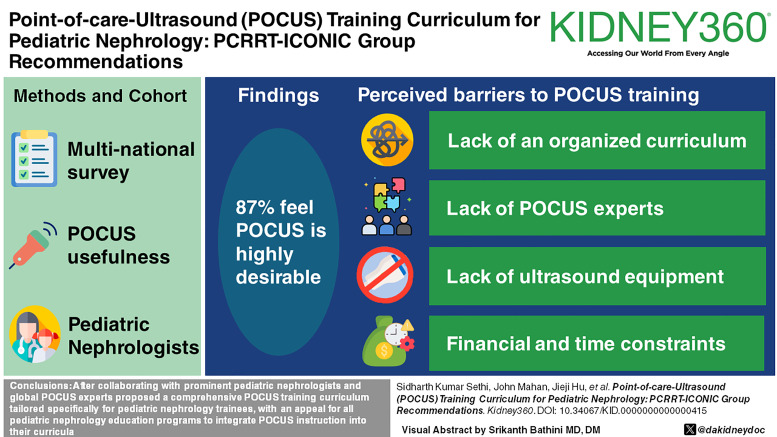
Visual Abstract
Keywords: AKI, pediatrics
Abstract
Key Points
Despite a high need and interest in point-of-care ultrasound (POCUS) in trainees and faculty of Pediatric Nephrology, the majority are not receiving POCUS training.
There is a need to establish a structured pediatric nephrology POCUS program for clinicians and fellows.
This study suggests a blueprint of POCUS curriculum which can serve as a foundation for POCUS education in pediatric nephrology centers worldwide.
Background
Point-of-care ultrasound (POCUS) is commonly used in adult specialties, pediatric emergency medicine, and neonatal and pediatric critical care. Specifically, in the field of pediatric nephrology, POCUS plays a valuable role in the critical inpatient and outpatient settings. However, the lack of guidelines and a standardized curriculum for POCUS in pediatric nephrology has led to substantial discrepancies in both clinical practice and training.
Methods
A multinational, multicenter survey regarding POCUS usefulness and training was sent to 225 pediatric nephrology residents, fellows, and physicians with expertise in pediatric nephrology. On the basis of the results, an ideal pediatric nephrology POCUS curriculum was formulated with a panel of experts from across the world. Eighteen experts were included, with each expert having >10 years of experience in using POCUS in adult and pediatric nephrology. A Delphi method was used to further solidify guidelines regarding the content, curriculum, and vital skills of using POCUS in pediatric nephrology.
Results
A total of 134 pediatric nephrology trainees, specialists, and faculty responded to the survey (59.6% completion rate). A total of 87.4% of respondents believe that formal POCUS training is either highly desirable or should be mandatory in pediatric nephrology fellowship programs. Identified barriers to receiving training included lack of an organized curriculum, lack of POCUS experts and pediatric intensivists, lack of ultrasound equipment, lack of financial support, and lack of dedicated time during training. An expert panel was convened, and a Delphi survey was conducted to formulate guidelines to overcome the barriers to pediatric nephrology POCUS and standardize the training process.
Conclusions
After collaborating with prominent pediatric nephrologists, global POCUS experts proposed a comprehensive POCUS training curriculum tailored specifically for pediatric nephrology trainees, with an appeal for all pediatric nephrology education programs to integrate POCUS instruction into their curricula.
Introduction
Point-of-care ultrasound (POCUS) is a bedside imaging tool that enables clinicians to assess patients with precision and effectiveness, aiding in the diagnosis of various underlying pathologies. It is becoming so ubiquitous that postgraduate training programs, such as those in pediatric emergency medicine, have formally incorporated POCUS training into their curricula.1 In adult nephrology, the cultivation of clinical proficiency in POCUS is highly valued by fellows and faculty members. This emphasis extends to sonographic applications that go beyond kidney ultrasound, encompassing lung and focused cardiac ultrasound as well.2 However, despite the availability of 1-year POCUS fellowships and POCUS workshops at various national meetings, substantial obstacles still hinder the widespread adoption of POCUS in adult nephrology.3 In the field of pediatric nephrology, formal education opportunities within training programs are sparse, in contrast to emergency medicine, critical care medicine, and some internal medicine programs, which have relatively better defined curricula.4,5
Need for POCUS in Pediatric Nephrology
