Abstract
As hematopoietic cell transplantation (HCT) and cellular therapy expand to new indications and international access improves, the number of HCTs performed annually continues to rise. Parallel improvements in HCT techniques and supportive care entails more patients surviving long term, creating further emphasis on survivorship needs. Survivors are at risk for developing late complications secondary to pretransplantation, peritransplantation, and post-transplantation exposures and other underlying risk factors. Guidelines for screening and preventive practices for HCT survivors were originally published in 2006 and then updated in 2012. An international group of experts was convened to review the contemporary literature and update the recommendations while considering the changing practices of HCT and cellular therapy. This review provides updated pediatric and adult survivorship guidelines for HCT and cellular therapy. The contributory role of chronic graft-versus-host disease (cGVHD) to the development of late effects is discussed, but cGVHD management is not covered in detail. These guidelines emphasize the special needs of patients with distinct underlying HCT indications or comorbidities (eg, hemoglobinopathies, older adults) but do not replace more detailed group-, disease-, or condition-specific guidelines. Although these recommendations should be applicable to the vast majority of HCT recipients, resource constraints may limit their implementation in some settings.
Keywords: TCT, Survivorship, Recommendations, Late-effects, Screening, Prevention, BMT, HCT, Transplantation
INTRODUCTION
Hematopoietic cell transplantation (HCT) is a potentially lifesaving treatment for many diseases. With expansion to new indications, better international access, and improved outcomes, the population of long-term HCT survivors is rapidly growing [1–6]. However, survivors face serious long-term medical issues, psychosocial challenges that often impact quality of life (QoL), and decreased life expectancy [7–10]. Consequently, prevention and recognition of late effects, followed by prompt intervention, are crucial to improving long-term outcomes in survivors. Additionally, there is an urgent need to better understand the biology and patient experience of HCT’s late effects, as well as the ideal health care delivery infrastructure for managing this growing population [11–17].
Previous guidelines for long-term survivors of HCT were produced as collaborative efforts by multiple societies in 2006 and 2012 [18–23]. To update guidelines and provide further geographic diversity, we convened a working group of experts from multiple international organizations as well as patient advocates (Figure 1). We set out to design these recommendations to adapt to evolving treatment paradigms in transplantation and cellular therapy. The topics are organized by organ system or complication type. Tables with recommendations have been created by organ system, and supplementary tables that include more detailed information are also provided. Owing to the overall scope of the topic, several appendices are included.
Figure 1.
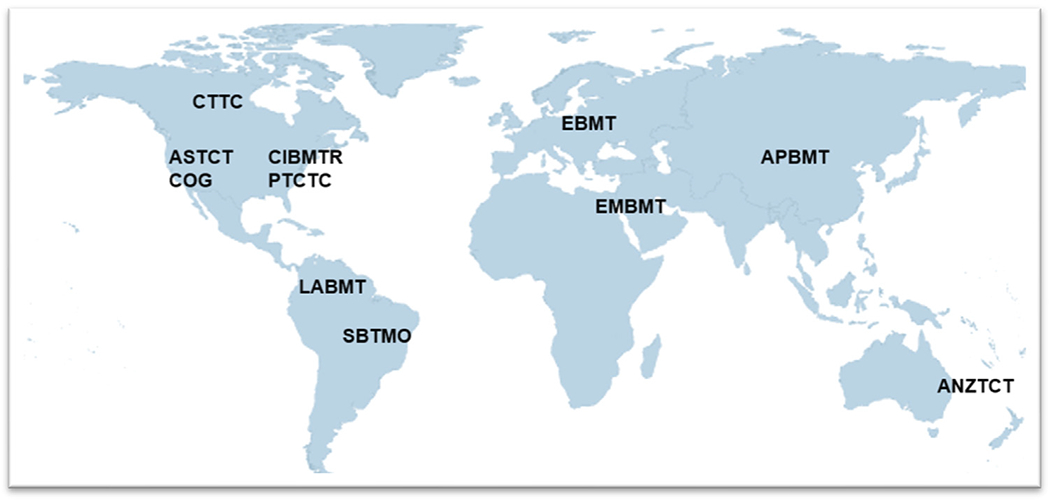
International societies represented. American Society for Transplantation and Cellular Therapy (ASTCT), Asia-Pacific Blood and Marrow Transplantation Group (APBMT), Australia and New Zealand Transplant and Cellular Therapies (ANZTCT), Children’s Oncology Group (COG), Cell Therapy Transplant Canada (CTTC), Center for International Blood and Marrow Transplantation Research (CIBMTR), East Mediterranean Blood and Marrow Transplantation Group (EMBMT), European Society for Blood and Marrow Transplantation (EBMT), Latin American Bone Marrow Transplantation Group (LABMT), Pediatric Transplantation and Cellular Therapy Consortium (PTCTC), and Sociedade Brasileira de Transplante de Medula Ossea (SBTMO).
It should be noted that many late effects may take years or even decades to manifest, and recommendations generally can be followed in perpetuity (unless specified otherwise); however, for some clinical situations, eventual discontinuation of screening may be reasonable. Additionally, although these recommendations can be helpful at a population level, patient-specific risk factors also should be considered, and these recommendations are not meant to replace the judgment or advice of clinicians caring for individual patients. The recommendations in this document rely heavily on expert consensus given the lack of prospective randomized trials for screening, prevention, or treatment [5]. Survivorship care may take many forms, and these recommendations may be adapted as appropriate. Furthermore, currently available data are derived largely from North American and European centers and might not be generalizable to all populations, and resource constraints may limit guideline implementation, especially in certain geographic regions. Therefore, consideration of local data-driven guidance is valuable for survivor care.
METHODOLOGY
First, a core group of 7 participants (S.J.R., N.S.B., B.K.H., C.D., K.S.B., N.S.M., and R.P.) reviewed the 2012 guidelines and suggested new topics for inclusion, areas to emphasize, and changes in formatting. These suggestions were reviewed with the larger group of 30 participants, additional changes were suggested and implemented, and the overall format was agreed upon. Subgroups of 2 to 4 members reviewed the relevant literature to draft topic section content and recommendations; all participants had the opportunity to provide feedback. All participants were then surveyed to determine agreement with each screening, prevention, and treatment recommendation. The recommendation was adopted if ≥85% agreement occurred but was further edited before a second round of voting if agreement was <85%. If >50% consensus ultimately could not be reached, the recommendation was abandoned. Specific recommendations were then categorized similarly to the National Comprehensive Cancer Network (NCCN) approach; all were classified as either 2A or 2B, indicating a lower level of evidence with uniform consensus (2A; ≥85%) or consensus (2B; >50% to <85%) [24].
HEMATOPOIETIC COMPLICATIONS
Common hematopoietic complications include autoimmune cytopenias (AICs), clonal hematopoiesis of indeterminate potential (CHIP), iron overload, and venous thromboembolism (VTE). Mixed chimerism also may present challenges for some patients (Table 1, Supplementary Table S1). AICs can occur weeks to years after allogeneic HCT, with risk factors including younger age, nonmalignant disease, umbilical cord blood graft source, unrelated or haploidentical donor, conditioning with antithymocyte globulin (ATG) or alemtuzumab, absence of total body irradiation (TBI), presence of GVHD, and cytomegalovirus (CMV) reactivation [25–27]. Cytopenias should prompt an etiologic investigation, especially to exclude autoimmunity or therapy-related myeloid neoplasm (tMN; see Subsequent Malignant Neoplasms); treatment is based on underlying etiologies.
Table 1.
Hematologic Complications
| Recommendation | Grade | Ref | Comments |
|---|---|---|---|
| • CBC at most routine clinical visits for at least 10 years post-HCT, and as needed | 2A | ||
| • Hemoglobinopathy: chimerism at least every 3 months in year 1 post-HCT and every 6 months in year 2. Further chimerism based on previous results | 2A | ||
| • Regular monitoring of serum ferritin until normalized | 2A | [33,362,363] | • Serum ferritin is a good, albeit nonspecific, initial screening test for iron overload. |
| • Iron quantification by MRI more accurately evaluates iron overload than serum ferritin; recommended to assess liver and cardiac iron levels and follow progress after phlebotomies and/or iron chelation. | 2A | [33,362,363] | • Risk based on prior transfusion history or underlying HCT indication (eg, hemoglobinopathy, Diamond-Blackfan anemia, high-risk leukemia, neuroblastoma) |
| • Post-HCT phlebotomy is the treatment of choice for significant iron overload. | 2A | [33,364,365] | • Iron chelation may be considered in patients ineligible for phlebotomy; prolonged or combined modality treatment may be necessary. • In females, resumption of menstruation (either naturally or via cyclical hormone replacement regimens) may reduce iron burden. |
| • VTE prophylaxis is indicated in patients with multiple myeloma receiving immunomodulatory imide drugs (eg, lenalidomide) and chemotherapy and/or dexamethasone after HCT. | 2B | [366,367] | |
| • Before initiating anticoagulation, the risk of bleeding should be assessed. | 2A | ||
| • Inherited bone marrow failure syndromes require specialized follow up with a multidisciplinary specialist team. | 2A | • Hematologist familiar with the underlying condition, HCT physician, other sub-specialty providers |
The clonal expansion of hematopoietic progenitors in CHIP appears to be due to age-associated somatic mutation without an overt hematologic malignancy [28–30]. CHIP is associated with the development of subsequent hematologic malignancies and cardiovascular disease in the general population [28–30], as well as inferior overall survival, increased risk of tMN, and higher rates of cGVHD in the HCT setting [31,32]. Currently available data are too sparse to allow for specific recommendations regarding CHIP-associated late effects monitoring; however, all survivors should undergo an individualized cardiovascular disease risk assessment (see Cardiovascular Disease), and CHIP may be considered among those risk factors.
Iron overload from pre-HCT transfusion burden is common, and patients with disorders associated with ineffective erythropoiesis are at particular risk [33]. Post-HCT iron overload is associated with infections, chronic liver disease, pituitary dysfunction, glucose dysregulation, and cardiomyopathy [33]. Survivors of both autologous and allogenic HCT are at increased risk for VTE [34–37], and long-term HCT survivors with a history of VTE have greater nonrelapse mortality [38]. Risk factors include indwelling catheters, acute GVHD (aGVHD) or cGVHD, infections, prolonged immobilization, HCT for malignancy, endothelial damage from conditioning, and prior history of VTE [34–36,39,40]. Patients receiving immunomodulatory drugs for myeloma also are at higher risk.
IMMUNITY AND INFECTIONS
HCT survivors are at risk for developing infections and autoimmune diseases post-HCT; however, significant gaps still remain in our knowledge of immune dysfunction as a late effect of HCT [16]. Infection is a significant cause of late mortality after allogeneic HCT, even in individuals without cGVHD [7,8,41]. Late CMV infections are seen most frequently in patients with early CMV disease, cGVHD, and late immune manipulation (eg, lymphocyte infusions). Other viral infections that may lead to significant hospitalization, morbidity, and mortality include varicella zoster virus (VZV), influenza, and coronavirus disease 2019 (COVID-19) [42,43]. Survivors also are at risk for Epstein-Barr virus (EBV), post-transplantation lymphoproliferative disorder (PTLD) (see Subsequent Malignant Neoplasms), and hepatitis B and C viruses (see Gastrointestinal Complications). Several risk factors affect the incidence of late fungal infections, including cGVHD with ongoing immunosuppression, history of relapse, age, underlying disease, type of conditioning (especially with TBI), umbilical cord blood graft source, and the use of T cell depletion (Table 2, Supplementary Table S2) [16,44–46]. Pneumocystis jirovecii pneumonia is rare unless there is nonadherence with prescribed prophylaxis, although when it does occur, the mortality rate is high [47–49]. Finally, bacterial infections pose a risk for long-term survivors with asplenia, cGVHD, a central line, unvaccinated status, or other risk factors.
Table 2.
Immunity and Infections
| Recommendation | Grade | Ref | Comments |
|---|---|---|---|
| • All survivors should be offered a full vaccination program according to published guidelines considering patient age and country recommendations. • Inactivated vaccines may begin 3 to 6 months after HCT. Includes patients with GVHD and/or on IST given higher risk of infection. • Vaccinate patients with asplenia or functional asplenia for S. pneumoniae and N. meningitidis (MCV4, group B); educate on sepsis/fever management; consider antimicrobial prophylaxis. |
2A | [63–66,368] | • We recognize the potential limitation of early vaccination in some groups of patients with impaired immunity and the potential value of monitoring immune responses in these patients to guide ongoing management. • Splenic presence and function (ie, SCD and autoinfarction, high-dose splenic irradiation), lymphocyte function (ie, hypogammaglobulinemia), and overall immune status should be considered in overall vaccine timing/prioritization. |
| • Routine use of IVIG in adults generally not recommended. • Supplemental IVIG may be considered for selected HCT recipients with IgG levels <400 mg/dL |
2B | [57,72–79] | • No demonstrated survival advantage in unselected adult patients • Consider for those with IgG levels <400 mg/dL and recurrent sino-pulmonary infections or those receiving anti-B cell or CAR T-Cell therapy or patients with very low IgG levels (<200 mg/dL) |
| • For patients with IEI, pay careful attention to immune reconstitution and mixed chimerism. Assess lymphocyte subsets, mitogen proliferation, immunoglobulin levels and antibody responses every 3-6 months until normalized and as needed | 2A | ||
| • Patients with MM are at increased risk for infection; specific anti-myeloma medications warrant specific antimicrobial prophylaxis | 2A |
General guidelines for prophylaxis and treatment of HCT-associated infections (both early and late) and advice for safe living are beyond the scope of these recommendations and have been reviewed elsewhere [50–59]. Dietary restrictions and guidelines on returning to work or school practices also lack uniform consensus [60–62]. Nonetheless, chronically immune suppressed patients should be aware of infection risks and how to recognize signs and symptoms of infection and instructed to adhere to antimicrobial prophylaxis and vaccination guidelines.
Vaccine-preventable late infections are 3 times more common in ≥2-year HCT cancer survivors compared to non-HCT cancer survivors and >30 times more common compared to the general population [45]. All survivors should be offered a full vaccination program according to published guidelines, taking into account patient age and country recommendations [63–66], as detailed in reports from the Infectious Disease Society of America and the 2017 European Conference on Infections in Leukemia (Appendix 1) [63,67,68]. At the time of this publication, COVID-19 vaccination is recommended at 100 days post-HCT, although immunogenicity remains variable, and this is a rapidly changing area of study [69–71].
The routine use of i.v. immune globulin (IVIG) for hypogammaglobulinemia in adults generally is not recommended, given the lack of survival advantage or infection prevention with routine use in unselected patients after HCT [72], as well as potential side effects. Certain populations may benefit from IVIG supplementation, however [57,72–79].
OCULAR COMPLICATIONS
Ocular complications after HCT can be broadly divided into GVHD-related and non-GVHD-related, although overlap often exists (Table 3, Supplementary Table S3) [80–86]. Lacrimal gland dysfunction is the most common feature of ocular GVHD. Conjunctival involvement in GVHD is rare in children but more frequent in adults. Dry eyes also can be seen with radiation effects, chemotherapy, lid dysfunction, medications, and meibomian gland dysfunction. Post-HCT cataract formation has been associated with glucocorticoid treatment for GVHD, busulfan conditioning, and TBI [86]. Glaucoma may be a late complication of TBI, although systemic or topical corticosteroid therapy for cGVHD also can elevate intraocular pressure in susceptible patients, with children at greater risk. Infectious complications include viral bacterial, fungal, and toxoplasma. Retinal hemorrhage and detachment are rare but can be associated with CMV retinitis or the neovascularization seen in ischemic retinopathy.
Table 3.
Ocular, Oral and Dental Complications
| Recommendation | Grade | Ref | Comments |
|---|---|---|---|
| • Question about eye concerns at each follow-up visit. | 2A | [84,85,369] | • Advise to report dryness, light sensitivity, excessive tearing, foreign body sensation, pain, redness, swelling, mucoid aggregates, vision changes. |
| • Inform about risk of premature cataracts for TBI recipients | 2A | • Busulfan and glucocorticoids are also risk factors. | |
| • Ocular exam recommended at onset of any cGVHD, dry eye symptoms, changes in vision or other eye symptoms. | 2A | [84,369] | • The NIH Consensus Development Project recommends consultation with an eye specialist every 3 months during the first year post-HCT and hen at longer intervals thereafter, with recommendations on best practice eye examination; currently unknown if this approach reduces long-term ocular morbidity. |
| • Monitoring of IOP important in patients receiving any form of glucocorticoids. | 2A | • IOP may be elevated with topical glucocorticoids, particularly in children. | |
| • Hurler syndrome: ongoing ophthalmologic assessment for glaucoma, cataracts, progression of corneal clouding. | 2A | ||
| • Evaluation by a dentist or oral medicine specialist at 6 months, 1 year, and annually thereafter may be beneficial. • More frequent dental consultations and screening (eg, every 6 months) for those at a high risk for oral cancer (eg, FA, radiation to head/neck, refractory cGVHD. • Oral/radiologic tooth development assessment for children. |
2A | • Inform regarding preventive oral health, routine dental hygiene, and risks/symptoms of oral cancer. | |
| • At each survivorship visit screen for cGVHD by history and exam, ask about high-risk habits; head/neck/oral exam. | 2A | [370] | • Symptoms: dry mouth, difficulty swallowing, pain in the oral cavity. |
| • Council to avoid smoking, vaping, and chewing tobacco, decrease regular intake of sugar containing beverages, avoid intraoral piercing, pursue post-HCT HPV vaccination. | 2A | [66,342] | |
| • Patients with xerostomia should receive meticulous oral hygiene, undertake preventive measures for dental/periodontal disease, and aggressive treatment of oral infections. Trauma to oral mucosa should be avoided. | 2A | • Mouthguards may be useful. • Avoid medications that can cause or exacerbate xerostomia. |
ORAL AND DENTAL COMPLICATIONS
Oral and dental complications may result from cGVHD, chemotherapy, and irradiation therapy (Table 3, Supplementary Table S4). Oral cGVHD is common and can involve the mucosa, salivary glands (xerostomia), oral and lingual muscles, taste buds, and gingiva. Patients may report oral pain, dryness, odynophagia, dysphagia, and sensitivity to normally tolerated flavors [80,87,88]. Gingivitis due to cGVHD may further limit tooth-brushing. Presence of cGVHD is also a risk factor for squamous cell cancer (see Subsequent Malignant Neoplasms) [89–95]. Late complications also include increased dental demineralization and caries, teeth staining, gingival enlargement, symptomatic acute periodontal infection, and asymptomatic chronic periodontal infection [96]. Salivary gland dysfunction predisposes to caries, oral herpes simplex and candidiasis, mechanical and epithelial injuries, and impaired tooth mineralization [97]. Protracted xerostomia also may occur in patients without cGVHD due to chemotherapy or radiation or as medication side effect. Chemoradiotherapy exposure may disturb dental development in 50% to 80% of children; younger age at HCT and receipt of TBI are important risk factors [96,98]. TBI also may lead to mandibular underdevelopment and mandibular joint anomalies. Routine dental care is imperative for optimal oral health. Frequent self and professional oral examinations are the mainstays of early diagnosis of oral cancer. Patients should report lesions that do not heal, localized pain, leukoplakia, or other mucosal changes.
RESPIRATORY COMPLICATIONS
Late pulmonary complications include idiopathic pneumonia syndrome (IPS), pulmonary fibrosis, bronchiolitis obliterans syndrome (BOS), and cryptogenic organizing pneumonia (COP) (Table 4, Supplementary Table S5) [22]. IPS usually develops within the first 120 days post-HCT, although later cases can occur. IPS increases the risk of transplantation-related mortality and is thought to be multifactorial, with risk factors including allogeneic HCT, chest radiation or TBI, certain chemotherapies, increasing age, and GVHD [99–101]. Pulmonary fibrosis may occur late after HCT and is generally characterized by pre- or post-HCT lung injury with specific risk factors including radiation, bleomycin, busulfan, carmustine, smoking, history of acute lung injury, and post-transplantation CMV pneumonitis.
Table 4.
Respiratory Complications
| Recommendation | Grade | Ref | Comments |
|---|---|---|---|
| • Assessment for pulmonary symptoms (cough, wheezing, dyspnea) and physical examination at each visit | 2A | ||
| • Expert consensus recommends PFT screening every 3 months for the first year after HCT, every six months for the second year, and then annually for 5 years after HCT (or until final adult height in children, whichever occurs later) | 2B | [103–105,369,372–377] | • Spirometry and hemoglobin corrected DLCO • Age <6 usually unable to perform PFTs; alternative screening with pulse oximetry, multiple breath washout testing, parametric response mapping by CT may be considered if available, but this requires further study. |
| • PFTs at initial diagnosis of any cGVHD, then at least spirometry every 3 to 6 months until discontinuation of all systemic IST for cGVHD. | 2A | [369,375–377] | • Survivors, especially those with cGVHD, can develop moderate to severe PFT abnormalities before becoming symptomatic. |
| • PFTs recommended at regular intervals following HCT for patients with DKC; referral to a pulmonologist if abnormalities are noted. | 2A | [378] | |
| • CT chest imaging (high resolution where available) recommended in symptomatic individuals/abnormal PFTs. | 2A | ||
| • Consider pulmonology consultation for those with symptomatic pulmonary dysfunction or new asymptomatic PFT abnormalities, especially irreversible air flow obstruction | 2A | ||
| • Recommend vaccinations against respiratory pathogens (eg, pneumococcus) and avoidance of tobacco, smoking, vaping. | 2A |
BOS, considered a lung manifestation of cGVHD, is often diagnosed within the first 2 years post-HCT [102–105]. Patients maybe asymptomatic initially, making diagnosis difficult without screening. cGVHD is the most important risk factor for developing BOS; other risk factors include aGVHD, lung toxic medications, ABO incompatibility, peripheral blood grafts, and early post-HCT viral infections [102,106]. Early detection and treatment of BOS impacts outcomes. The use of National Institutes of Health (NIH) diagnostic criteria usually establishes the diagnosis of BOS without the need for lung biopsy [80]. Cryptogenic organizing pneumonia, previously known as bronchiolitis obliterans organizing pneumonia (BOOP), typically presents at <1 year post-HCT with fever, cough, and dyspnea; a chest computed tomography scan shows solitary or multifocal pulmonary infiltrates, whereas pulmonary function tests classically show a restrictive pattern [107,108]. cGVHD is a risk factor, along with drug toxicity, radiation, HLA mismatch, donor-recipient sex mismatch, and use of peripheral blood grafts [108–110]. The diagnoses of IPS, COP, and BOS can be confirmed through lung biopsy; however, less invasive means are typically sufficient. IPS and COP are diagnoses of exclusion and typically require bronchoalveolar lavage to rule out infection.
