The introduction of techniques for treating infertility have given real hope to those who have been unable to have children. It is therefore prudent to review our management of these patients, to be aware of the likelihood of success and to carry out only those investigations and treatments that are likely to be of benefit.
Summary points
Investigation of infertility should include both partners, and ideally the same general practitioner should be involved with each partner
It is good practice to consider the welfare of the future child as well as the needs of the couple
Duration of infertility and age of female partner are the most important factors when making a prognosis for treatment
Early referral for specialist assessment is indicated if there is a specific problem or when the female partner is aged over 35 years
Semen analysis should be carried out in all cases, and if the result is abnormal it should be repeated
General advice should be given to all couples on, for example, folic acid supplements, rubella immunity, and stopping smoking
Methods
For this review, we made extensive use of background material from a major consultation process commissioned by the European Society for Human Reproduction, in which TBH was involved,1 and also used the review of effective health care itself.1 We have both worked for more than 10 years in the field, and we used our experience to include those aspects of infertility practice relevant to general practitioners and primary care physicians.
When to refer for specialist assessment
If a couple have not conceived within three years of stopping contraception then the chance of a spontaneous (treatment independent) pregnancy in the next year is not more than 25% irrespective of the results of semen analysis (table 1), and it is therefore appropriate to refer them to a specialist clinic. If the female partner is aged over 35 years there is a substantial fall in the chance of success with in vitro fertilisation.5 Since it takes time to complete the investigations necessary before in vitro fertilisation, it is appropriate to refer a couple immediately when the female partner is aged over 35 and the couple have been attempting conception for more than a year. Other patients who should be referred early to a specialist clinic include those with amenorrhoea or gross menstrual irregularity and those with a history of significant pelvic inflammation.
Table 1.
Percentage chance of spontaneous conception leading to live birth in next year according to duration of involuntary infertility and man’s motile sperm concentration*
| Sperm concentration† | Duration of involuntary infertility (months)
|
|||
|---|---|---|---|---|
| 12 | 24 | 48 | 96 | |
| Azoospermia | 0 | 0 | 0 | 0 |
| 0 | 0 | 0 | 0 | 0 |
| 0.5 | 16 | 12 | 9 | 6 |
| 1 | 25 | 19 | 14 | 9 |
| 2 | 34 | 26 | 19 | 13 |
| 5 | 36 | 28 | 21 | 14 |
| ⩾10 | 37 | 28 | 21 | 14 |
Assuming that female partner has spontaneous ovulation and patent fallopian tubes and aged under 35. Data derived from mathematical model based on follow up of 876 couples during 1978-83 (Hargreave and Elton2 3). Although more complex models have been published,4 the above model is practical to apply.
Millions of motile sperm/ml.
Clinical examination
The female partner
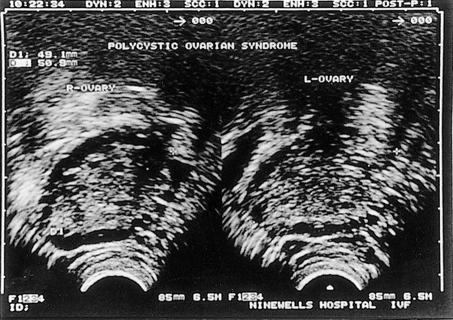
Clinical examination may reveal vaginal infection, which should obviously be treated, and it is worth bearing in mind that any form of ablative treatment for abnormal cervical smears may result in cervical stenosis. Bimanual examination may reveal fibroids or an ovarian cyst, and tenderness may indicate endometriosis. Polycystic ovarian syndrome may be associated with hirsutism and acne. Galactorrhoea with menstrual irregularity suggests hyperprolactinaemia.
The male partner
Men with abnormal semen analysis should be examined. Phimosis and balanitis can cause an infected ejaculate and may interfere with in vitro fertilisation, and circumcision is indicated. It is useful to note testicular size and consistency. Small soft testicles indicate damage to spermatogenesis. Any hard lump within the body of the testis should raise the possibility of a testicular tumour. It is important to remember the association between infertility, maldescended testes, and testicular tumour6 and that testicular tumour, although rare, is the commonest malignancy in men aged 15-45. Varicoceles will be found in about 25% of men seeking assessment for infertility, and there is conflicting evidence about the efficacy of treatment.7 For men aged over 30, the fertility benefits of treatment are minimal.
