Abstract
Background/Aims
In this meta-analysis, we studied the safety and efficacy of endoscopic submucosal dissection (ESD) for colorectal dysplasia in patients with inflammatory bowel disease (IBD).
Methods
Multiple databases were searched, and studies were retrieved based on pre-specified criteria until October 2022. The outcomes assessed were resection rates, procedural complications, local recurrence, metachronous tumors, and the need for surgery after ESD in IBD. Standard meta-analysis methods were followed using the random-effects model, and I2% was used to assess heterogeneity.
Results
Twelve studies comprising 291 dysplastic lesions in 274 patients were included with a median follow-up of 25 months. The pooled en-bloc resection, R0 resection, and curative resection rates were 92.5% (95% confidence interval [CI], 87.9%–95.4%; I2=0%), 81.5% (95% CI, 72.5%–88%; I2=43%), and 48.9% (95% CI, 32.1%–65.9%; I2=87%), respectively. The local recurrence rate was 3.9% (95% CI, 2%–7.5%; I2=0%). The pooled rates of bleeding and perforation were 7.7% (95% CI, 4.5%–13%; I2=10%) and 5.3% (95% CI, 3.1%–8.9%; I2=0%), respectively. The rates of metachronous recurrence and additional surgery following ESD were 10% (95% CI, 5.2%–18.2%; I2=55%) and 13% (95% CI, 8.5%–19.3%; I2=54%), respectively.
Conclusions
ESD is safe and effective for the resection of dysplastic lesions in IBD with an excellent pooled rate of en-bloc and R0 resection.
Keywords: Dysplasia, Endoscopic submucosal dissection, Inflammatory bowel diseases
Graphical abstract
INTRODUCTION
Inflammatory bowel disease (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC), is associated with an increased risk of colorectal cancer (CRC), especially in patients with extensive inflammation and longer disease duration without remission.1,2 Frequent screening colonoscopy and surveillance of colorectal dysplasia in patients with IBD have demonstrated a decreased risk of advanced and interval CRC. However, this entirely depends on identifying and effectively resecting the colorectal dysplasia.3
Endoscopic removal of dysplastic lesions by endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) in IBD can be challenging because of chronic inflammation and extensive submucosal fibrosis. In the past, dysplasia in IBD was managed by surgical resection; however, the emergence of endoscopic resection has reduced the need for surgical intervention.4 Current guidelines recommend surgery to be reserved for endoscopically unresectable and invisible high-grade dysplasia in IBD. The American Society of Gastrointestinal Endoscopy (ASGE) guidelines and the Surveillance for Colorectal Endoscopic Neoplasia Detection and Management in Inflammatory Bowel Disease recommend endoscopic resection of visible dysplastic lesions with distinct borders and absence of submucosal invasion.5,6
EMR may not be effective for large dysplastic lesions (>2 cm), especially with the presence of submucosal invasion or friable mucosa.4,7,8 The ESD technique overcomes the limitations of EMR for dysplastic lesions in IBD by allowing en-bloc resection of lesions, regardless of size and presence of submucosal fibrosis.9-11 It facilitates detailed histological examination of the resected lesion and significantly reduces the risk of recurrence.4,8 Evidence regarding the outcomes of ESD for colorectal dysplasia in IBD is limited to smaller retrospective, single-center studies. We conducted this meta-analysis to appraise the current literature regarding the safety and efficacy of ESD for colorectal dysplasia in IBD.
METHODS
Search strategy
Multiple databases, including PubMed, Scopus, Embase, and Cochrane, were comprehensively searched from their inception until October 2022. The search was limited to studies in the English language only, and animal studies were excluded. The search strategy was designed and conducted by an experienced librarian with input from the study’s principal investigator. Keywords and controlled vocabulary were used to search for studies on ESD in patients with IBD. The full literature search strategy is provided in Supplementary Material 1. Reference lists of articles were analyzed to identify studies missed on the initial search. Preferred reporting items in meta-analysis,12 and meta-analysis of observational studies checklists were followed,13 and are summarized in Supplementary Materials 2 and 3.
Study selection
Studies reporting outcomes of ESD for colorectal dysplasia in patients with IBD; comprising UC, CD, or both UC and CD; and with appropriate data including resection and adverse event rate regardless of study setting, geographical location, or follow-up period were included.
Studies were excluded based on the following criteria: (1) involving animal subjects, (2) involving patients aged <18 years, (3) not published in the English language, (4) involving hybrid ESD, (5) with a sample size of less than five, and (6) not published as full manuscripts (abstract or conference proceedings). Two reviewers carefully reviewed each study for eligibility based on the above-mentioned criteria. The authors were contacted by e-mail for any clarifications regarding study data.
Data extraction
Data extraction was performed by two reviewers (TFM and VS), and a third author analyzed the data (BPM). Data regarding study and patient characteristics and outcomes were extracted onto a standardized form. In case of any discrepancy, a consensus was achieved by discussion with the senior author (GSK). Authors of the included studies were contacted by e-mail if further information on study data was needed.