CARDIAC AND VASCULAR COMPLICATIONS
Cardiovascular complications that occur frequently and contribute to late mortality include hypertension (see Renal and Urinary Complications), dyslipidemia, congestive heart failure, arrhythmias, valvular heart disease, premature coronary artery disease, stroke (see Neurologic and Cognitive Complications), CHIP (see Hematopoietic Complications), and peripheral vascular disease (Table 5, Supplementary Table S6) [17,22,111–120]. Metabolic syndrome (MetS) includes parameters that together increase the risk for diabetes and cardiovascular disease and is associated with increased all-cause mortality. The prevalence of MetS among HCT survivors is 31% to 53%, higher than that seen in background populations [121–123]. Diagnostic criteria include the presence of visceral obesity, elevated blood pressure, hyperglycemia or insulin resistance, and high triglyceride or low high-density lipoprotein levels [124].
Table 5.
Cardiac and Vascular Complications
| Recommendation | Grade | Ref | Comments |
|---|---|---|---|
| • Evaluate cardiovascular risk on personal/family history, lifestyle, autologous vs allogeneic HCT, cumulative anthracycline dose, history of chest radiotherapy, TBI, chronic CNI use, sirolimus, or glucocorticoids. Further surveillance, prevention and treatment should be tailored according to those individual risks | 2A | [379,380] | • Healthy lifestyle is advised: normal weight, eating fruits and vegetables, tobacco abstinence, frequent physical activity; a minimum standard would be to follow USPTF and NHLBI general population guidelines. |
| • Measurement of blood pressure, weight, and BMI at each survivorship visit | 2A | ||
| • For patients with or at very high risk for cardiovascular disease, consultation with a cardiologist • Patients with abnormal imaging studies or concerning symptoms should be referred for cardiology consultation |
2A | • Preferably familiar in late effects of cancer and HCT | |
| • Start lipid assessment for adults at 6 months post-HCT and then annually if low risk for cardiovascular disease; screen high-risk patients or on glucocorticoids, CNI or sirolimus, every 3-6 months | 2A | • Pediatric survivors: less frequent monitoring reasonable | |
| • Start HbA1c screening for insulin resistance/diabetes at 3-6 months post-HCT, then annually if low risk; high risk: every 6 months | 2A | • Pediatric survivors: less frequent monitoring reasonable | |
| • Children exposed to CRT and/or TBI, and survivors treated with abdominal radiation and/or TBI are considered high risk for metS |
2A | ||
| • Multimodal weight loss treatment for obese adults | 2A | • With geographically appropriate, population-based definitions for abnormal BMI or abdominal circumference, when available | |
| • HTN management should follow general population guidance | 2A | [381] | |
| • Dyslipidemia management should follow the AHA/ACC recommendations or local guidelines | 2A | [382] | • Consultation with a pharmacist to review potential drug interactions especially if on systemic IST |
| • Cardiomyopathy pediatric survivors: radiation and anthracycline chemotherapy are significant risk factors; serial screening with ECHO and ECG per COG guidelines | 2A | [383,384] | • COG Guidelines (http://survivorshipguidelines.org/) • Pre-HCT chemotherapy, HCT condition and clinical course should all be included in assessment of risk |
| • Cardiomyopathy adult survivors: For those receiving anthracyclines, ECHO may be considered within a year of therapy completion for those with high cumulative anthracycline exposure (≥250 mg/m2), or those with lower exposure and additional heart failure risk factors. • Adults who never received anthracyclines ECHO and ECG may not be routinely required, however a low threshold to request these studies based on shared decision making in high-risk groups |
2A | [383,385] | • Ongoing surveillance for adults should be based on individual risk factors |
| • Hurler Syndrome: post-HCT cardiopulmonary assessment | 2A | • Valvular dysplasia, regurgitation, stenosis, and progression of pre-existing pulmonary disease may worsen | |
| • Amyloidosis: close monitoring of cardiac function longer-term | 2A | • Cardiac issues may persist long-term |
AHA/ACC, American Heart Association/American College of Cardiology; BMI, body mass index; CHIP, clonal hematopoiesis of indeterminate pathology; COG, Children’s Oncology Group; CRT, cranial radiation; ECHO, echocardiogram; ECG, electrocardiogram; HTN, hypertension; MetS, metabolic syndrome; NHLBI, National Heart, Lung, and Blood Institute; USPTF, United States Preventive Service Task Force.
Doxorubicin equivalent: daunorubicin, .5; epirubicin, .67; idarubicin, 5; mitoxantrone, 10(may consider 4:1). [383]
Allogeneic HCT recipients have higher rates of abdominal obesity, lipid disorders, and impaired glucose metabolism compared with autologous HCT recipients, possibly related to the use of glucocorticoids, sirolimus, or calcineurin inhibitors (CNIs); alloreactivity; or cranial radiation or TBI [122,125–131]. TBI has been associated with hyperglycemia, diabetes, and dyslipidemia, and pancreatic irradiation can lead to diabetes; GVHD also has been associated with hypertension [129,132–134]. Ischemic events are more frequent after allogeneic HCT than after autologous HCT [135]. Hypertension, diabetes, dyslipidemia, smoking, sedentarism, and obesity have been identified as important additive risk factors [115,135,136]. Cardiomyopathy and heart failure are strongly related to anthracycline exposure (particularly at cumulative doses ≥250 mg/m2), hypertension, history of chest irradiation, diabetes, and age, whereas data on the associations with TBI and conditioning intensity are conflicting [115,117,137]. Because genetic polymorphisms play a role in anthracycline-related cardiomyopathy, there is no clear “safe” dose of anthracyclines [138]. It is important to note that the incidence of cardiovascular events increases with greater time since HCT [135], and the presence or absence of cardiovascular disease or echocardiographic findings soon after HCT does not necessarily predict the risk of long-term cardiac toxicities.
GASTROINTESTINAL COMPLICATIONS
Long-term gastrointestinal complications of HCT involve luminal and solid organs (Table 6, Supplementary Table S7). cGVHD of the gastrointestinal tract may lead to dysphagia, esophageal webs, strictures, and stenosis [139]. Previous radiation therapy (eg, mediastinal for Hodgkin lymphoma) also may increase the risk for esophageal strictures [140]. Esophageal cGVHD and/or targeted radiation or TBI are risk factors for esophageal cancer (see Subsequent Malignant Neoplasms) [95,140,141]. Likewise, luminal strictures may occur in patients with a history of severe gastrointestinal GVHD, abdominal surgery, or abdominal radiation and may be considered in the differential diagnosis of intermittent abdominal pain or small bowel obstruction [142]. Abdominopelvic radiation also increases the risk for colon cancer in childhood cancer survivors (see Subsequent Malignant Neoplasms) [143–145].
Table 6.
Gastrointestinal, Renal, and Urinary Complications
| Recommendation | Grade | Ref | Comments |
|---|---|---|---|
| • Elicit symptoms of GI cGVHD at follow-up visits. | 2A | • Positive review of systems should warrant further workup. | |
| • Check total bilirubin, alkaline phosphatase, and ALT at least every 1-2 months during the first year; then at least yearly in allogeneic HCT recipients without risk factors for liver disorders. | 2A | • Patients with chronic hepatitis, or those tapering IST for cGVHD typically require more frequent monitoring. | |
| • DKC: ongoing liver function evaluation and referral to a hepatologist if abnormalities noted. | 2A | ||
| • HBV antiviral prophylaxis for patients with chronic HBV regardless of HBV DNA levels and continue ≥1 year after withdrawal of IST. • Monitor patients with chronic HBV infection at least every 2 months with HBV DNA. |
2A | [151,386] | • Monthly monitoring of HBV DNA and ALT should be done after the withdrawal of antiviral treatment. • For patients with chronic HBV infection, monitoring of HBV DNA should be lifelong. |
| • Patients with resolved HBV infection who received allogeneic HCT, HBV DNA (monitoring at least every 2 months) guided preemptive antiviral therapy. | 2A | [387,388] | • Consider prophylactic anti-HBV therapy for patients at centers without resources to perform HBV DNA monitoring. • Continue monitoring of HBV DNA or prophylactic anti-HBV therapy for ≥3 years after discontinuation of IST. |
| • Antiviral prophylaxis for those receiving grafts from donors with chronic HBV infection. • Preemptive approach (based on viral monitoring) in those receiving grafts from donors with resolved HBV infection. |
2B | ||
| • Offer antiviral therapy if available (and not contraindicated) to HCV-infected survivors. • Evaluate for progressive liver disease every 6-12 months with bilirubin, albumin, PT/INR, and CBC. |
2A | [389] | • In general, refer to a hepatologist for counseling, monitoring, and treatment considerations. • Evaluate and counsel for fibrosis/cirrhosis risk factors (obesity, ethanol, medications, hepatotoxic herbal supplements). |
| • In chronic HCV infection, routine monitoring of quantitative serum HCV RNA not recommended except at baseline, or if unexplained serum ALT elevation, or during HCV antiviral therapy. | 2A | [152,389] | |
| • Monitor patients with cirrhosis for esophageal varices, hepatocellular carcinoma, and other sequelae with an experienced hepatologist. | 2A | [390] | • Screening for HCC in HCT recipients with cirrhosis may follow general guidelines available from the AASLD. • Liver transplantation may be considered in any HCT survivor with hepatic decompensation or early HCC. |
| • Evaluate renal function with UA, urine protein-to-Cr ratio, BUN, and Cr at 6 months, 1 year, and ≥ yearly thereafter | 2A | • MM and amyloidosis: renal function should be monitored more frequently. | |
| • For patients with progressive CKD, avoid nephrotoxins and refer to a nephrologist early. | 2A | ||
| • Monitor blood pressure at every clinic visit; persistent hypertension should prompt intervention and/or referral. | 2A | [112] | • Lifestyle modification including weight reduction, dietary sodium restriction, regular physical activity generally first interventional step, followed by antihypertensive medications. |
AASLD, American Association for the Study of Liver Diseases; ALT, alanine aminotransferase; BUN, blood urea nitrogen; Cr, creatinine; GI, gastrointestinal; HCC, hepatocellular carcinoma; PT/INR, prothrombin time/international normalized ratio; UA, urinalysis.
Hepatic complications may be multifactorial and potentially associated with GVHD, infections, medication, underlying acquired or genetic liver disease, and iron overload (see Hematopoietic Complications). Focal nodular hyperplasia is a common incidental radiologic finding that may be associated with oral contraceptive use, younger age at HCT, and abdominal radiation and occurs frequently in children with neuroblastoma [146–149]. Although malignant transformation is uncommon [147], consultation with a hepatologist may be warranted in cases with lesion growth or diagnostic uncertainty [149]. The prevalence of chronic hepatitis B virus (HBV) infection varies widely depending on patient age and geographic location. HBV antibody titers might not be detectible owing to immunosuppression and should not be relied on entirely. Pre-HCT chronic HBV infection (surface antigen-positive) or resolved HBV infection (core antibody-positive but surface antigen-negative) may result in fulminant post-HCT hepatitis [150,151]. Survivors with chronic HBV infection need regular monitoring to assess viral load, liver status, and need for antiviral therapy and are usually referred to a hepatologist. Hepatitis C virus (HCV) infection usually results in chronic hepatitis, presenting as asymptomatic alanine aminotransferase (ALT) elevation at 2 to 4 months post-HCT when immunosuppressive therapy (IST) is tapered. Chronic HCV infection may cause liver-related mortality only rarely in the first 10 years but is the leading cause of post-HCT cirrhosis [112,152,153].
Although uncommon, pancreatic complications are related mainly to biliary stone passage and rarely to tacrolimus-associated pancreatic damage [154]. Pancreatic exocrine insufficiency occasionally presents with steatorrhea and weight loss despite adequate caloric intake. Its pathogenesis is speculative but thought to involve pancreatic atrophy from prior damage, possibly GVHD-associated; response to a trial of enzyme supplementation may be diagnostic [155].
RENAL AND URINARY COMPLICATIONS
Renal and urinary complications after HCT include chronic kidney disease (CKD), transplantation associated-thrombotic microangiopathy (TA-TMA), nephrotic syndrome (NS), and hypertension. CKD can be caused by a number of pre-, peri-, and post-HCT exposures, with risk factors including previous acute kidney injury, GVHD, older age at HCT, baseline renal insufficiency, hypertension, and TBI [22,156]. Most cases of CKD are multifactorial owing to an accumulation of peritransplantation events and/or risk factors (Table 6, Supplementary Table S8). The cumulative incidence of CKD varies from 7% to 48%, and it may develop between 6 months and 10 years post-HCT, with ~4% of cases progressing to end-stage renal disease [156]. A progressive glomerular filtration rate decline is associated with increasingly higher risk for mortality [157]. TA-TMA is a well-recognized complication, but diagnosis is often been delayed and confounded [158–160]. TA-TMA occurs most frequently early post-HCT but may occur late after HCT, often in association with cGVHD [158–161]. Elevated lactate dehydrogenase, rising urine protein-to-creatinine ratio, and hypertension are the earliest markers of TA-TMA and should prompt clinicians to pursue further workup [112,156]. NS is usually characterized by proteinuria, hypoalbuminemia, and/or edema, occurring most often after IST is tapered for GVHD (at 6 to 12 months post-HCT) [17,156]. As many as 70% of patients develop hypertension at <2 years post-HCT [17,156]. Known risk factors include CNI therapy, acute kidney injury, TBI, autologous HCT, obesity, and diabetes [156]. Effective antihypertensive therapy is important for reducing cardiovascular disease risk (see Cardiac and Vascular Complications) and progression of CKD [316].
ENDOCRINE COMPLICATIONS
HCT survivors are at risk of developing growth impairment, gonadal insufficiency and infertility, thyroid dysfunction, and adrenal insufficiency. Growth can be impacted by multiple factors, including treatment exposures and post-HCT complications (Table 7, Supplementary Table S9) [162]. The reported incidence of post-HCT growth hormone deficiency due to hypothalamic-pituitary injuries varies from 20% to 85% [163–166]. Cranial irradiation (particularly ≥18 Gy) and TBI are established risk factors; the final impact on growth depends on age at exposure, patient sex, and dose of and time since radiation therapy [163,167–172]. Nutritional deficiencies also may impact growth and development. The prevalence of gonadal dysfunction exceeds 90% in some studies and can manifest as delayed pubertal development or otherwise as gonadal insufficiency and infertility (see Sexual Health, Fertility, and Pregnancy) [65]. If untreated, it may lead to sexual dysfunction, low bone mineral density, cardiovascular disease, and poor QoL [173]. TBI, cranial or gonadal irradiation, alkylating agents, and platinum chemotherapy are risk factors; age at exposure also may impact the risk. Thyroid dysfunction is the most common post-HCT endocrinopathy, with reported prevalence ranging from 10% to 47% [174–177]. Hypothyroidism is diagnosed at a median of 4 years post-HCT, although the risk persists for longer [175]. Risk factors for thyroid dysfunction are younger age, head and neck radiation, high-dose TBI, busulfan and cyclophosphamide conditioning, and prolonged cGVHD [175,176,178–180]. Primary adrenal insufficiency is uncommon; most adrenal insufficiency is secondary owing to prolonged glucocorticoid treatment, which suppresses the hypothalamic-pituitary-adrenal axis [181].
Table 7.
Endocrine Complications
| Recommendation | Grade | Ref | Comments |
|---|---|---|---|
| • In children, height, weight, and body mass index should be monitored. • Patients with suspected growth velocity abnormality should be evaluated by a pediatric endocrinologist. |
2A | [391] | • Males without signs of puberty by age 14 years or with failure of pubertal progression or abnormal growth velocity: early morning testosterone, FSH, and LH levels and/or endocrinology consultation. • Females without signs of puberty by age 13 years or with pubertal progression failure, abnormal menstrual patterns, or menopausal symptoms: FSH and estradiol levels and/or endocrinology/gynecology consultation. |
| • Monitor children for onset and progression of puberty with annual Tanner staging until sexually mature. | 2A | • Monitoring frequency should increase as survivors approach and undergo puberty, or if puberty appears delayed. | |
| • Assessment of menarche/menstrual history and menopausal symptoms at least annually. | 2A | ||
| • Adult survivors should have gonadal assessment at least at 1 year post-HCT. • Gonadal dysfunction should be assessed by appropriate subspecialties for potential HRT. |
2A | • Subsequent frequency according to clinical need. | |
| • Serum TSH and free T4 levels should be checked at 1 year post-HCT or sooner in case of symptoms and annually thereafter. | 2A | • Patients with exposure to CNS radiation are at risk for central hypothyroidism, and as such TSH alone is unreliable; hypothyroidism can be identified by a low free T4 plus low TSH with a history of hypothalamic-pituitary insult. | |
| • Patients on long-term systemic glucocorticoids may benefit from ACTH stimulation testing during or after glucocorticoid withdrawal, particularly if symptoms of adrenal insufficiency develop. | 2A | • Patients on topical and inhaled steroids also are at risk for adrenal insufficiency. • Patients should carry notification of adrenal insufficiency to alert emergency medical providers. |
SEXUAL HEALTH, FERTILITY, AND PREGNANCY
Sexual health, fertility, and pregnancy concerns of HCT survivors are summarized in Table 8 and Supplementary Table S10. Approximately one-third of survivors report the inability to perform sexually, inability to derive pleasure from sex, and/or little or no interest in sex [182,183]. Women are more likely than men to report being sexually inactive in the preceding year (39% versus 27%) and among those sexually active, to report low sexual function (64% versus 32%) [184]. Factors associated with being sexually inactive include older age, <4 years of college education, low clinical performance status, and not being in a committed relationship. Additional factors for men include nonmyeloablative conditioning and not being employed or in school. Lower sexual function also has been associated with TBI in men and cGVHD in both men and women [182–187].
Table 8.
Sexual Health, Fertility and Pregnancy
| Recommendation | Grade | Ref | Comments |
|---|---|---|---|
| • Discuss sexual function with patients at 3-6 months post-HCT and annually thereafter. | 2A | [393–396] | • Potentially modifiable symptoms: genital cGVHD, ED, vaginal dryness/dyspareunia, relationship quality, treatment related distress, depression. • Screening/managing sexual dysfunction includes individualized multimodal approach addressing medical and psychosocial (including partner) needs. |
| • Timely assessments of hypogonadism and/or urogenital GVHD. | 2A | [393] | • GYN/GU referrals to address reversible risk factors relevant to sexual dysfunction. • POI is treated with HRT if not otherwise contraindicated. • Refer women with vaginal dryness ± cGVHD to GYN/GU; may benefit from lubricants, topical estrogens, dilator therapies. • Consider ED therapies, testosterone replacement in males. |
| • Patients desiring pregnancy should meet with a fertility specialist to best understand current fertility potential and what methods (ie, IVF, donor oocyte, donor sperm) may be considered if applicable. • Semen analysis or assessment of ovarian function for those contemplating future parenthood when age appropriate. |
2A | [393] | • Reassess fertility potential at intervals; partial or full fertility potential may recover for some patients. |
| • Contraception advised if fertility potential unknown, wishing to avoid parenthood. • Counseling regarding safer sex practices/contraception should be discussed, even if infertile, to prevent sexually transmitted infections. |
2A | ||
| • Women with gonadal recovery should be advised about the risks of POI. | 2A | ||
| • Pregnant patients should be followed by MFM (high-risk obstetrics). | 2A | [393] | • May require review by an anesthetist before delivery. |
| • Pregnant women with systolic dysfunction/significant cardiac risk factors to be followed by cardiologist with expertise in cardiac late effects. | 2A | [196,393] | |
| • Counsel women who received radiation to the uterus (including TBI) and desire pregnancy on risk of uterine factor infertility, other pregnancy risks. | 2A | ||
| • Offer genetic counseling before pregnancy to those undergoing HCT for genetic disorder or cancer predisposition syndrome | 2A |
HCT is associated with infertility owing to pre-transplantation and transplantation-related treatment exposures and late effects [188,189]. Female sex, pre-HCT cytotoxic therapy, myeloablative conditioning, and germ cell tumor diagnosis have been associated with lower fertility post-HCT [190]. Underlying conditions also may impact fertility (eg, Fanconi anemia). In females, the degree of ovarian damage is related to the dose and type of exposure (eg, myeloablative conditioning, radiation), as well as to ovarian reserve, which is dependent on age and previous treatment. The use of alkylating agents has the highest age-adjusted odds ratio of ovarian failure [189,190]. The TBI dose that is potentially sterilizing appears to decrease with increasing age [190,191]. In males, chemoradiotherapy can impair spermatogenesis, but the testosterone level generally remains normal because Leydig cells are relatively resistant. Lower testosterone can be seen when affected by GVHD, particularly in the setting of chronic glucocorticoid exposure [192]. For women, embryo and oocyte cryopreservation remains the preferred method of fertility preservation. Ovarian tissue cryopreservation is becoming increasingly feasible and remains the sole option for prepubertal patients [193]. Despite success in animal models, the clinical value of gonadotropin-releasing hormone agonists to preserve ovarian function during chemotherapy remains uncertain [194]. Sperm cryopreservation is an established fertility preservation option for postpubertal males. In prepubertal males, the sole option is testicular tissue cryopreservation; although animal models are encouraging, to date there have been no reports of reimplanted testicular tissue leading to human live births [189].
Uterine radiotherapy exposures may lead to adverse reproductive outcomes [195]. Increased rates of infertility, miscarriage, preterm labor, intrauterine growth restriction, and low birth weight have been described, particularly when conception occurred within 1 year of radiotherapy [189,196]. However, in women who have not received radiation, the miscarriage rate is comparable to that of the background population without a significant increase in congenital malformations or genetic abnormalities [197,198]. Similarly, reported pregnancies and deliveries from partners of male recipients usually have been uncomplicated [199].
MUSCLE AND CONNECTIVE TISSUE COMPLICATIONS
Muscle and connective tissue complications after HCT are often associated with cGVHD and its treatment and include glucocorticoid-induced myopathy, fasciitis/deep sclerosis, polymyositis, and myasthenia gravis (Table 9, Supplementary Table S11) [200–206]. Steroid myopathy typically presents with proximal muscle weakness, difficulty rising from a squatting position, and atrophy of these muscle groups. Although an improvement in strength may occur by 2 to 3 weeks after steroid reduction, complete resolution can take longer. The use of fluorinated glucocorticoids (eg, dexamethasone) is associated with a higher risk of myopathy compared with nonfluorinated glucocorticoids (eg, prednisolone) [207]. Although there is significant variability in individual susceptibility to myopathy, ≤10 mg/day of prednisone or equivalent is unlikely to result in myopathy, but ≥40 mg/day for ≥1 month usually causes weakness [207].