Investigations in general practice
The female partner
Ovulation
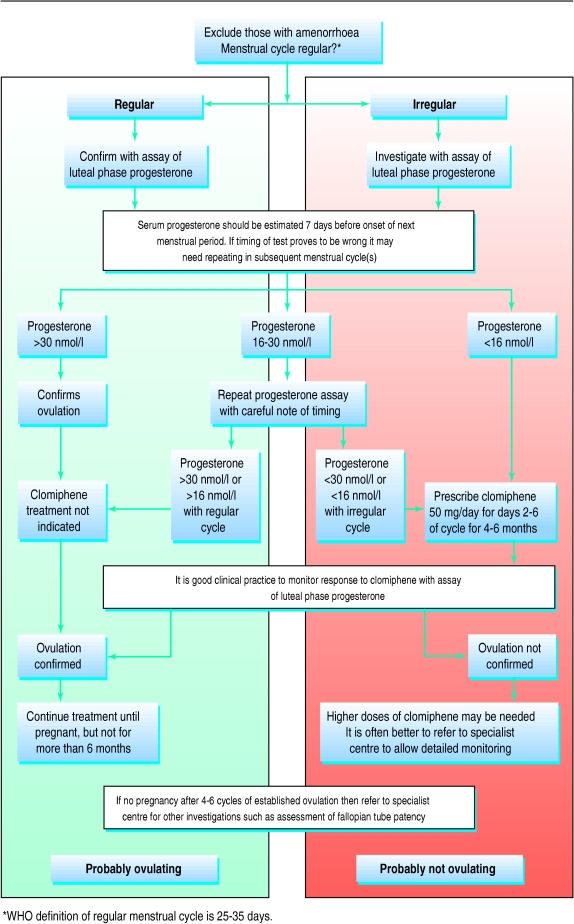
—The most common problem is irregularity of ovulation. This is often seen in the first few months after stopping oral contraception and requires no treatment. Simple problems with ovulation can be treated in general practice (fig 1). For those anovulatory patients who are referred, it is helpful to send blood samples to measure concentrations of follicle stimulating hormone, luteinising hormone, prolactin, oestradiol, and testosterone (table 2).
Figure 1.
Managing simple problems with ovulation. Women with anovulation, excluding ovarian failure (amenorrhoea alone), will achieve normal rates of pregnancy with appropriate treatment. Women with oligomenorrhoea usually have polycystic ovarian syndrome and their pregnancy rates approach normal. (Reproduced with permission of Professor M Hull)
Table 2.
Normal serum concentrations of sex hormones in women of childbearing age and changes associated with conditions causing female infertility*
| Concentration in conditions causing infertility
|
|||||
|---|---|---|---|---|---|
| Hormone | Normal concentration | Ovarian failure | Hypothalamic or pituitary failure | Hyperprolactinaemia | Polycystic ovarian syndrome |
| FSH | 1.0-9.6 IU/l | Increased (>25 IU/l) | Decreased | Normal | Normal |
| LH | 0.8-12.0 IU/l | Increased (>25 IU/l) | Decreased | Normal | Normal or increased |
| LH:FSH ratio | About 1:1 | Normal | Normal | Normal | Often >2.5:1 |
| Prolactin | 50-600 mU/l | Normal | Normal | Increased | Normal or increased |
| Oestradiol | 70-630 pmol/l | Decreased | Decreased | Decreased | Normal |
| Androstenedione | 2-10 nmol/l | Normal | Normal | Normal | Increased |
| Testosterone | 1-3 nmol/l | Normal | Normal | Normal | Increased |
FSH=follicle stimulating hormone, LH=luteinising hormone.
Data from Department of Biochemical Medicine, Ninewells Hospital, Dundee.
Rubella
—It is traditional to check the patient’s rubella status. For those who require immunisation the Department of Health currently advises avoidance of pregnancy for one month after immunisation.8
The male partner
Seminal analysis
—It is sufficient in general practice to note the sperm concentration and motility and volume of ejaculate. It is best to use a laboratory service that participates in the British quality control scheme (NEQAS). A source of confusion is the normal values for semen measurements published by World Health Organisation (⩾20 million sperm/ml and 60% progressive motility); these are derived by comparing results from normal and infertile populations, but they do not give good information about prognosis (table 1). If the results of the first semen analysis are poor then it is worth repeating. If no sperm are seen then referral is indicated. Careful physical examination of men with a low volume azoospermic ejaculate may reveal an absence of the vas deferens, which is associated with carrier status for cystic fibrosis.
