Abstract
Objective
This study used a national insurance claims database to analyze trends in procedural management of Meniere's disease.
Study Design
Retrospective cohort analysis.
Setting
Database study using United States inpatient and outpatient insurance claims submitted from January 2003 to December 2021.
Subjects and Methods
The Merative MarketScan Commercial and Medicare Claims Databases were queried for adults (≥18 years) with a diagnosis of Meniere's Disease according to International Classification of Diseases codes. Patients receiving procedures per Current Procedural Terminology codes for endolymphatic sac surgery, vestibular nerve section, labyrinthectomy, and intratympanic dexamethasone or gentamicin were identified. Temporal trends were analyzed by calculating annual percent change (APC) in the proportion of patients receiving procedures using Joinpoint regression.
Results
A total of 16,523 unique patients with MD receiving procedural management were identified. From 2003 to 2021, the proportion of patients managed with intratympanic dexamethasone increased (APC 1.76 [95% CI 1.53‐1.98], P < .001). The proportion of patients receiving intratympanic gentamicin increased from 2003 to 2015 (APC 4.43 [95% CI 1.29‐7.66], P = .008) but decreased from 2015 to 2021 (APC −10.87 [95% CI −18.31 to −2.76], P = .013). The proportion of patients receiving endolymphatic sac surgery (APC: −10.20 [95% CI −11.19 to −9.20], P < .001) and labyrinthectomy (APC: −6.29 [95% CI −8.12 to −4.42], P < .001) decreased from 2003 to 2021.
Conclusion
From 2003 to 2021, there has been an increase in the use of intratympanic dexamethasone and a decrease in the use of intratympanic gentamicin, endolymphatic sac surgery, and labyrinthectomy for procedural management of Meniere's Disease.
Keywords: endolymphatic sac surgery, Insurance Claims Database, intratympanic gentamicin, intratympanic steroids, Ménière's disease, migraine, practice patterns, procedural management
Meniere's disease (MD) is an inner ear disorder characterized by episodic vertigo, tinnitus, and hearing loss. 1 , 2 Vertiginous episodes in MD and hearing loss‐related quality of life concerns take a tremendous toll on patients, representing a major source of healthcare system burden and cost. 3 The pathophysiological mechanism of MD is thought to be an accumulation of endolymph within the inner ear, a phenomenon known as endolymphatic hydrops. 4 , 5 , 6 The 2020 American Academy of Otolaryngology–Head and Neck Surgery (AAO‐HNS) clinical practice guidelines suggest first‐line treatment for MD patients include lifestyle modifications such as low‐salt diets and diuretic therapy, which have grown in use for early‐stage MD over the last 15 years. 7 , 8 However, one‐third of MD patients have symptoms refractory to lifestyle and medical therapies and may be offered conservative procedural therapies such as intratympanic (IT) corticosteroid injections and endolymphatic sac surgery. If ineffective, destructive procedures such as IT gentamicin, surgical labyrinthectomy, and vestibular nerve section may be offered. Despite high degrees of efficacy, these destructive therapies result in vestibular loss and either guarantee or risk hearing loss, 9 prompting interest in alternative, less disabling management options.
In recent years, there appears to have been an anecdotal shift away from destructive management and towards conservative management of MD. It is important to formally evaluate the evolving landscape of MD management as improved understanding of utilization will aid the national conversation about future directions for clinical management of MD. The purpose of this study was to utilize a national insurance claims database, the Merative (formerly known as IBM Health and Truven Health Analytics) MarketScan Research Databases, to investigate trends in procedural management of MD over the last 2 decades. We hypothesized that over the last 20 years, there has been a decrease in the use of surgical or destructive management for MD while the use of conservative therapies such as IT dexamethasone has increased.
Methods
A retrospective study was performed using insurance claims between January 1, 2003 and December 31, 2021 from the Merative MarketScan Commercial Claims and Encounters and Medicare Supplemental Databases. These databases contain patient‐level data from insurance claims of nearly 60 million employees, dependents, and retirees in the United States who are covered via Medicare or via commercial, employer‐based health insurance plans. 10 This study was deemed exempt by the University of Chicago Institutional Review Board (IRB23‐0042).