Table 9.
Musculoskeletal, Connective Tissue, Skeletal, and Dermatologic Complications
| Recommendation | Grade | Ref | Comments |
|---|---|---|---|
| • Routinely evaluate patients on glucocorticoid treatment for glucocorticoid-induced myopathies • Patients with/at risk for steroid myopathy should engage in physical activity and physical therapy |
2A | • Observe patient rising from a squatting position • Physiatry referral may be helpful. • Low resistance exercise to prevent/slow loss of muscle mass |
|
| • cGVHD-associated polymyositis, statin toxicity, or myasthenia gravis should be included in differential diagnosis of myalgia/weakness if persistent or progressive, | 2A | • CPK, aldolase, anti-acetylcholine antibodies are a reasonable next step. If negative, muscle MRI, EMG or muscle biopsy may be considered | |
| • Encourage patients with cGVHD to perform self-assessment of ROM and perform ROM evaluation at each clinic visit | 2A | • Ideally with medical photos for subsequent comparison | |
| • Standard risk patients: DEXA at 1-year post-HCT. If abnormal, repeat every 1-2 years, sooner if ongoing risks, or response assessment. • High risk patients pre-HCT, or post-HCT high-dose glucocorticoids: Obtain DEXA at 3 months post-HCT. |
2B | [211,398–400] | • <5 years old, lumbar spine BMD may be measured. DEXA hip measurements less reliable for age <13 • FRAX and vertebral fracture assessment (VFA) may help evaluation/management |
| • Optimize Ca and vitamin D intake through diet, supplementation. • Recommend regular, weight-bearing exercise. |
2A | • Vitamin D may be measured regularly in those at deficiency risk. | |
| • Consider bisphosphonates in high-risk patients, significant abnormalities on DEXA or FRAX assessments, or fragility fractures. | 2A | [211,401] | • Bisphosphonate choice made with consideration of the patient’s presentation, renal function, and respective adverse events. |
| • For patients with MM, supportive management with use of bisphosphonates for at least 2 years. | 2A | [211,402] | • Such as zoledronic acid and pamidronate |
| • Hormone replacement therapy should be discussed for patients with hypogonadism if age-appropriate, and not otherwise contraindicated (see Endocrine complications). | 2A | ||
| • Routine imaging screening for asymptomatic AVN not indicated. • Maintain a high index of suspicion for AVN in patients with prior AVN, radiation exposure or prolonged glucocorticoids. Those with joint symptoms should be evaluated promptly |
2A | [211] | • Symptomatic patients: non-contrast MRI is the most sensitive way to confirm and stage AVN; Once diagnosis of AVN prompt referral to orthopedic specialist recommended. |
| • Following HCT for Hurler Syndrome, neurologic screening for spinal canal narrowing and carpal tunnel syndrome should be considered | 2A | [403,404] | |
| • Inform patients about risk of dermatological complications, particularly related to cGVHD, medications, and radiation | 2B | • Advise to seek medical attention for non-healing skin lesions, skin tightening or other changes. | |
| • Undergo regular skin self-examination; refer to a dermatologist for further evaluation of suspicious lesions. • Frequency/extent of examination tailored to individual risk factors: prior or present GVHD, sun exposure and radiation history, voriconazole exposure, family history, and history of skin cancer |
2A | [57,80,232] | • Minimum of every 6-12 months for malignancy screening and general examination, including for cutaneous cGVHD based on NIH-criteria. • Regular skin exam involves exposure of all body areas and includes manual palpation to detect sclerosis |
| • Advise to avoid direct sun exposure without appropriate protection: proper clothing, hats, applying UVA/UVB sunscreen to exposed areas | 2A | • Particularly important for patients on immunosuppression, voriconazole, with a history of TBI or skin cGVHD |
Abbreviations: AVN: Avascular Necrosis, BMD: Bone Mineral Density, Ca: Calcium, CPK: Creatine Phosphokinase, DEXA: Dual Energy X-ray Absorptiometry, EMG: Electromyography, FRAX: Fracture Risk Assessment Tool, GVHD: Graft versus Host Disease, MRI: Magnetic Resonance Imaging, MM: Multiple Myeloma, ROM: range of motion, TBI: Total Body Irradiation, UVA: Ultraviolet A, UVB: Ultraviolet B
Fasciitis and polymyositis are cGVHD manifestations [206,208,209]. Fasciitis may cause tightness or restricted range of motion on a photographic range of motion scale [208], with various combinations of visibly tight tendons in volar forearms/palms and palpable deep tissue sclerosis with overlying hyperpigmentation and “groove” signs. Along with cGVHD treatment, patients with fasciitis may benefit from a multidisciplinary rehabilitation program to control edema and preserve range of motion. Polymyositis usually presents with moderate to severe proximal muscle weakness and myalgia [202]. Myasthenia gravis is a rare cGVHD complication that may be due to donor-derived antibodies against recipient acetylcholine receptors and manifests similar to classical myasthenia gravis, with most cases occurring >2 years post-HCT [200,210].
SKELETAL COMPLICATIONS
Skeletal complications following HCT include abnormal bone density and avascular necrosis (AVN). Low bone mineral density (BMD) or osteopenia is a common complication that if untreated may lead to osteoporosis and increased risk of bone fragility fractures (Table 9, Supplementary Table S12). The prevalence of low BMD is up to 75% among allogeneic HCT survivors and 65% in autologous HCT survivors [211]. Low BMD can be seen as early as 1 month post-HCT and often persists beyond 3 years post-transplantation [212–219]. Patient-related risk factors include extremes of age at HCT, female sex, low body weight or body mass index, inadequate calcium or vitamin D intake, physical inactivity, renal dysfunction, and hypogonadism. Disease-related risk factors include myeloma, hemophagocytic lymphohistiocytosis, hemoglobinopathies, and pre-HCT chemotherapy exposures [220]. Finally, HCT-related risk factors include TBI or craniospinal irradiation, GVHD, and prolonged IST including CNIs and glucocorticoids [212–224].
The cumulative incidence of AVN is 3% to 10% at 5 years post-HCT [211,225], and time of onset may range from 6 months to 10 years post-HCT [225]. Patients with a history of acute lymphoblastic leukemia or sickle cell disease may have AVN pre-HCT [226]. AVN most commonly affects the femoral head, although knees, ankles, elbows, vertebrae, and multiple concurrent joints often may be implicated [227]. The incidence of AVN is greater in females and with more intensive conditioning regimens (especially TBI), moderate to severe cGVHD, prior aGVHD, higher glucocorticoid exposures, and adolescents and young adults (AYA), in whom rapid bone growth occurs [224,226–231].
DERMATOLOGIC COMPLICATIONS
Cutaneous complications may occur in up to 70% of survivors [22] and is most commonly due to cGVHD but also may result from infections, subsequent neoplasms, or anti-infective and immunosuppressive drugs (Table 9, Supplementary Table S13). Excellent overviews of diagnosis and management of cutaneous cGVHD are available elsewhere [57,80,232–234], and the risk of skin cancers is reviewed below (see Subsequent Malignant Neoplasms). Health care providers should recognize potential cutaneous side effects of glucocorticoids (eg, easy bruising, loss of skin integrity) and cyclosporine (eg, hirsutism, malignancy); they should monitor for cutaneous atrophy in survivors on high-potency topical glucocorticoids and recommend low-potency glucocorticoids (eg, hydrocortisone 1% to 2.5%) only in high-risk areas, such as the face [80,233,234].
NEUROLOGIC AND COGNITIVE COMPLICATIONS
Late neurologic dysfunction after HCT may affect the central nervous system (CNS) and peripheral nervous system and are more frequent after allogeneic HCT (Table 10, Supplementary Table S14) [235–237]. Potential causes include infection or immunosuppression (with CNIs), neurotoxic chemotherapy (eg, methotrexate, cytarabine, busulfan, thiotepa) and other medications, TA-TMA, cranial radiation or TBI, radiation-induced vasculitis, underlying disease (eg, cerebrovascular disease, sickle cell disease, adenosine deaminase deficiency), CNS relapse of the original disease, PTLD, subsequent neoplasms (local effects or paraneoplastic syndromes) and, finally by exclusion, cGVHD [238].
Table 10.
Neurological, Cognitive Complications, Psychosocial Health, and Quality of Life
| Recommendation | Grade | Ref | Comments |
|---|---|---|---|
| • Clinical assessment for symptoms or signs of peripheral and CNS dysfunction at 6-12 months after HCT and at least yearly thereafter | 2A | • Earlier and more frequent evaluation to be considered in high-risk patients. • Careful history/examination/review of systems/medication history and assessment of time of onset of neurological signs and symptoms during survivorship visits. |
|
| • Patients with exposures to head and neck irradiation, platinum chemotherapy, aminoglycosides, or an inherited condition associated with hearing disability, audiologic evaluation within 1st year post-HCT. • Council patients about hearing loss prevention and to seek assessment for new symptoms. |
2A | [408] | • Follow-up evaluations as clinically warranted. • Hearing loss may be present in ADA deficiency prior to HCT and require developmental support, regular otolaryngology, and audiologicassessment post-HCT |
| • Perform Childhood cognitive developmental milestones ≥annually. • Neurocognitive testing and educational/vocational progress assessment in pediatric survivors |
2A | • Strongly consider before returning to work/school, major changes in school (ie, moving from elementary to middle school), or changes in school performance | |
| • Query adults annually for cognitive function changes which may be subtle. • Neuropsychological testing and imaging should be considered in cases of reported functional impairment. |
2A | [302] | • Inquire about difficulties multitasking, attention, remembering things or whether thinking feels slow. • Exclude reversible causes of cognitive decline: depression, fatigue, insomnia, or medication toxicity. • SCD: offer neurocognitive testing, if available. |
| • Perform CGA pre-HCT and at 6 months and 1 year post-HCT. | • To identify patients more likely to benefit from enhanced toxicity risk prediction and aid treatment decision making. | ||
| • At each survivorship visit, review current symptom patterns, distress, medications, comorbidities, and physical activity. | 2A | • Minimum: days +100, +180, and +365, then annually. | |
| • Discuss medication adherence and potential at each visit. | 2A | ||
| • Set incremental goals for healthy diet, activity, weight management. • Encourage adequate sleep and age-appropriate preventative measures. • Assess those with significant physical, visual, or auditory disabilities for appropriate support services and medical equipment needs. |
2A | • ie, vegetables, fruits, whole grains, low in excess sugars, dried foods, red/processed meat, and dietary supplements. | |
| • General screening of patient mental health, with standardized questionnaires (eg, NCCN distress thermometer, survivorship questionnaire). | 2A | [301,302] | • No gold standard for screening mental health after HCT; take care to not overburden patients with PRO tools. • To guide clinical investigations or behavioral or psychological support, particularly if multiple somatic complaints, new GVHD, major life events, or treatment changes. |
| • Regularly inquire to level of spousal/caregiver psychological adjustment, family functioning, educational, vocational activities, and financial toxicity. | 2A | • Appropriate referral if necessary. • Offer peer support and return to work/school programs |
|
| • For AYA, provide transition of care education and plans. | 2A |
Survivors of TBI or cranial irradiation are at increased risk for secondary brain tumors (see Subsequent Malignant Neoplasms). Radiation, cGVHD, and glucocorticoid treatment are major risk factors for stroke [239–243]. For asymptomatic recipients of CNS radiation (particularly at higher doses), brain magnetic resonance imaging (MRI)/magnetic resonance angiography (MRA) screening for vasculitis may be considered during shared decision making but consensus on its utility is lacking [244]. Likewise, in recipients of high-dose neck radiation, carotid ultrasound screening can be considered during shared decision making.
Hearing loss secondary to radiation, platinum agents, and other drugs or complications may develop and potentially lead to learning impairment [86,245,246]. Adenosine deaminase deficiency, osteopetrosis, lysosomal storage diseases, and leukodystrophies are also associated with hearing disabilities.
Encephalopathy, aphasia, hemiparesis, seizures, apraxia, and tremors can occur in patients who have received intrathecal chemotherapy, cranial radiation, monoclonal antibodies, or tyrosine kinase inhibitors. Progressive multifocal leukoencephalopathy (PML) is caused by JC polyomavirus and has been associated with alemtuzumab, ATG, or rituximab therapy [247–252]. Opportunistic bacterial, toxoplasmosis, and viral infections (eg CMV, HHV-6) can lead to serious morbidity [253,254]. Neurologic complications may impact cognitive function, affecting memory, concentration, speech and language skills, spatial abilities, and executive function [255–258]. Major risk factors include female sex, younger age at HCT, extensive cGVHD, use of narcotics, glucocorticoids, antidepressants, sedatives, and TBI in children [12,257]. Other potential risk factors include blinatumomab, intrathecal chemotherapy, posterior reversible encephalopathy syndrome, TA-TMA, and history of immune effector cell-associated neurotoxicity syndrome.
In addition to CNS complications, survivors less commonly develop immune mediated manifestations of peripheral nervous system, such as polymyositis, myasthenia gravis (see muscle and connective tissue complications) and chronic inflammatory demyelinating polyneuropathy, usually developing in association with tapering IST [259–264]. Guillain-Barre-like syndrome with peripheral neuropathy and chronic demyelinating polyneuropathy related to GVHD have also been reported [265–267].
PSYCHOSOCIAL HEALTH AND QUALITY OF LIFE
Understanding patient perspectives on health related QoL is an integral part of survivorship care (Table 10, Supplementary Table S15). Physical function limitations can adversely affect a survivor’s ability to carry out daily tasks [12]. Approximately 10% of survivors report somatic distress >10 years post-HCT, with cGVHD, glucocorticoid exposure, and depression being risk-factors [12,268,269]. As many as 68% of patients report fatigue which is one of the most consistent symptoms negatively impacting QoL [270]. Risk factors for fatigue include female gender, cGVHD, younger age, and chronic pain [12,271]. Similarly, up to half of survivors report sleep disturbance that does not seem to improve over time, and has been associated with female gender, older age, divorced status, unemployment, depression, distress, and autologous HCT [12]. Pain is reported among ~25% of survivors, often associated with musculoskeletal symptoms [12,237,269].
Anxiety and post-traumatic stress disorder (PTSD) affect 5-10% of long-term survivors [268,272], whereas depression seems to gradually increase over time, affecting 10-30% [5,273]. PTSD has been associated with GVHD and prolonged hospitalizations [272]. Anxiety has been associated with female gender, poor reported health status, lower household income, lower education, prednisone exposure and cGVHD [268,273]. Depression is more frequent in male patients, those with poor functional status, lower household income, less education, TBI, prednisone exposure and cGVHD [268,273,274].
While lower social function scores have been reported in survivors compared to controls, others have reported excellent support from family and friends [255,274,275]. 60-80% of survivors are able to resume social roles, such as returning to work and school, but up to one third of survivors report worrying about being able to maintain employment [274,276–284]. Financial burden of HCT is a major concern for >20% of North American survivors and is relevant in other locations as well [255,285–288]. AYAs seem to report lower social well-being and more difficulties establishing themselves in the labor market [281,287,289]. Pre-HCT lack of employment, less education, medical disability, late-effects, fatigue, pain, mental distress, GVHD, relapse and having a manual job have been associated with lower chances of post-HCT employment [279,281–284,287,289–295]. Financial difficulties are associated with worse physical and mental functioning, adverse medical outcome, and increased severity of GVHD [268,292,296–298].
There is no standard way of addressing perceived health status in HCT survivors, but many standardized patient-reported outcome questionnaires have been utilized, with accumulating evidence supporting the NIH-supported Patient-Reported Outcomes Measurement Information System (PROMIS) [299,300]. Additionally, though not specifically validated in HCT, the NCCN distress thermometer can be used to triage patient concerns [301,302]. For fatigue, NCCN survivorship guidelines may be helpful [302]. Sleep disorders can be investigated by detailed history and assessment of symptoms and potential interventions include review of medications, reviewing sleep/wake timing, physical activity, caffeine and other substance use and providing coping strategies such as relaxation and meditation techniques. For pain, appropriate mitigation strategies include non-pharmacologic interventions (eg, massage, physical therapy, acupuncture) and/or analgesics, with nonopiates prioritized [302]. Family members (including siblings) and informal caregivers can be even more affected by mental health issues than patients themselves, and their own QoL cannot be inferred from the patients’ results; referral to appropriate providers may be indicated [303–306].
It is essential that survivors be able to rely on their standard support system and also recognize they may get additional help from interacting with survivors with similar experiences. Online peer mentor programs are available (Appendix 2). Return to work programs can be instrumental, but practices vary widely (Appendix 3) [307,308]. Patients should be encouraged to evaluate their working/educational goals and identify barriers, working with human resources through their employer, occupational/vocational therapists, social workers, and financial counselors [302].
SUBSEQUENT MALIGNANT NEOPLASMS
HCT survivors have a 4- to 11-fold increased risk of developing subsequent malignant neoplasms (SMNs) compared with the general population [93,309]. Among allogeneic HCT recipients, the incidence of SMNs increases from 3.5% at 10 years to 12.8% at 15 years post-HCT [91,94,309]. SMNs can be categorized as hematologic tumors (tMNs, PTLD) or solid tumors (Table 11, Supplementary Table S16).
Table 11.
Subsequent Malignant Neoplasms
| Recommendation | Grade | Ref | Comments |
|---|---|---|---|
| • Counsel about SMN risk and encourage recommended screening. | 2A | • Based on treatment exposures, time from exposure, cGVHD history, and other modifying factors. | |
| • Encourage avoidance of high-risk behaviors, unhealthy diet. | 2A | • eg, tobacco and vaping, passive tobacco exposure, alcohol abuse; high-fat/low-fiber diet. | |
| • If risk not otherwise modified by HCT history, screening as regionally indicated and clinically based on other underlying medical, family, and genetic history. | 2A | ||
| • Patients at risk for tMN: annual CBC until at least 10 years post-HCT. | 2B | • Consider more frequent screening in those with greater risk (ie, chemotherapy exposures, age; autologous HCT). • Attention to unexplained cytopenias, macrocytosis, or cellular atypia. |
|
| • Prevention of PTLD includes EBV-DNA screening in high-risk patients, preemptive treatment with rituximab. | 2B | • eg, ATG, alemtuzumab, ex vivo T cell depletion. • Evaluation includes lymph node palpation and review of B symptoms (fever, drenching night sweats, ≥10% weight loss over 6 months). |
|
| • Oral exam should be part of annual survivor exam. • Advise reporting non-healing oral lesions, leukoplakia, localized pain, changes in mucosal color/texture. • HPV vaccination according to country-specific general population recommendations, unless otherwise contraindicated |
2A | [58,94,95,342,409] | • Consider every 6 months screening in patients at high risk for oral cancer (oral cGVHD, tobacco use, FA). • HPV’s role in mucocutaneous/genital cancers post-HCT unclear. • Endoscopic screening for esophageal cancer may be considered in high-risk patients (cGVHD receiving prolonged immunosuppression, symptoms of gastroesophageal reflux, dysphagia). |
| • Cervical cancer screening based on age and risk factors. | 2A | [325] | • FA: annual pap smear, gynecologic screening starting in adolescence. |
| • Pediatric survivors <age 45 years and RT exposed: CRC screening colonoscopy or multitarget stool DNA screening at 5 years post-RT exposure or age 30 years, whichever occurs later. • Adult survivors: as part of shared decision making, consider exposed to abdominal/pelvic RT or TBI who underwent HCT at ≥25 years of age, colonoscopy beginning 5 years post-RT exposure and no later than age 45 years |
2B | [342,410,411] | • Screen patients without RT exposure according to general population guidelines for their geographic region, individual risk factors, and family history. • Screen patients with colon CPS (eg, hereditary nonpolyposis colorectal cancer, FAP, DBA) based on underlying CPS. • Risk of subsequent CRC in those exposed to TBI likely dose-dependent; lower doses may not increase the risk of CRC to level that risk/benefit of early colonoscopy warranted. |
| • Female recipients of TBI or chest RT should begin breast cancer screening with mammogram and breast MRI (if available) at age 25, or 8 years post-RT, whichever occurs later, but no later than age 40. • In high-risk individuals, discussion with appropriate experts on risk reduction strategies (ie, prophylactic mastectomy, prophylactic medical therapies, lifestyle). |
2A | [330–335,412,413,342] | • Female HCT survivors without risk factors should participate in regular annual mammogram/clinical breast exam according to general population guidelines for geographical region and individual risk factors including family history. • Counsel on additional breast cancer risk factors (ie, BRCA1/2, family history). |
| • Patients should have an annual thyroid exam and review of potential symptoms of thyroid cancer. • As part of shared decision making, consider ultrasound screening in patients who received thyroid RT. |
2A | [323,414] | • Routine use of thyroid ultrasound may not provide additional benefit; some groups recommended. • Screen patients with inherited thyroid CPS (eg, multiple endocrine neoplasia, FAP) based on underlying condition. |
| • As part of shared decision making, consider meningioma screening in patients who received CNS RT. | 2B | [338,339,340] | |
| • FA survivors with mutations in BRCA2 (FANCD1) or PALB2 (FANCN) require screening for specific solid cancers. | 2A | [325,415–418] |
The overall incidence of tMNs is estimated to be 4% at 7 years post-HCT, with a median occurrence at 2.5 years post-HCT [310]. Recipients of pre-HCT alkylating agents (particularly etoposide or cyclophosphamide), and possibly post-HCT cyclophosphamide are at higher risk [311,312]. Survivors have a higher risk of developing tMN after autologous HCT, but tMN rarely can arise from donor hematopoiesis in allogeneic HCT recipients [313,314]. Patients who were conditioned with TBI, received ≥3 lines of chemotherapy, were poor stem cell mobilizers, or received lenalidomide maintenance for myeloma may be at higher risk for tMN [315–318]. The cumulative incidence of PTLD is 1% at 10 years after HCT and is associated with greater donor-recipient HLA disparity, T cell depletion, and GVHD [319]. Patients with primary immune deficiency also are at higher risk of developing lymphomas. Recommendations on prevention and treatment of PTLD have been developed by the sixth European Conference on Infections in Leukemia and are described in detail elsewhere [320].
