Abstract
Purpose
Brachytherapy for gynecological cancer is reported to cause pain, anxiety, and distress with no clear guidance for optimizing patient experiences. The aim of this study was to explore patient experiences of brachytherapy and views on improvement.
Methods and Materials
Semistructured interviews were undertaken with patients who had received brachytherapy for locally advanced cervical cancer. Two cohorts were recruited: cohort 1 had recently had brachytherapy, and cohort 2 was a year post brachytherapy. Four recruitment sites were selected, where brachytherapy is given in different ways, some with short day case procedures and others having 1 or 2 overnight stays with applicators in place. Consecutive patients were invited to interview. Participants were asked to retell their brachytherapy story, with views on their care and ideas for improvement. Interviews were audio recorded, transcribed, and data analyzed following Braun and Clarke's method for reflexive thematic analysis.
Results
Thirty-five interviews were conducted (20 in cohort 1 and 15 in cohort 2). Participant's ages ranged from 28 to 87 years. The interview duration ranged from 22 to 78 minutes. Difficult and traumatic experiences were reported, including periods of severe pain and perceptions of poor care. However, some participants described positive experiences and what went well.
Three themes were developed: (1) how the patient got through it, (2) unpleasantness, discomfort, and the aftermath, and (3) emotional consequences and trauma. Some aspects of medium and long duration brachytherapy were found to be more problematic compared with short duration brachytherapy. Exploring experiences at 1-year post brachytherapy has provided insights into the long-lasting impact of brachytherapy experiences.
Conclusions
Hearing the patient voice has demonstrated that further work is needed to improve patient care in modern brachytherapy techniques using different regimens and durations, to minimize difficult and traumatic patient experiences. Study insights will inform future work to develop clinical care recommendations.
Introduction
Brachytherapy for locally advanced cervical cancer (LACC) requires patients to have brachytherapy applicators positioned inside their uterus and vagina and to remain lying flat and still on a bed for the duration of planning and treatment delivery. Currently, delivery of brachytherapy for LACC is not standardized. It may be given as 3- or 4-day case procedures or as 1 or 2 inpatient stays for up to 3 days where the applicators stay in place for this duration.
Over the last 2 decades, brachytherapy techniques for treatment of LACC have been increasing in complexity, including development of magnetic resonance (MR) image guided brachytherapy and the addition of interstitial brachytherapy techniques. International guidelines for the implementation of new brachytherapy techniques focus on achieving high radiation doses to tumors and reducing doses to normal pelvic tissue and have achieved improved local tumor control and survival rates while also reducing physical side effects of treatment.1, 2, 3, 4, 5, 6, 7, 8 Increased complexity in imaging, treatment planning, and types of applicators has led to development of new ways of delivering services, including adoption of different scheduling regimens. A United Kingdom (UK) survey of health care professionals identified 11 different brachytherapy schedules for LACC, with duration of applicators remaining in place ranging from 3 to 52 hours.9 The prolonged duration of applicators being in place has the potential to cause patient discomfort and trauma. The use of interstitial needles has been shown to cause more pain than intracavitary applicators alone.3,10,11 Some providers are exploring improvements to managing pain and immobilization for prolonged periods and for the different types of applicators being used,11, 12, 13 but there is currently no consensus on best practice.
Brachytherapy for gynecological cancer can cause pain, anxiety, and distress, and there is a need for better pain management and patient information and support.14 Kirchheiner et al15 reported that 41% of women experienced symptoms of posttraumatic stress disorder at 3 months after treatment, associated with the brachytherapy procedure.
In light of the rapidly developing LACC services with variations in service provision and treatment duration, it is important to explore the patient's experience of brachytherapy to inform optimal care. Therefore, the aim of this study was to explore patient experiences of brachytherapy for LACC and identify aspects of care requiring improvement, to inform the development of patient care recommendations in brachytherapy for LACC.
Methods and Materials
A qualitative research approach was appropriate to explore and make sense of patients’ accounts of their lived experiences of brachytherapy. Semistructured interviews were selected because they can generate rich and detailed responses that capture the complexity and meaning of patients’ experiences of brachytherapy, without making assumptions about the effect of duration or number of procedures in terms of pain, anxiety, and distress.16
To reflect the demographic of patients having brachytherapy for LACC, consecutive eligible patients were invited to interview. Accessibility and inclusivity were facilitated by use of an easy-to-read study flyer and participant information sheet and encouraging health care staff to approach every eligible patient. To understand the shorter and the longer-term impacts of brachytherapy for LACC, patients were recruited to 2 distinct cohorts at different timepoints after brachytherapy. To consider the effect on experiences related to treatment schedule variations, participants were recruited from 4 National Health Service (NHS) sites using different brachytherapy schedules, with sites identified from previous survey data.9 Potential participants for cohort 1 were screened and approached by members of the recruitment site team during radiation therapy, typically at last brachytherapy. For cohort 2, potential participants were screened and approached at follow-up appointments. Potential participants posted or emailed their contact details to the research team. Each recruitment site determined whether clinical staff or members of their research staff would screen, approach, and recruit participants.