Although not always a substitute for a comprehensive ultrasound examination, POCUS is useful for answering focused clinical questions rapidly at the bedside that change management. This includes assessing various kidney characteristics such as structural abnormalities, kidney stones, urinary tract abnormalities, and cystic kidney diseases. In addition, POCUS can assist the pediatric nephrologist in assessing fluid status via focused cardiac and pulmonary assessments in critically ill children with kidney dysfunction.6 POCUS can help guide kidney biopsy and assess for postbiopsy complications and evaluate for complications in other relevant procedures such as suprapubic aspiration (SPA), dialysis catheter insertion (both peritoneal dialysis and hemodialysis), and dialysis vascular access patency.6,7 POCUS has been shown to increase success rates and decrease procedural complications. For example, use of POCUS improves the success rate of SPA in infants. Mahdipour et al. performed a randomized controlled trial on infants with suspected urinary tract infections. When compared with SPA and bladder catheterization, a combined POCUS-SPA approach had a significantly higher success rate compared with the other two groups. Thus, it can be very useful for clinicians to consider the use of POCUS-SPA for successful urine sampling in infants and neonates with urinary tract infections.8 Another advantage is that POCUS can be used in both inpatient and outpatient settings as a noninvasive test with high reproducibility and low risk for the patient.7
To foster POCUS training, core competencies and technical standards related to POCUS in pediatric nephrology should be developed to provide an educational framework for trainees and to standardize the use of POCUS among pediatric nephrologists. The European Society of Pediatric and Neonatal Intensive Care published guidelines regarding POCUS use in critically ill neonates and children.9 While the guidelines primarily focused on POCUS applications related to cardiopulmonary, neurological, and abdominal aspects, these could be relevant to pediatric nephrologists. Specifically, they can be extrapolated to assess fluid status and may be used for other various procedural applications of POCUS, such as dialysis catheter placements and arterial line insertions. However, there remains a distinct gap to address in the context of guidelines pertaining to the full breadth of pediatric nephrology. Challenges persist in the creation of POCUS guidelines tailored specifically for pediatric nephrology, establishing a certification process to ensure proficiency in POCUS and securing institutional backing for mentoring trainees. The implementation of a POCUS curriculum requires support at multiple levels, encompassing identification of proficient clinicians capable of mastering and instructing POCUS, ensuring trainees have the resources and structured time to hone these skills, and formulating and gaining approval for consensus guidelines by pediatric nephrology societies.10 This study seeks to identify the attitudes and opinions that pediatric nephrologists have regarding the implementation and challenges of POCUS and proposes a pediatric nephrology–centered POCUS curriculum.
Survey
A Qualtrics research survey (Supplemental Appendix 1 and 2) was distributed to a multinational cohort of 225 pediatric nephrology specialists to evaluate the utilization of POCUS in the practice of pediatric nephrology via a Health Insurance Portability and Accountability Act-compliant website.
Of the 225 pediatric nephrology specialists, 134 responded to the survey (59.6% completion rate). Nearly 85% (106/125) of respondents stated that they did not have a formal POCUS program integrated into their fellowship program (Supplemental Appendix 2). In addition, 57.4% (62/108) of respondents did not have any experience with POCUS. Interestingly, among the respondents who incorporated POCUS into their practice, 52.3% (34/65) reported that they achieved competency through self-directed learning.
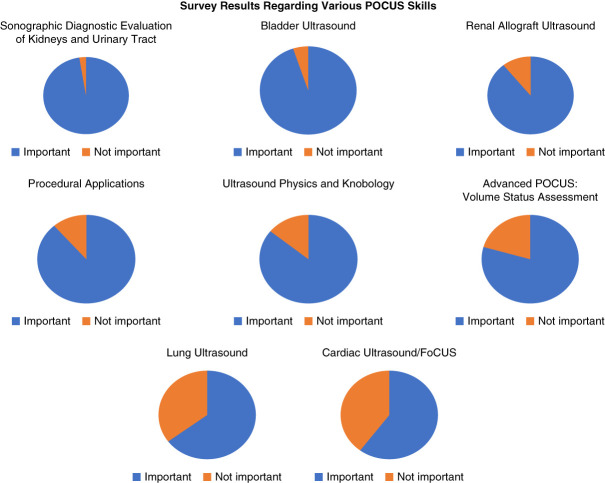
A total of 87% (111/127) of respondents expressed the belief that formal POCUS training should either be mandatory in pediatric nephrology fellowship programs or is of utmost importance for acquiring specific clinical skills (Figures 1 and 2). The details of the results of the survey are provided in Supplemental Appendix 1.
Figure 1.
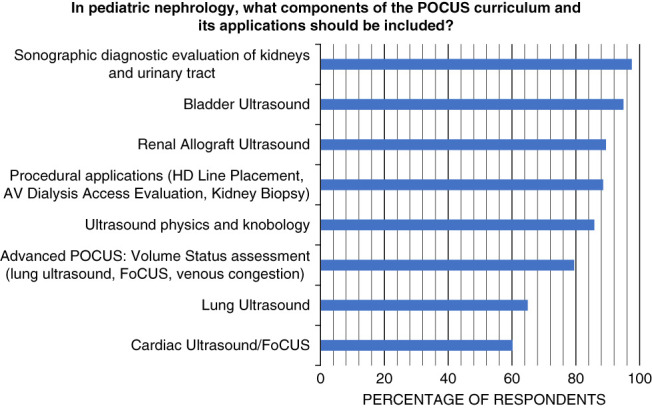
POCUS skills that respondents considered important in a formal POCUS curriculum for pediatric nephrology. Respondents who answered very important or somewhat important on the survey were combined into the total percentage of respondents. AV, arteriovenous; POCUS, point of care ultrasound.
Figure 2.
POCUS skills that respondents considered important in a formal POCUS curriculum for pediatric nephrology. Respondents who answered very important or somewhat important on the survey were combined into the total percentage of respondents.