Outcome assessment
We assessed the following outcomes: pooled rates of en-bloc resection, R0 resection, curative resection, adverse events (bleeding and perforation), local and metachronous recurrence, and additional surgery after ESD. Based on data availability and feasibility, predetermined subgroup analyses were planned based on the IBD type (UC, CD, and UC+CD), study sample size (<20 or >20), and geography (United States [US], Asia, and others). Meta-regression was planned based on lesion location (right or left), morphology (polypoid or nonpolypoid), lesion border (distinct or indistinct), and surrounding mucosa (remission or active) to assess potential causes of heterogeneity and predictors of clinical outcomes.
1) Assessment of methodology and definitions
The quality of each study was assessed using the Newcastle-Ottawa scale for cohort studies.14 Two authors assessed and scored each study independently (TFM and VS). Details of the individual study scoring are provided in Supplementary Table 1.
Data on resection, recurrence, and adverse event rates were collected from the original studies. En-bloc resection was defined as the complete removal of the lesion in one piece. The pooled rate of R0 resection was defined as the complete removal of the lesion with negative histological margins. Variability was observed with the definition of ‘curative resection’. The most consistent definition for ‘curative resection’ was when pathological findings revealed R0 resection without any of the following features: submucosal deep invasion (≥1,000 μm), lymphovascular involvement, or poorly differentiated adenocarcinoma component. Bleeding and perforation events, as reported in the original studies, were considered adverse events. Local recurrence was defined as the presence of dysplastic lesion at the resection site during follow-up colonoscopy. Metachronous tumor was defined as a new lesion detected in a colorectal area, other than the primary lesion site, more than six months following ESD.
Statistical analysis
We used meta-analysis techniques, particularly the random-effects model, to calculate the pooled estimates in each case following the methods suggested by DerSimonian and Laird. When the incidence of an outcome was zero in a study, a continuity correction of 0.01 was added to the number of incident cases before statistical analysis. Pooled proportions with corresponding 95% confidence intervals (CIs) were calculated for categorical outcomes, and pooled mean differences were calculated for continuous outcomes. We assessed heterogeneity between study-specific estimates using the Cochran Q statistical test for heterogeneity; 95% prediction interval (PI), which deals with the dispersion of the effects; and I2 statistics. We considered values of <30%, 30% to 60%, 61% to 75%, and >75% to indicate low, moderate, substantial, and considerable heterogeneity, respectively. Publication bias was ascertained qualitatively via visual inspection of the funnel plot and quantitatively using the Egger test. All analyses were performed using the Comprehensive Meta-Analysis (CMA) software ver. 4 (BioStat).
RESULTS
Search results and population characteristics
The initial search generated 103 studies, of which 47 duplicates were removed and 56 studies were screened and fully assessed. Twelve studies were included in the final analysis.15-26 The schematic flow diagram for the study selection process is illustrated in Supplementary Figure 1.
A total of 291 dysplastic lesions were removed by ESD in 274 patients. The median age was 62 years (interquartile range, 54–65). Of the patients, 56% were male (n=167), and 44% were female (n=132). The mean lesion size was 28.6 (18.3–40.7) mm. Approximately 77.3% of lesions were in the left colon (n=184), 80.7% were nonpolypoid (n=192), and 73.2% had submucosal fibrosis (n=161). The overall mean procedure time was 72.7 (95% CI, 53.2–92.2) minutes (Supplementary Fig. 2). The median study follow-up time was 25 months. Further study and baseline patient characteristics and study outcomes are summarized in Tables 1 and 2, respectively.15-26
Table 1.
Study and population characteristics