Patients were eligible for inclusion in the study if they had received brachytherapy for LACC at 1 of the 4 recruitment sites, were available to be interviewed either up to 6 months (cohort 1) or 12 to 18 months (cohort 2) after brachytherapy, were over 18 years old, and were able to communicate verbally in English and had capacity to consent to take part in the study. Patients were excluded if they had a previous diagnosis of a major psychiatric disorder or progressive disease since brachytherapy, confirmed by the recruitment site team. Participants from cohort 1 were excluded from being interviewed a second time in cohort 2.
To determine sample size, an “information power” approach was used, considering factors such as the aim of the study, sample specificity, use of established theory, quality of dialogue, and analysis strategy.17 It was estimated that 24 to 40 patients across the 4 recruitment sites would generate enough in-depth, rich data to answer the research question. Interview data were reviewed during the recruitment period to ensure sufficient information power.
Approvals were obtained from the NHS Research Ethics Committee (REC), Health Research Authority and The University of the West of England Faculty Ethics Committee (REC reference: 19/WS/0080; protocol number: HAS-AHP-18-005; UWE REC REF No: HAS.19.06.206).
Participants gave written informed consent, posted or emailed to the research team. Interviews were audio recorded, transcribed verbatim, and imported into NVivo 12 Pro, which was used to store and organize data and collate coded text for analysis. Data analysis followed Braun and Clarke's 6-step process of reflexive thematic analysis, moving iteratively between the steps: familiarization with the data set; coding; generating initial themes; developing and reviewing themes; refining, defining, and naming themes; and writing up.16,18, 19, 20, 21 PH carried out all interviews, coding, and data analysis. Subsets of the interviews, initial coding, analytical observations, insights, and development of thematic maps and themes were discussed and reviewed with the PhD supervisory team (co-authors). This provided opportunities to explore alternative ways of making sense of the data and engaging more deeply with the data from multiple viewpoints.
Reflexivity
The first author (PH) is a therapeutic radiographer with 20 years clinical experience in brachytherapy. Involvement in the UK Brachytherapy Radiographers Forum had raised awareness of disparities in brachytherapy service provision and highlighted concerns about poor patient experiences as brachytherapy complexity and duration have increased. The first author PH undertook this study as part of a program of research for a National Institute of Health Research funded doctoral fellowship, with support from a PhD supervisory team and 2 patient research partners. Recruitment sites were selected to ensure that PH was not known to any study participants or involved in the delivery of their care.
Results
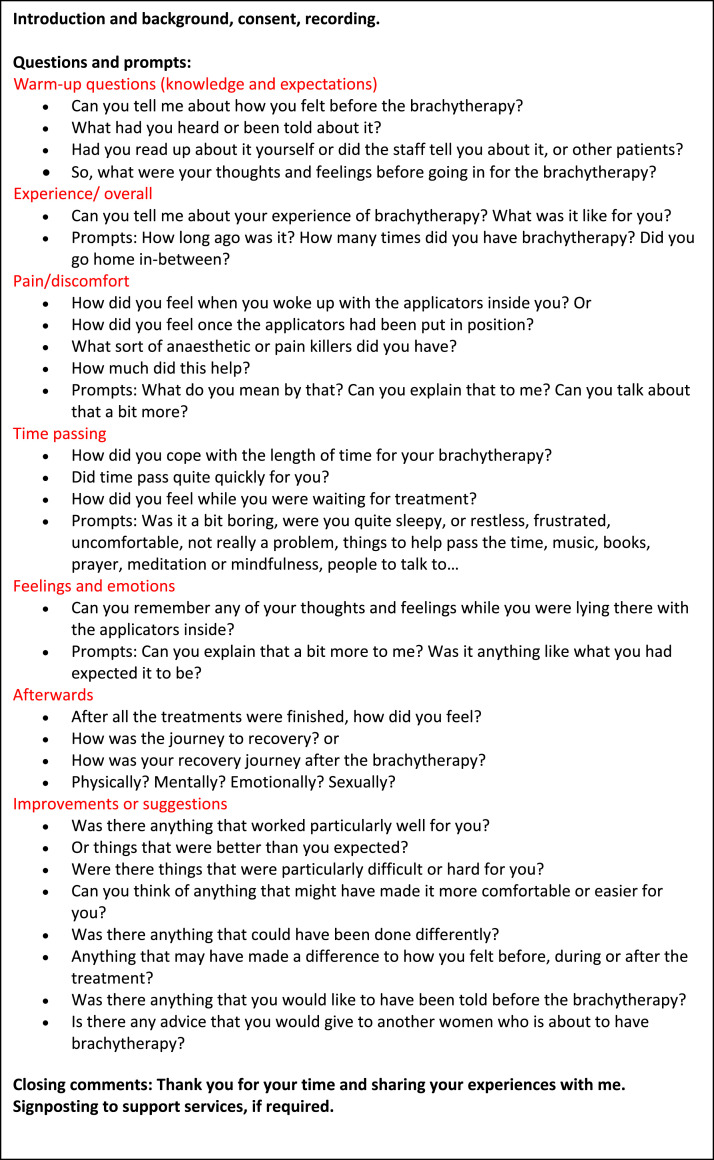
Interviews were conducted with 35 participants, 20 in cohort 1 and 15 in cohort 2, between September 2019 and April 2021. The study was paused for 4 months at the start of the COVID-19 pandemic. Interviews before COVID-19 were carried out face-to-face, then switched to remote interviews after additional ethics approval. The first 6 interviews took place in a variety of settings, including hospital clinic or research rooms, a patient's home, and a hired community center room. The remaining 29 interviews were carried out via telephone or videoconferencing. An interview schedule was used as a guide for the interviews (see Fig. 1).