Diagnostic codes from the International Classification of Diseases (ICD) ninth and tenth revisions (ICD‐9 and ICD‐10, respectively) were used to identify adult patients (≥18 years) with MD (“MD Records”), including ICD‐9 codes beginning with 386 and ICD‐10 codes beginning with H81.0. A subset of this group of receiving procedural management was identified via a query for Current Procedural Terminology (CPT) codes of interest defined in Table 1 (“Procedural MD Records”). Because IT corticosteroid and gentamicin injections are both coded in insurance claims using CPT code 69801 (labyrinthotomy, with perfusion of vestibuloactive drug[s]; transcanal) for IT perfusion of vestibuloactive drugs, a subanalysis was performed using Healthcare Common Procedure Coding System (HCPCS) J codes corresponding to dexamethasone and gentamicin (Table 1). To compare the trends in types of procedures used to manage MD, “Procedural MD Records” were subset to identify unique MD patients receiving procedures and the procedure type was identified using the CPT and HCPCS codes of interest (Table 1).
Table 1.
CPT and HCPCS Codes of Interest for Database Query
| CPT Code | Procedure (HCPCS) |
|---|---|
| 69801 | IT injection gentamicin (J1580) |
| IT injection dexamethasone (J1100) | |
| 69905 | Labyrinthectomy‐transcanal |
| 69910 | Labyrinthectomy‐transmastoid |
| 69950 | Vestibular nerve section |
| 69805/6 | Endolymphatic sac surgery |
Abbreviations: CPT, current procedural terminology; HCPCS, healthcare common procedure coding system; IT, intratympanic.
To ensure accuracy in the analysis of trends in utilization for procedures like IT injections of dexamethasone or gentamicin that MD patients might receive more than once, and which therefore have multiple associated records for a single patient, we eliminated double‐counting in our analysis. Double‐counting was eliminated by capturing index procedures and limiting the study population to unique patients receiving a procedure of interest each year. Therefore, the data in this study does not represent an individual patient's index procedure more than once in a calendar year.
Because the absolute numbers of billing records containing both MD‐associated ICD codes and CPT codes of interest might vary year‐to‐year based on the number of private health insurers contracting with and supplying data to Merative, the ratio of “Procedural MD Records” to “MD Records” was used to capture the trends in proportions of MD patients being managed with procedural therapy.
Descriptive statistics were performed to summarize data. Data extraction and analysis was performed using SAS (version 9.4; SAS Institute Inc.) and R Statistical Software (version 4.2.2; R Foundation for Statistical Computing). Joinpoint regression was performed to analyze annual percent change (APC) in procedural management of MD (Joinpoint Regression Program, v5.0.2; National Cancer Institute). Procedural proportions were converted to percentages and constant variance was used to estimate regression coefficients by the ordinary least squares model. Analysis allowed for 0‐1 joinpoints to be identified and for calculation of estimated annual percent change (APC) of proportions using a parametric method. Statistical significance was set at α = 0.05.
Results
A total of 1.75 million billing records with MD‐associated diagnostic codes were identified during the period of January 2003 to December 2021. Of these, a total of 44,831 billing records representing 16,523 unique patients contained CPT codes of interest (“Procedural MD Records”). The mean age of the final patient cohort (n = 16,523) was 53.1 years (SD 12.4 years).
From 2003 to 2021, the most utilized procedures for MD management were IT perfusion of vestibuloactive drugs, including dexamethasone and gentamicin, and endolymphatic sac surgery. The proportion of MD patients managed with endolymphatic sac surgery decreased from 23% in 2003 to 5% in 2021 (Figure 1). The proportion of MD patients managed with IT dexamethasone increased from 68% in 2003 to 91% in 2021 (Figure 1). IT gentamicin represented a minority of IT injections throughout the study period. The proportion of MD patients receiving IT injections of gentamicin peaked in 2011 at 4.7% and decreased to 2.8% in 2021.
Figure 1.
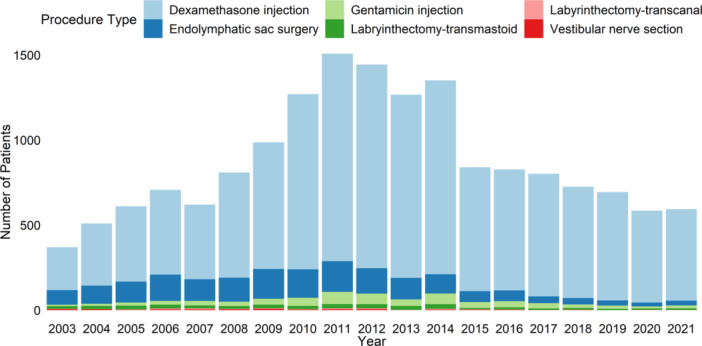
Number of unique Meniere's disease patients managed with procedures per year, stratified by procedure type.