Barriers to Dedicated POCUS Training
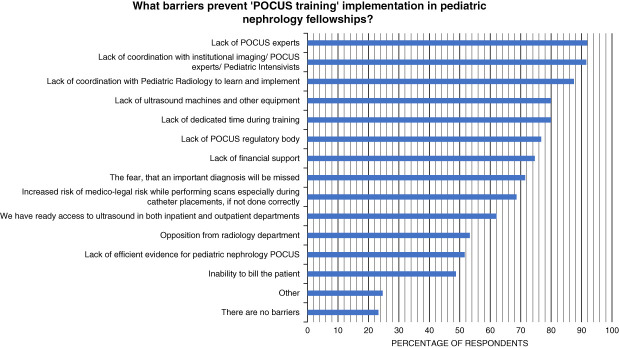
Key barriers to POCUS training were found to be a lack of POCUS experts along with other institutional issues. Most respondents, 91.8% (112/122), identified a lack of POCUS experts as being a very important or somewhat important barrier that prevents POCUS training implementation in pediatric nephrology fellowships (Figure 3).
Figure 3.
Barriers to POCUS training in pediatric nephrology fellowships. Respondents who answered very important or somewhat important on the survey were combined into the total percentage of respondents.
A total of 83% (103/124) of respondents believed that POCUS training would be useful in the pediatric nephrology outpatient setting, such as caring for febrile infants with suspected pyelonephritis. Finally, most respondents, 80.6%, were in favor of integrating a POCUS training program into pediatric nephrology fellowships to improve the doctor–patient relationship and trust. Additional results of the survey are shown in Supplemental Figure 1, A–C.
Delphi Survey for POCUS Curriculum
The authors feel that despite the moderately low response rate (60%), the respondents represented adequate and important part of pediatric nephrology community including program chairs, consultants, and directors of various pediatric nephrology departments (Supplemental Appendix 1). To add to the survey, we conducted a Delphi survey among experts to derive a proposed curriculum. Initially, the core Pediatric Continuous Renal Replacement Therapy-International Collaboration of Nephrologists and Intensivists for Critical Care in Children (PCRRT-ICONIC) leadership group created a list of 16 potential guidelines that incorporated a suggested blueprint for a pediatric nephrology POCUS curriculum, including skills for trainees, measurements of competence, and the scope of use of POCUS in pediatric nephrology. PCRRT-ICONIC is a multinational group of pediatric nephrologists and pediatric critical care physicians. The core leadership group for this project developed potential guidelines on the basis of previous published data on pediatric nephrology POCUS curriculum design and content. Panelists for the Delphi were recruited by the core leadership group on the basis of having >10 years of experience in using POCUS in the adult and pediatric nephrology settings. The panelists made recommendations regarding the guidelines initially generated, and subsequent Delphi rounds were used to finalize the changes and create the final pediatric nephrology POCUS guidelines. Items were considered to reach a consensus when at least 90% of responses were agree or stronger. For items that required revision, comments made by the panelists were considered, and the guideline was changed for subsequent rounds on the basis of the feedback provided. The first Delphi round consisted of ten participants, and the second Delphi round also consisted of ten participants. The Delphi rounds were modified to be electronic, allowing communication to take place via email and online survey platforms (Supplemental Appendix 3).
Qualtrics was used to create and distribute the electronic Delphi survey to participants. Participants were invited to join the panel with email, and three reminders were sent out for each round. All questions in the survey required a response before submission. The responses are provided in Table 1.
Table 1.
Delphi guidelines and results, with mean of answers, where absolutely agree=5, strongly agree=4, agree=3, disagree=2, and absolutely disagree=1
| Finalized Guideline/Practice Point | Round 1 Mean | Round 1 Number Endorsed | Round 2 Mean | Round 2 Number Endorsed |
|---|---|---|---|---|
| POCUS content in pediatric nephrology curriculum | ||||
| Pediatric nephrology POCUS should be introduced by describing ultrasound wave properties, transducer types, ultrasound modes, image orientation and optimization, and common ultrasound artifacts | 4.5 | 9/10 | Finalized in round 1 | Finalized in round 1 |
| Pediatric nephrology POCUS techniques taught should include detection of kidney size and appearance: length, cortical and parenchymal thickness, echogenicity variabilities in neonates and children, as well as pathologies like hydronephrosis, stone, cyst, and free fluid | 4.3 | 9/10 | Finalized in round 1 | Finalized in round 1 |
| Pediatric nephrology POCUS techniques taught should include usage during procedures such as temporary hemodialysis catheter placement, kidney biopsy, and suprapubic urine sample collection | 4.0 | 9/10 | Finalized in round 1 | Finalized in round 1 |
| Pediatric nephrology POCUS techniques taught should include ultrasound-guided placement with consideration of probe selection, measurement of depth, diameter, and volume of flow, as well as evaluation of hemodialysis catheters and PD access after placement | 3.5 | 9/10 | Finalized in round 1 | Finalized in round 1 |
| Pediatric nephrology POCUS techniques taught should include evaluation of renal allografts for hydronephrosis, perinephric collections, vascular anastomosis, and resistive index | 4.1 | 9/10 | Finalized in round 1 | Finalized in round 1 |
| Pediatric nephrology POCUS techniques taught should include lung ultrasound, consisting of detection of A and B lines, as well as detection of pleural effusion, consolidations, and atelectasis | 3.8 | 9/10 | Finalized in round 1 | Finalized in round 1 |
