ABSTRACT
Objectives
Self‐performed oral hygiene is essential for preventing dental caries, periodontal, and peri‐implant diseases. Oral irrigators are adjunctive oral home care aids that may benefit oral health. However, the effects of oral irrigation on oral health, its role in oral home care, and its mechanism of action are not fully understood. A comprehensive search of the literature revealed no existing broad scoping reviews on oral irrigators. Therefore, this study aimed to provide a comprehensive systematic review of the literature on oral irrigation devices and identify evidence gaps.
Methods
The Joanna Briggs Institute and Preferred Reporting Items for Systematic reviews and Meta‐Analyses extension for Scoping Reviews guidelines were utilized to prepare the review. Four databases and eight gray literature sources were searched for English publications across any geographical location or setting.
Results
Two hundred and seventy‐five sources were included, predominantly from scientific journals and academic settings. Most studies originated from North America. Research primarily involved adults, with limited studies in children and adolescents. Oral irrigation was safe and well‐accepted when used appropriately. It reduced periodontal inflammation, potentially by modulating the oral microbiota, but further research needs to clarify its mechanism of action. Promising results were reported in populations with dental implants and special needs. Patient acceptance appeared high, but standardized patient‐reported outcome measures were rarely used. Anti‐inflammatory benefits occurred consistently across populations and irrigant solutions. Plaque reduction findings were mixed, potentially reflecting differences in study designs and devices.
Conclusions
Oral irrigators reduce periodontal inflammation, but their impact on plaque removal remains unclear. Well‐designed, sufficiently powered trials of appropriate duration need to assess the clinical, microbiological, and inflammatory responses of the periodontium to oral irrigation, particularly those with periodontitis, dental implants, and special needs. Patient‐reported outcome measures, costs, caries prevention, and environmental impact of oral irrigation need to be compared to other oral hygiene aids.
Keywords: dental devices, home care; dental plaque; oral hygiene; periodontitis
1. Introduction
Despite being largely preventable, dental caries, gingivitis, and periodontitis remain the most prevalent chronic noncommunicable diseases worldwide (Bernabe et al. 2020). Not only can these diseases lead to edentulism, masticatory dysfunction, and disability, but they can also place a significant financial burden on individuals and the global economy. For example, global yearly costs of dental diseases reached a staggering USD544.41 billion in 2015 (Righolt et al. 2018). Furthermore, oral diseases negatively affect systemic health (Manoil et al. 2021; Silbereisen et al. 2023).
Dental biofilms are complex multispecies microbial communities forming on nonshedding tooth surfaces (Belibasakis et al. 2023). Dysbiotic dental biofilm is involved in the pathogenesis of both caries and periodontitis, with regular biofilm disruption playing a crucial role in preventing these diseases. As emphasized in the European Federation of Periodontology (EFP) S3 level clinical practice guideline for the treatment of Stage I–III periodontitis, adequate self‐performed oral hygiene is essential for optimal response to periodontal treatment and secondary prevention of periodontitis, as individuals successfully treated for periodontitis remain at an increased risk for the disease recurrence (Sanz et al. 2020). As periodontitis affects approximately half of people worldwide and negatively impacts oral and systemic health (Petersen and Ogawa 2012; Tonetti et al. 2017), effective and well‐accepted oral home care measures are essential for this population. However, due to the scarcity of high‐quality evidence, the EFP guideline does not make a strong conclusion on any specific interdental oral hygiene aid for individuals in periodontal maintenance (Sanz et al. 2020). Similarly, a Cochrane review on the effectiveness of interdental cleaning aids for caries and periodontal diseases prevention published in 2019 could not identify any studies assessing caries, with authors calling for long‐term trials to assess this outcome (Worthington et al. 2019).
Another common group of diseases induced by biofilms are peri‐implant diseases, with the prevalence of peri‐implant mucositis being 46.83% and peri‐implantitis 19.83% (Lee et al. 2017). The diseases may be associated with considerable morbidity and treatment costs (Herrera et al. 2023). Furthermore, peri‐implantitis can progress significantly faster than periodontitis, and its progression will often lead to implant loss (Schwarz et al. 2018). The EFP S3 level clinical practice guideline for the prevention and treatment of peri‐implant diseases emphasizes that appropriate biofilm control is essential for preserving peri‐implant health and achieving optimal peri‐implant treatment outcomes (Herrera et al. 2023). However, despite the importance of self‐performed oral care in this population, the guideline states it is not known which method of home care is the most effective in individuals treated for peri‐implantitis due to the absence of studies comparing different home care methods.
Toothbrushing can effectively disrupt biofilms and, thus, prevent the development or arrest of the progression of dental caries and periodontal diseases (Worthington et al. 2019). However, a toothbrush cannot disrupt biofilm on interproximal surfaces of the teeth and prostheses in close contact and may not access some hard‐to‐reach areas. This presents a significant problem, with approximal surfaces commonly affected by dental caries and periodontitis (Lorentz et al. 2009; Pretty and Ekstrand 2016). Adjunctive tools, such as interdental brushes and string floss, should supplement toothbrushing in these areas (Worthington et al. 2019). However, these tools require a certain level of dexterity from the operator and may be challenging to use in hard‐to‐reach areas. Furthermore, all oral hygiene aids have the potential to cause trauma, which necessitates monitoring their use and tailoring oral home care to the patient's situation (Sanz et al. 2020).
In addition, certain populations may experience difficulties maintaining good oral hygiene due to low manual dexterity or factors hindering appropriate biofilm control. For example, fixed orthodontic appliances increase oral disease risk by retaining dental biofilm (Mulimani and Popowics 2022). Meticulous oral hygiene is required in this population to prevent dental caries and periodontal diseases, but it may be challenging to achieve. Another example is intermaxillary fixation, which makes acceptable oral hygiene nearly impossible (Tsolov 2022). Further, individuals with mental and physical disabilities, who collectively represent about 16% of the global population (World Health Organization 2023), may not be able to maintain acceptable oral hygiene with conventional oral hygiene aids (Buda 2016). Additionally, both EFP guidelines for the prevention and treatment of peri‐implant diseases and treatment of Stage I–III periodontitis emphasize that clinicians need to consider their client's personal preferences when recommending oral home care aids to support compliance and adherence to oral hygiene measures (Herrera et al. 2023; Sanz et al. 2020). Therefore, oral health practitioners need to have a wide variety of aids to choose from.
One of the adjunctive aids, which is considered to be generally safe, well‐accepted by patients, and able to access hard‐to‐reach areas, is an oral irrigation device (Herrera et al. 2023; Sanz et al. 2020). The US Food & Drug Administration (2023) defines it as an electric device that creates “a pressurised stream of water to remove food particles between the teeth and promote good periodontal condition.” Oral irrigators (OIs) were launched into the market in 1962 (Ciancio 2009). They perform cleaning by a pulsating or continuous stream of pressured water and can also deliver antimicrobial solutions subgingivally. Most self‐contained oral irrigation units available in the market today are pulsating devices. The pulsating action of these devices produces a compression and decompression phase, which is key to their efficacy (Lyle 2012; Mancinelli‐Lyle et al. 2023).
Regular oral irrigation may reduce periodontal and peri‐implant inflammation (Gennai et al. 2023; Slot, Valkenburg, and Van der Weijden 2020). Adjunctive irrigation is suggested for individuals with periodontitis and peri‐implant mucositis when interdental brushes cannot be used or in addition to other home care measures (Herrera et al. 2023; Sanz et al. 2020). However, evidence regarding these devices' biofilm removal ability and mechanism of action has been inconclusive, with experts calling for more clinical studies on OIs (Gennai et al. 2023; Herrera et al. 2023; Sanz et al. 2020; Slot, Valkenburg, and Van der Weijden 2020).
To avoid wasting resources and prioritize areas requiring further investigation, future research should be guided by the available evidence and existing knowledge gaps (Feres et al. 2022). However, it is unclear what kind of research has been conducted on OIs, as no broad systematic reviews could be identified on the topic. Some existing reviews covered multiple oral hygiene aids and did not focus on a detailed investigation of OIs (Gennai et al. 2023; Slot, Valkenburg, and Van der Weijden 2020; Van der Weijden and van Loveren 2023). Reviews that have focused exclusively on OIs either answered narrow questions concerning OIs' efficacy and safety or focused on a specific condition or population and, therefore, included a limited number of studies identified through restricted search strategies (Allen 2019; AlMoharib et al. 2023; Husseini, Slot, and Van der Weijden 2008; Jolkovsky and Lyle 2015). A comprehensive scoping review is needed to map the evidence that has accumulated on these devices since their launch in the market and to identify research gaps to guide future research. Therefore, this scoping review aims to systematically map the evidence on oral irrigation devices and identify any research gaps.
2. Methods
The scoping review was conducted following the Joanna Briggs Institute (JBI) guidance for scoping reviews (Aromataris and Munn 2020), and the manuscript was prepared using the PRISMA‐ScR (Preferred Reporting Items for Systematic reviews and Meta‐Analyses extension for Scoping Reviews) guidelines (Tricco et al. 2018).
The research question was established using the JBI's ‘population, concept, context’ framework (Aromataris and Munn 2020). The concept identified was “oral irrigation devices.” Population and context are irrelevant as this review aims to identify a broad range of evidence on OIs irrespective of the population and setting. This review aims to answer the following primary research question: “What is known about oral irrigation devices?”; the subquestions addressed are: “What methodologies have been used in research? What research gaps exist concerning oral irrigation devices? What aspects require further investigation?” Primary and secondary research published in English across any geographical location or setting was considered for inclusion; letters, narratives, opinion pieces, commentaries, guidelines, registered trials with no results available, and historical reviews were excluded.
The search strategy was developed with the assistance of a health sciences librarian. The main searches of four databases (CINAHL, the Dentistry and Oral Sciences Source, MEDLINE, and Scopus) and eight sources of gray literature (Cochrane Library, Cochrane Oral Health's Trials Register, Google, Google Scholar, the ISRCTN Registry, Open Gray, ProQuest Dissertations and Theses Global, and the WHO Clinical Trials Registry Platform) were conducted on January 12, 2022, with no date limiters applied, with a follow‐up search to capture newly published sources on December 23 and 24, 2023. In addition, citation searching for eligible sources was performed via Scopus. The search strategy is presented in Table 1.
Table 1.
Search strategy.
| Search number | Search terms |
|---|---|
| 1 | “Water irrig*” OR “Water floss*” OR (“therapeutic irrig*” AND water) OR “oral irrigat*” OR monojet OR “subgingival irrigat*” OR “subgingival tip” OR “dental irrigat*” OR “interdental device*” OR “gingiv* therapeutic irrigation” OR “interdental cleaning device*” OR (“interdental cleaning” AND water) OR (“interdental cleaning” AND irrigat*) OR (“inter‐dental cleaning” AND water) OR (“inter‐dental cleaning” AND irrigat*) OR “irrigation device*” OR “supragingival irrigat*” OR “pulsated jet” OR “microdroplet device*” OR “micro droplet device*” OR “Water pik” OR waterpik OR waterpick OR “water pick” OR “water jet” OR waterjet OR “perio pik” OR “pick pocket” OR pickpocket OR “pik pocket” OR pikpocket |
| 2 | “Oral health” OR dental OR dentistry OR caries OR periodont* OR gingiv* OR “oral hygiene” |
Note: Search terms used for CINAHL, the Dentistry and Oral Sciences Source, MEDLINE, and Scopus; Steps 1 and 2 were combined for the final search. The gray literature search was conducted using the same search terms, with the search strategy customized for each database.
Sources identified through databases were uploaded into EndNote VX9 to remove duplicates before being transferred to RAYYAN (Ouzzani et al. 2016; The EndNote Team 2013); 1769 records were kept to screen titles and abstracts. A pilot test involving independent screening of titles and abstracts by two reviewers was conducted to ensure a 75% agreement rate before proceeding with full‐scale screening. Discrepancies were discussed and resolved through discussion. After the titles and abstracts screening, 418 sources were retrieved for the full‐text evaluation. Of those, 174 items did not meet the inclusion criteria, with 244 items included in the review from databases and an additional 31 sources included after the gray literature and Scopus citation searching (Figure 1).
Figure 1.
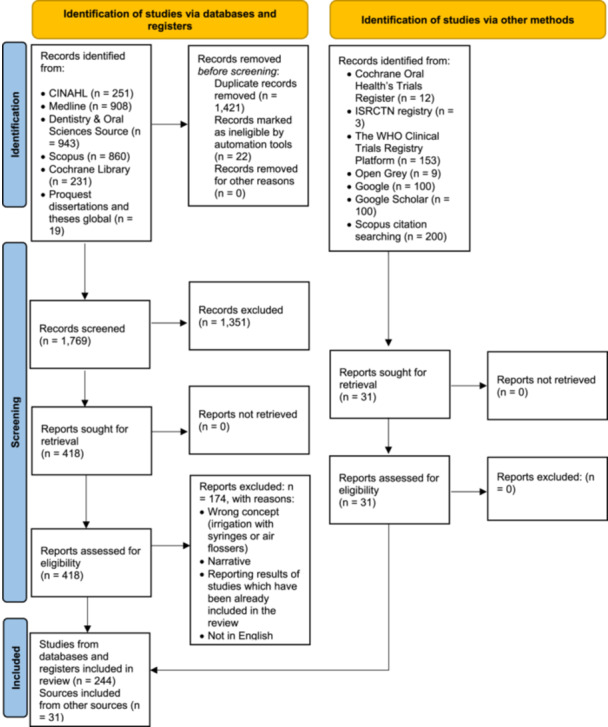
PRISMA flow diagram. Search results and source selection.
Although we identified several studies referring to air flossers as dental water jets, water flossers, or OIs (Bertl et al. 2022; Kim, Lee, and Jwa 2016; Mazzoleni et al. 2019; Sirinirund et al. 2023; Wiesmüller et al. 2023), these trials were excluded from this scoping review. Unlike conventional OIs, which produce a pressurized water stream, air flossers use a pressured air stream with water droplets (Wiesmüller et al. 2023). Such a significant technological difference calls for differentiation between research on conventional oral irrigation devices and air flossers.
Letters were excluded from the review. However, one letter was selected for inclusion because it presented a case report (Kaplan and Anderson 1977). Furthermore, while narrative reviews were not included in this scoping review, the review by Liang et al. (2020) was selected for inclusion, as the literature search for this evidence‐based practical decision tree was performed systematically.
Data extraction was performed using a refined version of the publicly available data extraction protocol (Sarkisova and Morse 2022). The changes to the data extraction table were based on initial findings to capture all the information necessary to answer the review questions. The aim was to provide a comprehensive overview of the literature, excluding bias risk assessment due to the broad nature of the review. Data were extracted by one reviewer and verified by another, with any disagreements resolved through discussion. We grouped the studies by methodology and further subgrouped them by broad themes, irrigating solutions, and populations.
3. Results
3.1. Characteristics of the Included Studies
A total of 275 sources were included in the review, predominantly from scientific journals (259) and conducted in academic settings (227), detailed in Supporting Information S1: Appendices 1 and 2.
