Overview:
The ABCD has published 34 guidelines in two Special Issues of the Journal of Feline Medicine and Surgery (JFMS): the first in July 2009 (Volume 11, Issue 7, pages 527–620) and the second in July 2013 (Volume 15, Issue 7, pages 528–652). The present article contains updates and new information on 18 of these (17 disease guidelines and one special article ‘Prevention of infectious diseases in cat shelters’). For detailed information, readers are referred to the guidelines published in the above-mentioned JFMS Special Issues.
Feline panleukopenia
Canine parvovirus type 2 (CPV-2), which is closely related to feline panleukopenia virus (FPV), was described in 1978 as a new parvovirus (cited in Carmichael 1 ). It evolved from FPV with the acquisition of five or six amino acid changes in the capsid protein 2 and does not infect cats. However, during further adaptation to the dog, which most likely occurred in the raccoon, the virus underwent amino acid changes that made the mutated virus bind more efficiently to the canine cellular receptor, while retaining the ability to infect cats.3,4 This led to the emergence of the new type, CPV-2a, which contains a series of further mutations including those at amino acid 426 of the VP2 that determine the antigenic types 2a, 2b and 2c. The parvoviruses currently circulating in dog populations worldwide (genetically and antigenically defined as types CPV-2a, -2b and -2c) can infect cats and may even cause disease.5 –7 However, CPV infections of cats are rare in Europe and the USA, and the virus has only sporadically been found in diagnostic material. 6 CPV was isolated from feline peripheral blood lymphocytes after numerous blind passages, and viral DNA was demonstrated subsequently by PCR. 8 Recently, however, a case of CPV-2c infection in a cat with severe clinical disease was described in Portugal. 9
During the evolution of FPV to CPV-2 with its various antigenic types, neutralising epitopes have become modified such that cross-neutralisation by FPV antisera is markedly lower against the newer viruses. 10
Persistent infections with viral shedding are rare; using PCR, healthy cats have been found positive for FPV in faeces over weeks, 11 and CPV-2 viruses could be isolated from the faeces of healthy cats in the UK in two shelters. 12 It is unknown whether these findings are of epidemiological significance.
The parvovirus sequences encountered in wild carnivores (pumas, coyotes, raccoons, and others) revealed a wide genotypic variation. This finding suggests infection of predators by their parvovirus-infected prey, and hence a new route of infection. 13
Following intrauterine infection, FPV antigen persists in the cerebellum of kittens for weeks. 14
Detailed information on the prevention and management of parvovirus infection in cats is provided in the ABCD guidelines 15 and a previous update. 16
Feline herpesvirus infection
Feline herpesvirus (FHV), together with feline calicivirus, is involved in the feline upper respiratory tract syndrome. In addition, FHV has been recognised as the most important cause of corneal ulceration, both superficial and deep, and in particular of dendritic ulcers. The infection becomes latent, allowing lifelong persistence of the virus, which is sporadically interrupted by episodes of viral reactivation and re-excretion. Thiry et al 17 and Horzinek et al 16 presented a table summarising recommendations for treatment of acute FHV ocular disease. The amino acid L-lysine has been proposed for systemic treatment, to be administered as a bolus, separate from food. No reports of side effects have been published, but findings on efficacy are conflicting.18 –25 Cave et al 26 investigated the effects of physiological concentrations of L-lysine on the in vitro replication of FHV at L-arginine levels sufficient to maintain cell growth. FHV was not inhibited at any L-lysine concentration studied. The in vivo efficacy of L-lysine treatment on primary and recurrent FHV infection is unknown.
Feline leukaemia virus infection
Feline leukaemia virus (FeLV) is a gamma retrovirus affecting domestic cats worldwide. It also infects small wild cats including Felis silvestris, European and Iberian lynxes, Florida panthers and the Chilean wildcat (Leopardus guigna).27 –30 The prevalence of FeLV infection in Europe and North America has greatly diminished. In individually kept cats it is low; often, but not everywhere, less than 1%.31 –35
After infection of bone marrow cells, viraemia develops within a few weeks. Mainly lymphocytes and monocytes are infected, whereas later infection involves mostly neutrophils. 36 Viraemia may be overcome by the immune system (transient viraemia) in some cats, 37 whereas others develop a persistent viraemia. A smaller proportion (~5%) exhibits an atypical course of infection, displaying antigenaemia, but no or only low-level viraemia.38,39 A cat that has overcome viraemia remains latently infected. Reactivation may occur; it is not clear how often this happens under field conditions, but it is believed to be rare. Generally, up to 10% of all feline blood samples submitted to a laboratory prove to be provirus-positive and p27-negative; since FeLV may be reactivated in some of these cats, they should be considered latently infected.35,40,41 Probably no cat can clear an FeLV infection from all cells.
Experimentally, susceptible kittens can be protected from FeLV infection after passive immunisation with high-titred specific antisera. 38 This observation suggests that antibodies have a role in protection; however, once persistent viraemia has become established, treatment with neutralising monoclonal antibodies to FeLV has proven ineffective. 42
In an experimental study, seroconversion was observed in cats as the sole evidence of FeLV infection. 43 These cats had been exposed once intranasally to low doses of FeLV (10,000 FFU). Since some of them seroconverted, it was concluded that the virus had replicated somewhere to sufficient levels to trigger antibody synthesis. PCR analysis of several organs was negative, indicating that further replication must have been controlled by the immune system.
In most situations, individual cats are tested for FeLV infection. However, when the cost of testing is a limitation, pooled saliva samples can be used to detect FeLV RNA; the RNA PCR is sufficiently sensitive to detect a single infected cat in a pool of up to 30 samples. This approach may be chosen when screening multi-cat households. 44 While all viraemic cats are positive for FeLV RNA in saliva, a few may shed FeLV RNA in saliva, but are not (yet) viraemic or antigenaemic. 45
The observation that antibodies can develop as the sole parameter of exposure to FeLV 43 led to the examination of various FeLV antigens to assess their diagnostic potential to detect antibodies. In contrast to published results, 46 a recombinant preparation of FeLV p15(E) proved highly effective for the detection of antibodies induced by FeLV infection and thus for the diagnosis of a previous infection. 47
The HIV integrase inhibitor raltegravir was found to inhibit FeLV replication in vitro. 48 The drug is tolerated well by cats, and within 1 week leads to a marked reduction in viral loads. However, this is not sufficient for the immune system to control the viraemia, and treatment must be continued over long periods in order to maintain low viral loads and prevent disease [EBM grade III]. 49
In many experiments it was shown that no FeLV vaccine provides complete protection or prevents infection. Cats that overcome p27 antigenaemia without exception test provirus-positive in blood, and also test positive for viral RNA in plasma, although at much lower levels than persistently viraemic cats [EBM grade III]. 50 These experiments confirm that FeLV vaccination does not induce sterilising immunity and does not protect cats from infection. However, cats vaccinated with conventional, adjuvanted, whole inactivated virus vaccines did not show p27, viral RNA or DNA after a low-dose challenge with the subgroup A virus FeLV A/61E. 51 Various factors may have played a role: the challenge virus was used at a very low dose (10,000 TCID50 injected once, intraperitoneally), the assays used were less sensitive than those used by Hofmann-Lehmann et al, 50 and the cats had a different genetic background. Testing for FeLV in internal organs would have resulted in observations as reported by Major et al. 43 Thus, the proposition remains valid that vaccination against FeLV protects cats from disease but not from infection.
Until recently, no data had been published to demonstrate that immunity lasts longer than 1 year after primary vaccination; most vaccine manufacturers therefore recommend annual boosters. However, the demonstration that one FeLV vaccine provided immunity for at least 2 years 52 [EBM grade II] suggests that this may also apply to other vaccines. Combined with the lower susceptibility of adult cats to FeLV infection, the ABCD recommends that, in cats older than 3 years, a booster immunisation every 2–3 years is sufficient.
Wherever possible, cats entering a shelter should be kept in quarantine for at least 3 weeks, if not (re)homed sooner. All incoming cats (at least in shelters that allow contact between cats after the quarantine period) should be screened for FeLV antigen and feline immunodeficiency virus (FIV) antibody, and ideally also for FeLV antibody. 47 Antigen-negative but antibody-positive results suggest that the cat is not viraemic/antigenaemic, but may be latently infected. Therefore, PCR for FeLV DNA should additionally be performed. If the PCR shows a high FeLV DNA load, this cat should prudently be considered latently infected; the cat should best be placed in a home without other cats for several months. If only an FeLV antigen test is performed, cats testing negative should ideally be retested 6 weeks later (and kept in quarantine for this time period), as it may take 4–6 weeks after infection for the test to return positive results. To prevent (re)activation of other infections caused by the stress of entering the shelter, newcomer cats should be kept isolated and observed for clinical signs. After quarantine, they can be introduced into small groups of healthy cats. FeLV antigen- and/or FIV antibody-positive cats should be kept separate, but may be housed together with other retrovirus-positive cats, and adopted out to suitable homes as soon as possible.