| In the pediatric nephrology POCUS curriculum, a focused cardiac and IVC ultrasound, consisting of usages of M-mode and color Doppler modes and evaluation of cardiac anatomy, and IVC anatomy can be taught to trainees interested in advanced POCUS applications | 3.2 | 6/10 | 4.5 | 10/10 |
| In the pediatric nephrology POCUS curriculum, venous Doppler (VExUS) consisting of selected Doppler echocardiographic parameters such as stroke volume assessment, right ventricular systolic pressure and pulmonary artery pressures as well as Doppler evaluation of the systemic veins including hepatic, portal, and intrarenal veins can be taught to trainees interested in advanced POCUS applications | 2.9 | 6/10 | 4.0 | 10/10 |
| Pediatric nephrology POCUS can be used to identify volume status and hemodynamic stability via a combination of cardiac and pulmonary assessments. This can be taught to trainees interested in advanced POCUS applications | 3.6 | 7/10 | 3.9 | 10/10 |
| Pediatric nephrology POCUS is suitable to answer focused clinical questions at the bedside and provide rapid diagnosis for the trained clinician | 3.9 | 8/10 | 4.4 | 10/10 |
| POCUS curriculum delivery method | ||||
| The ideal pediatric nephrology POCUS curriculum should be multi-modal and incorporate elements from online video-based lectures, in-person demonstrations, hands-on training including simulation sessions, and ongoing practice and assessment | 4.1 | 9/10 | Finalized in round 1 | Finalized in round 1 |
| Competency in pediatric nephrology POCUS should be assessed by trained teachers or objective assessments such as multiple choice question POCUS knowledge assessments and skill assessments with simulations or clinical examination exercises. A minimum number of scans performed should not be the sole assessment of competency | 3.8 | 8/10 | 4.7 | 10/10 |
| Pediatric nephrology POCUS programs require institutional support for billing and quality assurance of studies | 3.8 | 9/10 | Finalized in round 1 | Finalized in round 1 |
| A wide variety of probes is recommended for pediatric nephrology POCUS based on the organ being scanned and patient size | 4.3 | 9/10 | Finalized in round 1 | Finalized in round 1 |
| Need for POCUS curriculum | ||||
| Pediatric nephrology POCUS is a recommended skill for residents and fellows to learn and achieve competence before graduation | 3.9 | 8/10 | 4.6 | 10/10 |
| Pediatric nephrology POCUS is a skill that requires a formalized program and institutional support | 4.0 | 9/10 | Finalized in round 1 | Finalized in round 1 |
IVC, inferior vena cava; PD, peritoneal dialysis; POCUS, point-of-care ultrasound; VExUS, Venous Excess Ultrasonography Score.
POCUS Online Curriculum: Expert Consensus by the PCRRT-ICONIC Group
PCRRT-ICONIC foundation is a group of pediatric nephrologists and pediatric intensivists who are working toward increasing awareness and education regarding the care of critical children with AKI. The current recommendations are a part of the educational initiative of the group.
The optimal POCUS curriculum should be multimodal and incorporate elements from online video-based lectures, in-person demonstrations, hands-on training—including simulation sessions and ongoing practice and assessment. This comprehensive approach offers the most effective pathway to attain proficiency in POCUS. To establish foundational knowledge, trainees should initiate their learning by watching videos and lectures and attend live demonstrations to gain insight into the principles and physics underlying ultrasound and a grasp of the sonographic anatomy. Online resources can mitigate the impact of a shortage of POCUS experts to some extent as fellows can access expert demonstrations of POCUS techniques, particularly those relevant to pediatric nephrology. Resources, such as the pediatric intensive care unit nephrology courses online platform (https://www.picunephrologyvideos.com/s/store), include lessons on fundamentals of POCUS, pediatric kidney transplant, critical care nephrology, and pertinent procedures for pediatric nephrology fellows (Supplemental Figure 2). This has been developed by the pediatric nephrologists and POCUS experts and has been endorsed by the PCRRT-ICONIC group. The pediatric nephrology POCUS module consists of 25 videos that include image acquisition techniques, clinical vignettes, and pearls, followed by self-assessment questions, live sessions (held annually at PCRRT-ICONIC Critical Care Nephrology courses), and an online Objective Structured Clinical Examination (as a part of online self-assessment test and also part of the annual in-person courses which involve direct observation in a simulated environment) to solidify knowledge gains.
Blueprint of POCUS in Pediatric Nephrology Curriculum
Considering the limited literature on multiorgan POCUS in pediatric nephrology, our expert panel has derived recommendations from the adult nephrology literature, which is sparse as well. These suggestions may be revised in our subsequent works, as more data become available.
The POCUS curriculum should cover ultrasound physics, image acquisition techniques, image interpretation, and clinical integration across various sonographic scenarios. Table 2 presents a framework delineating the core topics and essential elements to include within a curriculum, derived from adult nephrology literature and adapted to suit the needs of pediatric nephrology.11,12
Table 2.
