Abstract
Relevance:
The high fertility rate of cats means that methods to control feline reproduction are a requirement for cat breeders and pet owners, as well as for those involved in the management of feral cat populations. Progestins continue to be used to prevent queens from cycling, and also as an adjunct or alternative to surgical sterilization within trap–neuter–return (TNR) programs.
Evidence base:
A considerable body of information exists on megestrol acetate (MA) and medroxyprogesterone acetate (MPA), thanks to the many studies and case reports published in the scientific literature over the past 50 years documenting their clinical use in cats. Comparatively less is known about the use in cats of more recent progestins such as levonorgestrel, proligestone, delmadinone, chlormadinone and altrenogest.
Dosing, safety and efficacy:
Based on a combination of dose, frequency and duration of treatment, MA can be categorized into low (0.625 mg/kg/week for up to 30 weeks), medium (0.625 mg/kg q24h for 1 week or q48h for up to 2 weeks) and high (0.625 mg/kg q24h or q48h for several weeks, or weekly for months or years) dosages. Studies suggest that low dosages can be used relatively safely in cats, while higher dosages increase the risk and severity of adverse reactions. Early work showing that an oral MPA dosage of 0.01 mg/kg administered q24h for 12 months suppresses oestrus in queens effectively and safely has not been considered, and much higher MPA dosages (>6.25 mg/kg q24h) have been used in cats over the past 40 years.
Recommendations:
Progestins should always be used with caution. Using the lowest possible dosages, MA and MPA may, however, continue to be used safely in pet queens as well as (in conjunction with TNR programs) for the control of feral cat colonies. More recent progestins appear to be effective and safe, albeit their efficacy and safety need to be further investigated.
Introduction
The high fertility rate of cats, and the presence of large free-roaming cat populations in many countries, have made control of feline reproduction an object of debate in the Western world for the past several decades. According to The American Society for the Prevention of Cruelty to Animals, an estimated 1.4 million cats are euthanized annually in US animal shelters alone. 1 Surgery is currently the preferred approach to small animal sterilization. Trap–neuter–return (TNR) programs have been effective at reducing the feline population size in many countries, 2 particularly in select areas or island-type communities. An example is Venice, Italy, where a TNR program was started in the early 1980s as a joint effort between the neighboring municipalities of Venice, Cavallino-Treporti, Marcon and Quarto D’Altino. Since 2005, no further neutering has been done within Venice’s city limits, while cat neutering continues in the adjacent municipalities (C Guadagno, 2015, personal communication).
Where TNR programs are unsuccessful in urban areas, this may be due to the fact that cats are abandoned or spontaneously migrate into areas where TNR is being performed, thereby reducing its effects; 3 in some situations, these new animals constitute up to 21% of the population. 3 Furthermore, issues such as veterinary infrastructure costs, availability of trained staff and volunteers, and high levels of stress that cats may experience during the trapping process have raised concerns and reduced the effectiveness of some TNR programs.3,4
For these reasons, programs dedicated to funding research on non-surgical approaches to feline contraception and sterilization have been developed. Through such programs several interesting new sterilants based on mechanisms such as gene silencing, immunocontraception and targeted delivery of cytotoxins are being researched (see accompanying article in this Special Issue). 5
While waiting for the perfect, single-shot sterilant, medical contraceptive methods using progestins (progestogens) may serve as an important adjunct or alternative to surgical sterilization through TNR programs. Furthermore, progestins can be the appropriate (and only) answer for some types of reproductive presenting complaints in domestic queens.
From a breeder’s perspective, achieving a short-term, reversible block of a queen’s fertility can be of the utmost importance. Most European cat fancy clubs do not allow more than a certain number of litters in a defined period of time (normally no more than three litters in 2 years). Therefore, a breeder needs to avoid any risk of their breeding queens becoming pregnant for at least 6–9 months every 2 years. While this should not be a problem for breeding catteries that do not house tom cats, this does not necessarily negate the requirement for reproduction control. Queens normally vocalize continuously and eat less when in season, and as a result lose condition and develop a rough coat, compromising their chance of success in the judging ring at cat shows. For such reasons veterinarians are frequently asked to administer reproduction control drugs to breeding queens.
Progestins such as megestrol acetate (MA) and medroxyprogesterone acetate (MPA) have long been used in cats to control reproduction, while less clinical information is available for other, more recent compounds such as levonorgestrel, proligestone, delmadinone, chlormadinone or altrenogest. In ‘the field’ these compounds generally suffer a widespread reputation of posing risks and serious side effects from a reproductive as well as a general health standpoint. However, such a reputation is unjustified as all side effects appear to have been associated with excessively high dosing or inappropriate patient selection for treatment. This is particularly true for MA and MPA, the two drugs that have been more widely used in cats over the past four decades and for which a wealth of information exists on pharmacology, safety, effective dosages and risk of side effects. Indeed, for these two drugs, it appears that initial work demonstrating their relative safety has been overlooked while a great deal of attention has focused on case reports documenting side effects that were, in fact, caused by improper use.
As a result, many feline veterinarians are reluctant to (or never) use progestins in their female patients, 6 which is unfortunate as progestins are the only type of drug approved for temporary or reversible control of reproduction in cats. If their use is discouraged and queens cannot be prevented from cycling, many more pharmacological abortions or kitten euthanasias will be performed, which clearly is not in the interest of cat welfare. The following discussion reviews the literature on dosages of all progestins marketed as veterinary drugs to control feline reproduction, with a particular focus on MA and MPA. It documents historical use of these drugs and makes the case that, at appropriate doses, they can be considered relatively safe for use in cats.
