filamentous) enveloped viruses, including two representatives which are pathogenic for humans, Human respiratory syncytial virus (HRSV) and Human metapneumovirus (HMPV), classified in the genera Orthopneumovirus and Metapneumovirus, respectively [348]. HRSV, like HMPV, causes respiratory diseases in humans; however, in some cases, extrapulmonary complications can manifest as encephalitis, epilepsy, myelitis, and encephalomyelitis [310,349].
Polyomaviruses. Polyomaviruses (Table 4) are a family of small non-enveloped viruses, the genome of which is represented by double-stranded DNA, averaging 5 Mb in size, infecting various mammals and birds [350]. This family includes John Cunningham virus (JCV), of which more than half of the adult population are asymptomatic carriers (i.e., have a latent or persistent infection). During immunosuppression, viral reactivation can lead to the development of progressive multifocal leukoencephalopathy (PML), a disease characterized by multiple foci of demyelination of neurons in the brain. Now an early rare disease, it has become more common with the advent of acquired immunodeficiency syndrome (AIDS) [350], and also in combination with various immunosuppressive treatments [46].
Retroviridae (Table 4). HIV infection leads to neurological complications in half of cases, including encephalitis [46]. In addition to encephalitis, HIV-associated neurocognitive disorder (HAND) is believed to remain a common cause of cognitive impairment, even in individuals treated with combination antiretroviral therapy (CART) [351]. HIV can enter the CNS early in infection, and persistent HIV infection and CNS inflammation are thought to contribute to the development of varying degrees of HAND [351], in approximately 50% of HIV-positive patients [352]. Latent HIV infection may persist in the brain even after systemic control is achieved using CART, thereby complicating and delaying treatment [351]. The pathogenesis of HAND involves either direct effects of the virus or the effects of viral proteins, and also the possible influence of antiretroviral drugs on amyloid metabolism, which in turn leads to changes in brain tissue [353].
Table 4.
List of common viral pathogens that cause neuroinflammation.
| Family | Genus | Species | Common Names or Subspecies/ Acronym(s) |
Genome | Source, Predisposing Conditions, Transmission |
NS Pathology | Reference |
|---|---|---|---|---|---|---|---|
| (Sub)Species Complex/ Acronym(s) | |||||||
| Adenoviridae | Mastadenovirus |
Human
mastadenovirus A |
Human adenovirus 12/ HAdV-12 |
dsDNA |
S: Infected human hosts Pc: Children under 5 y.o.; immunocompromised persons T: Inhalation of aerosolized droplets; Fecal–oral spread; Contact with infected tissue, water, environmental surfaces. |
Meningitis, meningoencephalitis, encephalitis | [354] |
|
Human
mastadenovirus B |
Human adenovirus 3/ HAdV-3 |
dsDNA | [307,354] | ||||
| Human adenovirus 7/ HAdV-7 |
dsDNA | [307,354,355] | |||||
| Human adenovirus 11/ HAdV-11 |
dsDNA | [307,354] | |||||
| Human adenovirus 14/ HAdV-14 |
dsDNA | [307,354] | |||||
| Human adenovirus 16/ HAdV-16 |
dsDNA | [307,354] | |||||
| Human adenovirus 21/ HAdV-21 |
dsDNA | [307,354] | |||||
| Human adenovirus 34/ HAdV-34 |
dsDNA | [307,354] | |||||
| Human adenovirus 35/ HAdV-35 |
dsDNA | [307,354] | |||||
| Human adenovirus 50/ HAdV-50 |
dsDNA | [307,354] | |||||
| Human adenovirus 55/ HAdV-55 |
dsDNA | [354] | |||||
| Human adenovirus 66 1;Human adenovirus B66 1 | dsDNA | [354] | |||||
| Human adenovirus 68 1;Human adenovirus 3–16 1 | dsDNA | [354] | |||||
| Human adenovirus B79 1 | dsDNA | [354] | |||||
|
Human
mastadenovirus C |
Human adenovirus 1/ HAdV-1 |
dsDNA |
S: Infected human hosts Pc: Children under 5 y.o.; immunocompromised persons T: Inhalation of aerosolized droplets; Fecal–oral spread; Contact with infected tissue, water, environmental surfaces. |
Meningitis, meningoencephalitis, encephalitis | [354] | ||
| Human adenovirus 2/ HAdV-2 |
dsDNA | [354,355] | |||||
| Human adenovirus 5/ HAdV-5 |
dsDNA | [354,355] | |||||
| Human adenovirus 6/ HAdV-6 |
dsDNA | [354] | |||||
|
Human
mastadenovirus D |
Human adenovirus 26; Adenovirus serotype 26/ HAdV-26 |
dsDNA |
S: Infected human hosts Pc: Children under 5 y.o.; immunocompromised persons T: Inhalation of aerosolized droplets; Fecal–oral spread; Contact with infected tissue, water, environmental surfaces. |
Meningitis, meningoencephalitis, encephalitis | [354] | ||
| Human adenovirus 32/ HAdV-32 |
dsDNA | [354] | |||||
|
Human
mastadenovirus E |
Human adenovirus 4/ HAdV-4 |
dsDNA | [354] | ||||
|
Human
mastadenovirus F |
Human adenovirus 41/ HAdV-41 |
dsDNA | [308,354] | ||||
| unclassified Human mastadenovirus 1 |
Human adenovirus 76 1 | dsDNA | [354] | ||||
| Human adenovirus 77 1 | dsDNA | [354] | |||||
| Human adenovirus 78 1 | dsDNA | [354] | |||||
| Astroviridae | Mamastrovirus | Human astrovirus 1 | Human astrovirus Virginia| Pudget Sound 1/ HuAstV-PS 1 |
ssRNA(+) |
S: Infected human hosts, HAI; zoonotic infection? Pc: Children under 5 years old (include immunocompetent), hereditary immunodeficiency, leukemia, HSCT, multiorgan dysfunction, immunocompromised patients T: Inhalation of aerosolized droplets; Fecal–oral spread; Contact with infected environmental surfaces. |
Encephalitis | [356] |
| Human astrovirus Virginia| Human-Mink-Ovine-like 1/ HAstV-VA 1|HMO-C-UK1(a) 1 |
ssRNA(+) | Encephalitis, progressive encephalitis, encephalopathy | [314,315,356] | ||||
| Human astrovirus Virginia| Human-Mink-Ovine-like 1/ HAstV-VA 1|HMO-C-PA 1 |
ssRNA(+) | Progressive encephalitis | [356] | ||||
| Human astrovirus Virginia| Human-Mink-Ovine-like 1/ HAstV-VA 1|HMO-C 1 |
ssRNA(+) | Encephalitis | [356] | ||||
| Human astrovirus Melbourne 2 1/ HAstV-MLB2 1; MLB2 1 |
ssRNA(+) | Meningitis, acute meningitis | [356] | ||||
| Mamastrovirus 1 | Mamastrovirus 1/ MAstV1; HAstV 1 |
ssRNA(+) | Encephalitis, encephalopathy | [313] | |||
| Mamastrovirus 4 | Mamastrovirus 4/ MAstV4; HAstV-4 1 |
ssRNA(+) | Meningoencephalitis | [356] | |||
| Coronaviridae | Alphacoronavirus | Human coronavirus 229E | Human coronavirus 229E; Human coronavirus A 1/ HCoV_229E |
ssRNA(+) |
S: Infected human hosts Pc: Children under 5 y.o.; immunocompromised persons T: Inhalation of aerosolized droplets; Fecal–oral spread; Contact with infected tissue, water, environmental surfaces. |
Encephalitis, ADEM | [310,316,335] |
| Human coronavirus NL63 | Human coronavirus NL63; Human coronavirus A 1/ HCoV_NL63 |
ssRNA(+) | [310,335] | ||||
| Betacoronavirus | Betacoronavirus 1 | Human coronavirus OC43; Human coronavirus B 1/ HCoV_OC43 |
ssRNA(+) | [310,316,335] | |||
| Human coronavirus HKU1 | Human coronavirus HKU1; Human coronavirus B 1/ HCoV_HKU1 |
ssRNA(+) | [310,335] | ||||
|
Middle East
respiratory syndrome-related coronavirus |
Middle East respiratory syndrome-related coronavirus/ MERS-CoV |
ssRNA(+) | Encephalitis, ADEM | [310,316,335] | |||
|
Severe acute
respiratory syndrome-related coronavirus |
Severe acute respiratory syndrome coronavirus |
ssRNA(+) | Encephalitis, ADEM | [310,335] | |||
| Severe acute respiratory syndrome coronavirus 2/ SARS-CoV-2 |
ssRNA(+) | Meningitis, encephalitis, ADEM, transverse myelitis, Guillain–Barré syndrome |
[38,139,310,316,335,356] | ||||
| Flaviviridae | Hepacivirus |
Hepacivirus
hominis |
Hepatitis C virus/ HCV |
ssRNA(+) |
S: Infected human hosts Pc/T: Blood-borne transmission by drug-injection equipment, blood transfusion, organ transplantation; Genital contact; Congenital infection. |
Peripheral neuropathy, disseminated encephalomyelitis, transverse myelitis, acute encephalitis | [38,321,322] |
| Matonaviridae | Rubivirus | Rubivirus rubellae | Rubella virus/ RuV |
ssRNA(+) |
S: Infected human hosts Pc/T: Children under 5 y.o.; Immunocompromised persons; Unvaccinated persons; Inhalation of aerosolized droplets; Congenital infection (TORCH). |
Meningitis, acute encephalitis, progressive rubella panencephalitis | [52,81,357] |
| Orthoherpesviridae | Cytomegalovirus |
Cytomegalovirus
humanbeta 5 |
Human betaherpesvirus 5; Human cytomegalovirus/ HuBHV5, HCMV |
dsDNA |
S: Infected human hosts Pc/T: Children under 5 y.o.; Immunocompromised persons; Inhalation of aerosolized droplets; Congenital infection (TORCH). |
Encephalitis, aseptic meningitis, neurodevelopmental deficits | [38,62,272,326,327] |
| Orthoherpesviridae | Lymphocryptovirus |
Lymphocryptovirus
humangamma 4 |
Human gammaherpesvirus 4; Epstein-Barr virus/ HuGHV4, EBV |
dsDNA |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets; Congenital infection. |
Aseptic meningitis, meningitis, encephalitis, myelitis | [38,62,272,326,327] |
| Roseolovirus |
Roseolovirus
humanbeta 6a |
Human betaherpesvirus 6A; Human herpesvirus 6A/ HuBHV6A, HHV6A |
dsDNA |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets; Person-to-person transmission; Congenital infection. |
Aseptic meningitis, encephalitis, multiple sclerosis | [38,62,326,327] | |
|
Roseolovirus
humanbeta 6b |
Human betaherpesvirus 6B; Human herpesvirus 6B/ HuBHV6B, HHV6B |
dsDNA | Aseptic meningitis, encephalitis, multiple sclerosis | [38,62,326,327] | |||
|
Roseolovirus
humanbeta 7 |
Human betaherpesvirus 7; Human herpesvirus 7/ HuBHV7, HHV7 |
dsDNA | Aseptic meningitis, encephalitis, meningoencephalitis, vestibular neuritis | [62,247,327] | |||
| Simplexvirus |
Simplexvirus
humanalpha 1 |
Human alphaherpesvirus 1; Herpes simplex virus type 1/ HuAHV1, HSV1 |
dsDNA |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets; Person-to-person transmission; Congenital infection (TORCH). |
Meningitis, meningoencephalitis, encephalitis, myelitis, Guillain–Barré syndrome | [38,110,327] | |
|
Simplexvirus
humanalpha 2 |
Human alphaherpesvirus 2; Herpes simplex virus type 2/ HuAHV2, HSV2 |
dsDNA | [38,110,327] | ||||
| Varicellovirus |
Varicellovirus
humanalpha 3 |
Human alphaherpesvirus 3; Varicella-zoster virus/ HuAHV3, VZV |
dsDNA |
S: Infected human hosts Pc/T: Person-to-person transmission; Congenital infection (TORCH). |
Aseptic meningitis, encephalitis, meningoencephalitis, myelitis | [110,327,358,359,360] | |
| Orthomyxoviridae | Alphainfluenzavirus |
Alphainfluenzavirus
influenzae |
Influenza A virus/ IAV |
ssRNA(−) |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets |
Meningitis, meningoencephalitis, encephalitis, myelitis, Guillain–Barré syndrome | [330,331,361] |
| Betainfluenzavirus |
Betainfluenzavirus
influenzae |
Influenza B virus/ IBV |
ssRNA(−) | [333] | |||
| Paramyxoviridae | Morbillivirus |
Morbillivirus
hominis |
Measles virus/ MV |
ssRNA(−) |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets |
Encephalitis | [362,363,364] |
| Orthorubulavirus |
Orthorubulavirus
parotitidis |
Mumps virus; Mumps orthorubulavirus 1/ MuV |
ssRNA(−) |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets |
Meningitis, encephalitis, myelitis | [365,366] | |
|
Orthorubulavirus
laryngotracheitidis |
Human parainfluenza virus 2; Human orthorubulavirus 2 1/ HPIV-2 |
ssRNA(−) |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets |
Encephalitis, severe acute encephalopathy | [367,368,369] | ||
| Respirovirus |
Respirovirus
laryngotracheitidis |
Human parainfluenza virus 1; Human respirovirus 1 1/ HPIV-1 |
ssRNA(−) |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets |
Encephalitis, multiple sclerosis | [367,370,371] | |
|
Respirovirus
pneumoniae |
Human parainfluenza virus 3/ HPIV-3 |
ssRNA(−) |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets |
Meningitis, encephalitis, Guillain–Barré syndrome | [367,369,372,373,374,375] | ||
| Parvoviridae | Bocaparvovirus |
Bocaparvovirus
primate 1 |
Human bocavirus 1/ HBoV1 |
ssDNA |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets |
Meningitis, meningoencephalitis, encephalitis | [339,376,377,378,379] |
| Erythroparvovirus |
Erythroparvovirus
primate 1 |
Human parvovirus B19/ B19V |
ssDNA |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets |
Meningitis, meningoencephalitis | [339,380,381,382] | |
| Tetraparvovirus |
Tetraparvovirus
primate 1 |
Human parvovirus 4/ PARV4 |
ssDNA |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets |
Encephalitis | [383] | |
| Picornaviridae | Enterovirus | Enterovirus A | Coxsackievirus A2/ CVA2 |
ssRNA(+) |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets; Fecal–oral spread; Contact with infected tissue, water, environmental surfaces. |
Encephalitis, acute flaccid paralysis, aseptic meningitis | [45,384] |
| Coxsackievirus A3/ CVA3 |
ssRNA(+) | Encephalitis, acute flaccid paralysis, aseptic meningitis | [45] | ||||
| Enterovirus A | Coxsackievirus A4/ CVA4 |
ssRNA(+) |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets; Fecal–oral spread; Contact with infected tissue, water, environmental surfaces. |
Encephalitis, acute flaccid paralysis, aseptic meningitis | [45] | ||
| Coxsakievirus A5/ CVA5 |
ssRNA(+) | Encephalitis, acute flaccid paralysis, aseptic meningitis | [45,385] | ||||
| Coxsakievirus A6/ CVA6 |
ssRNA(+) | Meningoencephalitis, encephalitis, acute flaccid paralysis, aseptic meningitis | [45] | ||||
| Coxsakievirus A7/ CVA7 |
ssRNA(+) | Aseptic meningitis, encephalitis, acute flaccid paralysis | [386,387] | ||||
| Coxsakievirus A8/ CVA8 |
ssRNA(+) | Acute flaccid paralysis, aseptic meningitis | [45] | ||||
| Coxsakievirus A10/ CVA10 |
ssRNA(+) | Meningoencephalitis, encephalitis, acute flaccid paralysis, aseptic meningitis | [45] | ||||
| Coxsakievirus A12/ CVA12 |
ssRNA(+) | Acute flaccid paralysis, aseptic meningitis | [45] | ||||
| Coxsakievirus A14/ CVA14 |
ssRNA(+) | Acute flaccid paralysis, aseptic meningitis | [45] | ||||
| Coxsakievirus A16/ CVA16 |
ssRNA(+) | Encephalitis, meningoencephalitis, rhombencephalitis, acute flaccid paralysis, aseptic meningitis | [45,388] | ||||
| Enterovirus A71/ EV-A71 |
ssRNA(+) | Aseptic meningitis, acute flaccid myelitis/acute flaccid paralysis, encephalitis | [344,389,390,391,392,393,394] | ||||
| Enterovirus B | Coxsakievirus A9/ CVA9 |
ssRNA(+) |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets; Fecal–oral spread; Contact with infected tissue, water, environmental surfaces. |
Encephalitis, aseptic meningitis, meningoencephalitis, rhombencephalitis, acute flaccid paralysis, acute transverse myelitis | [45,389,395] | ||
| Enterovirus B | Coxsackievirus B1/ CVB1 |
ssRNA(+) |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets; Fecal–oral spread; Contact with infected tissue, water, environmental surfaces. |
Encephalitis, aseptic meningitis, meningoencephalitis, rhombencephalitis, acute flaccid paralysis, acute transverse myelitis | [45,384] | ||
| Coxsakievirus B2/ CVB2 |
ssRNA(+) | Encephalitis, aseptic meningitis, meningoencephalitis, rhombencephalitis, acute flaccid paralysis, acute transverse myelitis | [45,389,396] | ||||
| Coxsakievirus B3/ CVB3 |
ssRNA(+) | Encephalitis, aseptic meningitis, meningoencephalitis, acute flaccid paralysis, acute transverse myelitis | [45,389] | ||||
| Coxsakievirus B4/ CVB4 |
ssRNA(+) | Encephalitis, aseptic meningitis, meningoencephalitis, rhombencephalitis, acute flaccid paralysis, acute transverse myelitis | [45,389,397,398] | ||||
| Coxsakievirus B5/ CVB5 |
ssRNA(+) | Encephalitis, aseptic meningitis, meningoencephalitis, acute flaccid paralysis, acute transverse myelitis | [45,389] | ||||
| Coxsakievirus B6/ CVB6 |
ssRNA(+) | Aseptic meningitis, acute flaccid paralysis | [45] | ||||
| Echovirus 4/ E4 |
ssRNA(+) | Aseptic meningitis, encephalitis | [399,400,401,402] | ||||
| Echovirus 5/ E5 |
ssRNA(+) | Aseptic meningitis, encephalitis | [402,403] | ||||
| Echovirus 6/ E6 |
ssRNA(+) | Meningitis, encephalitis, Guillain–Barré syndrome | [389,402,404,405,406] | ||||
| Echovirus 7/ E7 |
ssRNA(+) | Meningitis, encephalitis, encephalomyelitis | [402,407,408] | ||||
| Echovirus 9/ E9 |
ssRNA(+) | Meningitis, encephalitis | [402] | ||||
| Echovirus 11/ E11 |
ssRNA(+) | Aseptic meningitis, encephalitis (HFMD) | [402,409,410] | ||||
| Echovirus 13/ E13 |
ssRNA(+) | Meningitis, encephalitis | [389,402,411] | ||||
| Enterovirus B | Echovirus 14/ E14 |
ssRNA(+) |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets; Fecal–oral spread; Contact with infected tissue, water, environmental surfaces. |
Aseptic meningitis, encephalitis | [402] | ||
| Echovirus 15/ E15 |
ssRNA(+) | Aseptic meningitis, encephalitis | [389,402] | ||||
| Echovirus 16/ E16 |
ssRNA(+) | Aseptic meningitis | [402,412] | ||||
| Echovirus 17/ E17 |
ssRNA(+) | Aseptic meningitis, encephalitis | [402] | ||||
| Echovirus 18/ E18 |
ssRNA(+) | Aseptic meningitis, encephalitis | [402] | ||||
| Echovirus 19/ E19 |
ssRNA(+) | Aseptic meningitis, encephalitis | [389,402,413] | ||||
| Echovirus 22 1 | ssRNA(+) | Aseptic meningitis, Guillain–Barré syndrome | [402] | ||||
| Echovirus 25/ E25 |
ssRNA(+) | Aseptic meningitis, encephalitis | [402,414,415] | ||||
| Echovirus 30/ E30 |
ssRNA(+) | Meningitis, encephalitis | [364,380,381,402] | ||||
| Echovirus 31/ E31 |
ssRNA(+) | Aseptic meningitis | [402] | ||||
| Enterovirus B75/ EV-B75 |
ssRNA(+) | Aseptic meningitis, encephalitis | [416,417] | ||||
| Enterovirus C | Coxsackievirus A1/ CVA-1 |
ssRNA(+) |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets; Fecal–oral spread; Contact with infected tissue, water, environmental surfaces. |
Acute flaccid paralysis, aseptic meningitis | [45] | ||
| Coxsackievirus A11/ CVA-11 |
ssRNA(+) | Acute flaccid paralysis, meningoencephalitis | [45] | ||||
| Coxsackievirus A13/ CVA-13 |
ssRNA(+) | Acute flaccid paralysis, aseptic meningitis | [45] | ||||
| Coxsackievirus A17/ CVA-17 |
ssRNA(+) | Acute flaccid paralysis, aseptic meningitis | [45] | ||||
| Coxsackievirus A19/ CVA-19 |
ssRNA(+) | Acute flaccid paralysis, aseptic meningitis | [45] | ||||
| Coxsackievirus A20/ CVA-20 |
ssRNA(+) | Acute flaccid paralysis | [45] | ||||
| Coxsackievirus A21/ CVA-21 |
ssRNA(+) | Acute flaccid paralysis, encephalitis, aseptic meningitis | [45] | ||||
| Coxsackievirus A22/ CVA-22 |
ssRNA(+) | Acute flaccid paralysis | [45] | ||||
| Coxsackievirus A24/ CVA-24 |
ssRNA(+) | Acute flaccid paralysis, aseptic meningitis | [45] | ||||
| Polioviruses 1 Include: Serotypes of the species Enterovirus C (types 1, 2 and 3 of wild Poliovirus (WPV)) |
ssRNA(+) |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets; Fecal–oral spread; Contact with infected tissue, water, environmental surfaces. |
Poliomyelitis, meningitis, aseptic meningitis | [418,419,420] | |||
| Enterovirus D | Enterovirus D68; Human rhinovirus 87/ EV-D68 |
ssRNA(+) |
S: Infected human hosts Pc/T: Inhalation of aerosolized droplets; Fecal–oral spread; Contact with infected tissue, water, environmental surfaces. |
Meningo–myeloencephalitis, acute flaccid myelitis/acute flaccid paralysis | [20,344,421,422,423,424,425] | ||
| Enterovirus D70/ EV-D70 |
ssRNA(+) | Acute flaccid myelitis | [392,426] | ||||
| Hepatovirus | Hepatovirus A | Hepatovirus A1; Hepatitis A virus/ HAV |
ssRNA(+) |
S: Infected human hosts Pc/T: Blood-borne transmission by drug-injection equipment, blood transfusion, organ transplantation; Genital contact; Congenital infection. |
Encephalitis (extremely rare) |
[427] | |
| Parechovirus | Parechovirus A | Human parechovirus 3/ HPeV-3 |
ssRNA(+) |
S: Infected human hosts T: Inhalation of aerosolized droplets; Neonatal infection. |
Meningitis, meningoencephalitis, encephalitis |
[345,346,347,428] | |
| Pneumoviridae | Orthopneumovirus |
Orthopneumovirus
hominis |
Human orthopneumovirus; Human respiratory syncytial virus/ HRSV |
ssRNA(−) |
S: Infected human hosts T: Inhalation of aerosolized droplets |
Meningitis, encephalitis (?), encephalopathy | [429,430,431,432,433] |
| Metapneumovirus |
Metapneumovirus
hominis |
Human metapneumovirus/ HMPV |
ssRNA(−) |
S: Infected human hosts T: Inhalation of aerosolized droplets |
Encephalitis | [310,434,435,436,437,438] | |
| Polyomaviridae | Betapolyomavirus |
Betapolyomaviru
secuhominis |
JC polyomavirus; John Cunningham virus 1/ JC virus; JCV; JCPyV |
dsDNA |
S:/T: Autoinfection Pc: Immunocompromised condition |
Meningitis, encephalopathy |
[439,440] |
| Retroviridae | Lentivirus |
Human
immunodeficiency virus 1 |
Human immunodeficiency virus 1/ HIV-1 |
ssRNA-RT |
S: Infected human hosts Pc/T: Blood-borne transmission by drug-injection equipment, blood transfusion, organ transplantation; Genital contact; Congenital infection. |
Encephalitis (HAND) |
[46,351] |
|
Human
immunodeficiency virus 2 |
Human immunodeficiency virus 2/ HIV-2 |
ssRNA-RT |
S: Infected human hosts Pc/T: Blood-borne transmission by drug-injection equipment, blood transfusion, organ transplantation; Genital contact; Congenital infection. |
Encephalitis (HAND) |
[441] | ||
Taxonomic and trivial names are given according to the reports of the International Committee on Taxonomy of Viruses (ICTV) https://ictv.global/msl and https://ictv.global/vmr (versions from 2022/2023); 1 Commonly accepted alternative names not given in the reports of the International Committee on Taxonomy of Viruses (ICTV) (see above); ADEM—Acute disseminated encephalomyelitis; HAI—Hospital acquired infection; HAND—HIV-associated neurocognitive disorder; HFMD—Hand, foot, and mouth disease; HSCT—Hematopoietic stem-cell transplantation; TORCH—Acronym of hazardous for pregnancy infection agents: Toxoplasma gondii (or other agents like HIVs etc.), Rubella virus, Cytomegalovirus, Herpes simplex virus type 2.
