Abstract
Introduction
Musculoskeletal disorders affect over a third of the UK adult population and are a common reason for sick leave from work. The aims of this study were to describe the reported provision of work participation support for adults with hand and upper limb conditions by UK hand therapists, and to identify potential training needs in this area.
Methods
A previous survey of the Australian Hand Therapy Association was adapted for the UK. The electronic questionnaire was distributed to members of the British Association of Hand Therapists. Eligible individuals were UK-based occupational therapists or physiotherapists whose role included the assessment and/or treatment of patients ≥18 years with hand or upper limb issues.
Results
There were 123 participants (17% response rate). The most frequently reported work participation interventions were discussing graded return to work and sign-posting patients to speak with their doctor. The Allied Health Professionals Health and Work Report and Fit Note were not regularly used, and respondents reported low levels of confidence in issuing these documents. Barriers to providing work recommendations included a perceived lack of time, skills, knowledge and training. Facilitators included the patient discussing work as a rehabilitation goal.
Conclusion
Development opportunities for UK hand therapists include increasing patient awareness that they can ask for work-related advice and documentation, promoting existing health and work training, developing hand therapy-specific resources, and ensuring access to electronic Fit Notes. International opportunities include the continuation of this survey with a focus on generating exemplar work participation strategies to inform further research.
Keywords: Work participation, fit note, allied health professional health and work report, return to work, hand therapy
Introduction
Musculoskeletal disorders (MSDs) affect more than a third of the UK adult population 1 and comprise over a quarter of all UK surgical interventions. 2 MSDs incorporate a variety of diagnoses, including inflammatory conditions such as rheumatoid arthritis; conditions of musculoskeletal pain, for example osteoarthritis and non-specific arm pain; and trauma, including fractures, tendon and joint injuries. Many individuals who develop MSDs are within working ages and their condition may prevent them from working to their full potential according to their preferences. More than 10% of reported UK sickness absences in 2022 were attributed to musculoskeletal problems, 3 making MSDs the third most common reason for sick leave, after minor illness, and ‘other’, including COVID-19. For individuals claiming UK Employment and Support Allowance (a financial allowance for those with a long-term disability or health condition that affects work participation), 13% had an MSD listed as their primary diagnosis. 4 People from the most deprived quintile of UK society are most likely to report a long-term MSD, 4 and subsequent low work participation may result in further social inequalities and poor health. Conversely, remaining in work, or returning to work after long or short-term sickness absence or unemployment, has been associated with enhanced recovery after illness and improved wellbeing. 5
Supporting people to return to, or remain in, work following injury or other MSD is a key role for occupational therapists and physiotherapists 6 and is an important component of patient-centred care. 7 However, a recent survey of 99 Australian Hand Therapists found that most respondents reported a limited role in return-to-work processes for their patients. 8 Reported barriers to providing work-related recommendations included the perception that this was outside scope of practice, a lack of time within consultations, and experiencing employers who were unwilling to act upon the recommendations. 8 Furthermore, nearly half of respondents were dissatisfied with the quality of the return-to-work programmes that they were able to provide themselves.
In the UK, there are two official documents that occupational therapists and physiotherapists can use to provide work recommendations for their patients: the Allied Health Professional (AHP) Health and Work Report 9 and the Fit Note (Statement of Fitness for Work). 10 Both include the option to indicate that the patient is ‘not fit for work’ or that they ‘may be fit for work’ considering the recommendations provided by the treating clinician. Both include tick boxes for four recommendations: phased return to work, altered hours, amended duties, and workplace adaptations. Additionally, they include space for free-text comments, although this is more structured in the AHP Health and Work Report, with sections specifically for reported difficulties and recommendations or goals. Both forms can be used as evidence to claim occupational sick pay, however only the Fit Note can be used as evidence to claim ill health benefits, such as Statutory Sick Pay or Employment Support Allowance. 11 Fit Notes were initially only certifiable by clinical doctors, but in July 2022, UK legislation was amended to include physiotherapists, occupational therapists, nurses and pharmacists. 10
AHP Health and Work Reports do not appear to be routinely used in either physiotherapy or occupational therapy practice.12,13 Reported barriers to their use in clinical practice include the time needed to complete the document, the format of the form, concerns that employers would not accept the document as legitimate supporting documentation 12 and concerns about potential medicolegal implications. 14 To date, there are no existing data showing the use of Fit Notes within hand therapy or other musculoskeletal services.
This cross-sectional study had two key aims. The first was to describe the reported provision of work participation support for adults with hand and upper limb conditions by UK hand therapists. The second was to identify potential training needs in this area.
Methods
Research team
The research team comprised clinical hand therapists (LN, DC and FS) and work and health researchers (LN, IM and VP).