Clinical use of progestins in cats
Progestins are synthetic derivatives of progesterone that bind to the progesterone receptor on target organs, producing the same biological effect as endogenous progesterone but with a much higher potency. These compounds are commonly used to control the reproductive cycle of female domestic animals and achieve their main contraceptive effect by suppressing clinical manifestations of oestrus as well as preventing ovulation. In bitches, progestins effectively suppress the ovulatory process by altering ovarian secretion of oestradiol, inhibin and/or activin, resulting in insufficient stimulation of the pituitary and no preovulatory peak of follicle-stimulating hormone and luteinizing hormone.7,8 Although not as well defined in cats, the similarity of clinical outcome in queens treated with progestins strongly indicates that the mechanism of action in cats is the same as in bitches.
All progestins administered to queens clearly suppress oestrus signs. The effect is short-lived in the case of MA9,10 and of variable duration for all other progestins tested in cats, including MPA, proligestone, chlormadinone acetate, delmadinone acetate, levonorgestrel and altrenogest.11 –14
Megestrol acetate
MA (6-methyl-6-dehydro-17α-acetoxyprogesterone) is a potent progestin with an activity estimated to be several times greater than that of endogenous progesterone, 15 and with a 75% and 37% affinity for the androgen and glucocorticoid receptors, respectively. 16 With a half-life of a few hours, MA is the shortest acting progestin available on the veterinary market and, in fact, the only product that can justifiably be labelled as ‘short acting’. It is currently commercially available as an oral formulation (pills or syrup) in many European countries including the UK, the Netherlands, Belgium, France, Switzerland and Italy.
Launched in 1975 and continuing for several decades, MA was commercially available in the USA as a Food and Drug Administration (FDA) approved veterinary drug for female dogs (Ovaban; Intervet Schering-Plough); off-label use in cats was common. 17 An extralabel formulation of MA (FeralStat) was also developed in North America for use in cats and privately marketed from 2008 by a veterinarian (Dr John Caltabiano) outside of regulatory oversight. 4 FeralStat was popular with some American cat colony managers, although no scientific data exist on this particular product’s efficacy and safety in cats. By 2011, after the passing of Dr Caltabiano, FeralStat orders were no longer being fulfilled. Since then, compounding pharmacies have been selling MA to feral cat colony managers with a veterinary prescription.
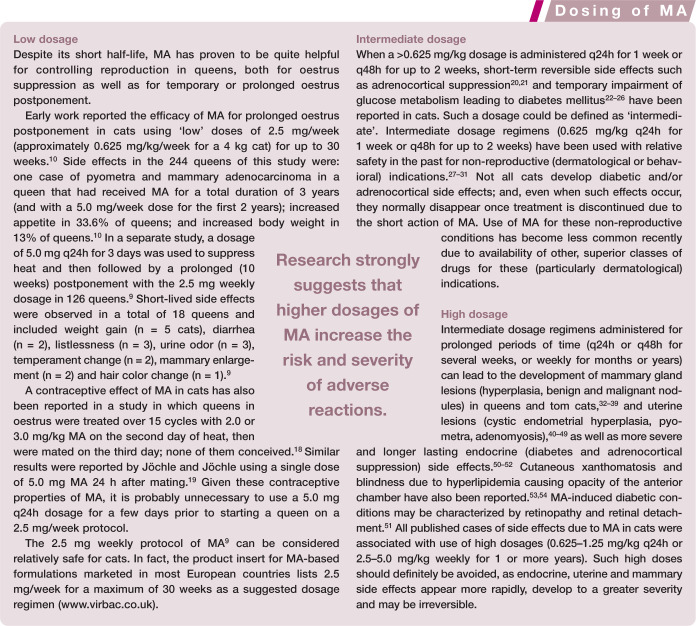
MA dosages can be categorized into low, medium and high (see box), based on a combination of the dose given in a single treatment, the frequency and the duration of treatment. Research strongly suggests that higher dosages increase the risk and severity of adverse reactions.
Treatment protocols using dosages of MA lower than the ‘low’ dosage of 0.625 mg/kg/week may be effective in controlling oestrus activity and ovulation in cats. The dosage of FeralStat was 0.1–0.2 mg/kg/week, 4 corresponding to a dosage of 0.014–0.028 mg/kg q24h. Another non-FDA-approved oral formulation of MA anecdotally reported as being effective for reproductive control in feral cat colonies has a suggested dosage of 5.0 mg/week for groups of five to seven cats, which corresponds (for groups of 4 kg cats) to 0.7–1.0 mg/cat/week or 0.18–0.25 mg/kg/ week or 0.025–0.035 mg/kg q24h (www.birthcontrolforcats). An Italian oral formulation of MA (Estropill; MSD) is administered to cats at a dosage of 0.011 mg/kg q24h and has recently been used by the author successfully to control oestrus in queens (unpublished data).
Further studies are required to establish the efficacy and safety of very low (0.01–0.03 mg/kg q24h) doses of MA administered to cats for prolonged periods of time.
Medroxyprogesterone acetate
MPA (17α-hydroxy-6α-methylprogesterone acetate) is a synthetic derivative of progesterone that is also more potent than progesterone. 55 MPA also acts as an agonist of the androgen and glucocorticoid receptors, although its affinity for the androgen and glucocorticoid receptors is much lower than that of MA. 56 Its half-life is 12–17 h following an oral dose and 40–50 days following an intramuscular (IM) dose. It has long been available as a veterinary drug in Europe with an indication for use in cats, and it is still available in several countries including Austria, Germany, the Netherlands, Belgium, Luxembourg, Sweden, Norway, Spain, Portugal and Italy.