| Study | Study details | Patients (n) | Sex (M/F) | Median age (y) | UC duration (y) | Colitis extent (E/L/P) | Lesions (n) | Mean size (mm) | Location (n, R/L) | Morphology (n, P/NP) | Border (n, distinct/indistinct) | Surrounding mucosa (n, R/A) | Submucosal fibrosis (n, present/absent) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Iacopini et al. (2015)15 | Prospective cohort, multicenter, Italy and Japan | 9 | 4/5 | 62 | 13 | 6/ 3/ 0 | 10 | 36.3 | 2/8 | 0/10 | 10/0 | 10/0 | 9/1 |
| Kasuga et al. (2021)16 | Retrospective cohort, single-center, Japan | 9 | 4/5 | 65 | 20 | 7/0 /2 | 11 | 30 | 3/8 | 3/8 | 11/0 | NA | 11/0 |
| Kochhar et al. (2018)17 | Prospective cohort, single-center, Cleveland OH | 7 | 5/2 | 54 | NA | NA | 7 | 40.7 | 5/2 | 1/6 | NA | NA | NA |
| Kinoshita et al. (2019)18 | Retrospective cohort, multicenter, Japan | 25 | 18/7 | 62 | 19 | 19/3/3 | 25 | 21.6 | 8/17 | 5/20 | 25/0 | 25/0 | 25/0 |
| Lightner et al. (2021)19 | Retrospective cohort, single-center, Cleveland OH | 25 | 19/6 | 63 | 20.5 | 6/9/0 | 25 | 30 | 14/11 | 25/0 | NA | 7/18 | NA |
| Matsumoto et al. (2021)20 | Retrospective, case control, single-center, Japan | 7 | 5/2 | 55 | 15 | 4/2/1 | 12 | 18.3 | 0/12 | 2/10 | 12/0 | 10/2 | 12/0 |
| Manta et al. (2021)21 | Prospective cohort, multicenter, Italy | 53 | 31/22 | 65 | 17 | 30/23/0 | 53 | 34 | NA | NA | NA | 53/0 | 29/24 |
| Matsui et al. (2021)22 | Retrospective, case control, single-center, Japan | 12 | 6/6 | 59 | 20 | 10/2/0 | 17 | 25.1 | 2/15 | 1/16 | 17/0 | NA | 1/16 |
| Ngamruengphong et al. (2022)23 | Retrospective, cohort, multicenter, United States | 41 | 25/41 | 60.4 | 25 | NA | 45 | 30 | 7/38 | 2/43 | NA | NA | 33/12 |
| Nishio et al. (2021)24 | Retrospective, case control, single-center, Japan | 39 | 22/17 | 56 | 17 | 30/0/9 | 39 | 19 | 12/27 | 4/35 | 39/0 | 39/0 | NA |
| Suzuki et al. (2017)25 | Retrospective cohort, multicenter, United Kingdom and Japan | 32 | 18/14 | 65 | 20 | NA | 32 | 33 | 0/32 | 2/30 | 32/0 | 29/3 | 31/1 |
| Yang et al. (2019)26 | Retrospective case control, single-center, Korea | 15 | 10/5 | 60 | 14 | 12/2/0 | 15 | 26.5 | 1/14 | 1/14 | 15/0 | 15/0 | 10/5 |
M, male; F, female; UC, ulcerative colitis; E, extensive; L, left-sided; P, proctitis; R, right; L, left; P, polypoid; NP, nonpolypoid; R, reactive; A, active; NA, not applicable.
Table 2.
Study outcomes
| Study | Median follow-up (mo) | Mean procedure time (min) | En-bloc resection (n) | R0 resection (n) | Curative resection (n) | Bleeding | Perforation | Local recurrence (n) | Metachronous tumors (n) | Additional surgery after ESD (n) | Histopathology (n) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Iacopini et al. (2015)15 | 24 | 75.3 | 8 | 8 | 7 | 1 | 0 | 0 | 0 | 1 | SSA 1, LGD 4, HGD 3, adenocarcinoma 2 |
| Kasuga et al. (2021)16 | 25 | 95 | 10 | 9 | 9 | 3 | 0 | 0 | 2 | 1 | LGD 6, HGD 2, SSP/A 2, adenocarcinoma 1 |
| Kochhar et al. (2018)17 | 6 | NA | 6 | NA | NA | 0 | 0 | 0 | NA | 1 | LGD 3, HGD 2, IND 2 |
| Kinoshita et al. (2019)18 | 21 | 71.1 | 25 | 19 | 14 | 0 | 1 | 0 | 1 | 5 | LGD 19, HGD 7, adenocarcinoma 4, regenerative atypia 2 |
| Lightner et al. (2021)19 | 19 | 41 | 23 | 23 | NA | 0 | 1 | 0 | 0 | 10 | LGD 8, HGD 9, adenocarcinoma 3 |
| Matsumoto et al. (2021)20 | 180 | 55 | 10 | 8 | 8 | 0 | 0 | 0 | 5 | 4 | LGD 9, HGD 3 |
| Manta et al. (2021)21 | 37 | NA | 53 | 51 | 51 | 7 | 3 | 0 | 2 | 2 | LGD 37, HGD 14, IND 1, hyperplastic polyp 1 |
| Matsui et al. (2021)22 | 25 | 155 | 17 | 12 | 12 | 0 | 0 | 0 | 1 | 1 | Adenoma 2, LGD 4, HGD 4, adenocarcinoma 7 |
| Ngamruengphong et al. (2022)23 | 18 | 93 | 43 | 34 | 3 | 4 | 1 | 1 | 11 | 2 | LGD 28, HGD 9, SSA/P 4, adenocarcinoma 4 |
| Nishio et al. (2021)24 | 37 | 67 | 38 | 38 | 38 | 0 | 4 | 0 | 2 | 4 | LGD 17, HGD 13, serrated polyps 9 |
| Suzuki et al. (2017)25 | 33 | 87 | 29 | 23 | NA | 1 | 0 | 1 | 3 | 4 | LGD 19, HGD 7, adenocarcinoma 4, regenerative atypia 2 |
| Yang et al. (2019)26 | 25 | 73.5 | 14 | 12 | NA | 0 | 0 | 2 | 2 | 2 | SSA/P 1, IND 1, LGD 8, HGD 3, adenocarcinoma 2 |
ESD, endoscopic submucosal dissection; SSA, sessile serrated adenoma; LGD, low-grade dysplasia: HGD, high-grade dysplasia; IND, indefinite dysplasia; SSA/P, SSA/polyp; NA, not applicable.
Characteristics and quality of included studies
Three studies were prospectively conducted,15,17,21 and five studies were multicenter studies.15,18,21,23,25 The assessment of study quality is detailed in Supplementary Table 1. Overall, two studies were considered high quality, and ten studies were medium quality. No low-quality studies were identified.
