Abstract
Hypertension is the leading cause of cardiovascular diseases and nephropathies. Its treatment and management require long-term follow-up which can be facilitated by the emergence of device-based therapies. Novel recommendations have been well described in the latest ESH guidelines as well as new risk factors have been identified. The authors summarized the published evidence on hypertension management. The authors also cited in this review novel treatment approaches in different settings and the intervention of medication adherence in treatment success. Such non-communicable disease requires long-term follow-up and monitoring, which is quite facilitated in the era of digitalization by cuff-less devices based on prediction tools.
Keywords: cuff-less devices, hypertension, management, medication adherence
Introduction
Highlights
We have attempted in this review to highlight the latest research findings and clinical guidelines related to hypertension management.
This review highlights the assessment of digital health potential on patient engagement and treatment adherence.
Currently, we aimed to offer a valuable resource for healthcare professionals to enhance their understanding of contemporary hypertension management practices.
Hypertension is a critical burden of public health worldwide. The WHO states 1.28 billion adults whose ages vary between 30 and 79 years, in developing and underdeveloped countries mostly, have hypertension1, with older age known to be a risk factor and according to this range, the numbers of patients with hypertension keep on increasing. It had doubled from 331 million women and 317 million men in 1990 to 626 million women and 652 million men in 20192.
According to the Centers for Disease Control and Prevention, 48.1% which is 119.9 million of hypertensive patients in the United States3. In Europe, hypertension prevalence is reported at 55%4.
Hypertension itself is a risk factor leading to a decreasing age onset of cardiovascular diseases (CVD), making it the top-tier cause of mortality in 20305. Complications such as CVD, chronic kidney disease (CKD), and stroke increase the rates of morbidity and mortality6.
There are numerous risk factors, such as environmental, behavioural, dietary, psychosocial, socio-economic factors, and other comorbidities like sleep disorders, that could play a significant role in the advent of hypertension7–9.
Hypertension control requires pharmacological and non-pharmacological interventions and could be affected by cultural differences, social and educational backgrounds10.
In fact, hypertension management is based on the combination of lifestyle modifications, adherence to the prescribed medication regimen, and adequate patient education. For this matter, artificial intelligence (AI), an innovative scientific approach armed with a widespread of analytic techniques that could unlock the future of health, has begun to emerge and might play a significant role in hypertension management11. Various studies have validated its application in the field of hypertension treatment12. Despite the lack of research on a large sample size, AI represents a complementary tool alongside healthcare professionals. When used effectively, they both can exacerbate the challenges involved with the high prevalence of non-communicable diseases (NCD). The aim of this review is to assess the current data related to hypertension management. Efforts should be maximized in order to implement strategies as well as guidelines for the prevention and better management of this NCD among different population age categories.
Methods
We relied on PubMed and Web Of Science databases in order to extract reviews that were published from 2019 to 2023 (5 years). We followed the 2020 Preferred Reporting for Systematic Reviews and Meta-Analysis (Fig. 1). The term we used for our research is “hypertension” in parallel to this combination ((((Hypertension) OR High blood pressure) OR Blood pressure) OR Hyperten*). Any record that does not consist of essential hypertension was excluded from our narrative review. Papers containing pulmonary, portal, intracranial hypertension, preeclampsia, pregnancy, women, children, infants, adolescents, cancer, perioperative were excluded from our study.
Figure 1.
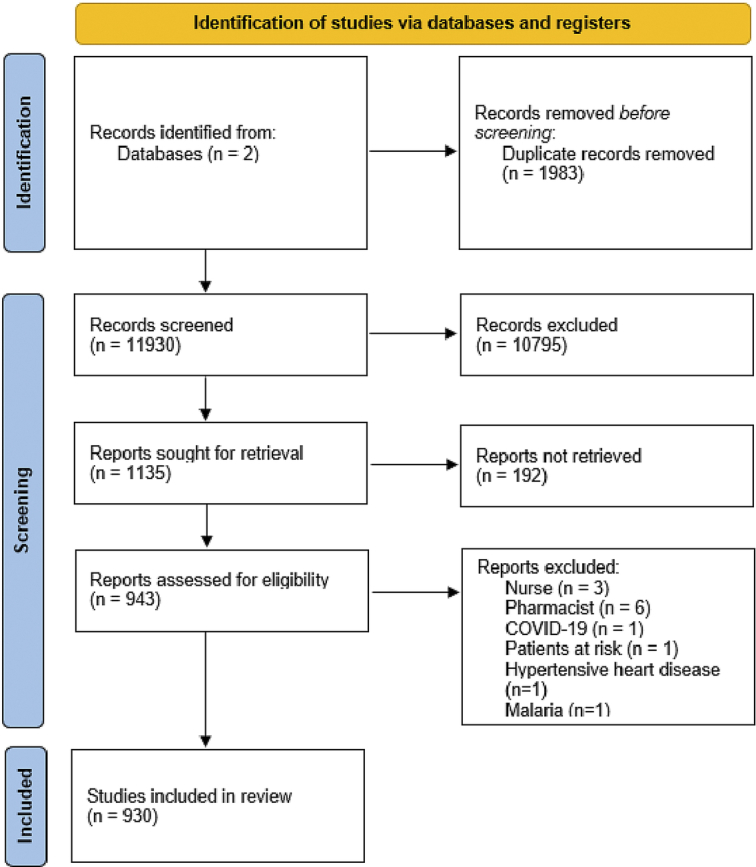
Flow chart diagram.
Epidemiology
Hypertension numbers are remarkably rising globally. In 2010, the number of hypertensive adults was estimated at 1.39 billion accounting for 349 million in high-income countries and 1.04 billion in low-middle-income countries (LMIC)13. Studies predict an increase of the total number of patients to reach 1·56 billion in 2025. The high prevalence is predominant in LMIC due to the lack of awareness and limited access to healthcare services14. A study of 20 years, performed in the Middle East and North Africa (MENA) regions, revealed a prevalence of hypertension ranging from 2.2 to 67.3%. The highest prevalence was of Iraq (54.7%) followed by Algeria (44.1%) and Morocco (39.8%), whereas the lowest one is attributed to Yemen with a proportion of 12.9%10.