The majority of studies originated from North America (148), followed by Western Europe (49) and Asia (47). Smaller numbers originated from the Middle East (22), South America (4), Africa (2), and Oceania (1), while two did not report location (Figure 2). Publication trends over time are shown in Figure 3.
Figure 2.
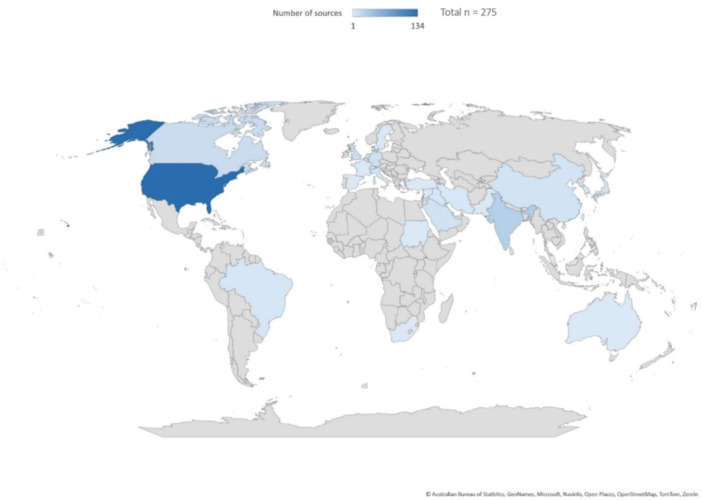
Number of included sources by country (n = 275; two sources did not report the location).
Figure 3.
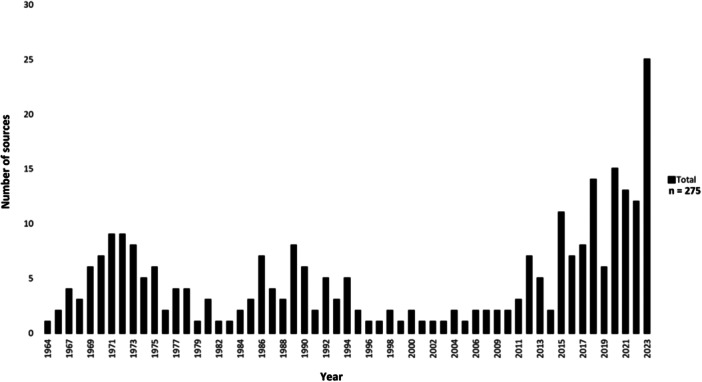
Number of included sources by year (all study types, n = 275).
Regarding study design, 185 were clinical trials, 30 were in vitro studies, 15 systematic reviews, 13 were animal models, 12 were observational studies, 9 were descriptive studies, and 11 described nonoral hygiene applications of OIs (Supporting Information S1: Appendix 3).
Research primarily involved adults, with limited studies on children (6) and adolescents (26). The studies with adolescents often focused on those with fixed orthodontic appliances (15 trials). Children performed self‐irrigation under clinical supervision in only one trial (Murthy et al. 2018).
Industry funding or affiliation was declared in 69 studies (Supporting Information S1: Appendix 4).
3.1.1. Clinical Experimental Studies
The majority of clinical experimental studies were conducted in North America (97), Asia (35), Western Europe (33), and the Middle East (15), with two studies not specifying their location. None were from Eastern Europe or Oceania (Supporting Information S1: Appendix 5).
Sample sizes ranged from two to 240 participants, with a mean of 44.1 (SD 36.2). Study durations ranged from a single irrigation episode to 56 weeks. Most trials focused on periodontitis (57), gingivitis (44), or gingivitis and early stages of periodontitis (15). Participants with healthy periodontal status were in 13 studies, a combination of periodontal health and conditions in 8, peri‐implant mucositis in 5, a mix of peri‐implant health and mucositis in 1, and peri‐implantitis in 1; information on periodontal status was not reported in 39 studies (Figure 4).
Figure 4.
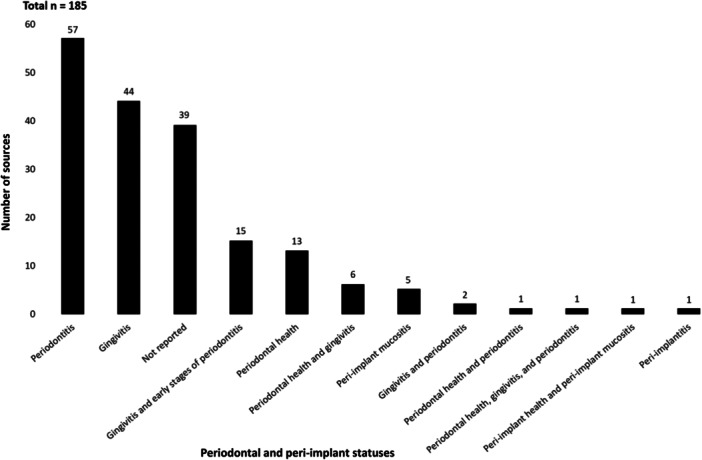
Periodontal and peri‐implant statuses of the populations in the included clinical experimental studies (n = 185).
As shown in Figure 5, most trials (170/185) evaluated oral irrigation effects with various solutions on oral hygiene and oral health in the general population (128), those with fixed orthodontic appliances (21), dental implant recipients (9), special needs groups (6), intermaxillary fixation patients (3), individuals with diabetes (2), and pregnant participants (1 study).
Figure 5.
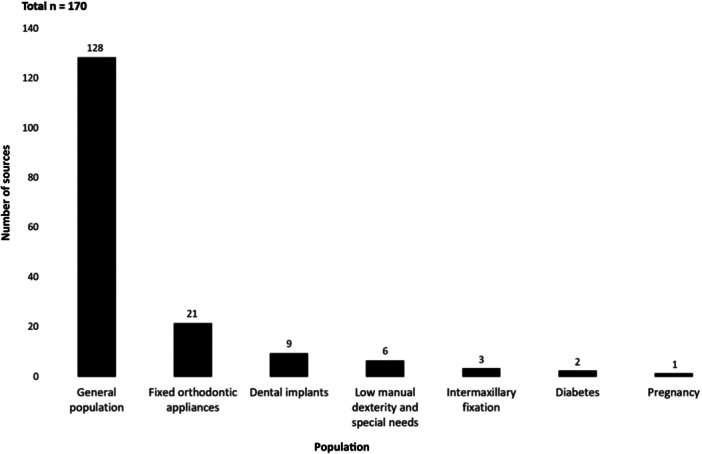
Populations in clinical experimental studies that assessed the effects of oral irrigation on oral hygiene and health (number of studies by population type, n = 170).
The most common irrigant was water (101). Other solutions tested included antimicrobials other than ozonated water (31), ozonated water (13), herbal extracts (10), and antibiotics compared to antiseptics, water, or saline (9). Specific solutions like acetylsalicylic acid and magnetized water were explored in a few studies (Supporting Information S1: Appendix 6).
Most studies evaluating oral irrigation effectiveness focused only on clinical outcome measures. Indexes used were mainly bleeding, plaque, gingival, periodontal, and calculus. The most commonly used plaque index (37) was the one introduced by Silness and Löe (1964), whereas the index by Löe and Silness (1963) was the most commonly used gingival index (40). Probing depth, clinical attachment loss, and bleeding on probing were also evaluated frequently. Chlorhexidine irrigation staining was assessed in nine trials. In most trials that evaluated the effects of water oral irrigation on clinical outcome measures, OIs were used adjunctively to toothbrushing (69 trials). Only 13 trials had at least one study group that used OIs as a sole oral home care aid. Out of these, irrigation was performed only once in six trials to measure its plaque removal ability.
3.1.2. Systematic Reviews
Fifteen systematic reviews met the inclusion criteria. Of these, only three focused primarily on adjunctive oral irrigation compared to other oral home care aids (Allen 2019; AlMoharib 2023; Husseini, Slot, and Van der Weijden 2008), while the rest reviewed the comparative effectiveness of various oral hygiene aids, including OIs.
Most reviews included studies with healthy adults with gingivitis or periodontitis (Supporting Information S1: Appendix 7). Three assessed home care for dental implants (Bidra et al. 2016; Gennai et al. 2023; Zhao et al. 2022), and two focused on fixed orthodontic appliances (AlMoharib et al. 2023; Pithon et al. 2017).
3.2. Descriptive Analysis of the Reported Results
Table 2 summarizes the results of all studies included in the review.
Table 2.
Summary of the effects of oral irrigation.
| Outcome | Summary of the reported results | Number of sources (n = 275)a |
|---|---|---|
| Properties of water sprays | Two zones observed: Impact and flushing zones may aid debris removal | 2 |
| Types and brands of devices | Pulsating devices more effective than nonpulsating; faucet‐attached devices could exert higher pressure than self‐contained devices. Waterpik most studied brand (156 sources). Specialized devices for ozonated and magnetized water irrigation | 275 |
| Pressure and safety | Excessive pressure risks soft tissue damage and periodontal destruction. Up to 70–90 psi is deemed safe for nonulcerated attached gingiva; for nonkeratinized or ulcerated oral soft tissues, 50–70 psi recommended. Particulate penetration into soft tissue possible | 19 |
| Oral irrigation and bacteremia | Bacteremia risk; caution when recommending to individuals at risk of infective endocarditis | 10 |
| Effects on dental materials | Generally safe, with some risks to specific composite resins and inlay restorations. Noted increase in surface roughness for microhybrid composites at 100 psi | 6 |
| Depth of irrigant penetration | Supragingival tips help reach 44%–71% of pocket depth; subgingival tip potentially reaching the base of pockets | 6 |
| Clinical parameters of periodontal and peri‐implant inflammation | Consistent reductions in bleeding, edema, erythema, probing depths, and clinical attachment loss with various irrigants | 138 |
| Changes in soft tissue histology and cytology | Reduced inflammation histologically. No adverse implant effects; may enhance osseointegration | 12 |
| Dental biofilm | In vitro evidence of biofilm disruption. Clinical and review evidence on plaque reduction mixed. Improved biofilm removal in special needs groups | 164 |
| Calculus | Mixed results on calculus prevention | 12 |
| Staining | Chlorhexidine increases staining risk. Lower concentrations and subgingival delivery mitigate staining | 12 |
| Oral microbiome | Potential shifts away from dysbiosis; further research needed | 58 |
| Markers of inflammation | Reductions in select studies; more research warranted | 12 |
| GCF volume | Reduction or no significant change | 6 |
| Oral irrigators in endodontics | Encouraging in vitro evidence; merits in vivo research | 4 |
| Patients' acceptance | Generally high, though studies often lack validated assessment tools | 21 |
| Practitioners' and patients' knowledge and attitudes | OIs increasingly recommended by dental practitioners. Low usage rates among the general population | 8 |
| Other outcomes | Gingival abrasion: No effect | 1 |
| Halitosis: Mixed results | 2 | |
| Capillary wall strength: May increase | 1 | |
| Leukocyte chemotactic activity in saliva: May reduce | 1 | |
| Calcium and phosphate levels in dental biofilm: No effect | 1 | |
| Acidic mouthwash irrigation: Can temporarily reduce oral tissue pH | 1 | |
| Alkaline mouthwash irrigation: Can increase pH in the oral cavity | 1 | |
| Hydrogen peroxide and sodium hypochlorite irrigation: Reduce drop in plaque pH after a sucrose challenge compared to water irrigation | 1 | |
| Water irrigation: No effect on saliva pH | 1 |
Abbreviation: GCF, gingival crevicular fluid.
Full list of sources is in Supporting Information S1: Appendix 8.
3.2.1. The Qualities of a Water Spray Produced by OIs
Early studies identified two primary zones in the water spray from OIs: A direct impact zone and a flushing zone, highlighting their potential for efficient debris removal (Lugassy and Lautenschlager 1970; Lugassy, Lautenschlager, and Katrana 1971).
3.2.2. Types and Brands of OIs
Waterpik was the most researched brand, used in 139 studies and compared to other brands in 17 studies. Other pulsating and nonpulsating, self‐contained, and faucet‐attached devices were also studied. Faucet‐attached irrigators generated higher forces and were difficult to attach, causing some participants to cease irrigation (Lainson, Bergquist, and Fraleigh 1972; Lugassy, Lautenschlager, and Katrana 1971). All irrigator types could force particulate matter into tissues (O'Leary et al. 1970). Pulsating devices were more effective in reducing inflammation because of the decompression phase (Bhaskar et al. 1971). Faucet‐attached and self‐contained units had similar clinical efficacy (Lainson, Bergquist, and Fraleigh 1970; Oshrain et al. 1987). Specialized devices produced ozonated water (Kent Ozone Aquolab, PURECARE) and magnetized water (Hydro Floss).
3.2.3. Pressure and Safety
Nineteen sources examined irrigation pressure and safety. In vitro, pressures depended on the tip used and could damage tissues (Cutright, Bhaskar, and Larson 1972; Kesavan, Reddy, and Yazdani‐Ardakani 1986; Reddy, Kesavan, and Costarella 1985; Selting and Bhaskar 1973). Excessive pressure caused soft tissue trauma in animals (Bhaskar, Cutright, and Frisch 1969; Cutright et al. 1973). However, 70–90 psi is deemed to be safe for nonulcerated attached gingiva, and 50–70 psi is safe for ulcerated oral soft tissues (Bhaskar et al. 1971). Pressure above 8 g caused pain in inflamed tissue (Lobene 1971). Irrigation has been reported to have caused hemorrhage but no epithelial changes in healthy tissue or in periodontitis (Cobb, Rodgers, and Killoy 1988; Krajewski, Rubach, and Pope 1967). Irrigators had lower pressures than syringes for subgingival use (Kelly et al. 1985). Pressure under 20 psi reduced biofilm (Oshrain et al. 1987), but higher pressures reduced gingival bleeding (Ren et al. 2023).
3.2.4. Oral Irrigation and Bacteremia
Seven studies examined the effects of irrigation on bacteremia. Listerine subgingival irrigation reduced bacteremia after instrumentation in periodontitis (Fine et al. 1996). However, water and chlorhexidine irrigation did not affect bacteremia incidence (Lofthus et al. 1991; Waki et al. 1990). In contrast, irrigation increased bacteremia in those with healthy periodontium (Berger 1974), gingivitis (Romans and App 1971), and periodontitis (Felix, Rosen, and App 1971). Two case reports and one observational study also linked oral irrigation to bacterial endocarditis (Drapkin 1977; Duval et al. 2017; Kaplan and Anderson 1977).
3.2.5. Effects on Dental Materials
Six in vitro studies examined irrigation effects on dental materials over 30 s to 40 years equivalent (Akama et al. 2022; Kotsakis et al. 2021; McDevitt and Eames 1971). Most materials showed no significant surface changes, including composites (Alharbi and Farah 2020), implants (Kotsakis et al. 2021; Matthes et al. 2023), and orthodontic brackets (Akama et al. 2022). However, long‐term irrigation damaged microhybrid composites at 100 psi (Alharbi and Farah 2020), inlay restoration with unacceptable margins (McDevitt and Eames 1971), and bulk fill composites at 63 psi (Naser‐Alavi et al. 2022).