The incidence of solid cancers increases from approximately 2% at 10 years to 3% to 5% at 15 years post-HCT, varying widely based on exposure, family/genetic history, age at HCT, and time since HCT [95,321,322]. Younger age at HCT, TBI, female sex, and cGVHD are risk factors for thyroid cancer in survivors [179,323]. Survivors have a 7- to 16-fold higher risk for oral cancer compared to the general population; this risk is particularly increased in survivors with cGVHD and/or Fanconi anemia [90,91,94,95,324–326]. Genital cancer risk is also increased in recipients of reduced-intensity conditioning and limited field radiation and in patients with cGVHD and/or a diagnosis of Fanconi anemia [89,91,327]. Allogeneic HCT recipients are at an increased risk for gastrointestinal malignancies, with one report citing an standardized incidence ratio in survivors at 5 to 10 years post-HCT of 74.0 for cancer of the esophagus, 46.6 for cancer of the oral cavity, and 2.3 for colon cancer [328]. Patients exposed to TBI are at risk of colorectal cancer, and children exposed to TBI can develop polyps at an early age [144,329]. Patients with inflammatory bowel disease are at very high risk of developing colon cancer, although it remains to be seen whether similar issues occur in patients with gastrointestinal GVHD. Colonoscopy has been shown to be cost-effective in patients who received abdominal radiation exposure [143]. Recipients of chest irradiation (eg, Hodgkin lymphoma) are at increased risk for breast cancer [330,331]. Recipients of TBI without other radiation are also at increased risk [332]. Although rare, breast cancer in male childhood cancer survivors may be related to radiation therapy [333]. Anthracycline exposure, endogenous hormones and hormone replacement, and family history also should be considered when determining a patient’s overall risk [334,335].
The 20-year post-HCT cumulative incidence is 6.5% for basal cell carcinoma and 3.4% for cutaneous squamous cell carcinoma [336]. The risk of melanoma is also significantly increased [337]. Areas of previously irradiated skin are the most vulnerable to developing carcinomas, further exacerbated by a history of excessive sun exposure and chronic skin GVHD, which itself can be triggered or aggravated by sun exposure. The role of IST in precipitating skin cancer is another a concern. Screening and prevention of skin malignancies mimic the guidance offered for skin cGVHD (see Dermatologic Complications).
Survivors also are at higher risk for CNS tumors and sarcoma. Meningioma is the most frequent CNS tumor, although more aggressive histologies may occur [338,339,340]. Heightened awareness for symptoms should be emphasized in patients after cranial irradiation or TBI. Survivors are at risk for secondary bone cancers, with a standardized incidence ratio of 8.5 to 13 [341,342]. Risk factors may include underlying cancer predisposition syndromes (eg, Li-Fraumeni syndrome, Diamond-Blackfan anemia) and radiation therapy. Clinicians should maintain a high level of suspicion in patients who present with relevant symtoms [342].
SPECIAL POPULATIONS
Although there are many commonalities in risk factors and chronic health conditions in all HCT survivors, certain populations are at elevated risk for late effects due to their underlying disease, treatment regimen, or age-related late effects and warrant long-term follow-up with multidisciplinary population-specific teams. Appendix 4 outlines considerations for special populations, including hemoglobinopathies, marrow failure syndromes, inborn errors of immunity, enzymopathies, metabolic and other disorders, autoimmune disorders, myeloma, amyloidosis, infants, AYAs, and older adults (ie, geriatric population). Appendix 5 provides a nonexhaustive list of additional references that may be helpful in managing the late effects of these specific populations, along with specific recommendations for these populations.
MODELS OF SURVIVORSHIP CARE DELIVERY
As survivorship care has become an integral part of cancer treatment, guidelines from the Foundation for the Accreditation of Cellular Therapy and the Joint Accreditation Committee of International Society for Cell and Gene Therapy and European Society for Blood and Marrow Transplantation (FACT-JACIE) mandate the monitoring and treatment of late effects after HCT, including the transition from pediatric care to adult care providers [343]. Survivorship care is being increasingly recognized by patients as a basic need [288,344,345], and evidence for the added value of such practice is emerging. Indeed, recipients of HCT performed at centers with survivorship programs have improved survival [346]. However, at present in the United States, only 45% of programs have an HCT-specific long-term follow-up clinic [347]. Several different models of late effects follow-up have been proposed [4,11,347]; however, barriers to the establishment of survivorship clinics include lack of expertise, logistical challenges, and financial and reimbursement issues [347]. The implementation of programs and specific guidelines remains a challenge, and ensuring that survivors receive the recommended guidance is crucial [348–350].
Patients indicate a preference for holistic care, ideally with continued direct contact with the transplant center, particularly when they have developed GVHD, but this can be challenging when they live remote from their HCT team [288,344,345]. Survivorship care plans have been shown to decrease cancer-related distress and improve mental health in long-term survivors, although they do not exclusively replace comprehensive survivorship care [351]. Models to overcome barriers using telehealth, mobile apps, and wearable devices are currently being tested [352–356]. However, technology use and uptake may be challenging, and patients often value human contact [288,345,357,358]. In summary, a specific optimal survivorship care model has not been determined, and different models continue to evolve based on HCT program and system strengths and abilities.
FUTURE DIRECTIONS
As the transplantation and cellular therapy field continues to evolve and expand, so will the need for survivorship care. The long-term impact of novel small molecule cancer therapies and immunotherapies have not yet been well studied but have mechanisms of action generally distinct from conventional chemotherapy; some have idiosyncratic side effects particularly relevant to specific populations (eg, acute endocrine complications from certain immunotherapies), but long-term impacts are unclear [359]. Multiple chimeric antigen receptor T cell therapies are available, and indications for these and additional cellular therapy products are expanding rapidly. Cellular therapies may be associated with acute and subacute postinfusion complications mostly from altered immune function (eg, cytokine release syndrome, immune effector cell-associated neurotoxicity syndrome) or from the elimination of cells expressing common antigens with the target cells (eg, B cell aplasia, CD19+ cell therapy) [77]. Gene therapies using an autologous HCT platform have moved to late-stage clinical trial testing, with some products now approved by regulatory agencies. Most clinical trial protocols require prolonged follow-up and are typically geared toward monitoring the underlying disease, specific genomic modifications, and surveillance for clonal hematopoiesis/tMN [360,361]. Although these trial-mediated outcomes will provide crucial information for the long-term care of these patients, routine post-HCT care–immune reconstitution and revaccination, monitoring for late-effects of conditioning chemotherapy–remains equally important. Given that many participants in these clinical trials have traveled great distances to enroll, often internationally, ensuring ongoing local follow-up and partnership with the research team is critical. Further, as these therapies become more established it will become increasingly important to provide data and encourage provider awareness of the long-term issues. All these novel approaches are likely to impact the range of late effects in future HCT and cellular therapy survivors, and further investigation is of the utmost importance.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank the following individuals: Dr Shigeru Kusumoto (Department of Hematology and Oncology, Nagoya City University Graduate School of Medical Sciences) for his expert review and commentary of management of HBV; Dr Mehdi Hamadani (Medical College of Wisconsin), Ms Jessica Scott (ASTCT), and Mr Haedyn Smith for their work in reviewing the overall approach and coordinating with the ASTCT guidelines committee; Dr Miguel-Angel Perales (Memorial Sloan Kettering Cancer Center), Dr Corey Cutler (Dana Farber Cancer Center), Dr David Porter (University of Pennsylvania), Dr Brenda Sandmaier (Fred Hutchinson Cancer Center), and Dr Uday Popat (MD Anderson Cancer Center) for their work in reviewing the guidelines with the ASTCT Executive Committee.
Financial disclosure:
This work was supported in part by a grant from the National Center for Advancing Translational Sciences (2KL2TR002547, to S.J.R.) and a grant from the National Cancer Institute (NCI) (R01 CA215134 to K.S.B. and N.S.M.). The CIBMTR is supported primarily by Public Health Service Grant U24CA076518 from the NCI, the National Heart, Lung, and Blood Institute, and the National Institute of Allergy and Infectious Diseases; Grant 75R60222C00011 from the Health Resources and Services Administration, and Awards N00014-21-1-2954 and N00014-23-1-2057 from the Office of Naval Research. Support is also provided by Be the Match Foundation, the Medical College of Wisconsin, the National Marrow Donor Program, Gateway for Cancer Research, Pediatric Transplantation and Cellular Therapy Consortium, and the following commercial entities: AbbVie, Actinium Pharmaceuticals, Adaptimmune, Adaptive Biotechnologies, ADC Therapeutics, Adienne SA, Allogene, AlloVir, Amgen, Angiocrine, Anthem, Astellas Pharma US, Atara Biotherapeutics, BeiGene, bluebird bio, Bristol Myers Squibb, CareDx, CRISPR, CSL Behring, CytoSen Therapeutics, Elevance Health, Eurofins Viracor, Gamida-Cell, GlaxoSmithKline, HistoGenetics, Incyte, Janssen Research & Development, Janssen/Johnson & Johnson, Jasper Therapeutics, Jazz Pharmaceuticals, Karius, Kiadis Pharma, Kite Pharma, Kyowa Kirin, Legend Biotech, Magenta Therapeutics, Mallinckrodt Pharmaceuticals, Medexus Pharma, Merck & Co, Mesoblast, Millennium, Miltenyi Biotec, MorphoSys, Novartis Pharmaceuticals, Omeros, Orca Biosystems, Ossium Health, Pfizer, Pharmacyclics, Pluristem, PPD Development, Regimmune, Sanofi, Sanofi-Aventis US, Sobi, Stemcyte, Takeda Pharmaceuticals, Talaris Therapeutics, Vertex Pharmaceuticals, Vor Biopharma, and Xenikos BV.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Conflict of interest statement:
Y.A. reports lecture fees from Otsuka Pharmaceutical, Chugai Pharmaceutical, Novartis Pharma KK, and AbbVie GK; honoraria from Meiji Seika Pharma; and consultant fees from JCR Pharmaceuticals and Kyowa Kirin. G.G. reports serving as Principal Investigator of Project Sickle Cure, a Sickle Cell Transplant Advocacy and Research Alliance Study partially funded by bluebird bio, and serving on the steering committee of a STAR clinical trial for which Bristol Myers Squibb has provided funding. N.M. reports consulting for Anthem, Inc and stock ownership in HCA Healthcare. R.P. reports advisory board participation for bluebird bio, and research funding from Amgen. S.R. reports serving as a medical monitor for the Resource for Clinical Investigation in Blood and Marrow Transplantation (RCI BMT). H.S. reports personal fees from Incyte, Janssen, Novartis, Sanofi, and the Belgian Hematological Society (BHS); research grants from Novartis and the BHS; and nonfinancial support from Gilead, Pfizer, the European Society for Blood and Marrow Transplantation, and the Center for International Bone Marrow Transplantation Research. A.S. reports consulting fees from Spotlight Therapeutics, Medexus, Vertex Pharmaceuticals, Sangamo Therapeutics, and Editas Medicine; serving as a medical monitor for RCI BMT; research funding from CRISPR Therapeutics; and honoraria from Vindico Medical Education. Dr Sharma is the St Jude Children’s Research Hospital site principal investigator of clinical trials for genome editing of sickle cell disease sponsored by Vertex Pharmaceuticals/CRISPR Therapeutics (NCT03745287), Novartis Pharmaceuticals (NCT04443907), and Beam Therapeutics (NCT05456880). The industry sponsors provide funding for the clinical trial, which includes salary support paid to Dr Sharma’s institution.
Footnotes
SUPPLEMENTARY MATERIALS
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jtct.2023.12.001.
REFERENCES
- 1.Aljurf M, Weisdorf D, Hashmi SK, et al. Worldwide Network for Blood and Marrow Transplantation (WBMT) recommendations for establishing a hematopoietic stem cell transplantation program in countries with limited resources (Part II): Clinical, technical and socio-economic considerations. Hematol Oncol Stem Cell Ther. 2020;13:7–16. [DOI] [PubMed] [Google Scholar]
- 2.Passweg JR, Baldomero H, Chabannon C, et al. Hematopoietic cell transplantation and cellular therapy survey of the EBMT: monitoring of activities and trends over 30 years. Bone Marrow Transplant. 2021;56:1651–1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.D’Souza A, Fretham C, Lee SJ, et al. Current Use of and Trends in Hematopoietic Cell Transplantation in the United States. Biol Blood Marrow Transplant. 2020;26: e177–e182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hashmi S, Carpenter P, Khera N, Tichelli A, Savani BN. Lost in transition: the essential need for long-term follow-up clinic for blood and marrow transplantation survivors. Biol Blood Marrow Transplant. 2015;21:225–232. [DOI] [PubMed] [Google Scholar]
- 5.Majhail NS, Rizzo JD. Surviving the cure: long term followup of hematopoietic cell transplant recipients. Bone Marrow Transplant. 2013;48:1145–1151. [DOI] [PubMed] [Google Scholar]
- 6.Majhail NS, Tao L, Bredeson C, et al. Prevalence of hematopoietic cell transplant survivors in the United States. Biol Blood Marrow Transplant. 2013;19:1498–1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wingard JR, Majhail NS, Brazauskas R, et al. Long-term survival and late deaths after allogeneic hematopoietic cell transplantation. J Clin Oncol. 2011;29:2230–2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Socie G, Stone JV, Wingard JR, et al. Long-term survival and late deaths after allogeneic bone marrow transplantation. Late Effects Working Committee of the International Bone Marrow Transplant Registry. N Engl J Med. 1999;341:14–21. [DOI] [PubMed] [Google Scholar]
- 9.Chow EJ, Cushing-Haugen KL, Cheng GS, et al. Morbidity and Mortality Differences Between Hematopoietic Cell Transplantation Survivors and Other Cancer Survivors. Journal of Clinical Oncology. 2017;35.306-+. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mitchell SA, Wiener L, Hoag J, Fry A, Bevans MF. Health-related quality of life in adult and pediatric survivors. Blood and Marrow Transplantation Long Term Management: Survivorship after Transplant. 2021:355–380. [Google Scholar]
- 11.Hashmi SK, Bredeson C, Duarte RF, et al. National Institutes of Health Blood and Marrow Transplant Late Effects Initiative: The Healthcare Delivery Working Group Report. Biol Blood Marrow Transplant. 2017;23:717–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bevans M, El-Jawahri A, Tierney DK, et al. National Institutes of Health Hematopoietic Cell Transplantation Late Effects Initiative: The Patient-Centered Outcomes Working Group Report. Biol Blood Marrow Transplant. 2017;23:538–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Battiwalla M, Hashmi S, Majhail N, Pavletic S, Savani BN, Shelburne N. National Institutes of Health Hematopoietic Cell Transplantation Late Effects Initiative: Developing Recommendations to Improve Survivorship and Long-Term Outcomes. Biol Blood Marrow Transplant. 2017;23:6–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shaw BE, Hahn T, Martin PJ, et al. National Institutes of Health Hematopoietic Cell Transplantation Late Effects Initiative: The Research Methodology and Study Design Working Group Report. Biol Blood Marrow Transplant. 2017;23:10–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morton LM, Saber W, Baker KS, et al. National Institutes of Health Hematopoietic Cell Transplantation Late Effects Initiative: The Subsequent Neoplasms Working Group Report. Biol Blood Marrow Transplant. 2017;23:367–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gea-Banacloche J, Komanduri KV, Carpenter P, et al. National Institutes of Health Hematopoietic Cell Transplantation Late Effects Initiative: The Immune Dys-regulation and Pathobiology Working Group Report. Biol Blood Marrow Transplant. 2017;23:870–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Armenian SH, Chemaitilly W, Chen M, et al. National Institutes of Health Hematopoietic Cell Transplantation Late Effects Initiative: The Cardiovascular Disease and Associated Risk Factors Working Group Report. Biol Blood Marrow Transplant. 2017;23:201–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rizzo JD, Wingard JR, Tichelli A, et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation: joint recommendations of the European Group for Blood and Marrow Transplantation, Center for International Blood and Marrow Transplant Research, and the American Society for Blood and Marrow Transplantation (EBMT/CIBMTR/ASBMT). Bone Marrow Transplant. 2006;37:249–261. [DOI] [PubMed] [Google Scholar]
- 19.Rizzo JD, Wingard JR, Tichelli A, et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation: joint recommendations of the European Group for Blood and Marrow Transplantation, the Center for International Blood and Marrow Transplant Research, and the American Society of Blood and Marrow Transplantation. Biology of Blood and Marrow Transplantation. 2006;12:138–151. [DOI] [PubMed] [Google Scholar]
- 20.Majhail NS, Rizzo JD, Lee SJ, et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation. Hematol Oncol Stem Cell Ther. 2012;5:1–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Majhail NS, Rizzo JD, Lee SJ, et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation. Bone Marrow Transplant. 2012;47:337–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Majhail NS, Rizzo JD, Lee SJ, et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2012;18:348–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Majhail NS, Rizzo JD, Lee SJ, et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation. Rev Bras Hematol Hemoter. 2012;34:109–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Desai AP, Go RS, Poonacha TK. Category of evidence and consensus underlying National Comprehensive Cancer Network guidelines: Is there evidence of progress? International Journal of Cancer. 2021;148:429–436. [DOI] [PubMed] [Google Scholar]
- 25.Neunert CE, Despotovic JM. Autoimmune hemolytic anemia and immune thrombocytopenia following hematopoietic stem cell transplant: A critical review of the literature. Pediatr Blood Cancer. 2019;66:e27569. [DOI] [PubMed] [Google Scholar]
- 26.Baur K, Buser AS, Infanti L, Halter JP, Passweg JR, Holbro A. Immune cytopenia after allogeneic haematopoietic stem-cell transplantation: challenges, approaches, and future directions. Lancet Haematol. 2021;8:e229–e239. [DOI] [PubMed] [Google Scholar]
- 27.Gabelli M, Ademokun C, Cooper N, Amrolia PI. Pathogenesis, risk factors and therapeutic options for autoimmune haemolytic anaemia in the post-transplant setting. Br J Haematol. 2021. [DOI] [PubMed] [Google Scholar]
- 28.Gibson CJ, Steensma DP. New Insights from Studies of Clonal Hematopoiesis. Clin Cancer Res. 2018;24:4633–4642. [DOI] [PubMed] [Google Scholar]
- 29.Nawas MT, Schetelig J, Damm F, et al. The clinical implications of clonal hematopoiesis in hematopoietic cell transplantation. Blood reviews. 2021;46:100744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jaiswal S, Natarajan P, Silver AJ, et al. Clonal Hematopoiesis and Risk of Atherosclerotic Cardiovascular Disease. N Engl J Med. 2017;377:111–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Frick M, Chan W, Arends CM, et al. Role of Donor Clonal Hematopoiesis in Allogeneic Hematopoietic Stem-Cell Transplantation. J Clin Oncol. 2019;37:375–385. [DOI] [PubMed] [Google Scholar]
- 32.Gibson CJ, Lindsley RC, Tchekmedyian V, et al. Clonal Hematopoiesis Associated With Adverse Outcomes After Autologous Stem-Cell Transplantation for Lymphoma. J Clin Oncol. 2017;35:1598–1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Majhail NS, Lazarus HM, Burns LJ. Iron overload in hematopoietic cell transplantation. Bone Marrow Transplantation. 2008;41:997–1003. [DOI] [PubMed] [Google Scholar]