Meta-analysis outcomes
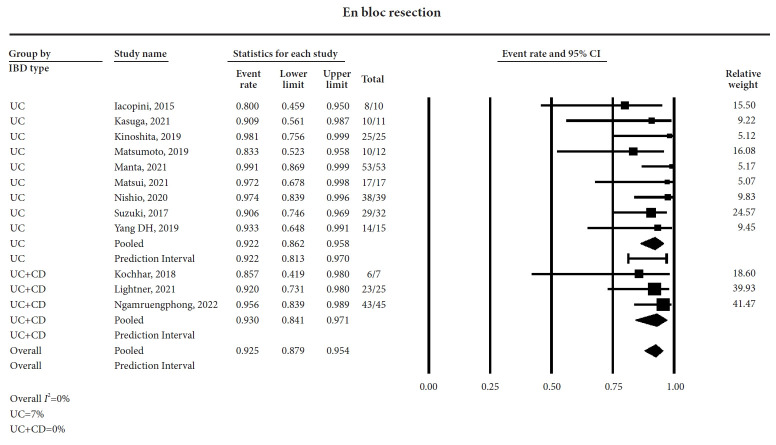
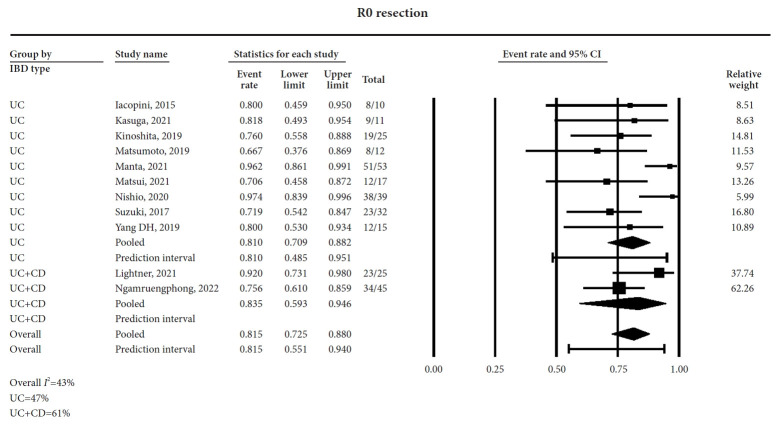
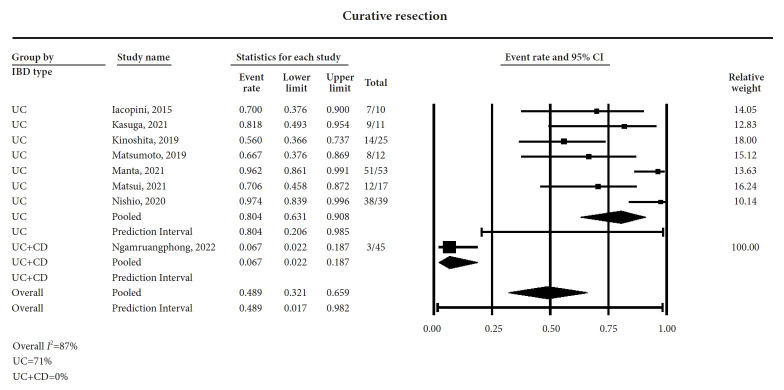
ESD was performed for a total of 291 dysplastic lesions in 274 patients with IBD. The pooled rates of en-bloc, R0, and curative resections were 92.5% (95% CI, 87.9%–95.4%; I2=0%) (forest plot, Fig. 1), 81.5% (95% CI, 72.5%–88%; I2=43%) (Forest plot, Fig. 2), and 48.9% (95% CI, 32.1%–65.9%; I2=87%) (forest plot, Fig. 3), respectively. The local recurrence and metachronous recurrence rates were 3.9% (95% CI, 2%–7.5%; I2=0%) (forest plot, Supplementary Fig. 3) and 10% (95% CI, 5.2%–18.2%; I2=55%) (forest plot, Supplementary Fig. 4), respectively.
Fig. 1.
Forest plot for en-bloc resection. IBD, inflammatory bowel disease; CI, confidence interval; UC, ulcerative colitis; CD, Crohn’s disease.
Fig. 2.
Forest plot for R0 resection. IBD, inflammatory bowel disease; CI, confidence interval; UC, ulcerative colitis; CD, Crohn’s disease.
Fig. 3.
Forest plot for curative resection. IBD, inflammatory bowel disease; CI, confidence interval; UC, ulcerative colitis; CD, Crohn’s disease.
The rate of additional surgery following ESD was 13% (95% CI, 8.5%–19.3%; I2=54%) (forest plot, Supplementary Fig. 5). The causes for requiring additional surgery after ESD included presence of superficial or submucosal tumor invasion, lymphatic and vascular involvement, metachronous lesions, invasive adenocarcinoma, and medically refractory disease. One patient with severe submucosal fibrosis received surgery after unsuccessful ESD.
The pooled rates of bleeding and perforation were 7.7% (95% CI, 4.5%–13%; I2=10%) (forest plot, Supplementary Fig. 6) and 5.3% (95% CI, 3.1%–8.9%; I2=0%) (forest plot, Supplementary Fig. 7), respectively. When perforation occurred during ESD, it was treated endoscopically using clip placement and did not require surgery. The pooled rates and I2% values are summarized in Table 3.
Table 3.
