Abstract
The oral squamous cell carcinoma (OSCC) 5 year survival rate of 41% has marginally improved in the last few years, with less than a 1% improvement per year from 2005 to 2017, with higher survival rates when detected at early stages. Based on histopathological grading of oral dysplasia, it is estimated that severe dysplasia has a malignant transformation rate of 7%–50%. Despite these numbers, oral dysplasia grading does not reliably predict its clinical behavior. Thus, more accurate markers predicting oral dysplasia progression to cancer would enable better targeting of these lesions for closer follow‐up, especially in the early stages of the disease. In this context, molecular biomarkers derived from genetics, proteins, and metabolites play key roles in clinical oncology. These molecular signatures can help predict the likelihood of OSCC development and/or progression and have the potential to detect the disease at an early stage and, support treatment decision‐making and predict treatment responsiveness. Also, identifying reliable biomarkers for OSCC detection that can be obtained non‐invasively would enhance management of OSCC. This review will discuss biomarkers for OSCC that have emerged from different biological areas, including genomics, transcriptomics, proteomics, metabolomics, immunomics, and microbiomics.
Keywords: biomarkers, genomics, human papilloma virus (HPV), immunomics, metabolomics, microbiomics, OPMD, oral potentially malignant disorders, oral squamous cell carcinoma, OSCC, proteomics
1. INTRODUCTION
Oral squamous cell carcinoma (OSCC) is the most common oral cancer type, accounting for about 90% of all oral cancer cases. 1 , 2 , 3 The OSCC 5 years survival rate of 41% has marginally improved in the last few years, with less than a 1% improvement per year from 2005 to 2017. 4 , 5 Conversely, when OSCC is detected in the early stages, the survival rates increase to >85%, highlighting the importance of early detection and need for early biomarkers. Unfortunately, almost half of OSCC cases worldwide are diagnosed at later stages. 6 , 7 Primary risk factors for OSCC include tobacco use and heavy alcohol consumption 8 and the presence of oral potentially malignant disorders (OPMDs). 9 , 10 , 11 OPMDs are a group of lesions that “carry a risk of cancer development in the oral cavity, whether in a clinically definable precursor lesion or in clinically normal mucosa”, 12 with oral leukoplakia being the most frequent OPMD. 13 Based on histopathological grading of oral dysplasia, it is estimated that severe dysplasia has a malignant transformation rate of 7%–50%, followed by moderate dysplasia (3%–15%) and mild dysplasia (<5%). 10 Despite these numbers, oral dysplasia grading does not reliably predict its clinical behavior and is by nature imprecise, with a high intra‐ and inter‐observer variability in diagnosis, 14 , 15 making it currently impossible to predict accurately which dysplastic lesions will progress to OSCC. 16 Thus, more accurate markers predicting oral dysplasia progression to cancer would enable better targeting of these lesions for closer follow‐up, especially in the early stages of the disease. 16
In this context, molecular biomarkers derived from genetics, proteins, metabolites, autoantibodies and microbiome play key roles in clinical oncology (Figure 1). These molecular signatures can help predict the likelihood of OSCC development and/or progression and have the potential to detect the disease at an early stage, and support treatment decision‐making and predict treatment responsiveness. 17 Also, identifying reliable biomarkers for OSCC detection that can be obtained noninvasively would enhance management of OSCC. This review will discuss biomarkers for OSCC that have emerged from different biological areas, including genomics, transcriptomics, proteomics, metabolomics, immunomics and microbiomics and their tissue/cell or biofluid of origin.
FIGURE 1.
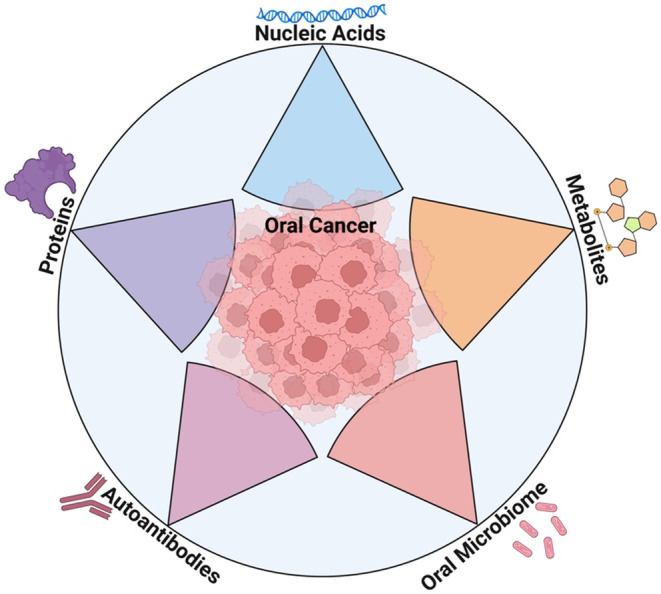
Biological biomarkers of oral cancer.
2. NUCLEIC ACID‐BASED BIOMARKERS
2.1. Genomics
The growing development of molecular technology has made it possible to use nucleic acid molecules as potential noninvasive diagnostic biomarkers, as genetic materials can be amplified from trace amounts, enabling highly specific detection via the pairing of complementary nucleotides. 18 In fact, genetic materials‐based diagnostics has become the gold standard for many diseases and it was fundamental for effective coronavirus disease 2019 (COVID‐19) disease control during the 2020 pandemic. 18 , 19
Besides standard cellular genetic materials, it is now possible to detect and isolate cancer stem cells (CSCs) and circulating tumor cells (CTCs) from a background of normal cells in blood 20 , 21 , 22 , 23 , 24 ; Exosomes, extracellular vesicles released by normal and tumor cells into the bloodstream, which can contain tumor‐specific proteins and nucleic acids 21 , 22 , 25 ; or even cell‐free nucleic acids, fragmented nucleic acids released into the bloodstream through apoptosis or necrosis, which includes cell‐free DNA (cfDNA) and cell‐free RNA (cfRNA). In patients with cancer, cfDNA that is released from tumor cells is often referred to as circulating tumor DNA (ctDNA). 20 , 21 , 22 , 26 Table 1 summarizes the recent studies in the literature.
TABLE 1.
Nucleic acid‐based biomarkers of OSCC.
| Author/Year | Sources of biomarkers | Type of markers | Method | Sample size | Potential Biomarkers | Expression in OSCC |
|---|---|---|---|---|---|---|
| Genomic biomarkers for HPV‐positive OSCC | ||||||
| Campo et al. 157 | Plasma | HPV cfDNA | Systematic review and Meta‐analysis | 457 | cfHPV DNA | Increased in OSCC compared to control |
| Tang et al. 158 | Saliva | HPV DNA | Nested PCR | 650 | HPV16 | Increased in OSCC compared to control |
| Rosenthal et al. 29 | Saliva | HPV DNA | qPCR and Cobas® HPV Test | 45 | fHPV16, p16INK4a | Increased in OSCC compared to control |
| Rettig et al. 159 | Plasma | HPV ctDNA | Droplet Digital PCR | 110 | ctHPV DNA16, 18, 31, 33, and 35 | Increased in OSCC compared to control |
| Cao et al. 160 | Plasma | HPV ctDNA | Droplet Digital PCR | 34 | HPV ctDNA | Increased in OSCC compared to control |
| Haring et al. 161 | Plasma | HPV ctDNA | Droplet Digital PCR | 12 | ctHPV16 DNA | Increased in OSCC compared to control |
| Veyer et al. 162 | Plasma | HPV ctDNA | Droplet Digital PCR | 66 | ctHPV16 DNA | Increased in OSCC compared to control |
| Reder et al. 163 | Plasma | HPV cfDNA | qPCR | 50 | HPV oncogenes E6 and E7 | Increased in OSCC compared to control |
| Mazurek et al. 30 | Plasma | HPV cfDNA | qPCR | 263 | cfHPV‐DNA | Increased in OSCC compared to control |
| Chera et al. 164 | Plasma | HPV ctDNA | Digital droplet PCR | 218 | ctHPV16 DNA | Increased in OSCC compared to control |
| Lee et al. 165 | Plasma | HPV ctDNA | RT‐qPCR | 55 | ctHPV16 DNA | Increased in OSCC compared to control |
| Simoens et al. 166 | Tissue | HPV DNA | RT‐PCR | 99 | E6/E7 + P16(INK4a) | 30.9% prevalence in OSCC |
| Gillison et al. 31 | Tissue | Gene Mutations | Whole genome sequencing | 484 | PIK3CA, ZNF750, FGFR3, CASZ1, PTEN, CYLD, and DDX3X | Increased gene mutation frequency in HPV‐positive OSCC, compared to HPV‐negative OSCC |
| TP53, FAT1, CDKN2A, NOTCH1, CASP8, and HRAS | Increased gene mutation frequency in HPV‐negative OSCC, compared to HPV‐positive OSCC | |||||
| Genomic biomarkers for HPV‐negative OSCC | ||||||
| Yang et al. 167 | Saliva | ctDNA mutations | Review article | 274 | TP53, CDKN2A, PIK3CA, FAT1, and NOTCH1 | Increased in OSCC compared to control |
| Puttipanyalears et al. 168 | Saliva | Gene methylation | RT‐PCR | 24 | Thyroid Releasing Hormone gene cg01009664 | Increased in OSCC compared to control |
| D'Cruz et al. 169 | Oral Rinse | Gene mutations | PCR | 15 | TP53 | Two identified mutations; 67% of the patients had codon 72 polymorphisms |
| Shanmugam et al. 170 | Oral Rinse | Gene expression | Digital Droplet PCR | 121 | TP53, CDKN2A, FAT1, CASP8, NOTCH1, HRAS and PIK3CA | 87.6% of the samples presented at least 1 mutation on the genes |
| Wise‐Draper et al. 33 | Plasma | Gene expression | ELISA | 36 | DEK | Decreased in poor prognosis compared to control |
| Schneider et al. 171 | Tissue | Gene expression | TCGA Database Analysis | 499 | GRP78/BiP | Increased gene expression in OSCC compared to control and associated with poor patient survival |
| Sato et al. 172 | Tissue | Protein expression | Immunohistochemistry | 32 | Casein kinase 1ε (cK‐1ε) and CD44 | Downregulated in OSCC compared to control |
| Differentiated embryonic chondrocyte gene 1 (DEC1) | Upregulated in OSCC compared to control | |||||
| Wilde et al. 173 | Tissue | Protein expression | Immunohistochemistry | 297 | p16 | Increased in OSCC compared to control |
| Shieu et al. 174 | Tissue | Single‐Nucleotide Polymorphisms | RT‐qPCR | 568 | Lysine methyltransferase 2C (KMT2C) SNPs rs4725443 and rs6943984 | TC or TC + CC genotype of rs4725443 > TT genotype. |
| Shi et al. 175 | Tissue | Gene expression | TCGA and GEO databases | 520 | SEC61G | Increased in OSCC compared to control |
| Rapado‐González et al. 176 | Tissues, blood and saliva | cfDNA | qPCR | 34 | ALU60 | Increased in OSCC patients compared to control, but not statistically significant |
| Burcher et al. 177 | Tissue/Blood | DNA Damage Repair gene mutation | ELISA | 170 | BRCA1, BRCA2, ATM, PALB2, ARID1A and CDK12 | Increased in OSCC compared to control |
| Shi et al. 32 | Cell line derived from an oral cancer‐induced mouse model | Gene Mutation | Whole‐exome sequencing (WES), | N/A | TP53, Fat1, Notch1, Kmt2d, Fat3, and Fat4 | TP53 mutations have 75%–85% prevalence in OSCC |
| Arora et al. 178 | Databases and in vitro | Gene expression | Bioinformatics | 545 | TFRC and NCBP2 | Increased in OSCC compared to control; NCBP2 depletion reduced OSCC cell proliferation, migration, and invasion |
| Yang et al. 179 | Databases | Gene dysregulation | Bioinformatics | 335 | SPP1, FN1, CXCL8, BIRC5, PLAUR, and AURKA | Upregulated in OSCC compared to Control |
| TEX101, DSG2, SCG5, ADA, BOC, SCARA5, FST, SOCS1, and STC2 | Can be utilized to predict prognosis of OSCC patients | |||||
| Transcriptomic biomarkers | ||||||
| Dioguardi et al. 180 | Tissue | MicroRNAs | Systematic review and Meta analysis | 708 | miR‐21 | Upregulated in OSCC compared to control; Aggregated Hazard Ratio 1.29 |
| Xie & Wu 181 | Tissue | MicroRNA | Systematic Review and Meta analysis | 777 | miR‐21 | Upregulated in OSCC compared to control; Aggregated Hazard Ratio 1.93; |
| Niklander et al. 182 | Tissue, In vivo and In vitro | MicroRNAs | Systematic Review | N/D | miR‐21, mir‐146a, miR‐181b, miR‐184, miR‐345 | Increased in OSCC compared to control and oncogenic |
| miR‐375 | Downregulated and tumor suppressor | |||||
| Palaia et al. 34 | N/D | MicroRNA | Systematic Review | 3102 | miR‐16‐let‐7b, miR‐21, miR‐24, miR‐24‐3p, miR‐27a‐3p, miR‐27b, miR‐31, miR‐92b, miR‐136, miR‐147, miR‐148a, miR‐150‐5p, miR‐155, miR‐181a, miR181b, miR‐184, miR‐187, miR‐191, miR‐196a, miR‐196b, miR‐200b‐2p, miR‐210, miR‐220a, miR‐223, miR‐323‐5p, miR‐412‐3p, miR‐423‐5p, miR‐483‐5p, miR‐494, miR‐503, miR‐512‐3p, miR‐626, miR‐632, miR‐646, miR‐668, miR‐887, miR‐1250, miR‐3262, miR‐3651, miR‐5100 | Upregulated in OSCC compared to control |
| miR‐let‐7d, miR‐9, miR‐29a, miR‐30a‐5p, miR‐99a, miR‐125a, miR‐139‐5p, miR‐145, miR‐186, mir‐200a, miR‐223, miR‐223‐3p, miR‐320a, miR‐338‐3p, miR‐758, miR‐769‐5p | Downregulated in OSCC compared to control | |||||
| Troiano et al. 183 | Blood, Serum, and Plasma | MicroRNA | Systematic Review | 1586 | miR‐21, miR‐455‐5p, miR‐155‐5p, miR‐372, miR‐373, miR‐29b, miR‐1246, miR‐196a, and miR‐181 | Upregulated in OSCC compared to control |
| miR‐204, miR‐101, miR‐32, miR‐20a, miR‐16, miR‐17, and miR‐125b | Downregulated in OSCC compared to control | |||||
| Scholtz et al. 36 | Saliva | MicroRNAs | RT‐qPCR | 87 | miR‐345 miR‐31‐5p, and miR‐424‐3p miR‐21 miR‐184 miR‐191 | Upregulated in OSCC compared to control |
| Shen et al. 184 | Tissue | MicroRNA | RT‐qPCR | 70 for miR and 50 for target genes | miR‐21‐5p | Upregulated in OSCC compared to control |
| ADH7 gene | Downregulated in OSCC compared to control | |||||
| Robison et al. 185 | Tissue | MicroRNAs | RT‐qPCR | 16 | miR‐155, miR‐196a, miR‐375, and miR‐221 | Upregulated in OSCC compared to control; Gender bias toward lymphatic invasion in lesions presenting around the perineal and abdominal regions |
| Shan et al. 186 | Tissue | Long Noncoding RNA | RT‐PCR | 368 | M6A‐related lncRNAs HMOX1, NFE2L2, NOS2, NOS3, and TP53 | Downregulated in OSCC compared to control; Oxidative Stress in Oral Cancer |
| Rajthala et al. 187 | Tissue and OSCC‐derived cancer‐associated fibroblasts | MicroRNAs | In Situ Hybridization and miRNA Semi‐Quantification. | 50 tissues +18 OSCC‐derived cancer‐associated fibroblasts | miR‐138 | Downregulated in OSCC compared to control |
| Qin et al 188 | Tissue and In vitro | MicroRNAs | RT‐qPCR and Western blot. | 60 tissues +6 cell lines | miR‐32‐5p | Upregulated in OSCC compared to control |
| Jia et al. (2021) 37 | Tissue, In vivo PDX and In vitro | Circulating RNA | RT‐qPCR | 100 | circFAT1, circ_0000231, circ_0001742, circ_0000264, circ_0002837, circ_0007976 | Increased in OSCC compared to Control. CircFAT1 promotes cancer stemness and immune evasion by promoting STAT3 activation. |
| Extracellular Vesicles‐Omics | ||||||
| Saito et al. 189 | N/A | Oncogene | Review | N/A | NANOG and SOX | Increased in OSCC compared to control |
| Benecke et al. 39 | Plasma | Extracellular vesicles markers | Flow Cytometry | 21 | CD9, CD63, CD81 and TSG101 | Increased in OSCC compared to control |
| Zhuang et al. 40 | In vitro and In vivo | Exosomal MicroRNAs | Exosomal miRNAs sequencing | N/A | miR‐1246 and miR‐205 | Upregulated in OSCC compared to control |
| Wu et al. 41 | In vitro and In vivo | MicroRNAs | RT‐qPCR | N/A | Cancer stem cell small extracellular vesicles, M2‐tumor‐associated macrophages | Increased in OSCC compared to control |
| Cancer Stem Cells and Circulating Tumor Cell markers | ||||||
| Fukumoto et al. 24 | N/A | Cancer Stem Cells | Review | N/A | OCT4, NANOG, and SOX2 | No specific markers for OSCC CSC other than those of general embryonic stem cells |
| Varun et al. 45 | N/A | Cancer Stem Cells | Review | N/A | OCT4, SOX2, NANOG, ALDH1, CD44, CD24, CD133 and Musashi‐1 | Display CSC characteristics |
| Rodini et al. 42 | N/A | Cancer Stem Cells | Review | N/A | CD44 and ALDH1 | Display CSC characteristics; Majority of OSCC CSC isolations performed with CD44 marker |
| Baillie et al. 190 | N/A | Cancer Stem Cells | Review | N/A | OCT4, NANOG, SOX2, STAT3, CD44, CD24, CD133, Musashi‐1, ALDH1, PRR, ATR1 and ATR2 | Display CSC characteristics |
| Philouze et al. 191 | Tissue | Cancer Stem Cells | Immunohistochemistry | 28 | CD44, gamma‐H2AX, and p‐ATM | Display CSC characteristics |
| Ma et al. 46 | Tissue | Cancer Stem Cells | Magnetic‐activated cell sorting | 6 | CD133, NANOG, SOX2, ALDH1A1, and OCT4 | Display CSC characteristics; CD133 is negatively correlated with OSCC patients' survival |
| Curtin et al. 55 | N/A | Circulating Tumor Cells | Systematic review | N/A | N/A | CTCs does not appear to be related to tumor differentiation or size; CTCs may be prognostic for both disease‐free survival and overall survival |
| Qayyumi et al. 52 | Blood | Circulating Tumor Cells | Immuno‐magnetic beads separation | 192 | N/A | Progressively increased counts of CTC cells as OSCC progresses from stage I to IV. CTC detection Sensitivity ‐ 94.32%, CTC detection specificity ‐ 98%, and CTC detection accuracy ‐ 95.17% |
| Wang et al. 192 | Blood | Circulating Tumor Cells | Flow cytometry | 53 | N/A | CTC counts were significantly reduced within 2–4 weeks of chemoradiation |
| Morgan et al. 53 | Blood | Circulating Tumor Cells | Surface‐enhanced Raman scattering nanoparticle‐based separation | 125 | N/A | Higher CTC counts associated with survival. CTC count of 675 defined as threshold between OSCC recurrence and distant disease, with sensitivity of 69%, and specificity of 68%. |
| Chang et al. 54 | Blood | Circulating Tumor Cells and circulating Cancer Stem Cells | Flow cytometry | 34 | N/A | Overall survival associated with higher CTC counts; Higher CSC ratio predicted disease progression within the first 3 months of chemotherapy. |
| Fanelli et al. 193 | Blood | Circulating Tumor Cells | Filtration and immunocytochemistry | 53 | TGF‐β Receptor I | Expression correlated with poor progression‐free survival |
Both cfDNA in plasma 27 and ctDNA in saliva 28 have shown promise as DNA biomarkers for human papillomavirus (HPV)‐positive OSCC patients. DNA biomarkers play an important role in OSCC detection and they can be used to detect both HPV‐positive and HPV‐negative OSCC. For HPV‐positive OSCC, the HPV DNA can be extracted from liquid biopsies, such as saliva and plasma. HPV ctDNA from oral rinses can be used to detect oropharyngeal cancers including OSCC with a 94% specificity and 78% sensitivity. 29 In addition to the ctDNA in saliva, HPV cell free DNA (cfDNA) in the plasma can be used to detect OSCC with a specificity of 100% and sensitivity of 72%. 30 Therefore, ctDNA and cfDNA have been used to diagnose the disease, predict prognosis, and monitor treatment outcomes.