- 34.Chaturvedi S, Neff A, Nagler A, Savani U, Mohty M, Savani BN. Venous thromboembolism in hematopoietic stem cell transplant recipients. Bone Marrow Transplant. 2016;51:473–478. [DOI] [PubMed] [Google Scholar]
- 35.Zahid MF, Murad MH, Litzow MR, et al. Venous thromboembolism following hematopoietic stem cell trans-plantation-a systematic review and meta-analysis. Ann Hematol. 2016;95:1457–1464. [DOI] [PubMed] [Google Scholar]
- 36.Gangaraju R, Chen Y, Hageman L, et al. Venous Thromboembolism in Autologous Blood or Marrow Transplantation Survivors: A Report from the Blood or Marrow Transplant Survivor Study. Biol Blood Marrow Transplant. 2019;25:2261–2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rangarajan HG, Stanek JR, Abu-Arja R, et al. Venous Thromboembolism in Pediatric Hematopoietic Cell Transplant: A Multicenter Cohort Study. Biol Blood Marrow Transplant. 2018;24:337–342. [DOI] [PubMed] [Google Scholar]
- 38.Gangaraju R, Chen Y, Hageman L, et al. Late mortality in blood or marrow transplant survivors with venous thromboembolism: report from the Blood or Marrow Transplant Survivor Study. Br J Haematol. 2019;186:367–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gangaraju R, Chen Y, Hageman L, et al. Late-occurring venous thromboembolism in allogeneic blood or marrow transplant survivors: a BMTSS-HiGHS2 risk model. Blood Adv. 2021;5:4102–4111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kekre N, Kim HT, Ho VT, et al. Venous thromboembolism is associated with graft-versus-host disease and increased non-relapse mortality after allogeneic hematopoietic stem cell transplantation. Haematologica. 2017;102:1185–1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Norkin M, Shaw BE, Brazauskas R, et al. Characteristics of Late Fatal Infections after Allogeneic Hematopoietic Cell Transplantation. Biol Blood Marrow Transplant. 2019;25:362–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ljungman P, de la Camara R, Mikulska M, et al. COVID-19 and stem cell transplantation; results from an EBMT and GETH multicenter prospective survey. Leukemia. 2021;35:2885–2894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ljungman P, de la Camara R, Perez-Bercoff L, et al. Outcome of pandemic H1N1 infections in hematopoietic stem cell transplant recipients. Haematologica. 2011;96:1231–1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Perkins JL, Chen Y, Harris A, et al. Infections Among Long-Term Survivors of Childhood and Adolescent Cancer A Report From the Childhood Cancer Survivor Study. Cancer. 2014;120:2514–2521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Foord AM, Cushing-Haugen KL, Boeckh MJ, et al. Late infectious complications in hematopoietic cell transplantation survivors: a population-based study. Blood Adv. 2020;4:1232–1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dadwal SS, Hohl TM, Fisher CE, et al. American Society of Transplantation and Cellular Therapy Series, 2:Management and Prevention of Aspergillosis in Hematopoietic Cell Transplantation Recipients. Transplant Cell Ther. 2021;27:201–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Torres HA, Chemaly RF, Storey R, et al. Influence of type of cancer and hematopoietic stem cell transplantation on clinical presentation of Pneumocystis jiroveci pneumonia in cancer patients. Eur J Clin Microbiol Infect Dis. 2006;25:382–388. [DOI] [PubMed] [Google Scholar]
- 48.Chen CS, Boeckh M, Seidel K, et al. Incidence, risk factors, and mortality from pneumonia developing late after hematopoietic stem cell transplantation. Bone Marrow Transplant. 2003;32:515–522. [DOI] [PubMed] [Google Scholar]
- 49.Caselli D, Petris MG, Rondelli R, et al. Single-day trimethoprim/sulfamethoxazole prophylaxis for Pneumocystis pneumonia in children with cancer. J Pediatr. 2014;164. 389–392 e381. [DOI] [PubMed] [Google Scholar]
- 50.Carpenter PA, Papanicolaou G, Chemaly RF, Boeckh M, Savani BN. American Society for Transplantation and Cellular Therapy Infectious Disease Guidelines: Preface to the Series. Transplant Cell Ther. 2021;27:103–104. [DOI] [PubMed] [Google Scholar]
- 51.Yong MK, Shigle TL, Kim Y-J, Carpenter PA, Chemaly RF, Papanicolaou GA. American Society for Transplantation and Cellular Therapy Series:# 4-Cytomegalovirus treatment and management of resistant or refractory infections after hematopoietic cell transplantation. Transplantation and Cellular Therapy. 2021;27:957–967. [DOI] [PubMed] [Google Scholar]
- 52.Satlin MJ, Weissman SJ, Carpenter PA, Seo SK, Shelburne SA. American Society of Transplantation and Cellular Therapy Series, 1: Enterobacterales infection prevention and management after hematopoietic cell transplantation. Transplantation and Cellular Therapy. 2021;27:108–114. [DOI] [PubMed] [Google Scholar]
- 53.Dadwal SS, Hohl TM, Fisher CE, et al. American Society of Transplantation and Cellular Therapy Series, 2:Management and prevention of aspergillosis in hematopoietic cell transplantation recipients. Transplantation and cellular therapy. 2021;27:201–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hakki M, Aitken SL, Danziger-Isakov L, et al. American Society for Transplantation and Cellular Therapy Series: #3—Prevention of Cytomegalovirus Infection and Disease After Hematopoietic Cell Transplantation. Transplantation and Cellular Therapy. 2021;27:707–719. [DOI] [PubMed] [Google Scholar]
- 55.Alonso CD, Maron G, Kamboj M, et al. American Society for Transplantation and Cellular Therapy Series: #5—Management of Clostridioides difficile Infection in Hematopoietic Cell Transplant Recipients. Transplantation and Cellular Therapy. 2022;28:225–232. [DOI] [PubMed] [Google Scholar]
- 56.Neofytos D, Steinbach WJ, Hanson K, Carpenter PA, Papanicolaou GA, Slavin MA. American Society for Transplantation and Cellular Therapy Series, #6: Management of Invasive Candidiasis in Hematopoietic Cell Transplantation Recipients. Transplantation and Cellular Therapy. 2023;29:222–227. [DOI] [PubMed] [Google Scholar]
- 57.Carpenter PA, Kitko CL, Elad S, et al. National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft-versus-Host Disease: V. The 2014 Ancillary Therapy and Supportive Care Working Group Report. Biol Blood Marrow Transplant. 2015;21:1167–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tomblyn M, Chiller T, Einsele H, et al. Guidelines for preventing infectious complications among hematopoietic cell transplantation recipients: a global perspective. Biol Blood Marrow Transplant. 2009;15:1143–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pallasch T, Shulman ST, Rowley AH, et al. Prevention of Infective Endocarditis: Guidelines From the American Heart Association: A. 2007. [Google Scholar]
- 60.Taggart C, Neumann N, Alonso PB, et al. Comparing a Neutropenic Diet to a Food Safety-Based Diet in Pediatric Patients Undergoing Hematopoietic Stem Cell Transplantation. Biol Blood Marrow Transplant. 2019;25:1382–1386. [DOI] [PubMed] [Google Scholar]
- 61.Bhatt NS, Brazauskas R, Salit RB, et al. Return to Work Among Young Adult Survivors of Allogeneic Hematopoietic Cell Transplantation in the United States. Transplantation and Cellular Therapy. 2021:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bhatt NS, Meyer C, Mau LW, et al. Return-to-School Practices for Pediatric Hematopoietic Cell Transplantation Recipients during the COVID-19 Pandemic. Transplant Cell Ther. 2022;28:54.e51–54.e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cordonnier C, Einarsdottir S, Cesaro S, et al. Vaccination of haemopoietic stem cell transplant recipients: guidelines of the 2017 European Conference on Infections in Leukaemia (ECIL 7). Lancet Infect Dis. 2019;19:e200–e212. [DOI] [PubMed] [Google Scholar]
- 64.FACT-JACIE. International standards for hematopoietic cellular therapy product collection, processing, and administration. Foundation for the Accreditation of Cellular Therapy (FACT) and Joint; 2018. [Google Scholar]
- 65.Chow EJ, Anderson L, Baker KS, et al. Late Effects Surveillance Recommendations among Survivors of Childhood Hematopoietic Cell Transplantation: A Children’s Oncology Group Report. Biology of Blood and Marrow Transplantation. 2016;22:782–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Carpenter PA, Englund JA. How I vaccinate blood and marrow transplant recipients. Blood. 2016;127:2824–2832. [DOI] [PubMed] [Google Scholar]
- 67.Rubin LG, Levin MJ, Ljungman P, et al. 2013 IDSA clinical practice guideline for vaccination of the immunocompromised host. Clinical infectious diseases. 2014;58:e44–e100. [DOI] [PubMed] [Google Scholar]
- 68.(CDC) CfDCaP. Advisory Committee on Immunization Practices (ACIP) General Best Guidance for Immunization. Altered Immunocompetence; 2022. [Google Scholar]
- 69.Shem-Tov N, Yerushalmi R, Danylesko I, et al. Immu-nogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in haematopoietic stem cell transplantation recipients. Br J Haematol. 2022;196:884–891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dioverti V, Boghdadly ZE, Shahid Z, et al. Revised Guidelines for Coronavirus Disease 19 Management in Hematopoietic Cell Transplantation and Cellular Therapy Recipients (August 2022). Transplant Cell Ther. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Murray SM, Barbanti M, Campbell C, et al. Impaired humoral and cellular response to primary COVID-19 vaccination in patients less than 2 years after allogeneic bone marrow transplant. British Journal ofHaema-tology. 2022;198:668–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Raanani P, Gafter-Gvili A, Paul M, Ben-Bassat I, Leibovici L, Shpilberg O. Immunoglobulin prophylaxis in hematopoietic stem cell transplantation: systematic review and meta-analysis. J Clin Oncol. 2009;27:770–781. [DOI] [PubMed] [Google Scholar]
- 73.Hill JA, Giralt S, Torgerson TR, Lazarus HM. CAR-T—and a side order of IgG, to go?-Immunoglobulin replacement in patients receiving CAR-T cell therapy. Blood reviews. 2019;38: 100596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Doan A, Pulsipher MA. Hypogammaglobulinemia due to CAR T-cell therapy. Pediatric blood & cancer. 2018:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hayden PJ, Roddie C, Bader P, et al. Management of adults and children receiving CAR T-cell therapy:2021 best practice recommendations of the European Society for Blood and Marrow Transplantation (EBMT) and the Joint Accreditation Committee of ISCT and EBMT (JACIE) and the European Haematology Association (EHA). Ann Oncol. 2022;33:259–275. [DOI] [PubMed] [Google Scholar]
- 76.Hill JA, Seo SK. How I prevent infections in patients receiving CD19-targeted chimeric antigen receptor T cells for B-cell malignancies. Blood. 2020;136:925–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shalabi H, Gust J, Taraseviciute A, et al. Beyond the storm - subacute toxicities and late effects in children receiving CAR T cells. Nature Reviews Clinical Oncology. 2021;18:363–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Orange JS, Grossman WJ, Navickis RJ, Wilkes MM. Impact of trough IgG on pneumonia incidence in primary immunodeficiency: A meta-analysis of clinical studies. Clin Immunol. 2010;137:21–30. [DOI] [PubMed] [Google Scholar]
- 79.Tomblyn M, Chiller T, Einsele H, et al. Guidelines for preventing infectious complications among hematopoietic cell transplant recipients: a global perspective PREFACE. Bone Marrow Transplantation. 2009;44.453-+. [DOI] [PubMed] [Google Scholar]
- 80.Jagasia MH, Greinix HT, Arora M, et al. National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft-versus-Host Disease: I. The 2014 Diagnosis and Staging Working Group report. Biol Blood Marrow Transplant. 2015;21. 389–401 e381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nair S, Vanathi M, Mukhija R, Tandon R, Jain S, Ogawa Y. Update on ocular graft-versus-host disease. Indian J Ophthalmol. 2021;69:1038–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tabbara KF, Al-Ghamdi A, Al-Mohareb F, et al. Ocular findings after allogeneic hematopoietic stem cell transplantation. Ophthalmology. 2009;116:1624–1629. [DOI] [PubMed] [Google Scholar]
- 83.Nassar A, Tabbara KF, Aljurf M. Ocular manifestations of graft-versus-host disease. Saudi J Ophthalmol. 2013;27:215–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Inamoto Y, Valdes-Sanz N, Ogawa Y, et al. Ocular graft-versus-host disease after hematopoietic cell transplantation: Expert review from the Late Effects and Quality of Life Working Committee of the CIBMTR and Transplant Complications Working Party of the EBMT. Bone Marrow Transplant. 2019;54:662–673. [DOI] [PubMed] [Google Scholar]
- 85.Inamoto Y, Petriček I, Burns L, et al. Non-GVHD ocular complications after hematopoietic cell transplantation: expert review from the Late Effects and Quality of Life Working Committee of the CIBMTR and Transplant Complications Working Party of the EBMT. Bone marrow transplantation. 2019;54:648–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gurney JG, Ness KK, Rosenthal J, Forman SJ, Bhatia S, Baker KS. Visual, auditory, sensory, and motor impairments in long-term survivors of hematopoietic stem cell transplantation performed in childhood: results from the Bone Marrow Transplant Survivor study. Cancer. 2006;106:1402–1408. [DOI] [PubMed] [Google Scholar]
- 87.Pavletic SZ, Lee SJ, Socie G, Vogelsang G. Chronic graft-versus-host disease: implications of the National Institutes of Health consensus development project on criteria for clinical trials. Bone Marrow Transplant. 2006;38:645–651. [DOI] [PubMed] [Google Scholar]
- 88.Meier JK, Wolff D, Pavletic S, et al. Oral chronic graft-versus-host disease: report from the International Consensus Conference on clinical practice in cGVHD. Clin Oral Investig. 2011;15:127–139. [DOI] [PubMed] [Google Scholar]
- 89.Curtis RE, Rowlings PA, Deeg HJ, et al. Solid cancers after bone marrow transplantation. N Engl J Med. 1997;336:897–904. [DOI] [PubMed] [Google Scholar]
- 90.Majhail NS, Brazauskas R, Rizzo JD, et al. Secondary solid cancers after allogeneic hematopoietic cell transplantation using busulfan-cyclophosphamide conditioning. Blood. 2011;117:316–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Rizzo JD, Curtis RE, Socie G, et al. Solid cancers after allogeneic hematopoietic cell transplantation. Blood. 2009;113:1175–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chen MH, Chang PM, Li WY, et al. High incidence of oral squamous cell carcinoma independent of HPV infection after allogeneic hematopoietic SCT in Taiwan. Bone Marrow Transplant. 2011;46:567–572. [DOI] [PubMed] [Google Scholar]
- 93.Yokota A, Ozawa S, Masanori T, et al. Secondary solid tumors after allogeneic hematopoietic SCT in Japan. Bone Marrow Transplant. 2012;47:95–100. [DOI] [PubMed] [Google Scholar]
- 94.Curtis RE, Metayer C, Rizzo JD, et al. Impact of chronic GVHD therapy on the development of squamous-cell cancers after hematopoietic stem-cell transplantation:an international case-control study. Blood. 2005;105:3802–3811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Atsuta Y, Suzuki R, Yamashita T, et al. Continuing increased risk of oral/esophageal cancer after allogeneic hematopoietic stem cell transplantation in adults in association with chronic graft-versus-host disease. Ann Oncol. 2014;25:435–441. [DOI] [PubMed] [Google Scholar]
- 96.Elad S, Raber-Durlacher JE, Brennan MT, et al. Basic oral care for hematology-oncology patients and hematopoietic stem cell transplantation recipients: a position paper from the joint task force of the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO) and the European Society for Blood and Marrow Transplantation (EBMT). Support Care Cancer. 2015;23:223–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Castellarin P, Stevenson K, Biasotto M, Yuan A, Woo SB, Treister NS. Extensive dental caries in patients with oral chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2012;18:1573–1579. [DOI] [PubMed] [Google Scholar]
- 98.Holtta P, Alaluusua S, Saarinen-Pihkala UM, Peltola J, Hovi L. Agenesis and microdontia of permanent teeth as late adverse effects after stem cell transplantation in young children. Cancer-Am Cancer Soc. 2005;103:181–190. [DOI] [PubMed] [Google Scholar]
- 99.Solh M, Arat M, Cao Q, Majhail NS, Weisdorf D. Late-onset noninfectious pulmonary complications in adult allogeneic hematopoietic cell transplant recipients. Transplantation. 2011;91:798–803. [DOI] [PubMed] [Google Scholar]
- 100.Wenger DS, Triplette M, Crothers K, et al. Incidence, Risk Factors, and Outcomes of Idiopathic Pneumonia Syndrome after Allogeneic Hematopoietic Cell Transplantation. Biol Blood Marrow Transplant. 2020;26:413–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Panoskaltsis-Mortari A, Griese M, Madtes DK, et al. An official American Thoracic Society research statement: noninfectious lung injury after hematopoietic stem cell transplantation: idiopathic pneumonia syndrome. Am J Respir Crit Care Med. 2011;183:1262–1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Williams KM. How I treat bronchiolitis obliterans syndrome after hematopoietic stem cell transplantation. Blood. 2017;129:448–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chien JW, Martin PJ, Gooley TA, et al. Airflow obstruction after myeloablative allogeneic hematopoietic stem cell transplantation. Am J Respir Crit Care Med. 2003;168:208–214. [DOI] [PubMed] [Google Scholar]
- 104.Williams KM, Chien JW, Gladwin MT, Pavletic SZ. Bronchiolitis obliterans after allogeneic hematopoietic stem cell transplantation. JAMA. 2009;302:306–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Thompson PA, Lim A, Panek-Hudson Y, et al. Screening with Spirometry Is a Useful Predictor of Later Development of Noninfectious Pulmonary Syndromes in Patients Undergoing Allogeneic Stem Cell Transplantation. Biology of Blood and Marrow Transplantation. 2014;20:781–786. [DOI] [PubMed] [Google Scholar]
- 106.Ditschkowski M, Elmaagacli AH, Koldehoff M, Gromke T, Trenschel R, Beelen DW. Bronchiolitis obliterans after allogeneic hematopoietic SCT: further insight-new perspectives? Bone Marrow Transplant. 2013;48:1224–1229. [DOI] [PubMed] [Google Scholar]
- 107.Fitch T, Myers KC, Dewan M, Towe C, Dandoy C. Pulmonary Complications After Pediatric Stem Cell Transplant. Front Oncol. 2021;11: 755878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Freudenberger TD, Madtes DK, Curtis JR, Cummings P, Storer BE, Hackman RC. Association between acute and chronic graft-versus-host disease and bronchiolitis obliterans organizing pneumonia in recipients of hematopoietic stem cell transplants. Blood. 2003;102:3822–3828. [DOI] [PubMed] [Google Scholar]
- 109.Nakasone H, Onizuka M, Suzuki N, et al. Pre-transplant risk factors for cryptogenic organizing pneumonia/bronchiolitis obliterans organizing pneumonia after hematopoietic cell transplantation. Bone Marrow Transplant. 2013;48:1317–1323. [DOI] [PubMed] [Google Scholar]
- 110.Afessa B, Litzow MR, Tefferi A. Bronchiolitis obliterans and other late onset non-infectious pulmonary complications in hematopoietic stem cell transplantation. Bone Marrow Transplant. 2001;28:425–434. [DOI] [PubMed] [Google Scholar]
- 111.Bhatia S, Francisco L, Carter A, et al. Late mortality after allogeneic hematopoietic cell transplantation and functional status of long-term survivors: report from the Bone Marrow Transplant Survivor Study. Blood. 2007;110:3784–3792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Inamoto Y, Lee SJ. Late effects of blood and marrow transplantation. Haematologica. 2017;102:614–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Rotz SJ, Ryan TD, Hayek SS. Cardiovascular disease and its management in children and adults undergoing hematopoietic stem cell transplantation. J Thromb Thrombolysis. 2021;51:854–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chow EJ, Mueller BA, Baker KS, et al. Cardiovascular hospitalizations and mortality among recipients of hematopoietic stem cell transplantation. Ann Intern Med. 2011;155:21–32. [DOI] [PubMed] [Google Scholar]
- 115.Armenian SH, Yang D, Teh JB, et al. Prediction of cardiovascular disease among hematopoietic cell transplantation survivors. Blood Adv. 2018;2:1756–1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rotz SJ, Ryan TD, Hlavaty J, George SA, El-Bietar J, Dandoy CE. Cardiotoxicity and cardiomyopathy in children and young adult survivors of hematopoietic stem cell transplant. Pediatr Blood Cancer. 2017;64. [DOI] [PubMed] [Google Scholar]
- 117.Armenian SH, Sun CL, Shannon T, et al. Incidence and predictors of congestive heart failure after autologous hematopoietic cell transplantation. Blood. 2011;118: 6023–6029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Tichelli A, Passweg J, Wojcik D, et al. Late cardiovascular events after allogeneic hematopoietic stem cell transplantation: a retrospective multicenter study of the Late Effects Working Party of the European Group for Blood and Marrow Transplantation. Haematologica. 2008;93:1203–1210. [DOI] [PubMed] [Google Scholar]
