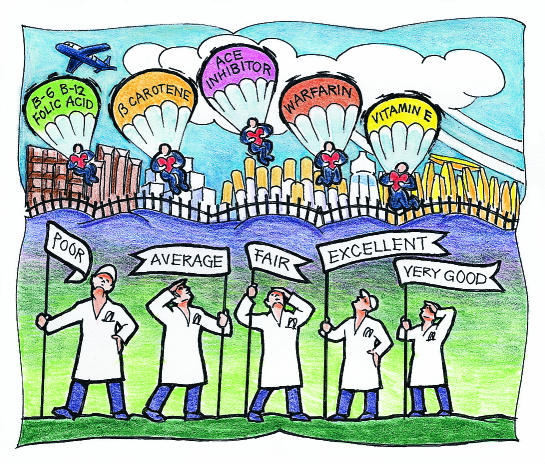
Reducing cholesterol and blood pressure, as well as smoking cessation, have been shown to be effective strategies for preventing cardiovascular diseases.1 However, these “classical” risk factors, along with known non-modifiable risk factors such as age, sex, and family history, cannot fully explain why some people develop myocardial infarction and stroke, while others do not.2–4 Additional factors may have a role in the pathogenesis of atherosclerosis, and new preventive strategies may be of use. In this article we briefly review the use of antioxidants, the use of angiotensin converting enzyme inhibitors, and homocysteine lowering; other “emerging” cardiovascular risk factors and potential preventive strategies that are under investigation are summarised in table 1.
Summary points
Classical risk factors for atherosclerosis cannot fully explain why certain people develop coronary heart disease and stroke, while others do not
Other potential (“emerging”) risk factors for atherosclerosis and new preventive therapies are currently being studied
Promising new preventive therapies include antioxidants, lowering of homocysteine concentrations, decreasing the activation of the renin-angiotensin and the coagulation systems, antibiotics, and anti-inflammatory agents
These therapies have not been proved in clinical trials; at present, the emphasis should be on treating established risk factors and consistently applying therapies that are known to reduce cardiovascular morbidity and mortality
Table 1.
Emerging cardiovascular risk factors and new preventive strategies
| Emerging cardiovascular risk factors | New preventive strategies |
|---|---|
| “Normal” cholesterol, blood pressure, and blood glucose | Lower thresholds of treatment in high risk individuals |
| Oxidation of low density lipoprotein cholesterol | Antioxidants (such as vitamin E) |
| Activation of the renin-angiotensin-aldosterone system | Angiotensin converting enzyme inhibitors |
| Hyperhomocysteinaemia | Folic acid, vitamin B-6, vitamin B-12 |
| Abnormalities of coagulation: | |
| Fibrinogen | New antithrombotic approaches (such as preventive use of warfarin, new antiplatelet drugs) |
| Factor VII | |
| Von Willebrand factor | |
| Plasminogen activator inhibitor-1 | |
| Lipoprotein Lp(a) | Niacin, oestrogens |
| Postmenopausal state | Oestrogens, selective oestrogen receptor modulators |
| Chronic infection and inflammation | Antibiotics, anti-inflammatory agents |
| Genetic abnormalities | “Targeted” treatment aimed at specific genes or their phenotypic expression |
| Nutritional factors | |
| Psychological factors | |
| Environmental factors | |
| Socioeconomic factors |
Oxidative stress and antioxidants
Extensive laboratory data show that oxidative modification of low density lipoprotein cholesterol is an important step in the pathogenesis of atherosclerosis, and experimental studies in different animal models show that antioxidants decrease oxidation of low density lipoprotein cholesterol and reduce plaque formation.5,6
Epidemiological studies have generally reported that increased intake of antioxidants through diet or supplements, particularly vitamins E and C and β carotene, is associated with a lower risk of coronary heart disease.7–9 Other antioxidants, such as other carotenoids, flavonoids, selenium, magnesium, and monounsaturated fat, are also found in natural food products and may reduce oxidation of low density lipoprotein cholesterol. The most compelling results have been with vitamin E supplementation.10–12 However, these epidemiological studies have several methodological limitations. While most observational studies have attempted to “statistically” adjust for other factors that could affect the cardiovascular risk, such adjustments are difficult and not always adequate. Lifestyle and dietary patterns not accounted for could contribute to some of the observed apparent lower cardiovascular risk in people who use supplemental vitamins in comparison to non-users, and similar confounders could bias the results of epidemiological studies evaluating dietary intake of antioxidant vitamins.Therefore, the role of specific vitamins in the prevention of coronary heart disease is best evaluated in randomised clinical trials.