5. Conclusions
In this review, we systematized and summarized information about human viral pathogens that can cause infections of the central nervous system. We based the systematization on the taxonomic affiliation of the corresponding infectious agents, dividing them into groups according to the predominant routes of transmission, accompanying the resulting list with information about their geographic distribution. In addition, special attention was paid to cases of infection with atypical pathogens, in order to present the most comprehensive list.
We hope that this work will be useful to healthcare professionals and researchers involved in this area and will contribute to the clarification of the etiological structure of viral neuroinfections.
Author Contributions
Conceptualization, V.N. and A.M.; information collection and curation, V.N. and A.M.; writing—original draft preparation, V.N.; writing, V.N. and A.M.; review and editing, A.M., V.N., M.G. and G.S. All authors have read and agreed to the published version of the manuscript. https://credit.niso.org/.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
This research was supported by the state assignment No 388-00099-23-02.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Wang H., Zhao S., Wang S., Zheng Y., Wang S., Chen H., Pang J., Ma J., Yang X., Chen Y. Global Magnitude of Encephalitis Burden and Its Evolving Pattern over the Past 30 Years. J. Infect. 2022;84:777–787. doi: 10.1016/j.jinf.2022.04.026. [DOI] [PubMed] [Google Scholar]
- 2.Glaser C.A., Honarmand S., Anderson L.J., Schnurr D.P., Forghani B., Cossen C.K., Schuster F.L., Christie L.J., Tureen J.H. Beyond Viruses: Clinical Profiles and Etiologies Associated with Encephalitis. Clin. Infect. Dis. 2006;43:1565–1577. doi: 10.1086/509330. [DOI] [PubMed] [Google Scholar]
- 3.Wright C., Blake N., Glennie L., Smith V., Bender R., Kyu H., Wunrow H.Y., Liu L., Yeung D., Knoll M.D., et al. The Global Burden of Meningitis in Children: Challenges with Interpreting Global Health Estimates. Microorganisms. 2021;9:377. doi: 10.3390/microorganisms9020377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zunt J.R., Kassebaum N.J., Blake N., Glennie L., Wright C., Nichols E., Abd-Allah F., Abdela J., Abdelalim A., Adamu A.A., et al. Global, Regional, and National Burden of Meningitis, 1990–2016: A Systematic Analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17:1061–1082. doi: 10.1016/S1474-4422(18)30387-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murphy O.C., Messacar K., Benson L., Bove R., Carpenter J.L., Crawford T., Dean J., DeBiasi R., Desai J., Elrick M.J., et al. Acute Flaccid Myelitis: Cause, Diagnosis, and Management. Lancet. 2021;397:334–346. doi: 10.1016/S0140-6736(20)32723-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Venkatesan A., Tunkel A.R., Bloch K.C., Lauring A.S., Sejvar J., Bitnun A., Stahl J.-P., Mailles A., Drebot M., Rupprecht C.E., et al. Case Definitions, Diagnostic Algorithms, and Priorities in Encephalitis: Consensus Statement of the International Encephalitis Consortium. Clin. Infect. Dis. 2013;57:1114–1128. doi: 10.1093/cid/cit458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Global Burden of Disease (GBD) by Institute for Health Metrics and Evaluation. [(accessed on 7 May 2024)]. Available online: https://www.healthdata.org/research-analysis/gbd.
- 8.Ghia C.J., Rambhad G.S. A Systematic Literature Review on the Prevalence and Etiology of Meningitis among Critically Ill and Hospitalized Patients in India. Ther. Adv. Infect. 2021;8:204993612110464. doi: 10.1177/20499361211046453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meningitis Research Foundation. [(accessed on 7 May 2024)]. Available online: https://www.meningitis.org/
- 10.Meningitis Progress Tracker Tracking Progress towards Defeating Meningitis—Visualising the Story of Meningitis for the First Time Meningitis Progress Tracker (Meningitis Research Foundation) [(accessed on 7 May 2024)]. Available online: https://www.meningitis.org/mpt.
- 11.John C.C., Carabin H., Montano S.M., Bangirana P., Zunt J.R., Peterson P.K. Global Research Priorities for Infections That Affect the Nervous System. Nature. 2015;527:S178–S186. doi: 10.1038/nature16033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patel J.C., Soeters H.M., Diallo A.O., Bicaba B.W., Kadadé G., Dembélé A.Y., Acyl M.A., Nikiema C., Lingani C., Hatcher C., et al. MenAfriNet: A Network Supporting Case-Based Meningitis Surveillance and Vaccine Evaluation in the Meningitis Belt of Africa. J. Infect. Dis. 2019;220:S148–S154. doi: 10.1093/infdis/jiz308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Park J.J., Narayanan S., Tiefenbach J., Lukšić I., Ale B.M., Adeloye D., Rudan I. Estimating the Global and Regional Burden of Meningitis in Children Caused by Haemophilus influenzae Type b: A Systematic Review and Meta-Analysis. J. Glob. Health. 2022;12:04014. doi: 10.7189/jogh.12.04014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thompson C., Kneen R., Riordan A., Kelly D., Pollard A.J. Encephalitis in Children. Arch. Dis. Child. 2012;97:150–161. doi: 10.1136/archdischild-2011-300100. [DOI] [PubMed] [Google Scholar]
- 15.Go Y.Y., Balasuriya U.B.R., Lee C. Zoonotic Encephalitides Caused by Arboviruses: Transmission and Epidemiology of Alphaviruses and Flaviviruses. Clin. Exp. Vaccine Res. 2014;3:58. doi: 10.7774/cevr.2014.3.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Бoлезни нервнoй системы: Рукoвoдствo для врачей: В 2-х тoмах. Volume 1. Медицина; Мoсква, Рoссия: 2001. Издание втoрoе, перерабoтаннoе и дoпoлненнoе. [Google Scholar]
- 17.World Health Organization: Poliomyelitis WHO 2022. [(accessed on 7 May 2024)]. Available online: https://www.who.int/news-room/fact-sheets/detail/poliomyelitis.
- 18.Sejvar J.J., Lopez A.S., Cortese M.M., Leshem E., Pastula D.M., Miller L., Glaser C., Kambhampati A., Shioda K., Aliabadi N., et al. Acute Flaccid Myelitis in the United States, August–December 2014: Results of Nationwide Surveillance. Clin. Infect. Dis. 2016;63:737–745. doi: 10.1093/cid/ciw372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Helfferich J., Knoester M., Van Leer-Buter C.C., Neuteboom R.F., Meiners L.C., Niesters H.G., Brouwer O.F. Acute Flaccid Myelitis and Enterovirus D68: Lessons from the Past and Present. Eur. J. Pediatr. 2019;178:1305–1315. doi: 10.1007/s00431-019-03435-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Messacar K., Asturias E.J., Hixon A.M., Van Leer-Buter C., Niesters H.G.M., Tyler K.L., Abzug M.J., Dominguez S.R. Enterovirus D68 and Acute Flaccid Myelitis—Evaluating the Evidence for Causality. Lancet Infect. Dis. 2018;18:e239–e247. doi: 10.1016/S1473-3099(18)30094-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McEntire C.R.S., Anand P., Cervantes-Arslanian A.M. Neuroinfectious Disease Emergencies. Neurol. Clin. 2021;39:565–588. doi: 10.1016/j.ncl.2021.02.003. [DOI] [PubMed] [Google Scholar]
- 22.Guo Y., Yang Y., Xu M., Shi G., Zhou J., Zhang J., Li H. Trends and Developments in the Detection of Pathogens in Central Nervous System Infections: A Bibliometric Study. Front. Cell. Infect. Microbiol. 2022;12:856845. doi: 10.3389/fcimb.2022.856845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Riddell J., Shuman E.K. Epidemiology of Central Nervous System Infection. Neuroimaging Clin. N. Am. 2012;22:543–556. doi: 10.1016/j.nic.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 24.Lu Y., Zhang X., Ni F., Xia W. Cutaneous Protothecosis with Meningitis Due to Prototheca Wickerhamii in an Immunocompetent Teenager: Case Report and Literature Review. Infect. Drug Resist. 2021;14:2787–2794. doi: 10.2147/IDR.S320795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang Q.-Q., Zhu L.-P., Weng X.-H., Li L., Wang J.-J. Meningitis Due to Prototheca Wickerhamii: Rare Case in China. Med. Mycol. 2007;45:85–88. doi: 10.1080/13693780601003835. [DOI] [PubMed] [Google Scholar]
- 26.Leveque N., Van Haecke A., Renois F., Boutolleau D., Talmud D., Andreoletti L. Rapid Virological Diagnosis of Central Nervous System Infections by Use of a Multiplex Reverse Transcription-PCR DNA Microarray. J. Clin. Microbiol. 2011;49:3874–3879. doi: 10.1128/JCM.01214-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Llor C., Bjerrum L. Antimicrobial Resistance: Risk Associated with Antibiotic Overuse and Initiatives to Reduce the Problem. Ther. Adv. Drug Saf. 2014;5:229–241. doi: 10.1177/2042098614554919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ustinov M.V. Empirical therapy of inflammatory lesion of large skin folds// Эмпирическая терапия вoспалительных пoражений кoжи крупных складoк. RMJ//РМЖ. 2016;14:945–948. [Google Scholar]
- 29.Gu W., Deng X., Lee M., Sucu Y.D., Arevalo S., Stryke D., Federman S., Gopez A., Reyes K., Zorn K., et al. Rapid Pathogen Detection by Metagenomic Next-Generation Sequencing of Infected Body Fluids. Nat. Med. 2021;27:115–124. doi: 10.1038/s41591-020-1105-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jourdan A., Sangha B., Kim E., Nawaz S., Malik V., Vij R., Sekhsaria S. Antibiotic Hypersensitivity and Adverse Reactions: Management and Implications in Clinical Practice. Allergy Asthma Clin. Immunol. 2020;16:6. doi: 10.1186/s13223-020-0402-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Blumenthal K.G., Peter J.G., Trubiano J.A., Phillips E.J. Antibiotic Allergy. Lancet. 2019;393:183–198. doi: 10.1016/S0140-6736(18)32218-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shallcross L.J., Davies D.S.C. Antibiotic Overuse: A Key Driver of Antimicrobial Resistance. Br. J. Gen. Pract. 2014;64:604–605. doi: 10.3399/bjgp14X682561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang Y., Cui P., Zhang H.-C., Wu H.-L., Ye M.-Z., Zhu Y.-M., Ai J.-W., Zhang W.-H. Clinical Application and Evaluation of Metagenomic Next-Generation Sequencing in Suspected Adult Central Nervous System Infection. J. Transl. Med. 2020;18:199. doi: 10.1186/s12967-020-02360-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilson M.R., Sample H.A., Zorn K.C., Arevalo S., Yu G., Neuhaus J., Federman S., Stryke D., Briggs B., Langelier C., et al. Clinical Metagenomic Sequencing for Diagnosis of Meningitis and Encephalitis. N. Engl. J. Med. 2019;380:2327–2340. doi: 10.1056/NEJMoa1803396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Meyer T., Franke G., Polywka S.K.A., Lütgehetmann M., Gbadamosi J., Magnus T., Aepfelbacher M. Improved Detection of Bacterial Central Nervous System Infections by Use of a Broad-Range PCR Assay. J. Clin. Microbiol. 2014;52:1751–1753. doi: 10.1128/JCM.00469-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kanjilal S., Cho T.A., Piantadosi A. Diagnostic Testing in Central Nervous System Infection. Semin. Neurol. 2019;39:297–311. doi: 10.1055/s-0039-1688441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zanella M.-C., Lenggenhager L., Schrenzel J., Cordey S., Kaiser L. High-Throughput Sequencing for the Aetiologic Identification of Viral Encephalitis, Meningoencephalitis, and Meningitis. A Narrative Review and Clinical Appraisal. Clin. Microbiol. Infect. 2019;25:422–430. doi: 10.1016/j.cmi.2018.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wouk J., Rechenchoski D.Z., Rodrigues B.C.D., Ribelato E.V., Faccin-Galhardi L.C. Viral Infections and Their Relationship to Neurological Disorders. Arch. Virol. 2021;166:733–753. doi: 10.1007/s00705-021-04959-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vigasova D., Nemergut M., Liskova B., Damborsky J. Multi-Pathogen Infections and Alzheimer’s Disease. Microb. Cell Fact. 2021;20:25. doi: 10.1186/s12934-021-01520-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bjornevik K., Cortese M., Healy B.C., Kuhle J., Mina M.J., Leng Y., Elledge S.J., Niebuhr D.W., Scher A.I., Munger K.L., et al. Longitudinal Analysis Reveals High Prevalence of Epstein-Barr Virus Associated with Multiple Sclerosis. Science. 2022;375:296–301. doi: 10.1126/science.abj8222. [DOI] [PubMed] [Google Scholar]
- 41.Leblanc P., Vorberg I.M. Viruses in Neurodegenerative Diseases: More than Just Suspects in Crimes. PLoS Pathog. 2022;18:e1010670. doi: 10.1371/journal.ppat.1010670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mariani M.M., Kielian T. Microglia in Infectious Diseases of the Central Nervous System. J. Neuroimmune Pharmacol. 2009;4:448–461. doi: 10.1007/s11481-009-9170-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jorgačevski J., Potokar M. Immune Functions of Astrocytes in Viral Neuroinfections. IJMS. 2023;24:3514. doi: 10.3390/ijms24043514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lin C.-H., Lin W.-D., Chou I.-C., Lee I.-C., Hong S.-Y. Epilepsy and Neurodevelopmental Outcomes in Children with Etiologically Diagnosed Central Nervous System Infections: A Retrospective Cohort Study. Front. Neurol. 2019;10:528. doi: 10.3389/fneur.2019.00528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Machado R.S., Tavares F.N., Sousa I.P. Global Landscape of Coxsackieviruses in Human Health. Virus Res. 2024;344:199367. doi: 10.1016/j.virusres.2024.199367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Swanson P.A., McGavern D.B. Viral Diseases of the Central Nervous System. Curr. Opin. Virol. 2015;11:44–54. doi: 10.1016/j.coviro.2014.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smuts I., Lamb G.V. Viral Infections of the Central Nervous System. In: Green R.J., editor. Viral Infections in Children, Volume II. Springer International Publishing; Cham, Switzerland: 2017. pp. 83–123. [Google Scholar]
