Abstract
Intellectual disability (ID) commonly co-occurs in children with autism. Although diagnostic criteria for ID require impairments in both cognitive and adaptive functioning, most population-based estimates of the frequency of co-occurring ID in children with autism—including studies of racial and ethnic disparities in co-occurring autism and ID—base the definition of ID solely on cognitive scores. The goal of this analysis was to examine the effect of including both cognitive and adaptive behavior criteria on estimates of co-occurring ID in a well-characterized sample of 2- to 5-year-old children with autism. Participants included 3264 children with research or community diagnoses of autism enrolled in the population-based Study to Explore Early Development (SEED) phases 1–3. Based only on Mullen Scales of Early Learning (MSEL) composite cognitive scores, 62.9% (95% confidence interval [CI]: 61.1, 64.7%) of children with autism were estimated to have co-occurring ID. After incorporating Vineland Adaptive Behavior Scales, Second Edition (VABS-II) composite or domains criteria, co-occurring ID estimates were reduced to 38.0% (95% CI: 36.2, 39.8%) and 45.0% (95% CI: 43.1, 46.9%), respectively. The increased odds of meeting ID criteria observed for non-Hispanic (NH) Black and Hispanic children relative to NH White children when only MSEL criteria were used were substantially reduced, though not eliminated, after incorporating VABS-II criteria and adjusting for selected socioeconomic variables. This study provides evidence for the importance of considering adaptive behavior as well as socioeconomic disadvantage when describing racial and ethnic disparities in co-occurring ID in epidemiologic studies of autism.
Keywords: adaptive behavior, adaptive functioning, cognitive ability, cognitive development, co-occurring conditions, intellectual disability, IQ, Mullen scales of early learning, Vineland adaptive behavior scales
Lay Summary
Many studies of children with autism classify children as having intellectual disability (ID) if they have very low scores on intelligence tests, without considering their adaptive functioning, which are the skills needed for activities of daily living, social interaction, and communication. However, impairments in both intellectual and adaptive functioning are required for an ID diagnosis. We found that when both IQ and adaptive functioning are used to define ID, the percent of children with autism classified as having co-occurring ID is reduced from 63% to 38%, and racial and ethnic differences are reduced. This analysis demonstrated the importance of considering adaptive functioning when describing the frequency of ID in children with autism, including for the accurate and equitable characterization of diverse populations.
INTRODUCTION
Autism spectrum disorder (ASD) and intellectual disability (ID) are two distinct but commonly co-occurring forms of neurodevelopmental disability (American Psychiatric Association, 2013). According to recent epidemiologic data from the Centers for Disease Control and Prevention’s (CDC) Autism and Developmental Disabilities Monitoring (ADDM) Network, the frequency of co-occurring ID in children with autism was estimated to be 48.5% at age 4 years, 37.9% at age 8 years, and 36.6% at age 16 years (Hughes et al., 2023; Maenner et al., 2023; Shaw et al., 2023). The ADDM Network and other epidemiologic studies of ASD in the United States (US) have consistently found that the proportion of children with co-occurring ID varies across racial and ethnic groups and is significantly higher among non-Hispanic (NH) Black and, less frequently, among Hispanic children than among NH White children with autism (ADDM Network Surveillance Year 2010 Principal Investigators, 2014; Baio et al., 2018; Christensen et al., 2018; Constantino et al., 2020; Hewitt et al., 2016; Maenner et al., 2020; Maenner et al., 2023; Shaw et al., 2023; Van Naarden Braun et al., 2015). These disparities in ID prevalence mirror those seen in children without autism (Patrick et al., 2021; Van Naarden Braun et al., 2015). The increased ID prevalence in minoritized populations occurs in the context of historical racism and accompanying socioeconomic disadvantage, which is a leading risk factor for ID globally and disproportionately affects Black and Hispanic children in the US (Beech et al., 2021; Durkin & Yeargin-Allsopp, 2018; Emerson, 2007; Patrick et al., 2021). The elevated prevalence of ID in minoritized groups may also be related to racial, linguistic, and cultural biases in the diagnostic process and cognitive testing instruments (Dahl et al., 2023; Fisher et al., 2023; Gonthier, 2022; Guthrie et al., 2019; Kalb et al., 2022; Lozano-Ruiz et al., 2021; Mandell & Novak, 2005) as well as stigma surrounding ID diagnoses (Fisher et al., 2023; Mitter et al., 2019), and disparities in early identification and referral for services (Guthrie et al., 2019).
Observed racial and ethnic disparities in the frequency of co-occurring ID among children with ASD in population-based data could also be due in part to how ID is defined in epidemiologic studies of ASD. Whereas widely accepted definitions of ID require significant deficits in both intelligence (e.g., intelligence quotient [IQ] scores) and adaptive behavior scores (American Association on Intellectual and Developmental Disabilities, n.d.; American Psychiatric Association, 2013), most population-based epidemiologic estimates of co-occurring ID in children with autism use the criterion of an IQ score two or more standard deviations (SD) below the population mean without considering adaptive scores (CDC, 2023; Fombonne, 2003; Fombonne, 2009; Hughes et al., 2023; Maenner et al., 2021; Zeidan et al., 2022), often because adaptive test scores are less likely to be available for review in children’s health and education records than IQ scores. This practice is applied not only to school-aged children (e.g., Hughes et al., 2023; Maenner et al., 2021), but also to epidemiologic studies of preschool-aged children with autism (e.g., Shaw et al., 2023), whose cognitive scores often improve over time, especially after participation in intensive early intervention programs and therapies (Dawson et al., 2010).
Early studies of the impact of considering adaptive behavior in the definition of ID (Heber, 1961; Leonard & Wen, 2002; Reschly & Ward, 1991; Witt & Martens, 1984) showed that the addition of the adaptive behavior score criterion lowered the number of children meeting ID criteria by as much as 80% (Childs, 1982) and narrowed disparities in ID prevalence between different racial and ethnic groups (Fisher, 1977; Heflinger et al., 1987; Mascari & Forgnone, 1982; Scott, 1979). Conversely, a more recent population-based study examining the effects of incorporating an adaptive behavior criterion for ID surveillance concluded that the impact on estimated ID prevalence was small and that using IQ alone was sufficient for measuring ID prevalence in population studies (Obi et al., 2011). These previous studies were not limited to and may not have included children with autism. Considering adaptive functioning may be especially important for identifying ID in children with autism because of the well-documented gaps between cognitive and adaptive functioning in this population, which have been reported in children as young as preschool and increase with age in cross-sectional studies (Alvares et al., 2020; Duncan & Bishop, 2015; Kanne et al., 2011; Matthews et al., 2015; McQuaid et al., 2021; Pathak et al., 2019; Perry et al., 2009; Tillmann et al., 2019). Some children with cognitive scores below the cutoff for ID may have no significant adaptive delays or impairments and thus not meet diagnostic criteria for ID (Furnier et al., 2023; Pathak et al., 2019). Additionally, studies looking at cognitive testing in young children have found that testability can be problematic in children with autism, resulting in underestimation of their cognitive ability by some commonly used cognitive tests, such as the Mullen Scales of Early Learning (MSEL) (Akshoomoff, 2006; Courchesne et al., 2019; Nader et al., 2016). Thus, the salience of the adaptive behavior criterion for ID classification may emerge early.
The purpose of this study was to describe the impact of using both IQ and adaptive behavior scores versus IQ scores alone in estimating the prevalence of co-occurring ID in an epidemiologic study of young children with autism. Although we recognize in clinical practice ID is not typically diagnosed in preschool children due to the instability of cognitive scores, our goal was to take advantage of comprehensive data available from a large population-based sample of preschool children to evaluate the impact of including both IQ and adaptive scores versus IQ scores alone in describing the percentage with co-occurring ID. We hypothesized that (1) defining ID based on having both cognitive (IQ) and adaptive behavior scores two or more SDs below the mean will result in a substantial reduction of estimated prevalence of co-occurring ID compared to estimates based only on cognitive scores below that threshold; and (2) incorporating an adaptive behavior criterion to classify ID will result in a greater reduction in estimated prevalence of co-occurring ID for NH Black and Hispanic children with autism than for NH White children with autism, reducing racial and ethnic disparity in the estimated co-occurrence of ID among children with autism.
METHODS
Study sample
Our study sample included 3264 children aged2–5 years with a research or community diagnosis of ASD from phases 1–3 of the Study to Explore Early Development (SEED), a large case–control study. Children with and without prior ASD diagnoses were identified through health, education, early intervention, and other service programs at study sites in eight states (California, Colorado, Georgia, Maryland, Missouri, North Carolina, Pennsylvania, and Wisconsin). Eligible children were born and continued to reside when first contacted by SEED study staff in the geographic catchment area between September 2003–August 2006 (phase 1), January 2008–December 2011 (phase 2), or March 2017–March 2020 (phase 3), and had lived with a caregiver since the age of 6 months who was at least 18 years of age and fluent in English or Spanish. The study was approved by Institutional Review Boards at the CDC and every SEED site. Written informed consent was obtained from every participating family.
Caregivers completed the Childhood Behavior Checklist (CBCL) (Achenbach & Rescorla, 2000). Children with a prior ASD diagnosis or a Social Communication Questionnaire (Rutter, Bailey, & Lord, 2003b; Rutter, Le Couteur, & Lord, 2003a) score ≥11 were administered the Autism Diagnostic Observation Schedule (ADOS; Lord et al., 1999; Lord et al., 2012), and their caregivers completed the Autism Diagnostic Interview-Revised (ADI-R; Lord et al., 1994; Rutter, Le Couteur, & Lord, 2003a; Rutter, Bailey, & Lord, 2003b) as well as Vineland Adaptive Behavior Scales, Second Edition (VABS-II; Sparrow et al., 2005). The (MSEL; Mullen, 1995) was administered to participating children at an in-person clinical assessment. Final ASD classification was based on results of the ADOS or ADOS, 2nd Edition and the ADI-R, and for children with an early learning age equivalent less than 24 months, clinical judgment (Schendel et al., 2012; Wiggins et al., 2015).