The NCD Risk Factor Collaboration2 conducted an age-standardized study, stratified by gender, encompassing 200 countries in which they revealed the highest prevalence for both genders in the MENA regions is represented by Iraq which is consistent with the previous study. Furthermore, another study has been performed on 15 countries of the Sub-Saharan region in which they revealed a pooled prevalence of 57%15. East, South and South East Asia and Sub-Saharan Africa witnessed a mortality rate duplication associated with high blood pressure13,16.
Hypertension in Canada doesn’t surpass 30%17 as it is the case for high-income countries of Asia-Pacific and Western whilst in Central and Eastern Europe it exceeds 34.2% and 40% for women and men, respectively2. Based on the recent findings of the European Society of Hypertension (ESH), without screening, a large number of individuals who may be hypertensive are neglected like men, younger adults, people with lower sociodemographic backgrounds. Hypertension screening is a crucial aspect that aims at detecting high blood pressure earlier allowing for timely effective interventions18.
Types of hypertension
Hypertension is either primary or secondary. Primary hypertension is the most common form accounting for 90–95%. Its development is influenced by genetic background as well as lifestyle choices19. It is a multifactorial disease. For this, some authors consider it as idiopathic20. Secondary hypertension affects ~5–10% and is a treatable hypertension that is caused by a medical condition for example renal impairment or medications such as non-steroidal anti-inflammatory drugs which influence the production of prostaglandin that has a hormone-like effect and is involved in regulating vasoconstriction and vasodilation and in controlling blood pressure. Amphetamine, methylphenidate dexmethylphenidate, and dextroamphetamine have the potential to increase blood pressure. There are decongestants such as phenylephrine or pseudoephedrine and systemic corticosteroids like dexamethasone as well as estrogens, androgens, oral contraceptives, and immunosuppressants that may contribute to an increase in blood pressure. Prolonged utilization of recombinant human erythropoietin also has the potential to induce hypertension19,21,22. Furthermore, there are other categories, such as malignant, resistant, labile, and white-coat hypertension20, that highlight the complexity of the disease that once understood would be of great help to medical care.
Risk factors
Numerous risk factors influence the advent of hypertension. Age, sex (physiological, psychological and hormonal variations), ethnicity, family history, insulin resistance and genetic heritage constitute unalterable risk factors23,24. Meanwhile, other risk factors include smoking, alcohol consumption, sedentariness, waist-to-hip ratio, socio-economic status, high cholesterol, poor nutrition, obesity, low potassium intake, CKD13, lack of education, lack of knowledge, and a history of vascular disease13,25–27. Other studies report a positive link between obstructive sleep apnoea (OSA)-induced sympathetic activation, sleep deprivation, gut dysbiosis, gut barrier dysfunction, anxiety, traffic noise exposure, organic compounds of air pollution and hypertension (Fig. 2)24,28–32. For dietary habits, high sodium intake is a well-established factor associated with high blood pressure. Processed food such as red meat contains a large amount of sodium compared to unprocessed red meat. Along with that, nitrite which functions as a preservative has been considered as a trigger of endothelial dysfunction33.
Figure 2.
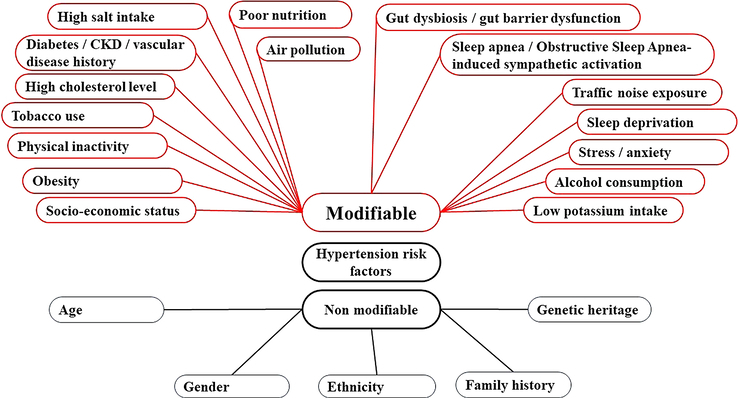
Modifiable and non-modifiable hypertension risk factors.
Pathophysiology
The pathogenesis of hypertension is complex and is underlied by different intertwined mechanisms, which is congruent to the original mosaic theory of Page9,34.
Hypertension is influenced by genetics. The light has been shed on primary hypertension, and 1477 single-nucleotide polymorphisms have been identified in more than 30 genes. Blood pressure heritability is estimated from 30 to 50% and 27% of the cases have been explained by genome-wide association studies (GWAS)35. Another study stated that some variants are implied in the mitochondrial function, which explains the maternally inherited hypertension36. The monogenic form is manifested in syndromes such as Liddle, Gitelman and Bartter syndrome or familial cases that exhibited a Mendelian pattern through pedigrees linkage analysis and mostly, they affect renal sodium handling pathways37. Salt intake is known to cause hypertension. A Mendelian Randomization study suggests that a genetic predisposition to excessive sodium consumption is possible38. Whereas, higher genetically predicted HDL-C is associated with a lower risk of hypertension39.
Besides genetics, the relationship between hypertension and other factors has been investigated. The physiology of vasculature is disturbed not only with advanced age (vascular senescence), but also when bad lifestyle-related habits intervene such as smoking which will lead to vasculature inflammation, an increase in mitochondrial oxidative stress, a decrease in nitric oxide (NO) and an alteration of the autonomic nervous system responsible for the control of blood pressure.