Fig. 1.
Interview schedule.
Six participants were recruited from site 1, 9 from site 2, and 10 from sites 3 and 4. The age of participants ranged from 28 to 87 years (median, 65). Interview duration ranged from 22 to 78 minutes (median, 42). A pseudonym was allocated to each participant (see Table 1).
Table 1.
Recruitment and participant demographic data
| Pseudonym | Recruitment site | Cohort | Duration (minutes) | Interview format | Age |
|---|---|---|---|---|---|
| Diane | 2 | 1 | 41 | Face-to-face | 72 |
| Laura | 2 | 2 | 37 | Face-to-face | 31 |
| Amy | 3 | 1 | 78 | Face-to-face | 37 |
| Anita | 3 | 2 | 37 | Face-to-face | 66 |
| Caroline | 2 | 1 | 36 | Face-to-face | 66 |
| Dawn | 1 | 1 | 65 | Face-to-face | 61 |
| Gina | 4 | 2 | 36 | Telephone | 77 |
| Nicola | 2 | 1 | 34 | Videoconference | 69 |
| Rebecca | 1 | 1 | 38 | Videoconference | 47 |
| Anna | 2 | 2 | 37 | Videoconference | 37 |
| Ruth | 1 | 2 | 45 | Videoconference | 69 |
| Hazel | 4 | 2 | 53 | Videoconference | 43 |
| Dorothy | 1 | 1 | 38 | Telephone | 66 |
| Charlotte | 2 | 1 | 64 | Videoconference | 51 |
| Rita | 1 | 1 | 52 | Videoconference | 70 |
| Elsie | 1 | 1 | 22 | Videoconference | 72 |
| Annie | 3 | 1 | 56 | Videoconference | 41 |
| Bethany | 4 | 1 | 31 | Videoconference | 56 |
| Vicky | 3 | 2 | 58 | Videoconference | 28 |
| Monica | 3 | 2 | 38 | Videoconference | 87 |
| Eleanor | 3 | 2 | 48 | Videoconference | 85 |
| Marion | 3 | 1 | 67 | Telephone | 77 |
| Claire | 4 | 2 | 58 | Videoconference | 65 |
| Rosie | 3 | 2 | 60 | Videoconference | 32 |
| Joanna | 2 | 1 | 41 | Videoconference | 77 |
| Theresa | 2 | 2 | 45 | Videoconference | 75 |
| Linda | 2 | 2 | 42 | Telephone | 46 |
| Maureen | 4 | 2 | 39 | Videoconference | 76 |
| Molly | 4 | 1 | 39 | Videoconference | 30 |
| Bridget | 3 | 1 | 51 | Telephone | 57 |
| Juliet | 4 | 1 | 47 | Videoconference | 59 |
| Lucy | 4 | 1 | 43 | Videoconference | 42 |
| Justine | 4 | 2 | 34 | Videoconference | 58 |
| Lilian | 3 | 1 | 49 | Videoconference | 75 |
| Karen | 4 | 1 | 41 | Telephone | 68 |
Reflexive thematic analysis
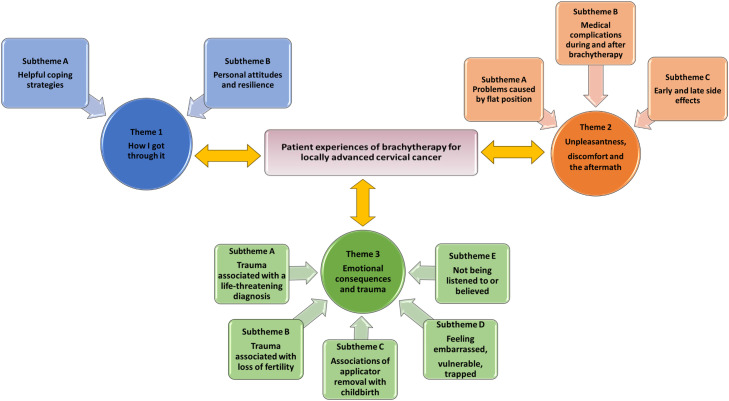
Across the data set, participants’ reports included difficult and traumatic experiences of brachytherapy with periods of severe pain and poor nursing care on the wards. However, some participants described more positive experiences, reporting what had gone well and examples of good care and support from dedicated staff. When analyzing the 2 data sets, it was found that themes developed from cohort 1 and 2 were indistinguishable, and therefore they were integrated and reported as a whole. A thematic map was developed with 3 overarching themes and 10 subthemes (Fig. 2). An analytical commentary was written to illustrate the analysis process, including the interpretation of interview data. For the purpose of the analysis, brachytherapy was categorized into short, medium, and long duration. For day case brachytherapy, most women lay flat for 4 to 5 hours with applicators in place, repeated 3 or 4 times over a 2- to 3-week period (referred to in this study as “short duration brachytherapy”). For inpatient brachytherapy, they lay flat for around 24 hours if 2 treatments were delivered (referred to as "medium duration") or over 48 hours if 4 treatments were delivered (referred to as "long duration"). Interpretation of the data included comparison in patterns of experiences between participants who had short, medium, or long duration brachytherapy.