Trials of vitamin E
Three large randomised placebo controlled trials of vitamin E have been completed (table 2). The alpha-tocopherol beta carotene cancer prevention study (ATBC) was designed primarily to assess the effects of daily supplementation with α tocopherol and β carotene on cancer.13 A total of 29 133 Finnish male smokers were randomly assigned to α tocopherol (vitamin E) 50 mg daily or placebo and β carotene 20 mg daily or placebo for 5-7 years. Vitamin E did not prevent death from cardiovascular disease or myocardial infarction. The incidence of angina pectoris was modestly reduced (relative risk reduction=9%, 95% confidence interval 1% to 17%; P=0.04).14 In the subgroup of individuals with previous myocardial infarction, modest benefits on non-fatal coronary events but no effect on cardiac mortality were reported.15 The major limitation of this trial was the vitamin E dose used (50 mg/day), which is much lower than the doses suggested by most of the epidemiological data to be cardioprotective.
Table 2.
Large randomised trials of antioxidant vitamins
| Trial | Study participants | Follow up (years) | Vitamin dose | Outcomes | % Reduction in relative risk (95% CI) |
|---|---|---|---|---|---|
| Trials of vitamin E | |||||
| Alpha-tocopherol, beta carotene cancer prevention study (ATBC)13 14 15 | 29 133 male smokers in Finland | 6.1 | 50 mg/day | Total mortality | −2 (−9 to 5)† |
| Death from cardiovascular disease | 2 (−8 to 11) | ||||
| Angina | 9 (1 to 17) | ||||
| Chinese study16 | 29 584 adults in Linxian province | 5.2 | 30 mg/day* | Total mortality | 9 (0 to 17) |
| Death from cerebrovascular disease | 9 (−8 to 24) | ||||
| Cambridge heart antioxidant study (CHAOS)17 | 2002 patients with coronary artery disease in the United Kingdom | 1.4 | 800 IU or 400 IU/day | Total mortality | −29 (−119 to 24) |
| Death from cardiovascular disease | −10 (−96 to 39) | ||||
| Non-fatal myocardial infarction | 77 (53 to 89) | ||||
| Trials of β carotene | |||||
| Alpha-tocopherol, beta carotene cancer prevention study (ATBC)13 14 | 29 133 male smokers in Finland | 6.1 | 20 mg/day | Total mortality | −9 (−17 to −2)† |
| Death from cardiovascular disease | −11 (−23 to 1) | ||||
| Death from cancer | −9 (−23 to 3) | ||||
| β Carotene and retinol efficacy trial (CARET)18 | 18 314 male smokers, former smokers and workers exposed to asbestos in the United States | 4.0 | 30 mg/day‡ | Total mortality | −17 (−33 to −3) |
| Death from cardiovascular disease | −26 (−61 to 1) | ||||
| Death from cancer | −46 (−100 to −7) | ||||
| Physicians health study (PHS)19 | 22 071 male physicians in the United States | 12.0 | 50 mg/alternate days | Total mortality | −2 (−11 to 7) |
| Death from cardiovascular disease | −9 (−27 to 7) | ||||
| Death from cancer | −2 (−18 to 11) | ||||
| Skin cancer prevention study (SCPS)19a | 1188 men and 532 women in the United States | 8.2 | 50 mg/day | Total mortality | −3 (−30 to 18) |
| Death from cardiovascular disease | −16 (−64 to 18) | ||||
| Death from cancer | 17 (−29 to 56) | ||||
In addition to vitamin E, selenium and β carotene supplements were used.
Minus sign indicates an increased risk.
Patients randomised to β carotene also received 25 000 U/day of retinol (vitamin A)
A second large primary prevention trial conducted in China reported a marginally significant reduction in total mortality (9%, 0% to 70%) for a combination of vitamin E, β carotene, and selenium, with a trend towards reduced cerebrovascular mortality.16 The vitamin E dose was also low (30 mg/day), and the population studied was very different from Western populations, having a lower risk of cardiac events and possibly an overall lower consumption of dietary antioxidants. Furthermore, the study design does not allow the identification of the particular antioxidant that contributed to the reduction in mortality.