- 119.Lyon AR, López-Fernández T, Couch LS, et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS) Developed by the task force on cardio-oncology of the European Society of Cardiology (ESC). European Heart Journal-Cardiovascular Imaging. 2022;23:e333–e465. [DOI] [PubMed] [Google Scholar]
- 120.Aziz-Bose R, Margossian R, Ames BL, et al. Delphi Panel Consensus Recommendations for Screening and Managing Childhood Cancer Survivors at Risk for Cardiomyopathy. JACC CardioOncol. 2022;4:354–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Majhail NS, Flowers ME, Ness KK, et al. High prevalence of metabolic syndrome after allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2009;43:49–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Baker KS, Chow EJ, Goodman PJ, et al. Impact of treatment exposures on cardiovascular risk and insulin resistance in childhood cancer survivors. Cancer Epidemiol Biomarkers Prev. 2013;22:1954–1963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Greenfield DM, Salooja N, Peczynski C, et al. Metabolic syndrome and cardiovascular disease after haematopoietic cell transplantation (HCT) in adults: an EBMT cross-sectional non-interventional study. Bone Marrow Transplant. 2021;56:2820–2825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Alberti kG Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. [DOI] [PubMed] [Google Scholar]
- 125.Kockx M, Jessup W, Kritharides L. Cyclosporin A and atherosclerosis-cellular pathways in atherogenesis. Pharmacol Ther. 2010;128:106–118. [DOI] [PubMed] [Google Scholar]
- 126.Nottage KA, Ness KK, Li C, Srivastava D, Robison LL, Hudson MM. Metabolic syndrome and cardiovascular risk among long-term survivors of acute lymphoblastic leukaemia - From the St. Jude Lifetime Cohort. Br J Haematol. 2014;165:364–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.DeFilipp Z, Duarte RF, Snowden JA, et al. Metabolic Syndrome and Cardiovascular Disease after Hematopoietic Cell Transplantation: Screening and Preventive Practice Recommendations from the CIBMTR and EBMT. Biol Blood Marrow Transplant. 2016;22:1493–1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Baker KS, Chow E, Steinberger J. Metabolic syndrome and cardiovascular risk in survivors after hematopoietic cell transplantation. Bone Marrow Transplant. 2012;47:619–625. [DOI] [PubMed] [Google Scholar]
- 129.Blaser BW, Kim HT, Alyea EP, et al. Hyperlipidemia and statin use after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2012;18:575–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Pophali PA, Klotz JK, Ito S, et al. Male survivors of allogeneic hematopoietic stem cell transplantation have a long term persisting risk of cardiovascular events. Experimental Hematology. 2014;42:83–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Kyle UG, Chalandon Y, Miralbell R, et al. Longitudinal follow-up of body composition in hematopoietic stem cell transplant patients. Bone Marrow Transplant. 2005;35:1171–1177. [DOI] [PubMed] [Google Scholar]
- 132.Friedman DN, Moskowitz CS, Hilden P, et al. Radiation Dose and Volume to the Pancreas and Subsequent Risk of Diabetes Mellitus: A Report from the Childhood Cancer Survivor Study. J Natl Cancer Inst. 2020;112:525–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Armenian SH, Sun CL, Vase T, et al. Cardiovascular risk factors in hematopoietic cell transplantation survivors: role in development of subsequent cardiovascular disease. Blood. 2012;120:4505–4512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Oudin C, Auquier P, Bertrand Y, et al. Metabolic syndrome in adults who received hematopoietic stem cell transplantation for acute childhood leukemia: an LEA study. Bone Marrow Transplant. 2015;50:1438–1444. [DOI] [PubMed] [Google Scholar]
- 135.Tichelli A, Bucher C, Rovo A, et al. Premature cardiovascular disease after allogeneic hematopoietic stem-cell transplantation. Blood. 2007;110:3463–3471. [DOI] [PubMed] [Google Scholar]
- 136.Leger KJ, Baker KS, Cushing-Haugen KL, et al. Lifestyle factors and subsequent ischemic heart disease risk after hematopoietic cell transplantation. Cancer. 2018;124:1507–1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Leger KJ, Cushing-Haugen K, Hansen JA, et al. Clinical and Genetic Determinants of Cardiomyopathy Risk among Hematopoietic Cell Transplantation Survivors. Biol Blood Marrow Transplant. 2016;22:1094–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Armenian S, Bhatia S. Predicting and Preventing Anthracycline-Related Cardiotoxicity. Am Soc Clin Oncol Educ Book. 2018;38:3–12. [DOI] [PubMed] [Google Scholar]
- 139.Flowers ME, Martin PJ. How we treat chronic graft-versus-host disease. Blood, The Journal of the American Society of Hematology. 2015;125:606–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Jorgensen AY, Maraldo MV, Brodin NP, et al. The effect on esophagus after different radiotherapy techniques for early stage Hodgkin’s lymphoma. Acta Oncol. 2013;52:1559–1565. [DOI] [PubMed] [Google Scholar]
- 141.Nomura K, Iizuka T, Kaji D, et al. Secondary esophageal squamous cell carcinoma after hematopoietic stem cell transplantation. J Cancer Res Clin Oncol. 2021;147:2137–2144. [DOI] [PubMed] [Google Scholar]
- 142.Gutierrez CA, Raval MV, Vester HR, Chaudhury S, von Allmen D, Rothstein DH. Surgical treatment of intestinal complications of graft versus host disease in the pediatric population: Case series and review of literature. J Pediatr Surg. 2017;52:1718–1722. [DOI] [PubMed] [Google Scholar]
- 143.Gini A, Meester RGS, Keshavarz H, et al. Cost-Effectiveness of Colonoscopy-Based Colorectal Cancer Screening in Childhood Cancer Survivors. J Natl Cancer Inst. 2019;111:1161–1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Teepen JC, Kok JL, van Leeuwen FE, et al. Colorectal Adenomas and Cancers After Childhood Cancer Treatment: A DCOG-LATER Record Linkage Study. J Natl Cancer Inst. 2018;110:758–767. [DOI] [PubMed] [Google Scholar]
- 145.Nottage K, McFarlane J, Krasin MJ, et al. Secondary colorectal carcinoma after childhood cancer. J Clin Oncol. 2012;30:2552–2558. [DOI] [PubMed] [Google Scholar]
- 146.Haghiri S, Fayech C, Mansouri I, et al. Long-term follow-up of high-risk neuroblastoma survivors treated with high-dose chemotherapy and stem cell transplantation rescue. Bone Marrow Transplant. 2021;56:1984–1997. [DOI] [PubMed] [Google Scholar]
- 147.Sudour H, Mainard L, Baumann C, Clement L, Salmon A, Bordigoni P. Focal nodular hyperplasia of the liver following hematopoietic SCT. Bone Marrow Transplant. 2009;43:127–132. [DOI] [PubMed] [Google Scholar]
- 148.Pillon M, Carucci NS, Mainardi C, et al. Focal nodular hyperplasia of the liver: an emerging complication of hematopoietic SCT in children. Bone Marrow Transplant. 2015;50:414–419. [DOI] [PubMed] [Google Scholar]
- 149.Anderson L, Gregg D, Margolis D, Casper J, Talano J. Focal nodular hyperplasia in pediatric allogeneic hematopoietic cell transplant: case series. Bone Marrow Transplant. 2010;45:1357–1359. [DOI] [PubMed] [Google Scholar]
- 150.Liang R. How I treat and monitor viral hepatitis B infection in patients receiving intensive immunosuppressive therapies or undergoing hematopoietic stem cell transplantation. Blood. 2009;113:3147–3153. [DOI] [PubMed] [Google Scholar]
- 151.Mallet V, van Bommel F, Doerig C, et al. Management of viral hepatitis in patients with haematological malignancy and in patients undergoing haemopoietic stem cell transplantation: recommendations of the 5th European Conference on Infections in Leukaemia (ECIL-5). Lancet Infect Dis. 2016;16:606–617. [DOI] [PubMed] [Google Scholar]
- 152.Torres HA, Chong PP, De Lima M, et al. Hepatitis C Virus Infection among Hematopoietic Cell Transplant Donors and Recipients: American Society for Blood and Marrow Transplantation Task Force Recommendations. Biol Blood Marrow Transplant. 2015;21:1870–1882. [DOI] [PubMed] [Google Scholar]
- 153.McDonald GB. Hepatobiliary complications of hematopoietic cell transplantation, 40 years on. Hepatology. 2010;51:1450–1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Sastry J, Young S, Shaw PJ. Acute pancreatitis due to tacrolimus in a case of allogeneic bone marrow transplantation. Bone Marrow Transplant. 2004;33:867–868. [DOI] [PubMed] [Google Scholar]
- 155.Akpek G, Valladares JL, Lee L, Margolis J, Vogelsang GB. Pancreatic insufficiency in patients with chronic graft-versus-host disease. Bone Marrow Transplant. 2001;27:163–166. [DOI] [PubMed] [Google Scholar]
- 156.Hingorani S. Renal Complications of Hematopoietic-Cell Transplantation. N Engl J Med. 2016;374:2256–2267. [DOI] [PubMed] [Google Scholar]
- 157.Hingorani S, Pao E, Stevenson P, et al. Changes in Glomerular Filtration Rate and Impact on Long-Term Survival among Adults after Hematopoietic Cell Transplantation: A Prospective Cohort Study. Clin J Am Soc Nephrol. 2018;13:866–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Young JA, Pallas CR, Knovich MA. Transplant-associated thrombotic microangiopathy: theoretical considerations and a practical approach to an unrefined diagnosis. Bone Marrow Transplant. 2021;56:1805–1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Schoettler M, Carreras E, Cho B, et al. Harmonizing Definitions for Diagnostic Criteria and Prognostic Assessment of Transplant Associated Thrombotic Microangiopathy: A Report on Behalf of the European Society for Blood and Marrow Transplantation (EBMT), American Society for Transplantation and Cellular Therapy (ASTCT), Asia-Pacific Blood and Marrow Transplantation Group (APBMT) and the Center for International Blood and Marrow Transplant Research (CIBMTR). Transplant Cell Ther. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.CE Dandoy, Rotz S, Alonso PB, et al. A pragmatic multi-institutional approach to understanding transplant-associated thrombotic microangiopathy after stem cell transplant. Blood Adv. 2021;5:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Heybeli C, Sridharan M, Alkhateeb HB, et al. Characteristics of late transplant-associated thrombotic microangiopathy in patients who underwent allogeneic hematopoietic stem cell transplantation. Am J Hematol. 2020;95:1170–1179. [DOI] [PubMed] [Google Scholar]
- 162.Sklar C. Growth and endocrine disturbances after bone marrow transplantation in childhood. Acta Paediatr Suppl. 1995;411:57–61. discussion 62. [DOI] [PubMed] [Google Scholar]
- 163.Brauner R, Adan L, Souberbielle JC, et al. Contribution of growth hormone deficiency to the growth failure that follows bone marrow transplantation. J Pediatr. 1997;130:785–792. [DOI] [PubMed] [Google Scholar]
- 164.Ogilvy-Stuart AL, Clark DJ, Wallace WH, et al. Endocrine deficit after fractionated total body irradiation. Arch Dis Child. 1992;67:1107–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Alter CA, Thornton PS, Willi SM, Bunin N, Moshang T Growth in children after bone marrow transplantation for acute myelogenous leukemia as compared to acute lymphocytic leukemia. J Pediatr Endocrinol Metab. 1996;9:51–57. [DOI] [PubMed] [Google Scholar]
- 166.Shalet SM, Toogood A, Rahim A, Brennan BM. The diagnosis of growth hormone deficiency in children and adults. Endocr Rev. 1998;19:203–223. [DOI] [PubMed] [Google Scholar]
- 167.Sanders JE, Buckner CD, Sullivan KM, et al. Growth and development in children after bone marrow transplantation. Horm Res. 1988;30:92–97. [DOI] [PubMed] [Google Scholar]
- 168.Sanders JE, Pritchard S, Mahoney P, et al. Growth and development following marrow transplantation for leukemia. Blood. 1986;68:1129–1135. [PubMed] [Google Scholar]
- 169.Shalet SM, Crowne EC, Didi MA, Ogilvy-Stuart AL, Wallace WH. Irradiation-induced growth failure. Baillieres Clin Endocrinol Metab. 1992;6:513–526. [DOI] [PubMed] [Google Scholar]
- 170.Couto-Silva AC, Trivin C, Esperou H, et al. Final height and gonad function after total body irradiation during childhood. Bone Marrow Transplant. 2006;38:427–432. [DOI] [PubMed] [Google Scholar]
- 171.Chemaitilly W, Boulad F, Heller G, et al. Final height in pediatric patients after hyperfractionated total body irradiation and stem cell transplantation. Bone Marrow Transplant. 2007;40:29–35. [DOI] [PubMed] [Google Scholar]
- 172.Sanders JE, Guthrie KA, Hoffmeister PA, Woolfrey AE, Carpenter PA, Appelbaum FR. Final adult height of patients who received hematopoietic cell transplantation in childhood. Blood. 2005;105:1348–1354. [DOI] [PubMed] [Google Scholar]
- 173.Wilcox NS, Rotz SJ, Mullen M, et al. Sex-Specific Cardiovascular Risks of Cancer and Its Therapies. Circ Res. 2022;130:632–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Baker KS, Ness KK, Weisdorf D, et al. Late effects in survivors of acute leukemia treated with hematopoietic cell transplantation: a report from the Bone Marrow Transplant Survivor Study. Leukemia. 2010;24:2039–2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Sanders JE, Hoffmeister PA, Woolfrey AE, et al. Thyroid function following hematopoietic cell transplantation in children: 30 years’ experience. Blood. 2009;113:306–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Farhadfar N, Stan MN, Shah P, et al. Thyroid dysfunction in adult hematopoietic cell transplant survivors: risks and outcomes. Bone Marrow Transplant. 2018;53:977–982. [DOI] [PubMed] [Google Scholar]
- 177.Medinger M, Zeiter D, Heim D, et al. Hypothyroidism following allogeneic hematopoietic stem cell transplantation for acute myeloid leukemia. Leuk Res. 2017;58:43–47. [DOI] [PubMed] [Google Scholar]
- 178.Savani BN, Koklanaris EK, Le Q, Shenoy A, Goodman S, Barrett AJ. Prolonged chronic graft-versus-host disease is a risk factor for thyroid failure in long-term survivors after matched sibling donor stem cell transplantation for hematologic malignancies. Biol Blood Marrow Transplant. 2009;15:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Cattoni A, Molinari S, Gaiero A, et al. Thyroid Disorders Following Hematopoietic Stem Cell Transplantation in Childhood: Impact of Conditioning Regimen on Thyroid Dysfunction, Volume Changes, and Occurrence of Nodules. Transplant Cell Ther. 2022;28:506.e501–506.e512. [DOI] [PubMed] [Google Scholar]
- 180.Tatevossian R, Blair JC, Plowman PN, Savage MO, Shankar AG. Thyrotoxicosis after matched unrelated bone marrow transplantation. J Pediatr Hematol Oncol. 2004;26:529–531. [DOI] [PubMed] [Google Scholar]
- 181.Khera N, Storer B, Flowers ME, et al. Nonmalignant late effects and compromised functional status in survivors of hematopoietic cell transplantation. J Clin Oncol. 2012;30:71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Thygesen KH, Schjodt I, Jarden M. The impact of hematopoietic stem cell transplantation on sexuality: a systematic review of the literature. Bone Marrow Transplant. 2012;47:716–724. [DOI] [PubMed] [Google Scholar]
- 183.Haavisto A, Mathiesen S, Suominen A, et al. Male Sexual Function after Allogeneic Hematopoietic Stem Cell Transplantation in Childhood: A Multicenter Study. Cancers (Basel). 2020:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Syrjala KL, Schoemans H, Yi JC, et al. Sexual Functioning in Long-Term Survivors of Hematopoietic Cell Transplantation. Transplant Cell Ther. 2021;27:80.e81.–80.e112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Nørskov KH, Schmidt M, Jarden M. Patients’ experience of sexuality 1-year after allogeneic Haematopoietic Stem Cell Transplantation. European Journal of Oncology Nursing. 2015;19:419–426. [DOI] [PubMed] [Google Scholar]
- 186.Wong FL, Francisco L, Togawa K, et al. Longitudinal trajectory of sexual functioning after hematopoietic cell transplantation: impact of chronic graft-versus-host disease and total body irradiation. Blood. 2013;122:3973–3981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Tsatsou I, Mystakidou K, Panagou E, et al. Sexuality and quality of life of patients with hematologic malignancy and hematopoietic stem cell transplantation: a critical review. J BUON. 2020;25:1693–1706. [PubMed] [Google Scholar]
- 188.Gerstl B, Sullivan E, Koch J, et al. Reproductive outcomes following a stem cell transplant for a haematological malignancy in female cancer survivors: a systematic review and meta-analysis. Support Care Cancer. 2019;27:4451–4460. [DOI] [PubMed] [Google Scholar]
- 189.Salooja N, Shoham Z, Dalle JH. Endocrine Disorders, Fertility and Sexual Health. In: Carreras Dufour, Mohty Kröger, eds. The EBMT Handbook: Hematopoietic Stem Cell Transplantation and Cellular Therapies. Cham (CH): Springer; Copyright 2019, EBMT and the Author(s); 2019:421–427. [PubMed] [Google Scholar]
- 190.Bourlon C, Riviello-Goya S, Acosta-Medina AA, et al. Outcomes and Challenges of Reproductive Health in Hematopoietic Stem Cell Transplantation Survivors. Biol Blood Marrow Transplant. 2020;26:2127–2131. [DOI] [PubMed] [Google Scholar]
- 191.Wallace WH, Thomson AB, Saran F, Kelsey TW. Predicting age of ovarian failure after radiation to a field that includes the ovaries. Int J Radiat Oncol Biol Phys. 2005;62:738–744. [DOI] [PubMed] [Google Scholar]
- 192.Phelan R, Im A, Hunter RL, et al. Male-Specific Late Effects in Adult Hematopoietic Cell Transplantation Recipients: A Systematic Review from the Late Effects and Quality of Life Working Committee of the Center for International Blood and Marrow Transplant Research and Transplant Complications Working Party of the European Society of Blood and Marrow Transplantation. Transplant Cell Ther. 2022;28:335.e317–335.e331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Nahata L, Woodruff TK, Quinn GP, et al. Ovarian tissue cryopreservation as standard of care: what does this mean for pediatric populations? Journal of assisted reproduction and genetics. 2020;37:1323–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Chen H, Xiao L, Li J, Cui L, Huang W. Adjuvant gonadotropin-releasing hormone analogues for the prevention of chemotherapy-induced premature ovarian failure in premenopausal women. Cochrane Database Syst Rev. 2019;3: Cd008018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Hur C, Rehmer J, Flyckt R, Falcone T. Uterine Factor Infertility: A Clinical Review. Clin Obstet Gynecol. 2019;62:257–270. [DOI] [PubMed] [Google Scholar]
- 196.Fenig E, Mishaeli M, Kalish Y, Lishner M. Pregnancy and radiation. Cancer Treat Rev. 2001;27:1–7. [DOI] [PubMed] [Google Scholar]
- 197.Meirow D, Schiff E. Appraisal of chemotherapy effects on reproductive outcome according to animal studies and clinical data. J Natl Cancer Inst Monogr. 2005:21–25. [DOI] [PubMed] [Google Scholar]
- 198.Green DM, Sklar CA, Boice JD, et al. Ovarian failure and reproductive outcomes after childhood cancer treatment: results from the Childhood Cancer Survivor Study. J Clin Oncol. 2009;27:2374–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Phelan R, Im A, Hunter RL, et al. Male-specific late effects in adult hematopoietic cell transplantation recipients: a systematic review from the Late Effects and Quality of Life Working Committee of the Center for International Blood and Marrow Transplant Research and Transplant Complications Working Party of the European Society of Blood and Marrow Transplantation. Transplant Cell Ther. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Tse S, Saunders EF, Silverman E, Vajsar J, Becker L, Meaney B. Myasthenia gravis and polymyositis as manifestations of chronic graft-versus-host-disease. Bone Marrow Transplant. 1999;23:397–399. [DOI] [PubMed] [Google Scholar]
- 201.Couriel DR, Beguelin GZ, Giralt S, et al. Chronic graft-versus-host disease manifesting as polymyositis: an uncommon presentation. Bone Marrow Transplant. 2002;30:543–546. [DOI] [PubMed] [Google Scholar]
- 202.Parker P, Chao NJ, Ben-Ezra J, et al. Polymyositis as a manifestation of chronic graft-versus-host disease. Medicine (Baltimore). 1996;75:279–285. [DOI] [PubMed] [Google Scholar]
- 203.Stevens AM, Sullivan KM, Nelson JL. Polymyositis as a manifestation of chronic graft-versus-host disease. Rheumatology (Oxford). 2003;42:34–39. [DOI] [PubMed] [Google Scholar]
- 204.Janin A, Socie G, Devergie A, et al. Fasciitis in chronic graft-versus-host disease. A clinicopathologic study of 14 cases. Ann Intern Med. 1994;120:993–998. [DOI] [PubMed] [Google Scholar]
- 205.Markusse HM, Dijkmans BA, Fibbe WE. Eosinophilic fasciitis after allogeneic bone marrow transplantation. J Rheumatol. 1990;17:692–694. [PubMed] [Google Scholar]
- 206.Oda K, Nakaseko C, Ozawa S, et al. Fasciitis and myositis: an analysis of muscle-related complications caused by chronic GVHD after allo-SCT. Bone Marrow Transplant. 2009;43:159–167. [DOI] [PubMed] [Google Scholar]
- 207.Pereira RM, Freire de Carvalho J. Glucocorticoid-induced myopathy. Joint Bone Spine. 2011;78:41–44. [DOI] [PubMed] [Google Scholar]