Comparing HPV‐positive with HPV‐negative gene mutations in OSCC cases, Gillison et al. 31 reports increased frequencies on phosphatidylinositol‐4,5‐bisphosphate 3‐kinase catalytic subunit alpha (PIK3CA), zinc finger protein 750 (ZNF750), fibroblast growth factor receptor 3 (FGFR3), castor zinc finger 1 (CASZ1), phosphatase and tensin homolog (PTEN), CYLD lysine 63 deubiquitinase (CYLD) and DEAD‐box helicase 3 X‐linked (DDX3X) genes in HPV‐positive cases, whereas HPV‐negative OSCC cases presented increased frequencies on tumor protein p53 (TP53), FAT atypical cadherin 1 (FAT1), cyclin dependent kinase inhibitor 2A (CDKN2A), notch receptor 1 (NOTCH1), caspase 9 (CASP8), HRas proto‐oncogene, and GTPase (HRAS) genes. Shi et al. 32 also validates increased TP53 gene mutations in 75%–85% of HPV‐negative head and neck squamous cell carcinomas (HNSCC), including OSCCs compared to controls.
2.2. Transcriptomics
In addition to genetic mutations, changes in gene expression levels and profiles, also known as the transcriptome, have also served as biomarkers for OSCC. 33 For example, the DEK proto‐oncogene (DEK), a known oncogene, was shown to modulate the chromatin structure and remodel proteins. HPV‐negative status and advanced tumor stage in HNSCC patients were found in conjunction with a downregulation in plasma DEK oncogene levels. 33 Besides changes in genetic expression, epigenetic modifications, such as alterations in DNA methylation patterns, can also be used as biomarkers for OSCC. Palaia et al. 34 reported that the differentially methylated CpG site, cg01009664, of the thyrotropin‐releasing hormone (TRH) gene had a sensitivity of 82.61% and specificity of 92.59%, as assessed via bioinformatic approaches, and demonstrated the potential of epigenetic modifications as biomarkers for OSCC diagnosis.
RNA biomarkers, including microRNAs (miR) are known to serve an oncogenic or suppressor functions for their target genes under certain conditions, 35 and their up‐ or down‐regulation can used for prediction of OSCC prognosis. For example, miR‐345 and miR‐31‐5p are upregulated in OSCC patients. 36 By influencing mRNA translation and transcript degradation, microRNA expression can further influence its target gene expression through a common axis. Therefore, microRNA upregulation and downregulation has been used to make predictions about good or poor prognosis of OSCC. 34 Recently, Jia et al. 37 determined that circular RNA for FAT1 (circFAT1,) is specifically expressed in OSCC, but not in normal adjacent epithelial tissues. CircFAT1 was significantly increased in human OSCC with lymph node metastasis compared with human OSCC without lymph node metastasis. Importantly, they found that circFAT1 promotes cancer stemness and immune evasion through enhancing signal transducer and activator of transcription 3 (STAT3) activation, suggesting that circFAT1 is not only a biomarker for OSCC but also an important therapeutic target.
2.3. Multi‐omics of extracellular vesicles
Extracellular vesicles (EVs)—vesicles released by cells to communicate with other cells 38 —have also been demonstrated to be a powerful source of biomarkers for OSCC detection. For instance, Benecke et al. 39 report significantly elevated levels of tumor‐derived extracellular vesicles positive for PanEV makers (tetraspanins CD9, CD63, and CD81) in OSCC patients compared to healthy controls. Additionally, EVs carry nucleic acids and proteins as their cargo, which may be useful as biomarkers. 38 MiRs carried in EVs are altered in OSCC patients and have been used to detect OSCC. 40 , 41
2.4. Cancer stem cells (CSC) and circulating tumor cells (CTC)
Cancer stem cells (CSCs) are a subset of cancer cells that have characteristics of stem cells, such as self‐renewal and asymmetrical cell division, which can produce heterogeneous populations of cancer cells. Further, CSCs show greater malignant potential, such as higher anti‐apoptosis activity, invasiveness, metastatic potential, chemo‐resistance, and survivability compared to other subsets of cancer cells. 24
In OSCC, it has been reported that CSCs play important roles in the development and progression of the disease. 24 , 42 , 43 , 44 Yet, no specific markers defining CSCs in OSCC have been found to date, and thus, the majority of CSC isolated from oral cancers have mainly been based on the P‐glycoprotein 1 (CD44) marker, which is also a marker for breast CSC, or other generic embryonic stem cell markers, such as octamer‐binding transcription factor 4 (OCT4), nanog homeobox (NANOG), and SRY‐box transcription factor 2 (SOX2). 24 , 45 In addition, Ma et al. 46 isolated OSCC cells positive and negative for prominin‐1 (CD133) and reports that CD133‐positive cells presented higher growth rate, self‐renewal, cisplatin resistance in vitro, and stronger tumourigenic potential in vivo compared to those negative for CD133.
Circulating tumor cells (CTCs) are cells that actively or passively detach themselves from a primary tumor and pass through the bloodstream. Various spontaneous or iatrogenic factors are implicated in this process and, thus CTCs showcase tumor heterogeneity without the need for an invasive tissue biopsy. 47 , 48 , 49 Since CTCs can be quickly eliminated by several different processes, such as immune attacks, shear stress, cell death due to loss of contact with the extracellular matrix or neighboring cells (anoikis), oxidative stress and the lack of cytokines and growth factors, they undergo a series of adaptations in order to survive. These adaptations include losing the expression of epithelial cellular adhesion molecule (EpCAM), keratins, and E‐cadherin and upregulating matrix metalloproteinase (MMP) activity, which enables these cells to navigate through the local extracellular matrix and enter the microvasculature. 50 , 51
In OSCC, Qayyumi et al. 52 demonstrate progressive increased counts of CTC cells as OSCC progresses from stage I to IV. Remarkably, the authors also demonstrate that CTC cells have a very high detection sensitivity and specificity (94% and 98%, respectively), leading to an overall detection accuracy of 95%. Counterintuitively, Morgan et al. 53 and Chang et al. 54 report higher CTC counts were associated with overall survival. In this context, Curtin et al. 55 performed a systematic review of the literature and found that the presence of CTCs does not appear to be related to tumor differentiation or size. Additionally, the authors point out that specific CTC results for oral cancer patients were either inconsistent or mixed with data from other anatomical sites and pathologies within the head and neck. Given the increasing evidence suggesting that CTCs have diagnostic and prognostic potential as biomarkers for OSCC, there is a clear need for studies that can elucidate the relevance of CTCs in OSCC. 55
3. PROTEIN‐BASED BIOMARKERS FOR OSCC
Over 2200 different proteins have been cataloged in saliva, which is close to the amount of proteins found in plasma (over 2600), thus making both fluids potential sources of biomarkers for OSCC. 56 , 57 , 58 Table 2 summarizes the recent studies in the literature.
TABLE 2.
Protein‐based biomarkers for OSCC.
| Author/Year | Source of biomarkers | Method | Sample size | Proteins identified | Findings |
|---|---|---|---|---|---|
| Riccardi et al. 57 | Saliva | Systematic Review | N/D | IL‐1α, IL‐1β, IL‐6, IL‐8, IL‐1Ra, IL‐10, TNFα, VEGF‐α, MMP1, MMP2, MMP3, MMP9, AATα, HAPβ, C3, hemopexin, serotransferrin, transthyretin, fibrinogen β, resistin and proline‐rich proteins (a, b and g) | Increased in OSCC compared to Control. |
| Pillai et al. 116 | Saliva and Serum | Systematic review | N/D | EGFR, Vitamin D‐binding protein, Fibrinogen, CEA, | Increased in OSCC compared to Control. |
| Arroyo et al. 70 | Saliva | Systematic review and meta‐analysis | 986 | CEA, CRP, CYFRA‐21‐1, Her‐2/neu, erbB‐2, IL‐1α, IL‐1β, IL‐6, IL‐8, TNF α and Naa10p | Increased in OSCC and OPMD compared to Control for CEA and CYFRA21‐1 only |
| Ferrari et al. 71 | Saliva | Systematic review | 948 | IL‐6, IL‐8, IL‐17, IL‐1β, TNF‐α, IFN‐γ, MIP‐1β, GRO, VEGF and IP‐10 | OSCC > OPMD > Control |
| AlAli et al. 194 | Saliva | Systematic review | 775 | CYFRA 21‐1 and MMP‐9 | Non‐conclusive evidence due to the presence of biases and limitations in the studies evaluated |
| Dikova et al. 195 | Saliva | Multiplex ELISA | 157 | IL‐1α, IL‐6, IL‐8, TNF‐α, HCC‐1, MCP‐1 and PF‐4 | OSCC > OPMD > Control |
| Sivadasan et al. 196 | Saliva | ELISA | 67 | CD44 | OSCC > OPMD > Control |
| Ameena et al. 197 | Saliva | ELISA | 90 | TNF‐α | OSCC > OPMD > Control |
| Deepthi et al. 198 | Saliva | ELISA | 90 | TNF‐α | OSCC > OPMD > Control |
| Zheng et al. 62 | Saliva and Serum | ELISA | 202 | CEA, Naa10p |
OSCC > OPMD > Control Salivary detection had the greatest sensitivity and specificity compared to Serum |
| Lee et al. 199 | Saliva | Multiplex ELISA | 65 | IL‐6, IL‐8, IL‐1β, TNF‐α, IFN‐γ, MIP‐1β, Eotaxin and GRO | Increased in OSCC compared to Control |
| Abbas et al. 200 | Saliva | ELISA | 50 | IL‐17 | Increased in OSCC compared to Control |
| Seyedmajidi et al. 201 | Saliva and Serum | ELISA | 40 | CD44 | Increased in OSCC compared to Control, although not statistically significant |
| Awasthi et al. 202 | Saliva | ELISA | 64 | CYFRA 21‐1 and LDH | Increased in OSCC and OPMD compared to Control |
| Amylase | Increased in Control compared to OSCC and OPMD | ||||
| Khyani et al. 68 | Saliva | ELISA | 105 | IL‐6 and IL‐8 | Increased in OSCC and OPMD compared to Control |
| Peisker et al. 203 | Saliva | ELISA | 60 | MMP‐9 | Increased in OSCC compared to Control |
| Yu et al. 204 | Saliva | LC–MS | 478 | MMP1, KNG1, ANXA2 and HSPA5 | Increased in OSCC compared to OPMD and Control |
| Polz‐Dacewicz et al. 205 | Saliva | ELISA | 118 | IL‐10, TNF‐α, TGF‐β and VEGF | Increased in OSCC compared to Control |
| Gleber‐Netto et al. 206 | Saliva | ELISA | 180 | IL‐1β and IL‐8 | OSCC > OPMD > Control |
| Dineshkumar et al. 207 | Saliva | ELISA | 300 | IL‐6 | OSCC > OPMD > Control |
| Ghallab & Shaker 208 | Saliva and Serum | ELISA | 45 | Chemerin and MMP‐9 | OSCC > OPMD and Control |
| Rajkumar et al. 63 | Saliva and Serum | ELISA | 200 | CYFRA 21‐1 |
OSCC > OPMD > Control Salivary CYFRA 21‐1 levels were three‐fold higher when compared to serum levels |
| Aziz et al. 209 | Saliva | Multiplex ELISA | 63 | IL‐10 and IL‐13 | Increased in OSCC compared to Control |
| Gautam et al. 61 | Plasma | nanoLC‐MS/MS | 28 | CRP, Fibrinogen alpha and Beta Chains, Fibronectin‐1, Serum amyloid A‐1, C4b‐binding protein beta chain | Increased in OSCC compared to Control up to 5.36‐fold |
| Catalase, Flavin reductase, Carbonic anhydrase 1 and 2, SOD1, Purine nucleoside phosphorylase, APOA4, Desmoplakin, Desmoglein‐1, Lumican | Decreased in OSCC compared to Control up to 4.28‐fold | ||||
| Zhang et al. 210 | Serum | Protein Microarray Assay | 50 | GDF15, MCSF, I309, MMP‐3, CTACK, AXL | Increased in OSCC compared to Control |
| Schiegnitz et al. 69 | Serum | ELISA | 205 | IL‐6 and IL‐8 | Increased in OSCC compared to OPMD and Control |
| Xu et al. 66 | Serum, Tissue | Western blot | 68 | GLUT‐1 | Increased in OSCC compared to Control |
| Ramos‐García et al. 211 | Tissue | Systematic review and meta‐analysis | 1210 | p53 | OSCC > OPMD > Control |
| Ramos‐García & González‐Moles 212 | Tissue | Systematic review and meta‐analysis | 2746 | β‐Catenin |
Increased aberrant expression in OSCC compared to control Aberrant Expression ‐ Aggregated Hazard Ratio 1.77 Membrane loss – Aggregated Hazard Ratio 2.29 |
| Botha et al. 67 | Tissue and cell lines | Systematic review | N/D | GLUT‐1, GLUT‐3, | Increased in OSCC compared to Control |
| GLUT‐2, GLUT‐4, GLUT‐8, GLUT‐13, SGLT‐1 and SGLT‐2 | Not significantly difference | ||||
| Upadhaya et al. 213 | Tissue | Immunohistochemistry | 40 | ZO‐1 and E‐cad | Control > OPMD > OSCC |
| Ghazi et al. 64 | Tissue | Immunohistochemistry | 55 | CD44 | OSCC > OPMD > Control |
| Zhang et al. 214 | Tissue | Immunohistochemistry | 178 | p53, Ki‐67, P16, β‐catenin, c‐jun, c‐met, IMP‐3, COX‐2, PDPN, CA9 | Increased in OSCC compared to Control |
| Gissi et al. 215 | Tissue | Immunohistochemistry | 77 | p53 and Ki‐67 | Increased in OSCC compared to Control |
| Mumtaz et al. 216 | Cell line/Tissue | NanoLC‐MS/MS | 14 | Transferrin receptor, THBS2, LGALS3BP and DNAJB11 | Increased in OSCC compared to Control |
Abbreviations: AXL, receptor tyrosine kinase; CA9, carbonic anhydrase 9; CEA, Carcinoembryonic Antigen; CEA, Carcinoembryonic Antigen; COX‐2, cyclooxygenase‐2; CTACK, cutaneous T cell‐attracting chemokine; CYFRA 21, cytokeratin‐19 fragment; MCP‐1, monocyte chemoattractant protein‐1; MIP‐1β, Macrophage Inflammatory Protein‐1 beta; MMP‐1, Matrix metallopeptidase 1; MMP‐3, Matrix metallopeptidase 3; MMP‐9, Matrix metallopeptidase 9; N/D, not disclosed; Naa10p, N‐α‐acetyltransferase 10 protein; Naa10p, N‐α‐acetyltransferase 10 protein; OPMD, Oral Potentially Malignant Disorders; OSCC, Oral Squamous Cell Carcinoma; PDPN, podoplanin; PF‐4, platelet factor‐4; VEGF, Vascular endothelial growth factors.
The majority of the studies presented here (68%) used saliva as the source of biomarkers, possibly due to saliva sampling being fast, noninvasive, and well tolerated, besides being a safe procedure for healthcare providers. 59 Additionally, saliva is a very promising source of protein OSCC biomarkers given that it is in direct contact with the cancerous lesions and the oral mucosa. 60
A minority of studies (26%) focused on blood‐based biopsies. Gautam et al. 61 identified 16 potential biomarkers for OSCC, using high‐throughput screening methods, including Fibrinogen alpha and Beta Chains, Fibronectin‐1, and Serum amyloid A‐1, which were increased in the OSCC group up to 5.36‐fold. One major difference, however, is the greater sensitivity that a saliva‐based approach has compared to a serum‐based approach. Zheng et al. 62 examined both saliva and serum carcinoembryonic antigen (CEA) and N‐α‐acetyltransferase 10 protein (Naa10p) expression individually. The sensitivity and specificity of CEA and Naa10p in saliva were 80.2%, 81.7% and 81.1%, 83.3%, respectively, while the sensitivity and specificity of CEA and Naa10p in serum were 68.9%, 73.3% and 70.8%, 75.0% respectively. The combined detection of CEA and Naa10p in saliva led to the greatest sensitivity and specificity (92.5% and 85.0%, respectively). Similarly, Rajkumar et al. 63 demonstrated 3‐fold higher levels of cytokeratin‐19 fragment CYFRA 21‐1 in saliva compared to serum levels. Noteworthy, though, is that in their systematic review, Ali et al. (2020) found non‐conclusive evidence for increased CYFRA 21‐1 in saliva samples, due to the presence of biases and limitations in the studies evaluated.
A minority of studies (20%) used more invasive biopsy methods (i.e., tissue biopsy) and determined that CD44 was differentially expressed in OSCC and OPMD, versus healthy tissues, with significantly increased levels in OSCC, followed by OPMD, compared to controls. 64 Similarly, other studies 65 , 66 , 67 identified glucose transporters, especially Glucose transporter 1 (GLUT‐1) and 3 (GLUT‐3), as significantly increased in OSCC compared to controls.
A third of the studies (36%) demonstrated that inflammatory cytokines, such as interleukin 6 (IL‐6), interleukin 8 (IL‐8), tumor necrosis factor alpha (TNF‐α), and interleukin 1 beta (IL‐1β) are significantly increased in OSCC compared to controls. Regarding OPMDs, most of these studies indicated a significantly progressive increase in the inflammatory cytokines, with OSCC levels being significantly higher than those in OPMD, and both were significantly higher than controls (OSCC > OPMD > Controls). Two reports 68 , 69 contradict these studies. Khyani et al. 68 indicated no significant differences between OSCC and OPMD, with both being significantly higher than controls, whereas Schiegnitz et al. 69 indicated no significant difference between OPMD and controls, and both were significantly lower than OSCC. These differences, however, could be due to the use of a higher detection limit for these particular reports compared to the rest of the studies, thus, reducing the ability to distinguish OPMD from OSCC and controls. The systematic reviews, however, do not agree with each other in this regard. Arroyo et al. 70 reported that both OSCC and OPMD levels were significantly elevated compared to controls, but not significantly different between each other (i.e., OSCC and OPMD > Controls), whereas Ferrari et al. 71 reported that all studies demonstrated that OPMD levels were significantly higher than controls, but significantly lower than OSCC (OSCC > OPMD > Control), with an effective power of discrimination among the samples—Area under the curve (AUC) ranging from 0.70 to 0.99. Given these findings, additional systematic review studies are needed to determine whether OPMD are a different group compared to OSCC and controls.