Hypertension arises from the cardiovascular regulatory systems alteration including the renin-angiotensin-aldosterone system (RAAS), increased activation of the sympathetic nervous system. Reactive oxygen species and oxidative stress generation imply some of the blood pressure regulators that intervene in the RAAS pathway. Hence, an endothelial dysfunction will lead to oxidation-reduction state imbalance and an increase in reactive oxygen species (ROS), which are responsible for a decrease in NO bioavailability and a dysregulation of immuno-inflammation18.
Metabolomics have broadened our understanding of several diseases. From disruptions in glucose and lipid metabolism that may be affected by the pleiotropic role of insulin to the study of the gut microbiota. An imbalance of the gut microbiota is manifested by the decrease of the diversity of the microbiota and their beneficial metabolites resulting in gut barrier dysfunction and increased intestinal permeability leading to endotoxin bacterial translocation in the bloodstream followed by inflammation and to a greater extent endothelial dysfunction31,37.
Diagnosis and assessment
Based on office blood pressure values, there are grades that are restricted to blood pressure (BP) values and stages that involve hypertension-related complications (including chronic kidney disease stages, diabetes, hypertension-mediated organ damage (HMOD) and established CVD.
Blood pressure can be measured by office blood pressure measurement (OBPM), Ambulatory Blood Pressure Monitoring (ABPM), or home blood pressure monitoring (HBPM). The presence of a high cardiovascular risk, elevated grade 3 hypertension or HMOD are a sign of approbation of the diagnosis from the first visit to office. Other than that, two to three visits are required at 1–4 weeks intervals in which the measurement on both arms is necessary, and a higher systolic blood pressure (SBP) in one of the arms is to be taken into consideration with repeated measurements since it is thought to be a predictor of cardiovascular risks.
Arm circumference is crucial for the choice of the cuff size for both manual auscultatory and automated electronic devices for the accuracy of blood pressure measurements.
When multiple measurements of blood pressure are not stable at office, then ABPM or HBPM ought to be taken into account.
Office blood pressure remains limited to the detection of the white-coat effect, thus leading to inaccurate readings compared to HBPM. OBPM is preferred for initial diagnosis and immediate interventions as it extends to the identification of hypotension during patient visits meanwhile HBPM is favourable for long-term monitoring, but it is prone to user error and lack of professional assessment. It must be measured with upper arm cuff devices of automated storage, averaging of multiple readings, and transferred to a health professional in order to avoid inaccurate readings. The recommendations for home and office are alike for the conditions (quiet room with comfortable temperature, no smoking, caffeine, food drug intake or exercise 30 min prior to measurement, no talking during or between measurements and remaining seated and relaxed for 3–5 min), and posture (sitting in a back supporting chair, feet flat on the floor and bare arm on the table) except for the number of readings with 1 min interval between each reading and averaging the last 2 readings (HBPM necessitates 2 readings while OBPM takes 3). Likely to OBPM, considered as a better predictor of outcomes and HMOD than HBPM, in addition to daily activities, ABPM offers the possibility to measure BP at night during sleep and make a difference between BP surges in the morning and resistant hypertension. The ABPM is marked by lower values of hypertension (130/80 mmHg) compared to OBPM (140/90 mmHg) and HBPM is in between (135/85 mmHg). Experiences have led to the application of the appropriate procedure which is to measure blood pressure every 20 min in order to provide information of high-quality data for the night-time BP measures9.
Complications and target organ damage
The mechanisms underlying the pathophysiology of hypertension represent the infrastructure of the onset of several diseases. Endothelial dysfunction constitutes the first step of atherosclerosis genesis40. The ESH has summed up the organs affected by this chronic disease. On long terms, hypertension exerts tension on the heart and blood vessels leading other organs such as the brain, the eye, the kidney to deterioration. Hypertensive diseases are divided into 2 groups. The first one targets the different organs, and the second is characterized specifically by cardiovascular events such as myocardial infarction, stroke, cardiovascular death or heart failure. Myocardial infarction, fibrosis and collagen synthesis in vascular and cardiac injuries may be induced by aldosterone overexpression41. Alongside these complications the endothelium plays a role in secreting pro-inflammatory and prothrombotic factors resulting in thromboembolic events42. Hypertensive vascular remodelling has been remarked by an increased M1 macrophage pro-inflammatory activity to which curcumin dose-dependent has been demonstrated to prove an inhibitory effect. Thereby offering a new therapeutic agent in the form of nanoparticles with anti-inflammatory and immunomodulatory actions43.
Matrix metalloproteinases (MMPs) are enzymes that are found to play a molecular basis for organ damage and are present at high levels in hypertensive patients. Their activity increases during inflammation processes and may affect cardiomyocytes and vascular smooth cells. In order to prevent target organ damage, patients should be regularly diagnosed in this direction44. The latest ESH guidelines recommend a regular follow-up for the identification of any organ damage9.
Lifestyle modifications
Hypertension can be managed by non-pharmacological approaches considered as a preventive tool particularly in early age. Healthy lifestyle habits include healthy eating, drinking coffee (up to 3 cups of caffeine), sleep and stress levels as well as exercising, maintaining a healthy body weight and reducing exposure to pollution. These lifestyle habits are effective in reducing blood pressure. Although observational studies have shown high consumption of coffee may protect only nonsmokers from hypertension based on their CYP1A2 genetic profile9.