Surgical labyrinthectomy via a transmastoid or transcanal route remained an infrequently utilized procedure for MD management throughout the study period with a decrease in the proportion of patients receiving a labyrinthectomy via a transmastoid approach from 4.1% in 2003 to 1.7% in 2021. A transcanal approach for labyrinthectomy was less commonly utilized than a transmastoid approach, which represented the majority of records corresponding to MD patients receiving labyrinthectomy. Vestibular nerve section also remained a rarely utilized procedure for MD management throughout the study period with less than ten MD patients per year receiving vestibular nerve sections (Figure 1).
Joinpoint analysis of temporal trends revealed an overall increase in the use of IT dexamethasone from 2003 to 2021 (APC 1.76 [95% CI 1.53‐1.98], P < .001, Figure 2). The proportion of patients receiving IT gentamicin increased from 2003 to 2015 (APC 4.43 [95% CI 1.29‐7.66], P = .008) but decreased from 2015 to 2021 (APC −10.87 [95% CI −18.31 to −2.76], P = .013, Figure 2). The proportion of patients receiving endolymphatic sac surgery (APC: −10.20 [95% CI −11.19 to −9.20], P < .001) and labyrinthectomy via a transmastoid or transcanal approach (APC: −6.29 [95% CI −8.12 to −4.42], P < .001) decreased from 2003 to 2021 (Figure 3).
Figure 2.
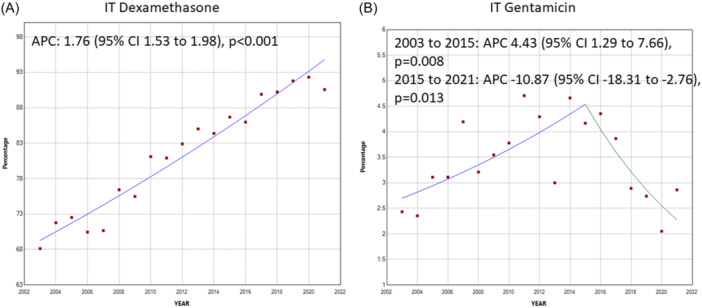
Joinpoint regression trends for annual percent change of intratympanic treatments for Meniere's disease (MD) from 2003 to 2021. (A) IT Dexamethasone. (B) IT Gentamicin. Percentages were calculated using number of procedural MD patients receiving treatment divided by number of total MD patients receiving procedural therapy per year. APC, annual percent change. IT, intratympanic.
Figure 3.
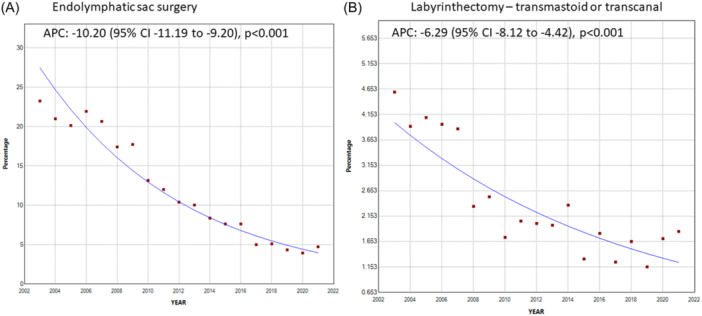
Joinpoint regression trends for annual percent change of surgical management for Meniere's disease (MD) from 2003 to 2021. (A) Endolymphatic sac surgery. (B) Labyrinthectomy–transmastoid or transcanal. Percentages were calculated using number of procedural MD patients receiving surgery divided by number of total MD patients receiving procedural therapy per year. APC, annual percent change.