- 48.Bonthius D.J., Bale J.F. Swaiman’s Pediatric Neurology. Elsevier; New York, NY, USA: 2017. Viral Infections of the Nervous System; pp. 895–906. [Google Scholar]
- 49.Bonthius D.J. Lymphocytic Choriomeningitis Virus: An Underrecognized Cause of Neurologic Disease in the Fetus, Child, and Adult. Semin. Pediatr. Neurol. 2012;19:89–95. doi: 10.1016/j.spen.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Di Vito A., Donato A., Bria J., Donato F., Donato G. Encephalitis Lethargica. What Is Still Wrong? Int. J. Immunopathol. Pharmacol. 2023;37:039463202311549. doi: 10.1177/03946320231154997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Foley P.B. Encephalitis lethargica. Springer; New York, NY, USA: 2018. What Caused Encephalitis Lethargica; pp. 683–780. [Google Scholar]
- 52.Tselis A.C., Booss J. Handbook of Clinical Neurology. Elsevier; Edinburgh, UK: 2014. Neurovirology. [Google Scholar]
- 53.Lipton H.L. Human Vilyuisk Encephalitis. Rev. Med. Virol. 2008;18:347–352. doi: 10.1002/rmv.585. [DOI] [PubMed] [Google Scholar]
- 54.Liang Z., Kumar A.S.M., Jones M.S., Knowles N.J., Lipton H.L. Phylogenetic Analysis of the Species Theilovirus: Emerging Murine and Human Pathogens. J. Virol. 2008;82:11545–11554. doi: 10.1128/JVI.01160-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Eibach D., Hogan B., Sarpong N., Winter D., Struck N.S., Adu-Sarkodie Y., Owusu-Dabo E., Schmidt-Chanasit J., May J., Cadar D. Viral Metagenomics Revealed Novel Betatorquevirus Species in Pediatric Inpatients with Encephalitis/Meningoencephalitis from Ghana. Sci. Rep. 2019;9:2360. doi: 10.1038/s41598-019-38975-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tan L.V., van Doorn H.R., Nghia H.D.T., Chau T.T.H., Tu L.T.P., de Vries M., Canuti M., Deijs M., Jebbink M.F., Baker S., et al. Identification of a New Cyclovirus in Cerebrospinal Fluid of Patients with Acute Central Nervous System Infections. mBio. 2013;4:e00231-13. doi: 10.1128/mBio.00231-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Viglietta M., Bellone R., Blisnick A.A., Failloux A.-B. Vector Specificity of Arbovirus Transmission. Front. Microbiol. 2021;12:773211. doi: 10.3389/fmicb.2021.773211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shi J., Hu Z., Deng F., Shen S. Tick-Borne Viruses. Virol. Sin. 2018;33:21–43. doi: 10.1007/s12250-018-0019-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rochlin I., Toledo A. Emerging Tick-Borne Pathogens of Public Health Importance: A Mini-Review. J. Med. Microbiol. 2020;69:781–791. doi: 10.1099/jmm.0.001206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rosenberg R., Lindsey N.P., Fischer M., Gregory C.J., Hinckley A.F., Mead P.S., Paz-Bailey G., Waterman S.H., Drexler N.A., Kersh G.J., et al. Vital Signs: Trends in Reported Vectorborne Disease Cases—United States and Territories, 2004–2016. MMWR Morb. Mortal. Wkly. Rep. 2018;67:496–501. doi: 10.15585/mmwr.mm6717e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Labuda M., Nuttall P.A. Viruses Transmitted by Ticks. In: Bowman A.S., Nuttall P.A., editors. Ticks. Cambridge University Press; Cambridge, UK: 2008. pp. 253–280. [Google Scholar]
- 62.McGill F., Griffiths M.J., Solomon T. Viral Meningitis: Current Issues in Diagnosis and Treatment. Curr. Opin. Infect. Dis. 2017;30:248–256. doi: 10.1097/QCO.0000000000000355. [DOI] [PubMed] [Google Scholar]
- 63.Pustijanac E., Buršić M., Talapko J., Škrlec I., Meštrović T., Lišnjić D. Tick-Borne Encephalitis Virus: A Comprehensive Review of Transmission, Pathogenesis, Epidemiology, Clinical Manifestations, Diagnosis, and Prevention. Microorganisms. 2023;11:1634. doi: 10.3390/microorganisms11071634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ličková M., Fumačová Havlíková S., Sláviková M., Klempa B. Alimentary Infections by Tick-Borne Encephalitis Virus. Viruses. 2021;14:56. doi: 10.3390/v14010056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Venugopal K., Buckley A., Reid H.W., Gould E.A. Nucleotide Sequence of the Envelope Glycoprotein of Negishi Virus Shows Very Close Homology to Louping III Virus. Virology. 1992;190:515–521. doi: 10.1016/0042-6822(92)91245-P. [DOI] [PubMed] [Google Scholar]
- 66.Hubálek Z., Rudolf I., Nowotny N. Advances in Virus Research. Volume 89. Elsevier; New York, NY, USA: 2014. Arboviruses Pathogenic for Domestic and Wild Animals; pp. 201–275. [DOI] [PubMed] [Google Scholar]
- 67.Jeffries C.L., Mansfield K.L., Phipps L.P., Wakeley P.R., Mearns R., Schock A., Bell S., Breed A.C., Fooks A.R., Johnson N. Louping Ill Virus: An Endemic Tick-Borne Disease of Great Britain. J. Gen. Virol. 2014;95:1005–1014. doi: 10.1099/vir.0.062356-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gritsun T.S., Nuttall P.A., Gould E.A. Advances in Virus Research. Volume 61. Elsevier; New York, NY, USA: 2003. Tick-Borne Flaviviruses; pp. 317–371. [DOI] [PubMed] [Google Scholar]
- 69.Leonova G.N., Kondratov I.G., Maystrovskaya O.S., Takashima I., Belikov S.I. Louping Ill Virus (LIV) in the Far East. Arch. Virol. 2015;160:663–673. doi: 10.1007/s00705-014-2310-1. [DOI] [PubMed] [Google Scholar]
- 70.Holding M., Dowall S.D., Medlock J.M., Carter D.P., Pullan S.T., Lewis J., Vipond R., Rocchi M.S., Baylis M., Hewson R. Tick-Borne Encephalitis Virus, United Kingdom. Emerg. Infect. Dis. 2020;26:90–96. doi: 10.3201/eid2601.191085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rollin P.E., Memish Z.A. Emerging Infectious Diseases. Elsevier; New York, NY, USA: 2014. Alkhurma Hemorrhagic Fever; pp. 61–71. [Google Scholar]
- 72.Carletti F., Castilletti C., Di Caro A., Capobianchi M.R., Nisii C., Suter F., Rizzi M., Tebaldi A., Goglio A., Tosi C.P., et al. Alkhurma Hemorrhagic Fever in Travelers Returning from Egypt, 2010. Emerg. Infect. Dis. 2010;16:1979–1982. doi: 10.3201/eid1612.101092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bhatia B., Feldmann H., Marzi A. Kyasanur Forest Disease and Alkhurma Hemorrhagic Fever Virus—Two Neglected Zoonotic Pathogens. Microorganisms. 2020;8:1406. doi: 10.3390/microorganisms8091406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Al-Tawfiq J.A., Memish Z.A. Alkhurma Hemorrhagic Fever Virus. Microbes Infect. 2017;19:305–310. doi: 10.1016/j.micinf.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 75.Munivenkatappa A., Sahay R., Yadav P., Viswanathan R., Mourya D. Clinical & Epidemiological Significance of Kyasanur Forest Disease. Indian J. Med. Res. 2018;148:145. doi: 10.4103/ijmr.IJMR_688_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Růžek D., Yakimenko V.V., Karan L.S., Tkachev S.E. Omsk Haemorrhagic Fever. Lancet. 2010;376:2104–2113. doi: 10.1016/S0140-6736(10)61120-8. [DOI] [PubMed] [Google Scholar]
- 77.Rudakov N.V., Yastrebov V.K., Yakimenko V.V. Epidemiology of Omsk Haemorragic Fever. Epidemiol. Vaccine Prev. 2015;14:39–48. doi: 10.31631/2073-3046-2015-14-1-39-48. [DOI] [Google Scholar]
- 78.Wagner E., Shin A., Tukhanova N., Turebekov N., Nurmakhanov T., Sutyagin V., Berdibekov A., Maikanov N., Lezdinsh I., Shapiyeva Z., et al. First Indications of Omsk Haemorrhagic Fever Virus beyond Russia. Viruses. 2022;14:754. doi: 10.3390/v14040754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lvov D.K., Shchelkanov M.Y., Alkhovsky S.V., Deryabin P.G. Zoonotic Viruses in Northern Eurasia. Elsevier; New York, NY, USA: 2015. Single-Stranded RNA Viruses; pp. 135–392. [Google Scholar]
- 80.Birge J., Sonnesyn S. Powassan Virus Encephalitis, Minnesota, USA. Emerg. Infect. Dis. 2012;18:1669–1671. doi: 10.3201/eid1810.120621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lyons J.L. Viral Meningitis and Encephalitis. Contin. Lifelong Learn. Neurol. 2018;24:1284–1297. doi: 10.1212/CON.0000000000000650. [DOI] [PubMed] [Google Scholar]
- 82.Tavakoli N.P., Wang H., Dupuis M., Hull R., Ebel G.D., Gilmore E.J., Faust P.L. Fatal Case of Deer Tick Virus Encephalitis. N. Engl. J. Med. 2009;360:2099–2107. doi: 10.1056/NEJMoa0806326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lledó L., Giménez-Pardo C., Gegúndez M.I. Epidemiological Study of Thogoto and Dhori Virus Infection in People Bitten by Ticks, and in Sheep, in an Area of Northern Spain. IJERPH. 2020;17:2254. doi: 10.3390/ijerph17072254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hubálek Z., Rudolf I. Tick-Borne Viruses in Europe. Parasitol. Res. 2012;111:9–36. doi: 10.1007/s00436-012-2910-1. [DOI] [PubMed] [Google Scholar]
- 85.Koch J., Xin Q., Tischler N.D., Lozach P.-Y. Entry of Phenuiviruses into Mammalian Host Cells. Viruses. 2021;13:299. doi: 10.3390/v13020299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Matsuno K., Weisend C., Travassos da Rosa A.P.A., Anzick S.L., Dahlstrom E., Porcella S.F., Dorward D.W., Yu X.-J., Tesh R.B., Ebihara H. Characterization of the Bhanja Serogroup Viruses (Bunyaviridae): A Novel Species of the Genus Phlebovirus and Its Relationship with Other Emerging Tick-Borne Phleboviruses. J. Virol. 2013;87:3719–3728. doi: 10.1128/JVI.02845-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hubálek Z. Biogeography of Tick-Borne Bhanja Virus (Bunyaviridae) in Europe. Interdiscip. Perspect. Infect. Dis. 2009;2009:372691. doi: 10.1155/2009/372691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.DeBiasi R.L., Tyler K.L. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. Elsevier; New York, NY, USA: 2015. Orthoreoviruses and Orbiviruses; pp. 1848–1850. [Google Scholar]
- 89.Dilcher M., Hasib L., Lechner M., Wieseke N., Middendorf M., Marz M., Koch A., Spiegel M., Dobler G., Hufert F.T., et al. Genetic Characterization of Tribeč Virus and Kemerovo Virus, Two Tick-Transmitted Human-Pathogenic Orbiviruses. Virology. 2012;423:68–76. doi: 10.1016/j.virol.2011.11.020. [DOI] [PubMed] [Google Scholar]
- 90.Lvov D.K., Shchelkanov M.Y., Alkhovsky S.V., Deryabin P.G. Zoonotic Viruses in Northern Eurasia. Elsevier; New York, NY, USA: 2015. Double-Stranded RNA Viruses; pp. 113–133. [Google Scholar]
- 91.Padgett K.A., Kjemtrup A., Novak M., Velez J.O., Panella N. Colorado Tick Fever Virus in the Far West: Forgotten, but Not Gone. Vector-Borne Zoonotic Dis. 2022;22:443–448. doi: 10.1089/vbz.2022.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yendell S.J., Fischer M., Staples J.E. Colorado Tick Fever in the United States, 2002–2012. Vector-Borne Zoonotic Dis. 2015;15:311–316. doi: 10.1089/vbz.2014.1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Shah T., Li Q., Wang B., Baloch Z., Xia X. Geographical Distribution and Pathogenesis of Ticks and Tick-Borne Viral Diseases. Front. Microbiol. 2023;14:1185829. doi: 10.3389/fmicb.2023.1185829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Attoui H., Jaafar F.M., de Micco P., de Lamballerie X. Coltiviruses and Seadornaviruses in North America, Europe, and Asia. Emerg. Infect. Dis. 2005;11:1673–1679. doi: 10.3201/eid1111.050868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Charrel R.N., Attoui H., Butenko A.M., Clegg J.C., Deubel V., Frolova T.V., Gould E.A., Gritsun T.S., Heinz F.X., Labuda M., et al. Tick-Borne Virus Diseases of Human Interest in Europe. Clin. Microbiol. Infect. 2004;10:1040–1055. doi: 10.1111/j.1469-0691.2004.01022.x. [DOI] [PubMed] [Google Scholar]
- 96.Günther G., Haglund M. Tick-Borne Encephalopathies: Epidemiology, Diagnosis, Treatment and Prevention. CNS Drugs. 2005;19:1009–1032. doi: 10.2165/00023210-200519120-00004. [DOI] [PubMed] [Google Scholar]
- 97.Ungureanu A., van der Meer J., Bicvic A., Abbuehl L., Chiffi G., Jaques L., Suter-Riniker F., Leib S.L., Bassetti C.L.A., Dietmann A. Meningitis, Meningoencephalitis and Encephalitis in Bern: An Observational Study of 258 Patients. BMC Neurol. 2021;21:474. doi: 10.1186/s12883-021-02502-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Buczek A.M., Buczek W., Buczek A., Wysokińska-Miszczuk J. Food-Borne Transmission of Tick-Borne Encephalitis Virus—Spread, Consequences, and Prophylaxis. IJERPH. 2022;19:1812. doi: 10.3390/ijerph19031812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Tick-Borne Encephalitis (TBE) Virus: Geographic Distribution. [(accessed on 7 May 2024)]; Available online: https://www.cdc.gov/tick-borne-encephalitis/geographic-distribution/index.html.