In one of the first scientific studies on the use of MPA in cats, oestrus was suppressed using oral doses of 0.05 and 0.01 mg/kg administered q24h for 12 months to two groups of six queens, respectively. 57 Only one case of breakthrough heat occurred after 7 months of treatment in the 0.01 mg/kg group, while the 0.05 mg/kg dose showed 100% efficacy, with no oestrus reported in treated queens. All queens from the latter group were in good health throughout the study, came back in heat at the end of the study and queened 83–184 days following discontinuation of the treatment. According to the authors, ‘… many of the kittens of these first litters were stillborn or small and weak; however, succeeding litters were normal.’ 57
The results of this study point to a negative effect of prolonged treatment with a 0.05 mg/kg q24h dosage of MPA on fertility at the first post-treatment heat in queens. However, long-term fertility of treated queens was not altered. Also, although general and mammary health, as well as haematology and biochemistry, were not assessed, one could speculate that MPA did not cause major health problems in these queens based on the fact that, firstly, they all queened normal litters later on and, secondly, negative effects of MPA on the uterus, mammary glands, glucose tolerance and general health have only been reported using dosages >100 times higher than those used in this study. 57
Unfortunately, there is almost no trace of this publication in the subsequent MPA-related scientific literature. In 1965, a study by Colton 58 investigating either an oral dosage of 5.0 mg/cat q24h (12.5 mg/kg q24h for a 4 kg cat) for 3–5 days or a single subcutaneous injection of 25–100 mg (equivalent to 6.25–25 mg/kg in a 4 kg cat) suggested both as being effective treatments to achieve oestrus suppression of at least 2–4 months. 58 Two subsequent case reports described the occurrence of mammary hyperplasia in a queen treated with a single 50 mg MPA injection 59 and mammary tumors in five queens treated with 25–50 mg/cat every 3–4 months for several years. 60
Despite these two case reports pointing to an evident risk of high doses of MPA, all authors of reviews and book chapters published over the following 20 years continued to advise prolonged oestrus suppression in queens with MPA using a single parenteral injection of 25–100 mg to be repeated every 4–6 months, sometimes even preceded by a 5 day course of 5.0 mg/day if the queen was in heat at the beginning of the treatment.61 –64 The same high-dosage protocols (25–100 mg parenteral injections every 4–6 months, sometimes with an initial 5 day oral treatment) are reported in later reviews during the 1990s,65 –67 as well as in more recent publications.68 –72 Admittedly, side effects of MPA in cats are always carefully described; however, no discussion on MPA dosages can be found, sometimes dosages are generically reported (if at all) and readers are simply warned about the risk of side effects, with no mention of a distinction between a high risk of side effects with high dosing and low or no risk with low dosing.
Interestingly, the aforementioned two case reports on MPA side effects in queens59,60 are almost never cited in the subsequent literature, which means that the MPA side effects in cats referred to in publications until the early 2000s were either assumed to be similar to those caused by another progestin, MA (again used at much higher doses than normal), or assumed to be similar to the side effects of MPA in the bitch. One might speculate that mammary, uterine and endocrine side effects in cats may be similar for all progestins, and/or that side effects may be similar across the canine and feline species. However, unlike MA, there is a lack of reports on diabetogenic side effects in cats treated with even very high doses of MPA. This may be due to the lower affinity of MPA for the glucocorticoid receptor when compared with MA, 56 and it shows that extrapolating between drugs and across species is not always appropriate. Extrapolation has led some authors to state that MPA is not recommended for use in cats, 73 based on the many side effects of high doses of MA in cats. Such unsubstantiated claims have been subsequently cited,69,72 contributing to the negative reputation of MPA among feline practitioners.
As with many other drugs, MPA should be used with caution and only in healthy animals. However, if used judiciously, it may be helpful in feline practice. Case reports documenting side effects of MPA in cats due to overdosing clearly indicate that the mammary gland is the first target organ to suffer,59,60,74 –77 while glucose or mineralocorticoid metabolism derangements have never been reported in cats following the use of high MPA dosages. Thus, MPA and MA seem to be characterized by a different range of side effects, and this might be important when deciding upon a treatment. Provision of complete and accurate information on the safety of MPA could allow veterinarians to implement appropriate control of reproduction in queens in countries in which MPA is the only available progestin.
Other progestins
Although MA and MPA have been used most widely in cats, other progestins tested with some degree of success for reproductive control in cats include levonorgestrel, chlormadinone acetate, delmadinone acetate, proligestone and altrenogest.
Levonorgestrel (LEV) is frequently used as a component of combined hormonal contraceptives in humans. When administered for 12 months as a 16–36 mg subdermal slow release implant in queens, LEV suppressed reproductive activity without any relevant side effects on the mammary glands, body weight, and glucose or adrenocortical metabolism.13,78,79 Cessation of ovarian activity is quite rapid following placement of the implant, although there is often no effect on the oestrous cycle that starts before treatment. 79 One study demonstrated normal fertility following cessation of treatment in the majority of treated queens (3/4 queens exhibited estrus and conceived within 54 days following implant removal), although endometrial hyperplasia was observed and fluid accumulation occurred in one case, suggesting the development of pyometra. 13
Chlormadinone acetate (CMA) administered for 1 year either in oral weekly doses of 2.0–12.5 mg in 28 queens, 12 or as 2.5, 5.0 or 20 mg/kg implants in 13 queens,80,81 suppressed oestrus signs for the duration with only an increase in body weight for the oral treatment 12 or endometrial hyperplasia with mild uterine fluid accumulation with the 20 mg/kg implant. 81 When the 2.0 mg CMA dose was administered weekly for several years, there were no clinical signs of abnormality for 4.6 years in 24 queens except for the increase in body weight. 81 In a longitudinal study involving 24 queens, 19, 16 and four cats were treated for 6, 8 and 10 years, respectively. 82 Mammary nodules and vaginal discharge or pyometra were recorded in 11% of cats treated for 6 years, 38% of cats treated for 8 years, and 25% of cats treated for 10 years. 82
Delmadinone acetate (DMA) administered as a single oral dose (2.5 mg) is reportedly effective as a contraceptive when given once 24 h after the onset of heat. 19 The same study found a single dose of 5.0 mg CMA likewise to be effective.