4. METABOLITE‐BASED BIOMARKERS FOR OSCC
In addition to protein‐ and proteomic‐based studies, recent studies also include the detection and analysis of the metabolomic biomarkers associated with oral cancer. Nuclear magnetic resonance (NMR) spectroscopy, mass spectrometry (MS) combined with liquid chromatography (LC), gas chromatography (GC), capillary electrophoresis (CE), or ultra‐high‐performance liquid chromatography (UHPLC) are often utilized for detection of small molecules and metabolomic investigations. 72 , 73 Table 3 summarizes the recent studies in the literature.
TABLE 3.
Metabolite‐based biomarkers for OSCC.
| Author/Year | Source of biomarkers | Method | Sample size | Metabolites | Findings |
|---|---|---|---|---|---|
| Rodríguez‐Molinero et al. 217 | Saliva | Systematic review | 3883 | L‐Fucose | Increased levels in OSCC compared to Control; |
| Glycine, proline, citrulline, ornithine, 1‐octen‐3‐ol, hexanoic acid, E‐2octenal, heptanoic acid, octanoic acid, E‐2‐nonenal, nonanoic acid, 2,4‐decadienal, 9‐undecenoic acid, 3‐Heptanone, 1,3‐Butanediol, 1,2‐Pentanediol, 1‐Hexadecanol, Putrescine, cadaverine, thymidine, adenosine, 5‐aminopentoate, hippuric acid, phosphocholine, glucose, serine, adrenic acid, Choline, BBCA, urea, 3‐hydroxybutyric acid, Pipecolate, Sadenosylmethionine, | Significantly different levels in OSCC compared to Control; There is still a need for more studies, with a larger sample size. | ||||
| Ethanol, 2‐Pentanone, phenol, Hexadecanoic acid, Undecane, 1‐octanol, Butyrolactone, benzyl alcohol | Decreased levels in OSCC compared to Control | ||||
| Grootveld et al. 87 | Saliva | Review | N/A | 1‐methylhistidine, 2‐oxoarginine and γ‐aminobutyryl‐lysine l‐homocysteate, polyamines (amino acid metabolism); 2‐phosphoglycerate (carbohydrate metabolism); pseudouridine (nucleotide biosynthesis pathway); 4‐nitroquinoline‐1‐oxide, ubiquinone and reduced glutathione (oxidative stress pathway); choline, S‐adenosylmethionine and methionine (quaternary amine metabolism); BCAAs (TCA cycle, BCAA degradation); urea (urea cycle); and the ketone bodies 3‐D‐hydroxybutyrate and hydroxy‐isovalerate (lipid metabolism) | Perturbations pathways involved in the metabolism of amino acids, proteins, carbohydrates and nucleic acids throughout multistage carcinogenesis developments |
| Panneerselvam et al. 88 | Saliva | Review | N/A | N/D | Establishing standard operating procedures for the use of saliva samples is mandatory. An effective screening system should be developed by combining conventional and modern technologies. |
| Patil & More 77 | Saliva | Review | N/A | Glutathione, polyamines, branched chain amino acids, S‐adenosylmethionine, pipecolate, choline, glycine, proline, inositol 1,3,4‐triphosphate, indole‐3‐acetate and ethanolamine phosphate, urea, 3‐hydroxybutyric acid, pseudouridine, D‐glycerate‐ 2‐ phosphate, 4‐nitroquinoline‐ 1‐ oxide, ubiquinone and estradiol valerate | Increased in OSCC compared to Control; Carcinogenesis causes disturbances in the metabolism of carbohydrates, proteins, amino acids and nucleic acids |
| Vitório et al. 104 | Saliva, serum, plasma and tissue | Review | N/A | Alanine, choline, leucine, isoleucine, glycyl‐leucine, glutamic acid, 120.0801 m/z, phenylalanine, alpha‐aminobutyric acid, serine, indole‐3‐acetate, ethanolamine phosphate, s‐adenosylmethionine, pipecolate, choline, betaine, pipecolinic acid, propionylcholine, lactic acid, acetone, acetate, putrescine, aspartic acid, glutamate, proline, aspartic acid | Increased in OSCC compared to Control |
| Ornithine, o‐hydroxybenzoate, ribose‐5‐phosphate, l‐carnitine, acetylphenylalanine, sphinganine, phytosphingosine, s‐carboxymethyl‐l‐cysteine, phenylalanine, valine, l‐leucine, glutamine, 6‐hydroxynicotinic acid | Decreased in OSCC compared to Control | ||||
| Ishikawa et al. 74 | Saliva | CE‐TOF‐MS | 72 |
Proline, carnitine, 5‐hydroxylysine, 3‐methylhistidine, adenosine, inosine, and N‐acetylglucosamine Multivariate analysis: 3‐methylhistidine and 5‐hydroxylysine |
Only 3‐methylhistidine found to be a significant prognostic factor |
| Tantray et al. 76 | Saliva | GC–MS | 90 | Decanedioic acid, 2‐methyloctacosane, octane, 3,5‐dimethyl, pentadecane, eicosane, hentriacontane, 5, 5‐diethylpentadecane, nonadecane, oxalic acid, 6‐phenylundecanea, l‐proline, 2‐furancarboxamide, 2‐isopropyl‐5‐methyl‐1‐heptanol, pentanoic acid, and docosane | Increased in OSCC compared to OPMD and Control |
| Supawat et al. 79 | Saliva | NMR | 25 | Tyrosine, tryptophan, unk1, unk3, trimethylamine N‐oxide and glycine | Increased in OSCC compared to Control |
| de Sá Alves et al. 78 | Saliva | GC–MS | 68 | Malic acid, methionine, maltose, protocatechuic acid, inosine, pantothenic acid, dihydroxyacetone phosphate, hydroxyphenylatic acid, galacturonic acid, indole‐3‐acetic acid, uracil, isocitric acid, ribose‐5‐phosphate, o‐phospho serine, lactitol, gluconic acid, hippuric acid, 3‐hydroxypropionic acid and spermidine | Increased in OSCC compared to Control |
| Lactose, catechol, 2‐ketoadipic acid, leucine, urea, maleic acid, palmitic acid, ornithine, margaric acid, sucrose, octadecanol, threitol, acetoacetic acid, methionine sulfone, phosphoric acid, elaidic acid, mannose, sorbitol, citric acid, and 3‐aminopropanoic acid | Decreased in OSCC compared to Control | ||||
| Song et al. 83 | Saliva | CPSI‐MS | 373 | Putrescine, cadaverine, thymidine, adenosine and 5‐aminopentoate | Increased in OSCC compared to Control |
| Hippuric acid, phosphocholine, glucose, serine and adrenic acid | Decreased in OSCC compared to Control | ||||
| Ishikawa et al. 80 | Saliva | CE‐TOF‐MS | 60 | Trimethylamine N‐oxide, putrescine, creatinine, 5‐aminovalerate, pipecolate, N‐acetylputrescine, gamma‐butyrobetaine, indole‐3‐acetate, N1‐acetylspermine, 2′‐deoxyinosine, ethanolamine phosphate and N‐acetylglucosamine | Increased in OSCC compared to OPMD |
| N‐acetylhistidine and o‐acetylcarnitine | Decreased in OSCC compared to OPMD | ||||
| Ishikawa et al. 81 | Saliva | CE‐TOF‐MS | 48 | Ornithine, carnitine, arginine, o‐hydroxybenzoate, N‐acetylglucosamine‐1‐phosphate, and ribose 5‐phosphate | Decreased in OSCC compared to OPMD |
| Shigeyama et al. 218 | Saliva | GC–MS | 74 | Ethanol, 2‐pentanone, phenol, hexadecanoic acid, disappeared undecane, 1‐octanol, butyrolactone and benzyl alcohol and newly produced 3‐heptanone, 1,3‐butanediol, 1,2‐pentanediol and 1‐hexadecanol | Decreased in OSCC compared to Control |
| Sridharan et al. 219 | Saliva | UPLC‐QTOFMS | 61 | D‐glycerate‐2‐ phosphate, estrone‐3‐glucuronide, 4‐nitroquinoline‐1‐oxide, sphinganine‐1 phosphate, 1‐methyl histidine, inositol 1,3,4‐triphosphate, d‐glycerate‐2‐phosphate, 2‐oxoarginine, norcocaine nitroxide, pseudouridine, galactosphingosine, and ubiquinone | Increased in OSCC compared to OPMD |
| Taware et al. 220 | Saliva | HS‐SPME‐GC–MS | 59 | 1,4‐dichlorobenzene, 1,2‐decanediol, 2,5‐Bis1,1‐dimethylethylphenol, propanoic acid (ethyl ester), E‐3‐decen‐2‐ol, acetic acid, propanoic acid, ethyl acetate, 2,4‐dimethyl‐1‐heptene, 1‐chloro‐2‐propanol, 1‐chloro‐2‐butanol, 2‐propenoic acid, 2,3,3‐trimethylpentane, ethanol, and 1,2,3,4‐tetrachlorobutane | Increased in OSCC compared to Control |
| Mikkonen et al. 84 | Saliva | NMR | 75 | Fucose, glycine, methanol, proline and 1,2‐propanediol. | Increased in HNSCC compared to Control, except proline |
| Lohavanichbutr et al. 85 | Saliva | NMR and LC–MS/MS | 194 | Glycine, proline, ornithine and citrulline | Decreased in OSCC compared to Control |
| Ohshima et al. 86 | Saliva | CE‐TOF‐MS | 43 | Choline, p‐hydroxyphenylacetic acid and 2‐hydroxy‐4‐methylvaleric acid, valine, 3‐phenyllactic acid, leucine, hexanoic acid, octanoic acid, terephthalic acid, γ‐butyrobetaine and 3‐(4‐hydroxyphenyl)propionic acid, isoleucine, tryptophan, 3‐phenylpropionic acid, 2‐hydroxyvaleric acid, butyric acid, cadaverine, 2‐oxoisovaleric acid, N6,N6,N6‐trimethyllysine, taurine, glycolic acid, 3‐hydroxybutyric acid, heptanoic acid, urea and alanine | Increased in OSCC compared to Control, except Urea |
| Kamarajan et al. 102 | Saliva, Plasma and Tissue | UPLC‐MS/MS for profiling; GC–MS and PCR for validation | Tissue – 103; Saliva – 75; Plasma ‐ 14 | Glutamine and glutaminase | Confirmed involvement of glutamate and glutaminolysis. Exogenous glutamine induced stemness via glutaminase, whereas inhibiting glutaminase suppressed stemness in vitro and tumorigenesis in vivo |
| Ishikawa et al. 82 | Saliva and tissue | CE‐TOF‐MS | 68 | 3PG, pipecolate, spermidine, Met, SAM, 2AB, Trp, Val, hypoxanthine, Gly‐Gly, trimethylamine, N‐oxide, guanine, guanosine, taurine, choline, cadaverine, Thr. | Increased in OSCC compared to Control |
| Zuo et al. 93 | Serum | UHPLC‐Q‐Orbitrap HRMS | 103 | Succinic acid, arginine, 9‐decanoylcarnitine, asparagine‐valine, glutamine, hypoxanthine, sphingosine, and palmitoyl ethanolamide | Increased in OSCC compared to Control |
| Hexanoylcarnitine, orotic acid, uric acid, vanillyl mandelic acid, ethyl acetate, and thromboxane B2 | Decreased in OSCC compared to Control | ||||
| Tsai et al. 100 | Plasma, urine, and tissue | NMR | 110 | Creatine, creatine phosphate, glycine, and tyramine | Downregulated in OSCC (Plasma) |
| Aspartate, butyrate, carnitine, glutamate, glutathione, glycine, glycolate, guanosine, and sucrose | Upregulated in OSCC (Tissue) | ||||
| Alanine, choline, glucose, isoleucine, lactate, leucine, myo‐inositol, O‐acetylcholine, oxypurinol, phenylalanine, pyruvate, succinate, tyrosine, valine, and xanthine | Downregulated in OSCC compared to Control (Tissue) | ||||
| Wu et al. 92 | Serum | UHPLC‐QE‐MS |
Discovery: 60 Validation: 77 |
Serine and lactic acid | Increased in OSCC compared to Control; enhanced diagnostic efficacy when combined |
| Li et al. 91 | Plasma | UHPLC/Q‐Orbitrap HRMS | 194 | Decanoylcarnitine, cholic acid, cysteine, uridine, taurine, glutamate, citric acid and lyso‐phosphatydilcholine | Decreased in OSCC compared to Control and OPMD. |
| Sridharan et al. 94 | Serum | Q‐TOF‐MS | 71 | Estradiol‐17‐beta‐3‐sulfate, L‐carnitine, 5‐methylthioadenosine, 8‐hydroxyadenine, 2‐methylcitric acid, putrescine, and estrone‐3‐sulfate, 5,6‐dihydrouridine, 4‐hydroxypenbutolol glucuronide, 8‐hydroxyadenine, and putrescine | Increased in OSCC and OPMD compared to Control |
| Zhang et al. 221 | Tissue | GC–MS | 40 | Nicotinamide N‐methyltransferase | Increased in OSCC and fibroblast‐like cells compared to Control, but absent in tumor‐infiltrating lymphocytes |
| Yang et al. 95 | Tissue | GC–MS | 180 | Glutamate, aspartic acid, and proline | Increased in OSCC compared to Control |
| Paul et al. 99 | Tissue | NMR | 180 | 1,3‐Dihydroxyacetone, 2‐oxoglutarate, 4‐aminobutyrate, acetate, adenine, alanine, asparagine, aspartate, betaine, carnitine, choline, creatine, ethanol, fumarate, glucose, glutamate, glutamine, glycine, guanidoacetate, histidine, homocysteine, inosine, isoleucine, isopropanol, lactate, leucine, lysine, methanol, methionine, o‐acetylcarnitine, o‐phosphocholine, phenylalanine, serine, taurine, threonine, tyrosine, uracil, valine, myo‐inositol, sn‐glycero‐3‐phosphocholine, linoleic acid, MUFA, SFA, triglyceride, total fatty acids, and free fatty acids | Upregulated in OSCC compared to Control, except glucose |
| Yoshimura et al. 101 | Tissue | IHC | 22 | Glucose‐6‐phosphate and lactic acid | Upregulated in OPMD and OSCC |
| Musharraf et al. 97 | Tissue | GC–MS | 51 | (6E)‐2,6‐Dimethyl‐2,6‐octadiene, 2‐Methyl‐4‐keto‐pentan‐2‐ol, 4‐Hydroxybenzaldehyde, cis‐p‐Menthan‐3‐one, geraniol formate, and stearic acid | Increased in OSCC compared to Control |
| Glycine, threonine, glutamine, lysine, proline, alanine, glutamic acid, leucine, serine, 3‐heptanol, ethylene glycol, melibiose, and urea | Decreased in OSCC compared to Control | ||||
| Ogawa et al. 98 | Tissue | CE‐TOF‐MS | 64 | Lactate, Fum, Mal, Glu, Gly, Asp, Pro, Cys, Hyp, creatinine, putrescine, AMP, GTP, GDP, GMP | Increased in OSCC compared to Control |
| Glucose, 3PG, 2PG, creatine, adenylate and guanylate energy charge | Decreased in OSCC compared to Control | ||||
| Chen et al. 222 | Cell line | GC–MS | N/A | Glyoxylate and dicarboxylate, fructose, malate, serine, alanine, sorbose, and glutamate. | Glyoxylate and dicarboxylate increased in OSCC compared to Control |
| Tripathi et al. 223 | Cell line | NMR | N/A | Acetate, alanine, aspartate, AXP, choline, creatine, fumarate, glutamate, glutamine, glutathione, glycerophosphocholine, glycine, histidine, isoleucine, lactate, leucine, lysine, myo‐inositol, N‐acetyl‐aspartate, phenylalanine, phosphocholine, phosphocreatine, proline, pyruvate, taurine, threonine, tryptophan, tyrosine, UDP‐sugars, valine | Alterations of phosphatidylcholine/lysophosphatidylcholine and phosphocholine/glycerophosphocholine ratios, and elevated arachidonic acid in HNSCC; Dysregulation in multiple metabolic events, including Warburg effect, oxidative phosphorylation, energy metabolism, TCA cycle anaplerotic flux, glutaminolysis, hexosamine pathway, osmo‐regulatory and antioxidant mechanism |
Abbreviations: N/D, not disclosed; N/A, not available.
4.1. Salivary metabolomic biomarkers
Salivaomics is a broad collection of technologies used to investigate the different types of molecules found in saliva. Several investigators have proposed the use of salivary metabolomics to differentiate precancerous from malignant OSCC to help improve the diagnosis and prognosis of OSCC. For instance, Ishikawa et al. 74 identified 3‐methylhistidine as a significant prognostic factor, which is consistent with Cadoni's study, 75 which reported serum 3‐methylhistidine as a biomarker for predicting head and neck cancer. Tantray et al. 76 identified 15 signature salivary metabolites that could differentiate OSCC from OPMD and controls. Recently, Patil & More 77 conducted a systemic review of 10 publications on the use of salivary metabolomics for diagnosing oral cancer and they found that 1‐methylhistidine is also one of the metabolic biomarkers for oral cancer. Additionally, they concluded that the salivary biomarkers found were a result of perturbations in pathways involved in the metabolism of amino acids, proteins, carbohydrates, and nucleic acids throughout multistage carcinogenesis developments in oral cancer. Furthermore, de Sá Alves et al. 78 concluded that the malate–aspartate shuttle, the beta‐alanine metabolism pathway, and the Warburg effect were three important altered metabolic pathways identified in OSCC.
Multiple studies reported different metabolic profiles in saliva samples from OSCC cases. Supawat et al.'s study 79 determined that trimethylamine N‐oxide (TMAO) and glycine were significantly higher in oral cancer patients when compared with saliva samples taken from normal subjects. Consistent with Supawat et al.'s study, Ishikawa et al. 80 , 81 , 82 determined that trimethylamine N‐oxide was significantly higher in the OSCC group than in the OPMD group. Using different identification platforms, trimethylamine N‐oxide, choline, cadaverine, proline, glutamine, lactate, fucose, and glycine were determined to be consistently different between OSCC and controls. 79 , 82 , 83 , 84 , 85 , 86 Song et al. 83 used a combination of conductive polymer spray ionization mass spectrometry (CPSI‐MS) and machine learning (ML) analysis and found this approach as a feasible tool for accurate, automated diagnosis of OSCC in clinical practice.
Recently, Grootveld et al. 87 and Panneerselvam et al. 88 conducted a summative assessment of the latest progress on applications dedicated to the diagnostic and prognostic monitoring of oral cancer, especially focused on salivary metabolomic analysis, and suggested that optimal screening programs should involve a combination of both conventional and newly developed technologies. For example, several ML‐based data processing and analysis strategies include oral cancer identification, automated disease progression staging, and the application of image processing to distinguish between cancerous and precancerous cells. 89 , 90
4.2. Plasma/serum metabolomic biomarkers
Multiple studies have shown differential metabolic profiles in the plasma and serum of OSCC patients. In a recent study, Li et al. 91 demonstrated that the biomarkers associated with OSCC were closely related to cholic acid metabolism and amino acid metabolism. Additionally, Wu et al. 92 determined that serine and lactic acid gradually increased in benign and malignant salivary gland tumors. Zou et al. 93 used ultra‐high‐performance liquid chromatography‐high resolution mass spectrometry serum metabolomic analysis to demonstrate that succinic acid changes (low levels), hypoxanthine changes (high levels), and tumor grade provided the highest predictive accuracy of patients with OSCC. Further, Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analysis showed that the imbalance in the amino acid and purine metabolic pathway may affect the prognosis of OSCC. Further, integrative analysis of metabolomic and transcriptomic data can identify prognostic biomarkers associated with OSCC. Using quadrupole time of flight‐liquid chromatography‐mass spectrometry, Sridharan et al. 94 identified a significant upregulation of putrescine, 8‐hydroxyadenine, and 5,6‐dihydrouridine in OSCC compared to OPMD, indicating that these metabolites play a potential role in predicting the malignant transformation of OPMD.