The Cambridge heart antioxidant study (CHAOS) is a secondary prevention study of 2002 patients with coronary atherosclerosis randomised to vitamin E 800 IU daily or 400 IU daily or placebo. It reported marked reductions in non-fatal myocardial infarction (77%, 53% to 89%; P<0.001) and in the combined end point of any major cardiovascular event (47%, 17% to 66%; P=0.005).17 Although the results are encouraging, this study has many methodological problems and remains inconclusive. The study groups were not balanced at baseline and follow up may not have been complete. The duration of the study was short (median of 510 days), yet the observed magnitude of benefit with vitamin E was large; the experimental and epidemiological data make such a large effect unlikely. Total mortality was slightly higher in the α tocopherol group than in the placebo group (3.5% v 2.7%, P=0.31). Therefore, it would be premature to conclude that vitamin E use reduces coronary risk, and routine use of vitamin E should await the results of the ongoing large trials.9
Other antioxidants
β Carotene has been evaluated in three large primary prevention trials in men—all of which failed to show any reduction in the risk of cardiovascular events and cancer (table 2).13,18,19 Furthermore, in two studies there were concerns about increased risk of cancer. These data suggest that raised β carotene concentrations may have been a marker associated with other cardioprotective factors.
There have been no large trials of vitamin C supplementation. In a trial of 578 patients admitted to a geriatric hospital, supplementation with 200 mg of vitamin C daily did not reduce mortality at six months.20 In the Chinese trial discussed above there was no reduction in total mortality and in mortality from cerebrovascular disease in people randomised to a combination of vitamin C and molybdenum.16
Probucol is a lipid lowering agent which also reduces high density lipoprotein cholesterol and has potent antioxidant properties. In the probucol quantitative regression Swedish trial (PQRST), probucol failed to retard progression of femoral atherosclerosis.21 More recently a reduction in restenosis rates after coronary angioplasty was reported in a randomised trial of probucol,22 providing renewed interest in this agent, although this study has several limitations and conclusions should await confirmation in additional trials.
Summary
Though it is attractive, the antioxidant hypothesis has not been proved in clinical trials. The most promising data relate to vitamin E, but these are inconclusive and do not warrant its widespread use at present. The strong biological rationale and epidemiological data relating antioxidants to lower cardiovascular risk justify ongoing trials of vitamin E and experimentation with new antioxidant agents in further evaluating this hypothesis.
Impact of angiotensin converting enzyme inhibitors
Experimental and clinical studies show that angiotensin converting enzyme inhibitors may reduce cardiovascular risk through cardioprotective and vasculoprotective effects mediated by blocking both circulating and tissue renin-angiotensin systems, as well as by bradykinin potentiation.23 Angiotensin converting enzyme inhibitors are antiproliferative, have antimigratory effects on smooth muscle cells, improve endothelial function, may act as antioxidants, and act as antithrombotic agents by decreasing platelet aggregation and enhancing endogenous fibrinolysis.23–25 Several epidemiological and genetic studies have shown a link between the renin-angiotensin system and the risk for myocardial infarction,26,27 although these findings were not confirmed in other reports and remain controversial.28,29
Risk reduction
Randomised clinical trials in symptomatic and asymptomatic patients with documented coronary heart disease and left ventricular dysfunction who were treated with angiotensin converting enzyme inhibitors for approximately 40 months showed a significant reduction in the risk of myocardial infarction. Pooled analyses of the five major trials of angiotensin converting enzyme inhibitors in patients with low left ventricular ejection fraction indicate a 23% reduction in the risk for myocardial infarction associated with treatment with angiotensin converting enzyme inhibitors (table 3). In addition, reductions in other ischaemic end points were also significant in treated patients: hospital admissions for unstable angina in the studies of left ventricular dysfunction (SOLVD) trials, 20%, 9% to 29%; P=0.001; revascularisation procedures in the survival and ventricular enlargement trial (SAVE), 24%, 6% to 39%; P=0.01. Because these trials were conducted in patients with low left ventricular ejection fraction or symptomatic heart failure, who were likely to have raised concentrations of renin and angiotensin, these data cannot be extrapolated to other patient populations. However, the reduction in ischaemic events was seen in several different subgroups and was not explained by the haemodynamic action of the angiotensin converting enzyme inhibitors alone. The role of these drugs in preventing myocardial infarction in high risk patients with preserved left ventricular function is under investigation in several large clinical trials.34
SUE SHARPLES
Table 3.