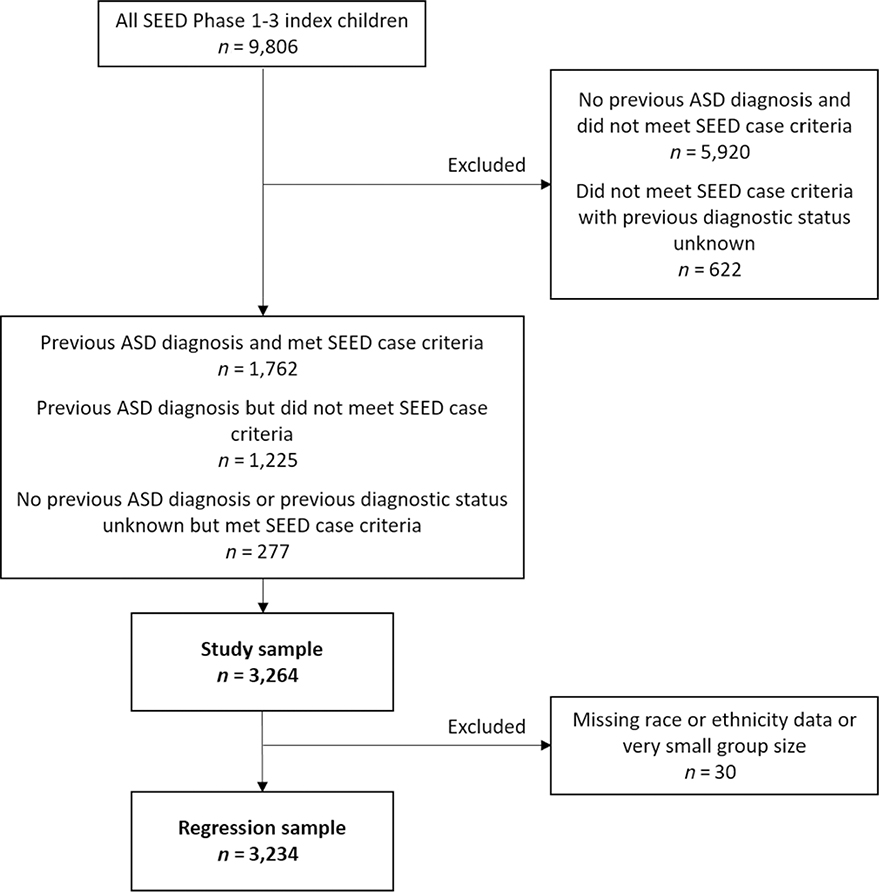
Inclusion criteria for this analysis were meeting SEED ASD criteria or having a previous ASD diagnosis, and for regression analysis, having race and ethnicity information (Figure 1). Distributions of key test scores and model covariates in our sample, overall and broken down by child’s race and ethnicity, are shown in Table 1. Our sample was 80% male with a mean age at in-person assessment of 4.6 (range: 2.4–5.8) years (Table 1). The majority of children were from households with a current income above the federal poverty level (76%), and a plurality had mothers with a college or advanced degree (45%). Socioeconomic indicators varied by race and ethnicity (Tables 1 ).
FIGURE 1.
Selection of the final study sample, Study to Explore Early Development (SEED) Phases 1–3. ASD, autism spectrum disorder.
TABLE 1.
Selected child, maternal, and sociodemographic characteristics of children with autism spectrum disorder (ASD) in the Study to Explore Early Development (SEED) phases 1–3, by child’s race & ethnicity; n (column %) given unless otherwise specified.
| Child and family characteristics |
Overall |
Child’s race & ethnicity |
||||
|---|---|---|---|---|---|---|
| Non-Hispanic White |
Non-Hispanic Black |
Hispanic |
Non-Hispanic Asian or Pacific Islander |
Non-Hispanic multiracial |
||
| Total (row percent) | 3264 | 1413 (43) | 729 (22) | 567 (17) | 166 (5) | 359 (11) |
|
| ||||||
| Child’s age at assessment (years) | ||||||
| Mean (standard deviation) | 4.6 (0.7) | 4.5 (0.7) | 4.8 (0.7) | 4.6 (0.7) | 4.8 (0.7) | 4.6 (0.7) |
| Range | 2.4–5.8 | 2.5–5.8 | 2.6–5.8 | 2.7–5.7 | 3.0–5.7 | 2.4–5.7 |
| Missing | 820 (25) | 345 (24) | 190 (26) | 126 (22) | 47 (28) | 86 (24) |
| Child’s sex | ||||||
| Male | 2605 (80) | 1129 (80) | 587 (81) | 439 (77) | 130 (78) | 294 (82) |
| Female | 659 (20) | 284 (20) | 142 (19) | 128 (23) | 36 (22) | 65 (18) |
| Met SEED ASD criteria | ||||||
| Yes | 2039 (62) | 919 (65) | 433 (59) | 355 (63) | 104 (63) | 224 (62) |
| No | 1225 (38) | 494 (35) | 296 (41) | 212 (37) | 62 (37) | 135 (38) |
| Previous ASD diagnosis | ||||||
| Yes | 2987 (92) | 1280 (91) | 665 (91) | 523 (92) | 155 (93) | 335 (93) |
| No | 271 (8) | 130 (9) | 62 (9) | 43 (8) | 11 (7) | 24 (7) |
| Missing | 6 (0) | 3 (0) | 2 (0) | 1 (0) | 0 (0) | 0 (0) |
| Child’s birth order | ||||||
| First born | 1424 (44) | 679 (48) | 247 (34) | 237 (42) | 89 (54) | 162 (45) |
| Second born or later | 1629 (50) | 678 (58) | 400 (55) | 302 (53) | 70 (42) | 169 (47) |
| Missing | 211 (6) | 56 (4) | 82 (11) | 28 (5) | 7 (4) | 28 (8) |
| Autism diagnostic observation schedule calibrated severity score | ||||||
| <4 | 207 (6) | 69 (5) | 57 (8) | 51 (9) | ** | 26 (7) |
| 4–6 | 830 (25) | 367 (26) | 184 (25) | 147 (26) | ** | 103 (29) |
| 7–10 | 1370 (42) | 619 (44) | 288 (40) | 236 (42) | 84 (51) | 139 (39) |
| Missing | 857 (26) | 358 (25) | 200 (27) | 133 (23) | 49 (30) | 91 (25) |
| Childhood behavior checklist total problems T-score | ||||||
| <65 | 1440 (44) | 644 (46) | 323 (44) | 249 (44) | 79 (48) | 143 (40) |
| ≥65 | 1162 (36) | 500 (35) | 253 (35) | 218 (38) | 46 (28) | 142 (40) |
| Missing | 662 (20) | 269 (19) | 153 (21) | 100 (18) | 41 (25) | 74 (21) |
| Current household income, relative to federal poverty threshold | ||||||
| ≤100% | 342 (10) | 59 (4) | 151 (21) | 91 (16) | ** | 37 (10) |
| 101%–200% | 601 (18) | 175 (12) | 191 (26) | 138 (24) | ** | 79 (22) |
| 201%–300% | 469 (14) | 208 (15) | 108 (15) | 84 (15) | 16 (10) | 52 (14) |
| 301%–399% | 426 (13) | 246 (17) | 64 (9) | 63 (11) | 15 (9) | 38 (11) |
| ≥400% | 979 (30) | 572 (40) | 95 (13) | 118 (21) | 90 (54) | 104 (29) |
| Missing | 447 (14) | 153 (11) | 120 (16) | 73 (13) | 26 (16) | 49 (14) |
| Child health insurancea | ||||||
| Private or dual | 1095 (34) | 597 (42) | 152 (21) | 159 (28) | 69 (42) | 118 (33) |
| Public only | 717 (22) | 175 (12) | 276 (38) | 171 (30) | ** | 85 (24) |
| Missing | 1452 (44) | 641 (45) | 301 (41) | 237 (42) | ** | 156 (43) |
| Maternal education | ||||||
| High school graduate or less | 519 (16) | 136 (10) | 153 (21) | 173 (31) | ** | 47 (13) |
| Some college | 964 (30) | 364 (26) | 256 (35) | 197 (35) | 18 (11) | 127 (35) |
| College graduate or advanced degree | 1458 (45) | 788 (56) | 233 (32) | 159 (28) | 124 (75) | 154 (43) |
| Missing | 323 (10) | 125 (9) | 87 (12) | 38 (7) | ** | 31 (9) |
| Paternal education | ||||||
| High school graduate or less | 858 (26) | 253 (18) | 252 (35) | 243 (43) | 12 (7) | 98 (27) |
| Some college | 713 (22) | 308 (22) | 171 (23) | 121 (21) | 13 (8) | 98 (27) |
| College graduate or advanced degree | 1268 (39) | 709 (50) | 167 (23) | 146 (26) | 123 (74) | 123 (34) |
| Missing | 425 (13) | 143 (10) | 139 (19) | 57 (10) | 18 (11) | 40 (11) |
| Maternal age at enrollment (years) | ||||||
| Mean (standard deviation) | 35.0 (5.8) | 35.8 (5.3) | 34.1 (6.4) | 33.8 (6.0) | 35.9 (4.7) | 35.1 (6.1) |
| Range | 18.0–52.0 | 18.0–52.0 | 19.0–51.0 | 20.0–52.0 | 22.0–48.0 | 21.0–52.0 |
| Missing | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Primary language spoken in the home | ||||||
| English | 2631 (81) | 1263 (89) | 616 (84) | 357 (63) | 72 (43) | 320 (89) |
| Other | 314 (10) | 26 (2) | 29 (4) | 171 (30) | 79 (48) | ** |
| Missing | 319 (10) | 124 (9) | 84 (12) | 39 (7) | 15 (9) | ** |
| Mother born outside the United States | ||||||
| Yes | 569 (17) | 82 (6) | 85 (12) | 217 (38) | 129 (78) | 56 (16) |
| No | 2376 (73) | 1208 (85) | 558 (77) | 312 (55) | 22 (13) | 273 (76) |
| Missing | 319 (10) | 123 (9) | 86 (12) | 38 (7) | 15 (9) | 30 (8) |
| Study site | ||||||
| California | 389 (12) | 99 (7) | 19 (3) | 132 (23) | 77 (46) | 59 (16) |
| Colorado | 499 (15) | 250 (18) | ** | 182 (32) | ** | 53 (15) |
| Georgia | 662 (20) | 171 (12) | 297 (41) | 82 (14) | 29 (17) | 65 (18) |
| Maryland | 502 (15) | 246 (17) | 140 (19) | 38 (7) | 17 (10) | 55 (15) |
| Missouri | 172 (5) | 102 (7) | 29 (4) | 14 (2) | ** | 27 (8) |
| North Carolina | 510 (16) | 281 (20) | 118 (16) | 50 (9) | 14 (8) | 45 (13) |
| Pennsylvania | 394 (12) | 177 (13) | 113 (16) | 52 (9) | 17 (10) | 34 (9) |
| Wisconsin | 136 (4) | 87 (6) | ** | 17 (3) | ** | 21 (6) |
| Mullen Scales of Early Learning | ||||||
| Early learning composite | ||||||
| Mean (standard deviation) | 67.6 (20.0) | 71.8 (21.4) | 61.8 (16.3) | 64.8 (18.6) | 66.5 (19.9) | 67.8 (19.5) |
| Range | 20.0–132.0 | 49.0–132.0 | 49.0–117.0 | 49.0–132.0 | 49.0–130.0 | 49.0–121.0 |
| Missing | 884 (27) | 382 (27) | 199 (27) | 133 (23) | 49 (30) | 95 (26) |
| Visual reception T-score | ||||||
| Mean (standard deviation) | 35.3 (15.4) | 38.1 (16.1) | 30.6 (13.2) | 34.0 (14.7) | 34.7 (15.5) | 35.8 (15.4) |
| Range | 20.0–80.0 | 20.0–80.0 | 20.0–79.0 | 20.0–79.0 | 20.0–80.0 | 20.0–74.0 |
| Missing | 829 (25) | 348 (25) | 192 (26) | 127 (22) | 48 (29) | 88 (25) |
| Vineland Adaptive Behavior Scales, Second Edition | ||||||
| Adaptive behavior composite | ||||||
| Mean (standard deviation) | 73.8 (13.4) | 75.4 (13.5) | 71.9 (13.0) | 72.5 (13.8) | 73.2 (13.3) | 73.3 (12.5) |
| Range | 38.0–122.0 | 39.0–114.0 | 38.0–108.0 | 38.0–114.0 | 46.0–108.0 | 44.0–122.0 |
| Missing | 831 (25) | 341 (24) | 192 (26) | 138 (24) | 46 (28) | 88 (25) |
| Communication | ||||||
| Mean (standard deviation) | 77.8 (17.6) | 81.2 (17.6) | 73.8 (17.1) | 74.3 (17.4) | 79.2 (17.4) | 77.6 (16.4) |
| Range | 34.0–131.0 | 36.0–131.0 | 36.0–116.0 | 34.0–112.0 | 40.0–118.0 | 40.0–118.0 |
| Missing | 809 (25) | 333 (24) | 189 (26) | 130 (23) | 45 (27) | 86 (24) |
| Socialization | ||||||
| Mean (standard deviation) | 73.3 (12.9) | 74.6 (13.1) | 72.5 (12.2) | 72.6 (13.2) | 69.4 (13.9) | 72.8 (12.1) |
| Range | 22.0–132.0 | 22.0–112.0 | 48.0–108.0 | 44.0–114.0 | 44.0–112.0 | 48.0–132.0 |
| Missing | 811 (25) | 335 (24) | 189 (26) | 130 (23) | 45 (27) | 86 (24) |
| Daily living skills | ||||||
| Mean (standard deviation) | 75.3 (15.0) | 76.5 (15.2) | 73.9 (14.3) | 74.9 (15.5) | 74.5 (15.0) | 74.9 (14.3) |
| Range | 34.0–121.0 | 38.0–121.0 | 40.0–121.0 | 36.0–119.0 | 41.0–105.0 | 34.0–111.0 |
| Missing | 809 (25) | 333 (24) | 189 (26) | 130 (23) | 45 (27) | 86 (24) |
Note: Small cell sizes were suppressed to preserve participant anonymity.