Suggested blueprint of point of care ultrasound curriculum
| Topic | Key Elements |
|---|---|
| 1. Ultrasound physics and knobology | • Ultrasound wave properties, transducer types • Introduction to basic modes: B, M, color flow, power Doppler, spectral Doppler • Basics of image optimization and image orientation • Common ultrasound artifacts |
| 2. Sonography of the kidneys in children | • Technique: probe selection in neonates and children, positioning, and description of movements • Sonographic anatomy • Kidney size and appearance: length, cortical and parenchymal thickness, echogenicity variabilities in neonates and children • Core pathologies: hydronephrosis, stone, cyst, free fluid |
| 3. Ultrasound-guided procedures in PICU | • Temporary hemodialysis catheter placement: probe selection, vessel selection, needle tip visualization, catheter insertion, placement confirmation • Renal biopsy (native and transplant): probe and site selection, visualization of the renal cortex, vasculature, needle tip and surrounding anatomy (e.g., bowel loop interference in the case of allograft), evaluation of post-biopsy hematoma/Doppler signs • Suprapubic urine sample collection |
| 4. Lung ultrasound | • Technique: probe selection, positioning, and normal movements • Sonographic zones of evaluation • A and B lines • Other abnormalities: pleural effusion, consolidations, atelectasis |
| 5. IVC and cardiac ultrasound for assessment of intravascular volume status in children | • Rationale and limitations • Technique: probe and preset selection, probe positioning, basic cardiac views • M-mode and color Doppler • Cardiac anatomy and evaluation of five Es • IVC ultrasound: basics and pitfalls |
| 6. Access for dialysis: hemodialysis and PD | • Anatomy of vascular access: gross and sonographic correlations • Technique: probe selection, measurement of depth, diameter, volume flow • Core pathologies and assessment of newly placed AV fistula and PD access |
| 7. Integrative assessment of fluid volume status | • Basics of multiorgan POCUS for objective evaluation of hemodynamics • Patient case studies to understand the clinical integration of multi-organ ultrasound |
| 8. Renal allograft ultrasound and urinary bladder ultrasound | • Technique: probe selection, positioning, and description of movements • Allograft anatomy: basics • Allograft core pathologies: hydronephrosis, perinephric collections, vascular anastomosis, and resistive index • Urinary bladder: anatomy, volume calculation, urinary retention, indwelling urinary catheter malposition |
| 9. Advanced skill: limited Doppler echocardiography, venous Doppler (VExUS) | • Rationale, basics of technique, probe selection, and positioning • Selected Doppler echocardiographic parameters such as stroke volume assessment, right ventricular systolic pressure and pulmonary artery pressures. Doppler evaluation of the systemic veins including hepatic, portal and intrarenal veins • Case studies highlighting use of Doppler echocardiography and VExUS in selected pediatric subsets |
AV, arteriovenous; IVC, inferior vena cava; PD, peritoneal dialysis; PICU, pediatric intensive care unit; POCUS, point-of-care ultrasound; VExUS, Venous Excess Ultrasonography Score.
The essential components mentioned above should be delivered to trainees through methods tailored to local requirements and resources. This may involve in-person lectures, self-directed online learning, hands-on training under the direct or indirect guidance of experts, and simulation exercises. Some challenges associated with training novice POCUS users involve the absence of established pediatric nephrology-specific guidelines, limited training opportunities for practicing nephrologists, and absence of certification mechanisms to validate competency.11 Several of the challenges outlined by the respondents concerning the establishment of a dedicated pediatric nephrology POCUS program were associated with institutional factors. The primary obstacles in developing a POCUS curriculum included a shortage of pediatric nephrologists trained in POCUS, insufficient coordination with various departments such as radiology, limited financial support, and inadequate equipment availability.
Potential solutions encompass cost-sharing initiatives with other departments interested in POCUS, seeking reimbursement by billing for the studies, investing in more cost-effective handheld devices albeit acknowledging their limitations (e.g., lower image quality), and participating in workshops conducted in partnership with specialties already performing POCUS, such as critical care or emergency medicine. Furthermore, seeking guidance from external experts located in affiliated institutions through online consultations is another effective approach until sufficient faculty members attain proficiency in basic sonographic applications.3,12–14 As more faculty in the department acquire proficiency in POCUS, the potential for improved patient experiences and outcomes could result in increased institutional support.
An essential aspect to consider when developing the pediatric nephrology POCUS curriculum is determining the optimal duration for training. Although it has been demonstrated that brief workshops can boost learners' confidence, it remains uncertain whether this enhanced confidence translates into competence.13 Furthermore, without ongoing, consistent practice after a short training program, the retention of acquired ultrasound skills tends to be suboptimal.15 The development of a POCUS program needs to be based on the concept of longitudinal learning. While there is limited pediatric literature in this area, Bhargava et al. conducted a single-center study in which they implemented a 7-week training program. This initiative resulted in a noteworthy enhancement in participants' self-reported knowledge and learning.16
Furthermore, there is a need to determine the most effective means of assessing competency and granting certification. While setting minimum standards, such as requiring a specific number of scans, is crucial to ensure learners engage in repetitive learning, this alone certainly does not guarantee competency. Therefore, future research should explore how to assess competency in a manner tailored to individual learners. Until more data are available, guidelines for the minimum number of scans in adult nephrology certification programs (e.g. POCUS Certification Academy, American Society of Diagnostic and Interventional Nephrology) and expert panels (e.g. International Alliance for POCUS in Nephrology) may be tentatively applied to pediatric programs. Presently, these range from 25 to 50 scans, depending on whether the sonographic application is deemed basic or advanced.17–20
Table 3 lists milestones according to the level of proficiency in POCUS that trainees are expected to attain during the course of their nephrology fellowship training.12 This can be adapted to suit local needs and practice patterns in different countries.