Effects of angiotensin converting enzyme (ACE) inhibitors on myocardial infarction in patients with low ejection fraction
| Trial | Patient characteristics | No (%) with myocardial infarction
|
% Reduction in relative risk (95% CI) |
P value | |
|---|---|---|---|---|---|
| ACE inhibitor | Placebo | ||||
| Acute infarction ramipril efficacy (AIRE)30 | Clinical evidence of heart failure soon after infarct | 81 (8.0) | 88 (8.9) | 9 (−22 to 35)* | >0.05 |
| Trandolapril cardiac evaluation study (TRACE)31 | Left ventricular ejection fraction ⩽35% soon after infarct | 97 (11.1) | 111 (12.7) | 14 (−10 to 31) | >0.05 |
| Studies of left ventricular dysfunction (SOLVD)32: | |||||
| Prevention | Left ventricular ejection fraction ⩽35% without heart failure | 161 (7.6) | 204 (9.1) | 24 (6 to 38) | 0.01 |
| Treatment | Left ventricular ejection fraction ⩽35% with heart failure | 127 (9.9) | 158 (12.3) | 23 (2 to 39) | 0.02 |
| Survival and ventricular enlargement trial (SAVE)33 | Left ventricular ejection fraction ⩽40% soon after infarct | 133 (11.9) | 170 (15.2) | 25 (5 to 40) | 0.05 |
| Total | 23 (11 to 32) | ||||
Long term follow up of the UK component of AIRE (AIREX) showed a significant reduction in fatal myocardial infarctions.
Summary
Angiotensin converting enzyme inhibitors are currently indicated in all patients with clinical manifestations of heart failure and in individuals with asymptomatic left ventricular dysfunction. These agents have also a proved role in the treatment of acute myocardial infarction, hypertension and diabetic nephropathy. The preventive use of angiotensin converting enzyme inhibitors in high risk individuals with preserved left ventricular function, while promising, should await results of ongoing large clinical trials.
Homocysteine and vascular disease
Homocysteine, an amino acid containing sulphur, is produced during catabolism of the essential amino acid methionine. It can be irreversibly degraded by cystathionine β-synthase; the process requires vitamin B-6 as a cofactor. It can be remethylated to conserve methionine in a process requiring methionine synthase and methylcobalamin (vitamin B-12) as a cofactor and methyltetrahydrofolate reductase (MTHFR) as a cosubstrate. This metabolic pathway requires an adequate supply of folate and the enzyme MTHFR. Genetic and acquired abnormalities in the function of these enzymes, or deficiencies in folate or vitamin B-6 or B-12 cofactors, can therefore lead to raised homocysteine concentrations. Extremely high concentrations are accompanied by homocystinuria and are caused by rare genetic enzyme deficiencies. People with these distinct genetic abnormalities typically develop severe premature atherosclerotic and thromboembolic disease, and this led McCully to formulate the homocysteine theory of atherosclerosis.35 More recently, a role for modest increases in homocysteine, caused by a variety of genetic, physiological, pathological, and nutritional factors, has been proposed in the aetiology of atherosclerotic and thromboembolic vascular disease.