High adherence to Dietary Approaches to Stop Hypertension (DASH) or its equivalent which is the Mediterranean diet shows a beneficial effect on the risk of hypertension45–47. High fruit and vegetable intake leads to reduced blood pressure given the nutrients they contain. Meta-analyses were realized in order to prove the inverse association between fruit and vegetable combined consumption and the risk of hypertension. Fibres have a role in reducing weight as well as beneficially affecting vascular endothelial function, mineral absorption and reducing insulin resistance. Minerals including potassium and magnesium contribute to the regulation of vascular resistance, vasodilation, and modulation of baroreflex sensitivity. The ESH guidelines specifically recommend increased potassium intake as a dietary modification for patients with high BP with a preference of potassium-rich diets over potassium chloride pills since they both exert the same lowering BP response9. A decreased risk of hypertension is also associated with the antioxidative activity exerted by vitamins such as folic acid and vitamin E48. Pharmacologically active dietary supplements, also called as nutraceuticals are capturing attention. Spices were also found to have a lowering effect of BP including capsaicin, pepper, chilli, ginger, garlic, onion, fenugreek, turmeric, which are variously used in different culture foods. This effect could be attributed to the role of transient receptor potential vanilloid 1 (TRPV1) activation49. Although, studies on this receptor have not been validated in humans yet50. Recently, it has been attributed to curcumin the role of reconstructing the gut microbiota and normalizing gut-brain communication43. The nutraceuticals are heterogeneous including foods, nutrients and nonnutrients. Among the foods recommended, there are pomegranate juice, green or black tea, beetroot juice, sesame as well as nutrients such as proteins, peptides, amino acids and ions. Nonnutrients are botanical compounds such as phenolic, flavanols and carotenoids. They are plant-derived dietary compounds that exert either an antioxidant activity or beneficial effect on the vasculature by inducing NO production51.
Obese people are at risk of hypertension. Decreasing weight can be targeted either by fibre consumption or exercising. Physical activity is followed by postexercise hypotension, a condition in which the parasympathetic mechanisms are activated after the deactivation of sympathetic patterns lead to blood pressure lowering through decreasing reflex sensitivity. It may also affect cerebral blood flow. Specifically, guidelines and systematic reviews have highly recommended aerobics, known as cardiorespiratory fitness, and isometric exercises as a mean exercise for systolic, diastolic blood pressure (DBP) reduction as well as mean arterial pressure (MAP) office and night-time ambulatory SBP and DBP for the latter. Additionally, flexibility activities such as yoga, tai chi, mindfulness-based stress reduction, and deep breathing exercises have been highlighted as antihypertensive lifestyle therapies. Exercising tai chi, known as a traditional Chinese and a low-intensity aerobic exercise, for a duration greater or equal to 3 months has been demonstrated to lower SBP, DBP and, at the same time increase blood lipid metabolism and NO production and, therefore relax blood vessels52–59.
These lifestyle variations should accompany hypertensive patients under treatment as it may decrease the prescription of additional antihypertensive drugs or doses52. On the contrary, the ESH guidelines emphasize the importance of the use of lifestyle measures as a first approach in the management of hypertension9.
Lifestyle adjustment through behaviour change techniques provided by healthcare professionals, along with the use of digital technologies, including only accurate digital blood pressure devices, are facilitating hypertension control and may increase patient adherence55,60. On this matter, randomized clinical trials (RCTs) should be realized in order to assess their efficacy.
Pharmaceutical treatment and management
The diagnosis of hypertension leads to its treatment and management. The antihypertensive drugs target the renin-angiotensin system (RAS), calcium channels, and beta and α1-adrenergic receptors and are used not only to lower the blood pressure but also to prevent cardiovascular disease onset61. They can be used as monotherapy or combined with different classes according to the severity of the condition. Despite their protective role and their beneficial effects on comorbidities, beta-blockers are not the first-choice treatment due to their pharmacological differences62. They have been demonstrated to show side effects such as fatigue or sleep-related disorders in older patients. Contemporary data reveals Angiotensin Converting Enzyme (ACE) inhibitors as first-line therapy in hypertension management along with thiazide diuretics, calcium channel blockers, and angiotensin receptor blockers (ARBs) by dint of their protective properties and reduced mortality remarkably recognized in cardiac patients having congestive heart failure, acute myocardial infarction or left ventricular dysfunction63,64. ACE-inhibitory activities are also provided by probiotics, such as Bifidobacterium and Lactobacillus, found in fermented dietary foods as well as egg and fish-derived bioactive peptides (BPs)65. According to Wang and colleagues, amlodipine, a calcium channel blocker, is considered effective in hypertension management in different ethnic groups and hypertension-related comorbidities, therefore decreasing cardiovascular and stroke risks. It is cost-effective. On the other hand, it is cost-saving as it limits patients from returning to the health system due to the absence of electrolyte abnormalities. Its long bioavailability protects from incidental non-compliance66. Monotherapy effectiveness is affected by the presence of an underlying comorbidity which complicates the management; therefore, it gives an urge to a tailored treatment approach. Hypertension management is also challenged by non-adherence which is one of the components studied for treatment success. Medication adherence has been promoted by the implementation of combined therapies, which relies on the use of a couple of antihypertensive drugs with different mechanisms of action. Furthermore, it is considered as a better approach compared to using an antihypertensive monotherapy at the beginning for cardiovascular risk reduction. Nonetheless, triple combination therapy is confronted against its cost, which remains one of the challenging reasons for poor treatment adherence67.
Overactivity of the sympathetic nervous system (SNS) alters the physiological activity of the kidneys. In this case, the latest ESH guidelines and the first guidelines that considered renal denervation (RDN) an alternative or complementary option in the treatment and management in hypertension with increased sympathetic nerve activity as well as in uncontrolled and resistant hypertension. Ultrasound and radiofrequency RDN showed remarkable BP lowering in off-medicated uncontrolled hypertension patients by 6.3 and 5 mmHg, respectively9,68. Purinoceptor-mediated effects and purines such as adenosine tri phosphate (ATP) has been observed to increase BP making it a novel target for hypertension treatment that might have an impact on the regulation patterns69.