The ABCD does not recommend euthanasia of healthy FeLV-positive cats. However, if no adequate home can be found, if separation from the rest of the population is impossible, or if the cat is sick, euthanasia should be considered. Detailed recommendations are provided in the ABCD guidelines ‘Prevention of infectious diseases in cat shelters’. 53
Detailed information on the prevention and management of feline leukaemia virus infection is provided in the ABCD guidelines 54 and a previous update. 16
Feline immunodeficiency virus infection
It is generally accepted that feline immunodeficiency virus (FIV) infection can induce clinical signs of immunodeficiency, leading to opportunistic infections or lymphomas, and clinical signs consistent with immunodeficiency in natural infection have been documented. 55 However, in some cats the clinical signs are mild, which likely reflects both heterogeneity among circulating field isolates as well as host factors, and it has been reported that many FIV-infected cats have a normal life expectancy.56 –58 Therefore, surrogate markers are required to provide an objective assessment of FIV progression in individual cats. Recently it was shown that viruses dominating in early infection display a distinct receptor usage phenotype and that the emergence of viruses with an altered receptor usage phenotype coincides with the onset of immunodeficiency. 59 Accordingly, viral phenotyping might assist in the clinical staging of individual cats diagnosed with FIV infection.
FIV infection was found to be prevalent in a survey of four large-scale hoarding situations; 60 this high prevalence was probably related to the fact that the cats were living in close confinement under stressful conditions, and exhibiting aggressive behaviour. Therefore, it is recommended that cats should be tested for FIV infection at the time of seizure during hoarding investigations, as the results will influence housing decisions, medical care and adoption options.
FIV infection is also common in rescue shelters and it is recommended that all cats in rescue centres should be neutered and kept indoors, in order to reduce the risk of territorial aggression, which can result in penetrating bite wounds and consequently FIV transmission. This recommendation is supported by studies linking cat bite wounds and abscesses with FIV infection.61,62 A recent survey of cats in a rescue shelter, in which FIV-infected cats were housed together with uninfected cats, found no evidence of FIV transmission, in spite of the cats having unrestricted access, and sharing food and water bowls, litter trays and bedding for several years. 63 However, it is possibly significant that the cats had been neutered before entering this shelter and the median age of the uninfected cats was 4 months; kittens are a low risk group for FIV infection 64 because territorial aggression has not yet developed. Similarly, neutered cats are less likely to display territorial aggression than intact cats and, therefore, FIV transmission might be more likely to occur in rescue centres housing older cats, especially if those cats exhibit aggressive behaviour.
Detailed information on the prevention and management of feline immunodeficiency virus infection is provided in the ABCD guidelines 65 and a previous update. 16
Rabies
Rabies is caused by a Lyssavirus, a member of the Rhabdoviridae family. The genus Lyssavirus contains 12 species: rabies virus, Mokola virus, Lagos bat virus and Duvenhage virus from Africa, European bat lyssaviruses (EBLV) 1 and 2, Australian bat lyssavirus, and five recently recognised species (International Committee on Taxonomy of Viruses, 2012). Each of these viruses is considered capable of causing a rabies-like disease in animals and humans.
Various control measures (eg, vaccination of wildlife, immunisation of dogs and cats, diagnostic measures, control of pet movements) eliminated rabies from large regions of Europe, especially its western and northern parts. In rabies-free countries, however, though sporadic, the illegal importation of pets from regions where this disease is endemic poses an increasing risk. 66 Rabies was recently recognised in a kitten imported into France from Morocco, 67 and a few cases in dogs were documented in Europe recently.
As a result of the mass vaccination of dogs in many areas affected by wildlife rabies, cats have become the companion animal species most commonly reported as rabid, as is the case in many states of the USA. 68 In a recent report from Pennsylvania, among 2755 rabid animals with reported human exposure, as many as 799 (29.0%) were free-ranging cats, whereas only 57 (2.1%) were dogs. 69
Because of the public health risk associated with susceptible domestic cats becoming infected following exposure to rabid wild or domestic animals, all cats with outdoor access in endemic areas should be vaccinated. The vaccine should be administered in accordance with local or state regulations. In countries where rabies is absent, rabies vaccination is indicated when a cat moves or travels to an area where rabies is endemic.
EU Regulation 576/2013 established new rules for the non-commercial movement of pet animals (dogs, cats and ferrets) between EU countries as of 29 December 2014. According to these rules, all such cats should be identified by microchip (or tattoo, if applied before 4 July 2011) and vaccinated against rabies; a 21-day waiting period following primary vaccination is required. This means that for the purpose of travel, cats generally must be at least 15 weeks old, as 12 weeks is the minimum age for rabies vaccination. Some countries accept younger animals without rabies vaccination under certain conditions, but most do not (for details see http://ec.europa.eu/food/animal/liveanimals/pets/nat_rules_dogscatferret_en.htm). According to the recent pet movement regulation, serological testing for rabies neutralising antibodies is no longer required before entry into any EU member state.
Detailed information on the prevention and management of rabies in cats is provided in the ABCD guidelines 70 and a previous update. 16
Feline infectious peritonitis
Given the number of major recent developments in the field of feline coronavirus (FCoV) and feline infectious peritonitis (FIP), fully updated ABCD guidelines on FIP will be published in the near future. For the purpose of this interim update, some key developments in FIP diagnosis and treatment are outlined below.
Among the most interesting of the developments relating to FIP diagnosis is the advent of a commercially available reverse transcription PCR (RT-PCR) test which distinguishes mutations on the spike of type I FCoVs that are associated with the development of systemic spread of the virus. 71 There is a question of this test not being as sensitive as conventional FCoV RT-PCR, not only because it does not detect type II FCoVs, but also because the spike protein is the protein most subject to evolutionary immune pressure, and so the spike gene is the most variable of the coronavirus genes, and thus primers may not bind, giving a false negative result.
It is the view of the ABCD that RT-PCR is a preferred method of FIP confirmation for effusions, over immunofluorescence of macrophages, which is less widely available and more prone to human error.
In a comparison of commercially available FCoV antibody tests, 16 applications of FCoV antibody tests were considered: sensitivity was deemed extremely important because many uses of FCoV antibody tests involve ruling out a diagnosis of FIP or FCoV infection. 72 An in-house ELISA fared best, both in terms of sensitivity/specificity and quantity of sample required (only 5 µl). The most sensitive rapid immunomigration (RIM) tests were identified. RIM tests fared best in terms of rapidity of result, which is useful when screening a healthy cat, but they may give false negative results if used to support FIP diagnosis on effusion samples, due to binding of virus to antibody, rendering the antibody unavailable for the test antigen. 73
For treatment, Polyprenyl Immunostimulant (Sass & Sass) is only for use in non-effusive FIP, having no efficacy in effusive FIP. One study of three non-effusive FIP cases reported survival of 14 months for one cat and over 2 years for two cats [EBM grade IV]. 74 However, a conference abstract report of 58 cats showed only 22% survival at 6 months, with just one cat surviving at a year [EBM grade III]. 75 A placebo-controlled study is required.
Gil et al 76 showed that in cats with FeLV or FIV infection, feline interferon omega therapy resulted in a tendency towards reduced FCoV shedding [EBM grade III].
Chloroquine inhibits FCoV replication in vitro and has anti-inflammatory effects in vivo. 77 However, reported survival times were only around 30 days at best and the drug increased alanine aminotransferase levels. Thus, the ABCD does not recommend its use until further studies have demonstrated significant benefit.