Vascular injury has been experimentally induced by homocysteine. Typical features include endothelial dysfunction, due to direct toxic endothelial cell damage and impaired production of nitric oxide, smooth muscle cell proliferation, increased production of reactive oxygen radicals, increased susceptibility of low density lipoprotein cholesterol to oxidation, and increased thrombogenicity.36
Graded relation to risk
A large number of investigations, mostly cross sectional or retrospective case-control epidemiological studies, found associations between raised homocysteine concentrations and increased cardiovascular risk. A meta-analysis of the major epidemiological studies up to 1995 reported a linear, independent relation between homocysteine concentrations and cardiovascular risk.37 Every 5 μmol/l increment in homocysteine was found to be associated with increased risk for coronary artery disease (odds ratio=1.7, 1.5 to 1.9), for cerebrovascular disease (1.5, 1.3 to 1.9) and for peripheral vascular disease (fewer studies available and less robust quantitation of risk). Importantly, a graded risk of adverse cardiovascular events throughout the “normal” range of homocysteine concentrations was shown, suggesting that even people with “normal” homocysteine concentrations might benefit from treatments that lowered homocysteine (a similar relation to cardiovascular risk as cholesterol). More recently the European Concerted Action Project reported an increased relative risk per 5 μmol/l increment in fasting total homocysteine concentration of 1.35 (1.1 to 1.6) for men and 1.42 (0.99 to 2.05) for women,38 and Nygard et al found a strong graded relation between homocysteine concentration and mortality in patients with angiographically confirmed coronary artery disease.39 Low dietary intake as well as low circulating concentrations of folate and vitamins B-6 and B-12 have also been associated with increased cardiovascular risk, presumably due to resultant hyperhomocysteinaemia.40,41 Prospective cohort studies have not always found a consistently clear relation between raised homocysteine concentrations and cardiovascular risk.42
Homocysteine can be easily and effectively reduced by supplementation with folic acid alone or in combination with vitamins B-6 and B-12. These represent very simple, inexpensive, and generally risk free interventions, but clinical trials of homocysteine lowering have not been conducted thus far. Several randomised clinical trials evaluating the impact of folate supplementation alone or combined with vitamin B-6 and B-12 in reducing major clinical cardiovascular events and on progression of atherosclerosis are currently underway.
Summary
The current experimental and epidemiological data suggest that reducing homocysteine concentrations represents an effective, cheap, and simple intervention. Until confirmation from clinical trials is available, it seems prudent to ensure adequate dietary intake of folate and vitamins B-6 and B-12.
Conclusions
This review summarises the evidence on antioxidants, modulating the renin-angiotensin axis, and reducing homocysteine concentrations as potential new preventive cardiovascular interventions. These areas are promising, but definite conclusions must await the results of randomised clinical trials. Other promising preventive strategies include aggressive lowering of blood glucose in diabetic patients and in people with only modest increases in plasma glucose; postmenopausal use of hormone replacement and of selective oestrogen receptor modulators; use of antibiotics; modifcation of determinants of coagulation; enhancing fibrinolysis; lowering lipoprotein Lp(a); and modifying psychosocial factors.
Acknowledgments
This article is adapted from Evidence-Based Cardiology, edited by S Yusuf, J A Cairns, A J Camm, E L Fallen, and B J Gersh, which was published by BMJ Books in 1998.
Footnotes