Hypertensive patients with CKD should be treated by renin-angiotensin system antihypertensives since they reduce albuminuria or combined to a calcium channel blocker (CCB), thiazide or thiazide-like diuretics. The combination therapy is adjusted to the stage of CKD depending on estimated glomerular filtration rate (eGFR). The Sodium-glucose Cotransporter 2 Inhibitors (SGLT2is) are recommended for CKD patients with or without diabetes if eGFR is at least 20 ml/min/1.73 m2 to reduce cardiac and renal outcomes. Likely to SGLT2is, Glucagon-Like Peptide-1 Receptor Agonists (GLP-1 RA) have shown both a reduction in macrovascular and microvascular complications in type 2 diabetes. In addition to their antidiabetic activity, they can both lower office and ambulatory BP despite the use of other antihypertensive agents. However, SGLT2is are more recommended than GLP-1 RA for their accurate cardiorenal protection. Another new drug, finerenone, belongs to the non-steroidal mineralocorticoid receptor antagonists (nsMRA) has been proved to exert cardiorenal properties and is recommended for use in diabetic patients with CKD9,41.
Kidney transplantation is the ideal solution for patients in the last stage of CKD. Nevertheless, hypertension remains one of the most prevalent post-transplantation comorbidities as it was estimated in more than 95% of the patients by ABPM, which is the recommended measurement for hypertension management in this setting. In patients with CKD and early post-transplantation, the primary goal is to reduce office BP to less than 140/90 mmHg and 130/80 mmHg, respectively. If SBP greater than or equal to 140 mmHg or DBP greater than or equal to 90 mmHg cases of type 2 diabetes or CKD, lifestyle interventions and antihypertensive drug treatment should be recommended immediately. In cases of uncontrolled hypertension, the maximum dosages of a triple combination containing a CCB, a RAS inhibitor in addition to a beta-blocker is permitted in order to reduce its rates. The latest ESH guidelines covered the part of onco-hypertension as well in which they mentioned that hypertension is induced by diverse cancer treatments causing cardiorenal toxicity such as vascular endothelial growth factor (VEGF) inhibitors, and its management is emphasized by the use of HBPM for the long follow-up. Taking into consideration the pharmacokinetic interactions, the use of non-DHP CCBs is not recommended in treatment with anticancer drugs9.
Access to treatment and healthcare services consists of challenges that contribute to lower proportions of treatment and control in low- and middle-income countries than those of higher income. The role of telemedicine has been assessed and demonstrated to be a promising approach to increase access to care encouraging its use in LMIC in order to improve outcomes of hypertension70.
The high prevalence of hypertension is still noticed both in developed and developing countries, which may be due to limitations in diagnostic and therapeutic approaches. However, the evolution of information and communication technology and the large possession of smartphones facilitate hypertension’s management by patients themselves. Studies revealed the effectiveness of dietary self-monitoring via apps with theory-based interventions that imply the patient’s participation and responsibility in order to reach the desirable outcomes71. Home BP telemonitoring has shown promising results in BP reduction during the COVID-19 pandemic9.
Medicine is on the way of applying “high benefit approach” rather than “high risk approach” since the machine-learning-based high-benefit approach is able to identify individuals who will gain the most from the intervention, thereby lowering cardiovascular outcomes at the population level72. ABPM and HBPM are out-of-office settings that assist in evaluating hypertension burden, and their limitations are overcome by continuous BP measurement offered by accurate wearable BP measuring devices continuously as it may accurately detect different clinical phenotypes. The era of digitalization is promoting the shift from conventional BP measurements to advanced ones leading to personalized management, therefore facilitating the doctor’s access to data through remote BP monitoring programs. However, the implementation of these cuff-less devices in hypertension relies on the design of specific validation protocols, which refer to a static test, a test with BP change from the calibration point, device position test, treatment test, awake/asleep test, exercise test and a test after a certain period of time from calibration which is the recalibration for effective accuracy. The necessary tests addressed are the individual cuff calibration that can be automatic or manual and the measurement in multiple positions to ensure accurate measurements. In addition, for remote BP monitoring, an efficient storage of data is required for handling and ensuring the privacy of personal information complying with personal data protection law. Subsequently, it is crucial to conduct extensive prospective clinical investigations to determine the reference point for “normal” blood pressure values as well as blood pressure values linked to events in everyday situations using these devices73–76. In regard of physiological conditions, cuff-less BP measurements vary between individuals, which make its adoption in clinical practice difficult.
Treatments based on devices include renal denervation, carotid baroreceptor stimulation and the dual chamber of the Moderato system. After the latter device activation, the 24 h SBP reduced and this effect was maintained through the 6 months. However, on the long term, consequences of cardiac neuromodulation should be assessed through clinical trials with a larger population9.
In the era of digitalization, hypertension can be diagnosed by alternative methods. Artificial intelligence represents is a revolutionising in the domain of health. Hypertension is a common medical condition that affects a large number of people while the number of primary care doctors or specialists for hypertension is limited resulting in an unbalanced healthcare system marked by a shortage of healthcare professionals. The shift of responsibility towards patients themselves in monitoring hypertension or by using AI-driven intelligent systems in order to alleviate the burden of hypertension. Applications based on health data are a source of help to health assessment and the development of predictive tools as well as the improvement of AI models accuracy74. AI algorithms can improve precision, accuracy and reproducibility of BP measurements. Hence, their combination with a wearable device would give more insight about ABPM. Hypertension is a multifaceted disease. Thus, research is focusing on delivering AI-driven applications adaptable to the patient’s history, treatment and lifestyle modifications12. Good training of the model using large datasets is required in order to overcome technical limitations such as overfitting or underfitting leading to poor generalization77.
AI has been applied in predicting the risk of hypertension or its development, identifying new genes associated with hypertension, diagnosing hypertension by using demographic data, vital signs, cardiovascular risk factors, and routine laboratories in large patient cohorts. Many risk prediction models have been developed, and they have demonstrated better results than traditional techniques that are based on several assumptions, as the normality of the distribution, linear relationship between independent and dependent variables, homoscedasticity. The amount of data is transforming society and its use in parallel with artificial intelligence algorithms is the key to new findings of robust diagnosis and accurate predictions. The limitations of AI remain in its application on large sample sizes in order to approve their accuracy12.