Variable was not available for SEED Phase 1.
Child’s race and ethnicity
Maternal and paternal self-reported race and ethnicity were obtained from a maternal interview or, if not available from the interview, linked birth records, and children’s race and ethnicity were derived from parental values. Categories included Hispanic, NH White, NH Black or African American, NH Asian or Pacific Islander (“HHS implementation guidance”, 2011). Children with parents with different racial and ethnic identities or whose parents themselves indicated they were multiracial were included in a NH multiracial category. If either parent self-reported Hispanic ethnicity, the child was classified as Hispanic. If both parents’ racial classifications matched, the child was assigned the same classification. Finally, if one parent was missing a race and ethnicity classification, the child’s race was classified based on the non-missing parent’s classification.
Our final study sample was 1413 (43%) NH White, 729 (22%) NH Black, 567 (17%) Hispanic, 359 (11%) NH multiracial, and 166 (5%) NH Asian or Pacific Islander children. NH American Indian or Native Alaskan children were not included in regression analyses due to very small sample size, but they were included in the overall group in all other analyses, as were children who had no race and ethnicity recorded.
Estimates of intellectual disability
Because of the young age of our sample, we used cognitive ability as measured by the MSEL (Mullen, 1995), a standardized assessment that measures early learning in young children up to 68 months of age, to represent IQ for alternative ID prevalence estimates in our study. The MSEL produces an Early Learning Composite (ELC) score (mean 100, SD 15) as well as visual reception (VR), fine motor, expressive language, and receptive language subscale T-scores (mean 50, SD 10).
Adaptive ability was measured using the VABS-II, a semi-structured interview administered by a clinician to caregivers to gauge a child’s current behavior. Domains included in the VABS-II are communication, socialization, daily living skills, and motor skills. The adaptive behavior composite is derived from the domain scores and represents overall adaptive ability. For the composite and each domain score, we used standard scores (mean 100, SD 15).
We used two approaches to characterize cognitive functioning and describe co-occurring ID (Table 2): one based on cognitive scores alone, as is frequently done in epidemiologic studies of autism, and one based on both cognitive and adaptive scores, in accordance with ID diagnostic criteria. Separate definitions were based on either the MSEL ELC or the VR score as a proxy of non-verbal cognitive ability. Use of VR scores may avoid underestimating communication abilities by accounting for temporary language delays, which might be present in preschool-aged children but eventually resolve with intervention or maturation (Ellis Weismer et al., 2021); for this reason, for our VR-based estimates of cognitive functioning, we focused on the VABS-II daily living skills and socialization domains. For the adaptive behavior criterion, we incorporated measures of the conceptual, social, and practical adaptive skill domains described in the AAIDD and Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) definitions of ID through use of the VABS-II composite, communication, daily living skills, and socialization scores (American Association on Intellectual and Developmental Disabilities, n.d.; American Psychiatric Association, 2013). Because the DSM-5 definition of ID requires impairments in only one or more of the adaptive domains, we included definitions of ID that included impairments in only communication, daily living skills, or socialization (Table 2, Estimates 3 and 6) (Papazoglou et al., 2014). Finally, for every score, we utilized a score cutoff of two or more SDs below the population mean, resulting in the following six estimates of ID.
TABLE 2.
Definitions of intellectual disability, including formal diagnostic definitions from the American Association of Intellectual and Developmental Disabilities (AAIDD) and the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) and present study-specific definitions incorporating the Mullen Scales of Early Learning (MSEL) and Vineland Adaptive Behavior Scales, Second Edition (VABS-II).
| Source | Definition | |
|---|---|---|
|
| ||
| AAIDDa | “Intellectual disability is a condition characterized by significant limitations in both intellectual functioning and adaptive behavior that originates before the age of 22.” | |
| DSM-5b | “Intellectual disability…is a disorder with onset during the developmental period that includes both intellectual and adaptive functioning deficits in conceptual, social, and practical domains.” | |
|
| ||
| Present Study | Cognitive Criterion | Adaptive Criterion |
|
| ||
| 1 | MSEL early learning composite ≤70 | None |
| 2 | MSEL early learning composite ≤70 | VABS-II adaptive behavior composite ≤70 |
| 3 | MSEL early learning composite ≤70 | VABS-II communication, daily living skills, and/or socialization ≤70 |
| 4 | MSEL visual reception T-score ≤ 30 | None |
| 5 | MSEL visual reception T-score ≤ 30 | VABS-II adaptive behavior composite ≤70 |
| 6 | MSEL visual reception T-score ≤ 30 | VABS-II daily living skills and/or socialization ≤70 |
Statistical analysis
To examine the effect of incorporating an adaptive behavior criterion on the percentage of children considered to have co-occurring ID, we estimated this percentage, with 95% Wald confidence intervals (CI), for all six definitions of ID overall and stratified by child’s race and ethnicity. To determine if the addition of an adaptive criterion reduced racial and ethnic disparities in the percentage of children meeting ID criteria, we also calculated both unadjusted and adjusted odds ratios (OR) and 95% CIs using multiple logistic regression. We controlled for potential confounders based on previous literature and identification of variables univariately associated with meeting ID criteria and with child’s race and ethnicity in our study sample, which included child’s birth order, current household income relative to the federal poverty level, current maternal and paternal education, study site, CBCL total T-score, ADOS calibrated severity score (Gotham et al., 2009), and primary language spoken in the home. We considered other factors which past research suggests are associated with having co-occurring ID, such as child’s sex and low birth weight, but did not include them in the adjusted models because they were not associated with either child’s race and ethnicity or meeting ID criteria in our observed data. To further examine whether relationships between cognitive and adaptive scores differed by race and ethnicity, we also calculated Spearman correlations between MSEL and VABS-II scores within each racial and ethnic group; 95% CIs were calculated using the standard error formula proposed by Bonett and Wright (2000). Correlations were compared using Z-tests with NH White as the reference group.
Statistical analyses were performed using SAS Version 9.4 (SAS Institute Inc., 2010). Statistical precision was limited for the NH Asian or Pacific Islander and NH multiracial groups due to smaller sample sizes, but we included these groups in an exploratory analysis.
To account for missing covariates and missing test scores, we performed multiple imputation using the mice package in R version 4.2.2 (R Core Team, 2022; van Buuren & Groothuis-Oudshoorn, 2011), which utilizes a chained equations approach and allows the user to specify the type of regression model used for imputation of each variable (e.g., logistic regression may be specified for imputation of a binary variable). We performed 50 imputations, and imputation models included all model variables as well as auxiliary variables that were associated with model variables. More details on the imputation procedure, missingness, and auxiliary variables are available in the Supplementary Materials (Tables S1–S3). The percentage of children meeting ID criteria, ORs, and Spearman correlation coefficients were then estimated in each of the 50 imputed datasets, and the results were pooled using the PROC MIANALYZE SAS procedure to produce estimates and 95% CIs that accounted for both within- and between-imputation variance. Results from complete case analysis as well as a sensitivity analysis including only individuals with non-imputed test scores are available in the Supplementary Materials (Table S8, Figures S1–S5).
RESULTS
Percentage of children with ASD who would be classified as having co-occurring ID under different approaches
MSEL early learning composite
More than 60% of children with ASD had MSEL composite scores that were at least two SDs below the mean (62.9% [95% CI: 61.1%–64.7%]). Addition of adaptive criteria reduced the overall percentage classified as having co-occurring ID, to 38.0% (95% CI: 36.2%–39.8%) using both MSEL composite and the VABS-II composite scores, and to 45.0% (95% CI: 43.1%–46.9%) using an MSEL composite and VABS-II domain scores (Table 3).
TABLE 3.