A placebo-controlled double blind trial on propentofylline showed no efficacy [EBM grade I]. 78
Detailed information on the prevention and management of feline infectious peritonitis is provided in the ABCD guidelines 79 and a previous update. 16
Influenza A virus infection in cats
Recommendations for the prevention of influenza A H5N1 and H1N1 infections in cats were published in the ABCD guidelines 80 and subsequently updated. 16
Cats were recently found to be susceptible to the H3N2 and H5N2 influenza viruses, the agents of canine influenza in Asia, leading to morbidity and mortality in cats for H3N2, but only to mild clinical signs for H5N2.81,82 Experimental infection of cats with the recent H5N8 influenza A virus was successful, but remained subclinical. 83
Feline viral papillomatosis
Papillomaviruses cause cutaneous lesions in man and several animal species, including cats. The ABCD has published guidelines on the prevention and management of feline viral papillomatosis. 84
In each host, including cats, 85 different papillomavirus (PV) types exist. To date, four feline PVs from domestic cats have been fully sequenced and classified. 85 These viruses were designated as Felis domesticus PVs (FdPVs), but recently changed to Felis catus PVs (FcaPVs). 86
A clear association between papillomavirus DNA (the Felis domesticus papillomavirus 2 – FdPV-2) and squamous cell carcinomas (SCCs) was reported; DNA was detected in all 20 Bowenoid in situ carcinomas (BISCs) examined, and in 17 of 20 cases of invasive SCC. 87 However, FdPV-2 DNA was also present in 52% of normal skin swabs. 88 Although FdPV-2 has been detected most frequently in BISCs and SCCs, other PV types have also been identified. Recently, a novel PV type, designated FcaPV-3, was detected in a feline BISC. 86 In one study, 50% of the sequenced PV DNA was most closely related to human PV DNA. 89 In another study, PV DNA could not be detected in any of 30 oral SCC samples screened, 90 which is at variance with earlier observations.
Bartonella species infection in cats
The ABCD guidelines on Bartonella species infection in cats 91 list various species and subspecies of Bartonella that are confirmed or potential human pathogens: B bacilliformis, B quintana, B elizabethae, B grahamii, B henselae, B clarridgeiae, B koehlerae, B vinsonii subspecies berkhoffii, B vinsonii subspecies arupensis, B washoensis and B asiatica. Additionally B rochalimae should now be included, for which reservoir hosts may be raccoons, coyotes, red foxes and cats. The vectors are fleas, and humans may be accidental hosts.
The important role of fleas in the transmission of B henselae and B clarridgeiae among cats has been demonstrated. Using a quantitative molecular approach, B henselae DNA was detected in both fleas and their faeces for the entire life span of the arthropod (ie, 12 days) starting from 24 h after the blood meal. 92
Recently, the possible role of several bat fly species (Nycteribiidae) as Bartonella vectors has been studied. It remains a subject of debate, but a reservoir function should be considered in addition to pathogenic, parasitic or mutualistic interactions. 93
The role of Bartonella as a pathogen after natural transmission is still unclear; however, B henselae was found in association with pyogranulomatous myocarditis and diaphragmatic myositis in two cats. 94
For laboratory diagnosis, a real-time PCR and pyrosequencing-based algorithm was described that allowed rapid differentiation of at least 11 medically relevant Bartonella species within 5 h from receipt of the specimens. 95
Coxiellosis/Q fever in cats
Q fever is a zoonotic disease caused by Coxiella burnetii. ABCD guidelines on prevention and management of coxiellosis/Q fever in cats have been published. 96
Farm animals and pets are the main reservoir hosts of the bacterium, and exposure of cats is relatively common. In the UK, a seroprevalence as high as 61.5% was recently demonstrated. 97
A Q fever outbreak among veterinary hospital personnel was linked to a caesarean section on a parturient queen. The breeding queen was C burnetii seropositive, and antibodies were demonstrated in 26% of the cats living in the same cattery. 98
Francisella tularensis infection in cats
Tularaemia is a potentially fatal zoonosis. Various clinical syndromes occur, but most patients either present with a localised infection of the skin and draining lymph nodes (ulceroglandular form) or with a systemic infection (typhoidal tularaemia). Oropharyngeal and pneumonic forms are rare.
The risk of acquiring the infection from cats is low, but exists for owners of cats with outdoor access, as well as for veterinarians and technicians. 99 Regular parasiticidal treatment to prevent tick infestations is recommended for outdoor cats. When handling animals with suppurative or draining skin or lymph node lesions in endemic areas, gloves and goggles should be worn. Gloves should be also be worn when examining the oral mucosa. Handling of diagnostic samples by laboratory staff requires adherence to appropriate biosafety procedures. 100
Detailed information on the prevention and management of tularaemia in cats is provided in the ABCD guidelines. 101
Mycobacterioses in cats
In recent years, awareness of the importance of mycobacterial infections in humans and animals has been increasing. ABCD guidelines on the prevention and management of mycobacteriosis in cats were published in 2013. 102
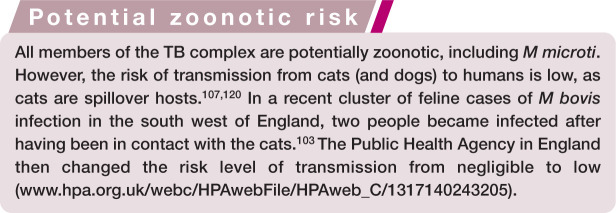
An unsual cluster of Mycobacterium bovis infection in cats was recently reported from the UK. Cat-to-cat transmission was suspected, and two humans became infected. 103 Also nosocomial infection was reported in a cluster of cases that had attended a veterinary practice in Ireland. 104
For diagnostic purposes, PCR is recommended; it should ideally be performed on fresh tissue samples, but fixed stained smears and formalin-fixed paraffin-embedded tissues can be used with good sensitivity. 105
The zoonotic risk has to be considered when planning therapeutic measures. 102 It is complicated by the fact that confirmation of the mycobacterial species takes time, and antibiotic therapy requires several months. Therefore, euthanasia rather than treatment should be considered as a sensible course of action, in view of the public health implications and the prognostic uncertainties of treatment.
For the tuberculosis complex and non-tuberculous mycobacteria (NTM) groups, double or triple therapy is currently recommended: rifampicin (10–15 mg/kg q24h), plus a quinolone (marbofloxacin [2 mg/kg q24h] or pradofloxacin [3–5 mg/kg q24h]), plus a macrolide (clarithromycin [125 mg/cat q24h or 7–15 mg/kg q24h] or azythromycin [5–15 mg/kg q24h]) for 6–9 months. Ideally, the three drugs should be administered during an initial phase of 2 months, followed by two of the drugs for 4–7 months [EBM grade III].106,107
The newer fluoroquinolones (moxifloxacin and pradofloxacin) might be more effective than the older ones.108,109 Unpublished clinical experience suggests that pradofloxacin is a good choice; in localised disease, pradofloxacin would be a good initial treatment pending species confirmation [EBM grade IV]. 110
Treatment of NTM infections is ideally based on culture and susceptibility tests for each case, as different mycobacterial species or strains may have different antibiotic sensitivity. However, this is not always possible, as specific culture systems are unavailable or results take too long.
Disseminated M avium-intracellulare complex (MAC) infections usually respond poorly to treatment, and older generation quinolones are not very effective.111 –113 The recommended first choice treatment is clarithromycin with clofazimine (4–8 mg/kg q24h) or rifampicin or doxycycline (5–10 mg/kg q12h) based on the few cases reported with good outcomes [EBM grade IV].114 –116 Limited clinical experience with pradofloxacin suggests that it is more effective than the older fluoroquinolones. 110
Most cats with feline leprosy can be cured by surgery (small lesions), and treatment with combinations of rifampicin, clofazimine, clarithromycin and pradofloxacin for several months [EBM grade IV].117,118 Spontaneous remission has been documented in one cat. 119
Keeping the cat indoors and avoiding contact with wild rodents are the only measures for preventing mycobacterial infection.
Euthanasia or treatment of cats with confirmed M bovis infection should be a consensus decision between the owner and the veterinarian, but due to the risk of cat-to- human transmission (see box above) and antimicrobial resistance, euthanasia has been suggested by some authorities and experts (www.bva.co.uk/News-campaigns-and-policy/Newsroom/News-releases/Updated-statement-on-TB-in-cats/). Similarly, euthanasia might be considered after infection with any of the other potentially zoonotic species (M tuberculosis, M microti and M avium).
Cryptococcosis in cats
Feline cryptococcosis occurs rarely or sporadically, but Cryptococcus gattii has a worldwide distribution with a high prevalence along the Pacific coast of North America. It has been reported also from Brazil, 121 and in Europe from Austria, Denmark, France, Germany, Greece, Italy, the Netherlands, Portugal, Spain, Sweden and the United Kingdom. 122 C neoformans var grubii also has a worldwide distribution and is commonly isolated from affected individuals of various animal species. C neoformans is considered a cosmopolitan opportunistic pathogen in human urban populations, whereas C gattii is a true pathogen, more prevalent in rural areas. 123
Feline cryptococcosis caused by C neoformans or C gattii is clinically indistinguishable.