- 100.Madison-Antenucci S., Kramer L.D., Gebhardt L.L., Kauffman E. Emerging Tick-Borne Diseases. Clin. Microbiol. Rev. 2020;33:10–1128. doi: 10.1128/CMR.00083-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kholodilov I.S., Belova O.A., Ivannikova A.Y., Gadzhikurbanov M.N., Makenov M.T., Yakovlev A.S., Polienko A.E., Dereventsova A.V., Litov A.G., Gmyl L.V., et al. Distribution and Characterisation of Tick-Borne Flavi-, Flavi-like, and Phenuiviruses in the Chelyabinsk Region of Russia. Viruses. 2022;14:2699. doi: 10.3390/v14122699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lindquist L. Handbook of Clinical Neurology. Volume 123. Elsevier; New York, NY, USA: 2014. Tick-Borne Encephalitis; pp. 531–559. [DOI] [PubMed] [Google Scholar]
- 103.Chiba N., Iwasaki T., Mizutani T., Kariwa H., Kurata T., Takashima I. Pathogenicity of Tick-Borne Encephalitis Virus Isolated in Hokkaido, Japan in Mouse Model. Vaccine. 1999;17:779–787. doi: 10.1016/S0264-410X(98)00262-X. [DOI] [PubMed] [Google Scholar]
- 104.Yoshii K., Song J.Y., Park S.-B., Yang J., Schmitt H.-J. Tick-Borne Encephalitis in Japan, Republic of Korea and China. Emerg. Microbes Infect. 2017;6:e82. doi: 10.1038/emi.2017.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kemenesi G., Bányai K. Tick-Borne Flaviviruses, with a Focus on Powassan Virus. Clin. Microbiol. Rev. 2018;32:e00106-17. doi: 10.1128/CMR.00106-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Mansfield K.L., Jizhou L., Phipps L.P., Johnson N. Emerging Tick-Borne Viruses in the Twenty-First Century. Front. Cell. Infect. Microbiol. 2017;7:298. doi: 10.3389/fcimb.2017.00298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.El Khoury M.Y., Camargo J.F., White J.L., Backenson B.P., Dupuis A.P., Escuyer K.L., Kramer L., St. George K., Chatterjee D., Prusinski M., et al. Potential Role of Deer Tick Virus in Powassan Encephalitis Cases in Lyme Disease–Endemic Areas of New York, USA. Emerg. Infect. Dis. 2013;19:1926. doi: 10.3201/eid1912.130903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Michelitsch A., Wernike K., Klaus C., Dobler G., Beer M. Exploring the Reservoir Hosts of Tick-Borne Encephalitis Virus. Viruses. 2019;11:669. doi: 10.3390/v11070669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Cunha M.S., Luchs A., da Costa A.C., Ribeiro G.d.O., dos Santos F.C.P., Nogueira J.S., Komninakis S.V., dos Santos Souza Marinho R., Witkin S.S., Villanova F., et al. Detection and Characterization of Ilheus and Iguape Virus Genomes in Historical Mosquito Samples from Southern Brazil. Acta Trop. 2020;205:105401. doi: 10.1016/j.actatropica.2020.105401. [DOI] [PubMed] [Google Scholar]
- 110.Sousa I.P., dos Santos F.B., de Paula V.S., Vieira T.C.R.G., Dias H.G., Barros C.A., da Silva E.E. Viral and Prion Infections Associated with Central Nervous System Syndromes in Brazil. Viruses. 2021;13:1370. doi: 10.3390/v13071370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Nanaware N., Banerjee A., Mullick Bagchi S., Bagchi P., Mukherjee A. Dengue Virus Infection: A Tale of Viral Exploitations and Host Responses. Viruses. 2021;13:1967. doi: 10.3390/v13101967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Weyer J., Blumberg L.H. Emerging Zoonotic and Vector-Borne Viral Diseases. In: Green R.J., editor. Viral Infections in Children, Volume I. Springer International Publishing; Cham, Switzerland: 2017. pp. 125–150. [Google Scholar]
- 113.Rezende I.M.D., Cenachi A.R.C., Costa T.A., Oliveira G.F.G., Rabelo L., Menezes L.M., Penido I., Pereira L.S., Arruda M.S., Gonçalves A.P., et al. Wild-Type Yellow Fever Virus in Cerebrospinal Fluid from Fatal Cases in Brazil, 2018. Front. Virol. 2022;2:936191. doi: 10.3389/fviro.2022.936191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.McMahon A.W., Eidex R.B., Marfin A.A., Russell M., Sejvar J.J., Markoff L., Hayes E.B., Chen R.T., Ball R., Braun M.M., et al. Neurologic Disease Associated with 17D-204 Yellow Fever Vaccination: A Report of 15 Cases. Vaccine. 2007;25:1727–1734. doi: 10.1016/j.vaccine.2006.11.027. [DOI] [PubMed] [Google Scholar]
- 115.Silva N.I.O., Sacchetto L., de Rezende I.M., Trindade G.d.S., LaBeaud A.D., de Thoisy B., Drumond B.P. Recent Sylvatic Yellow Fever Virus Transmission in Brazil: The News from an Old Disease. Virol. J. 2020;17:9. doi: 10.1186/s12985-019-1277-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Oyono M.G., Kenmoe S., Abanda N.N., Takuissu G.R., Ebogo-Belobo J.T., Kenfack-Momo R., Kengne-Nde C., Mbaga D.S., Tchatchouang S., Kenfack-Zanguim J., et al. Epidemiology of Yellow Fever Virus in Humans, Arthropods, and Non-Human Primates in Sub-Saharan Africa: A Systematic Review and Meta-Analysis. PLoS Negl. Trop. Dis. 2022;16:e0010610. doi: 10.1371/journal.pntd.0010610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Marinho P.E.S., Alvarenga P.P.M., Crispim A.P.C., Candiani T.M.S., Alvarenga A.M., Bechler I.M., Alves P.A., Dornas F.P., de Oliveira D.B., Bentes A.A., et al. Wild-Type Yellow Fever Virus RNA in Cerebrospinal Fluid of Child. Emerg. Infect. Dis. 2019;25:1567–1570. doi: 10.3201/eid2508.181479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Karunamoorthi K. Yellow Fever Encephalitis: An Emerging and Resurging Global Public Health Threat in a Changing Environment. In: Tkachev S., editor. Encephalitis. InTech; London, UK: 2013. [Google Scholar]
- 119.Сизикoва Татьяна Евгеньевна, Савенкo Сергей Вадимoвич, Лебедев Виталий Никoлаевич, Бoрисевич Сергей Владимирoвич Энцефалит Рoссиo. Инфекциoнные бoлезни. 2022;11:113–118. [Google Scholar]
- 120.Srivastava K.S., Jeswani V., Pal N., Bohra B., Vishwakarma V., Bapat A.A., Patnaik Y.P., Khanna N., Shukla R. Japanese Encephalitis Virus: An Update on the Potential Antivirals and Vaccines. Vaccines. 2023;11:742. doi: 10.3390/vaccines11040742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Vahey G.M., Mathis S., Martin S.W., Gould C.V., Staples J.E., Lindsey N.P. West Nile Virus and Other Domestic Nationally Notifiable Arboviral Diseases—United States, 2019. MMWR Morb. Mortal. Wkly. Rep. 2021;70:1069–1074. doi: 10.15585/mmwr.mm7032a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Danforth M.E., Snyder R.E., Feiszli T., Bullick T., Messenger S., Hanson C., Padgett K., Coffey L.L., Barker C.M., Reisen W.K., et al. Epidemiologic and Environmental Characterization of the Re-Emergence of St. Louis Encephalitis Virus in California, 2015–2020. PLoS Negl. Trop. Dis. 2022;16:e0010664. doi: 10.1371/journal.pntd.0010664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Diaz A., Coffey L.L., Burkett-Cadena N., Day J.F. Reemergence of St. Louis Encephalitis Virus in the Americas. Emerg. Infect. Dis. 2018;24:2150–2157. doi: 10.3201/eid2412.180372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hills S.L., Fischer M., Lindsey N.P., Curren E.J. St. Louis Encephalitis Virus Disease in the United States, 2003–2017. Am. J. Trop. Med. Hyg. 2018;99:1074–1079. doi: 10.4269/ajtmh.18-0420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Floridis J., McGuinness S., Kurucz N., Burrow J., Baird R., Francis J. Murray Valley Encephalitis Virus: An Ongoing Cause of Encephalitis in Australia’s North. Trop. Med. Infect. Dis. 2018;3:49. doi: 10.3390/tropicalmed3020049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Niven D.J., Afra K., Iftinca M., Tellier R., Fonseca K., Kramer A., Safronetz D., Holloway K., Drebot M., Johnson A.S. Fatal Infection with Murray Valley Encephalitis Virus Imported from Australia to Canada, 2011. Emerg. Infect. Dis. 2017;23:280–283. doi: 10.3201/eid2302.161161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Ong O.T.W., Skinner E.B., Johnson B.J., Old J.M. Mosquito-Borne Viruses and Non-Human Vertebrates in Australia: A Review. Viruses. 2021;13:265. doi: 10.3390/v13020265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Mackenzie J.S., Lindsay M.D.A., Smith D.W., Imrie A. The Ecology and Epidemiology of Ross River and Murray Valley Encephalitis Viruses in Western Australia: Examples of One Health in Action. Trans. R. Soc. Trop. Med. Hyg. 2017;111:248–254. doi: 10.1093/trstmh/trx045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Wanzeller A.L.M., da Silva F.S., Hernández L.H.A., Barros L.J.L., Freitas M.N.O., Santos M.M., Gonçalves E.d.J., Pantoja J.A.S., Lima C.d.S., Lima M.F., et al. Isolation of Flaviviruses and Alphaviruses with Encephalitogenic Potential Diagnosed by Evandro Chagas Institute (Pará, Brazil) in the Period of 1954–2022: Six Decades of Discoveries. Viruses. 2023;15:935. doi: 10.3390/v15040935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Gould E., Pettersson J., Higgs S., Charrel R., de Lamballerie X. Emerging Arboviruses: Why Today? One Health. 2017;4:1–13. doi: 10.1016/j.onehlt.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Habarugira G., Suen W.W., Hobson-Peters J., Hall R.A., Bielefeldt-Ohmann H. West Nile Virus: An Update on Pathobiology, Epidemiology, Diagnostics, Control and “One Health” Implications. Pathogens. 2020;9:589. doi: 10.3390/pathogens9070589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Byas A.D., Ebel G.D. Comparative Pathology of West Nile Virus in Humans and Non-Human Animals. Pathogens. 2020;9:48. doi: 10.3390/pathogens9010048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Bauerfeind R., Graevenitz A.V., Kimmig P., Schiefer H.G., Schwarz T., Slenczka W., Zahner H. Zoonoses: Infectious Diseases Transmissible from Animals to Humans. 4th ed. ASM Books; ASM Press; Washington, DC, USA: 2015. [Google Scholar]
- 134.Hall R.A., Scherret J.H., Mackenzie J.S. Kunjin Virus: An Australian Variant of West Nile? Ann. N. Y. Acad. Sci. 2001;951:153–160. doi: 10.1111/j.1749-6632.2001.tb02693.x. [DOI] [PubMed] [Google Scholar]
- 135.Clé M., Beck C., Salinas S., Lecollinet S., Gutierrez S., Van de Perre P., Baldet T., Foulongne V., Simonin Y. Usutu Virus: A New Threat? Epidemiol. Infect. 2019;147:e232. doi: 10.1017/S0950268819001213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Cadar D., Becker N., Campos R.d.M., Börstler J., Jöst H., Schmidt-Chanasit J. Usutu Virus in Bats, Germany, 2013. Emerg. Infect. Dis. 2014;20:1771–1773. doi: 10.3201/eid2010.140909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Ben Hassine T., De Massis F., Calistri P., Savini G., BelHaj Mohamed B., Ranen A., Di Gennaro A., Sghaier S., Hammami S. First Detection of Co-Circulation of West Nile and Usutu Viruses in Equids in the South-West of Tunisia. Transbound. Emerg. Dis. 2014;61:385–389. doi: 10.1111/tbed.12259. [DOI] [PubMed] [Google Scholar]
- 138.Diagne M., Ndione M., Di Paola N., Fall G., Bedekelabou A., Sembène P., Faye O., Zanotto P., Sall A. Usutu Virus Isolated from Rodents in Senegal. Viruses. 2019;11:181. doi: 10.3390/v11020181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.McEntire C.R.S., Song K.-W., McInnis R.P., Rhee J.Y., Young M., Williams E., Wibecan L.L., Nolan N., Nagy A.M., Gluckstein J., et al. Neurologic Manifestations of the World Health Organization’s List of Pandemic and Epidemic Diseases. Front. Neurol. 2021;12:634827. doi: 10.3389/fneur.2021.634827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Mwaliko C., Nyaruaba R., Zhao L., Atoni E., Karungu S., Mwau M., Lavillette D., Xia H., Yuan Z. Zika Virus Pathogenesis and Current Therapeutic Advances. Pathog. Glob. Health. 2021;115:21–39. doi: 10.1080/20477724.2020.1845005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Wen Z., Song H., Ming G. How Does Zika Virus Cause Microcephaly? Genes Dev. 2017;31:849–861. doi: 10.1101/gad.298216.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Roth N.M., Reynolds M.R., Lewis E.L., Woodworth K.R., Godfred-Cato S., Delaney A., Akosa A., Valencia-Prado M., Lash M., Elmore A., et al. Zika-Associated Birth Defects Reported in Pregnancies with Laboratory Evidence of Confirmed or Possible Zika Virus Infection—U.S. Zika Pregnancy and Infant Registry, December 1, 2015–March 31, 2018. MMWR Morb. Mortal. Wkly. Rep. 2022;71:73–79. doi: 10.15585/mmwr.mm7103a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Edridge A.W.D., van der Hoek L. Emerging Orthobunyaviruses Associated with CNS Disease. PLoS Negl. Trop. Dis. 2020;14:e0008856. doi: 10.1371/journal.pntd.0008856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Braack L., Gouveia de Almeida A.P., Cornel A.J., Swanepoel R., de Jager C. Mosquito-Borne Arboviruses of African Origin: Review of Key Viruses and Vectors. Parasites Vectors. 2018;11:29. doi: 10.1186/s13071-017-2559-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Dutuze M.F., Nzayirambaho M., Mores C.N., Christofferson R.C. A Review of Bunyamwera, Batai, and Ngari Viruses: Understudied Orthobunyaviruses with Potential One Health Implications. Front. Vet. Sci. 2018;5:69. doi: 10.3389/fvets.2018.00069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Binder L.d.C., Tauro L.B., Farias A.A., Labruna M.B., Diaz A. Molecular Survey of Flaviviruses and Orthobunyaviruses in Amblyomma Spp. Ticks Collected in Minas Gerais, Brazil. Rev. Bras. Parasitol. Vet. 2019;28:764–768. doi: 10.1590/s1984-29612019071. [DOI] [PubMed] [Google Scholar]
- 147.McIntosh B.M., Kokernot R.H., Smithburn K.C., Paterson H.E. Isolation of Germiston Virus, a Hitherto Unknown Agent, from Culicine Mosquitoes, and a Report of Infection in Two Laboratory Workers. Am. J. Trop. Med. Hyg. 1960;9:62–69. doi: 10.4269/ajtmh.1960.9.62. [DOI] [PubMed] [Google Scholar]
- 148.Beran G.W. Handbook of Zoonoses, Section B Viral Zoonoses. 2nd ed. Volume B. CRC Press; Boca Raton, FL, USA: 1994. [Google Scholar]
- 149.Campbell G.L., Mataczynski J.D., Reisdorf E.S., Powell J.W., Martin D.A., Lambert A.J., Haupt T.E., Davis J.P., Lanciotti R.S. Second Human Case of Cache Valley Virus Disease. Emerg. Infect. Dis. 2006;12:854–856. doi: 10.3201/eid1205.051625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Yang Y., Qiu J., Snyder-Keller A., Wu Y., Sun S., Sui H., Dean A.B., Kramer L., Hernandez-Ilizaliturri F. Fatal Cache Valley Virus Meningoencephalitis Associated with Rituximab Maintenance Therapy. Am. J. Hematol. 2018;93:590–594. doi: 10.1002/ajh.25024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Wilson M.R., Suan D., Duggins A., Schubert R.D., Khan L.M., Sample H.A., Zorn K.C., Rodrigues Hoffman A., Blick A., Shingde M., et al. A Novel Cause of Chronic Viral Meningoencephalitis: Cache Valley Virus: Orthobunyavirus Encephalitis. Ann. Neurol. 2017;82:105–114. doi: 10.1002/ana.24982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Nguyen N.L., Zhao G., Hull R., Shelly M.A., Wong S.J., Wu G., St. George K., Wang D., Menegus M.A. Cache Valley Virus in a Patient Diagnosed with Aseptic Meningitis. J. Clin. Microbiol. 2013;51:1966–1969. doi: 10.1128/JCM.00252-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Rodriguez C., Gricourt G., Ndebi M., Demontant V., Poiteau L., Burrel S., Boutolleau D., Woerther P.-L., Calvez V., Stroer S., et al. Fatal Encephalitis Caused by Cristoli Virus, an Emerging Orthobunyavirus, France. Emerg. Infect. Dis. 2020;26:1287–1290. doi: 10.3201/eid2606.191431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Poglazov A.B., Shliapnikova O.V., Prilipov A.G. Characteristic of the new Khatanga virus genotype. Vestn. Ross. Akad. Med. Nauk. 2011;5:45–49. [PubMed] [Google Scholar]
- 155.Lavrent’ev M.V., Prilipov A.G., L’vov S.D., L’vov D.K. Phylogenetic analysis of the nucleotide sequences of Chatanga virus strains, the new representative of California encephalitis serocomplex, isolated in different regions of the Russian Federation. Vopr. Virusol. 2008;53:25–29. [PubMed] [Google Scholar]
- 156.Francy D.B., Jaenson T.G., Lundström J.O., Schildt E.B., Espmark A., Henriksson B., Niklasson B. Ecologic Studies of Mosquitoes and Birds as Hosts of Ockelbo Virus in Sweden and Isolation of Inkoo and Batai Viruses from Mosquitoes. Am. J. Trop. Med. Hyg. 1989;41:355–363. doi: 10.4269/ajtmh.1989.41.355. [DOI] [PubMed] [Google Scholar]
- 157.Butenko A.M., Vladimirtseva E.A., Lvov S.D., Calisher C.H., Karabatsos N. California Serogroup Viruses from Mosquitoes Collected in the USSR. Am. J. Trop. Med. Hyg. 1991;45:366–370. doi: 10.4269/ajtmh.1991.45.366. [DOI] [PubMed] [Google Scholar]
- 158.Traavik T., Mehl R., Wiger R. California encephalitis group viruses isolated from mosquitoes collected in Southern and Arctic Norway. Acta Pathol. Microbiol. Scand. Sect. B Microbiol. 2009;86:335–342. doi: 10.1111/j.1699-0463.1978.tb00053.x. [DOI] [PubMed] [Google Scholar]
- 159.Demikhov V.G. Outcomes and prognosis of diseases caused by Inkoo and Tahyna viruses. Vopr. Virusol. 1995;40:72–74. [PubMed] [Google Scholar]
- 160.Li W., Cao Y., Fu S., Wang J., Li M., Jiang S., Wang X., Xing S., Feng L., Wang Z., et al. Tahyna Virus Infection, a Neglected Arboviral Disease in the Qinghai-Tibet Plateau of China. Vector-Borne Zoonotic Dis. 2014;14:353–357. doi: 10.1089/vbz.2013.1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Mravcová K., Camp J.V., Hubálek Z., Šikutová S., Vaux A.G.C., Medlock J.M., Rudolf I. Ťahyňa Virus—A Widespread, but Neglected Mosquito-borne Virus in Europe. Zoonoses Public Health. 2023;70:371–382. doi: 10.1111/zph.13042. [DOI] [PubMed] [Google Scholar]
- 162.Pilaski J., Mackenstein H. Isolation of Tahyna virus from mosquitoes in 2 different European natural foci. Zentralbl Bakteriol. Mikrobiol. Hyg. B. 1985;180:394–420. [PubMed] [Google Scholar]
- 163.Bárdos V. The Role of Mammals in the Circulation of Tahyna Virus. Folia Parasitol. 1975;22:257–264. [PubMed] [Google Scholar]
- 164.Chastel C., Bach-Hamba D., Launay H., Le Lay G., Hellal H., Beaucournu J.C. Arbovirus infections in Tunisia: New serological survey of small wild mammals. Bull. Soc. Pathol. Exot. Fil. 1983;76:21–33. [PubMed] [Google Scholar]
- 165.Demikhov V.G., Chaĭtsev V.G. Neurologic characteristics of diseases caused by Inkoo and Tahyna viruses. Vopr. Virusol. 1995;40:21–25. [PubMed] [Google Scholar]
- 166.Sluka F. Recognition of clinical forms of Valtice fever, a new arbovirus infection. Wien. Med. Wochenschr. 1969;119:765–769. [PubMed] [Google Scholar]