Survey design and distribution
The lead author developed an electronic survey using Online Surveys (Jisc) based on questions previously described by O’Brien et al. 8 Content and wording was adapted for the UK context, and refined with feedback from the research team and British Association of Hand Therapists (BAHT) Clinical Evidence Committee. Main differences were the removal of questions relating to types of health insurance that are not applicable to the UK, and the addition of specific questions relating to the AHP Health and Work Report and Fit Note. The survey used a cross-sectional design with a combination of tick box and open text questions and was formatted for electronic completion using phone, tablet or computer. There were three sections: (i) general demographics, (ii) information about typical patient caseloads, and (iii) work advice. The full list of questions and response options are provided via the Open Science Framework (OSF) repository. 15 Survey responses were anonymous, and a forced response option was used for tick box questions to prevent missing data.
The survey was launched at the BAHT annual conference (6 October 2023) and emailed to BAHT members as part of the November 2023 e-bulletin. The link was also shared via social media. BAHT membership numbers at the time of the survey were 730 individuals (personal communication, Eve Dunn, BAHT administrative assistant 10/10/23). The target response rate was 100 (∼14%) based on previous practice surveys with individuals from the hand therapy community.8,16–18 Study reporting followed the CROSS recommendations (Checklist for Reporting of Survey Studies, Supplemental File 1). 19
Eligibility
Eligible participants were clinical occupational therapists or physiotherapists practising in the UK who treat adult patients with hand and upper limb conditions. This included both acute trauma and long-term musculoskeletal conditions. This did not include individuals working solely in academic, managerial or leadership roles. Respondents who answered ‘no’ to the following eligibility screening question were directed to the end of the survey: does your role include providing assessment and/or treatment for adult patients (aged 18 or over) with hand or upper limb issues?
Analysis
Quantitative data were analysed using descriptive statistics in R (version 4.3.1, R Core Team 2023). Data processing and analysis was completed by the lead author and reviewed by the co-authors. For continuous variables, data were summarised using mean and standard deviation if normally distributed, and median and interquartile range if skewed. Normality was assessed by comparing mean and median values and through visualisation of the histogram plot with the normal distribution curve. Open text responses were reviewed by the lead author and coded to categorical variables using a content analysis framework and these were reviewed by at least one other author.
Governance and approvals
The study was approved by Queen Mary University of London Research Ethics Committee (QME23.0112) and Guy’s and St Thomas’ NHS Foundation Trust Therapies Audit Committee (15415). Survey distribution through BAHT was approved following review by BAHT Clinical Evidence Committee.
Results
The survey was open from 5 October to 30 November 2023 and yielded 124 responses. One participant was excluded because they did not meet the study eligibility criteria of practising in the UK. The denominator for all results included in this report is therefore 123, unless otherwise specified, giving an estimated response rate of 17%.
Participant demographics
Participant demographics are provided in Table 1. Most respondents were female (87%), occupational therapists (60%), working in the NHS (national health service, 89%) and managing a mixed caseload of patients with traumatic and non-traumatic upper limb conditions (48%). Thirty-one percent of respondents (n = 38) worked in more than one setting, with private practice as the most common additional workplace (n = 21, 82%). Respondents had completed or were working towards a range of post-registration hand therapy-related qualifications, most frequently BAHT accredited hand therapist (46%) and NHS advanced clinical practice qualifications (31%). Fifteen individuals (12%) provided additional information about other qualifications, including BAHT accredited courses, relevant postgraduate certificates and master’s modules.
Table 1.
Participant demographics.
| Respondents (%) n = 123 | |||
|---|---|---|---|
| Gender | Female | 107 (87) | |
| Male | 16 (13) | ||
| Geographical region | England | 106 (86) | |
| Northern Ireland | 2 (2) | ||
| Scotland | 10 (8) | ||
| Wales | 5 (4) | ||
| Clinical background | Occupational therapist | 74 (60) | |
| Physiotherapist | 49 (40) | ||
| Time since qualification | <2 years | 0 | |
| 2-5 years | 9 (7) | ||
| 6-10 years | 18 (15) | ||
| 11-20 years | (34 (28) | ||
| >20 years | 62 (50) | ||
| Years in hand therapy | <2 years | 8 (7) | |
| 2-5 years | 16 (13) | ||
| 6-10 years | 20 (16) | ||
| 11-20 years | 42 (34) | ||
| >20 years | 37 (30) | ||
| Additional qualifications | Completed | Undertaking | |
| Accredited hand therapist (BAHT) | 23 (19) | 33 (27) | |
| Other accredited/certified hand therapist | 5 (4) | 2 (2) | |
| Advanced practice certificate, diploma, master’s | 28 (23) | 10 (8) | |
| Hand therapy master’s | 23 (19) | 12 (10) | |
| PhD or professional doctorate | 3 (2) | 6 (5) | |
| Main work setting | National health service | 110 (89) | |
| Private healthcare (for an employer) | 8 (7) | ||
| Private healthcare (own business) | 0 | ||
| University of other educational setting | 3 (2) | ||
| Military | 2 (2) | ||
| Additional work setting (n = 38, multiple responses allowed) | National health service | 4 | |
| Private healthcare (for an employer) | 20 | ||
| Private healthcare (own business) | 11 | ||
| University or other educational setting | 2 | ||
| Medicolegal | 2 | ||
| Charity | 2 | ||
| Caseload composition | Mainly trauma | 52 (42) | |
| Mainly acquired conditions | 12 (10) | ||
| Roughly equal mix of trauma and acquired conditions | 59 (48) | ||
| Percentage of caseload aged 18-66 years (mean [SD]) | 80 [15.3] | ||
BAHT – British Association of Hand Therapists; ASHT – American Society of Hand Therapists.