This disease can manifest after a long incubation period 124 and presents in different clinical forms, including the nasal form, central nervous system (CNS) form (which can derive from the nasal form or occur independently), the cutaneous form and the systemic form. 125 CNS involvement most likely arises following local dissemination through the cribriform plate. 126 Recently, otitis interna following systemic spread of the fungus was reported. 127
Detailed information on the prevention and management of cryptococcosis in cats is provided in the ABCD guidelines. 125
Sporotrichosis in cats
Sporotrichosis is a deep cutaneous mycosis caused by the dimorphic saprophytic fungus Sporothrix schenckii. S schenckii is not a unique species but a complex containing at least four distinct species. Most feline cases reported from Brazil are caused by S brasiliensis. 128
The prevalence of the disease varies markedly between regions. In Central and South America, it represents the most common deep mycosis. In Brazil it is endemic, and an important epidemic affecting humans, cats and dogs was reported in Rio de Janeiro.129 –131 More than 2000 feline cases over 7 years have been seen by just one institution, showing the magnitude of the epidemics and the challenges of disease control. 132
Using histopathology and staining procedures, the organisms are readily visualised. Cats with few and well organised granulomas tend to have low numbers of fungal organisms in the lesions. Cats in poor general condition and with large numbers of granulomas have the greatest numbers of fungal organisms. 133
Detailed information on the prevention and management of sporotrichosis in cats is provided in the ABCD guidelines. 134
Toxoplasma gondii infection in cats
Several antibody tests have been used to detect infection with Toxoplasma gondii and to diagnose toxoplasmosis in cats. The indirect immunofluorescence assay can be adapted to detect immunoglobulin M (IgM), IgG and IgA antibodies.
Antibody test results from healthy cats are useful to assess the health risk for humans. An antibody-negative cat could be shedding oocysts (early after infection, before antibodies have developed) or will shed oocysts if exposed; this cat poses the greatest public health risk.
An antibody-positive cat is unlikely to shed oocysts, because antibodies need 2–3 weeks to develop, by which time the infection has been controlled; also, shedding usually occurs only once in the cat’s lifetime. Furthermore, a cat with antibodies is unlikely to shed oocysts if re-exposed or immunosuppressed. 135 In one study, cats inoculated with T gondii tissue cysts were orally re-challenged several years later, and a few of them did shed oocysts after this second challenge (although only low amounts and over a short time). 136 This, however, has never been shown to occur in naturally infected cats. Thus, the risk of shedding by an antibody-positive cat is very low.
Antibodies are common in both healthy and diseased cats and, therefore, do not prove clinical toxoplasmosis. Not only IgG antibodies, but also antibodies of the IgM class are commonly detected in healthy cats and stay high over long periods; thus their detection is also of no use for diagnosing toxoplasmosis. T gondii-specific IgM is detected in the serum of cats with latent or reactivated infection and titres, therefore, do not indicate recent exposure. If increasing IgM titres are detected, however, this can raise the suspicion of clinical toxoplasmosis.
Clinical toxoplasmosis is ideally diagnosed by detection of the organism in muscle biopsies or bronchoalveolar lavage fluid, or by PCR performed on cerebrospinal fluid (CSF) or aqueous humour. During acute illness, tachyzoites can be detected in tissues and body fluids by cytology. They are rarely found in blood, but occasionally in CSF, fine-needle aspirates of organs (eg, lymph nodes), and transtracheal or bronchoalveolar washings, and are common in the peritoneal and thoracic fluid of animals developing thoracic effusions or ascites. Detection of tachyzoites confirms the diagnosis.
A tentative diagnosis can be based on increasing IgM titres, exclusion of other causes of the clinical signs, and a positive clinical response to an anti-Toxoplasma drug.135,137
Detailed information on the prevention and management of T gondii infection in cats is provided in the ABCD guidelines. 138
Leishmaniosis in cats
Leishmania infection is less well known in cats than in dogs, but it may be underestimated in endemic areas and is of zoonotic concern. Detailed information on the prevention and management of leishmaniosis in cats was published in the ABCD guidelines. 139
The information available for treatment is based only on case reports. Despite clinical improvements following long term oral administration of allopurinol (10–20 mg/kg q12h or q24h), the infection is not cleared, and recurrence of clinical signs may occur after cessation of therapy, as in dogs [EBM grade IV].140,141 Meglumine antimoniate (5–50 mg/kg or 375 mg/cat q24h SC/IM under different protocols) was used for therapy in four cases and led to good clinical responses, but long term follow-up is lacking [EBM grade IV]. 140
Giardiasis in cats
Giardia is a protozoan parasite of the small intestine. Seven genotypes have been identified and designated A to G. Types F and G are the subgroups commonly seen in cats, whereas A and B occur mainly in man and are considered as potentially zoonotic. 142 Giardiasis in cats is not considered a zoonotic risk.143,144 However, recent European studies demonstrated the presence of subgroup A in cats,145 –147 either alone or as a dual infection (A and F). 146 Genotype B has also been identified in cats, but A is most prevalent, according to a Canadian study. 148
A correlation between body condition score, presence of diarrhoea and infection with G intestinalis has been observed; 149 but, in other studies, agent presence has not been notably different in cats with diarrhoea as compared with healthy cats. Co-infections with other enteropathogens have been demonstrated to be frequent in the UK. 150
Detailed information on the prevention and management of giardiasis in cats is provided in the ABCD guidelines. 151
Footnotes
Funding: The authors received no specific grant from any funding agency in the public, commercial or not-for-profit sectors for the preparation of this article. The ABCD is supported by Merial, but is a scientifically independent body and its members receive no stipends from Merial.
The authors do not have any potential conflicts of interest to declare.
References
Feline panleukopenia
- 1. Carmichael LE. An annotated historical account of canine parvovirus. J Vet Med B Infect Dis Vet Public Health 2005; 52: 303–311. [DOI] [PubMed] [Google Scholar]
- 2. Truyen U. Emergence and recent evolution of canine parvovirus. Vet Microbiol 1999; 69: 47–50. [DOI] [PubMed] [Google Scholar]
- 3. Hueffer K, Parrish CR. Parvovirus host range, cell tropism and evolution. Curr Opin Microbiol 2003; 6: 392–398. [DOI] [PubMed] [Google Scholar]
- 4. Allison AB, Harbison CE, Pagan I, et al. Role of multiple hosts in the cross-species transmission and emergence of a pandemic parvovirus. J Virol 2012; 86: 865–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Truyen U, Gruenberg A, Chang SF, et al. Evolution of the feline subgroup parvoviruses and the control of canine host range. J Virol 1995; 69: 4702–4710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Truyen U, Evermann JF, Vieler E, et al. Evolution of canine parvovirus involved loss and gain of the feline host range. Virology 1996; 215: 186–189. [DOI] [PubMed] [Google Scholar]
- 7. Mochizuki M, Horiuchi M, Hiragi H, et al. Isolation of canine parvovirus from a cat manifesting clinical signs of feline panleukopenia. J Clin Microbiol 1996; 34: 2101–2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ikeda Y, Mochizuki M, Naito R, et al. Predominance of canine parvovirus (CPV) in unvaccinated cat populations and emergence of new antigenic types of CPVs in cats. Virology 2000; 278: 13–19. [DOI] [PubMed] [Google Scholar]