- 167.da Rosa J.F.T., de Souza W.M., de Paula Pinheiro F., Figueiredo M.L., Cardoso J.F., Acrani G.O., Nunes M.R.T. Oropouche Virus: Clinical, Epidemiological, and Molecular Aspects of a Neglected Orthobunyavirus. Am. J. Trop. Med. Hyg. 2017;96:1019–1030. doi: 10.4269/ajtmh.16-0672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.de Souza Bastos M., Pivoto João G., Naveca F.G., Monte R.L., Bastos M.d.S., Ramasawmy R., Mourão M.P.G., Lessa N., de Lima Gimaque J.B., Figueiredo L.T.M. Identification of Oropouche Orthobunyavirus in the Cerebrospinal Fluid of Three Patients in the Amazonas, Brazil. Am. J. Trop. Med. Hyg. 2012;86:732–735. doi: 10.4269/ajtmh.2012.11-0485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Aguilar P.V., Vargas J., Beingolea L., Kochel T.J., Guevara C., Watts D.M., Tesh R.B., Cruz C., Rocha C., Suarez V., et al. Guaroa Virus Infection among Humans in Bolivia and Peru. Am. J. Trop. Med. Hyg. 2010;83:714–721. doi: 10.4269/ajtmh.2010.10-0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Dias H.G., dos Santos F.B., Pauvolid-Corrêa A. An Overview of Neglected Orthobunyaviruses in Brazil. Viruses. 2022;14:987. doi: 10.3390/v14050987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Pinheiro F.P., Rocha A.G., Freitas R.B., Ohana B.A., Travassos da Rosa A.P., Rogério J.S., Linhares A.C. Meningitis associated with Oropouche virus infections. Rev. Inst. Med. Trop. Sao Paulo. 1982;24:246–251. [PubMed] [Google Scholar]
- 172.Pachler K., Růžek D., Nowotny N. Molecular Characterization of the African Orthobunyavirus Ilesha Virus. Infect. Genet. Evol. 2013;20:124–130. doi: 10.1016/j.meegid.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 173.Edridge A.W.D., van den Brekel N., Mukungu P., Nakayima R., Bbosa S., Isagara P., van Boele Hensbroek M., van der Hoek L., Kayiwa J., Lutwama J.J., et al. No Evidence of Ntwetwe Virus Infections in Children Presenting to Kiboga Hospital, Uganda. Trop. Med. Infect. Dis. 2022;8:21. doi: 10.3390/tropicalmed8010021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Pérot P., Bielle F., Bigot T., Foulongne V., Bolloré K., Chrétien D., Gil P., Gutiérrez S., L’Ambert G., Mokhtari K., et al. Identification of Umbre Orthobunyavirus as a Novel Zoonotic Virus Responsible for Lethal Encephalitis in 2 French Patients with Hypogammaglobulinemia. Clin. Infect. Dis. 2021;72:1701–1708. doi: 10.1093/cid/ciaa308. [DOI] [PubMed] [Google Scholar]
- 175.Balenghien T., Cardinale E., Chevalier V., Elissa N., Failloux A.-B., Jean Jose Nipomichene T.N., Nicolas G., Rakotoharinome V.M., Roger M., Zumbo B. Towards a Better Understanding of Rift Valley Fever Epidemiology in the South-West of the Indian Ocean. Vet. Res. 2013;44:78. doi: 10.1186/1297-9716-44-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Peyrefitte C.N., Devetakov I., Pastorino B., Villeneuve L., Bessaud M., Stolidi P., Depaquit J., Segura L., Gravier P., Tock F., et al. Toscana Virus and Acute Meningitis, France. Emerg. Infect. Dis. 2005;11:778–780. doi: 10.3201/eid1105.041122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Baldelli F., Grazia Ciufolini M., Francisci D., Marchi A., Venturi G., Fiorentini C., Laura Luchetta M., Bruto L., Pauluzzi S. Unusual Presentation of Life-Threatening Toscana Virus Meningoencephalitis. Clin. Infect. Dis. 2004;38:515–520. doi: 10.1086/381201. [DOI] [PubMed] [Google Scholar]
- 178.Gratz N.G. The Vector-Borne Human Infections of Europe: Their Distribution and Burden on Public Health/by Norman G. Gratz. World Health Organization, Regional Office for Europe; Geneva, Switzerland: 2004. [Google Scholar]
- 179.Menghani S., Chikhale R., Raval A., Wadibhasme P., Khedekar P. Chandipura Virus: An Emerging Tropical Pathogen. Acta Trop. 2012;124:1–14. doi: 10.1016/j.actatropica.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 180.Liu H., Li M.-H., Zhai Y.-G., Meng W.-S., Sun X.-H., Cao Y.-X., Fu S.-H., Wang H.-Y., Xu L.-H., Tang Q., et al. Banna Virus, China, 1987–2007. Emerg. Infect. Dis. 2010;16:514–517. doi: 10.3201/eid1603.091160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Carrera J.-P., Forrester N., Wang E., Vittor A.Y., Haddow A.D., López-Vergès S., Abadía I., Castaño E., Sosa N., Báez C., et al. Eastern Equine Encephalitis in Latin America. N. Engl. J. Med. 2013;369:732–744. doi: 10.1056/NEJMoa1212628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.García M., Cisneros J., Carrera J.-P., Luciani K., Guerra I., Abadía I., Martínez-Torres A.O., Estripeaut D. Madariaga Virus Infection Associated with a Case of Acute Disseminated Encephalomyelitis. Am. J. Trop. Med. Hyg. 2015;92:1130–1132. doi: 10.4269/ajtmh.14-0845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Blohm G.M., Lednicky J.A., White S.K., Mavian C.N., Márquez M.C., González-García K.P., Salemi M., Morris J.G., Paniz-Mondolfi A.E. Madariaga Virus: Identification of a Lineage III Strain in a Venezuelan Child with Acute Undifferentiated Febrile Illness, in the Setting of a Possible Equine Epizootic. Clin. Infect. Dis. 2018;67:619–621. doi: 10.1093/cid/ciy224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Lednicky J.A., White S.K., Mavian C.N., El Badry M.A., Telisma T., Salemi M., OKech B.A., Beau De Rochars V.M., Morris J.G. Emergence of Madariaga Virus as a Cause of Acute Febrile Illness in Children, Haiti, 2015–2016. PLoS Negl. Trop. Dis. 2019;13:e0006972. doi: 10.1371/journal.pntd.0006972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Vosoughi R., Walkty A., Drebot M.A., Kadkhoda K. Jamestown Canyon Virus Meningoencephalitis Mimicking Migraine with Aura in a Resident of Manitoba. CMAJ. 2018;190:E262–E264. doi: 10.1503/cmaj.170940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Fagre A.C., Lyons S., Staples J.E., Lindsey N. West Nile Virus and Other Nationally Notifiable Arboviral Diseases—United States, 2021. MMWR Morb. Mortal. Wkly. Rep. 2023;72:901–906. doi: 10.15585/mmwr.mm7234a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.van Niekerk S., Human S., Williams J., van Wilpe E., Pretorius M., Swanepoel R., Venter M. Sindbis and Middelburg Old World Alphaviruses Associated with Neurologic Disease in Horses, South Africa. Emerg. Infect. Dis. 2015;21:2225–2229. doi: 10.3201/eid2112.150132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Fourie I., Williams J., Ismail A., Jansen van Vuren P., Stoltz A., Venter M. Detection and Genome Characterization of Middelburg Virus Strains Isolated from CSF and Whole Blood Samples of Humans with Neurological Manifestations in South Africa. PLoS Negl. Trop. Dis. 2022;16:e0010020. doi: 10.1371/journal.pntd.0010020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Lucas R.E., Qiao M. A Case of Encephalitis in Central Australia Due to Ross River Virus? Aust. N. Z. J. Med. 1999;29:268–270. doi: 10.1111/j.1445-5994.1999.tb00695.x. [DOI] [PubMed] [Google Scholar]
- 190.Harley D., Sleigh A., Ritchie S. Ross River Virus Transmission, Infection, and Disease: A Cross-Disciplinary Review. Clin. Microbiol. Rev. 2001;14:909–932. doi: 10.1128/CMR.14.4.909-932.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Lednicky J.A., White S.K., Stephenson C.J., Cherabuddi K., Loeb J.C., Moussatche N., Lednicky A., Morris J.G. Keystone Virus Isolated From a Florida Teenager with Rash and Subjective Fever: Another Endemic Arbovirus in the Southeastern United States? Clin. Infect. Dis. 2019;68:143–145. doi: 10.1093/cid/ciy485. [DOI] [PubMed] [Google Scholar]
- 192.Azar S.R., Campos R.K., Bergren N.A., Camargos V.N., Rossi S.L. Epidemic Alphaviruses: Ecology, Emergence and Outbreaks. Microorganisms. 2020;8:1167. doi: 10.3390/microorganisms8081167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Hommel D., Heraud J.M., Hulin A., Talarmin A. Association of Tonate Virus (Subtype IIIB of the Venezuelan Equine Encephalitis Complex) with Encephalitis in a Human. Clin. Infect. Dis. 2000;30:188–190. doi: 10.1086/313611. [DOI] [PubMed] [Google Scholar]
- 194.Coimbra T.L.M., Nassar E.S., Nagamori A.H., Ferreira I.E., Pereira L.E., Rocco I.M., Ueda-Ito M., Romano N.S. Iguape: A Newly Recognized Flavivirus from São Paulo State, Brazil. Intervirology. 1993;36:144–152. doi: 10.1159/000150333. [DOI] [PubMed] [Google Scholar]
- 195.Trivedi S., Chakravarty A. Neurological Complications of Dengue Fever. Curr. Neurol. Neurosci. Rep. 2022;22:515–529. doi: 10.1007/s11910-022-01213-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Li G.-H., Ning Z.-J., Liu Y.-M., Li X.-H. Neurological Manifestations of Dengue Infection. Front. Cell. Infect. Microbiol. 2017;7:449. doi: 10.3389/fcimb.2017.00449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Withana M., Rodrigo C., Chang T., Karunanayake P., Rajapakse S. Dengue Fever Presenting with Acute Cerebellitis: A Case Report. BMC Res. Notes. 2014;7:125. doi: 10.1186/1756-0500-7-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Osnaya-Romero N., Perez-Guille M.-G., Andrade-García S., Gonzalez-Vargas E., Borgaro-Payro R., Villagomez-Martinez S., de Jesús Ortega-Maldonado J., Arredondo-García J.L. Neurological Complications and Death in Children with Dengue Virus Infection: Report of Two Cases. J. Venom. Anim. Toxins Incl. Trop. Dis. 2017;23:25. doi: 10.1186/s40409-017-0115-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Murugesan A., Manoharan M. Dengue Virus. Emerg. Reemerging Viral Pathog. 2020;1:281–359. doi: 10.1016/B978-0-12-819400-3.00016-8. [DOI] [Google Scholar]
- 200.Kok B.H., Lim H.T., Lim C.P., Lai N.S., Leow C.Y., Leow C.H. Dengue Virus Infection—A Review of Pathogenesis, Vaccines, Diagnosis and Therapy. Virus Res. 2022;324:199018. doi: 10.1016/j.virusres.2022.199018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Singh S., Alallah J., Amrit A., Maheshwari A., Boppana S. Neurological Manifestations of Perinatal Dengue. Newborn. 2023;2:158–172. doi: 10.5005/jp-journals-11002-0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Gainor E.M., Harris E., LaBeaud A.D. Uncovering the Burden of Dengue in Africa: Considerations on Magnitude, Misdiagnosis, and Ancestry. Viruses. 2022;14:233. doi: 10.3390/v14020233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Saivish M.V., Gomes da Costa V., de Lima Menezes G., Alves da Silva R., Dutra da Silva G.C., Moreli M.L., Sacchetto L., Pacca C.C., Vasilakis N., Nogueira M.L. Rocio Virus: An Updated View on an Elusive Flavivirus. Viruses. 2021;13:2293. doi: 10.3390/v13112293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Auerswald H., Maquart P.-O., Chevalier V., Boyer S. Mosquito Vector Competence for Japanese Encephalitis Virus. Viruses. 2021;13:1154. doi: 10.3390/v13061154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Mulvey P., Duong V., Boyer S., Burgess G., Williams D.T., Dussart P., Horwood P.F. The Ecology and Evolution of Japanese Encephalitis Virus. Pathogens. 2021;10:1534. doi: 10.3390/pathogens10121534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Pommier J.D., Gorman C., Crabol Y., Bleakley K., Sothy H., Santy K., Tran H.T.T., Nguyen L.V., Bunnakea E., Hlaing C.S., et al. Childhood Encephalitis in the Greater Mekong Region (the SouthEast Asia Encephalitis Project): A Multicentre Prospective Study. Lancet Glob. Health. 2022;10:e989–e1002. doi: 10.1016/S2214-109X(22)00174-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Kumar S., Verma A., Yadav P., Dubey S.K., Azhar E.I., Maitra S.S., Dwivedi V.D. Molecular Pathogenesis of Japanese Encephalitis and Possible Therapeutic Strategies. Arch. Virol. 2022;167:1739–1762. doi: 10.1007/s00705-022-05481-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Rajaiah P., Kumar A. Japanese Encephalitis Virus in India: An Update on Virus Genotypes. Indian J. Med. Res. 2022;156:588–597. doi: 10.4103/ijmr.IJMR_2606_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Chowdhury P., Khan S.A. Global Emergence of West Nile Virus: Threat & Preparedness in Special Perspective to India. Indian J. Med. Res. 2021;154:36–50. doi: 10.4103/ijmr.IJMR_642_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Hayes E.B., Komar N., Nasci R.S., Montgomery S.P., O’Leary D.R., Campbell G.L. Epidemiology and Transmission Dynamics of West Nile Virus Disease. Emerg. Infect. Dis. 2005;11:1167–1173. doi: 10.3201/eid1108.050289a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Antoniou E., Orovou E., Sarella A., Iliadou M., Rigas N., Palaska E., Iatrakis G., Dagla M. Zika Virus and the Risk of Developing Microcephaly in Infants: A Systematic Review. IJERPH. 2020;17:3806. doi: 10.3390/ijerph17113806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Combarnous Y., Guillou F., Martinat N. Functional States of the Luteinizing Hormone/Choriogonadotropin-Receptor Complex in Rat Leydig Cells. J. Biol. Chem. 1986;261:6868–6871. doi: 10.1016/S0021-9258(19)62696-7. [DOI] [PubMed] [Google Scholar]
- 213.Schneider E.F., Robich R.M., Elias S.P., Lubelczyk C.B., Cosenza D.S., Smith R.P. Jamestown Canyon Virus in Collected Mosquitoes, Maine, United States, 2017–2019. Emerg. Infect. Dis. 2022;28:2330–2333. doi: 10.3201/eid2811.212382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Weiler N.S., Niendorf E., Dumic I. Two Insects, Two Bites, One Patient: A Lyme Disease and Jamestown Canyon Co-Infection. Cureus. 2023;15:e40222. doi: 10.7759/cureus.40222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Henry C.J., Pillai A.N., Lednicky J.A., Morris J.G., Hladish T.J. Ecology and Public Health Burden of Keystone Virus in Florida. Epidemics. 2022;39:100555. doi: 10.1016/j.epidem.2022.100555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Artsob H., Spence L. Imported Arbovirus Infections in Canada 1974-89. Can. J. Infect. Dis. 1991;2:95–100. doi: 10.1155/1991/678906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Gaensbauer J.T., Lindsey N.P., Messacar K., Staples J.E., Fischer M. Neuroinvasive Arboviral Disease in the United States: 2003 to 2012. Pediatrics. 2014;134:e642–e650. doi: 10.1542/peds.2014-0498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Carson P.K., Holloway K., Dimitrova K., Rogers L., Chaulk A.C., Lang A.S., Whitney H.G., Drebot M.A., Chapman T.W. The Seasonal Timing of Snowshoe Hare Virus Transmission on the Island of Newfoundland, Canada. J. Med. Entomol. 2017;54:712–718. doi: 10.1093/jme/tjw219. [DOI] [PubMed] [Google Scholar]
- 219.Drebot M. Emerging Mosquito-Borne Bunyaviruses in Canada. CCDR. 2015;41:117–123. doi: 10.14745/ccdr.v41i06a01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.May L.P., Watts S.L., Maruniak J.E. Molecular Survey for Mosquito-Transmitted Viruses: Detection of Tensaw Virus in North Central Florida Mosquito Populations. J. Am. Mosq. Control Assoc. 2014;30:61–64. doi: 10.2987/13-6361.1. [DOI] [PubMed] [Google Scholar]
- 221.Xia H., Liu H., Zhao L., Atoni E., Wang Y., Yuan Z. First Isolation and Characterization of a Group C Banna Virus (BAV) from Anopheles Sinensis Mosquitoes in Hubei, China. Viruses. 2018;10:555. doi: 10.3390/v10100555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Liu H., Gao X.-Y., Fu S.-H., Li M.-H., Zhai Y.-G., Meng W.-S., Sun X.-H., Lv Z., Wang H.-Y., Shen X.-X., et al. Molecular Evolution of Emerging Banna Virus. Infect. Genet. Evol. 2016;45:250–255. doi: 10.1016/j.meegid.2016.08.034. [DOI] [PubMed] [Google Scholar]
- 223.Chinedu Eneh S., Uwishema O., Nazir A., El Jurdi E., Faith Olanrewaju O., Abbass Z., Mustapha Jolayemi M., Mina N., Kseiry L., Onyeaka H. Chikungunya Outbreak in Africa: A Review of the Literature. Ann. Med. Surg. 2023;85:3545–3552. doi: 10.1097/MS9.0000000000000979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Hughes H.R., Velez J.O., Davis E.H., Laven J., Gould C.V., Panella A.J., Lambert A.J., Staples J.E., Brault A.C. Fatal Human Infection with Evidence of Intrahost Variation of Eastern Equine Encephalitis Virus, Alabama, USA, 2019. Emerg. Infect. Dis. 2021;27:1886–1892. doi: 10.3201/eid2707.210315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Heberlein-Larson L.A., Tan Y., Stark L.M., Cannons A.C., Shilts M.H., Unnasch T.R., Das S.R. Complex Epidemiological Dynamics of Eastern Equine Encephalitis Virus in Florida. Am. J. Trop. Med. Hyg. 2019;100:1266–1274. doi: 10.4269/ajtmh.18-0783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Armstrong P.M., Andreadis T.G. Eastern Equine Encephalitis Virus in Mosquitoes and Their Role as Bridge Vectors. Emerg. Infect. Dis. 2010;16:1869–1874. doi: 10.3201/eid1612.100640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Diagne C.T., Bengue M., Choumet V., Hamel R., Pompon J., Missé D. Mayaro Virus Pathogenesis and Transmission Mechanisms. Pathogens. 2020;9:738. doi: 10.3390/pathogens9090738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Acosta-Ampudia Y., Monsalve D.M., Rodríguez Y., Pacheco Y., Anaya J.-M., Ramírez-Santana C. Mayaro: An Emerging Viral Threat? Emerg. Microbes Infect. 2018;7:163. doi: 10.1038/s41426-018-0163-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Adouchief S., Smura T., Sane J., Vapalahti O., Kurkela S. Sindbis Virus as a Human Pathogen-Epidemiology, Clinical Picture and Pathogenesis: Sindbis Virus as a Human Pathogen. Rev. Med. Virol. 2016;26:221–241. doi: 10.1002/rmv.1876. [DOI] [PubMed] [Google Scholar]
- 230.Meno K., Yah C., Mendes A., Venter M. Incidence of Sindbis Virus in Hospitalized Patients with Acute Fevers of Unknown Cause in South Africa, 2019–2020. Front. Microbiol. 2022;12:798810. doi: 10.3389/fmicb.2021.798810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Guzmán-Terán C., Calderón-Rangel A., Rodriguez-Morales A., Mattar S. Venezuelan Equine Encephalitis Virus: The Problem Is Not over for Tropical America. Ann. Clin. Microbiol. Antimicrob. 2020;19:19. doi: 10.1186/s12941-020-00360-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Aguilar P.V., Estrada-Franco J.G., Navarro-Lopez R., Ferro C., Haddow A.D., Weaver S.C. Endemic Venezuelan Equine Encephalitis in the Americas: Hidden under the Dengue Umbrella. Future Virol. 2011;6:721–740. doi: 10.2217/fvl.11.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Zacks M.A., Paessler S. Encephalitic Alphaviruses. Vet. Microbiol. 2010;140:281–286. doi: 10.1016/j.vetmic.2009.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Contigiani M.S., Diaz L.A., Spinsanti L.I. General Aspects on Arboviruses. In: Marcondes C.B., editor. Arthropod Borne Diseases. Springer International Publishing; Cham, Switzerland: 2017. pp. 61–71. [Google Scholar]
- 235.Asante J., Noreddin A., El Zowalaty M. Systematic Review of Important Bacterial Zoonoses in Africa in the Last Decade in Light of the ‘One Health’ Concept. Pathogens. 2019;8:50. doi: 10.3390/pathogens8020050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Venkatesan G., Balamuruga V., Gandhale P.N., Singh R.K., Bhanupraka V. Viral Zoonosis: A Comprehensive Review. Asian J. Anim. Vet. Adv. 2010;5:77–92. doi: 10.3923/ajava.2010.77.92. [DOI] [Google Scholar]