Both partners
Chlamydia trachomatis
—Infection can now be diagnosed from a first void urine sample in both sexes.9
General advice
Folic acid
—All women should be encouraged to take prophylactic folic acid while trying for pregnancy and during the first 12 weeks in order to reduce the risk of spina bifida in the baby.
Smoking
—Both partners should be encouraged to give up smoking to reduce risk during early pregnancy. There is evidence that smoking reduces fertility.10
Prescribed drugs
—A detailed drug history should be taken. Drugs best avoided by men include sulphasalazine (use 5-aminosalicylic acid),11 nitrofurantoin, tetracycline, and colchicine. Cancer chemotherapy is likely to damage spermatogenesis, and sperm banking should be offered before treatment is started.
Misuse of drugs
—There is a well documented association between male infertility and the use of anabolic steroids by body builders. This is usually reversible once self medication is stopped. Alcoholic men with cirrhosis have fertility problems, but there is little evidence of any substantial fertility problem associated with misuse of cocaine or marihuana.
Obesity
—Pregnancy rates are reduced in women who are obese, and weight reduction should be advised for all women with a body mass index greater than 30.12
Scrotal temperature
—Showers and sauna baths do not increase the intrascrotal temperature, but soaking in a hot bath should be avoided by men.13
Frequency and timing of intercourse
—There is no evidence that attempts to time intercourse in the menstrual cycle will result in improved conception rates, and it is stressful.14 Couples should continue their normal sexual habit and not to resort to the use of temperature charts or kits for detecting luteinising hormone in the urine.
Specialist centre investigation and treatments
Oligomenorrhoea or amenorrhoea
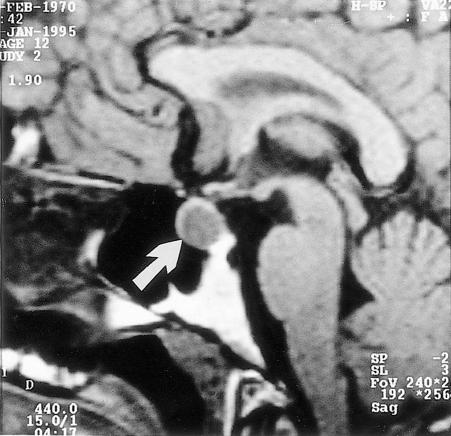
Patients can be treated with appropriate drugs and will achieve pregnancy at the same rate as normally fertile women, unless the basis for anovulation is that of ovarian failure such as premature menopause or gonadal dysgenesis (fig 1). Commonly used treatments include dopamine agonists for hyperprolactinaemia (fig 2), clomiphene, follicle stimulating hormone, and ovarian diathermy for polycystic ovarian syndrome (fig 3). The rarer case of pituitary failure can be treated successfully with replacement of follicle stimulating hormone or with gonadotrophin releasing hormone.
Figure 2.
Nuclear magnetic resonance scan of microadenoma of the pituitary. This is a rare disorder, but appropriate treatment with bromocriptine results in normal rates of pregnancy, with no increase in multiple pregnancy or complications
Figure 3.
Ultrasound scan of ovary with follicles around periphery, characteristic appearance of polycystic ovarian syndrome. This is the commonest endocrine disorder in women and can be successfully treated with clomiphene, gonadotrophin therapy, or ovarian diathermy. Diagnosis of syndrome is based on ultrasound scan and hormone changes, which may include rise in androgens and luteinising hormone
Assessment of fallopian tube patency
Tubal patency is best assessed by laparoscopy and dye hydrotubation: this allows visualisation not only of the tubes but also of the ovaries and will reveal any pelvic adhesion or endometriosis. Hysterosalpingography is a useful alternative, particularly for those for whom laparoscopy is contraindicated. For couples who will require in vitro fertilisation or intracytoplasmic sperm injection because of male infertility, there is generally no need to test fallopian tube patency.
Surgery for female infertility
The advent of assisted conception has altered the indications for surgical procedures, and these are much less commonly performed. Surgery is still indicated in some cases of endometriosis and to divide adhesions.