- 9. Miranda C, Parrish CR, Thompson G. Canine parvovirus 2c infection in a cat with severe clinical disease. J Vet Diagn Invest 2014; 26: 462–464. [DOI] [PubMed] [Google Scholar]
- 10. Truyen U, Parrish CR. Feline panleukopenia virus: its interesting evolution and current problems in immunoprophylaxis against a serious pathogen. Vet Microbiol 2013; 165: 29–32. [DOI] [PubMed] [Google Scholar]
- 11. Jakel V, Cussler K, Hanschmann K-M, et al. Vaccination against feline panleukopenia: implications from a field study in kittens. BMC Vet Res 2012; 8: 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Clegg SR, Coyne KP, Dawson S, et al. Canine parvovirus in asymptomatic feline carriers. Vet Microbiol 2012; 157: 78–85. [DOI] [PubMed] [Google Scholar]
- 13. Allison AB, Kohler DJ, Fox KA, et al. Frequent cross-species transmission of parvoviruses among diverse carnivore hosts. J Virol 2013; 87: 2342–2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Csiza CK, De Lahunta A, Scott FW, et al. Pathogenesis of feline panleukopenia virus in susceptible newborn kittens II. Pathology and immunofluorescence. Infect Immun 1971; 3: 838–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Truyen U, Addie D, Bélak S, et al. Feline panleukopenia. ABCD guidelines on prevention and management. J Feline Med Surg 2009; 11: 538–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Horzinek MC, Addie D, Bélak S, et al. ABCD: update of the 2009 guidelines on prevention and management of feline infectious diseases. J Feline Med Surg 2013; 15: 530–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
Feline herpesvirus infection
- 17. Thiry E, Addie D, Bélak S, et al. Feline herpesvirus infection. ABCD guidelines on prevention and management. J Feline Med Surg 2009; 11: 547–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Maggs DJ. Update on the diagnosis and management of feline herpesvirus-1 infection. In: August JR. (ed). Consultations in feline internal medicine. Volume 4, Philadelphia: WB Saunders, 2001, pp 51–61. [Google Scholar]
- 19. Maggs DJ, Nasisse MP, Kass PH. Efficacy of oral supplementation with L-lysine in cats latently infected with feline herpesvirus. Am J Vet Res 2003; 64: 37–42. [DOI] [PubMed] [Google Scholar]
- 20. Maggs DJ, Sykes JE, Clarke HE, et al. Effects of dietary lysine supplementation in cats with enzootic upper respiratory disease. J Feline Med Surg 2007; 9: 97–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Stiles J, Townsend WM, Rogers QR, et al. Effect of oral administration of L-lysine on conjunctivitis caused by feline herpesvirus in cats. Am J Vet Res 2002; 63: 99–103. [DOI] [PubMed] [Google Scholar]
- 22. Rees TM, Lubinski JL. Oral supplementation with L-lysine did not prevent upper respiratory infection in a shelter population of cats. J Feline Med Surg 2008; 10: 510–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Drazenovich TL, Fascetti AJ, Westermeyer HD, et al. Effects of dietary lysine supplementation on upper respiratory and ocular disease and detection of infectious organisms in cats within an animal shelter. Am J Vet Res 2009; 70: 1391–1400. [DOI] [PubMed] [Google Scholar]
- 24. Maggs DJ. Antiviral therapy for feline herpesvirus infections. Vet Clin North Am Small Anim Pract 2010; 40: 1055–1062. [DOI] [PubMed] [Google Scholar]
- 25. Gould D. Feline herpesvirus-1. Ocular manifestations, diagnosis and treatment options. J Feline Med Surg 2011; 13: 333–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cave NJ, Dennis K, Gopakumar G, et al. Effects of physiologic concentrations of l-lysine on in vitro replication of feline herpesvirus 1. Am J Vet Res 2014; 75: 572–580. [DOI] [PubMed] [Google Scholar]
Feline leukaemia virus infection
- 27. Leutenegger CM, Hofmann-Lehmann R, Riols C, et al. Viral infections in free-living populations of the European wildcat. J Wildl Dis 1999; 35: 678–686. [DOI] [PubMed] [Google Scholar]
- 28. Cunningham MW, Brown MA, Shindle DB, et al. Epizootiology and management of feline leukemia virus in the Florida puma. J Wildl Dis 2008; 44: 537–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Meli ML, Cattori V, Martinez F, et al. Feline leukemia virus and other pathogens as important threats to the survival of the critically endangered Iberian lynx (Lynx pardinus). PLoS One 2009; 4: e4744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mora M, Napolitano C, Ortega R, et al. Feline immunodeficiency virus and feline leukemia virus infection in free-ranging guignas (Leopardus guigna) and sympatric domestic cats in human perturbed landscapes on Chiloe Island, Chile. J Wildl Dis 2015; 51: 199–208. [DOI] [PubMed] [Google Scholar]
- 31. Hosie MJ, Robertson C, Jarrett O. Prevalence of feline leukaemia virus and antibodies to feline immunodeficiency virus in cats in the United Kingdom. Vet Rec 1989; 125: 293. [DOI] [PubMed] [Google Scholar]
- 32. Lutz H, Lehmann R, Winkler G, et al. Feline immunodeficiency virus in Switzerland: clinical aspects and epidemiology in comparison with feline leukemia virus and coronaviruses. Schweiz Arch Tierheilkd 1990; 132: 217–225. [PubMed] [Google Scholar]
- 33. Levy JK, Scott HM, Lachtara JL, et al. Seroprevalence of feline leukemia virus and feline immunodeficiency virus infection among cats in North America and risk factors for seropositivity. J Am Vet Med Assoc 2006; 228: 371–376. [DOI] [PubMed] [Google Scholar]
- 34. Little S. A review of feline leukemia virus and feline immunodeficiency virus seroprevalence in cats in Canada. Vet Immunol Immunopathol 2011; 143: 243–245. [DOI] [PubMed] [Google Scholar]
- 35. Englert T, Lutz H, Sauter-Louis C, et al. Survey of the feline leukemia virus infection status of cats in Southern Germany. J Feline Med Surg 2012; 14: 392–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Cattori V, Pepin AC, Tandon R, et al. Real-time PCR investigation of feline leukemia virus proviral and viral RNA loads in leukocyte subsets. Vet Immunol Immunopathol 2008; 123: 124–128. [DOI] [PubMed] [Google Scholar]
- 37. Lutz H, Pedersen N, Higgins J, et al. Humoral immune reactivity to feline leukemia virus and associated antigens in cats naturally infected with feline leukemia virus. Cancer Res 1980; 40: 3642–3651. [PubMed] [Google Scholar]
- 38. Hoover EA, Schaller JP, Mathes LE, et al. Passive immunity to feline leukemia: evaluation of immunity from dams naturally infected and experimentally vaccinated. Infect Immun 1977; 16: 54–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lutz H, Pedersen NC, Theilen GH. Course of feline leukemia virus infection and its detection by enzyme-linked immunosorbent assay and monoclonal antibodies. Am J Vet Res 1983; 44: 2054–2059. [PubMed] [Google Scholar]
- 40. Hofmann-Lehmann R, Huder JB, Gruber S, et al. Feline leukaemia provirus load during the course of experimental infection and in naturally infected cats. J Gen Virol 2001; 82: 1589–1596. [DOI] [PubMed] [Google Scholar]
- 41. Boretti FS, Ossent P, Bauer-Pham K, et al. Recurrence of feline leukemia virus (FeLV) and development of fatal lymphoma concurrent with feline immunodeficiency virus (FIV) induced immune suppression. Presented at the 7th International Feline Retrovirus Research Symposium, Pisa, Italy, 2004. [Google Scholar]
- 42. Weijer K, UytdeHaag FG, Jarrett O, et al. Post-exposure treatment with monoclonal antibodies in a retrovirus system: failure to protect cats against feline leukemia virus infection with virus neutralizing monoclonal antibodies. Int J Cancer 1986; 38: 81–87. [DOI] [PubMed] [Google Scholar]
- 43. Major A, Cattori V, Boenzli E, et al. Exposure of cats to low doses of FeLV: seroconversion as the sole parameter of infection. Vet Res 2010; 41: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Gomes-Keller MA, Tandon R, Gonczi E, et al. Shedding of feline leukemia virus RNA in saliva is a consistent feature in viraemic cats. Vet Microbiol 2006; 112: 11–21. [DOI] [PubMed] [Google Scholar]