- 237.Rahman M.T., Sobur M.A., Islam M.S., Ievy S., Hossain M.J., El Zowalaty M.E., Rahman A.T., Ashour H.M. Zoonotic Diseases: Etiology, Impact, and Control. Microorganisms. 2020;8:1405. doi: 10.3390/microorganisms8091405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Dharmarajan G., Li R., Chanda E., Dean K.R., Dirzo R., Jakobsen K.S., Khan I., Leirs H., Shi Z.-L., Wolfe N.D., et al. The Animal Origin of Major Human Infectious Diseases: What Can Past Epidemics Teach Us About Preventing the Next Pandemic? Zoonoses. 2022;2 doi: 10.15212/ZOONOSES-2021-0028. [DOI] [Google Scholar]
- 239.Tapia-Ramírez G., Lorenzo C., Navarrete D., Carrillo-Reyes A., Retana Ó., Carrasco-Hernández R. A Review of Mammarenaviruses and Rodent Reservoirs in the Americas. EcoHealth. 2022;19:22–39. doi: 10.1007/s10393-022-01580-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Bedi J.S., Vijay D., Dhaka P. Textbook of Zoonoses. Wiley-Blackwell; Hoboken, NJ, USA: 2022. [Google Scholar]
- 241.Koyuncu O.O., Hogue I.B., Enquist L.W. Virus Infections in the Nervous System. Cell Host Microbe. 2013;13:379–393. doi: 10.1016/j.chom.2013.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Sakabe S., Cubitt B., Martinez-Sobrido L., de la Torre J.C. Molecular Engineering of a Mammarenavirus with Unbreachable Attenuation. J. Virol. 2023;97:e01385-22. doi: 10.1128/jvi.01385-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Hallam S.J., Koma T., Maruyama J., Paessler S. Review of Mammarenavirus Biology and Replication. Front. Microbiol. 2018;9:1751. doi: 10.3389/fmicb.2018.01751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Radoshitzky S.R., de la Torre J.C. Encyclopedia of Virology. Elsevier; New York, NY, USA: 2019. Human Pathogenic Arenaviruses (Arenaviridae) pp. 507–517. [Google Scholar]
- 245.Fornůsková A., Hiadlovská Z., Macholán M., Piálek J., de Bellocq J.G. New Perspective on the Geographic Distribution and Evolution of Lymphocytic Choriomeningitis Virus, Central Europe. Emerg. Infect. Dis. 2021;27:2638–2647. doi: 10.3201/eid2710.210224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Reuter G., Boros Á., Takáts K., Mátics R., Pankovics P. A Novel Mammarenavirus (Family Arenaviridae) in Hedgehogs (Erinaceus roumanicus) in Europe. Arch. Virol. 2023;168:174. doi: 10.1007/s00705-023-05804-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Tuppeny M. Viral Meningitis and Encephalitis. Crit. Care Nurs. Clin. N. Am. 2013;25:363–380. doi: 10.1016/j.ccell.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 248.Billioux B.J., Smith B., Nath A. Neurological Complications of Ebola Virus Infection. Neurotherapeutics. 2016;13:461–470. doi: 10.1007/s13311-016-0457-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Beltz L.A. Bats and Human Health: Ebola, SARS, Rabies and Beyond. John Wiley & Sons; Hoboken, NJ, USA: 2017. [Google Scholar]
- 250.Abir M.H., Rahman T., Das A., Etu S.N., Nafiz I.H., Rakib A., Mitra S., Emran T.B., Dhama K., Islam A., et al. Pathogenicity and Virulence of Marburg Virus. Virulence. 2022;13:609–633. doi: 10.1080/21505594.2022.2054760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Laenen L., Vergote V., Calisher C.H., Klempa B., Klingström J., Kuhn J.H., Maes P. Hantaviridae: Current Classification and Future Perspectives. Viruses. 2019;11:788. doi: 10.3390/v11090788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Jonsson C.B., Figueiredo L.T.M., Vapalahti O. A Global Perspective on Hantavirus Ecology, Epidemiology, and Disease. Clin. Microbiol. Rev. 2010;23:412–441. doi: 10.1128/CMR.00062-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Бернштейн А.Д., Гаврилoвская И.Н., Апекина Н.С., Дзагурoва Т.К., Ткаченкo Е.А. Осoбеннoсти Прирoднoй Очагoвoсти Хантавирусных Зooнoзoв. Эпидемиoлoгия и Вакцинoпрoфилактика. 2010;2:5–13. [Google Scholar]
- 254.Fawcett S.J., Chen J.S., Fawcett R.W. Acute Hantavirus Infection Presenting with Fever and Altered Mentation in the Absence of Pulmonary or Renal Manifestations. Open Forum Infect. Dis. 2022;9:ofac430. doi: 10.1093/ofid/ofac430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Sing A., editor. Zoonoses: Infections Affecting Humans and Animals; Focus on Public Health Aspects. Springer; Dordrecht, The Netherlands: 2015. [Google Scholar]
- 256.Monika N., Rohith M.G., Ravi K., Kandagal S.A. Clinical Profile and Outcome of Patients with Meningoencephalitis in a Tertiary Care Hospital. Int. J. Res. Med. Sci. 2023;11:1012–1018. doi: 10.18203/2320-6012.ijrms20230591. [DOI] [Google Scholar]
- 257.Talamonti L., Padula P.J., Canteli M.S., Posner F., Marczeski F.P., Weller C. Hantavirus Pulmonary Syndrome: Encephalitis Caused by Virus Andes. J. Neurovirol. 2011;17:189–192. doi: 10.1007/s13365-010-0011-4. [DOI] [PubMed] [Google Scholar]
- 258.Cerar D., Avšič-Županc T., Jereb M., Strle F. Case Report: Severe Neurological Manifestation of Dobrava Hantavirus Infection. J. Med. Virol. 2007;79:1841–1843. doi: 10.1002/jmv.21021. [DOI] [PubMed] [Google Scholar]
- 259.Bergmann F., Krone B., Bleich S., Prange H., Paulus W. Encephalitis Due to a Hantavirus Infection. J. Infect. 2002;45:58–59. doi: 10.1053/jinf.2002.1014. [DOI] [PubMed] [Google Scholar]
- 260.Hautala N., Partanen T., Kubin A.-M., Kauma H., Hautala T. Central Nervous System and Ocular Manifestations in Puumala Hantavirus Infection. Viruses. 2021;13:1040. doi: 10.3390/v13061040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Huisa B.N., Chapin J.E., Adair J.C. Central Nervous System Complications Following Hanta Virus Cardiopulmonary Syndrome. J. Neurovirol. 2009;15:202–205. doi: 10.1080/13550280802491485. [DOI] [PubMed] [Google Scholar]
- 262.Liu E., Lv S., Yi P., Feng L., Deng X., Xia H., Xu Y. Central Nervous System Infection with Seoul Orthohantavirus in a Child after Hematopoietic Stem Cell Transplantation: A Case Report. Virol. J. 2022;19:75. doi: 10.1186/s12985-022-01766-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Malik Y.S., Singh R.K., Dhama K., editors. Animal-Origin Viral Zoonoses. Springer; Singapore: 2020. Livestock Diseases and Management. [Google Scholar]
- 264.Quarleri J., Galvan V., Delpino M.V. Henipaviruses: An Expanding Global Public Health Concern? GeroScience. 2022;44:2447–2459. doi: 10.1007/s11357-022-00670-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Billioux B.J., Mbaya O.T., Sejvar J., Nath A. Neurologic Complications of Smallpox and Monkeypox: A Review. JAMA Neurol. 2022;79:1180. doi: 10.1001/jamaneurol.2022.3491. [DOI] [PubMed] [Google Scholar]
- 266.Banyard A., Evans J., Luo T., Fooks A. Lyssaviruses and Bats: Emergence and Zoonotic Threat. Viruses. 2014;6:2974–2990. doi: 10.3390/v6082974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Paweska J.T., Blumberg L.H., Liebenberg C., Hewlett R.H., Grobbelaar A.A., Leman P.A., Croft J.E., Nel L.H., Nutt L., Swanepoel R. Fatal Human Infection with Rabies-Related Duvenhage Virus, South Africa. Emerg. Infect. Dis. 2006;12:1965–1967. doi: 10.3201/eid1212.060764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.van Thiel P.-P.A.M., de Bie R.M.A., Eftimov F., Tepaske R., Zaaijer H.L., van Doornum G.J.J., Schutten M., Osterhaus A.D.M.E., Majoie C.B.L.M., Aronica E., et al. Fatal Human Rabies Due to Duvenhage Virus from a Bat in Kenya: Failure of Treatment with Coma-Induction, Ketamine, and Antiviral Drugs. PLoS Negl. Trop. Dis. 2009;3:e428. doi: 10.1371/journal.pntd.0000428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Shipley R., Wright E., Selden D., Wu G., Aegerter J., Fooks A.R., Banyard A.C. Bats and Viruses: Emergence of Novel Lyssaviruses and Association of Bats with Viral Zoonoses in the EU. Trop. Med. Infect. Dis. 2019;4:31. doi: 10.3390/tropicalmed4010031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Hanna J.N., Carney I.K., Deverill J.E., Botha J.A., Smith G.A., Serafin I.L., Harrower B.J., Tannenberg A.E.G., Fitzpatrick P.F., Searle J.W. Australian Bat Lyssavirus Infection: A Second Human Case, with a Long Incubation Period. Med. J. Aust. 2000;172:597–599. doi: 10.5694/j.1326-5377.2000.tb124126.x. [DOI] [PubMed] [Google Scholar]
- 271.Nathwani D., McIntyre P.G., White K., Shearer A.J., Reynolds N., Walker D., Orange G.V., Fooks A.R. Fatal Human Rabies Caused by European Bat Lyssavirus Type 2a Infection in Scotland. Clin. Infect. Dis. 2003;37:598–601. doi: 10.1086/376641. [DOI] [PubMed] [Google Scholar]
- 272.Irani D.N. Aseptic Meningitis and Viral Myelitis. Neurol. Clin. 2008;26:635–655. doi: 10.1016/j.ncl.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Logan S.A.E., MacMahon E. Viral Meningitis. BMJ. 2008;336:36–40. doi: 10.1136/bmj.39409.673657.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Fakhri S., Mohammadi Pour P., Piri S., Farzaei M.H., Echeverría J. Modulating Neurological Complications of Emerging Infectious Diseases: Mechanistic Approaches to Candidate Phytochemicals. Front. Pharmacol. 2021;12:742146. doi: 10.3389/fphar.2021.742146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Guidance Ebola: Overview, History, Origins and Transmission GOV.UK; UK Health Security Agency 2023. [(accessed on 7 May 2024)]; Available online: https://www.gov.uk/government/publications/ebola-origins-reservoirs-transmission-and-guidelines/ebola-overview-history-origins-and-transmission.
- 276.History of Ebola Disease Outbreaks CDC. [(accessed on 7 May 2024)];2023 Available online: https://www.cdc.gov/vhf/ebola/history/chronology.html.
- 277.Reuben R.C., Abunike S.A. Marburg Virus Disease: The Paradox of Nigeria’s Preparedness and Priority Effects in Co-Epidemics. Bull. Natl. Res. Cent. 2023;47:10. doi: 10.1186/s42269-023-00987-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Ferrés M., Martínez-Valdebenito C., Angulo J., Henríquez C., Vera-Otárola J., Vergara M.J., Pérez J., Fernández J., Sotomayor V., Valdés M.F., et al. Mother-to-Child Transmission of Andes Virus through Breast Milk, Chile1. Emerg. Infect. Dis. 2020;26:1885–1888. doi: 10.3201/eid2608.200204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Larsen B.B., Gryseels S., Otto H.W., Worobey M. Evolution and Diversity of Bat and Rodent Paramyxoviruses from North America. J. Virol. 2022;96:e01098-21. doi: 10.1128/jvi.01098-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Martinez-Valdebenito C., Calvo M., Vial C., Mansilla R., Marco C., Palma R.E., Vial P.A., Valdivieso F., Mertz G., Ferrés M. Person-to-Person Household and Nosocomial Transmission of Andes Hantavirus, Southern Chile, 2011. Emerg. Infect. Dis. 2014;20:1637–1644. doi: 10.3201/eid2010.140353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Papa A. Dobrava-Belgrade Virus: Phylogeny, Epidemiology, Disease. Antivir. Res. 2012;95:104–117. doi: 10.1016/j.antiviral.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 282.Lvov D.K., Shchelkanov M.Y., Alkhovsky S.V., Deryabin P.G. Zoonotic Viruses in Northern Eurasia. Elsevier; New York, NY, USA: 2015. Introduction; pp. 3–15. [Google Scholar]
- 283.Steiner T., Ettinger J., Peng Z., Hofmann J., Hartmann M., Burkhardt U., Schnitzler P. Hyperintense Lesion in the Corpus Callosum Associated with Puumala Hantavirus Infection. J. Neurol. 2012;259:1742–1745. doi: 10.1007/s00415-012-6437-2. [DOI] [PubMed] [Google Scholar]
- 284.Marsh G.A., Netter H.J. Henipavirus Infection: Natural History and the Virus-Host Interplay. Curr. Treat. Options Infect. Dis. 2018;10:197–216. doi: 10.1007/s40506-018-0155-y. [DOI] [Google Scholar]
- 285.Clayton B.A., Wang L.F., Marsh G.A. Henipaviruses: An Updated Review Focusing on the Pteropid Reservoir and Features of Transmission: Henipaviruses: The Pteropid Reservoir and Features of Transmission. Zoonoses Public Health. 2013;60:69–83. doi: 10.1111/j.1863-2378.2012.01501.x. [DOI] [PubMed] [Google Scholar]
- 286.Calderon A., Guzman C., Salazar-Bravo J., Figueiredo L.T., Mattar S. Viral Zoonoses That Fly with Bats: A Review. MANTER J. Parasite Biodivers. 2016. [DOI]
- 287.Wong K.T., Robertson T., Ong B.B., Chong J.W., Yaiw K.C., Wang L.F., Ansford A.J., Tannenberg A. Human Hendra Virus Infection Causes Acute and Relapsing Encephalitis. Neuropathol. Appl. Neurobiol. 2009;35:296–305. doi: 10.1111/j.1365-2990.2008.00991.x. [DOI] [PubMed] [Google Scholar]
- 288.Ong K.C., Wong K.T. Henipavirus Encephalitis: Recent Developments and Advances: Update on Henipavirus Encephalitis. Brain Pathol. 2015;25:605–613. doi: 10.1111/bpa.12278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Alam A.M. Nipah Virus, an Emerging Zoonotic Disease Causing Fatal Encephalitis. Clin. Med. 2022;22:348–352. doi: 10.7861/clinmed.2022-0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Ang B.S.P., Lim T.C.C., Wang L. Nipah Virus Infection. J. Clin. Microbiol. 2018;56:e01875-17. doi: 10.1128/JCM.01875-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Sepehrinezhad A., Ashayeri Ahmadabad R., Sahab-Negah S. Monkeypox Virus from Neurological Complications to Neuroinvasive Properties: Current Status and Future Perspectives. J. Neurol. 2023;270:101–108. doi: 10.1007/s00415-022-11339-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Money K.M., Barnett T.A., Rapaka S., Osborn R., Kitani T., Fuguet D., Amjad F., Clark J.R., Chakravarty D., Copeland M.J., et al. Monkeypox-Associated Central Nervous System Disease: A Case Series and Review. Ann. Neurol. 2023;93:893–905. doi: 10.1002/ana.26597. [DOI] [PubMed] [Google Scholar]
- 293.Pastula D.M., Copeland M.J., Hannan M.C., Rapaka S., Kitani T., Kleiner E., Showler A., Yuen C., Ferriman E.M., House J., et al. Two Cases of Monkeypox-Associated Encephalomyelitis—Colorado and the District of Columbia, July–August 2022. MMWR Morb. Mortal. Wkly. Rep. 2022;71:1212–1215. doi: 10.15585/mmwr.mm7138e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Banyard A.C., Hayman D., Johnson N., McElhinney L., Fooks A.R. Advances in Virus Research. Volume 79. Elsevier; New York, NY, USA: 2011. Bats and Lyssaviruses; pp. 239–289. [DOI] [PubMed] [Google Scholar]
- 295.Francis J.R., McCall B.J., Hutchinson P., Powell J., Vaska V.L., Nourse C. Australian Bat Lyssavirus: Implications for Public Health. Med. J. Aust. 2014;201:647–649. doi: 10.5694/mja13.00261. [DOI] [PubMed] [Google Scholar]
- 296.Kohl C., Kurth A. European Bats as Carriers of Viruses with Zoonotic Potential. Viruses. 2014;6:3110–3128. doi: 10.3390/v6083110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Poleshchuk E.M., Tagakova D.N., Sidorov G.N., Orlova T.S., Gordeiko N.S., Kaisarov A.Z. Lethal Cases of Lyssavirus Encephalitis in Humans after Contact with Bats in the Russian Far East in 2019–2021. Probl. Virol. 2023;68:45–58. doi: 10.36233/0507-4088-156. [DOI] [PubMed] [Google Scholar]
- 298.Leonova G.N., Somova L.M., Belikov S.I., Kondratov I.G., Plekhova N.G., Krylova N.V., Pavlenko E.V., Tiunov M.P., Thachev S.E. The Fatal Case of Lyssavirus Encephalitis in the Russian Far East. In: Tkachev S., editor. Encephalitis. InTech; London, UK: 2013. [Google Scholar]
- 299.Kgaladi J., Wright N., Coertse J., Markotter W., Marston D., Fooks A.R., Freuling C.M., Müller T.F., Sabeta C.T., Nel L.H. Diversity and Epidemiology of Mokola Virus. PLoS Neglected Trop. Dis. 2013;7:e2511. doi: 10.1371/journal.pntd.0002511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Le Govic Y., Demey B., Cassereau J., Bahn Y.-S., Papon N. Pathogens Infecting the Central Nervous System. PLoS Pathog. 2022;18:e1010234. doi: 10.1371/journal.ppat.1010234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Johnson N., Aréchiga-Ceballos N., Aguilar-Setien A. Vampire Bat Rabies: Ecology, Epidemiology and Control. Viruses. 2014;6:1911–1928. doi: 10.3390/v6051911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Fenner’s Veterinary Virology. Elsevier; New York, NY, USA: 2017. Rhabdoviridae; pp. 357–372. [Google Scholar]
- 303.Soler-Rangel S., Jiménez-Restrepo N., Nariño D., Rosselli D. Rabies Encephalitis and Extra-Neural Manifestations in a Patient Bitten by a Domestic Cat. Rev. Inst. Med. Trop. São Paulo. 2020;62:e1. doi: 10.1590/s1678-9946202062001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Lion T. Adenovirus Infections in Immunocompetent and Immunocompromised Patients. Clin. Microbiol. Rev. 2014;27:441–462. doi: 10.1128/CMR.00116-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Lynch J., Kajon A. Adenovirus: Epidemiology, Global Spread of Novel Serotypes, and Advances in Treatment and Prevention. Semin. Respir. Crit. Care Med. 2016;37:586–602. doi: 10.1055/s-0036-1584923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Khanal S., Ghimire P., Dhamoon A. The Repertoire of Adenovirus in Human Disease: The Innocuous to the Deadly. Biomedicines. 2018;6:30. doi: 10.3390/biomedicines6010030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Saint-Pierre Contreras G., Conei Valencia D., Lizama L., Vargas Zuñiga D., Avendaño Carvajal L.F., Ampuero Llanos S. An Old Acquaintance: Could Adenoviruses Be Our Next Pandemic Threat? Viruses. 2023;15:330. doi: 10.3390/v15020330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Tamiya M., Komatsu H., Hirabayashi M., Imura M., Hoshino H. Neonatal Meningoencephalitis Caused by Human Adenovirus Species F Infection. Pediatr. Int. 2019;61:99–101. doi: 10.1111/ped.13722. [DOI] [PubMed] [Google Scholar]
- 309.Zhao H., Liu Y., Feng Z., Feng Q., Li K., Gao H., Qian S., Xu L., Xie Z. A Fatal Case of Viral Sepsis and Encephalitis in a Child Caused by Human Adenovirus Type 7 Infection. Virol. J. 2022;19:154. doi: 10.1186/s12985-022-01886-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Robinson C.P., Busl K.M. Neurologic Manifestations of Severe Respiratory Viral Contagions. Crit. Care Explor. 2020;2:e0107. doi: 10.1097/CCE.0000000000000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Ivanova O.E., Yurashko O.V., Eremeeva T.P., Baikova O.Y., Morozova N.S., Lukashev A.N. Adenovirus Isolation Rates in Acute Flaccid Paralysis Patients. J. Med. Virol. 2012;84:75–80. doi: 10.1002/jmv.22265. [DOI] [PubMed] [Google Scholar]
- 312.Bosch A., Guix S., Krishna N.K., Méndez E., Monroe S.S., Pantin-Jackwood M., Schultz-Cherry S., Family: Astroviridae Chapter Version: ICTV Ninth Report. 2009 Taxonomy Release International Committee on Taxonomy of Viruses: ICTV. [(accessed on 7 May 2024)]. Available online: https://ictv.global/report_9th/RNApos/Astroviridae.