The percentage of children with autism meeting intellectual disability (ID) criteria under six classifications of ID in the Study to Explore Early Development phases 1–3, overall and by child’s race and ethnicity.
| n | Intellectual disability Percentagea Estimate (95% confidence interval) |
|||
|---|---|---|---|---|
| MSEL score only |
MSEL score & VABS-II composite criterion |
MSEL score & VABS-II domains criterion |
||
| Est (95% CI) | Est (95% CI) | Est (95% CI) | ||
|
| ||||
| MSEL early learning composite | ||||
| Overall | 3264 | 62.9 (61.1–64.7) | 38.0 (36.2–39.8) | 45.0 (43.1–46.9) |
| Child’s race & ethnicity | ||||
| NH White | 1413 | 54.3 (51.4–57.2) | 32.5 (29.8–35.2) | 38.6 (35.7–41.4) |
| NH Black | 729 | 74.9 (71.4–78.5) | 44.8 (40.9–48.8) | 52.7 (48.7–56.6) |
| Hispanic | 567 | 68.6 (64.4–72.8) | 41.9 (37.3–46.5) | 49.9 (45.3–54.4) |
| NH Asian or Pacific Islander | 166 | 64.5 (55.8–73.2) | 41.3 (32.5–50.1) | 48.3 (39.3–57.3) |
| NH Multiracial | 359 | 61.8 (56.3–67.2) | 37.2 (31.8–42.5) | 44.7 (39.0–50.4) |
| MSEL visual reception T-score | ||||
| Overall | 3264 | 48.7 (46.8–50.6) | 33.6 (31.8–35.4) | 36.3 (34.5–38.1) |
| Child’s race & ethnicity | ||||
| NH White | 1413 | 41.3 (38.4–44.2) | 28.2 (25.6–30.8) | 30.9 (28.3–33.6) |
| NH Black | 729 | 60.9 (56.9–64.8) | 41.7 (37.8–45.5) | 43.7 (39.7–47.7) |
| Hispanic | 567 | 51.1 (46.6–55.6) | 35.6 (31.2–40.0) | 38.8 (34.4–43.2) |
| NH Asian or Pacific Islander | 166 | 50.2 (41.2–59.1) | 37.6 (29.0–46.1) | 41.7 (33.0–50.4) |
| NH Multiracial | 359 | 47.6 (41.9–53.4) | 32.2 (27.0–37.4) | 34.9 (29.6–40.3) |
Abbreviations: CI, confidence interval; Est, estimate; ID, intellectual disability; MSEL, Mullen Scales of Early Learning; NH, Non-Hispanic; VABS-II, Vineland
Adaptive Behavior Scales, Second Edition.
Estimates are from multiply imputed data.
The percentages of children with ASD and MSEL composite scores at least two SDs below the mean were significantly higher for NH Black children (74.9% [95% CI: 71.4%–78.5%]) and Hispanic children (68.6% [95% CI: 64.4%–72.8%]) relative to NH White children (54.3% [95% CI: 51.4%–57.2%]) (Table 3). The largest absolute reduction in the percentage classified as having co-occurring ID after adding the VABS-II composite criterion was for NH Black children (30.1 percentage points), followed by Hispanic (26.7), NH multiracial (24.6), NH Asian or Pacific Islander (23.2), and NH White (21.8) children (Table 3). The pattern was similar using the VABS-II communication/daily living skills/socialization domains criterion, though reductions were smaller (Table 3).
MSEL visual reception T-score
Compared to using MSEL composite scores, using MSEL VR T-scores resulted in a lower percentage of children with scores at least two SD below the population mean (48.7% [95% CI: 46.8%–50.6%]) (Table 3). Addition of adaptive criteria reduced the overall percentage of children with ASD classified as having co-occurring ID to 33.6% (95% CI: 31.8%–35.4%) using the VABS-II composite criterion and 36.3% (95% CI: 34.5%–38.1%) using the daily living skills/socialization domains criterion. The percentages with MSEL VR T-scores below the threshold for ID were greater for NH Black children (60.9% [95% CI: 56.9%–64.8%]) and Hispanic children (51.1% [95% CI: 46.6%–55.6%]) relative to NH White children (41.3% [95% CI: 38.4%–44.2%]) (Table 3), and patterns were similar using the VABS-II domain scores (Table 3).
Variations in the odds of co-occurring ID by race and ethnicity
MSEL early learning composite
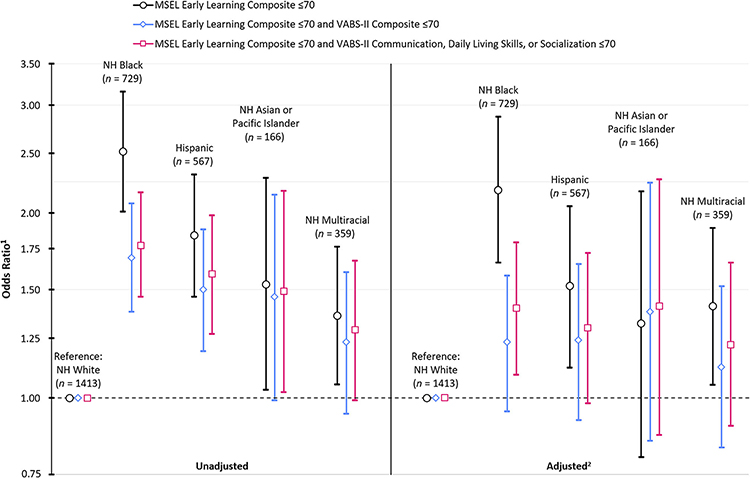
In unadjusted analysis, relative to NH White children, all other racial and ethnic groups had significantly higher odds of a co-occurring ID classification based on MSEL composite scores only, with ORs ranging from 1.36 (95% CI: 1.05–1.76) for NH multiracial children to 2.52 (95% CI: 2.01–3.15) for NH Black children. These ORs were reduced although still elevated after addition of either the VABS-II composite or domains criteria with the largest reductions for NH Black and Hispanic children (Figure 2).
FIGURE 2.
Association between child’s race and ethnicity and meeting intellectual disability criteria under three classifications of intellectual disability incorporating the Mullen Scales of Early Learning (MSEL) Early Learning Composite and Vineland Adaptive Behavior Scales, Second Edition (VABS-II), scores in children with autism in the Study to Explore Early Development phases 1–3. 1Estimates are from multiply imputed data. 2Adjusted for: child’s birth order, current household income relative to the federal poverty level, current maternal and paternal education, study site, childhood behavior checklist total T-score, autism diagnostic observation schedule calibrated severity score, and the primary language spoken in the home. MSEL, Mullen Scales of Early Learning; NH, Non-Hispanic; VABS-II, Vineland Adaptive Behavior Scales, Second Edition.
The observed racial and ethnic disparities in the percentage of children meeting ID was reduced after adjustment for potential confounders, and they were further reduced with the addition of the adaptive criteria (Figure 2). NH Black (OR 2.18 [95% CI: 1.66–2.87]) and Hispanic (OR 1.52 [95% CI: 1.12–2.05]) children had significantly higher odds of meeting the MSEL composite-only ID criterion relative to NH White children. However, with the addition of the VABS-II composite criterion, no racial or ethnic group had significantly higher odds of meeting ID criteria relative to NH White children (NH Black OR 1.23 [95% CI: 0.95–1.58]; Hispanic OR 1.24 [95% CI: 0.92–1.65]; NH Asian or Pacific Islander OR 1.38 [95% CI: 0.85–2.24]; NH multiracial OR 1.12 [95% CI: 0.83–1.52]), although all point estimates were higher than one. Using the communication/daily living skills/socialization domains criterion, only NH Black (OR 1.40 [95% CI: 1.09–1.79]) children had significantly higher odds of meeting ID criteria than NH White children, but these disparities were also reduced relative to those observed when ID was measured by the MSEL composite only (Figure 2).
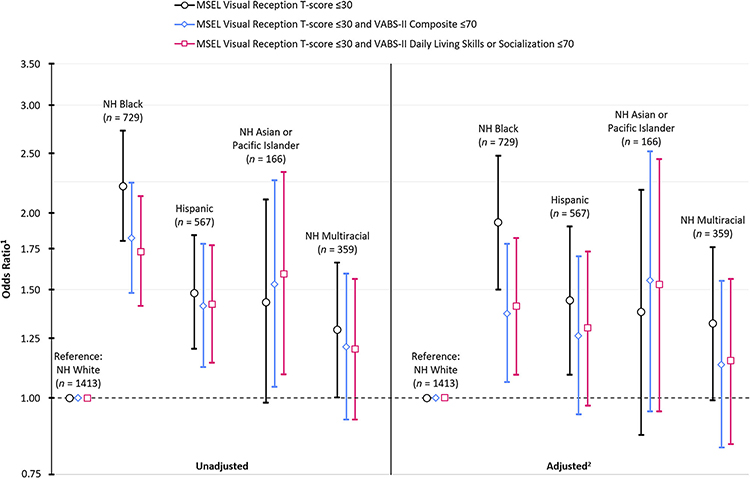
MSEL VR T-score
In unadjusted regression analysis, relative to NH White children, NH Black (OR 2.21 [95% CI: 1.80–2.72]), Hispanic (OR 1.48 [95% CI: 1.20–1.84]), and NH multiracial (OR 1.29 [95% CI: 1.00–1.66]) children had significantly higher odds of meeting MSEL VR T-score-only ID criteria, and these disparities remained significant for NH Black and Hispanic children after addition of either the VABS-II composite or domain criteria (Figure 3). The borderline statistically significantly increased odds of ID for NH Asian or Pacific Islander relative to NH white children increased slightly after addition of the adaptive criteria (OR 1.53 [95% CI: 1.04–2.26] for the composite criterion; OR 1.59 [95% CI: 1.09–2.33] for the domain criterion) (Figure 3).
FIGURE 3.
Association between child’s race and ethnicity and meeting intellectual disability criteria under three classifications of intellectual disability incorporating the Mullen Scales of Early Learning (MSEL) Visual Reception T-score and Vineland Adaptive Behavior, Second Edition (VABS-II), scores in children with autism in the Study to Explore Early Development phases 1–3. 1Estimates are from multiply imputed data. 2Adjusted for: child’s birth order, current household income relative to the federal poverty level, current maternal and paternal education, study site, Childhood Behavior Checklist Total T-score, Autism Diagnostic Observation Schedule calibrated severity score, and the primary language spoken in the home. MSEL: Mullen Scales of Early Learning; NH, Non-Hispanic; VABS-II: Vineland Adaptive Behavior Scales, Second Edition.
In adjusted analysis, NH Black (OR 1.93 [95% CI: 1.50–2.48]) and Hispanic (OR 1.44 [95% CI: 1.09–1.90]) children had significantly higher odds of meeting the MSEL VR T-score-only ID criterion relative to NH White children. After incorporating VABS-II criteria, NH Black children still had significantly higher odds of meeting ID criteria relative to NH White children (OR 1.37 [95% CI: 1.06–1.78] for the VABS-II composite criterion; OR 1.41 [95% CI: 1.09–1.82] for the VABS-II daily living skills/socialization criterion), although point estimates were reduced relative to MSEL VR T-score-only estimates (Figure 3).