4.3. Tumor tissue metabolomic biomarkers
Oral cancer tissue biopsy is an invasive approach and remains the current clinical gold standard for detection and diagnosis of oral cancer. Tumor tissue metabolomics is used to identify significant metabolic alterations in tumors compared to normal tissues. Recently, Yang et al. 95 summarized findings from a systemic review of oral biopsies, sample types, and detection techniques applied to oral cancer detection, and concluded that tissue biopsies provide increased diagnostic value compared to liquid biopsies. Kasiappan et al. 96 summarized the published metabolomic data for head and neck cancer and identified significant metabolites that differentiate head and neck cancer from normal controls based on tissue, serum, saliva, cell lines, and urine. Additionally, the authors also discussed the various tools used in metabolomics to identify important metabolites from these sample types. Multiple studies have confirmed that OSCC tissues undergo significant changes in metabolic pathways, including glycolysis, amino acid metabolism, and the pentose phosphate pathway. 72 , 82 , 95 , 97 , 98 , 99 , 100 , 101 Using Ultra performance liquid chromatography in tandem mass spectrometer (UPLC‐MS/MS)‐profiling and gas chromatography mass spectrometry (GC–MS)‐validation studies, Kamarajan et al. 102 demonstrated that highly active glutaminolysis was involved in primary and metastatic HNSCC tissues; this was marked by high glutamate and low glutamine levels in human head and neck cancer tissue, saliva, and plasma compared to controls. Further, Ishikawa et al. 82 also showed that the glycolysis‐Embden–Meyerhof–Parnas (EMP) pathway, tricarboxylic acid cycle (TCA) cycle, and glutathione pathway were aligned with cancer metabolic changes and could be potential discriminant biomarkers, which is consistent with the previous studies by Ogawa and colleagues. 98 Additionally, increased glucose consumption and rise in lactate levels with a concomitant decrease in the levels of glycolysis intermediates in OSCC is possibly the result of the Warburg effect. 82 , 98 , 99 , 100 , 101 These studies suggest that glucose metabolism may be more important for survival and proliferation, whereas glutamine/glutamate metabolism may be essential for subsequent aggressive transitions, including metastasis. 102 Furthermore, Shin et al. 103 highlighted that several publications suggest that the oral and gut microbiome contribute to the etiology of different types of cancers due to their ability to alter the community composition and induce inflammatory reactions, DNA damage, apoptosis, and altered metabolism. Thus, when considering cancer‐associated metabolomics, the influence of the microbiota and its repertoire of metabolites should also be considered, since the microbiota are profoundly abundant in the human body and on cancerous tissues. Recently, Vitorio et al. 104 summarized the metabolic landscape of OSCC and evaluated the studies focused on metabolomic analysis and metabolomic biomarker signatures identified so far in saliva, serum, plasma, urine, and tissue, and concluded that validation and optimization are still required to translate these findings into clinical applications.
5. TUMOR‐ASSOCIATED AUTOANTIBODIES–BIOMARKERS FOR OSCC
The discovery of novel potential biomarkers for a disease may shed new light on potentially novel pathophysiological mechanisms. This is particularly true for the field of immunology and the study of antibodies as they are at the center of the human immune defense system against infectious diseases yet are also key components in autoimmune diseases and carcinogenesis. 105 , 106 Particularly in carcinogenesis, tumors must evade and subvert the host immune response in order to escape immuno‐elimination and thereby grow and proliferate. Furthermore, tumors also exploit the immune system together with other host factors to promote angiogenesis to further support their growth. 106 This whole process leads to the production of many abnormal substances that are no longer recognized as the host's own, and this leads to the production of what it is known as tumor‐associated autoantibodies. 107
Autoantibodies are regular Immunoglobulin M (IgM) antibodies, produced by B cells that react with the host's own molecules, such as host proteins, nucleic acids, carbohydrates, lipids, or a combination of these. 108 Although the majority of these antibodies are polyreactive with a moderate affinity, some of these autoantibodies can be highly specific for a particular antigen in one specific cell type in the body, 108 making them promising biomarkers in cancer diagnosis. 109
For OSCC, in particular, salivary autoantibodies may be more clinically applicable compared to other molecules due to the antibodies having higher specificity, stability, and abundance in saliva, and reagents and platforms required for antibody detection are well‐established and readily accessible. 107 , 110 , 111 , 112 , 113 , 114 Table 4 summarizes the recent studies in the literature.
TABLE 4.
OSCC‐associated autoantibodies as biomarkers for OSCC
| Author/Year | Source of Biomarkers | Method | Sample size | Antigens Identified | Findings |
|---|---|---|---|---|---|
| Pillai et al. 116 | Saliva and Serum | Systematic Review | N/D | p53 and Hsp70 | Increased in OSCC compared to Control |
| Chu et al. 119 | Saliva | LC–MS/MS | 30 | CPPED1, GLUD1, LMAN2, PTGR1, RAB13, RAC1, UQCRC2 and p53 | Increased in OSCC compared to Control, especially in early stage OSCC. |
| Hsueh et al. 110 | Saliva | Multiplexed Immunoassay | 300 | ANXA2, CA2, ISG15, KNG1, MMP1, MMP3, PRDX2, SPARC, and HSPA5 |
Increased in OSCC compared to Control, especially in early stage OSCC ANXA2, KNG1, and MMP1 IgM were significantly higher in relapsed OSCC group, compared to primary OSCC group |
| Tseng et al. 115 | Saliva | LC‐MRM‐MS | 337 | ANXA2, CA2, ISG15, KNG1, MMP1, MMP3, PRDX2, SPARC, and HSPA5 | Increased in OSCC compared to Control |
| Wu et al. 114 | Saliva | Multiplexed immunoassay | 348 | p53, survivin, Hsp60, and RPLP0 | Increased in OSCC compared to Control, especially in early stage OSCC; Late stage OSCC group not significant different compared to Control |
| Liu et al. 117 | Plasma | ELISA | 193 | CD47 | Increased in OSCC compared to Control; Anti‐CD47 autoantibody plasma induces apoptosis via p‐AKT (in vitro) |
| Lin et al. 224 | Serum | Immunoassay | 4 | p53 | Increased in OSCC compared to Control |
| Schutt et al. 225 | Tissue and Serum | IHC and Elisa | 59 | Sperm Protein 17 (SP17) | Increased in OSCC compared to Control |
| Liu et al. 118 | In vitro | ELISA | N/A | ATP‐binding cassette subfamily C member 3 (ABCC3) | Plasma containing the autoantibody inducted apoptosis and cell cycle arrest |
Abbreviation: N/D, not disclosed.
Several antigens can elicit OSCC‐associated autoantibodies, including metalloproteinase 1 (MMP1) and 3 (MMP3), and Sperm protein 17 (SP17), and these autoantibodies can be uniquely and significantly increased in OSCC compared to controls. Hsueh et al., 110 demonstrated that a panel of 10 autoantibodies were significantly increased in the OSCC group compared to the control group. The authors also demonstrated that a panel with 4 of these autoantibodies (anti‐MMP3, anti‐peroxiredoxin 2 (PRDX2), anti‐ secreted protein acidic and cysteine rich (SPARC), and anti‐heat shock protein family A member 5 (HSPA5) was enough to achieve a sensitivity of 63.8% for detection of early‐stage OSCC. Tseng et al., 115 further developed the idea of a ML‐based risk prediction model to detect OSCC and found that a panel of 8 autoantibodies improved prediction performance by 13.9% (from 0.698 to 0.795). These studies demonstrate the potential for the use of autoantibodies as OSCC biomarkers, however, further investigations are needed to validate their use.
Other autoantibodies, such as anti‐p53, and anti‐Survivin, are elevated in more than 50% of tumor types, thus they have become known as “universal” tumor autoantibodies. 105 In a systematic review, Pillai et al. 116 reported increased levels of anti‐p53 and anti‐Hsp70 autoantibodies in OSSC patients, compared to controls. Similarly, Wu et al. 114 found increased levels of anti‐p53, anti‐Survivin, anti‐heat shock protein 60 (Hsp60), and anti‐ribosomal protein lateral stalk subunit P0 (RPLP0) autoantibodies in OSCC, compared to controls. However, upon progression, in the late‐stage OSCC group the levels were not significantly different when compared to controls, suggesting that OSCC may subvert the autoantibody processes over time.
Interestingly, autoantibodies may also have some antitumor capabilities. Liu et al. 117 , 118 demonstrated that plasma containing higher levels of autoantibodies positive for integrin‐associated protein (CD47) or Adenosine triphosphate‐binding cassette subfamily C member 3 (ABCC3) induced apoptosis and cell cycle arrest in 5 different OSCC cell lines, compared to plasma negative for these antigens. In their earlier work, Liu et al. 118 showed that anti‐ABCC3 immunoglobulin G (IgG) significantly induced apoptosis and cell cycle arrest in the CAL27 cell line, while no significant effects were found for the SCC15 cell line, even though ABCC3 was expressed in both cell lines. The authors hypothesized that the ABCC3 structure might be different between the two cell lines, resulting in different responses to the autoantibodies. On the other hand, in their more recent work, Liu et al., 117 demonstrated that plasma containing anti‐CD47 autoantibodies induced cell apoptosis and inhibited the invasion of all three OSCC cell lines (CAL27, SCC25, and SCC9 cell lines) via p‐AKT suppression.
To demonstrate the feasibility of using autoantibodies to diagnose OSCC, Chu et al. 119 showed that the sensitivity of 8 autoantibodies for OSCC, ranged from 16% to 62%, with an area under the curve (AUC) ranging from 0.656 to 0.796. A panel containing 4 autoantibodies (anti‐ lectin, mannose binding 2 (LMAN2), anti‐ prostaglandin reductase 1 (PTGR1), anti‐ras‐related protein 13 (RAB13), and anti‐ ubiquinol‐cytochrome c reductase core protein 2 (UQCRC2) presented a sensitivity of 76% and AUC of 0.863.
6. ORAL MICROBIOME‐BASED BIOMARKERS FOR OSCC
The oral cavity contains up to 1000 microbial species, comprised of bacterial, fungal, viral, archaeal, and protozoan species, which are known as the oral microbiome. These species interact among themselves and with their host, thus forming symbiotic interactions known as the oralome. 8 , 120 Even though the oral microbiome is known to be resilient, insults or changes to the microbiome, such as those due to tobacco and alcohol use, can shift the oralome to an unbalanced state of host–microbe interactions, in part characterized by dysbiosis, which can promote diseases in the host, including OSCC. 8 , 120 Recent cohort studies have demonstrated that poor oral hygiene increases the risk and decreases the survival rates of patients with head‐and‐neck cancer (HNC), 121 , 122 while epidemiological data shows that the odds ratio of OSCC are up to 4.6‐fold higher in patients with severe periodontitis compared to controls, 123 , 124 , 125 , 126 suggesting that oral microbial dysbiosis may play an important role in HNC and OSCC pathogenesis. In fact, early association studies by Nagy and colleagues found that many oral pathogens including Porphyromonas spp. and Fusobacterium spp. are enriched in OSCC tissues as compared with adjacent heathy ones. 127 , 128 Interestingly, in a mouse model of oral tumorigenesis, co‐infection by the two anaerobic periodontal pathogens Porphyromonas gingivalis and Fusobacterium nucleatum significantly enhanced the severity of tongue tumors, concomitant with increased STAT3 activation and increased IL‐6 levels in tongue epithelium. 129 Further, anaerobic and facultative bacteria can colonize and grow in tumors. 8 , 130 For instance, Abed et al., 131 reported that F. nucleatum was detected in CT26 colon tumors 2 h after tail vein injection in vivo, and bacterial proliferation was observed inside of the tumors 24 h and 72 h post‐injection.
Given its nature and the recent evidence linking the oral microbiome to cancer, specifically OSCC, 8 the oral microbiome has an immense potential to be a diagnostic biomarker for OSCC. Table 5 summarizes the recent studies in the literature.
TABLE 5.
Oral microbiome‐based biomarker for OSCC
| Authors/Year | Source of biomarker | Method | Sample size | Microbiome | Findings |
|---|---|---|---|---|---|
| Katirachi et al. 140 | N/D | Systematic Review and meta‐analysis | 5007 | Human papillomavirus | 6% (95% CI; 3%–10%) HPV prevalence in OSCC |
| Peter et al. 226 | Swabs, Saliva, Tissue, Oral rinse and Tissue scraping | Systematic review and meta‐analysis | 970 | Fusobacterium, Peptostreptococcus, and Parvimonas | Enriched in OSCC compared to Control |
| Haemophilus and Granulicatella | Decreased in OSCC compared to Control | ||||
| Mauceri et al. 227 | Saliva | Systematic review | 1335 | Porphyromonas gingivalis, Fusobacterium nucleatum, Neisseria flavescens, Fusobacterium periodonticum, Prevotella intermedia and Campylobacter spp, | Enriched in OSCC compared to Control, but it was not possible to profile a specific microbiota associated with OSCC due to the great heterogeneity of the studies |
| Mun et al. 132 | Saliva, Tissue, Oral rinse and Oral swab | Systematic review | 2809 | Fusobacteria, Firmicutes, and Bacteroidetes | Enriched in OSCC compared to Control; All the studies identified microbial dysbiosis to be associated with OSCC |
| Melo et al. 141 | Tissue | Systematic review | 383 | Human papillomavirus | 4.4% of the patients were HPV positive; None of the studies found had a control group |
| Lafuente Ibañez de Mendoza et al. 228 | In vitro and In vivo | Systematic review | N/A | Porphyromonas gingivalis | Enriched in OSCC compared to Control; Bacterium involved in epithelial‐mesenchymal transition of malignant epithelial cells, neoplastic cell growth, proliferation and invasion |
| Ramos et al. 229 | Saliva, Tissue, Oral rinse and Oral swab | Systematic review | 859 | Fusobacterium nucleatum subsp. Polymorphum and Pseudomonas aeruginosa | Enriched in OSCC compared to Control; Corroborated dysbiosis in OSCC. Enrichment of taxa associated with inflammation and production of acetaldehyde |
| She et al. 139 | Tissue | Systematic review | 1119 | Epstein–Barr virus | Positive association with an increased risk of OSCC |
| Vyhnalova et al. 136 | N/D | Review article | N/A | Candida albicans, Candida etchellsii, Candida famata, Gibberella, Hannaella, Rhodotorula, mucilaginosa | Enriched in OSCC compared to Control |
| Aspergillus tamarii, Alternaria, Cladosporium, Halotolerans, Emericella, Malassezia restricta, Pichia anomala, Trametes | Decreased in OSCC compared to Control | ||||
| Radaic et al. 8 | Saliva and tissues | Review article | N/A | Treponema denticola, Porphyromonas gingivalis, Fusobacteria Nucleatum, Tannarella Forsythia, Lactobacillus spp., Capnocytophaga gingivalis, Prevotella melaninogenica, Streptococcus mitis. Fusobacteria genera | Enriched in OSCC compared to Control |
| Streptococcus, Capnocytiphaga, Neisseria, Haemophillus and Aggreggatibacter | Decreased in OSCC compared to Control | ||||
| Radaic & Kapila 120 | N/D | Review article | N/A | Candida mycotype, Treponema denticola, Porphyromonas gingivalis, Fusobacteria Nucleatum, Tannarella Forsythia Capnocytophaga gingivalis, Prevotella melaninogenica, Streptococcus mitis | Enriched in OSCC compared to Control |
| Malassezia mycotype, Streptococcus, Neisseria, Haemophillus and Aggreggatibacter | Decreased in OSCC compared to Control | ||||
| Chattopadhyay et al. 133 | N/D | Review article | N/A | P. melaninogenica, Capnocytophaga gingivalis, Lactobacillus vaginalis, L. gasseri: L. johnsonii, L. fermentum, L. salivarius, L. rhamnosus, Fusobacterium nucleatum, F. periodonticum, Streptococcus vestibularis, S. mitis, S. salivarius, Prevotella oris, and Rothia mucilaginosa | Enriched in OSCC compared to Control |
| Aggregatibacter, Lautropia, Haemophillus, Neisseria, Leptotrichia, P. jejuni: P. melaninogenica, and Prevotella pallens | Decreased in OSCC compared to Control | ||||
| Perera et al. 128 | Saliva, swab, and tissues | Review article | 885 | Fusobacterium, Porphyromonas, Actinomyces, Propionibacterium spp., Candida albicans, Porphyromonas gingivalis, Streptococcus anginosus, Capnocytophaga gingivalis, Prevotella melaninogenica, Streptococcus mitis, Micrococcus luteus, Prevotella melaninogenica, Exiguobacterium oxidotolerans, Fusobacterium naviforme, Staphylococcus aureus, Veillonella parvula, Bacteroides fragilis, Ralstonia insidiosa, Fusobacterium naviforme, Peptostreptococcus micros, Clavibacter michiganensis subsp. tessellarius, Capnocytophaga sp. oral strain S3, Prevotella sp. oral clone BE073, Parvimonas sp. oral taxon 110, Eubacterium infirmum, Eubacterium brachy, Gemella haemolysans, Gemella morbillorum, Gemella sanguinis, Johnsonella ignava, Streptococcus parasanguinis I Peptostreptococcus stomatis, Streptococcus gordonii and Streptococcus salivarius | Taxa associated with OSCC |
| Yang et al. 230 | Saliva and whole blood | 16S Sequencing | 428 | Lachnoanaerobaculum, Kingella, Parvimonas | Enriched in OSCC compared to Control and correlated to genes in regulation of oncogenic and angiogenic responses |
| Gopinath et al. 231 | Whole mouth fluid and Oral Swab | 16S Sequencing | 94 | Enterobacteriae, Neisseria, Streptococcus and Fusobacteria, Prevotella, Treponema, Sphingomonas, Meiothermus, and Mycoplasma | Enriched in OSCC compared to Control; Tumor surfaces elevated abundances of Porphyromonas, Enterobacteriae, Neisseria, Streptococcus and Fusobacteria, whereas Prevotella, Treponema, Sphingomonas, Meiothermus and Mycoplasma genera were significantly more abundant in deep tissue. |
| Gopinath et al. 232 | Whole mouth fluid | 16S Sequencing | 74 | Porphyromonas | Correlated to OSCC |
| Megasphaera, unclassified Enterobacteria, Salmonella and Prevotella | Correlated to OPMD | ||||
| Streptococcus, Rothia and Fusobacterium | Correlated to Control | ||||
| Ganly et al. 233 | Oral rinse | 16S Sequencing | 38 | Fusobacterium, Prevotella, Alloprevotella | Enriched in OSCC compared to Control |
| Streptococcus | Decreased in OSCC compared to Control | ||||