Table 3.
Expected milestones according to level of proficiency in point-of-care ultrasonography
| Competency | Level I | Level II | Level III |
|---|---|---|---|
| Technical skills/image interpretation | Obtain adequate grayscale images of vascular access, lung, lower urinary tract, bladder, abdomen (for ascites), and kidney | Obtain adequate grayscale and color Doppler images of heart (images such as internal vena cava) | Obtain adequate spectral images of cardiovascular system (heart, vascular access, abdominal veins) |
| Distinguish normal/abnormal structures | Locate common abnormalities | Identify rarely encountered findings | |
| Appropriate guide of internal jugular/femoral dialysis access placement | |||
| Practice-based learning and professionalism | Appropriate explanation and consideration when discussing with patients and their families | Identify and improve on gaps in knowledge and skill set | Integrate clinical practice guidelines to create plan for management from POCUS results |
| Inform POCUS staff of upcoming scan in timely manner | Sound understanding of when to present POCUS patients based on nephrology literature | Understand and apply appropriate billing compliance and policies | |
| Encourage feedback from staff for improvement | Report incidental findings to POCUS staff in timely manner while taking responsibility for scans | Integrate findings for publication in medical journal or presentation at a conference | |
| Handle/store equipment in appropriate fashion |
POCUS, point-of-care ultrasound.
There is an imminent need for pediatric nephrology societies to establish committees comprising multidisciplinary POCUS experts to shape the future of this essential skill. The primary focus of these expert committees should be to determine the optimal learning duration for acquiring these skills and set competency standards for granting institutional privileges to perform and bill for the scans. At this time, privileges are typically granted on the basis of local criteria or guidelines set forth by professional organizations such as the American College of Emergency Physicians. It is worth noting that in some cases, conditional privileges may be granted, contingent on periodic quality assessments conducted by institutional experts.10,14
In our survey, approximately half (52%) of the participants indicated attaining competency through self-directed learning, and the overwhelming majority (87%) emphasized the necessity for mandatory training within pediatric nephrology fellowship programs. Unlike structured longitudinal training during residency or fellowship, which involves graded supervision, self-learning presents challenges such as overlooking core concepts, fostering overconfidence, and neglecting one's own or equipment limitations. In fact, the Emergency Care Research Institute has recognized the adoption of POCUS without necessary safeguards as a significant health technology hazard.21 However, we acknowledge that practicing physicians face resource constraints and must invest time to acquire proficiency. Collaborating with other POCUS-performing departments within the hospital, seeking feedback and direct supervision where feasible, can be beneficial. This collaboration should aim to meet the minimum competency criteria set forth by the hospital credentialing committee. Another challenge is the maintenance of competency once acquired. A study examining 30 internal medicine graduates, who had received POCUS training during residency but did not routinely use it, found that after 2 years, nearly all failed the same competency test they had passed during training.22 Therefore, it is crucial to implement a recredentialing and quality assessment program to ensure that the highest standards of POCUS practices are maintained. Establishing a centralized image archiving system, akin to radiology, facilitates quality assessment by allowing the retrieval of images from the patient's chart. It also helps seeking expert opinion when in doubt and providing timely feedback to trainees. For credentialed physicians, the quality assessment committee should review a sample of studies performed by each physician periodically to ensure proper interpretation and clinical integration. While recognizing the variability in image archiving processes across different countries, it is important to emphasize that quality assurance is a fundamental component of any successful program, aiming to prevent inadvertent harm to patients. We anticipate that this POCUS training curriculum for pediatric nephrology marks the initial phase in assisting fellowship programs and hospital credentialing committees in developing local standards.
POCUS is a bedside diagnostic tool that is steadily gaining popularity across various pediatric specialties. Its purpose is to provide anatomical and physiological information that facilitates prompt diagnosis and guides various bedside procedures. In pediatric nephrology, POCUS can be helpful across all the practice settings, including the outpatient clinic, inpatient ward, critical care unit, and the dialysis unit. A multicenter, multinational group of respondents have identified current challenges in implementing POCUS at their institutions. The main challenges include lack of formal training, lack of certification, and lack of equipment for use. The standardized use of POCUS among pediatric nephrologists will potentially lead to earlier and more accurate diagnosis and decreased complications of the procedures and improve patient outcomes. This is, however, a challenging endeavor that demands institutional backing and multidisciplinary collaboration to establish guidelines and certification processes to ensure optimal and safe use of POCUS. The establishment of a structured pediatric nephrology POCUS program is essential to train practicing clinicians and fellows in becoming POCUS experts. The suggested POCUS curriculum in the present recommendations is expected to serve as a foundation for POCUS education in pediatric nephrology centers worldwide.
Supplementary Material
Footnotes
S.K.S. and J.M. share first authorship.
Disclosures
Disclosure forms, as provided by each author, are available with the online version of the article at http://links.lww.com/KN9/A455.
Funding
None.