Discussion
This study evaluated trends in the procedural management of MD from 2003 to 2021 using the Merative Marketscan database. We found that there has been an overall increase in the use of IT dexamethasone and an overall decrease in the use of IT gentamicin, endolymphatic sac surgery, and labyrinthectomy for procedural management of MD. We also found that the most ablative procedures, including IT gentamicin, endolymphatic sac surgery, labyrinthectomy, and vestibular nerve section, were the least commonly utilized of all procedural management options for MD.
Our findings of a decrease in the use of endolymphatic sac surgery, though still the most common surgical procedure used for MD, as well as labyrinthectomy are in line with recent database studies and survey studies. 8 , 11 However, while a recent database demonstrated that IT injection usage within 12 months of MD diagnosis was stable from 2008 to 2022, 8 our analysis demonstrated an evolution in the use of IT injections any time after MD diagnosis. We delineated between IT dexamethasone and IT gentamicin and demonstrated an overall increase in the use of IT dexamethasone and an overall decrease in the use of IT gentamicin from 2003 to 2021.
The factors contributing to our findings of an apparent increase in utilization of IT dexamethasone and shift away from other procedural modalities, particularly IT gentamicin and endolymphatic sac surgery, are not immediately clear. Despite the existence of clinical guidelines, there is still a lack of consensus on treatment recommendations for MD, particularly with regard to the timeline and criteria for offering procedural and surgical options. 12 While chemical labyrinthectomy via IT gentamicin still lacks robust randomized controlled trial data supporting its efficacy, 13 , 14 new data has emerged in the last decade supporting the efficacy of IT corticosteroids. 15 , 16 The increasing body of evidence supporting IT corticosteroids, which is not ototoxic when compared to ablative and/or surgical treatments, might be responsible in part for the increased employment of IT corticosteroids to preserve hearing function for patients with severe MD.
This study has several limitations to consider when interpreting the results. Our study leveraged the Merative MarketScan family of databases. These commercially available insurance claims databases include data provided by private health insurers who contract with and supply data to Merative each year. The data represented in the database may therefore fluctuate year‐to‐year depending on changes to these data sharing relationships. There may also be fluctuations secondary to changes in payer mixes, billing practices, or even clinical documentation (such as with adoption of electronic medical record systems). To account for these possible year‐to‐year fluctuations, we utilized a long‐term temporal regression analysis to identify more stable temporal trends. Because MarketScan data do not contain clinical data regarding treatment severity or treatment rationale, future studies might investigate whether there is a decreasing incidence of severe MD that could account for a decrease in the number of patients for whom procedural therapy is indicated. With regards to representation, MarketScan data only represents patients who have health insurance. Therefore, patients who are uninsured or insured by smaller insurers are not represented, and there may be overrepresentation of claims for patients with employer‐based health insurance from large employers. 10 Finally, the data in MarketScan is only as accurate as the coding of diagnoses and procedures by providers and billers. It is therefore possible that our study was biased by inaccurate coding such as failure to include each of the relevant CPT and HCPCS codes for procedures like IT injection of gentamicin.
Conclusion
IT dexamethasone is the most common procedure for managing MD. IT gentamicin, endolymphatic sac surgery, and surgical labyrinthectomy have decreased in utilization over the last decade. These findings suggest that providers may be taking a more conservative approach for management of MD. Further studies investigating the factors contributing to these observed trends in procedural management of MD are warranted.
Author Contributions
Nihar Rama, substantial contribution to study design, data acquisition, analysis and interpretation, initial manuscript creation and significant revisions, and approval of the final submitted version; Samuel Auger, substantial contribution to study design, data acquisition, analysis and interpretation, significant revisions to and approval of the final submitted manuscript; Terence Imbery, substantial contribution to study concept and design, data interpretation, significant revisions to and approval of the final submitted manuscript.
Disclosure
Competing interests
None.
Funding source
This project was supported by the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) through Grant Number 2UL1TR002389‐06 that funds the Institute for Translational Medicine (ITM) at the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. All authors account for the integrity of the research and data presented here.
This research was presented at the AAO‐HNSF 2023 Annual Meeting & OTO Experience; September 30‐October 4, 2023; Nashville, Tennessee
Contributor Information
Nihar Rama, Email: Nihar@uchicagomedicine.org.
Terence E. Imbery, Email: timbery@bsd.uchicago.edu.