- 45. Cattori V, Tandon R, Riond B, et al. The kinetics of feline leukaemia virus shedding in experimentally infected cats are associated with infection outcome. Vet Microbiol 2009; 133: 292–296. [DOI] [PubMed] [Google Scholar]
- 46. Fontenot JD, Hoover EA, Elder JH, et al. Evaluation of feline immunodeficiency virus and feline leukemia virus transmembrane peptides for serological diagnosis. J Clin Microbiol 1992; 30: 1885–1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Boenzli E, Hadorn M, Hartnack S, et al. Detection of antibodies to the feline leukemia Virus (FeLV) transmembrane protein p15E: an alternative approach for serological FeLV detection based on antibodies to p15E. J Clin Microbiol 2014; 52: 2046–2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Cattori V, Weibel B, Lutz H. Inhibition of Feline leukemia virus replication by the integrase inhibitor Raltegravir. Vet Microbiol 2011; 152: 165–168. [DOI] [PubMed] [Google Scholar]
- 49. Boesch A, Cattori V, Riond B, et al. Evaluation of the effect of short-term treatment with the integrase inhibitor raltegravir (Isentress) on the course of progressive feline leukemia virus infection. Vet Microbiol 2015; 175: 167–178. [DOI] [PubMed] [Google Scholar]
- 50. Hofmann-Lehmann R, Cattoi V, Tandon R, et al. Vaccination against the feline leukaemia virus: outcome and response categories and long-term follow-up. Vaccine 2007; 25: 5531–5539. [DOI] [PubMed] [Google Scholar]
- 51. Torres AN, O’Halloran KP, Larson LJ, et al. Feline leukemia virus immunity induced by whole inactivated virus vaccination. Vet Immunol Immunopathol 2010; 134: 122–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Jirjis F, Davis T, Lane J, et al. Protection against feline leukemia virus challenge for at least 2 years after vaccination with an inactivated feline leukemia virus vaccine. Vet Ther 2010; 11: E1–6. [PubMed] [Google Scholar]
- 53. Möstl K, Egberink H, Addie D, et al. Prevention of infectious diseases in cat shelters. ABCD guidelines. J Feline Med Surg 2013; 15: 546–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lutz H, Addie D, Bélak S, et al. Feline leukaemia. ABCD guidelines on prevention and management. J Feline Med Surg 2009; 11: 565–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
Feline immunodeficiency virus infection
- 55. Barrs VR, Martin P, Nicoll RG, et al. Pulmonary cryptococcosis and Capillaria aerophila infection in an FIV-positive cat. Aust Vet J 2000; 78: 154–158. [DOI] [PubMed] [Google Scholar]
- 56. Addie DD, Dennis JM, Toth S, et al. Long-term impact on a closed household of pet cats of natural infection with feline coronavirus, feline leukaemia virus and feline immunodeficiency virus. Vet Rec 2000; 146: 419–424. [DOI] [PubMed] [Google Scholar]
- 57. Ravi M, Wobeser GA, Taylor SM, et al. Naturally acquired feline immunodeficiency virus (FIV) infection in cats from western Canada: prevalence, disease associations, and survival analysis. Can Vet J 2010; 51: 271–276. [PMC free article] [PubMed] [Google Scholar]
- 58. Liem BP, Dhand NK, Pepper AE, et al. Clinical findings and survival in cats naturally infected with feline immunodeficiency virus. J Vet Intern Med 2013; 27: 798–805. [DOI] [PubMed] [Google Scholar]
- 59. Bęczkowski PM, Techakriengkrai N, Logan N, et al. Emergence of CD134 cysteine-rich domain 2 (CRD2)-independent strains of feline immunodeficiency virus (FIV) is associated with disease progression in naturally infected cats. Retrovirology 2014; 11: 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Polak KC, Levy JC, Crawford PC, et al. Infectious diseases in large-scale cat hoarding investigations. Vet J 2014; 201: 189–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Goldkamp CE, Levy JK, Edinboro CH, et al. Seroprevalences of feline leukemia virus and feline immunodeficiency virus in cats with abscesses or bite wounds and rate of veterinarian compliance with current guidelines for retrovirus testing. J Am Vet Med Assoc 2008; 232: 1152–1158. [DOI] [PubMed] [Google Scholar]
- 62. Chang-Fung-Martel J, Gummow B, Burgess G, et al. A door-to-door prevalence study of feline immunodeficiency virus in an Australian suburb. J Feline Med Surg 2013; 15: 1070–1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Litster AL. Transmission of feline immunodeficiency virus (FIV) among cohabiting cats in two cat rescue shelters. Vet J 2014; 201: 184–188. [DOI] [PubMed] [Google Scholar]
- 64. Levy JK, Scott HM, Lachtara JL, et al. Seroprevalence of feline leukemia virus and feline immunodeficiency virus infection among cats in North America and risk factors for seropositivity. J Am Vet Med Assoc 2006; 228: 371–376. [DOI] [PubMed] [Google Scholar]
- 65. Hosie MJ, Addie D, Bélak S, et al. Feline immunodeficiency. ABCD guidelines on prevention and management. J Feline Med Surg 2009; 11: 575–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rabies
- 66. BBC. Dog smuggling into UK on increase. http://www.bbc.com/news/uk-25957668.2014.
- 67. Anon. Rabies confirmed in an imported kitten in France. Vet Rec 2013; 173: 435. [DOI] [PubMed] [Google Scholar]
- 68. Gerhold RW, Jessup DA. Zoonotic diseases associated with free-roaming cats. Zoonoses Public Health 2013; 60: 189–195. [DOI] [PubMed] [Google Scholar]
- 69. Campagnolo ER, Lind LR, Long JM, et al. Human exposure to rabid free-ranging cats: a continuing public health concern in Pennsylvania. Zoonoses Public Health 2014; 61: 346–355. [DOI] [PubMed] [Google Scholar]
- 70. Frymus T, Addie D, Bélak S, et al. Feline rabies. ABCD guidelines on prevention and management. J Feline Med Surg 2009; 11: 585–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
Feline infectious peritonitis
- 71. Porter E, Tasker S, Day MJ, et al. Amino acid changes in the spike protein of feline coronavirus correlate with systemic spread of virus from the intestine and not with feline infectious peritonitis. Vet Res 2014; 45: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Addie DD, le Poder S, Burr P, et al. Utility of feline coronavirus antibody tests. J Feline Med Surg 2015; 17: 152–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Meli ML, Burr P, Decaro N, et al. Samples with high virus load cause a trend toward lower signal in feline coronavirus antibody tests. J Feline Med Surg 2013; 15: 295–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Legendre AM, Bartges JW. Effect of Polyprenyl Immunostimulant on the survival times of three cats with the dry form of feline infectious peritonitis. J Feline Med Surg 2009; 11: 624–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Legendre AM. FIP treatments: what might work, what doesn’t work. Presentation at the American Animal Hospital Association meeting; 2013 March 14–17; Phoenix, AZ, USA. [Google Scholar]
- 76. Gil S, Leal RO, Duarte A, et al. Relevance of feline interferon omega for clinical improvement and reduction of concurrent viral excretion in retrovirus infected cats from a rescue shelter. Res Vet Sci 2013; 94: 753–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Takano T, Katoh Y, Doki T, et al. Effect of chloroquine on feline infectious peritonitis virus infection in vitro and in vivo. Antiviral Res 2013; 99: 100–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Fischer Y, Ritz S, Weber K, et al. Randomized, placebo controlled study of the effect of propentofylline on survival time and quality of life of cats with feline infectious peritonitis. J Vet Intern Med 2011; 25: 1270–1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Addie D, Bélak S, Boucraut-Baralon C, et al. Feline infectious peritonitis. ABCD guidelines on prevention and management. J Feline Med Surg 2009; 11: 594–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
Infuenza A virus infection in cats