Author Contributions
Conceptualization: Carolyn Abitbol, Khalid A. Alhasan, Eduardo R. Argaiz, Hamidreza Badeli, Timothy Bunchman, Marissa DeFreitas, Jieji Hu, Meenal Kalra, Abhilash Koratala, John Mahan, Mignon McCulloch, Nikhil Nair, Rupesh Raina, James Raynor, Nathaniel Reisinger, Sidharth Kumar Sethi, Vivek Sharma, Yogen Singh, Kritika Soni, Jonathan VanGeest, Hui Kim Yap.
Data curation: Carolyn Abitbol, Khalid A. Alhasan, Eduardo R. Argaiz, Hamidreza Badeli, Timothy Bunchman, Marissa DeFreitas, Jieji Hu, Meenal Kalra, John Mahan, Mignon McCulloch, Nikhil Nair, Rupesh Raina, James Raynor, Nathaniel Reisinger, Sidharth Kumar Sethi, Vivek Sharma, Yogen Singh, Kritika Soni, Jonathan VanGeest, Hui Kim Yap.
Formal analysis: Carolyn Abitbol, Khalid A. Alhasan, Eduardo R. Argaiz, Timothy Bunchman, Marissa DeFreitas, Jieji Hu, Meenal Kalra, Abhilash Koratala, John Mahan, Mignon McCulloch, Nikhil Nair, Rupesh Raina, James Raynor, Nathaniel Reisinger, Sidharth Kumar Sethi, Vivek Sharma, Yogen Singh, Kritika Soni, Jonathan VanGeest, Hui Kim Yap.
Investigation: Rupesh Raina, Sidharth Kumar Sethi.
Methodology: Rupesh Raina.
Project administration: John Mahan, Rupesh Raina.
Resources: Rupesh Raina.
Supervision: Carolyn Abitbol, Khalid A. Alhasan, Eduardo R. Argaiz, Hamidreza Badeli, Timothy Bunchman, Marissa DeFreitas, Abhilash Koratala, Mignon McCulloch, Nikhil Nair, Rupesh Raina, James Raynor, Vivek Sharma, Yogen Singh, Kritika Soni, Hui Kim Yap.
Validation: Carolyn Abitbol, Khalid A. Alhasan, Eduardo R. Argaiz, Hamidreza Badeli, Timothy Bunchman, Marissa DeFreitas, Abhilash Koratala, Mignon McCulloch, Nikhil Nair, Rupesh Raina, James Raynor, Nathaniel Reisinger, Sidharth Kumar Sethi, Vivek Sharma, Yogen Singh, Kritika Soni, Jonathan VanGeest, Hui Kim Yap.
Visualization: Carolyn Abitbol, Khalid A. Alhasan, Eduardo R. Argaiz, Hamidreza Badeli, Timothy Bunchman, Marissa DeFreitas, Jieji Hu, Meenal Kalra, Abhilash Koratala, John Mahan, Mignon McCulloch, Nikhil Nair, Rupesh Raina, James Raynor, Nathaniel Reisinger, Sidharth Kumar Sethi, Vivek Sharma, Yogen Singh, Kritika Soni, Jonathan VanGeest, Hui Kim Yap.
Writing – original draft: Carolyn Abitbol, Khalid A. Alhasan, Eduardo R. Argaiz, Hamidreza Badeli, Timothy Bunchman, Marissa DeFreitas, Jieji Hu, Meenal Kalra, Abhilash Koratala, John Mahan, Mignon McCulloch, Nikhil Nair, Rupesh Raina, James Raynor, Nathaniel Reisinger, Sidharth Kumar Sethi, Vivek Sharma, Yogen Singh, Kritika Soni, Jonathan VanGeest, Hui Kim Yap.
Writing – review & editing: Carolyn Abitbol, Khalid A. Alhasan, Eduardo R. Argaiz, Hamidreza Badeli, Timothy Bunchman, Marissa DeFreitas, Jieji Hu, Meenal Kalra, Abhilash Koratala, John Mahan, Mignon McCulloch, Nikhil Nair, Rupesh Raina, James Raynor, Nathaniel Reisinger, Sidharth Kumar Sethi, Vivek Sharma, Yogen Singh, Kritika Soni, Jonathan VanGeest, Hui Kim Yap.
Data Sharing Statement
All data are included in the manuscript and/or supporting information.
Supplemental Material
This article contains the following supplemental material online at http://links.lww.com/KN9/A454.
Supplemental Appendix 1. Details of the POCUS survey results.
Supplemental Appendix 2. POCUS survey questionnaire circulated to Pediatric Nephrology community.
Supplemental Appendix 3. Delphi methods.
Supplemental Figure 1. (A–C) Additional results of POCUS in Pediatric Nephrology survey.
Supplemental Figure 2. Online dashboard of lectures for POCUS in pediatric nephrology curriculum.