Work participation interventions
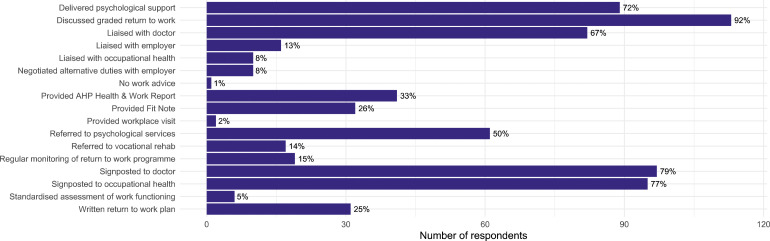
Participants were asked to select all types of work participation support that they had used with their patients in the previous 12 months. Only one respondent reported that they had not provided any work support. The most prevalent interventions were the provision of graded return to work recommendations (92%), signposting to discuss work with the general practitioner, surgeon or other doctor (79%), and signposting to occupational health within the patient’s workplace (77%, Figure 1). A comparison of this data with that reported by O’Brien et al. 8 is provided in Supplementary File 2.
Figure 1.
Reported use of different work participation interventions in the past 12 months.
Work participation assessments
Forty-nine participants (40%) reported that they used specific tools, guidelines or assessments when planning or implementing return to work plans with their patients. Responses were grouped into seven categories: patient-reported outcome measures (n = 15); clinical assessments (n = 15); departmental guidelines, including clinical healing timescales (n = 14); goal setting or discussions based on work requirements (n = 10); documentation for employers (n = 5); and national-level guidelines designed to support patients with MSD in work (n = 4).
Where specified, the patient-reported outcome measures were: Disabilities of the Arm, Shoulder and Hand standard and quick versions (n = 9); 20 Patient Specific Functional Scale (n = 5); 21 Patient Rated Wrist/Hand Evaluation (n = 4); 22 visual or numerical rating scale for pain (n = 3), the Canadian Occupational Performance Measure (n = 1), 23 and the Work Experience Survey-Rheumatic Conditions (n = 1). 24 Clinical assessment methods included grip or pinch strength (n = 12), range of movement (n = 7), dexterity (n = 3), sensation testing (n = 2) and work-specific assessments (n = 4). Four participants reported that the AHP Health and Work Report was a useful tool to documenting work recommendations, and one reported writing letters for employers. Suggested national-level guidance included “National Rheumatoid Arthritis Society booklets - ‘I want to work’ and ‘when an employee has arthritis’”; “wellness action plans for work”; “information from the HSE [Health and Safety Executive] website”; and “defence rehabilitation best practice guidelines”.
Sixty-two individuals (50%) reported that they collected specific data to inform their management of patients’ return-to-work process. Responses were similar to those outlined above and included patient-reported outcome measures (n = 32), clinical assessment (n = 37), assessment of work requirements (n = 10), and patient goals, expectations or feedback (n = 11). Only two individuals reported collecting data on duration of work absence, including return to modified and full duties.
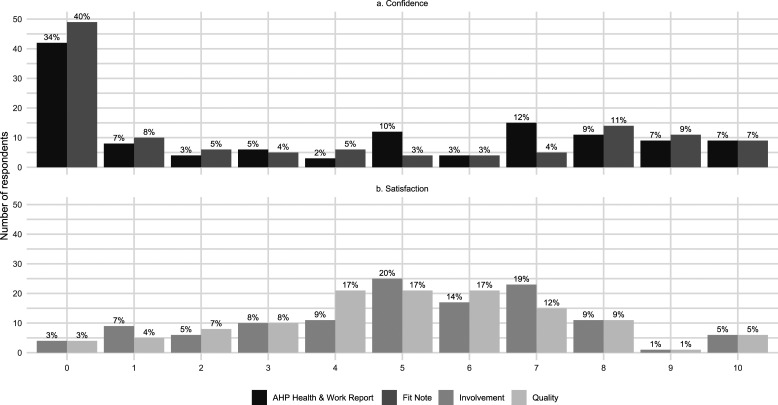
Hand therapist satisfaction
On a numerical rating scale (with 0 representing not at all satisfied and 10 representing completely satisfied), the median level of satisfaction was five for both the amount of involvement in supporting patients with work participation, and the quality of the work participation service that they were able to provide (IQR 4-7 for both questions, Figure 2).