3.2.6. Depth of Subgingival Penetration by Irrigating Solutions
Six studies measured subgingival solution delivery. Irrigant through a supragingival tip reached 44%–71% of pocket depth, with no difference with tip placement at 90° or 45° (Eakle, Ford, and Boyd 1986). Rams and Keyes (1984) first described modifying tips for subgingival use. Subgingival tips delivered to 64%–100% of pocket depth (Braun and Ciancio 1992; Dunkin, Sumner, and Hughes 1989a), and were better than supragingival tips (Larner and Greenstein 1993). An irrigating toothbrush delivered solutions into the pockets more effectively than rinsing (Brackett et al. 2006).
3.2.7. Oral Irrigation and Clinical Parameters of Periodontal and Peri‐Implant Inflammation
A broad range of studies demonstrated oral irrigation's effectiveness in reducing periodontal and peri‐implant inflammation, with significant improvements noted in bleeding, gingival indices, clinical attachment loss, and probing depth. Reduced inflammation was consistently shown in healthy adults, those with diabetes or implants, and children with Papillon–Lefèvre syndrome (3 descriptive and 3 observational studies). Less inflammation occurred with irrigation versus brushing alone or with floss, air flosser, or interdental brushes (119 clinical trials and 13 systematic reviews assessed these outcomes). This was irrespective of the solution, methods, or population. Systematic reviews have reported a reduction in gingival bleeding scores by adjunctive oral water irrigation in patients with gingivitis (Allen 2019; AlMoharib et al. 2023; Edlund et al. 2023; Kotsakis et al. 2018b; Volman, Stellrecht, and Scannapieco 2021); a reduction in gingival index, bleeding scores, and probing depth in periodontitis (Slot, Valkenburg, and Van der Weijden 2020); and a reduction in gingival inflammation in gingivitis and periodontitis (Husseini, Slot, and Van der Weijden 2008; Sälzer et al. 2015; Worthington et al. 2019).
3.2.8. Histological and Cytological Changes
Seven histological and five cytological studies assessed irrigation effects. Irrigation reduced marginal periodontal inflammation but not inflammation in the pocket base (Beget 1967; Cantor and Stahl 1969; Crumley and Sumner 1965; Dunkin 1965; Lainson et al. 1971). It increased keratin layer thickness (Krajewski, Giblink, and Gargiulo 1964), but caused no changes in keratinization patterns (Cantor and Stahl, 1969), epithelial maturation (Covin et al. 1973), or white blood cell counts (Herzog and Hodges 1988). Irrigation enhanced bone formation around dental implants in dogs and preserved implant biocompatibility and osteoblastic growth in vitro (Kotsakis et al. 2021; Matthes et al. 2022; Park et al. 2015).
3.2.9. Oral Irrigation and Biofilm Removal
Numerous studies assessed plaque indices. In vitro studies consistently show efficacy in OIs dislodging biofilm from dental surfaces and restorations, though these outcomes may not replicate clinical experiences. Observational and descriptive research indicates that oral irrigation contributes to lower plaque levels, suggesting a beneficial role in oral hygiene practices (Costa, Costa, and Cota 2020; Hentenaar et al. 2020; Rüdiger, Petersilka, and Flemmig 1999). Clinical trials had conflicting results on natural dentition. Some found no biofilm reduction (23 studies), with a similar number of studies showing improvements over traditional brushing, with or without the addition of floss, air flosser, or interdental brushes (31 studies). Adjunctive irrigation consistently improved biofilm removal in special needs populations (Al‐Mubarak et al. 2002; Deepika et al. 2022; Isshiki 1970). Studies also highlighted effective implant decontamination using oral irrigation with cold atmospheric plasma and Superfloss in vitro and in animal models (Matthes et al. 2023; Park et al. 2015).
Systematic review assessment of the plaque removal ability was not performed because of the high heterogeneity of the included trials (Amarasena, Gnanamanickam, and Miller 2019; Pithon et al. 2017), or found no positive plaque reduction effects (Edlund et al. 2023; Gennai et al. 2023; Husseini, Slot, and Van der Weijden 2008; Kotsakis et al. 2018b; Sälzer et al. 2015; Slot, Valkenburg, and Van der Weijden 2020; Volman, Stellrecht, and Scannapieco 2021; Worthington et al. 2019). Only two reviews showed improvements in plaque scores (Allen 2019; AlMoharib et al. 2023).
3.2.10. Irrigation With Antimicrobial Solutions
Most studies showed significant biofilm reduction with chlorhexidine and ozonated water irrigation. Improvements occurred in individuals with mental disabilities (Tatuskar et al. 2023), pregnant participants (Tecco et al. 2022), orthodontic patients (Dhingra and Vandana 2011; Sandra et al. 2019, 2021), individuals with dental implants (Felo et al. 1997), and intermaxillary fixation patients (Aijima and Yamashita 2023; Soltanianzadeh 2020).
Irrigation with chlorhexidine was more effective in decreasing gingival bleeding in gingivitis and reducing the probing depth and clinical attachment loss in periodontitis compared to rinsing with chlorhexidine mouthwash while also resulting in lower staining scores (Brownstein et al. 1990; Jain et al. 2020). Further, one systematic review reports that irrigation with chlorhexidine is more effective for reducing peri‐implant inflammation in peri‐implant mucositis than rinsing with chlorhexidine mouthwash or applying it as a gel (Zhao et al. 2022). Another potentially clinically relevant solution that effectively reduced biofilm on apatite, metal, and resin material surfaces in vitro is neutral electrolyzed water containing 30 and 100 ppm chlorine (Akama et al. 2022).
3.2.11. Oral Irrigation and Calculus Formation
Twelve studies assessed the effects on calculus. Five found no effect (Gupta, O'Toole, and Hammermeister 1973; Hoover, Robinson, and Billingsley 1968; Lainson, Bergquist, and Fraleigh 1970, 1972; Meklas and Stewart 1972). Three showed decreased calculus with water irrigation (Hoover and Robinson 1971; Kim, Yoo, et al. 2023; Lobene 1969). Benefits occurred with magnetized water (Johnson et al. 1998; Watt, Rosenfelder, and Sutton 1993), and chlorhexidine (Felo et al. 1997). However, one study found increased calculus with chlorhexidine (Flemmig et al. 1990).
3.2.12. Staining
Water and stannous fluoride irrigation did not affect staining (Boyd et al. 1985; Walsh et al. 1989). Chlorhexidine irrigation increased staining in several studies (Agerbaek, Melsen, and Rölla 1975; Flemmig et al. 1990; Lang and Räber 1981; Walsh, Glenwright, and Hull 1992). Watts and Newman (1986) found no staining and lower concentrations of chlorhexidine caused less staining while retaining efficacy (Cumming and Löe 1973; Lang and Ramseier‐Grossmann 1981). Subgingival chlorhexidine irrigation resulted in less staining than rinsing with chlorhexidine mouthwash (Felo et al. 1997; Jain et al. 2020). This may help utilize benefits while mitigating side effects.
3.2.13. Oral Irrigation and Oral Microbiome
Microbiological outcomes were examined in 58 studies using culture, microscopy, polymerase chain reaction, and sequencing. Few assessed periodontitis patients using molecular biology techniques (Deepa et al. 2023; Genovesi et al. 2013; Kshitish and Laxman 2010; Perayil et al. 2016). Overall, oral irrigation reduced pathogens, acidogenic bacteria, anaerobes, spirochetes, and motile rods. Increased periodontal health‐associated species, primary colonizers, and aerobes were reported (Supporting Information S1: Appendix 9).
3.2.14. Oral Irrigation and Markers of Inflammation
Twelve studies on oral irrigation's influence on markers of inflammation showed positive results. Water irrigation did not increase inflammation in vitro (Matthes et al. 2023), or reduce gingival crevicular fluid (GCF) and salivary markers in gingivitis and periodontitis in two trials (Kaur et al. 2023; Ramseier et al. 2021). However, adjunctive water irrigation decreased GCF cytokines versus routine home care (Cutler et al. 2000); adjunctive interdental brushing (Moore et al. 2023); was more effective in participants with peri‐implant mucositis (Tütüncüoğlu et al. 2022); and reduced blood markers in periodontitis and diabetes patients (Al‐Mubarak et al. 2002; Cutler et al. 2000). Ozonated water significantly lowered GCF cytokines (Dhingra and Vandana 2011; Jose et al. 2017; Sandra et al. 2019). Irrigation with water and pomegranate peel extract was comparable in reducing inflammation (Eltay et al. 2021).
3.2.15. GCF Volume
Six studies measured GCF volume changes with irrigation. Most found no effects on GCF flow in gingivitis and periodontitis with various solutions (Ciancio et al. 1989; Ernst et al. 2004; Hugoson 1978; Ravishankar, Venugopal, and Nadkerny 2015). However, pulsated saline irrigation reduced GCF flow more than syringe irrigation in periodontitis (Itic and Serfaty 1992). Ozonated water decreased GCF in orthodontic patients (Dhingra and Vandana 2011).
3.2.16. Oral Irrigation in Special Needs Populations
Oral irrigation showed enhanced biofilm control and reduced gingival inflammation in populations with low manual dexterity and special needs, indicating its utility as an adjunctive or alternative oral hygiene measure in these groups. Notably, modified and cordless irrigators significantly improved oral health outcomes for these populations (Murthy et al. 2018; Yuen 2013; Yuen and Pope 2009). Ozonated water irrigation reduced biofilm, inflammation, and periodontitis‐associated microorganisms in individuals with mental disabilities (Tatuskar et al. 2023).
3.2.17. OIs in Endodontics
The application of OIs for root canal irrigation was studied by two research groups in a total of four in vitro trials (Hemalatha et al. 2022; Shalan and Al‐huwaizi 2017; Shalan, Al‐huwaizi, and Fatalla 2018; Shalan et al. 2018). These studies highlighted OIs' safety and effectiveness in delivering solutions and removing smear layers in root canal systems, suggesting potential applications beyond traditional oral hygiene uses (Hemalatha et al. 2022; Shalan and Al‐huwaizi 2017; Shalan et al. 2018). Although needle choice and placement impacted the apical extrusion of debris and irrigants, overall, the application of OIs resulted in a lower amount of peri‐apically extruded debris and irrigants compared to syringe irrigation and achieved a better smear layer removal efficacy in the apical third of the root canal compared to a sonically driven irrigation system (Shalan and Al‐huwaizi 2017; Shalan, Al‐huwaizi, and Fatalla 2018). The findings from this limited number of in vitro trials call for further in vitro research and clinical validation.
3.2.18. Acceptance, Compliance, and Patient Experiences
There was high satisfaction and compliance with irrigators (Bordabeheres 2012; Flint 2014; Lyle et al. 2020; Peterson and Shiller 1968; Ren et al. 2023; Salles et al. 2021; Sarlati et al. 2016; Sgarbanti et al. 2021). This included populations with fixed orthodontic appliances (Alexander 2006; Schumacher 1978) and tetraplegia (Yuen 2013; Yuen and Pope 2009). However, some patients found irrigation too time‐consuming and messy, and faucet‐attached irrigators were hard to attach (Lainson, Bergquist, and Fraleigh 1972; Peterson and Shiller 1968). Evaluating compliance was difficult if diaries were not returned (Tyler, Kang, and Goh 2023). Clinician‐performed subgingival irrigation (Dunkin, Sumner, and Hughes 1989b), as well as self‐administered supra‐ and subgingival irrigation with various solutions, was well‐tolerated (Flemmig et al. 1990; Walsh, Glenwright, and Hull 1992; Watts and Newman 1986; Wolff et al. 1989).
3.2.19. Practitioners' and Patients' Knowledge and Attitudes
The popularity of oral irrigation devices has been increasing among dental professionals, with recommendations extending to patients with various oral health needs (Hygienetown 2010; Zellmer et al. 2020). In 2020, OIs were the US hygienists' most recommended home care aid for dental implants (Zellmer et al. 2020). Despite this, awareness and usage rates among the general population and nondental practitioners appear low (Stelmakh, Slot, and van der Weijden 2017; Sun et al. 2023; Varela‐Centelles et al. 2020), suggesting an opportunity for broader education and advocacy.
3.2.20. Less Commonly Researched Outcomes
Some studies examined uncommon outcomes. No effect on gingival abrasion was found (Sun et al. 2023). Conflicting results were seen for halitosis improvement (Mishal AlHarbi, Al‐Kadhi, and Al‐Sanea 2020; Xu et al. 2023). Other findings included increased capillary strength (Kozam 1973), reduced salivary leukocyte activity (Wright and Tempel 1974), and variable impacts on oral pH (Aijima and Yamashita 2023; Esposito and Gray 1975; Lobene et al. 1972). No further research followed up on these initial studies.
3.2.21. Applications Other Than Oral Hygiene
In the 1970s, US healthcare providers experimented with pulsating OIs for wound cleaning (Bhaskar et al. 1971; Gross et al. 1971), ophthalmic decontamination (Blumberg 1973), debridement and symptom relief in oral cancer (Bagshaw 1967), kidney stone removal and fecal impaction resolution (Gibbons et al. 1974; Korn 1972), and colonoscopy preparation (Katz et al. 1977). Devices were modified with special attachments in most cases. OIs may help relieve xerostomia symptoms in head and neck cancer patients. This innovative use of OIs was most prominent when the technology first entered the commercial market, with a notable instance of continued interest in the early 2000s (Loud 2001).
3.2.22. Novel and Experimental Oral Irrigators
Some studies focused on experimental devices. Multichannel irrigators with aspiration can be used in bedridden patients and individuals with disabilities, reducing plaque and inflammation (Kim, Yoo, et al. 2023; Kim, Bae et al. 2023). An irrigating toothbrush, which can be used in special needs patients, improved cleaning (Brackett et al. 2006). Experimental oral hygiene need stations were designed to help young children with closed dentition perform interproximal hygiene (Murthy et al. 2018), and improve compliance with interproximal care in people who struggle with interdental cleaning (Fan et al. 2018; Nie 2017).
Other devices focused on subgingival debridement. One creates negative pressure to access deep pockets (Hentenaar et al. 2020; Van Dijk et al. 2018), while others decontaminate implants (Matthes et al. 2022, 2023; Yamada et al. 2017, 2018). An irrigation device delivering antimicrobial gels into periodontal pockets reduced probing depth and bleeding in peri‐implantitis more than regular oral hygiene alone (Levin et al. 2015). While most of these devices are intended for professional in‐office applications, modifying them for at‐home use might be possible.
3.2.23. Research Limitations and Future Directions
In vitro studies were limited by the inability to replicate intraoral conditions, necessitating clinical trials (Abdul Aziz, Afifah, and Syahmi 2018; Ioannidis et al. 2015; Lin, Chuang, and Chang 2018; Matthes et al. 2022, 2023; Tawakoli et al. 2015). Commonly cited clinical limitations included small samples, short durations, lack of blinding, and variability in methods and compliance (Gennai et al. 2023; Volman, Stellrecht, and Scannapieco 2021; Zhao et al. 2022). Future research could include larger trials, longer follow‐ups, comparison of irrigators and air flossers, standardized protocols, clear diagnoses, cost analyses, and patient‐reported outcomes (Amarasena, Gnanamanickam, and Miller 2019; Kotsakis et al. 2018b; Sharma et al. 2012; Worthington et al. 2019).