Summary of pooled rates
| Outcome | Pooled rate (95% confidence interval)/no. of study | I2% heterogeneity |
|---|---|---|
| En-bloc resection | Overall: 92.5 (87.9–95.4)/12 | 0 |
| UC: 92.2 (86.2–95.8)/9 | 7 | |
| UC+CD: 93(84.1–97.1)/3 | 0 | |
| R0 resection | Overall: 81.5 (72.5–88)/11 | 43 |
| UC: 81 (70.9–88.2)/9 | 47 | |
| UC+CD: 83.5 (59.3–94.6)/2 | 61 | |
| Curative resection | Overall: 48.9 (32.1–65.9)/8 | 87 |
| UC: 80.4 (63.1–90.8)/7 | 71 | |
| UC+CD: 6.7 (2.2–18.7)/1 | 0 | |
| Bleeding | Overall: 7.7 (4.5–13)/12 | 10 |
| UC: 7.9 (3.9–15.4)/9 | 26 | |
| UC+CD: 7.5 (3.1–16.7)/3 | 0 | |
| Perforation | Overall: 5.3 (3.1–8.9)/12 | 0 |
| UC: 5.9 (3.3–10.3)/9 | 0 | |
| UC+CD: 3.5 (1–11.5)/3 | 0 | |
| Local recurrence | Overall: 3.9 (2–7.5)/12 | 0 |
| UC: 4.3 (2–9)/9 | 0 | |
| UC+CD: 2.9 (0.7–10.8)/3 | 0 | |
| Metachronous recurrence | Overall: 10 (5.2–18.2)/11 | 55 |
| UC: 10 (5.1–18.6)/9 | 48 | |
| UC+CD: 10.3 (0.8–61.3)/2 | 71 | |
| Additional surgery after ESD | Overall: 13 (8.5–19.3)/12 | 54 |
| UC: 12.8 (8.3–19.4)/9 | 81 | |
| UC+CD: 15.7 (2.9–54)/3 studies | 16 | |
| Procedure time (min) | Overall: 72.7 (53.2–92.2) | 92 |
| Publication bias | Absent (Egger’s 2-tailed p=0.06) |
UC, ulcerative colitis; CD, Crohn’s disease; ESD, endoscopic submucosal dissection.
Subgroup and meta-regression analysis
1) Subgroup analysis based on IBD type (UC only and UC+CD)
In nine studies, ESD for colorectal dysplasia was performed in patients with UC only. Three studies have reported on ESD for colorectal dysplasia in both UC and CD. The en-bloc resection rates were 92.2% (95% CI, 86.2%–95.8%) in studies with UC and 93% (95% CI, 84.1%–97.1%) in studies with UC+CD. The R0 resection rates were 81% (95% CI, 70.9%–88.2%) for UC and 83.5% (95% CI, 59.3%–94.6%) for UC+CD. The rest of the subgroup analyses were limited owing to fewer studies on the UC+CD group. The results are summarized in Table 3.
2) Subgroup analysis based on sample size (<20 or >20) and study geography
Six studies had a sample size of <20 patients. Equally, six studies had a sample size of >20 patients. Three, six, and three studies were conducted within the US, Asia, and outside the US and Asia (Italy and United Kingdom), respectively. The subgroup analysis based on study sample size and geography was primarily performed for sensitivity analysis to ascertain potential contribution toward the observed heterogeneity. The outcomes were comparable in studies performed in the US, Asia, and other regions. The results are summarized in Supplementary Table 2.
A meta-regression analysis was performed based on lesion location (right or left), morphology (polypoid or nonpolypoid), lesion borders (distinct or indistinct), and surrounding mucosa (remission or active). However, statistical analysis was not feasible due to the limited number of studies.
Validation of meta-analysis results
1) Sensitivity analysis
To assess whether any study had a dominant effect on the meta-analysis outcomes, we excluded one study at a time and analyzed its effects on the main summary estimate. In this analysis, no single study significantly affected the outcome or heterogeneity.
2) Heterogeneity
No heterogeneity was noted for the primary outcomes of en-bloc resection, whereas moderate heterogeneity was observed for R0 resection. Overall, heterogeneity was moderate except for curative resection (87%). This was most likely attributable to the lack of a uniform definition for curative resection among the studies. The subgroup analysis demonstrated sample size (<20 vs. >20) as a significant contributor toward the pooled local recurrence. Since the random-effects model was used, the 95% CIs are illustrated in the respective forest plots.
3) Publication bias
No publication bias was noted based on the qualitative assessment of the funnel plot (Supplementary Fig. 8) and quantitatively by Egger’s regression analysis (two-tailed p-value = 0.06).
4) Quality of evidence
The GRADE working group approach was used to rate the quality of evidence for results from this meta-analysis.27 Based on the retrospective nature of included studies and moderate heterogeneity, this meta-analysis would be considered to have low-quality of evidence.
DISCUSSION
In this meta-analysis of twelve studies, ESD demonstrated an excellent pooled en-bloc (92.5%) and R0 (81.5%) resection rate for colorectal dysplasia in patients with IBD. The local recurrence rate was 3.9%, with low pooled rates of adverse events, including bleeding (7.7%) and perforation (5.3%). To the best of our knowledge, with 291 dysplastic lesions in 274 patients with IBD, this study reports the largest pooled data of ESD for colorectal dysplasia in patients with IBD.