Figure 2.
Reported confidence and satisfaction with work participation activities (a) Confidence in issuing fit notes and AHP (Allied Health Professional) health and work reports. (b) Satisfaction with the amount of involvement in supporting work participation and the quality of the work participation service provided.
AHP health and work reports and fit notes
Twenty-six respondents (21%) had completed the national Fit Note e-learning module, with another 81 (66%) currently working through the training. Thirty-one individuals (25%) reported that they had issued Fit Notes in the past 12 months and 44 (36%) reported that they had issued AHP Health and Work Reports. Fit Note format and relevant policies are shown in Table 2.
Table 2.
Documentation of work guidance and training needs.
| Respondents (%) n = 123 | |
|---|---|
| Issued AHP health and work report in last 12 months | 44 (36) |
| Confidence in completing AHP health and work reports (median [IQR]) | 4 [0-7] |
| Issued fit note in last 12 months | 31 (25) |
| Confidence in completing fit notes (median [IQR]) | 2 [0-8] |
| Fit note format within the organisation | |
| Electronic | 16 (13) |
| Paper | 66 (54) |
| Unsure | 41 (33) |
| Local policy for physiotherapists and occupational therapists to issue fit notes | |
| Able to issue after completing national training | 17 (14) |
| Able to issue after completing national and local training | 11 (9) |
| Able to issue, but not sure of a specific policy | 3 (2) |
| Cannot issue, but the organisation is developing a policy | 20 (16) |
| Cannot issue, and not aware of any local policy development | 40 (33) |
| Unsure | 32 (26) |
| Preferred content a | |
| Specific Fit Note training | 5 (4) |
| Specific AHP Health and Work Reporting training | 6 (5) |
| Training for both Fit Notes and AHP Health and Work Reports | 42 (34) |
| Broader work participation training, also including Fit Notes and AHP Health and Work reports | 42 (34) |
| No desire for additional training | 10 (8) |
| Unsure | 18 (15) |
| Preferred format b | |
| One-off webinar, seminar or lecture | 90 (73) |
| Short course (up to 12 h of study) | 62 (50) |
| Longer course (e.g. 2 h per week over a semester) | 18 (15) |
| Post-graduate certificate or diploma | 10 (8) |
| Mentoring, supervision or coaching | 32 (26) |
| Have sufficient experience, no additional training needed | 2 (2) |
| Not interested in additional training | 1 (1) |
| Not part of current role | 1 (1) |
AHP – Allied Health Professional, IQR – interquartile range.
aSingle response option.
bMultiple response options.
Barriers and facilitators for the provision of work guidance
One hundred and four individuals (85%) documented factors that supported or encouraged them to provide return to work guidance for their patients, and 97 (79%) listed barriers to providing such guidance. Provision of work participation guidance was perceived to be facilitated by the patient raising return to work as a rehabilitation goal (n = 53). It was also considered to be part of the hand therapy role and therefore a component of usual practice (n = 30). 30 individuals reported that they were encouraged to provide work guidance for their patients because they believed this to be beneficial to their rehabilitation, and two cited broader societal benefits.
Other facilitators included relevant support or training, or access to work-related services (n = 8), and treatment guidelines or information from charities or other organisations that indicate relevant work recommendations (n = 7). Two individuals highlighted that they found the AHP Health and Work Report helpful.
Reported barriers were categorised into nine themes. 1) Lack of time to provide work recommendations alongside clinical care (n = 41). 2) Lack of skills, knowledge or training relating to work recommendations (n = 30); within this category, nine individuals specifically reported that they were not authorised to issue fit notes by their organisation, and two reported that there was a lack of evidence to provide work recommendations. 3) Concerns about managing patient expectations both with regard to early return to work or extended periods of work absence (n = 16). 4) Organisational or workplace constraints, including inflexible employers (n = 15). 5) Limited understanding of the patients’ job requirements (n = 14). 6) No access to workplace visits, occupational health, or psychological support for the patient (n = 11). 7) Lack of access to suitable assessment or rehabilitation facilities (n = 10). 8) Concerns about the potential legal implications of providing work recommendations (n = 5). 9) Concerns about providing advice conflicting with that given by other healthcare professionals (n = 3).
Work participation training and mentoring
Most respondents desired further training on Fit Notes and AHP Health and Work reports (68%). Of these, exactly half would prefer the training alongside broader education targeted at supporting work participation. The preferred format for any training was via a one-off session (73%) or short course (50%, Table 2).
Discussion
This survey of UK hand therapists describes the self-reported provision of work participation support for adults with hand and upper limb conditions. The questions were similar to a previous survey of Australian Hand Therapists 8 which allows comparison of these different locations.