ESH guidelines, the global standard evidence-based guidelines, are focused on using a personalized perspective in hypertension management.
Accurate use of artificial intelligence devices is pivotal in public health. It will assist clinicians in the early detection and prevention of hypertension and its outcomes. The call of revolutionary AI interventions is not limited, and it may be applied to other chronic diseases referring to digital management.
Conclusion
Conducting blood pressure measurements in a clinical setting is a fundamental initial step for accurately diagnosing hypertension and tracking its progression. Obtaining multiple readings is recommended to assess the effectiveness of hypertension management strategies. Embracing a healthier lifestyle, which involves practices like reducing salt intake, requires behavioural changes supported by healthcare professionals, aligning with broader public health initiatives. In summary, digital health tools, including telehealth interventions and mobile applications, hold promise in hypertension management. They enhance patient education, facilitate remote monitoring, and potentially contribute to better blood pressure control. However, further research is necessary to thoroughly understand their benefits and effectiveness in real-world clinical practice.
Ethical approval
We have written a literature review. So, we didn’t need the approval of the ethics committee.
Consent
We realized a literature review. We didn’t supply any patients’ or volunteers’ names.
Source of funding
We haven’t received any funding.
Author contribution
S.R. wrote the manuscript. I.H. designed the study, reviewed and edited the manuscript.
Conflicts of interest disclosure
We claim we don’t have any conflict of interest that could inappropriately influence our work.
Research registration unique identifying number (UIN)
Our work is a literature review.
Guarantor
The guarantor is S.R.
Data availability statement
Data sharing is not applicable to this work.
Provenance and peer review
Nothing to mention.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 23 April 2024
Contributor Information
Sara Ramdani, Email: sara.ramdani001@gmail.com.
Intissar Haddiya, Email: intissarhaddiya@yahoo.fr.
References
- 1. World Health Organization. Hypertension [Internet]. 2023. https://www.who.int/fr/news-room/fact-sheets/detail/hypertension .
- 2. (NCD-RisC) NRFC . Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet (London, England) 2021;398:957–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Prevention CfDCa. Facts About Hypertension [Internet]. 2023. https://www.cdc.gov/bloodpressure/facts.htm .
- 4. Reuter H, Jordan J. Status of hypertension in europe. Curr Opin Cardiol 2019;34:342–349. [DOI] [PubMed] [Google Scholar]
- 5. Elahi A, Ali AA, Khan AH, et al. Challenges of managing hypertension in Pakistan-a review. Clin Hypertens 2023;29:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kim HL, Lee EM, Ahn SY, et al. The 2022 focused update of the 2018 korean hypertension society guidelines for the management of hypertension. Clin Hypertens 2023;29:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Abboud M, Karam S. Hypertension in the middle east: current state, human factors, and barriers to control. J Hum Hypertens 2022;36:428–436. [DOI] [PubMed] [Google Scholar]
- 8. Abukanna AMA, Alanazi BFA, Alanazi STA, et al. Sleep deficiency as a risk factor for hypertension: a systematic review. Pharmacophore 2022;13:35–41. [Google Scholar]
- 9. Mancia Chairperson G, Kreutz Co-Chair R, Brunström M, et al. 2023 esh guidelines for the management of arterial hypertension the task force for the management of arterial hypertension of the european society of hypertension endorsed by the european renal association (era) and the international society of hypertension (ish). J Hypertens 2023;41. [DOI] [PubMed] [Google Scholar]
- 10. Balouchi A, Rafsanjani M, Al-Mutawaa K, et al. Hypertension and pre-hypertension in middle east and north africa (mena): A meta-analysis of prevalence, awareness, treatment, and control. Curr Probl Cardiol 2022;47:101069. [DOI] [PubMed] [Google Scholar]
- 11. WHO. WHO outlines considerations for regulation of artificial intelligence for health [Internet]. 2023. https://www.who.int/news/item/19-10-2023-who-outlines-considerations-for-regulation-of-artificial-intelligence-for-health .
