Infants do not come into the world as “empty slates” but bring with them complex behavioural systems. One system that has been well studied protects the child from danger during the long period of extra-uterine immaturity. It involves the development of mutual attachment behaviour (box), which ensures that the child does not stray far from a caretaker. Infants are active partners in the development of this behaviour, using instinctive behaviours to engage caretakers in protecting them. These include smiling, vocalising, crying, and, later, returning frequently to the secure base of the adult after exploratory forays.1 Infant attachment is at its height at about 3 years of age and then becomes increasingly diffused by the development of other relationships, but it remains important throughout life, with later relationships qualitatively echoing the earlier ones.
For optimal emotional, social, and psychosexual development to occur, children need a warm, secure, affectionate, individualised, and continuous experience of care from a few caretakers who interact with them in a sensitive way and who can live in harmony with each other.
Summary points
The pattern of attachment between infant and parent is rooted in instinct but modified by experience. It is an important source of security throughout life
Separation from a parent in early childhood is followed, in succession, by protest, despair, and detachment; feeding difficulties, bedwetting, constipation, and sleeping difficulties may arise
In later childhood the loss of a parent commonly gives rise to emotional and behaviour problems
Children bereaved in childhood may be vulnerable to psychiatric disorder later in life
Forewarning can help children to prepare for bereavement, and they usually benefit from viewing a dead parent and attending funerals and other rituals
Family support meetings can reduce morbidity after bereavement
Separation and loss in childhood
Infants and toddlers react to separation from an attachment figure by protesting vigorously. If their cries are not successful in restoring the adult, protest eventually gives way to despair, and eventually, if they are not restored to their attachment figure, pathological states of detachment and indifference may ensue. They probably have little concept of death, and the disappearance of a parent, whatever the cause, will evoke similar reactions. Thus a parent away for a few hours and one absent for longer both evoke the same separation anxiety in infants and toddlers older than a few weeks or months.2 Even very young children can mourn for a lost parent, although the form of their grief differs from that of adults and older children.2,3 Their reactions tend to be bodily ones such as feeding difficulties, bedwetting, constipation, and sleeping difficulties.
By 5 years of age, most children can understand the difference between a temporary separation and death. They know that death is irreversible and universal, has a cause, and involves permanent separation and that dead people differ from live people in several respects: they are immobile, unfeeling, and cannot hear, see, smell, or speak. It is more difficult for children to understand that dead people change in their appearance, and this concept does not develop until nearer puberty.4 
Children from 5 to 11 years are more likely to understand the physical changes that death brings and are helped by seeing these changes for themselves. They should be told what to expect, and they should be allowed to view the body if they wish. Exceptions may arise if the body is severely mutilated or if the child or parents have a strong aversion to the idea of viewing. In such cases additional support may be needed.
Children’s characteristic response to the death of a parent is an increase in activity, and behavioural problems may result. Hallucinations of the dead person are a common feature of grief in adult life.5 They can also be experienced by young children, who may interpret them as evidence of the parent’s return, or as evidence of persecution by the ghost of the dead parent because of imagined shortcomings on the part of the child, in which case they can give rise to severe anxiety. Because of their need for parenting, children who lose one parent often become anxious about the survival of the other, and they may protect that parent from knowing of their distress. That, and the difficulty of sustaining mood states in childhood, may lead the parent or teacher to believe the child has recovered from, or has not been affected by, a bereavement.
Components of attachment behaviour in infants
Behaviour that maintains attachment:
Smiling
Vocalising (babbling)
Clinging
Following
Behaviour on separation:
Crying (protest)
Restless searching
High anxiety
Irritability
Reactions to bereavement in childhood
The florid reactions tend not to last beyond a few weeks, with most children regaining their previous level of psychosocial functioning.6 However, as assessed by parental reports, children have higher levels of emotional disturbance and symptoms than non-bereaved children for up to two years, and up to 40% of bereaved children show disturbance one year after bereavement.7,8 In direct assessments of bereaved children, Weller and colleagues found that 37% of their sample of 38 bereaved prepubertal children had a major depressive disorder one year after bereavement.9
Longing for reunion is common and may lead to suicidal thoughts in bereaved children and adolescents, although they are rarely acted upon.9 Other difficulties include learning problems and failure to maintain school progress.10
Long term effects of bereavement on children
Children who are bereaved early are more likely to develop psychiatric disorders in later childhood.11 Rutter found a fivefold increase in childhood psychiatric disorder in bereaved children compared with the general population.12
Adults bereaved of a parent in childhood seem to be more vulnerable than the general population to psychiatric disorder, particularly depression and anxiety, and this is often precipitated by further losses.13,14 Attempted suicide is more common in adults bereaved in childhood.15
Children who lose their mother suffer a reduction in the quantity as well as quality of care, and this may account for the finding of differential effect according to the sex of the deceased parent.9
Effects of the death of a sibling
Children compete for parental attention and often feel resentful of the attention given to a sick sibling. This can be heightened if a parent has spent time in hospital with the sibling. Guilt may be the predominant emotion that follows triumph at having survived when a sibling dies. Young children may believe that their hostile or ambivalent feelings actually caused their sibling’s death, and this may lead to profound behavioural changes. If the sibling was older, and carried out some parental functions, the reaction may be similar to that after loss of a parent.