Proligestone (PRG) has been marketed since the 1990s in many European countries as a veterinary drug with an indication for use in cats, at a dosage of 100 mg/cat (or 25–30 mg/kg) to be repeated every 5 months. In comparison with other progestins, PRG is claimed to be as effective for the control of oestrus (ie, on the hypothalamic–pituitary– gonadal axis) but less active on the reproductive system (uterus and mammary glands) in queens. 11 In a study comparing the efficacy of 30 mg/kg PRG with 25 mg/cat MA in two groups of 15 queens, a duration of efficacy of approximately 8 months was reported for PRG vs 3–5 months for MA. 83 No mammary or uterine side effects were observed in the queens in the PRG group, while no mammary disease but two cases of pyometra were observed in the queens in the MA group. 83 However, the treatment protocol included for both drugs the induction of ovulation with gonadotropin-releasing hormone (GnRH) when queens were in heat. Although induction of ovulation should not be performed prior to administration of a progestin (as the occurrence of diestrus will cause overdosing), these results suggest that PRG may stimulate the feline mammary gland to a lower degree than MA.
When compared with MA in an acute toxicity study, PRG had fewer effects on adrenocorticotropic hormone (ACTH) and blood glycaemia, and no effect on insulin levels. 84 In a single-cat case report, a 7-month-old Maine Coon queen weighing 4.2 kg developed benign mammary hyperplasia 2 months after being treated with a fairly low dose of 0.75 ml (17.8 mg/kg) PRG. 85 Also, a case of calcinosis circumscripta has been reported in another single-cat case report describing a 9-month-old Burmese queen treated with 100 mg PRG to suppress oestrus 4 months previously. 86 Calcinosis circumscripta has been reported in the bitch following the use of MPA.87,88
Although the above studies and case reports point to a similarity in the range of side effects between PRG and other progestins, currently available information on uterine and endocrine side effects of PRG in cats could indicate a lower affinity of PRG for the uterus and for glucose and adrenal metabolism in cats.
Altrenogest (ALG) has been used at an oral dose of 0.044, 0.088 and 0.352 mg/kg for 38 days in groups of five, five and six queens, respectively. 14 All three doses investigated in this study were effective in suppressing and controlling heat, although queens with elevated estrogen concentrations at the beginning of treatment completed their heat before entering a drug-induced anestrus. 14 Post-treatment follicular activity resumed soon after the end of the study, and in a fairly synchronous way (within 10–16 days) for the 0.088 mg/kg treatment. There were no side effects in treated queens. 14 Beyond this single study, little is known about the safety of ALG use in queens, although the compound seems effective for the control of reproduction.
Further studies are necessary to assess the safety and efficacy of prolonged use of LEV, CMA, DMA, PRG and ALG in queens.
Considerations for safe use of progestins in cats
Several factors must be taken into account to optimize the likelihood of safe use of progestins in queens, as reviewed below.
Client-owned cats
Queens to be treated with progestins should be healthy and in post-estrus or anestrus (not oestrus or diestrus). This requires a careful evaluation.
Sadly, the package insert of several progestin drugs marketed in Europe for small animal use, including queens, still reports diestrus as being one of the reproductive cycle stages in which progestin treatment may be initiated. Assaying P4 is costly and involves drawing a blood sample. Consequently, a P4 assay is often not advised prior to administering progestins on the assumption that queens cannot be in diestrus if not bred. However, research has found that 35–87% of queens may ovulate spontaneously.79,89,90 Therefore, when considering progestin treatment the possibility of a queen being in diestrus should not be underestimated.
Use of progestins in male cats is not advised for the following reasons:
Lack of efficacy for reproductive indications (post-castration urine marking or aggressiveness can only be solved temporarily with progestins and should be addressed from a behavioral perspective);
Lack of efficacy for dermatological presentations; 91
Males are at a significantly higher risk of developing a diabetic condition when treated with MA compared with females. 92
Feral cat colonies
While the above precautions can and should be adopted when treating client-owned animals, a ‘population level’ or ‘herd health’ approach may be warranted when using a progestin in colonies of feral cats (Figure 1).
Figure 1.
Potentially, lowdose progestins may be a useful adjunct to TNR in the control of free-roaming or feral cats, by preventing pregnancies in animals waiting to be spayed. Courtesy of Valerie Benka/ACC&D
When the history of a patient is not available, or when clinical examination or any further testing cannot be performed for practical or financial reasons, clinicians must be guided by the ethical principle of doing the least harm to each individual cat while ensuring the maximum possible level of health for the entire colony. On this basis, a low dose treatment of MA or MPA may have potential to be employed in feral cat colonies in conjunction with a TNR program to prevent pregnancies in animals waiting to be spayed.
The use of reproductive control drugs in feral cat colonies remains highly controversial. Issues such as environmental fate (ingestion of baits by non-target species, including humans), human safety (progestins are absorbed through intact skin), stability (shelf-life in the intended packaging before and after being opened), food interaction, dose accuracy and use as a prescription-only medication (a bait-based drug may have to be prescribed by a veterinarian who would not themselves be administering it) raise more concern than target animal safety (which could actually be acceptable when using ‘very low’ doses of MA or MPA).