- 12. Chaikijurajai T, Laffin LJ, Tang WHW. Artificial intelligence and hypertension: recent advances and future outlook. Am J Hypertens 2020;33:967–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol 2020;16:223–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Burnier M, Egan BM. Adherence in hypertension a review of prevalence, risk factors, impact, and management. Circ Res 2019;124:1124–1140. [DOI] [PubMed] [Google Scholar]
- 15. Bosu WK, Reilly ST, Aheto JMK, et al. Hypertension in older adults in africa: a systematic review and meta-analysis. PLoS One 2019;14:e0214934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhou B, Perel P, Mensah GA, et al. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol 2021;18:785–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension canada’s 2020 comprehensive guidelines for the prevention, diagnosis, risk assessment, and treatment of hypertension in adults and children. Can J Cardiol 2020;36:596–624. [DOI] [PubMed] [Google Scholar]
- 18. Mancia G, Kreutz R, Brunström M, et al. 2023 esh guidelines for the management of arterial hypertension the task force for the management of arterial hypertension of the european society of hypertension endorsed by the international society of hypertension (ish) and the european renal association (era). J Hypertens 2023;41:1874–2071. [DOI] [PubMed] [Google Scholar]
- 19. Wahl L, Tubbs RS. A review of the clinical anatomy of hypertension. Clin Anat 2019;32:678–681. [DOI] [PubMed] [Google Scholar]
- 20. Habas E, Habas E, Khan FY, et al. Blood pressure and chronic kidney disease progression: an updated review. Cureus J Med Sci 2022;14:e24244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brouwers S, Sudano I, Kokubo Y, et al. Arterial hypertension. Lancet 2021;398:249–261. [DOI] [PubMed] [Google Scholar]
- 22. Aronow WS. Drug-induced causes of secondary hypertension. Ann Transl Med 2017;5:349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Benenson I, Waldron FA, Jadotte YT, et al. Risk factors for hypertensive crisis in adult patients: a systematic review. JBI Evid Synth 2021;19:1292–1327. [DOI] [PubMed] [Google Scholar]
- 24. Perumareddi P. Prevention of hypertension related to cardiovascular disease. Prim Care 2019;46:27–39. [DOI] [PubMed] [Google Scholar]
- 25. Meher M, Pradhan S, Pradhan SR. Risk factors associated with hypertension in young adults: a systematic review. Cureus J Med Sci 2023;15:e37467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Oliveira V, Kwitek AE, Sigmund CD, et al. Recent advances in hypertension: Intersection of metabolic and blood pressure regulatory circuits in the central nervous system. Hypertension (Dallas, Tex: 1979) 2021;77:1061–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Poznyak AV, Sadykhov NK, Kartuesov AG, et al. Hypertension as a risk factor for atherosclerosis: Cardiovascular risk assessment. Front Cardiovasc Med 2022;9:959285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hahad O, Rajagopalan S, Lelieveld J, et al. Noise and air pollution as risk factors for hypertension: Part ii-pathophysiologic insight. Hypertension (Dallas, Tex: 1979) 2023;80:1384–1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Han B, Chen WZ, Li YC, et al. Sleep and hypertension. Sleep Breathing Schlaf Atmung 2020;24:351–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Duttaroy AK. Role of gut microbiota and their metabolites on atherosclerosis, hypertension and human blood platelet function: a review. Nutrients 2021;13:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Yang Z, Wang Q, Liu Y, et al. Gut microbiota and hypertension: association, mechanisms and treatment. Clin Exp Hypertens (New York, NY: 1993) 2023;45:2195135. [DOI] [PubMed] [Google Scholar]
- 32. Qiu TT, Jiang ZM, Chen XC, et al. Comorbidity of anxiety and hypertension: common risk factors and potential mechanisms. Int J Hypertens 2023;2023:9619388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Allen TS, Bhatia HS, Wood AC, et al. State-of-the-art review: evidence on red meat consumption and hypertension outcomes. Am J Hypertens 2022;35:679–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Harrison DG, Coffman TM, Wilcox CS. Pathophysiology of hypertension: the mosaic theory and beyond. Circ Res 2021;128:847–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lip S, Padmanabhan S. Genomics of blood pressure and hypertension: extending the mosaic theory toward stratification. Can J Cardiol 2020;36:694–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tian Z, Liang M. Renal metabolism and hypertension. Nat Commun 2021;12:963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Louca P, Menni C, Padmanabhan S. Genomic determinants of hypertension with a focus on metabolomics and the gut microbiome. Am J Hypertens 2020;33:473–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Jeong S, Kim JY, Cho Y, et al. Genetically, dietary sodium intake is causally associated with salt-sensitive hypertension risk in a community-based cohort study: a mendelian randomization approach. Curr Hypertens Rep 2020;22:45. [DOI] [PubMed] [Google Scholar]
- 39. van Oort S, Beulens JWJ, van Ballegooijen AJ, et al. Association of cardiovascular risk factors and lifestyle behaviors with hypertension: a mendelian randomization study. Hypertension (Dallas, Tex: 1979) 2020;76:1971–1979. [DOI] [PubMed] [Google Scholar]
- 40. Rizzoni D, Agabiti-Rosei C, De Ciuceis C, et al. Subclinical hypertension-mediated organ damage (hmod) in hypertension: atherosclerotic cardiovascular disease (ASCVD) and calcium score. High Blood Pressure Cardiovasc Prevent 2023;30:17–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Piskorz D. Hypertensive mediated organ damage and hypertension management. How to assess beneficial effects of antihypertensive treatments? High Blood Pressure Cardiovasc Prevent 2020;27:9–17. [DOI] [PubMed] [Google Scholar]
- 42. Młynarczyk M, Kasacka I. The role of the Wnt / β-catenin pathway and the functioning of the heart in arterial hypertension—a review. Adv Med Sci 2022;67:87–94. [DOI] [PubMed] [Google Scholar]
- 43. Li KX, Wang ZC, Machuki JO, et al. Benefits of curcumin in the vasculature: a therapeutic candidate for vascular remodeling in arterial hypertension and pulmonary arterial hypertension? Front Physiol 2022;13:848867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kucmierz J, Frak W, Mlynarska E, et al. Molecular interactions of arterial hypertension in its target organs. Int J Mol Sci 2021;22:9669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Theodoridis X, Chourdakis M, Chrysoula L, et al. Adherence to the dash diet and risk of hypertension: a systematic review and meta-analysis. Nutrients 2023;15:3261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Haghighatdoost F, Hajihashemi P, Romeiro AMD, et al. Coffee consumption and risk of hypertension in adults: systematic review and meta-analysis. Nutrients 2023;15:3060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Surma S, Oparil S. Coffee and arterial hypertension. Curr Hypertens Rep 2021;23:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Madsen H, Sen A, Aune D. Fruit and vegetable consumption and the risk of hypertension: a systematic review and meta-analysis of prospective studies. Eur J Nutr 2023;62:1941–1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wang M, Huang W, Xu Y. Effects of spicy food consumption on overweight/obesity, hypertension and blood lipids in china: a meta-analysis of cross-sectional studies. Nutr J 2023;22:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Szallasi A. The vanilloid (capsaicin) receptor TRPV1 in blood pressure regulation: a novel therapeutic target in hypertension? Int J Mol Sci 2023;24:8769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Borghi C, Tsioufis K, Agabiti-Rosei E, et al. Nutraceuticals and blood pressure control: a european society of hypertension position document. J Hypertens 2020;38:799–812. [DOI] [PubMed] [Google Scholar]