- 208.Inamoto Y, Lee SJ, Onstad LE, et al. Refined National Institutes of Health response algorithm for chronic graft-versus-host disease in joints and fascia. Blood Adv. 2020;4:40–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Inamoto Y, Pidala J, Chai X, et al. Assessment of joint and fascia manifestations in chronic graft-versus-host disease. Arthritis Rheumatol. 2014;66:1044–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Buxbaum NP, Pavletic SZ. Autoimmunity Following Allogeneic Hematopoietic Stem Cell Transplantation. Front Immunol. 2020;11:2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Bar M, Ott SM, Lewiecki EM, et al. Bone Health Management After Hematopoietic Cell Transplantation: An Expert Panel Opinion from the American Society for Transplantation and Cellular Therapy. Biol Blood Marrow Transplant. 2020;26:1784–1802. [DOI] [PubMed] [Google Scholar]
- 212.Savani BN, Donohue T, Kozanas E, et al. Increased risk of bone loss without fracture risk in long-term survivors after allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2007;13:517–520. [DOI] [PubMed] [Google Scholar]
- 213.Tauchmanova L, Colao A, Lombardi G, Rotoli B, Selleri C. Bone loss and its management in long-term survivors from allogeneic stem cell transplantation. J Clin Endocrinol Metab. 2007;92:4536–4545. [DOI] [PubMed] [Google Scholar]
- 214.Pirsl F, Curtis LM, Steinberg SM, et al. Characterization and Risk Factor Analysis of Osteoporosis in a Large Cohort of Patients with Chronic Graft-versus-Host Disease. Biol Blood Marrow Transplant. 2016;22:1517–1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Schimmer AD, Mah K, Bordeleau L, et al. Decreased bone mineral density is common after autologous blood or marrow transplantation. Bone Marrow Transplant. 2001;28:387–391. [DOI] [PubMed] [Google Scholar]
- 216.Yao S, McCarthy PL, Dunford LM, et al. High prevalence of early-onset osteopenia/osteoporosis after allogeneic stem cell transplantation and improvement after bisphosphonate therapy. Bone Marrow Transplant. 2008;41:393–398. [DOI] [PubMed] [Google Scholar]
- 217.Petropoulou AD, Porcher R, Herr AL, et al. Prospective assessment of bone turnover and clinical bone diseases after allogeneic hematopoietic stem-cell transplantation. Transplantation. 2010;89:1354–1361. [DOI] [PubMed] [Google Scholar]
- 218.Stern JM, Sullivan KM, Ott SM, et al. Bone density loss after allogeneic hematopoietic stem cell transplantation: a prospective study. Biol Blood Marrow Transplant. 2001;7:257–264. [DOI] [PubMed] [Google Scholar]
- 219.Bechard LJ, Gordon C, Feldman HA, et al. Bone loss and vitamin D deficiency in children undergoing hematopoietic cell transplantation. Pediatr Blood Cancer. 2015;62:687–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Swauger S, Sabulski A, Hornung L, Wasserman H, Myers KC, Howell JC. Bone Health Outcomes at 1 Year after Hematopoietic Stem Cell Transplantation in a Heterogeneous Pediatric Population. Transplant Cell Ther. 2022;28:44.e41–44.e46. [DOI] [PubMed] [Google Scholar]
- 221.Schulte CM, Beelen DW. Bone loss following hematopoietic stem cell transplantation: a long-term follow-up. Blood. 2004;103:3635–3643. [DOI] [PubMed] [Google Scholar]
- 222.Yao S, Smiley SL, West K, et al. Accelerated bone mineral density loss occurs with similar incidence and severity, but with different risk factors, after autologous versus allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2010;16:1130–1137. [DOI] [PubMed] [Google Scholar]
- 223.Petryk A, Polgreen LE, Zhang L, et al. Bone mineral deficits in recipients of hematopoietic cell transplantation: the impact of young age at transplant. Bone Marrow Transplant. 2014;49:258–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.McClune BL, Polgreen LE, Burmeister LA, et al. Screening, prevention and management of osteoporosis and bone loss in adult and pediatric hematopoietic cell transplant recipients. Bone Marrow Transplant. 2011;46:1–9. [DOI] [PubMed] [Google Scholar]
- 225.McClune B, Majhail NS, Flowers ME. Bone loss and avascular necrosis of bone after hematopoietic cell transplantation. Semin Hematol. 2012;49:59–65. [DOI] [PubMed] [Google Scholar]
- 226.Milner PF, Kraus AP, Sebes JI, et al. Sickle cell disease as a cause of osteonecrosis of the femoral head. N Engl J Med. 1991;325:1476–1481. [DOI] [PubMed] [Google Scholar]
- 227.Li X, Brazauskas R, Wang Z, et al. Avascular necrosis of bone after allogeneic hematopoietic cell transplantation in children and adolescents. Biol Blood Marrow Transplant. 2014;20:587–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Law AD, Bhella S, Pasic I, et al. Moderate-severe grade of chronic graft versus host disease and younger age (less than 45 years old) are risk factors for avascular necrosis in adult patients undergoing allogeneic hematopoietic cell transplantation. Ann Hematol. 2021;100:1311–1319. [DOI] [PubMed] [Google Scholar]
- 229.Lee CJ, Kim S, Tecca HR, et al. Late effects after ablative allogeneic stem cell transplantation for adolescent and young adult acute myeloid leukemia. Blood Adv. 2020;4:983–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Socie G, Cahn JY, Carmelo J, et al. Avascular necrosis of bone after allogeneic bone marrow transplantation: analysis of risk factors for 4388 patients by the Societe Francaise de Greffe de Moelle (SFGM). Br J Haematol. 1997;97:865–870. [DOI] [PubMed] [Google Scholar]
- 231.McAvoy S, Baker KS, Mulrooney D, et al. Corticosteroid dose as a risk factor for avascular necrosis of the bone after hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2010;16:1231–1236. [DOI] [PubMed] [Google Scholar]
- 232.Carpenter PA. How I conduct a comprehensive chronic graft-versus-host disease assessment. Blood. 2011;118:2679–2687. [DOI] [PubMed] [Google Scholar]
- 233.Couriel D, Carpenter PA, Cutler C, et al. Ancillary therapy and supportive care of chronic graft-versus-host disease: national institutes of health consensus development project on criteria for clinical trials in chronic Graft-versus-host disease: V. Ancillary Therapy and Supportive Care Working Group Report. Biol Blood Marrow Transplant. 2006;12:375–396. [DOI] [PubMed] [Google Scholar]
- 234.Sarantopoulos S, Cardones AR, Sullivan KM. How I treat refractory chronic graft-versus-host disease. Blood. 2019;133:1191–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.de Brabander C, Cornelissen J, Smitt PA, Vecht CJ, van den Bent MJ. Increased incidence of neurological complications in patients receiving an allogenic bone marrow transplantation from alternative donors. J Neurol Neurosurg Psychiatry. 2000;68:36–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Sostak P, Padovan CS, Yousry TA, Ledderose G, Kolb HJ, Straube A. Prospective evaluation of neurological complications after allogeneic bone marrow transplantation. Neurology. 2003;60:842–848. [DOI] [PubMed] [Google Scholar]
- 237.Lehky T, Fernandez IP, Krakow EF, et al. Neuropathy and Muscle Cramps in Autologous and Allogeneic Hematopoietic Cell Transplantation Survivors. Transplant Cell Ther. 2022;28:608.e601–608.e609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Dowling MR, Li S, Dey BR, et al. Neurologic complications after allogeneic hematopoietic stem cell transplantation: risk factors and impact. Bone Marrow Transplant. 2018;53:199–206. [DOI] [PubMed] [Google Scholar]
- 239.Pihusch R, Salat C, Schmidt E, et al. Hemostatic complications in bone marrow transplantation: a retrospective analysis of 447 patients. Transplantation. 2002;74:1303–1309. [DOI] [PubMed] [Google Scholar]
- 240.Labrador J, Lopez-Anglada L, Perez-Lopez E, et al. Analysis of incidence, risk factors and clinical outcome of thromboembolic and bleeding events in 431 allogeneic hematopoietic stem cell transplantation recipients. Haematologica. 2013;98:437–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Bruno B, Gooley T, Sullivan KM, et al. Secondary failure of platelet recovery after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2001;7:154–162. [DOI] [PubMed] [Google Scholar]
- 242.Coplin WM, Cochran MS, Levine SR, Crawford SW. Stroke after bone marrow transplantation: frequency, aetiology and outcome. Brain. 2001;124:1043–1051. [DOI] [PubMed] [Google Scholar]
- 243.Gangaraju R, Chen Y, Hageman L, et al. Stroke Risk in Blood or Marrow Transplant (BMT) Survivors-a Report from the BMT Survivor Study (BMTSS). Washington, DC: American Society of Hematology; 2019. [Google Scholar]
- 244.Kenney LB, Ames BL, Huang MS, et al. Consensus Recommendations for Managing Childhood Cancer Survivors at Risk for Stroke After Cranial Irradiation: A Delphi Study. Neurology. 2022. [DOI] [PubMed] [Google Scholar]
- 245.Gurney JG, Tersak JM, Ness KK, et al. Hearing loss, quality of life, and academic problems in long-term neuroblastoma survivors: a report from the Children’s Oncology Group. Pediatrics. 2007;120:e1229–e1236. [DOI] [PubMed] [Google Scholar]
- 246.Holmqvist AS, Chen YJ, Wu J, et al. Severe/Life-Threatening/Fatal Chronic Health Conditions (CHCs) after Allogeneic Blood or Marrow Transplantation (BMT) in Childhood - a Report from the BMT Survivor Study (BMTSS). Blood. 2020;136:12–13. [Google Scholar]
- 247.Przybylyski A, Esper P. Early Recognition and Management of Posterior Reversible Encephalopathy Syndrome: A Newly Recognized Complication in Patients Receiving Tyrosine Kinase Inhibitors. Clinical Journal of Oncology Nursing. 2016;20:305–308. [DOI] [PubMed] [Google Scholar]
- 248.Tavil B, Isgandarova F, Bayhan T, et al. Sorafenib-induced Posterior Reversible Encephalopathy Syndrome in a Child With FLT3-ITD-positive Acute Myeloid Leukemia. J Pediatr Hematol Oncol. 2016;38:240–242. [DOI] [PubMed] [Google Scholar]
- 249.Goebeler ME, Knop S, Viardot A, et al. Bispecific T-Cell Engager (BiTE) Antibody Construct Blinatumomab for the Treatment of Patients With Relapsed/Refractory Non-Hodgkin Lymphoma: Final Results From a Phase I Study. J Clin Oncol. 2016;34:1104–1111. [DOI] [PubMed] [Google Scholar]
- 250.Carson KR, Evens AM, Richey EA, et al. Progressive multifocal leukoencephalopathy after rituximab therapy in HIV-negative patients: a report of 57 cases from the Research on Adverse Drug Events and Reports project. Blood. 2009;113:4834–4840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Isidoro L, Pires P, Rito L, Cordeiro G. Progressive multifocal leukoencephalopathy in a patient with chronic lymphocytic leukaemia treated with alemtuzumab. BMJ Case Rep. 2014;2014: bcr2013201781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Takao M. [Targeted therapy and progressive multifocal leukoencephalopathy (PML): PML in the era of monoclonal antibody therapies]. Brain Nerve. 2013;65:1363–1374. [PubMed] [Google Scholar]
- 253.Ogata M, Fukuda T, Teshima T. Human herpesvirus-6 encephalitis after allogeneic hematopoietic cell transplantation: what we do and do not know. Bone marrow transplantation. 2015;50:1030–1036. [DOI] [PubMed] [Google Scholar]
- 254.Schmidt-Hieber M, Schwender J, Heinz WJ, et al. Viral encephalitis after allogeneic stem cell transplantation: a rare complication with distinct characteristics of different causative agents. Haematologica. 2011;96:142–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Syrjala KL, Langer SL, Abrams JR, Storer BE, Martin PJ. Late effects of hematopoietic cell transplantation among 10-year adult survivors compared with case-matched controls. J Clin Oncol. 2005;23:6596–6606. [DOI] [PubMed] [Google Scholar]
- 256.Syrjala KL, Artherholt SB, Kurland BF, et al. Prospective neurocognitive function over 5 years after allogeneic hematopoietic cell transplantation for cancer survivors compared with matched controls at 5 years. J Clin Oncol. 2011;29:2397–2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Buchbinder D, Kelly DL, Duarte RF, et al. Neurocognitive dysfunction in hematopoietic cell transplant recipients: expert review from the late effects and Quality of Life Working Committee of the CIBMTR and complications and Quality of Life Working Party of the EBMT. Bone Marrow Transplant. 2018;53:535–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Schofield HT, Fabrizio VA, Braniecki S, et al. Monitoring Neurocognitive Functioning After Pediatric Cellular Therapy or Hematopoietic Cell Transplant: Guidelines From the COG Neurocognition in Cellular Therapies Task Force. Transplant Cell Ther. 2022;28:625–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Lefvert AK, Bjorkholm M. Antibodies against the acetylcholine receptor in hematologic disorders: implications for the development of myasthenia gravis after bone marrow grafting. N Engl J Med. 1987;317:170. [DOI] [PubMed] [Google Scholar]
- 260.Romi F. Thymoma in myasthenia gravis: from diagnosis to treatment. Autoimmune Dis. 2011;2011: 474512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Tse S, Saunders EF, Silverman E, Vajsar J, Becker L, Meaney B. Myasthenia gravis and polymyositis as manifestations of chronic graft-versus-host-disease. Bone Marrow Transplantation. 1999;23:397–399. [DOI] [PubMed] [Google Scholar]
- 262.Dalakas MC. The role of high-dose immune globulin intravenous in the treatment of dermatomyositis. Int Immunopharmacol. 2006;6:550–556. [DOI] [PubMed] [Google Scholar]
- 263.Stephenson AL, Mackenzie IRA, Levy RD, Road J. Myositis associated graft-versus-host-disease presenting as respiratory muscle weakness. Thorax. 2001;56:82–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Choi W-C, Jung Y-H, Yang Y-I, Bae J-S. Polymyositis After Bone Marrow Transplantation: As an Uncommon Manifestation of Chronic Graft-Versus-Host Disease? or Autoimmune Process? Annals of Clinical Neurophysiology. 2011;13:58–60. [Google Scholar]
- 265.Matsuo Y, Kamezaki K, Takeishi S, et al. Encephalomyelitis mimicking multiple sclerosis associated with chronic graft-versus-host disease after allogeneic bone marrow transplantation. Intern Med. 2009;48:1453–1456. [DOI] [PubMed] [Google Scholar]
- 266.Sostak P, Padovan CS, Eigenbrod S, et al. Cerebral angiitis in four patients with chronic GVHD. Bone Marrow Transplant. 2010;45:1181–1188. [DOI] [PubMed] [Google Scholar]
- 267.Grauer O, Wolff D, Bertz H, et al. Neurological manifestations of chronic graft-versus-host disease after allogeneic haematopoietic stem cell transplantation: report from the Consensus Conference on Clinical Practice in chronic graft-versus-host disease. Brain. 2010;133:2852–2865. [DOI] [PubMed] [Google Scholar]
- 268.Sun CL, Francisco L, Baker KS, Weisdorf DJ, Forman SJ, Bhatia S. Adverse psychological outcomes in long-term survivors of hematopoietic cell transplantation: a report from the Bone Marrow Transplant Survivor Study (BMTSS). Blood. 2011;118:4723–4731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Fraser CJ, Bhatia S, Ness K, et al. Impact of chronic graft-versus-host disease on the health status of hematopoietic cell transplantation survivors: a report from the Bone Marrow Transplant Survivor Study. Blood. 2006;108:2867–2873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Esser P, Kuba K, Scherwath A, et al. Stability and Priority of Symptoms and Symptom Clusters Among Allogeneic HSCT Patients Within a 5-Year Longitudinal Study. Journal of pain and symptom management. 2017;54:493–500. [DOI] [PubMed] [Google Scholar]
- 271.Esser P, Kuba K, Mehnert A, et al. Investigating the temporal course, relevance and risk factors of fatigue over 5 years: a prospective study among patients receiving allogeneic HSCT. Bone Marrow Transplant. 2017;52:753–758. [DOI] [PubMed] [Google Scholar]
- 272.Esser P, Kuba K, Scherwath A, et al. Posttraumatic stress disorder symptomatology in the course of allogeneic HSCT: a prospective study. Journal of Cancer Survivorship. 2017;11:203–210. [DOI] [PubMed] [Google Scholar]
- 273.Kuba K, Esser P, Mehnert A, et al. Depression and anxiety following hematopoietic stem cell transplantation: a prospective population-based study in Germany. Bone Marrow Transplant. 2017;52:1651–1657. [DOI] [PubMed] [Google Scholar]
- 274.Mosher CE, DuHamel KN, Rini C, Corner G, Lam J, Redd WH. Quality of life concerns and depression among hematopoietic stem cell transplant survivors. Support Care Cancer. 2011;19:1357–1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Andrykowski MA, Bishop MM, Hahn EA, et al. Long-term health-related quality of life, growth, and spiritual well-being after hematopoietic stem-cell transplantation. J Clin Oncol. 2005;23:599–608. [DOI] [PubMed] [Google Scholar]
- 276.Bhatt NS. Prevalence and Determinants of Return to Work as a Patient-Centered Outcome in Survivors of Hematopoietic Cell Transplantation. Current hematologic malignancy reports. 2022;17:228–242. [DOI] [PubMed] [Google Scholar]
- 277.Syrjala KL, Langer SL, Abrams JR, et al. Recovery and long-term function after hematopoietic cell transplantation for leukemia or lymphoma. JAMA. 2004;291:2335–2343. [DOI] [PubMed] [Google Scholar]
- 278.Bush NE, Donaldson GW, Haberman MH, Dacanay R, Sullivan KM. Conditional and unconditional estimation of multidimensional quality of life after hematopoietic stem cell transplantation: A longitudinal follow-up of 415 patients. Biology of Blood and Marrow Transplantation. 2000;6:576–591. [DOI] [PubMed] [Google Scholar]
- 279.Tichelli A, Gerull S, Holbro A, et al. Inability to work and need for disability pension among long-term survivors of hematopoietic stem cell transplantation. Bone Marrow Transplantation. 2017;52:1436. [DOI] [PubMed] [Google Scholar]
- 280.Bieri S, Roosnek E, Helg C, et al. Quality of life and social integration after allogeneic hematopoietic SCT. Bone Marrow Transplant. 2008;42:819–827. [DOI] [PubMed] [Google Scholar]
- 281.Wong FL, Francisco L, Togawa K, et al. Long-term recovery after hematopoietic cell transplantation: predictors of quality-of-life concerns. Blood. 2010;115:2508–2519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Heinonen H, Volin L, Uutela A, Zevon M, Barrick C, Ruutu T. Quality of life and factors related to perceived satisfaction with quality of life after allogeneic bone marrow transplantation. Ann Hematol. 2001;80:137–143. [DOI] [PubMed] [Google Scholar]
- 283.Morrison EJ, Ehlers SL, Bronars CA, et al. Employment Status as an Indicator of Recovery and Function One Year after Hematopoietic Stem Cell Transplantation. Biol Blood Marrow Transplant. 2016;22:1690–1695. [DOI] [PubMed] [Google Scholar]
- 284.Bhatt NS, Brazauskas R, Salit RB, et al. Return to Work Among Young Adult Survivors of Allogeneic Hematopoietic Cell Transplantation in the United States. Transplant Cell Ther. 2021;27:679.e671–679.e678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Hahn T, Paplham P, Austin-Ketch T, et al. Ascertainment of Unmet Needs and Participation in Health Maintenance and Screening of Adult Hematopoietic Cell Transplantation Survivors Followed in a Formal Survivorship Program. Biol Blood Marrow Transplant. 2017;23:1968–1973. [DOI] [PubMed] [Google Scholar]
- 286.Grulke N, Albani C, Bailer H. Quality of life in patients before and after haematopoietic stem cell transplantation measured with the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Core Questionnaire QLQ-C30. Bone Marrow Transplant. 2012;47:473–482. [DOI] [PubMed] [Google Scholar]
- 287.Lof CM, Winiarski J, Ljungman P, Forinder U. The socio-economic and psychosocial circumstances of adult long-term survivors of hematopoietic stem cell transplantation in childhood. Pediatr Transplant. 2011;15:691–698. [DOI] [PubMed] [Google Scholar]
- 288.Parisek M, Loss J, Holler E, et al. “This Graft-vs.-Host Disease Determines My Life. That’s It.”-A Qualitative Analysis of the Experiences and Needs of Allogenic Hematopoietic Stem Cells Transplantation Survivors in Germany. Front Public Health. 2021;9: 687675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Hamilton BK, Rybicki L, Dabney J, et al. Quality of life and outcomes in patients⩾60 years of age after allogeneic hematopoietic cell transplantation. Bone Marrow Transplantation. 2014;49:1426–1431. [DOI] [PubMed] [Google Scholar]
- 290.Gruber U, Fegg M, Buchmann M, Kolb HJ, Hiddemann W. The long-term psychosocial effects of haematopoetic stem cell transplantation. Eur J Cancer Care (Engl). 2003;12:249–256. [PubMed] [Google Scholar]
- 291.Kurosawa S, Yamaguchi T, Oshima K, et al. Employment status was highly associated with quality of life after allogeneic hematopoietic cell transplantation, and the association may differ according to patient age and graft-versus-host disease status: analysis of a nationwide QOL survey. Bone Marrow Transplant. 2019;54:611–615. [DOI] [PubMed] [Google Scholar]
- 292.Hamilton BK, Rybicki L, Arai S, et al. Association of Socioeconomic Status with Chronic Graft-versus-Host Disease Outcomes. Biol Blood Marrow Transplant. 2018;24:393–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Worel N, Biener D, Kalhs P, et al. Long-term outcome and quality of life of patients who are alive and in complete remission more than two years after allogeneic and syngeneic stem cell transplantation. Bone Marrow Transplant. 2002;30:619–626. [DOI] [PubMed] [Google Scholar]
- 294.Boberg E, Kadri N, Winterling J, et al. Mental fatigue after allogeneic hematopoietic stem cell transplantation is associated with cognitive dysfunction, but not central nervous system inflammation. Haematologica. 2020;105:e310–e314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.!!! INVALID CITATION !!!.