4. Discussion
This scoping review provides a broad, systematic overview of the evidence on oral irrigation devices and identifies research gaps to help direct future research, development, and evidence‐based clinical practice. Oral irrigation was reported as generally safe and well‐accepted when used appropriately as per the manufacturer's guidelines. However, high pressures above 90 psi may cause soft tissue damage (Bhaskar et al. 1971; Lobene 1971; Winter 1982), and the potential for irrigation to cause transient bacteremia indicates caution for individuals at risk of infective endocarditis (Drapkin 1977; Kaplan and Anderson 1977). Overall, evidence indicates that oral irrigation effectively reduces periodontal inflammation, but there are varying results regarding plaque reduction that aligns with systematic reviews (Edlund et al. 2023; Gennai et al. 2023; Husseini, Slot, and Van der Weijden 2008; Kotsakis et al. 2018a; Sälzer et al. 2015; Slot, Valkenburg, and Van der Weijden 2020; Volman, Stellrecht, and Scannapieco 2021; Worthington et al. 2019).
The mechanism underlying anti‐inflammatory effects likely involves shifting oral microbiota away from dysbiosis toward those more consistent with periodontal and dental health rather than completely removing biofilms. Some in vitro evidence showed that oral irrigation disrupted biofilms without fully eliminating them (Brady, Gray, and Bhaskar 1973; Kato, Tamura, and Nakagaki 2012). Furthermore, regular oral irrigation has been reported to result in changes in dental biofilm composition in clinical trials. Ge et al. (2023) observed a reduction in the relative abundance of late colonizers and anaerobic periodontal pathogens, with an increase in early colonizers in the subgingival biofilm of individuals with gingivitis using OIs. A more aerobic phenotype was also observed in supragingival plaque in gingivitis when OIs were used in addition to toothbrushing compared to toothbrushing alone (Xu et al. 2023). Similarly, using multichannel OIs prevented an increase in Porphyromonas species in the saliva of individuals with healthy periodontium who discontinued other forms of oral hygiene (Kim, Yoo, et al. 2023). These findings indicate a potential microbiome‐modulating, host‐response–altering mechanism of oral irrigation. Further research using modern molecular biology techniques is needed to clarify the effects on oral microbiota, especially in periodontitis patients where few such studies exist (Deepa et al. 2023; Genovesi et al. 2013; Kshitish and Laxman 2010; Perayil et al. 2016).
Patient acceptance and satisfaction with oral irrigation appear high based on reported experiences (Bordabeheres 2012; Flint 2014; Lyle et al. 2020; Peterson and Shiller 1968; Ren et al. 2023; Salles et al. 2021; Sarlati et al. 2016; Sgarbanti et al. 2021). However, standardized, validated patient‐reported outcome measures were seldom utilized. Incorporating tools quantifying satisfaction, quality‐of‐life impacts, ease of use, and other patient perspectives would strengthen future research (Stelmakh, Slot, and van der Weijden 2017; Sun et al. 2023). Qualitative methods may also help capture patient experiences more comprehensively.
The observed anti‐inflammatory benefits occurred consistently across various populations and irrigant solutions. However, plaque reduction findings were mixed, potentially reflecting differences in study designs, cohorts, devices, follow‐up times, and plaque indices. Standardizing these factors in future trials may improve consistency (Worthington et al. 2019). Controlling for confounders like baseline oral hygiene, pretrial professional plaque removal, specific oral irrigator models, and appropriate statistical analyses would also strengthen reliability.
Evidence in pediatric and special needs populations is sparse but warrants investigation, given oral irrigation's potential in those unable to maintain adequate oral hygiene. Promising results were found in children, physically disabled groups (Isshiki 1970; Yuen 2013), and individuals with mental disabilities (Tatuskar et al. 2023), indicating that feasibility assessments in these cohorts would be justified and clinically valuable if positive. A dearth of research on caries prevention potential needs investigating, as has been previously recommended (Amarasena, Gnanamanickam, and Miller 2019; Worthington et al. 2019).
Sufficiently powered trials with adequate follow‐up periods are required to determine the long‐term effects on periodontal, peri‐implant, and caries outcome measures (Worthington et al. 2019). Achieving sufficient power and follow‐up is particularly challenging in research evaluating caries incidence. Indeed, studies on caries prevention commonly enroll hundreds of participants and require years of follow‐up (Marinho et al. 2013), which may be challenging to achieve with an intervention requiring participant compliance, such as using a home care aid. Furthermore, the results of our review suggest that oral irrigation with water may not be able to remove biofilm completely and is unlikely to affect the pH of dental plaque. Therefore, the successful application of oral irrigation for caries prevention may involve the introduction of irrigation solutions that can significantly reduce biofilm formation or increase biofilm pH without considerable side effects. One possible candidate is electrolyzed water. It is an environmentally friendly and nontoxic solution with potential antiplaque, pH‐neutralizing, and anticariogenic effects (Krishnan et al. 2023). Our review identified one in vitro trial on irrigation with electrolyzed water, and it reported significant antimicrobial and antiplaque results (Akama et al. 2022). Further in vitro and in vivo studies on the application of electrolyzed water as an irrigant for preventing dental caries, periodontal, and peri‐implant diseases may be warranted. Comparing the environmental impacts and costs of using OIs with various irrigants to existing oral hygiene aids would also benefit clinical guidelines and recommendations (Herrera et al. 2023).
Oral irrigation has the potential to be incorporated into oral home care for the secondary prevention of peri‐implantitis, that is, the prevention of disease recurrence in individuals successfully treated for peri‐implantitis. Currently, the EFP clinical practice guideline for the prevention and treatment of peri‐implant diseases suggests that water oral irrigation may be considered an adjunct to regular oral hygiene methods in individuals with peri‐implant mucositis but calls for more research (Herrera et al. 2023). It is also unknown which oral home care method is most effective for individuals treated for peri‐implantitis because of the absence of trials comparing different oral hygiene methods in this population. The results of the present scoping review are consistent with these findings. We identified nine clinical trials that included populations with dental implants, but only one was conducted with a peri‐implantitis population (Levin et al. 2015). Future clinical trials need to assess the effects of oral irrigation on peri‐implantitis and peri‐implant mucositis.
The EFP clinical practice guideline for the treatment of Stage I–III periodontitis suggests that the use of adjunctive chemical agents, particularly chlorhexidine, may be considered in the second (cause‐related) step of periodontal therapy and periodontal maintenance (Sanz et al. 2020). The EFP clinical practice guideline for the prevention and treatment of peri‐implant diseases also supports the time‐limited use of chlorhexidine in individuals with peri‐implant mucositis (Herrera et al. 2023). One important advantage of OIs is their ability to deliver solutions subgingivally (Dunkin, Sumner, and Hughes 1989a; Eakle, Ford, and Boyd 1986). Indeed, OIs are the only oral home care tools that can deliver solutions to the base of deep periodontal pockets (Dunkin, Sumner, and Hughes 1989a). This property of OIs may make them the perfect vehicle for delivering chemical agents in periodontal pockets and peri‐implant sulci. The place of irrigation with antimicrobial solutions in managing periodontitis and peri‐implant mucositis and the possible side effects of such interventions, such as antibiotic crossresistance (Laumen et al. 2021), need to be explored further. In addition, the environmental impact of irrigation with antimicrobials, such as its effects on the water ecosystem and plastic pollution, needs to be studied.
This review has several limitations to consider. Only English‐language sources were included, potentially overlooking research in other languages. No analysis was performed on differences between brands and models. However, as variations in device properties can impact effectiveness, the findings may not be generalizable across all irrigator models. Scoping reviews aim to map the breadth of literature by design, irrespective of the risk of bias or the quality of studies (Tricco et al. 2018). Therefore, the findings must be interpreted cautiously, as no quality assessment was conducted. Further, it is difficult to isolate the effect of oral irrigation because, in the majority of clinical trials, it was used adjunctively to toothbrushing and was compared to an adjunctive use of other interdental cleaning aids, with only a few studies using oral irrigators as the sole oral home care aid. The major strength of this review is that it provides a comprehensive overview of both primary and secondary studies across various regions and settings, providing extensive coverage of the literature over decades.
5. Conclusions
Oral irrigation effectively reduces periodontal inflammation, potentially by modulating the oral microbiota. However, knowledge gaps exist regarding its mechanism, effectiveness in plaque removal, impacts on dental caries, patient‐reported outcomes, applicability in pediatric and special needs populations, and environmental and economic considerations. Future trials could address these areas to clarify oral irrigation's role in promoting oral health across diverse populations and conditions.
Author Contributions
Farzana Sarkisova and Zac Morse were involved in conceptualizing the study; sources identification and screening; data analysis and synthesis; and drafting, revision, and the final approval of the manuscript. Kevin Lee and Nagihan Bostanci contributed to the interpretation of data; revision; and the final approval of the manuscript.
Ethics Statement
The authors have nothing to report.
Conflicts of Interest
The authors declare no conflicts of interest.
Supporting information
Supporting information.
Acknowledgments
The authors would like to express their gratitude to Andrew South for their assistance with developing the search strategy. The authors received no specific funding for this work. Open access publishing facilitated by Auckland University of Technology, as part of the Wiley ‐ Auckland University of Technology agreement via the Council of Australian University Librarians.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- Abdul Aziz, A. H. , Afifah N. A., and Syahmi N. M.. 2018. “New Water Irrigator for Cleaning Dental Plaque.” International Journal for Innovation Education and Research 6, no. 10: 299–305. 10.31686/ijier.Vol6.Iss10.1190. [DOI] [Google Scholar]
- Agerbaek, N. , Melsen B., and Rölla G.. 1975. “Application of Chlorhexidine by Oral Irrigation Systems.” European Journal of Oral Sciences 83, no. 5: 284–287. 10.1111/j.1600-0722.1975.tb00439.x. [DOI] [PubMed] [Google Scholar]
- Aijima, R. , and Yamashita Y.. 2023. “Effectiveness of Perioperative Oral Hygiene Management Using a Cetylpyridinium Chloride‐, Dipotassium Glycyrrhizinate, and Tranexamic Acid‐Based Mouthwash as an Adjunct to Mechanical Oral Hygiene in Patients With Maxillomandibular Fixation: A Randomized Controlled Clinical Trial.” Clinical and Experimental Dental Research 9, no. 6: 1044–1050. 10.1002/cre2.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akama, Y. , Nagamatsu Y., and Ikeda H.. 2022. “Applicability of Neutral Electrolyzed Water for Cleaning Contaminated Fixed Orthodontic Appliances.” American Journal of Orthodontics and Dentofacial Orthopedics 161, no. 6: e507–e523. 10.1016/j.ajodo.2022.02.007. [DOI] [PubMed] [Google Scholar]
- Al‐Mubarak, S. , Ciancio S., and Aljada A.. 2002. “Comparative Evaluation of Adjunctive Oral Irrigation on Diabetics.” Journal of Clinical Periodontology 29, no. 4: 295–300. 10.1034/j.1600-051x.2002.290404.x. [DOI] [PubMed] [Google Scholar]
- Alexander, K. M. 2006. “A Clinical Evaluation of the Effects of Oral Irrigation on the Gingival Health of Adult Orthodontic Patients.” Master of Science, The State University of New York at Buffalo. ProQuest Dissertations & Theses Global. https://www.proquest.com/docview/304940501?pq-origsite=gscholar&fromopenview=true&sourcetype=Dissertations%20&%20Theses.