- 52. Hayes P, Ferrara A, Keating A, et al. Physical activity and hypertension. Rev Cardiovasc Med 2022;23:302. [Google Scholar]
- 53. Lu ZH, Song Y, Chen HR, et al. A mixed comparisons of aerobic training with different volumes and intensities of physical exercise in patients with hypertension: a systematic review and network meta-analysis. Front Cardiovasc Med 2022;8:770975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Baffour-Awuah B, Pearson MJ, Dieberg G, et al. Isometric resistance training to manage hypertension: systematic review and meta-analysis. Curr Hypertens Rep 2023;25:35–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Charchar FJ, Prestes PR, Mills C, et al. Lifestyle management of hypertension: International society of hypertension position paper endorsed by the world hypertension league and european society of hypertension. J Hypertens 2024;42:23–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Wu Y, Johnson BT, Acabchuk RL, et al. Yoga as antihypertensive lifestyle therapy: a systematic review and meta-analysis. Mayo Clin Proc 2019;94:432–446. [DOI] [PubMed] [Google Scholar]
- 57. Conversano C, Orrù G, Pozza A, et al. Is mindfulness-based stress reduction effective for people with hypertension? A systematic review and meta-analysis of 30 years of evidence. Int J Environ Res Public Health 2021;18:2882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Yin YK, Yu ZZ, Wang JL, et al. Effects of the different tai chi exercise cycles on patients with essential hypertension: a systematic review and meta-analysis. Front Cardiovasc Med 2023;10:1016629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Guan YY, Hao Y, Guan Y, et al. Effects of tai chi on essential hypertension and related risk factors: a meta-analysis of randomized controlled trials. J Rehabil Med 2020;52:jrm00057. [DOI] [PubMed] [Google Scholar]
- 60. Ojangba T, Boamah S, Miao YD, et al. Comprehensive effects of lifestyle reform, adherence, and related factors on hypertension control: a review. J Clin Hypertens 2023;25:509–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Ahmad H, Khan H, Haque S, et al. Angiotensin-converting enzyme and hypertension: a systemic analysis of various ace inhibitors, their side effects, and bioactive peptides as a putative therapy for hypertension. Je Renin-Angiotensin-Aldosterone Syst JRAAS 2023;2023:7890188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Mancia G, Kjeldsen SE, Kreutz R, et al. Individualized beta-blocker treatment for high blood pressure dictated by medical comorbidities: Indications beyond the 2018 european society of cardiology/european society of hypertension guidelines. Hypertension 2022;79:1153–1166. [DOI] [PubMed] [Google Scholar]
- 63. Cutrell S, Alhomoud IS, Mehta A, et al. Ace-inhibitors in hypertension: a historical perspective and current insights. Curr Hypertens Rep 2023;25:243–250. [DOI] [PubMed] [Google Scholar]
- 64. Khalil ME, Basher AW, Brown EJ, et al. A remarkable medical story: Benefits of angiotensin-converting enzyme inhibitors in cardiac patients. J Am Coll Cardiol 2001;37:1757–1764. [DOI] [PubMed] [Google Scholar]
- 65. Jabbari M, Eini-Zinab H, Safaei E, et al. Determination of the level of evidence for the association between different food groups/items and dietary fiber intake and the risk of cardiovascular diseases and hypertension: an umbrella review. Nutr Res 2023;111:1–13. [DOI] [PubMed] [Google Scholar]
- 66. Wang JG, Palmer BF, Anderson KV, et al. Amlodipine in the current management of hypertension. J Clin Hypertens 2023;25:801–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Zaman MA, Awais N, Satnarine T, et al. Comparing triple combination drug therapy and traditional monotherapy for better survival in patients with high-risk hypertension: a systematic review. Cureus J Med Sci 2023;15:e41398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Lauder L, Mahfoud F, Azizi M, et al. Hypertension management in patients with cardiovascular comorbidities. Eur Heart J 2023;44:2066–2077. [DOI] [PubMed] [Google Scholar]
- 69. Li X, Zhu LJ, Lv J, et al. Purinoceptor: a novel target for hypertension. Purinergic Signal 2023;19:185–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Hoffer-Hawlik M, Moran A, Zerihun L, et al. Telemedicine interventions for hypertension management in low- and middle-income countries: a scoping review. PLoS ONE 2021;16:e025422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Alnooh G, Alessa T, Noorwali E, et al. Identification of the most suitable mobile apps to support dietary approaches to stop hypertension (dash) diet self-management: Systematic search of app stores and content analysis. Nutrients 2023;15:3476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Inoue K, Athey S, Tsugawa Y. Machine-learning-based high-benefit approach versus conventional high-risk approach in blood pressure management. Int J Epidemiol 2023;52:1243–1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Konstantinidis D, Iliakis P, Tatakis F, et al. Wearable blood pressure measurement devices and new approaches in hypertension management: the digital era. J Hum Hypertens 2022;36:945–951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Tsoi K, Yiu K, Lee H, et al. Applications of artificial intelligence for hypertension management. J Clin Hypertens (Greenwich, Conn) 2021;23:568–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Stergiou GS, Mukkamala R, Avolio A, et al. Cuffless blood pressure measuring devices: Review and statement by the european society of hypertension working group on blood pressure monitoring and cardiovascular variability. J Hypertens 2022;40:1449–1460. [DOI] [PubMed] [Google Scholar]
- 76. Stergiou GS, Avolio AP, Palatini P, et al. European society of hypertension recommendations for the validation of cuffless blood pressure measuring devices: European society of hypertension working group on blood pressure monitoring and cardiovascular variability. J Hypertens 2023;41:2074–2087. [DOI] [PubMed] [Google Scholar]
- 77. Padmanabhan S, Tran TQB, Dominiczak AF. Artificial intelligence in hypertension: Seeing through a glass darkly. Circ Res 2021;128:1100–1118. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this work.