Helping bereaved children
Children are rarely prepared for the death of a parent or a sibling, and yet we know from studies of bereaved adults that mourning is aided by a foreknowledge of the imminence and inevitability of death.16 Children who are forewarned have lower levels of anxiety than those who are not, even within the same family.17
When death occurs, young children in particular may need the concrete experience of seeing the parent after death. Bereaved adults find it particularly difficult to help a child in this way, and the general practitioner could offer to accompany the child. Similarly, children benefit from attending the funeral but need some protection from the raw expressed grief that may be shown at that time. Attending in the company of someone less affected by the death than the immediate relatives is desirable. This could be the child’s teacher or someone from the family practice with whom he is familiar.
The monitoring and help with practical matters (applying for a home help, mobilising family support, ensuring adequate income, etc) needs to be accompanied by specific bereavement counselling for both the child and the surviving parent. A controlled trial of family therapy with children bereaved of a parent showed that the postbereavement morbidity of 40% at one year could be reduced to 20% by six sessions of family meetings which focused on promoting shared mourning within the family and encouraging communication about the dead parent.8,9 Preventive counselling is properly the responsibility of the primary care team, utilising the resources of bereavement counselling services as necessary. Cruse (the national charity for bereavement care) publishes useful literature for bereaved children and their carers and provides training and bereavement counselling services. Dyregrov’s excellent handbook for adults deserves a place in a practice library,18 and workbooks for children of primary school age can aid those counselling them.19,20
Finally, the practitioner needs to be aware of the small number of children who may need more specialised help in recovering from depressive or other symptoms that may be associated with bereavement. These will include children who may have been partly instrumental in causing death (of a sibling perhaps), those who have gone through sudden and particularly traumatic bereavements, children who have suffered more than one bereavement, adolescents who express suicidal ideas, and children who do not respond to the initial preventive interventions.
Figure.
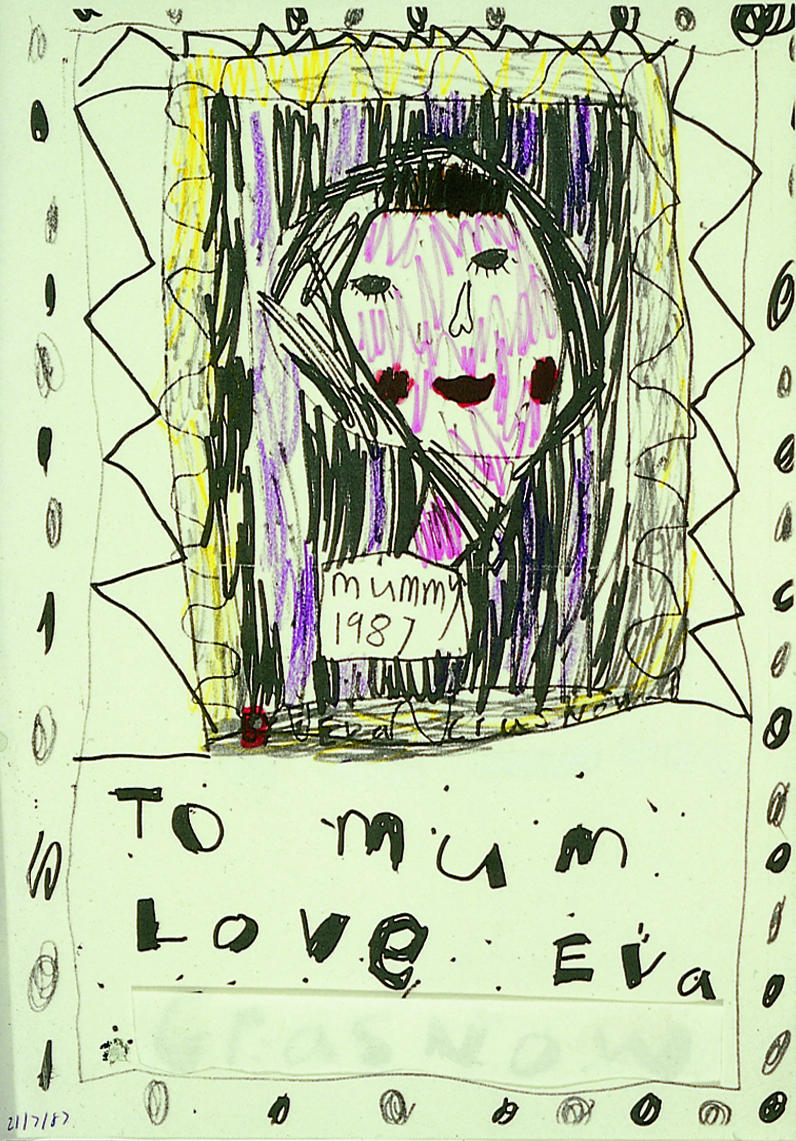
Asked to draw her mother as she imagined she might be after radiotherapy for carcinoma of the breast, 6 year old Eva at first drew mother with a scarf to hide her bald head and then attempted to hide the scarf in a similar coloured background (purple). Subsequently she filled in the background with black and drew the “tombstone” below. Although she had not been told directly that mother was dying, she showed her therapist that she was aware of the likely future for her mother
Footnotes
Funding: No additional funding.