Competing interests: EML has received reimbursement for presentations (honorarium as speaker) from several companies, including Hoechst Marion Roussel, Parke-Davis, Merck Sharpe Dohme, Fournier, and has attended several symposiums which included a reimbursement fee. She is coprincipal, principal, or coinvestigator on several grants with industry support (Hoechst Marion Roussel, Parke-Davis).
References
- 1.Goldman L, Cook EF. The decline in ischemic heart disease mortality rates. An analysis of the comparative effects of medical interventions and changes in lifestyle. Ann Intern Med. 1984;101:825–836. doi: 10.7326/0003-4819-101-6-825. [DOI] [PubMed] [Google Scholar]
- 2.Gordon T, Garcia-Palmieri MR, Kagan A, Kannel WB, Schiffman J. Differences in coronary heart disease in Framingham, Honolulu and Puerto Rico. J Chron Dis. 1974;27:329–344. doi: 10.1016/0021-9681(74)90013-7. [DOI] [PubMed] [Google Scholar]
- 3.Verschuren WMM, Jacobs DR, Bloemberg BPM, Kromhout D, Menotti A, Aravanis C, et al. Serum total cholesterol and long-term coronary heart disease mortality in different cultures. Twenty-five-year follow-up of the seven countries study. JAMA. 1995;274:131–136. [PubMed] [Google Scholar]
- 4.Kannel WB, Castelli WP, Gordon T. Cholesterol in the prediction of atherosclerotic disease. New perspectives based on the Framingham Study. Ann Intern Med. 1979;90:85–91. doi: 10.7326/0003-4819-90-1-85. [DOI] [PubMed] [Google Scholar]
- 5.Steinberg D. Antioxidants in the prevention of human atherosclerosis. Summary of the proceedings of a National Heart, Lung and Blood Institute workshop: September 5-6, 1991, Bethesda, Maryland. Circulation. 1992;85:2338–2343. doi: 10.1161/01.cir.85.6.2337. [DOI] [PubMed] [Google Scholar]
- 6.Berliner JA, Navab M, Fogelman AM, Frank JS, Demer LL, Edwards PA, et al. Atherosclerosis: basic mechanisms. Oxidation, inflammation and genetics. Circulation. 1995;91:2488–2496. doi: 10.1161/01.cir.91.9.2488. [DOI] [PubMed] [Google Scholar]
- 7.Rimm EB, Ascherio A, Giovannucci E, Spiegelman D, Stampfer MJ, Willett WC. Vegetable, fruit, and cereal fiber intake and risk of coronary heart disease among men. JAMA. 1996;275:447-51. [DOI] [PubMed]
- 8.Jha P, Flather M, Lonn E, Farkouh M, Yusuf S. The antioxidant vitamins (E,C and beta-carotene) and cardiovascular disease: a critical summary of epidemiological and clinical trial data. Ann Intern Med. 1995;123:860–872. doi: 10.7326/0003-4819-123-11-199512010-00009. [DOI] [PubMed] [Google Scholar]
- 9.Lonn EM, Yusuf S. Is there a role for antioxidant vitamins in the prevention of cardiovascular diseases? An update on epidemiological and clinical trials data. Can J Cardiol. 1997;13:957–965. [PubMed] [Google Scholar]
- 10.Stampfer MJ, Hennekens CH, Manson JE, Colditz GA, Rosner B, Willett WC. Vitamin E consumption and the risk of coronary disease in women. N Engl J Med. 1993;328:1444–1449. doi: 10.1056/NEJM199305203282003. [DOI] [PubMed] [Google Scholar]
- 11.Kushi LH, Fulsom AR, Prineas RJ, Mink PJ, Wu Y, Bostick RM. Dietary antioxidant vitamins and death from coronary heart disease in postmenopausal women. N Engl J Med. 1996;334:1156–1162. doi: 10.1056/NEJM199605023341803. [DOI] [PubMed] [Google Scholar]
- 12.Rimm EB, Stampfer MJ, Ascherio A, Giovannucci E, Colditz GA, Willett WC. Vitamin E consumption and the risk of coronary heart disease in men. N Engl J Med. 1993;328:1450–1456. doi: 10.1056/NEJM199305203282004. [DOI] [PubMed] [Google Scholar]
- 13.Alpha-Tocopherol, Beta Carotene Cancer Prevention Study Group. The effect of vitamin E and beta carotene on the incidence of lung cancer and other cancers in male smokers. N Engl J Med. 1994;330:1029–1035. doi: 10.1056/NEJM199404143301501. [DOI] [PubMed] [Google Scholar]
- 14.Rapola JM, Virtamo J, Haukka JK, Heinonen OP, Albanes D, Taylor PR, et al. Effect of vitamin E and beta carotene on the incidence of angina pectoris: a randomized, double-blind, controlled trial. JAMA. 1996;275:693–698. doi: 10.1001/jama.1996.03530330037026. [DOI] [PubMed] [Google Scholar]