The reported frequency of different work participation interventions were broadly similar between countries (Supplemental File 2). The most common intervention in the UK and the second most common in Australia was discussing a graded return to work plan with patients (95% and 88% of participants, respectively). This is consistent with findings from qualitative interviews with hand therapists in South Africa, which described the processes deployed to support the transition of return to work. 25
The primary factor encouraging therapists to discuss work recommendations with their patients was reported to be when the patients directly requested assistance. A similar finding was reported in interviews with physiotherapist and occupational therapists in the Netherlands. 26 While this demonstrates patient-centred care, it also relies on patients to understand that hand therapists are equipped to provide work advice. As less than half of UK workers have access to occupational health services, 27 it is important that patients are prompted and educated to discuss any impact of their upper limb condition on their work with their treating clinicians.
Interestingly in both the UK and Australian surveys, few respondents reported creating a formal documented return-to-work plan that included specific functional milestones (UK 25%, Australia 40%). In the UK, the AHP Health and Work Report and Fit Note include free-text space to document this information, but these documents were used by less than a third of the sample. In both the UK and Australia, it appears that hand therapists commonly provide patients with work-related guidance, but this does not necessarily involve written recommendations for the patient and employer. Previous qualitative interviews in the UK found that patients valued tailored written information, perceiving this as validation for any time off work or changes to work patterns/schedules following upper limb surgery. 28 Additionally, qualitative research with worker’s compensation patients in Canada found that injured workers were frequently relied upon as a conduit for information between healthcare workers, employers, and other stakeholders. 29 This was perceived to have negative impacts on clinical recovery and return to work.
One potential issue with providing written work recommendations in any format, is the time required to write and print or email this document. In the current survey, a lack of time was documented as a barrier to providing work recommendations by 39% of the sample, followed by a lack of knowledge (31%). Previous studies have also cited a lack of time as a barrier to providing written guidance. 12 In the current time- and resource-pressed NHS, it is important to evaluate the impacts of hand therapists providing written work guidance. For example, does the use of AHP Health and Work Reports and Fit Notes support earlier return to work after injury, reduce visits to primary care, facilitate fewer hand therapy appointments, improve clinical outcomes and patient satisfaction? If so, might additional staffing be justified to optimise this intervention? 30
Another potential outcome might be therapist job satisfaction. In the current survey, median scores for the amount of involvement in providing return to work recommendations, and the quality of the service provided were both 5/10. This was lower than reported by the Australian sample (7/10 and 6/10, respectively), 8 and equates to unhappy staff (detractors) when categorised according to the net promoter score (0-6/10). 31
A challenge in evaluating work recommendations is that, where completed, AHP Health and Work Reports and Fit Notes are commonly issued in paper form. This may not always be scanned into the electronic health records, or easily accessible for data evaluation. Electronic Fit Notes were rolled out in primary care from 2012 and a target was set to extend this to all NHS secondary care services by November 2023 32 however only 13% of the current survey reported that Fit Notes were provided in an electronic format in their organisation.
More than a third of the sample reported that they were not at all confident in issuing the AHP Health and Work Report (i.e. scored 0/10), increasing to 40% for Fit Notes. These documents are specific to the UK and therefore a comparative assessment with the Australian survey was not possible. 8 The lack of confidence was also illustrated with the reported training needs; more than two thirds of the sample requested training on these documents in addition to broader work and health learning opportunities. Existing training is freely available,33,34 but the reported uptake was low. Only 22% of the sample had completed the e-learning modules for Fit Note certification, despite this being available for 14 months prior to the launch of the survey. Ideally, service leads would sign-post these resources and facilitate appropriate non-clinical time for their staff to complete this training. Additionally, as the existing training is generic to physiotherapists and occupational therapists across the clinical spectrum, specific training relating to MSDs of the hand and upper limb may be beneficial. Interestingly, none of the respondents referred to the UK Faculty of Occupational Medicine ‘Guidance for healthcare professionals on the management of upper limb disorders in working-age people’. 35 Further dissemination of this document may be beneficial.
Occupational health competencies have recently been developed for musculoskeletal first contact practitioners (FCPs) working in primary care 36 These involve seven knowledge-based and 12 skills-based competencies, including: a) knowledge of the relevant legislative frameworks, b) appropriately issuing AHP Health and Work Reports and Fit Notes, c) understanding of health promotion, ergonomic advice and graduated return to work, d) ensuring that work is a consistent focus in every consultation, and e) being able to select and use a work-related outcome measure or screening tool. 36 These competencies appear relevant to hand therapists based in secondary or primary care, although consensus agreement would be required to ensure that they map appropriately to the differences in roles. Collaboration between the FCP, occupational health and hand therapy specialities could support the development of training packages that are relevant to all AHPs working in musculoskeletal settings. As with the previous survey, the preferred training format in the current survey was a singular training session. 8
Only 23% of the sample reported that their organisation had established a pathway for physiotherapists and occupational therapists to issue Fit Notes and several respondents highlighted this as a barrier to supporting work participation. This issue is not unique to hand therapy; there have been national calls for organisations to do more to support the incorporation of this 2022 legislative change into practice. 14
Limitations
The study response rate was higher than previous surveys with a similar population,8,16–18 however we acknowledge the impact of response bias. Individuals with a particular interest in work participation may have been more likely to participate. Sixty-four percent of our sample had more than 10 years of experience in hand therapy, and held specific hand therapy qualifications, suggesting those with high-level clinical skills and expertise were more likely to participate. This was similar to the 70% with more than 10 years of experience reported by O’Brien et al. 8 The views reported may therefore not reflect those of early career hand therapists: however, departmental practice will often be guided by more senior members of the team, which were captured in this survey.