Nonetheless, when using a bait system there is the potential for overdosing as well as inadvertent treatment of prepubertal or mature males, and prepubertal or pregnant females, which may cause side effects (ie, mammary hyperplasia in male and female cats). However, in queens, mammary hyperplasia occurs (sporadically) only at the first luteal phase; there are no case reports of this condition occurring more than once in the same queen. Thus, when mammary hypertrophy occurs in a young queen following use of a progestin, one might argue that it would have occurred anyway in that individual queen at her first ovulation. The specific risks with regard to tom cats have been discussed above. However, it is worth noting that the risks for diabetes and mammary hypertrophy in males have been reported following use of high dosages; therefore, from a feral cat perspective, the use of progestins (particularly MA) at very low dosages is probably less dangerous.
In countries of the European Union a pre-prepared progestin-based bait for use in feral cats would represent an entirely new product, even if the active pharmaceutical agent was a well known one. Because of all the above concerns there is no guarantee that a competent authority would accept the risk/benefit analysis that is necessary for the registration dossier, particularly on the grounds of environmental 93 and human 94 safety. For these reasons, interest among drug companies to invest in a reproductive control bait-type drug for feral cats in Europe is realistically likely to be minimal at this time.
Key Points
Further studies are needed to establish the longest possible treatment with progestins (MA or MPA) that is free of side effects, incorporating information on haematobiochemical as well as uterine ultrasonographic changes in queens on long-term progestin treatment.
Most importantly, there is a need to change our approach to the use of progestins in queens (and bitches alike) and clarify best protocols when using a progestin.
Too many queens have been treated with excessively high doses of progestins, and many more are at risk because of inaccurate or incomplete information on their use that persists around the world.

Footnotes
Funding: The author received no specific grant from any funding agency in the public, commercial or not-for-profit sectors for the preparation of this article.
The author has no conflict of interest to declare.
References
- 1. ASPCA. Pet statistics: How many pets are in the United States? How many animals are in shelters? https://www.aspca.org/about-us/faq/pet-statistics (2015, accessed 10 June, 2015).
- 2. Wallace JL, Levy JK. Population characteristics of feral cats admitted to seven trap–neuter–return programs in the United States. J Feline Med Surg 2006; 8: 279–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Natoli E, Maragliano L, Cariola G, et al. Management of feral domestic cats in the urban environment of Rome (Italy). Prev Vet Med 2006; 77: 180–185. [DOI] [PubMed] [Google Scholar]
- 4. Greenberg M, Lawler D, Zawistowski S, et al. Low-dose megestrol acetate revisited: a viable adjunct to surgical sterilization in free roaming cats? Vet J 2013; 196: 304–308. [DOI] [PubMed] [Google Scholar]
- 5. Johnston S, Rhodes L. No surgery required: the future of feline sterilization. An overview of the Michelson Prize & Grants in Reproductive Biology. J Feline Med Surg 2015; 17: 777–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Elliott JE. Use of progesterone-based medications in cats – neutered or otherwise [Letter]. J Feline Med Surg 2011; 13: 536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Beijerink NJ, Bhatti SFM, Okkens AC, et al. Adenohypophysial function in bitches treated with medroxyprogesterone acetate. Domest Anim Endocrinol 2007; 32: 63–78. [DOI] [PubMed] [Google Scholar]
- 8. Beijerink NJ, Bhatti SF, Okkens AC, et al. Pulsatile plasma profiles of FSH and LH before and during medroxyprogesterone acetate treatment in the bitch. Theriogenology 2008; 70: 179–185. [DOI] [PubMed] [Google Scholar]
- 9. Houdeshell JW, Hennessey PW. Megestrol acetate for control of estrus in the cat. Vet Med Small Anim Clin 1977; 72: 1013–1017. [PubMed] [Google Scholar]
- 10. Oen EO. The oral administration of megestrol acetate to postpone oestrus in cats. Nord Vet Med 1977; 29: 287–291. [PubMed] [Google Scholar]
- 11. Evans JM, Sutton DJ. The use of hormones, especially progestagens, to control oestrus in bitches. J Reprod Fertil Suppl 1989; 39: 163–173. [PubMed] [Google Scholar]
- 12. Sawada T, Tamada H, Inaba T, et al. Prevention of estrus in the queen with chlormadinone acetate administered orally. J Vet Med Sci 1992; 54: 1061–1062. [DOI] [PubMed] [Google Scholar]
- 13. Baldwin CJ, Peter AT, Bosu WT, et al. The contraceptive effects of levonorgestrel in the domestic cat. Lab Anim Sci 1994; 44: 261–269. [PubMed] [Google Scholar]
- 14. Stewart RA, Pelican KM, Brown JL, et al. Oral progestin induces rapid, reversible suppression of ovarian activity in the cat. Gen Comp Endocrinol 2010; 166: 409–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Janne O, Kontula K, Vihko R, et al. Progesterone receptor and regulation of progestin action in mammalian tissues. Med Biol 1978; 56: 225–248. [PubMed] [Google Scholar]