The current ASGE guidelines regarding the management of colorectal dysplasia in IBD recommend en-bloc resection by EMR or ESD of endoscopically visible lesions with distinct borders instead of surgery.8 EMR has been associated with a 27%–63% en-bloc resection rate and a 14% to 50% local recurrence rate.11,28,29 In this study, although 73.1% of dysplastic lesions had submucosal fibrosis, ESD demonstrated excellent en-bloc and R0 resection rates along with low rates of local recurrence, perforation, and bleeding.
ESD in patients with IBD can present technical challenges if the submucosal fibrosis is extensive. This is reflected in our study with a metachronous recurrence rate of 20%. Despite this, we demonstrate that the need for surgery was low at 13%, with a curative resection rate of 48.9%. This may be attributed to not all patients with failed resection receiving surgery. Additionally, the rate of curative resection needs to be interpreted with caution as a certain level of variability was observed in how the individual studies defined ‘curative resection’, which also explains the high heterogeneity (87%). The most consistent definition for ‘curative resection’ was when pathological findings revealed R0 resection without any of the following features: submucosal deep invasion (≥1000 μm), lymphovascular involvement, or poorly differentiated adenocarcinoma component. The reported pooled rates are encouraging and highlight the importance of frequent endoscopic surveillance following ESD to monitor for local and metachronous recurrence in patients with IBD.
EMR is increasingly being performed in the US, whereas ESD remains a complex procedure only performed by experienced endoscopists in select IBD centers.30 In our analysis, the pooled mean procedure time was 72.7 minutes, which is comparable to the mean procedure time in ESD for sporadic CRC (75–106 minutes).31,32 As the current literature demonstrates the increasing feasibility of ESD for complex lesions in IBD, we anticipate increased utilization of this technique with additional focused training.
In our subgroup analyses, we observed that pooled rates from studies with a sample size of >20 patients demonstrated lower rates of local recurrence (2% vs 7.3%). Although no studies that were exclusively performed in patients with CD were identified, we noted that the outcomes were slightly better in study samples that included both CD and UC compared to UC alone. Whether this is directly related to the differences in the underlying pathology of CD vs. UC or to the higher risk of dysplastic lesions in UC with varying grades of active inflammation contributing to indistinct lesion borders remains unknown.
A meta-analysis by Mohapatra et al.33 summarized the results of 190 colorectal dysplastic lesions undergoing ESD and revealed an en-bloc resection rate of 85.7% in patients with IBD. Similarly, a meta-analysis by Chen et al.34 demonstrated an en-bloc resection rate of 86% with ESD for non-polypoid dysplasia in patients with IBD. Our study demonstrated a higher en-bloc resection rate (92.5%) than the previous studies which may be attributed to the larger sample size with more recent studies included in our analysis. Recent advances in ESD techniques and emphasis on advanced training may have contributed to these findings.
Our study has several strengths. The literature search was rigorously performed to include studies that used ESD for colorectal dysplasia in IBD. No low-quality studies were identified in this analysis, and no heterogeneity was reported on the primary outcomes of en-bloc and R0 resection. As noted above, although studies reporting outcomes of advanced endoscopic resection techniques for colorectal dysplasia exist, the present study is the most up-to-date meta-analysis specifically evaluating outcomes of ESD technique for colorectal dysplasia in IBD.
This study had some limitations, most of which are inherent to any meta-analysis of retrospective studies with a potential risk of selection bias. Patient-level granular information regarding the severity of disease, extent of disease, and endoscopic remission status at the time of ESD was not available. Furthermore, information regarding the criteria of lesion selection, degree of dysplasia, timing of bleeding (immediate/delayed), and outcomes of patients who did not receive additional surgery after ESD could not be ascertained from all the studies. Additionally, concomitant high-risk features, such as positive family history, prior personal history of high-risk dysplasia, and primary sclerosing cholangitis, were not reported. Nevertheless, the pooled data from this study adds valuable information to the current literature on this topic.
In conclusion, this meta-analysis demonstrates ESD to be safe and effective for colorectal dysplasia in IBD. ESD demonstrates excellent en-bloc and R0 resection rate, with low rates of local recurrence and adverse events. The reported rates of curative resection warrant further studies with uniform definition to validate our findings.
Footnotes
Ethical Statements
Not applicable.
Conflicts of Interest
Mohamed O. Othman is a consultant for Olympus, Boston Scientific, Creo Medical, Lumendi, Abbvie, Nestle, Ambu, and Conmed. Peter V. Draganov is a consultant for Olympus, Fujifilm, Boston Scientific, Microtech, and Medtronic. Gursimran S. Kochhar is on the Advisor board for GIE Medical, Lilly Pharmaceuticals, and Corvetas Research Foundation. Gursimran S. Kochhar is a consultant for Pentax Endoscopy, Boston Scientific Endoscopy and Olympus Endoscopy. Gursimran S. Kochhar is a speaker for Lilly Pharma. The other authors have no potential conflicts of interest.
Funding
None.