- 15.Rapola JM, Virtamo J, Ripatti S, Huttunen JK, Albanes D, Taylor PR, et al. Randomised trial of α-tocopherol and β-carotene supplements on incidence of major coronary events in men with previous myocardial infarction. Lancet. 1997;349:1715–1720. doi: 10.1016/S0140-6736(97)01234-8. [DOI] [PubMed] [Google Scholar]
- 16.Blot WJ, Li JY, Taylor PR, Guo W, Dawsey S, Wang GQ, et al. Nutrition intervention trials in Linxian, China: supplementation with specific vitamin/mineral combinations, cancer incidence, and disease-specific mortality in the general population. J Natl Cancer Inst. 1993;85:1483–1492. doi: 10.1093/jnci/85.18.1483. [DOI] [PubMed] [Google Scholar]
- 17.Stephens NG, Parsons A, Schofield PM, Kelly F, Cheeseman K, Mitchinson MJ, et al. Randomised controlled trial of vitamin E in patients with coronary disease: Cambridge heart antioxidant study (CHAOS) Lancet. 1996;347:781–786. doi: 10.1016/s0140-6736(96)90866-1. [DOI] [PubMed] [Google Scholar]
- 18.Omenn GS, Goodman GE, Thornquist MD, Balmes J, Cullen MR, Glass A, et al. Effects of a combination of beta carotene and vitamin A on lung cancer and cardiovascular disease. N Engl J Med. 1996;334:1150–1155. doi: 10.1056/NEJM199605023341802. [DOI] [PubMed] [Google Scholar]
- 19.Hennekens CH, Buring JE, Manson JE, Stampfer M, Rosner B, Cook NR, et al. Lack of effect of long-term supplementation with beta carotene on the incidence of malignant neoplasms and cardiovascular disease. N Engl J Med. 1996;334:1145–1149. doi: 10.1056/NEJM199605023341801. [DOI] [PubMed] [Google Scholar]
- 19a.Greenberg ER, Bacon JA, Karagas MR, Stukel TA, Nierenberg DW, Stevens MM, et al. Mortality associated with low plasma concentration of beta carotene and the effect of oral supplementation. JAMA. 1996;275:699–703. doi: 10.1001/jama.1996.03530330043027. [DOI] [PubMed] [Google Scholar]
- 20.Wilson TS, Datta SB, Murrell JS, Andrews CT. Relation of vitamin C levels to mortality in a geriatric hospital: a study of the effect of vitamin C administration. Age Aging. 1973;2:163–171. doi: 10.1093/ageing/2.3.163. [DOI] [PubMed] [Google Scholar]
- 21.Walldius G, Erikson U, Olsson AG, Bergstrand L, Hadell K, Johansson J, et al. The effect of probucol on femoral atherosclerosis: the probucol quantitative regression Swedish trial (PQRST) Am J Cardiol. 1994;74:875–883. doi: 10.1016/0002-9149(94)90579-7. [DOI] [PubMed] [Google Scholar]
- 22.Rodes J, Cote G, Lesperance J, Bourassa MG, Doucet S, Bilodeau L, et al. Prevention of restenosis after angioplasty in small coronary arteries with probucol. Circulation. 1998;97:429–436. doi: 10.1161/01.cir.97.5.429. [DOI] [PubMed] [Google Scholar]
- 23.Lonn EM, Yusuf S, Prabhat J, Montague TJ, Teo KK, Benedict CR, et al. Emerging role of angiotensin-converting enzyme inhibitors in cardiac and vascular protection. Circulation. 1994;90:2056–2069. doi: 10.1161/01.cir.90.4.2056. [DOI] [PubMed] [Google Scholar]
- 24.Mancini GBJ, Henry GC, Macaya C, O’Neill BJ, Pucillo AL, Carere RG, et al. Angiotensin-converting enzyme inhibition with quinapril improves endothelial vasomotor dysfunction in patients with coronary artery disease. The TREND (Trial on Reversing ENdothelial Dysfunction) study. Circulation. 1996;94:258–265. doi: 10.1161/01.cir.94.3.258. [DOI] [PubMed] [Google Scholar]
- 25.Wright RA, Flapan AD, Alberti KG, Ludlam CA, Fox KAA, et al. Effects of captopril therapy on endogenous fibrinolysis in men with recent uncomplicated myocardial infarction. J Am Coll Cardiol. 1994;24:67–73. doi: 10.1016/0735-1097(94)90543-6. [DOI] [PubMed] [Google Scholar]
- 26.Cambien F, Poirier O, Lecerf L, Evans A, Cambou J-P, Arveller D, et al. Deletion polymorphism in angiotensin-converting enzyme gene associated with parental history of myocardial infarction. Nature. 1992;359:641–644. doi: 10.1038/359641a0. [DOI] [PubMed] [Google Scholar]