| Yang et al. 234 | Oral rinse | 16S Sequencing | 248 | Fusobacterium periodonticum, Parvimonas micra, Streptococcus constellatus, Haemophilus influenza, and Filifactor alocis (in contrast to decrease of Streptococcus mitis, Haemophilus parainfluenzae, Porphyromonas pasteri, Veillonella parvula) |
Enriched in OSCC compared to Control; Higher complexity of oral microbiota communities in stage 4 patients |
| Hsiao et al. 235 | Saliva | 16S Sequencing | 289 | Prevotella tannerae, Fusobacterium nucleatum, and Prevotella intermedia | Enriched in OSCC compared to Control |
| Streptococcus tigurinus | Decreased compared to Control | ||||
| Lee et al. 236 | Saliva | 16S Sequencing | 376 | Bacillus, Enterococcus, Parvimonas, Peptostreptococcus, and Slackia | Enriched in OSCC compared to Control |
| Al‐Hebshi et al. 237 | Swabs and tissues | 16S Sequencing | 20 OSCC biopsies and 20 swabs | F. nucleatum and P. aeruginosa | Enriched in OSCC compared to Control |
| Wang et al. 238 | Saliva and oral swab | 16S Sequencing | 55 | Porphyromonas and Solobacterium g | Enriched in OSCC compared to Control |
| Haemophilus, Corynebacterium, Cellulosimicrobium, and Campylobacter | Decreased in OPMD compared to Control | ||||
| Hu et al. 239 | Non‐stimulated saliva | 16S Sequencing | 35 | Haemophilus, and Bacillus | Bacillus enriched in OSCC compared to Control, while Haemophilus Enriched in OPMD compared to Control |
| Streptococcus | Decreased in OPMD and OSCC | ||||
| Yost et al. 240 | Oral swab | Metatranscriptome sequencing | 15 | Genera Fusobacteria, Selenomonas, Capnocytophaga, Dialister, and Johnsonella (genus Bacillus; species Porphyromonas catoniae, Kingella denitricans, Capnocytophaga gingivalis, among others, were associated with healthy, tumor‐matching sites) | Enriched in OSCC compared to Control |
| Zhao et al. 241 | Oral swab | 16S Sequencing | 80 | Fusobacterium, Dialister, Peptostreptococcus, Filifactor, Peptococcus, Catonella and Parvimonas | Enriched in OSCC compared to Control |
| Nie et al. 242 | Tissue | 16S Sequencing | 305 | Fusobacterium, Prevotella, Porphyromonas, Campylobacter, Aggregatibacter, Lautropia, Asteroleplasma, Parvimonas, Peptostreptococcus, Pyramidobacter, Roseburia, and Propionibacterium | Enriched in OSCC compared to Control. The microbiome was highly correlated with tumor clinicopathological features, with several genera |
| de Abreu et al. 148 | Tissue | Nested PCR | 90 | Human papillomavirus | 3.3% of the OSCC patients were positive for HPV. All cases were HPV‐16 |
| Nieminen et al. 243 | Tissue | Immunohistochemistry | 149 | Treponema denticola | Dentilisin present in OSCC and the majority of orodigestive tumor samples |
| Perera et al. 244 | Tissue | ITS2 sequencing | 52 | C. albicans, C. etchellsii, and Hannaella luteola–like species | Enriched in OSCC compared to Control |
| A Hanseniaspora uvarum–like species, Malassezia spp., Aspergillus tamarii, Cladosporium halotolerans, and Alternaria alternata | Decreased in OSCC compared to Control | ||||
| Listyarifah et al. 245 | Tissue | Immunohistochemistry | 60 | Treponema Denticola | Dentilisin present in 95% of OSCC tumor samples and 40% were immunopositive for dentilisin. |
| Shin et al. 246 | Tissue | 16S Sequencing | 72 | Fusobacteria, Firmicutes, Actinobacteria, Proteobacteria and Streptococcus | Fusobacterium enriched in OSCC compared to Control |
| Streptococcus | Decreased in OSCC compared to Control | ||||
| Kikuchi et al. 144 | Tissue | PCR | 233 | Epstein–Barr virus | 50.2% of OSCC; 66.7% of severe dysplasia; 43.1% of mild dysplasia were positive for EBV. |
| Mokhtari & Beiraghdar 142 | Tissue | PCR | 60 | Herpes simplex‐1 | 5% of the OSCC patients were potivite for HSV |
| Saravani et al. 143 | Tissue | qPCR | 48 | Human Cytomegalovirus | 6.3% of the OSCC patients were positive for HCMV |
| Harrandah et al. 135 | In vivo | ELISA and Western blot | N/A | Fusobacteria | Mice infected with bacteria developed significantly larger and more numerous lesions compared to those not infected. |
| Kamarajan et al. 134 | In vivo and in vitro | Western blot | N/A | Treponema denticola, Fusobacterium nucleatum, and Prophyromonas gingivalis | Periodontal pathogens promote cancer aggressivity in mice via TLR2/MyD88 triggered activation of integrin/FAK signaling |
| Gallimidi et al. 129 | In vivo and in vitro | Immunohistochemistry | N/A | Fusobacterium nucleatum, and Prophyromonas gingivalis | Periodontal pathogens promote cancer aggressivity in mice; Increased STAT3 and IL‐6 levels in infected mice compared to control |
Specifically for OSCC, a systematic review with 2809 patients indicated an association between oral microbial dysbiosis and OSCC. 132 Moreover, the majority of these studies (75%) indicated a significant increase in Fusobacteria, especially F. nucleatum species, and P. gingivalis abundance in OSCC. These bacteria are known to induce the production of inflammatory cytokines, cellular proliferation, migration, and invasion, and inhibition apoptosis, through host cell genomic alterations in OSCC. 133 Additionally, two studies reported significantly larger tumors and larger numbers of lesions in mice infected with F. nucleatum, P gingivalis and Treponema denticola compared to controls. 134 , 135
Despite numerous studies on the oral microbiome and OSCC, the focus of these studies has traditionally been on bacterial dysbiosis. 120 Yet, OSCC has also been linked to dysbiosis in the oral mycobiome and virome. Specific changes in OSCC mycobiome have been identified by several studies, such as the enrichment of Candida, Gibberella and Hannaella genera, as well the decrease of Malassezia and Aspergillus genera in OSCC compared to healthy controls. 136 Moreover, several studies have demonstrated that Candida albicans is able to induce carcinogenesis through induction of pro‐inflammatory T‐helper 17 cells, as well as induction of IL‐6 and IL‐8 cytokines by oral cells. 136 , 137 , 138 Yet, due to the relatively low prevalence of individual fungal species and the lack of well‐characterized reference genomes, further studies are needed on the relationship between mycobial dysbiosis and OSCC. 136 , 138
Several viruses has been identified in OSCC tissues, including Epstein–Barr Virus (EBV), 139 Human papillomavirus (HPV), 140 , 141 herpes simplex virus (HSV) 142 and Human cytomegalovirus (HCMV). 143 EBV prevalence is between 48.18%–50.2%, depending on the specimen type (i.e., paraffin‐embeded or fresh frozen, respectively). 139 , 144 Further, She et al. 139 meta‐analyzed 13 case–control studies and found that EBV infection is statistically associated with increased risk of OSCC (OR 5.03%–95% CI; 1.80–14.01) compared to controls. These data highlight that EBV infection may be a high‐risk factor for OSCC. Although HPV status has been used in clinical settings to categorize OSCC patients, HPV's carcinogenic role in OSCC is still debatable. 145 HPV‐positive OSCC has been significantly associated with younger patients with no history of smoking and drinking. 146 Moreover, a distinct oral microbial composition has been reported for HPV–positive OSCC‐namely an enrichment in Lactobacillus, Gemella, Leuconostoc and Weeksellaceae genera in HPV‐Positive OSCC compared with HPV‐negative tissues–suggesting that HPV presence may influence the oral microbiome composition toward dysbiosis. 8 , 147 However, the lack of molecular evidence, 145 heterogeneity due to geographic location and detection methods, 146 and its low prevalence (3%–6%), 140 , 141 , 148 with no significant association with OSCC 148 has raised questions whether HPV does in fact drive OSCC carcinogenesis. 145 HSV and HCMV prevalence in OSCC, are 5% 142 and 3%, 143 respectively, which seems to indicate that these viruses may not be high‐risk factors for OSCC development, but may instead play a minor role in the disease, since they are known to act as mutagens in other tissues. 149 Nonetheless, more studies are needed to further understand the role of these viruses in OSCC pathogenesis.
Several mechanisms have been proposed to explain the carcinogenic potential of the oral microbiome, including promoting epithelial barrier dysfunction, chronic inflammation, and epigenetic modulation. 8 Kamarajan et al., 134 for instance, demonstrated that bacteria found in periodontal disease, including Treponema denticola promote cancer aggressivity via toll‐like receptor 2 (TLR2)/myeloid differentiation primary response 88(MyD88) triggered activation of integrin/FAK signaling. It is intriguing to note that F. nucleatum has also been linked to colorectal cancer (CRC), breast cancer and pancreatic cancer. 150 , 151 , 152 In CRC, F. nucleatum promotes colorectal carcinogenesis via the adhesin FadA by modulating E‐cadherin/β‐catenin signaling, 153 especially. via induction of the Wnt/β‐catenin modulator Annexin A1. 154 Furthermore, F. nucleatum induces autophagy activation and apoptosis inhibition that is dependent on toll‐like receptor 4 (TLR4)/MyD88 signaling. 150 It remains to be investigated if similar pathways in OSCC are modulated by F. nucleatum.
7. CURRENT CHALLENGES AND FUTURE PERSPECTIVES
Advancements in genomics, proteomics, metabolomics, immunomics, and microbiomics, as shown in this review, have expanded the understanding of OSCC tumorigenesis and progression, and also the discovery of biomarkers that facilitate the diagnosis and prognosis of the disease. However, tumorigenesis complexity, including synergistic genomic, transcriptomic, proteomic and metabolomic alterations, coupled with an oral microbiome dysbiosis, and patient heterogeneity make it unlikely for a single diagnostic biomarker to be effective for cancer diagnosis. In fact, panels integrating multiple omics may be required for a comprehensive patient evaluation and would enhance the panel reliability, sensitivity and specificity. 8 , 120 , 155 Additionally, methodological standardization and reproducible validation of oral cancer biomarkers are still required, since multiple methodologies were used to obtain these biomarkers and contradicting results can still be found in the literature.
As future perspectives, we expect a rise in the use of liquid biopsies, especially the use of saliva for OPMD and OSCC diagnosis and prognosis, as saliva has been widely investigated as a source of OSCC biomarkers in the majority (over 50%) of the studies analyzed. Additionally, saliva use may improve the ability to monitor OPMD and OSCC in patients over time, given its simple and safe collection protocols and ability for collection of larger volumes of samples. 155 , 156
Together with liquid‐based biopsies, multi‐omic panels, such as those containing genomic, transcriptomic, proteomic, metabolomic, immunomic and microbiomic biomarkers may help us to diagnose early lesions or even prevent the onset of OPMDs and OSCC.
CONFLICT OF INTEREST STATEMENT
David T. Wong has equity in Liquid Diagnostics LLC and RNAmeTRIX Inc.
ACKNOWLEDGMENTS
This study was supported by an NIH funding (R01CA269950) to Dr. Yvonne Kapila.
Radaic A, Kamarajan P, Cho A, et al. Biological biomarkers of oral cancer. Periodontol 2000. 2024;96:250‐280. doi: 10.1111/prd.12542
DATA AVAILABILITY STATEMENT
Not applicable; All materials/information are provided in the manuscript.
REFERENCES
- 1. Bai X‐X, Zhang J, Wei L. Analysis of primary oral and oropharyngeal squamous cell carcinoma in inhabitants of Beijing, China—a 10‐year continuous single‐center study. BMC Oral Health. 2020;20:208. doi: 10.1186/s12903-020-01192-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lingen MW, Kalmar JR, Karrison T, Speight PM. Critical evaluation of diagnostic aids for the detection of oral cancer. Oral Oncol. 2008;44:10‐22. doi: 10.1016/j.oraloncology.2007.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rivera C. Essentials of oral cancer. Int J Clin Exp Pathol. 2015;8:11884‐11894. [PMC free article] [PubMed] [Google Scholar]
- 4. Tajmirriahi N, Razavi SM, Shirani S, Homayooni S, Gasemzadeh G. Evaluation of metastasis and 5‐year survival in oral squamous cell carcinoma patients in Isfahan (2001–2015). Dent Res J. 2019;16:117‐121. [PMC free article] [PubMed] [Google Scholar]
- 5. Surveillance Epidemiology and End Results (SEER) Program , SEER Oral Cancer Statistics Review. 1975. –2017. Available online: https://seer.cancer.gov/archive/csr/1975_2017/results_merged/sect_20_oral_cavity_pharynx.pdf. (Accessed on 25 October 2021).
- 6. Le Campion ACOV, Ribeiro CMB, Luiz RR, et al. Low survival rates of oral and oropharyngeal squamous cell carcinoma. Int J Dent. 2017;2017:5815493. doi: 10.1155/2017/5815493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wang Q, Gao P, Wang X, Duan Y. The early diagnosis and monitoring of squamous cell carcinoma via saliva metabolomics. Sci Rep. 2014;4:6802. doi: 10.1038/srep06802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Radaic A, Ganther S, Kamarajan P, Grandis J, Yom SS, Kapila YL. Paradigm shift in the pathogenesis and treatment of oral cancer and other cancers focused on the oralome and antimicrobial‐based therapeutics. Periodontol 2000. 2000;2021(87):76‐93. doi: 10.1111/prd.12388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McCord C, Achita P, Magalhaes M, Darling M, Kiss A, Bradley G. Progression to malignancy in oral potentially malignant disorders: a retrospective study of 5110 patients. Oral Surg Oral Med Oral Pathol Oral Radiol. 2022;133:e149‐e150. doi: 10.1016/j.oooo.2021.12.084 [DOI] [PubMed] [Google Scholar]
- 10. Speight PM. Update on oral epithelial dysplasia and progression to cancer. Head Neck Pathol. 2007;1:61‐66. doi: 10.1007/s12105-007-0014-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Al‐Dakkak I. Oral dysplasia and risk of progression to cancer. Evid Based Dent. 2010;11:91‐92. doi: 10.1038/sj.ebd.6400745 [DOI] [PubMed] [Google Scholar]
- 12. Woo S‐B. Oral epithelial dysplasia and Premalignancy. Head Neck Pathol. 2019;13:423‐439. doi: 10.1007/s12105-019-01020-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Parlatescu I, Gheorghe C, Coculescu E, Tovaru S. Oral leukoplakia‐an update. Maedica. 2014;9:88‐93. [PMC free article] [PubMed] [Google Scholar]
- 14. Nevanpää TT, Terävä AE, Laine HK, Rautava J. Malignant transformation of oral epithelial dysplasia in Southwest Finland. Sci Rep. 2022;12:8261. doi: 10.1038/s41598-022-12441-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shubhasini AR, Praveen BN, Usha H, et al. Inter‐ and intra‐observer variability in diagnosis of oral dysplasia. Asian Pac J Cancer Prev APJCP. 2017;18:3251‐3254. doi: 10.22034/APJCP.2017.18.12.3251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Smith J, Rattay T, McConkey C, Helliwell T, Mehanna H. Biomarkers in dysplasia of the oral cavity: a systematic review. Oral Oncol. 2009;45:647‐653. doi: 10.1016/j.oraloncology.2009.02.006 [DOI] [PubMed] [Google Scholar]
- 17. Goetze S, Schüffler P, Athanasiou A, et al. Use of MS‐GUIDE for identification of protein biomarkers for risk stratification of patients with prostate cancer. Clin Proteomics. 2022;19:9. doi: 10.1186/s12014-022-09349-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kaminski MM, Abudayyeh OO, Gootenberg JS, Zhang F, Collins JJ. CRISPR‐based diagnostics. Nat Biomed Eng. 2021;5:643‐656. doi: 10.1038/s41551-021-00760-7 [DOI] [PubMed] [Google Scholar]
- 19. Weissleder R, Lee H, Ko J, Pittet MJ. COVID‐19 diagnostics in context. Sci Transl Med. 2020;12:eabc1931. doi: 10.1126/scitranslmed.abc1931 [DOI] [PubMed] [Google Scholar]
- 20. Haber DA, Velculescu VE. Blood‐based analyses of cancer: circulating tumor cells and circulating tumor DNA. Cancer Discov. 2014;4:650‐661. doi: 10.1158/2159-8290.CD-13-1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Corcoran RB, Chabner BA. Application of cell‐free DNA analysis to cancer treatment. N Engl J Med. 2018;379:1754‐1765. doi: 10.1056/NEJMra1706174 [DOI] [PubMed] [Google Scholar]
- 22. Siravegna G, Marsoni S, Siena S, Bardelli A. Integrating liquid biopsies into the Management of Cancer. Nat Rev Clin Oncol. 2017;14:531‐548. doi: 10.1038/nrclinonc.2017.14 [DOI] [PubMed] [Google Scholar]
- 23. Alix‐Panabières C, Pantel K. Circulating tumor cells: liquid biopsy of cancer. Clin Chem. 2013;59:110‐118. doi: 10.1373/clinchem.2012.194258 [DOI] [PubMed] [Google Scholar]
- 24. Fukumoto C, Uchida D, Kawamata H. Diversity of the origin of cancer stem cells in oral squamous cell carcinoma and its clinical implications. Cancer. 2022;14:3588. doi: 10.3390/cancers14153588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ruivo CF, Adem B, Silva M, Melo SA. The biology of cancer exosomes: insights and new perspectives. Cancer Res. 2017;77:6480‐6488. doi: 10.1158/0008-5472.CAN-17-0994 [DOI] [PubMed] [Google Scholar]
- 26. Fan HC, Blumenfeld YJ, Chitkara U, Hudgins L, Quake SR. Analysis of the size distributions of fetal and maternal cell‐free DNA by paired‐end sequencing. Clin Chem. 2010;56:1279‐1286. doi: 10.1373/clinchem.2010.144188 [DOI] [PubMed] [Google Scholar]
- 27. Babji D, Nayak R, Bhat K, Kotrashetti V. Cell‐free tumor DNA: emerging reality in oral squamous cell carcinoma. J Oral Maxillofac Pathol. 2019;23:273‐279. doi: 10.4103/jomfp.JOMFP_36_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Payne K, Spruce R, Beggs A, et al. Circulating tumor DNA as a biomarker and liquid biopsy in head and neck squamous cell carcinoma. Head Neck. 2018;40:1598‐1604. doi: 10.1002/hed.25140 [DOI] [PubMed] [Google Scholar]
- 29. Rosenthal M, Huang B, Katabi N, et al. Detection of HPV related oropharyngeal cancer in oral rinse specimens. Oncotarget. 2017;8:109393‐109401. doi: 10.18632/oncotarget.22682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mazurek AM, Rutkowski T, Śnietura M, Pigłowski W, Suwiński R, Składowski K. Detection of circulating HPV16 DNA as a biomarker in the blood of patients with human papillomavirus‐positive oropharyngeal squamous cell carcinoma. Head Neck. 2019;41:632‐641. doi: 10.1002/hed.25368 [DOI] [PubMed] [Google Scholar]