Assisted conception
In vitro fertilisation was initially used to overcome infertility associated with fallopian tube occlusion, and now it has replaced most fallopian tube surgery. More recently, it was realised that, by placing sperm close to egg, in vitro fertilisation is an effective treatment for male infertility associated with reduced number of motile sperm. This has led to the development of effective treatments for extreme oligozoospermia by recovery of sperm from the epididymis (percutaneous epididymal sperm aspiration) and testicle (testicular sperm aspiration) and direct injection of a single sperm into the egg (intracytoplasmic sperm injection).
The success rate of in vitro fertilisation and intracytoplasmic sperm injection exceeds that of normal conception in a fertile couple in a month. The likelihood of pregnancy for a particular couple using assisted conception depends greatly on the woman’s age and the duration of infertility5; it may range from 8% to 25% for each treatment cycle started, but it is worth bearing in mind that some treatment cycles will be abandoned because of poor response to stimulation. If a couple have an opportunity for three treatment cycles then the cumulative pregnancy rate will reach 50%,15 and couples should be encouraged to plan for three cycles of treatment.
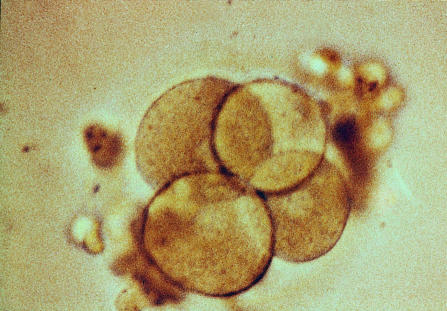
It is customary to transfer more than one embryo to the uterus to increase the chance of at least one embryo implanting; the risk of multiple pregnancies must be balanced with the chance of achieving a pregnancy at all (fig 4). It is not appropriate to replace more than two embryos in women under the age of 37. High multiple pregnancies are much more likely to be the result of inappropriate ovulation induction in polycystic ovarian syndrome than they are of in vitro fertilisation and embryo transfer.
Figure 4.
Human embryo at four cell stage 48 hours after fertilisation. Two or three embryos will be transferred to uterine cavity at this stage
Complications
—Ovarian hyperstimulation syndrome is the most common complication of assisted conception and occurs in 3-5% of treatment cycles (fig 5). This may present in a mild case as lower abdominal discomfort and distension with some nausea, or in a more severe case with quite marked abdominal pain, abdominal distension, ascites, pleural effusion, and even venous thrombotic episodes. Treatment in a specialist unit is appropriate, and any unit offering ovulation induction or assisted conception should ensure that information leaflets are given to the patients and their general practitioners to cover this problem.
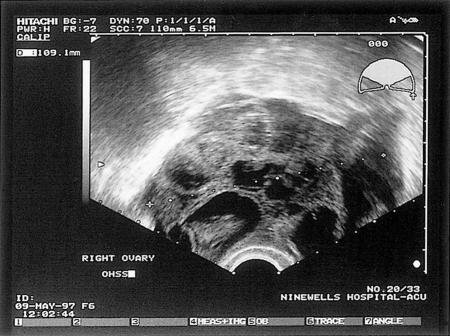
Figure 5.
Abdominal ultrasound scan of patient with ovarian hyperstimulation syndrome showing ovary 10.9 cm in diameter. This common side effect (10%) of in vitro fertilisation is associated with ovarian enlargement and discomfort and may result in occasional ascites and pleural effusion and, rarely, venous thromboembolism. It is more common in treatment cycles that result in pregnancy, and if it is anticipated it would be appropriate to freeze all fertilised embryos and carry out embryo transfer only when overstimulation has settled
Risks to the child
—Recent analysis of births after intracytoplasmic sperm injection suggest that there may be a small rise in congenital abnormalities,16 but this is controversial. There is a small increase in the frequency of abnormalities in sex chromosomes in babies conceived with this technique. There is also evidence that 0-20% of men with greatly reduced sperm counts may have microdeletions on the long arm of the Y chromosome, and it is likely that these will be passed on to any sons born as a result of these techniques and that these sons may in turn have impaired fertility.17
Reversal of sterilisation
Successful reversal of vasectomy or of tubal ligation may be anticipated in 50-60% of cases provided that the partner’s fertility is normal. If the partner also has problems then assisted conception will almost certainly be more cost effective.
Donor gametes
The number of couples seeking donor insemination is falling as they turn to intracytoplasmic sperm injection to try to have their own child. Donor oocytes may be used with in vitro fertilisation to enable women with ovarian failure to bear a child. This can be appropriate for women with gonadal dysgenesis, a premature menopause, or iatrogenic ovarian failure after chemotherapy or radiotherapy for malignancy.