- 80. Thiry E, Addie D, Bélak S, et al. H5N1 avian influenza in cats. ABCD guidelines on prevention and management. J Feline Med Surg 2009; 11: 615–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Hai-xia F, Yuan-yuan L, Qian-qian S, et al. Interspecies transmission of canine influenza virus H5N2 to cats and chickens by close contact with experimentally infected dogs. Vet Microbiol 2014; 170: 414–417. [DOI] [PubMed] [Google Scholar]
- 82. Lei N, Yuan ZG, Huang SF, et al. Transmission of avian-origin canine influenza viruses A (H3N2) in cats. Vet Microbiol 2012; 160: 481–483. [DOI] [PubMed] [Google Scholar]
- 83. Kim Y-I, Pascua PNQ, Kwon H-I, et al. Pathobiological features of a novel, highly pathogenic avian influenza A (H5N8) virus. Emerg Microbes Inf 2014; 3: e75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Feline viral papillomatosis
- 84. Egberink H, Thiry E, Möstl K, et al. Feline viral papillomatosis. ABCD guidelines on prevention and management. J Feline Med Surg 2013; 15: 560–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Munday JS. Papillomaviruses in felids. Vet J 2014; 199: 340–347. [DOI] [PubMed] [Google Scholar]
- 86. Munday JS, Dunowska M, Hills SF, et al. Genomic characterization of Felis catus papillomavirus-3: a novel papillomavirus detected in a feline Bowenoid in situ carcinoma. Vet Microbiol 2013; 165: 319–325. [DOI] [PubMed] [Google Scholar]
- 87. Munday JS, French AF, Peters-Kennedy J, et al. Amplification of papillomaviral DNA sequences from a high proportion of feline cutaneous in situ and invase squamous cell carcinomas using a nested polymerase chain reaction. Vet Dermatol 2008; 19: 259–263. [DOI] [PubMed] [Google Scholar]
- 88. Munday JS, Witham AI. Frequent detection of papillomavirus DNA in clinically normal skin of cats infected and noninfected with feline immunodeficiency virus. Vet Dermatol 2010; 21: 307–310. [DOI] [PubMed] [Google Scholar]
- 89. O’Neill SH, Newkirk KM, Anis EA, et al. Detection of human papillomavirus DNA in feline premalignant and invasive squamous cell carcinoma. Vet Dermatol 2011; 22: 68–74. [DOI] [PubMed] [Google Scholar]
- 90. Munday JS, Knight CG, French AF. Evaluation of feline oral squamous cell carcinomas for p16CDKN2A protein immunoreactivity and the presence of papillomaviral DNA. Res Vet Sci 2011; 90: 280–283. [DOI] [PubMed] [Google Scholar]
Bartonella species infection in cats
- 91. Pennisi MG, Marsilio F, Hartmann K, et al. Bartonella species infection in cats. ABCD guidelines on prevention and management. J Feline Med Surg 2013; 15: 563–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Bouhsira E, Ferrandez Y, Liu M, et al. Ctenocephalides felis an in vitro potential vector for five Bartonella species. Comp Immunol Microbiol Inf Dis 2013; 36: 105–111. [DOI] [PubMed] [Google Scholar]
- 93. Morse SF, Olival KJ, Kosoy M, et al. Global distribution and genetic diversity of Bartonella in bat flies (Hippoboscoidea, Strebilidae, Nycteribiidae). Infect Genet Evol 2012; 12: 1717–1723. [DOI] [PubMed] [Google Scholar]
- 94. Varanat M, Broadhurst J, Linder KE, et al. Identification of Bartonella henselae in 2 cats with pyogranulomatous myocarditis and diaphragmatic myositis. Vet Pathol 2012; 49: 608–611. [DOI] [PubMed] [Google Scholar]
- 95. Buss SN, Gebhardt LL, Musser KA. Real-time PCR and pyrosequencing for diffentiation of medically relevant Bartonella species. J Microbiol Meth 2012; 91: 252–256. [DOI] [PubMed] [Google Scholar]
Coxiellosis/Q fever in cats
- 96. Egberink H, Addie D, Bélak S, et al. Coxiellosis/Q fever in cats. ABCD guidelines on prevention and management. J Feline Med Surg 2013; 15: 573–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Meredith AL, Cleaveland SC, Denwood MJ, et al. Coxiella burnetii (Q-fever) seroprevalence in prey and predators in the United Kingdom: evaluation of infection in wild rodents, foxes and domestic cats using a modified ELISA. Transbound Emerg Dis 2014; DOI: 10.1111/tbed.12211. [DOI] [PubMed] [Google Scholar]
- 98. Kopecny L, Bosward KL, Shapiro A, et al. Investigating Coxiella burnetii infection in a breeding cattery at the centre of a Q fever outbreak. J Feline Med Surg 2013; 15: 1037–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
Francisella tularensis infection in cats
- 99. Liles WC, Burger RJ. Tularaemia from domestic cats. West J Medicine 1993; 158: 619–622. [PMC free article] [PubMed] [Google Scholar]
- 100. Greene CE. Francisella and Coxiella infections. In: Greene CE. (ed). Infectious diseases of the dog and cat. 4th ed. St Louis, MO: Elsevier, 2012, pp 476–482. [Google Scholar]
- 101. Pennisi MG, Egberink H, Hartmann K, et al. Francisella tularensis infection in cats. ABCD guidelines on prevention and management. J Feline Med Surg 2013; 15: 585–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mycobacterioses in cats
- 102. Lloret A, Hartmann K, Pennisi MG, et al. Mycobacteriosis in cats. ABCD guidelines on prevention and management. J Feline Med Surg 2013; 15: 591–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Roberts T, O’Connor C, Nuñez-Garcia J, et al. Unusual cluster of Mycobacterium bovis infection in cats. Vet Rec 2014; 174: 326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Murray A, Dineen A, Kelly P, et al. Nosocomial spread of Mycobacterium bovis in domestic cats. J Feline Med Surg 2014; 17: 173–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Reppas G, Fyfe J, Foster S, et al. Detection and identification of mycobacteria in fixed stained smears and formalin-fixed paraffin-embedded tissues using PCR. J Small Anim Pract 2013; 54: 638–646. [DOI] [PubMed] [Google Scholar]
- 106. Gunn-Moore DA, Jenkins PA, Lucke VM. Feline tuberculosis: a literature review and discussion of 19 cases caused by an unusual mycobacterial variant. Vet Rec 1996; 138: 53–58. [DOI] [PubMed] [Google Scholar]
- 107. Gunn-Moore DA. Mycobacterial infections in cats and dogs. In: Ettinger S, Feldman E. (eds). Textbook of veterinary internal medicine. 7th ed. Philadelphia: WB Saunders, 2010, pp 875–881. [Google Scholar]
- 108. Govendir M, Hansen T, Kimble B, et al. Susceptibility of rapidly growing mycobacteria isolated from cats and dogs, to ciprofloxacin, enrofloxacin and moxifloxacin. Vet Microbiol 2011; 147: 113–118. [DOI] [PubMed] [Google Scholar]
- 109. Govendir M, Norris JM, Hansen T, et al. Susceptibility of rapidly growing mycobacteria and Nocardia isolates from cats and dogs to pradofloxacin. Vet Microbiol 2011; 153: 240–245. [DOI] [PubMed] [Google Scholar]
- 110. Gunn-Moore DA. Feline mycobacterial infections. Vet J 2014; 201: 230–238. [DOI] [PubMed] [Google Scholar]
- 111. Rivière D, Pringet JL, Etievant M, et al. Disseminated Mycobacterium avium subspecies infection in a cat. J Feline Med Surg 2011; 13: 125–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Barry M, Taylor J, Woods JP. Disseminated Mycobacterium avium in a cat. Can Vet J 2002; 43: 369–371. [PMC free article] [PubMed] [Google Scholar]
- 113. de Groot PH, van Ingen J, de Zwaan R, et al. Disseminated Mycobacterium avium subsp. avium infection in a cat, the Netherlands. Vet Microbiol 2010; 144: 527–529. [DOI] [PubMed] [Google Scholar]
- 114. Malik R, Hughes MS, James G, et al. Feline leprosy: two different syndromes. J Feline Med Surg 2002; 4: 43–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Kaufman AC, Greene CE, Rakich PM, et al. Treatment of localized Mycobacterium avium complex infection with clofazimine and doxycycline in a cat. J Am Vet Med Assoc 1995; 207: 457–459. [PubMed] [Google Scholar]
- 116. Sieber-Ruckstuhl NS, Sessions JK, Sanchez S, et al. Long-term cure of disseminated Mycobacterium avium infection in a cat. Vet Rec 2007; 160: 131–132. [DOI] [PubMed] [Google Scholar]
- 117. Greene CE, Gunn-Moore DA. Mycobacterial infections. In: Greene CE. (ed). Infectious diseases of the dog and cat. 3rd ed. St Louis, MO: Saunders Elsevier, 2006, pp 462–488. [Google Scholar]