Physiotherapists working in musculoskeletal services may also treat patients with upper limb conditions and their views were not specifically captured through this survey. We limited recruitment to hand therapists because this allowed a clearly defined sample and replicated the approach taken by O’Brien et al., who sampled the Australian Hand Therapy Association. 8 Our findings may not be generalisable to musculoskeletal physiotherapy, however this was not the intention of the study.
The previous survey included questions on the estimated proportion of patients who were in receipt of various types of employment or healthcare insurance, including workers’ compensation, private healthcare insurance and transport/motor accident insurance. Within the NHS, there is no routinely collected data outlining patients’ employment or insurance status and these questions were removed. Contextual factors relating to healthcare and occupational policies vary internationally and we recommend that these factors are clearly documented in hand therapy and hand surgery research.
The survey was deliberately anonymous to encourage respondents to answer freely, but this prevents identification of the number of responses from the same hospital or clinic, where clinical practice might be expected to be similar, or detection of multiple participation. Furthermore, given the self-reported nature of the survey, feedback on individual clinical practice, may not accurately reflect actual practice. However, by using the same format and question structure to the previous Australian survey, 8 national-level comparison is possible, and this study adds to the work participation literature.
Conclusions
UK hand therapists reported using a range of work participation interventions with their patients. The most commonly cited initiator to provide work-related guidance was that the patient identified work or return to work as a goal. Few individuals reported providing written work recommendations, including AHP Health and Work Reports or Fit Notes. Open text responses highlighted examples of organisations that did not permit Fit Note certification, despite changes in government legislation more than a year before the survey opened that added occupational therapists and physiotherapists as Fit Notes providers. Overall, therapists reported low levels of confidence in issuing these documents and desired targeted training, alongside broader learning opportunities in relation to MSDs and work. Compared with the Australian version of this survey, UK hand therapists reported lower satisfaction with their amount of involvement in work participation support and the quality of the work participation service that they were able to provide, which highlights key areas for service improvement.
Future opportunities for UK hand therapists include (i) raising awareness that patients can ask hand therapists for work-related advice and formal work-related documentation, (ii) promoting the existing AHP Health and Work Report and Fit Note training, (iii) creating specific work participation training for hand therapists, and (iv) ensuring that NHS organisations provide hand therapists (and wider occupational therapy and physiotherapy disciplines) with access to electronic Fit Notes to enable certification, and evaluation of use.
Opportunities for the international hand therapy community include continuing this survey in other countries with an aim of collaboratively developing exemplar work participation strategies for patients with hand and upper limb conditions. This will inform future research, and support the development of shared learning resources.
Supplemental Material
Supplemental Material for Supporting work participation for adults with hand and upper limb conditions: A survey of the British Association of hand therapists by Lisa Newington, Daniel Ceh, Fiona Sandford, Vaughan Parsons and Ira Madan in Hand Therapy
Supplemental Material for Supporting work participation for adults with hand and upper limb conditions: A survey of the British Association of hand therapists by Lisa Newington, Daniel Ceh, Fiona Sandford, Vaughan Parsons and Ira Madan in Hand Therapy
Acknowledgements
Thank you to: Dr Lisa O’Brien and team for their previous research that inspired this project, the BAHT Clinical Evidence Committee for their peer review of our survey questions, and Barbara Smiley for reviewing the manuscript prior to submission. Finally, thank you to all the participants for giving up their time to contribute to this research. This work acknowledges the support of the National Institute for Health Research Barts Biomedical Research Centre (NIHR203330).
Author Contributions: LN conceived the study with feedback from FS, VP and IM. All authors developed the survey questions. LN created the electronic survey and analysed the data with review by all authors. LN wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclose receipt of the following financial support for the research authorship and/or publication of this article: LN, DC and FS were supported by the Chartered Society of Physiotherapy Charitable Trust Postdoctoral Research Grant (reference PRF-22-POD04).
Guarantor: LN.
Supplemental Material: Supplemental material for this article is available online.
Ethical statement
Ethical approval
Approval was provided by Queen Mary University of London Research Ethics Committee (QME23.0112) and Guy’s and St Thomas’ NHS Foundation Trust Therapies Audit Committee (15415).