Surrogacy
The role of surrogacy is currently being reviewed. In the United Kingdom it is illegal to enter into any commercial surrogacy arrangement.
References
- 1.Infertility revisited: the state of the art today and tomorrow. The ESHRE Capri workshop. Hum Reprod. 1996;11:1779–1808. [PubMed] [Google Scholar]
- 2.Hargreave TB, Elton RA. Is conventional sperm analysis of any use? Br J Urol. 1983;55:774–779. doi: 10.1111/j.1464-410x.1983.tb03424.x. [DOI] [PubMed] [Google Scholar]
- 3.Hargreave TB, Elton RA. Fecundability rates from an infertile population. Br J Urol. 1986;58:194–197. doi: 10.1111/j.1464-410x.1986.tb09025.x. [DOI] [PubMed] [Google Scholar]
- 4.Collins JA. Unexplained infertility: a review of diagnosis, prognosis, treatment efficacy and management. Int J Gynaecol Obstet. 1992;39:267–275. doi: 10.1016/0020-7292(92)90257-j. [DOI] [PubMed] [Google Scholar]
- 5.Templeton A, Morris JK, Parslow W. Factors that affect outcome of in vitro fertilisation treatment. Lancet. 1996;343:1402–1406. doi: 10.1016/S0140-6736(96)05291-9. [DOI] [PubMed] [Google Scholar]
- 6.Swerdlow AJ, Higgins CD, Pike MC. Risk of testicular cancer in cohort of boys with cryptorchidism. BMJ. 1997;314:1507–1511. doi: 10.1136/bmj.314.7093.1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hargreave TB. Varicocele: overview and commentary on the results of the World Health Organisation varicocele trial. In: Waites GMH, Frick J, Baker GWH, editors. Current advances in andrology. Bologna, Italy: Letosei-Rastignano; 1997. [Google Scholar]
- 8.Department of Health. Immunisation against infectious disease. London: HMSO; 1996. pp. 193–202. [Google Scholar]
- 9.Østergaard L, Moller JK, Andersen B, Olesen F. Diagnosis of urogenital Chlamydia trachomatis infection in women based on mailed samples obtained at home: multipractice comparative study. BMJ. 1996;313:1186–1189. doi: 10.1136/bmj.313.7066.1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Howe G, Westhoff C, Vessey M, Yeates D. Effects of age, cigarette smoking, and other factors on fertility: findings in a large prospective study. BMJ. 1985;290:1697–1700. doi: 10.1136/bmj.290.6483.1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marmor D. The effects of sulphasalazine on male fertility. Reprod Toxicol. 1995;9:219–223. doi: 10.1016/0890-6238(95)00002-r. [DOI] [PubMed] [Google Scholar]
- 12.Reid RL, Van Vugt DA. Weight-related changes in reproductive function. Fertil Steril. 1996;48:905–913. doi: 10.1016/s0015-0282(16)59581-8. [DOI] [PubMed] [Google Scholar]
- 13.Brindley GS. Deep scrotal temperature and the effect on it of clothing, air temperature, activity, posture and paraplegia. Br J Urol. 1982;54:49–55. doi: 10.1111/j.1464-410x.1982.tb13510.x. [DOI] [PubMed] [Google Scholar]
- 14.Kopitzke EJ, Berg BJ, Wilson JF, Owens D. Physical and emotional stress associated with components of infertility investigations: perspectives of professionals and patients. Fertil Steril. 1991;55:1137–1143. doi: 10.1016/s0015-0282(16)54365-9. [DOI] [PubMed] [Google Scholar]
- 15.Tan SL, Royston P, Campbell S, Jacobs HS, Betts J, Mason B, et al. Cumulative conception and live birth rates after in vitro fertilisation. Lancet. 1992;339:1390–1394. doi: 10.1016/0140-6736(92)91205-m. [DOI] [PubMed] [Google Scholar]
- 16.Kurinczuk J, Bower C. Birth defects in infants conceived by intracytoplasmic sperm injection: an alternative interpretation. BMJ. 1997;315:1260–1266. doi: 10.1136/bmj.315.7118.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cooke H, Hargreave TB, Elliott D. Understanding the genes involved in spermatogenesis, a progress report. Fertil Steril (in press). [DOI] [PubMed]