- 16. Briggs MH, Briggs M. Glucocorticoid properties of progestogens. Steroids 1973; 22: 555–559. [DOI] [PubMed] [Google Scholar]
- 17. Romatowski J. Use of megestrol acetate in cats. J Am Vet Med Assoc 1989; 194: 700–702. [PubMed] [Google Scholar]
- 18. David A, Edwards K, Fellowes KP, et al. Anti- ovulatory and other biological properties of megestrol acetate: 17α-acetoxy-6 methyl pregna 4:6-diene-3:20-dione (B.D.H. 1298). J Reprod Fertil 1963; 5: 331–346. [Google Scholar]
- 19. Jöchle W, Jöchle M. Reproductive and behavioral control in the male and female cat with progestins: long-term field observations in individual animals. Theriogenology 1975; 3: 179–185. [DOI] [PubMed] [Google Scholar]
- 20. Chastain CB, Graham CL, Nichols CE. Adrenocortical suppression in cats given megestrol acetate. Am J Vet Res 1981; 42: 2029–2035. [PubMed] [Google Scholar]
- 21. Middleton DJ, Watson AD, Howe CJ, et al. Suppression of cortisol responses to exogenous adrenocorticotrophic hormone, and the occurrence of side effects attributable to glucocorticoid excess, in cats during therapy with megestrol acetate and prednisolone. Can J Vet Res 1987; 51: 60–65. [PMC free article] [PubMed] [Google Scholar]
- 22. Werner RE. A warning. Feline Pract 1978; 8: 4. [Google Scholar]
- 23. Moise NS, Reimers TJ. Insulin therapy in cats with diabetes mellitus. J Am Vet Med Assoc 1983; 182: 158–164. [PubMed] [Google Scholar]
- 24. Middleton DJ, Watson AD. Glucose intolerance in cats given short-term therapies of prednisolone and megestrol acetate. Am J Vet Res 1985; 46: 2623–2625. [PubMed] [Google Scholar]
- 25. Mansfield PD, Kemppainen RJ, Sartin JL. The effects of megestrol acetate treatment on plasma glucose concentration and insulin response to glucose administration in cats. J Am Anim Hosp Assoc 1986; 22: 515–518. [Google Scholar]
- 26. Peterson ME. Effects of megestrol acetate on glucose tolerance and growth hormone secretion in the cat. Res Vet Sci 1987; 42: 354–357. [PubMed] [Google Scholar]
- 27. Turner WT. Use of megestrol acetate in the treatment of miliary eczema in the cat. Vet Rec 1971; 88: 315–316. [DOI] [PubMed] [Google Scholar]
- 28. Hutchison JA. Progestogen therapy for certain skin diseases of cats. Can Vet J 1978; 19: 324. [PMC free article] [PubMed] [Google Scholar]
- 29. Hart BL. Objectionable urine spraying and urine marking in cats: evaluation of progestin treatment in gonadectomized males and females. J Am Vet Med Assoc 1980; 177: 529–533. [PubMed] [Google Scholar]
- 30. Gosselin Y, Chalifoux A, Papageorges M. The use of megestrol acetate in some feline dermatological problems. Can Vet J 1981; 22: 382–384. [PMC free article] [PubMed] [Google Scholar]
- 31. Browning MJ, Herbert WJ, White RG. Feline miliary eczema: megestrol acetate does not suppress immune responses. Res Vet Sci 1983; 35: 245–246. [PubMed] [Google Scholar]
- 32. Hinton M, Gaskell CJ. Non-neoplastic memmary hypertrophy in the cat associated either with pregnancy or with oral progestagen therapy. Vet Rec 1977; 100: 277–280. [DOI] [PubMed] [Google Scholar]
- 33. Hayden DW, Johnston SD, Kiang DT, et al. Feline mammary hypertrophy/fibroadenoma complex: clinical and hormonal aspects. Am J Vet Res 1981; 42: 1699–1703. [PubMed] [Google Scholar]
- 34. Pukay BP, Stevenson DA. Mammary hypertrophy in an ovariohysterectomized cat. Can Vet J 1983; 24: 143–144. [PMC free article] [PubMed] [Google Scholar]
- 35. Dorn AS, Legendre AM, McGavin MD. Mammary hyperplasia in a male cat receiving progesterone. J Am Vet Med Assoc 1983; 182: 621–622. [PubMed] [Google Scholar]
- 36. Tomlinson MJ, Barteaux L, Ferns LE, et al. Feline mammary carcinoma: a retrospective evaluation of 17 cases. Can Vet J 1984; 25: 435–439. [PMC free article] [PubMed] [Google Scholar]
- 37. Hayden DW, Barnes DM, Johnson KH. Morphologic changes in the mammary gland of megestrol acetate-treated and untreated cats: a retrospective study. Vet Pathol 1989; 26: 104–113. [DOI] [PubMed] [Google Scholar]
- 38. Mol JA, van Garderen E, Selman PJ, et al. Growth hormone mRNA in mammary gland tumors of dogs and cats. J Clin Invest 1995; 95: 2028–2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. MacDougall LD. Mammary fibroadenomatous hyperplasia in a young cat attributed to treatment with megestrol acetate. Can Vet J 2003; 44: 227–229. [PMC free article] [PubMed] [Google Scholar]
- 40. Teale ML. Pyometritis in spayed cats [Letter]. Vet Rec 1972; 91: 129. [DOI] [PubMed] [Google Scholar]
- 41. Long RD. Pyometritis in spayed cats [Letter]. Vet Rec 1972; 91: 105–106. [DOI] [PubMed] [Google Scholar]
- 42. Orhan UA. Pyometritis in spayed cats [Letter]. Vet Rec 1972; 91: 77. [DOI] [PubMed] [Google Scholar]
- 43. Wilkins DB. Pyometritis in a spayed cat [Letter]. Vet Rec 1972; 91: 24. [DOI] [PubMed] [Google Scholar]
- 44. Skerritt GC. Oral progestagens and pyometra in the cat [Letter]. Vet Rec 1975; 96: 573. [DOI] [PubMed] [Google Scholar]
- 45. Ellis CP. Oral progestagens in cats [Letter]. Vet Rec 1975; 96: 513–514. [DOI] [PubMed] [Google Scholar]