Informed consent
The purposes of the survey were summarised at the start of the survey and provided in more detail through a linked electronic participant information sheet. Respondents were asked to consent to participation at the start of the survey and again prior to submitting their responses.
ORCID iDs
Lisa Newington https://orcid.org/0000-0001-6954-2981
Daniel Ceh https://orcid.org/0009-0005-7260-1977
Fiona Sandford https://orcid.org/0000-0002-1778-891X
Vaughan Parsons https://orcid.org/0000-0003-0523-3770
Ira Madan https://orcid.org/0000-0003-2200-7329
References
- 1.NHS England . Musculoskeletal Health. NHS England, 2023, https://www.england.nhs.uk/elective-care-transformation/best-practice-solutions/musculoskeletal/ (accessed 6 June 2023). [Google Scholar]
- 2.Versus Arthritis. The State of Musculoskeletal Health. Versus Arthritis, 2022, https://www.versusarthritis.org/about-arthritis/healthcare-professionals/professional-network-and-clinical-updates/network-news/december-2021-network-news/state-of-musculoskeletal-health-2021-statistics-now-published/ (accessed 1 May 2022). [Google Scholar]
- 3.Office for National Statistics . Sickness Absence in the UK Labour Market. Office for National Statistics, 2022, https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/labourproductivity/articles/sicknessabsenceinthelabourmarket/2022 (accessed 21 December 2023). [Google Scholar]
- 4.Versus Arthritis . The State of Musculoskeletal Health 2023. Versus Arthritis, 2023, https://versusarthritis.org/media/duybjusg/versus-arthritis-state-msk-musculoskeletal-health-2023pdf.pdf (accessed 21 December 2023). [Google Scholar]
- 5.Modini M, Joyce S, Mykletun A, et al. The mental health benefits of employment: results of a systematic meta-review. Australas Psychiatry 2016; 24: 331–336. [DOI] [PubMed] [Google Scholar]
- 6.Hutting N, Boucaut R, Gross DP, et al. Work-focused health care: the role of physical therapists. Physical Therapy 2020; 100: 2231–2236. [DOI] [PubMed] [Google Scholar]
- 7.Hutting N, Caneiro JP, Ong’wen OM, et al. Patient-centered care in musculoskeletal practice: key elements to support clinicians to focus on the person. Musculoskelet Sci Pract 2022; 57: 102434. [DOI] [PubMed] [Google Scholar]
- 8.O’Brien L, Robinson L, Parsons D, et al. Hand therapy role in return to work for patients with hand and upper limb conditions. Journal of Hand Therapy 2022; 35: 226–232. [DOI] [PubMed] [Google Scholar]
- 9.Allied Health Professions Federation . AHP Health and Work Report. Allied Health Professions Federation, 2019, https://www.ahpf.org.uk/AHP_Health_and_Work_Report.htm (accessed 20 July 2022). [Google Scholar]
- 10.Department for Work and Pensions . Fit Note: Guidance for Healthcare Professionals. Gov.UK, 2022, https://www.gov.uk/government/publications/fit-note-guidance-for-healthcare-professionals (accessed 1 July 2022). [Google Scholar]
- 11.Allied Health Professions Federation . AHP Health and Work Report: Guidance for AHP Practitioners on the Use and Completion of the Report. Allied Health Professions Federation, 2019, https://www.ahpf.org.uk/files/Guidance-on-completion-of-AHP-Health-and-Work-Report.pdf (accessed 21 December 2023). [Google Scholar]
- 12.Saunders B, Foster NE, Hill JC, et al. First contact practitioners’ ( FCPs ) and general practitioners’ perceptions towards FCPs delivering vocational advice to patients with musculoskeletal conditions : a qualitative Investigation of the Implementation potential of the I - SWAP initiative. Journal of Occupational Rehabilitation 2022; 32: 147–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nouri F, Coole C, Smyth G, et al. The allied health professions health and work report and the fit note: perspectives of patients and stakeholders. British Journal of Occupational Therapy 2021; 84: 72–78. [Google Scholar]
- 14.Drummond A, Smyth G. Fit notes: A call to arms. British Journal of Occupational Therapy. 2023; 0(0). DOI: 10.1177/03080226231213525 [DOI] [Google Scholar]
- 15.Newington L. Work-related recommendations in hand therapy: a survey of practice. Open Science Framework (OSF) 2023, DOI: 10.17605/OSF.IO/D3KJ7 (accessed 4 January 2024). [DOI] [Google Scholar]
- 16.Newington L, Francis K, Ntani G, et al. Return to work recommendations after carpal tunnel release: a survey of UK hand surgeons and hand therapists. J Hand Surg Eur Vol 2018; 43: 875–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scott H, Robinson L, Brown T. Scar massage as an intervention for post-surgical scars: a practice survey of Australian hand therapists. Hand Ther. 2024; 29(1): 21–29. DOI: 10.1177/17589983231205666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cook S, Daniels N, Woodbridge S. How do hand therapists conservatively manage acute, closed mallet finger? A survey of members of the British association of hand therapists. Hand Therapy 2017; 22: 13–25. [Google Scholar]