Fig. 2.
Thematic map.
Theme 1: How I got through it
Many participants described the fears and worries they had before brachytherapy and reflected on ways that they had managed to get through it. Two subthemes were developed.
Subtheme A: Helpful coping strategies
Because of the requirement to lie flat for long periods of time, many participants had been advised to bring items into hospital, such as reading material, audio books, or music and headphones. Some said they had not been given advice on what to take, while others forgot or chose not to take any items. Some of the suggested items were difficult to use while lying flat; however, others found them manageable and useful. Some said they were unable to concentrate or were in too much pain to make use of any distractions.
“I think just being prepared and taking stuff, because the second time I had my book, I had music and time went a little bit quicker.” [Laura]
Amy found that large headphones helped her to listen to music and block out what was going on around her on the ward, especially when she found it upsetting to see very sick patients. Anita found listening to music and reading was helpful when in pain and unable to get to sleep. Some participants were able to watch television, but others had no access and 1 participant reported that it made her feel nauseous. Some reported being sleepy and groggy, helping time pass more quickly, while others reported that people watching or talking to other patients helped pass the time. However, some participants chose to withdraw or disengage as their way of coping.
Some participants at 1 recruitment site were able to experience relaxation and comfort through complementary therapies such as foot massage, reiki, or reflexology. Other helpful coping strategies included relaxation, prayer, and complementary therapies, thinking and making plans, and using humor when interacting with health care staff.
Subtheme B: Personal attitudes and resilience
Some participants explained how they set their mind to get through brachytherapy. They knew that this was an important part of the treatment for a life-threatening condition. Many described their determination to fight for life and a resolve to get through the final hurdle in their cancer pathway. Some described an attitude of acceptance or resignation about the short-term pain and discomfort, resolving to put up with the procedure as there was no way of making it any less unpleasant.
“It was very, very hard for me going back that second time. All the way on the train going to [name of radiation therapy department], I was thinking, ‘Why are you doing this? Why are you doing this?’ I'm doing it because I'm in a process, I want to get better, I'm not ready to die yet.” [Anita]
Some participants talked about their personal attitudes and life experiences, which helped give them the resilience to cope with a difficult procedure.
“Life throws everything at you, and you have to be resilient, otherwise, you'll go under. I've had cancer before, so, I got through that, so I think about being positive, but I've got it now, I'll get through it again.” [Lilian]
Theme 2: Unpleasantness, discomfort, and the aftermath
Many participants described the difficulties endured during and after brachytherapy. Unpleasantness and discomfort arose from insertion of applicators, duration of applicators being inside them, lying flat for a long time, removal of applicators, and side effects. Descriptions of the long and difficult recovery after brachytherapy was referred to as “the aftermath.” Three subthemes were developed.
Subtheme A: Problems caused by flat position
Overall, the negative effect of lying flat was more pronounced in reports from participants who had medium or long duration brachytherapy.
Some participants talked about the embarrassment of passing wind, particularly when in a general ward. Trapped wind sometimes caused severe pain and loss of appetite or nausea.
Backache was a common problem, with some reporting that opiates helped. Changing position was reportedly not allowed because of a risk of moving applicators, leading to pain or incorrect treatment. Pre-existing back problems led to additional anxieties regarding pain.
“…but it was the pain was really bad in my back, and the morphine didn't do anything for it, it really didn't. It's very difficult with your back, if you have pain in your back, honestly, I don't know anything that really kills the pain. I don't know whether it was because I was in the one position for so long that my back started to act up.” [Bridget]
Many had difficulties with eating, drinking, and swallowing tablets while lying flat. In some cases, visitors were asked to leave the ward during mealtimes, so potential helpers were unavailable. Some participants were not offered help with eating by ward staff, and food and drink were placed out of reach. Some were not given appropriate food choices or utensils to minimize spillages. Some were upset by loss of independence, having to ask for and accept help to eat and drink and for personal care. Theresa complained that her food and drink were always placed out of reach:
“The food was brought to me and it went away untouched, nobody noticed.” [Theresa]
Subtheme B: Medical complications during and after brachytherapy
Overall, the severity of medical complications was more evident in reports from participants who had medium and long duration brachytherapy. Complications such as development of venous thrombotic emboli, pressure sores, allergic reactions, and collapses during or after brachytherapy were only reported by participants who had medium or long duration brachytherapy.
“I think I had a bit of a drug reaction, because I was sick, I was nauseous and then I was sick, and I was incredibly sleepy that second day, after my last brachytherapy treatment I had to stay another night or 2 because of that, my reaction to the drug, which I think was a form of morphine.” [Marion]
Subtheme C: Early and late side effects
Many participants reported physical effects during or after brachytherapy, which may have been related to recent external beam radiation therapy and/or chemotherapy or due to anesthesia and analgesia given at brachytherapy.