- 31. Gillison ML, Akagi K, Xiao W, et al. Human papillomavirus and the landscape of secondary genetic alterations in oral cancers. Genome Res. 2019;29:1‐17. doi: 10.1101/gr.241141.118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Shi Y, Xie T, Wang B, et al. Mutant P53 drives an immune cold tumor immune microenvironment in oral squamous cell carcinoma. Commun Biol. 2022;5:757. doi: 10.1038/s42003-022-03675-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wise‐Draper T, Sendilnathan A, Palackdharry S, et al. Decreased plasma DEK oncogene levels correlate with P16‐negative disease and advanced tumor stage in a case–control study of patients with head and neck squamous cell carcinoma. Transl Oncol. 2018;11:168‐174. doi: 10.1016/j.tranon.2017.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Palaia G, Pippi R, Rocchetti F, et al. Liquid biopsy in the assessment of MicroRNAs in oral squamous cell carcinoma: a systematic review. J. Clin. Exp Dent. 2022;14:e875‐e884. doi: 10.4317/jced.59736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Peng Y, Croce CM. The role of MicroRNAs in human cancer. Signal Transduct Target Ther. 2016;1:15004. doi: 10.1038/sigtrans.2015.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Scholtz B, Horváth J, Tar I, Kiss C, Márton IJ. Salivary MiR‐31‐5p, MiR‐345‐3p, and MiR‐424‐3p are reliable biomarkers in patients with oral squamous cell carcinoma. Pathogens. 2022;11:229. doi: 10.3390/pathogens11020229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Jia L, Wang Y, Wang C. CircFAT1 promotes cancer Stemness and immune evasion by promoting STAT3 activation. Adv Sci. 2021;8:2003376. doi: 10.1002/advs.202003376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pitt JM, Kroemer G, Zitvogel L. Extracellular vesicles: masters of intercellular communication and potential clinical interventions. J Clin Invest. 2016;126:1139‐1143. doi: 10.1172/JCI87316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Benecke L, Chiang D, Ebnoether E, Pfaffl M, Muller L. Isolation and analysis of tumor‐derived extracellular vesicles from head and neck squamous cell carcinoma plasma by galectin‐based glycan recognition particles. Int J Oncol. 2022;61:133. doi: 10.3892/ijo.2022.5423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Zhuang D, Wang S, Liu G, et al. Phenformin suppresses angiogenesis through the regulation of exosomal MicroRNA‐1246 and MicroRNA‐205 levels derived from oral squamous cell carcinoma cells. Front Oncol. 2022;12:943477. doi: 10.3389/fonc.2022.943477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wu L, Ye S, Yao Y, Zhang C, Liu W. Oral cancer stem cell‐derived small extracellular vesicles promote M2 macrophage polarization and suppress CD4+ T‐cell activity by transferring UCA1 and targeting LAMC2. Stem Cells Int. 2022;2022:1‐16. doi: 10.1155/2022/5817684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rodini CO, Lopes NM, Lara VS, Mackenzie IC. Oral cancer stem cells‐properties and consequences. J Appl Oral Sci. 2017;25:708‐715. doi: 10.1590/1678-7757-2016-0665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Ohnishi Y, Yasui H, Nozaki M, Nakajima M. Molecularly‐targeted therapy for the oral cancer stem cells. Jpn Dent Sci Rev. 2018;54:88‐103. doi: 10.1016/j.jdsr.2017.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Shahoumi LA. Oral cancer stem cells: therapeutic implications and challenges. Front Oral Health. 2021;2:685236. doi: 10.3389/froh.2021.685236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Varun B, Jayanthi P, Ramani P. Cancer stem cells: a comprehensive review on identification and therapeutic implications. J Oral Maxillofac Pathol. 2020;24:190. doi: 10.4103/jomfp.JOMFP_336_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ma Z, Zhang C, Liu X, et al. Characterisation of a subpopulation of CD133+ cancer stem cells from Chinese patients with oral squamous cell carcinoma. Sci Rep. 2020;10:8875. doi: 10.1038/s41598-020-64947-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Prakash N, Pradeep GL. Circulating biomarkers in oral cancer: unravelling the mystery. J Oral Maxillofac Pathol JOMFP. 2022;26:300‐306. doi: 10.4103/jomfp.jomfp_338_22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Adeola HA, Bello IO, Aruleba RT, et al. The practicality of the use of liquid biopsy in early diagnosis and treatment monitoring of oral cancer in resource‐limited settings. Cancer. 2022;14:1139. doi: 10.3390/cancers14051139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Parikh AR, Corcoran RB. Monitoring resistance through liquid biopsy. Ann Oncol. 2018;29:8‐11. doi: 10.1093/annonc/mdx650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ju S, Chen C, Zhang J, et al. Detection of circulating tumor cells: opportunities and challenges. Biomark Res. 2022;10:58. doi: 10.1186/s40364-022-00403-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Micalizzi DS, Maheswaran S, Haber DA. A conduit to metastasis: circulating tumor cell biology. Genes Dev. 2017;31:1827‐1840. doi: 10.1101/gad.305805.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Qayyumi B, Bharde A, Aland G, et al. Circulating tumor cells as a predictor for poor prognostic factors and overall survival in treatment Naïve oral squamous cell carcinoma patients. Oral Surg Oral Med Oral Pathol Oral Radiol. 2022;134:73‐83. doi: 10.1016/j.oooo.2022.02.018 [DOI] [PubMed] [Google Scholar]
- 53. Morgan TM, Wang X, Qian X, et al. Measurement of circulating tumor cells in squamous cell carcinoma of the head and neck and patient outcomes. Clin Transl Oncol. 2019;21:342‐347. doi: 10.1007/s12094-018-1930-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Chang P‐H, Wu M‐H, Liu S‐Y, et al. The prognostic roles of pretreatment circulating tumor cells, circulating cancer stem‐like cells, and programmed cell Death‐1 expression on peripheral lymphocytes in patients with initially Unresectable, recurrent or metastatic head and neck cancer: an exploratory study of three biomarkers in one‐time blood drawing. Cancer. 2019;11:540. doi: 10.3390/cancers11040540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Curtin J, Choi S‐W, Thomson PJ, Lam AKY. Characterization and clinicopathological significance of circulating tumour cells in patients with oral squamous cell carcinoma. Int J Oral Maxillofac Surg. 2022;51:289‐299. doi: 10.1016/j.ijom.2021.05.020 [DOI] [PubMed] [Google Scholar]
- 56. Loo JA, Yan W, Ramachandran P, Wong DT. Comparative human salivary and plasma proteomes. J Dent Res. 2010;89:1016‐1023. doi: 10.1177/0022034510380414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Riccardi G, Bellizzi MG, Fatuzzo I, et al. Salivary biomarkers in oral squamous cell carcinoma: a proteomic overview. Proteomes. 2022;10:37. doi: 10.3390/proteomes10040037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Chattopadhyay I, Panda M. Recent trends of saliva omics biomarkers for the diagnosis and treatment of oral cancer. J Oral Biosci. 2019;61:84‐94. doi: 10.1016/j.job.2019.03.002 [DOI] [PubMed] [Google Scholar]
- 59. Martina E, Campanati A, Diotallevi F, Offidani A. Saliva and oral diseases. J Clin Med. 2020;9:466. doi: 10.3390/jcm9020466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Yakob M, Fuentes L, Wang MB, Abemayor E, Wong DTW. Salivary biomarkers for detection of oral squamous cell carcinoma: current state and recent advances. Curr Oral Health Rep. 2014;1:133‐141. doi: 10.1007/s40496-014-0014-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Gautam SS, Singh RP, Karsauliya K, et al. Label‐free plasma proteomics for the identification of the putative biomarkers of oral squamous cell carcinoma. J Proteomics. 2022;259:104541. doi: 10.1016/j.jprot.2022.104541 [DOI] [PubMed] [Google Scholar]
- 62. Zheng J, Sun L, Yuan W, et al. Clinical value of Naa10p and CEA levels in saliva and serum for diagnosis of oral squamous cell carcinoma. J Oral Pathol Med. 2018;47:830‐835. doi: 10.1111/jop.12767 [DOI] [PubMed] [Google Scholar]
- 63. Rajkumar K, Ramya R, Nandhini G, Rajashree P, Ramesh Kumar A, Nirmala Anandan S. Salivary and serum level of CYFRA 21‐1 in oral precancer and oral squamous cell carcinoma. Oral Dis. 2015;21:90‐96. doi: 10.1111/odi.12216 [DOI] [PubMed] [Google Scholar]
- 64. Ghazi N, Saghravanian N, Shakeri M, Jamali M. Evaluation of CD44 and TGF‐B expression in oral carcinogenesis. J Dent. 2021;22:33‐40. doi: 10.30476/dentjods.2020.84393.1079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Demeda CF, de Carvalho CHP, de Aquino ARL, Nonaka CFW, de Souza LB, Pinto LP. Expression of glucose transporters 1 and 3 in metastatic and non‐metastatic lower lip squamous cell carcinoma. Braz Dent J. 2014;25:372‐378. doi: 10.1590/0103-6440201300054 [DOI] [PubMed] [Google Scholar]
- 66. Xu X‐J, Yuan J, Sun W‐J, et al. Inhibition of MicroRNA‐218 promotes oral squamous cell carcinoma growth by targeting GLUT1 to affect glucose metabolism. Eur Rev Med Pharmacol Sci. 2018;22:7726‐7734. doi: 10.26355/eurrev_201811_16394 [DOI] [PubMed] [Google Scholar]
- 67. Botha H, Farah CS, Koo K, et al. The role of glucose transporters in oral squamous cell carcinoma. Biomolecules. 2021;11:1070. doi: 10.3390/biom11081070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Khyani IAM, Qureshi MA, Mirza T, Farooq MU. Detection of Interleukins‐6 and 8 in saliva as potential biomarkers of oral pre‐malignant lesion and oral carcinoma: a breakthrough in salivary diagnostics in Pakistan. Pak J Pharm Sci. 2017;30:817‐823. [PubMed] [Google Scholar]
- 69. Schiegnitz E, Kämmerer PW, Schön H, et al. Proinflammatory cytokines as serum biomarker in oral carcinoma‐a prospective multi‐biomarker approach. J Oral Pathol Med. 2018;47:268‐274. doi: 10.1111/jop.12670 [DOI] [PubMed] [Google Scholar]
- 70. Arroyo E, Donís SP, Petronacci CMC, et al. Usefulness of protein‐based salivary markers in the diagnosis of oral potentially malignant disorders: a systematic review and meta‐analysis. Cancer Biomark. 2021;32:411‐424. doi: 10.3233/CBM-203043 [DOI] [PubMed] [Google Scholar]
- 71. Ferrari E, Pezzi ME, Cassi D, Pertinhez TA, Spisni A, Meleti M. Salivary cytokines as biomarkers for oral squamous cell carcinoma: a systematic review. Int J Mol Sci. 2021;22:6795. doi: 10.3390/ijms22136795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Segers K, Declerck S, Mangelings D, Heyden YV, Eeckhaut AV. Analytical techniques for Metabolomic studies: a review. Bioanalysis. 2019;11:2297‐2318. doi: 10.4155/bio-2019-0014 [DOI] [PubMed] [Google Scholar]
- 73. Iwasaki Y, Sawada T, Hatayama K, et al. Separation technique for the determination of highly polar metabolites in biological samples. Metabolites. 2012;2:496‐515. doi: 10.3390/metabo2030496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Ishikawa S, Sugimoto M, Konta T, et al. Salivary metabolomics for prognosis of oral squamous cell carcinoma. Front Oncol. 2022;11:789248. doi: 10.3389/fonc.2021.789248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Cadoni G, Giraldi L, Chiarla C, et al. Prognostic role of serum amino acids in head and neck cancer. Dis Markers. 2020;2020:1‐8. doi: 10.1155/2020/2291759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Tantray S, Sharma S, Prabhat K, Nasrullah N, Gupta M. Salivary metabolite signatures of oral cancer and leukoplakia through gas chromatography‐mass spectrometry. J Oral Maxillofac Pathol. 2022;26:31‐37. doi: 10.4103/jomfp.jomfp_335_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Patil DJ, More CB. Salivary metabolomics–a diagnostic and biologic signature for oral cancer. J Oral Maxillofac Surg Med Pathol. 2021;33:546‐554. doi: 10.1016/j.ajoms.2021.02.003 [DOI] [Google Scholar]
- 78. de Sá Alves M, de Sá Rodrigues N, Bandeira CM, et al. Identification of possible salivary metabolic biomarkers and altered metabolic pathways in south American patients diagnosed with oral squamous cell carcinoma. Metabolites. 2021;11:650. doi: 10.3390/metabo11100650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Supawat B, Aye KT, Ritpanja J, et al. Differences in spectroscopic properties of saliva taken from Normal subjects and oral cancer patients: comparison studies. J Fluoresc. 2021;31:747‐754. doi: 10.1007/s10895-021-02707-2 [DOI] [PubMed] [Google Scholar]
- 80. Ishikawa S, Sugimoto M, Edamatsu K, Sugano A, Kitabatake K, Iino M. Discrimination of oral squamous cell carcinoma from oral lichen planus by salivary metabolomics. Oral Dis. 2020;26:35‐42. doi: 10.1111/odi.13209 [DOI] [PubMed] [Google Scholar]
- 81. Ishikawa S, Wong DTW, Sugimoto M, et al. Identification of salivary metabolites for oral squamous cell carcinoma and oral epithelial dysplasia screening from persistent suspicious Oral mucosal lesions. Clin Oral Investig. 2019;23:3557‐3563. doi: 10.1007/s00784-018-2777-3 [DOI] [PubMed] [Google Scholar]
- 82. Ishikawa S, Sugimoto M, Kitabatake K, et al. Identification of salivary Metabolomic biomarkers for oral cancer screening. Sci Rep. 2016;6:31520. doi: 10.1038/srep31520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Song X, Yang X, Narayanan R, et al. Oral squamous cell carcinoma diagnosed from saliva metabolic profiling. Proc Natl Acad Sci. 2020;117:16167‐16173. doi: 10.1073/pnas.2001395117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Mikkonen J, Singh S, Akhi R, et al. Potential role of nuclear magnetic resonance spectroscopy to identify salivary metabolite alterations in patients with head and neck cancer. Oncol Lett. 2018;16:6795‐6800. doi: 10.3892/ol.2018.9419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Lohavanichbutr P, Zhang Y, Wang P, et al. Salivary metabolite profiling distinguishes patients with oral cavity squamous cell carcinoma from Normal controls. PloS One. 2018;13:e0204249. doi: 10.1371/journal.pone.0204249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Ohshima M, Sugahara K, Kasahara K, Katakura A. Metabolomic analysis of the saliva of Japanese patients with oral squamous cell carcinoma. Oncol Rep. 2017;37:2727‐2734. doi: 10.3892/or.2017.5561 [DOI] [PubMed] [Google Scholar]
- 87. Grootveld M, Percival BC, Page G, et al. Updates and original case studies focused on the NMR‐linked metabolomics analysis of human oral fluids part II: applications to the diagnosis and prognostic monitoring of oral and systemic cancers. Metabolites. 2022;12:778. doi: 10.3390/metabo12090778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Panneerselvam K, Ishikawa S, Krishnan R, Sugimoto M. Salivary metabolomics for oral cancer detection: a narrative review. Metabolites. 2022;12:436. doi: 10.3390/metabo12050436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Ren R, Luo H, Su C, Yao Y, Liao W. Machine learning in dental, oral and craniofacial imaging: a review of recent Progress. PeerJ. 2021;9:e11451. doi: 10.7717/peerj.11451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Shah P, Roy N, Dhandhukia P. Algorithm mediated early detection of oral cancer from image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2022;133:70‐79. doi: 10.1016/j.oooo.2021.07.011 [DOI] [PubMed] [Google Scholar]
- 91. Li X, Liu L, Li N, et al. Metabolomics based plasma biomarkers for diagnosis of oral squamous cell carcinoma and oral erosive lichen planus. J Cancer. 2022;13:76‐87. doi: 10.7150/jca.59777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Wu M, Li B, Zhang X, Sun G. Serum metabolomics reveals an innovative diagnostic model for salivary gland tumors. Anal Biochem. 2022;655:114853. doi: 10.1016/j.ab.2022.114853 [DOI] [PubMed] [Google Scholar]
- 93. Zuo L, Chen Z, Chen L, et al. Integrative analysis of metabolomics and Transcriptomics data identifies prognostic biomarkers associated with oral squamous cell carcinoma. Front Oncol. 2021;11:750794. doi: 10.3389/fonc.2021.750794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Sridharan G, Ramani P, Patankar S. Serum metabolomics in oral leukoplakia and oral squamous cell carcinoma. J Cancer Res Ther. 2017;13(3):556‐561. doi: 10.4103/jcrt.JCRT_1233_16 [DOI] [PubMed] [Google Scholar]
- 95. Yang X‐H, Jing Y, Wang S, et al. Integrated non‐targeted and targeted metabolomics uncovers amino acid markers of oral squamous cell carcinoma. Front Oncol. 2020;10:426. doi: 10.3389/fonc.2020.00426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Kasiappan R, Kamarajan P, Kapila YL. Metabolomics in head and neck cancer. In: Sonis ST, Villa A, eds. Translational Systems Medicine and Oral Disease. Elsevier; 2020:119‐135 ISBN 978‐0‐12‐813762‐8. [Google Scholar]
- 97. Musharraf SG, Shahid N, Naqvi SMA, Saleem M, Siddiqui AJ, Ali A. Metabolite profiling of Preneoplastic and neoplastic lesions of oral cavity tissue samples revealed a biomarker pattern. Sci Rep. 2016;6:38985. doi: 10.1038/srep38985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Ogawa T, Washio J, Takahashi T, Echigo S, Takahashi N. Glucose and glutamine metabolism in oral squamous cell carcinoma: insight from a quantitative metabolomic approach. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118:218‐225. doi: 10.1016/j.oooo.2014.04.003 [DOI] [PubMed] [Google Scholar]
- 99. Paul A, Srivastava S, Roy R, et al. Malignancy prediction among tissues from oral SCC patients including neck invasions: a 1H HRMAS NMR based metabolomic study. Metabolomics. 2020;16:38. doi: 10.1007/s11306-020-01660-8 [DOI] [PubMed] [Google Scholar]
- 100. Tsai C‐K, Lin C‐Y, Kang C‐J, et al. Nuclear magnetic resonance metabolomics biomarkers for identifying high risk patients with Extranodal extension in oral squamous cell carcinoma. J Clin Med. 2020;9:951. doi: 10.3390/jcm9040951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Yoshimura N, Yamada S, Aizawa H, Xiao T, Nishimaki F, Kurita H. Glycogen metabolism in an oral dysplastic/cancerous (iodine‐negative) epithelium: glycogen was consumed in the pentose phosphate pathway, not in glycolysis. J Oral Maxillofac Surg Med Pathol. 2019;31:288‐294. doi: 10.1016/j.ajoms.2019.01.002 [DOI] [Google Scholar]
- 102. Kamarajan P, Rajendiran TM, Kinchen J, Bermúdez M, Danciu T, Kapila YL. Head and neck squamous cell carcinoma metabolism draws on Glutaminolysis, and Stemness is specifically regulated by Glutaminolysis via aldehyde dehydrogenase. J Proteome Res. 2017;16:1315‐1326. doi: 10.1021/acs.jproteome.6b00936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Shin JM, Kamarajan P, Fenno JC, Rickard AH, Kapila YL. Metabolomics of head and neck cancer: a mini‐review. Front Physiol. 2016;7:526. doi: 10.3389/fphys.2016.00526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Vitório JG, Duarte‐Andrade FF, Pereira TDSF, et al. Metabolic landscape of oral squamous cell carcinoma. Metabolomics. 2020;16:105. doi: 10.1007/s11306-020-01727-6 [DOI] [PubMed] [Google Scholar]
- 105. de Jonge H, Iamele L, Maggi M, Pessino G, Scotti C. Anti‐cancer auto‐antibodies: roles, applications and open issues. Cancers. 2021;13:813. doi: 10.3390/cancers13040813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Upadhyay S, Sharma N, Gupta KB, Dhiman M. Role of immune system in tumor progression and carcinogenesis. J Cell Biochem. 2018;119:5028‐5042. doi: 10.1002/jcb.26663 [DOI] [PubMed] [Google Scholar]