- 19.Sharma A, Minh Duc NT, Luu Lam Thang T, et al. A consensus-based Checklist for reporting of survey studies (CROSS). Journal of General Internal Medicine 2021; 36: 3179–3187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The upper extremity collaborative group (UECG). American Journal of Industrial Medicine 1996; 29: 602–608. [DOI] [PubMed] [Google Scholar]
- 21.Stratford P. Assessing disability and change on individual patients: a report of a patient specific measure. Physiotherapy Canada 1995; 47: 258–263. [Google Scholar]
- 22.MacDermid JC. The PRWE/PRWHE update. Journal of Hand Therapy 2019; 32: 292–294. [DOI] [PubMed] [Google Scholar]
- 23.Law M, Baptiste S, McColl M, et al. The Canadian occupational Performance measure: an outcome measure for occupational therapy. Canadian Journal of Occupational Therapy 1990; 57: 82–87. [DOI] [PubMed] [Google Scholar]
- 24.Allaire S, Keysor JJ. Development of a structured interview tool to help patients identify and solve rheumatic condition-related work barriers. Arthritis & Rheumatism 2009; 61: 988–995. [DOI] [PubMed] [Google Scholar]
- 25.Buchanan H, van Niekerk L. Work transitions after serious hand injury: current occupational therapy practice in a middle-income country. Australian Occupational Therapy Journal 2022; 69: 151–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oswald W, Ummels I, Raaijmakers T, et al. Therapists’ experiences and needs with regard to providing work-focused care: a focus group study. BMC Musculoskelet Disord 2021; 22: 923–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Department of Work and Pensions D of H and SC . Occupational Health: Working Better. UK: Public consultation, 2023, https://assets.publishing.service.gov.uk/media/64b8f7baef5371000d7aef2d/occupational-health-working-better-consultation.pdf (accessed 21 December 2023). [Google Scholar]
- 28.Newington L, Brooks C, Warwick D, et al. Return to work after carpal tunnel release surgery: a qualitative interview study. BMC Musculoskelet Disord 2019; 20: 242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Russell E, Kosny A. Communication and collaboration among return-to-work stakeholders. Disability & Rehabilitation 2019; 41: 2630–2639. [DOI] [PubMed] [Google Scholar]
- 30.Wynne-Jones G, Artus M, Bishop A, et al. Effectiveness and costs of a vocational advice service to improve work outcomes in patients with musculoskeletal pain in primary care: a cluster randomised trial (SWAP trial ISRCTN 52269669). Pain 2018; 159: 128–138. [DOI] [PubMed] [Google Scholar]
- 31.Dawes JG. The net promoter score: what should managers know? International Journal of Market Research. 2023; 0(0). DOI: 10.1177/14707853231195003 [DOI] [Google Scholar]
- 32.NHS Digital . For action: launch of electronic fit notes in secondary care. Essential Information for Digital Leaders, 2022, https://digital.nhs.uk/about-nhs-digital/essential-information-and-alerts-for-stakeholders/essential-information-for-digital-leaders/launch-of-electronic-fit-notes-in-secondary-care (accessed 21 December 2023). [Google Scholar]
- 33.University of Nottingham: Health e-learning Media . Reusable Learning Object Exploring the Completion of the Allied Health Professional (AHP) Health and Work Report. University of Nottingham, 2020, https://www.nottingham.ac.uk/helmopen/rlos/professional-development/AHP-health-and-work-report/index.html (accessed 21 December 2023). [Google Scholar]
- 34.NHS England: e-learning for health . The Fit Note. NHS England, 2022, https://www.e-lfh.org.uk/programmes/the-fit-note/ (accessed 21 December 2023). [Google Scholar]
- 35.Faculty of Occupational Medicine . Guidance for Healthcare Professionals on the Management of Upper Limb Disorders in Working-Age People. Faculty of Occupational Medicine, 2023, https://www.fom.ac.uk/wp-content/uploads/FOM-Guidance-on-management-of-ULD_healthcare-professionals.pdf (accessed 4 January 2024). [Google Scholar]
- 36.Black C, Shanmugam S, Gray H. Consensus on occupational health competencies for UK first contact physiotherapists. Physiotherapy 2023; 121: 58–68. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Supporting work participation for adults with hand and upper limb conditions: A survey of the British Association of hand therapists by Lisa Newington, Daniel Ceh, Fiona Sandford, Vaughan Parsons and Ira Madan in Hand Therapy
Supplemental Material for Supporting work participation for adults with hand and upper limb conditions: A survey of the British Association of hand therapists by Lisa Newington, Daniel Ceh, Fiona Sandford, Vaughan Parsons and Ira Madan in Hand Therapy