Nausea and vomiting during brachytherapy were especially problematic because of the need to remain in a flat position. This increased anxiety levels because of fear of choking or not being able to reach a vomit bowl.
Participants described a range of pain experiences, including pelvic pain from the applicators, back pain, pain from the urinary catheter, and pain at a cannula site. Key timepoints when pain occurred or was exacerbated were identified, such as the interval between a spinal anesthetic wearing off and intravenous or oral analgesia taking effect; during transfers for imaging; and most commonly at applicator removal. Descriptions of pain varied from those who said they had no pain or manageable pain to those who described pain as unbearable or their worst pain ever. For example:
“But this was just constant, like something was squeezing my insides really tight and then punching me at the same time. No that's how it felt, like I was being punched from the inside and stretched and like fingernails clawing at my insides.” [Annie]
Many participants described pain at applicator removal.
“The first week when they took the applicator out, they didn't give me any pain relief whatsoever, so literally they ripped it out, with nothing (sighing), so like, like somebody was literally ripping my insides out, it was horrendous.” [Vicky]
Some participants compared applicator removal to medieval torture. Sometimes their experiences were not as bad as their preconceptions, but for others their reflection afterward was that it was like a torture chamber or similar to being “hung, drawn, and quartered.”
Many participants expressed dissatisfaction with the information given about potential side effects after brachytherapy and would have liked more information when being discharged from hospital. Reported side effects included bowel and bladder problems, fatigue, loss of appetite and weight loss, insufficiency fractures, lymphoedema, and vaginal stenosis, which caused difficulty with sex. However, some participants reported no complications or side effects during any or only during some of their brachytherapy procedures. Joanna was surprised that having lain flat for 2 and a half days for long duration brachytherapy, that she had no pain and was able to get up and walk out of the hospital very soon after applicator removal.
Overall, reports of some side effects were more strongly expressed by participants who had medium and long duration compared with short duration brachytherapy. For example, multiple episodes of nausea and vomiting, uncontrolled severe pain, and feelings of lethargy and drowsiness were reported exclusively by those having medium or long duration brachytherapy.
Theme 3: Emotional consequences and trauma
Participant brachytherapy narratives included reports of psychological and emotional challenges. Five subthemes were developed.
Subtheme A: Trauma associated with a life-threatening diagnosis
Many participants talked about brachytherapy in the context of the shock of having received a cancer diagnosis, living with uncertainties about their future life trajectory and survival. They talked of their fears that treatment might be unsuccessful or the cancer might recur. Some participants spoke of their fear of dying specifically in relation to worries about their young children. Some described being emotional or “tearful” during or after their brachytherapy, and the retelling of these events generated emotional points at interview, with tears and apologies for getting upset. Vicky reported symptoms of posttraumatic stress disorder, having flashbacks of when she was initially told she had cancer and panic attacks at follow-up appointments where she was convinced that she was going to be given bad news. Bethany recalled her thoughts on the day of her final treatment:
“You know, in my head I'm still thinking, well nothing's set in stone, nothing, you know, just because it's my last treatment, I might still have got it. There's nothing that's said I'm cured. They're all so nice and positive, but deep down in, inside my head I'm going out thinking what if, what if, what if?” [Bethany]
Subtheme B: Trauma associated with loss of fertility
The issue of loss of fertility was raised at interview by all participants under the age of 40 regardless of whether or not they had children. These participants expressed feelings of grief and loss for children they could not have and choices being taken away by cancer. Some talked about being upset by insensitive comments from health care staff about terminations or applicator removal being like childbirth or friends suggesting that after treatment “miracles can happen.”
“Things catch me unawares every now and again, like the news sort of thing [sounding upset at this point]. Yeah, maybe because I was like, at least you guys can have a chance.” [Amy]
Others described having to make difficult choices before treatment began, such as egg harvesting and surrogacy, potentially delaying treatment and reducing chances of cure.
Subtheme C: Associations of applicator removal with childbirth
The removal of brachytherapy applicators was likened by some to childbirth, as a way of describing a physical experience, but for some this analogy added to their trauma. The association of applicator removal with childbirth caused prolonged upset, including flashbacks and intrusive thoughts for some participants. Laura had not experienced childbirth herself but had been a birth partner for her friend, so had witnessed a delivery and use of gas and air:
“And when they removed the packing, it was a sensation of what I would imagine giving birth was like. Sorry, I‘m getting quite emotional, and that kind of like really traumatizing, more so than the pain [sounding very upset at this point]. I think it was because they were pulling all the packing out and it was like, that vacuum of you know, totally, with my friend when she was like giving birth.” [Laura]
Subtheme D: Feeling embarrassed, vulnerable, trapped
Participants described feeling vulnerable during their brachytherapy procedures, often associating the applicators inside an intimate part of their body with a sense of loss of privacy or dignity and embarrassment. Being unable to move because of the effect of spinal or epidural anesthesia, along with the fear of moving the applicator, which would cause pain or make the treatment inaccurate, left some women feeling vulnerable, alone, isolated, trapped, or helpless.