- 107. Macdonald IK, Parsy‐Kowalska CB, Chapman CJ. Autoantibodies: opportunities for early cancer detection. Trends Cancer. 2017;3:198‐213. doi: 10.1016/j.trecan.2017.02.003 [DOI] [PubMed] [Google Scholar]
- 108. Elkon K, Casali P. Nature and functions of autoantibodies. Nat Clin Pract Rheumatol. 2008;4:491‐498. doi: 10.1038/ncprheum0895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Heo C‐K, Bahk YY, Cho E‐W. Tumor‐associated autoantibodies as diagnostic and prognostic biomarkers. BMB Rep. 2012;45:677‐685. doi: 10.5483/BMBRep.2012.45.12.236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Hsueh P‐C, Chang K‐P, Liu H‐P, et al. Development of a salivary autoantibody biomarker panel for diagnosis of oral cavity squamous cell carcinoma. Front Oncol. 2022;12:968570. doi: 10.3389/fonc.2022.968570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Cabral‐Marques O, Marques A, Giil LM, et al. GPCR‐specific autoantibody signatures are associated with physiological and pathological immune homeostasis. Nat Commun. 2018;9:5224. doi: 10.1038/s41467-018-07598-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Luo H, Wang L, Bao D, et al. Novel autoantibodies related to cell death and DNA repair pathways in systemic lupus erythematosus. Genomics Proteomics Bioinformatics. 2019;17:248‐259. doi: 10.1016/j.gpb.2018.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Xu Y‐W, Chen H, Hong C‐Q, et al. Serum IGFBP‐1 as a potential biomarker for diagnosis of early‐stage upper gastrointestinal tumour. EBioMedicine. 2020;51:102566. doi: 10.1016/j.ebiom.2019.11.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Wu C‐C, Chang Y‐T, Chang K‐P, et al. Salivary auto‐antibodies as noninvasive diagnostic markers of oral cavity squamous cell carcinoma. Cancer Epidemiol Biomarkers Prev. 2014;23:1569‐1578. doi: 10.1158/1055-9965.EPI-13-1269 [DOI] [PubMed] [Google Scholar]
- 115. Tseng Y‐J, Wang Y‐C, Hsueh P‐C, Wu C‐C. Development and validation of machine learning‐based risk prediction models of oral squamous cell carcinoma using salivary autoantibody biomarkers. BMC Oral Health. 2022;22:534. doi: 10.1186/s12903-022-02607-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Pillai J, Chincholkar T, Dixit R, Pandey M. A systematic review of proteomic biomarkers in oral squamous cell cancer. World J Surg Oncol. 2021;19:315. doi: 10.1186/s12957-021-02423-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Liu X, Liang C, Meng Q, et al. Inhibitory effects of circulating natural autoantibodies to CD47‐derived peptides on OSCC cells. Oral Dis. 2021;29:445‐457. doi: 10.1111/odi.13922 [DOI] [PubMed] [Google Scholar]
- 118. Liu X, Huang Z, He Z, Meng Q, Wang X, Hu Y. A study of natural IgG antibodies against ATP‐binding cassette subfamily C member 3 in oral squamous cell carcinoma. J Cancer Res Ther. 2019;15:921‐926. doi: 10.4103/jcrt.JCRT_150_18 [DOI] [PubMed] [Google Scholar]
- 119. Chu H, Chang K, Yen W, et al. Identification of salivary autoantibodies as biomarkers of oral cancer with immunoglobulin a enrichment combined with affinity mass spectrometry. Proteomics. 2023;9:e2200321. doi: 10.1002/pmic.202200321 [DOI] [PubMed] [Google Scholar]
- 120. Radaic A, Kapila Y. The oralome and its dysbiosis: new insights into oral microbiome‐host interactions. Comput Struct Biotechnol J. 2021;19:1335‐1360. doi: 10.1016/j.csbj.2021.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Farquhar DR, Divaris K, Mazul AL, Weissler MC, Zevallos JP, Olshan AF. Poor oral health affects survival in head and neck cancer. Oral Oncol. 2017;73:111‐117. doi: 10.1016/j.oraloncology.2017.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Hashim D, Sartori S, Brennan P, et al. The role of oral hygiene in head and neck cancer: results from international head and neck cancer epidemiology (INHANCE) consortium. Ann Oncol. 2016;27:1619‐1625. doi: 10.1093/annonc/mdw224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Tezal M, Grossi SG, Genco RJ. Is periodontitis associated with oral neoplasms? J Periodontol. 2005;76:406‐410. doi: 10.1902/jop.2005.76.3.406 [DOI] [PubMed] [Google Scholar]
- 124. Shin YJ, Choung HW, Lee JH, Rhyu IC, Kim HD. Association of periodontitis with oral cancer: a case‐control study. J Dent Res. 2019;98:526‐533. doi: 10.1177/0022034519827565 [DOI] [PubMed] [Google Scholar]
- 125. Komlós G, Csurgay K, Horváth F, Pelyhe L, Németh Z. Periodontitis as a risk for oral cancer: a case‐control study. BMC Oral Health. 2021;21:640. doi: 10.1186/s12903-021-01998-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Nwizu N, Wactawski‐Wende J, Genco RJ. Periodontal disease and cancer: epidemiologic studies and possible mechanisms. Periodontol 2000. 2000;83(1):213‐233. doi: 10.1111/prd.12329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Nagy KN, Sonkodi I, Szöke I, Nagy E, Newman HN. The microflora associated with human oral carcinomas. Oral Oncol. 1998;34:304‐308. doi: 10.1016/S1368-8375(98)80012-2 [DOI] [PubMed] [Google Scholar]
- 128. Perera M, Al‐hebshi NN, Speicher DJ, Perera I, Johnson NW. Emerging role of bacteria in oral carcinogenesis: a review with special reference to Perio‐pathogenic bacteria. J Oral Microbiol. 2016;8:32762. doi: 10.3402/jom.v8.32762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Gallimidi AB, Fischman S, Revach B, et al. Periodontal pathogens Porphyromonas Gingivalis and Fusobacterium Nucleatum promote tumor progression in an oral‐specific chemical carcinogenesis model. Oncotarget. 2015;6:22613‐22623. doi: 10.18632/oncotarget.4209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Alon‐Maimon T, Mandelboim O, Bachrach G. Fusobacterium Nucleatum and cancer. Periodontol 2000. 2000;89(1):166‐180. doi: 10.1111/prd.12426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Abed J, Maalouf N, Manson AL, et al. Colon cancer‐associated Fusobacterium Nucleatum may originate from the oral cavity and reach colon tumors via the circulatory system. Front Cell Infect Microbiol. 2020;10:400. doi: 10.3389/fcimb.2020.00400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Mun, L.S. ; Wye Lum, S. ; Sze G.K.Y., et al. Association of microbiome with oral squamous cell carcinoma: a systematic review of the metagenomic studies. Int J Environ Res Public Health 2021, 18, 7224, 10.3390/ijerph18147224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Chattopadhyay I, Verma M, Panda M. Role of oral microbiome signatures in diagnosis and prognosis of oral cancer. Technol Cancer Res Treat. 2019;18:1533033819867354. doi: 10.1177/1533033819867354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Kamarajan P, Ateia I, Shin JM, et al. Periodontal pathogens promote cancer aggressivity via TLR/MyD88 triggered activation of integrin/FAK signaling that is therapeutically reversible by a probiotic Bacteriocin. PLoS Pathog. 2020;16:e1008881. doi: 10.1371/journal.ppat.1008881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Harrandah AM, Chukkapalli SS, Bhattacharyya I, Progulske‐Fox A, Chan EKL. Fusobacteria modulate oral carcinogenesis and promote cancer progression. J Oral Microbiol. 2021;13:1849493. doi: 10.1080/20002297.2020.1849493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Vyhnalova T, Danek Z, Gachova D, Linhartova PB. The role of the oral microbiota in the Etiopathogenesis of oral squamous cell carcinoma. Microorganisms. 2021;9:1549. doi: 10.3390/microorganisms9081549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Ramirez‐Garcia A, Rementeria A, Aguirre‐Urizar JM, et al. Candida Albicans and cancer: can this yeast induce cancer development or progression? Crit Rev Microbiol. 2016;42:181‐193. doi: 10.3109/1040841X.2014.913004 [DOI] [PubMed] [Google Scholar]
- 138. Kaźmierczak‐Siedlecka K, Dvořák A, Folwarski M, Daca A, Przewłócka K, Makarewicz W. Fungal gut microbiota Dysbiosis and its role in colorectal, oral, and pancreatic carcinogenesis. Cancer. 2020;12:1326. doi: 10.3390/cancers12051326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. She Y, Nong X, Zhang M, Wang M. Epstein‐Barr virus infection and oral squamous cell carcinoma risk: a meta‐analysis. PloS One. 2017;12:e0186860. doi: 10.1371/journal.pone.0186860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Katirachi SK, Grønlund MP, Jakobsen KK, Grønhøj C, Von Buchwald C. The prevalence of HPV in oral cavity squamous cell carcinoma. Viruses. 2023;15:451. doi: 10.3390/v15020451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Melo BADC, Vilar LG, Oliveira NRD, et al. Human papillomavirus infection and oral squamous cell carcinoma ‐ a systematic review. Braz J Otorhinolaryngol. 2021;87:346‐352. doi: 10.1016/j.bjorl.2020.10.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Mokhtari M, Beiraghdar M. Evaluation of the prevalence of herpes Simplex‐1 infection in oral squamous cell carcinoma specimens in Alzahra and Kashani hospitals with polymerase chain reaction method in 2012‐2013. Adv Biomed Res. 2015;4:173. doi: 10.4103/2277-9175.163996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Saravani S, Kadeh H, Miri‐Moghaddam E, Zekri A, Sanadgol N, Gholami A. Human cytomegalovirus in oral squamous cell carcinoma in southeast of Iran. Jundishapur J Microbiol. 2015;8:e21838. doi: 10.5812/jjm.21838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Kikuchi K, Noguchi Y, de Rivera MWG‐N, et al. Detection of Epstein‐Barr virus genome and latent infection gene expression in normal epithelia, epithelial dysplasia, and squamous cell carcinoma of the oral cavity. Tumour Biol J Int Soc Oncodevelopmental Biol Med. 2016;37:3389‐3404. doi: 10.1007/s13277-015-4167-7 [DOI] [PubMed] [Google Scholar]
- 145. Hübbers CU, Akgül B. HPV and cancer of the oral cavity. Virulence. 2015;6:244‐248. doi: 10.1080/21505594.2014.999570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Gupta S, Gupta S. Role of human papillomavirus in oral squamous cell carcinoma and oral potentially malignant disorders: a review of the literature. Indian J Dent. 2015;6:91‐98. doi: 10.4103/0975-962X.155877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Lin D, Kouzy R, Abi Jaoude J, et al. Microbiome factors in HPV‐driven carcinogenesis and cancers. PLoS Pathog. 2020;16:e1008524. doi: 10.1371/journal.ppat.1008524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. De Abreu PM, Có ACG, Azevedo PL, et al. Frequency of HPV in oral cavity squamous cell carcinoma. BMC Cancer. 2018;18:324. doi: 10.1186/s12885-018-4247-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Gupta K, Metgud R. Evidences suggesting involvement of viruses in oral squamous cell carcinoma. Patholog Res Int. 2013;2013:1‐17. doi: 10.1155/2013/642496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Yu T, Guo F, Yu Y, et al. Fusobacterium Nucleatum promotes Chemoresistance to colorectal cancer by modulating autophagy. Cell. 2017;170:548‐563. doi: 10.1016/j.cell.2017.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Parhi L, Alon‐Maimon T, Sol A, et al. Breast cancer colonization by Fusobacterium Nucleatum accelerates tumor growth and metastatic progression. Nat Commun. 2020;11:3259. doi: 10.1038/s41467-020-16967-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Udayasuryan B, Ahmad RN, Nguyen TTD, et al. Fusobacterium Nucleatum induces proliferation and migration in pancreatic cancer cells through host autocrine and paracrine signaling. Sci Signal. 2022;15:eabn4948. doi: 10.1126/scisignal.abn4948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Rubinstein MR, Wang X, Liu W, Hao Y, Cai G, Han YW. Fusobacterium Nucleatum promotes colorectal carcinogenesis by modulating E‐cadherin/Beta‐catenin signaling via its FadA Adhesin. Cell Host Microbe. 2013;14:195‐206. doi: 10.1016/j.chom.2013.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Rubinstein MR, Baik JE, Lagana SM, et al. Fusobacterium Nucleatum promotes colorectal cancer by inducing Wnt/Β‐catenin modulator Annexin A1. EMBO Rep. 2019;20:e47638. doi: 10.15252/embr.201847638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Siak PY, Khoo AS‐B, Leong CO, Hoh B‐P, Cheah S‐C. Current status and future perspectives about molecular biomarkers of nasopharyngeal carcinoma. Cancer. 2021;13:3490. doi: 10.3390/cancers13143490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Cristaldi M, Mauceri R, Di Fede O, Giuliana G, Campisi G, Panzarella V. Salivary biomarkers for oral squamous cell carcinoma diagnosis and follow‐up: current status and perspectives. Front Physiol. 2019;10:1476. doi: 10.3389/fphys.2019.01476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Campo F, Zocchi J, Moretto S, et al. Cell‐free human papillomavirus‐ dna for monitoring treatment response of head and neck squamous cell carcinoma: systematic review and meta‐analysis. Laryngoscope. 2022;132:560‐568. doi: 10.1002/lary.29739 [DOI] [PubMed] [Google Scholar]
- 158. Tang KD, Vasani S, Menezes L, et al. Oral HPV16 DNA as a screening tool to detect early oropharyngeal squamous cell carcinoma. Cancer Sci. 2020;111:3854‐3861. doi: 10.1111/cas.14585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Rettig EM, Wang AA, Tran N‐A, et al. Association of pretreatment circulating tumor tissue–modified viral HPV DNA with clinicopathologic factors in HPV‐positive oropharyngeal cancer. JAMA Otolaryngol Neck Surg. 2022;148:1120‐1130. doi: 10.1001/jamaoto.2022.3282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Cao Y, Haring CT, Brummel C, et al. Early HPV CtDNA kinetics and imaging biomarkers predict therapeutic response in P16+ oropharyngeal squamous cell carcinoma. Clin Cancer Res. 2022;28:350‐359. doi: 10.1158/1078-0432.CCR-21-2338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Haring CT, Bhambhani C, Brummel C, et al. Human papilloma virus circulating tumor DNA assay predicts treatment response in recurrent/metastatic head and neck squamous cell carcinoma. Oncotarget. 2021;12:1214‐1229. doi: 10.18632/oncotarget.27992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Veyer D, Wack M, Mandavit M, et al. HPV circulating Tumoral DNA quantification by droplet‐based digital PCR: a promising predictive and prognostic biomarker for HPV‐associated oropharyngeal cancers. Int J Cancer. 2020;147:1222‐1227. doi: 10.1002/ijc.32804 [DOI] [PubMed] [Google Scholar]
- 163. Reder H, Taferner VF, Wittekindt C, et al. Plasma cell‐free human papillomavirus oncogene E6 and E7 DNA predicts outcome in oropharyngeal squamous cell carcinoma. J Mol Diagn. 2020;22:1333‐1343. doi: 10.1016/j.jmoldx.2020.08.002 [DOI] [PubMed] [Google Scholar]
- 164. Chera BS, Kumar S, Beaty BT, et al. Rapid clearance profile of plasma circulating tumor HPV type 16 DNA during Chemoradiotherapy correlates with disease control in HPV‐associated oropharyngeal cancer. Clin Cancer Res. 2019;25:4682‐4690. doi: 10.1158/1078-0432.CCR-19-0211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Lee JY, Garcia‐Murillas I, Cutts RJ, et al. Predicting response to radical (chemo)radiotherapy with circulating HPV DNA in locally advanced head and neck squamous carcinoma. Br J Cancer. 2017;117:876‐883. doi: 10.1038/bjc.2017.258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Simoens C, Gheit T, Ridder R, et al. Accuracy of high‐risk HPV DNA PCR, P16(INK4a) immunohistochemistry or the combination of both to diagnose HPV‐driven oropharyngeal cancer. BMC Infect Dis. 2022;22:676. doi: 10.1186/s12879-022-07654-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Yang X, Song H, Ji T, Du G, Liu W. The implications of gene mutations in salivary DNA for noninvasive diagnosis of head and neck cancer with a focus on oral cancer. Oral Oncol. 2022;130:105924. doi: 10.1016/j.oraloncology.2022.105924 [DOI] [PubMed] [Google Scholar]
- 168. Puttipanyalears C, Arayataweegool A, Chalertpet K, et al. TRH site‐specific methylation in oral and oropharyngeal squamous cell carcinoma. BMC Cancer. 2018;18:786. doi: 10.1186/s12885-018-4706-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. D'Cruz A, Dechamma P, Saldanha M, Maben S, Shetty P, Chakraborty A. Non‐invasive saliva‐based detection of gene mutations in oral cancer patients by oral rub and rinse technique. Asian Pac J Cancer Prev. 2021;22:3287‐3291. doi: 10.31557/APJCP.2021.22.10.3287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Shanmugam A, Hariharan AK, Hasina R, et al. Ultrasensitive detection of tumor‐specific mutations in saliva of patients with oral cavity squamous cell carcinoma. Cancer. 2021;127:1576‐1589. doi: 10.1002/cncr.33393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Schneider M, Winkler K, Kell R, Pfaffl MW, Atkinson MJ, Moertl S. The chaperone protein GRP78 promotes survival and migration of head and neck cancer after direct radiation exposure and extracellular vesicle‐transfer. Front Oncol. 2022;12:842418. doi: 10.3389/fonc.2022.842418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Sato F, Bhawal U, Osaki S, Sugiyama N, Oikawa K, Muragaki Y. Differential Immunohistochemical expression of DEC1, CK‐1ε, and CD44 in oral atypical squamous epithelium and carcinoma in situ . Mol Med Rep. 2022;25:159. doi: 10.3892/mmr.2022.12676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Wilde DC, Castro PD, Bera K, et al. Oropharyngeal cancer outcomes correlate with P16 status, multinucleation and immune infiltration. Mod Patho. 2022;35:1045‐1054. doi: 10.1038/s41379-022-01024-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Shieu M‐K, Ho H‐Y, Lin S‐H, et al. Association of KMT2C genetic variants with the Clinicopathologic development of oral cancer. Int J Environ Res Public Health. 2022;19:3974. doi: 10.3390/ijerph19073974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Shi Y, Liang Y, Wang W, Zhang G. SEC61G identified as a prognostic biomarker of head and neck squamous cell carcinoma. Eur Arch Otorhinolaryngol. 2022;279:2039‐2048. doi: 10.1007/s00405-021-06955-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Rapado‐González Ó, López‐Cedrún JL, Lago‐Lestón RM, et al. Integrity and quantity of salivary cell‐free dna as a potential molecular biomarker in oral cancer: a preliminary study. J Oral Pathol Med. 2022;51:429‐435. doi: 10.1111/jop.13299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Burcher KM, Faucheux AT, Lantz JW, et al. Prevalence of DNA repair gene mutations in blood and tumor tissue and impact on prognosis and treatment in HNSCC. Cancer. 2021;13:3118. doi: 10.3390/cancers13133118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Arora R, Haynes L, Kumar M, et al. NCBP2 and TFRC are novel prognostic biomarkers in oral squamous cell carcinoma. Cancer Gene Ther. 2023;30:752‐765. doi: 10.1038/s41417-022-00578-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Yang W, Zhou W, Zhao X, et al. Prognostic biomarkers and therapeutic targets in oral squamous cell carcinoma: a study based on cross‐database analysis. Hereditas. 2021;158:15. doi: 10.1186/s41065-021-00181-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Dioguardi M, Spirito F, Sovereto D, et al. MicroRNA‐21 expression as a prognostic biomarker in oral cancer: systematic review and meta‐analysis. Int J Environ Res Public Health. 2022;19:3396. doi: 10.3390/ijerph19063396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Xie Y, Wu J. MicroRNA‐21 as prognostic molecular signatures in oral cancer: a meta‐analysis. Int J Clin Exp Med. 2017;10:9848‐9856. [Google Scholar]