- 313.Koukou G., Niendorf S., Hornei B., Schlump J.-U., Jenke A.C., Jacobsen S. Human Astrovirus Infection Associated with Encephalitis in an Immunocompetent Child: A Case Report. J. Med. Case Rep. 2019;13:341. doi: 10.1186/s13256-019-2302-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Naccache S.N., Peggs K.S., Mattes F.M., Phadke R., Garson J.A., Grant P., Samayoa E., Federman S., Miller S., Lunn M.P., et al. Diagnosis of Neuroinvasive Astrovirus Infection in an Immunocompromised Adult with Encephalitis by Unbiased Next-Generation Sequencing. Clin. Infect. Dis. 2015;60:919–923. doi: 10.1093/cid/ciu912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Brown J.R., Morfopoulou S., Hubb J., Emmett W.A., Ip W., Shah D., Brooks T., Paine S.M.L., Anderson G., Virasami A., et al. Astrovirus VA1/HMO-C: An Increasingly Recognized Neurotropic Pathogen in Immunocompromised Patients. Clin. Infect. Dis. 2015;60:881–888. doi: 10.1093/cid/ciu940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Bohmwald K., Andrade C.A., Gálvez N.M.S., Mora V.P., Muñoz J.T., Kalergis A.M. The Causes and Long-Term Consequences of Viral Encephalitis. Front. Cell. Neurosci. 2021;15:755875. doi: 10.3389/fncel.2021.755875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Baig A.M., Sanders E.C. Potential Neuroinvasive Pathways of SARS-CoV-2: Deciphering the Spectrum of Neurological Deficit Seen in Coronavirus Disease-2019 (COVID-19) J. Med. Virol. 2020;92:1845–1857. doi: 10.1002/jmv.26105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Haddadi K., Asadian L. Coronavirus Disease 2019: Latest Data on Neuroinvasive Potential. Iran. J. Med. Sci. 2020;45:325–332. doi: 10.30476/ijms.2020.85980.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Yang D., Li X.-J., Tu D.-Z., Li X.-L., Wei B. Advances in Viral Encephalitis: Viral Transmission, Host Immunity, and Experimental Animal Models. Zool. Res. 2023;44:525–542. doi: 10.24272/j.issn.2095-8137.2023.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Martínez-Mármol R., Giordano-Santini R., Kaulich E., Cho A.-N., Przybyla M., Riyadh M.A., Robinson E., Chew K.Y., Amor R., Meunier F.A., et al. SARS-CoV-2 Infection and Viral Fusogens Cause Neuronal and Glial Fusion That Compromises Neuronal Activity. Sci. Adv. 2023;9:eadg2248. doi: 10.1126/sciadv.adg2248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Moretti R., Giuffrè M., Merli N., Caruso P., Di Bella S., Tiribelli C., Crocè L.S. Hepatitis C Virus-Related Central and Peripheral Nervous System Disorders. Brain Sci. 2021;11:1569. doi: 10.3390/brainsci11121569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Mathew S., Faheem M., Ibrahim S.M., Iqbal W., Rauff B., Fatima K., Qadri I. Hepatitis C Virus and Neurological Damage. WJH. 2016;8:545. doi: 10.4254/wjh.v8.i12.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Mankertz A., Chen M.-H., Goldberg T.L., Hübschen J.M., Pfaff F., Ulrich R.G., ICTV Report Consortium ICTV Virus Taxonomy Profile: Matonaviridae 2022: This Article Is Part of the ICTV Virus Taxonomy Profiles Collection. J. Gen. Virol. 2022;103:001817. doi: 10.1099/jgv.0.001817. [DOI] [PubMed] [Google Scholar]
- 324.Woyessa A.B., Ali M.S., Korkpor T.K., Tuopileyi R., Kohar H.T., Dogba J., Baller A., Monday J., Abdullahi S., Nagbe T., et al. Rubella Transmission and the Risk of Congenital Rubella Syndrome in Liberia: A Need to Introduce Rubella-Containing Vaccine in the Routine Immunization Program. BMC Infect. Dis. 2019;19:813. doi: 10.1186/s12879-019-4464-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Gatherer D., Depledge D.P., Hartley C.A., Szpara M.L., Vaz P.K., Benkő M., Brandt C.R., Bryant N.A., Dastjerdi A., Doszpoly A., et al. ICTV Virus Taxonomy Profile: Herpesviridae 2021. J. Gen. Virol. 2021;102:001673. doi: 10.1099/jgv.0.001673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Wright W.F., Pinto C.N., Palisoc K., Baghli S. Viral (Aseptic) Meningitis: A Review. J. Neurol. Sci. 2019;398:176–183. doi: 10.1016/j.jns.2019.01.050. [DOI] [PubMed] [Google Scholar]
- 327.Carneiro V.C.D.S., Pereira J.G., De Paula V.S. Family Herpesviridae and Neuroinfections: Current Status and Research in Progress. Mem. Inst. Oswaldo Cruz. 2022;117:e220200. doi: 10.1590/0074-02760220200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Meyding-Lamadé U., Strank C. Herpesvirus Infections of the Central Nervous System in Immunocompromised Patients. Ther. Adv. Neurol. Disord. 2012;5:279. doi: 10.1177/1756285612456234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.McCauley J.W., Hongo S., Kaverin N.V., Kochs G., Lamb R.A., Matrosovich M.N., Perez D.R., Palese P., Presti R.M., Rimstad E., et al. Family: Orthomyxoviridae Chapter Version: ICTV Ninth Report; 2009 Taxonomy Release. International Committee on Tax-onomy of Viruses: ICTV. [(accessed on 7 May 2024)]. Available online: https://ictv.global/report_9th/RNAneg/Orthomyxoviridae.
- 330.Radzišauskienė D., Vitkauskaitė M., Žvinytė K., Mameniškienė R. Neurological Complications of Pandemic A(H1N1)2009pdm, Postpandemic A(H1N1)v, and Seasonal Influenza A. Brain Behav. 2021;11:e01916. doi: 10.1002/brb3.1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Davis L.E., Koster F., Cawthon A. Handbook of Clinical Neurology. Volume 123. Elsevier; New York, NY, USA: 2014. Neurologic Aspects of Influenza Viruses; pp. 619–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Frankl S., Coffin S.E., Harrison J.B., Swami S.K., McGuire J.L. Influenza-Associated Neurologic Complications in Hospitalized Children. J. Pediatr. 2021;239:24–31.e1. doi: 10.1016/j.jpeds.2021.07.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Popescu C.P., Florescu S.A., Lupulescu E., Zaharia M., Tardei G., Lazar M., Ceausu E., Ruta S.M. Neurologic Complications of Influenza B Virus Infection in Adults, Romania. Emerg. Infect. Dis. 2017;23:574–581. doi: 10.3201/eid2304.161317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Rima B., Balkema-Buschmann A., Dundon W.G., Duprex P., Easton A., Fouchier R., Kurath G., Lamb R., Lee B., Rota P., et al. ICTV Virus Taxonomy Profile: Paramyxoviridae. J. Gen. Virol. 2019;100:1593–1594. doi: 10.1099/jgv.0.001328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Wilson M.R. Encyclopedia of the Neurological Sciences. Elsevier; New York, NY, USA: 2014. Meningitis, Viral; pp. 1077–1081. [Google Scholar]
- 336.Sumlivaya O.N., Vorobeva N.N., Zernina M.G., Kadebskaya M.A. Clinical Case of Parainfluenza Meningitis. Sci. Rev. Med. Sci. 2022;6:65–69. doi: 10.17513/srms.1305. [DOI] [Google Scholar]
- 337.Farahmand M., Shatizadeh Malekshahi S., Jabbari M.R., Shayestehpour M. The Landscape of Extrapulmonary Manifestations of Human Parainfluenza Viruses: A Systematic Narrative Review. Microbiol. Immunol. 2021;65:1–9. doi: 10.1111/1348-0421.12865. [DOI] [PubMed] [Google Scholar]
- 338.Cotmore S.F., Agbandje-McKenna M., Canuti M., Chiorini J.A., Eis-Hubinger A.-M., Hughes J., Mietzsch M., Modha S., Ogliastro M., Pénzes J.J., et al. ICTV Virus Taxonomy Profile: Parvoviridae. J. Gen. Virol. 2019;100:367–368. doi: 10.1099/jgv.0.001212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Vilmane A., Terentjeva A., Tamosiunas P.L., Suna N., Suna I., Petraityte-Burneikiene R., Murovska M., Rasa-Dzelzkaleja S., Nora-Krukle Z. Human Parvoviruses May Affect the Development and Clinical Course of Meningitis and Meningoencephalitis. Brain Sci. 2020;10:339. doi: 10.3390/brainsci10060339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Zell R., Delwart E., Gorbalenya A.E., Hovi T., King A.M.Q., Knowles N.J., Lindberg A.M., Pallansch M.A., Palmenberg A.C., Reuter G., et al. ICTV Virus Taxonomy Profile: Picornaviridae. J. Gen. Virol. 2017;98:2421–2422. doi: 10.1099/jgv.0.000911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Ramalho E., Sousa I., Burlandy F., Costa E., Dias A., Serrano R., Oliveira M., Lopes R., Debur M., Burger M., et al. Identification and Phylogenetic Characterization of Human Enteroviruses Isolated from Cases of Aseptic Meningitis in Brazil, 2013–2017. Viruses. 2019;11:690. doi: 10.3390/v11080690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Chen P., Lin X., Liu G., Wang S., Song L., Tao Z., Xu A. Analysis of Enterovirus Types in Patients with Symptoms of Aseptic Meningitis in 2014 in Shandong, China. Virology. 2018;516:196–201. doi: 10.1016/j.virol.2018.01.022. [DOI] [PubMed] [Google Scholar]
- 343.Sousa I.P., Oliveira M.D.L.A., Burlandy F.M., Machado R.S., Oliveira S.S., Tavares F.N., Gomes-Neto F., Da Costa E.V., Da Silva E.E. Molecular Characterization and Epidemiological Aspects of Non-Polio Enteroviruses Isolated from Acute Flaccid Paralysis in Brazil: A Historical Series (2005–2017) Emerg. Microbes Infect. 2020;9:2536–2546. doi: 10.1080/22221751.2020.1850181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Bitnun A., Yeh E.A. Acute Flaccid Paralysis and Enteroviral Infections. Curr. Infect. Dis. Rep. 2018;20:34. doi: 10.1007/s11908-018-0641-x. [DOI] [PubMed] [Google Scholar]
- 345.Pandit T., Pandit R., Goyal L., Ajmera K., Dasari N. Novel Presentation of Parechovirus Encephalitis in Children: Two Unique Cases. Cureus. 2022;14:e26456. doi: 10.7759/cureus.26456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Suthar P.P., Hughes K., Kadam G., Jhaveri M., Gaddikeri S. Human Parechovirus Meningoencephalitis. S. Afr. J. Radiol. 2023;27:a2589. doi: 10.4102/sajr.v27i1.2589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Sarma A., Hanzlik E., Krishnasarma R., Pagano L., Pruthi S. Human Parechovirus Meningoencephalitis: Neuroimaging in the Era of Polymerase Chain Reaction–Based Testing. AJNR Am. J. Neuroradiol. 2019;40:1418–1421. doi: 10.3174/ajnr.A6118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Rima B., Collins P., Easton A., Fouchier R., Kurath G., Lamb R.A., Lee B., Maisner A., Rota P., Wang L.-F. Problems of Classification in the Family Paramyxoviridae. Arch. Virol. 2018;163:1395–1404. doi: 10.1007/s00705-018-3720-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Saravanos G.L., King C.L., Deng L., Dinsmore N., Ramos I., Takashima M., Crawford N., Clark J.E., Dale R.C., Jones C.A., et al. Respiratory Syncytial Virus–Associated Neurologic Complications in Children: A Systematic Review and Aggregated Case Series. J. Pediatr. 2021;239:39–49. doi: 10.1016/j.jpeds.2021.06.045. [DOI] [PubMed] [Google Scholar]
- 350.Moens U., Calvignac-Spencer S., Lauber C., Ramqvist T., Feltkamp M.C.W., Daugherty M.D., Verschoor E.J., Ehlers B., ICTV Report Consortium ICTV Virus Taxonomy Profile: Polyomaviridae. J. Gen. Virol. 2017;98:1159–1160. doi: 10.1099/jgv.0.000839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Saylor D., Dickens A.M., Sacktor N., Haughey N., Slusher B., Pletnikov M., Mankowski J.L., Brown A., Volsky D.J., McArthur J.C. HIV-Associated Neurocognitive Disorder—Pathogenesis and Prospects for Treatment. Nat. Rev. Neurol. 2016;12:234–248. doi: 10.1038/nrneurol.2016.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Canet G., Dias C., Gabelle A., Simonin Y., Gosselet F., Marchi N., Makinson A., Tuaillon E., Van de Perre P., Givalois L., et al. HIV Neuroinfection and Alzheimer’s Disease: Similarities and Potential Links? Front. Cell. Neurosci. 2018;12:307. doi: 10.3389/fncel.2018.00307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Chemparthy D.T., Kannan M., Gordon L., Buch S., Sil S. Alzheimer’s-Like Pathology at the Crossroads of HIV-Associated Neurological Disorders. Vaccines. 2021;9:930. doi: 10.3390/vaccines9080930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Shieh W.-J. Human Adenovirus Infections in Pediatric Population—An Update on Clinico–Pathologic Correlation. Biomed. J. 2022;45:38–49. doi: 10.1016/j.bj.2021.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Vidal L.R., de Almeida S.M., Cavalli B.M., Dieckmann T.G., Raboni S.M., Salvador G.L.O., Pereira L.A., Rotta I., Nogueira M.B. Human Adenovirus Meningoencephalitis: A 3-Years’ Overview. J. Neurovirol. 2019;25:589–596. doi: 10.1007/s13365-019-00758-7. [DOI] [PubMed] [Google Scholar]
- 356.Reuter G., Pankovics P., Boros Á. Nonsuppurative (Aseptic) Meningoencephalomyelitis Associated with Neurovirulent Astrovirus Infections in Humans and Animals. Clin. Microbiol. Rev. 2018;31:e00040-18. doi: 10.1128/CMR.00040-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Tkachev S., editor. Encephalitis. InTech; Houston, TX, USA: 2013. [Google Scholar]
- 358.Lizzi J., Hill T., Jakubowski J. Varicella Zoster Virus Encephalitis. Clin. Pract. Cases Emerg. Med. 2019;3:380–382. doi: 10.5811/cpcem.2019.8.43010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Alvarez J.C., Alvarez J., Ticono J., Medallo P., Miranda H., Ferrés M., Forero J., Álvarez C. Varicella-Zoster Virus Meningitis and Encephalitis: An Understated Cause of Central Nervous System Infections. Cureus. 2020;12:e11583. doi: 10.7759/cureus.11583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Herlin L.K., Hansen K.S., Bodilsen J., Larsen L., Brandt C., Andersen C.Ø., Hansen B.R., Lüttichau H.R., Helweg-Larsen J., Wiese L., et al. Varicella Zoster Virus Encephalitis in Denmark From 2015 to 2019—A Nationwide Prospective Cohort Study. Clin. Infect. Dis. 2021;72:1192–1199. doi: 10.1093/cid/ciaa185. [DOI] [PubMed] [Google Scholar]
- 361.Dou Y., Li Y. Influenza A H3N2-Associated Meningoencephalitis in an Older Adult with Viral RNA in Cerebrospinal Fluid: Case Report. Front. Neurol. 2022;13:874078. doi: 10.3389/fneur.2022.874078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Ferren M., Horvat B., Mathieu C. Measles Encephalitis: Towards New Therapeutics. Viruses. 2019;11:1017. doi: 10.3390/v11111017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Al-Qayoudhi A., Al-Kindi H., Meki N., Al-Maani A. Acute Measles Encephalitis in an Immigrant Syrian Child: Case Report and Review of the Literature. Oman Med. J. 2016;31:150–153. doi: 10.5001/omj.2016.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Diwan M.N., Samad S., Mushtaq R., Aamir A., Allahuddin Z., Ullah I., Ullah Afridi R., Ambreen A., Khan A., Ehsan N., et al. Measles Induced Encephalitis: Recent Interventions to Overcome the Obstacles Encountered in the Management Amidst the COVID-19 Pandemic. Diseases. 2022;10:104. doi: 10.3390/diseases10040104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Saijo M., Fujita K. Central nervous system infection caused by mumps virus. Nihon Rinsho. 1997;55:870–875. [PubMed] [Google Scholar]
- 366.Herndon R.M. Ependymitis in Mumps Virus Meningitis: Electron Microscopical Studies of Cerebrospinal Fluid. Arch. Neurol. 1974;30:475. doi: 10.1001/archneur.1974.00490360051010. [DOI] [PubMed] [Google Scholar]
- 367.Bitnun A., Ford-Jones E.L., Petric M., MacGregor D., Heurter H., Nelson S., Johnson G., Richardson S. Acute Childhood Encephalitis and Mycoplasma pneumoniae. Clin. Infect. Dis. 2001;32:1674–1684. doi: 10.1086/320748. [DOI] [PubMed] [Google Scholar]
- 368.Sugai K., Tsukagoshi H., Nojima I., Fujiwara K., Kodera A., Kimura N., Tsuchimoto K., Sekimoto K., Kitada K., Takahashi N., et al. Severe Acute Encephalopathy Related to Human Parainfluenza Virus Type 2 Infection in an Infant: A Case Report. JMM Case Rep. 2015;2:e000072. doi: 10.1099/jmmcr.0.000072. [DOI] [Google Scholar]
- 369.Ahn S.-J., Moon J., Sunwoo J.-S., Jun J.-S., Lee S.-T., Park K.-I., Jung K.-H., Jung K.-Y., Kim M., Lee S.K., et al. Respiratory Virus-Related Meningoencephalitis in Adults. Encephalitis. 2020;1:14–19. doi: 10.47936/encephalitis.2020.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Lewandowski L.J., Lief F.S., Verini M.A., Pienkowski M.M., ter Meulen V., Koprowski H. Analysis of a Viral Agent Isolated from Multiple Sclerosis Brain Tissue: Characterization as a Parainfluenzavirus Type 1. J. Virol. 1974;13:1037–1045. doi: 10.1128/jvi.13.5.1037-1045.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Ter Meulen V., Iwasaki Y., Koprowski H., Käckell Y.M., Müller D. Fusion of cultured multiple-sclerosis brain cells with indicator cells: Presence of nucleocapsids and virions and isolation of parainfluenza-type virus. Lancet. 1972;300:1–5. doi: 10.1016/S0140-6736(72)91273-1. [DOI] [PubMed] [Google Scholar]
- 372.Román G., Phillips C.A., Poser C.M. Parainfluenza Virus Type 3: Isolation from CSF of a Patient with Guillain-Barré Syndrome. JAMA. 1978;240:1613–1615. doi: 10.1001/jama.1978.03290150059026. [DOI] [PubMed] [Google Scholar]
- 373.Arguedas A., Stutman H.R., Blanding J.G. Parainfluenza Type 3 Meningitis: Report of Two Cases and Review of the Literature. Clin. Pediatr. 1990;29:175–178. doi: 10.1177/000992289002900307. [DOI] [PubMed] [Google Scholar]
- 374.Wong V.K., Steinberg E., Warford A. Parainfluenza virus type 3 meningitis in an 11-month-old infant. Pediatr. Infect. Dis. J. 1988;7:300. doi: 10.1097/00006454-198804000-00017. [DOI] [PubMed] [Google Scholar]
- 375.Vreede R.W., Schellekens H., Zuijderwijk M. Isolation of Parainfluenza Virus Type 3 from Cerebrospinal Fluid. J. Infect. Dis. 1992;165:1166. doi: 10.1093/infdis/165.6.1166. [DOI] [PubMed] [Google Scholar]