References
- 1.Conlon TW Nishisaki A Singh Y, et al. Moving beyond the stethoscope: diagnostic point-of-care ultrasound in pediatric practice. Pediatrics. 2019;144(4):e20191402. doi: 10.1542/peds.2019-1402 [DOI] [PubMed] [Google Scholar]
- 2.Moore CA, Ross DW, Pivert KA, Lang VJ, Sozio SM, O'Neill WC, IV. Point-of-Care ultrasound training during nephrology fellowship: a national survey of fellows and program directors. Clin J Am Soc Nephrol. 2022;17(10):1487–1494. doi: 10.2215/CJN.01850222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reisinger NC, Koratala A. Incorporating training in POCUS in nephrology fellowship curriculum. Clin J Am Soc Nephrol. 2022;17(10):1442–1445. doi: 10.2215/CJN.09580822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evans N Gournay V Cabanas F, et al. Point-of-care ultrasound in the neonatal intensive care unit: international perspectives. Semin Fetal Neonatal Med. 2011;16(1):61–68. doi: 10.1016/j.siny.2010.06.005 [DOI] [PubMed] [Google Scholar]
- 5.Ambasta A Balan M Mayette M, et al. Education indicators for internal medicine point-of-care ultrasound: a consensus report from the Canadian internal medicine ultrasound (CIMUS) group. J Gen Intern Med. 2019;34(10):2123–2129. doi: 10.1007/s11606-019-05124-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hassanzadeh Rad A, Badeli H. Point-of-care ultrasonography: is it time nephrologists were equipped with the 21th century’s stethoscope? Iran J Kidney Dis. 2017;11(4):259–262. PMID: 28794287 [PubMed] [Google Scholar]
- 7.Wolters K, Herget-Rosenthal S, Langenbeck M. Renal sonography. Internist (Berl). 2012;53(3):282–290. doi: 10.1007/s00108-011-2960-y [DOI] [PubMed] [Google Scholar]
- 8.Mahdipour S, Saadat SNS, Badeli H, Rad AH. Strengthening the success rate of suprapubic aspiration in infants by integrating point-of-care ultrasonography guidance: a parallel-randomized clinical trial. PLoS One. 2021;16(7):e0254703. doi: 10.1371/journal.pone.0254703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh Y Tissot C Fraga MV, et al. International evidence-based guidelines on point of care ultrasound (POCUS) for critically ill neonates and children issued by the POCUS working group of the European Society of Paediatric and Neonatal Intensive Care (ESPNIC). Crit Care. 2020;24(1):65. doi: 10.1186/s13054-020-2787-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sethi SK, Raina R, Koratala A, Rad AH, Vadhera A, Badeli H. Point-of-care ultrasound in pediatric nephrology. Pediatr Nephrol. 2023;38(6):1733–1751. doi: 10.1007/s00467-022-05729-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sethi SK, Raina R, McCulloch M, Bunchman TE. Advances in Critical Care Pediatric Nephrology: Point of Care Ultrasound and Diagnostics. Springer; 2021. [Google Scholar]
- 12.Koratala A, Olaoye OA, Bhasin-Chhabra B, Kazory A. A blueprint for an integrated point-of-care ultrasound curriculum for nephrology trainees. Kidney360. 2021;2(10):1669–1676. doi: 10.34067/KID.0005082021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koratala A, Bhattacharya D, Kazory A. Helping patients and the profession: nephrology-oriented point-of-care ultrasound program for internal medicine residents. Clin Nephrol. 2019;91(5):321–322. doi: 10.5414/CN109652 [DOI] [PubMed] [Google Scholar]
- 14.Koratala A, Reisinger N. POCUS for nephrologists: basic principles and a general approach. Kidney360. 2021;2(10):1660–1668. doi: 10.34067/KID.0002482021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hempel D Stenger T Campo Dell’ Orto M, et al. Analysis of trainees’ memory after classroom presentations of didactical ultrasound courses. Crit Ultrasound J. 2014;6(1):10. doi: 10.1186/2036-7902-6-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bhargava V, Haileselassie B, Rosenblatt S, Baker M, Kuo K, Su E. A point-of-care ultrasound education curriculum for pediatric critical care medicine. Ultrasound J. 2022;14(1):44. doi: 10.1186/s13089-022-00290-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koratala A, Segal MS, Kazory A. Integrating point-of-care ultrasonography into nephrology fellowship training: a model curriculum. Am J Kidney Dis. 2019;74(1):1–5. doi: 10.1053/j.ajkd.2019.02.002 [DOI] [PubMed] [Google Scholar]
- 18.Romero-González G Argaiz ER Koratala A, et al. Towards standardization of POCUS training in Nephrology: the time is NOW. Nefrologia (Engl Ed). 2024;44(1):5–9. doi: 10.1016/j.nefro.2023.01.003 [DOI] [PubMed] [Google Scholar]
- 19.American Society of Diagnostic and Interventional Nephrology. POCUS Certification. 2023. Accessed December 24, 2023. https://cdn.ymaws.com/www.asdin.org/resource/resmgr/certification/Final_POCUS_Application_.pdf [Google Scholar]
- 20.Point-of-Care Ultrasound Nephrology Certification. POCUS Certification Academy. 2022. Accessed December 24, 2023. https://www.pocus.org/start-your-pocus-journey/point-of-care-ultrasound-pocus-nephrology-certification/ [Google Scholar]
- 21.ECRI. 2020 Top 10 Health Technology Hazards Executive Brief. 2020. Accessed December 24, 2023. https://www.ecri.org/landing-2020-top-ten-health-technology-hazards [Google Scholar]
- 22.Kimura BJ, Sliman SM, Waalen J, Amundson SA, Shaw DJ. Retention of ultrasound skills and training in "Point-of-Care" cardiac ultrasound. J Am Soc Echocardiogr. 2016;29(10):992–997. doi: 10.1016/j.echo.2016.05.013 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data are included in the manuscript and/or supporting information.