- 27.Alderman MH, Madhavan SH, Ooi WL, Cohen H, Sealey JE, Laragh JH, et al. Association of the renin-sodium profile with the risk of myocardial infarction in patients with hypertension. N Engl J Med. 1991;324:1098–1104. doi: 10.1056/NEJM199104183241605. [DOI] [PubMed] [Google Scholar]
- 28.Meade TW, Cooper JA, Peart WS. Plasma renin activity and ischemic heart disease. N Engl J Med. 1993;329:616–619. doi: 10.1056/NEJM199308263290905. [DOI] [PubMed] [Google Scholar]
- 29.Samani NJ, Thompson JR, O’Toole L, Channer K, Woods KL. A meta-analysis of the associations of the deletion allele of the angiotensin-converting enzyme gene with myocardial infarction. Circulation. 1996;94:708–712. doi: 10.1161/01.cir.94.4.708. [DOI] [PubMed] [Google Scholar]
- 30.Acute Infarction Ramipril Efficacy (AIRE) Study Investigators. Effect of ramipril on mortality and morbidity of survivors of acute myocardial infarction with clinical evidence of heart failure. Lancet. 1993;342:821–828. [PubMed] [Google Scholar]
- 31.Kober L, Torp-Peterson C, Carlsen JE, Bagger H, Eliasen P, Lyngborg K, et al. for the Trandolapril Cardiac Evaluation (TRACE) Study Group. A clinical trial of the angiotensin-converting enzyme inhibitor trandolapril in patients with left ventricular dysfunction after myocardial infarction N Engl J Med 19953331670–1676. [DOI] [PubMed] [Google Scholar]
- 32.Rutherford JD, Pfeffer MA, Moye LA, Davis BR, Flaker GC, Kowey PR, et al. on behalf of the SAVE investigators. Effects of captopril on ischemic events after myocardial infarction. Results of the survival and ventricular enlargement trial Circulation 1994901731–1738. [DOI] [PubMed] [Google Scholar]
- 33.Yusuf S, Pepine CJ, Garces C, Pouleur H, Salem D, Kostis J, et al. Effect of enalapril on myocardial infarction and unstable angina in patients with low ejection fractions. Lancet. 1992;340:1173–1178. doi: 10.1016/0140-6736(92)92889-n. [DOI] [PubMed] [Google Scholar]
- 34.Yusuf S, Lonn EM. Anti-ischemic effects of ACE-inhibitors: Review of current clinical evidence and ongoing clinical trials. Eur Heart J. 1998;19(suppl J):J36–J44. [PubMed] [Google Scholar]
- 35.McCully KS, Wilson RB. Homocysteine theory of arteriosclerosis. Atherosclerosis. 1975;22:215–227. doi: 10.1016/0021-9150(75)90004-0. [DOI] [PubMed] [Google Scholar]
- 36.Mayer EL, Jacobson DW, Robinson K. Homocysteine and coronary atherosclerosis. J Am Coll Cardiol. 1996;27:517–527. doi: 10.1016/0735-1097(95)00508-0. [DOI] [PubMed] [Google Scholar]
- 37.Boushey CJ, Beresford SAA, Omenn GS, Motulsky AG. A quantitative assessment of plasma homocysteine as a risk factor for vascular disease. Probable benefits of increasing folic acid intakes. JAMA. 1995;274:1049–1057. doi: 10.1001/jama.1995.03530130055028. [DOI] [PubMed] [Google Scholar]
- 38.Graham IM, Daly LE, Refsum HM, Robinson K, Brattstrom LE, Ueland PM, et al. Plasma homocysteine as a risk factor for vascular disease. JAMA. 1997;277:1775–1781. doi: 10.1001/jama.1997.03540460039030. [DOI] [PubMed] [Google Scholar]
- 39.Nygard O, Nordrehaug JE, Refsum HM, Ueland PM, Farstad M, Vollset SE. Plasma homocysteine levels and mortality in patients with coronary artery disease. N Engl J Med. 1997;337:230–236. doi: 10.1056/NEJM199707243370403. [DOI] [PubMed] [Google Scholar]
- 40.Rimm EB, Willett WC, Hu FB, Sampson L, Colditz GA, Manson JE, et al. Folate and vitamin B6 from diet and supplements in relation to risk of coronary heart disease in women. JAMA. 1998;279:359–364. doi: 10.1001/jama.279.5.359. [DOI] [PubMed] [Google Scholar]
- 41.Robinson K, Arheart K, Refsum H, Brattstrom L, Boers G, Ueland P, et al. for the European COMAC Group. Low circulating folate and vitamin B6 concentrations. Risk factors for stroke, peripheral vascular disease and coronary artery disease Circulation 199897437–443. [DOI] [PubMed] [Google Scholar]
- 42.Danesh J, Lewington S. Plasma homocysteine and coronary heart disease: systematic review of published epidemiological studies. J Cardiovasc Risk. 1998;5:229–232. [PubMed] [Google Scholar]