“Then you go down to the brachy area, pellet administration, and they start unscrewing you. But it's just weird, because you just can't move and you're so vulnerable aren't you.” [Juliet]
Subtheme E: Not being listened to/believed
Some participants were distressed by experiences of health care staff not understanding their pain. They felt they were not listened to, understood, or believed when they were in severe pain and asked for help. For example:
“I almost felt like they were trying to say ‘Oh stop being silly.’ I don't think my view of how much it was hurting was taken into account at all.” [Annie]
This experience further reduced Annie's trust in health care professionals after her experience of doctors ignoring her symptoms for many months before her cervix cancer diagnosis.
Discussion
This study has provided evidence of 35 women's experiences of brachytherapy across 4 UK treatment centers using modern brachytherapy techniques, including interstitial needles and MR image guided brachytherapy. Across the 4 recruitment sites, brachytherapy regimens included short duration (day case) regimens and medium and long duration (inpatient) regimens, including overnight stays with applicators in place for a longer time.
Findings demonstrate variability in participants’ experiences of brachytherapy, ranging from unproblematic to episodes of severe uncontrolled pain, significant psychological trauma, and an unexpected and prolonged physical aftermath. Similar variability was reported in an interview study of 32 women after low dose rate (LDR) brachytherapy, reporting that the variation in the incidence and severity of problems presented challenges for those providing care to meet their patients’ needs.22 Velji and Fitch23 found that the quality of the women's experiences of brachytherapy was dependant on the nursing care received, information before brachytherapy, and stresses related to context and environmental factors. With this variability in mind, it is worth considering whether those at greatest risk of poor experiences can be identified and potentially targeted for increased support before, during, and after brachytherapy.
The introduction of more complex brachytherapy techniques, with the addition of interstitial needles and planning using MR imaging, have been accompanied by the development of more advanced anesthesia and analgesia techniques.24 The use of interstitial needles has been reported to cause more pain compared with intracavitary applicators alone, possibly because of the more invasive nature of the procedure and the increased duration with applicators in place.10,11,24 In this study, all 4 recruitment sites had access to complex or hybrid techniques (intracavitary and interstitial applicators), and applicator type would be selected based on residual tumor size, following international guidelines.25,26 From interview data, it was not possible to distinguish which participants had intracavitary, interstitial, or hybrid applicators, as most participants did not know which type of applicator was used. Reports of anesthesia and analgesia were unclear. It may be seen as a limitation of this study that differences in the experiences of women may have been related to the type of applicators used or anesthesia and analgesia techniques, and this was not discernible from interview data. Future work could explore optimal anesthesia and analgesia along with specific applicator types and duration of applicators in place with additional medical information provided by recruitment sites.
In this study it was reported that “total pain” was a term used by a participant's oncologist to explain why her pain was so difficult to manage. The concept of total pain, first introduced by Dame Cicely Saunders, founder of the modern hospice movement and discipline of palliative care, suggests that distress (including pain) may have emotional, social, and spiritual dimensions, not just the physical.27,28 The International Association for the Study of Pain advises that29:
“Pain is always a subjective experience that is influenced to varying degrees by biologic, psychological, and social factors…Through their life experiences, individuals learn the concept of pain and its applications…A person's report of an experience as pain should be accepted as such and respected…Although pain usually serves an adaptive role, it may have adverse effects on function and social and psychological well-being.”
Some of these nuances and complexities of pain were demonstrated in the participants’ narratives, such as explanations of how participants coped with pain during brachytherapy in the context of a cancer diagnosis, their previous health experiences, and the distress caused by their pain not being understood or believed by their health care providers. Additional training may be needed so that health care professionals can provide appropriate pain management with consideration for the emotional, social, and spiritual as well as physical aspects.
Previous studies have shown examples of inconsistent and fragmented care.22,23,30 In this study, many interview participants spoke of the excellent treatment and care that they had received and expressed their gratitude for having been given a curative treatment. However, some participants gave examples of poor nursing care or a lack of consistency in care, especially those who had experienced overnight stays with applicators in place. Exploration of the effect of treatment scheduling on patient experiences has shown that in terms of medical complications and side effects during brachytherapy, a longer duration of brachytherapy appears to negatively affect experiences. This was likely related to the need for more nursing and medical interventions over the longer time with applicators in place, with more opportunities for interventions to be inconsistent or suboptimal. Previous studies have not reported patient experiences for different scheduling regimens; therefore, these findings provide novel insights relating to the effect of the duration of brachytherapy. These findings indicate that there is scope to improve experiences through development and implementation of standardized minimum care protocols. For example, ward staff making sure that food and drink are placed in reach in suitable receptacles and offering help to patients.
Previous studies reported mixed experiences of care, with some finding the nurses and doctors to be caring and comforting and others finding them to have an uncaring attitude or lack of understanding about the “ordeal” of brachytherapy.23,31 This study also included some dissatisfaction with attitudes of health care professionals. It is not known whether the participants’ negative experiences were related to insufficient allocation or under-prioritization of staff resources to meet the needs of brachytherapy patients or deployment of bank or agency staff with less experience in caring for brachytherapy patients. Additional health care professional training in care and compassion to support patients and an understanding of the difficult nature of the treatment may be warranted to try to improve consistency of care. Further research could be carried out to explore current barriers to good or consistent patient care from a staff perspective.