Conflict of interest: None.
The articles in this series are adapted from Coping with Loss, edited by Colin Murray Parkes and Andrew Markus, which will be published in May.
References
- 1.Bowlby J. A secure base. London: Routledge Kegan Paul; 1988. [Google Scholar]
- 2.Bowlby J. Attachment and loss. Vols 1-3. London: Hogarth Press, 1969-80.
- 3.Furman E. A child’s parent dies. New Haven: Yale Univeristy Press; 1974. [Google Scholar]
- 4.Lansdown R, Benjamin G. The development of the concept of death in children aged 5-9 years. Child Care Health Dev. 1985;11:13–20. doi: 10.1111/j.1365-2214.1985.tb00445.x. [DOI] [PubMed] [Google Scholar]
- 5.Parkes CM. Bereavement in adult life. BMJ. 1998;316:000–000. doi: 10.1136/bmj.316.7134.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fristad MA, Jedel R, Weller RA, Weller EB. Psychosocial functioning in children after the death of a parent. Am J Psychiatry. 1993;150:511–513. doi: 10.1176/ajp.150.3.511. [DOI] [PubMed] [Google Scholar]
- 7.Black D, Urbanowicz MA. Bereaved children-family intervention. In: Stevenson JE, ed. Recent research in developmental psychopathology. Oxford: Pergammon, 1985;179-87.
- 8.Black D, Urbanowicz MA. Family intervention with bereaved children. J Child Psychol Psychiatry. 1987;28:467–476. doi: 10.1111/j.1469-7610.1987.tb01767.x. [DOI] [PubMed] [Google Scholar]
- 9.Weller RA, Weller EB, Fristad MA, Bowes JM. Depression in recently bereaved prepubertal children. Am J Psychiatry. 1991;148:1536–1540. doi: 10.1176/ajp.148.11.1536. [DOI] [PubMed] [Google Scholar]
- 10.Van Eerdewegh MM, Bieri MD, Parrilla RH, Clayton PJ. The bereaved child. Br J Psychiatry. 1982;140:23–29. doi: 10.1192/bjp.140.1.23. [DOI] [PubMed] [Google Scholar]
- 11.Black D. Annotation: the bereaved child. J Child Psychol Psychiatry. 1978;19:287–292. doi: 10.1111/j.1469-7610.1978.tb00471.x. [DOI] [PubMed] [Google Scholar]
- 12.Rutter M. Children of sick parents. Oxford: Oxford University Press; 1966. [Google Scholar]
- 13.Birtchnell J. Early parent death and mental illness. Br J Psychiatry. 1970;116:281–288. doi: 10.1192/bjp.116.532.281. [DOI] [PubMed] [Google Scholar]
- 14.Brown GW, Harris T, Copeland JR. Depression and loss. Br J Psychiatry. 1971;130:1–18. doi: 10.1192/bjp.130.1.1. [DOI] [PubMed] [Google Scholar]
- 15.Birtchnell J. The relationship between attempted suicide, depression and parent death. Br J Psychiatry 1970;116:307-13. [DOI] [PubMed]
- 16.Parkes CM. Bereavement: studies of grief in adult life. Harmondsworth: Penguin; 1986. [Google Scholar]
- 17.Rosenheim E, Reicher R. Informing children about a parent’s terminal illness. J Child Psychol Psychiatry. 1985;26:995–998. doi: 10.1111/j.1469-7610.1985.tb00613.x. [DOI] [PubMed] [Google Scholar]
- 18.Dyregrov A. Grief in childhood; a handbook for adults. London: Jessica Kingsley; 1991. [Google Scholar]
- 19.Heegaard M. When someone very special dies—children can learn to cope with grief. Minneapolis: Woodland; 1991. [Google Scholar]
- 20.Heegaard M. When something terrible happens—children can learn to cope with grief. Minneapolis: Woodland; 1991. [Google Scholar]