- 296.Hong S, Rybicki L, Abounader DM, et al. Association of socioeconomic status with autologous hematopoietic cell transplantation outcomes for lymphoma. Bone Marrow Transplant. 2016;51:1191–1196. [DOI] [PubMed] [Google Scholar]
- 297.Knight JM, Syrjala KL, Majhail NS, et al. Patient-Reported Outcomes and Socioeconomic Status as Predictors of Clinical Outcomes after Hematopoietic Stem Cell Transplantation: A Study from the Blood and Marrow Transplant Clinical Trials Network 0902 Trial. Biol Blood Marrow Transplant. 2016;22:2256–2263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Sun CL, Kersey JH, Francisco L, et al. Burden of morbidity in 10+ year survivors of hematopoietic cell transplantation: report from the bone marrow transplantation survivor study. Biol Blood Marrow Transplant. 2013;19:1073–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Shaw BE, Lee SJ, Horowitz MM, Wood WA, Rizzo JD, Flynn KE. Can we agree on patient-reported outcome measures for assessing hematopoietic cell transplantation patients? A study from the CIBMTR and BMT CTN. Bone Marrow Transplant. 2016;51:1173–1179. [DOI] [PubMed] [Google Scholar]
- 300.Shaw BE, Brazauskas R, Millard HR, et al. Centralized patient-reported outcome data collection in transplantation is feasible and clinically meaningful. Cancer. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.NCCN Guidelines Version 2. Distress Management; 2021. [Google Scholar]
- 302.The NCCN survivorship guidelines (version 3.2021). [Google Scholar]
- 303.Buchbinder D, Patel SK, Casillas JN, et al. Parent proxy assessment of sibling quality of life following pediatric hematopoietic cell transplantation. Health Qual Life Outcomes. 2019;17:162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Gizli Coban O, Surer Adanir A, Ozatalay E. Post-traumatic stress disorder and health-related quality of life in the siblings of the pediatric bone marrow transplantation survivors and post-traumatic stress disorder in their mothers. Pediatr Transplant. 2017;21:e13003. [DOI] [PubMed] [Google Scholar]
- 305.Posluszny DM, Bovbjerg DH, Syrjala KL, Agha M, Dew MA. Correlates of anxiety and depression symptoms among patients and their family caregivers prior to allogeneic hematopoietic cell transplant for hematological malignancies. Support Care Cancer. 2019;27:591–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Sannes TS, Simoneau TL, Mikulich-Gilbertson SK, et al. Distress and quality of life in patient and caregiver dyads facing stem cell transplant: identifying overlap and unique contributions. Support Care Cancer. 2019;27:2329–2337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Salit RB, Lee SJ, Burns LJ, et al. Return-to-Work Guidelines and Programs for Post-Hematopoietic Cell Transplantation Survivors: An Initial Survey. Biology of Blood and Marrow Transplantation. 2020;26:1520–1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Salit RB, Schoeppner K, De Biase C, et al. American Society for Transplantation and Cellular Therapy Return to Work Guidance Committee Recommendations for Health Care Providers Who Take Care of Hematopoietic Cell Transplantation Patients. Transplant Cell Ther. 2022;28:822–828. [DOI] [PubMed] [Google Scholar]
- 309.Socie G, Baker KS, Bhatia S. Subsequent malignant neoplasms after hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2012;18:S139–S150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Metayer C, Curtis RE, Vose J, et al. Myelodysplastic syndrome and acute myeloid leukemia after autotransplantation for lymphoma: a multicenter case-control study. Blood. 2003;101:2015–2023. [DOI] [PubMed] [Google Scholar]
- 311.Bhatia S, Armenian SH, Landier W. How I monitor long-term and late effects after blood or marrow transplantation. Blood, The Journal of the American Society of Hematology. 2017;130:1302–1314. [DOI] [PubMed] [Google Scholar]
- 312.Akhtari M, Bhatt VR, Tandra PK, et al. Therapy-related myeloid neoplasms after autologous hematopoietic stem cell transplantation in lymphoma patients. Cancer Biol Ther. 2013;14:1077–1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Wiseman DH. Donor cell leukemia: a review. Biol Blood Marrow Transplant. 2011;17:771–789. [DOI] [PubMed] [Google Scholar]
- 314.Williams L, Doucette K, Karp JE, Lai C. Genetics of donor cell leukemia in acute myelogenous leukemia and myelodysplastic syndrome. Bone Marrow Transplant. 2021;56:1535–1549. [DOI] [PubMed] [Google Scholar]
- 315.Radivoyevitch T, Dean RM, Shaw BE, et al. Risk of acute myeloid leukemia and myelodysplastic syndrome after autotransplants for lymphomas and plasma cell myeloma. Leuk Res. 2018;74:130–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Tarella C, Passera R, Magni M, et al. Risk factors for the development of secondary malignancy after high-dose chemotherapy and autograft, with or without rituximab: a 20-year retrospective follow-up study in patients with lymphoma. J Clin Oncol. 2011;29:814–824. [DOI] [PubMed] [Google Scholar]
- 317.Soerensen JF, Aggerholm A, Kerndrup GB, et al. Clonal hematopoiesis predicts development of therapy-related myeloid neoplasms post-autologous stem cell transplantation. Blood Adv. 2020;4:885–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Nadiminti K, Sidiqi MH, Meleveedu K, et al. Characteristics and outcomes of therapy-related myeloid neoplasms following autologous stem cell transplantation for multiple myeloma. Blood Cancer J. 2021;11:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Landgren O, Gilbert ES, Rizzo JD, et al. Risk factors for lymphoproliferative disorders after allogeneic hematopoietic cell transplantation. Blood. 2009;113:4992–5001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Styczynski J, van der Velden W, Fox CP, et al. Management of Epstein-Barr Virus infections and post-transplant lymphoproliferative disorders in patients after allogeneic hematopoietic stem cell transplantation: Sixth European Conference on Infections in Leukemia (ECIL-6) guidelines. Haematologica. 2016;101:803–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Bilmon IA, Ashton LJ, Le Marsney RE, et al. Second cancer risk in adults receiving autologous haematopoietic SCT for cancer: a population-based cohort study. Bone Marrow Transplant. 2014;49:691–698. [DOI] [PubMed] [Google Scholar]
- 322.Bomken S, Skinner R. Secondary Malignant Neoplasms Following Haematopoietic Stem Cell Transplantation in Childhood. Children (Basel). 2015;2:146–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Cohen A, Rovelli A, Merlo DF, et al. Risk for secondary thyroid carcinoma after hematopoietic stem-cell transplantation: an EBMT Late Effects Working Party Study. J Clin Oncol. 2007;25:2449–2454. [DOI] [PubMed] [Google Scholar]
- 324.Yabe M, Morio T, Tabuchi K, et al. Long-term outcome in patients with Fanconi anemia who received hematopoietic stem cell transplantation: a retrospective nationwide analysis. Int J Hematol. 2021;113:134–144. [DOI] [PubMed] [Google Scholar]
- 325.Anak S, Yalman N, Bilgen H, et al. Squamous cell carcinoma development in Fanconi anemia patients who underwent hematopoietic stem cell transplantation. Pediatr Transplant. 2020;24:e13706. [DOI] [PubMed] [Google Scholar]
- 326.Danylesko I, Shimoni A. Second Malignancies after Hematopoietic Stem Cell Transplantation. Curr Treat Options Oncol. 2018;19:9. [DOI] [PubMed] [Google Scholar]
- 327.Ringden O, Brazauskas R, Wang Z, et al. Second solid cancers after allogeneic hematopoietic cell transplantation using reduced-intensity conditioning. Biol Blood Marrow Transplant. 2014;20:1777–1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Tanaka Y, Kurosawa S, Tajima K, et al. Increased incidence of oral and gastrointestinal secondary cancer after allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2017;52:789–791. [DOI] [PubMed] [Google Scholar]
- 329.Knight B, Anderson L, Lerner D, Phelan R, Thakar MS. Case Series: Development of Polyps as a Late Effect After Total Body Irradiation-based Hematopoietic Cell Transplantation in Children With High-risk Leukemia. Journal of Pediatric Hematology Oncology. 2021;43:E1159–E1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Mulder RL, Kremer LC, Hudson MM, et al. Recommendations for breast cancer surveillance for female survivors of childhood, adolescent, and young adult cancer given chest radiation: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Oncol. 2013;14:e621–e629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Moskowitz CS, Chou JF, Wolden SL, et al. Breast cancer after chest radiation therapy for childhood cancer. J Clin Oncol. 2014;32:2217–2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.McDonald AM, Chen Y, Wu J, et al. Total Body Irradiation and Risk of Breast Cancer After Blood or Marrow Transplantation: A Blood or Marrow Transplantation Survivor Study Report. J Clin Oncol. 2020;38:2872–2882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Wang Y, Reulen RC, Kremer LCM, et al. Male breast cancer after childhood cancer: Systematic review and analyses in the PanCareSurFup cohort. Eur J Cancer. 2022;165:27–47. [DOI] [PubMed] [Google Scholar]
- 334.Moskowitz CS, Chou JF, Sklar CA, et al. Radiation-associated breast cancer and gonadal hormone exposure: a report from the Childhood Cancer Survivor Study. Br J Cancer. 2017;117:290–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Mulder RL, Hudson MM, Bhatia S, et al. Updated Breast Cancer Surveillance Recommendations for Female Survivors of Childhood, Adolescent, and Young Adult Cancer From the International Guideline Harmonization Group. J Clin Oncol. 2020;38:4194–4207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Szlauer-Stefanska A, Kaminska-Winciorek G, Giebel S, Baglaj M. Secondary skin neoplasms in patients after autologous and allogeneic hematopoietic stem cell transplantation procedures. Adv Clin Exp Med. 2020;29:1221–1230. [DOI] [PubMed] [Google Scholar]
- 337.Herr MM, Curtis RE, Tucker MA, et al. Risk factors for the development of cutaneous melanoma after allogeneic hematopoietic cell transplantation. J Am Acad Dermatol. 2020;83:762–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Bowers DC, Nathan PC, Constine L, et al. Subsequent neoplasms of the CNS among survivors of childhood cancer: a systematic review. The Lancet Oncology. 2013;14:e321–e328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Meignin V, Gluckman E, Gambaraelli D, et al. Meningioma in long-term survivors after allogeneic bone marrow transplantation. Bone Marrow Transplant. 1998;22:723–724. [DOI] [PubMed] [Google Scholar]
- 340.Schmiegelow K, Levinsen MF, Attarbaschi A, et al. Second malignant neoplasms after treatment of childhood acute lymphoblastic leukemia. J Clin Oncol. 2013;31:2469–2476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Danner-Koptik KE, Majhail NS, Brazauskas R, et al. Second malignancies after autologous hematopoietic cell transplantation in children. Bone Marrow Transplant. 2013;48:363–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Inamoto Y, Shah NN, Savani BN, et al. Secondary solid cancer screening following hematopoietic cell transplantation. Bone Marrow Transplant. 2015;50:1013–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.FACT-JACIE. FACT-JACIE International Standards for Hemopoietic Cellular Therapy Product Collection, Processing, and Administration. Seventh Edition 2018. [Google Scholar]
- 344.Morrison CF, Pai ALH, Martsolf D. Facilitators and Barriers to Self-Management for Adolescents and Young Adults Following a Hematopoietic Stem Cell Transplant [Formula: see text]. Journal of pediatric oncology nursing: official journal of the Association of Pediatric Oncology Nurses. 2018;35:36–42. [DOI] [PubMed] [Google Scholar]
- 345.Dyer G, Gilroy N, Brown L, et al. What They Want: Inclusion of Blood and Marrow Transplantation Survivor Preference in the Development of Models of Care for Long-Term Health in Sydney, Australia. Biol Blood Marrow Transplant. 2016;22:731–743. [DOI] [PubMed] [Google Scholar]
- 346.Majhail NS, Mau LW, Chitphakdithai P, et al. Transplant center characteristics and survival after allogeneic hematopoietic cell transplantation in adults. Bone Marrow Transplant. 2020;55:906–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Hashmi SK, Lee SJ, Savani BN, et al. ASBMT Practice Guidelines Committee Survey on Long-Term Follow-Up Clinics for Hematopoietic Cell Transplant Survivors. Biol Blood Marrow Transplant. 2018;24:1119–1124. [DOI] [PubMed] [Google Scholar]
- 348.Kapadia M, Lehmann L, Auletta J, et al. Quality Improvement in Hematopoietic Stem Cell Transplant and Cellular Therapy: Using the Model for Improvement to impact Outcomes. Transplant Cell Ther. 2022;28:233–241. [DOI] [PubMed] [Google Scholar]
- 349.Armenian SH, Sun CL, Francisco L, et al. Health behaviors and cancer screening practices in long-term survivors of hematopoietic cell transplantation (HCT): a report from the BMT Survivor Study. Bone Marrow Transplant. 2012;47:283–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Thaw SS, Holtan S, Cao Q, Franklin M, Paye N, Blaes A. Inadequate survivorship care after allogeneic hematopoietic cell transplantation: A retrospective chart review. F1000Research. 2018;7:1389. [Google Scholar]
- 351.Majhail NS, Murphy E, Laud P, et al. Randomized controlled trial of individualized treatment summary and survivorship care plans for hematopoietic cell transplantation survivors. Haematologica. 2019;104:1084–1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Syrjala KL, Yi JC, Artherholt SB, et al. An online randomized controlled trial, with or without problem solving treatment, for long-term cancer survivors after hematopoietic cell transplantation. J Cancer Surviv. 2018;12:560–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Nawas MT, Landau HJ, Sauter CS, et al. Pilot Study of Telehealth Evaluations in Patients Undergoing Hematopoietic Cell Transplantation. Biol Blood Marrow Transplant. 2020;26:e135–e137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Chang E, Iukuridze A, Echevarria M, et al. Feasibility and Acceptability of Using a Telehealth Platform to Monitor Cardiovascular Risk Factors in Hematopoietic Cell Transplantation Survivors at Risk for Cardiovascular Disease. Biol Blood Marrow Transplant. 2020;26:1233–1237. [DOI] [PubMed] [Google Scholar]
- 355.Racioppi A, Dalton T, Ramalingam S, et al. Assessing the Feasibility of a Novel mHealth App in Hematopoietic Stem Cell Transplant Patients. Transplant Cell Ther. 2021;27:181.e181–181.e189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Leppla L, Schmid A, Valenta S, et al. Development of an integrated model of care for allogeneic stem cell transplantation facilitated by eHealth-the SMILe study. Support Care Cancer. 2021;29:8045–8057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Syrjala KL, Crouch ML, Leisenring WM, et al. Engagement with INSPIRE, an Online Program for Hematopoietic Cell Transplantation Survivors. Biol Blood Marrow Transplant. 2018;24:1692–1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Leppla L, Mielke J, Kunze M, et al. Clinicians and patients perspectives on follow-up care and eHealth support after allogeneic hematopoietic stem cell transplantation: A mixed-methods contextual analysis as part of the SMILe study. European journal of oncology nursing: the official journal of European Oncology Nursing Society. 2020;45: 101723. [DOI] [PubMed] [Google Scholar]
- 359.Chang LS, Barroso-Sousa R, Tolaney SM, Hodi FS, Kaiser UB, Min L. Endocrine Toxicity of Cancer Immunotherapy Targeting Immune Checkpoints. Endocr Rev. 2019;40:17–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Jones RJ, DeBaun MR. Leukemia after gene therapy for sickle cell disease: insertional mutagenesis, busulfan, both, or neither. Blood. 2021;138:942–947. [DOI] [PubMed] [Google Scholar]
- 361.Tucci F, Galimberti S, Naldini L, Valsecchi MG, Aiuti A. A systematic review and meta-analysis of gene therapy with hematopoietic stem and progenitor cells for monogenic disorders. Nat Commun. 2022;13:1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Jarisch A, Salzmann-Manrique E, Cario H, et al. Serum ferritin is not a reliable predictor to determine iron overload in thalassemia major patients post-hematopoietic stem cell transplantation. Eur J Haematol. 2018;101:791–797. [DOI] [PubMed] [Google Scholar]
- 363.Pepe A, Pistoia L, Gamberini MR, et al. The Close Link of Pancreatic Iron With Glucose Metabolism and With Cardiac Complications in Thalassemia Major: A Large, Multicenter Observational Study. Diabetes Care. 2020;43:2830–2839. [DOI] [PubMed] [Google Scholar]
- 364.Bardi E, Mulder RL, van Dalen EC, et al. Late hepatic toxicity surveillance for survivors of childhood, adolescent and young adult cancer: Recommendations from the international late effects of childhood cancer guideline harmonization group. Cancer Treat Rev. 2021;100: 102296. [DOI] [PubMed] [Google Scholar]
- 365.Aboobacker FN, Dixit G, Lakshmi KM, et al. Outcome of iron reduction therapy in ex-thalassemics. PLoS One. 2021;16:e0238793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Lyman GH, Bohlke K, Khorana AA, et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: american society of clinical oncology clinical practice guideline update 2014. J Clin Oncol. 2015;33:654–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Group IMW. IMWG guidelines for the prevention of thalidomide and lenalidomide-associated thrombosis in myeloma. 2022. Vol. [DOI] [PubMed] [Google Scholar]
- 368.Carpenter PA, Englund JA. Commentary: Is Immune Recovery-Based Post-Transplantation Vaccination in Children Better Than Time-Based Revaccination? Transplantation and Cellular Therapy, Official Publication of the American Society for Transplantation and Cellular Therapy. 2021;27:281–283. [DOI] [PubMed] [Google Scholar]
- 369.Kitko CL, Pidala J, Schoemans HM, et al. National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft-versus-Host Disease: IIa. The 2020 Clinical Implementation and Early Diagnosis Working Group Report. Transplant Cell Ther. 2021;27:545–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Flowers ME, Inamoto Y, Carpenter PA, et al. Comparative analysis of risk factors for acute graft-versus-host disease and for chronic graft-versus-host disease according to National Institutes of Health consensus criteria. Blood. 2011;117:3214–3219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Hölttä P, Alaluusua S, Saarinen-Pihkala UM, Peltola J, Hovi L. Agenesis and microdontia of permanent teeth as late adverse effects after stem cell transplantation in young children. Cancer. 2005;103:181–190. [DOI] [PubMed] [Google Scholar]
- 372.Hildebrandt GC, Fazekas T, Lawitschka A, et al. Diagnosis and treatment of pulmonary chronic GVHD: report from the consensus conference on clinical practice in chronic GVHD. Bone Marrow Transplant. 2011;46:1283–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Cheng GS, Selwa KE, Hatt C, et al. Multicenter evaluation of parametric response mapping as an indicator of bronchiolitis obliterans syndrome after hematopoietic stem cell transplantation. Am J Transplant. 2020;20:2198–2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Rayment JH, Sandoval RA, Roden JP, Schultz KR. Multiple Breath Washout Testing to Identify Pulmonary Chronic Graft Versus Host Disease in Children After Hematopoietic Stem Cell Transplantation. Transplant Cell Ther. 2022;28:328.e321–328.e327. [DOI] [PubMed] [Google Scholar]
- 375.Jamani K, He Q, Liu Y, et al. Early Post-Transplantation Spirometry Is Associated with the Development of Bronchiolitis Obliterans Syndrome after Allogeneic Hematopoietic Cell Transplantation. Biol Blood Marrow Transplant. 2020;26:943–948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Turner J, He Q, Baker K, et al. Home Spirometry Telemonitoring for Early Detection of Bronchiolitis Obliterans Syndrome in Patients with Chronic Graft-versus-Host Disease. Transplant Cell Ther. 2021;27:616.e611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Cheng GS, Storer B, Chien JW, et al. Lung Function Trajectory in Bronchiolitis Obliterans Syndrome after Allogeneic Hematopoietic Cell Transplant. Ann Am Thorac Soc. 2016;13:1932–1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Dietz AC, Mehta PA, Vlachos A, et al. Current Knowledge and Priorities for Future Research in Late Effects after Hematopoietic Cell Transplantation for Inherited Bone Marrow Failure Syndromes: Consensus Statement from the Second Pediatric Blood and Marrow Transplant Consortium International Conference on Late Effects after Pediatric Hematopoietic Cell Transplantation. Biol Blood Marrow Transplant. 2017;23:726–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Schmitz KH, Courneya KS, Matthews C, et al. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc. 2010;42:1409–1426. [DOI] [PubMed] [Google Scholar]
- 380.DeFilipp Z, Duarte RF, Snowden JA, et al. Metabolic syndrome and cardiovascular disease following hematopoietic cell transplantation: screening and preventive practice recommendations from CIBMTR and EBMT. Bone Marrow Transplant. 2017;52:173–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381.Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020;75:1334–1357. [DOI] [PubMed] [Google Scholar]
- 382.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology. 2019;74:e177–e232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Feijen EAM, Leisenring WM, Stratton KL, et al. Derivation of Anthracycline and Anthraquinone Equivalence Ratios to Doxorubicin for Late-Onset Cardiotoxicity. JAMA Oncol. 2019;5:864–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384.Armenian SH, Hudson MM, Mulder RL, et al. Recommendations for cardiomyopathy surveillance for survivors of childhood cancer: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Oncol. 2015;16: e123–e136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Survivorship. Vol 2022. Version 1.2022 ed2022. [Google Scholar]
- 386.Terrault NA, Lok ASF, McMahon BJ, et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67:1560–1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Kusumoto S, Tanaka Y, Suzuki R, et al. Monitoring of hepatitis B virus (HBV) DNA and risk of HBV reactivation in B-cell lymphoma: a prospective observational study. Clinical Infectious Diseases. 2015;61:719–729. [DOI] [PubMed] [Google Scholar]
- 388.Gentile G, Antonelli G. HBV Reactivation in Patients Undergoing Hematopoietic Stem Cell Transplantation: A Narrative Review. Viruses. 2019:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.AASLD/IDSA/IASeUSA. Recommendations for testing, managing, and treating hepatitis C. [Google Scholar]
- 390.Bruix J, Sherman M. American Association for the Study of Liver D. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.Chemaitilly W, Sklar CA. Endocrine complications of hematopoietic stem cell transplantation. Endocrinol Metab Clin North Am. 2007;36:983–998. ix. [DOI] [PubMed] [Google Scholar]
- 392.Chemaitilly W, Sklar CA. Endocrine Complications of Hematopoietic Stem Cell Transplantation. Endocrinology and Metabolism Clinics of North America. 2007;36:983–998. [DOI] [PubMed] [Google Scholar]
- 393.In: th Salooja N, Shoham Z, Dalle JH. Endocrine Disorders, Fertility and Sexual Health. In: Carreras Dufour, Mohty Kroger, eds. The EBMT Handbook: Hematopoietic Stem Cell Transplantation and Cellular Therapies. Cham (CH): Springer; Copyright 2019, EBMT and the Author(s); 2019:421–427. [PubMed] [Google Scholar]
- 394.Syrjala KL, Kurland BF, Abrams JR, Sanders JE, Heiman JR. Sexual function changes during the 5 years after high-dose treatment and hematopoietic cell transplantation for malignancy, with case-matched controls at 5 years. Blood. 2008;111:989–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.El-Jawahri A, Fishman SR, Vanderklish J, et al. Pilot study of a multimodal intervention to enhance sexual function in survivors of hematopoietic stem cell transplantation. Cancer. 2018;124:2438–2446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Brotto LA, Yule M, Breckon E. Psychological interventions for the sexual sequelae of cancer: a review of the literature. J Cancer Surviv. 2010;4:346–360. [DOI] [PubMed] [Google Scholar]
- 397.Meacham LR, Burns K, Orwig KE, Levine J. Standardizing Risk Assessment for Treatment-Related Gonadal Insufficiency and Infertility in Childhood Adolescent and Young Adult Cancer: The Pediatric Initiative Network Risk Stratification System. J Adolesc Young Adult Oncol. 2020;9:662–666. [DOI] [PubMed] [Google Scholar]
- 398.Bachrach LK, Gordon CM, Section On E. Bone Densitometry in Children and Adolescents. Pediatrics. 2016:138. [DOI] [PubMed] [Google Scholar]
- 399.Lewiecki EM, Laster AJ. Clinical review: Clinical applications of vertebral fracture assessment by dualenergy x-ray absorptiometry. J Clin Endocrinol Metab. 2006;91:4215–4222. [DOI] [PubMed] [Google Scholar]
- 400.Pundole X, Murphy WA, Ebede CC, et al. Fracture risk prediction using FRAX in patients following hematopoietic stem cell transplantation. Arch Osteoporos. 2018;13:38. [DOI] [PubMed] [Google Scholar]
- 401.Pundole X, Cheema HI, Petitto GS, Lopez-Olivo MA, Suarez-Almazor ME, Lu H. Prevention and treatment of bone loss and fractures in patients undergoing a hematopoietic stem cell transplant: a systematic review and meta-analysis. Bone Marrow Transplant. 2017;52:663–670. [DOI] [PubMed] [Google Scholar]
- 402.Anderson K, Ismaila N, Flynn PJ, et al. Role of Bone Modifying Agents in Multiple Myeloma: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol. 2018;36:812–818. [DOI] [PubMed] [Google Scholar]
- 403.Guffon N, Pettazzoni M, Pangaud N, et al. Long term disease burden post-transplantation: three decades of observations in 25 Hurler patients successfully treated with hematopoietic stem cell transplantation (HSCT). Orphanet J Rare Dis. 2021;16:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404.Eisengart JB, Rudser KD, Xue Y, et al. Long-term outcomes of systemic therapies for Hurler syndrome: an international multicenter comparison. Genet Med. 2018;20:1423–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.McClune B, Majhail NS, Flowers ME. Bone loss and avascular necrosis of bone after hematopoietic cell transplantation. Seminars in hematology. 2012;49:59–65. [DOI] [PubMed] [Google Scholar]
- 406.Inamoto Y, Martin PJ, Flowers ME, et al. Genetic risk factors for sclerotic graft-versus-host disease. Blood. 2016;128:1516–1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407.Martires KJ, Baird K, Steinberg SM, et al. Sclerotic-type chronic GVHD of the skin: clinical risk factors, laboratory markers, and burden of disease. Blood. 2011;118:4250–4257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Kuo CY, Garabedian E, Puck J, et al. Adenosine Deaminase (ADA)-Deficient Severe Combined Immune Deficiency (SCID) in the US Immunodeficiency Network (USIDNet) Registry. J Clin Immunol. 2020;40:1124–1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409.Bonfim C. Special pre- and posttransplant considerations in inherited bone marrow failure and hematopoietic malignancy predisposition syndromes. Hematology Am Soc Hematol Educ Program. 2020;2020:107–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410.Baker KS, Leisenring WM, Goodman PJ, et al. Total body irradiation dose and risk of subsequent neoplasms following allogeneic hematopoietic cell transplantation. Blood. 2019;133:2790–2799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 411.Tanaka Y, Kurosawa S, Tajima K, et al. Increased incidence of oral and gastrointestinal secondary cancer after allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplantation. 2017;52:789–791. [DOI] [PubMed] [Google Scholar]
- 412.Network. NCC. Breast Cancer Risk Reduction. NCCN Clinical Practice Guidelines in Oncology. 2021;2021. [Google Scholar]
- 413.Bozzuto LM. Breast Cancer Risk Reduction: who, why and what? Best Practice & Research Clinical Obstetrics & Gynaecology. 2021. [DOI] [PubMed] [Google Scholar]
- 414.Clement SC, Kremer LCM, Verburg FA, et al. Balancing the benefits and harms of thyroid cancer surveillance in survivors of Childhood, adolescent and young adult cancer: Recommendations from the international Late Effects of Childhood Cancer Guideline Harmonization Group in collaboration with the PanCareSurFup Consortium. Cancer Treat Rev. 2018;63:28–39. [DOI] [PubMed] [Google Scholar]
- 415.Alter BP, Rosenberg PS, Brody LC. Clinical and molecular features associated with biallelic mutations in FANCD1/BRCA2. J Med Genet. 2007;44:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416.Myers K, Davies SM, Harris RE, et al. The clinical phenotype of children with Fanconi anemia caused by biallelic FANCD1/BRCA2 mutations. Pediatr Blood Cancer. 2012;58:462–465. [DOI] [PubMed] [Google Scholar]
- 417.Reid S, Schindler D, Hanenberg H, et al. Biallelic mutations in PALB2 cause Fanconi anemia subtype FA-N and predispose to childhood cancer. Nat Genet. 2007;39:162–164. [DOI] [PubMed] [Google Scholar]
- 418.Wagner JE, Tolar J, Levran O, et al. Germline mutations in BRCA2: shared genetic susceptibility to breast cancer, early onset leukemia, and Fanconi anemia. Blood. 2004;103:3226–3229. [DOI] [PubMed] [Google Scholar]
- 419.Kratz CP, Achatz MI, Brugieres L, et al. Cancer Screening Recommendations for Individuals with Li-Fraumeni Syndrome. Clin Cancer Res. 2017;23:e38–e45. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