- 46. Walker CE. Oral progestagens in cats [Letter]. Vet Rec 1975; 96: 458. [DOI] [PubMed] [Google Scholar]
- 47. Remfry J. Control of feral cat populations by long-term administration of megestrol acetate. Vet Rec 1978; 103: 403–404. [DOI] [PubMed] [Google Scholar]
- 48. Bellenger CR, Chen JC. Effect of megestrol acetate on the endometrium of the prepubertally ovariectomised kitten. Res Vet Sci 1990; 48: 112–118. [PubMed] [Google Scholar]
- 49. Bulman-Fleming J. A rare case of uterine adenomyosis in a Siamese cat. Can Vet J 2008; 49: 709–712. [PMC free article] [PubMed] [Google Scholar]
- 50. Pukay BP. A hyperglycemia-glucosuria syndrome in cats following megestrol acetate therapy. Can Vet J 1979; 20: 117. [PMC free article] [PubMed] [Google Scholar]
- 51. Herrtage ME, Barnett KC, MacDougall DF. Diabetic retinopathy in a cat with megestrol acetate-induced diabetes. J Small Anim Pract 1985; 26: 595–601. [Google Scholar]
- 52. Watson AD, Church DB, Emslie DR, et al. Comparative effects of proligestone and megestrol acetate on basal plasma glucose concentrations and cortisol responses to exogenous adrenocorticotrophic hormone in cats. Res Vet Sci 1989; 47: 374–376. [PubMed] [Google Scholar]
- 53. Kwochka KW, Short BG. Cutaneous xanthomatosis and diabetes mellitus following long-term therapy with megestrol acetate in a cat. Comp Contin Educ Pract Vet 1984; 6: 185–192. [Google Scholar]
- 54. Ghaffari MS. Iatrogenic hyperlipidemia associated with lipid-laden aqueous humor in a cat following administration of megestrol acetate. Turk J Vet Anim Sci 2008; 32: 399–401. [Google Scholar]
- 55. Elton RL, Edgren RA, Calhoun DW. Biological activities of some 6-methylated progesterones. Proc Soc Exp Biol Med 1960; 103: 175–177. [DOI] [PubMed] [Google Scholar]
- 56. Schindler AE, Campagnoli C, Druckmann R, et al. Classification and pharmacology of progestins. Maturitas 2003; 46 Suppl 1: 7–16. [DOI] [PubMed] [Google Scholar]
- 57. Harris TW, Wolchuk N. The suppression of oestrus in the dog and cat with long term administration of synthetic progestational steroids. Am J Vet Res 1963; 24: 1003–1006. [PubMed] [Google Scholar]
- 58. Colton MW. Progestational agents in pet practice, indications, agents and doses, precautions. Mod Vet Pract 1965; June 1965: 53–56. [Google Scholar]
- 59. Thorton DA, Kear M. Uterine cystic hyperplasia in a siamese Cat following treatment with medroxyprogesterone. Vet Rec 1967; 80: 380–381. [DOI] [PubMed] [Google Scholar]
- 60. Hernandez FJ, Chertack M, Gage PA. Feline mammary carcinoma and progestogens. Feline Pract 1975; 5: 45–48. [PubMed] [Google Scholar]
- 61. Shille V, Stabenfeldt GH. Current concepts in reproduction of the dog and cat. Adv Vet Sci Comp Med 1980; 24: 211–243. [PubMed] [Google Scholar]
- 62. Colby E. Suppression/induction of estrus in cats. In: Morrow DA. (ed). Current therapy in theriogenology. Philadelphia: WB Saunders, 1980, pp 861–865. [Google Scholar]
- 63. Henik RA, Olson PN, Rosychuk RA. Progestogen therapy in cats. Compend Contin Educ Pract Vet 1985; 7: 132–141. [Google Scholar]
- 64. Wildt DE. Estrous cycle control – induction and prevention in cats. In: Morrow DA. (ed). Current therapy in theriogenology: diagnosis, treatment, and prevention of reproductive diseases in small and large animals (v. 2). Philadelphia: WB Saunders, 1986, pp 808–812. [Google Scholar]
- 65. Jöchle W. Pet population control in Europe. J Am Vet Med Assoc 1991; 198: 1225–1230. [PubMed] [Google Scholar]
- 66. Concannon PW, Meyers-Wallen VN. Current and proposed methods for contraception and termination of pregnancy in dogs and cats. J Am Vet Med Assoc 1991; 198: 1214–1225. [PubMed] [Google Scholar]
- 67. Concannon PW. Contraception in the dog. Vet Annual 1995; 35: 177–187. [Google Scholar]
- 68. Johnston SD, Root-Kustritz MV, Olson PNS. Prevention and termination of feline pregnancy. In: Johnston SD, Root-Kustritz MV, Olson PNS. (eds). Canine and feline theriogenology. Philadelphia: WB Saunders, 2001, pp 447–452. [Google Scholar]
- 69. Kutzler M, Wood A. Non-surgical methods of contraception and sterilization. Theriogenology 2006; 66: 514–525. [DOI] [PubMed] [Google Scholar]
- 70. Munson L. Contraception in felids. Theriogenology 2006; 66: 126–134. [DOI] [PubMed] [Google Scholar]
- 71. Goericke-Pesch S. Reproduction control in cats: new developments in non-surgical methods. J Feline Med Surg 2010; 12: 539–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Goericke-Pesch S, Wehrend A, Georgiev P. Suppression of fertility in adult cats. Reprod Dom Animals 2014; 49 Suppl 2: 33–40. [DOI] [PubMed] [Google Scholar]
- 73. Jackson EKM. Contraception in the dog and cat. Brit Vet J 1984; 140: 132–137. [DOI] [PubMed] [Google Scholar]
- 74. Loretti AP, Ilha MR, Ordas J, et al. Clinical, pathological and immunohistochemical study of feline mammary fibroepithelial hyperplasia following a single injection of depot medroxyprogesterone acetate. J Feline Med Surg 2005; 7: 43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Keskin A, Yilmazbas G, Yilmaz R, et al. Pathological abnormalities after long-term administration of medroxyprogesterone acetate in a queen. J Feline Med Surg 2009; 11: 518–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Enginler SO, Senunver A. The effects of progesterone hormone applications used for suppression of estrus on mammary glands in queens. Kafkas Üniv Vet Fak Derg 2011; 17: 277–284. [Google Scholar]