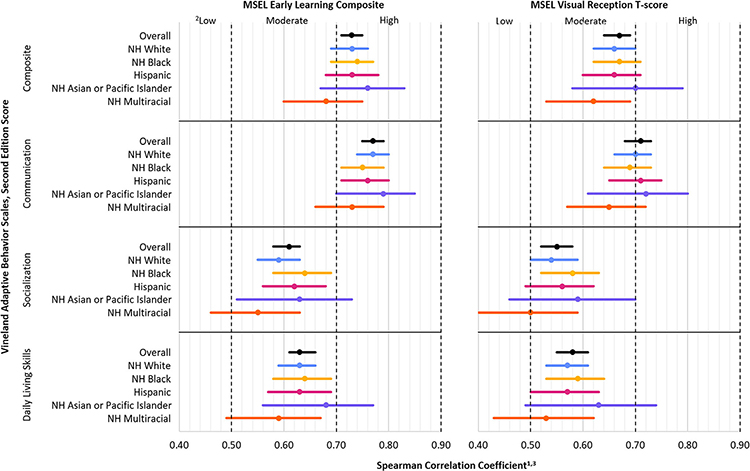
Correlation analysis
Spearman correlation coefficients between MSEL and VABS-II scores were similar across racial and ethnic groups, regardless of the MSEL or VABS-II score examined (Figure 4), and correlations did not differ significantly from NH White children for any other racial or ethnic group. Correlations were generally stronger for the MSEL ELC than MSEL VR T-scores and were stronger between MSEL and VABS-II communication scores than other domains, overall and within each racial and ethnic group.
FIGURE 4.
Spearman correlations (with 95% confidence intervals)1 between Mullen Scales of Early Learning (MSEL) and Vineland Adaptive Behavior Scales, Second Edition (VABS-II), scores in children with autism in the Study to Explore Early Development phases 1–3, overall and by child’s race and ethnicity. 1Estimates are from multiply imputed data. 2Interpretation of correlation strength taken from Mukaka (2012). 3No correlations were statistically significantly different from correlations in NH White children at p < .05. MSEL, Mullen Scales of Early Learning; NH, Non-Hispanic; VABS-II, Vineland Adaptive Behavior Scales, Second Edition.
DISCUSSION
The addition of an adaptive functioning criterion substantially reduced the percentage of children with ASD classified as having co-occurring ID relative to defining ID based only on cognitive scores; the estimated percentage of children who were classified with co-occurring ID was reduced from over 60% using the MSEL composite-only criterion to 38% when the MSEL composite and VABS-II composite criteria were used. In each racial and ethnic group, the VABS-II composite criterion resulted in larger reductions in the percentage classified with ID than the criterion requiring impairment in only one adaptive domain. These findings are consistent with past research documenting large discrepancies between IQ and adaptive scores in children with autism, with gaps sometimes exceeding one or even two SDs and adaptive scores often exceeding cognitive scores among children with IQ scores within the ID range (Alvares et al., 2020; Bölte & Poustka, 2002; Duncan & Bishop, 2015; Furnier et al., 2023; Kanne et al., 2011; Klin et al., 2007; Saulnier & Klin, 2007). These findings suggest epidemiologic studies of co-occurring ID in children with autism based on IQ alone likely overestimate the prevalence of co-occurring ID. Our study focused on young children; the impact of considering adaptive scores might differ for older children, as past research has found a negative association between age and adaptive functioning, potentially resulting in increasing adaptive delays relative to cognitive ability as children age (Alvares et al., 2020; Bradshaw et al., 2019; Kanne et al., 2011; Klin et al., 2007; Pathak et al., 2019).
Consistent with our second hypothesis, addition of an adaptive functioning criterion resulted in larger absolute reductions in the percent of children classified with co-occurring ID for NH Black and Hispanic children than for NH White children. In addition, disparities in the odds of meeting ID criteria in NH Black and Hispanic children relative to NH White children were reduced, although not eliminated, when adaptive score criteria were used. After adjusting for socioeconomic confounders and using both MSEL composite and VABS-II composite scores to define ID, the disparities in estimated ID prevalence were diminished and not significantly different from NH White children for any other racial and ethnic groups. However, point estimates were still elevated, indicating that disparities remained when incorporating the VABS-II domains criteria and using ID definitions based on the MSEL VR T-score.
These findings raise the question of why racial and ethnic disparities in co-occurring ID among children with ASD are not entirely eliminated after controlling for selected socioeconomic factors and incorporating adaptive scores. Extensive racial and ethnic disparities in the US in autism screening and access to autism diagnostic and intervention services (Angell et al., 2018; Čolić et al., 2022; Constantino et al., 2020; Fisher et al., 2023; Guthrie et al., 2019; Magaña et al., 2013; Mandell et al., 2002; Mandell et al., 2007; Mandell et al., 2009; Pham et al., 2022) may explain the persistence of these differences, as exposure to intensive early intervention has been shown to boost IQ with little impact on autism severity (Asta & Persico, 2022; Dawson et al., 2010; Reichow et al., 2018; Shi et al., 2021). Persistence of these disparities might also be explained by disparities within the diagnostic process leading to under-identification of autism in Black and Hispanic children who have cognitive scores in the average or above average range, thereby inflating the proportions with low cognitive scores. Children with autism with cognitive delays may be more likely than children with autism without those delays to be identified early and referred for developmental assessments. Considerable family resources to cover out-of-pocket expenses, time off work, and travel may be required to obtain an autism diagnosis. Such resources are less available to Black relative to White children in the US (Čolić et al., 2022; Liu et al., 2023). Additionally, studies describing the experience of parents of children with autism from underrepresented racial and ethnic groups have found that parents report numerous barriers to having their children evaluated, including long wait times or low availability of service providers, racial and ethnic bias from providers, a lack of serious attention given to their concerns about their child’s behavior or development, and language barriers that limited caregivers’ ability to communicate effectively with their child’s healthcare provider (Čolić et al., 2022; Constantino et al., 2020; Fisher et al., 2023; Zuckerman et al., 2017). All of these factors likely lead to preventable delays in diagnosis and subsequent delays in receipt of early intervention services shown to improve both cognitive scores and adaptive behavior.
Cultural expectations of child behavior and stigma surrounding developmental disabilities may also contribute to delayed identification of autism in certain populations (Fisher et al., 2023; Pham & Charles, 2023; Zuckerman et al., 2018). Studies of parent reports of autism symptoms have found Black parents to be less likely than White parents to report concerns about their children’s social skills or restricted and repetitive behaviors and interests (Azad et al., 2022; Donohue et al., 2019), even after controlling for autism severity (Donohue et al., 2019), and may place more emphasis on behavioral concerns (Mandell et al., 2007). Persistent racial and ethnic disparities in the prevalence of autism with co-occurring ID point to the need for increased access to culturally appropriate autism diagnostic and treatment services (Dababnah et al., 2018) and improved outreach to provide parents the resources to recognize symptoms of ASD (Čolić et al., 2022; Fisher et al., 2023).
Upstream disparities in exposures that are causally associated with ID may also contribute to disparities in rates of co-occurring ID in children with autism. Exposures that have been found to disproportionately affect underserved populations include lead poisoning and other environmental toxins (Carrington et al., 2019; Emerson et al., 2019; Gaylord et al., 2020; Grineski et al., 2022; Thompson et al., 2022) and pre- and perinatal complications (Bilder et al., 2013; Huang et al., 2016; Yeargin-Allsopp et al., 1995). These factors may also contribute to the higher prevalence of ID in NH Black children without autism (Patrick et al., 2021; Van Naarden Braun et al., 2015).
Biases in the instruments used to measure both cognitive and adaptive functioning could also contribute to racial and ethnic disparities in the proportion of children with autism classified as having co-occurring ID. Cultural bias may result from the items included in standardized tests (Gonthier, 2022), nonrepresentative norming samples (Lozano-Ruiz et al., 2021), and differential performance of autism assessment tools across racial and ethnic groups (Dahl et al., 2023; Guthrie et al., 2019; Kalb et al., 2022; Pham & Charles, 2023). Lack of reliable translations of ASD screening and diagnostic tools may complicate the diagnostic process as well and could potentially negatively affect test performance in some groups (Scarpa et al., 2013).
It is also possible that residual or unmeasured confounding contributed to the elevated odds of ID among Black and Hispanic children relative to White children in our adjusted analyses. Although we were able to adjust for household income and parental education, these measures are likely insufficient for capturing the intersectionality of racism and socioeconomic disadvantage in the US (Bowleg, 2012; Hull et al., 2023) and their impacts on cognitive development and adaptive functioning of young children. Further, we had limited information on family, home, or community environment, which have been shown to be associated with cognitive development (Breslau et al., 2001; Tong et al., 2007).
An important limitation of this study is the young age of our study sample. Preschool children are not typically given an ID diagnosis because of IQ instability at this age, although early childhood IQ has been shown to be predictive of adult outcomes among people with autism (Pickles et al., 2020). Despite the young age of the sample, data from the SEED study provides a valuable opportunity to evaluate the impact of considering adaptive scores on racial and ethnic disparities in the classification of ID. Because verbal IQ has been shown to increase significantly with maturation in childhood (Chawarska et al., 2009), it is likely that our sample would exhibit gains in verbal scores as they age and receive intervention services. Although we examined definitions of ID focused on the MSEL VR subscale in an attempt to mitigate the impact of these potentially impermanent communication delays, it is important to note that certain items in the VR subscale, particularly at the older ages, include verbal instructions that accompany examiner gestures and models of the desired response, for example, matching, categorizing, and visual memory. Thus, use of the MSEL VR subscale does not eliminate, but may mitigate, the influence of language difficulties on cognition. Additionally, issues related to the ability of children with autism to complete the MSEL may have also influenced the MSEL scores obtained, potentially underestimating the cognitive ability of our sample (Akshoomoff, 2006; Courchesne et al., 2019). We observed a floor effect in MSEL scores in our sample; among children with an MSEL ELC recorded, 31% obtained the minimum score, whereas among children with a VR T-score recorded, 37% obtained the minimum possible score. Hispanic children whose primary language was Spanish were assessed with measures that were translated into Spanish but have not been normed in this population. Also, children were diagnosed with ASD using the DSM, Fourth Edition, Text Revised, before 2013, and these findings may have differed if we had included only children who were diagnosed with the DSM-5. Missing data were another limitation of our analyses. Although we used multiple imputation to account for this missingness, multiple imputation assumes that the data are missing at random, an assumption which we believe to be reasonable but cannot formally test. However, of note, we saw similar patterns in analyses in complete cases (see Supplementary Materials Table S8, Figures S1–S3) and our multiply imputed data. An additional limitation of this study is that sample sizes for NH Asian or Pacific Islander and NH multiracial children were small, and while we included these groups in analyses for exploratory purposes, we had less power to detect significant differences for these groups.