- Alharbi, M. , and Farah R.. 2020. “Effect of Water‐jet Flossing on Surface Roughness and Color Stability of Dental Resin‐Based Composites.” Journal of Clinical and Experimental Dentistry 12, no. 2: e169–e177. 10.4317/jced.56153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen, J. 2019. “Efficacy of Oral Irrigators on Gingival Health: A Review of Three Papers.” Dental Health 58, no. 1: 34–40. [Google Scholar]
- AlMoharib, H. S. 2023. “The Effectiveness of Water Jet Flossing and Interdental Flossing for Oral Hygiene in Orthodontic Patients With Fixed Appliances: A Randomised Clinical Trial.” Thai Clinical Trials Registry. https://www.thaiclinicaltrials.org/show/TCTR20230926005. [DOI] [PMC free article] [PubMed]
- AlMoharib, H. S. , AlAskar M. H., AlShabib A. N., Almadhoon H. W., and AlMohareb T. S.. 2023. “The Effectiveness of Dental Water Jet in Reducing Dental Plaque and Gingival Bleeding in Orthodontic Patients: A Systematic Review and Meta‐analysis of Randomized Clinical Trials.” International Journal of Dental Hygiene 22, no. 1: 56–64. 10.1111/idh.12741. [DOI] [PubMed] [Google Scholar]
- Amarasena, N. , Gnanamanickam E., and Miller J.. 2019. “Effects of Interdental Cleaning Devices in Preventing Dental Caries and Periodontal Diseases: A Scoping Review.” Australian Dental Journal 64, no. 4: 327–337. 10.1111/adj.12722. [DOI] [PubMed] [Google Scholar]
- Aromataris, E. , and Munn Z.. 2020. “JBI Manual for Evidence Synthesis.” JBI. 10.46658/JBIMES-20-01. [DOI]
- Bagshaw, M. A. 1967. “A Water‐Jet Device for Supportive Care in Oral Cancer.” American Journal of Roentgenology 99, no. 4: 842. 10.2214/ajr.99.4.842. [DOI] [PubMed] [Google Scholar]
- Beget, B. C. 1967. Oral Irrigation and Inflammation [Abstract]. Washington, DC: International Association for Dental Research. [Google Scholar]
- Belibasakis, G. N. , Belstrøm D., Eick S., Gursoy U. K., Johansson A., and Könönen E.. 2023. “Periodontal Microbiology and Microbial Etiology of Periodontal Diseases: Historical Concepts and Contemporary Perspectives.” Periodontology 2000. Published ahead of print, January 20, 2023. 10.1111/prd.12473. [DOI] [PubMed] [Google Scholar]
- Berger, S. A. 1974. “Bacteremia After the Use of an Oral Irrigation Device: A Controlled Study in Subjects with Normal‐Appearing Gingiva: Comparison with Use of Toothbrush.” Annals of Internal Medicine 80, no. 4: 510–511. 10.7326/0003-4819-80-4-510. [DOI] [PubMed] [Google Scholar]
- Bernabe, E. , Marcenes W., Hernandez C. R., et al. 2020. “Global, Regional, and National Levels and Trends in Burden of Oral Conditions From 1990 to 2017: A Systematic Analysis for the Global Burden of Disease 2017 Study.” Journal of Dental Research 99, no. 4: 362–373. 10.1177/0022034520908533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertl, K. , Geissberger C., Zinndorf D., et al. 2022. “Bacterial Colonisation During Regular Daily Use of a Power‐Driven Water Flosser and Risk for Cross‐contamination. Can it Be Prevented?” Clinical Oral Investigations 26: 1903–1913. 10.1177/0022034520908533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhaskar, S. N. , Cutright D. E., and Frisch J.. 1969. “Effect of High Pressure Water Jet on Oral Mucosa of Varied Density.” Journal of Periodontology‐Periodontics 40, no. 10: 593–598. 10.1902/jop.1969.40.10.593. [DOI] [PubMed] [Google Scholar]
- Bhaskar, S. N. , Cutright D. E., Gross A., Frisch J., Beasley J. D., 3rd, and Perez B.. 1971. “Water Jet Devices in Dental Practice.” Journal of Periodontology 42, no. 10: 658–664. 10.1902/jop.1971.42.10.658. [DOI] [PubMed] [Google Scholar]
- Bidra, A. S. , Daubert D. M., Garcia L. T., et al. 2016. “A Systematic Review of Recall Regimen and Maintenance Regimen of Patients With Dental Restorations. Part 2: Implant‐Borne Restorations.” Supplement, Journal of Prosthodontics 25, no. S1: S16–S31. 10.1111/jopr.12415. [DOI] [PubMed] [Google Scholar]
- Blumberg, E. J. 1973. “Use of Water‐Piks in Acute Chemical Burns of the Eye.” Texas Medicine 69, no. 8: 92. [PubMed] [Google Scholar]
- Bordabeheres, C. 2012. “Water Flosser and Type 2 Diabetes: Case Report of Bleeding and Inflammation Reduction.” RDH 32, no. 4: 64–82. [Google Scholar]
- Boyd, R. L. , Leggott P., Quinn R., Buchanan S., Eakle W., and Chambers D.. 1985. “Effect of Self‐administered Daily Irrigation With 0.02% SnF2 on Periodontal Disease Activity.” Journal of Clinical Periodontology 12, no. 6: 420–431. 10.1111/j.1600-051X.1985.tb01378.x. [DOI] [PubMed] [Google Scholar]
- Brackett, M. G. , Drisko C. L., Thompson A. L., Waller J. L., Marshall D. L., and Schuster G. S.. 2006. “Penetration of Fluids Into Periodontal Pockets Using a Powered Toothbrush/Irrigator Device.” Journal of Contemporary Dental Practice 7, no. 3: 30–39. [PubMed] [Google Scholar]
- Brady, J. M. , Gray W. A., and Bhaskar S. N.. 1973. “Electron Microscopic Study of the Effect of Water Jet Lavage Devices on Dental Plaque.” Journal of Dental Research 52, no. 6: 1310–1313. 10.1177/00220345730520062601. [DOI] [PubMed] [Google Scholar]
- Braun, R. E. , and Ciancio S. G.. 1992. “Subgingival Delivery by an Oral Irrigation Device.” Journal of Periodontology 63, no. 5: 469–472. 10.1902/jop.1992.63.5.469. [DOI] [PubMed] [Google Scholar]
- Brownstein, C. N. , Briggs S. D., Schweitzer K. L., Briner W. W., and Kornman K. S.. 1990. “Irrigation With Chlorhexidine to Resolve Naturally Occurring Gingivitis.” Journal of Clinical Periodontology 17, no. 8: 588–593. 10.1111/j.1600-051x.1990.tb01110.x. [DOI] [PubMed] [Google Scholar]
- Buda, L. V. 2016. “Ensuring Maintenance of Oral Hygiene in Persons With Special Needs.” Dental Clinics of North America 60, no. 3: 593–604. 10.1016/j.cden.2016.02.006. [DOI] [PubMed] [Google Scholar]
- Cantor, M. T. , and Stahl S. S.. 1969. “Interdental Col Tissue Responses to the Use of a Water Pressure Cleansing Device.” Journal of Periodontology‐Periodontics 40, no. 5: 292–295. 10.1902/jop.1969.40.5.292. [DOI] [PubMed] [Google Scholar]
- Ciancio, S. G. 2009. “The Dental Water Jet: A Product Ahead of Its Time.” Compendium of Continuing Education in Dentistry 30, spec no. 1: 7–13. [PubMed] [Google Scholar]
- Ciancio, S. G. , Mather M. L., Zambon J. J., and Reynolds H. S.. 1989. “Effect of a Chemotherapeutic Agent Delivered by an Oral Irrigation Device on Plaque, Gingivitis, and Subgingival Microflora.” Journal of Periodontology 60, no. 6: 310–315. 10.1902/jop.1989.60.6.310. [DOI] [PubMed] [Google Scholar]
- Cobb, C. M. , Rodgers R. L., and Killoy W. J.. 1988. “Ultrastructural Examination of Human Periodontal Pockets Following the Use of an Oral Irrigation Device In Vivo.” Journal of Periodontology 59, no. 3: 155–163. 10.1902/jop.1988.59.3.155. [DOI] [PubMed] [Google Scholar]
- Costa, F. O. , Costa A. A., and Cota L. O. M.. 2020. “The Use of Interdental Brushes or Oral Irrigators as Adjuvants to Conventional Oral Hygiene Associated With Recurrence of Periodontitis in Periodontal Maintenance Therapy: A 6‐year Prospective Study.” Journal of Periodontology 91, no. 1: 26–36. 10.1002/JPER.18-0637. [DOI] [PubMed] [Google Scholar]
- Covin, N. R. , Lainson P. A., Belding J. H., and Fraleigh C. M.. 1973. “The Effects of Stimulating the Gingiva by a Pulsating Water Device.” Journal of Periodontology 44, no. 5: 286–293. 10.1902/jop.1973.44.5.286. [DOI] [PubMed] [Google Scholar]
- Crumley, P. J. , and Sumner C. F.. 1965. “Effectiveness of a Water Pressure Cleansing Device.” Periodontics 3, no. 4: 193–195. [PubMed] [Google Scholar]
- Cumming, B. R. , and Löe H.. 1973. “Optimal Dosage and Method of Delivering Chlorhexidine Solutions for the Inhibition of Dental Plaque.” Journal of Periodontal Research 8, no. 2: 57–62. 10.1111/j.1600-0765.1973.tb00751.x. [DOI] [PubMed] [Google Scholar]
- Cutler, C. W. , Stanford T. W., Abraham C., Cederberg R. A., Boardman T. J., and Ross C.. 2000. “Clinical Benefits of Oral Irrigation for Periodontitis Are Related to Reduction of Pro‐inflammatory Cytokine Levels and Plaque.” Journal of Clinical Periodontology 27, no. 2: 134–143. 10.1034/j.1600-051x.2000.027002134.x. [DOI] [PubMed] [Google Scholar]
- Cutright, D. E. , Beasley J. D., 3rd, Bhaskar S. N., and Larson W. J.. 1973. “Water Lavage and Tissue Calibration Study in Rats.” Journal of Dental Research 52, no. 1: 26–29. 10.1177/00220345730520012901. [DOI] [PubMed] [Google Scholar]
- Cutright, D. E. , Bhaskar S. N., and Larson W. J.. 1972. “Variable Tissue Forces Produced by Water Jet Devices.” Journal of Periodontology 43, no. 12: 765–771. 10.1902/jop.1972.43.12.765. [DOI] [PubMed] [Google Scholar]
- Deepa, A. , Katuri K. K., Swetha C., Shivani C. R. N., Boyapati R., and Ravindranath D.. 2023. “Clinical and Microbiological Efficacy of 0.25% Sodium Hypochlorite as a Subgingival Irrigant in Chronic Periodontitis Patients: A Pilot Study.” World Journal of Dentistry 14, no. 9: 745–750. 10.5005/jp-journals-10015-2306. [DOI] [Google Scholar]
- Deepika, V. , Chandrasekhar R., Uloopi K. S., Ratnaditya A., Vinay C., and RojaRamya K. S.. 2022. “A Randomized Controlled Trial for Evaluation of the Effectiveness of Oral Irrigator and Interdental Floss for Plaque Control in Children With Visual Impairment.” International Journal of Clinical Pediatric Dentistry 15, no. 4: 389–393. 10.5005/jp-journals-10005-2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhingra, K. , and Vandana K.. 2011. “Management of Gingival Inflammation in Orthodontic Patients With Ozonated Water Irrigation—A Pilot Study.” International Journal of Dental Hygiene 9, no. 4: 296–302. 10.1111/j.1601-5037.2011.00506.x. [DOI] [PubMed] [Google Scholar]
- Drapkin, M. S. 1977. “Endocarditis After the Use of an Oral Irrigation Device.” Annals of Internal Medicine 87, no. 4: 455. 10.7326/0003-4819-87-4-455_1. [DOI] [PubMed] [Google Scholar]
- Dunkin, R. T. 1965. “A New Approach to Oral Physiotherapy With a New Index of Evaluation.” The Journal of Periodontology 36, no. 4: 315–321. 10.1902/jop.1965.36.4.315. [DOI] [PubMed] [Google Scholar]
- Dunkin, R. T. , Sumner C. S., 3rd, and Hughes W. R.. 1989a. “An Effectiveness Study of a Subgingival Delivery System.” Quintessence International 20, no. 5: 345–346. [PubMed] [Google Scholar]
- Dunkin, R. T. , Sumner C. S., 3rd, and Hughes W. R.. 1989b. “Safety Study of a Subgingival Delivery System.” Quintessence International 20, no. 6: 401–402. [PubMed] [Google Scholar]
- Duval, X. , Millot S., Chirouze C., et al. 2017. “Oral Streptococcal Endocarditis, Oral Hygiene Habits, and Recent Dental Procedures: A Case–Control Study.” Clinical Infectious Diseases 64, no. 12: 1678–1685. 10.1093/cid/cix237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eakle, W. S. , Ford C., and Boyd R. L.. 1986. “Depth of Penetration in Periodontal Pockets With Oral Irrigation.” Journal of Clinical Periodontology 13, no. 1: 39–44. 10.1111/j.1600-051x.1986.tb01412.x. [DOI] [PubMed] [Google Scholar]
- Edlund, P. , Bertl K., Pandis N., and Stavropoulos A.. 2023. “Efficacy of Power‐Driven Interdental Cleaning Tools: A Systematic Review and Meta‐Analysis.” Clinical and Experimental Dental Research 9, no. 1: 3–16. 10.1002/cre2.691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eltay, E. G. , Gismalla B. G., Mukhtar M. M., and Awadelkarim M. O. A.. 2021. “ Punica granatum Peel Extract as Adjunct Irrigation to Nonsurgical Treatment of Chronic Gingivitis.” Complementary Therapies in Clinical Practice 43: 101383. 10.1016/j.ctcp.2021.101383. [DOI] [PubMed] [Google Scholar]
- Ernst, C. P. , Pittrof M., Fürstenfelder S., and Willershausen B.. 2004. “Does Professional Preventive Care Benefit From Additional Subgingival Irrigation?” Clinical Oral Investigations 8, no. 4: 211–218. 10.1007/s00784-004-0266-3. [DOI] [PubMed] [Google Scholar]
- Esposito, E. J. , and Gray W. A.. 1975. “Effect of Water and Mouthwashes on pH of Oral Monkey Mucosa.” Pharmacology and Therapeutics in Dentistry 2, no. 1: 33–41. [PubMed] [Google Scholar]
- Fan, B. , Ouyang Z., Niu J., Yu S., and Rodrigues J.. 2018. “Smart Water Flosser: A Novel Smart Oral Cleaner With IMU Sensor.” 2018 IEEE Global Communications Conference (GLOBECOM), 1–7. 10.1109/GLOCOM.2018.8647697. [DOI] [Google Scholar]
- Felix, J. E. , Rosen S., and App G. R.. 1971. “Detection of Bacteremia After the Use of an Oral Irrigation Device in Subjects With Periodontitis.” Journal of Periodontology 42, no. 12: 785–787. 10.1902/jop.1971.42.12.785. [DOI] [PubMed] [Google Scholar]
- Felo, A. , Shibly O., Ciancio S. G., Lauciello F. R., and Ho A.. 1997. “Effects of Subgingival Chlorhexidine Irrigation on Peri‐Implant Maintenance.” American Journal of Dentistry 10, no. 2: 107–110. [PubMed] [Google Scholar]
- Feres, M. , M. Duarte P., Figueiredo L. C., Gonçalves C., Shibli J., and Retamal‐Valdes B.. 2022. “Systematic and Scoping Reviews to Assess Biological Parameters.” Journal of Clinical Periodontology 49, no. 9: 884–888. 10.1111/jcpe.13681. [DOI] [PubMed] [Google Scholar]
- Fine, D. H. , Korik I., Furgang D., et al. 1996. “Assessing Pre‐Procedural Subgingival Irrigation and Rinsing With an Antiseptic Mouthrinse to Reduce Bacteremia.” The Journal of the American Dental Association 127, no. 5: 641–646. 10.14219/jada.archive.1996.0276. [DOI] [PubMed] [Google Scholar]