- 77. Ochota M, Nowak M, Dzieciol M, et al. Mammary adenocarcinoma after 10-year medroxyprogesterone acetate supplementation in an ovariectomized cat. Pakistan Vet J 2014; 34: 406–409. [Google Scholar]
- 78. Baldwin CJ, Peter AT, Bosu WT. Adrenocortical function in the domestic cat during treatment with levonorgestrel. Res Vet Sci 1996; 60: 205–208. [DOI] [PubMed] [Google Scholar]
- 79. Pelican KM, Brown JL, Wildt DE, et al. Short term suppression of follicular recruitment and spontaneous ovulation in the cat using levonorgestrel versus a GnRH antagonist. Gen Comp Endocrinol 2005; 144: 110–121. [DOI] [PubMed] [Google Scholar]
- 80. Murakoshi M, Tagawa M, Ikeda R. Histopathological studies of subcutaneous implantation of chlormadinone acetate (CMA) for preventing estrus in queens. Tokai J Exp Clin Med 2000; 25: 7–10. [PubMed] [Google Scholar]
- 81. Murakoshi M, Tagawa M, Ikeda R. The effect of subcutaneous implantation of chlormadinone acetate for preventing estrus in queens. J Toxicol Pathol 1996; 9: 185–190. [PubMed] [Google Scholar]
- 82. Tamada H, Kawate N, Inaba T, et al. Long-term prevention of estrus in the bitch and queen using chlormadinone acetate. Can Vet J 2003; 44: 416–417. [PMC free article] [PubMed] [Google Scholar]
- 83. Findik M, Erunal Maral N, Asian S. The use of proligestone, megestrol acetate and GnRH on queens with the aim of hormonal contraception. Turk J Vet Anim Sci 1999; 23: 455–460. [Google Scholar]
- 84. Church DB, Watson AD, Emslie DR, et al. Effects of proligestone and megestrol on plasma adrenocorticotrophic hormone, insulin and insulin-like growth factor-1 concentrations in cats. Res Vet Sci 1994; 56: 175–178. [DOI] [PubMed] [Google Scholar]
- 85. Vitasek R, Dendisova H. Treatment of feline mammary fibroepithelial hyperplasia following a single injection of proligestone. Acta Vet Brno 2006; 75: 295–297. [Google Scholar]
- 86. O’Brien CR, Wilkie JS. Calcinosis circumscripta following an injection of proligestone in a Burmese cat. Aust Vet J 2001; 79: 187–189. [DOI] [PubMed] [Google Scholar]
- 87. Ginel P, Perez J, Rivas R, et al. Calcinosis circumscripta associated with medroxyprogesterone in two poodle bitches. J Am Anim Hosp Assoc 1992; 28: 391–394. [Google Scholar]
- 88. Ginel P, Lopez R, Perez J, et al. A further case of medroxyprogesterone acetate associated with calcinosis circumscripta in the dog. Vet Rec 1995; 136: 44–45. [DOI] [PubMed] [Google Scholar]
- 89. Lawler DF, Johnston SD, Hegstad RL, et al. Ovulation without cervical stimulation in domestic cats. J Reprod Fertil Suppl 1993; 47: 57–61. [PubMed] [Google Scholar]
- 90. Gudermuth DF, Newton L, Daels P, et al. Incidence of spontaneous ovulation in group-housed cats based on serum and faecal concentrations of progesterone. J Reprod Fertil Suppl 1997; 51: 177–184. [PubMed] [Google Scholar]
- 91. Simpson BS, Papich MG. Pharmacologic management in veterinary behavioral medicine. Vet Clin North Am Small Anim Pract 2003; 33: 365–404. [DOI] [PubMed] [Google Scholar]
- 92. McCann TM, Simpson KE, Shaw DJ, et al. Feline diabetes mellitus in the UK: the prevalence within an insured cat population and a questionnaire-based putative risk factor analysis. J Feline Med Surg 2007; 9: 289–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. European Medicines Agency. Reflection paper on risk mitigation measures related to the environmental risk assessment of veterinary medicinal products. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2012/03/WC500124187.pdf (2012, accessed 10 June 2015).
- 94. European Medicines Agency. Guidance on user safety evaluation for pharmaceutical veterinary medicinal products – development of existing and future guidance. http://www.ema.europa.eu/docs/en_GB/document_library/Presentation/2014/03/WC500163689.pdf (2014, accessed 10 June 2015).
- 95. Romagnoli S, Concannon PW. Clinical use of progestins in bitches and queens: a review. In: Concannon PW, England G, Verstegen J, III, et al. (eds). Recent advances in small animal reproduction. International Veterinary Information Service. http://www.ivis.org/advances/Concannon/romagnoli2/chapter.asp?LA=1 (2003, accessed June 10, 2015).
- 96. Romagnoli S, Sontas H. Prevention of breeding in the female. In: England GCW, von Heimendahl A. (eds). BSAVA manual of canine and feline reproduction and neonatology. 2nd ed. Gloucester: British Small Animal Veterinary Association, 2010, pp 23–33. [Google Scholar]
- 97. Romagnoli S. Reproduction control – new developments, old debates [Letter]. J Feline Med Surg 2010; 12: 724. [DOI] [PubMed] [Google Scholar]
- 98. Sarchahi AA, Emadi M, Azarpeykan S. Effects of three steroidal compounds on oestrus suppression in queens. Iran J Vet Res 2008; 9: 144–149. [Google Scholar]
- 99. Misdorp W, Romijn A, Hart AAM. Feline mammary tumors: a case-control study of hormonal factors. Anticancer Res 1991; 11: 1793–1797. [PubMed] [Google Scholar]