CONCLUSION
In summary, this study provides evidence for the importance of the adaptive behavior criterion in describing the co-occurrence of ID in children with autism and in evaluating racial and ethnic disparities. Studies that quantify the co-occurrence of ID in children with autism based solely on IQ scores, often due to lack of availability of adaptive test information, likely overestimate this co-occurrence. Accurate estimation of the proportion of children with autism with co-occurring ID may be important for understanding the magnitude and nature of racial, ethnic, and socioeconomic disparities in autism and for addressing these disparities. These findings point to the need for future research into the root causes of racial and ethnic disparities in co-occurring ID and strategies for improving early identification and treatment of children with autism from underserved racial and ethnic groups. Although our findings may be specific to the unique intersection of race and ethnicity, socioeconomic status, and disability in the context of historical racism in the US, they also suggest the need for future research to assess the racial, linguistic, and cultural appropriateness and validity of tools used in diagnosis of both autism and ID. Although the association between low socioeconomic status and ID has been observed across the world (Durkin & Yeargin-Allsopp, 2018; Leonard et al., 2022), less is known from diverse countries about this association among children with autism.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to thank the SEED Data Coordinating Center team at the Clinical and Translational Sciences Institute of Michigan State University for their support. The authors would also like to thank Olivia M. Pokoski for her assistance in data verification. The authors also gratefully acknowledge SEED staff and the children and families who participated in SEED.
FUNDING INFORMATION
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by seventeen cooperative agreements from the Centers for Disease Control and Prevention (CDC): Cooperative Agreement Number U10DD000180, Colorado Department of Public Health, U01DD000750 University of Colorado Denver; Cooperative Agreement Number U10DD000181, Kaiser Foundation Research Institute (CA); Cooperative Agreement Number U10DD000182, University of Pennsylvania; Cooperative Agreement Number U10DD000183, Johns Hopkins University; Cooperative Agreement Number U10DD000184, University of North Carolina at Chapel Hill; Cooperative Agreement Number U10DD000498, Michigan State University; Cooperative Agreement Number U01000750, University of Colorado Denver; Cooperative Agreement Number U01000748, Kaiser Foundation Research Institute (CA); Cooperative Agreement Number U01000752, University of Pennsylvania; Cooperative Agreement Number U01000746, Johns Hopkins University; Cooperative Agreement Number U01000749, University of North Carolina at Chapel Hill; Cooperative Agreement Number U10DD000901, Michigan State University; Cooperative Agreement Number U01DD001210, The Regents of the University of Colorado; Cooperative Agreement Number U01DD001214 and 1U01DD001209, Johns Hopkins University; Cooperative Agreement Number U01DD001205, University of North Carolina at Chapel Hill; Cooperative Agreement Number U01DD001216, Washington University; and Cooperative Agreement Number U01DD001215, University of Wisconsin System and the Waisman Center [Eunice Kennedy Shriver National Institute of Child Health and Human Development grant number U54 HD090256]. SMF received additional funding from the Wisconsin Distinguished Graduate Fellowship awarded by the University of Wisconsin-Madison. These data were independently verified at the University of Wisconsin-Madison. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Footnotes
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
The study was approved by institutional review boards at the Centers for Disease Control and Prevention and every SEED study site. Written informed consent was obtained from every participating family. All procedures performed in SEED were in accordance with ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
SUPPORTING INFORMATION
Additional supporting information can be found online in the Supporting Information section at the end of this article.
DATA AVAILABILITY STATEMENT
Research data are not shared.
REFERENCES
- Achenbach TM, & Rescorla LA (2000). Manual for the ASEBA preschool forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Akshoomoff N (2006). Use of the Mullen scales of early learning for the assessment of young children with autism spectrum disorders. Child Neuropsychology, 12(4–5), 269–277. 10.1080/09297040500473714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvares GA, Bebbington K, Cleary D, Evans K, Glasson EJ, Maybery MT, Pillar S, Uljarević M, Varcin K, Wray J, & Whitehouse AJ (2020). The misnomer of ‘high functioning autism’: Intelligence is an imprecise predictor of functional abilities at diagnosis. Autism, 24(1), 221–232. [DOI] [PubMed] [Google Scholar]
- American Association on Intellectual and Developmental Disabilities. (n.d.). Defining criteria for intellectual disability. AAID. https://www.aaidd.org/intellectual-disability/definition [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association. 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- Angell AM, Empey A, & Zuckerman KE (2018). A review of diagnosis and service disparities among children with autism from racial and ethnic minority groups in the United States. In Hodapp RM & Fidler DJ (Eds.), International Review of Research in Developmental Disabilities (Vol. 55, pp. 145–180). Academic Press. 10.1016/bs.irrdd.2018.08.003 [DOI] [Google Scholar]
- Asta L, & Persico AM (2022). Differential predictors of response to early start Denver model vs. early intensive behavioral intervention in young children with autism spectrum disorder: A systematic review and meta-analysis. Brain Sciences, 12(11), 1499. 10.3390/brainsci12111499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Autism and Developmental Disabilities Monitoring Network Surveillance Year 2010 Principal Investigators. (2014). Prevalence of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2010. Morbidity and Mortality Weekly Report: Surveillance Summaries, 63(2), 1–21. [PubMed] [Google Scholar]
- Azad G, Holingue C, Pfeiffer D, Dillon E, Reetzke R, Kalb L, Menon D, Hong JS, & Landa R (2022). The influence of race on parental beliefs and concerns during an autism diagnosis: A mixed-method analysis. Autism, 26(5), 1176–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baio J, Wiggins L, Christensen DL, Maenner MJ, Daniels J, Warren Z, … Dowling NF (2018). Prevalence of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2014. MMWR Surveillance Summaries, 67(6), 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beech BM, Ford C, Thorpe RJ Jr., Bruce MA, & Norris KC (2021). Poverty, racism, and the public health crisis in America. Frontiers in Public Health, 9, 699049. 10.3389/fpubh.2021.699049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilder DA, Bakian AV, Viskochil J, Clark EAS, Botts EL, Smith KR, Pimentel R, McMahon WM, & Coon H (2013). Maternal Prenatal Weight Gain and Autism Spectrum Disorders. Pediatrics, 132(5), e1276–e1283. 10.1542/peds.2013-1188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bölte S, & Poustka F (2002). The relation between general cognitive level and adaptive behavior domains in individuals with autism with and without co-morbid mental retardation. Child Psychiatry and Human Development, 33, 165–172. [DOI] [PubMed] [Google Scholar]
- Bonett DG, & Wright TA (2000). Sample size requirements for estimating Pearson, Kendall and spearman correlations. Psychometrika, 65(1), 23–28. 10.1007/BF02294183 [DOI] [Google Scholar]
- Bowleg L (2012). The problem with the phrase women and minorities: Intersectionality-an important theoretical framework for public health. American Journal of Public Health, 102(7), 1267–1273. 10.2105/AJPH.2012.300750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradshaw J, Gillespie S, Klaiman C, Klin A, & Saulnier C (2019). Early emergence of discrepancy in adaptive behavior and cognitive skills in toddlers with autism spectrum disorder. Autism, 23(6), 1485–1496. 10.1177/1362361318815662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Chilcoat HD, Susser ES, Matte T, Liang KY, & Peterson EL (2001). Stability and change in children’s intelligence quotient scores: A comparison of two socioeconomically disparate communities. American Journal of Epidemiology, 154(8), 711–717. [DOI] [PubMed] [Google Scholar]
- Carrington C, Devleesschauwer B, Gibb HJ, & Bolger PM (2019). Global burden of intellectual disability resulting from dietary exposure to lead, 2015. Environmental Research, 172, 420–429. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2023). Autism prevalence studies. Centers for Disease Control and Prevention. https://data.cdc.gov/Public-Health-Surveillance/autism-prevalence-studies/9mw4-6adp [Google Scholar]
- Chawarska K, Klin A, Paul R, Macari S, & Volkmar F (2009). A prospective study of toddlers with ASD: short-term diagnostic and cognitive outcomes. Journal of Child Psychology and Psychiatry, 50(10), 1235–1245. Portico. 10.1111/j.1469-7610.2009.02101.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Childs RE (1982). A study of the adaptive behavior of retarded children and the resultant effects of this use in the diagnosis of mental retardation. Education and Training of the Mentally Retarded, 17(2),109–113. [Google Scholar]
- Christensen DL, Braun KVN, Baio J, Bilder D, Charles J, Constantino JN, Daniels J, Durkin MS, Fitzgerald RT, Kurzius-Spencer M, Lee L-C, Pettygrove S, Robinson C, Schulz E, Wells C, Wingate MS, Zahorodny W, & Yeargin-Allsopp M (2018). Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2012. MMWR Surveillance Summaries, 65(13), 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Čolić M, Araiba S, Lovelace TS, & Dababnah S (2022). Black caregivers’ perspectives on racism in ASD services: Toward culturally responsive ABA practice. Behavior Analysis in Practice, 15(4), 1032–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantino JN, Abbacchi AM, Saulnier C, Klaiman C, Mandell DS, Zhang Y, Hawks Z, Bates J, Klin A, Shattuck P, Molholm S, Fitzgerald R, Roux A, Lowe JK, & Geschwind DH (2020). Timing of the diagnosis of autism in African American children. Pediatrics, 146(3), e20193629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courchesne V, Girard D, Jacques C, & Soulières I (2019). Assessing intelligence at autism diagnosis: Mission impossible? Testability and cognitive profile of autistic preschoolers. Journal of Autism and Developmental Disorders, 49, 845–856. 10.1007/s10803-018-3786-4 [DOI] [PubMed] [Google Scholar]
- Dababnah S, Shaia WE, Campion K, & Nichols HM (2018). “We had to keep pushing”: Caregivers’ perspectives on autism screening and referral practices of black children in primary care. Intellectual and Developmental Disabilities, 56(5), 321–336. 10.1352/1934-9556-56.5.321 [DOI] [PubMed] [Google Scholar]