Author Contributions
Conceptualization: TFM, BPM, GSK, AUR, MOO, PVD; Data curation: TFM, BPM, VS; Formal analysis: BPM; Investigation: TFM, BPM; Project administration: TFM, BPM; Resources: TFM, BPM; Software: TFM, BPM; Writing–original draft: TFM, BPM; Writing–review & editing: all authors.
Supplementary Material
Supplementary Table 1. Study quality assessment using the Newcastle-Ottawa scale.
Supplementary Table 2. Subgroup sensitivity analyses.
Supplementary Fig. 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart.
Supplementary Fig. 2. Forest plot for procedure time.
Supplementary Fig. 3. Forest plot for bleeding.
Supplementary Fig. 4. Forest plot for perforation.
Supplementary Fig. 5. Forest plot for local recurrence.
Supplementary Fig. 6. Forest plot for metachronous tumors.
Supplementary Fig. 7. Forest plot for additional surgery after endoscopic submucosal dissection.
Supplementary Fig. 8. Funnel plot for publication bias.
Supplementary Material 1. Literature search strategy.
Supplementary Material 2. Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist.
Supplementary Material 3. Meta-analyses of Observational Studies in Epidemiology checklist.
Supplementary materials related to this article can be found online at https://doi.org/10.5946/ce.2023.205.
REFERENCES
- 1.Jess T, Simonsen J, Jørgensen KT, et al. Decreasing risk of colorectal cancer in patients with inflammatory bowel disease over 30 years. Gastroenterology. 2012;143:375–381. doi: 10.1053/j.gastro.2012.04.016. [DOI] [PubMed] [Google Scholar]
- 2.Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001;48:526–535. doi: 10.1136/gut.48.4.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Choi CH, Rutter MD, Askari A, et al. Forty-year analysis of colonoscopic surveillance program for neoplasia in ulcerative colitis: an updated overview. Am J Gastroenterol. 2015;110:1022–1034. doi: 10.1038/ajg.2015.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, et al. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47:829–854. doi: 10.1055/s-0034-1392882. [DOI] [PubMed] [Google Scholar]
- 5.Laine L, Kaltenbach T, Barkun A, et al. SCENIC international consensus statement on surveillance and management of dysplasia in inflammatory bowel disease. Gastroenterology. 2015;148:639–651. doi: 10.1053/j.gastro.2015.01.031. [DOI] [PubMed] [Google Scholar]
- 6.American Society for Gastrointestinal Endoscopy Standards of Practice Committee. Shergill AK, Lightdale JR, et al. The role of endoscopy in inflammatory bowel disease. Gastrointest Endosc. 2015;81:1101–1121. doi: 10.1016/j.gie.2014.10.030. [DOI] [PubMed] [Google Scholar]
- 7.Rutter MD, Riddell RH. Colorectal dysplasia in inflammatory bowel disease: a clinicopathologic perspective. Clin Gastroenterol Hepatol. 2014;12:359–367. doi: 10.1016/j.cgh.2013.05.033. [DOI] [PubMed] [Google Scholar]
- 8.Draganov PV, Wang AY, Othman MO, et al. AGA institute clinical practice update: endoscopic submucosal dissection in the United States. Clin Gastroenterol Hepatol. 2019;17:16–25. doi: 10.1016/j.cgh.2018.07.041. [DOI] [PubMed] [Google Scholar]
- 9.Uraoka T, Parra-Blanco A, Yahagi N. Colorectal endoscopic submucosal dissection in Japan and Western countries. Dig Endosc. 2012;24 Suppl 1:80–83. doi: 10.1111/j.1443-1661.2012.01279.x. [DOI] [PubMed] [Google Scholar]
- 10.Hurlstone DP, Sanders DS, Atkinson R, et al. Endoscopic mucosal resection for flat neoplasia in chronic ulcerative colitis: can we change the endoscopic management paradigm? Gut. 2007;56:838–846. doi: 10.1136/gut.2006.106294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang J, Zhang XH, Ge J, et al. Endoscopic submucosal dissection vs endoscopic mucosal resection for colorectal tumors: a meta-analysis. World J Gastroenterol. 2014;20:8282–8287. doi: 10.3748/wjg.v20.i25.8282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10:89. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 14.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 15.Iacopini F, Saito Y, Yamada M, et al. Curative endoscopic submucosal dissection of large nonpolypoid superficial neoplasms in ulcerative colitis (with videos) Gastrointest Endosc. 2015;82:734–738. doi: 10.1016/j.gie.2015.02.052. [DOI] [PubMed] [Google Scholar]
- 16.Kasuga K, Yamada M, Shida D, et al. Treatment outcomes of endoscopic submucosal dissection and surgery for colorectal neoplasms in patients with ulcerative colitis. United European Gastroenterol J. 2021;9:964–972. doi: 10.1002/ueg2.12118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kochhar G, Steele S, Sanaka M, et al. Endoscopic submucosal dissection for flat colonic polyps in patients with inflammatory bowel disease: a single-center experience. Inflamm Bowel Dis. 2018;24:e14–e15. doi: 10.1093/ibd/izy101. [DOI] [PubMed] [Google Scholar]