- 118. Horne KS, Kunkle GA. Clinical outcome of cutaneous rapidly growing mycobacterial infections in cats in the south-eastern United States: a review of 10 cases (1996–2006). J Feline Med Surg 2009; 11: 627–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Roccabianca P, Caniatti M, Scanziani E, et al. Feline leprosy: spontaneous remission in a cat. J Am Anim Hosp Assoc 1996; 32: 189–193. [DOI] [PubMed] [Google Scholar]
- 120. Xavier Emmanuel F, Seagar AL, Doig C, et al. Human and animal infections with Mycobacterium microti, Scotland. Emerg Infect Dis 2007; 13: 1924–1927. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cryptococcosis in cats
- 121. Cardoso PH, Baroni FdeA, Silva EG, et al. Feline nasal granuloma due to Cryptococcus gattii type VGII. Mycopathologia 2013; 176: 303–307. [DOI] [PubMed] [Google Scholar]
- 122. Lester SJ, Malik R, Bartlett KH, et al. Cryptococcosis: update and emergence of Cryptococcus gattii. Vet Clin Pathol 2011; 40: 4–17. [DOI] [PubMed] [Google Scholar]
- 123. Sykes JE, Malik R. Cryptococcosis. In: Greene CE. (ed). Infectious diseases of the dog and cat. 4th ed. St Louis, MO: Saunders Elsevier, 2012, pp 621–634. [Google Scholar]
- 124. Castrodale LJ, Gerlach RF, Preziosi DE, et al. Prolonged incubation period for Cyptococcus gattii infection in cat, Alaska, USA. Emerg Infect Dis 2014; 19: 1034–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Pennisi MG, Hartmann K, Lloret A, et al. Cryptococcosis in cats. ABCD guidelines on prevention and management. J Feline Med Surg 2013; 15: 611–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Espino L, Barreiro JD, Gonzalez A, et al. Intracranial epidural empyema due to Cryptococcus neoformans in a 5-year-old neutered male European short hair cat. Vet Q 2014; 28: 1–16. [DOI] [PubMed] [Google Scholar]
- 127. Paulin J, Morshed M, Armién AG. Otitis interna induced by Cryptococcus neoformans var. grubii in a cat. Vet Pathol 2013; 50: 260–263. [DOI] [PubMed] [Google Scholar]
Sporotrichosis in cats
- 128. Rodrigues AM, de Melo Teixeira M, de Hoog GS, et al. Phylogenetic analysis reveals a high prevalence of Sporothrix brasiliensis in feline sporotrichosis outbreaks. PloS Negl Trop Dis 2013; 7: e2281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Galhardo MC, de Oliveira RM, Valle AC, et al. Molecular epidemiology and antifungal susceptibility pattern of Sporothrix schenckii isolates from a cat-transmitted epidemic of sporotrichosis in Rio de Janeiro, Brazil. Med Mycol 2008; 46: 141–151. [DOI] [PubMed] [Google Scholar]
- 130. Schubach TM, Schubach AO, dos-Reis RS, et al. Sporothrix schenkii isolated from domestic cats with and without sporotrichosis in Rio de Janeiro, Brazil. Mycopathologia 2002; 153: 83–86. [DOI] [PubMed] [Google Scholar]
- 131. Schubach A, Barros MB, Wanke B. Epidemic sporotrichosis. Curr Opin Infect Dis 2008; 21: 129–133. [DOI] [PubMed] [Google Scholar]
- 132. Pereira SA, Gremiao ID, Kitada AA. The epidemiological scenario of feline sporotrichosis in Rio de Janeiro, State of Rio de Janeiro, Brazil. Rev Soc Bras Med Trop 2014; 47: 392–393. [DOI] [PubMed] [Google Scholar]
- 133. Miranda LH, Conceiçao-Silva F, Quintella LP, et al. Feline sporotrichosis: histopathological profile of cutaneous lesions and their correlation with clinical presentation. Comp Immunol Microbiol Infect Dis 2013; 36: 425–432. [DOI] [PubMed] [Google Scholar]
- 134. Lloret A, Hartmann K, Pennisi MG, et al. Sporotrichosis in cats. ABCD guidelines on prevention and management. J Feline Med Surg 2013; 15: 619–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
Toxoplasma gondii infection in cats
- 135. Dubey JP. Toxoplasma update. WSAVA Proceedings. Available at http://www.vin.com/proceedings/Proceedings.plx?CID=WSAVA2005&PID=10951&O=Generic. 2005.
- 136. Dubey JP. Duration of immunity to shedding of Toxoplasma gondii oocysts by cats. J Parasitol 1995; 81: 410–415. [PubMed] [Google Scholar]
- 137. Dubey JP, Lappin MR. Toxoplasmosis and neosporosis. In: Greene CE. (ed). Infectious diseases of the dog and cat. 3rd ed. St Louis, MO: Elsevier, 2006, pp 754–775. [Google Scholar]
- 138. Hartmann K, Addie D, Bélak S, et al. Toxoplasma gondii infection in cats. ABCD guidelines on prevention and management. J Feline Med Surg 2013; 15: 631–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
Leishmaniosis in cats
- 139. Pennisi MG, Hartmann K, Lloret A, et al. Leishmaniosis in cats. ABCD guidelines on prevention and management. J Feline Med Surg 2013; 15: 638–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Pennisi MG. La leishmaniosi felina dalla A alla Z. In: Leishmaniosi canina: recenti acquisizioni su epidemiologia, implicazioni cliniche, diagnosi, terapia e prevenzione. Cremona: Edizioni Veterinarie, 2010, pp 59–64. [Google Scholar]
- 141. Sobrinho LS, Rossi CN, Vides JP, et al. Coinfection of Leishmania chagasi with Toxoplasma gondii, feline immunodeficiency virus (FIV) and feline leukemia virus (FeLV) in cats from an endemic area of zoonotic visceral leishmaniasis. Vet Parasitol 2012; 187: 302–306. [DOI] [PubMed] [Google Scholar]
Giardiasis in cats
- 142. Lebbad M, Mattson JG, Christensson B, et al. From mouse to moose: multilocus genotyping of Giardia isolates from various animal species. Vet Parasitol 2010; 168: 231–239. [DOI] [PubMed] [Google Scholar]
- 143. Xiao L, Fayer R. Molecular characterisation of species and genotypes of Cryptosporidium and Giardia and assessment of zoonotic transmission. Int J Parasitol 2008; 38: 1239–1255. [DOI] [PubMed] [Google Scholar]
- 144. Ballweber LR, Xiao L, Bowman DD, et al. Giardiasis in dogs and cats: update on epidemiology and public health significance. Trends Parasitol 2010; 26: 180–189. [DOI] [PubMed] [Google Scholar]
- 145. Paoletti B, Otranto D, Weigl S, et al. Prevalence and genetic characterization of Giardia and Cryptosporidium in cats from Italy. Res Vet Sci 2010; 91: 397–399. [DOI] [PubMed] [Google Scholar]
- 146. Dado D, Montoya A, Blanco MA, et al. Prevalence and genotypes of Giardia duodenalis from dogs in Spain: possible zoonotic transmission and public health importance. Parasitol Res 2012; 111: 2419–2422. [DOI] [PubMed] [Google Scholar]
- 147. Sotiriadou I, Pantchev N, Gassmann D, et al. Molecular identification of Giardia and Cryptosporidium from dogs and cats. Parasite 2013; 20: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. McDowall RM, Peregrine AS, Leonard EK, et al. Evaluation of the zoonotic potential of Giardia duodenalis in fecal samples from dogs and cats in Ontario. Can Vet J 2011; 12: 1329–1333. [PMC free article] [PubMed] [Google Scholar]
- 149. Spada E, Proverbio D, Della Pepa A, et al. Prevalence of faecal-borne parasites in colony stray cats in northern Italy. J Feline Med Surg 2013; 15: 672–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Paris JK, Wills S, Balzer HJ, et al. Enteropathogen co-infection in UK cats with diarrhea. BMC Vet Res 2014; 10: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Gruffydd-Jones T, Addie D, Bélak S, et al. Giardiasis in cats. ABCD guidelines on prevention and management. J Feline Med Surg 2013; 15: 650–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
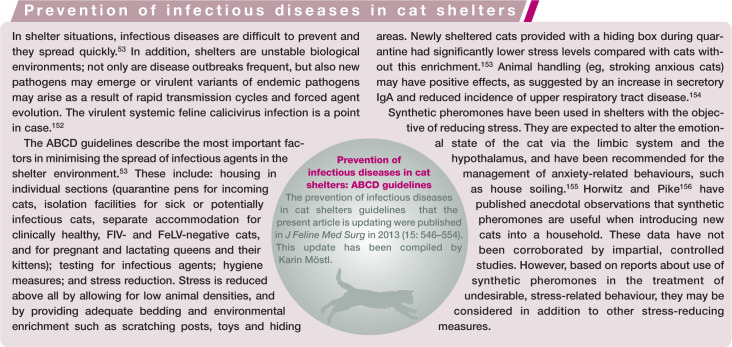
Prevention of infectious diseases in cat shelters
- 152. Pesavento PA, Murphy BG. Common and emerging infectious diseases in the animal shelter. Vet Pathol 2014; 51: 478–491. [DOI] [PubMed] [Google Scholar]
- 153. Vinke CM, Godijn LM, Van der Leij WJR. Will a hiding box provide stress reduction for shelter cats? Appl Anim Behav Sci 2014; 160: 86–93. [Google Scholar]
- 154. Gourkow N, Hamon SC, Phillips CJC. Effect of gentle stroking and vocalization on behaviour, mucosal immunity and upper respiratory tract disease in anxious shelter cats. Prev Vet Med 2014; 117: 266–275. [DOI] [PubMed] [Google Scholar]
- 155. Carney HC, Sadek TP, Curtis TM, et al. AAFP and ISFM guidelines for diagnosing and solving house-soiling behavior in cats. J Feline Med Surg 2014; 16: 579–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Horwitz DF, Pike AL. Common sense behavior modification: a guide for practitioners. Vet Clin Small Anim 2014; 44: 401–426. [DOI] [PubMed] [Google Scholar]