The study design included exploring patients’ experiences soon after or at 1 year after brachytherapy to consider the effect of time on their views of treatment and recalled experiences. Comparing narratives and theme development, there was no distinguishable difference between the 2 cohorts, with some experiences discussed in greater detail and depth than others. Current literature reports interviews immediately or soon after brachytherapy. Reporting experiences a year after brachytherapy has given new insights to the long-lasting impact of brachytherapy experiences.
This study has shown that distress caused by brachytherapy is due to complex interrelations between pain, anxiety, and the wider context of the cancer diagnosis and treatment pathway. Some participants described what had worked well for them with examples of great care and support. Some reported no pain or very little discomfort, few or manageable side effects, and good information and support before, during, and after brachytherapy. Many participants suggested ideas to improve care for future brachytherapy patients. Their suggestions involved complex issues such as the need for better and more consistent pain management, more psychological support while lying flat, and better training of staff to understand the effect of brachytherapy and be able to deliver compassionate care. More simple suggestions included providing better support for nutrition such as making sure food and drinks were within reach and in suitable receptacles. From these data, future work is planned for the development of patient care recommendations, to advocate for the delivery of consistent and standardized minimum care. Patient care recommendations could include a wide range of approaches, such as regular audits of pain and discomfort; development of specific anesthesia and analgesia protocols to cover the key timepoints where pain may be increased; and personal care, nutritional support, and additional training for health care professionals.
Limitations of the study included exclusion of non-English speaking participants. While this may have provided data from a broader demographic, there would have been risks of inaccuracy involved with real-time translation during interview and translation post interview. Another possible limitation was the exclusion of patients with progressive disease because of potential harm and distress to this cohort with no anticipated benefits.
Conclusion
Hearing the patient voice through exploration and examination of interview participants’ experiences across 4 recruitment sites using modern brachytherapy techniques and different regimens, with 2 different time frames after brachytherapy has led to a large data set, demonstrating a wide range of experiences. This substantial body of data has contributed to a better understanding of patient experiences of brachytherapy in these settings. Overall, patient experiences were reported to have been more problematic for those who had medium or long duration brachytherapy. Study insights will be used to inform future work to develop clinical care recommendations.
Footnotes
Disclosures: P.H., clinical doctoral research fellow (ICA-CDRF-2017-03-079) was funded by Health Education England (HEE)/National Institute for Health and Care Research (NIHR) for this research project. The views expressed in this publication are those of the authors and not necessarily those of the NIHR, UWE Bristol, NHS, or the UK Department of Health and Social Care.
Data Sharing Statement: Research data are not available.
Acknowledgments—The first author would like to thank the PhD supervisory team and patient research partners for their help and support during the clinical research doctoral fellowship. A special thanks to the health care professionals at the 4 recruitment sites and the interview participants who were so generous in sharing their brachytherapy stories and their time.
References
- 1.Sturdza A, Pötter R, Ulrik L, et al. Image guided brachytherapy in locally advanced cervical cancer: Improved pelvic control and survival in RetroEMBRACE, a multicenter cohort study. Radiother Oncol. 2016;120:428–433. doi: 10.1016/j.radonc.2016.03.011. [DOI] [PubMed] [Google Scholar]
- 2.Lindegaard JC, Fokdal LU, Nielsen SK, et al. MRI-guided adaptive radiotherapy in locally advanced cervical cancer from a Nordic perspective. Acta Oncol. 2013;52:1510–1519. doi: 10.3109/0284186X.2013.818253. [DOI] [PubMed] [Google Scholar]
- 3.Viswanathan AN, Thomadsen B. American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part I: General principles. Brachytherapy. 2012;11:33–46. doi: 10.1016/j.brachy.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 4.Viswanathan AN, Beriwal S, De Los, Santos JF, et al. American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part II: High-dose-rate brachytherapy. Brachytherapy. 2012;11:47–52. doi: 10.1016/j.brachy.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pötter R, Haie-Meder C, Van Limbergen E, et al. Recommendations from gynaecological (GYN) GEC ESTRO working group (II): Concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy - 3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. Radiother Oncol. 2006;78:67–77. doi: 10.1016/j.radonc.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 6.Pötter R, Dimopoulos J, Georg P, et al. Clinical impact of MRI assisted dose volume adaptation and dose escalation in brachytherapy of locally advanced cervix cancer. Radiother Oncol. 2007;83:148–155. doi: 10.1016/j.radonc.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 7.Pötter R, Georg P, Dimopoulos JCA, et al. Clinical outcome of protocol based image (MRI) guided adaptive brachytherapy combined with 3D conformal radiotherapy with or without chemotherapy in patients with locally advanced cervical cancer. Radiother Oncol. 2011;100:116–123. doi: 10.1016/j.radonc.2011.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haie-Meder C, Pötter R, Van Limbergen E, et al. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (I): Concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother Oncol. 2005;74:235–245. doi: 10.1016/j.radonc.2004.12.015. [DOI] [PubMed] [Google Scholar]