- Flemmig, T. F. , Newman M. G., Doherty F. M., Grossman E., Meckel A. H., and Bakdash M. B.. 1990. “Supragingival Irrigation With 0.06% Chlorhexidine in Naturally Occurring Gingivitis. I. 6 Month Clinical Observations.” Journal of Periodontology 61, no. 2: 112–117. 10.1902/jop.1990.61.2.112. [DOI] [PubMed] [Google Scholar]
- Flint, K. 2014. “Water Flossers Preferred Over String Floss.” Perio Reports 26, no. 11. [Google Scholar]
- Ge, Y. , Bamashmous S., Mancinelli‐Lyle D., Zadeh M., Mohamadzadeh M., and Kotsakis G. A.. 2023. “Interdental Oral Hygiene Interventions Elicit Varying Compositional Microbiome Changes in Naturally Occurring Gingivitis: Secondary Data Analysis From a Clinical Trial.” Journal of Clinical Periodontology 51, no. 3: 309–318. 10.1111/jcpe.13899. [DOI] [PubMed] [Google Scholar]
- Gennai, S. , Bollain J., Ambrosio N., Marruganti C., Graziani F., and Figuero E.. 2023. “Efficacy of Adjunctive Measures in Peri‐Implant Mucositis. A Systematic Review and Meta‐analysis.” Supplement, Journal of Clinical Periodontology 50, no. S26: 161–187. 10.1111/jcpe.13791. [DOI] [PubMed] [Google Scholar]
- Genovesi, A. M. , Lorenzi C., Lyle D. M., et al. 2013. “Periodontal Maintenance Following Scaling and Root Planing. A Randomized Single‐Center Study Comparing Minocycline Treatment and Daily Oral Irrigation With Water.” Minerva Stomatologica 62, no. 12: 1–9. [PubMed] [Google Scholar]
- Gibbons, R. P. , Correa R. J., Jr, Cummings K. B., and Tate Mason J.. 1974. “Use of Water‐Pik and Nephroscope.” Urology 4, no. 5: 605. 10.1016/0090-4295(74)90504-4. [DOI] [PubMed] [Google Scholar]
- Gross, A. , Bhaskar S. N., Cutright D. E., Beasley J. D., and Perez B.. 1971. “The Effect of Pulsating Water Jet Lavage on Experimental Contaminated Wounds.” Journal of Oral Surgery 29, no. 3: 187–190. [PubMed] [Google Scholar]
- Gupta, O. P. , O'Toole E. T., and Hammermeister R. O.. 1973. “Effects of a Water Pressure Device on Oral Hygiene and Gingival Inflammation.” Journal of Periodontology 44, no. 5: 294–298. 10.1902/jop.1973.44.5.294. [DOI] [PubMed] [Google Scholar]
- Hemalatha, S. , Srinivasan A., Srirekha A., Santhosh L., Champa C., and Shetty A.. 2022. “An In Vitro Radiological Evaluation of Irrigant Penetration in the Root Canals Using Three Different Irrigation Systems: Waterpik WP‐100 Device, Passive Irrigation, and Manual Dynamic Irrigation Systems.” Journal of Conservative Dentistry 25, no. 4: 403–408. 10.4103/jcd.jcd_162_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hentenaar, D. F. M. , De Waal Y. C. M., Van Winkelhoff A. J., Meijer H. J. A., and Raghoebar G. M.. 2020. “Non‐Surgical Peri‐Implantitis Treatment Using a Pocket Irrigator Device; Clinical, Microbiological, Radiographical and Patient‐Centred Outcomes—A Pilot Study.” International Journal of Dental Hygiene 18, no. 4: 403–412. 10.1111/idh.12462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrera, D. , Berglundh T., Schwarz F., et al. 2023. “Prevention and Treatment of Peri‐Implant Diseases—The EFP S3 Level Clinical Practice Guideline.” Journal of Clinical Periodontology 50, no. S26: 4–76. 10.1111/jcpe.13823. [DOI] [PubMed] [Google Scholar]
- Herzog, A. , and Hodges K. O.. 1988. “Subgingival Irrigation With Chloramine‐T.” Journal of Dental Hygiene 62, no. 10: 515–521. [PubMed] [Google Scholar]
- Hoover, D. R. , and Robinson H. B. G.. 1971. “The Comparative Effectiveness of a Pulsating Oral Irrigator as an Adjunct in Maintaining Oral Health.” Journal of Periodontology 42, no. 1: 37–39. 10.1902/jop.1971.42.1.37. [DOI] [PubMed] [Google Scholar]
- Hoover, D. R. , Robinson H. B., and Billingsley A.. 1968. “The Comparative Effectiveness of the Water‐Pik in a Noninstructed Population [Abstract].” Journal of Periodontology 39, no. 1: 43. [PubMed] [Google Scholar]
- Hugoson, A. 1978. “Effect of the Water Pik® Device on Plaque Accumulation and Development of Gingivitis.” Journal of Clinical Periodontology 5, no. 2: 95–104. 10.1111/j.1600-051x.1978.tb01911.x. [DOI] [PubMed] [Google Scholar]
- Husseini, A. , Slot D., and Van der Weijden G.. 2008. “The Efficacy of Oral Irrigation in Addition to a Toothbrush on Plaque and the Clinical Parameters of Periodontal Inflammation: A Systematic Review.” International Journal of Dental Hygiene 6, no. 4: 304–314. 10.1111/j.1601-5037.2008.00343.x. [DOI] [PubMed] [Google Scholar]
- Hygienetown . 2010. “Hygienists' Opinions About Oral Irrigation.” Hygienetown 6, no. 4 (May): 12. [Google Scholar]
- Ioannidis, A. , Thurnheer T., Hofer D., Sahrmann P., Guggenheim B., and Schmidlin P. R.. 2015. “Mechanical and Hydrodynamic Homecare Devices to Clean Rough Implant Surfaces—An In Vitro Polyspecies Biofilm Study.” Clinical Oral Implants Research 26, no. 5: 523–528. 10.1111/clr.12436. [DOI] [PubMed] [Google Scholar]
- Isshiki, Y. 1970. “Effect of Oral Cleansing in Cerebral Palsied Children (Application of a Water Jet Device).” The Bulletin of Tokyo Dental College 11, no. 2: 121–131. [PubMed] [Google Scholar]
- Itic, J. , and Serfaty R.. 1992. “Clinical Effectiveness of Subgingival Irrigation With a Pulsated Jet Irrigator Versus Syringe.” Journal of Periodontology 63, no. 3: 174–181. 10.1902/jop.1992.63.3.174. [DOI] [PubMed] [Google Scholar]
- Jain, R. , Chaturvedi R., Pandit N., Grover V., Lyle D., and Jain A.. 2020. “Evaluation of the Efficacy of Subgingival Irrigation in Patients With Moderate‐to‐Severe Chronic Periodontitis Otherwise Indicated for Periodontal Flap Surgeries.” Journal of Indian Society of Periodontology 24, no. 4: 348–353. 10.4103/jisp.jisp_54_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, K. E. , Sanders J. J., Gellin R. G., and Palesch Y. Y.. 1998. “The Effectiveness of a Magnetized Water Oral Irrigator (Hydro Fioss®) on Plaque, Calculus and Gingival Health.” Journal of Clinical Periodontology 25, no. 4: 316–321. 10.1111/j.1600-051x.1998.tb02447.x. [DOI] [PubMed] [Google Scholar]
- Jolkovsky, D. L. , and Lyle D. M.. 2015. “Safety of a Water Flosser: A Literature Review.” Compendium of Continuing Education in Dentistry 36, no. 2: 146–149. [PubMed] [Google Scholar]
- Jose, P. , Ramabhadran B. K., Emmatty R., and Paul T. P.. 2017. “Assessment of the Effect of Ozonated Water Irrigation on Gingival Inflammation in Patients Undergoing Fixed Orthodontic Treatment.” Journal of Indian Society of Periodontology 21, no. 6: 484–488. 10.4103/jisp.jisp_265_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan, E. , and Anderson R.. 1977. “Infective Endocarditis After Use of Dental Irrigation Device.” Lancet 310, no. 8038: 610. 10.1016/s0140-6736(77)91460-x. [DOI] [PubMed] [Google Scholar]
- Kato, K. , Tamura K., and Nakagaki H.. 2012. “Quantitative Evaluation of the Oral Biofilm‐Removing Capacity of a Dental Water Jet Using an Electron‐Probe Microanalyzer.” Archives of Oral Biology 57, no. 1: 30–35. 10.1016/j.archoralbio.2011.08.006. [DOI] [PubMed] [Google Scholar]
- Katz, S. , Katzka I., Platt N., Hajdu E. O., and Bassett E.. 1977. “Cancer in Chronic Ulcerative Colitis. Diagnostic Role of Segmental Colonic Lavage.” The American Journal of Digestive Diseases 22, no. 4: 355–364. 10.1007/BF01072194. [DOI] [PubMed] [Google Scholar]
- Kaur, J. , Grover V., Gupta J., et al. 2023. “Effectiveness of Subgingival Irrigation and Powered Toothbrush as Home Care Maintenance Protocol in Type 2 Diabetic Patients With Active Periodontal Disease: A 4‐Month Randomized Controlled Trial.” Journal of Indian Society of Periodontology 27, no. 5: 515–523. 10.4103/jisp.jisp_509_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly, A. , Resteghini R., Williams B., and Dolby A. E.. 1985. “Pressures Recorded During Periodontal Pocket Irrigation.” Journal of Periodontology 56, no. 5: 297–299. 10.1902/jop.1985.56.5.297. [DOI] [PubMed] [Google Scholar]
- Kesavan, S. K. , Reddy N. P., and Yazdani‐Ardakani S.. 1986. “Experimental Measurement of Impact Pressures Delivered by Oral Water Irrigation Devices.” IEEE Transactions on Biomedical Engineering 33, no. 9: 898–900. 10.1109/TBME.1986.325788. [DOI] [PubMed] [Google Scholar]
- Kim, J. M. , Yoo S. Y., An J. S., et al. 2023. “Effect of a Multichannel Oral Irrigator on Periodontal Health and the Oral Microbiome.” Scientific Reports 13, no. 1: 12043. 10.1038/s41598-023-38894-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, J. S. , Lee E. K., and Jwa S. K.. 2016. “The Gingival Subside Effect by Use of the High Pressure Dental Water Jet.” International Journal of Clinical Preventive Dentistry 12, no. 3: 127–135. 10.15236/ijcpd.2016.12.3.127. [DOI] [Google Scholar]
- Kim, J. Y. , Bae E. B., Sung E. C., et al. 2023. “Effects of the Multi‐Channeled Oral Irrigation (MCOI) Unit in Preventing Dental Plaque Formation and Gingivitis: A Randomized Controlled Trial.” American Journal of Dentistry 36, no. 5: 215–221. [PubMed] [Google Scholar]
- Korn, E. R. 1972. “Use of a Dental Irrigating Unit in the Treatment of Fecal Impactions.” Gastrointestinal Endoscopy 19, no. 2: 88. 10.1016/s0016-5107(72)73966-8. [DOI] [PubMed] [Google Scholar]
- Kotsakis, G. A. , Black R., Kum J., et al. 2021. “Effect of Implant Cleaning on Titanium Particle Dissolution and Cytocompatibility.” Journal of Periodontology 92, no. 4: 580–591. 10.1002/JPER.20-0186. [DOI] [PubMed] [Google Scholar]
- Kotsakis, G. A. , Lian Q., Ioannou A. L., Michalowicz B. S., John M. T., and Chu H.. 2018a. “A Network Meta‐analysis of Interproximal Oral Hygiene Methods in the Reduction of Clinical Indices of Inflammation.” Journal of Periodontology 89, no. 5: 558–570. 10.1002/JPER.17-0368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotsakis, G. A. , Lian Q., Ioannou A. L., Michalowicz B. S., John M. T., and Chu H. A.. 2018b. “A Network Meta‐analysis of Interproximal Oral Hygiene Methods in the Reduction of Clinical Indices of Inflammation.” Journal of Periodontology 89, no. 5: 558–570. 10.1002/JPER.17-0368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozam, G. 1973. “The Effect of Hydromassage on Capillary Strength.” The New York State Dental Journal 39, no. 9: 551–559. [PubMed] [Google Scholar]
- Krajewski, J. , Giblink J., and Gargiulo A.. 1964. “Evaluation of a Water Pressure Cleaning Device as an Adjunct to Periodontal Treatment.” Periodontics 2, no. 2: 76–78. [Google Scholar]
- Krajewski, J. J. , Rubach W. C., and Pope J. W.. 1967. “The Effect of Water Pressure Cleansing on the Clinically Normal Gingival Crevice.” Journal of the California Dental Association 43, no. 5: 452–454. [PubMed] [Google Scholar]
- Krishnan, C. S. , Tompkins G. R., Lyons K. M., and Cannon R. D.. 2023. “Electrolysed Oxidising Water as a Multi‐Purpose Biocide in Dental Healthcare—A Scoping Review.” Gerodontology 40, no. 4: 422–462. 10.1111/ger.12712. [DOI] [PubMed] [Google Scholar]
- Kshitish, D. , and Laxman V. K.. 2010. “The Use of Ozonated Water and 0.2% Chlorhexidine in the Treatment of Periodontitis Patients: A Clinical and Microbiologic Study.” Indian Journal of Dental Research 21, no. 3: 341–348. 10.4103/0970-9290.70796. [DOI] [PubMed] [Google Scholar]
- Lainson, P. A. , Bergquist J. J., and Fraleigh C. M.. 1970. “Clinical Evaluation of Pulsar, a New Pulsating Water Pressure Cleansing Device.” Journal of Periodontology 41, no. 7: 401–405. 10.1902/jop.1970.41.7.401. [DOI] [PubMed] [Google Scholar]
- Lainson, P. A. , Bergquist J. J., and Fraleigh C. M.. 1972. “A Longitudinal Study of Pulsating Water Pressure Cleansing Devices.” Journal of Periodontology 43, no. 7: 444–446. 10.1902/jop.1972.43.7.444. [DOI] [PubMed] [Google Scholar]
- Lainson, P. A. , Bergquist J. J., Tade W. H., and Fraleigh C. M.. 1971. “A Histopathological Study of Tissue Responses to the Pulsar Pulsating Water Pressure Cleansing Device.” Journal of Periodontology 42, no. 2: 101–104. 10.1902/jop.1971.42.2.101. [DOI] [PubMed] [Google Scholar]
- Lang, N. P. , and Räber K.. 1981. “Use of Oral Irrigators as Vehicle for the Application of Antimicrobial Agents in Chemical Plaque Control.” Journal of Clinical Periodontology 8, no. 3: 177–188. 10.1111/j.1600-051X.1981.tb02029.x. [DOI] [PubMed] [Google Scholar]
- Lang, N. P. , and Ramseier‐Grossmann K.. 1981. “Optimal Dosage of Chlorhexidine Digluconate in Chemical Plaque Control When Applied by the Oral Irrigator.” Journal of Clinical Periodontology 8, no. 3: 189–202. 10.1111/j.1600-051X.1981.tb02030.x. [DOI] [PubMed] [Google Scholar]
- Larner, J. R. , and Greenstein G.. 1993. “Effect of Calculus and Irrigator Tip Design on Depth of Subgingival Irrigation.” The International Journal of Periodontics & Restorative Dentistry 13, no. 3: 288–297. [PubMed] [Google Scholar]
- Laumen, J. G. E. , Van Dijck C., Manoharan‐Basil S. S., et al. 2021. “Sub‐Inhibitory Concentrations of Chlorhexidine Induce Resistance to Chlorhexidine and Decrease Antibiotic Susceptibility in Neisseria gonorrhoeae .” Frontiers in Microbiology 12: 776909. 10.3389/fmicb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, C. T. , Huang Y. W., Zhu L., and Weltman R.. 2017. “Prevalences of Peri‐Implantitis and Peri‐Implant Mucositis: Systematic Review and Meta‐Analysis.” Journal of Dentistry 62: 1–12. 10.1016/j.jdent.2017.04.011. [DOI] [PubMed] [Google Scholar]