- 18.Kinoshita S, Nishizawa T, Yahagi N, et al. Endoscopic submucosal dissection in patients with ulcerative colitis. Digestion. 2019;99:27–32. doi: 10.1159/000494409. [DOI] [PubMed] [Google Scholar]
- 19.Lightner AL, Vaidya P, Allende D, et al. Endoscopic submucosal dissection is safe and feasible, allowing for ongoing surveillance and organ preservation in patients with inflammatory bowel disease. Colorectal Dis. 2021;23:2100–2107. doi: 10.1111/codi.15746. [DOI] [PubMed] [Google Scholar]
- 20.Matsumoto K, Oka S, Tanaka S, et al. Long-term outcomes after endoscopic submucosal dissection for ulcerative colitis-associated dysplasia. Digestion. 2021;102:205–215. doi: 10.1159/000503341. [DOI] [PubMed] [Google Scholar]
- 21.Manta R, Zullo A, Telesca DA, et al. Endoscopic submucosal dissection for visible dysplasia treatment in ulcerative colitis patients: cases series and systematic review of literature. J Crohns Colitis. 2021;15:165–168. doi: 10.1093/ecco-jcc/jjaa158. [DOI] [PubMed] [Google Scholar]
- 22.Matsui A, Hoteya S, Hayasaka J, et al. Real-world experience of endoscopic submucosal dissection for ulcerative colitis-associated neoplasia. Inflamm Intest Dis. 2021;6:70–77. doi: 10.1159/000512292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ngamruengphong S, Aihara H, Friedland S, et al. Endoscopic submucosal dissection for colorectal dysplasia in inflammatory bowel disease: a US multicenter study. Endosc Int Open. 2022;10:E354–E360. doi: 10.1055/a-1783-8756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nishio M, Hirasawa K, Ozeki Y, et al. An endoscopic treatment strategy for superficial tumors in patients with ulcerative colitis. J Gastroenterol Hepatol. 2021;36:498–506. doi: 10.1111/jgh.15207. [DOI] [PubMed] [Google Scholar]
- 25.Suzuki N, Toyonaga T, East JE. Endoscopic submucosal dissection of colitis-related dysplasia. Endoscopy. 2017;49:1237–1242. doi: 10.1055/s-0043-114410. [DOI] [PubMed] [Google Scholar]
- 26.Yang DH, Kim J, Song EM, et al. Outcomes of ulcerative colitis-associated dysplasia patients referred for potential endoscopic submucosal dissection. J Gastroenterol Hepatol. 2019;34:1581–1589. doi: 10.1111/jgh.14623. [DOI] [PubMed] [Google Scholar]
- 27.Puhan MA, Schünemann HJ, Murad MH, et al. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2014;349:g5630. doi: 10.1136/bmj.g5630. [DOI] [PubMed] [Google Scholar]
- 28.Alkandari A, Thayalasekaran S, Bhandari M, et al. Endoscopic resections in inflammatory bowel disease: a multicentre European outcomes study. J Crohns Colitis. 2019;13:1394–1400. doi: 10.1093/ecco-jcc/jjz075. [DOI] [PubMed] [Google Scholar]
- 29.Yadav S, Loftus EV, Jr, Harmsen WS, et al. Outcome of endoscopic resection of colonic polyps larger than 10 mm in patients with inflammatory bowel disease. Endosc Int Open. 2019;7:E994–E1001. doi: 10.1055/a-0953-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yu JX, Lin JL, Oliver M, et al. Trends in EMR for nonmalignant colorectal polyps in the United States. Gastrointest Endosc. 2020;91:124–131. doi: 10.1016/j.gie.2019.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Akintoye E, Kumar N, Aihara H, et al. Colorectal endoscopic submucosal dissection: a systematic review and meta-analysis. Endosc Int Open. 2016;4:E1030–E1044. doi: 10.1055/s-0042-114774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Patel N, Patel K, Ashrafian H, et al. Colorectal endoscopic submucosal dissection: systematic review of mid-term clinical outcomes. Dig Endosc. 2016;28:405–416. doi: 10.1111/den.12597. [DOI] [PubMed] [Google Scholar]
- 33.Mohapatra S, Sankaramangalam K, Lopimpisuth C, et al. Advanced endoscopic resection for colorectal dysplasia in inflammatory bowel disease: a meta-analysis. Endosc Int Open. 2022;10:E593–E601. doi: 10.1055/a-1784-7063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen W, Zhang YL, Zhao Y, et al. Endoscopic resection for non-polypoid dysplasia in inflammatory bowel disease: a systematic review and meta-analysis. Surg Endosc. 2021;35:1534–1543. doi: 10.1007/s00464-020-08225-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1. Study quality assessment using the Newcastle-Ottawa scale.
Supplementary Table 2. Subgroup sensitivity analyses.
Supplementary Fig. 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart.
Supplementary Fig. 2. Forest plot for procedure time.
Supplementary Fig. 3. Forest plot for bleeding.
Supplementary Fig. 4. Forest plot for perforation.
Supplementary Fig. 5. Forest plot for local recurrence.
Supplementary Fig. 6. Forest plot for metachronous tumors.
Supplementary Fig. 7. Forest plot for additional surgery after endoscopic submucosal dissection.
Supplementary Fig. 8. Funnel plot for publication bias.
Supplementary Material 1. Literature search strategy.
Supplementary Material 2. Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist.
Supplementary Material 3. Meta-analyses of Observational Studies in Epidemiology checklist.