References
- 1. Goebel JA. Equilibrium committee amendment to the 1995 AAO‐HNS guidelines for the definition of Ménière's disease. Otolaryngol Neck Surg. 2015;154(3):403‐404. 10.1177/0194599816628524 [DOI] [PubMed] [Google Scholar]
- 2. Lopez‐Escamez JA, Carey J, Chung WH, et al. Diagnostic criteria for Menière's disease. J Vestibular Res. 2015;25(1):1‐7. 10.3233/VES-150549 [DOI] [PubMed] [Google Scholar]
- 3. Tyrrell J, Whinney DJ, Taylor T. The cost of Ménière's disease: a novel multisource approach. Ear Hearing. 2016;37(3):e202‐e209. 10.1097/AUD.0000000000000264 [DOI] [PubMed] [Google Scholar]
- 4. Semaan MT, Megerian CA. Contemporary perspectives on the pathophysiology of Meniere's disease: implications for treatment. Curr Opin Otolaryngol Head Neck Surg. 2010;18(5):392‐398. 10.1097/MOO.0b013e32833d3164 [DOI] [PubMed] [Google Scholar]
- 5. Paparella MM, Djalilian HR. Etiology, pathophysiology of symptoms, and pathogenesis of Meniere's disease. Otolaryngol Clin North Am. 2002;35(3):529‐545. 10.1016/S0030-6665(02)00019-1 [DOI] [PubMed] [Google Scholar]
- 6. Gluth MB. On the relationship between Menière's disease and endolymphatic hydrops. Otol Neurotol. 2020;41(2):242‐249. 10.1097/MAO.0000000000002502 [DOI] [PubMed] [Google Scholar]
- 7. Basura GJ, Adams ME, Monfared A, et al. Clinical practice guideline: Ménière's disease. Otolaryngol Head Neck Surg. 2020;162(S2):S1‐S55. 10.1177/0194599820909438 [DOI] [PubMed] [Google Scholar]
- 8. Gallagher TJ, Adams ME, Choi JS. Trends in management of Ménière disease: a TriNetX network database analysis. OTO Open. 2024;8(1):e123. 10.1002/oto2.123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chia SH, Gamst AC, Anderson JP, Harris JP. Intratympanic gentamicin therapy for Ménière's disease: a meta‐analysis. Otol Neurotol. 2004;25(4):544‐552. 10.1097/00129492-200407000-00023 [DOI] [PubMed] [Google Scholar]
- 10. Kulaylat A, Schaefer E, Messaris E, Hollenbeak C. Truven health analytics MarketScan databases for clinical research in colon and rectal surgery. Clin Colon Rectal Surg. 2019;32(01):054‐060. 10.1055/s-0038-1673354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Clyde JW, Oberman BS, Isildak H. Current management practices in Ménière's disease. Otol Neurotol. 2017;38(6):e159‐e167. 10.1097/MAO.0000000000001421 [DOI] [PubMed] [Google Scholar]
- 12. Nevoux J, Barbara M, Dornhoffer J, Gibson W, Kitahara T, Darrouzet V. International consensus (ICON) on treatment of Ménière's disease. Eur Ann Otorhinolaryngol Head Neck Dis. 2018;135(1):S29‐S32. 10.1016/j.anorl.2017.12.006 [DOI] [PubMed] [Google Scholar]
- 13. Webster KE, Galbraith K, Lee A, et al. Intratympanic gentamicin for Ménière's disease. Cochrane Database Syst Rev. 2023;2:CD015246. 10.1002/14651858.CD015246.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rah YC, Han JJ, Park J, Choi BY, Koo JW. Management of intractable ménière's disease after intratympanic injection of Gentamicin. Laryngoscope. 2015;125(4):972‐978. 10.1002/lary.25009 [DOI] [PubMed] [Google Scholar]
- 15. Hao W, Yu H, Li H. Effects of intratympanic gentamicin and intratympanic glucocorticoids in Ménière's disease: a network meta‐analysis. J Neurol. 2022;269(1):72‐86. 10.1007/s00415-020-10320-9 [DOI] [PubMed] [Google Scholar]
- 16. Lee SY, Kim YS, Jeong B, et al. Intratympanic steroid versus gentamicin for treatment of refractory Meniere's disease: a meta‐analysis. Am J Otolaryngol. 2021;42(6):103086. 10.1016/j.amjoto.2021.103086 [DOI] [PubMed] [Google Scholar]