- Levin, L. , Frankenthal S., Joseph L., Rozitsky D., Levi G., and Machtei E. E.. 2015. “Water Jet With Adjunct Chlorhexidine Gel for Nonsurgical Treatment of Peri‐Implantitis.” Quintessence International 46, no. 2: 133–137. 10.3290/j.qi.a32819. [DOI] [PubMed] [Google Scholar]
- Liang, P. , Ye S., McComas M., Kwon T., and Wang C. W.. 2020. “Evidence‐Based Strategies for Interdental Cleaning: A Practical Decision Tree and Review of the Literature.” Quintessence International 51, no. 1: 84–95. 10.3290/j.qi.a45268. [DOI] [PubMed] [Google Scholar]
- Lin, P. J. , Chuang M. C., and Chang S. C.. 2018. “Efficacy of Using Oxygen Microbubble Device for Facultative Anaerobe Removal.” IET Nanobiotechnology 12, no. 7: 973–980. 10.1049/iet-nbt.2017.0232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobene, R. R. 1969. “The Effect of a Pulsed Water Pressure Cleansing Device on Oral Health.” Journal of Periodontology‐Periodontics 40, no. 1: 667–670. 10.1902/jop.1969.40.11.667. [DOI] [PubMed] [Google Scholar]
- Lobene, R. R. 1971. “A Study of the Force of Water Jets in Relation to Pain and Damage to Gingival Tissues.” Journal of Periodontology 42, no. 3: 166–169. 10.1902/jop.1971.42.3.166. [DOI] [PubMed] [Google Scholar]
- Lobene, R. R. , Soparkar P. M., Hein J. W., and Quigley G. A.. 1972. “A Study of the Effects of Antiseptic Agents and a Pulsating Irrigating Device on Plaque and Gingivitis.” Journal of Periodontology 43, no. 9: 564–568. 10.1902/jop.1972.43.9.564. [DOI] [PubMed] [Google Scholar]
- Löe, H. , and Silness J.. 1963. “Periodontal Disease in Pregnancy. I. Prevalence and Severity.” Acta Odontologica Scandinavica 21: 533–551. 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- Lofthus, J. E. , Waki M. Y., Jolkovsky D. L., et al. 1991. “Bacteremia Following Subgingival Irrigation and Scaling and Root Planing.” Journal of Periodontology 62, no. 10: 602–607. 10.1902/jop.1991.62.10.602. [DOI] [PubMed] [Google Scholar]
- Lorentz, T. C. M. , Miranda Cota L. O., Cortelli J. R., Vargas A. M. D., and Costa F. O.. 2009. “Prospective Study of Complier Individuals Under Periodontal Maintenance Therapy: Analysis of Clinical Periodontal Parameters, Risk Predictors and the Progression of Periodontitis.” Journal of Clinical Periodontology 36, no. 1: 58–67. 10.1111/j.1600-051X.2008.01342.x. [DOI] [PubMed] [Google Scholar]
- Loud, B. 2001. “A WaterPik to Clear Sinuses?” Rn 64, no. 1: 48–49. [PubMed] [Google Scholar]
- Lugassy, A. A. , and Lautenschlager E. P.. 1970. “Water Spray Cleansing Action in Oral Hygiene.” The Journal of the American Dental Hygienists' Association 45, no. 4: 51–53. [PubMed] [Google Scholar]
- Lugassy, A. A. , Lautenschlager E. P., and Katrana D.. 1971. “Characterization of Water Spray Devices.” Journal of Dental Research 50, no. 2: 466–473. 10.1177/00220345710500025901. [DOI] [PubMed] [Google Scholar]
- Lyle, D. M. 2012. “Relevance of the Water Flosser: 50 Years of Data.” Compendium of Continuing Education in Dentistry 33, no. 4: 278–280. [PubMed] [Google Scholar]
- Lyle, D. M. , Qaqish J. G., Goyal C. R., and Schuller R.. 2020. “Efficacy of the Use of a Water Flosser in Addition to an Electric Toothbrush on Clinical Signs of Inflammation: 4‐Week Randomized Controlled Trial.” Compendium of Continuing Education in Dentistry 41, no. 3: 170–177. [PubMed] [Google Scholar]
- Mancinelli‐Lyle, D. , Qaqish J. G., Goyal C. R., and Schuller R.. 2023. “Efficacy of Water Flossing on Clinical Parameters of Inflammation and Plaque: A 4‐Week Randomized Controlled Trial.” International Journal of Dental Hygiene 21, no. 4: 659–668. 10.1111/idh.12770. [DOI] [PubMed] [Google Scholar]
- Manoil, D. , Bostanci N., Mumcu G., et al. 2021. “Novel and Known Periodontal Pathogens Residing in Gingival Crevicular Fluid Are Associated With Rheumatoid Arthritis.” Journal of Periodontology 92, no. 3: 359–370. 10.1002/JPER.20-0295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marinho, V. C. , Higgins J. P., Logan S., and Sheiham A.. 2013. “Fluoride Varnishes for Preventing Dental Caries in Children and Adolescents.” Cochrane Database of Systematic Reviews no. 7. 10.1002/14651858.CD002279.pub2. [DOI] [PubMed] [Google Scholar]
- Matthes, R. , Jablonowski L., Miebach L., et al. 2023. “In‐Vitro Biofilm Removal Efficacy Using Water Jet in Combination With Cold Plasma Technology on Dental Titanium Implants.” International Journal of Molecular Sciences 24, no. 2. 1606. 10.3390/ijms24021606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthes, R. , Jablonowski L., Pitchika V., et al. 2022. “Efficiency of Biofilm Removal By Combination of Water Jet and Cold Plasma: An In‐Vitro Study.” BMC Oral Health 22, no. 1: 157. 10.1186/s12903-022-02195-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazzoleni, S. , De Stefani A., Bordin C., Balasso P., Bruno G., and Gracco A.. 2019. “Dental Water Jet Efficacy in the Plaque Control of Orthodontic Patients Wearing Fixed Appliance: A Randomized Controlled Trial.” Journal of Clinical and Experimental Dentistry 11, no. 11:e957–e963. 10.4317/jced.55411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDevitt, M. J. , and Eames W. B.. 1971. “Attrition of Dental Restorations by a Pulsating Water Device.” Virginia Dental Journal 48, no. 1: 6–10. [PubMed] [Google Scholar]
- Meklas, J. F. , and Stewart J. L.. 1972. “Investigation of the Safety and Effectiveness of an Oral Irrigating Device.” Journal of Periodontology 43, no. 7: 441–443. 10.1902/jop.1972.43.7.441. [DOI] [PubMed] [Google Scholar]
- Mishal AlHarbi, A. , Al‐Kadhi O., and Al‐Sanea J.. 2020. “The Efficacy of Different Methods of Teeth Cleaning on the Levels of Volatile Sulfur Compounds in Patients With Orthodontic Fixed Appliances.” Oral Health and Care 5: 1–8. 10.15761/OHC.1000196. [DOI] [Google Scholar]
- Moore, G. C. , Smith K. T., Christiansen M. M., et al. 2023. “Effect of Interproximal Home Oral Hygiene on Clinical Parameters and Inflammatory Biomarkers in Patients Receiving Periodontal Maintenance.” Journal of Periodontology 94, no. 7: 848–857. 10.1002/JPER.22-0631. [DOI] [PubMed] [Google Scholar]
- Mulimani, P. , and Popowics T.. 2022. “Effect of Orthodontic Appliances on the Oral Environment and Microbiome.” Frontiers in Dental Medicine 3: 924835. 10.3389/fdmed.2022.924835. [DOI] [Google Scholar]
- Murthy, P. , Shaik N., Deshmukh S., and Girish M.. 2018. “Effectiveness of Plaque Control With Novel Pediatric Oral Hygiene Need Station (Modified Oral Irrigation Device) as Compared With Manual Brushing and Flossing: Randomized Controlled Pilot Trial.” Contemporary Clinical Dentistry 9, no. 2: 170–173. 10.4103/ccd.ccd74917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naser‐Alavi, F. , Salari A., Moein N., and Talebzadeh A.. 2022. “Effect of Oral Irrigation Device and Its Solution Type on the Surface Roughness and Topography of Bulk‐Fill Composite Resins.” Journal of Clinical and Experimental Dentistry 14, no. 2: e123–e130. 10.4317/jced.59004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nie, J. 2017. “Oral Hygiene System Design.” Master's thesis, Rochester Institute of Technology. RIT Scholar Works. https://scholarworks.rit.edu/theses/9436/.
- O'Leary, T. J. , Shafer W. G., Swenson H. M., Nesler D. C., and Van Dorn P. R.. 1970. “Possible Penetration of Crevicular Tissue From Oral Hygiene Procedures. I. Use of Oral Irrigating Devices.” Journal of Periodontology 41, no. 3: 158–162. 10.1902/jop.1970.41.41.158. [DOI] [PubMed] [Google Scholar]
- Oshrain, R. L. , Fiorello L. A., Harper D. S., and Lamster I. B.. 1987. “Oral Irrigation Devices. A Clinical Evaluation.” Dental Hygiene 61, no. 12: 551–555. [PubMed] [Google Scholar]
- Ouzzani, M. , Hammady H., Fedorowicz Z., and Elmagarmid A.. 2016. “Rayyan—A Web and Mobile App for Systematic Reviews.” Systematic Reviews 5: 210. 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, S. Y. , Kim K. H., Shin S. Y., et al. 2015. “Decontamination Methods Using a Dental Water Jet and Dental Floss for Microthreaded Implant Fixtures in Regenerative Periimplantitis Treatment.” Implant Dentistry 24, no. 3: 307–316. 10.1097/ID.0000000000000208. [DOI] [PubMed] [Google Scholar]
- Perayil, J. , Menon K., Biswas R., Fenol A., and Vyloppillil R.. 2016. “Comparison of the Efficacy of Subgingival Irrigation With 2% Povidone–Iodine and Tetracycline HCl in Subjects With Chronic Moderate Periodontitis: A Clinico‐Microbiological Study.” Dental Research Journal 13, no. 2: 98–109. [PMC free article] [PubMed] [Google Scholar]
- Petersen, P. E. , and Ogawa H.. 2012. “The Global Burden of Periodontal Disease: Towards Integration With Chronic Disease Prevention and Control.” Periodontology 2000 60, no. 1: 15–39. 10.1111/j.1600-0757.2011.00425.x. [DOI] [PubMed] [Google Scholar]
- Peterson, W. A. , and Shiller W. R.. 1968. “Unsupervised Use of a Water Spray Device by Naval Personnel.” The Journal of Periodontology 39, no. 6: 335–337. 10.1902/jop.1968.39.6.335. [DOI] [PubMed] [Google Scholar]
- Pithon, M. M. , Sant'Anna L. I. D. A., Baião F. C. S., Coqueiro R. S., Maia L. C., and Paranhos L. R.. 2017. “Effectiveness of Different Mechanical Bacterial Plaque Removal Methods in Patients With Fixed Orthodontic Appliance: A Systematic Review/Meta‐Analysis.” Bioscience Journal 33, no. 2: 537–554. 10.14393/BJ-v33n2-35755. [DOI] [Google Scholar]
- Pretty, I. A. , and Ekstrand K. R.. 2016. “Detection and Monitoring of Early Caries Lesions: A Review.” European Archives of Paediatric Dentistry 17, no. 1: 13–25. 10.1007/s40368-015-0208-6. [DOI] [PubMed] [Google Scholar]
- Rams, T. E. , and Keyes P. H.. 1984. “Modifying Oral Irrigation Devices for Subgingival Periodontal Chemotherapy.” General Dentistry 32, no. 4: 302–305. [PubMed] [Google Scholar]
- Ramseier, C. A. , Petitat C., Trepp S., et al. 2021. “Clinical Parameters and Oral Fluid Biomarkers in Gingivitis Subjects Using an Electric Toothbrush With Irrigator vs a Manual Toothbrush Alone Over 8 Weeks: A Randomised Controlled Clinical Trial.” Oral Health & Preventive Dentistry 19, no. 1: 137–147. 10.3290/j.ohpd.b966767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravishankar, P. L. , Venugopal K., and Nadkerny P.. 2015. “Effect of Tetracycline Hydrochloride and Spiramycin Subgingival Irrigation With Pulsated Jet Irrigator in Chronic Periodontitis Patients: A Clinical Study.” Journal of International Oral Health 7, no. 7: 102–107. [PMC free article] [PubMed] [Google Scholar]
- Reddy, N. P. , Kesavan S. K., and Costarella B. R.. 1985. “Evaluation of Oral Water Irrigation Devices.” Engineering in Medicine 14, no. 3: 141–145. 10.1243/emedjour198501403302. [DOI] [PubMed] [Google Scholar]
- Ren, X. , He J., Cheng R., et al. 2023. “The Efficacy and Safety of Oral Irrigator on the Control of Dental Plaque and Gingivitis: A Randomized, Single‐Blind, Parallel‐Group Clinical Trial.” International Journal of Environmental Research and Public Health 20, no. 4: 3726. 10.3390/ijerph20043726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Righolt, A. J. , Jevdjevic M., Marcenes W., and Listl S.. 2018. “Global‐, Regional‐, and Country‐Level Economic Impacts of Dental Diseases in 2015.” Journal of Dental Research 97, no. 5: 501–507. 10.1177/0022034517750572. [DOI] [PubMed] [Google Scholar]
- Romans, A. R. , and App G. R.. 1971. “Bacteremia, a Result from Oral Irrigation in Subjects with Gingivitis.” Journal of Periodontology 42, no. 12: 757–760. 10.1902/jop.1971.42.12.757. [DOI] [PubMed] [Google Scholar]
- Rüdiger, S. , Petersilka G., and Flemmig T. F.. 1999. “Combined Systemic and Local Antimicrobial Therapy of Periodontal Disease in Papillon–Lefèvre Syndrome. A Report of 4 Cases.” Journal of Clinical Periodontology 26, no. 12: 847–854. [PubMed] [Google Scholar]
- Salles, M. M. , de Cássia Oliveira V., Macedo A. P., Silva‐Lovato C. H., and de Freitas de Oliveira Paranhos H.. 2021. “Effectiveness of Brushing Associated With Oral Irrigation in Maintenance of Peri‐implant Tissues and Overdentures: Clinical Parameters and Patient Satisfaction.” Journal of Oral Implantology 47, no. 2: 117–123. 10.1563/aaid-joi-D-19-00092. [DOI] [PubMed] [Google Scholar]
- Sälzer, S. , Slot D. E., Van der Weijden F. A., and Dörfer C. E.. 2015. “Efficacy of Inter‐Dental Mechanical Plaque Control in Managing Gingivitis—A Meta‐Review.” Journal of Clinical Periodontology 42, no. 16: S92–S105. 10.1111/jcpe.12363. [DOI] [PubMed] [Google Scholar]
- Sandra, V. , Nagireddy R., Nooney A., and Nadhamuni M.. 2019. “Comparison of Efficiency of Ozone and Chlorhexidine Subgingival Irrigation in Orthodontic Patients for Controlling Gingival Inflammation.” South African Dental Journal 74, no. 2: 82–86. 10.17159/2519-0105/2019/v74no2a5. [DOI] [Google Scholar]
- Sandra, V. , Shaik Z., Simhadri G., Obili Govindu Gari L. R., Siddamreddy B. P., and Makem N.. 2021. “Comparison of Laser Therapy and Ozonated Water on Gingival Inflammation in Orthodontic Patients With Fixed Appliances.” Journal of Clinical and Translational Research 7, no. 5: 625–630. [PMC free article] [PubMed] [Google Scholar]