- Dahl E, Moody EJ, Barger B, Rosenberg S, DiGuiseppi C, Fallin MD, … Wiggins L (2023). Differential performance of social communication questionnaire items in African American/Black vs. White children. Journal of Autism and Developmental Disorders. 10.1007/s10803-023-05931-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson G, Rogers S, Munson J, Smith M, Winter J, Greenson J, Donaldson A, & Varley J (2010). Randomized, controlled trial of an intervention for toddlers with autism: The early start Denver model. Pediatrics, 125(1), e17–e23. 10.1542/peds.2009-0958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donohue MR, Childs AW, Richards M, & Robins DL (2019). Race influences parent report of concerns about symptoms of autism spectrum disorder. Autism, 23(1), 100–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan AW, & Bishop SL (2015). Understanding the gap between cognitive abilities and daily living skills in adolescents with autism spectrum disorders with average intelligence. Autism, 19(1), 64–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkin MS, & Yeargin-Allsopp M (2018). Socioeconomic status and pediatric neurologic disorders: Current evidence. Seminars in Pediatric Neurology, 27, 16–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis Weismer S, Rubenstein E, Wiggins L, & Durkin MS (2021). A preliminary epidemiologic study of social (pragmatic) communication disorder relative to autism spectrum disorder and developmental disability without social communication deficits. Journal of Autism and Developmental Disorders, 51, 2686–2696. 10.1007/s10803-020-04737-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emerson E (2007). Poverty and people with intellectual disabilities. Mental Retardation and Developmental Disabilities Research Reviews, 13(2), 107–113. 10.1002/mrdd.20144 [DOI] [PubMed] [Google Scholar]
- Emerson E, Robertson J, Hatton C, & Baines S (2019). Risk of exposure to air pollution among British children with and without intellectual disabilities. Journal of Intellectual Disability Research, 63(2), 161–167. [DOI] [PubMed] [Google Scholar]
- Fisher AP, Lynch JD, Jacquez FM, Mitchell MJ, Kamimura-Nishimura KI, & Wade SL (2023). A systematic review examining caregivers’ of color experiences with the diagnostic process of autism spectrum disorder. Autism, 27(4), 876–889. [DOI] [PubMed] [Google Scholar]
- Fisher AT (1977). Adaptive behavior in non-biased assessment: Effects on special education [Paper presentation]. Annual Convention of the American Psychological Association 1977, San Francisco, CA, United States. [Google Scholar]
- Fombonne E (2003). Epidemiological surveys of autism and other pervasive developmental disorders: An update. Journal of Autism and Developmental Disorders, 33(4), 365–382. [DOI] [PubMed] [Google Scholar]
- Fombonne E (2009). Epidemiology of pervasive developmental disorders. Pediatric Research, 65(6), 591–598. [DOI] [PubMed] [Google Scholar]
- Furnier SM, Ellis Weismer S, Rubenstein E, Gangnon R, Rosenberg S, Nadler C, Wiggins LD, & Durkin MS (2023). Using adaptive behavior scores to convey level of functioning in children with autism spectrum disorder: Evidence from the study to explore early development. Autism. 10.1177/13623613231193194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaylord A, Osborne G, Ghassabian A, Malits J, Attina T, & Trasande L (2020). Trends in neurodevelopmental disability burden due to early life chemical exposure in the USA from 2001 to 2016: A population-based disease burden and cost analysis. Molecular and Cellular Endocrinology, 502, 110666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonthier C (2022). Cross-cultural differences in visuo-spatial processing and the culture-fairness of visuo-spatial intelligence tests: An integrative review and a model for matrices tasks. Cognitive Research: Principles and Implications, 7(1), 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotham K, Pickles A, & Lord C (2009). Standardizing ADOS scores for a measure of severity in autism spectrum disorders. Journal of Autism and Developmental Disorders, 39, 693–705. 10.1007/s10803-008-0674-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grineski SE, Renteria R, Collins TW, Mangadu A, Alexander C, Bilder D, & Bakian A (2022). Associations between estimates of perinatal industrial pollution exposures and intellectual disability in Utah children. Science of the Total Environment, 836, 155630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guthrie W, Wallis K, Bennett A, Brooks E, Dudley J, Gerdes M, … Miller JS (2019). Accuracy of autism screening in a large pediatric network. Pediatrics, 144(4), e20183963. 10.1542/peds.2018-3963 [DOI] [PubMed] [Google Scholar]
- Heber R (1961). Modifications in the manual on terminology and classification in mental retardation. American Journal of Mental Deficiency, 65, 499–500. [PubMed] [Google Scholar]
- Heflinger CA, Cook VJ, & Thackrey M (1987). Identification of mental retardation by the system of multicultural pluralistic assessment: Nondiscriminatory or nonexistent? Journal of School Psychology, 25(2), 177–183. [Google Scholar]
- Hewitt A, Hall-Lande J, Hamre K, Esler AN, Punyko J, Reichle J, & Gulaid AA (2016). Autism spectrum disorder (ASD) prevalence in Somali and non-Somali children. Journal of Autism and Developmental Disorders, 46(8), 2599–2608. [DOI] [PubMed] [Google Scholar]
- HHS implementation guidance on data collection standards for race, ethnicity, sex, primary language, and disability status. ASPE. (2011). Retrieved March 14, 2023, from https://aspe.hhs.gov/reports/hhs-implementation-guidance-data-collection-standards-race-ethnicity-sex-primary-language-disability-0 [Google Scholar]
- Huang J, Zhu T, Qu Y, & Mu D (2016). Prenatal, perinatal and neonatal risk factors for intellectual disability: A systemic review and meta-analysis. PLoS One, 11(4), e0153655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes MM, Shaw KA, Patrick ME, DiRienzo M, Bakian AV, Bilder DA, Durkin MS, Hudson A, Spivey MH, DaWalt LS, Salinas A, Schwenk YD, Lopez M, Baroud TM, & Maenner MJ (2023). Adolescents with autism Spectrum disorder: Diagnostic patterns, co-occurring conditions, and transition planning. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 73(2), 271–278. 10.1016/j.jadohealth.2022.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hull SJ, Massie JS, Holt SL, & Bowleg L (2023). Intersectionality policymaking toolkit: Key principles for an intersectionality-informed policymaking process to serve diverse women, children, and families. Health Promotion Practice, 24(4), 623–635. 10.1177/15248399231160447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalb LG, Singh V, Hong JS, Holingue C, Ludwig NN, Pfeiffer D, Reetzke R, Gross AL, & Landa R (2022). Analysis of race and sex bias in the autism diagnostic observation schedule (ADOS-2). JAMA Network Open, 5(4), e229498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanne SM., Gerber AJ., Quirmbach LM., Sparrow SS., Cicchetti DV., & Saulnier CA. (2011). The role of adaptive behavior in autism spectrum disorders: Implications for functional outcome. Journal of Autism and Developmental Disorders, 41, 1007–1018. 10.1007/s10803-010-1126-4 [DOI] [PubMed] [Google Scholar]
- Klin A, Saulnier CA, Sparrow SS, Cicchetti DV, Volkmar FR, & Lord C (2007). Social and communication abilities and disabilities in higher functioning individuals with autism spectrum disorders: The Vineland and the ADOS. Journal of Autism and Developmental Disorders, 37(4), 748–759. [DOI] [PubMed] [Google Scholar]
- Leonard H, Montgomery A, Wolff B, Strumpher E, Masi A, Woolfenden S, Williams K, Eapen V, Finlay-Jones A, Whitehouse A, Symons M, Licari M, Varcin K, Alvares G, Evans K, Downs J, & Glasson E (2022). A systematic review of the biological, social, and environmental determinants of intellectual disability in children and adolescents. Frontiers in Psychiatry, 13, 926681. 10.3389/fpsyt.2022.926681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard H, & Wen X (2002). The epidemiology of mental retardation: Challenges and opportunities in the new millennium. Mental Retardation and Developmental Disabilities Research Reviews, 8(3), 117–134. [DOI] [PubMed] [Google Scholar]
- Liu BM, Paskov K, Kent J, McNealis M, Sutaria S, Dods O, Harjadi C, Stockham N, Ostrovsky A, & Wall DP (2023). Racial and ethnic disparities in geographic access to autism resources across the US. JAMA Network Open, 6(1), e2251182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, & Risi S (1999). Autism diagnostic observation schedule. Western Psychological Services. [Google Scholar]
- Lord C, Rutter M, DiLavore PC, & Risi S (2012). Autism diagnostic observation schedule (2nd ed.). Western Psychological Services. [Google Scholar]
- Lord C, Rutter M, & Le Couteur AL (1994). Autism diagnostic interview-revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders, 24(5), 659–685. [DOI] [PubMed] [Google Scholar]
- Lozano-Ruiz A, Fasfous AF, Ibanez-Casas I, Cruz-Quintana F, Perez-Garcia M, & Pérez-Marfil MN (2021). Cultural bias in intelligence assessment using a culture-free test in Moroccan children. Archives of Clinical Neuropsychology, 36(8), 1502–1510. [DOI] [PubMed] [Google Scholar]
- Maenner MJ, Shaw KA, & Baio J (2020). Prevalence of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2016. MMWR Surveillance Summaries, 69(4), 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maenner MJ, Shaw KA, Bakian AV, Bilder DA, Durkin MS, Esler A, Furnier SM, Hallas L, Hall-Lande J, Hudson A, Hughes MM, Patrick M, Pierce K, Poynter JN, Salinas A, Shenouda J, Vehorn A, Warren Z, Constantino JN, & Cogswell ME (2021). Prevalence of autism spectrum disorder among children aged 8 years–Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2018. MMWR Surveillance Summaries, 70(11), 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maenner MJ, Warren Z, Williams AR, Amoakohene E, Bakian AV, Bilder DA, Durkin MS, Fitzgerald RT, Furnier SM, Hughes MM, Ladd-Acosta CM, McArthur D, Pas ET, Salinas A, Vehorn A, Williams S, Esler A, Grzybowski A, Hall-Lande J, … Shaw KA (2023). Prevalence and characteristics of autism Spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2020. Morbidity and Mortality Weekly Report. Surveillance Summaries (Washington, D.C: 2002), 72(2), 1–14. 10.15585/mmwr.ss7202a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magaña S, Lopez K, Aguinaga A, & Morton H (2013). Access to diagnosis and treatment services among latino children with autism spectrum disorders. Intellectual and Developmental Disabilities, 51(3), 141–153. 10.1352/1934-9556-51.3.141 [DOI] [PubMed] [Google Scholar]
- Mandell DS, Ittenbach RF, Levy SE, & Pinto-Martin JA (2007). Disparities in diagnoses received prior to a diagnosis of autism spectrum disorder. Journal of Autism and Developmental Disorders, 37, 1795–1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandell DS, Listerud J, Levy SE, & Pinto-Martin JA (2002). Race differences in the age at diagnosis among medicaid-eligible children with autism. Journal of the American Academy of Child and Adolescent Psychiatry, 41(12), 1447–1453. 10.1097/00004583-200212000-00016 [DOI] [PubMed] [Google Scholar]