- 376.Mori D., Ranawaka U., Yamada K., Rajindrajith S., Miya K., Perera H.K.K., Matsumoto T., Dassanayake M., Mitui M.T., Mori H., et al. Human Bocavirus in Patients with Encephalitis, Sri Lanka, 2009–2010. Emerg. Infect. Dis. 2013;19:1859–1862. doi: 10.3201/eid1911.121548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Yu J., Chen Q., Hao Y., Yu T., Zeng S., Wu X., Zhang B., Duan Z. Identification of Human Bocaviruses in the Cerebrospinal Fluid of Children Hospitalized with Encephalitis in China. J. Clin. Virol. 2013;57:374–377. doi: 10.1016/j.jcv.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 378.Ergul A.B., Altug U., Aydin K., Guven A.S., Altuner Torun Y. Acute Necrotizing Encephalopathy Causing Human Bocavirus. Neuroradiol. J. 2017;30:164–167. doi: 10.1177/1971400916687586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Mitui M.T., Shahnawaz Bin Tabib S.M., Matsumoto T., Khanam W., Ahmed S., Mori D., Akhter N., Yamada K., Kabir L., Nishizono A., et al. Detection of Human Bocavirus in the Cerebrospinal Fluid of Children with Encephalitis. Clin. Infect. Dis. 2012;54:964–967. doi: 10.1093/cid/cir957. [DOI] [PubMed] [Google Scholar]
- 380.Douvoyiannis M., Litman N., Goldman D.L. Neurologic Manifestations Associated with Parvovirus B19 Infection. Clin. Infect. Dis. 2009;48:1713–1723. doi: 10.1086/599042. [DOI] [PubMed] [Google Scholar]
- 381.Barah F., Whiteside S., Batista S., Morris J. Neurological Aspects of Human Parvovirus B19 Infection: A Systematic Review. Rev. Med. Virol. 2014;24:154–168. doi: 10.1002/rmv.1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Watanabe T. Acute Encephalitis and Encephalopathy Associated with Human Parvovirus B19 Infection in Children. World J. Clin. Pediatr. 2015;4:126. doi: 10.5409/wjcp.v4.i4.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Benjamin L. Human Parvovirus 4 as Potential Cause of Encephalitis in Children, India. Emerg. Infect. Dis. 2011;17:1484–1487. doi: 10.3201/eid1708.110165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384.Nagai T., Hanaoka N., Katano H., Konagaya M., Tanaka-Taya K., Shimizu H., Mukai T., Fujimoto T. A Fatal Case of Acute Encephalopathy in a Child Due to Coxsackievirus A2 Infection: A Case Report. BMC Infect. Dis. 2021;21:1167. doi: 10.1186/s12879-021-06858-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Kon Y., Takahashi S., Takahata N., Onodera I., Sato M. Case of chronic encephalitis with Coxsackie A 5 virus isolated from the cerebrospinal fluid. Rinsho Shinkeigaku. 1974;14:752–759. [PubMed] [Google Scholar]
- 386.Grist N.R. Type A7 Coxsackie (Type 4 Poliomyelitis) Virus Infection in Scotland. J. Hyg. 1962;60:323–332. doi: 10.1017/S002217240002043X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Seitsonen J.J.T., Shakeel S., Susi P., Pandurangan A.P., Sinkovits R.S., Hyvönen H., Laurinmäki P., Ylä-Pelto J., Topf M., Hyypiä T., et al. Structural Analysis of Coxsackievirus A7 Reveals Conformational Changes Associated with Uncoating. J. Virol. 2012;86:7207–7215. doi: 10.1128/JVI.06425-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Eyckmans T., Wollants E., Janssens A., Schoemans H., Lagrou K., Wauters J., Maertens J. Coxsackievirus A16 Encephalitis during Obinutuzumab Therapy, Belgium, 2013. Emerg. Infect. Dis. 2014;20:913–915. doi: 10.3201/eid2005.131766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Fowlkes A.L., Honarmand S., Glaser C., Yagi S., Schnurr D., Oberste M.S., Anderson L., Pallansch M.A., Khetsuriani N. Enterovirus-Associated Encephalitis in the California Encephalitis Project, 1998–2005. J. Infect. Dis. 2008;198:1685–1691. doi: 10.1086/592988. [DOI] [PubMed] [Google Scholar]
- 390.Perez-Velez C.M., Anderson M.S., Robinson C.C., McFarland E.J., Nix W.A., Pallansch M.A., Oberste M.S., Glode M.P. Outbreak of Neurologic Enterovirus Type 71 Disease: A Diagnostic Challenge. Clin. Infect. Dis. 2007;45:950–957. doi: 10.1086/521895. [DOI] [PubMed] [Google Scholar]
- 391.Huang C.-C., Liu C.-C., Chang Y.-C., Chen C.-Y., Wang S.-T., Yeh T.-F. Neurologic Complications in Children with Enterovirus 71 Infection. N. Engl. J. Med. 1999;341:936–942. doi: 10.1056/NEJM199909233411302. [DOI] [PubMed] [Google Scholar]
- 392.Majer A., McGreevy A., Booth T.F. Molecular Pathogenicity of Enteroviruses Causing Neurological Disease. Front. Microbiol. 2020;11:540. doi: 10.3389/fmicb.2020.00540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Chonmaitree T., Menegus M.A., Schervish-Swierkosz E.M., Schwalenstocker E. Enterovirus 71 Infection: Report of an Outbreak with Two Cases of Paralysis and a Review of the Literature. Pediatrics. 1981;67:489–493. doi: 10.1542/peds.67.4.489. [DOI] [PubMed] [Google Scholar]
- 394.Lin T.-Y., Twu S.-J., Ho M.-S., Chang L.-Y., Lee C.-Y. Enterovirus 71 Outbreaks, Taiwan: Occurrence and Recognition. Emerg. Infect. Dis. 2003;9:291–293. doi: 10.3201/eid0903.020285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Moreau B., Bastedo C., Michel R.P., Ghali P. Hepatitis and Encephalitis Due to Coxsackie Virus A9 in an Adult. Case Rep. Gastroenterol. 2011;5:617–622. doi: 10.1159/000333135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Kamei S., Hersch S.M., Kurata T., Takei Y. Coxsackie B Antigen in the Central Nervous System of a Patient with Fatal Acute Encephalitis: Immunohistochemical Studies of Formalin-Fixed Paraffin-Embedded Tissue. Acta Neuropathol. 1990;80:216–221. doi: 10.1007/BF00308928. [DOI] [PubMed] [Google Scholar]
- 397.Brunner J., Litwicki A., Aliani S., Gärtner B. Coxsackie Virus B 4 Encephalitis in a 7 Year Old Boy. Klin. Padiatr. 2004;216:297–299. doi: 10.1055/s-2004-822636. [DOI] [PubMed] [Google Scholar]
- 398.Klapper P.E., Bailey A.S., Longson M., Barton B.W., Davies-Jones G.A.B. Meningo-Encephalitis Caused by Coxsackievirus Group B Type 2. Diagnosis Confirmed by Measuring Intrathecal Antibody. J. Infect. 1984;8:227–231. doi: 10.1016/S0163-4453(84)93931-8. [DOI] [PubMed] [Google Scholar]
- 399.Gobbi F., Calleri G., Spezia C., Lipani F., Balbiano R., De Agostini M., Milia M.G., Caramello P. Echovirus-4 Meningitis Outbreak Imported from India: Table 1. J. Travel Med. 2010;17:66–68. doi: 10.1111/j.1708-8305.2009.00375.x. [DOI] [PubMed] [Google Scholar]
- 400.Handsher R., Shulman L.M., Abramovitz B., Silberstein I., Neuman M., Tepperberg-Oikawa M., Fisher T., Mendelson E. A New Variant of Echovirus 4 Associated with a Large Outbreak of Aseptic Meningitis. J. Clin. Virol. 1999;13:29–36. doi: 10.1016/S1386-6532(99)00014-1. [DOI] [PubMed] [Google Scholar]
- 401.Smura T., Blomqvist S., Kolehmainen P., Schuffenecker I., Lina B., Böttcher S., Diedrich S., Löve A., Brytting M., Hauzenberger E., et al. Aseptic Meningitis Outbreak Associated with Echovirus 4 in Northern Europe in 2013–2014. J. Clin. Virol. 2020;129:104535. doi: 10.1016/j.jcv.2020.104535. [DOI] [PubMed] [Google Scholar]
- 402.Kopecka H. Encyclopedia of Virology. Elsevier; New York, NY, USA: 1999. Echoviruses (Picornaviridae) pp. 411–417. [Google Scholar]
- 403.Foncin J.F., Maurin J., Gaches J., Stilhart B., Le Beau J. Curable ECHO 5 virus encephalitis. Clinical, electroencephalographic, virologic and ultrastructural study. Ann. Med. Interne. 1977;128:335–343. [PubMed] [Google Scholar]
- 404.Kim H.-J., Kang B., Hwang S., Hong J., Kim K., Cheon D.-S. Epidemics of Viral Meningitis Caused by Echovirus 6 and 30 in Korea in 2008. Virol. J. 2012;9:38. doi: 10.1186/1743-422X-9-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.Ashwell M.J.S., Smith D.W., Phillips P.A., Rouse I.L. Viral Meningitis Due to Echovirus Types 6 and 9: Epidemiological Data from Western Australia. Epidemiol. Infect. 1996;117:507–512. doi: 10.1017/S0950268800059185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406.Fratty I.S., Kriger O., Weiss L., Vasserman R., Erster O., Mendelson E., Sofer D., Weil M. Increased Detection of Echovirus 6-Associated Meningitis in Patients Hospitalized during the COVID-19 Pandemic, Israel 2021–2022. J. Clin. Virol. 2023;162:105425. doi: 10.1016/j.jcv.2023.105425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407.Jarvis W.R. Echovirus Type 7 Meningitis in Young Children. Arch. Pediatr. Adolesc. Med. 1981;135:1009. doi: 10.1001/archpedi.1981.02130350013006. [DOI] [PubMed] [Google Scholar]
- 408.Lum L.C.S., Chua K.B., McMinn P.C., Goh A.Y.T., Muridan R., Sarji S.A., Hooi P.S., Chua B.H., Lam S.K. Echovirus 7 Associated Encephalomyelitis. J. Clin. Virol. 2002;23:153–160. doi: 10.1016/S1386-6532(01)00214-1. [DOI] [PubMed] [Google Scholar]
- 409.Li J., Yan D., Chen L., Zhang Y., Song Y., Zhu S., Ji T., Zhou W., Gan F., Wang X., et al. Multiple Genotypes of Echovirus 11 Circulated in Mainland China between 1994 and 2017. Sci. Rep. 2019;9:10583. doi: 10.1038/s41598-019-46870-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410.Chen Y.-C., Yang S.-L., Yang H., Lin T.-Y., Hsieh Y.-C., Huang K.-Y.A., Kuo C.-Y., Chiu C.-H., Huang Y.-C., Chu S.-M., et al. Clinical Characteristics of Echovirus 11 and Coxsackievirus B5 Infections in Taiwanese Children Requiring Hospitalization. J. Microbiol. Immunol. Infect. 2021;54:581–587. doi: 10.1016/j.jmii.2020.06.008. [DOI] [PubMed] [Google Scholar]
- 411.Somekh E., Cesar K., Handsher R., Hanukoglu A., Dalal I., Ballin A., Shohat T. An Outbreak of Echovirus 13 Meningitis in Central Israel. Epidemiol. Infect. 2003;130:257–262. doi: 10.1017/S095026880200818X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Sarmiento L., Mas P., Goyenechea A., Palomera R., Morier L., Capó V., Quintana I., Santin M. First Epidemic of Echovirus 16 Meningitis in Cuba. Emerg. Infect. Dis. 2001;7:887–889. doi: 10.3201/eid0705.017520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.Singh D.V., Kumar A., Kumar P., Baluni M., Ghildiyal S., Kumar R., Misra U.K., Dhole T.N. An Outbreak of Encephalitis Associated with Echovirus 19 in Uttar Pradesh, India, in 2011. Arch. Virol. 2016;161:967–970. doi: 10.1007/s00705-015-2714-6. [DOI] [PubMed] [Google Scholar]
- 414.Kelen A.E., Lesiak J.M., Labzoffsky N.A. An outbreak of aseptic meningitis due to ECHO 25 virus. Can. Med. Assoc. J. 1964;90:1349–1351. [PMC free article] [PubMed] [Google Scholar]
- 415.Peters A.C.B., Vielvoye G.J., Versteeg J., Bots G.T.A.M., Lindeman J. ECHO 25 Focal Encephalitis and Subacute Hemichorea. Neurology. 1979;29:676. doi: 10.1212/WNL.29.5.676. [DOI] [PubMed] [Google Scholar]
- 416.Lewthwaite P., Perera D., Ooi M.H., Last A., Kumar R., Desai A., Begum A., Ravi V., Shankar M.V., Tio P.H., et al. Enterovirus 75 Encephalitis in Children, Southern India. Emerg. Infect. Dis. 2010;16:1780–1782. doi: 10.3201/eid1611.100672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417.Avellon A., Rubio G., Palacios G., Casas I., Rabella N., Reina G., Perez C., Lipkin W.I., Trallero G. Enterovirus 75 and Aseptic Meningitis, Spain, 2005. Emerg. Infect. Dis. 2006;12:1609–1611. doi: 10.3201/eid1210.060353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Gutierrez K., Abzug M.J. Vaccine-Associated Poliovirus Meningitis in Children with Ventriculoperitoneal Shunts. J. Pediatr. 1990;117:424–427. doi: 10.1016/S0022-3476(05)81085-6. [DOI] [PubMed] [Google Scholar]
- 419.Zevakov V.F., Semak S.I., Titarenko V.I., Andreĭchenko N.V., Gedzul O.V. Role of poliomyelitis viruses in the etiology of serous meningitis in Odessa 1979–1983. Vopr. Virusol. 1987;32:459–464. [PubMed] [Google Scholar]
- 420.Saslaw S. Aseptic Meningitis and Nonparalytic Poliomyelitis. Arch. Intern. Med. 1961;107:568. doi: 10.1001/archinte.1961.03620040094010. [DOI] [PubMed] [Google Scholar]
- 421.Chen B.-S., Lee H.-C., Lee K.-M., Gong Y.-N., Shih S.-R. Enterovirus and Encephalitis. Front. Microbiol. 2020;11:261. doi: 10.3389/fmicb.2020.00261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Hixon A.M., Frost J., Rudy M.J., Messacar K., Clarke P., Tyler K.L. Understanding Enterovirus D68-Induced Neurologic Disease: A Basic Science Review. Viruses. 2019;11:821. doi: 10.3390/v11090821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.Kreuter J.D., Barnes A., McCarthy J.E., Schwartzman J.D., Oberste M.S., Rhodes C.H., Modlin J.F., Wright P.F. A Fatal Central Nervous System Enterovirus 68 Infection. Arch. Pathol. Lab. Med. 2011;135:793–796. doi: 10.5858/2010-0174-CR.1. [DOI] [PubMed] [Google Scholar]
- 424.Giombini E., Rueca M., Barberi W., Iori A.P., Castilletti C., Scognamiglio P., Vairo F., Ippolito G., Capobianchi M.R., Valli M.B. Enterovirus D68–Associated Acute Flaccid Myelitis in Immunocompromised Woman, Italy. Emerg. Infect. Dis. 2017;23:1690–1693. doi: 10.3201/eid2310.170792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425.González-Sanz R., Taravillo I., Reina J., Navascués A., Moreno-Docón A., Aranzamendi M., Romero M.P., del Cuerpo M., Pérez-González C., Pérez-Castro S., et al. Enterovirus D68-Associated Respiratory and Neurological Illness in Spain, 2014–2018. Emerg. Microbes Infect. 2019;8:1438–1444. doi: 10.1080/22221751.2019.1668243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Bharucha E.P., Mondkar V.P., Wadia N.H., Irani P.F., Katrak S.M. Neurological complications of a new conjunctivitis. Lancet. 1972;300:970–971. doi: 10.1016/S0140-6736(72)92492-0. [DOI] [PubMed] [Google Scholar]
- 427.Lee J.-J., Kang K., Park J.-M., Kwon O., Kim B.-K. Encephalitis Associated with Acute Hepatitis A. J. Epilepsy Res. 2011;1:27–28. doi: 10.14581/jer.11005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428.Abedi G.R., Watson J.T., Pham H., Nix W.A., Oberste M.S., Gerber S.I. Enterovirus and Human Parechovirus Surveillance—United States, 2009–2013. MMWR Morb. Mortal. Wkly. Rep. 2015;64:940–943. doi: 10.15585/mmwr.mm6434a3. [DOI] [PubMed] [Google Scholar]
- 429.Shirota G., Morozumi M., Ubukata K., Shiro H. Infantile Meningitis Caused by Respiratory Syncytial Virus. J. Jpn. Assoc. Infect. Dis. 2011;85:682–685. doi: 10.11150/kansenshogakuzasshi.85.682. [DOI] [PubMed] [Google Scholar]
- 430.Xu L., Gao H., Zeng J., Liu J., Lu C., Guan X., Qian S., Xie Z. A Fatal Case Associated with Respiratory Syncytial Virus Infection in a Young Child. BMC Infect. Dis. 2018;18:217. doi: 10.1186/s12879-018-3123-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 431.Yu S., Hua Y., Qian J., Sun M., Kang Y.-J. The Presence of Human Respiratory Syncytial Virus in the Cerebrospinal Fluid of a Child with Anti-N-Methyl-D-Aspartate Receptor Encephalitis of Unknown Trigger. Virol. J. 2023;20:34. doi: 10.1186/s12985-023-01997-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432.Sugimoto M., Morichi S., Kashiwagi Y., Suzuki S., Nishimata S., Yamanaka G., Sawada A., Kawashima H. A Case of Respiratory Syncytial Virus-Associated Encephalopathy in Which the Virus Was Detected in Cerebrospinal Fluid and Intratracheal Aspiration despite Negative Rapid Test Results. J. Infect. Chemother. 2020;26:393–396. doi: 10.1016/j.jiac.2019.11.008. [DOI] [PubMed] [Google Scholar]
- 433.Bohmwald K., Gálvez N.M.S., Ríos M., Kalergis A.M. Neurologic Alterations Due to Respiratory Virus Infections. Front. Cell. Neurosci. 2018;12:386. doi: 10.3389/fncel.2018.00386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.Schildgen O., Glatzel T., Geikowski T., Scheibner B., Simon A., Bindl L., Born M., Viazov S., Wilkesmann A., Knöpfle G., et al. Human Metapneumovirus RNA in Encephalitis Patient. Emerg. Infect. Dis. 2005;11:467–470. doi: 10.3201/eid1103.040676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 435.Fok A., Mateevici C., Lin B., Chandra R.V., Chong V.H.T. Encephalitis-Associated Human Metapneumovirus Pneumonia in Adult, Australia. Emerg. Infect. Dis. 2015;21:2074–2076. doi: 10.3201/eid2111.150608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 436.Sánchez Fernández I. Human Metapneumovirus in the Cerebrospinal Fluid of a Patient with Acute Encephalitis. Arch. Neurol. 2012;69:649. doi: 10.1001/archneurol.2011.1094. [DOI] [PubMed] [Google Scholar]
- 437.Mergeay M., Coeckelbergh E., De Cauwer H., Viaene M., Van der Mieren G. An Adult Case of Metapneumovirus-Induced Acute Encephalitis. Acta Neurol. Belg. 2019;119:645–648. doi: 10.1007/s13760-019-01128-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 438.Arnold J.C., Singh K.K., Milder E., Spector S.A., Sawyer M.H., Gavali S., Glaser C. Human Metapneumovirus Associated with Central Nervous System Infection in Children. Pediatr. Infect. Dis. J. 2009;28:1057–1060. doi: 10.1097/INF.0b013e3181acd221. [DOI] [PubMed] [Google Scholar]
- 439.Agnihotri S.P., Wuthrich C., Dang X., Nauen D., Karimi R., Viscidi R., Bord E., Batson S., Troncoso J., Koralnik I.J. A Fatal Case of JC Virus Meningitis Presenting with Hydrocephalus in a Human Immunodeficiency Virus-Seronegative Patient: JCV Meningitis. Ann. Neurol. 2014;76:140–147. doi: 10.1002/ana.24192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 440.Miskin D.P., Koralnik I.J. Novel Syndromes Associated with JC Virus Infection of Neurons and Meningeal Cells: No Longer a Gray Area. Curr. Opin. Neurol. 2015;28:288–294. doi: 10.1097/WCO.0000000000000201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 441.Wood B.R., Klein J.P., Lyons J.L., Milner D.A., Phillips R.E., Schutten M., Folkerth R.D., Ciarlini P., Henrich T.J., Johnson J.A. HIV-2 Encephalitis: Case Report and Literature Review. AIDS Patient Care STDs. 2012;26:383–387. doi: 10.1089/apc.2012.0048. [DOI] [PubMed] [Google Scholar]