- Sanz, M. , Herrera D., Kebschull M., et al. 2020. “Treatment of Stage I–III Periodontitis—The EFP S3 Level Clinical Practice Guideline.” Journal of Clinical Periodontology 47, no. S22: 4–60. 10.1111/jcpe.13290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkisova, F. , and Morse Z.. 2022. “Oral Irrigation Devices: A Scoping Review Protocol.” International Journal of Scientific Reports 8, no. 10: 291–295. 10.18203/issn.2454-2156.IntJSciRep20222378. [DOI] [PubMed] [Google Scholar]
- Sarlati, F. , Azizi A., Zokaei N., Mohaghegh Dolatabadi N., Hasanzadegan Roudsari M., and Moradi Hajiabadi A.. 2016. “Comparison of the Plaque Removal Efficacy of Aquajet Water Flosser and Dental Floss in Adults After a Single Use. (A Preliminary Study).” Journal of Research in Dental and Maxillofacial Sciences 1, no. 4: 16–25. [Google Scholar]
- Schumacher, H. A. 1978. “Experiences with the Water‐Pik Irrigating Device in Multi‐Band Treatment.” Quintessence International, Dental Digest 9, no. 1: 47–49. [PubMed] [Google Scholar]
- Schwarz, F. , Derks J., Monje A., and Wang H. L.. 2018. “Peri‐Implantitis.” Journal of Clinical Periodontology 45, no. S20: S246–S266. 10.1111/jcpe.12954. [DOI] [PubMed] [Google Scholar]
- Selting, W. J. , and Bhaskar S. N.. 1973. “Target Tissue Pressures in Three Water Jet Devices.” Journal of Dental Research 52, no. 3: 441–446. 10.1177/00220345730520030901. [DOI] [PubMed] [Google Scholar]
- Sgarbanti, C. , Kelekis‐Cholakis A., Stavropoulou C., and Halas G.. 2021. “A Comparison of the Efficacy of Interdental Floss to Water Flosser Around Dental Implants.” Cochrane Library. 10.1002/central/CN-01968624/full. [DOI]
- Shalan, L. A. , and Al‐huwaizi H. F.. 2017. “Cleaning Efficiency of Root Canal After Irrigation With New Irrigation Technique: A Scanning Electron Microscopic Study.” Iranian Endodontic Journal 13, no. 1: 102–107. 10.22037/iej.v1i1.17285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shalan, L. A. , Al‐huwaizi H. F., and Fatalla A. A.. 2018. “Apical Extrusion of Debris and Irrigants After Using Different Irrigation Needles and Systems With Different Depth of Penetration: (A Comparative Study).” Biomedical & Pharmacology Journal 11, no. 1: 519–523. 10.13005/bpj/1402. [DOI] [Google Scholar]
- Shalan, L. A. , Al‐huwaizi H. F., Fatalla A. A., and Hameed A. S.. 2018. “Intra‐Canal Pressure Produced by Three Irrigation System: A Comparative Study.” Journal of Research in Medical and Dental Science 6, no. 5: 161–164. [Google Scholar]
- Sharma, N. C. , Lyle D. M., Qaqish J. G., and Schuller R.. 2012. “Comparison of Two Power Interdental Cleaning Devices on Plaque Removal.” The Journal of Clinical Dentistry 23, no. 1: 17–21. [PubMed] [Google Scholar]
- Silbereisen, A. , Lira‐Junior R., Åkerman S., Klinge B., Boström E. A., and Bostanci N.. 2023. “Association of Salivary TREM‐1 and PGLYRP1 Inflammatory Markers With Non‐communicable Diseases.” Journal of Clinical Periodontology 50, no. 11: 1467–1475. 10.1111/jcpe.13858. [DOI] [PubMed] [Google Scholar]
- Silness, J. , and Löe H.. 1964. “Periodontal Disease in Pregnancy. II Correlation Between Oral Hygiene and Periodontal Condition.” Acta Odontologica Scandinavica 22: 121–135. 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- Sirinirund, B. , Siqueira R., Li J., Mendonça G., Zalucha J., and Wang H. L.. 2023. “Effects of Crown Contour on Artificial Biofilm Removal Efficacy With Interdental Cleaning AIDS: An In Vitro Study.” Clinical Oral Implants Research 34, no. 8: 783–792. 10.1111/clr.14105. [DOI] [PubMed] [Google Scholar]
- Slot, D. E. , Valkenburg C., and Van der Weijden G. A.. 2020. “Mechanical Plaque Removal of Periodontal Maintenance Patients: A Systematic Review and Network Meta‐analysis.” Journal of Clinical Periodontology 47, no. S22: 107–124. 10.1111/jcpe.13275. [DOI] [PubMed] [Google Scholar]
- Soltanianzadeh, M. 2020. “Evaluation of Complementary Supragingival Irrigation on the Periodontal Health in the Management of Jaw and Dentoalveolar Fractures Using Arch Bar and Dentoalveolar Wiring.” Postgraduate Degree in Oral and Maxillofacial Surgery, Kerman University of Medical Sciences. The WHO Clinical Trials Registry Platform. https://trialsearch.who.int/.
- Stelmakh, V. , Slot D., and van der Weijden G.. 2017. “Self‐Reported Periodontal Conditions Among Dutch Women During Pregnancy.” International Journal of Dental Hygiene 15, no. 4: e9–e15. 10.1111/idh.12210. [DOI] [PubMed] [Google Scholar]
- Sun, J. , Tong D., Sun C., et al. 2023. “Knowledge, Attitude, and Practice Toward Self‐control of Dental Plaque Among Patients With Periodontal Diseases: A Cross‐Sectional Study.” BMC Oral Health 23, no. 1: 628. 10.1186/s12903-023-03352-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tatuskar, P. V. , Karmakar S., Walavalkar N. N., and Vandana K. L.. 2023. “Effect of Ozone Irrigation and Powered Toothbrushing on Dental Plaque, Gingival Inflammation, and Microbial Status in Institutionalized Mentally Challenged Individuals: A Double‐blinded, Randomized, Controlled Clinical Trial.” Journal of Indian Society of Periodontology 27, no. 3: 315–319. 10.4103/jisp.jisp_69_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tawakoli, P. N. , Sauer B., Becker K., Buchalla W., and Attin T.. 2015. “Interproximal Biofilm Removal by Intervallic Use of a Sonic Toothbrush Compared to an Oral Irrigation System.” BMC Oral Health 15: 91. 10.1186/s12903-015-0079-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tecco, S. , Nota A., D'Amicantonio T., Pittari L., Monti M., and Polizzi E.. 2022. “Effects of an Ozonated Water Irrigator on the Plaque Index and Bleeding Index of Pregnant Women.” Journal of Clinical Medicine 11, no. 14: 4107. 10.3390/jcm11144107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The EndNote Team . 2013. EndNote (Version EndNote X9) [64 bit]. Philadelphia, PA: Clarivate.
- Tonetti, M. S. , Jepsen S., Jin L., and Otomo‐Corgel J.. 2017. “Impact of the Global Burden of Periodontal Diseases on Health, Nutrition and Wellbeing of Mankind: A Call for Global Action.” Journal of Clinical Periodontology 44, no. 5: 456–462. 10.1111/jcpe.12732. [DOI] [PubMed] [Google Scholar]
- Tricco, A. C. , Lillie E., Zarin W., et al. 2018. “PRISMA Extension for Scoping Reviews (PRISMA‐ScR): Checklist and Explanation.” Annals of Internal Medicine 169, no. 7: 467–473. 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- Tsolov, R. 2022. “Periodontal Status in Patients With Mandibular Fractures.” Journal of IMAB—Annual Proceeding (Scientific Papers) 28, no. 1: 4247–4250. 10.5272/jimab.2022281.4247. [DOI] [Google Scholar]
- Tütüncüoglu, S. , Cetinkaya B. O., Pamuk F., et al. 2022. “Clinical and Biochemical Evaluation of Oral Irrigation in Patients With Peri‐Implant Mucositis: A Randomized Clinical Trial.” Clinical Oral Investigations 26, no. 1: 659–671. 10.1007/s00784-021-04044-x. [DOI] [PubMed] [Google Scholar]
- Tyler, D. , Kang J., and Goh H. H.. 2023. “Effectiveness of Waterpik® for Oral Hygiene Maintenance in Orthodontic Fixed Appliance Patients: A Randomised Controlled Trial.” Journal of Orthodontics 50, no. 4: 367–377. 10.1177/14653125231173708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Food & Drug Administration . 2023. “Oral Irrigation Unit.” https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/cfrsearch.cfm?fr=872.6510.
- Van der Weijden, G. A. , and van Loveren C.. 2023. “Mechanical Plaque Removal in Step‐1 of Care.” Periodontology 2000. Published ahead of print, December 26, 2023. 10.1111/prd.12541. [DOI] [PubMed] [Google Scholar]
- Van Dijk, L. J. , Lie M. A., Van den Heuvel E. R., and Van der Weijden G. A.. 2018. “Adult Periodontitis Treated With a New Device for Subgingival Lavage—A Randomized Controlled Clinical Trial Using a Split‐Mouth Design.” International Journal of Dental Hygiene 16, no. 4: 559–568. 10.1111/idh.12344. [DOI] [PubMed] [Google Scholar]
- Varela‐Centelles, P. , Bugarín‐González R., Blanco‐Hortas A., Estany‐Gestal A., Varela‐Centelles A., and Seoane‐Romero J. M.. 2020. “Family Nurses, Oral Hygiene, and Educational Implications: A Cross‐Sectional Study.” Stomatologija 22, no. 4: 120–124. [PubMed] [Google Scholar]
- Volman, E. I. , Stellrecht E., and Scannapieco F. A.. 2021. “Proven Primary Prevention Strategies for Plaque‐Induced Periodontal Disease—An Umbrella Review.” Journal of the International Academy of Periodontology 23, no. 4: 350–367. [Google Scholar]
- Waki, M. Y. , Jolkovsky D. L., Otomo‐Corgel J., et al. 1990. “Effects of Subgingival Irrigation on Bacteremia Following Scaling and Root Planing.” Journal of Periodontology 61, no. 7: 405–411. 10.1902/jop.1990.61.7.405. [DOI] [PubMed] [Google Scholar]
- Walsh, M. , Heckman B., Leggott P., Armitage G., and Robertson P. B.. 1989. “Comparison of Manual and Power Toothbrushing, With and Without Adjunctive Oral Irrigation, for Controlling Plaque and Gingivitis.” Journal of Clinical Periodontology 16, no. 7: 419–427. 10.1111/j.1600-051x.1989.tb01670.x. [DOI] [PubMed] [Google Scholar]
- Walsh, T. F. , Glenwright, H. D. , and Hull, P. S. 1992. “Clinical Effects of Pulsed Oral Irrigation With 0.2% Chlorehexidine Digluconate in Patients With Adult Periodontitis.” Journal of Clinical Periodontology 19, no. 4: 245–248. 10.1111/j.1600-051x.1992.tb00461.x. [DOI] [PubMed] [Google Scholar]
- Watt, D. L. , Rosenfelder C., and Sutton C. D.. 1993. “The Effect of Oral Irrigation With a Magnetic Water Treatment Device on Plaque and Calculus.” Journal of Clinical Periodontology 20, no. 5: 314–317. 10.1111/j.1600-051x.1993.tb00366.x. [DOI] [PubMed] [Google Scholar]
- Watts, E. A. , and Newman H. N.. 1986. “Clinical Effects on Chronic Periodontitis of a Simplified System of Oral Hygiene Including Subgingival Pulsated Jet Irrigation With Chlorhexidine.” Journal of Clinical Periodontology 13, no. 7: 666–670. 10.1111/j.1600-051x.1986.tb00863.x. [DOI] [PubMed] [Google Scholar]
- Wiesmüller, V. , Kasslatter M., Zengin B., et al. 2023. “Cleansing Efficacy of an Oral Irrigator With Microburst Technology in Orthodontic Patients—A Randomized‐Controlled Crossover Study.” Clinical Oral Investigations 27: 2089–2095. 10.1007/s00784-023-05003-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winter, A. A. 1982. “Rapid Destruction Caused by a Water‐Irrigating Device.” Dental Health 21, no. 5: 18–20. [PubMed] [Google Scholar]
- Wolff, L. F. , Bakdash M. B., Pilhlstrom B. L., Bandt C. L., and Aeppli D. M.. 1989. “The Effect of Professional and Home Subgingival Irrigation With Antimicrobial Agents on Gingivitis and Early Periodontitis.” Journal of Dental Hygiene 63, no. 5: 222–225, 241. [PubMed] [Google Scholar]
- World Health Organization . 2023. “Disability.” https://www.who.int/news-room/fact-sheets/detail/disability-and-health.
- Worthington, H. V. , MacDonald L., Poklepovic Pericic T., et al. 2019. “Home Use of Interdental Cleaning Devices, in Addition to Toothbrushing, for Preventing and Controlling Periodontal Diseases and Dental Caries.” Cochrane Database of Systematic Reviews no. 4. 10.1002/14651858.CD012018.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright, W. E. , and Tempel T. R.. 1974. “Effect of Oral Hygiene on Clearance of Soluble Chemotactic Bacterial Products From Human Saliva.” Journal of Periodontology 45, no. 3: 134–138. 10.1902/jop.1974.45.3.134. [DOI] [PubMed] [Google Scholar]
- Xu, X. , Zhou Y., Liu C., et al. 2023. “Effects of Water Flossing on Gingival Inflammation and Supragingival Plaque Microbiota: A 12‐Week Randomized Controlled Trial.” Clinical Oral Investigations 27, no. 8: 4567–4577. 10.1007/s00784-023-05081-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamada, J. , Peng K., and Kokubun T., et al. 2018. “Optimization of a Cavitating Jet for Removing Dental Plaque From the Surface of the Screw of an Implant and Its Practical Application.” Journal of Biomechanical Science and Engineering 13, no. 2: 17‐00102. 10.1299/jbse.17-00102. [DOI] [Google Scholar]
- Yamada, J. , Takiguchi T., Saito A., Odanaka H., Soyama H., and Yamamoto M.. 2017. “Removal of Oral Biofilm on an Implant Fixture by a Cavitating Jet.” Implant Dentistry 26, no. 6: 904–910. 10.1097/ID.0000000000000681. [DOI] [PubMed] [Google Scholar]
- Yuen, H. K. 2013. “Effect of a Home Telecare Program on Oral Health Among Adults With Tetraplegia: A Pilot Study.” Spinal Cord 51, no. 6: 477–481. 10.1038/sc.2012.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuen, H. K. , and Pope C.. 2009. “Oral Home Telecare for Adults With Tetraplegia: A Feasibility Study.” Special Care in Dentistry 29, no. 5: 204–209. 10.1111/j.1754-4505.2009.00094.x. [DOI] [PubMed] [Google Scholar]
- Zellmer, I. H. , Couch E. T., Berens L., and Curtis D. A.. 2020. “Dental Hygienists' Knowledge Regarding Dental Implant Maintenance Care: A National Survey.” Journal of Dental Hygiene 94, no. 6: 6–15. [PubMed] [Google Scholar]
- Zhao, R. , Liu S., Liu Y., and Cui S.. 2022. “Adjunctive Use of Active Compounds Such As Chlorhexidine in the Nonsurgical Treatment of Peri‐Implant Mucositis for Oral Health: A Systematic Review and Meta‐analysis.” Oxidative Medicine and Cellular Longevity 2022: 2312784. 10.1155/2022/2312784. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