- 9.Humphrey P, Dures E, Hoskin P, Cramp F. Brachytherapy for locally advanced cervical cancer : A survey of UK provision of care and support. Radiother Oncol. 2021;159:60–66. doi: 10.1016/j.radonc.2021.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Janaki M, Nirmala S, Kadam A, Ramesh B, Sunitha K. Epidural analgesia during brachytherapy for cervical cancer patients. J Cancer Res Ther. 2008;4:60–63. doi: 10.4103/0973-1482.40825. [DOI] [PubMed] [Google Scholar]
- 11.Amsbaugh AK, Amsbaugh MJ, El-Ghamry MN, Derhake BM. Optimal epidural analgesia for patients diagnosed as having gynecologic cancer undergoing interstitial brachytherapy. J Clin Anesth. 2016;35:509–515. doi: 10.1016/j.jclinane.2016.08.025. [DOI] [PubMed] [Google Scholar]
- 12.Brown M. Patient-controlled analgesia following cervical brachytherapy: A 12-month Trust review. Anaesthesia. 2018;73(Supplement 4):33. [Google Scholar]
- 13.Wiebe E, Surry K, Derrah L, et al. Pain and symptom assessment during multiple fractions of gynecologic high-dose-rate brachytherapy. Brachytherapy. 2011;10:352–356. doi: 10.1016/j.brachy.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 14.Humphrey P, Bennett C, Cramp F. The experiences of women receiving brachytherapy for cervical cancer: a systematic literature review. Radiography. 2018;24:396–403. doi: 10.1016/j.radi.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 15.Kirchheiner K, Czajka-Pepl A, Ponocny-Seliger E, et al. Posttraumatic stress disorder after high-dose-rate brachytherapy for cervical cancer with 2 fractions in 1 application under spinal/epidural anesthesia: Incidence and risk factors. Int J Radiat Oncol Biol Phys. 2014;89:260–267. doi: 10.1016/j.ijrobp.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 16.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. [Google Scholar]
- 17.Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: Guided by information power. Qual Health Res. 2016;26:1753–1760. doi: 10.1177/1049732315617444. [DOI] [PubMed] [Google Scholar]
- 18.Braun V, Clarke V. SAGE Publications Ltd; 2022. Thematic Analysis: A Practical Guide. In: Maher A, ed. [Google Scholar]
- 19.Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Heal. 2019;11:589–597. [Google Scholar]
- 20.Braun V, Clarke V, Hayfield N. ‘A starting point for your journey, not a map’: Nikki Hayfield in conversation with Virginia Braun and Victoria Clarke about thematic analysis. Qual Res Psychol. 2022;19:424–445. [Google Scholar]
- 21.Braun V, Clarke V. Sage; 2013. Successful Qualitative Research a Practical Guide for Beginners. In Carmichael M, ed. [Google Scholar]
- 22.Warnock C. Patients’ experiences of intracavity brachytherapy treatment for gynaecological cancer. Eur J Oncol Nurs. 2005;9:44–55. doi: 10.1016/j.ejon.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 23.Velji K, Fitch M. The experience of women receiving brachytherapy for gynecologic cancer. Oncol Nurs Forum. 2001;28:743–751. [PubMed] [Google Scholar]
- 24.Petitt M, Ackermann RS, Hanna MM, et al. Anesthetic and analgesic methods for gynecologic brachytherapy: A meta-analysis and systematic review. Brachytherapy. 2020;19:328–336. doi: 10.1016/j.brachy.2020.01.006. [DOI] [PubMed] [Google Scholar]
- 25.Fokdal L, Tanderup K, Hokland SB, et al. Clinical feasibility of combined intracavitary /interstitial brachytherapy in locally advanced cervical cancer employing MRI with a tandem / ring applicator in situ and virtual preplanning of the interstitial component. Radiother Oncol. 2013;107:63–68. doi: 10.1016/j.radonc.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 26.Pötter R, Tanderup K, Kirisits C, et al. The EMBRACE II study: The outcome and prospect of two decades of evolution within the GEC-ESTRO GYN working group and the EMBRACE studies. Clin Transl Radiat Oncol. 2018;9:48–60. doi: 10.1016/j.ctro.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saunders C. The evolution of palliative care. Patient Educ Couns. 2000;41:7–13. doi: 10.1016/s0738-3991(00)00110-5. [DOI] [PubMed] [Google Scholar]
- 28.Mehta A, Chan LS. Understanding of the concept of ‘“ total pain ”’ a prerequisite for pain control. J Hosp Palliat Nurs. 2008;10:26–32. [Google Scholar]
- 29.Raja SN, Carr DB, Cohen M, et al. The revised ISAP definition of pain: Concepts, challenges, and compromises. Pain. 2020;161:1976–1982. doi: 10.1097/j.pain.0000000000001939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Duncan P, Mason TM, Thirlwell S. Radiation via intracavitary-interstitial pelvic implants for gynecological cancers: Clinical nurse specialists affecting change. Clin Nurse Spec. 2015;29:290–294. doi: 10.1097/NUR.0000000000000151. [DOI] [PubMed] [Google Scholar]
- 31.Dzaka A, Maree J. Experiences of women receiving high dose rate brachytherapy for cervical cancer at an academic hospital. South African J Gynaecol Oncol. 2016;8:42–45. [Google Scholar]