- Mandell DS, & Novak M (2005). The role of culture in families’ treatment decisions for children with autism spectrum disorders. Mental Retardation and Developmental Disabilities Research Reviews, 11(2), 110–115. [DOI] [PubMed] [Google Scholar]
- Mandell DS, Wiggins LD, Carpenter LA, Daniels J, DiGuiseppi C, Durkin MS, Giarelli E, Morrier MJ, Nicholas JS, Pinto-Martin JA, Shattuck PT, Thomas KC, Yeargin-Allsopp M, & Kirby RS (2009). Racial/ethnic disparities in the identification of children with autism spectrum disorders. American Journal of Public Health, 99(3), 493–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mascari BG, & Forgnone C (1982). A follow-up study of EMR students four years after dismissal from the program. Education and Training of the Mentally Retarded, 17(4), 288–292. [Google Scholar]
- Matthews NL, Smith CJ, Pollard E, Ober-Reynolds S, Kirwan J, & Malligo A (2015). Adaptive functioning in autism spectrum disorder during the transition to adulthood. Journal of Autism and Developmental Disorders, 45(8), 2349–2360. [DOI] [PubMed] [Google Scholar]
- McQuaid GA, Pelphrey KA, Bookheimer SY, Dapretto M, Webb SJ, Bernier RA, McPartland JC, Van Horn JD, & Wallace GL (2021). The gap between IQ and adaptive functioning in autism spectrum disorder: Disentangling diagnostic and sex differences. Autism, 25(6), 1565–1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitter N, Ali A, & Scior K (2019). Stigma experienced by families of individuals with intellectual disabilities and autism: A systematic review. Research in Developmental Disabilities, 89, 10–21. [DOI] [PubMed] [Google Scholar]
- Mukaka MM (2012). A guide to appropriate use of correlation coefficient in medical research. Malawi Medical Journal, 24(3), 69–71. [PMC free article] [PubMed] [Google Scholar]
- Mullen E (1995). Mullen scales of early learning. Pearson. [Google Scholar]
- Nader AM, Courchesne V, Dawson M, & Soulières I (2016). Does WISC-IV underestimate the intelligence of autistic children? Journal of Autism and Developmental Disorders, 46, 1582–1589. [DOI] [PubMed] [Google Scholar]
- Obi O, Van Naarden Braun K, Baio J, Drews-Botsch C, Devine O, & Yeargin-Allsopp M (2011). Effect of incorporating adaptive functioning scores on the prevalence of intellectual disability. American Journal on Intellectual and Developmental Disabilities, 116(5), 360–370. [DOI] [PubMed] [Google Scholar]
- Papazoglou A, Jacobson LA, McCabe M, Kaufmann W, & Zabel TA (2014). To ID or not to ID? Changes in classification rates of intellectual disability using DSM-5. Mental Retardation, 52(3), 165–174. [DOI] [PubMed] [Google Scholar]
- Pathak M, Bennett A, & Shui AM (2019). Correlates of adaptive behavior profiles in a large cohort of children with autism: The autism speaks autism treatment network registry data. Autism, 23(1), 87–99. [DOI] [PubMed] [Google Scholar]
- Patrick ME, Shaw KA, Dietz PM, Baio J, Yeargin-Allsopp M, Bilder DA, Kirby RS, Hall-Lande JA, Harrington RA, Lee L-C, Lopez MLC, Daniels J, & Maenner MJ (2021). Prevalence of intellectual disability among eight-year-old children from selected communities in the United States, 2014. Disability and Health Journal, 14(2), 101023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry A, Flanagan HE, Dunn Geier J, & Freeman NL (2009). Brief report: The Vineland adaptive behavior scales in young children with autism spectrum disorders at different cognitive levels. Journal of Autism and Developmental Disorders, 39(7), 1066–1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pham AV, & Charles LC (2023). Racial disparities in autism diagnosis, assessment, and intervention among minoritized youth: Sociocultural issues, factors, and context. Current Psychiatry Reports, 25, 1–11. [DOI] [PubMed] [Google Scholar]
- Pham HH., Sandberg N., Trinkl J., & Thayer J. (2022). Racial and ethnic differences in rates and age of diagnosis of autism spectrum disorder. JAMA Network Open, 5(10), e2239604. 10.1001/jamanetworkopen.2022.39604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickles A, McCauley JB, Pepa LA, Huerta M, & Lord C (2020). The adult outcome of children referred for autism: Typology and prediction from childhood. Journal of Child Psychology and Psychiatry, 61(7), 760–767. 10.1111/jcpp.13180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. (2022). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/ [Google Scholar]
- Reichow B, Hume K, Barton EE, & Boyd BA (2018). Early intensive behavioral intervention (EIBI) for young children with autism spectrum disorders (ASD). The Cochrane Database of Systematic Reviews, 5(5), CD009260. 10.1002/14651858.CD009260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reschly DJ, & Ward SM (1991). Use of adaptive behavior measures and overrepresentation of Black students in programs for students with mild mental retardation. American Journal on Mental Retardation, 96, 257–268. [PubMed] [Google Scholar]
- Rutter M, Le Couteur A, & Lord C (2003a). ADI-R: The autism diagnostic interview-revised. Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Rutter ML, Bailey A, & Lord C (2003b). The social communication questionnaire: Manual. Western Psychological Services. [Google Scholar]
- SAS Institute Inc. (2010). SAS (Version 9.4). Cary, North Carolina, USA: SAS Institute Inc. [Google Scholar]
- Saulnier CA, & Klin A (2007). Brief report: Social and communication abilities and disabilities in higher functioning individuals with autism and Asperger syndrome. Journal of Autism and Developmental Disorders, 37(4), 788–793. [DOI] [PubMed] [Google Scholar]
- Scarpa A, Reyes NM, Patriquin MA, Lorenzi J, Hassenfeldt TA, Desai VJ, & Kerkering KW (2013). The modified checklist for autism in toddlers: Reliability in a diverse rural American sample. Journal of Autism and Developmental Disorders, 43, 2269–2279. [DOI] [PubMed] [Google Scholar]
- Schendel DE, DiGuiseppi C, Croen LA, Fallin MD, Reed PL, Schieve LA, Wiggins LD, Daniels J, Grether J, Levy S, Miller L, Newschaffer C, Pinto-Martin J, Robinson C, Windham GC, Alexander A, Aylsworth AS, Bernal P, Bonner JD, … Yeargin-Allsopp M (2012). The study to explore early development (SEED): A multisite epidemiologic study of autism by the centers for autism and developmental disabilities research and epidemiology (CADDRE) network. Journal of Autism and Developmental Disorders, 42, 2121–2140. 10.1007/s10803-012-1461-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott LS (1979). Identification of declassified students: Characteristics and needs of the population [Paper presentation]. Annual Convention of the American Psychological Association 1979, New York, NY, United States. [Google Scholar]
- Shaw KA, Bilder DA, McArthur D, Williams AR, Amoakohene E, Bakian AV, Durkin MS, Fitzgerald RT, Furnier SM, Hughes MM, Pas ET, Salinas A, Warren Z, Williams S, Esler A, Grzybowski A, Ladd-Acosta CM, Patrick M, Zahorodny W, … Maenner MJ (2023). Early identification of autism Spectrum disorder among children aged 4 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2020. Morbidity and Mortality Weekly Report. Surveillance Summaries (Washington, D.C: 2002), 72(1), 1–15. 10.15585/mmwr.ss7201a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi B, Wu W, Dai M, Zeng J, Luo J, Cai L, Wan B, & Jing J (2021). Cognitive, language, and behavioral outcomes in children with autism spectrum disorders exposed to early comprehensive treatment models: A meta-analysis and meta-regression. Frontiers in Psychiatry, 12, 691148. 10.3389/fpsyt.2021.691148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparrow S, Balla D, & Cicchetti D (2005). Vineland adaptive behavior scales (2nd ed.). Pearson. [DOI] [PubMed] [Google Scholar]
- Thompson R, Smith RB, Karim YB, Shen C, Drummond K, Teng C, & Toledano MB (2022). Noise pollution and human cognition: An updated systematic review and meta-analysis of recent evidence. Environment International, 158, 106905. [DOI] [PubMed] [Google Scholar]
- Tillmann J, San José Caceres A, Chatham CH, Crawley D, Holt R, Oakley B, Banaschewski T, Baron-Cohen S, Bölte S, Buitelaar JK, Durston S, Ham L, Loth E, Simonoff E, Spooren W, Murphy DG, Charman T, & the EU-AIMS LEAP group. (2019). Investigating the factors underlying adaptive functioning in autism in the EU-AIMS longitudinal European autism project. Autism Research, 12(4), 645–657. 10.1002/aur.2081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong S, Baghurst P, Vimpani G, & McMichael A (2007). Socioeconomic position, maternal IQ, home environment, and cognitive development. The Journal of Pediatrics, 151(3), 284–288. [DOI] [PubMed] [Google Scholar]
- Van Buuren S, & Groothuis-Oudshoorn K (2011). Mice: Multivariate imputation by chained equations in R. Journal of Statistical Software, 45(3), 1–67. 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- Van Naarden Braun K, Christensen D, Doernberg N, Schieve L, Rice C, Wiggins L, Schendel D, & Yeargin-Allsopp M (2015). Trends in the prevalence of autism spectrum disorder, cerebral palsy, hearing loss, intellectual disability, and vision impairment, metropolitan Atlanta, 1991–2010. PLoS One, 10(4), e0124120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiggins LD, Reynolds A, Rice CE, Moody EJ, Bernal P, Blaskey L, Rosenberg SA, Lee LC, & Levy SE (2015). Using standardized diagnostic instruments to classify children with autism in the study to explore early development. Journal of Autism and Developmental Disorders, 45, 1271–1280. 10.1007/s10803-014-2287-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witt JC, & Martens BK (1984). Adaptive behavior: Tests and assessment issues. School Psychology Review, 13(4), 478–484. [Google Scholar]
- Yeargin-Allsopp M, Drews CD, Decouflé P, & Murphy CC (1995). Mild mental retardation in black and white children in metropolitan Atlanta: A case-control study. American Journal of Public Health, 85(3), 324–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeidan J, Fombonne E, Scorah J, Ibrahim A, Durkin MS, Saxena S, Yusuf A, Shih A, & Elsabbagh M (2022). Global prevalence of autism: A systematic review update. Autism Research: Official Journal of the International Society for Autism Research, 15(5), 778–790. 10.1002/aur.2696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman KE, Lindly OJ, Reyes NM, Chavez AE, Cobian M, Macias K, Reynolds AM, & Smith KA (2018). Parent perceptions of community autism spectrum disorder stigma: Measure validation and associations in a multi-site sample. Journal of Autism and Developmental Disorders, 48, 3199–3209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman KE, Lindly OJ, Reyes NM, Chavez AE, Macias K, Smith KN, & Reynolds A (2017). Disparities in diagnosis and treatment of autism in Latino and non-Latino white families. Pediatrics, 139(5), e20163010. 10.1542/peds.2016-3010 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Research data are not shared.