- 182. Niklander S, Guerra D, Contreras F, González‐Arriagada W, Marín C. MicroRNAs and their role in the malignant transformation of oral leukoplakia: a scoping review. Med Oral Patol Oral Cirugia Bucal. 2022;27:e77‐e84. doi: 10.4317/medoral.24975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183. Troiano G, Boldrup L, Ardito F, Gu X, Lo Muzio L, Nylander K. Circulating MiRNAs from blood, plasma or serum as promising clinical biomarkers in oral squamous cell carcinoma: a systematic review of current findings. Oral Oncol. 2016;63:30‐37. doi: 10.1016/j.oraloncology.2016.11.001 [DOI] [PubMed] [Google Scholar]
- 184. Shen M, Zhou Z, Li BB, et al. Investigation of MiR‐21‐5p key target genes and pathways in head and neck squamous cell carcinoma based on TCGA database and bioinformatics analysis. Technol Cancer Res Treat. 2022;21:153303382210812. doi: 10.1177/15330338221081245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Robinson S, Ngwenya S, Molaudzi M, Molepo J, Adeola H, Magangane P. The clinicopathological and Microrna expression signature associated with Lymphovascular invasion in squamous cell carcinoma: a basic descriptive study. Health Sci Rep. 2022;5:e958. doi: 10.1002/hsr2.958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Shan L, Lu Y, Song Y, et al. Identification of nine M6A‐related Long noncoding RNAs as prognostic signatures associated with oxidative stress in oral cancer based on data from the cancer genome atlas. Oxid Med Cell Longev. 2022;2022:1‐18. doi: 10.1155/2022/9529814 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 187. Rajthala S, Parajuli H, Dongre HN, et al. MicroRNA‐138 abates fibroblast motility with effect on invasion of adjacent cancer cells. Front Oncol. 2022;12:833582. doi: 10.3389/fonc.2022.833582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Qin S, Li B, Chen M, Qin M, Liu J, Lv Q. MiR‐32‐5p promoted epithelial‐to‐mesenchymal transition of oral squamous cell carcinoma cells via regulating the KLF2/CXCR4 pathway. Kaohsiung J Med Sci. 2022;38:120‐128. doi: 10.1002/kjm2.12450 [DOI] [PubMed] [Google Scholar]
- 189. Saito M. Novel roles of Nanog in cancer cells and their extracellular vesicles. Cell. 2022;11:3881. doi: 10.3390/cells11233881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Baillie R, Tan ST, Itinteang T. Cancer stem cells in oral cavity squamous cell carcinoma: a review. Front Oncol. 2017;7:112. doi: 10.3389/fonc.2017.00112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Philouze P, Gauthier A, Lauret A, et al. CD44, γ‐H2AX, and p‐ATM expressions in short‐term ex vivo culture of tumour slices predict the treatment response in patients with oral squamous cell carcinoma. Int J Mol Sci. 2022;23:877. doi: 10.3390/ijms23020877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192. Wang H, Wu M, Chang P, et al. The change in circulating tumor cells before and during concurrent Chemoradiotherapy is associated with survival in patients with locally advanced head and neck cancer. Head Neck. 2019;41:2676‐2687. doi: 10.1002/hed.25744 [DOI] [PubMed] [Google Scholar]
- 193. Fanelli MF, Oliveira TB, Braun AC, et al. Evaluation of incidence, significance, and prognostic role of circulating tumor microemboli and transforming growth factor‐β receptor I in head and neck cancer. Head Neck. 2017;39:2283‐2292. doi: 10.1002/hed.24899 [DOI] [PubMed] [Google Scholar]
- 194. AlAli AM, Walsh T, Maranzano M. CYFRA 21‐1 and MMP‐9 as salivary biomarkers for the detection of oral squamous cell carcinoma: a systematic review of diagnostic test accuracy. Int J Oral Maxillofac Surg. 2020;49:973‐983. doi: 10.1016/j.ijom.2020.01.020 [DOI] [PubMed] [Google Scholar]
- 195. Dikova V, Jantus‐Lewintre E, Bagan J. Potential non‐invasive biomarkers for early diagnosis of oral squamous cell carcinoma. J Clin Med. 2021;10:1658. doi: 10.3390/jcm10081658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Sivadasan P, Gupta MK, Sathe G, et al. Salivary proteins from dysplastic leukoplakia and oral squamous cell carcinoma and their potential for early detection. J Proteomics. 2020;212:103574. doi: 10.1016/j.jprot.2019.103574 [DOI] [PubMed] [Google Scholar]
- 197. Ameena M, Rathy R. Evaluation of tumor necrosis factor: alpha in the saliva of oral cancer, leukoplakia, and healthy controls – a comparative study. J Int Oral Health. 2019;11:92‐99. [Google Scholar]
- 198. Deepthi G, Nandan SRK, Kulkarni PG. Salivary tumour necrosis factor‐α as a biomarker in oral leukoplakia and oral squamous cell carcinoma. Asian Pac J Cancer Prev. 2019;20:2087‐2093. doi: 10.31557/APJCP.2019.20.7.2087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Lee LT, Wong YK, Hsiao HY, Wang YW, Chan MY, Chang KW. Evaluation of saliva and plasma cytokine biomarkers in patients with oral squamous cell carcinoma. Int J Oral Maxillofac Surg. 2018;47:699‐707. doi: 10.1016/j.ijom.2017.09.016 [DOI] [PubMed] [Google Scholar]
- 200. Abbas MJ, Rawi NAA, Al‐Duboni GI. The role of salivary interleukin 17 as a dependent positive predictive biomarker among Iraqi patients with oral squamous cell carcinoma. J Phamaceutical Sci Res. 2018;10:3149‐3152. [Google Scholar]
- 201. Seyedmajidi S, Seyedmajidi M, Foroughi R, et al. Comparison of salivary and serum soluble CD44 levels between patients with oral SCC and healthy controls. Asian Pac J Cancer Prev. 2018;19:3059‐3063. doi: 10.31557/APJCP.2018.19.11.3059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Awasthi N. Role of salivary biomarkers in early detection of oral squamous cell carcinoma. Indian J Pathol Microbiol. 2017;60:464. doi: 10.4103/IJPM.IJPM_140_16 [DOI] [PubMed] [Google Scholar]
- 203. Peisker A, Raschke G, Fahmy M, et al. Salivary MMP‐9 in the detection of oral squamous cell carcinoma. Med Oral Patol Oral Cirugia Bucal. 2017;22:e270‐e275. doi: 10.4317/medoral.21626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Yu J‐S, Chen Y‐T, Chiang W‐F, et al. Saliva protein biomarkers to detect oral squamous cell carcinoma in a high‐risk population in Taiwan. Proc Natl Acad Sci. 2016;113:11549‐11554. doi: 10.1073/pnas.1612368113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. Polz‐Dacewicz M, Strycharz‐Dudziak M, Dworzański J, Stec A, Kocot J. Salivary and serum IL‐10, TNF‐α, TGF‐β, VEGF levels in oropharyngeal squamous cell carcinoma and correlation with HPV and EBV infections. Infect Agent Cancer. 2016;11:45. doi: 10.1186/s13027-016-0093-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Gleber‐Netto FO, Yakob M, Li F, et al. Salivary biomarkers for detection of oral squamous cell carcinoma in a Taiwanese population. Clin Cancer Res. 2016;22:3340‐3347. doi: 10.1158/1078-0432.CCR-15-1761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Dineshkumar T, Ashwini BK, Rameshkumar A, Rajashree P, Ramya R, Rajkumar K. Salivary and serum Interleukin‐6 levels in oral premalignant disorders and squamous cell carcinoma: diagnostic value and Clinicopathologic correlations. Asian Pac J Cancer Prev. 2016;17:4899‐4906. doi: 10.22034/APJCP.2016.17.11.4899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. Ghallab NA, Shaker OG. Serum and salivary levels of Chemerin and MMP‐9 in oral squamous cell carcinoma and oral premalignant lesions. Clin Oral Investig. 2017;21:937‐947. doi: 10.1007/s00784-016-1846-8 [DOI] [PubMed] [Google Scholar]
- 209. Aziz S, Ahmed SS, Ali A, et al. Salivary immunosuppressive cytokines IL‐10 and IL‐13 are significantly elevated in oral squamous cell carcinoma patients. Cancer Invest. 2015;33:318‐328. doi: 10.3109/07357907.2015.1041642 [DOI] [PubMed] [Google Scholar]
- 210. Zhang M, Chen X, Chen H, et al. Identification and validation of potential novel biomarkers for oral squamous cell carcinoma. Bioengineered. 2021;12:8845‐8862. doi: 10.1080/21655979.2021.1987089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211. Ramos‐García P, González‐Moles MÁ, Warnakulasuriya S. Significance of P53 overexpression in the prediction of the malignant transformation risk of oral potentially malignant disorders: a systematic review and meta‐analysis. Oral Oncol. 2022;126:105734. doi: 10.1016/j.oraloncology.2022.105734 [DOI] [PubMed] [Google Scholar]
- 212. Ramos‐García P, González‐Moles MÁ. Prognostic and clinicopathological significance of the aberrant expression of β‐catenin in oral squamous cell carcinoma: a systematic review and meta‐analysis. Cancer. 2022;14:479. doi: 10.3390/cancers14030479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. Upadhaya P, Giri S, Barhoi D, Bhattacharjee A. Altered expression of junctional proteins as a potential biomarker in oral precancerous and cancerous patients. Tissue Barriers. 2022;10:1973329. doi: 10.1080/21688370.2021.1973329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214. Zhang X, Kim K‐Y, Zheng Z, Bazarsad S, Kim J. Nomogram for risk prediction of malignant transformation in oral leukoplakia patients using combined biomarkers. Oral Oncol. 2017;72:132‐139. doi: 10.1016/j.oraloncology.2017.07.015 [DOI] [PubMed] [Google Scholar]
- 215. Gissi DB, Gabusi A, Servidio D, Cervellati F, Montebugnoli L. Predictive role of P53 protein as a single marker or associated with Ki67 antigen in oral leukoplakia: a retrospective longitudinal study. Open Dent J. 2015;9:41‐45. doi: 10.2174/1874210601509010041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216. Mumtaz M, Bijnsdorp IV, Böttger F, et al. Secreted protein markers in oral squamous cell carcinoma (OSCC). Clin Proteomics. 2022;19:4. doi: 10.1186/s12014-022-09341-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217. Rodríguez‐Molinero J, del Carmen Migueláñez‐Medrán B, Delgado‐Somolinos E, Carreras‐Presas CM, López‐Sánchez AF. Advances in the diagnosis, monitoring, and progression of oral cancer through saliva: an update. Biomed Res Int. 2022;2022:1‐21. doi: 10.1155/2022/2739869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218. Shigeyama H, Wang T, Ichinose M, Ansai T, Lee S‐W. Identification of volatile metabolites in human saliva from patients with oral squamous cell carcinoma via zeolite‐based thin‐film microextraction coupled with GC–MS. J Chromatogr B. 2019;1104:49‐58. doi: 10.1016/j.jchromb.2018.11.002 [DOI] [PubMed] [Google Scholar]
- 219. Sridharan G, Ramani P, Patankar S, Vijayaraghavan R. Evaluation of salivary metabolomics in oral leukoplakia and oral squamous cell carcinoma. J Oral Pathol Med. 2019;48:299‐306. doi: 10.1111/jop.12835 [DOI] [PubMed] [Google Scholar]
- 220. Taware R, Taunk K, Pereira JAM, et al. Volatilomic insight of head and neck cancer via the effects observed on saliva metabolites. Sci Rep. 2018;8:17725. doi: 10.1038/s41598-018-35854-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221. Zhang W, Jing Y, Wang S, et al. Identification of biological functions and prognostic value of NNMT in oral squamous cell carcinoma. Biomolecules. 2022;12:1487. doi: 10.3390/biom12101487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222. Chen X, Kuang S, He Y, et al. The differential metabolic response of Oral squamous cell carcinoma cells and normal oral epithelial cells to cisplatin exposure. Metabolites. 2022;12:389. doi: 10.3390/metabo12050389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223. Tripathi P, Kamarajan P, Somashekar BS, et al. Delineating metabolic signatures of head and neck squamous cell carcinoma: phospholipase A2, a potential therapeutic target. Int J Biochem Cell Biol. 2012;44:1852‐1861. doi: 10.1016/j.biocel.2012.06.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224. Lin Y‐H, Wu C‐C, Chen W‐L, Chang K‐P. Anti‐P53 autoantibody detection in automatic glass capillary immunoassay platform for screening of oral cavity squamous cell carcinoma. Sensors. 2020;20:971. doi: 10.3390/s20040971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225. Schutt CA, Mirandola L, Figueroa JA, et al. The cancer‐testis antigen, sperm protein 17, a new biomarker and immunological target in head and neck squamous cell carcinoma. Oncotarget. 2017;8:100280‐100287. doi: 10.18632/oncotarget.22213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226. Peter TK, Withanage MHH, Comnick CL, et al. Systematic review and meta‐analysis of oral squamous cell carcinoma associated oral microbiome. Front Microbiol. 2022;13:968304. doi: 10.3389/fmicb.2022.968304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227. Mauceri R, Coppini M, Vacca D, et al. Salivary microbiota composition in patients with oral squamous cell carcinoma: a systematic review. Cancer. 2022;14:5441. doi: 10.3390/cancers14215441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228. Ibáñez L, de Mendoza I, Maritxalar Mendia X, García de la Fuente AM, Quindós Andrés G, Aguirre Urizar JM. Role of Porphyromonas Gingivalis in oral squamous cell carcinoma development: a systematic review. J Periodontal Res. 2020;55:13‐22. doi: 10.1111/jre.12691 [DOI] [PubMed] [Google Scholar]
- 229. Ramos RT, Sodré CS, de Sousa Rodrigues PMGR, et al. High‐throughput nucleotide sequencing for Bacteriome studies in oral squamous cell carcinoma: a systematic review. Oral Maxillofac Surg. 2020;24:387‐401. doi: 10.1007/s10006-020-00873-4 [DOI] [PubMed] [Google Scholar]
- 230. Yang SF, Lin CW, Chuang CY, et al. Host genetic associations with salivary microbiome in oral cancer. J Dent Res. 2022;101:590‐598. doi: 10.1177/00220345211051967 [DOI] [PubMed] [Google Scholar]
- 231. Gopinath D, Menon RK, Wie CC, et al. Differences in the Bacteriome of swab, saliva, and tissue biopsies in oral cancer. Sci Rep. 2021;11:1181. doi: 10.1038/s41598-020-80859-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232. Gopinath D, Kunnath Menon R, Chun Wie C, et al. Salivary bacterial shifts in oral leukoplakia resemble the dysbiotic oral cancer Bacteriome. J Oral Microbiol. 2020;13:1857998. doi: 10.1080/20002297.2020.1857998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233. Ganly I, Yang L, Giese RA, et al. Periodontal pathogens are a risk factor of oral cavity squamous cell carcinoma, independent of tobacco and alcohol and human papillomavirus: periodontal pathogens are a risk factor for Oral cancer. Int J Cancer. 2019;145:775‐784. doi: 10.1002/ijc.32152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234. Yang C‐Y, Yeh Y‐M, Yu H‐Y, et al. Oral microbiota community dynamics associated with oral squamous cell carcinoma staging. Front Microbiol. 2018;9:862. doi: 10.3389/fmicb.2018.00862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235. Hsiao J‐R, Chang C‐C, Lee W‐T, et al. The interplay between oral microbiome, lifestyle factors and genetic polymorphisms in the risk of oral squamous cell carcinoma. Carcinogenesis. 2018;39:778‐787. doi: 10.1093/carcin/bgy053 [DOI] [PubMed] [Google Scholar]
- 236. Lee W‐H, Chen H‐M, Yang S‐F, et al. Bacterial alterations in salivary microbiota and their association in oral cancer. Sci Rep. 2017;7:16540. doi: 10.1038/s41598-017-16418-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237. Al‐Hebshi NN, Nasher AT, Maryoud MY, et al. Inflammatory Bacteriome featuring Fusobacterium Nucleatum and pseudomonas aeruginosa identified in association with oral squamous cell carcinoma. Sci Rep. 2017;7:1834. doi: 10.1038/s41598-017-02079-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238. Wang K, Lu W, Tu Q, et al. Preliminary analysis of salivary microbiome and their potential roles in oral lichen planus. Sci Rep. 2016;6:22943. doi: 10.1038/srep22943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239. Hu X, Zhang Q, Hua H, Chen F. Changes in the salivary microbiota of oral leukoplakia and oral cancer. Oral Oncol. 2016;56:e6‐e8. doi: 10.1016/j.oraloncology.2016.03.007 [DOI] [PubMed] [Google Scholar]
- 240. Yost S, Stashenko P, Choi Y, et al. Increased virulence of the oral microbiome in oral squamous cell carcinoma revealed by Metatranscriptome analyses. Int J oral Sci. 2018;10:32. doi: 10.1038/s41368-018-0037-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241. Zhao H, Chu M, Huang Z, et al. Variations in oral microbiota associated with oral cancer. Sci Rep. 2017;7:11773. doi: 10.1038/s41598-017-11779-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242. Nie F, Wang L, Huang Y, et al. Characteristics of microbial distribution in different oral niches of oral squamous cell carcinoma. Front Cell Infect Microbiol. 2022;12:905653. doi: 10.3389/fcimb.2022.905653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243. Nieminen MT, Listyarifah D, Hagström J, et al. Treponema Denticola chymotrypsin‐like proteinase may contribute to Orodigestive carcinogenesis through immunomodulation. Br J Cancer. 2018;118:428‐434. doi: 10.1038/bjc.2017.409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244. Perera M, Al‐hebshi NN, Perera I, et al. A dysbiotic mycobiome dominated by Candida Albicans is identified within oral squamous‐cell carcinomas. J Oral Microbiol. 2017;9:1385369. doi: 10.1080/20002297.2017.1385369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245. Listyarifah D, Nieminen MT, Mäkinen LK, et al. Treponema Denticola chymotrypsin‐like proteinase is present in early‐stage Mobile tongue squamous cell carcinoma and related to the Clinicopathological features. J Oral Pathol Med. 2018;47:764‐772. doi: 10.1111/jop.12729 [DOI] [PubMed] [Google Scholar]
- 246. Shin JM, Luo T, Kamarajan P, Fenno JC, Rickard AH, Kapila YL. Microbial communities associated with primary and metastatic head and neck squamous cell carcinoma ‐ a high fusobacterial and low streptococcal signature. Sci Rep. 2017;7:9934. doi: 10.1038/s41598-017-09786-x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable; All materials/information are provided in the manuscript.


